Abstract
There are serious concerns with rising antimicrobial resistance (AMR) across countries increasing morbidity, mortality and costs. These concerns have resulted in a plethora of initiatives globally and nationally including national action plans (NAPs) to reduce AMR. Africa is no exception, especially with the highest rates of AMR globally. Key activities in NAPs include gaining a greater understanding of current antimicrobial utilization patterns through point prevalence surveys (PPS) and subsequently instigating antimicrobial stewardship programs (ASPs). Consequently, there is a need to comprehensively document current utilization patterns among hospitals across Africa coupled with ASP studies. In total, 33 PPS studies ranging from single up to 18 hospitals were documented from a narrative review with typically over 50% of in-patients prescribed antimicrobials, up to 97.6% in Nigeria. The penicillins, ceftriaxone and metronidazole, were the most prescribed antibiotics. Appreciable extended prescribing of antibiotics up to 6 days or more post-operatively was seen across Africa to prevent surgical site infections. At least 19 ASPs have been instigated across Africa in recent years to improve future prescribing utilizing a range of prescribing indicators. The various findings resulted in a range of suggested activities that key stakeholders, including governments and healthcare professionals, should undertake in the short, medium and long term to improve future antimicrobial prescribing and reduce AMR across Africa.
Keywords: Africa, antimicrobials, antimicrobial stewardship programs, antimicrobial resistance, national action plans, quality indicators, strategies, surgical site infections, utilization patterns
1. Introduction
There are serious concerns globally with growing antimicrobial resistance (AMR), with an associated increase in morbidity, mortality and costs [1,2,3,4]. A recent study estimated that in 2019 alone there were 1.27 million deaths globally attributable to bacterial AMR and 4.95 million deaths associated with bacterial AMR, with the greatest burden in Western sub-Saharan Africa [2]. The high rates of AMR among African countries may reflect the fact that the greatest burden of all infectious diseases worldwide, including human immunodeficiency virus (HIV) and acquired immunodeficiency syndrome (AIDS), acute respiratory diseases, malaria and tuberculosis (TB), is currently in Africa [5,6,7,8,9], with associated prescribing of antimicrobials. This includes prophylaxis against opportunistic infections for patients with HIV/AIDS in view of their impact on morbidity and mortality [10]. Alongside this, high rates of inappropriate prescribing and dispensing of antibiotics across all sectors in Africa, including for viral infections such as acute respiratory tract infections, are exacerbated by appreciable purchasing of antibiotics without a prescription [9,11,12,13,14,15,16,17,18,19,20]. Self-purchasing of antibiotics is common across sub-Saharan Africa, enhanced by high patient co-payments, a lack of access to certain antibiotics coupled with the convenience of community drug stores and pharmacies as well as concerns with the public healthcare system alongside porous supply chains for medicines [11,12,21,22,23,24,25,26,27]. Having said this, Klein et al. (2019) in their recent study showed that whilst low- and middle-income countries (LMICs) had the highest rates of AMR, there was a less clear-cut link between consumption and resistance rates compared with high-income countries [28]. However, this study only involved South Africa among the African countries in its analysis, with currently very limited self-purchasing of antibiotics in South Africa with strict regulations [28,29]. There is also appreciable consumption of antibiotics in agricultural and farming sectors across Africa, often with antibiotics of concern, adding selection pressure for AMR [30,31,32,33]. This is leading to increasing calls for a One Health approach across Africa, coupled with measures to prohibit the self-purchasing of antibiotics to reduce future AMR [34,35,36,37].
The costs associated with AMR are also considerable and will continue to rise unless addressed [38]. The World Bank (2017) recently estimated that even in a low-AMR scenario, the loss of world output due to AMR could exceed USD 1 trillion annually after 2030 [39]. This could potentially increase up to USD 3.4 trillion annually, equivalent to 3.8% of annual global Gross Domestic Product [39]. As a result, increasing AMR could be devastating, becoming the next pandemic unless considerable activities are undertaken to improve the future use of antibiotics [40].
Concerns with increasing morbidity, mortality and costs associated with AMR have resulted in a plethora of international, regional, national, and local activities and strategies to try and address the situation [41]. International activities include those among the Interagency Coordination Group on Antimicrobial Resistance (ICGAR) Global Leaders group, ongoing activities within the Organisation for Economic Co-operation and Development (OECD), the Fleming Fund, and the World Bank alongside activities by the World Health Organization (WHO) including the One Health Approach and the development of Global Action Plans (GAP) to tackle AMR [36,37,42,43,44,45,46,47,48]. Regional initiatives within Africa include activities by the Africa CDC, the African Society for Laboratory Medicine (ASLM), the Southern Africa Centre for Infectious Disease Surveillance, other Civil Society Organisations in Africa as well as the development of African guidelines to treat common bacterial infections across age groups [49,50,51,52,53,54].
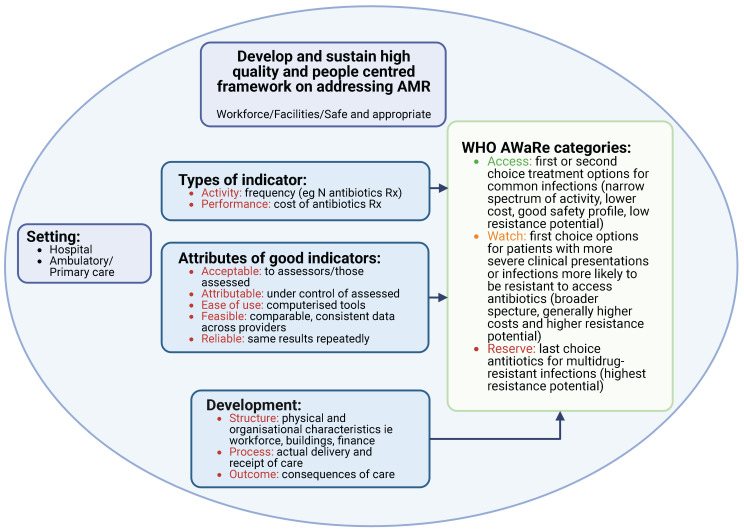
Alongside this, the WHO has reclassified antibiotics into the AWaRe list (‘Access’, ‘Watch’ and ‘Reserve’) taking into account the impact of different antibiotics and classes on resistance potential to reduce future AMR [55,56]. The ‘Access’ group are considered as first- or second-line antibiotics for up to 26 common or severe clinical syndromes, typically with a narrow spectrum and low resistance potential. The ‘Watch’ group have a higher resistance potential and side-effects, with the ‘Reserve’ group only recommended as last resort antibiotics and prioritized for Antimicrobial Stewardship Programs (ASPs) using agreed quality indicators (QIs) (Figure 1) [55,56,57,58,59]. Assessing antimicrobial prescribing against current guidance, and monitoring their use based on the WHO AWaRe list, is increasingly being undertaken across Africa and beyond to improve prescribing given the extent of current prescribing of ‘Watch’ and ‘Reserve’ antibiotics in Africa [13,15,58,59,60,61,62,63,64,65,66,67].
The WHO GAP resulted in the development of National Action Plans (NAPs) across countries to combat rising levels of AMR [68,69]. Africa is no exception; currently, African countries are at different stages of implementation and monitoring of their NAPs [70,71,72,73,74]. A key activity within the NAPs is understanding current antimicrobial utilization and resistance patterns. Some African countries have high antimicrobial utilization rates within hospitals, with published studies across Africa reporting prevalence rates between 52.0% and 88.2% of in-patients [13,14,15,16,19,63,75,76,77,78,79,80,81,82]. There has also been considerable disquiet with high rates of extended antibiotic prophylaxis to prevent surgical site infections (SSIs) across Africa [83]. This is a concern as such practices may increase adverse reactions, AMR and costs with limited or no evidence on further reducing SSIs [83]. We are already seeing high rates of AMR among patients undergoing surgery who develop SSIs among patients in African hospitals, and this urgently needs to be reversed [84].
The use of antibiotics in patients with COVID-19 in hospitals has increased exponentially since the start of the pandemic. This is despite only a limited number of patients actually being diagnosed with bacterial or fungal infections reflecting current challenges with routine culture and sensitivity testing across Africa [14,76,85,86,87,88,89]. This misuse of antibiotics has been exacerbated by national guidelines in Africa which advocated the prescribing of a number of antibiotics in patients with COVID-19 [90]. The authors were concerned with this worrisome development with only a limited number of patients likely to have a bacterial co-infection [90], with others documenting similar concerns [88,91,92,93]. This mirrors similar activities regarding the purchasing of antibiotics in patients with COVID-19 without a prescription [94,95], and both situations urgently need to be addressed to avoid further pressures to increase AMR [88,96,97,98]. Alongside this, whilst the use of antibiotics has changed during the COVID-19 epidemic, and even during different waves of the epidemic over time in the same country [99], which needs addressing, there remains a lack of availability and access to a number of antibiotics in many LMICs [100,101]. While ‘Access’ antibiotics are placed in this group due in part to their availability in hard-to-reach areas, the availability of/access to other groups of antibiotics including ‘Watch’ and ‘Reserve’ antibiotics for use in hospitals, together with newly developed antibiotics, which may be necessary to use in areas of high resistance where antibiotic stewardship systems are available, is sorely missing and desperately needed [102]. We will be pressing for this in the future along with measures to increase COVID-19 vaccine equity. African Governments and others need to ensure that healthcare professionals (HCPs) can readily administer COVID-19 vaccines to reduce future hospitalisations [103,104]. Increasing vaccinations will reduce infection rates and subsequent consequences including hospitalisations, thereby reducing unnecessary prescribing of antimicrobials and associated AMR [96,97,98,105,106]. However, this requires comprehensive programs across Africa to address current high vaccine hesitancy [107,108,109].
A key activity to reduce AMR is the instigation of pertinent ASPs containing quality indicators [110,111]. Current indicators include adherence to prescribing guidance, which is increasingly being used to improve future antimicrobial prescribing across Africa and beyond given concerns with adherence to guidelines in practice along with rising AMR rates [112,113,114,115,116,117,118,119,120,121].
The role of quality indicators, whether as part of ASPs or separately, is also growing across countries, including African countries, to improve antibiotic prescribing in hospitals, including those based on the AWaRe classification [58,60,64,112,122,123]. This is because one way of measuring, monitoring and improving the quality of care is to use indicators, which are standardized measures of healthcare quality that make use of readily available, easy-to-use data independent of subjective judgement.
There are three main types of indicators used in healthcare (Figure 1) and there must be a clear a priori purpose for both developing, collecting and using indicator data across Africa.
Figure 1.
Key principles for indicator development for antimicrobials across Africa (adapted from [56,124,125,126,127]). NB: Created via Biorender (https://biorender.com/) with permission granted to Catrin Moore (accessed on 14 November 2022)).
However, there can be concerns instigating ASPs, with issues of resources, manpower, and knowledge among key stakeholders especially among low- and middle-income countries (LMICs) including African countries (Box S1—Supplementary Material) [128,129,130,131]. This though is also starting to change among African countries as well as among other LMICs [111,132,133,134,135,136,137]. We are likely to see more ASPs being instigated across Africa and beyond as part of NAPs to reduce AMR, enhanced by the availability of toolkits from the WHO and others [67,70,132,137,138,139,140].
Consequently, this study aims to comprehensively document current antimicrobial utilization patterns in hospitals right across Africa from published point-prevalence surveys (PPS) with no discrimination based on geography and income status. Here we also concentrate on the extent of inappropriate prescribing of antibiotics post-operatively to prevent SSIs. It is important that antibiotic prophylaxis is administered for the appropriate duration to prevent SSIs as they are responsible for an appreciable number of hospital-acquired infections, impacting on morbidity, mortality and costs [141,142,143,144,145]. However, as mentioned, extended prophylaxis increases AMR and adverse reactions with limited or no impact on further reducing SSIs [83,141,146].
Alongside this, we will document potential prescribing and quality indicators that can be used across hospitals in Africa to improve future antibiotic prescribing based on published studies. In addition, document examples of successful ASPs that have been instigated across Africa to provide future guidance. We started with hospitals as more information is currently available regarding the prescribing of antibiotics in hospitals versus ambulatory care across Africa [70]. We will not discuss potential programs to address COVID-19 vaccine hesitancy across Africa as this has already been discussed [107,109]. Similarly, programs to reduce inappropriate use of antibiotics in agriculture and farming, with the emphasis on hospital in-patient prescribing. However, both are important under a One Health approach.
2. Results
The key issues we identified to improve future antimicrobial prescribing in hospitals across Africa are described below. These include current high utilization rates among a number of African countries where studies have been undertaken; post-operative prescribing for more than one day to prevent SSIs as well as concerns with the lack of adherence to guidelines and high empiric use of antibiotics. Several potential prescribing and quality indicators have been identified to improve future antimicrobial prescribing as part of ASPs. These are being utilized among a growing number of successful ASPs across Africa to improve future prescribing. Our results can provide exemplars going forward.
2.1. Current Antimicrobial Utilization Patterns in Hospitals across Africa
Table S1 in the Supplementary Material documents current antimicrobial utilization patterns from 33 PPS studies that have recently been undertaken across Africa to a baseline for future ASPs. The documented studies include surveys from a single hospital within a country, with up to 18 hospitals in a country. However, Table S1 excludes the 12 African hospitals who were part of the Global PPS of Versporten et al. (2018) [112]. In addition, the 44 hospitals from sub-Saharan Africa that were part the updated Global PPS analysis, which includes the extent of Access, Watch and Reserve antibiotics prescribed [60]. These studies were excluded due to insufficient data for completion of Table S1 in the two publications [60,112]; the summary results though have been included. As seen, multiple PPS studies have been undertaken in low- and low-middle-income African countries despite concerns with available resources and personnel.
Antimicrobial utilization was typically high across most of the studied African countries (over 50% of patients), with similar rates in a recent study in Zambia [147]. Hospitals in Nigeria saw the highest antimicrobial utilization rates at 59.6–97.6% of in-patients surveyed Table 1. The lowest antimicrobial utilization rates were seen in South Africa (33.6–49.7% of patients). Incidentally, a similar range was seen among the 12 African hospitals taking part in the Global PPS of Versporten et al. (2018) [112].
There have also been studies assessing antimicrobial use among selected wards in hospitals in Uganda, with similar high utilization rates (79%) as seen among hospitals in Nigeria (Table S1) [148].
The penicillin group (which are typically in the AWaRe ‘Access’ group) and the cephalosporins (typically third-generation cephalosporins, in the AWaRe ‘Watch’ category) were the most prescribed antibiotics among the African countries reporting their PPS results, followed by metronidazole. There was also high use of metronidazole (23.6%) and ceftriaxone (23.2%) and cefuroxime (8.3%) among the 44 hospitals from sub-Saharan Africa taking part in the Global PPS study of Pauwels et al. (2021) [60].
2.2. Antibiotic Prophylaxis to Prevent Surgical Site Infections
Table 1 documents the extent of extended antimicrobial prophylaxis within hospitals among African countries documenting their findings to prevent SSIs alongside details of the antimicrobials prescribed where documented. Antimicrobials prescribed for SAP were mainly third-generation cephalosporins including ceftriaxone (‘Watch’ antibiotic), metronidazole (‘Access’ antibiotic) and the penicillins including co-amoxiclav (typically ‘Access’ antibiotics). This is similar to the findings of Pauwels et al. (2021) who found that the most common antibiotics prescribed for SAP were ceftriaxone and metronidazole [60].
Published reasons for extended prophylaxis included resistance to change among HCPs, overcrowding in hospitals, concerns with hospital cleanliness, proper aseptic techniques not being followed during the operation, poor knowledge regarding antibiotics among physicians, concerns with malnutrition in some patients and patient expectations [114,149,150,151,152]. There can also be concerns with repeated door openings during surgery impacting on the potential development of SSIs [153].
Programs, including consistent and comparable ASPs, are urgently needed across Africa to reduce the extent of prolonged prescribing to reduce adverse reactions, AMR and costs [83]. Details of some of the interventions that have been successfully introduced across Africa to improve the prescribing of antibiotics to prevent SSIs, building on possible prescribing/quality indicators Table 2, are summarized in Table 3.
Table 1.
Extent of prolonged antimicrobial prophylaxis to prevent SSIs across sub-Saharan Africa.
| Country | Year (and Reference) | Findings |
|---|---|---|
| Low Income * | ||
| Burkina Faso | 2019 [154] |
|
| Ethiopia | 2018 [155] |
|
| 2018 [156] |
|
|
| 2022 [157] |
|
|
| Rwanda | 2019 [158] |
|
| Tanzania | 2020 [159] |
|
| 2020 [160] |
|
|
| 2021 [81] |
|
|
| Uganda | 2020 [161] |
|
| 2021 [81] |
|
|
| 2022 [13] |
|
|
| Low-Middle Income * | ||
| Congo | 2020 [162] |
|
| Ghana | 2019 [163] |
|
| 2020 [76] |
|
|
| 2021 [81] |
|
|
| 2021 [164] |
|
|
| 2022 [141] |
|
|
| Kenya | 2017 [165] |
|
| 2018 [78] |
|
|
| 2018 [166] |
|
|
| 2019 [79] |
|
|
| Nigeria | 2016 [167] |
|
| 2017 [168] |
|
|
| 2020 [82,169] |
|
|
| 2020 [114] |
|
|
| 2021 [16] |
|
|
| 2022 [14] |
|
|
| Zambia | 2021 [81] |
|
| Upper-Middle Income * | ||
| Botswana | 2018 [170] |
|
| 2019 [19] |
|
|
| South Africa | 2021 [171] |
|
| 2022 [61] |
|
|
A and W: Access and Watch (AWaRe classification); SAP: Surgical Antibiotic Prophylaxis; SSIs: Surgical Site Infections; * World Bank Status (Based on [59]).
2.3. Prescribing Indicators Currently Being Used in Hospitals to Improve Antimicrobial Prescribing
A variety of prescribing indicators have been used among hospitals across Africa to enhance future prescribing as described in Table 2. These reflect increasing activities among hospitals across Africa to improve the future prescribing of antimicrobials in their countries thereby helping to reduce AMR.
However, a major concern across Africa is the current lack of electronic healthcare systems in hospitals to routinely track standards of care using consistent and comparable coding across countries. As a result, periodic surveys are typically undertaken to monitor care. This is likely to change as more applications and other electronic tools become available across Africa to track prescribing, building on current initiatives [61,62,172].
Table 2.
Indicators that have been used among in-patients in hospitals across Africa to assess the prescribing of antibiotics.
| Indicator | References |
|---|---|
| Activity/Performance Indicators | |
| % of in-patients prescribed antibiotics in a single PPS/ over specific time periods, e.g., successive waves of COVID-19 | [19,61,112,172] |
| % of antibiotics prescribed by defined daily doses (DDDs), e.g., DDDs/1000 patient-days in a PPS or over a specified time | [171,173,174,175] |
| % of a course of antibiotics prescribed (duration) in accordance with agreed guidance/ Days of antibiotic therapy per 1000 patient-days | [166,176] |
| % of antibiotics administered to in-patients within the first hour of prescribing within a designated period of time | [177] |
| % of patients where the indication for prescribing and/ or stop and review dates are included in patients’ notes | [15,19,76,81,114,168,169,178,179] |
| % oral vs. IV antibiotics (including as part of de-escalation policies) | [15,76,82,114,166,168,171,178,179,180,181] |
| % of missed doses documented in patients’ notes, e.g., as part of a PPS | [19,148] |
| % of antibiotics prescribed by their international non-proprietary name, e.g., as part of a PPS | [182,183] |
| % compliance to agreed process measures surrounding AMS | [184] |
| % of patients prescribed antibiotics within the country’s essential medicine list over an agreed period of time | [61,171,180,182,183] |
| Process quality indicators | |
| % of in-patients prescribed antibiotics in adherence to agreed guidelines within a specified time period/part of a PPS | [81,112,134,168,184,185,186,187,188,189,190,191] |
| % of patients prescribed a course of antibiotics in accordance with guideline duration recommendations within a specified time period/ part of a PPS | [166,176] |
| % of patients where cultures are taken and sent for analysis to guide antibiotic prescribing/ targeted therapy within a specified time period/ part of a PPS | [76,114,169,192] |
| % of antibiotics prescribed based on the AWaRe classification/% reduction in the prescribing of target antibiotics, e.g., ‘Watch’ cephalosporins to potential ‘Access’ antibiotics (current target is 60% of current prescribing should be ‘Access’ antibiotics) | [60,76,81,193] |
| % of patients prescribed antibiotics post-operatively to prevent SSIs/% appropriate use of antibiotics to prevent SSIs during an agreed time period | [194,195] |
| % of key antibiotics available for prescribing/ Whether there are agreed therapeutic interchange policies in the hospital when there are likely to be shortages of standard antibiotics for the condition (over a specific time period) | [183,196] |
| % of all admitted patients with pneumonia to the hospital correctly classified and treated to agreed guidelines (over a specified time period) | [187,190] |
| Outcome Indicators | |
| % SSIs following operations (over an agreed time period) | [160,194,197] |
| % Mortality rates (post-intervention versus pre-intervention) following changes in antimicrobial prescribing, e.g., reducing extensive antimicrobial prescribing post-surgery for SAP or reducing extensive prescribing of ‘Watch’ antibiotics | [175,176,193] |
AMS: Antimicrobial Stewardship; DDDs: Defined Daily Doses; SAP: Surgical Antibiotic prophylaxis; SSIs: surgical site infections.
2.4. Antimicrobial Stewardship Programs
At least 20 ASPs have been successfully instigated across Africa in recent years (between 2013 and 2022) to improve antimicrobial prescribing, with checklists and guidance now being developed for sub-Saharan Africa and beyond to help with their development and implementation [135,139,198]. Box 1 contains key areas for hospitals to concentrate on when seeking to introduce sustainable programs to improve future antimicrobial use in hospitals.
Box 1. Selected Antimicrobial Stewardship Checklist (adapted from [135]).
Has your hospital management formally identified AMS as a priority objective and included it as a key performance indicator?
Does your hospital have a formalized structure and group responsible for AMS activities including researching and promoting appropriate antibiotic use as part of agreed ASPs?
Is this currently a multidisciplinary AMS group available in your hospital to implement agreed ASPs, and does this group include a designated leader?
Is there access to HCPs in infection management and stewardship in the hospital willing to be part of AMS teams?
Does your hospital currently offer educational resources to support training of HCPs regarding antimicrobial prescribing and its monitoring to improve future care?
Is there dedicated and sufficient budget to support AMS activities
Do you have access to laboratory/imaging services to support improved antibiotic use and away from untargeted and unnecessary prescribing, and are the results available in a timely manner to support diagnosis and appropriate antibiotic prescribing?
Does your ASP currently monitor compliance with one or more agreed interventions, e.g., improved compliance to national or local guidelines, and report back the findings to improve future care including any changes in the quality/ appropriateness of antimicrobial prescribing in agreed areas?
Has your hospital conducted a PPS in the past year and used the findings to improve future antimicrobial prescribing?
Does your hospital have available and up-to-date recommendations for infection management, and are these readily available to prescribers?
Does your hospital currently have any published AMS protocols such as a restricted antimicrobial list especially surrounding ‘Watch’ and ‘Reserve’ antibiotics and IV to oral switching policies
Does your hospital currently have any published Infection Prevention and Control protocols, and are these regularly monitored, e.g., surrounding hand hygiene protocols?
AMS—Antimicrobial Stewardship; ASP—Antimicrobial Stewardship program; HCP—Healthcare Professional.
Their details and documented impact are summarized in Table 3. Typically, multiple interventions are more successful with improving future prescribing than single interventions. In addition, activities need to be continually followed up. Otherwise, prescribing habits could drift back towards pre-intervention levels.
One problem is the regular turn-around of junior staff, who subsequently need training on antimicrobial prescribing for continuous improvement. The increasing availability of electronic tools should help in this regard in the future [199].
Table 3.
Summary of published studies across Africa documenting ASPs and their impact.
| Author, Country and Year | Intervention and Aim | Impact of the Intervention |
|---|---|---|
| Low Income * | ||
| Gebretekle et al., Ethiopia, 2020 [176] |
|
|
| Alabi et al., Liberia, 2022 [134] |
|
Improvements were seen in all QIs:
|
| Lester et al., Malawi, 2020 [193] |
|
|
| Suliman et al., Sudan, 2020 [188] |
|
|
| Gentilotti et al., Tanzania, 2020 [160] |
|
|
| Ashiru-Oredope et al., 2022 [135] |
|
|
| Ngonzi et al., Uganda, 2021 [197] |
|
|
| Low-Middle Income * | ||
| Aitken et al., Kenya, 2013 [152] |
|
|
| Amdany et al., Kenya, 2014 [181] |
|
|
| Ntumba et al., Kenya, 2015 [194] |
|
|
| Ayieko et al., Kenya, 2019 [187] |
|
|
| Allegranzi et al., Kenya, Uganda, Zambia, and Zimbabwe, 2018 [195] |
|
|
| Abubakar et al., Nigeria, 2019 [200] |
|
|
| Upper-Middle Income * | ||
| Messina et al., South Africa, 2015 [177] |
|
|
| Brink et al., South Africa, 2016 [174] |
|
|
| Boyles et al., South Africa, 2017 [175] |
|
|
| Brink et al., South Africa, 2017 [189] |
|
|
| Junaid et al., South Africa, 2018 [192] |
|
|
| van den Bergh et al., South Africa, 2020 [184] |
|
|
| Bashar et al., South Africa, 2021 [173] |
|
|
AMS: Antimicrobial Stewardship; ASP: Antimicrobial Stewardship Program; CAP: Community Acquired Pneumonia; ECS: Emergency Caesarean Sections; ICU: Intensive Care Unit; HCP: Healthcare Professional; IPC: Infection, Prevention and Control; PPS: Point Prevalence Survey; QI: Quality Indicator; SSI: Surgical Site Infection; * World Bank Status.
2.5. Suggested Activities to Improve Future Antimicrobial Prescribing in Hospitals
The suggested strategies to improve antibiotic utilization among hospitals across Africa, which will be crucial to reduce AMR, have been divided into short- and long-term initiatives (Table 4). These build on the potential for developing and expanding the use of digital technologies surrounding electronic health records and electronic prescribing to improve appropriate antibiotic use [199,201,202,203]. Such developments are essential to develop and regularly monitor antimicrobial prescribing against agreed prescribing/quality indicators.
Table 4.
Suggested strategies to improve future antimicrobial utilization among hospitals across Africa.
| Timescale | Potential Strategies |
|---|---|
| Short to Medium Term (e.g., 1 to 5 years) |
Health authorities/Governments (if not already instigated)
|
| Long Term (5 to 10 years) |
Potential long-term strategies include:
|
AMR: Antimicrobial Resistance; AMS: Antimicrobial stewardship; ASPs: Antimicrobial Stewardship Programs; CST: Culture and Sensitivity Testing; DTC: Drug and Therapeutic Committees; HCP: Healthcare Professional; IPC: Infection, Prevention and Control; NAP: National Action Plans for AMR; PPS: Point Prevalence Surveys; SSIs: Surgical Site Infections.
3. Discussion
Reducing the burden of AMR is a high priority across Africa given its appreciable impact on morbidity, mortality and costs [38,39,43,232]. This is in part driven by the inappropriate and overuse of antimicrobials; however, this association appears less clear cut in LMICs due to the risks of contagion [28,232,233,234,235,236,237]. The multiple PPS studies undertaken across Africa in recent years (Table 1) have shown considerable usage across most African countries compared with other countries and continents [112], with the highest rates seen in Nigeria between 59.6 and 97.6% of surveyed patients. These utilization rates are appreciably higher than the suggested WHO target of 40% of hospital in-patients [238]. The lower utilization rates seen in South Africa, at 33.6% to 49.7% of hospital in-patients, may reflect the fact that the South African Government launched its ‘Antimicrobial Resistance National Strategy Framework’ in 2014, coupled with the availability of microbiology laboratories and the performance of hospitals being regularly monitored since 2014 [171,239]. Greater implementation of the NAPs is needed to reduce future utlization rates in hospitals; however, some African countries have only just started on this activity [70]. An average compliance of 59.5% to the National strategy was recently recorded among 26 public sector facilities across South Africa helping to improve antimicrobial prescribing and reducing AMR [239].
Encouragingly, the penicillins (typically in the Access group) and metronidazole were among the most prescribed antibiotics across Africa (Table S1), with currently limited prescribing of ‘Reserve’ antibiotics. However, there was appreciable prescribing of cephalosporins, which are typically third-generation cephalosporins incorporating ceftriaxone, in hospitals including for SAP, which is a concern as ceftriaxone is a ‘Watch’ category antibiotic. Greater prescribing of ‘Access’ antibiotics in hospitals, where appropriate, can be achieved through establishing pertinent prescribing/ quality targets as well as monitoring subsequent utilization patterns in hospitals as part of ASPs. This can be part of a plethora of both short- and longer-term initiatives that can be undertaken across Africa to improve future antimicrobial use and combat AMR (Table 4). Other prescribing/quality targets are needed to ensure appropriate use of SAP to prevent SSIs by moving away from extended use post-operatively. As seen (Table 1), there is currently appreciable extended use of antibiotics for SAP across Africa, which needs urgently to be addressed to reduce adverse reactions, AMR and costs [83]. Successful ASPs have been implemented among African countries to improve antimicrobial use for SAP (Table 3) providing exemplars.
The number of PPS studies have grown across Africa over time (Table S1) despite concerns with available resources and personnel, providing future guidance, and this acceleration will continue. In addition, we are seeing the number of successful ASPs increase across Africa (Table 3), despite again initial concerns regarding available financial resources and personnel to conduct ASPs in LMICs, providing exemplars to others [128,132,137,138]. This will continue as part of NAPs to reduce rising AMR rates across Africa [2,70].
Potential strategies for all key stakeholders to improve future prescribing of antimicrobials in the hospital sector have been consolidated into suggested short-, medium- and longer-term activities to provide future direction (Table 4). The key is Government commitment and activities through NAPs, and we are already seeing African countries develop and implement these [70]. However, considerable challenges still remain in terms of available finances to undertake agreed activities as well as available personnel to undertake suggested ASP activities and monitor their progress in hospitals. We will continue to monitor the situation given, as mentioned, concerns with rising AMR rates across Africa and the resultant impact on mortality and costs.
It is imperative that Africa progresses with activities to reduce AMR, with AMR seen as the next pandemic and the highest resistance rates are currently in Africa [2,40]. Suggested future research activities will also include a greater understanding of current antimicrobial utilization patterns in ambulatory care given the extent of utilization in this sector versus hospital use, especially for self-limiting conditions such as acute respiratory tract infections [12,70]. Increased digitalization of patient records within healthcare systems across Africa will assist with this [240].
We are aware of a number of limitations with this paper. These include the fact that we have not undertaken full systematic reviews for each topic including PPS and SSI studies as well as QIs and ASPs for the reasons discussed. However, we have documented an appreciable number of PPS and SSI studies across Africa, together with current prescribing/ quality indicators in use and ASPs. This has been achieved with the considerable knowledge of the senior level co-authors, similar to discussions on potential future strategies. Despite these limitations, we believe our findings and suggestions are robust given the extent of examples coupled with our methodology providing future direction.
4. Materials and Methods
The principal approach was a narrative review of key areas. This was supplemented by the considerable experience of the co-authors across countries and continents dealing with patients with infectious diseases as well as recording current utilization patterns, implementing policies to improve future prescribing including the development of pertinent quality indicators as well as researching and implementing ASPs.
This mirrors similar studies undertaken by the co-authors across a number of African countries and wider when providing future guidance regarding the management of both infectious and non-infectious diseases, as well as more general approaches, and is in line with institutional guidance [9,12,70,83,95,107,221,241,242,243,244,245,246].
4.1. Antimicrobial Utilization Patterns in Hospitals across Africa
The methodology built on a recent systematic review of PPS studies undertaken by some of the co-authors [247], and involved studies from 2016 onwards until October 2022. This methodology was employed since some of the sourced studies known to the co-authors would not have been incorporated in databases including PubMed and Web of Science. In addition, the principal objective of this paper was to document the findings from across Africa to provide a basis for the future. As such, we did not pre-specify which African countries would be included in this narrative review in order to provide as complete a picture as possible to provide exemplars for the future.
Similar to the systematic review of Saleem et al. (2020) [247], key categories included the number of participating hospitals, the PPS methodology, e.g., ECDC, Global PPS or WHO [16,65,77,81,238]; first, second or third most prescribed antibiotic broken down by ATC code and AWaRe classification [56,58,248]; whether prescribed for prophylaxis or treatment and the average number of antibiotics prescribed per patient.
As mentioned, we did not include the 12 hospitals taking part in the Global PPS study of Versporten et al. (2018) in the collation of published PPS studies alongside the African hospitals taking part in the study of Pauwels et al. (2021) as different parameters were collected in these studies including details of the most prescribed antibiotics across the indications [60,112]. However, we did include the study of D’Arcy et al. (2021) involving several African countries as this did contain relevant detailed information [81].
We are aware that some of the PPS studies referenced may contain the same hospital. For this reason, we did not include in the Table (Table S1) the total number of hospitals per country in the various PPS studies. The intention was to list the various studies as exemplars going forward. The various African countries were broken down by their World Bank classification, i.e., low-income, low-middle and upper-middle-income countries, building on the recent study of Adekoya et al. (2021) for consistency [59]. This is because, as mentioned, there have been concerns with available resources and personnel within hospitals among LMICs to undertake PPS studies, and we wanted to explore this further.
4.2. Antibiotic Prophylaxis to Prevent Surgical Site Infections
The principal approach was a narrative review, building on recent publications involving some of the co-authors [83,150]. This was supplemented by additional studies from 2016 onwards known to the co-authors, which included details of antibiotics being prescribed to prevent SSIs incorporated in the sourced PPS studies (Table S1). This is similar to the approach adopted by the co-authors in other studies. The various African countries were again broken down by their World Bank classification, i.e., low-income, low-middle and upper-middle-income countries, building on the recent study of Adekoya et al. (2021) for consistency [59].
4.3. Prescribing Indicators
The principal approach was again a narrative review building on recent publications involving the co-authors supplemented by additional studies known to the senior-level co-authors. This is similar to the approach adopted by the co-authors for the PPS and SSI studies.
4.4. Antimicrobial Stewardship Programs
The principal approach was a narrative review of recent ASPs that had been instigated across Africa. This built on recent reviews coupled with additional studies known to the co-authors from 2013 onwards [132,137,138]. The objective was again to provide guidance to African countries planning ASPs rather than undertaking a systematic review of the studies.
In order to enhance understanding, the different activities that can be undertaken by groups within hospitals when instigating ASPs will be broken down into the 4Es. These are Education, Engineering, Economics and Enforcement [83,249]. Education incorporates a number of activities including developing and communicating formularies as well as developing and monitoring adherence to agreed guidance [116,214,215,249,250]. Engineering includes organizational or managerial interventions [240]. This incorporates for instance prescribing targets such as an agreed percentage of antibiotics being prescribed according to accepted guidelines, an agreed percentage of prescribing of ‘Access’ antibiotics from the WHO AWaRe list, as well as an agreed percentage of patients prescribed short courses of antibiotics to prevent SSIs [9,58,116]. Economics includes financial incentives to clinicians, patients, pharmacists or hospitals to improve the rational use of medicines such as incentives for clinicians when reaching agreed prescribing targets as well as fining pharmacists for dispensing an antibiotic without a prescription when this is prohibited [249,251]. Enforcement includes enforcing regulations by law including prohibiting the dispensing of antibiotics within pharmacies without a prescription or regulations banning the use of colistin unless under strict regulations [9,251,252,253].
The various African countries were again broken down by their World Bank classification, i.e., low-income, low-middle and upper-middle-income countries, building on the recent study of Adekoya et al. (2021) for consistency [59]. This is because, as mentioned, there have been serious concerns about the ability of especially low- and low-middle-income countries to undertake ASPs in practice due to lack of resources and personnel [128].
5. Conclusions
In conclusion, reducing AMR has to be a high priority among all African countries given its clinical and economic impact. Without such activities, AMR will become the next pandemic. However, reducing AMR rates requires multiple coordinated activities across sectors driven by Governments and others across Africa as part of NAPs. This includes an urgent need for HCPs to appreciably reduce inappropriate prescribing of antibiotics across hospitals as well as increased cognisance of classifications and their implications such as the AWaRe classification when prescribing. This necessitates active surveillance of current utilization and resistance patterns across hospitals as well as initiating ASPs for target areas. Such activities include reducing the extent of antibiotic prophylaxis post-operatively for SAP, routinely incorporating the rationale for prescribing of antibiotics in patients’ notes alongside inserting start and stop dates, as well as developing and disseminating locally agreed guidelines.
This is essential given limited new antimicrobials being developed as well as concerns with the routine availability of specific antibiotics to tackle resistance; however, this is compensated, to some extent, by developments in vaccine technologies. The latter will require strategies to address the current high rates of vaccine hesitancy that exist across Africa as seen in the recent COVID-19 pandemic. A coordinated approach including all key stakeholder groups is also essential to minimize misinformation and maximize the impact of future interventions to reduce AMR rates. This can be part of an agreed One Health approach incorporated into NAPs.
Acknowledgments
The authors would like to thank the Deanship of Scientific research at the Umm Al-Qura University for their help with this work via grant code: 22UQU4290073DSR05.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/antibiotics11121824/s1, Box S1: Potential barriers to instigating ASPs in hospitals and improving future antimicrobial prescribing, Table S1: Literature review of point prevalence surveys across Africa.
Author Contributions
Conceptualization, Z.S., B.G., S.M.C., L.S., I.A.S., J.C.M. and C.E.M.; methodology, Z.S., B.G., A.C., M.A.K., S.M.C., L.S., A.H., A.A., J.O.F., H.N. and C.E.M.; validation, Z.S., B.G., A.C., M.A.K., S.M.C., R.A.S., L.S., A.H., A.A., A.K., J.C.M. (Julius C. Mwita), I.A.S., S.A.O., J.O.F., O.O.O., J.C.M. (Johanna C. Meyer), A.M., D.K., A.C.K., M.S., H.N., G.P. and C.E.M.; investigation, Z.S., B.G., A.C., M.A.K., S.M.C., R.A.S., L.S., A.H., A.A., A.K., J.C.M. (Julius C. Mwita), I.A.S., S.A.O., J.O.F., O.O.O., J.C.M. (Johanna C. Meyer), A.M., D.K., A.C.K., M.S., H.N., G.P. and C.E.M.; resources, Z.S., B.G., A.C., L.S. and C.E.M.; data curation, Z.S., B.G., A.C., M.A.K., S.M.C., R.A.S., L.S., A.H., A.A., A.K., J.C.M. (Julius C. Mwita), I.A.S., S.A.O., J.O.F., O.O.O., J.C.M. (Johanna C. Meyer), A.M., D.K., A.C.K., M.S., G.P. and C.E.M.; writing—original draft preparation, B.G.; writing—review and editing, Z.S., B.G., A.C., M.A.K., S.M.C., R.A.S., L.S., A.H., A.A., A.K., J.C.M. (Julius C. Mwita), I.A.S., S.A.O., J.O.F., O.O.O., J.C.M. (Johanna C. Meyer), A.M., D.K., A.C.K., M.S., H.N. and C.E.M.; visualization, Z.S., B.G., A.C., S.M.C., L.S. and C.E.M.; supervision, B.G.; project administration, B.G. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
There was no ethical approval as this study did not involve direct contact with humans or animals. We have used this approach before when undertaking similar studies. This is in line with previous similar papers published by the co-authors [9,12,70,83,241,245,247,253,254].
Informed Consent Statement
There was no informed consent as this study did not involve direct contact with patients.
Data Availability Statement
Additional data are available on reasonable request from the corresponding author. However, all informational sources and papers have been extensively referenced. References [255,256,257,258,259,260,261,262,263,264,265,266] are cited in Supplementary Materials file.
Conflicts of Interest
The authors declare no relevant conflict of interest.
Funding Statement
A.C. and C.E.M. are funded by the Welcome Trust (222051/Z/20/Z) for the ADILA project.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hofer U. The cost of antimicrobial resistance. Nat. Rev. Microbiol. 2019;17:3. doi: 10.1038/s41579-018-0125-x. [DOI] [PubMed] [Google Scholar]
- 2.Murray C.J., Ikuta K.S., Sharara F., Swetschinski L., Aguilar G.R., Gray A., Han C., Bisignano C., Rao P., Wool E., et al. Global burden of bacterial antimicrobial resistance in 2019: A systematic analysis. Lancet. 2022;399:629–655. doi: 10.1016/S0140-6736(21)02724-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cassini A., Högberg L.D., Plachouras D., Quattrocchi A., Hoxha A., Simonsen G.S., Colomb-Cotinat M., Kretzschmar M.E., Devleesschauwer B., Michele Cecchini M., et al. Attributable deaths and disability-adjusted life-years caused by infections with antibiotic-resistant bacteria in the EU and the European Economic Area in 2015: A population-level modelling analysis. Lancet Infect. Dis. 2019;19:56–66. doi: 10.1016/S1473-3099(18)30605-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Founou R.C., Founou L.L., Essack S.Y. Clinical and economic impact of antibiotic resistance in developing countries: A systematic review and meta-analysis. PLoS ONE. 2017;12:e0189621. doi: 10.1371/journal.pone.0189621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nkengasong J.N., Tessema S.K. Africa Needs a New Public Health Order to Tackle Infectious Disease Threats. Cell. 2020;183:296–300. doi: 10.1016/j.cell.2020.09.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bell D., Schultz Hansen K. Relative Burdens of the COVID-19, Malaria, Tuberculosis, and HIV/AIDS Epidemics in Sub-Saharan Africa. Am. J. Trop. Med. Hyg. 2021;105:1510–1515. doi: 10.4269/ajtmh.21-0899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dwyer-Lindgren L., Cork M.A., Sligar A., Steuben K.M., Wilson K.F., Provost N.R., Mayala B.K., VanderHeide J.D., Collison M.L., Hall J.B., et al. Mapping HIV prevalence in sub-Saharan Africa between 2000 and 2017. Nature. 2019;570:189–193. doi: 10.1038/s41586-019-1200-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Williams P.C.M., Isaacs D., Berkley J.A. Antimicrobial resistance among children in sub-Saharan Africa. Lancet Infect. Dis. 2018;18:e33–e44. doi: 10.1016/S1473-3099(17)30467-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Godman B., Egwuenu A., Haque M., Malande O., Schellack N., Kumar S., Saleem Z., Sneddon J., Hoxha I., Islam S., et al. Strategies to Improve Antimicrobial Utilization with a Special Focus on Developing Countries. Life. 2021;11:528. doi: 10.3390/life11060528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.StatPearls. StatPearls Publishing LLC.; Treasure Island, FL, USA: 2022. Prevention of Opportunistic Infections in HIV/AIDS. StatPearls Publishing Copyright © 2022. [Google Scholar]
- 11.Belachew S.A., Hall L., Selvey L.A. Non-prescription dispensing of antibiotic agents among community drug retail outlets in Sub-Saharan African countries: A systematic review and meta-analysis. Antimicrob. Resist. Infect. Control. 2021;10:13. doi: 10.1186/s13756-020-00880-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Godman B., Haque M., McKimm J., Abu Bakar M., Sneddon J., Wale J., Campbell S., Martin A.P., Hoxha I., Abilova V., et al. Ongoing strategies to improve the management of upper respiratory tract infections and reduce inappropriate antibiotic use particularly among lower and middle-income countries: Findings and implications for the future. Curr. Med. Res. Opin. 2020;36:301–327. doi: 10.1080/03007995.2019.1700947. [DOI] [PubMed] [Google Scholar]
- 13.Kiggundu R., Wittenauer R., Waswa J., Nakambale H.N., Kitutu F.E., Murungi M., Okuna N., Morries S., Lawry L.L., Joshi M.P., et al. Point Prevalence Survey of Antibiotic Use across 13 Hospitals in Uganda. Antibiotics. 2022;11:199. doi: 10.3390/antibiotics11020199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ogunleye O.O., Oyawole M.R., Odunuga P.T., Kalejaye F., Yinka-Ogunleye A.F., Olalekan A., Ogundele S.O., Ebruke B.E., Richard A.K., Paramadhas B.D.A., et al. A multicentre point prevalence study of antibiotics utilization in hospitalized patients in an urban secondary and a tertiary healthcare facilities in Nigeria: Findings and implications. Expert Rev. Anti-Infect. Ther. 2022;20:297–306. doi: 10.1080/14787210.2021.1941870. [DOI] [PubMed] [Google Scholar]
- 15.Gwebu P.C., Meyer J.C., Schellack N., Matsebula-Myeni Z.C., Godman B. A web-based point prevalence survey of antimicrobial use and quality indicators at Raleigh Fitkin Memorial Hospital in the Kingdom of Eswatini and the implications. Hosp. Pract. 2022;50:214–221. doi: 10.1080/21548331.2022.2069247. [DOI] [PubMed] [Google Scholar]
- 16.Aboderin A.O., Adeyemo A.T., Olayinka A.A., Oginni A.S., Adeyemo A.T., Oni A.A., Olabisi O.F., Fayomi O.D., Anuforo A.C., Egwuenu A., et al. Antimicrobial use among hospitalized patients: A multi-center, point prevalence survey across public healthcare facilities, Osun State, Nigeria. Germs. 2021;11:523–535. doi: 10.18683/germs.2021.1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sulis G., Adam P., Nafade V., Gore G., Daniels B., Daftary A., Das J., Gandra S., Pai M. Antibiotic prescription practices in primary care in low- and middle-income countries: A systematic review and meta-analysis. PLoS Med. 2020;17:e1003139. doi: 10.1371/journal.pmed.1003139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gasson J., Blockman M., Willems B. Antibiotic prescribing practice and adherence to guidelines in primary care in the Cape Town Metro District, South Africa. S. Afr. Med. J. 2018;108:304–310. doi: 10.7196/SAMJ.2018.v108i4.12564. [DOI] [PubMed] [Google Scholar]
- 19.Anand Paramadhas B.D., Tiroyakgosi C., Mpinda-Joseph P., Morokotso M., Matome M., Sinkala F., Gaolebe M., Malone B., Molosiwa E., Shanmugam M.G., et al. Point prevalence study of antimicrobial use among hospitals across Botswana; findings and implications. Expert Rev. Anti-Infect. Ther. 2019;17:535–546. doi: 10.1080/14787210.2019.1629288. [DOI] [PubMed] [Google Scholar]
- 20.Guma S.P., Godman B., Campbell S.M., Mahomed O. Determinants of the Empiric Use of Antibiotics by General practitioners in South Africa: Observational, Analytic, Cross-Sectional Study. Antibiotics. 2022;11:1423. doi: 10.3390/antibiotics11101423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ndaki P.M., Mushi M.F., Mwanga J.R., Konje E.T., Ntinginya N.E., Mmbaga B.T., Keenan K., Sabiiti W., Kesby M., Benitez-Paez F., et al. Dispensing Antibiotics without Prescription at Community Pharmacies and Accredited Drug Dispensing Outlets in Tanzania: A Cross-Sectional Study. Antibiotics. 2021;10:1025. doi: 10.3390/antibiotics10081025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Auta A., Hadi M.A., Oga E., Adewuyi E.O., Abdu-Aguye S.N., Adeloye D., Strickland-Hodge B., Morgan D.J. Global access to antibiotics without prescription in community pharmacies: A systematic review and meta-analysis. J. Infect. 2019;78:8–18. doi: 10.1016/j.jinf.2018.07.001. [DOI] [PubMed] [Google Scholar]
- 23.Batista A.D., Rodrigues D.A., Figueiras A., Zapata-Cachafeiro M., Roque F., Herdeiro M.T. Antibiotic Dispensation without a Prescription Worldwide: A Systematic Review. Antibiotics. 2020;9:786. doi: 10.3390/antibiotics9110786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kalungia A.C., Burger J., Godman B., Costa J.O., Simuwelu C. Non-prescription sale and dispensing of antibiotics in community pharmacies in Zambia. Expert Rev. Anti-Infect. Ther. 2016;14:1215–1223. doi: 10.1080/14787210.2016.1227702. [DOI] [PubMed] [Google Scholar]
- 25.Kibuule D., Kagoya H.R., Godman B. Antibiotic use in acute respiratory infections in under-fives in Uganda: Findings and implications. Expert Rev. Anti-Infect. Ther. 2016;14:863–872. doi: 10.1080/14787210.2016.1206468. [DOI] [PubMed] [Google Scholar]
- 26.Sakeena M.H.F., Bennett A.A., McLachlan A.J. Non-prescription sales of antimicrobial agents at community pharmacies in developing countries: A systematic review. Int. J. Antimicrob. Agents. 2018;52:771–782. doi: 10.1016/j.ijantimicag.2018.09.022. [DOI] [PubMed] [Google Scholar]
- 27.Afari-Asiedu S., Oppong F.B., Tostmann A., Abdulai M.A., Boamah-Kaali E., Gyaase S., Agyei O., Kinsman J., Hulscher M., Wertheim H.F.L., et al. Determinants of Inappropriate Antibiotics Use in Rural Central Ghana Using a Mixed Methods Approach. Front Public Health. 2020;8:90. doi: 10.3389/fpubh.2020.00090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Klein E.Y., Tseng K.K., Pant S., Laxminarayan R. Tracking global trends in the effectiveness of antibiotic therapy using the Drug Resistance Index. BMJ Glob. Health. 2019;4:e001315. doi: 10.1136/bmjgh-2018-001315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mokwele R.N., Schellack N., Bronkhorst E., Brink A.J., Schweickerdt L., Godman B. Using mystery shoppers to determine practices pertaining to antibiotic dispensing without a prescription among community pharmacies in South Africa—A pilot survey. JAC-Antimicrob. Resist. 2022;4:dlab196. doi: 10.1093/jacamr/dlab196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kaupitwa C.J., Nowaseb S., Godman B., Kibuule D. Analysis of policies for use of medically important antibiotics in animals in Namibia: Implications for antimicrobial stewardship. Expert Rev. Anti-Infect. Ther. 2022;20:1365–1379. doi: 10.1080/14787210.2022.2108404. [DOI] [PubMed] [Google Scholar]
- 31.Mudenda S., Mukosha M., Godman B., Fadare J., Malama S., Munyeme M., Hikaambo C.N., Kalungia A.C., Hamachila A., Kainga H., et al. Knowledge, Attitudes, and Practices of Community Pharmacy Professionals on Poultry Antibiotic Dispensing, Use, and Bacterial Antimicrobial Resistance in Zambia: Implications on Antibiotic Stewardship and WHO AWaRe Classification of Antibiotics. Antibiotics. 2022;11:1210. doi: 10.3390/antibiotics11091210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Van Boeckel T.P., Pires J., Silvester R., Zhao C., Song J., Criscuolo N.G., Gilbert M., Bonhoeffer S., Laxminarayan R. Global trends in antimicrobial resistance in animals in low- and middle-income countries. Science. 2019;365:eaaw1944. doi: 10.1126/science.aaw1944. [DOI] [PubMed] [Google Scholar]
- 33.Jibril A.H., Okeke I.N., Dalsgaard A., Olsen J.E. Association between antimicrobial usage and resistance in Salmonella from poultry farms in Nigeria. BMC Vet. Res. 2021;17:234. doi: 10.1186/s12917-021-02938-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Njoga E.O., Ogugua A.J., Nwankwo I.O., Awoyomi O.J., Okoli C.E., Buba D.M., Oyeleye F.A., Ajibo F.E., Azor N., Ogunniran T.M. Antimicrobial drug usage pattern in poultry farms in Nigeria: Implications for food safety, public health and poultry disease management. Vet. Ital. 2021;57:5–12. doi: 10.12834/VetIt.2117.11956.1. [DOI] [PubMed] [Google Scholar]
- 35.Hedman H.D., Vasco K.A., Zhang L. A Review of Antimicrobial Resistance in Poultry Farming within Low-Resource Settings. Animals. 2020;10:264. doi: 10.3390/ani10081264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Aslam B., Khurshid M., Arshad M.I., Muzammil S., Rasool M., Yasmeen N., Shah T., Chaudhry T.H., Rasool M.H., Shahid A., et al. Antibiotic Resistance: One Health One World Outlook. Front. Cell. Infect. Microbiol. 2021;11:771510. doi: 10.3389/fcimb.2021.771510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hernando-Amado S., Coque T.M., Baquero F., Martínez J.L. Defining and combating antibiotic resistance from One Health and Global Health perspectives. Nat. Microbiol. 2019;4:1432–1442. doi: 10.1038/s41564-019-0503-9. [DOI] [PubMed] [Google Scholar]
- 38.Dadgostar P. Antimicrobial Resistance: Implications and Costs. Infect. Drug Resist. 2019;12:3903–3910. doi: 10.2147/IDR.S234610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.The World Bank Final Report—DRUG-RESISTANT INFECTIONS. A Threat to Our Economic Future March 2017. [(accessed on 15 November 2022)]. Available online: http://documents1.worldbank.org/curated/en/323311493396993758/pdf/final-report.pdf.
- 40.Gautam A. Antimicrobial Resistance: The Next Probable Pandemic. JNMA J. Nepal Med. Assoc. 2022;60:225–228. doi: 10.31729/jnma.7174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lim J.M., Singh S.R., Duong M.C., Legido-Quigley H., Hsu L.Y., Tam C.C. Impact of national interventions to promote responsible antibiotic use: A systematic review. J. Antimicrob. Chemother. 2020;75:14–29. doi: 10.1093/jac/dkz348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kamere N., Garwe S.T., Akinwotu O.O., Tuck C., Krockow E.M., Yadav S., Olawale A.G., Diyaolu A.H., Munkombwe D., Muringu E., et al. Scoping Review of National Antimicrobial Stewardship Activities in Eight African Countries and Adaptable Recommendations. Antibiotics. 2022;11:1149. doi: 10.3390/antibiotics11091149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Interagency Coordination Group on Antimicrobial Resistance No Time to Wait: Securing the Future from Drug-Resistant Infections—Report to the Secretary-General of the United Nations. 2019. [(accessed on 15 November 2022)]. Available online: https://www.who.int/antimicrobial-resistance/interagency-coordination-group/IACG_final_report_EN.pdf?ua=1.
- 44.OECD Health Policy Studies Stemming the Superbug Tide. 2018. [(accessed on 15 November 2022)]. Available online: https://www.oecd-ilibrary.org/sites/9789264307599-en/index.html?itemId=/content/publication/9789264307599-en&mimeType=text/html.
- 45.World Health Organization (WHO) Food and Agriculture Organization of the United Nations (FAO) World Organisation for Animal Health (OIE) Monitoring Global Progress on Antimicrobial Resistance: Tripartite Amr Country Self-Assessment Survey (Tracss) 2019–2020 Global Analysis Report. 2021. [(accessed on 14 November 2022)]. Available online: https://www.who.int/publications/i/item/monitoring-global-progress-on-antimicrobial-resistance-tripartite-amr-country-self-assessment-survey-(tracss)-2019-2020.
- 46.BSAC Global Antimicrobial Stewardship Accreditation Scheme. 2021. [(accessed on 15 November 2022)]. Available online: https://bsac.org.uk/global-antimicrobial-stewardship-accreditation-scheme/
- 47.World Bank Group Pulling Together to Beat Superbugs Knowledge and Implementation Gaps in Addressing Antimicrobial Resistance. 2019. [(accessed on 14 November 2022)]. Available online: https://openknowledge.worldbank.org/bitstream/handle/10986/32552/Pulling-Together-to-Beat-Superbugs-Knowledge-and-Implementation-Gaps-in-Addressing-Antimicrobial-Resistance.pdf?sequence=1&isAllowed=y.
- 48.WHO Global Action Plan on Antimicrobial Resistance—Report by the Secretariat. 2016. [(accessed on 15 November 2022)]. Available online: https://apps.who.int/gb/ebwha/pdf_files/WHA69/A69_24-en.pdf.
- 49.Matee M. Antimicrobial resistance (AMR) at the Southern Africa Centre for Infectious Disease Surveillance. 2018. [(accessed on 14 November 2022)]. Available online: https://www.openaccessgovernment.org/southern-africa-centre-for-infectious-disease/52063/
- 50.Craig J., Frost I., Sriram A., Nuttall J., Kapoor G., Alimi Y., Varma J. Development of the first edition of African treatment guidelines for common bacterial infections and syndromes. J. Public Health Afr. 2021;12:2009. doi: 10.4081/jphia.2021.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Africa Centres for Disease Control and Prevention and Center for Disease Dynamics, Economics & Policy African Antibiotic Treatment Guidelines for Common Bacterial Infections and Syndromes—Recommended Antibiotic Treatments in Neonatal and Pediatric Patients. 2021. [(accessed on 15 November 2022)]. Available online: https://africaguidelines.cddep.org/wp-content/uploads/2021/11/Quick-Reference-Guide_Peds_English.pdf.
- 52.ASLM The African Society for Laboratory Medicine. [(accessed on 14 November 2022)]. Available online: https://aslm.org/
- 53.Tornimbene B., Eremin S., Abednego R., Abualas E.O., Boutiba I., Egwuenu A., Fuller W., Gahimbare L., Githii S., Kasambara W., et al. Global Antimicrobial Resistance and Use Surveillance System on the African continent: Early implementation 2017–2019. Afr. J. Lab. Med. 2022;11:1594. doi: 10.4102/ajlm.v11i1.1594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Fraser J.L., Alimi Y.H., Varma J.K., Muraya T., Kujinga T., Carter V.K., Schultsz C., Vilas V.J.D.R. Antimicrobial resistance control efforts in Africa: A survey of the role of Civil Society Organisations. Glob. Health Action. 2021;14:1868055. doi: 10.1080/16549716.2020.1868055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sharland M., Pulcini C., Harbarth S., Zeng M., Gandra S., Mathur S., Magrini N. Classifying antibiotics in the WHO Essential Medicines List for optimal use-be AWaRe. Lancet Infect. Dis. 2018;18:18–20. doi: 10.1016/S1473-3099(17)30724-7. [DOI] [PubMed] [Google Scholar]
- 56.Sharland M., Gandra S., Huttner B., Moja L., Pulcini C., Zeng M., Mendelson M., Cappello B., Cooke G., Magrini N., et al. Encouraging AWaRe-ness and discouraging inappropriate antibiotic use-the new 2019 Essential Medicines List becomes a global antibiotic stewardship tool. Lancet Infect. Dis. 2019;19:1278–1280. doi: 10.1016/S1473-3099(19)30532-8. [DOI] [PubMed] [Google Scholar]
- 57.Klein E.Y., Milkowska-Shibata M., Tseng K.K., Sharland M., Gandra S., Pulcini C., Laxminarayan R. Assessment of WHO antibiotic consumption and access targets in 76 countries, 2000–2015: An analysis of pharmaceutical sales data. Lancet Infect. Dis. 2021;21:107–115. doi: 10.1016/S1473-3099(20)30332-7. [DOI] [PubMed] [Google Scholar]
- 58.Hsia Y., Lee B.R., Versporten A., Yang Y., Bielicki J., Jackson C., Newland J., Goossens H., Magrini N., Sharland M., et al. Use of the WHO Access, Watch, and Reserve classification to define patterns of hospital antibiotic use (AWaRe): An analysis of paediatric survey data from 56 countries. Lancet Glob. Health. 2019;7:e861–e871. doi: 10.1016/S2214-109X(19)30071-3. [DOI] [PubMed] [Google Scholar]
- 59.Adekoya I., Maraj D., Steiner L., Yaphe H., Moja L., Magrini N., Cooke G., Loeb M., Persaud N. Comparison of antibiotics included in national essential medicines lists of 138 countries using the WHO Access, Watch, Reserve (AWaRe) classification: A cross-sectional study. Lancet Infect. Dis. 2021;21:1429–1440. doi: 10.1016/S1473-3099(20)30854-9. [DOI] [PubMed] [Google Scholar]
- 60.Pauwels I., Versporten A., Drapier N., Vlieghe E., Goossens H. Hospital antibiotic prescribing patterns in adult patients according to the WHO Access, Watch and Reserve classification (AWaRe): Results from a worldwide point prevalence survey in 69 countries. J. Antimicrob. Chemother. 2021;76:1614–1624. doi: 10.1093/jac/dkab050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Skosana P., Schellack N., Godman B., Kurdi A., Bennie M., Kruger D., Meyer J. A national, multicentre, web-based point prevalence survey of antimicrobial use and quality indices among hospitalised paediatric patients across South Africa. J. Glob. Antimicrob. Resist. 2022;29:542–550. doi: 10.1016/j.jgar.2021.12.003. [DOI] [PubMed] [Google Scholar]
- 62.Skosana P.P., Schellack N., Godman B., Kurdi A., Bennie M., Kruger D., Meyer J.C. A national, multicentre web-based point prevalence survey of antimicrobial use in community healthcare centres across South Africa and the implications. Hosp. Pract. 2022;50:306–317. doi: 10.1080/21548331.2022.2114251. [DOI] [PubMed] [Google Scholar]
- 63.Amponsah O.K.O., Buabeng K.O., Owusu-Ofori A., Ayisi-Boateng N.K., Hämeen-Anttila K., Enlund H. Point prevalence survey of antibiotic consumption across three hospitals in Ghana. JAC Antimicrob. Resist. 2021;3:dlab008. doi: 10.1093/jacamr/dlab008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Seni J., Mapunjo S.G., Wittenauer R., Valimba R., Stergachis A., Werth B.J., Saitoti S., Mhadu N.H., Lusaya E., Konduri N. Antimicrobial use across six referral hospitals in Tanzania: A point prevalence survey. BMJ Open. 2020;10:e042819. doi: 10.1136/bmjopen-2020-042819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hsia Y., Sharland M., Jackson C., Wong I.C.K., Magrini N., Bielicki J.A. Consumption of oral antibiotic formulations for young children according to the WHO Access, Watch, Reserve (AWaRe) antibiotic groups: An analysis of sales data from 70 middle-income and high-income countries. Lancet Infect. Dis. 2019;19:67–75. doi: 10.1016/S1473-3099(18)30547-4. [DOI] [PubMed] [Google Scholar]
- 66.Moolla M.S., Whitelaw A., Decloedt E.H., Koegelenberg C.F.N., Parker A. Opportunities to enhance antibiotic stewardship: Colistin use and outcomes in a low-resource setting. JAC Antimicrob. Resist. 2021;3:dlab169. doi: 10.1093/jacamr/dlab169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Prusakov P., Goff D.A., Wozniak P.S., Cassim A., Scipion C.E., Urzúa S., Ronchi A., Zeng L., Ladipo-Ajayi O., Aviles-Otero N., et al. A global point prevalence survey of antimicrobial use in neonatal intensive care units: The no-more-antibiotics and resistance (NO-MAS-R) study. eClinicalMedicine. 2021;32:100727. doi: 10.1016/j.eclinm.2021.100727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Munkholm L., Rubin O. The global governance of antimicrobial resistance: A cross-country study of alignment between the global action plan and national action plans. Glob. Health. 2020;16:109. doi: 10.1186/s12992-020-00639-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Iwu C.D., Patrick S.M. An insight into the implementation of the global action plan on antimicrobial resistance in the WHO African region: A roadmap for action. Int. J. Antimicrob. Agents. 2021;58:106411. doi: 10.1016/j.ijantimicag.2021.106411. [DOI] [PubMed] [Google Scholar]
- 70.Godman B., Egwuenu A., Wesangula E., Schellack N., Kalungia A.C., Tiroyakgosi C., Kgatlwane J., Mwita J.C., Patrick O., Niba L.L., et al. Tackling antimicrobial resistance across sub-Saharan Africa: Current challenges and implications for the future. Expert Opin. Drug Saf. 2022;21:1089–1111. doi: 10.1080/14740338.2022.2106368. [DOI] [PubMed] [Google Scholar]
- 71.Federal Ministries of Agriculture, Rural Development, Environment and Health, Abuja, Nigeria National Action Plan for Antimicrobial Resistance, 2017–2022. [(accessed on 15 November 2022)];2017 Available online: https://ncdc.gov.ng/themes/common/docs/protocols/77_1511368219.pdf.
- 72.Ghana Ministry of Health, Ministry of Food and Agriculture, Ministry of Environment, Science, Technology and Innovation, Ministry of Fisheries and Aquaculture Development Ghana National Action Plan for Antimicrobial Use and Resistance. 2017–2021. [(accessed on 14 November 2022)]; Available online: http://www.moh.gov.gh/wp-content/uploads/2018/04/NAP_FINAL_PDF_A4_19.03.2018-SIGNED-1.pdf.
- 73.Sangeda R.Z., Kibona J., Munishi C., Arabi F., Manyanga V.P., Mwambete K.D., Horumpende P.G. Assessment of Implementation of Antimicrobial Resistance Surveillance and Antimicrobial Stewardship Programs in Tanzanian Health Facilities a Year After Launch of the National Action Plan. Front. Public Health. 2020;8:454. doi: 10.3389/fpubh.2020.00454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Koduah A., Gyansa-Lutterodt M., Hedidor G.K., Sekyi-Brown R., Asiedu-Danso M., Asare B.A., Ackon A.A., Annan E.A. Antimicrobial resistance national level dialogue and action in Ghana: Setting and sustaining the agenda and outcomes. One Health Outlook. 2021;3:18. doi: 10.1186/s42522-021-00051-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Labi A.-K., Obeng-Nkrumah N., Dayie N.T.K.D., Egyir B., Sampane-Donkor E., Newman M.J., Opintan J.A. Antimicrobial use in hospitalized patients: A multicentre point prevalence survey across seven hospitals in Ghana. JAC Antimicrob. Resist. 2021;3:dlab087. doi: 10.1093/jacamr/dlab087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Afriyie D.K., Sefah I.A., Sneddon J., Malcolm W., McKinney R., Cooper L., Kurdi A., Godman B., Seaton R.A. Antimicrobial point prevalence surveys in two Ghanaian hospitals: Opportunities for antimicrobial stewardship. JAC Antimicrob. Resist. 2020;2:dlaa001. doi: 10.1093/jacamr/dlaa001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Dodoo C., Orman E., Alalbila T., Mensah A., Jato J., Mfoafo K., Folitse I., Hutton-Nyameaye A., Ben I.O., Mensah-Kane P., et al. Antimicrobial Prescription Pattern in Ho Teaching Hospital, Ghana: Seasonal Determination Using a Point Prevalence Survey. Antibiotics. 2021;10:199. doi: 10.3390/antibiotics10020199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Okoth C., Opanga S., Okalebo F., Oluka M., Baker Kurdi A., Godman B. Point prevalence survey of antibiotic use and resistance at a referral hospital in Kenya: Findings and implications. Hosp. Pract. 2018;46:128–136. doi: 10.1080/21548331.2018.1464872. [DOI] [PubMed] [Google Scholar]
- 79.Momanyi L., Opanga S., Nyamu D., Oluka M., Kurdi A., Godman B. Antibiotic Prescribing Patterns at a Leading Referral Hospital in Kenya: A Point Prevalence Survey. J. Res. Pharm. Pract. 2019;8:149–154. doi: 10.4103/jrpp.JRPP_18_68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Omulo S., Oluka M., Ombajo L., Osoro E., Kinuthia R., Guantai A., Ndegwa L., Verani J., Opanga S., Wesangula E., et al. Point-Prevalence Surveys of Antibiotic Use at Three Large Public Hospitals in Kenya. Infect. Control Hosp. Epidemiol. 2020;41:s353–s354. doi: 10.1017/ice.2020.971. [DOI] [Google Scholar]
- 81.D’Arcy N., Ashiru-Oredope D., Olaoye O., Afriyie D., Akello Z., Ankrah D., Asima D.M., Banda D.C., Barrett S., Brandish C., et al. Antibiotic Prescribing Patterns in Ghana, Uganda, Zambia and Tanzania Hospitals: Results from the Global Point Prevalence Survey (G-PPS) on Antimicrobial Use and Stewardship Interventions Implemented. Antibiotics. 2021;10:1122. doi: 10.3390/antibiotics10091122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Abubakar U. Antibiotic use among hospitalized patients in northern Nigeria: A multicenter point-prevalence survey. BMC Infect. Dis. 2020;20:86. doi: 10.1186/s12879-020-4815-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Mwita J.C., Ogunleye O.O., Olalekan A., Kalungia A.C., Kurdi A., Saleem Z., Sneddon J., Godman B. Key Issues Surrounding Appropriate Antibiotic Use for Prevention of Surgical Site Infections in Low- and Middle-Income Countries: A Narrative Review and the Implications. Int. J. Gen. Med. 2021;14:515–530. doi: 10.2147/IJGM.S253216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Bediako-Bowan A., Owusu E., Debrah S., Kjerulf A., Newman M., Kurtzhals J., Mølbak K. Surveillance of surgical site infection in a teaching hospital in Ghana: A prospective cohort study. J. Hosp. Infect. 2020;104:321–327. doi: 10.1016/j.jhin.2020.01.004. [DOI] [PubMed] [Google Scholar]
- 85.Alshaikh F.S., Godman B., Sindi O.N., Seaton R.A., Kurdi A. Prevalence of bacterial coinfection and patterns of antibiotics prescribing in patients with COVID-19: A systematic review and meta-analysis. PLoS ONE. 2022;17:e0272375. doi: 10.1371/journal.pone.0272375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Langford B.J., So M., Raybardhan S., Leung V., Westwood D., MacFadden D.R., Soucy J.-P.R., Daneman N. Bacterial co-infection and secondary infection in patients with COVID-19: A living rapid review and meta-analysis. Clin. Microbiol. Infect. 2020;26:1622–1629. doi: 10.1016/j.cmi.2020.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Langford B.J., So M., Raybardhan S., Leung V., Soucy J.-P.R., Westwood D., Daneman N., MacFadden D.R. Antibiotic prescribing in patients with COVID-19: Rapid review and meta-analysis. Clin. Microbiol. Infect. 2021;27:520–531. doi: 10.1016/j.cmi.2020.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Jeon K., Jeong S., Lee N., Park M.-J., Song W., Kim H.-S., Kim H.S., Kim J.-S. Impact of COVID-19 on Antimicrobial Consumption and Spread of Multidrug-Resistance in Bacterial Infections. Antibiotics. 2022;11:535. doi: 10.3390/antibiotics11040535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Fukushige M., Ngo N.-H., Lukmanto D., Fukuda S., Ohneda O. Effect of the COVID-19 pandemic on antibiotic consumption: A systematic review comparing 2019 and 2020 data. Front. Public Health. 2022;10:946077. doi: 10.3389/fpubh.2022.946077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Adebisi Y.A., Jimoh N.D., Ogunkola I.O., Uwizeyimana T., Olayemi A.H., Ukor N.A., Lucero-Prisno D.E. The use of antibiotics in COVID-19 management: A rapid review of national treatment guidelines in 10 African countries. Trop. Med. Health. 2021;49:51. doi: 10.1186/s41182-021-00344-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Al-Hadidi S.H., Alhussain H., Hadi H.A., Johar A., Yassine H.M., Al Thani A.A., Eltai N.O. The Spectrum of Antibiotic Prescribing During COVID-19 Pandemic: A Systematic Literature Review. Microb. Drug Resist. 2021;27:1705–1725. doi: 10.1089/mdr.2020.0619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Founou R.C., Blocker A.J., Noubom M., Tsayem C., Choukem S.P., Dongen M.V., Founou L.L. The COVID-19 pandemic: A threat to antimicrobial resistance containment. Future Sci. OA. 2021;7:Fso736. doi: 10.2144/fsoa-2021-0012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Ghosh S., Bornman C., Zafer M.M. Antimicrobial Resistance Threats in the emerging COVID-19 pandemic: Where do we stand? J. Infect. Public Health. 2021;14:555–560. doi: 10.1016/j.jiph.2021.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Quincho-Lopez A., Benites-Ibarra C.A., Hilario-Gomez M.M., Quijano-Escate R., Taype-Rondan A. Self-medication practices to prevent or manage COVID-19: A systematic review. PLoS ONE. 2021;16:e0259317. doi: 10.1371/journal.pone.0259317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Sefah I.A., Ogunleye O.O., Essah D.O., Opanga S.A., Butt N., Wamaitha A., Guantai A.N., Chikowe I., Khuluza F., Kibuule D., et al. Rapid Assessment of the Potential Paucity and Price Increases for Suggested Medicines and Protection Equipment for COVID-19 Across Developing Countries With a Particular Focus on Africa and the Implications. Front. Pharmacol. 2020;11:588106. doi: 10.3389/fphar.2020.588106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Hsu J. How COVID-19 is accelerating the threat of antimicrobial resistance. Bmj. 2020;369:m1983. doi: 10.1136/bmj.m1983. [DOI] [PubMed] [Google Scholar]
- 97.Iwu C.J., Jordan P., Jaja I.F., Iwu C.D., Wiysonge C.S. Treatment of COVID-19: Implications for antimicrobial resistance in Africa. Pan Afr. Med. J. 2020;35((Suppl. S2)):119. doi: 10.11604/pamj.supp.2020.35.2.23713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Lai C.C., Chen S.Y., Ko W.C., Hsueh P.R. Increased antimicrobial resistance during the COVID-19 pandemic. Int. J. Antimicrob. Agents. 2021;57:106324. doi: 10.1016/j.ijantimicag.2021.106324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Ramzan K., Shafiq S., Raees I., Mustafa Z.U., Salman M., Khan A.H., Meyer J.C., Godman B. Co-Infections, Secondary Infections, and Antimicrobial Use in Patients Hospitalized with COVID-19 during the First Five Waves of the Pandemic in Pakistan; Findings and Implications. Antibiotics. 2022;11:789. doi: 10.3390/antibiotics11060789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Do N.T.T., Vu H.T.L., Nguyen C.T.K., Punpuing S., Khan W.A., Gyapong M., Asante K.P., Munguambe K., Gómez-Olivé F.X., John-Langba J., et al. Community-based antibiotic access and use in six low-income and middle-income countries: A mixed-method approach. Lancet Glob. Health. 2021;9:e610–e619. doi: 10.1016/S2214-109X(21)00024-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Laxminarayan R., Matsoso P., Pant S., Brower C., Røttingen J.-A., Klugman K., Davies S. Access to effective antimicrobials: A worldwide challenge. Lancet. 2016;387:168–175. doi: 10.1016/S0140-6736(15)00474-2. [DOI] [PubMed] [Google Scholar]
- 102.Kållberg C., Årdal C., Salvesen Blix H., Klein E., MMartinez E., Lindbæk M., Outterson K., Røttingen J.A., Laxminarayan R. Introduction and geographic availability of new antibiotics approved between 1999 and 2014. PLoS ONE. 2018;13:e0205166. doi: 10.1371/journal.pone.0205166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Wang K., Wang L., Li M., Xie B., He L., Wang M., Zhang R., Hou N., Zhang Y., Jia F. Real-Word Effectiveness of Global COVID-19 Vaccines Against SARS-CoV-2 Variants: A Systematic Review and Meta-Analysis. Front. Med. 2022;9:820544. doi: 10.3389/fmed.2022.820544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Mohammed I., Nauman A., Paul P., Ganesan S., Chen K.-H., Jalil S.M.S., Jaouni S.H., Kawas H., Khan W.A., Vattoth A.L., et al. The efficacy and effectiveness of the COVID-19 vaccines in reducing infection, severity, hospitalization, and mortality: A systematic review. Hum. Vaccines Immunother. 2022;18:2027160. doi: 10.1080/21645515.2022.2027160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Martínez-Baz I., Miqueleiz A., Casado I., Navascués A., Trobajo-Sanmartín C., Burgui C., Guevara M., Ezpeleta C., Castilla J. Effectiveness of COVID-19 vaccines in preventing SARS-CoV-2 infection and hospitalisation, Navarre, Spain, January to April 2021. Eurosurveillance. 2021;26:2100438. doi: 10.2807/1560-7917.ES.2021.26.21.2100438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Korang S.K., von Rohden E., Veroniki A.A., Ong G., Ngalamika O., Siddiqui F., Juul S., Nielsen E.E., Feinberg J.B., Petersen J.J., et al. Vaccines to prevent COVID-19: A living systematic review with Trial Sequential Analysis and network meta-analysis of randomized clinical trials. PLoS ONE. 2022;17:e0260733. doi: 10.1371/journal.pone.0260733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Ogunleye O.O., Godman B., Fadare J.O., Mudenda S., Adeoti A.O., Yinka-Ogunleye A.F., Ogundele S.O., Oyawole M.R., Schönfeldt M., Rashed W.M., et al. Coronavirus Disease 2019 (COVID-19) Pandemic across Africa: Current Status of Vaccinations and Implications for the Future. Vaccines. 2022;10:1553. doi: 10.3390/vaccines10091553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Njoga E.O., Mshelbwala P.P., Abah K.O., Awoyomi O.J., Wangdi K., Pewan S.B., Oyeleye F.A., Galadima H.B., Alhassan S.A., Okoli C.E., et al. COVID-19 Vaccine Hesitancy and Determinants of Acceptance among Healthcare Workers, Academics and Tertiary Students in Nigeria. Vaccines. 2022;10:626. doi: 10.3390/vaccines10040626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Njoga E.O., Awoyomi O.J., Onwumere-Idolor O.S., Awoyomi P.O., Ugochukwu I.C.I., Ozioko S.N. Persisting Vaccine Hesitancy in Africa: The Whys, Global Public Health Consequences and Ways-Out-COVID-19 Vaccination Acceptance Rates as Case-in-Point. Vaccines. 2022;10:1934. doi: 10.3390/vaccines10111934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Nathwani D., Varghese D., Stephens J., Ansari W., Martin S., Charbonneau C. Value of hospital antimicrobial stewardship programs [ASPs]: A systematic review. Antimicrob. Resist. Infect. Control. 2019;8:35. doi: 10.1186/s13756-019-0471-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.de Carvalho F.R.T., Telles J.P., Tuon F.F.B., Rabello Filho R., Caruso P., Correa T.D. Antimicrobial Stewardship Programs: A Review of Strategies to Avoid Polymyxins and Carbapenems Misuse in Low Middle-Income Countries. Antibiotics. 2022;11:378. doi: 10.3390/antibiotics11030378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Versporten A., Zarb P., Caniaux I., Gros M.-F., Drapier N., Miller M., Jarlier V., Nathwani D., Goossens H., Koraqi A., et al. Antimicrobial consumption and resistance in adult hospital inpatients in 53 countries: Results of an internet-based global point prevalence survey. Lancet Glob. Health. 2018;6:e619–e629. doi: 10.1016/S2214-109X(18)30186-4. [DOI] [PubMed] [Google Scholar]
- 113.Le Maréchal M., Tebano G., Monnier A.A., Adriaenssens N., Gyssens I.C., Huttner B., Milanic R., Schouten J., Benic M.S., Versporten A., et al. Quality indicators assessing antibiotic use in the outpatient setting: A systematic review followed by an international multidisciplinary consensus procedure. J. Antimicrob. Chemother. 2018;73((Suppl. S6)):vi40–vi49. doi: 10.1093/jac/dky117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Nnadozie U.U., Umeokonkwo C.D., Maduba C.C., Igwe-Okomiso D., Onah C.K., Madubueze U.C., Anikwe C.C., Versporten A., Pauwels I., Goossens H., et al. Antibiotic use among surgical inpatients at a tertiary health facility: A case for a standardized protocol for presumptive antimicrobial therapy in the developing world. Infect. Prev. Pract. 2020;2:100078. doi: 10.1016/j.infpip.2020.100078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Niaz Q., Godman B., Massele A., Campbell S., Kurdi A., Kagoya H.R., Kibuule D. Validity of World Health Organisation prescribing indicators in Namibia’s primary healthcare: Findings and implications. Int. J. Qual. Health Care. 2018;31:338–345. doi: 10.1093/intqhc/mzy172. [DOI] [PubMed] [Google Scholar]
- 116.Campbell S.M., Meyer J.C., Godman B. Why Compliance to National Prescribing Guidelines is Important Especially across Sub-Saharan Africa and Suggestions for the Future. Biomed. Pharm. Sci. 2021;4:1–7. [Google Scholar]
- 117.Sulis G., Sayood S., Gandra S. Antimicrobial resistance in low- and middle-income countries: Current status and future directions. Expert Rev. Anti-Infect. Ther. 2022;20:147–160. doi: 10.1080/14787210.2021.1951705. [DOI] [PubMed] [Google Scholar]
- 118.Haldeman M.S., Kishimbo P., Seddon M., Sangare A., Mwasomola D., Hall J., Shaffer M., Leclair R., Caulder C., Bookstaver P.B., et al. Evaluation of Antimicrobial Utilization and Concordance with National Guidelines at a Tertiary Hospital in the Southern Highlands Zone of Tanzania. Am. J. Trop. Med. Hyg. 2020;102:370–376. doi: 10.4269/ajtmh.19-0231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Alsaeed O.M., Bukhari A.A., Alshehri A.A., Alsumairi F.A., Alnami A.M., Elsheikh H.A. The Use of Antibiotics for the Prevention of Surgical Site Infections in Two Government Hospitals in Taif, Saudi Arabia: A Retrospective Study. Cureus. 2022;14:e26731. doi: 10.7759/cureus.26731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Alagha H.Z., Al Telbani M.J. Investigating antibiotic use in Gaza Strip hospitals: A retrospective cross-sectional analysis. J. Infect. Dev. Ctries. 2022;16:1739–1747. doi: 10.3855/jidc.16985. [DOI] [PubMed] [Google Scholar]
- 121.Eticha E.M., Gemechu W.D. Adherence to Guidelines for Assessment and Empiric Antibiotics Recommendations for Community-Acquired Pneumonia at Ambo University Referral Hospital: Prospective Observational Study. Patient Prefer. Adherence. 2021;15:467–473. doi: 10.2147/PPA.S295118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Mugada V., Mahato V., Andhavaram D., Vajhala S.M. Evaluation of Prescribing Patterns of Antibiotics Using Selected Indicators for Antimicrobial Use in Hospitals and the Access, Watch, Reserve (AWaRe) Classification by the World Health Organization. Turk. J. Pharm. Sci. 2021;18:282–288. doi: 10.4274/tjps.galenos.2020.11456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Dechasa M., Chelkeba L., Jorise A., Sefera B., Melaku T. Antibiotics use evaluation among hospitalized adult patients at Jimma Medical Center, southwestern Ethiopia: The way to pave for antimicrobial stewardship. J. Pharm. Policy Pract. 2022;15:84. doi: 10.1186/s40545-022-00490-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.WHO. World Bank. OECD Delivering Quality Health Services: A Global Imperative for Universal Health Coverage. 2018. [(accessed on 14 November 2022)]. Available online: https://documents1.worldbank.org/curated/en/482771530290792652/pdf/127816-REVISED-quality-joint-publication-July2018-Complete-vignettes-ebook-L.pdf.
- 125.Campbell S.M., Braspenning J., Hutchinson A., Marshall M. Research methods used in developing and applying quality indicators in primary care. Qual. Saf. Health Care. 2002;11:358–364. doi: 10.1136/qhc.11.4.358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Campbell S.M., Kontopantelis E., Hannon K., Burke M., Barber A., Lester H.E. Framework and indicator testing protocol for developing and piloting quality indicators for the UK quality and outcomes framework. BMC Fam. Pract. 2011;12:85. doi: 10.1186/1471-2296-12-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Campbell S.M., Godman B., Diogene E., Fürst J., Gustafsson L.L., MacBride-Stewart S., Malmström R.E., Pedersen H., Selke G., Vlahović-Palčevski V., et al. Quality indicators as a tool in improving the introduction of new medicines. Basic Clin. Pharmacol. Toxicol. 2015;116:146–157. doi: 10.1111/bcpt.12295. [DOI] [PubMed] [Google Scholar]
- 128.Cox J.A., Vlieghe E., Mendelson M., Wertheim H., Ndegwa L., Villegas M.V., Gould I., Hara G.L. Antibiotic stewardship in low- and middle-income countries: The same but different? Clin. Microbiol. Infect. 2017;23:812–818. doi: 10.1016/j.cmi.2017.07.010. [DOI] [PubMed] [Google Scholar]
- 129.Fadare J.O., Ogunleye O., Iliyasu G., Adeoti A., Schellack N., Engler D., Massele A., Godman B. Status of antimicrobial stewardship programmes in Nigerian tertiary healthcare facilities: Findings and implications. J. Glob. Antimicrob. Resist. 2019;17:132–136. doi: 10.1016/j.jgar.2018.11.025. [DOI] [PubMed] [Google Scholar]
- 130.Kalungia A.C., Mwambula H., Munkombwe D., Marshall S., Schellack N., May C., Jones A.S.C., Godman B. Antimicrobial stewardship knowledge and perception among physicians and pharmacists at leading tertiary teaching hospitals in Zambia: Implications for future policy and practice. J. Chemother. 2019;31:378–387. doi: 10.1080/1120009X.2019.1622293. [DOI] [PubMed] [Google Scholar]
- 131.Hall J.W., Bouchard J., Bookstaver P.B., Haldeman M.S., Kishimbo P., Mbwanji G., Mwakyula I., Mwasomola D., Seddon M., Shaffer M., et al. The Mbeya Antimicrobial Stewardship Team: Implementing Antimicrobial Stewardship at a Zonal-Level Hospital in Southern Tanzania. Pharmacy. 2020;8:107. doi: 10.3390/pharmacy8020107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Akpan M.R., Isemin N.U., Udoh A.E., Ashiru-Oredope D. Implementation of antimicrobial stewardship programmes in African countries: A systematic literature review. J. Glob. Antimicrob. Resist. 2020;22:317–324. doi: 10.1016/j.jgar.2020.03.009. [DOI] [PubMed] [Google Scholar]
- 133.Ackers L., Ackers-Johnson G., Seekles M., Odur J., Opio S. Opportunities and Challenges for Improving Anti-Microbial Stewardship in Low- and Middle-Income Countries; Lessons Learnt from the Maternal Sepsis Intervention in Western Uganda. Antibiotics. 2020;9:315. doi: 10.3390/antibiotics9060315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Alabi A.S., Picka S.W., Sirleaf R., Ntirenganya P.R., Ayebare A., Correa N., Anyango S., Ekwen G., Agu E., Cook R., et al. Implementation of an antimicrobial stewardship programme in three regional hospitals in the south-east of Liberia: Lessons learned. JAC Antimicrob. Resist. 2022;4:dlac069. doi: 10.1093/jacamr/dlac069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Ashiru-Oredope D., Garraghan F., Olaoye O., Krockow E.M., Matuluko A., Nambatya W., Babigumira P.A., Tuck C., Amofah G., Ankrah D., et al. Development and Implementation of an Antimicrobial Stewardship Checklist in Sub-Saharan Africa: A Co-Creation Consensus Approach. Healthcare. 2022;10:170. doi: 10.3390/healthcare10091706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Gulumbe B.H., Haruna U.A., Almazan J., Ibrahim I.H., Faggo A.A., Bazata A.Y. Combating the menace of antimicrobial resistance in Africa: A review on stewardship, surveillance and diagnostic strategies. Biol. Proced. Online. 2022;24:19. doi: 10.1186/s12575-022-00182-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Siachalinga L., Mufwambi W., Lee I.H. Impact of antimicrobial stewardship interventions to improve antibiotic prescribing for hospital inpatients in Africa: A systematic review and meta-analysis. J. Hosp. Infect. 2022;129:124–143. doi: 10.1016/j.jhin.2022.07.031. [DOI] [PubMed] [Google Scholar]
- 138.Otieno P.A., Campbell S., Maley S., Obinju Arunga T., Otieno Okumu M. A Systematic Review of Pharmacist-Led Antimicrobial Stewardship Programs in Sub-Saharan Africa. Int. J. Clin. Pract. 2022;2022:3639943. doi: 10.1155/2022/3639943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.WHO Antimicrobial stewardship programmes in health-care facilities in low- and middle-income countries: A WHO practical toolkit. JAC Antimicrob. Resist. 2019;1:dlz072. doi: 10.1093/jacamr/dlz072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.WHO Antimicrobial Stewardship Programmes in Health-Care Facilities in Low- and Middle-Income Countries. A WHO Practical Toolkit. 2019. [(accessed on 15 November 2022)]. Available online: https://apps.who.int/iris/bitstream/handle/10665/329404/9789241515481-eng.pdf. [DOI] [PMC free article] [PubMed]
- 141.Sefah I.A., Denoo E.Y., Bangalee V., Kurdi A., Sneddon J., Godman B. Appropriateness of surgical antimicrobial prophylaxis in a teaching hospital in Ghana: Findings and implications. JAC Antimicrob. Resist. 2022;4:dlac102. doi: 10.1093/jacamr/dlac102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Abubakar U. Point-prevalence survey of hospital acquired infections in three acute care hospitals in Northern Nigeria. Antimicrob. Resist. Infect. Control. 2020;9:63. doi: 10.1186/s13756-020-00722-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Martinez-Sobalvarro J.V., Júnior A.A.P., Pereira L.B., Baldoni A.O., Ceron C.S., Dos Reis T.M. Antimicrobial stewardship for surgical antibiotic prophylaxis and surgical site infections: A systematic review. Int. J. Clin. Pharm. 2022;44:301–319. doi: 10.1007/s11096-021-01358-4. [DOI] [PubMed] [Google Scholar]
- 144.Forrester J.D., Maggio P.M., Tennakoon L. Cost of Health Care-Associated Infections in the United States. J. Patient Saf. 2022;18:e477–e479. doi: 10.1097/PTS.0000000000000845. [DOI] [PubMed] [Google Scholar]
- 145.Liu X., Cui D., Li H., Wang Q., Mao Z., Fang L., Ren N., Sun J. Direct medical burden of antimicrobial-resistant healthcare-associated infections: Empirical evidence from China. J. Hosp. Infect. 2020;105:295–305. doi: 10.1016/j.jhin.2020.01.003. [DOI] [PubMed] [Google Scholar]
- 146.Branch-Elliman W., O’Brien W., Strymish J., Itani K., Wyatt C., Gupta K. Association of Duration and Type of Surgical Prophylaxis With Antimicrobial-Associated Adverse Events. JAMA Surg. 2019;154:590–598. doi: 10.1001/jamasurg.2019.0569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Kalungia A.C., Mukosha M., Mwila C., Banda D., Mwale M., Kagulura S., Ogunleye O.O., Meyer J.C., Godman B. Antibiotic Use and Stewardship Indicators in the First- and Second-Level Hospitals in Zambia: Findings and Implications for the Future. Antibiotics. 2022;11:1626. doi: 10.3390/antibiotics11111626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Kiguba R., Karamagi C., Bird S.M. Extensive antibiotic prescription rate among hospitalized patients in Uganda: But with frequent missed-dose days. J. Antimicrob. Chemother. 2016;71:1697–1706. doi: 10.1093/jac/dkw025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Butt S.Z., Ahmad M., Saeed H., Saleem Z., Javaid Z. Post-surgical antibiotic prophylaxis: Impact of pharmacist’s educational intervention on appropriate use of antibiotics. J. Infect. Public Health. 2019;12:854–860. doi: 10.1016/j.jiph.2019.05.015. [DOI] [PubMed] [Google Scholar]
- 150.Cooper L., Sneddon J., Afriyie D.K., Sefah I.A., Kurdi A., Godman B., Seaton R.A. Supporting global antimicrobial stewardship: Antibiotic prophylaxis for the prevention of surgical site infection in low- and middle-income countries (LMICs): A scoping review and meta-analysis. JAC-Antimicrob. Resist. 2020;2:dlaa070. doi: 10.1093/jacamr/dlaa070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Abubakar U., Syed Sulaiman S.A., Adesiyun A.G. Utilization of surgical antibiotic prophylaxis for obstetrics and gynaecology surgeries in Northern Nigeria. Int. J. Clin. Pharm. 2018;40:1037–1043. doi: 10.1007/s11096-018-0702-0. [DOI] [PubMed] [Google Scholar]
- 152.Aiken A.M., Wanyoro A.K., Mwangi J., Juma F., Mugoya I.K., Scott J.A. Changing use of surgical antibiotic prophylaxis in Thika Hospital, Kenya: A quality improvement intervention with an interrupted time series design. PLoS ONE. 2013;8:e78942. doi: 10.1371/annotation/6506cc0b-2878-4cf8-b663-23a2f32a199a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Bediako-Bowan A.A.A., Mølbak K., Kurtzhals J.A.L., Owusu E., Debrah S., Newman M.J. Risk factors for surgical site infections in abdominal surgeries in Ghana: Emphasis on the impact of operating rooms door openings. Epidemiol. Infect. 2020;148:e147. doi: 10.1017/S0950268820001454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Ouedraogo A.S., Versporten A., Nagalo A., Pauwels I., Goossens H., Ouedraogo A., Poda A. The Global Point Prevalence Survey of Antimicrobial Consumptionand Resistance (Global-PPS)—Results of antimicrobial prescribing in Burkina Faso. 2019. [(accessed on 15 November 2022)]. Available online: https://www.global-pps.com/wp-content/uploads/2021/02/The-Global-PPS_results-of-antimicrobial-prescribing-in-Burkina-Faso.pdf.
- 155.Halawi E., Assefa T., Hussen S. Pattern of antibiotics use, incidence and predictors of surgical site infections in a Tertiary Care Teaching Hospital. BMC Res. Notes. 2018;11:538. doi: 10.1186/s13104-018-3643-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Alemkere G. Antibiotic usage in surgical prophylaxis: A prospective observational study in the surgical ward of Nekemte referral hospital. PLoS ONE. 2018;13:e0203523. doi: 10.1371/journal.pone.0203523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Fentie A.M., Degefaw Y., Asfaw G., Shewarega W., Woldearegay M., Abebe E., Gebretekle G.B. Multicentre point-prevalence survey of antibiotic use and healthcare-associated infections in Ethiopian hospitals. BMJ Open. 2022;12:e054541. doi: 10.1136/bmjopen-2021-054541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Nkurunziza T., Kateera F., Sonderman K., Gruendl M., Nihiwacu E., Ramadhan B., Cherian T., Nahimana E., Ntakiyiruta G., Habiyakare C., et al. Prevalence and predictors of surgical-site infection after caesarean section at a rural district hospital in Rwanda. Br. J. Surg. 2019;106:e121–e128. doi: 10.1002/bjs.11060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Horumpende P.G., Mshana S.E., Mouw E.F., Mmbaga B.T., Chilongola J.O., de Mast Q. Point prevalence survey of antimicrobial use in three hospitals in North-Eastern Tanzania. Antimicrob. Resist. Infect. Control. 2020;9:149. doi: 10.1186/s13756-020-00809-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Gentilotti E., De Nardo P., Nguhuni B., Piscini A., Damian C., Vairo F., Chaula Z., Mencarini P., Torokaa P., Zumla A., et al. Implementing a combined infection prevention and control with antimicrobial stewardship joint program to prevent caesarean section surgical site infections and antimicrobial resistance: A Tanzanian tertiary hospital experience. Antimicrob. Resist. Infect. Control. 2020;9:69. doi: 10.1186/s13756-020-00740-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Saito H., Inoue K., Ditai J., Weeks A.D. Pattern of Peri-Operative Antibiotic Use among Surgical Patients in a Regional Referral and Teaching Hospital in Uganda. Surg. Infect. 2020;21:540–546. doi: 10.1089/sur.2019.176. [DOI] [PubMed] [Google Scholar]
- 162.Bunduki G.K., Mukululi M.P., Masumbuko C.K., Uwonda S.A. Compliance of antibiotics used for surgical site infection prophylaxis among patients undergoing surgery in a Congolese teaching hospital. Infect. Prev. Pract. 2020;2:100075. doi: 10.1016/j.infpip.2020.100075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Bediako-Bowan A.A.A., Owusu E., Labi A.-K., Obeng-Nkrumah N., Sunkwa-Mills G., Bjerrum S., Opintan J.A., Bannerman C., Mølbak K., Kurtzhals J.A.L., et al. Antibiotic use in surgical units of selected hospitals in Ghana: A multi-centre point prevalence survey. BMC Public Health. 2019;19:797. doi: 10.1186/s12889-019-7162-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Ankrah D., Owusu H., Aggor A., Osei A., Ampomah A., Harrison M., Nelson F., Aboagye G.O., Ekpale P., Laryea J., et al. Point Prevalence Survey of Antimicrobial Utilization in Ghana’s Premier Hospital: Implications for Antimicrobial Stewardship. Antibiotics. 2021;10:1528. doi: 10.3390/antibiotics10121528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Opanga S.A., Mwangombe N.J., Okalebo F.A., Godman B., Oluka M., Kuria K.A.M. Determinants of the Effectiveness of Antimicrobial Prophylaxis among Neurotrauma Patients at a Referral Hospital in Kenya: Findings and Implications. Infect. Dis. Prev. Med. 2017;5:169. [Google Scholar]
- 166.Talaam R.C., Abungana M.M., Ooko P.B. An antibiotic audit of the surgical department at a rural hospital in Western Kenya. Pan Afr. Med. J. 2018;29:219. doi: 10.11604/pamj.2018.29.219.14510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Nsofor C., Es A., Obijuru C., Ohalete C., Ukwandu N. Prevalence of Antimicrobial Use in Major Hospitals in Owerri, Nigeria. EC Microbiol. 2016;3:522–527. [Google Scholar]
- 168.Oduyebo O., Olayinka A., Iregbu K., Versporten A., Goossens H., Nwajiobi-Princewill P., Jimoh O., Ige T., Aigbe A., Ola-Bello O., et al. A point prevalence survey of antimicrobial prescribing in four Nigerian Tertiary Hospitals. Ann. Trop. Pathol. 2017;8:42–46. doi: 10.4103/atp.atp_38_17. [DOI] [Google Scholar]
- 169.Fowotade A., Fasuyi T., Aigbovo O., Versporten A., Adekanmbi O., Akinyemi O., Goossens H., Kehinde A., Oduyebo O. Point Prevalence Survey of Antimicrobial Prescribing in a Nigerian Hospital: Findings and Implications on Antimicrobial Resistance. West Afr. J. Med. 2020;37:216–220. [PubMed] [Google Scholar]
- 170.Mwita J.C., Souda S., Magafu M., Massele A., Godman B., Mwandri M. Prophylactic antibiotics to prevent surgical site infections in Botswana: Findings and implications. Hosp. Pract. 2018;46:97–102. doi: 10.1080/21548331.2018.1450605. [DOI] [PubMed] [Google Scholar]
- 171.Skosana P., Schellack N., Godman B., Kurdi A., Bennie M., Kruger D., Meyer J. A point prevalence survey of antimicrobial utilisation patterns and quality indices amongst hospitals in South Africa; findings and implications. Expert Rev. Anti-Infect. Ther. 2021;19:1353–1366. doi: 10.1080/14787210.2021.1898946. [DOI] [PubMed] [Google Scholar]
- 172.Kruger D., Dlamini N., Meyer J., Godman B., Kurdi A., Lennon M., Bennie M., Schellack N. Development of a web-based application to improve data collection of antimicrobial utilization in the public health care system in South Africa. Hosp. Pract. 2021;49:184–193. doi: 10.1080/21548331.2021.1889213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Bashar M.A., Miot J., Shoul E., van Zyl R.L. Impact of an antibiotic stewardship programme in a surgical setting. S. Afr. J. Infect. Dis. 2021;36:307. doi: 10.4102/sajid.v36i1.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Brink A.J., Messina A.P., Feldman C., Richards G.A., Becker P.J., Goff D.A., Bauer K.A., Nathwani D., van den Bergh D., on behalf of the Netcare Antimicrobial Stewardship Study Alliance Antimicrobial stewardship across 47 South African hospitals: An implementation study. Lancet Infect. Dis. 2016;16:1017–1025. doi: 10.1016/S1473-3099(16)30012-3. [DOI] [PubMed] [Google Scholar]
- 175.Boyles T.H., Naicker V., Rawoot N., Raubenheimer P.J., Eick B., Mendelson M. Sustained reduction in antibiotic consumption in a South African public sector hospital; Four year outcomes from the Groote Schuur Hospital antibiotic stewardship program. S. Afr. Med. J. 2017;107:115–118. doi: 10.7196/SAMJ.2017.v107i2.12067. [DOI] [PubMed] [Google Scholar]
- 176.Gebretekle G.B., Mariam D.H., Taye W.A., Fentie A.M., Degu W.A., Alemayehu T., Beyene T., Libman M., Fenta T.G., Yansouni C.P., et al. Half of Prescribed Antibiotics Are Not Needed: A Pharmacist-Led Antimicrobial Stewardship Intervention and Clinical Outcomes in a Referral Hospital in Ethiopia. Front. Public Health. 2020;8:109. doi: 10.3389/fpubh.2020.00109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Messina A.P., van den Bergh D., Goff D.A. Antimicrobial Stewardship with Pharmacist Intervention Improves Timeliness of Antimicrobials Across Thirty-three Hospitals in South Africa. Infect. Dis. Ther. 2015;4((Suppl. S1)):5–14. doi: 10.1007/s40121-015-0082-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Labi A.-K., Obeng-Nkrumah N., Nartey E.T., Bjerrum S., Adu-Aryee N.A., Ofori-Adjei Y.A., Yawson A.E., Newman M.J. Antibiotic use in a tertiary healthcare facility in Ghana: A point prevalence survey. Antimicrob. Resist. Infect. Control. 2018;7:15. doi: 10.1186/s13756-018-0299-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Nakwatumbah S., Kibuule D., Godman B., Haakuria V., Kalemeera F., Baker A., Mubita M. Compliance to guidelines for the prescribing of antibiotics in acute infections at Namibia’s national referral hospital: A pilot study and the implications. Expert Rev. Anti-Infect. Ther. 2017;15:713–721. doi: 10.1080/14787210.2017.1320220. [DOI] [PubMed] [Google Scholar]
- 180.Dlamini N.N., Meyer J.C., Kruger D., Kurdi A., Godman B., Schellack N. Feasibility of using point prevalence surveys to assess antimicrobial utilisation in public hospitals in South Africa: A pilot study and implications. Hosp. Pract. 2019;47:88–95. doi: 10.1080/21548331.2019.1592880. [DOI] [PubMed] [Google Scholar]
- 181.Amdany H.K., Mcmillan M. Metronidazole intravenous formulation use in in-patients in Kapkatet District Hospital, Kenya: A best practice implementation project. JBI Evid. Synth. 2014;12:419–432. doi: 10.11124/jbisrir-2014-1381. [DOI] [Google Scholar]
- 182.Umar L.W., Isah A., Musa S., Umar B. Prescribing pattern and antibiotic use for hospitalized children in a Northern Nigerian Teaching Hospital. Ann. Afr. Med. 2018;17:26–32. doi: 10.4103/aam.aam_44_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Amaha N.D., Berhe Y.H., Kaushik A. Assessment of inpatient antibiotic use in Halibet National Referral Hospital using WHO indicators: A retrospective study. BMC Res. Notes. 2018;11:904. doi: 10.1186/s13104-018-4000-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.van den Bergh D., Messina A.P., Goff D.A., van Jaarsveld A., Coetzee R., de Wet Y., Bronkhorst E., Brink A., Mendelson M., Richards G.A., et al. A pharmacist-led prospective antibiotic stewardship intervention improves compliance to community-acquired pneumonia guidelines in 39 public and private hospitals across South Africa. Int. J. Antimicrob. Agents. 2020;56:106189. doi: 10.1016/j.ijantimicag.2020.106189. [DOI] [PubMed] [Google Scholar]
- 185.Niaz Q., Godman B., Campbell S., Kibuule D. Compliance to prescribing guidelines among public health care facilities in Namibia; findings and implications. Int. J. Clin. Pharm. 2020;42:1227–1236. doi: 10.1007/s11096-020-01056-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Maina M., Mwaniki P., Odira E., Kiko N., McKnight J., Schultsz C., English M., Tosas-Auguet O. Antibiotic use in Kenyan public hospitals: Prevalence, appropriateness and link to guideline availability. Int. J. Infect. Dis. 2020;99:10–18. doi: 10.1016/j.ijid.2020.07.084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Ayieko P., Irimu G., Ogero M., Mwaniki P., Malla L., Julius T., Chepkirui M., Mbevi G., Oliwa J., Agweyu A., et al. Effect of enhancing audit and feedback on uptake of childhood pneumonia treatment policy in hospitals that are part of a clinical network: A cluster randomized trial. Implement. Sci. 2019;14:20. doi: 10.1186/s13012-019-0868-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Suliman S.M., Yousef B.A., Hamadelnil A.A. Impact of guidelines implementation for the rational use of prophylactic antibiotics in elective cesarean sections at Elqutainah Teaching Hospital. J. Fam. Med. Prim. Care. 2020;9:162–167. doi: 10.4103/jfmpc.jfmpc_903_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Brink A.J., Messina A.P., Feldman C., Richards G.A., van den Bergh D. From guidelines to practice: A pharmacist-driven prospective audit and feedback improvement model for peri-operative antibiotic prophylaxis in 34 South African hospitals. J. Antimicrob. Chemother. 2017;72:1227–1234. doi: 10.1093/jac/dkw523. [DOI] [PubMed] [Google Scholar]
- 190.Sefah I.A., Essah D.O., Kurdi A., Sneddon J., Alalbila T.M., Kordorwu H., Godman B. Assessment of adherence to pneumonia guidelines and its determinants in an ambulatory care clinic in Ghana: Findings and implications for the future. JAC Antimicrob. Resist. 2021;3:dlab080. doi: 10.1093/jacamr/dlab080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Nambasa V., Ndagije H.B., Serwanga A., Manirakiza L., Atuhaire J., Nakitto D., Kiguba R., Figueras A. Prescription of Levofloxacin and Moxifloxacin in Select Hospitals in Uganda: A Pilot Study to Assess Guideline Concordance. Antibiotics. 2020;9:439. doi: 10.3390/antibiotics9080439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Junaid E., Jenkins L., Swanepoel H., North Z., Gould T. Antimicrobial stewardship in a rural regional hospital—Growing a positive culture. S. Afr. Med. J. 2018;108:546–550. doi: 10.7196/SAMJ.2018.v108i7.13149. [DOI] [PubMed] [Google Scholar]
- 193.Lester R., Haigh K., Wood A., MacPherson E.E., Maheswaran H., Bogue P., Hanger S., Kalizang’oma A., Srirathan V., Kulapani D., et al. Sustained Reduction in Third-generation Cephalosporin Usage in Adult Inpatients Following Introduction of an Antimicrobial Stewardship Program in a Large, Urban Hospital in Malawi. Clin. Infect. Dis. 2020;71:e478–e486. doi: 10.1093/cid/ciaa162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Ntumba P., Mwangi C., Barasa J., Aiken A., Kubilay Z., Allegranzi B. Multimodal approach for surgical site infection prevention—Results from a pilot site in Kenya. Antimicrob. Resist. Infect. Control. 2015;4:P87. doi: 10.1186/2047-2994-4-S1-P87. [DOI] [Google Scholar]
- 195.Allegranzi B., Aiken A.M., Kubilay N.Z., Nthumba P., Barasa J., Okumu G., Mugarura R., Elobu A.E., Jombwe J., Maimbo M., et al. A multimodal infection control and patient safety intervention to reduce surgical site infections in Africa: A multicentre, before-after, cohort study. Lancet Infect. Dis. 2018;18:507–515. doi: 10.1016/S1473-3099(18)30107-5. [DOI] [PubMed] [Google Scholar]
- 196.Chigome A.K., Matlala M., Godman B., Meyer J.C. Availability and Use of Therapeutic Interchange Policies in Managing Antimicrobial Shortages among South African Public Sector Hospitals; Findings and Implications. Antibiotics. 2020;9:4. doi: 10.3390/antibiotics9010004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Ngonzi J., Bebell L.M., Boatin A.A., Owaraganise A., Tiibajuka L., Fajardo Y., Lugobe H.M., Wylie B.J., Jacquemyn Y., Obua C., et al. Impact of an educational intervention on WHO surgical safety checklist and pre-operative antibiotic use at a referral hospital in southwestern Uganda. Int. J. Qual. Health Care. 2021;33:mzab089. doi: 10.1093/intqhc/mzab089. [DOI] [PubMed] [Google Scholar]
- 198.BSAC Antimicrobial Stewardship from Principles to Practice. 2018. [(accessed on 14 November 2022)]. Available online: https://www.bsac.org.uk/antimicrobialstewardshipebook/BSAC-AntimicrobialStewardship-FromPrinciplestoPractice-eBook.pdf.
- 199.Olaoye O., Tuck C., Khor W.P., McMenamin R., Hudson L., Northall M., Panford-Quainoo E., Asima D.M., Ashiru-Oredope D. Improving Access to Antimicrobial Prescribing Guidelines in 4 African Countries: Development and Pilot Implementation of an App and Cross-Sectional Assessment of Attitudes and Behaviour Survey of Healthcare Workers and Patients. Antibiotics. 2020;9:555. doi: 10.3390/antibiotics9090555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Abubakar U., Syed Sulaiman S.A., Adesiyun A.G. Impact of pharmacist-led antibiotic stewardship interventions on compliance with surgical antibiotic prophylaxis in obstetric and gynecologic surgeries in Nigeria. PLoS ONE. 2019;14:e0213395. doi: 10.1371/journal.pone.0213395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Curtis C.E., Al Bahar F., Marriott J.F. The effectiveness of computerised decision support on antibiotic use in hospitals: A systematic review. PLoS ONE. 2017;12:e0183062. doi: 10.1371/journal.pone.0183062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Zahlanie Y., Mang N.S., Lin K., Hynan L.S., Prokesch B.C. Improved Antibiotic Prescribing Practices for Respiratory Infections Through Use of Computerized Order Sets and Educational Sessions in Pediatric Clinics. Open Forum Infect. Dis. 2021;8:ofaa601. doi: 10.1093/ofid/ofaa601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Holstiege J., Mathes T., Pieper D. Effects of computer-aided clinical decision support systems in improving antibiotic prescribing by primary care providers: A systematic review. J. Am. Med. Inform. Assoc. 2015;22:236–242. doi: 10.1136/amiajnl-2014-002886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Sulis G., Sayood S., Katukoori S., Bollam N., George I., Yaeger L.H., Chavez M.A., Tetteh E., Yarrabelli S., Pulcini C., et al. Exposure to World Health Organization’s AWaRe antibiotics and isolation of multidrug resistant bacteria: A systematic review and meta-analysis. Clin. Microbiol. Infect. 2022;28:1193–1202. doi: 10.1016/j.cmi.2022.03.014. [DOI] [PubMed] [Google Scholar]
- 205.Charani E., Smith I., Skodvin B., Perozziello A., Lucet J.C., Lescure F.X., Birgand G., Poda A., Ahmad R., Singh S., et al. Investigating the cultural and contextual determinants of antimicrobial stewardship programmes across low-, middle- and high-income countries-A qualitative study. PLoS ONE. 2019;14:e0209847. doi: 10.1371/journal.pone.0209847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Kakkar A.K., Shafiq N., Singh G., Ray P., Gautam V., Agarwal R., Muralidharan J., Arora P. Antimicrobial Stewardship Programs in Resource Constrained Environments: Understanding and Addressing the Need of the Systems. Front. Public Health. 2020;8:140. doi: 10.3389/fpubh.2020.00140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Pokharel S., Raut S., Adhikari B. Tackling antimicrobial resistance in low-income and middle-income countries. BMJ Glob. Health. 2019;4:e002104. doi: 10.1136/bmjgh-2019-002104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Björkhem-Bergman L., Andersén-Karlsson E., Laing R., Diogene E., Melien O., Jirlow M., Malmström R.E., Vogler S., Godman B., Gustafsson L.L. Interface management of pharmacotherapy. Joint hospital and primary care drug recommendations. Eur. J. Clin. Pharmacol. 2013;69((Suppl. S1)):73–78. doi: 10.1007/s00228-013-1497-5. [DOI] [PubMed] [Google Scholar]
- 209.Yoon C.H., Ritchie S.R., Duffy E.J., Thomas M.G., McBride S., Read K., Chen R., Humphrey G. Impact of a smartphone app on prescriber adherence to antibiotic guidelines in adult patients with community acquired pneumonia or urinary tract infections. PLoS ONE. 2019;14:e0211157. doi: 10.1371/journal.pone.0211157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Eriksen J., Gustafsson L.L., Ateva K., Bastholm-Rahmner P., Ovesjö M.L., Jirlow M., Juhasz-Haverinen M., Lärfars G., Malmström R.E., Wettermark B., et al. High adherence to the ‘Wise List’ treatment recommendations in Stockholm: A 15-year retrospective review of a multifaceted approach promoting rational use of medicines. BMJ Open. 2017;7:e014345. doi: 10.1136/bmjopen-2016-014345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Gustafsson L.L., Wettermark B., Godman B., Andersén-Karlsson E., Bergman U., Hasselström J., Hensjö L.-O., Hjemdahl P., Jägre I., Julander M., et al. The ‘wise list’- a comprehensive concept to select, communicate and achieve adherence to recommendations of essential drugs in ambulatory care in Stockholm. Basic Clin. Pharmacol. Toxicol. 2011;108:224–233. doi: 10.1111/j.1742-7843.2011.00682.x. [DOI] [PubMed] [Google Scholar]
- 212.Foxlee N.D., Townell N., Heney C., McIver L., Lau C.L. Strategies Used for Implementing and Promoting Adherence to Antibiotic Guidelines in Low- and Lower-Middle-Income Countries: A Systematic Review. Trop. Med. Infect. Dis. 2021;6:166. doi: 10.3390/tropicalmed6030166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Commonwealth Partnerships for Antimicrobial Stewardship Programme (CwPAMS) CwPAMS Antimicrobial Prescribing App—Antimicrobial Stewardship Mobile Application. [(accessed on 15 November 2022)]. Available online: https://commonwealthpharmacy.org/cwpams-ams-app/
- 214.Mashaba T.P., Matlala M., Godman B., Meyer J.C. Implementation and monitoring of decisions by pharmacy and therapeutics committees in South African public sector hospitals. Expert Rev. Clin. Pharmacol. 2019;12:159–168. doi: 10.1080/17512433.2018.1545572. [DOI] [PubMed] [Google Scholar]
- 215.Matlala M., Gous A.G.S., Meyer J.C., Godman B. Formulary Management Activities and Practice Implications Among Public Sector Hospital Pharmaceutical and Therapeutics Committees in a South African Province. Front. Pharmacol. 2020;11:1267. doi: 10.3389/fphar.2020.01267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Fadare J.O., Ogunleye O., Obiako R., Orubu S., Enwere O., Ajemigbitse A.A., Meyer J.C., Enato E., Massele A., Godman B., et al. Drug and therapeutics committees in Nigeria: Evaluation of scope and functionality. Expert Rev. Clin. Pharmacol. 2018;11:1255–1262. doi: 10.1080/17512433.2018.1549488. [DOI] [PubMed] [Google Scholar]
- 217.Zulu A., Matafwali S.K., Banda M., Mudenda S. Assessment of knowledge, attitude and practices on antibiotic resistance among undergraduate medical students in the school of medicine at the University of Zambia. Int. J. Basic Clin. Pharmacol. 2020;9:263–270. doi: 10.18203/2319-2003.ijbcp20200174. [DOI] [Google Scholar]
- 218.Nisabwe L., Brice H., Umuhire M.C., Gwira O., Harelimana J.D.D., Nzeyimana Z., Sebatunzi O.R., Rusingiza E.K., Hahirwa I., Muvunyi C.M. Knowledge and attitudes towards antibiotic use and resistance among undergraduate healthcare students at University of Rwanda. J. Pharm. Policy Pract. 2020;13:7. doi: 10.1186/s40545-020-00207-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Wasserman S., Potgieter S., Shoul E., Constant D., Stewart A., Mendelson M., Boyles T.H. South African medical students’ perceptions and knowledge about antibiotic resistance and appropriate prescribing: Are we providing adequate training to future prescribers? S. Afr. Med. J. 2017;107:405–410. doi: 10.7196/SAMJ.2017.v107i5.12370. [DOI] [PubMed] [Google Scholar]
- 220.Lubwama M., Onyuka J., Ayazika K.T., Ssetaba L.J., Siboko J., Daniel O., Mushi M.F. Knowledge, attitudes, and perceptions about antibiotic use and antimicrobial resistance among final year undergraduate medical and pharmacy students at three universities in East Africa. PLoS ONE. 2021;16:e0251301. doi: 10.1371/journal.pone.0251301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Etando A., Amu A.A., Haque M., Schellack N., Kurdi A., Alrasheedy A.A., Timoney A., Mwita J.C., Rwegerera G.M., Patrick O., et al. Challenges and Innovations Brought about by the COVID-19 Pandemic Regarding Medical and Pharmacy Education Especially in Africa and Implications for the Future. Healthcare. 2021;9:1722. doi: 10.3390/healthcare9121722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Sithole T., Mahlangu G., Walker S., Salek S. Regulatory Authority Evaluation of the Effectiveness and Efficiency of the ZaZiBoNa Collaborative Medicines Registration Initiative: The Way Forward. Front. Med. 2022;9:898743. doi: 10.3389/fmed.2022.898743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.WHO Launch of the Lomé Initiative. 2020. [(accessed on 14 November 2022)]. Available online: https://www.who.int/dg/speeches/detail/launch-of-the-lom%C3%A9-initiative.
- 224.Africa Centres for Disease Control and Prevention and Center for Disease Dynamics, Economics & Policy African Antibiotic Treatment Guidelines for Common Bacterial Infections and Syndromes—Recommended Antibiotic Treatments in Adult Patients. 2021. [(accessed on 15 November 2022)]. Available online: https://africaguidelines.cddep.org/wp-content/uploads/2021/11/Quick-Reference-Guide_Adults_English.pdf.
- 225.GASPH Global Antimicrobial Stewardship Partnership Hub. 2022. [(accessed on 15 November 2022)]. Available online: https://global-asp-hub.com/
- 226.Lorencatto F., Charani E., Sevdalis N., Tarrant C., Davey P. Driving sustainable change in antimicrobial prescribing practice: How can social and behavioural sciences help? J. Antimicrob. Chemother. 2018;73:2613–2624. doi: 10.1093/jac/dky222. [DOI] [PubMed] [Google Scholar]
- 227.Schellack N., Bronkhorst E., Coetzee R., Godman B., Gous A.G.S., Kolman S., Labuschagne Q., Malan L., Messina A.P., Naested C., et al. SASOCP position statement on the pharmacist’s role in antibiotic stewardship 2018. S. Afr. J. Infect. Dis. 2018;33:28–35. doi: 10.4102/sajid.v33i1.24. [DOI] [Google Scholar]
- 228.Ogunleye O.O., Fadare J.O., Yinka-Ogunleye A.F., Anand Paramadhas B.D., Godman B. Determinants of antibiotic prescribing among doctors in a Nigerian urban tertiary hospital. Hosp. Pract. 2019;47:53–58. doi: 10.1080/21548331.2018.1475997. [DOI] [PubMed] [Google Scholar]
- 229.Fadare J.O., Bankole I., Babatola A., Simeon Olatunya O., Aina F., Godman B. Adherence to WHO Criteria on Drug Promotion Literature: An Exploratory Study from a Tertiary Healthcare Facility in South-West Nigeria. Hosp. Pharm. 2022:00185787221123217. doi: 10.1177/00185787221123217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Modisakeng C., Matlala M., Godman B., Meyer J.C. Medicine shortages and challenges with the procurement process among public sector hospitals in South Africa; findings and implications. BMC Health Serv. Res. 2020;20:234. doi: 10.1186/s12913-020-05080-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Fürst J., Čižman M., Mrak J., Kos D., Campbell S., Coenen S., Gustafsson L.L., Fürst L., Godman B. The influence of a sustained multifaceted approach to improve antibiotic prescribing in Slovenia during the past decade: Findings and implications. Expert Rev. Anti-Infect. Ther. 2015;13:279–289. doi: 10.1586/14787210.2015.990381. [DOI] [PubMed] [Google Scholar]
- 232.O’Neill J. Tackling Drug-Resistant Infections Globally: Final Report and Recommendations. 2016. [(accessed on 14 November 2022)]. Available online: https://amr-review.org/sites/default/files/160518_Final%20paper_with%20cover.pdf.
- 233.Sartelli M., Hardcastle T.C., Catena F., Chichom-Mefire A., Coccolini F., Dhingra S., Haque M., Hodonou A., Iskandar K., Labricciosa F., et al. Antibiotic Use in Low and Middle-Income Countries and the Challenges of Antimicrobial Resistance in Surgery. Antibiotics. 2020;9:497. doi: 10.3390/antibiotics9080497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Tadesse B.T., Ashley E.A., Ongarello S., Havumaki J., Wijegoonewardena M., González I.J., Dittrich S. Antimicrobial resistance in Africa: A systematic review. BMC Infect. Dis. 2017;17:616. doi: 10.1186/s12879-017-2713-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Bell B.G., Schellevis F., Stobberingh E., Goossens H., Pringle M. A systematic review and meta-analysis of the effects of antibiotic consumption on antibiotic resistance. BMC Infect. Dis. 2014;14:13. doi: 10.1186/1471-2334-14-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Llor C., Bjerrum L. Antimicrobial resistance: Risk associated with antibiotic overuse and initiatives to reduce the problem. Ther. Adv. Drug Saf. 2014;5:229–241. doi: 10.1177/2042098614554919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Collignon P., Beggs J.J., Walsh T.R., Gandra S., Laxminarayan R. Anthropological and socioeconomic factors contributing to global antimicrobial resistance: A univariate and multivariable analysis. Lancet Planet. Health. 2018;2:e398–e405. doi: 10.1016/S2542-5196(18)30186-4. [DOI] [PubMed] [Google Scholar]
- 238.WHO WHO Methodology for Point Prevalence Survey on Antibiotic Use in Hospitals, Version 1.1. 2018. [(accessed on 14 November 2022)]. Available online: https://www.who.int/publications/i/item/WHO-EMP-IAU-2018.01.
- 239.Engler D., Meyer J.C., Schellack N., Kurdi A., Godman B. Compliance with South Africa’s Antimicrobial Resistance National Strategy Framework: Are we there yet? J. Chemother. 2021;33:21–31. doi: 10.1080/1120009X.2020.1789389. [DOI] [PubMed] [Google Scholar]
- 240.de Wit T.F.R., Janssens W., Antwi M., Milimo E., Mutegi N., Marwa H., Ndili N., Owino W., Waiyaiya E., Garcia Roja D.C., et al. Digital health systems strengthening in Africa for rapid response to COVID-19. Front. Health Serv. 2022;2:2035–2043. doi: 10.3389/frhs.2022.987828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Godman B., Grobler C., Van-De-Lisle M., Wale J., Barbosa W.B., Massele A., Opondo P., Petrova G., Tachkov K., Sefah I., et al. Pharmacotherapeutic interventions for bipolar disorder type II: Addressing multiple symptoms and approaches with a particular emphasis on strategies in lower and middle-income countries. Expert Opin. Pharmacother. 2019;20:2237–2255. doi: 10.1080/14656566.2019.1684473. [DOI] [PubMed] [Google Scholar]
- 242.Ogunleye O.O., Basu D., Mueller D., Sneddon J., Seaton R.A., Yinka-Ogunleye A.F., Wamboga J., Miljković N., Mwita J.C., Rwegerera G.M., et al. Response to the Novel Corona Virus (COVID-19) Pandemic Across Africa: Successes, Challenges, and Implications for the Future. Front. Pharmacol. 2020;11:1205. doi: 10.3389/fphar.2020.01205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Godman B., Haque M., Abubakar A.R., Ogunleye O.O., Sani I.H., Sefah I., Kurdi A., Islam S. Changes in Availability, Utilization, and Prices of Medicines and Protection Equipment for COVID-19 in an Urban Population of Northern Nigeria. J. Res. Pharm. Pract. 2021;10:17–22. doi: 10.4103/jrpp.JRPP_20_92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Godman B., Basu D., Pillay Y., Mwita J.C., Rwegerera G.M., Paramadhas B.D.A., Tiroyakgosi C., Okwen P.M., Niba L.L., Nonvignon J., et al. Review of Ongoing Activities and Challenges to Improve the Care of Patients With Type 2 Diabetes Across Africa and the Implications for the Future. Front. Pharmacol. 2020;11:108. doi: 10.3389/fphar.2020.00108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Godman B., Basu D., Pillay Y., Almeida P.H.R.F., Mwita J.C., Rwegerera G.M., Paramadhas B.D.A., Tiroyakgosi C., Patrick O., Niba L.L., et al. Ongoing and planned activities to improve the management of patients with Type 1 diabetes across Africa; implications for the future. Hosp. Pract. 2020;48:51–67. doi: 10.1080/21548331.2020.1745509. [DOI] [PubMed] [Google Scholar]
- 246.Gad M., Salem A., Oortwijn W., Hill R., Godman B. Mapping of Current Obstacles for Rationalizing Use of Medicines (CORUM) in Europe: Current Situation and Potential Solutions. Front. Pharmacol. 2020;11:144. doi: 10.3389/fphar.2020.00144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Saleem Z., Hassali M.A., Godman B., Versporten A., Hashmi F.K., Saeed H., Saleem F., Salman M., Rehman I.U., Khan T.M. Point prevalence surveys of antimicrobial use: A systematic review and the implications. Expert Rev. Anti-Infect. Ther. 2020;18:897–910. doi: 10.1080/14787210.2020.1767593. [DOI] [PubMed] [Google Scholar]
- 248.WHO Anatomical Therapeutic Chemical (ATC) Classification. 2021. [(accessed on 10 November 2022)]. Available online: https://www.who.int/tools/atc-ddd-toolkit/atc-classification.
- 249.Wettermark B., Godman B., Jacobsson B., Haaijer-Ruskamp F.M. Soft regulations in pharmaceutical policy making: An overview of current approaches and their consequences. Appl. Health Econ. Health Policy. 2009;7:137–147. doi: 10.1007/BF03256147. [DOI] [PubMed] [Google Scholar]
- 250.Matsitse T.B., Helberg E., Meyer J.C., Godman B., Massele A., Schellack N. Compliance with the primary health care treatment guidelines and the essential medicines list in the management of sexually transmitted infections in correctional centres in South Africa: Findings and implications. Expert Rev. Anti-Infect. Ther. 2017;15:963–972. doi: 10.1080/14787210.2017.1382354. [DOI] [PubMed] [Google Scholar]
- 251.Alrasheedy A.A., Alsalloum M.A., Almuqbil F.A., Almuzaini M.A., Aba Alkhayl B.S., Albishri A.S., Alharbi F.F., Alharbi S.R., Alodhayb A.K., Alfadl A.A., et al. The impact of law enforcement on dispensing antibiotics without prescription: A multi-methods study from Saudi Arabia. Expert Rev. Anti-Infect. Ther. 2020;18:87–97. doi: 10.1080/14787210.2020.1705156. [DOI] [PubMed] [Google Scholar]
- 252.Mendelson M., Brink A., Gouws J., Mbelle N., Naidoo V., Pople T., Schellack N., van Vuuren M., Rees H., Banoo S., et al. The One Health stewardship of colistin as an antibiotic of last resort for human health in South Africa. Lancet Infect. Dis. 2018;18:e288–e294. doi: 10.1016/S1473-3099(18)30119-1. [DOI] [PubMed] [Google Scholar]
- 253.Godman B., McCabe H., Leong T.D., Mueller D., Martin A.P., Hoxha I., Mwita J.C., Rwegerera G.M., Massele A., Costa J.D.O., et al. Fixed dose drug combinations—are they pharmacoeconomically sound? Findings and implications especially for lower- and middle-income countries. Expert Rev. Pharmacoecon. Outcomes Res. 2020;20:1–26. doi: 10.1080/14737167.2020.1734456. [DOI] [PubMed] [Google Scholar]
- 254.Godman B., Wettermark B., van Woerkom M., Fraeyman J., Alvarez-Madrazo S., Berg C., Bishop I., Bucsics A., Campbell S., Finlayson A.E., et al. Multiple policies to enhance prescribing efficiency for established medicines in Europe with a particular focus on demand-side measures: Findings and future implications. Front. Pharmacol. 2014;5:106. doi: 10.3389/fphar.2014.00106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.WHO Monitoring the Building Blocks of Health Systems: A Handbook of Indicators and Their Measurement Strategies. 2010. [(accessed on 10 November 2022)]. Available online: https://apps.who.int/iris/bitstream/handle/10665/258734/9789241564052-eng.pdf.
- 256.Campbell S.M., Roland M.O., Buetow S.A. Defining quality of care. Soc. Sci. Med. 2000;51:1611–1625. doi: 10.1016/S0277-9536(00)00057-5. [DOI] [PubMed] [Google Scholar]
- 257.NHS England and NHS Improvement A Model for Measuring Quality Care. 2022. [(accessed on 10 November 2022)]. Available online: https://www.england.nhs.uk/wp-content/uploads/2022/02/qsir-measuring-quality-care.pdf.
- 258.van den Bosch C.M., Hulscher M.E., Natsch S., Wille J., Prins J.M., Geerlings S.E. Applicability of generic quality indicators for appropriate antibiotic use in daily hospital practice: A cross-sectional point-prevalence multicenter study. Clin. Microbiol. Infect. 2016;22:888.e1–888.e9. doi: 10.1016/j.cmi.2016.07.011. [DOI] [PubMed] [Google Scholar]
- 259.van den Bosch C.M., Geerlings S.E., Natsch S., Prins J.M., Hulscher M.E. Quality indicators to measure appropriate antibiotic use in hospitalized adults. Clin. Infect. Dis. 2015;60:281–291. doi: 10.1093/cid/ciu747. [DOI] [PubMed] [Google Scholar]
- 260.Kallen M.C., Prins J.M. A Systematic Review of Quality Indicators for Appropriate Antibiotic Use in Hospitalized Adult Patients. Infect. Dis. Rep. 2017;9:6821. doi: 10.4081/idr.2017.6821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Wambale J.M.I.J., Mathe D.M., Kavuo S.K., Kikuni T. Point prevalence study of antibiotic use in hospitals in Butembo. Int. J. Med. Med. Sci. 2016;8:133–139. [Google Scholar]
- 262.Labi A.K., Obeng-Nkrumah N., Sunkwa-Mills G., Bediako-Bowan A., Akufo C., Bjerrum S., Owusu E., Enweronu-Laryea C., Opintan J.A., Kurtzhals J.A.L., et al. Antibiotic prescribing in paediatric inpatients in Ghana: A multi-centre point prevalence survey. BMC Pediatr. 2018;18:391. doi: 10.1186/s12887-018-1367-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Garcia-Vello P., Brobbey F., Gonzalez-Zorn B., Setsoafia Saba C.K. A cross-sectional study on antibiotic prescription in a teaching hospital in Ghana. Pan Afr. Med. J. 2020;35:12. doi: 10.11604/pamj.2020.35.12.18324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Umeokonkwo C.D., Madubueze U.C., Onah C.K., Okedo-Alex I.N., Adeke A.S., Versporten A., Goossens H., Igwe-Okomiso D., Okeke K., Azuogu B.N., et al. Point prevalence survey of antimicrobial prescription in a tertiary hospital in South East Nigeria: A call for improved antibiotic stewardship. J. Glob. Antimicrob. Resist. 2019;17:291–295. doi: 10.1016/j.jgar.2019.01.013. [DOI] [PubMed] [Google Scholar]
- 265.Chioma O. Rational Use of Antibiotics—A Point Prevalence Study Carried out at a Tertiary Hospital in South-South Nigeria. Int. J. Trop. Dis. Health. 2020;41:39–47. doi: 10.9734/ijtdh/2020/v41i1430352. [DOI] [Google Scholar]
- 266.Masich A.M., Vega A.D., Callahan P., Herbert A., Fwoloshi S., Zulu P.M., Chanda D., Chola U., Mulenga L., Hachaambwa L., et al. Antimicrobial usage at a large teaching hospital in Lusaka, Zambia. PLoS ONE. 2020;15:e0228555. doi: 10.1371/journal.pone.0228555. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Additional data are available on reasonable request from the corresponding author. However, all informational sources and papers have been extensively referenced. References [255,256,257,258,259,260,261,262,263,264,265,266] are cited in Supplementary Materials file.