Abstract
Reverse genetic systems are widely used to engineer recombinant viruses with desired mutations. In response to the COVID-19 pandemic, four types of reverse genetic systems have been developed for SARS-CoV-2: (i) a full-length infectious clone that can be used to prepare recombinant SARS-CoV-2 at biosafety level 3 (BSL3), (ii) a trans-complementation system that can be used to produce single-round infectious SARS-CoV-2 at BSL2, (iii) an attenuated SARS-CoV-2 vaccine candidate (with deletions of viral accessory genes) that may be developed for veterinary use as well as for antiviral screening at BSL2, and (iv) replicon systems with deletions of viral structural genes that can be used at BSL2. Each of these genetic systems has its advantages and disadvantages that can be used to address different questions for basic and translational research. Due to the long genomic size and bacteria-toxic sequences of SARS-CoV-2, several experimental approaches have been established to rescue recombinant viruses and replicons, including (i) in vitro DNA ligation, (ii) bacterial artificial chromosome (BAC) system, (iii) yeast artificial chromosome (YAC) system, and (iv) circular polymerase extension reaction (CPER). This review summarizes the current status of SARS-CoV-2 genetic systems and their applications for studying viral replication, pathogenesis, vaccines, and therapeutics.
1. Introduction
The ongoing global pandemic of coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has resulted in a significant crisis around the world, with more than 600 million infections and greater than 6.5 million deaths as of November 2022 (https://covid19.who.int/). In response to the pandemic, tremendous efforts from industry, government, and academia, has devoted to developing vaccines and therapeutics at lightning speed. Within a year, mRNA vaccines from Pfizer/BioNTech and Moderna were approved for emergency use in the USA, the fastest of any previously developed vaccines (Ball, 2021; Walsh et al., 2020). Such progress has been attributed to the development and implementation of numerous experimental platforms. Among them, reverse genetic systems for engineering recombinant SARS-CoV-2 have played a significant role in facilitating the development of the first-generation vaccines and therapeutics.
SARS-CoV-2 belongs to the Coronaviridae virus family in the order of Nidovirales. Besides SARS-CoV-2, several other coronaviruses can cause infections and diseases in humans, including Severe acute respiratory syndrome coronavirus (SARS-CoV), Middle East respiratory syndrome coronavirus (MERS-CoV), and four common cold coronaviruses, such as 229E, NL63, OC43, and HKU1. Coronaviruses are positive-sense single-strand RNA viruses with the largest viral genomes, ranging from 26.4 to 31.7 kb (V'Kovski et al., 2021). Like other positive-sense single-strand RNA viruses, the SARS-CoV-2 genome is flanked by 5′ and 3′ untranslated regions (UTR) that contain cis-acting secondary RNA structures essential for RNA synthesis. It contains a 5′ cap and a 3′ poly (A)-tail (Fig. 1 A). The first two-thirds of the viral genome from the 5′-end encodes open-reading-frame 1a (ORF1a) and ORF1b which are translated into two polyproteins (pp1a and pp1b) by cellular translational machinery. These two polyproteins are further processed by two viral proteases, papain-like protease (PLpro) and main-protease (Mpro) into sixteen nonstructural proteins Nsp1-Nsp16. These nonstructural proteins form the replication complex where viral RNA synthesis takes place. One-third of the 3′ terminal genome encodes four structural proteins spike (S), membrane (M), envelope (E), and nucleocapsid (N), as well as several accessory proteins ORF3a, ORF6, ORF7a, ORF7b, and ORF8, as well as potentially ORF3b and ORF9b (Hu et al., 2021; V'Kovski et al., 2021). The structural proteins make up the virion, and the accessory proteins modulate the host response to facilitate viral infection and pathogenesis (Kee et al., 2022; V'Kovski et al., 2021; Xia et al., 2020).
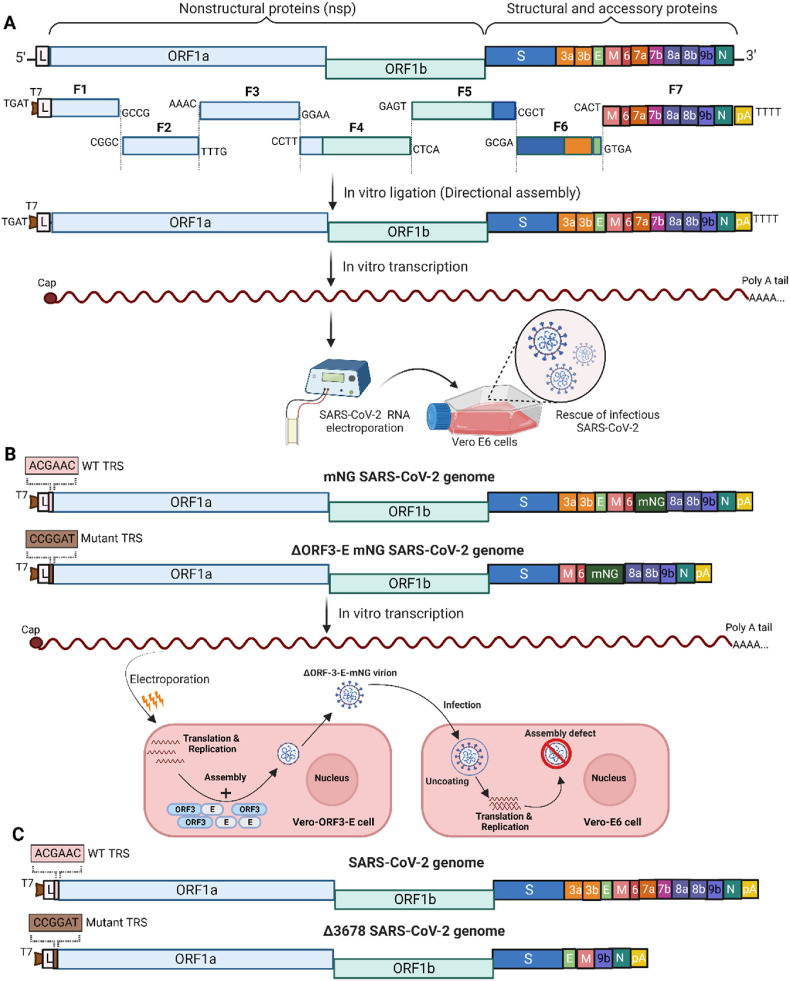
Fig. 1.
Diagrams for an infectious cDNA clone, a trans complementary genetic system, and a live attenuated SARS-CoV-2. (A) An in vitro ligation approach for making recombinant SARS-CoV-2. The genome structure of SARS-CoV-2 with the approach of in vitro ligation is shown. Approximate genome locations of the cohesive overhangs are indicated. Length is not to scale. The full-length cDNA of SARS-CoV-2 was directionally assembled using in vitro ligation. The full-length genomic cDNA is flanked by a T7 promoter (T7) on the 5′ end and a polyA tail on the 3′ end. The assembled full-length cDNA was in vitro transcribed to genomic RNA which is electroporated into Vero E6 cells to rescue recombinant SARS-CoV-2. (B) A trans complementation system of SARS-CoV-2. The genome structures of full-length mNG SARS-CoV-2 and trans complement ΔORF3-E mNG SARS-CoV-2 are shown. Wild-type (WT) and a mutant transcriptional regulatory sequence (TRS) are shown. Electroporation of in vitro transcribed RNA leads to its replication and translation followed by assembly with the help of ORF3 and E protein expressed in trans in the ORF3-E Vero E6 cells. ΔORF3-E mNG SARS-CoV-2 can lead to a single round of infection in Vero E6 cells. (C) Attenuated Δ3678 SARS-CoV-2. The genome structure of SARS-CoV-2 with WT TRS, Δ3678 SARS-CoV-2 with mutant TRS sequence and deletion of ORF3, 6, 7, and 8 are shown. T7, T7 promoter; L, leader sequence; TRS, transcription regulatory sequences; ORF, open-reading frame; E, envelope glycoprotein gene; M, membrane glycoprotein gene; N, nucleocapsid gene; pA, poly-A tails. Figures adapted and modified from (Liu et al., 2022c; Xie et al., 2020a; Zhang et al., 2021a).
A reverse genetic system is one of the most powerful tools in molecular virology by which the infectious recombinant virus can be genetically manipulated from a complementary DNA (cDNA) clone of the viral genome. However, the assembly of full-length cDNA clones for Coronavirus has remained challenging due to the large viral genome, the presence of bacteria-toxic elements, cryptic transcription, splicing, recombination, and/or termination signals, which often result in deleterious mutations and/or deletions (Almazan et al., 2014; Aubry et al., 2015). Before the full-length infectious cDNA clones were established, the initial reverse genetic system for CoV was generated based on the targeted RNA recombination strategy, which takes advantage of the high rate of homologous RNA recombination in CoVs (Baric et al., 1990; Kusters et al., 1990; Makino et al., 1986; Masters, 1999). However, this approach relies on viral replication, and the requirement of virus passage, which limits its ability to easily manipulate mutations across the entire genome, particularly the replication-related genes or lethal mutations (Almazan et al., 2014). During the past two decades, with the advance in modern molecular tools/reagents (restriction enzymes, high fidelity polymerase, and bacterial/yeast artificial chromosome), several creative approaches, including in vitro ligation (Scobey et al., 2013; Yount et al., 2000, 2002, 2003), bacterial/yeast artificial chromosomes (Almazan et al., 2000; Gonzalez et al., 2002), and circular polymerase extension reaction (Edmonds et al., 2013), have been taken to successfully generate infectious clones of positive-sense RNA viruses. Leveraging on the accumulated knowledge and expertise, the reverse genetic systems of SARS-CoV-2 have been rapidly established after the outbreak. In this minireview, we summarize current strategies for manipulating the infectious cDNA clones of SARS-CoV-2, which must be rescued at biosafety level 3 (BSL3). We then discuss three types of SARS-CoV-2 reverse genetic systems that can be adapted for use at BSL2, including a trans-complementation system, an attenuated SARS-CoV-2 vaccine candidate, and a replicon system. Those BSL2-adapted systems greatly expanded the accessibility to many researchers. We also compare the pros and cons of each system, highlighting their utilities in coronavirus biology and countermeasure development.
2. In vitro ligation-based SARS-CoV-2 reverse genetic system
The in vitro ligation-based strategy is to ligate multiple cDNA fragments of viral genome by DNA ligase into a full-length cDNA in vitro, which is used further as a template for synthesizing viral RNA by using RNA polymerases, such as T7 or SP6 polymerase. The divided cDNA fragments can be obtained through chemical synthesis, high-fidelity polymerase chain reaction (PCR) or plasmids propagated in E. coli. By eliminating the step of propagating the full-length cDNA in bacteria, gene toxicity can be minimized and authentic viral sequences can be obtained. This approach was first introduced by Rice et al. to make the recombinant yellow fever virus (Rice et al., 1989). Since then, this approach has also been widely used for generating full-length infectious clones of many other RNA viruses, including coronaviruses (Becker et al., 2008; Curtis et al., 2002; Yount et al., 2003).
Upon SARS-CoV-2 outbroke, we and others have adopted this old “trick” to directionally assemble the full-length cDNA of the SARS-CoV-2 strain 2019-nCoV/USA_WA1/2020, which was isolated from the first imported SARS-CoV-2 case in the USA (Hou et al., 2020; Xie et al., 2020a). Fig. 1A outlines the rationale and construction process. Seven consecutive fragments covering the entire SARS-CoV-2 genome were obtained through reverse transcribed (RT)-PCR from the viral genome or chemical synthesis. Two class IIS restriction endonucleases BsaI or Esp3I were used because they can recognize asymmetric DNA sequences, cleave outside their recognition sequences, and generate unique cohesive overhangs. The unique cohesive ends of each fragment ensured a one-directional, seamless assembly of the seven fragments with the concomitant loss of the restriction enzyme sites. A T7 promoter and a poly (A) tail of 29 bases were engineered at the 5′ and 3′ end of the viral genome, respectively. The ligated full-length DNA was used as a template for in vitro transcription by T7 RNA polymerase, resulting in 5′ capped and 3' polyadenylated full-length RNAs. Electroporation of these RNA transcripts into Vero E6 cells led to the rescue of recombinant SARS-CoV-2. Co-electroporation with the nucleocapsid RNA of SARS-CoV-2 is often used to increase the efficiency of rescuing coronaviruses (Curtis et al., 2002; Yount et al., 2002, 2003). Recovered infectious viruses resembled the clinical isolate 2019-nCoV/USA_WA1/2020 in forming plaque sizes and replication kinetics in cell culture. Using this infectious clone system, we have systematically addressed several aspects of CoV, including the functional characterization of mutations in Spike (Johnson et al., 2021; Liu et al., 2021, 2022bLiu et al., 2022b; Liu et al., 2021; Plante et al., 2021), nucleocapsid (Johnson et al., 2022), and accessory proteins (Kee et al., 2022). Also, our system was used to develop a mouse-adapted SARS-CoV-2 for in vivo studies (Muruato et al., 2021).
Moreover, using the same approach, fluorescent reporter (e.g. green fluorescent protein gene, mNG) or luciferase genes (e.g. Nanoluciferase, Nluc) were purposely engineered in place of ORF7 to generate reporter SARS-CoV-2 (Xie et al., 2020a, 2020b, 2021), which has been used extensively for neutralization studies of vaccinated or convalescent sera (Kurhade et al., 2022; Xia et al., 2022; Zou et al., 2022a, 2022b) and antiviral screening (Xie et al., 2020b). Using the mNG SARS-CoV-2, we discovered several monoclonal antibodies against SARS-CoV-2 and variants of concern (Fang et al., 2022; Ku et al., 2021a, 2021b, 2022). Using the Nanoluciferase SARS-CoV-2, we identified chloroquine, remdesivir, nelfinavir, rupintrivir, and cobicistat as the most selective inhibitors (Xie et al., 2020b). In vitro ligation can overcome the difficulty of propagation of viral genome in bacteria, and has very robustness in rescuing recombinant viruses. However, this approach requires intensive labor and good techniques in DNA and RNA preparation in vitro.
3. Bacterial artificial chromosome-based SARS-CoV-2 reverse genetic system
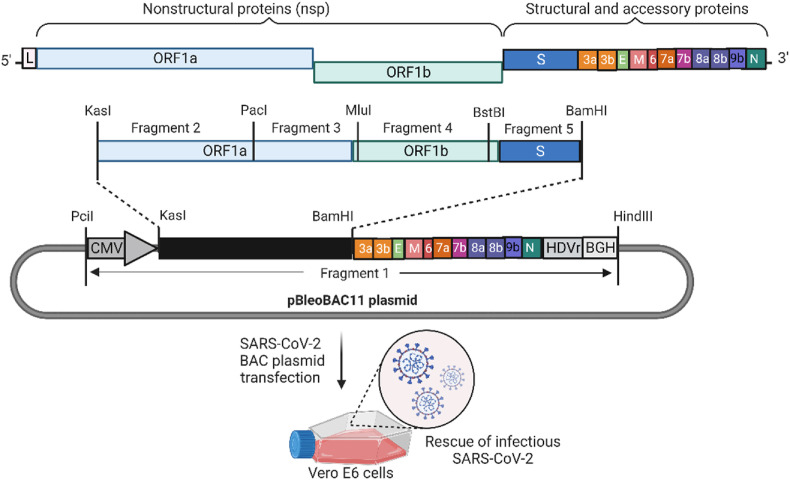
Bacterial artificial chromosome (BAC)-derived plasmids are circular self-replicating vectors capable of carrying inserts of up to 300 kb of DNA sequence. It is suitable for cloning DNA fragments in large sizes (Shizuya et al., 1992). In this system, a synthetic low-copy-number BAC plasmid containing the strictly replication-controlled Escherichia coli F-factor was used to propagate the viral genome (Shizuya et al., 1992). During propagation in E. coli cells, only one or two copies of BAC plasmids maintain per cell, which stabilizes the large DNA insertions and minimizes the CoV sequence-associated toxicity (Adler et al., 2003). This BAC plasmid-based reverse genetic system has been previously established for other coronaviruses including SARS, MERS and HCoV-OC43 (Almazan et al., 2006, 2013; St-Jean et al., 2006). Unlike the in vitro ligation approach, the BAC system could allow the propagation of the full-length cDNA of the viral genome in a single plasmid. Further, by coupling with the cytomegalovirus (CMV) immediate-early promoter, the BAC can launch viral RNA transcription in permissive cells after transfection, eliminating the RNA preparation steps. Using this approach, multiple DNA fragments of the SARS-CoV-2 genome have been successfully assembled into the BAC plasmid vector using standard molecular biology techniques with unique restriction enzymes (Chiem et al., 2021; Jin et al., 2021; Ye et al., 2020) (Fig. 2 ). In these SARS-CoV-2 infectious cDNA clones, the CMV promoter is added to the 5′ end of the SARS-CoV-2 genome. To ensure the correct processing of viral RNA, the Hepatitis Delta virus ribozyme (HDVr) and bovine growth hormone (BGH) or Simian virus (SV40) terminator sequence is engineered at the 3' terminus of the viral genome. Upon transfection into Vero E6 cells, the full-length SARS-CoV-2 RNA is synthesized by the cellular RNA polymerase II, leading to the rescue of recombinant SARS-CoV-2 (Ye et al., 2020). The recovered SARS-CoV-2 from the BAC system also exhibited similar growth properties and plaque sizes in cell culture as those of the natural SARS-CoV-2 isolate (Chiem et al., 2021; Jin et al., 2021; Ye et al., 2020). Alternatively, by using a T7 promoter, the BAC system can be used to generate full-length viral RNAs in vitro, allowing recovering recombinant SARS-CoV-2 after viral RNA transfection (Fahnoe et al., 2022). Similarly, Chiem et al., and Rihn et al., generated reporter SARS-CoV-2 using BAC plasmid by engineering a fluorescent reporter (Venus or mCherry) or luciferase gene (Nanoluciferase) at ORF7, allowing the development of the high throughput assays for antiviral screening (Chiem et al., 2021; Rihn et al., 2021). Manipulation of the BAC-based reverse genetic systems is relatively simple. However, viral gene-associated toxicity in bacteria during mutagenesis studies is unpredictable. The whole viral sequence in the plasmid should be confirmed by sequencing every time to avoid undesired mutations during propagation in bacteria.
Fig. 2.
BAC-derived SARS-CoV-2 reverse genetic system. The genome structure of SARS-CoV-2 followed by genome fragments with indicated restriction sites used for cloning the entire viral genome in pBeloBAC11 plasmid is shown. Length is not to scale. The Complete viral genome was covered by six fragments. The 5′ end of viral genome was flanked by the CMV promoter and the 3′ end by HDVr and BGH. Transfection of SARS-CoV-2 BAC plasmid into Vero E6 cells leads to the rescue of infectious SARS-CoV-2. ORF, open-reading frame; E, envelope glycoprotein gene; M, membrane glycoprotein gene; N, nucleocapsid gene; CMV, Cytomegalovirus promoter; HDVr, hepatitis delta virus ribozyme; BGH, bovine growth hormone termination and polyadenylation sequences. Figure adapted and modified from (Ye et al., 2020).
4. Yeast artificial chromosome-based SARS-CoV-2 reverse genetic system
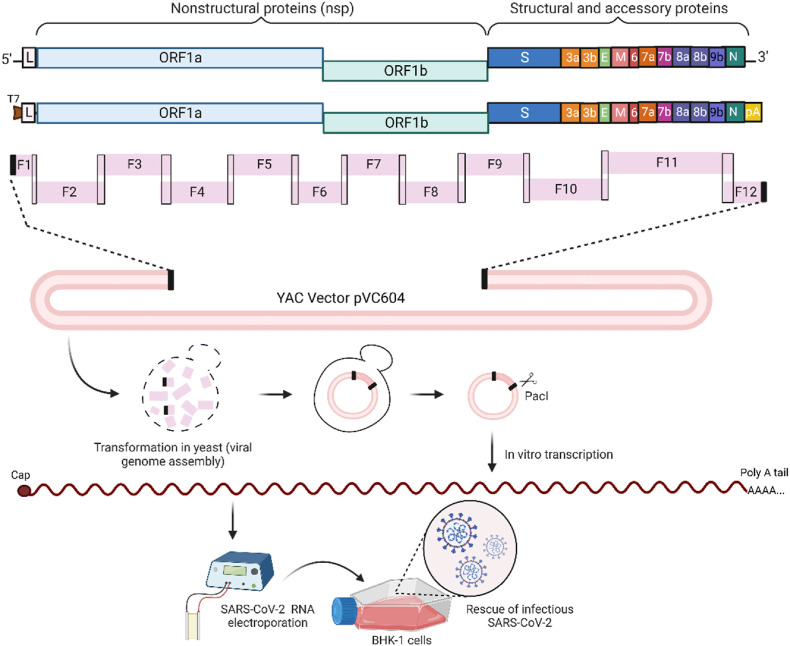
Compared to bacteria, yeast is less sensitive to toxic viral elements and has a higher capacity to maintain large segments of DNA (Ketner et al., 1994). In addition, yeast can efficiently recombine overlapping DNA fragments in vivo, which led to the development of a technique called transformation-associated recombination (TAR) cloning (Kouprina and Larionov, 2008). In TAR cloning, DNA fragments containing overlapping sequences at the ends along with linearized TAR vector are transformed into yeast where recombination occurs among homologous regions of all the fragments and linearized TAR vector, resulting in a circular yeast artificial chromosome (YAC) containing the full-length cDNA of the viral genome. Fuelling by synthetic biology, this system has been successfully used to rapidly reconstruct diverse RNA viruses, including members of the Coronaviridae, Flaviviridae, and Pneumoviridae families (Thi Nhu Thao et al., 2020). Specifically for SARS-CoV-2, Thao et al. used this approach to reconstruct SARS-CoV-2 within a week (Thi Nhu Thao et al., 2020). Briefly, the cDNA of the SARS-CoV-2 genome was divided into 12 overlapping DNA fragments, which are either synthesized or amplified by RT-PCR from viral RNA from an isolate of a Munich patient (BetaCoV/Germany/BavPat1/2020) (Fig. 3 ). T7 promoter was fused to the 5' end of the viral genome and a cleavage site (PacI) was engineered immediately after the polyA tail, which allows the transcription of an authentic full-length viral RNA by T7 polymerase in vitro. Overlap sequences for the TAR vector pVC604 were included in the primers that amplified the 5′- and 3′-end fragments. Transformation of all DNA fragments along with linearized TAR vector into yeast S. cerevisiae led to the assembly of the full-length cDNA clone based on homologous recombination. After selection, there were over 90% positive clones, indicating a remarkably efficient assembly in yeast. Purified YACs were linearized using PacI and subjected to in vitro transcription using T7 RNA polymerase to generate capped viral genomic RNA. The resulting RNAs were electroporated together with an mRNA that encodes the SARS-CoV-2 N protein into BHK-21 cells. After seeding electroporated cells on Vero E6 cells, the culture efficiently rescued infectious SARS-CoV-2. GFP reporter viruses were also generated by inserting the reporter gene in-frame of ORF7a. Similar viral replication was detected for the parental SARS-CoV-2 isolate and recombinant SARS-CoV-2 on Vero E6 cells; however, the replication of the GFP reporter virus was reduced compared with the wild-type recombinant virus. The rapidity and applicability of this approach make this system attractive for rapidly responding to any other emerging virus threats. However, the accuracy in generating site mutations through recombination in yeast should be carefully examined.
Fig. 3.
YAC-derived SARS-CoV-2 reverse genetic system. The genome structure of SARS-CoV-2 followed by schematic representation of twelve overlapping DNA fragments used to clone SARS-CoV-2 into YAC vector pVC604. Length is not to scale. Fragments 1 and 12 had overlapping sequences for the YAC vector pVC604. T7 promoter was fused to the 5′ end of the viral genome and a cleavage site (PacI) was added after the poly(A) sequence at the 3′ end. Transformation of SARS-CoV-2 genome fragments along with linearized pVC604 vector in yeast leads to whole-genome assembly in vector through homologous end recombination. Purified YAC plasmid DNA is linearized using PacI and subjected to in vitro transcription. The resulting RNAs were electroporated into BHK1 cells which are plated on Vero E6 cells, leading to the rescue of infectious SARS-CoV-2. T7, T7 promoter; L, leader sequence; ORF, open-reading frame; E, envelope glycoprotein gene; M, membrane glycoprotein gene; N, nucleocapsid gene; pA, poly-A tails. Figure adapted and modified from (Thi Nhu Thao et al., 2020).
5. Circular polymerase extension reaction-based SARS-CoV-2 reverse genetic system
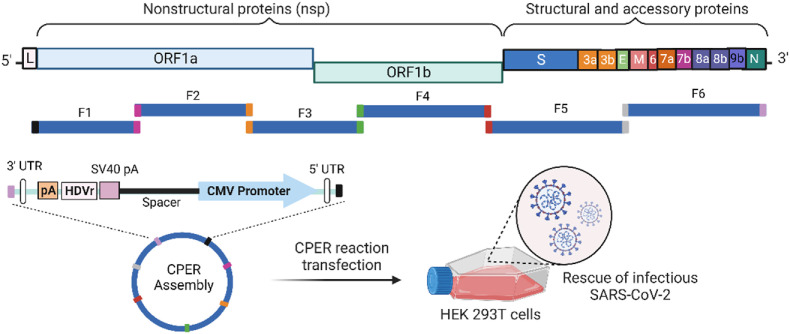
Circular Polymerase Extension Reaction (CPER) has just recently become another attractive strategy to generate infectious clones of viruses (Edmonds et al., 2013; Setoh et al., 2015). In this approach, the full-length cDNA of the viral genome and a linker fragment containing the promoter, poly(A) signal, and ribozyme sequence are fused and amplified by high-fidelity PCR. This novel bacterium-/yeast-free method has also been successfully adopted to establish the SARS-CoV-2 infectious clone (Fig. 4 ) (Amarilla et al., 2021; Torii et al., 2021). Specifically, six fragments were amplified directly from viral cDNA (viral RNA was used as a template to generate first-strand cDNA) that collectively encompassed the SARS-CoV-2 genome using high-fidelity DNA polymerase. Each fragment contained overlapping sequences of only 20 nucleotides with a high-GC content. A CMV promoter was engineered upstream of the 5′ UTR; an HDVr was engineered downstream of the 3' polyA tail of the viral genome, followed by an SV40 polyA signal for efficient transcription termination. A spacer sequence was added to separate the functional elements in the linker fragment (Fig. 4). To facilitate DNA circularization, an overlapping sequence was added in the linker fragment at both ends to facilitate recombination with fragments 1 and 6 (Fig. 4). After a single CPER reaction using a high-fidelity DNA polymerase, a circular DNA containing the full-length SARS-CoV-2 cDNA was assembled. Viruses were rescued by directly transfecting CPER reaction without any purification into either HEK 293T, which was later cocultured with Vero E6, or ACE2-expressing HEK 293T cells. Rescued viruses showed similar biological characteristics as parental WT viruses. The reporter virus was also constructed by replacing codons for amino acids 14–108 of ORF7a with a fluorescent protein (ZsGreen) gene. Using a similar approach, Torri et, al. Introduced the sfGFP and HiBiT luciferase gene into SARS-CoV-2 (Torii et al., 2021). The ability to easily and rapidly manipulate such a large viral genome by CPER makes it very attractive for fast rescuing positive-strand RNA viruses. However, the efficiency and accuracy in obtaining the desired point mutations in the viral genome during PCR should be examined.
Fig. 4.
CPER derived SARS-CoV-2 reverse genetic system. The complete genome of SARS-CoV-2 is covered by six overlapping DNA fragments. A linker fragment containing a CMV promoter is engineered upstream of the 5′ UTR. A sequence representing pA, HDVr, and SV40 pA signal is engineered downstream of the 3′ UTR. Linker and SARS-CoV-2 genome fragments are assembled in the CPER reaction. CPER reaction products are transfected in HEK 293T cells to rescue infectious SARS-CoV-2. ORF, open-reading frame; E, envelope glycoprotein gene; M, membrane glycoprotein gene; N, nucleocapsid gene; CMV, Cytomegalovirus promoter; pA, polyA tail; HDVr, hepatitis delta virus ribozyme; SV40 pA, SV40 polyA; UTR, untranslated region. Figure adapted and modified from (Amarilla et al., 2021).
6. Other strategies for constructing a SARS-CoV-2 reverse genetic system
Melade and colleagues described a simple method to generate infectious SARS-CoV-2 based on infectious subgenomic amplicon (ISA) technology without the need for reconstruction of the complete genomic cDNA (Melade et al., 2022). In this approach, the whole genome of SARS-CoV-2 was de novo synthesized through eight overlapping fragments. A CMV promoter and HDVr followed by SV40pA sequences were engineered at the 5′ end of the first fragment, and the 3' end of the last fragment, respectively. These synthetic subgenomic viral fragments were used as templates for PCR amplification and directly transfected into BHK-21 cells. Inside the BHK-21 cells, RNA polymerase II drives viral RNA transcription and HDVr/SV40pA facilitates transcription termination with RNA maturation, splicing, and polyadenylation. Five days after transfection, supernatants were passaged onto Vero E6 cells and infectious viral particles were successfully obtained after two passages. This approach is simple in DNA manipulation but required additional viral passage and viral sequence confirmation, which is not suitable for mutagenesis studies on replication-defective mutations.
Another strategy for constructing reverse genetic systems of RNA viruses is using the vaccinia virus vectors (Smith and Moss, 1983). It has been previously used for the generation of several recombinant coronaviruses, including HCoV-229E, MHV, SARS-CoV, and bat coronavirus IBV (Coley et al., 2005; Thiel et al., 2001; van den Worm et al., 2012). However, it has not been reported for SARS-CoV-2, probably due to its additional cloning steps and requirement of homologous recombination for site-directed mutagenesis in the vaccinia vector (Britton et al., 2005).
7. BSL2-adapted SARS-CoV-2 reverse genetic systems
SARS-CoV-2 is a BSL3 pathogen. The limit of the BSL3 facility hampered the accessibility of above mentioned full-length infectious clones, which constrain their wide use by many researchers. Therefore, BSL2 adapted SARS-CoV-2 reverse genetic system is highly demanded.
To fulfill this gap, we initially established a non-virulent trans-complementation system that recapitulates authentic viral replication at BSL2 settings (Zhang et al., 2021a). In this system, we first removed the E and ORF3 genes from the SARS-CoV-2 genome (named ΔORF3-E SARS-CoV-2) to abolish the ability of virion production (Fig. 1B). Second, we established a cell line Vero-ORF3-E that stably expresses E and ORF3 proteins. Through trans-complementation by ORF3 and E in the Vero-ORF3-E cells, large amounts of infectious ΔORF3-E SARS-CoV-2 could be produced. However, these ΔORF3-E SARS-CoV-2 can only cause single-round infection without further spreading in normal cells where ORF3 and E proteins are lacking. In addition, the transcriptional regulatory sequence (TRS) of the ΔORF3-E SARS-CoV-2 was mutated from the WT ACGAAC to CCGGAT to avoid TRS-mediated recombination (Graham et al., 2018; Yount et al., 2006). The ΔORF3-E SARS-CoV-2 is highly attenuated in hamsters and mice without causing any mortality and morbidity. Further, we engineered an mNG gene in the ΔORF3-E SARS-CoV-2 genome to facilitate high throughput neutralization and antiviral assays (Fig. 1B). Given the high attenuation, this trans-complementation system can be performed at BSL2 for high throughput antiviral testing.
Later, we developed a second generation of BSL2-adapted SARS-CoV-2 reverse genetic system. This system allows generating attenuated SARS-CoV-2 mimicking authentic viruses that could cause multiple rounds of infection in permissive cells (Liu et al., 2022c). This approach is based on the knowledge that SARS-CoV-2 accessory proteins are not essential for viral replication but can modulate replication and pathogenesis (Chen et al., 2022; Timilsina et al., 2022; Xia et al., 2020; Zandi et al., 2022). Deletion of accessory genes (ORF3678) would attenuate viral infection in immune-competent cells. In addition, the WT TRS was mutated to further attenuate viral replication and avoid recombination in generating reverted SARS-COV-2. Indeed, the resulting mutant viruses ΔORF3678 SARS-CoV-2, compared to WT SARS-CoV-2, replicated much less in primary human airway cultures but still robustly in interferon-deficient Vero E6 cells (Liu et al., 2022c). Moreover, ΔORF3678 SARS-CoV-2 was highly attenuated in both the hamster and K18-hACE2 mouse models. Such high safety profile and robustness of replication in cell culture suggest ΔORF3678 SARS-CoV-2's potential as a surrogate tool for studying SARS-CoV-2 biology at BSL2. Further, through engineering an mNG reporter into this live-attenuated virus, high-throughput neutralization, and antiviral testing can also be performed at BSL2.
Lastly, complementary to virus reverse genetic systems, replicon has been developed for many RNA viruses as an important BSL2 kit (Bartenschlager, 2002; Khan et al., 2020; Khromykh and Westaway, 1997; Shi et al., 2002; Xie et al., 2016). Replicons are self-amplifying viral RNA that lacks structural proteins but contains all viral proteins and RNA elements essential for viral RNA synthesis, making it a safe and attractive alternative to full-length infectious cDNAs, especially for BSL3 viruses, because no infectious viral particles can be produced during replicon replication in cell cultures. Moreover, by coupling fluorescent or luciferase reporters with antibiotic-resistant genes, stable cell lines containing non-cytopathic selectable reporter replicons can be obtained (Bartenschlager, 2002; Xie et al., 2016). The replicon cell lines have been recognized as a crucial toolkit in drug discovery for high throughput screening (Bartenschlager, 2002). Therefore, there is of great need for the SARS-CoV-2 replicon system for developing antivirals in response to the COVID-19 pandemic.
We reported previously a transient SARS-CoV-2 replicon using an in vitro ligation approach (Xia et al., 2020; Xie et al., 2020a). In this replicon, viral structural proteins (S, E, and M) and accessory genes (ORF3a, ORF3b, ORF6, ORF7a, ORF7b, and ORF8) were replaced by a gene cassette of Renilla luciferase (Rluc), foot-and-mouth disease virus 2A (FMDV-2A), and neomycin phosphotransferase under the control of the TRS of the deleted S gene. After electroporating this replicon RNA into Huh-7 cells, replicon replication can be monitored by examing the luciferase signals. This replicon was further proved suitable for screening antivirals (e.g., Remdesivir and chloroquine) against SARS-CoV-2. More SARS-CoV-2 replicon systems were reported using multiple construction approaches. Using a similar in vitro ligation approach, Kotaki et al. developed independently a transient replicon containing HiBiT-tag sequence based on a clinical SARS-CoV-2 isolate from Japan (Kotaki et al., 2021; Xie et al., 2020a). Zhang et al. developed a BAC-vectored SARS-CoV-2 replicon with secreted Gaussia luciferase (Zhang et al., 2021b). He et al. also developed a BAC-vector SARS-CoV-2 replicon with both luciferase and GFP reporter and further applied it for high throughput compound screening in semi-automated settings (He et al., 2021). Ricardo-Lax et al. reported the YAC-derived SARS-CoV-2 replication (Ricardo-Lax et al., 2021).
Generating a stable cell line harboring non-cytopathic SARS-CoV-2 replicon had proven challenging for us and many other groups, likely due to the intrinsic toxicity/cell stress caused by viral replication and translated protein(s) that mess up host transcription and translation (Finkel et al., 2021). Most recently, Liu et al. managed to generate a stable baby hamster kidney (BHK-21) cell line harboring non-cytopathic replicons of SARS-CoV-2 (Liu et al., 2022a). They introduced Nsp1 K164A/H165A mutations into the SARS-CoV-2 replicon that we constructed using in vitro ligation approach. The resulting replicon containing NanoLuc and Neomycine-resistant genes (SARS-CoV-2-Rep-NanoLuc-Neo-Nsp1K164A/H165A) were electroporated into BHK-21-NPDox-ON cells (nucleoprotein is expressed in a doxycycline-inducible manner) followed by selection in the presence of antibiotics G418. It's reported that these two Nsp1 mutations (K164A/H165A) could ablate Nsp1's interaction with host ribosome (Narayanan et al., 2008; Schubert et al., 2020), resulting in less Nsp1-mediated cytotoxicity (Lapointe et al., 2021; Schubert et al., 2020; Yuan et al., 2020). With this modification, Liu et al. could recover the stable SARS-CoV-2 replicon cell lines after G418 selection only on BHK-21 cells but not on Huh7.5.1 cells (Liu et al., 2022a). Interestingly, Ricardo-Lax et al. failed to select a stable cell line containing the YAC-derived SARS-CoV-2 replicon with the Nsp1 K164A/H165A mutations in both Huh-7.5 and BHK-21 cells. In contrast, Tanaka et al. successfully obtained a stable VeroE6 cell line that harbors the BAC plasmid-derived SARS-CoV-2 replicon without introducing any mutations into the SARS-CoV-2 genome (Tanaka et al., 2022), arguing different cell backgrounds and multiple adaptive mutations may be necessary. These two stable SARS-CoV-2 replicons have been proven effective in screening inhibitors against SARS-CoV-2 replication.
Lastly, it should be noted that BSL2-adapted reverse genetic systems could not completely resemble authentic viruses The replicon system contains only the steps of viral translation and RNA synthesis; the trans-complemented system only launches single-round infection on normal cells, which lacks the step of viral assembly and release. The live-attenuated ΔORF3678 SARS-CoV-2 can cause multiple rounds of infection in vitro but with slower replication kinetics. Additionally, ORF3678-mediated host response and pathogenesis are excluded. Therefore, caution should be taken on critical findings from BSL2-adapted reverse genetic systems. The authentic viruses would serve as the last step to validate the findings from BSL2-adapted systems.
8. Conclusions
The success of the rapid development of SARS-CoV-2 genetic systems is attributed to many years of previous research. Table 1 summarizes the advantages and disadvantages of the different genetic systems. These genetic systems have provided complementary tools to address different research questions. The ability to manipulate the SARS-CoV-2 genome has allowed researchers to gain insights into virus/host interactions and pathogenesis (Johnson et al., 2022; Vu et al., 2022), immune escape mutations (Kurhade et al., 2022), and the development of reporter assays for testing antiviral drugs (Xie et al., 2020b) and antibody neutralization (Zou et al., 2022b).
Table 1.
Advantages and disadvantages of different reverse genetics system of SARS-CoV-2.
| SARS-CoV-2 Reverse Genetics System | Pros | Cons |
|---|---|---|
| In Vitro Ligation | • The multi-plasmid system can eliminate the effect of bacteria-toxic elements in the viral genome. • Multiple mutations across the genome can be generated simultaneously. • High robustness in recovering recombinant viruses. |
• Labour intensive • Require good techniques and additional steps of DNA/RNA preparation. |
| Bacterial artificial chromosome (BAC) | • The single plasmid system allows the introduction of large DNA sequences in bacteria while minimizing their instability • Relatively easy manipulation and production of the cDNA clone. • No in vitro transcription is required if using a CMV promoter. |
• Toxicity or instability is unknown when new mutations are introduced. • Multiple steps of cloning may be required for mutagenesis if unique restriction sites are unavailable. |
| Yeast Artificial Chromosome (YAC) | • Highly tolerant of viral element-mediated toxicity or instability. • No restraint of unique restriction sites for cloning and mutagenesis. • Higher assembly efficiency of homologous end recombination in TAR cloning. • Single plasmid system. |
• Good techniques in yeast culture and plasmid manipulation. • Whole-genome sequencing is usually required to verify the viral cDNA. |
| Circular Polymerase Extension Reaction (CPER) | • Easy DNA manipulation and mutagenesis as plasmid and RNA preparation can be avoided. • No DNA plasmid instability issue. |
• The risk of unwanted mutations during high-fidelity PCR exists. • Longer time is needed to recover the infectious viruses after transfection. Additional viral passages may be needed. |
Despite the success of knowledge advancement driven by the reverse genetic system, the research community must take extra caution when making recombinant SARS-CoV-2 with new properties, particularly those that may expand host species, enhance viral pathogenesis, or resistant to clinically approved antiviral therapies or vaccines. Regulation and oversight should be placed to achieve the best benefit/risk management, which can only be achieved by robust communications among researchers, principal investigators, institutional biosafety committees, and government regulatory and funding agencies.
Declaration of competing interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: X.X. and P.-Y.S. have filed a patent on the reverse genetic system of SARS-CoV-2. C.K. does not have any conflict of interest.
Acknowledgments
P.-Y.S. was supported by NIH grant U19AI171413 and awards from the Sealy & Smith Foundation, the Kleberg Foundation, the John S. Dunn Foundation, the Amon G. Carter Foundation, the Summerfield Robert Foundation, and the Edith and Robert Zinn Foundation. All figures in this article are Created with BioRender.com.
Data availability
No data was used for the research described in the article.
References
- Adler H., Messerle M., Koszinowski U.H. Cloning of herpesviral genomes as bacterial artificial chromosomes. Rev. Med. Virol. 2003;13:111–121. doi: 10.1002/rmv.380. [DOI] [PubMed] [Google Scholar]
- Almazan F., Dediego M.L., Galan C., Escors D., Alvarez E., Ortego J., Sola I., Zuniga S., Alonso S., Moreno J.L., Nogales A., Capiscol C., Enjuanes L. Construction of a severe acute respiratory syndrome coronavirus infectious cDNA clone and a replicon to study coronavirus RNA synthesis. J. Virol. 2006;80:10900–10906. doi: 10.1128/JVI.00385-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almazan F., DeDiego M.L., Sola I., Zuniga S., Nieto-Torres J.L., Marquez-Jurado S., Andres G., Enjuanes L. Engineering a replication-competent, propagation-defective Middle East respiratory syndrome coronavirus as a vaccine candidate. mBio. 2013;4 doi: 10.1128/mBio.00650-13. e00650-00613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almazan F., Gonzalez J.M., Penzes Z., Izeta A., Calvo E., Plana-Duran J., Enjuanes L. Engineering the largest RNA virus genome as an infectious bacterial artificial chromosome. Proc. Natl. Acad. Sci. U. S. A. 2000;97:5516–5521. doi: 10.1073/pnas.97.10.5516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almazan F., Sola I., Zuniga S., Marquez-Jurado S., Morales L., Becares M., Enjuanes L. Coronavirus reverse genetic systems: infectious clones and replicons. Virus Res. 2014;189:262–270. doi: 10.1016/j.virusres.2014.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amarilla A.A., Sng J.D.J., Parry R., Deerain J.M., Potter J.R., Setoh Y.X., Rawle D.J., Le T.T., Modhiran N., Wang X., Peng N.Y.G., Torres F.J., Pyke A., Harrison J.J., Freney M.E., Liang B., McMillan C.L.D., Cheung S.T.M., Guevara D., Hardy J.M., Bettington M., Muller D.A., Coulibaly F., Moore F., Hall R.A., Young P.R., Mackenzie J.M., Hobson-Peters J., Suhrbier A., Watterson D., Khromykh A.A. A versatile reverse genetics platform for SARS-CoV-2 and other positive-strand RNA viruses. Nat. Commun. 2021;12:3431. doi: 10.1038/s41467-021-23779-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aubry F., Nougairede A., Gould E.A., de Lamballerie X. Flavivirus reverse genetic systems, construction techniques and applications: a historical perspective. Antivir. Res. 2015;114:67–85. doi: 10.1016/j.antiviral.2014.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ball P. The lightning-fast quest for COVID vaccines - and what it means for other diseases. Nature. 2021;589:16–18. doi: 10.1038/d41586-020-03626-1. [DOI] [PubMed] [Google Scholar]
- Baric R.S., Fu K., Schaad M.C., Stohlman S.A. Establishing a genetic recombination map for murine coronavirus strain A59 complementation groups. Virology. 1990;177:646–656. doi: 10.1016/0042-6822(90)90530-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartenschlager R. Hepatitis C virus replicons: potential role for drug development. Nat. Rev. Drug Discov. 2002;1:911–916. doi: 10.1038/nrd942. [DOI] [PubMed] [Google Scholar]
- Becker M.M., Graham R.L., Donaldson E.F., Rockx B., Sims A.C., Sheahan T., Pickles R.J., Corti D., Johnston R.E., Baric R.S., Denison M.R. Synthetic recombinant bat SARS-like coronavirus is infectious in cultured cells and in mice. Proc. Natl. Acad. Sci. U. S. A. 2008;105:19944–19949. doi: 10.1073/pnas.0808116105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Britton P., Evans S., Dove B., Davies M., Casais R., Cavanagh D. Generation of a recombinant avian coronavirus infectious bronchitis virus using transient dominant selection. J. Virol. Methods. 2005;123:203–211. doi: 10.1016/j.jviromet.2004.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen J., Lu Z., Yang X., Zhou Y., Gao J., Zhang S., Huang S., Cai J., Yu J., Zhao W., Zhang B. Severe acute respiratory syndrome coronavirus 2 ORF8 protein inhibits type I interferon production by targeting HSP90B1 signaling. Front. Cell. Infect. Microbiol. 2022;12 doi: 10.3389/fcimb.2022.899546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiem K., Morales Vasquez D., Park J.G., Platt R.N., Anderson T., Walter M.R., Kobie J.J., Ye C., Martinez-Sobrido L. Generation and Characterization of recombinant SARS-CoV-2 expressing reporter genes. J. Virol. 2021;95(7):2209–2220. doi: 10.1128/JVI.02209-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coley S.E., Lavi E., Sawicki S.G., Fu L., Schelle B., Karl N., Siddell S.G., Thiel V. Recombinant mouse hepatitis virus strain A59 from cloned, full-length cDNA replicates to high titers in vitro and is fully pathogenic in vivo. J. Virol. 2005;79:3097–3106. doi: 10.1128/JVI.79.5.3097-3106.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curtis K.M., Yount B., Baric R.S. Heterologous gene expression from transmissible gastroenteritis virus replicon particles. J. Virol. 2002;76:1422–1434. doi: 10.1128/JVI.76.3.1422-1434.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edmonds J., van Grinsven E., Prow N., Bosco-Lauth A., Brault A.C., Bowen R.A., Hall R.A., Khromykh A.A. A novel bacterium-free method for generation of flavivirus infectious DNA by circular polymerase extension reaction allows accurate recapitulation of viral heterogeneity. J. Virol. 2013;87:2367–2372. doi: 10.1128/JVI.03162-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fahnoe U., Pham L.V., Fernandez-Antunez C., Costa R., Rivera-Rangel L.R., Galli A., Feng S., Mikkelsen L.S., Gottwein J.M., Scheel T.K.H., Ramirez S., Bukh J. 2022. Versatile SARS-CoV-2 Reverse-Genetics Systems for the Study of Antiviral Resistance and Replication. Viruses 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang Y., Sun P., Xie X., Du M., Du F., Ye J., Kalveram B.K., Plante J.A., Plante K.S., Li B., Bai X.-c., Shi P.-Y., Chen Z.J. An antibody that neutralizes SARS-CoV-1 and SARS-CoV-2 by binding to a conserved spike epitope outside the receptor binding motif. Science Immunology. 2022;7 doi: 10.1126/sciimmunol.abp9962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finkel Y., Gluck A., Nachshon A., Winkler R., Fisher T., Rozman B., Mizrahi O., Lubelsky Y., Zuckerman B., Slobodin B., Yahalom-Ronen Y., Tamir H., Ulitsky I., Israely T., Paran N., Schwartz M., Stern-Ginossar N. SARS-CoV-2 uses a multipronged strategy to impede host protein synthesis. Nature. 2021;594:240–245. doi: 10.1038/s41586-021-03610-3. [DOI] [PubMed] [Google Scholar]
- Gonzalez J.M., Penzes Z., Almazan F., Calvo E., Enjuanes L. Stabilization of a full-length infectious cDNA clone of transmissible gastroenteritis coronavirus by insertion of an intron. J. Virol. 2002;76:4655–4661. doi: 10.1128/JVI.76.9.4655-4661.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham R.L., Deming D.J., Deming M.E., Yount B.L., Baric R.S. Evaluation of a recombination-resistant coronavirus as a broadly applicable, rapidly implementable vaccine platform. Commun Biol. 2018;1:179. doi: 10.1038/s42003-018-0175-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He X., Quan S., Xu M., Rodriguez S., Goh S.L., Wei J., Fridman A., Koeplinger K.A., Carroll S.S., Grobler J.A., Espeseth A.S., Olsen D.B., Hazuda D.J., Wang D. vol. 118. Proc Natl Acad Sci U S A; 2021. (Generation of SARS-CoV-2 Reporter Replicon for High-Throughput Antiviral Screening and Testing). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hou Y.J., Okuda K., Edwards C.E., Martinez D.R., Asakura T., Dinnon K.H., 3rd, Kato T., Lee R.E., Yount B.L., Mascenik T.M., Chen G., Olivier K.N., Ghio A., Tse L.V., Leist S.R., Gralinski L.E., Schafer A., Dang H., Gilmore R., Nakano S., Sun L., Fulcher M.L., Livraghi-Butrico A., Nicely N.I., Cameron M., Cameron C., Kelvin D.J., de Silva A., Margolis D.M., Markmann A., Bartelt L., Zumwalt R., Martinez F.J., Salvatore S.P., Borczuk A., Tata P.R., Sontake V., Kimple A., Jaspers I., O'Neal W.K., Randell S.H., Boucher R.C., Baric R.S. SARS-CoV-2 reverse genetics reveals a variable infection gradient in the respiratory tract. Cell. 2020;182:429–446 e414. doi: 10.1016/j.cell.2020.05.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu B., Guo H., Zhou P., Shi Z.L. Characteristics of SARS-CoV-2 and COVID-19. Nat. Rev. Microbiol. 2021;19:141–154. doi: 10.1038/s41579-020-00459-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin Y.Y., Lin H., Cao L., Wu W.C., Ji Y., Du L., Jiang Y., Xie Y., Tong K., Xing F., Zheng F., Shi M., Pan J.A., Peng X., Guo D. A convenient and biosafe replicon with accessory genes of SARS-CoV-2 and its potential application in antiviral drug discovery. Virol. Sin. 2021;36:913–923. doi: 10.1007/s12250-021-00385-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson B.A., Xie X., Bailey A.L., Kalveram B., Lokugamage K.G., Muruato A., Zou J., Zhang X., Juelich T., Smith J.K., Zhang L., Bopp N., Schindewolf C., Vu M., Vanderheiden A., Winkler E.S., Swetnam D., Plante J.A., Aguilar P., Plante K.S., Popov V., Lee B., Weaver S.C., Suthar M.S., Routh A.L., Ren P., Ku Z., An Z., Debbink K., Diamond M.S., Shi P.Y., Freiberg A.N., Menachery V.D. Loss of furin cleavage site attenuates SARS-CoV-2 pathogenesis. Nature. 2021;591:293–299. doi: 10.1038/s41586-021-03237-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson B.A., Zhou Y., Lokugamage K.G., Vu M.N., Bopp N., Crocquet-Valdes P.A., Kalveram B., Schindewolf C., Liu Y., Scharton D., Plante J.A., Xie X., Aguilar P., Weaver S.C., Shi P.Y., Walker D.H., Routh A.L., Plante K.S., Menachery V.D. Nucleocapsid mutations in SARS-CoV-2 augment replication and pathogenesis. PLoS Pathog. 2022;18 doi: 10.1371/journal.ppat.1010627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kee J., Thudium S., Renner D.M., Glastad K., Palozola K., Zhang Z., Li Y., Lan Y., Cesare J., Poleshko A., Kiseleva A.A., Truitt R., Cardenas-Diaz F.L., Zhang X., Xie X., Kotton D.N., Alysandratos K.D., Epstein J.A., Shi P.Y., Yang W., Morrisey E., Garcia B.A., Berger S.L., Weiss S.R., Korb E. SARS-CoV-2 disrupts host epigenetic regulation via histone mimicry. Nature. 2022;610:381–388. doi: 10.1038/s41586-022-05282-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ketner G., Spencer F., Tugendreich S., Connelly C., Hieter P. Efficient manipulation of the human adenovirus genome as an infectious yeast artificial chromosome clone. Proc. Natl. Acad. Sci. U. S. A. 1994;91:6186–6190. doi: 10.1073/pnas.91.13.6186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan S., Soni S., Veerapu N.S. HCV replicon systems: workhorses of drug discovery and resistance. Front. Cell. Infect. Microbiol. 2020;10:325. doi: 10.3389/fcimb.2020.00325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khromykh A.A., Westaway E.G. Subgenomic replicons of the flavivirus Kunjin: construction and applications. J. Virol. 1997;71:1497–1505. doi: 10.1128/jvi.71.2.1497-1505.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotaki T., Xie X., Shi P.Y., Kameoka M. A PCR amplicon-based SARS-CoV-2 replicon for antiviral evaluation. Sci. Rep. 2021;11:2229. doi: 10.1038/s41598-021-82055-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kouprina N., Larionov V. Selective isolation of genomic loci from complex genomes by transformation-associated recombination cloning in the yeast Saccharomyces cerevisiae. Nat. Protoc. 2008;3:371–377. doi: 10.1038/nprot.2008.5. [DOI] [PubMed] [Google Scholar]
- Ku Z., Xie X., Davidson E., Ye X., Su H., Menachery V.D., Li Y., Yuan Z., Zhang X., Muruato A.E., Ag I.E., Tyrell B., Doolan K., Doranz B.J., Wrapp D., Bates P.F., McLellan J.S., Weiss S.R., Zhang N., Shi P.Y., An Z. Molecular determinants and mechanism for antibody cocktail preventing SARS-CoV-2 escape. Nat. Commun. 2021;12:469. doi: 10.1038/s41467-020-20789-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ku Z., Xie X., Hinton P.R., Liu X., Ye X., Muruato A.E., Ng D.C., Biswas S., Zou J., Liu Y., Pandya D., Menachery V.D., Rahman S., Cao Y.A., Deng H., Xiong W., Carlin K.B., Liu J., Su H., Haanes E.J., Keyt B.A., Zhang N., Carroll S.F., Shi P.Y., An Z. Nasal delivery of an IgM offers broad protection from SARS-CoV-2 variants. Nature. 2021;595:718–723. doi: 10.1038/s41586-021-03673-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ku Z., Xie X., Lin J., Gao P., Wu B., El Sahili A., Su H., Liu Y., Ye X., Tan E.Y., Li X., Fan X., Goh B.C., Xiong W., Boyd H., Muruato A.E., Deng H., Xia H., Zou J., Kalveram B.K., Menachery V.D., Zhang N., Lescar J., Shi P.-Y., An Z. Engineering SARS-CoV-2 specific cocktail antibodies into a bispecific format improves neutralizing potency and breadth. Nat. Commun. 2022;13:5552. doi: 10.1038/s41467-022-33284-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurhade C., Zou J., Xia H., Liu M., Yang Q., Cutler M., Cooper D., Muik A., Sahin U., Jansen K.U., Ren P., Xie X., Swanson K.A., Shi P.Y. Neutralization of Omicron sublineages and Deltacron SARS-CoV-2 by three doses of BNT162b2 vaccine or BA.1 infection. Emerg. Microb. Infect. 2022;11:1828–1832. doi: 10.1080/22221751.2022.2099305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kusters J.G., Jager E.J., Niesters H.G., van der Zeijst B.A. Sequence evidence for RNA recombination in field isolates of avian coronavirus infectious bronchitis virus. Vaccine. 1990;8:605–608. doi: 10.1016/0264-410X(90)90018-H. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lapointe C.P., Grosely R., Johnson A.G., Wang J., Fernandez I.S., Puglisi J.D. Dynamic competition between SARS-CoV-2 NSP1 and mRNA on the human ribosome inhibits translation initiation. Proc. Natl. Acad. Sci. U. S. A. 2021;118 doi: 10.1073/pnas.2017715118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu S., Chou C.K., Wu W.W., Luan B., Wang T.T. Stable cell clones harboring self-replicating SARS-CoV-2 RNAs for drug screen. J. Virol. 2022;96 doi: 10.1128/jvi.02216-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y., Liu J., Johnson B.A., Xia H., Ku Z., Schindewolf C., Widen S.G., An Z., Weaver S.C., Menachery V.D., Xie X., Shi P.Y. Delta spike P681R mutation enhances SARS-CoV-2 fitness over Alpha variant. Cell Rep. 2022;39 doi: 10.1016/j.celrep.2022.110829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y., Liu J., Plante K.S., Plante J.A., Xie X., Zhang X., Ku Z., An Z., Scharton D., Schindewolf C., Menachery V.D., Shi P.Y., Weaver S.C. bioRxiv; 2021. The N501Y Spike Substitution Enhances SARS-CoV-2 Transmission. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y., Zhang X., Liu J., Xia H., Zou J., Muruato A.E., Periasamy S., Kurhade C., Plante J.A., Bopp N.E., Kalveram B., Bukreyev A., Ren P., Wang T., Menachery V.D., Plante K.S., Xie X., Weaver S.C., Shi P.Y. A live-attenuated SARS-CoV-2 vaccine candidate with accessory protein deletions. Nat. Commun. 2022;13:4337. doi: 10.1038/s41467-022-31930-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Makino S., Keck J.G., Stohlman S.A., Lai M.M. High-frequency RNA recombination of murine coronaviruses. J. Virol. 1986;57:729–737. doi: 10.1128/jvi.57.3.729-737.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masters P.S. Reverse genetics of the largest RNA viruses. Adv. Virus Res. 1999;53:245–264. doi: 10.1016/S0065-3527(08)60351-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melade J., Piorkowski G., Touret F., Fourie T., Driouich J.S., Cochin M., Bouzidi H.S., Coutard B., Nougairede A., de Lamballerie X. A simple reverse genetics method to generate recombinant coronaviruses. EMBO Rep. 2022;23 doi: 10.15252/embr.202153820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muruato A., Vu M.N., Johnson B.A., Davis-Gardner M.E., Vanderheiden A., Lokugamage K., Schindewolf C., Crocquet-Valdes P.A., Langsjoen R.M., Plante J.A., Plante K.S., Weaver S.C., Debbink K., Routh A.L., Walker D., Suthar M.S., Shi P.Y., Xie X., Menachery V.D. Mouse-adapted SARS-CoV-2 protects animals from lethal SARS-CoV challenge. PLoS Biol. 2021;19 doi: 10.1371/journal.pbio.3001284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narayanan K., Huang C., Lokugamage K., Kamitani W., Ikegami T., Tseng C.T., Makino S. Severe acute respiratory syndrome coronavirus nsp1 suppresses host gene expression, including that of type I interferon, in infected cells. J. Virol. 2008;82:4471–4479. doi: 10.1128/JVI.02472-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plante J.A., Liu Y., Liu J., Xia H., Johnson B.A., Lokugamage K.G., Zhang X., Muruato A.E., Zou J., Fontes-Garfias C.R., Mirchandani D., Scharton D., Bilello J.P., Ku Z., An Z., Kalveram B., Freiberg A.N., Menachery V.D., Xie X., Plante K.S., Weaver S.C., Shi P.Y. Spike mutation D614G alters SARS-CoV-2 fitness. Nature. 2021;592:116–121. doi: 10.1038/s41586-020-2895-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ricardo-Lax I., Luna J.M., Thao T.T.N., Le Pen J., Yu Y., Hoffmann H.H., Schneider W.M., Razooky B.S., Fernandez-Martinez J., Schmidt F., Weisblum Y., Trueb B.S., Berenguer Veiga I., Schmied K., Ebert N., Michailidis E., Peace A., Sanchez-Rivera F.J., Lowe S.W., Rout M.P., Hatziioannou T., Bieniasz P.D., Poirier J.T., MacDonald M.R., Thiel V., Rice C.M. Replication and single-cycle delivery of SARS-CoV-2 replicons. Science. 2021;374:1099–1106. doi: 10.1126/science.abj8430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rice C.M., Grakoui A., Galler R., Chambers T.J. Transcription of infectious yellow fever RNA from full-length cDNA templates produced by in vitro ligation. N. Biol. 1989;1:285–296. [PubMed] [Google Scholar]
- Rihn S.J., Merits A., Bakshi S., Turnbull M.L., Wickenhagen A., Alexander A.J.T., Baillie C., Brennan B., Brown F., Brunker K., Bryden S.R., Burness K.A., Carmichael S., Cole S.J., Cowton V.M., Davies P., Davis C., De Lorenzo G., Donald C.L., Dorward M., Dunlop J.I., Elliott M., Fares M., da Silva Filipe A., Freitas J.R., Furnon W., Gestuveo R.J., Geyer A., Giesel D., Goldfarb D.M., Goodman N., Gunson R., Hastie C.J., Herder V., Hughes J., Johnson C., Johnson N., Kohl A., Kerr K., Leech H., Lello L.S., Li K., Lieber G., Liu X., Lingala R., Loney C., Mair D., McElwee M.J., McFarlane S., Nichols J., Nomikou K., Orr A., Orton R.J., Palmarini M., Parr Y.A., Pinto R.M., Raggett S., Reid E., Robertson D.L., Royle J., Cameron-Ruiz N., Shepherd J.G., Smollett K., Stewart D.G., Stewart M., Sugrue E., Szemiel A.M., Taggart A., Thomson E.C., Tong L., Torrie L.S., Toth R., Varjak M., Wang S., Wilkinson S.G., Wyatt P.G., Zusinaite E., Alessi D.R., Patel A.H., Zaid A., Wilson S.J., Mahalingam S. A plasmid DNA-launched SARS-CoV-2 reverse genetics system and coronavirus toolkit for COVID-19 research. PLoS Biol. 2021;19 doi: 10.1371/journal.pbio.3001091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schubert K., Karousis E.D., Jomaa A., Scaiola A., Echeverria B., Gurzeler L.A., Leibundgut M., Thiel V., Muhlemann O., Ban N. SARS-CoV-2 Nsp1 binds the ribosomal mRNA channel to inhibit translation. Nat. Struct. Mol. Biol. 2020;27:959–966. doi: 10.1038/s41594-020-0511-8. [DOI] [PubMed] [Google Scholar]
- Scobey T., Yount B.L., Sims A.C., Donaldson E.F., Agnihothram S.S., Menachery V.D., Graham R.L., Swanstrom J., Bove P.F., Kim J.D., Grego S., Randell S.H., Baric R.S. Reverse genetics with a full-length infectious cDNA of the Middle East respiratory syndrome coronavirus. Proc. Natl. Acad. Sci. USA. 2013;110:16157–16162. doi: 10.1073/pnas.1311542110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Setoh Y.X., Prow N.A., Rawle D.J., Tan C.S.E., Edmonds J.H., Hall R.A., Khromykh A.A. Systematic analysis of viral genes responsible for differential virulence between American and Australian West Nile virus strains. J. Gen. Virol. 2015;96:1297–1308. doi: 10.1099/vir.0.000069. [DOI] [PubMed] [Google Scholar]
- Shi P.Y., Tilgner M., Lo M.K. Construction and characterization of subgenomic replicons of New York strain of West Nile virus. Virology. 2002;296:219–233. doi: 10.1006/viro.2002.1453. [DOI] [PubMed] [Google Scholar]
- Shizuya H., Birren B., Kim U.J., Mancino V., Slepak T., Tachiiri Y., Simon M. Cloning and stable maintenance of 300-kilobase-pair fragments of human DNA in Escherichia coli using an F-factor-based vector. Proc. Natl. Acad. Sci. U. S. A. 1992;89:8794–8797. doi: 10.1073/pnas.89.18.8794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith G.L., Moss B. Infectious poxvirus vectors have capacity for at least 25 000 base pairs of foreign DNA. Gene. 1983;25:21–28. doi: 10.1016/0378-1119(83)90163-4. [DOI] [PubMed] [Google Scholar]
- St-Jean J.R., Desforges M., Almazan F., Jacomy H., Enjuanes L., Talbot P.J. Recovery of a neurovirulent human coronavirus OC43 from an infectious cDNA clone. J. Virol. 2006;80:3670–3674. doi: 10.1128/JVI.80.7.3670-3674.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanaka T., Saito A., Suzuki T., Miyamoto Y., Takayama K., Okamoto T., Moriishi K. Establishment of a stable SARS-CoV-2 replicon system for application in high-throughput screening. Antivir. Res. 2022;199 doi: 10.1016/j.antiviral.2022.105268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thi Nhu Thao T., Labroussaa F., Ebert N., V'Kovski P., Stalder H., Portmann J., Kelly J., Steiner S., Holwerda M., Kratzel A., Gultom M., Schmied K., Laloli L., Husser L., Wider M., Pfaender S., Hirt D., Cippa V., Crespo-Pomar S., Schroder S., Muth D., Niemeyer D., Corman V.M., Muller M.A., Drosten C., Dijkman R., Jores J., Thiel V. Rapid reconstruction of SARS-CoV-2 using a synthetic genomics platform. Nature. 2020;582:561–565. doi: 10.1038/s41586-020-2294-9. [DOI] [PubMed] [Google Scholar]
- Thiel V., Herold J., Schelle B., Siddell S.G. Infectious RNA transcribed in vitro from a cDNA copy of the human coronavirus genome cloned in vaccinia virus. J. Gen. Virol. 2001;82:1273–1281. doi: 10.1099/0022-1317-82-6-1273. [DOI] [PubMed] [Google Scholar]
- Timilsina U., Umthong S., Ivey E.B., Waxman B., Stavrou S. SARS-CoV-2 ORF7a potently inhibits the antiviral effect of the host factor SERINC5. Nat. Commun. 2022;13:2935. doi: 10.1038/s41467-022-30609-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torii S., Ono C., Suzuki R., Morioka Y., Anzai I., Fauzyah Y., Maeda Y., Kamitani W., Fukuhara T., Matsuura Y. Establishment of a reverse genetics system for SARS-CoV-2 using circular polymerase extension reaction. Cell Rep. 2021;35 doi: 10.1016/j.celrep.2021.109014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- V'Kovski P., Kratzel A., Steiner S., Stalder H., Thiel V. Coronavirus biology and replication: implications for SARS-CoV-2. Nat. Rev. Microbiol. 2021;19:155–170. doi: 10.1038/s41579-020-00468-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van den Worm S.H., Eriksson K.K., Zevenhoven J.C., Weber F., Zust R., Kuri T., Dijkman R., Chang G., Siddell S.G., Snijder E.J., Thiel V., Davidson A.D. Reverse genetics of SARS-related coronavirus using vaccinia virus-based recombination. PLoS One. 2012;7 doi: 10.1371/journal.pone.0032857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vu M.N., Lokugamage K.G., Plante J.A., Scharton D., Bailey A.O., Sotcheff S., Swetnam D.M., Johnson B.A., Schindewolf C., Alvarado R.E., Crocquet-Valdes P.A., Debbink K., Weaver S.C., Walker D.H., Russell W.K., Routh A.L., Plante K.S., Menachery V.D. QTQTN motif upstream of the furin-cleavage site plays a key role in SARS-CoV-2 infection and pathogenesis. Proc. Natl. Acad. Sci. U. S. A. 2022;119 doi: 10.1073/pnas.2205690119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh E.E., Frenck R.W., Jr., Falsey A.R., Kitchin N., Absalon J., Gurtman A., Lockhart S., Neuzil K., Mulligan M.J., Bailey R., Swanson K.A., Li P., Koury K., Kalina W., Cooper D., Fontes-Garfias C., Shi P.Y., Tureci O., Tompkins K.R., Lyke K.E., Raabe V., Dormitzer P.R., Jansen K.U., Sahin U., Gruber W.C. Safety and immunogenicity of two RNA-based covid-19 vaccine candidates. N. Engl. J. Med. 2020;383:2439–2450. doi: 10.1056/NEJMoa2027906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xia H., Cao Z., Xie X., Zhang X., Chen J.Y., Wang H., Menachery V.D., Rajsbaum R., Shi P.Y. Evasion of type I interferon by SARS-CoV-2. Cell Rep. 2020;33 doi: 10.1016/j.celrep.2020.108234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xia H., Zou J., Kurhade C., Cai H., Yang Q., Cutler M., Cooper D., Muik A., Jansen K.U., Xie X., Swanson K.A., Shi P.Y. Neutralization and durability of 2 or 3 doses of the BNT162b2 vaccine against Omicron SARS-CoV-2. Cell Host Microbe. 2022;30:485–488 e483. doi: 10.1016/j.chom.2022.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie X., Lokugamage K.G., Zhang X., Vu M.N., Muruato A.E., Menachery V.D., Shi P.-Y. Engineering SARS-CoV-2 using a reverse genetic system. Nat. Protoc. 2021;16:1761–1784. doi: 10.1038/s41596-021-00491-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie X., Muruato A., Lokugamage K.G., Narayanan K., Zhang X., Zou J., Liu J., Schindewolf C., Bopp N.E., Aguilar P.V., Plante K.S., Weaver S.C., Makino S., LeDuc J.W., Menachery V.D., Shi P.Y. An infectious cDNA clone of SARS-CoV-2. Cell Host Microbe. 2020;27:841–848 e843. doi: 10.1016/j.chom.2020.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie X., Muruato A.E., Zhang X., Lokugamage K.G., Fontes-Garfias C.R., Zou J., Liu J., Ren P., Balakrishnan M., Cihlar T., Tseng C.K., Makino S., Menachery V.D., Bilello J.P., Shi P.Y. A nanoluciferase SARS-CoV-2 for rapid neutralization testing and screening of anti-infective drugs for COVID-19. Nat. Commun. 2020;11:5214. doi: 10.1038/s41467-020-19055-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie X., Zou J., Shan C., Yang Y., Kum D.B., Dallmeier K., Neyts J., Shi P.Y. Zika virus replicons for drug discovery. EBioMedicine. 2016;12:156–160. doi: 10.1016/j.ebiom.2016.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye C., Chiem K., Park J.G., Oladunni F., Platt R.N., 2nd, Anderson T., Almazan F., de la Torre J.C., Martinez-Sobrido L. Rescue of SARS-CoV-2 from a single bacterial artificial chromosome. mBio. 2020;11 doi: 10.1128/mBio.02168-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yount B., Curtis K.M., Baric R.S. Strategy for systematic assembly of large RNA and DNA genomes: transmissible gastroenteritis virus model. J. Virol. 2000;74:10600–10611. doi: 10.1128/jvi.74.22.10600-10611.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yount B., Curtis K.M., Fritz E.A., Hensley L.E., Jahrling P.B., Prentice E., Denison M.R., Geisbert T.W., Baric R.S. Reverse genetics with a full-length infectious cDNA of severe acute respiratory syndrome coronavirus. Proc. Natl. Acad. Sci. U. S. A. 2003;100:12995–13000. doi: 10.1073/pnas.1735582100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yount B., Denison M.R., Weiss S.R., Baric R.S. Systematic assembly of a full-length infectious cDNA of mouse hepatitis virus strain A59. J. Virol. 2002;76:11065–11078. doi: 10.1128/JVI.76.21.11065-11078.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yount B., Roberts R.S., Lindesmith L., Baric R.S. Rewiring the severe acute respiratory syndrome coronavirus (SARS-CoV) transcription circuit: engineering a recombination-resistant genome. Proc. Natl. Acad. Sci. U. S. A. 2006;103:12546–12551. doi: 10.1073/pnas.0605438103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan S., Peng L., Park J.J., Hu Y., Devarkar S.C., Dong M.B., Shen Q., Wu S., Chen S., Lomakin I.B., Xiong Y. Nonstructural protein 1 of SARS-CoV-2 is a potent pathogenicity factor redirecting host protein synthesis machinery toward viral RNA. Mol. Cell. 2020;80:1055–1066. doi: 10.1016/j.molcel.2020.10.034. e1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zandi M., Shafaati M., Kalantar-Neyestanaki D., Pourghadamyari H., Fani M., Soltani S., Kaleji H., Abbasi S. The role of SARS-CoV-2 accessory proteins in immune evasion. Biomed. Pharmacother. 2022;156 doi: 10.1016/j.biopha.2022.113889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang X., Liu Y., Liu J., Bailey A.L., Plante K.S., Plante J.A., Zou J., Xia H., Bopp N.E., Aguilar P.V., Ren P., Menachery V.D., Diamond M.S., Weaver S.C., Xie X., Shi P.Y. A trans-complementation system for SARS-CoV-2 recapitulates authentic viral replication without virulence. Cell. 2021;184:2229–2238 e2213. doi: 10.1016/j.cell.2021.02.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y., Song W., Chen S., Yuan Z., Yi Z. A bacterial artificial chromosome (BAC)-vectored noninfectious replicon of SARS-CoV-2. Antivir. Res. 2021;185 doi: 10.1016/j.antiviral.2020.104974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zou J., Kurhade C., Xia H., Liu M., Xie X., Ren P., Shi P.Y. Cross-neutralization of omicron BA.1 against BA.2 and BA.3 SARS-CoV-2. Nat. Commun. 2022;13:2956. doi: 10.1038/s41467-022-30580-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zou J., Xia H., Xie X., Kurhade C., Machado R.R.G., Weaver S.C., Ren P., Shi P.Y. Neutralization against Omicron SARS-CoV-2 from previous non-Omicron infection. Nat. Commun. 2022;13:852. doi: 10.1038/s41467-022-28544-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No data was used for the research described in the article.