ABSTRACT
This scoping review was conducted to systematically search and chronicle scientific literature pertinent to poultry intake and human health. The protocol (uploaded to Open Science Framework, https://osf.io/2k7bj/) was conducted in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for scoping reviews guidelines. Articles with observational and experimental research, narrative and systematic reviews, and meta-analyses were included. Among 13,141 articles identified, 525 met inclusion criteria. Among these 525 articles, 212 focused on cancer morbidity and mortality; 41 on cardiovascular disease (CVD) morbidity and mortality; 52 on CVD risk factors; 32 on type 2 diabetes mellitus (T2DM) morbidity and mortality; 33 on T2DM risk factors; and 42 on body weight and body composition. An “Other” category (181 articles) included nutrient status, psychological well-being/mental health, cognition, microbiome, chronic kidney disease, nonalcoholic fatty liver disease, skin disorders, and fertility, among others. Among the 525 included articles, 366 were observational, 64 were experimental, and 76 were reviews and meta-analyses. Eighty-three percent of articles focused on adults or older adults. A paucity of research exists to support poultry as health-promoting foods, with most research only indirectly assessing poultry intake compared with other foods of interest (e.g., red meats or plant-based protein foods). No randomized controlled trials and only 1% of OBS assessed the influence of processed poultry intake on human health. In the future, the relative health effects of consuming poultry will be compared with a widening array of traditional and new protein-rich food products, necessitating the need for research to assess poultry as foods of choice. Science and health professionals, the poultry industry, and the public will benefit from new observational and experimental research to address cutting-edge scientific, public policy, and consumer topics pertinent to poultry intake and human health.
Keywords: chicken, turkey, animal-based protein sources, cancer, type 2 diabetes, T2DM, cardiovascular disease, CVD
Statement of Significance: This systematically searched scoping review chronicles literature assessing the relation between poultry intake and human health, highlights knowledge gaps, and provides future directions for poultry research.
Introduction
The Dietary Guidelines for Americans, 2020–2025 (DGA) define poultry as all forms of chicken, turkey, duck, geese, guineas, and game birds (e.g., quail and pheasant) (1). Chicken provides 13.9% of animal protein consumed in the United States and 7.2% of total protein intake, whereas turkey, duck, and other poultry provides 0.2% of animal protein, and 0.1% of total protein (2). Chicken meat is the most consumed meat in the United States per capita. The amounts of chicken and total poultry consumed in the United States have steadily increased, more than tripling since 1960 according to reports in 2021 (3), and poultry is the most consumed animal meat worldwide (4).
The US public generally considers poultry meat as a healthy food, because poultry provides high-quality protein and other nutrients and is often lower in fat than meat products from other animal sources. Additionally, poultry meat is reasonably affordable and accessible, leading to high rates of consumption globally. The DGA recommend consuming protein foods, including poultry, as core foods of healthy omnivorous eating patterns. The DGA specify that poultry is a nutrient-dense food when prepared with little added sugar, saturated fat, or sodium. The DGA also specify that most poultry intake should be fresh, frozen, or canned, and should be lean cuts, like chicken breast or ground turkey. Consumption of processed poultry products, like cold cuts and sausages, should be kept to a minimum (1).
The forms of poultry consumed by Americans, however, are not necessarily in line with the guidance provided by the DGA. According to NHANES results from 2007–2010, whole pieces of chicken were the number 1 source of total protein intake (7.2% of total protein intake), with no specification of cooking method (2). Cold cuts and cured meats, including poultry, accounted for 3.6% of an adult's total protein intake. NHANES results from 2015–2016 further underscore the difference between the DGA poultry recommendations and actual intakes of American adults: 19.2% of total poultry, and 22.3% of chicken consumed in the United States were purchased from fast-food restaurants (2).
Rigorous scientific assessments to bolster the claim that poultry is “healthy” are not abundant. Although primary research articles have included assessments of how poultry consumption influences various facets of human health, a systematic search of the literature designed to chronicle the body of knowledge is lacking. Due to the discrepancy between the DGA recommendations and actual poultry intake, chronicling the types of poultry (including processing and cooking methods) assessed in the literature is of great interest. A scoping review compiling articles regarding the relation between and effects of consuming various poultry products on human health outcomes is warranted.
The purpose of this scoping review is to chronicle literature regarding poultry intake and human health outcomes, to identify areas of poultry research that are lacking, and to provide a research perspective on the current state of research regarding poultry intake for human health. This review does not present the article results, nor does it assess the quality of included literature.
Methods
Protocol
The protocol for this scoping review was uploaded to Open Science Framework (https://osf.io/2k7bj/) and was conducted in accordance with PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) extension for scoping reviews (PRIMSA-ScR) recommended guidelines for developing and reporting the evidence reviewed for this article (5). This scoping review includes articles containing results from observational (OBS) studies and randomized control trials (RCTs). This review also includes review articles (including narrative and literature reviews), and systematic reviews and/or meta-analyses of OBSs or RCTs that assessed associations between or effects of, respectively, poultry intake on human health.
Identifying the research questions
What scientific literature currently exists that is pertinent to poultry intake and human health?
What are current knowledge gaps based on quantity of articles?
Search strategy, article selection process, and data extraction
For this scoping review, the term “article” refers to a publication identified via the search process. Potentially eligible articles were identified via a systematic search of 4 electronic health research databases [PubMed, Cochrane Library, CINAHL (EBSCO), and Scopus] from inception up to March 4, 2020. The search did not include ongoing research. A health sciences librarian (JBR) in collaboration with other review team members developed the database search strategies (Supplemental Table 1). There were 4 total reviewers (AWB, CMC, GC, and REC); 2 reviewers independently assessed eligibility of each abstract using Rayyan (https://rayyan.qcri.org/). A fifth reviewer (WWC) was consulted if the 4 primary reviewers could not reach consensus on article inclusion or exclusion. The reference lists of articles included were searched for additional articles that might fulfill the inclusion criteria. The inclusion and exclusion criteria are presented in Table 1.
Table 1.
Inclusion and exclusion criteria used for article selection for this scoping review on poultry intake and human health outcomes
| Included | Excluded |
|---|---|
| Any article that used a qualitative or quantitative design that assessed poultry intake and health outcomes in humans of all ages | Articles not pertaining to human health |
| Published in the English language | Not published in the English language |
| Published up to March 2020 | Gray literature |
| Both unprocessed and processed poultry products were within the scope of this review | Articles assessing dietary patterns and health outcomes without assessing poultry intake as an independent component |
| Articles assessing chicken essence intake and health outcomes were within the scope of this review | Articles assessing trends in poultry purchase correlated with trends in health outcomes. These were excluded because poultry purchasing is not synonymous with poultry consumption |
| Articles assessing “white meat” intake without defining “white meat” | |
| Articles with a definition of white meat that included rabbit or other nonpoultry meats in the definition | |
| Articles that could not be accessed after contacting the authors |
The article selection and data extraction processes consisted of the following 3 stages: 1) potential eligibility based on information provided in the title and abstract, 2) confirmation of eligibility based on information provided in the purpose statement of the full text of qualified abstracts, and 3) data extraction from full-text articles if deemed qualified. The predetermined information extracted from all qualified full-text articles is shown in Table 2. A given article could fall within the parameters of multiple general health outcomes.
Table 2.
Data extracted from the articles that met the inclusion criteria for this scoping review on poultry intake and human health outcomes1
| Data extracted | Selections designateda priori to data extraction |
|---|---|
| Author | N/A |
| Journal of publication | N/A |
| Year of publication | N/A |
| Geographical location of research | North America, South America, Europe, Eastern Asia, Western Asia, Africa, and/or Australia/New Zealand, or not reported |
| General health outcome | Body composition, CVD, T2DM, cancer, and or/other, or not reported |
| Specific health outcome | N/A |
| Purpose statement as reported by authors at the end of the introduction | N/A |
| Article design | Observational case-control, observational nested case-control, observational cohort, observational cross-sectional, acute feeding RCT, chronic feeding RCT, narrative or literature review, systematic review, meta-analysis without a systematic search (including data pooled from multiple articles), or meta-analysis with systematic search |
| Age of participants | Children, adults, and/or older adults (≥50 years of age), or not reported |
| Sex of participants | Male, female, both, or not reported |
| Race of participants | White, Asian, Black/African American, American Indian/Alaskan Native, Native Hawaiian/other Pacific Islander, not reported |
| Ethnicity of participants | Hispanic/Latino, not Hispanic/Latino, not reported |
| Health status of participants | Healthy, cancer, heart disease, brain disorders (including mental illness as well as cognitive health problems), diabetic, and/or other, or not reported |
| BMI status of participants | Underweight, normal weight, overweight, and/or obese, or not reported Note: If the included range of BMIs of the population was not reported, the average BMI of the population was extracted |
| Poultry intake as an a priori independent variable or not | Yes, no |
| Description of type of poultry | Poultry, chicken, turkey, and/or other, or not reported |
| Description of cooking method | Baked, grilled, barbecued, fried, and/or other, or not reported |
| Skin on poultry | Yes, no, or not reported |
| Comments | Indicated whether processed poultry was assessed, other relevant comments |
Data were extracted in Microsoft Excel using predetermined selections for each category unless otherwise noted as N/A. N/A designates that data were extracted without preset options. CVD, cardiovascular disease; RCT, randomized controlled trial; T2DM, type 2 diabetes mellitus.
The data from each article were independently extracted by 2 reviewers and cross-checked to ensure accuracy. Article authors were contacted for additional information if required. Risk of bias for included articles was not assessed, and strength of evidence was not graded because the purpose of this scoping review was to systematically search and chronicle the body of existing searchable literature pertinent to poultry intake and human health and to identify knowledge gaps. The extracted data from each included article are presented in an Excel file in Supplemental Table 2. The data were then assessed to determine the number of articles pertaining to general and specific health outcomes, stratified by study design.
Results
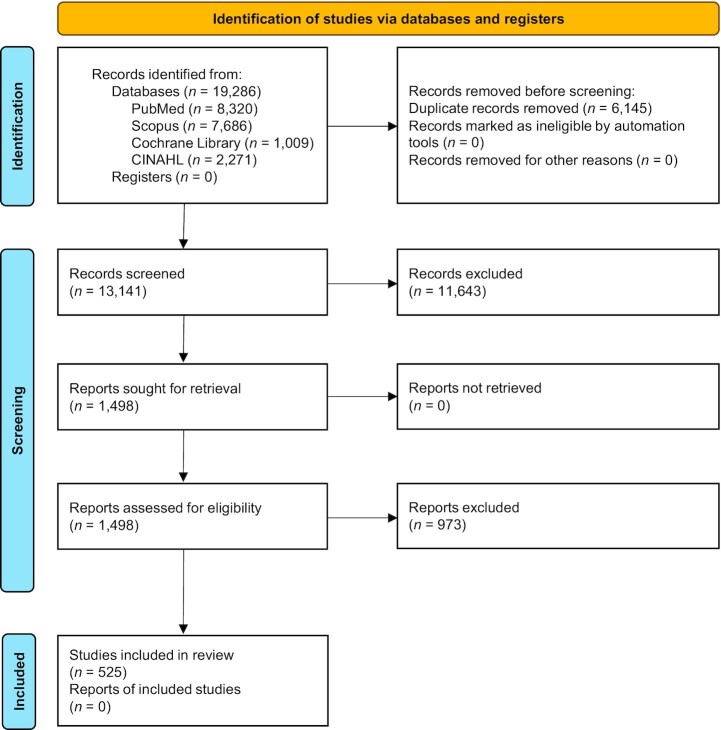
Information extracted from each article, including author names, publication date, PubMed ID number, and all predetermined data (see Table 2), is provided in an Excel file in Supplemental Table 2. Five hundred twenty-five articles met the inclusion criteria (Figure 1). Most articles (83.0%) assessed poultry intake and health outcomes in adults and older populations. Three percent were conducted in children, adolescents, and adults, 8% were conducted in children or adolescents, and 5% did not report the age of participants. The types of article designs and general health outcomes of the included articles are presented in Table 3. Of the 525 included articles, 70% of OBSs, 12% were RCTs, 7% were narrative reviews/literature reviews (NR/LRs), 4% were other, 3% included both systematic reviews with meta-analysis (SR/MAs), 3% were meta-analyses, and 1% were systematic reviews.
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram for this systematically searched scoping review assessing effects of poultry consumption on all facets of human health.
Table 3.
The included articles as designated by experimental design and health outcomes from studies with humans of all ages1
| Health outcomes | |||||||
|---|---|---|---|---|---|---|---|
| Experimental design | Body composition | Cancer morbidity/mortality | CVD risk factors | CVD morbidity/mortality | Diabetes risk factors | Diabetes morbidity/mortality | Other |
| Total articles | 42 | 212 | 52 | 41 | 33 | 32 | 181 |
| OBS | 32 | 164 | 27 | 31 | 16 | 25 | 111 |
| Case-control | 5 | 93 | 0 | 4 | 0 | 1 | 19 |
| Nested case-control | 0 | 7 | 1 | 2 | 0 | 1 | 1 |
| Cohort | 8 | 56 | 12 | 20 | 6 | 18 | 37 |
| Cross-sectional | 19 | 8 | 14 | 5 | 10 | 5 | 54 |
| RCTs | 8 | 0 | 18 | 0 | 13 | 0 | 37 |
| Acute feeding | 0 | 0 | 1 | 0 | 8 | 0 | 15 |
| Chronic feeding | 8 | 0 | 17 | 0 | 5 | 0 | 22 |
| NR/LRs | 1 | 18 | 4 | 8 | 2 | 5 | 13 |
| SRs | 0 | 4 | 0 | 0 | 0 | 1 | 1 |
| MAs | 1 | 13 | 0 | 1 | 0 | 1 | 0 |
| SR/MAs | 0 | 10 | 3 | 1 | 2 | 0 | 3 |
| Other | 0 | 3 | 0 | 0 | 0 | 0 | 16 |
CVD, cardiovascular disease; MA, meta-analysis; NR/LR, narrative review/literature review; OBS, observational study; RCT, randomized controlled trial; SR, systematic review; SR/MA, systematic review with meta-analysis.
Body composition
Forty-two articles contained assessments of relations between poultry intake and body composition indexes. The specific outcomes for body composition were primarily BMI and various anthropometric measurements. Ten articles contained measures of skeletal muscle and/or bone. Thirty-two articles were OBS (5 case-control, 8 cohort, 19 cross-sectional) in design. Eight articles were chronic feeding RCTs. One NR/LR described the relation between food intake and BMI in various Hawaiian ethnic groups. One meta-analysis examined associations between food and beverage groups and a myriad of health outcomes, including overweight and obesity.
Cancer morbidity and mortality
Two hundred twelve articles contained information on relations between poultry intake and cancer morbidity and mortality. All primary literature articles (n = 164) were OBS, conducted exclusively in adult and older populations. The majority (56.6%) were case-control in design (n = 94), with 7 nested case-control, 56 cohort, and 9 cross-sectional articles. Table 4 presents the number of primary articles identified by cancer subtype.
Table 4.
Primary research articles categorized by cancer subtype assessed for this scoping review on poultry intake and human health outcomes
| Cancer subtype | Number of articles | Cancer subtype | Number of articles |
|---|---|---|---|
| Colorectal | 40 | Lymphoma | 2 |
| Breast | 29 | Rectal | 2 |
| Prostate | 11 | Non-Hodgkin lymphoma | 2 |
| Pancreatic | 10 | Thyroid | 2 |
| Colon | 9 | Oral | 2 |
| Esophageal | 9 | Ovarian | 2 |
| Lung | 9 | Squamous cell carcinoma | 1 |
| Gastric | 7 | Unilateral retinoblastoma | 1 |
| Bladder | 6 | Upper-aerodigestive | 1 |
| Endometrial | 4 | Biliary tract | 1 |
| Leukemia | 4 | Brain | 1 |
| Liver | 3 | Head and neck | 1 |
| Renal | 3 | Hypopharyngeal | 1 |
Colorectal cancer was the most studied cancer subtype. One systematic review conducted in 2000 (6) qualitatively assessed poultry consumption and colorectal cancer. Three meta-analyses were conducted—in 2009 (7), 2013 (8), and 2015 (9)—assessing poultry intake and colorectal cancer morbidity and/or mortality. Three SR/MAs have been performed, with the most recent in 2017 (10).
Systematic reviews and meta-analyses have been conducted for several other cancer subtypes: endometrial cancer [2007 (11)], ovarian cancer [2010 (12)], esophageal cancer [2013 (13) and 2014 (14)], hematological cancers [2019 (15)], breast cancer [2016 (16)], and lung cancer [2012 (17)]. Meta-analyses exist for non-Hodgkin lymphoma [2006 (18)], renal cancer [2007 (19)], prostate cancer [2016 (20)], esophageal cancer [2016 (21)], brain cancer [2019 (22)], pancreatic cancer [2012 (23)], and total cancer mortality [2018 (24)]. Systematic reviews were conducted assessing poultry intake and esophageal cancer [2018 (25)] and prostate cancer [2014 (26)]. A 2016 (27) systematic review critically evaluated existing meta-analyses examining the relation between meat consumption (including poultry) and cancer risk.
Cardiovascular disease risk factors
Fifty-two articles contained information on relations between poultry intake and cardiovascular disease (CVD) risk factors. Notable risk factors assessed were hypertension, metabolic syndrome, body composition, and lipid profiles, among others. There were 27 OBS. There was 1 acute feeding RCT assessing plasma homocysteine concentrations and vascular endothelial function after the consumption of sources of dietary protein, including chicken. Seventeen chronic feeding RCTs were identified, assessing fatty acid profiles, lipid concentrations, and BMI, among other outcomes. A meta-analysis of RCTs examining CVD risk factors was conducted in 2019 (28). Systematically searched meta-analyses were performed assessing associations between meat consumption and metabolic syndrome [2018 (29)] and hypertension [2018 (30)].
CVD morbidity and mortality
Forty-one articles contained information on relations between poultry intake and CVD morbidity and mortality. Thirty-one OBS articles (4 case-control, 2 nested case-control, 20 cohort, and 5 cross-sectional) assessed the impact of poultry consumption on risk of stroke, heart failure, acute myocardial infarction, ischemic heart disease, and coronary heart disease, among others. The majority were OBS cohort designs. Eight NR/LRs were identified pertaining to poultry intake and CVD outcomes. A 2018 (31) meta-analysis assessed the relation between poultry intake and stroke.
Diabetes risk factors
Thirty-three articles contained information on relations between poultry intake and diabetes risk factors. Sixteen OBS articles were identified, 6 cohort and 10 cross-sectional in design. OBS articles assessed BMI, plasma or serum C-reactive protein concentrations, and advanced glycation end-product concentrations. Five chronic feeding RCTs were identified, assessing effects of diets containing poultry on risk factors such as blood pressure and lipid profiles. The 8 identified acute feeding RCTs measured glycemic and insulinemic responses to various foods, including poultry.
Diabetes morbidity and mortality
Thirty-two articles contained information on relations between poultry intake and diabetes morbidity and mortality. The 25 primary articles were all OBS in design (1 case-control, 18 cohort, 5 cross-sectional, and 1 nested case-control). Twenty-two articles examined type 2 diabetes mellitus (T2DM), and 3 assessed gestational diabetes. Four NR/LRs assessed the link between various food groups and T2DM, and 1 assessed high-protein diets and diabetic kidney disease. A 2012 (32) systematic review assessed food groups and the management of diabetes. A 2019 (33) dose–response meta-analysis of prospective articles examined the relation between dietary protein intake and diabetic morbidity but did not assess poultry as an independent variable.
Other health outcomes
The Other category contained 181 articles. The health outcomes examined in these articles included nutrient status, psychological well-being/mental health, cognitive outcomes, microbiome outcomes, chronic kidney disease, nonalcoholic fatty liver disease, skin disorders, and fertility, among others. Fifteen acute feeding RCTs were in this category, assessing appetite and satiety, mood, and renal hemodynamics, among others. Twenty-one chronic feeding RCTs were identified, covering a broad range of health outcomes including cognitive function, microbiome, and nutrient status. Sixteen articles were classified as “other” in design, because they did not fit the criteria for the other article design types. These 16 articles were case articles or a summary of medical treatments. Seven articles assessed poultry intake and food protein–induced enterocolitis syndrome in infants. Thirteen NR/LRs were identified. Three examined the link between poultry consumption and food protein–induced enterocolitis syndrome, and 2 assessed fertility (both male and female). The other NR/LRs assessed the relation between poultry consumption and BMI, nonalcoholic fatty liver disease, chronic kidney disease, general health status, diabetic kidney disease, diverticulitis, and health burden. Three SR/MAs exist for chicken essence intake and cognitive function. One systematic review was conducted assessing components of diet and male fertility.
Poultry as an a priori independent variable
Of the 366 OBSs identified, 24% did not specify poultry intake as an a priori variable of interest.
Assessments of processed poultry and health outcomes
Four OBS articles (of 366) assessed the influence of processed poultry on health outcomes. These do not include articles with a definition of poultry that might have included processed poultry in the assessment of poultry and health outcomes. Of 64 identified RCTs assessing poultry intake and health outcomes, zero included assessments of processed poultry intake.
Reporting of cooking methods
Of the 366 identified OBS articles, 52 reported on cooking methods of the poultry. Fifty-five percent of RCT articles did not report on cooking methods for poultry used in trials. Of the 64 RCT articles, the proportion assessing chicken essence (a chicken-based beverage) was 14% and 86% for poultry meat and poultry products.
Discussion
To the authors’ knowledge, this is the first scoping review to systematically search for and chronicle published literature pertinent to poultry intake and all facets of human health. This scoping review followed a rigorous process and conducted the search and review according to PRISMA-ScR guidelines. By gathering searchable literature, this review identifies areas where poultry research is apparently lacking and where current knowledge gaps exist. The majority of human nutrition and health research does not specifically focus on chicken, but more broadly on poultry. Importantly, a paucity of research exists to support poultry as a health-promoting food, with most existing research indirectly assessing poultry intake compared with other foods of interest (e.g., red meats or plant-based protein foods). The influences of processed poultry on human health require investigation. The current literature review found no RCTs assessing processed poultry intake and human health outcomes. In addition, cooking methods of poultry should be reported in both RCTs and OBS to understand the role of poultry more completely in human health outcomes. This review also provides recommendations for potential areas of future research that would help elucidate the effects of consuming poultry on human health outcomes, such as body composition, CVD, diabetes, and cancer. Given the high rates of poultry consumption, with poultry being the most consumed animal meat in the United States (3) and globally (4), the scientific community and the public would benefit from the establishment of strong, sustained, research-based initiatives to address cutting-edge scientific, public policy, and consumer topics.
Poultry products can be purchased as fresh unprocessed cuts (no preservation techniques other than refrigeration or freezing) (34) or as processed items (preserved by smoking, curing, salting, and/or the addition of chemical preservatives) (1). As such, processed poultry differs from fresh poultry in sodium content, preservative addition, and sometimes macronutrient composition if fats and carbohydrates are added (35). For example, the sodium and nitrate content of processed meats can be ≤400% and ≤50% higher, respectively, compared with unprocessed meats. These are important considerations. The higher sodium content in processed meats is attributable to more than two-thirds of the associations shown between processed meats and CVD, due to higher blood pressure (36, 37). Nitrates can result in endothelial cell dysfunction, thereby increasing coagulation, inflammatory cytokines, reactive oxygen species (38), and insulin resistance (39). Accumulating evidence shows associations and the potential for processed meat to be detrimental for human health-related outcomes, such as obesity, CVD, T2DM, and some cancers (1, 40–44).
In 2015, the International Agency for Research on Cancer advised that processed meat should be considered “carcinogenic to humans.” However, typically, studies assess “processed meat” as a total of all types of meats that have been processed or specify “processed red meat”; only 1% of OBS articles identified assessed relations between processed poultry consumption and human health-related parameters. This is likely attributable to the extensive use of FFQs in OBS (45), and assessment of broad food categories (46). As such, the vast majority of published OBS lack the granularity (46) to distinguish between processed and unprocessed poultry intakes. The apparent lack of granularity also occurs because information on commonly consumed animal muscle food products does not indicate the degree and method of processing, but is more broadly categorized as processed and unprocessed (46). This lack of specification of degree of processing or preservation method might contribute to unclear or erroneous conclusions regarding poultry consumption and human health (37, 47). It is recommended that commonly consumed animal muscle foods be differentiated by degree and type of preservation method (40, 48).
Importantly, broad and inconsistent classifications of animal muscle foods exist in scientific literature, including differences between and within observational and experimental studies, and food categories and descriptions are often inconsistent with regulatory definitions (46, 48). For example, some studies classified “white meat” as including poultry and fish, and/or rabbit. Rabbit meat, which is defined as a red meat, is commonly included as poultry due to similarities in nutrient profiles (49, 50). These broad and inconsistent classifications make it problematic when trying to determine the influence of such foods on health outcomes. The commonly used classification of “white meat” that includes fatty fish, lean fish, and poultry, can lead to erroneous results such as the cardioprotective benefits of fatty fish being attributed to lean fish and poultry products also, or that the inclusion of fatty fish does not have a cardioprotective benefit. Updated guidelines on muscle food categorization and definitions, including poultry products, are needed to support human health research (46, 48).
Cooking methods were inconsistently reported in both RCTs and OBS articles. Fifty-one percent of RCTs did not provide information regarding cooking methods of the poultry consumed by participants. Moreover, only 14% of OBS articles provided any information regarding the cooking methods of poultry in their assessments. Cooking method is an important consideration, because meats cooked at a high temperature associate with adverse health outcomes, such as CVD and T2DM, and most notably cancer. High-heat cooking methods promote the formation of advanced glycation end-products, which are linked to an increased risk of cardiometabolic complications (39, 51, 52). Thus, it is important to consider cooking method when assessing health effects of consuming poultry.
We are mindful that this scoping review only contains English language literature, and given the ubiquitous consumption of poultry worldwide there could be additional research published in non-English languages. As stated, the purpose of this scoping review was to chronicle literature regarding poultry intake and human health outcomes, and therefore this review does not present the article results, nor does it assess the quality of included literature.
Future research recommendations
Based on the available evidence and results from this comprehensive systematically searched scoping review pertaining to poultry intake and all facets of human health, the following suggestions can be considered for future research:
1) Chronic feeding RCTs are warranted assessing unprocessed compared with processed poultry products or vegetarian sources of protein, including processed plant-based poultry alternatives, on cardiometabolic health outcomes in humans across the life course.
Rationale: Zero RCTs were identified that assessed the relations between processed compared with unprocessed poultry products or vegetarian sources, including processed plant-based poultry alternatives, on cardiometabolic health outcomes in humans with poultry as the a priori food of interest. The lower sodium content, as well as potentially lower fat, carbohydrate, and energy contents, of fresh compared with processed poultry could have health-promoting effects on cardiometabolic disease risk factors. Given the current scientific and consumer interest in plant-based meat alternatives, this type of research is needed to assess the relative influence of consuming these animal-based compared with plant-based foods on health.
2) OBS are warranted assessing poultry as an a priori independent variable of interest, along with processed poultry products and poultry cooking methods on human health outcomes.
Rationale: Of the 373 OBS articles identified, 24.2% did not specify poultry as an a priori independent variable of interest. Only 1% of OBS articles included an assessment of the relation between processed poultry and a human health outcome. This is important to note, because different processing methods can influence both macronutrient content (especially protein and fat contents) as well as micronutrient content (especially sodium content). In addition, only 14% of OBS articles reported the cooking method of poultry consumed. This is important information when considering poultry consumption, because the cooking method of poultry influences the formation of chemical byproducts linked to adverse health outcomes.
3) The scientific community and poultry stakeholders could benefit from systematic reviews on several health outcomes, including body composition, and CVD and T2DM-related morbidities and mortality.
Rationale: The relation between poultry consumption and body composition assessed in primary literature (19 OBS articles with poultry as an a priori independent variable examine the relation between poultry intake and BMI, overweight/obesity, and/or other anthropometric measurements in adult populations, as well as 5 RCTs) has not been systematically reviewed. This scoping review found 31 OBS articles for CVD morbidities and mortalities. A systematic review assessing the impact of poultry intake on CVD morbidity and mortality is notably absent; there is a meta-analysis and an SR/MA assessing poultry intake and stroke, but not for other CVD outcomes. Four OBS articles assess poultry intake and risk of acute myocardial infarction, 3 assess coronary heart disease, and 8 assess CVD mortality (all of which identify poultry consumption as an a priori independent variable). A systematic review of the relations between poultry intake and T2DM morbidity and mortality is merited. A 2019 meta-analysis examined only prospective articles and did not isolate poultry as an independent variable. Additionally, SR/MAs exist for hypertension and metabolic syndrome, but a systematic review including all T2DM risk factors does not exist. There are 7 acute feeding RCTs assessing glycemic and insulinemic responses to meals including poultry as well as 5 chronic feeding RCTs assessing the role of poultry in other diabetic risk factors; these could be used alongside OBS articles examining T2DM incidence using the Bradford Hill causality model to assess a causal role of poultry intake in development of T2DM.
Conclusions
The prominence of poultry, especially chicken, as protein-rich foods consumed in the United States and globally, underscores the importance of knowing how it relates to and affects human health. The main intention of this article was to provide a scoping review to inform poultry industry stakeholders, nutrition and health scientists and clinicians, and policymakers about the scientific literature available, and knowledge gaps requiring research attention. Main findings from this project were: 1) historically, little research, especially randomized diet-controlled feeding trials, has been conducted to understand associations between and effects of consuming poultry products on human health; 2) the majority of research is from OBS assessing relations between poultry intake and risks of morbidity and mortality from various types of cancer; 3) a paucity of research exists to support chicken as a health-promoting food in children; and 4) research taking into account poultry product processing and cooking methods is needed. Hopefully, the limitations and gaps in scientific evidence regarding poultry consumption and health chronicled in this scoping review will spur new research.
Supplementary Material
Acknowledgements
The authors’ responsibilities were as follows—GC, CMC, WWC: designed the research; JBR: conducted the search; GC, CMC, REC, AWB: completed article selection and data collection; GC, CMC: analyzed the data, and wrote the manuscript with editorial assistance from all coauthors; WWC: had primary responsibility for final content; and all authors: read and approved the final manuscript.
Notes
This work was supported by the National Chicken Council. The funder had no role in the design, conduct, analysis, or interpretation of this research.
Author disclosures: During the time this research was conducted, WWC received funding for research grants, travel or honoraria for scientific presentations, or consulting services from the following organizations: Beef Checkoff, Pork Checkoff, North Dakota Beef Commission, Barilla Group, Mushroom Council, and the National Chicken Council. JBR received grant support from the National Chicken Council. All other authors report no conflicts of interest.
Supplemental Tables 1 and 2 are available from the “Supplementary data” link in the online posting of the article and from the same link in the online table of contents at https://academic.oup.com/advances/.
Abbreviations used: CVD, cardiovascular disease; DGA, Dietary Guidelines for Americans; NR/LR, narrative review/literature review; OBS, observational article; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses; PRIMSA-ScR, PRISMA extension for scoping reviews; RCT, randomized controlled trial; SR/MA, systematic review with meta-analysis; T2DM, type 2 diabetes mellitus.
Contributor Information
Gavin Connolly, Department of Nutrition Science, Purdue University, West Lafayette, IN, USA.
Caroline M Clark, Department of Nutrition Science, Purdue University, West Lafayette, IN, USA.
Robyn E Campbell, Department of Nutrition Science, Purdue University, West Lafayette, IN, USA.
Adam W Byers, Department of Nutrition Science, Purdue University, West Lafayette, IN, USA.
Jason B Reed, Libraries and School of Information Studies, Purdue University, West Lafayette, IN, USA.
Wayne W Campbell, Department of Nutrition Science, Purdue University, West Lafayette, IN, USA.
References
- 1. U.S. Department of Agriculture, U.S. Department of Health and Human Services . Dietary guidelines for Americans, 2020–2025. 9th ed[Internet]. 2020; [cited July 5, 2022]. Available from:DietaryGuidelines.gov [Google Scholar]
- 2. Pasiakos SM, Agarwal S, Lieberman HR, Fulgoni VL. Sources and amounts of animal, dairy, and plant protein intake of US adults in 2007–2010. Nutrients. 2015;7(8):7058–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. National Chicken Council. Per capita consumption of poultry and livestock, 1965 to estimated 2023, in pounds [Internet]. [cited July 5, 2022]. Available from: https://www.nationalchickencouncil.org/statistic/per-capita-consumption-poultry/
- 4. Food and Agriculture Organization of the United Nations . FAOSTAT: food and agriculture data [Internet]. 2020; [cited July 5, 2022]. Available from: https://www.fao.org/faostat/en/#home
- 5. Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac Det al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73. [DOI] [PubMed] [Google Scholar]
- 6. Yoon H, Benamouzig R, Little J, François-Collange M, Tomé D. Systematic review of epidemiological studies on meat, dairy products and egg consumption and risk of colorectal adenomas. Eur J Cancer Prev. 2000;9(3):151–64. [PubMed] [Google Scholar]
- 7. Huxley RR, Ansary-Moghaddam A, Clifton P, Czernichow S, Parr CL, Woodward M. The impact of dietary and lifestyle risk factors on risk of colorectal cancer: a quantitative overview of the epidemiological evidence. Int J Cancer. 2009;125(1):171–80. [DOI] [PubMed] [Google Scholar]
- 8. Xu B, Sun J, Sun Y, Huang L, Tang Y, Yuan Y. No evidence of decreased risk of colorectal adenomas with white meat, poultry, and fish intake: a meta-analysis of OBS. Ann Epidemiol. 2013;23(4):215–22. [DOI] [PubMed] [Google Scholar]
- 9. Shi Y, Yu PW, Zeng DZ. Dose-response meta-analysis of poultry intake and colorectal cancer incidence and mortality. Eur J Nutr. 2015;54(2):243–50. [DOI] [PubMed] [Google Scholar]
- 10. Vieira AR, Abar L, Chan DSM, Vingeliene S, Polemiti E, Stevens Cet al. Foods and beverages and colorectal cancer risk: a systematic review and meta-analysis of cohort studies, an update of the evidence of the WCRF-AICR Continuous Update Project. Ann Oncol. 2017;28(8):1788–802. [DOI] [PubMed] [Google Scholar]
- 11. Bandera EV, Kushi LH, Moore DF, Gifkins DM, McCullough ML. Consumption of animal foods and endometrial cancer risk: a systematic literature review and meta-analysis. Cancer Causes Control. 2007;18(9):967–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kolahdooz F, van der Pols JC, Bain CJ, Marks GC, Hughes MC, Whiteman DCet al. Meat, fish, and ovarian cancer risk: results from 2 Australian case-control studies, a systematic review, and meta-analysis. Am J Clin Nutr. 2010;91(6):1752–63. [DOI] [PubMed] [Google Scholar]
- 13. Salehi M, Moradi-Lakeh M, Salehi MH, Nojomi M, Kolahdooz F. Meat, fish, and esophageal cancer risk: a systematic review and dose-response meta-analysis. Nutr Rev. 2013;71(5):257–67. [DOI] [PubMed] [Google Scholar]
- 14. Zhu HC, Yang X, Xu LP, Zhao LJ, Tao GZ, Zhang Cet al. Meat consumption is associated with esophageal cancer risk in a meat- and cancer-histological-type dependent manner. Dig Dis Sci. 2014;59(3):664–73. [DOI] [PubMed] [Google Scholar]
- 15. Sergentanis TN, Ntanasis-Stathopoulos I, Tzanninis IG, Gavriatopoulou M, Sergentanis IN, Dimopoulos MAet al. Meat, fish, dairy products and risk of hematological malignancies in adults - a systematic review and meta-analysis of prospective studies. Leuk Lymphoma. 2019;60(8):1978–90. [DOI] [PubMed] [Google Scholar]
- 16. Wu J, Zeng R, Huang J, Li X, Zhang J, Ho JCet al. Dietary protein sources and incidence of breast cancer: a dose-response meta-analysis of prospective studies. Nutrients. 2016;8(11):730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Yang WS, Wong MY, Vogtmann E, Tang RQ, Xie L, Yang YSet al. Meat consumption and risk of lung cancer: evidence from OBS. Ann Oncol. 2012;23(12):3163–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Dong Y, Wu G. Lack of association of poultry and eggs intake with risk of non-Hodgkin lymphoma: a meta-analysis of OBS. Eur J Cancer Care (Engl), 2017;26(5):e12546. [DOI] [PubMed] [Google Scholar]
- 19. Faramawi MF, Johnson E, Fry MW, Sall M, Zhou Y. Consumption of different types of meat and the risk of renal cancer: meta-analysis of case-control studies. Cancer Causes Control. 2007;18(2):125–33. [DOI] [PubMed] [Google Scholar]
- 20. He Q, Wan ZC, Xu XB, Wu J, Xiong GL. Poultry consumption and prostate cancer risk: a meta-analysis. PeerJ. 2016;4:e1646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Jiang G, Li B, Liao X, Zhong C. Poultry and fish intake and risk of esophageal cancer: a meta-analysis of OBS. Asia Pac J Clin Oncol. 2016;12(1):e82–91. [DOI] [PubMed] [Google Scholar]
- 22. Luo H, Sun P, He S, Guo S, Guo Y. A meta-analysis of the association between poultry and egg consumption and the risk of brain cancer. Cell Mol Biol (Noisy-le-Grand, France). 2019;65(1):14–18. [PubMed] [Google Scholar]
- 23. Paluszkiewicz P, Smolińska K, Dębińska I, Turski WA. Main dietary compounds and pancreatic cancer risk. The quantitative analysis of case-control and cohort studies. Cancer Epidemiol. 2012;36(1):60–7. [DOI] [PubMed] [Google Scholar]
- 24. Zhang Z, Chen GC, Qin ZZ, Tong X, Li DP, Qin LQ. Poultry and fish consumption in relation to total cancer mortality: a meta-analysis of prospective studies. Nutr Cancer. 2018;70(2):204–12. [DOI] [PubMed] [Google Scholar]
- 25. Castro C, Peleteiro B, Lunet N. Modifiable factors and esophageal cancer: a systematic review of published meta-analyses. J Gastroenterol. 2018;53(1):37–51. [DOI] [PubMed] [Google Scholar]
- 26. Gathirua-Mwangi WG, Zhang J. Dietary factors and risk for advanced prostate cancer. Eur J Cancer Prev. 2014;23(2):96–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Lippi G, Mattiuzzi C, Cervellin G. Meat consumption and cancer risk: a critical review of published meta-analyses. Crit Rev Oncol Hematol. 2016;97:1–14. [DOI] [PubMed] [Google Scholar]
- 28. Guasch-Ferré M, Satija A, Blondin SA, Janiszewski M, Emlen E, O'Connor LEet al. Meta-analysis of randomized controlled trials of red meat consumption in comparison with various comparison diets on cardiovascular risk factors. Circulation. 2019;139(15):1828–45. [DOI] [PubMed] [Google Scholar]
- 29. Kim Y, Je Y. Meat consumption and risk of metabolic syndrome: results from the Korean population and a meta-analysis of OBS. Nutrients. 2018;10(4):390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Zhang Y, Zhang DZ. Red meat, poultry, and egg consumption with the risk of hypertension: a meta-analysis of prospective cohort studies. J Hum Hypertens. 2018;32(7):507–17. [DOI] [PubMed] [Google Scholar]
- 31. Mohammadi H, Jayedi A, Ghaedi E, Golbidi D, Shab-Bidar S. Dietary poultry intake and the risk of stroke: a dose-response meta-analysis of prospective cohort studies. Clin Nutr ESPEN. 2018;23:25–33. [DOI] [PubMed] [Google Scholar]
- 32. Wheeler ML, Dunbar SA, Jaacks LM, Karmally W, Mayer-Davis EJ, Wylie-Rosett Jet al. Macronutrients, food groups, and eating patterns in the management of diabetes: a systematic review of the literature, 2010. Diabetes Care. 2012;35(2):434–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Fan M, Li Y, Wang C, Mao Z, Zhou W, Zhang Let al. Dietary protein consumption and the risk of type 2 diabetes: a dose-response meta-analysis of prospective studies. Nutrients. 2019;11(11):2783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Wiseman M, Cannon G, Butrum R, Martin G, Higginbotham S, Seggie Set al. Food, nutrition, physical activity, and the prevention of cancer: a global perspective. Summary. Washington (DC): World Cancer Research Fund/American Institute for Cancer Research; 2007. [Google Scholar]
- 35. Marangoni F, Corsello G, Cricelli C, Ferrara N, Ghiselli A, Lucchin Let al. Role of poultry meat in a balanced diet aimed at maintaining health and wellbeing: an Italian consensus document. Food Nutr Res. 2015;59(1):27606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Micha R, Wallace SK, Mozaffarian D. Red and processed meat consumption and risk of incident coronary heart disease, stroke, and diabetes mellitus: a systematic review and meta-analysis. Circulation. 2010;121(21):2271–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Micha R, Michas G, Mozaffarian D. Unprocessed red and processed meats and risk of coronary artery disease and type 2 diabetes–an updated review of the evidence. Curr Atheroscler Rep. 2012;14(6):515–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Förstermann U. Oxidative stress in vascular disease: causes, defense mechanisms and potential therapies. Nat Clin Pract Cardiovasc Med. 2008;5(6):338–49. [DOI] [PubMed] [Google Scholar]
- 39. Kim Y, Keogh J, Clifton P. A review of potential metabolic etiologies of the observed association between red meat consumption and development of type 2 diabetes mellitus. Metabolism. 2015;64(7):768–79. [DOI] [PubMed] [Google Scholar]
- 40. IARC Working Group on the Evaluation of Carcinogenic Risks to Humans . Red meat and processed meat. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans, No. 114. Lyon: International Agency for Research on Cancer; 2018. [Google Scholar]
- 41. Wyness L. The role of red meat in the diet: nutrition and health benefits. Proc Nutr Soc. 2016;75(3):227–32. [DOI] [PubMed] [Google Scholar]
- 42. USDA Economic Research Service . USDA agricultural projections to 2027. 2018; [cited May 20, 2020]. Available from: https://www.ers.usda.gov/publications/pub-details/?pubid=87458
- 43. Micha R, Peñalvo JL, Cudhea F, Imamura F, Rehm CD, Mozaffarian D. Association between dietary factors and mortality from heart disease, stroke, and type 2 diabetes in the United States. JAMA. 2017;317(9):912–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. World Cancer Research Fund / American Institute for Cancer Research . Continuous update project report: diet, nutrition, physical activity and stomach cancer. A global perspective. A summary of the Third Expert Report. World Cancer Research Fund International. 2018; [cited May 20, 2020]. Available from: https://www.wcrf.org/wp-content/uploads/2021/02/Summary-of-Third-Expert-Report-2018.pdf [Google Scholar]
- 45. Shim JS, Oh K, Kim HC. Dietary assessment methods in epidemiologic studies. Epidemiol Health. 2014;36:e2014009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. O'Connor LE, Gifford CL, Woerner DR, Sharp JL, Belk KE, Campbell WW. Dietary meat categories and descriptions in chronic disease research are substantively different within and between experimental and OBS: a systematic review and landscape analysis. Adv Nutr. 2019;11(1):41–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. O'Connor LE, Campbell WW. Red meat and health: getting to the heart of the matter. Nutr Today. 2017;52(4):167–73. [Google Scholar]
- 48. Gifford CL, O'Connor LE, Campbell WW, Woerner DR, Belk KE. Broad and inconsistent muscle food classification is problematic for dietary guidance in the U.S. Nutrients. 2017;9(9):1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Cavani C, Petracci M, Trocino A, Xiccato G. Advances in research on poultry and rabbit meat quality. Ital J Anim Sci. 2009;8(Suppl 2):741–50. [Google Scholar]
- 50. Dalle Zotte A. Perception of rabbit meat quality and major factors influencing the rabbit carcass and meat quality. Livest Prod Sci. 2002;75(1):11–32. [Google Scholar]
- 51. White DL, Collinson A. Red meat, dietary heme iron, and risk of type 2 diabetes: the involvement of advanced lipoxidation endproducts. Adv Nutr. 2013;4(4):403–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Ulrich P, Cerami A. Protein glycation, diabetes, and aging. Recent Prog Horm Res. 2001;56(1):1–22. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.