Abstract
Simple Summary
Metastatic pancreatic ductal adenocarcinoma (PDAC) is an aggressive malignancy that has limited treatment options. Standard of care treatment involves systemic chemotherapy, although all tumors invariably develop resistance to these cytotoxic therapies. With the advent of genomic sequencing and identification of therapeutically actionable alterations, there are subsets of patients with PDAC who may benefit from targeted therapies matched to their molecular profile. As more molecularly matched therapies are developed, precision medicine has great potential in patients with PDAC.
Abstract
The aggressive biology of pancreatic ductal adenocarcinoma (PDAC), along with its limited sensitivity to many systemic therapies, presents a major challenge in the management of patients with metastatic PDAC. Over the past decade, the incorporation of combinatorial cytotoxic chemotherapy regimens has improved patient outcomes. Despite these advances, resistance to cytotoxic chemotherapy inevitably occurs, and there is a great need for effective therapies. A major focus of research has been to identify molecularly defined subpopulations of patients with PDAC who may benefit from targeted therapies that are matched to their molecular profile. Recent successes include the demonstration of the efficacy of maintenance PARP inhibition in PDAC tumors harboring deleterious BRCA1, BRCA2, and PALB2 alterations. In addition, while therapeutic targeting of KRAS was long thought to be infeasible, emerging data on the efficacy of KRAS G12C inhibitors have increased optimism about next-generation KRAS-directed therapies in PDAC. Meanwhile, KRAS wild-type PDAC encompasses a unique molecular subpopulation of PDAC that is enriched for targetable genetic alterations, such as oncogenic BRAF alterations, mismatch repair deficiency, and FGFR2, ALK, NTRK, ROS1, NRG1, and RET rearrangements. As more molecularly targeted therapies are developed, precision medicine has the potential to revolutionize the treatment of patients with metastatic PDAC.
Keywords: pancreatic adenocarcinoma, precision medicine, targeted therapy, DNA repair inhibitors
1. Introduction
Pancreatic ductal adenocarcinoma (PDAC) is the third leading cause of cancer-related death in the United States, and is projected to become the second leading cause by 2030 [1]. The 5-year survival rate of PDAC patients is only 11%, and the poor outcomes are mainly due to its aggressive biology and advanced stage of presentation at initial diagnosis [2]. The cornerstone of treatment for this lethal disease is cytotoxic chemotherapy, and the current standard of care is largely based on clinical trials of first-line therapy initially reported in 2011 and 2013 [3,4,5,6,7,8]. In this review, we describe the current treatment paradigms for metastatic PDAC and how precision medicine is beginning to improve patient outcomes by leveraging the increased identification of molecularly-defined populations of PDAC.
2. First-Line Chemotherapy
Outcomes for patients with PDAC have improved over the last three decades with the development of effective cytotoxic chemotherapy regimens [6,7,9]. Initially, the median overall survival (OS) of patients with advanced PDAC treated with gemcitabine alone was 5.7 months, setting an ominous benchmark for future generations to improve upon [10]. Compared to gemcitabine monotherapy, multi-drug cytotoxic chemotherapy regimens have significantly improved outcomes by prolonging the OS of patients with metastatic PDAC to about 1 year. In the landmark PRODIGE trial, patients with metastatic PDAC treated with first-line FOLFIRINOX (folinic acid, 5-fluorouracil [5-FU], irinotecan, and oxaliplatin) had a median OS of 11.1 months, compared to 6.8 months for gemcitabine alone [3]. In the MPACT trial, gemcitabine/nab-paclitaxel prolonged survival to 8.5 months, compared to 6.7 months with gemcitabine alone, in previously untreated patients with advanced PDAC [4].
While the results of head-to-head investigation of FOLFIRINOX and gemcitabine/nab-paclitaxel have not been reported, many believe that FOLFIRINOX may be more potent, as cross-trial comparisons suggest it may have a higher objective response rate (31.6% versus 23%). To date, the highest reported median OS for an unselected advanced PDAC population was in the control arm of SWOG 1313, a randomized phase II trial assessing FOLFIRINOX with and without pegylated recombinant human hyaluronidase (PEGPH20). The median OS was 14.4 months in the FOLFIRINOX arm, while it was 7.7 months in the arm combining FOLFIRINOX and PEGPH20 arm [11].
The American Society of Clinical Oncology (ASCO) Clinical Practice Guidelines have endorsed the use of either FOLFIRINOX or gemcitabine/nab-paclitaxel as first-line therapy in patients with a favorable comorbidity profile and ECOG performance status of 0 or 1 [12,13,14]. The toxicity profiles of these two regimens differ significantly; therefore, patient-centered decision making is necessary [15]. While it may be more potent, FOLFIRINOX is a more challenging regimen, with a higher rate of grade 3–4 toxicities and hospitalizations. The more favorable toxicity profile of gemcitabine/nab-paclitaxel leads some patients with substantial comorbidities or desire to prioritize quality of life to elect to be treated with gemcitabine/nab-paclitaxel [16].
In an effort to maximize the tolerability and efficacy of first-line therapy, the recently reported SEQUENCE trial used a novel strategy of alternating gemcitabine/nab-paclitaxel with 5-FU, folinic acid and oxaliplatin (FOLFOX) [17]. In this randomized phase III study, alternating gemcitabine/nab-paclitaxel and FOLFOX was compared to standard gemcitabine/nab-paclitaxel in patients with previously untreated metastatic PDAC. The trial met its primary endpoint of improving OS. Patients receiving alternating gemcitabine/nab-paclitaxel and FOLFOX had a median OS of 13.2 months versus 9.7 months in patients receiving standard gemcitabine/nab-paclitaxel. The ORR for the alternating combination was 39.7% versus 20.3% for gemcitabine/nab-paclitaxel. Notably, there were significantly more hematologic toxicities in patients receiving alternating gemcitabine/nab-paclitaxel and FOLFOX, along with a higher incidence of treatment-emergent neuropathy. The results from this trial suggest that alternating regimens may slow the development of acquired chemotherapy resistance; however, this approach needs further study before it can be adopted into the current treatment paradigm for metastatic PDAC.
3. Second-Line Chemotherapy
Several randomized phase III trials have investigated second-line cytotoxic chemotherapy regimens after progression on first-line gemcitabine-based chemotherapy. The use of 5-FU and oxaliplatin has shown mixed results. The CONKO-003 evaluated second-line oxaliplatin, 5-FU, and folinic acid (OFF regimen) versus 5-FU/Leucovorin in advanced PDAC [18]. Compared to patients receiving second-line 5-FU/Leucovorin, patients receiving OFF experienced improved OS (median OS 5.9 months versus 3.3 months) and PFS (median PFS 2.9 months versus 2.0 months). However, in the PANCREOX trial investigating a different dosing regimen of second-line folinic acid, 5-FU, and oxaliplatin (mFOLFOX6) versus 5-FU/Leucovorin, the primary endpoint of PFS was not met (median PFS 3.1 months versus 2.9 months, respectively), and median OS was actually reduced in patients treated with mFOLFOX6 compared to patients treated with 5-FU/Leucovorin (6.1 months versus 9.9 months) [19]. Recent clinical trials using second-line mFOLFOX6 as a comparator arm have demonstrated consistent outcomes, with median PFS of 2–3 months and median OS of 6–7 months [20,21].
Trials evaluating second-line irinotecan-containing regimens have demonstrated similar levels of modest efficacy. The NAPOLI-1 trial evaluated nanoliposomal irinotecan (Nal-IRI) combined with 5-FU/Leucovorin, compared to 5-FU/Leucovorin alone. Nal-IRI/5-FU was superior to 5-FU/Leucovorin, improving median OS (6.1 months versus 4.2 months), median PFS (3.1 months versus 1.5 months), and the ORR (16% versus 1%) [22]. A randomized phase II trial, SWOG S1513, assessed whether the addition of the poly (adenosine diphosphate-ribose) polymerase (PARP) inhibitor veliparib would enhance the effectiveness of second-line FOLFIRI in metastatic PDAC. While SWOG S1513 was stopped early for futility, because veliparib did not increase the effectiveness of FOLFIRI, results from this trial suggest that FOLFIRI has similar activity to Nal-IRI/5-FU. Patients treated on the FOLFIRI arm of SWOG S1513 had a median PFS of 2.9 months and a median OS of 6.5 months [23].
Contrary to the large number of published phase III trials assessing therapies after progression while on gemcitabine-based therapy, there are relatively few studies on the use of therapies after progression on 5-FU based therapies [15,24,25]. However, emerging data suggest that the efficacy of second-line gemcitabine/nab-paclitaxel is very similar to the efficacy of second-line 5-FU based regimens. Although it was a negative trial, a randomized phase II trial investigating the use of second-line gemcitabine/nab-paclitaxel with and without a MUC5AC antibody provided efficacy benchmarks of second-line gemcitabine/nab-paclitaxel [25]. In this trial, the median OS for patients receiving second-line gemcitabine/nab-paclitaxel alone was 6.6 months; the median PFS was 2.7 months; and the ORR was 3% [25]. The phase III Trybeca-1 trial, which evaluated second-line chemotherapy (investigator choice) with or without eryaspase, had similar efficacy results. In the Trybeca-1 trial, patients who received second-line gemcitabine/nab-paclitaxel had a median OS of 6.9 months and median PFS of 3.5 months [24].
4. Biomarker-Driven Therapy
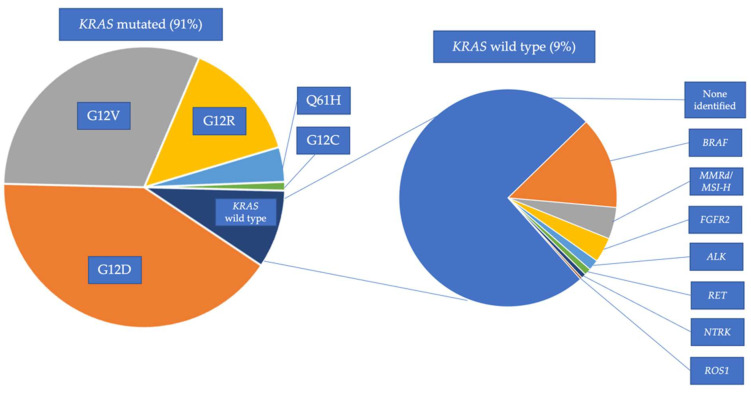
Given the impressive results of precision medicine using molecularly targeted therapy in other malignancies, there have been significant efforts to target oncogenic alterations in PDAC [26]. However, a major obstacle has been that the most frequently observed molecular alterations in PDAC have historically been undruggable. More than 90% of PDACs harbor an oncogenic Kirsten rat sarcoma virus (KRAS) mutation [27]. Other common oncogenic alterations in PDAC include tumor suppressor genes, such as CDKN2A, TP53, and SMAD4 [27,28]. While this mutational profile presents a clinical challenge, optimism for targeted therapy in PDAC is rising with the identification of molecularly defined subpopulations of PDAC that appear to be sensitive to targeted therapies. For instance, while KRAS is notoriously difficult to target, PDACs lacking KRAS mutations (KRAS wild type [WT] PDAC) frequently harbor targetable alterations, such as NTRK, FGFR2, ALK, RET, NRG1, and ROS1 fusions, as well as oncogenic BRAF alterations (Figure 1).
Figure 1.
Oncogenic driver alterations in KRAS-mutated and KRAS wild-type PDAC. The proportion of KRAS mutations in PDAC include KRAS G12D (41%), G12V (31%), G12R (14%), Q61H (4%), G12C (1%), and KRAS wild-type (WT) (9%) [29,30]. Actionable alterations in KRAS WT patients in PDAC and pancreatic acinar cell carcinoma include: BRAF alterations (13.7%), MMRd/MSI-H (4.7%), FGFR2 fusions (3.5%), ALK fusions (1.6%), RET fusions (1%), NTRK fusions (0.7%), and ROS1 fusions (0.3%). Frequencies of genomic alterations in KRAS WT were derived from Philip et al. and Singhi et al. [29,30].
In addition, there is significant enrichment of mismatch repair deficiency in KRAS WT PDAC [29]. Beyond KRAS WT PDAC, approximately 10% of PDACs have a deficiency in the homologous recombination (HR) DNA repair pathway, with inactivating germline or somatic mutations in BRCA1, BRCA2, and PALB2 [27]. The “Know Your Tumor” platform identified targetable alterations in 26% of PDAC tumors [31]. In a retrospective analysis, those who received molecularly matched targeted therapy had improved OS (median OS 2.6 years versus 1.5 years) compared to those who received unmatched therapies. Many of these targeted therapies hold FDA approval for tumors other than PDAC (Table 1). These data support the hypothesis that precision medicine has a role in the treatment of PDAC and should continue to be validated prospectively.
Table 1.
Recommended FDA-approved targeted therapy options for PDAC.
| Recommended FDA-Approved Targeted Therapies in PDAC | |
|---|---|
| Molecular Target | Drug Name |
| gBRCA1/2 mutations | Olaparib |
| Tumor agnostic FDA-approved targeted therapies | |
| Molecular Target | Drug Name |
| MSI-H/MMRd | Pembrolizumab |
| BRAF V600E | Dabrafenib/Trametinib |
| NTRK fusions | Larotrectinib, Entrectinib |
| RET fusions | Selpercatinib |
| Therapies that are FDA-approved in other tumors | |
| Molecular Target | Drug Name |
| KRAS G12C | Sotorasib, Adagrasib |
| FGFR2 fusions | Pemigatinib |
| ALK fusions | Crizotinib, Alectinib |
| ROS1 fusions | Entrectinib, Crizotinib |
| sBRCA1/2, gPALB2/sPALB2 1 | Niraparib, Olaparib, Rucaparib |
1 s: somatic; g: germline.
4.1. Homologous Recombination Deficiency
Double-strand DNA breaks are repaired by the homologous recombination (HR) repair pathway, and deficiency of this DNA repair pathway confers sensitivity to platinum chemotherapy and PARP inhibitors in multiple cancers [32,33]. Since approximately 17 genes are involved in the HR pathway, it is helpful to distinguish between core HR genes (BRCA1, BRCA2, PALB2) and the other non-core HR genes. Deleterious alterations in core HR genes are well-established markers of sensitivity to PARP inhibitors and platinum chemotherapy. Alternatively, while deleterious alterations in some non-core HR genes, like RAD51C, have been reported to impart PARP inhibitor sensitivity in ovarian cancer, the impact of other non-core HR genes is less clear [34]. Deleterious alterations in core HR genes occur in 10–12% of PDAC patients, while deleterious alterations in non-core HR genes are found in approximately 7% of PDACs [27,35]. Multiple studies have demonstrated that PDAC patients with mutations in a core HR gene have enhanced sensitivity to platinum chemotherapy, leading to improved PFS, compared to HR-proficient PDACs, when they are treated with first-line platinum-based chemotherapy [31,36,37,38].
A phase II trial evaluating gemcitabine/cisplatin with or without the PARP inhibitor veliparib in PDAC patients with germline BRCA1, BRCA2, or PALB2 mutations highlights the enhanced platinum-sensitivity in HR-deficient PDAC [39]. While veliparib did not improve the effectiveness of first-line gemcitabine/cisplatin, the trial clearly demonstrated the impressive efficacy of gemcitabine/cisplatin in HR-deficient PDAC. Patients treated in this trial with gemcitabine/cisplatin achieved a median OS of 16.4 months, median PFS of 9.7 months, and an ORR of 65.2%. Interestingly, in a separate trial studying an unselected population of patients with PDAC, gemcitabine/cisplatin did not statistically improve OS or ORR compared to gemcitabine alone [40]. There are no trials comparing gemcitabine/cisplatin to FOLFIRINOX in HR-deficient PDAC, although either is reasonable in PDAC tumors with deleterious mutations in BRCA1, BRCA2, or PALB2.
PARP inhibitors have shown significant efficacy in multiple HR-deficient tumors, with a toxicity profile more favorable than cytotoxic chemotherapy [41,42]. An important lesson from other malignancies, which has also proven true in PDAC, is that PARP inhibitors are only efficacious in platinum-sensitive tumors. This insight led to the design of the POLO trial, where maintenance olaparib versus placebo was studied in patients with PDAC with deleterious germline BRCA1 or BRCA2 mutations who had no evidence of disease progression following at least 16 weeks of platinum-based chemotherapy. The trial met its primary endpoint of improving PFS (7.4 months versus 3.8 months, olaparib versus placebo), but did not demonstrate a statistically significant improvement in OS [43,44]. On the basis of the POLO trial, the FDA approved maintenance olaparib in PDAC patients with germline BRCA mutations. However, a major question in the field is whether other PDAC patients can benefit from maintenance PARP inhibition. A phase II trial evaluating maintenance rucaparib in PDAC with deleterious germline or somatic BRCA1, BRCA2, and PALB2 mutations who did not progress on first-line platinum-based chemotherapy also demonstrated encouraging results, with a median PFS of 13.1 months [45]. These results suggest that maintenance PARP inhibition is a reasonable therapeutic strategy in this patient population [45,46]. Interestingly, a recent study demonstrated impressive efficacy of a maintenance strategy using the CTLA4 inhibitor ipilimumab combined with the PARP inhibitor niraparib in patients who had not progressed on platinum-based chemotherapy and tumors without an underlying BRCA1/2 or PALB2 mutation [47]. This may prove to be an effective maintenance strategy, but further investigation is needed.
4.2. KRAS Mutated PDAC
While the KRAS gene is mutated in approximately 14% of all human cancers, PDAC is the prototypical KRAS mutated malignancy, as over 90% of PDACs harbor a KRAS mutation [48]. KRAS is a GTPase that activates downstream effector proteins of the mitogen-activated protein kinase (MAPK) pathway [49]. Genomic studies investigating the frequency of different KRAS mutated alleles in PDAC have demonstrated the following distribution of KRAS mutations: G12D (41%), G12V (31%), G12R (14%), Q61H (4%), and G12C (<1%) [27,30]. Translational studies exploring patient outcomes and co-mutational patterns have begun to reveal differences amongst tumors harboring different KRAS mutation alleles (Figure 1) [50,51]. Patients with PDAC harboring a KRAS G12D mutation have decreased OS compared to PDAC patients with mutations in other KRAS alleles. Interestingly, PDAC with KRAS G12R mutations are more likely to harbor deleterious HR gene alterations and PI3-kinase pathway mutations [52,53].
In an encouraging step forward, KRAS G12C has been successfully targeted in PDAC patients with the direct irreversible KRAS G12C inhibitors sotorasib and adagrasib [54,55]. The CodeBreaK100 study was an open-label phase I/II clinical trial investigating the role of sotorasib in previously treated solid tumors harboring KRAS G12C mutations, including 38 patients with metastatic PDAC [54]. In the PDAC cohort, the ORR was 21%; the disease control rate (DCR) was 84%; the median PFS was 4.0 months; and the median OS was 6.9 months [54]. The drug was well-tolerated, with only 5.3% of patients experiencing grade 3 diarrhea or fatigue. The KRYSTAL-1 study was a multicohort phase I/II clinical trial investigating the role of adagrasib, another covalent irreversible KRAS G12C inhibitor, in advanced gastrointestinal cancers [55]. In a preliminary analysis of 10 evaluable PDAC patients enrolled on KRYSTAL-1, remarkably, 5 PDAC patients achieved a partial response, with a median duration of response of 7 months, and the other five patients had stable disease, yielding a median PFS of 6.6 months [55]. Overall, adagrasib was well to-erated. Gastrointestinal toxicity was the most common adverse event, while fatigue and QTc prolongation were the most common grade 3–4 toxicities.
There are currently no FDA-approved KRAS inhibitors available for patients with PDAC outside a clinical trial. However, the success of KRAS G12C inhibitors has inspired optimism that KRAS-directed therapy in PDAC is feasible, and investigational agents, such as KRAS G12D inhibitors, SOS inhibitors, and pan-RAS inhibitors, are being actively developed. Encouraging preclinical data have been presented on the KRAS G12D inhibitor MRTX1133 and the pan-RAS inhibitor RMC-6236 [56,57]. MRTX1133 is a non-covalent small molecule inhibitor that binds to GDP-loaded KRAS G12D and leads to impressive anti-tumor activity in KRAS G12D-mutated murine models [57]. RMC-6236 inhibits all RAS isoforms (i.e., K-, H-, and NRAS) by acting as a molecular glue to promote the binding RAS proteins to the cyclophilin A chaperone protein. Stable formation of the RAS/cyclophilin A complex inhibits the ability of RAS to activate downstream MAPK effectors. The RMC-6236 pan-RAS inhibitor demonstrated striking anti-tumor activity, with several complete responses, in murine KRAS-mutated xenografts [56].
In addition to targeted therapy approaches, immunotherapeutic strategies utilizing KRAS-directed vaccines and T-cell directed therapies are also being developed [28,58]. The potential of this approach was highlighted in a case report of a patient with KRAS G12D-mutated PDAC, who had a lung-only metastasis and experienced a partial response (72% tumor regression) following infusion of autologous T cells that were engineered to express HLA-C*08:02–restricted T-cell receptors (TCRs) targeting oncogenic KRAS G12D [59]. This demonstration of TCR-directed therapy in PDAC highlights the potential for broader application of immunotherapeutic approaches in this cancer, which has historically been resistant to immunotherapy [60].
4.3. KRAS Wild-Type (WT) PDAC
Given the historic difficulties in targeting KRAS, increasing attention has been given to KRAS WT PDAC [29,61]. In addition to being enriched for mismatch repair-deficient tumors, multiple reports have demonstrated that KRAS WT PDAC can harbor oncogenic BRAF alterations and gene fusions of ALK, RET, ROS1, NRG1, FGFR2, and NTRK [29,61,62,63]. KRAS WT PDAC is more common in younger patients and appears to have longer OS compared to patients with KRAS-mutated PDAC [29,61]. Interestingly, genomic studies have also observed that KRAS WT PDAC has a higher frequency of cancers that are ATM-mutated and TP53 WT [61,64,65]. However, given the rare incidence of KRAS WT PDAC, data regarding therapeutic targeting in patients is sparse.
The NOTABLE study provided proof-of-concept that KRAS WT PDAC is susceptible to molecularly targeted therapy [66]. The NOTABLE study was a randomized, double-blinded, phase III clinical trial conducted in China that investigated the role of gemcitabine combined with nimotuzumab, a humanized anti-epidermal growth factor receptor (EGFR) antibody, compared to gemcitabine monotherapy as first-line treatment for KRAS WT advanced PDAC [66]. Median OS was significantly improved at 10.9 months with gemcitabine/nimotuzumab compared to 8.5 months with gemcitabine alone. Median PFS was 4.2 months with gemcitabine/nimotuzumab compared to 3.6 months with gemcitabine alone. Clinically, although there was a slight improvement in OS in the NOTABLE study, it is difficult to put the results of this trial into context. since it did not include a modern chemotherapy regimen, such as FOLFIRINOX or gemcitabine/nab-paclitaxel.
4.4. BRAF Alterations
Activating mutations in BRAF activate downstream signaling in the MAPK pathway and targeting BRAF V600E class 1 mutations with BRAF-targeted therapy has proven effective in multiple malignancies [27,67,68]. In a report analyzing PDAC and pancreatic acinar cell carcinomas, oncogenic BRAF alterations accounted for 13% of the KRAS WT tumors [29]. Differing from the experience in melanoma, BRAF V600E mutations only accounted for 20–30% of the BRAF alterations seen in PDAC and pancreatic acinar cell carcinomas [27,29,65]. Other BRAF alterations included BRAF exon 11 insertion-deletion mutations (INDELs) and BRAF fusions. Clinical experience targeting BRAF alterations in pancreatic cancer is limited [27]. In a retrospective case series of PDAC and acinar cell carcinoma, two patients with BRAF V600E mutations achieved a partial response on combined BRAF/MEK inhibition [69]. In the same cohort of patients, there were responses to MEK inhibitor monotherapy in the BRAF fusion and BRAF INDEL subgroups, but survival outcomes were not reported due to the uncontrolled nature of the case series [27].
4.5. FGFR2 Fusions
Fibroblast growth factor receptor-2 (FGFR2) fusions account for 3.5% of the genomic alterations KRAS WT PDAC and pancreatic acinar cell carcinoma [29,70]. FGFR2 receptors typically become activated when its ligand, fibroblast growth factor, promotes FGFR2 dimerization. Fusion partners in FGFR2 translocations have intracellular dimerization domains that promote constitutive FGFR2 activation, resulting in downstream activation of the MAPK pathway [71,72]. While therapeutic targeting of FGFR2 translocations has been efficacious in intrahepatic cholangiocarcinoma, clinical experience in targeting of these alterations in PDAC is very limited. In the FIGHT-101 trial, a patient with KRAS WT PDAC harboring an FGFR2-USP33 fusion achieved a partial response to pemigatinib that was maintained for 10.7 months before disease progression [73]. A recent case series described four KRAS WT PDAC patients with FGFR2 fusions who benefited from an undisclosed FGFR2 inhibitor on an unpublished clinical trial [74]. Three of the patients with KRAS WT PDAC benefited from the use of an FGFR inhibitor for at least 6 months [74]. The most common side effects with FGFR inhibitors are hyperphosphatemia, cutaneous toxicities, and ocular toxicities, although these toxicities are manageable with dose and schedule modifications.
4.6. ALK Fusions
Anaplastic lymphoma kinase fusion (ALK) gene-rearrangement proteins promote tumor growth and cell survival by activating intracellular signaling cascades, including the MAPK pathway [75,76]. Therapeutic targeting of ALK fusions with small molecule inhibitors has been successful in other malignancies, such as lung cancer and anaplastic large cell lymphoma [77,78,79,80]. ALK fusions are seen in approximately 2.5% of KRAS WT PDAC, and recent reports have shown promising efficacy of ALK inhibitors in ALK-rearranged PDAC [77,81,82]. A case series of KRAS WT metastatic PDAC harboring ALK rearrangements described four patients who benefitted from ALK-directed therapy, with two of these patients being on therapy for over 1 year [83]. In a separate case series, five patients with KRAS WT PDAC harboring ALK rearrangements received ALK-directed therapy [84]. In this case series, a response to therapy was seen in one PDAC patient treated with crizotinib and one PDAC patient treated with alectinib [84]. Treatment with ALK inhibitors is generally well-tolerated, although gastrointestinal and pulmonary toxicities have been reported [78,82,85].
4.7. NTRK Fusions
The tropomysin receptor kinase (TRK) family of receptors are stimulated by binding to their ligand, neurotrophins, causing receptor dimerization and activation of downstream signaling pathways [86]. NTRK fusions of the genes that code for TRK receptors (NTRK1-3) encode proteins that lead to dimerization and constitutive receptor activity [86]. NTRK fusions occur in 1–3% of KRAS WT PDAC. In a pooled analysis of three tumor agnostic clinical trials for patients with NTRK fusions, there were two patients with NTRK-rearranged PDAC, and one of these patients had a partial response to the NTRK inhibitor larotrectinib [87]. In another case report, a KRAS WT PDAC patient with a CTRC-NTRK1 fusion responded to larotrectinib for 6 months prior to developing acquired resistance [88]. In a separate meta-analysis of three clinical trials investigating the NTRK inhibitor entrectinib, three patients with PDAC harboring NTRK rearrangements were treated; two of these achieved a partial response [89]. NTRK inhibitors are well-tolerated, and most adverse events are grade 1–2, including fatigue, nausea, neurologic events (cerebellar ataxia, cognitive disorder, and dizziness), weight gain, and anemia [62,87,88,89]. Both entrectinib and larotrectinib have tumor agnostic FDA approval for NTRK rearranged tumors.
4.8. NRG1 Fusions
Neuregulin 1 (NRG1) is a soluble ligand that ordinarily is released from cells and acts as a paracrine messenger [90,91]. NRG1 binds to HER3, promoting HER2/HER3 dimerization and PI3K/AKT/mTOR signaling [90,91]. NRG1 fusions are oncogenic drivers in PDAC and account for 1.3% of KRAS WT cases [63,92]. Mechanistically, NRG1 fusion proteins tether the NRG1 to the plasma membrane, resulting in hyperactivation of HER3 [90,91]. Zenocutuzumab, an investigational bispecific antibody targeting HER2 and HER3, has shown promising efficacy in patients with KRAS WT PDAC with NRG1 fusions [93]. In a phase II clinical trial investigating zenocutuzumab monotherapy, there was a 42% ORR in the 19 patients with KRAS WT PDAC patients harboring a NRG1 rearrangement [93]. In all patients, median time to response was 1.8 months and duration of response was 9.1 months. The toxicity profile of zenocutuzumab was generally favorable, although there was one grade 5 hypersensitivity reaction. The most common grade ≥ 3 adverse events were fatigue (4%), dyspnea (4%), anemia (3%), and liver test abnormality (3%). Afatinib, a pan-ERBB inhibitor, is also being explored in NRG1 fusion-associated PDAC [63,92]. There have been published reports of two patients with PDAC with NRG1 rearrangements responding to afatinib, and clinical trials of this agent are ongoing [63,92].
4.9. RET Fusions
The RET proto-oncogene encodes for a transmembrane receptor tyrosine kinase involved in embryonic development of the nervous system and kidneys [94]. RET fusions lead to aberrant activation of RET receptor tyrosine kinase and constitute 1.3% of KRAS WT PDAC [29]. In the LIBRETTO-001 phase I/II basket trial, 12 patients with PDAC harboring a RET rearrangement were enrolled and treated with the RET-specific inhibitor selpercatinib [95]. The patients on the trial had a 55% ORR, with a range of response duration from 2.5 months to 38.3 months. Approximately 38% of patients had at least one grade 3 adverse event (AE), which included mostly liver test abnormalities. In the ARROW phase I/II clinical trial investigating the RET inhibitor pralsetinib in solid-tumor patients with RET rearrangements, nine patients with PDAC were enrolled [94]. All four patients who were evaluable had an objective response (3 PRs and 1 CR with a treatment duration of 33.1 months) [94]. In the evaluable group of all solid tumor patients, the ORR was 57%, with a median duration of response of 11.7 months. On the trial, 69% of patients experienced grade ≥3 treatment-related adverse events. The most common grade ≥3 toxicities were neutropenia, anemia, and liver test abnormalities requiring dose interruptions (59%) or dose reductions (45%). Selpercatinib has been granted a tumor agnostic FDA-approval for treatment of RET-fusion positive tumors.
4.10. ROS1 Alterations
The ROS1 gene encodes for a receptor tyrosine kinase that is closely related to ALK. It is a transmembrane protein with an intracellular tyrosine kinase domain and large extracellular domain [96]. ROS1 fusions are rare subsets of KRAS WT PDAC accounting for less than 1% of all patients and published reports on the efficacy of targeting ROS1 in PDAC are extremely rare [27,29]. There has been one case report of a patient with KRAS WT PDAC who had stable disease on entrectinib for 7 months before progression of disease [62]. Due to its rare incidence, no other larger cohorts have been reported. No pancreatic cancer specific FDA approved therapy is available for ROS1 altered PDAC.
4.11. MMR Deficient PDAC
Mismatch repair deficient (MMRd) PDAC accounts for up to 2.5% of all PDAC and 4.7% of KRAS WT PDAC [29,97]. Often, MMRd PDAC is frequently TP53 WT and often has a medullary or mucinous/colloid histology [98]. In an early phase clinical trial studying pembrolizumab, eight MMRd PDAC patients were enrolled; five of these achieved a partial response to therapy (62% ORR) [99]. However, in the KEYNOTE-158 study, there was a more modest 18.2% (n = 4/22 patients) ORR in MMRd PDAC who had previously had progression on first-line therapies [100]. There were no unexpected immune-related adverse events in these trials, with 14.6% experiencing grade ≥ 3 adverse events, including liver test abnormalities (GGT and ALT), pneumonitis, Guillain Barre Syndrome, neutropenia, and autoimmune enterocolitis. Pembrolizumab has a tumor-agnostic FDA-approval for MSI-H/MMRd tumors, which allows patients with MMRd PDAC access to this promising therapy. While pembrolizumab is a recommended therapy for MMRd PDAC, there is currently no role for immunotherapy in microsatellite stable/mismatch repair proficient PDAC, as evidenced by multiple negative clinical trials investigating its use [60,101]. However, future investigations are trying to identify methods of overcoming immunotherapy resistance in mismatch repair-proficient PDAC.
5. Conclusions
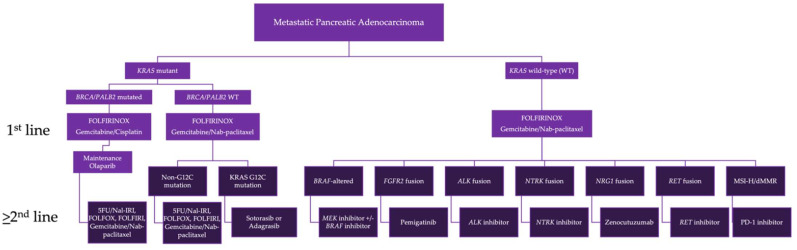
PDAC is a highly lethal malignancy, and patients are in desperate need of molecularly targeted therapies that can improve the current treatment paradigms (Figure 2). Cytotoxic chemotherapy remains the standard of care for most patients with PDAC. While combination chemotherapy regimens have improved outcomes in the first-line setting, the efficacy of second-line chemotherapy is modest. The use of next-generation sequencing (NGS) can identify patients who might benefit from targeted therapy. FDA-approved options are available for PDAC tumors with BRCA1/2 mutations (germline), MMRd, NTRK fusions, BRAF V600E mutations, and RET fusions. Investigational therapies, as well as off-label use of therapies that have FDA approval for other malignancies, are available to KRAS WT PDAC patients harboring other BRAF alterations and ALK, FGFR2, ROS1, and NRG1 translocations. However, there is a large portion of PDAC patients who do not have a targetable alteration, and innovative targeted and immunotherapies that can improve outcomes in these patients are greatly needed.
Figure 2.
Biomarker-driven treatment paradigm for metastatic pancreatic adenocarcinoma. Treatment algorithm describes first-line, maintenance, and second-line treatment options for PDAC patients, based upon the tumor’s molecular alterations. Multiple treatment options are listed in instances where more than one therapy is available. Abbreviations used include: FOLFIRINOX: folinic acid, 5-fluorouracil, irinotecan, and oxaliplatin; FOLFOX: folinic acid, 5-fluorouracil, and oxaliplatin; Nal-IRI: nanoliposomal irinotecan; FOLFIRI: folinic acid, 5-fluorouracil, and irinotecan; MSI-H: microsatellite instability-high; dMMR: mismatch repair deficient; WT: wild type.
Author Contributions
Conceptualization, B.M.H. and J.M.C.; writing—original draft preparation, B.M.H.; writing—review and editing, B.M.H., H.E., A.C.J., W.A.F.-P., K.P., D.A.R., N.S., H.S., R.S., B.M.W., A.J.A. and J.M.C. All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest
Brandon M. Huffman, Haley Ellis, and Rishi Surana have no conflicts of interest to report. Alexander C. Jordan received a conference travel grant partially funded by Amgen and Bristol-Myers Squibb. William A. Freed-Pastor has consulted for PMV Pharma and holds equity in Regeneron. He receives research support from Arcus Biosciences and Apexigen. Kimberly Perez served as a one-time Advisory Board Member for Ipsen, Lantheus, and Helssinn/QED. Douglas Rubinson reports Boston Scientific, AxialTx, and Instylla. Nilay Sethi is a consultant for Astrin Biosciences. Harshabad Singh receives research funding from Aztrazeneca. Brian Wolpin receives research support from Celgene, Eli Lilly, Novartis, and Revolution Medicine. He has received honoraria for consulting for BioLineRx, Celgene, Grail, and Mirati Therapeutics. Andrew J. Aguirre has consulted for Riva Therapeutics, Arrakis Therapeutics, Syros Pharmaceuticals, Boehringer Ingelheim, T-knife Therapeutics, AstraZeneca, Mirati Therapeutics and Merck & Co., Inc, and has research funding from Mirati Therapeutics, Syros Pharmaceuticals, Bristol Myers Squibb, Revolution Medicines, Novartis, and Novo Ventures that is unrelated to this work. James M. Cleary receives research funding to his institution from AbbVie, Merus, Roche, and Bristol Myers Squibb. He receives research support from Merck, AstraZeneca, Esperas Pharma, Bayer, Tesaro, Arcus Biosciences, and Apexigen; he has also received honoraria for being on the advisory boards of Syros Pharmaceuticals, Incyte, and Blueprint Medicines.
Funding Statement
This work is supported by Stand Up to Cancer and the Lustgarten Foundation. The work was also supported by a grant from the National Institutes of Health (P50CA127003).
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Rahib L., Smith B.D., Aizenberg R., Rosenzweig A.B., Fleshman J.M., Matrisian L.M. Projecting cancer incidence and deaths to 2030: The unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res. 2014;74:2913–2921. doi: 10.1158/0008-5472.CAN-14-0155. [DOI] [PubMed] [Google Scholar]
- 2.Siegel R.L., Miller K.D., Fuchs H.E., Jemal A. Cancer statistics, 2022. CA A Cancer J. Clin. 2022;72:7–33. doi: 10.3322/caac.21708. [DOI] [PubMed] [Google Scholar]
- 3.Conroy T., Desseigne F., Ychou M., Bouché O., Guimbaud R., Bécouarn Y., Adenis A., Raoul J.-L., Gourgou-Bourgade S., De La Fouchardière C., et al. FOLFIRINOX versus Gemcitabine for Metastatic Pancreatic Cancer. N. Engl. J. Med. 2011;364:1817–1825. doi: 10.1056/NEJMoa1011923. [DOI] [PubMed] [Google Scholar]
- 4.Von Hoff D.D., Ervin T., Arena F.P., Chiorean E.G., Infante J., Moore M., Seay T., Tjulandin S.A., Ma W.W., Saleh M.N., et al. Increased Survival in Pancreatic Cancer with nab-Paclitaxel plus Gemcitabine. N. Engl. J. Med. 2013;369:1691–1703. doi: 10.1056/NEJMoa1304369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chakrabarti S., Kamgar M., Mahipal A. Systemic Therapy of Metastatic Pancreatic Adenocarcinoma: Current Status, Challenges, and Opportunities. Cancers. 2022;14:2588. doi: 10.3390/cancers14112588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ryan D.P., Hong T.S., Bardeesy N. Pancreatic Adenocarcinoma. N. Engl. J. Med. 2014;371:1039–1049. doi: 10.1056/NEJMra1404198. [DOI] [PubMed] [Google Scholar]
- 7.Mizrahi J.D., Surana R., Valle J.W., Shroff R.T. Pancreatic cancer. Lancet. 2020;395:2008–2020. doi: 10.1016/S0140-6736(20)30974-0. [DOI] [PubMed] [Google Scholar]
- 8.Park W., Chawla A., O’Reilly E.M. Pancreatic Cancer. JAMA. 2021;326:851–862. doi: 10.1001/jama.2021.13027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rubinson D.A., Wolpin B.M. Therapeutic Approaches for Metastatic Pancreatic Adenocarcinoma. Hematol. Oncol. Clin. N. Am. 2015;29:761–776. doi: 10.1016/j.hoc.2015.04.012. [DOI] [PubMed] [Google Scholar]
- 10.Burris H.A., 3rd, Moore M.J., Andersen J., Green M.R., Rothenberg M.L., Modiano M.R., Cripps M.C., Portenoy R.K., Storniolo A.M., Tarassoff P., et al. Improvements in survival and clinical benefit with gemcitabine as first-line therapy for patients with advanced pancreas cancer: A randomized trial. J. Clin. Oncol. 1997;15:2403–2413. doi: 10.1200/JCO.1997.15.6.2403. [DOI] [PubMed] [Google Scholar]
- 11.Ramanathan R.K., McDonough S.L., Philip P.A., Hingorani S.R., Lacy J., Kortmansky J.S., Thumar J., Chiorean E.G., Shields A.F., Behl D., et al. Phase IB/II Randomized Study of FOLFIRINOX Plus Pegylated Recombinant Human Hyaluronidase Versus FOLFIRINOX Alone in Patients with Metastatic Pancreatic Adenocarcinoma: SWOG S1313. J. Clin. Oncol. 2019;37:1062–1069. doi: 10.1200/JCO.18.01295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sohal D.P., Mangu P.B., Khorana A., Shah M.A., Philip P.A., O’Reilly E.M., Uronis H.E., Ramanathan R.K., Crane C.H., Engebretson A., et al. Metastatic Pancreatic Cancer: American Society of Clinical Oncology Clinical Practice Guideline. J. Clin. Oncol. 2016;34:2784–2796. doi: 10.1200/JCO.2016.67.1412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sohal D.P.S., Kennedy E.B., Cinar P., Conroy T., Copur M.S., Crane C.H., Garrido-Laguna I., Lau M.W., Johnson T., Krishnamurthi S., et al. Metastatic Pancreatic Cancer: ASCO Guideline Update. J. Clin. Oncol. 2020;38:3217–3230. doi: 10.1200/JCO.20.01364. [DOI] [PubMed] [Google Scholar]
- 14.Sohal D.P.S., Kennedy E.B., Khorana A., Copur M.S., Crane C.H., Garrido-Laguna I., Krishnamurthi S., Moravek C., O’Reilly E.M., Philip P.A., et al. Metastatic Pancreatic Cancer: ASCO Clinical Practice Guideline Update. J. Clin. Oncol. 2018;36:2545–2556. doi: 10.1200/JCO.2018.78.9636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pijnappel E.N., Dijksterhuis W.P., van der Geest L.G., de Vos-Geelen J., de Groot J.W.B., Homs M.Y., Creemers G.-J., Mohammad N.H., Besselink M.G., van Laarhoven H.W., et al. First- and Second-Line Palliative Systemic Treatment Outcomes in a Real-World Metastatic Pancreatic Cancer Cohort. J. Natl. Compr. Cancer Netw. 2021;20:443–450.e3. doi: 10.6004/jnccn.2021.7028. [DOI] [PubMed] [Google Scholar]
- 16.Pusceddu S., Ghidini M., Torchio M., Corti F., Tomasello G., Niger M., Prinzi N., Nichetti F., Coinu A., Di Bartolomeo M., et al. Comparative Effectiveness of Gemcitabine plus Nab-Paclitaxel and FOLFIRINOX in the First-Line Setting of Metastatic Pancreatic Cancer: A Systematic Review and Meta-Analysis. Cancers. 2019;11:484. doi: 10.3390/cancers11040484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Carrato A., Pazo-Cid R., Macarulla T., Gallego J., Jiménez-Fonseca P., Rivera F., Cano M.T., Garrote M.R., Pericay C., Diaz I., et al. Sequential nab-paclitaxel/gemcitabine followed by modified FOLFOX for first-line metastatic pancreatic cancer: The SEQUENCE trial. J. Clin. Oncol. 2022;40:4022. doi: 10.1200/JCO.2022.40.16_suppl.4022. [DOI] [Google Scholar]
- 18.Oettle H., Riess H., Stieler J.M., Heil G., Schwaner I., Seraphin J., Görner M., Mölle M., Greten T.F., Lakner V., et al. Second-Line Oxaliplatin, Folinic Acid, and Fluorouracil Versus Folinic Acid and Fluorouracil Alone for Gemcitabine-Refractory Pancreatic Cancer: Outcomes from the CONKO-003 Trial. J. Clin. Oncol. 2014;32:2423–2429. doi: 10.1200/JCO.2013.53.6995. [DOI] [PubMed] [Google Scholar]
- 19.Gill S., Ko Y.-J., Cripps C., Beaudoin A., Dhesy-Thind S., Zulfiqar M., Zalewski P., Do T., Cano P., Lam W.Y.H., et al. PANCREOX: A Randomized Phase III Study of Fluorouracil/Leucovorin with or without Oxaliplatin for Second-Line Advanced Pancreatic Cancer in Patients Who Have Received Gemcitabine-Based Chemotherapy. J. Clin. Oncol. 2016;34:3914–3920. doi: 10.1200/JCO.2016.68.5776. [DOI] [PubMed] [Google Scholar]
- 20.Hecht J.R., Lonardi S., Bendell J., Sim H.-W., Macarulla T., Lopez C.D., Van Cutsem E., Martin A.J.M., Park J.O., Greil R., et al. Randomized Phase III Study of FOLFOX Alone or with Pegilodecakin as Second-Line Therapy in Patients with Metastatic Pancreatic Cancer That Progressed After Gemcitabine (SEQUOIA) J. Clin. Oncol. 2021;39:1108–1118. doi: 10.1200/JCO.20.02232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chung V., McDonough S., Philip P.A., Cardin D., Wang-Gillam A., Hui L., Tejani M.A., Seery T.E., Dy I.A., Al Baghdadi T., et al. Effect of Selumetinib and MK-2206 vs Oxaliplatin and Fluorouracil in Patients with Metastatic Pancreatic Cancer After Prior Therapy: SWOG S1115 Study Randomized Clinical Trial. JAMA Oncol. 2017;3:516–522. doi: 10.1001/jamaoncol.2016.5383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang-Gillam A., Li C.-P., Bodoky G., Dean A., Shan Y.-S., Jameson G., Macarulla T., Lee K.-H., Cunningham D., Blanc J.F., et al. Nanoliposomal irinotecan with fluorouracil and folinic acid in metastatic pancreatic cancer after previous gemcitabine-based therapy (NAPOLI-1): A global, randomised, open-label, phase 3 trial. Lancet. 2016;387:545–557. doi: 10.1016/S0140-6736(15)00986-1. [DOI] [PubMed] [Google Scholar]
- 23.Chiorean E.G., Guthrie K.A., Philip P.A., Swisher E.M., Jalikis F., Pishvaian M.J., Berlin J., Noel M.S., Suga J.M., Garrido-Laguna I., et al. Randomized Phase II Study of PARP Inhibitor ABT-888 (Veliparib) with Modified FOLFIRI versus FOLFIRI as Second-line Treatment of Metastatic Pancreatic Cancer: SWOG S1513. Clin. Cancer Res. 2021;27:6314–6322. doi: 10.1158/1078-0432.CCR-21-1789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hammel P., El-Hariry I., Macarulla T., Garcia-Carbonero R., Metges J.-P., Bouché O., Portales F., Cid R.A.P., Mineur L., Gracian A.M.C., et al. Trybeca-1: A randomized, phase 3 study of eryaspase in combination with chemotherapy versus chemotherapy alone as second-line treatment in patients with advanced pancreatic adenocarcinoma ( NCT03665441) J. Clin. Oncol. 2022;40:518. doi: 10.1200/JCO.2022.40.4_suppl.518. [DOI] [Google Scholar]
- 25.Huffman B.M., Mallick A.B., Horick N.K., Wang-Gillam A., Hosein P.J., Morse M., Beg M.S., Murphy J.E., Schlechter B.L., Sanoff H., et al. Abstract A019: A multicenter randomized phase II study of gemcitabine and nab-paclitaxel versus gemcitabine and nab-paclitaxel with a MUC5AC antibody (NPC-1C) in advanced pancreatic cancer previously treated with FOLFIRINOX ( NCT01834235) Cancer Res. 2022;82:A019. doi: 10.1158/1538-7445.PANCA22-A019. [DOI] [Google Scholar]
- 26.Xu Z., Hu K., Bailey P., Springfeld C., Roth S., Kurilov R., Brors B., Gress T., Buchholz M., An J., et al. Clinical Impact of Molecular Subtyping of Pancreatic Cancer. Front. Cell Dev. Biol. 2021;9:743908. doi: 10.3389/fcell.2021.743908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Aguirre A.J., Nowak J.A., Camarda N.D., Moffitt R.A., Ghazani A.A., Hazar-Rethinam M., Raghavan S., Kim J., Brais L.K., Ragon D., et al. Real-time Genomic Characterization of Advanced Pancreatic Cancer to Enable Precision Medicine. Cancer Discov. 2018;8:1096–1111. doi: 10.1158/2159-8290.CD-18-0275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hosein A.N., Dougan S.K., Aguirre A.J., Maitra A. Translational advances in pancreatic ductal adenocarcinoma therapy. Nat. Cancer. 2022;3:272–286. doi: 10.1038/s43018-022-00349-2. [DOI] [PubMed] [Google Scholar]
- 29.Philip P.A., Azar I., Xiu J., Hall M.J., Hendifar A.E., Lou E., Hwang J.J., Gong J., Feldman R., Ellis M., et al. Molecular Characterization of KRAS Wild-type Tumors in Patients with Pancreatic Adenocarcinoma. Clin. Cancer Res. 2022;28:2704–2714. doi: 10.1158/1078-0432.CCR-21-3581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Singhi A.D., George B., Greenbowe J.R., Chung J., Suh J., Maitra A., Klempner S., Hendifar A., Milind J.M., Golan T., et al. Real-Time Targeted Genome Profile Analysis of Pancreatic Ductal Adenocarcinomas Identifies Genetic Alterations That Might Be Targeted with Existing Drugs or Used as Biomarkers. Gastroenterology. 2019;156:2242–2253.e4. doi: 10.1053/j.gastro.2019.02.037. [DOI] [PubMed] [Google Scholar]
- 31.Pishvaian M.J., Blais E.M., Brody J.R., Lyons E., DeArbeloa P., Hendifar A., Mikhail S., Chung V., Sahai V., Sohal D.P.S., et al. Overall survival in patients with pancreatic cancer receiving matched therapies following molecular profiling: A retrospective analysis of the Know Your Tumor registry trial. Lancet Oncol. 2020;21:508–518. doi: 10.1016/S1470-2045(20)30074-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Marciano N.D., Kroening G., Dayyani F., Zell J.A., Lee F.-C., Cho M., Valerin J.G. BRCA-Mutated Pancreatic Cancer: From Discovery to Novel Treatment Paradigms. Cancers. 2022;14:2453. doi: 10.3390/cancers14102453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cleary J.M., Aguirre A.J., Shapiro G.I., D’Andrea A.D. Biomarker-Guided Development of DNA Repair Inhibitors. Mol. Cell. 2020;78:1070–1085. doi: 10.1016/j.molcel.2020.04.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kondrashova O., Nguyen M., Shield-Artin K., Tinker A.V., Teng N.N.H., Harrell M.I., Kuiper M.J., Ho G.Y., Barker H., Jasin M., et al. Secondary Somatic Mutations Restoring RAD51C and RAD51D Associated with Acquired Resistance to the PARP Inhibitor Rucaparib in High-Grade Ovarian Carcinoma. Cancer Discov. 2017;7:984–998. doi: 10.1158/2159-8290.CD-17-0419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Park W., Chen J., Chou J.F., Varghese A.M., Yu K.H., Wong W., Capanu M., Balachandran V., McIntyre C.A., El Dika I., et al. Genomic Methods Identify Homologous Recombination Deficiency in Pancreas Adenocarcinoma and Optimize Treatment Selection. Clin. Cancer Res. 2020;26:3239–3247. doi: 10.1158/1078-0432.CCR-20-0418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yurgelun M.B., Chittenden A.B., Morales-Oyarvide V., Rubinson D.A., Dunne R.F., Kozak M.M., Qian Z.R., Welch M.W., Brais L.K., Da Silva A., et al. Germline cancer susceptibility gene variants, somatic second hits, and survival outcomes in patients with resected pancreatic cancer. Genet. Med. 2019;21:213–223. doi: 10.1038/s41436-018-0009-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Golan T., Barenboim A., Lahat G., Nachmany I., Goykhman Y., Shacham-Shmueli E., Halpern N., Brazowski E., Geva R., Wolf I., et al. Increased Rate of Complete Pathologic Response After Neoadjuvant FOLFIRINOX for BRCA Mutation Carriers with Borderline Resectable Pancreatic Cancer. Ann. Surg. Oncol. 2020;27:3963–3970. doi: 10.1245/s10434-020-08469-8. [DOI] [PubMed] [Google Scholar]
- 38.Yadav S., Kasi P.M., Bamlet W.R., Ho T.P., Polley E.C., Hu C., Hart S.N., Rabe K.G., Boddicker N.J., Gnanaolivu R.D., et al. Effect of Germline Mutations in Homologous Recombination Repair Genes on Overall Survival of Patients with Pancreatic Adenocarcinoma. Clin. Cancer Res. 2020;26:6505–6512. doi: 10.1158/1078-0432.CCR-20-1788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.O’Reilly E.M., Lee J.W., Zalupski M., Capanu M., Park J., Golan T., Tahover E., Lowery M.A., Chou J.F., Sahai V., et al. Randomized, Multicenter, Phase II Trial of Gemcitabine and Cisplatin with or without Veliparib in Patients with Pancreas Adenocarcinoma and a Germline BRCA/PALB2 Mutation. J. Clin. Oncol. 2020;38:1378–1388. doi: 10.1200/JCO.19.02931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Heinemann V., Quietzsch D., Gieseler F., Gonnermann M., Schönekäs H., Rost A., Neuhaus H., Haag C., Clemens M., Heinrich B., et al. Randomized Phase III Trial of Gemcitabine Plus Cisplatin Compared with Gemcitabine Alone in Advanced Pancreatic Cancer. J. Clin. Oncol. 2006;24:3946–3952. doi: 10.1200/JCO.2005.05.1490. [DOI] [PubMed] [Google Scholar]
- 41.Moore K., Colombo N., Scambia G., Kim B.-G., Oaknin A., Friedlander M., Lisyanskaya A., Floquet A., Leary A., Sonke G.S., et al. Maintenance Olaparib in Patients with Newly Diagnosed Advanced Ovarian Cancer. N. Engl. J. Med. 2018;379:2495–2505. doi: 10.1056/NEJMoa1810858. [DOI] [PubMed] [Google Scholar]
- 42.Tutt A.N., Garber J.E., Kaufman B., Viale G., Fumagalli D., Rastogi P., Gelber R.D., de Azambuja E., Fielding A., Balmaña J., et al. Adjuvant Olaparib for Patients with BRCA1- or BRCA2-Mutated Breast Cancer. N. Engl. J. Med. 2021;384:2394–2405. doi: 10.1056/NEJMoa2105215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Golan T., Hammel P., Reni M., Van Cutsem E., Macarulla T., Hall M.J., Park J.-O., Hochhauser D., Arnold D., Oh D.-Y., et al. Maintenance Olaparib for Germline BRCA-Mutated Metastatic Pancreatic Cancer. N. Engl. J. Med. 2019;381:317–327. doi: 10.1056/NEJMoa1903387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kindler H.L., Hammel P., Reni M., Van Cutsem E., Macarulla T., Hall M.J., Park J.O., Hochhauser D., Arnold D., Oh D.-Y., et al. Overall Survival Results from the POLO Trial: A Phase III Study of Active Maintenance Olaparib Versus Placebo for Germline BRCA-Mutated Metastatic Pancreatic Cancer. J. Clin. Oncol. 2022;40:3929–3939. doi: 10.1200/JCO.21.01604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Reiss K.A., Mick R., O’Hara M.H., Teitelbaum U., Karasic T.B., Schneider C., Cowden S., Southwell T., Romeo J., Izgur N., et al. Phase II Study of Maintenance Rucaparib in Patients with Platinum-Sensitive Advanced Pancreatic Cancer and a Pathogenic Germline or Somatic Variant in BRCA1, BRCA2, or PALB2. J. Clin. Oncol. 2021;39:2497–2505. doi: 10.1200/JCO.21.00003. [DOI] [PubMed] [Google Scholar]
- 46.Rubinson D., Wolpin B.M., Warsofsky I.S., Ryan D.P., Perez K., Rahma O., Singh H., Yurgelun M.B., Shapiro G.I., Aguirre A.J., et al. Durable clinical benefit from PARP inhibition in a platinum-sensitive, BRCA2-mutated pancreatic cancer patient after earlier progression on placebo treatment on the POLO trial: A case report. J. Gastrointest. Oncol. 2021;12:3133–3140. doi: 10.21037/jgo-21-197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Reiss K.A., Mick R., Teitelbaum U., O’Hara M., Schneider C., Massa R., Karasic T., Tondon R., Onyiah C., Gosselin M.K., et al. Niraparib plus nivolumab or niraparib plus ipilimumab in patients with platinum-sensitive advanced pancreatic cancer: A randomised, phase 1b/2 trial. Lancet Oncol. 2022;23:1009–1020. doi: 10.1016/S1470-2045(22)00369-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Prior I.A., Hood F.E., Hartley J.L. The Frequency of Ras Mutations in Cancer. Cancer Res. 2020;80:2969–2974. doi: 10.1158/0008-5472.CAN-19-3682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gillson J., Ramaswamy Y., Singh G., Gorfe A.A., Pavlakis N., Samra J., Mittal A., Sahni S. Small Molecule KRAS Inhibitors: The Future for Targeted Pancreatic Cancer Therapy? Cancers. 2020;12:1341. doi: 10.3390/cancers12051341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Waters A.M., Der C.J. KRAS: The Critical Driver and Therapeutic Target for Pancreatic Cancer. Cold Spring Harb. Perspect. Med. 2018;8:a031435. doi: 10.1101/cshperspect.a031435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bamford S., Dawson E., Forbes S., Clements J., Pettett R., Dogan A., Flanagan A., Teague J., Futreal P.A., Stratton M.R., et al. The COSMIC (Catalogue of Somatic Mutations in Cancer) database and website. Br. J. Cancer. 2004;91:355–358. doi: 10.1038/sj.bjc.6601894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Qian Z.R., Rubinson D.A., Nowak J.A., Morales-Oyarvide V., Dunne R.F., Kozak M.M., Welch M.W., Brais L.K., Da Silva A., Li T., et al. Association of Alterations in Main Driver Genes with Outcomes of Patients with Resected Pancreatic Ductal Adenocarcinoma. JAMA Oncol. 2018;4:e173420. doi: 10.1001/jamaoncol.2017.3420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Diehl A.C., Hannan L.M., Zhen D.B., Coveler A.L., King G., Cohen S.A., Harris W.P., Shankaran V., Wong K.M., Green S., et al. KRAS Mutation Variants and Co-occurring PI3K Pathway Alterations Impact Survival for Patients with Pancreatic Ductal Adenocarcinomas. Oncologist. 2022;27:1025–1033. doi: 10.1093/oncolo/oyac179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Strickler J.H., Satake H., Hollebecque A., Sunakawa Y., Tomasini P., Bajor D.L., Schuler M.H., Yaeger R., George T.J., Garrido-Laguna I., et al. First data for sotorasib in patients with pancreatic cancer with KRAS p.G12C mutation: A phase I/II study evaluating efficacy and safety. J. Clin. Oncol. 2022;40:360490. doi: 10.1200/JCO.2022.40.36_suppl.360490. [DOI] [Google Scholar]
- 55.Bekaii-Saab T.S., Spira A.I., Yaeger R., Buchschacher G.L., McRee A.J., Sabari J.K., Johnson M.L., Barve M.A., Hafez N., Velastegui K., et al. KRYSTAL-1: Updated activity and safety of adagrasib (MRTX849) in patients (Pts) with unresectable or metastatic pancreatic cancer (PDAC) and other gastrointestinal (GI) tumors harboring a KRASG12C mutation. J. Clin. Oncol. 2022;40:519. doi: 10.1200/JCO.2022.40.4_suppl.519. [DOI] [Google Scholar]
- 56.Koltun E.S., Rice M.A., Gustafson W.C., Wilds D., Jiang J., Lee B.J., Wang Z., Chang S., Flagella M., Mu Y., et al. Abstract 3597: Direct targeting of KRASG12X mutant cancers with RMC-6236, a first-in-class, RAS-selective, orally bioavailable, tri-complex RASMULTI(ON) inhibitor. Cancer Res. 2022;82:3597. doi: 10.1158/1538-7445.AM2022-3597. [DOI] [Google Scholar]
- 57.Hallin J., Bowcut V., Calinisan A., Briere D.M., Hargis L., Engstrom L.D., Laguer J., Medwid J., Vanderpool D., Lifset E., et al. Anti-tumor efficacy of a potent and selective non-covalent KRASG12D inhibitor. Nat. Med. 2022;28:2171–2182. doi: 10.1038/s41591-022-02007-7. [DOI] [PubMed] [Google Scholar]
- 58.Balachandran V.P., Beatty G.L., Dougan S.K. Broadening the Impact of Immunotherapy to Pancreatic Cancer: Challenges and Opportunities. Gastroenterology. 2019;156:2056–2072. doi: 10.1053/j.gastro.2018.12.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Leidner R., Silva N.S., Huang H., Sprott D., Zheng C., Shih Y.-P., Leung A., Payne R., Sutcliffe K., Cramer J., et al. Neoantigen T-Cell Receptor Gene Therapy in Pancreatic Cancer. N. Engl. J. Med. 2022;386:2112–2119. doi: 10.1056/NEJMoa2119662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.O’Reilly E.M., Oh D.-Y., Dhani N., Renouf D.J., Lee M.A., Sun W., Fisher G., Hezel A., Chang S.-C., Vlahovic G., et al. Durvalumab with or without Tremelimumab for Patients with Metastatic Pancreatic Ductal Adenocarcinoma: A Phase 2 Randomized Clinical Trial. JAMA Oncol. 2019;5:1431–1438. doi: 10.1001/jamaoncol.2019.1588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Topham J.T., Tsang E.S., Karasinska J.M., Metcalfe A., Ali H., Kalloger S.E., Csizmok V., Williamson L.M., Titmuss E., Nielsen K., et al. Integrative analysis of KRAS wildtype metastatic pancreatic ductal adenocarcinoma reveals mutation and expression-based similarities to cholangiocarcinoma. Nat. Commun. 2022;13:5941. doi: 10.1038/s41467-022-33718-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Pishvaian M.J., Garrido-Laguna I., Liu S.V., Multani P.S., Chow-Maneval E., Rolfo C. Entrectinib in TRK and ROS1 Fusion-Positive Metastatic Pancreatic Cancer. JCO Precis. Oncol. 2018;2:1–7. doi: 10.1200/PO.18.00039. [DOI] [PubMed] [Google Scholar]
- 63.Jones M.R., Williamson L.M., Topham J.T., Lee M.K., Goytain A., Ho J., Denroche R.E., Jang G.-H., Pleasance E.D., Shen Y., et al. NRG1 Gene Fusions Are Recurrent, Clinically Actionable Gene Rearrangements in KRAS Wild-Type Pancreatic Ductal Adenocarcinoma. Clin. Cancer Res. 2019;25:4674–4681. doi: 10.1158/1078-0432.CCR-19-0191. [DOI] [PubMed] [Google Scholar]
- 64.Park W., O’Connor C.A., Bandlamudi C., Forman D., Chou J.F., Umeda S., Reyngold M., Varghese A.M., Keane F., Balogun F., et al. Clinico-genomic Characterization of ATM and HRD in Pancreas Cancer: Application for Practice. Clin. Cancer Res. 2022;28:4782–4792. doi: 10.1158/1078-0432.CCR-22-1483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Raphael B.J., Hruban R.H., Aguirre A.J., Moffitt R.A., Yeh J.J., Stewart C., Robertson A.G., Cherniack A.D., Gupta M., Getz G., et al. Integrated Genomic Characterization of Pancreatic Ductal Adenocarcinoma. Cancer Cell. 2017;32:185–203.e13. doi: 10.1016/j.ccell.2017.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Qin S., Bai Y., Wang Z., Chen Z., Xu R., Xu J., Zhang H., Chen J., Yuan Y., Liu T., et al. Nimotuzumab combined with gemcitabine versus gemcitabine in K-RAS wild-type locally advanced or metastatic pancreatic cancer: A prospective, randomized-controlled, double-blinded, multicenter, and phase III clinical trial. J. Clin. Oncol. 2022;40:LBA4011. doi: 10.1200/JCO.2022.40.17_suppl.LBA4011. [DOI] [Google Scholar]
- 67.Dummer R., Ascierto P.A., Gogas H.J., Arance A., Mandala M., Liszkay G., Garbe C., Schadendorf D., Krajsova I., Gutzmer R., et al. Encorafenib plus binimetinib versus vemurafenib or encorafenib in patients with BRAF -mutant melanoma (COLUMBUS): A multicentre, open-label, randomised phase 3 trial. Lancet Oncol. 2018;19:603–615. doi: 10.1016/S1470-2045(18)30142-6. [DOI] [PubMed] [Google Scholar]
- 68.Robert C., Grob J.J., Stroyakovskiy D., Karaszewska B., Hauschild A., Levchenko E., Chiarion Sileni V., Schachter J., Garbe C., Bondarenko I., et al. Five-Year Outcomes with Dabrafenib plus Trametinib in Metastatic Melanoma. N. Engl. J. Med. 2019;381:626–636. doi: 10.1056/NEJMoa1904059. [DOI] [PubMed] [Google Scholar]
- 69.Hendifar A., Blais E.M., Wolpin B., Subbiah V., Collisson E., Singh I., Cannon T., Shaw K., Petricoin E.F., III, Klempner S., et al. Retrospective Case Series Analysis of RAF Family Alterations in Pancreatic Cancer: Real-World Outcomes from Targeted and Standard Therapies. JCO Precis. Oncol. 2021:1325–1338. doi: 10.1200/PO.20.00494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Fusco M.J., Saeed-Vafa D., Carballido E.M., Boyle T.A., Malafa M., Blue K.L., Teer J.K., Walko C.M., McLeod H.L., Hicks J.K., et al. Identification of Targetable Gene Fusions and Structural Rearrangements to Foster Precision Medicine in KRAS Wild-Type Pancreatic Cancer. JCO Precis. Oncol. 2021;5:65–74. doi: 10.1200/PO.20.00265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Li F., Peiris M.N., Donoghue D.J. Functions of FGFR2 corrupted by translocations in intrahepatic cholangiocarcinoma. Cytokine Growth Factor Rev. 2020;52:56–67. doi: 10.1016/j.cytogfr.2019.12.005. [DOI] [PubMed] [Google Scholar]
- 72.Cleary J.M., Raghavan S., Wu Q., Li Y.Y., Spurr L.F., Gupta H.V., Rubinson D.A., Fetter I.J., Hornick J.L., Nowak J.A., et al. FGFR2 Extracellular Domain In-Frame Deletions Are Therapeutically Targetable Genomic Alterations That Function as Oncogenic Drivers in Cholangiocarcinoma. Cancer Discov. 2021;11:2488–2505. doi: 10.1158/2159-8290.CD-20-1669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Subbiah V., Iannotti N., Gutierrez M., Smith D., Féliz L., Lihou C., Tian C., Silverman I., Ji T., Saleh M. FIGHT-101, a first-in-human study of potent and selective FGFR 1-3 inhibitor pemigatinib in pan-cancer patients with FGF/FGFR alterations and advanced malignancies. Ann. Oncol. 2022;33:522–533. doi: 10.1016/j.annonc.2022.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Helal C., Valéry M., Ducreux M., Hollebecque A., Smolenschi C. FGFR2 fusion in metastatic pancreatic ductal adenocarcinoma: Is there hope? Eur. J. Cancer. 2022;176:168–170. doi: 10.1016/j.ejca.2022.09.016. [DOI] [PubMed] [Google Scholar]
- 75.Hallberg B., Palmer R. The role of the ALK receptor in cancer biology. Ann. Oncol. 2016;27:iii4–iii15. doi: 10.1093/annonc/mdw301. [DOI] [PubMed] [Google Scholar]
- 76.Cooper A.J., Sequist L.V., Lin J.J. Third-generation EGFR and ALK inhibitors: Mechanisms of resistance and management. Nat. Rev. Clin. Oncol. 2022;19:499–514. doi: 10.1038/s41571-022-00639-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Hida T., Nokihara H., Kondo M., Kim Y.H., Azuma K., Seto T., Takiguchi Y., Nishio M., Yoshioka H., Imamura F., et al. Alectinib versus crizotinib in patients with ALK -positive non-small-cell lung cancer (J-ALEX): An open-label, randomised phase 3 trial. Lancet. 2017;390:29–39. doi: 10.1016/S0140-6736(17)30565-2. [DOI] [PubMed] [Google Scholar]
- 78.Peters S., Camidge D.R., Shaw A.T., Gadgeel S., Ahn J.S., Kim D.W., Ou S.H.I., Pérol M., Dziadziuszko R., Rosell R., et al. Alectinib versus Crizotinib in Untreated ALK-Positive Non–Small-Cell Lung Cancer. N. Engl. J. Med. 2017;377:829–838. doi: 10.1056/NEJMoa1704795. [DOI] [PubMed] [Google Scholar]
- 79.Cleary J.M., Rodig S., Barr P.M., Shinagare A.B., Clark J.W., Shapiro G.I., Armand P. Crizotinib as salvage and maintenance with allogeneic stem cell transplantation for refractory anaplastic large cell lymphoma. J. Natl. Compr. Cancer Netw. 2014;12:323–326. doi: 10.6004/jnccn.2014.0034. [DOI] [PubMed] [Google Scholar]
- 80.Merino M., Kasamon Y., Li H., Ma L., Leong R., Zhou J., Reaman G., Chambers W., Richardson N., Theoret M., et al. FDA approval summary: Crizotinib for pediatric and young adult patients with relapsed or refractory systemic anaplastic large cell lymphoma. Pediatr. Blood Cancer. 2022;69:e29602. doi: 10.1002/pbc.29602. [DOI] [PubMed] [Google Scholar]
- 81.Singh H., Li Y.Y., Spurr L.F., Shinagare A.B., Abhyankar R., Reilly E., Brais L.K., Nag A., Ducar M.D., Thorner A.R., et al. Molecular Characterization and Therapeutic Targeting of Colorectal Cancers Harboring Receptor Tyrosine Kinase Fusions. Clin. Cancer Res. 2021;27:1695–1705. doi: 10.1158/1078-0432.CCR-20-4073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Shaw A.T., Kim D.-W., Nakagawa K., Seto T., Crinó L., Ahn M.-J., De Pas T., Besse B., Solomon B.J., Blackhall F., et al. Crizotinib versus Chemotherapy in AdvancedALK-Positive Lung Cancer. N. Engl. J. Med. 2013;368:2385–2394. doi: 10.1056/NEJMoa1214886. [DOI] [PubMed] [Google Scholar]
- 83.Singhi A.D., Ali S.M., Lacy J., Hendifar A., Nguyen K., Koo J., Chung J.H., Greenbowe J., Ross J.S., Nikiforova M.N., et al. Identification of Targetable ALK Rearrangements in Pancreatic Ductal Adenocarcinoma. J. Natl. Compr. Cancer Netw. 2017;15:555–562. doi: 10.6004/jnccn.2017.0058. [DOI] [PubMed] [Google Scholar]
- 84.Ambrosini M., Del Re M., Manca P., Hendifar A., Drilon A., Harada G., Ree A.H., Klempner S., Mælandsmo G.M., Flatmark K., et al. ALK Inhibitors in Patients with ALK Fusion–Positive GI Cancers: An International Data Set and a Molecular Case Series. JCO Precis. Oncol. 2022;6:e2200015. doi: 10.1200/PO.22.00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Shaw A.T., Kim T.M., Crinò L., Gridelli C., Kiura K., Liu G., Novello S., Bearz A., Gautschi O., Mok T., et al. Ceritinib versus chemotherapy in patients with ALK-rearranged non-small-cell lung cancer previously given chemotherapy and crizotinib (ASCEND-5): A randomised, controlled, open-label, phase 3 trial. Lancet Oncol. 2017;18:874–886. doi: 10.1016/S1470-2045(17)30339-X. [DOI] [PubMed] [Google Scholar]
- 86.Amatu A., Sartore-Bianchi A., Bencardino K., Pizzutilo E., Tosi F., Siena S. Tropomyosin receptor kinase (TRK) biology and the role of NTRK gene fusions in cancer. Ann. Oncol. 2019;30:viii5–viii15. doi: 10.1093/annonc/mdz383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Hong D.S., DuBois S.G., Kummar S., Farago A.F., Albert C.M., Rohrberg K.S., van Tilburg C.M., Nagasubramanian R., Berlin J.D., Federman N., et al. Larotrectinib in patients with TRK fusion-positive solid tumours: A pooled analysis of three phase 1/2 clinical trials. Lancet Oncol. 2020;21:531–540. doi: 10.1016/S1470-2045(19)30856-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.O’Reilly E., Hechtman J. Tumour response to TRK inhibition in a patient with pancreatic adenocarcinoma harbouring an NTRK gene fusion. Ann. Oncol. 2019;30:viii36–viii40. doi: 10.1093/annonc/mdz385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Doebele R.C., Drilon A., Paz-Ares L., Siena S., Shaw A.T., Farago A.F., Blakely C.M., Seto T., Cho B.C., Tosi D., et al. Entrectinib in patients with advanced or metastatic NTRK fusion-positive solid tumours: Integrated analysis of three phase 1–2 trials. Lancet Oncol. 2020;21:271–282. doi: 10.1016/S1470-2045(19)30691-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Werr L., Plenker D., Dammert M.A., Lorenz C., Brägelmann J., Tumbrink H.L., Klein S., Schmitt A., Büttner R., Persigehl T., et al. CD74-NRG1 Fusions Are Oncogenic In Vivo and Induce Therapeutically Tractable ERBB2:ERBB3 Heterodimerization. Mol. Cancer Ther. 2022;21:821–830. doi: 10.1158/1535-7163.MCT-21-0820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Laskin J., Liu S., Tolba K., Heining C., Schlenk R., Cheema P., Cadranel J., Jones M., Drilon A., Cseh A., et al. NRG1 fusion-driven tumors: Biology, detection, and the therapeutic role of afatinib and other ErbB-targeting agents. Ann. Oncol. 2020;31:1693–1703. doi: 10.1016/j.annonc.2020.08.2335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Aguirre A.J. Oncogenic NRG1 Fusions: A New Hope for Targeted Therapy in Pancreatic Cancer. Clin. Cancer Res. 2019;25:4589–4591. doi: 10.1158/1078-0432.CCR-19-1280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Schram A.M., Goto K., Kim D.-W., Martin-Romano P., Ou S.-H.I., O’Kane G.M., O’Reilly E.M., Umemoto K., Duruisseaux M., Neuzillet C., et al. Efficacy and safety of zenocutuzumab, a HER2 x HER3 bispecific antibody, across advanced NRG1 fusion (NRG1+) cancers. J. Clin. Oncol. 2022;40:105. doi: 10.1200/JCO.2022.40.16_suppl.105. [DOI] [Google Scholar]
- 94.Subbiah V., Cassier P.A., Siena S., Garralda E., Paz-Ares L., Garrido P., Nadal E., Vuky J., Lopes G., Kalemkerian G.P., et al. Pan-cancer efficacy of pralsetinib in patients with RET fusion–positive solid tumors from the phase 1/2 ARROW trial. Nat. Med. 2022;28:1640–1645. doi: 10.1038/s41591-022-01931-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Subbiah V., Wolf J., Konda B., Kang H., Spira A.I., Weiss J., Takeda M., Ohe Y., Khan S.A., Ohashi K., et al. Tumor agnostic efficacy of selpercatinib in patients with RET fusion+ solid tumors: A global, multicenter, registrational trial update (LIBRETTO-001) J. Clin. Oncol. 2022;40:3094. doi: 10.1200/JCO.2022.40.16_suppl.3094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Davies K.D., Doebele R.C. Molecular Pathways: ROS1 Fusion Proteins in Cancer. Clin. Cancer Res. 2013;19:4040–4045. doi: 10.1158/1078-0432.CCR-12-2851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Ahmad-Nielsen S.A., Nielsen M.F.B., Mortensen M.B., Detlefsen S. Frequency of mismatch repair deficiency in pancreatic ductal adenocarcinoma. Pathol. Res. Pract. 2020;216:152985. doi: 10.1016/j.prp.2020.152985. [DOI] [PubMed] [Google Scholar]
- 98.Luchini C., Brosens L.A.A., Wood L.D., Chatterjee D., Shin J.I., Sciammarella C., Fiadone G., Malleo G., Salvia R., Kryklyva V., et al. Comprehensive characterisation of pancreatic ductal adenocarcinoma with microsatellite instability: Histology, molecular pathology and clinical implications. Gut. 2021;70:148–156. doi: 10.1136/gutjnl-2020-320726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Le D.T., Durham J.N., Smith K.N., Wang H., Bartlett B.R., Aulakh L.K., Lu S., Kemberling H., Wilt C., Luber B.S., et al. Mismatch repair deficiency predicts response of solid tumors to PD-1 blockade. Science. 2017;357:409–413. doi: 10.1126/science.aan6733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Marabelle A., Le D.T., Ascierto P.A., Di Giacomo A.M., De Jesus-Acosta A., Delord J.-P., Geva R., Gottfried M., Penel N., Hansen A.R., et al. Efficacy of Pembrolizumab in Patients with Noncolorectal High Microsatellite Instability/Mismatch Repair–Deficient Cancer: Results from the Phase II KEYNOTE-158 Study. J. Clin. Oncol. 2020;38:1–10. doi: 10.1200/JCO.19.02105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Padrón L.J., Maurer D.M., O’Hara M.H., O’Reilly E.M., Wolff R.A., Wainberg Z.A., Ko A.H., Fisher G., Rahma O., Lyman J.P., et al. Sotigalimab and/or nivolumab with chemotherapy in first-line metastatic pancreatic cancer: Clinical and immunologic analyses from the randomized phase 2 PRINCE trial. Nat. Med. 2022;28:1167–1177. doi: 10.1038/s41591-022-01829-9. [DOI] [PMC free article] [PubMed] [Google Scholar]