Abstract
Alzheimer’s disease (AD) is a neurodegenerative disorder characterized by senile plaques formed by amyloid-beta (Aβ) extracellularly and neurofibrillary tangles (NFTs) formed by hyperphosphorylated tau protein intracellularly. Apart from these two features, insulin deficiency and insulin resistance have also been observed in AD brains. Thus, AD has also been referred to as type 3 diabetes by some of the scientists in this field. Insulin plays a pivotal role in learning and memory and is involved in regulating tau phosphorylation though the PI3KAkt-GSK3b signaling pathway. Interestingly, recent studies revealed that in AD brains the microglia transformed into a disease-associated microglia (DAM) status in a TREM2-dependent manner to restrain the toxicity of Aβ and propagation of tau. This also correlated with PI3K-Akt signaling through the adaptor of TREM2. Whether insulin has any effect on microglia activation in AD pathology is unclear so far. However, many studies demonstrated that diabetes increased the risk of AD. In this review, we summarize the main strategies for curing AD, including lowering the level of Aβ, suppressing the phosphorylation of tau, the ablation and/or repopulation of microglia, and especially the supply of insulin. We also propose that attention should be given to the influences of insulin on microglia in AD.
Keywords: Alzheimer’s disease, insulin resistance, amyloid-beta, tau phosphorylation, microglia
1. Introduction
Alzheimer’s disease (AD) is known as the most common form of dementia that occurs with aging. The histopathological characteristics of AD are defined by extracellular deposits of amyloid-beta (Aβ) and intracellular neurofibrillary tangles (NFTs) formed by hyperphosphorylated tau protein. Apparently, the initiation of AD is closely associated with the extent of Aβ production, as evidenced by familial AD cases. Those who carry the mutated amyloid precursor protein (APP) and/or presenilin-1/2 (PS1/2, the components of γ-secretase) tend to acquire an accumulation of Aβ plaques in the brain and probably suffer AD earlier. However, the degree of dementia is more strongly correlated with NFT burden than Aβ senile plaques [1], raising the notion that AD may be a secondary tau pathology.
In 2018, a research framework was suggested by the National Institute on Aging and Alzheimer’s disease Association (NIA-AA) to unify the pathological definition and staging of AD based on biological construct [2]. Those biomarkers are grouped into Aβ (A), pathologic tau (T), and neurodegeneration (N). Given that 30–40% of cognitively unimpaired elderly persons have abnormal amyloid biomarkers at autopsy, this proportion of amyloid-positive individuals will perfectly match the number of diagnosed AD patients 15–20 years later. This framework advised that Aβ alone with a normal pathologic tau biomarker (A+T−) can be assigned the label “Alzheimer’s pathologic change”, which refers to the earlier phases of the “Alzheimer’s continuum”. However, it may not be sufficient to cause tauopathy and neurodegeneration that finally lead to cognitive disorder. In addition, when the biomarker of both Aβ and tauopathy are present (A+T+), the term “Alzheimer’s disease” can be used to delegate the later phases of the “Alzheimer’s continuum”.
However, the overloading of Aβ is speculated to be a causal factor for AD onset in the “Aβ cascade” hypothesis [3]. The subsequent tauopathy and neurodegeneration is considered to be more correlated with dementia and other clinical features of AD. Therefore, in considering the “Alzheimer’s continuum”, different therapeutic strategies have been adopted in AD treatment. For example, preventing the overproduction of Aβ and/or accelerating the clearance of Aβ, avoiding the hyperphosphorylation of tau, restraining the spread of tau, and arresting the activation microglia. Here, we review the relationship between Aβ accumulation, the insulin signaling pathway, tau hyperphosphorylation, and microglia activation (Figure 1), and we summarize different strategies for AD treatment, particularly the intermediary role of insulin signaling in AD pathology.
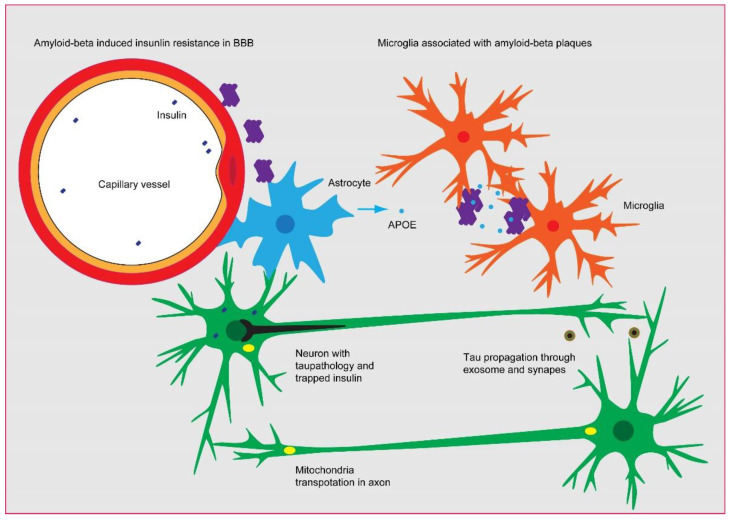
Figure 1.
The probable linkage between Aβ, insulin signaling, tau pathology, and microglia activation in AD. The constant production of Aβ needs to be eliminated by microglia through endocytosis and/or by the drainage of micro-vessels, as evidenced by the association of Aβ plaques with microglia and micro-vessels in AD brain. However, the overloading of Aβ leads to the impairment of insulin sensing in the brain–blood barrier and parenchyma, which triggers the phosphorylation of tau and subsequently perturbs mitochondria and insulin secretion. The tau pathology could be propagated via the synapse and exosome in a microglia-dependent manner, eventually leading to neural atrophy.
2. Restricting the Overload of Aβ
APP is a type I transmembrane protein, which is involved in regulating synaptic functions [4] and iron export [5]. APP has three common alternative splicing variants in the brain, and the size of each is 695, 751, and 770 amino acids, respectively. APP695 lacks the Kunitz-type protease inhibitor sequence in its ectodomain and is one of the most abundant proteins that is expressed by neurons. APP751 and APP770 are mainly expressed in glial cells. The cleavage of APP by α-secretase is a non-amyloidogenic pathway which produces a soluble APPα fragment and an 83-amino-acid C-terminal fragment (CTF-83). The CTF83 is further decomposed by γ-secretase, releasing a small P3 fragment into the extracellular space and the APP intracellular domain (AICD) into the cytoplasm. In contrast, the cleavage of APP by β-secretase is an amyloidogenic process, which releases a soluble APPβ ectodomain and a 99-amino-acid C-terminal fragment (CTF99). The cleavage of CTF99 by γ-secretase generates an Aβ and AICD fragment as well [6].
Mutations in the APP, ADAM10 (a disintegrin and metalloproteinase domain 10), and PS1/2 genes are closely related to the onset of AD. The APP gene is located on chromosome 21; not only do the mutations within and immediately flanking the Aβ region of APP cause an aggressive form of FAD, but an individual with trisomy 21 (Down’s syndrome) harboring three copies of APP also exhibits abundant diffuse Aβ plaques in their brain and invariably develops neuropathologically typical AD. In addition, mutations that attenuate secretase activity of ADAM10, the main α-secretase accounting for APP proteolysis, are associated with elevated Aβ levels [7,8]. Moreover, PS1 and PS2 are critical components of the γ-secretase complex. Missense mutations in PS1/PS2 are found to result in an increasing production of Aβ-42/43 peptides, which are an aggregation-prone species and lead to profound Aβ deposition [9]. The toxicity of soluble Aβ oligomer has been observed in various cellular processes. For example, Aβ oligomers could directly interact with membranes to form pores for ions and disrupt the proper permeability of the membranes [10], leading to the depolarization of neurons and microglia [11]. The soluble oligomers could also inhibit LTP through excessive activating of NR2B containing the NMDA receptor [12] (Figure 2) and perturb the synaptic plasticity through mitochondria [13,14]. In addition, Aβ oligomers could induce inflammation through receptor-mediated mechanisms [15] and impair the integrity of the blood–brain barrier [16].
Many efforts have been made to reduce the production of Aβ for the purpose of curing AD. For example, synthetic retinoid acitretin, which enhances the expression of ADAM10, the most effective α-secretase for APP, showed beneficial effects in AD patients [17]. In addition, an ADAM10 endocytosis inhibitor has been developed recently, which can upregulate the postsynaptic localization and activity of ADAM10 to increase the non-amyloidogenic process of APP [18]. On the other hand, the inhibitor of the β-site amyloid precursor protein cleaving enzyme-1 (BACE1), namely, β-secretase, has also been tested in the clinic. For example, verubecestat and lanabecestat could reduce the level of Aβ in cerebrospinal fluid by 63% to 81%. However, this had no beneficial effect on cognition, other than adverse side effects including sleep disturbance, weight loss, and decreased appetite [19,20]. Moreover, small molecule inhibitors of γ-secretase, such as semagacestat and avagacestat, have been found to successfully reduce Aβ production in AD transgenic mice and patients. Nevertheless, due to the nonselective inhibitory effects on both APP and Notch, they failed in clinical trials [21].
In the brain, ADAM10 is mainly localized in the synapse. Knockout of ADAM10 results in embryonic death in E9. BACE1 is usually found in the plasma membrane in the endosome and Golgi apparatus, functioning at an optimal pH of 4.5. Knockout of BACE1 leads to diabetes and hypomyelination. In contrast to ADAM10 and BACE1, γ-secretase is a transmembrane protein complex containing presenilin, nicastrin, anterior pharynx defective 1 (Aph-1), and presenilin enhancer-2 (Pen-2). The catalytic site of γ-secretase is located in the PS subunit, which has two homologs in mammalian cells, PS1 and PS2. Knockout of PS1 results in Notch signaling deficiency and is lethal for mice. PS2 knockout mice are normal. Moreover, both nicastrin and Aph-1 knockout mice have shown embryonic lethality. ADAM10, BACE1, and γ-secretase have many other substrates apart from APP, including the components of the Notch signaling pathway and other transmembrane proteins such as Neuroligin 1 and Neuregulin. BACE1 also plays an important role in insulin signaling conduction by the cleavage of the insulin receptor, reducing its expression on the cell surface [22,23]. Therefore, it is not surprising that the inhibition of BACE1 and γ-secretase result in undesirable outcomes.
Another way of lowering the accumulation of Aβ is to accelerate its clearance in the brain, either through the phagocytosis of microglia or the drainage of micro-vessels. It has been clearly demonstrated that the dysfunction of Aβ clearance is associated with the late onset of AD. For example, the rate of transport across the blood–brain barrier and perivascular drainage to the systemic circulation was slowed down for the Aβ Dutch variant compared with Aβ WT. Additionally, the APOE4 variant—the strongest genetic risk factor for AD except for mutations in APP and PS1/2—could affect the endocytosis process and increase Aβ accumulation at the blood–brain barrier (BBB) [24]. In addition, the cell surface triggering receptor expressed on myeloid cells 2 (TREM2), which is expressed in microglial, is found to be upregulated by Aβ and facilitates the phagocytosis of Aβ. The R47H mutation in TREM2, which is also one of the strongest genetic risk factors for AD, perturbed the activation of microglia and led to Aβ deposition [25]. Moreover, phospholipase D3 (PLD3), bridging integrator 1 (BIN1), phosphatidylinositol-binding clathrin assembly protein (PICALM) [26], and sortilin-related receptor (SORL1)—the next strongest genetic risk factors of AD after APOE4 and TREM2—were also involved in regulating the endocytosis process [27,28]. This indicates that the clearance of Aβ is an important way of curing AD. To improve the acceleration of Aβ, the monoclonal antibody of Aβ oligomers, such as aducanumab, has been clinically used [29]. It significantly reduced the level of Aβ plaque accumulation. However, the side effects, such as encephaledema, were also observed in a large portion of the subjects [30], implying that the elimination of Aβ through antibody-mediated endocytosis is feasible in AD, but researchers should be cautious of overactivating microglia and impairing endothelial cells in BBB.
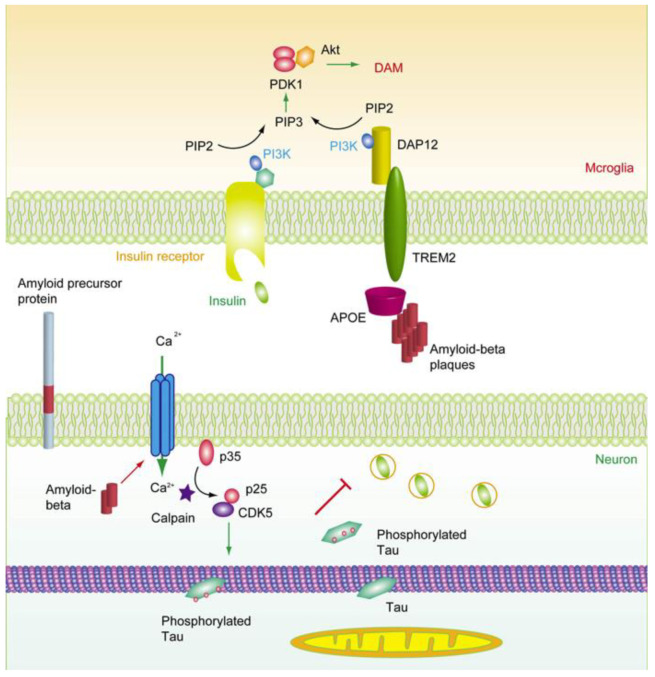
Figure 2.
The deductive role of insulin signaling in AD pathology. Aβ induced calcium influx and the activation of calpain, which further triggered the activation of CDK5 through the cleavage of p35 [31]. CDK5 induced phosphorylation of tau, triggered the detachment of tau from microtubules, and in turn perturbed the function of mitochondria. On the other hand, the microglia switch homeostasis to DAM status in an APOE- and TREM2-dependent manner to protect neurons from the damaging effect of Aβ overproduction [32,33]. TREM2 functions via its adaptor DAP12 (DNAX activation protein of 12 kDa) and PI3K-Akt pathway, which is also regulated by insulin signaling. Thus, insulin can inhibit tau phosphorylation by suppressing GSK3β in neurons and help microglia to maintain the proper DAM status via PI3K-Akt pathway.
3. Rescuing Insulin Signaling
In 2005, Eric et al., proposed to use “Type 3 diabetes” to reflect the abnormal changes in the levels of insulin, insulin-like growth factor (IGF) I/II, insulin receptor (IR), and insulin receptor substrate (IRS) in the brains of AD patients [34]. IR and IGF receptors were found to be highly expressed in neuron and glial cells throughout the brain [35,36]. However, more recently, single-cell transcriptomic analyses have indicated that the mRNA transcript of IR is found in higher concentrations in endothelial cells in the brain [37]. The insulin-induced activation of IR at the BBB was blunted in transgenic AD model mice [38,39]. Meanwhile, insulin deficiency was observed in mild cognitive impairment patients and early-stage AD patients [40]. Importantly, it has also been demonstrated that Aβ has a similar tertiary structure to insulin, leading to Aβ being a competitive inhibitor for insulin. Aβ oligomers have been shown to inactivate IRS-1 and reduce its level [41], which in turn abolishes the inhibitory activation of insulin on glycogen synthase kinase -3 (GSK-3β) and further results in tau hyperphosphorylation [42].
Insulin comes from either synthesis de novo in the brain [43] or passing through the blood–brain barrier (BBB) from the plasma to the brain via the capillary endothelial cells by a selective, saturable, receptor-dependent mechanism [44,45]. By binding to the IR and IGF receptors, insulin facilitates the phosphorylation of IRS and subsequently activates phosphatidylinositol-3-kinase (PI3K) and AKT (protein kinase B, PKB). Thus, the glucose transporter 4 (GLUT4) in cytosol is recruited onto the plasma membrane to promote glucose uptake [46]. Insulin-induced transportation of GLUT4 plays an important role in hippocampal-dependent memory [47]. The activation of AKT further regulates the activity of the mammalian target of rapamycin (mTOR), GSK-3β, and cAMP-responsive element-binding protein (CREB). The mTOR pathway regulates various cellular functions, including glucose metabolism, mitochondrial oxidative respiration, and autophagy. Of note, GSK-3β is involved in the phosphorylation of tau as well as energy metabolism. On the other hand, IRS can also activate growth factor receptor-bound protein 2 (Grb2) which in turn stimulates SOS1 and Ras, Raf, and mitogen-activated protein kinases (MAPK) [48]. Interestingly, APOE is also involved in modulating PI3K/Akt signaling [49,50]. The APOE4 variant can reduce the levels of insulin receptor substrate-1 and PI3K, decrease Akt phosphorylation [51], and impair neuronal insulin signaling by trapping the insulin receptor in the endosomes [52]. Moreover, the activation of TREM2 also modulated PI3K/Akt signaling [53,54]. The mutation of TREM2, which is correlated with the onset of AD, impaired its activity on PI3K-AKT-GSK3β through SYK [55]. The activation of microglia mediated by TREM2 also regulated the phosphorylation of tau through GSK3β [56] (Figure 2).
AD patients showed lower CSF insulin levels, higher plasma insulin levels, and reduced CSF/plasma insulin ratios compared to healthy controls [57]. It has been reported that the insulin-degrading enzyme (IDE) level was reduced in the hippocampus of AD patients; however, it was increased in the micro-vessels in AD with CAA [58]. IDE is able to degrade both insulin and Aβ [59] as well as many other molecules with amyloidogenic potential, such as glucagon, amylin, calcitonin, and atrial natriuretic peptide [58]. It has also been observed that in mice lacking IDE the accumulation of endogenous brain soluble Aβ was increased. In contrast, transgenic overexpression of IDE in neurons reduced the brain soluble Aβ level and delayed amyloid plaque formation in APP transgenic mice. In addition, the level of IDE in theAPOE4 carrier was reduced by approximately 50% [60], indicating that the shortage of insulin in AD brain may enhance Aβ accumulation through downregulating the IDE level. On the other hand, in the insulin knockout mice model, the phosphorylation of tau was enhanced, thereby leading to the formation of NFTs [61]. Using streptozotocin (STZ) to deplete insulin could also induce the tau pathology [62]. Insulin receptor substrate 2 (IRS2) knockout could promote the phosphorylation of tau as well [63]. Collectively, this evidence consistently demonstrates that insulin signaling dysfunction and abnormal insulin levels have a profound influence on AD pathology.
A previous study indicated that intranasal insulin administration was able to improve memory in humans [64]. The verbal memory in AD and MCI subjects without the APOE4 allele was improved 15 min after intranasal insulin 40 IU administration, and the plasma insulin or glucose levels were not perturbed [65]. Another trial administrated a placebo or 20 IU or 40 IU of insulin detemir with a nasal drug delivery device to treat adults diagnosed with MCI or mild to moderate AD. A 21-day treatment with 20 IU of insulin increased the plasma concentration of the Aβ-40 without affecting the level of Aβ-42, resulting in an increased Aβ 40/42 ratio [66]. The results also showed that 40 IU significantly improved the verbal working memory and visuospatial working memory. However, these effects were modulated by the APOE status. Insulin treatment reduced the insulin resistance in APOE4 carriers but not in APOE4-negative ones [67]. Craft et al., also reported that regular insulin treatment reduced the tau-p181/Aβ42 ratio in plasma and preserved the brain volume [68]. The intranasal administration allowed insulin arriving in the CNS to bypass the periphery and prevents the risks associated with hypoglycemia [69]. However, more recently, in a randomized clinical trial of 289 adults with mild cognitive impairment or AD, the intranasal insulin treatment showed no cognitive or functional benefits for the patients [70], but the limitation in this study was that the device used for intranasal insulin supply had not been tested before. Thus, further studies are still required to ascertain the underling mechanism of how insulin supply may work for curing AD.
Insulin sensitizers that were used in treating type 2 diabetes also showed positive effects for curing AD. The peroxisome proliferator-activated receptor (PPAR-γ) agonists such as pioglitazone [71] and rosiglitazone [72] improved memory and stabilized plasma Aβ42 concentrations. The administration of 10–30 mg/day of pioglitazone for 6 months to AD patients accompanied with type 2 diabetes mellitus decreased fasting plasma insulin levels. The administration of rosiglitazone 4 mg/day for a 6-month course improved the delayed recall and selective attention of AD subjects. The plasma Aβ levels were not increased with the progression of AD and declined compared with the control group which received a placebo [72,73]. Another study accomplished by Risner et al., demonstrated that 8 mg/day of rosiglitazone treatment for 24 weeks significantly improved the non-APOE4-positive AD patients [74]. However, a phase 3 trial showed no effects on cognition, regardless of APOE type [75]. The effects of antidiabetic drugs are also under evaluation in AD therapy. In transgenic AD mice, metformin increased the IDE level [76] and prevented amyloid plaque deposition and memory impairment [77]. A study on primary neurons from wild-type mice showed that metformin induced the PP2A-dependent dephosphorylation of tau [78]. Clinically, the use of metformin showed protective effects on brain volumes in non-demented elderly individuals with diabetes [79]. For mild cognitive impairment or mild dementia due to AD, metformin also improved executive functioning [80]. The vanadium compounds that were used in treating diabetes also showed a protective effect in AD transgenic mice models through regulating PPARγ [81,82,83]. However, it is unknown whether these antidiabetic agents are efficient in the late stage of AD.
4. Preventing Tau Pathology
Although Aβ overload is believed to be the most important risk factor for AD development, it is worth noting that there are a great many people bearing Aβ plaques in their brains who do not exhibit dementia symptoms unless the tau pathology or cerebral amyloid angiopathy (CAA) occurs. On the other hand, it was demonstrated that the presence of Aβ plaques facilitated local tau seeding in dystrophic neurites that led to the spreading and formation of phosphorylated forms of tau in neuritic plaques and NFTs in mice [84]. In addition, the reduction in tau has been found to protect neurons from the loss of mitochondrial membrane potential [85], excitotoxicity [86], and axonal transport inhibition [87] induced by Aβ [88], indicating that tau is a critical target for AD treatment. Tau is a microtubule-associated protein involved in microtubule stabilization and intracellular cargo transport. Tau is encoded by the MAPT gene, which is located on chromosome 17. In the human brain, exons 2 and 3 of MAPT account for the two N-terminal repeats (N), while exon 10 encodes the second microtubule-binding repeat (R) of four in total. Therefore, the alternative splicing of MAPT yields six distinct isoforms of tau, which are 0N3R, 0N4R, 1N3R, 1N4R, 2N3R, and 2N4R. Knockout of tau led to glucose intolerance [89] and impaired the hippocampal response to insulin by modulating the phosphatase and tension homologue on chromosome 10 (PTEN) [90]. Tau deletion also contributed to the accumulation of iron in the brain, resulting in conditions such as Parkinson’s disease [91]. However, it has also been found that in a type 1 diabetes model induced by STZ, tau knockout attenuated the cognitive impairment triggered by insulin deficiency [92], whereas human tau transgenic mice showed robust deficits in learning and memory processes under the same conditions [93]. These observations suggest that tau itself is closely related to cell signaling implementation rather than only taking part in stabilizing microtubules.
Notably, tau pathology is not only presented in AD but also associated with many other tau pathologies, such as chronic traumatic encephalopathy (CTE), a subclass of frontotemporal dementia with Parkinsonism linked to chromosome 17 (FTDP-17tau); Pick’s disease (PiD); progressive supranuclear palsy (PSP); corticobasal degeneration (CBD); and argyrophilic grain disease (AGD) [94]. As mentioned above, in AD the neurofibrillary tangles formed by tau aggregation usually initiate in the neurons of the medial temporal lobe regions (i.e., hippocampus, entorhinal cortex, and amygdala) in the form of both 3R and 4R tau. Likewise, in CTE, the tau filaments are also detected in frontal and temporal cortices in the form of both 3R and 4R. However, in PiD, tau pathology is mainly found in granular neurons in the hippocampal dentate gyrus, the hippocampal CA1 pyramidal neurons, and layer II of the frontal and temporal cortices in the form of 3R, while in PSP, CBD, and AGD it mainly presents in the form of 4R in astrocytes. The affected regions include the basal ganglia, subthalamic nucleus, substantia nigra, and limbic lobe.
Mutated human tau has been found in familial primary tau pathology but not in AD. Many mutations function in reducing the affinity of tau to microtubules, facilitating its phosphorylation by altering the interaction with other proteins, impairing the splicing of exon 10, or promoting the aggregation of tau into a beta-sheet structure. The mutation of tau is also known to induce insulin resistance [95,96] by increasing pSer-IRS1 [97] and to cause insulin accumulation as oligomers [98]. In addition, the MAPT gene has two main haplotypes, namely, H1 and H2, as a result of a 900 kb inversion in the q21 region of chromosome 17. The H1/H1genotype is considered a risk factor for PSP, CBD, and AGD. Moreover, the H1/H2 genotype confers a greater risk of developing dementia before the age of 45 years in individuals with Down’s syndrome. Tau species are capable of propagating from neuron to neuron through exosomes [99]. The propagation of tau raised the notion that tau is a prion protein which spreads in a conformational, strain-specific manner [100], and the toxicity of tau spreading is dependent on endogenous tau [101]. These above observations suggest that AD is likely a secondary tau pathology.
In the NFTs of AD and other tau pathologies, tau is hyperphosphorylated. The hyperphosphorylation of tau results in its dissociation from the microtubules; the detached tau misfolds and begins to aggregate and form the NFT. The posttranslational modifications of tau play an important role in tau aggregation. The phosphate group, methyl groups, and acetyl group to lysine residue change the basic character of tau. To evaluate the effects of phosphorylation on aggregation, scientists used Asp and/or Glu to replace the Ser320 and Ser324 on the R3 fragment of tau, which is the core of the NFT, and found that these pseudophosphorylations enhanced the aggregation of tau [102,103]. In another study, Briner et al., showed that in Src family non-receptor tyrosine kinase Fyn knockout mice the tau hyperphosphorylation was reduced, along with the near-complete ablation of NFTs [104]. However, when using chemical methods to synthesize the phosphorylated K18 fragment (four microtubule-binding repeats), the study showed that the phosphorylation at S258, S262, and S356 dramatically reduced the aggregation and fibril seeding activity of K18 in vitro [105]. Similarly, the phosphorylation at Tyr310 were also found to inhibit the aggregation and microtubule-binding activity of full-length tau and the K18 fragment [106]. Overall, it seems that the phosphorylation at different residues may have an alternative influence on the aggregating property [107]. Additionally, the phosphorylation of tau at the KXGS motifs in the C-terminal microtubule-binding domains prevented the ubiquitination and degradation of tau by proteasome. Likewise, the phosphorylation at S293, S324, and S356 inside the microtubule-binding domains diminished its degradation through the lysosome system. However, it seems that the NFT itself is not the direct reason for cognitive decline or neuronal death [108], whereas the phosphorylated tau promoted mitochondrial dysfunction in neurons with an FTLD mutant by impairing complex I of the electron transport chain [109,110]. The phosphorylated tau has also been demonstrated to interact with dynamin-related GTPase Drp1, thus promoting mitochondrial fission and morphology change [111]. Besides the hyperphosphorylation, the cleavage of tau has been found to precede and promote the tangle formation [112]. More importantly, the cleaved tau also induced the dysfunction of mitochondrial dynamics [113,114] (Figure 2).
Multiple kinases are involved in tau phosphorylation, including GSK-3β [115], AMP-activated protein kinase (AMPK) [116], cyclin-dependent protein kinase 5 (CDK5), CDK2, and CaMKII. Conversely, the dephosphorylation of tau is mainly afforded by protein phosphatase 2A (PP2A) [117]. Since the abnormal phosphorylation of tau is closely correlated with the aggregation, accumulation, and toxicity of tau pathology, the molecules that inhibit tau phosphorylation have been tested in curing AD. The functions of GSK3β have been extensively studied in cell proliferation, embryonic development, and immune response. It has been well established that phosphorylation at serine 9 and 389 inhibits GSK3β activity whereas phosphorylation at tyrosine 216 increases its activity. Lithium is a selective GSK3β inhibitor which acts by competition with magnesium in the ATP-binding pocket. In vitro and in vivo studies clearly showed that lithium treatment effectively reduced tau phosphorylation [118]. Other non-ATP-competitive GSK3β inhibitors, such as Tideglusib [119,120], oxadiazole containing small molecules, and pyrimidinone containing small molecules also showed beneficial effects in an AD model [121]. However, the adverse effects of GSK3β inhibitors were monitored in control animals [120], suggesting that a more specific inhibitor of GSKβ on tau phosphorylation is needed in future studies. In contrast to the kinases that induce the phosphorylation of tau, PP2A is responsible for the dephosphorylation of tau. In the brain of AD patients, the protein level and phosphatase activity of PP2A was reduced [122]. Transgenic mice with reduced PP2A activity presented somato-dendritic accumulation of hyperphosphorylated and aggregated tau in cortical pyramidal cells [123]. Using okadaic acid to inhibit PP2A and PP1 also increased tau phosphorylation [124]. The sphingosine-1-phosphate receptor selective agonist SEW2871 has been shown to reduce the tau Ser262 phosphorylation via the AMPK-PP2A pathway [125]. In addition, the zinc chelator clioquinol has been demonstrated to be capable of elevating PP2A activity and deceasing PP2A Tyr307 phosphorylation [126]. However, the problem with these PP2A agonists remains because of lacking specificity for different substrates.
5. Microglia Depletion and Repopulation
Microglia are innate immune cells in the brain which originate from erythromyeloid progenitor cells in the yolk sac [127]. Microglia exhibit a remarkable capacity for proliferation and self-regeneration in the central nervous system [128]. In the brain, microglia serve as resident phagocytes, playing an important role in pathogen defense and injury response. Microglia are also involved in sculpting synapses by phagocytizing inappropriate synaptic connections, which is necessary for normal brain development [129]. In the brain of AD patients, microglia are stably associated with Aβ deposition [130], and they are responsible for Aβ uptake and clearance [131]. However, Aβ aggregates can act as disease-associated molecular patterns and trigger microglia activation through pattern recognition receptors, such as Toll-like receptors and NRLP3 inflammasomes [132,133], leading to the secretion of TNFα, IL1β, and other inflammatory cytokines. Single-cell sequencing revealed that the mRNA profiles of microglia in the brain of AD patients were switched from the homeostatic stage to the disease-associated microglial (DAM) stage [134,135].
Chemically or genetically activating microglia significantly accelerated tau pathology and behavioral abnormalities in the human tau mouse model of tauopathy [136,137]. In addition, deleting the microglia protein Cx3cr1 in transgenic tau models showed that the onset and progression of tau pathology were accelerated by artificially activating microglia. Moreover, APOE4 variants were found to exacerbate the tau pathology in tau P301S transgenic mice in a microglia-dependent manner [138]. However, other studies demonstrated that the activated microglia mitigate Aβ-associated tau seeding and spreading [139]. TREM2 deficiency and mutation leads to a decrease in Aβ-plaque-associated microglia and facilitates the seeding and spreading of neuritic plaque tau aggregates [140,141]. It was suggested that, although DAM attenuated the progression of neurodegeneration in certain mouse models, inappropriate DAM activation accelerates neurodegenerative disease [142]. Interestingly, APOE [49] and TREM2 [55] are both implicated in regulating the DAM status through the PI3K and Akt signaling pathways (Figure 2). It is also worth noting that the mutation of TREM2 is not only associated with the onset of sporadic AD but also correlated with Parkinson’s disease, ALS, and frontotemporal dementia [143].
Microglia are critically dependent on the colony-stimulating factor-1 receptor (CSF1R) for their survival [144]. CSF1R is expressed on all myeloid cells, so the signaling interference through this receptor will not only affect microglia cells but also influence peripheral macrophages [145]. For this reason, Csf1r−/− mice display mononuclear phagocyte deficiency, neurodevelopmental abnormality, and a shortened lifespan [146,147]. Thus, a pharmacological method to deplete microglia were used in the AD model. GW2580 is the first reported CSF1R-kinase inhibitor as well as the first CSF1R inhibitor utilized in a mouse model of AD [148,149]. It blocks microglial proliferation, shifts the microglial transcriptomic profile to an anti-inflammatory profile in APP/PS1 mice, and prevents cognitive decline, although it did not modify the burden of Aβ [149]. Although the microglia are capable of clearing Aβ, the depletion of microglia in mice with established brain amyloid had no effect on Aβ deposition but resulted in less spine and neuronal loss [150]. It is suggested that following the initial period of plaque formation, microglia surround the plaques and subsequently mount a harmful and non-resolving inflammatory response; however, prolonged depletion of microglia throughout the plaque-forming period impaired the plaque formation, compaction, and growth [151].
Pexidartinib is a selective CSF1R/KIT/FLT3 inhibitor [152]. Treatment with pexidartinib enabled the depletion of more than 99% of all microglia for 3 or 8 weeks in adult mice with no deficits in any behavioral cognitive task administered [153,154]. The depletion of microglia by a CSF1R inhibitor was found to arrest tau propagation in PS19 mice and in C57 mice that were forced to express tau by an adeno-associated virus (AAV) [155], suggesting that microglia are involved in the cell-to-cell spread of tau. In mice with forced P301L tau overexpression, Calton et al., found that the depletion of microglia using PLX5622 dramatically reduced the propagation of phosphorylated tau [156]. Casali et al., demonstrated that in 5xFAD mice PLX5622 elicited microglial repopulation and subsequent plaque remodeling, resulting in more compact plaques predominating microglia-repopulated regions. Microglia limit diffuse plaques by maintaining compact-like plaque properties, thereby blocking the progression of neuritic dystrophy [157]. Similarly, Gratuze et al., found that after microglia depletion using PLX3397, repopulated microglia clustered around plaques, and they found a reduction in disease-associated microglia (DAM) gene expression [139]. However, another study stated that the repopulation of microglia induced by PLX5622 did not impact the amyloid pathology in 3xAD model mice but did change the phosphorylation style of tau [158].
6. Conclusions and Perspectives
To date, many hypotheses of AD etiology have been proposed based on clinical research and experimental data, including the amyloid cascade hypothesis [159], cholinergic hypothesis [160], neuroinflammatory hypothesis [161], mitochondrial hypothesis [162], oxidative stress hypothesis [163], insulin resistance hypothesis [164], and calcium hypothesis [165]. They are also supported by substantial evidence. In this review, we tried to piece together the evidence and find the key nodes that link amyloid-beta overproduction, neuroinflammation, insulin resistance, tau pathology, mitochondrial impairment, and neuron death.
Previously, the Aβ oligomer mono-antibody aducanumab had been approved by the FDA; it showed great efficiency in clearing Aβ from the parenchyma of the brain, though side effects, such as encephaledema, were also seen (Table 1). These observations suggest that accelerating the clearance of Aβ with an antibody is viable with the proper dose in an earlier stage of AD. However, with the presence of tau pathology it may not be enough to stop the progress of AD only by reducing the level of Aβ. Based on the evidence collected, we propose that the insulin signaling pathway may act as a linkage between Aβ, tau pathology, and microglia activation. Efficient insulin supply may prevent or postpone the initiation of tau pathology. On the other hand, it may be helpful to maintain microglia homeostasis through the PI3K-Akt pathway to restrain the propagation of tau (Figure 2).
Table 1.
Overview of different strategies for the treatment of AD.
| Strategies | Targets | Drugs or Methods | Anticipating Function | Side Effects |
|---|---|---|---|---|
| Lowering Aβ | ADAM 10 | Retinoid acitretin PEP3 |
Activating ADAM10 Upregulating the postsynaptic localization and activity of ADAM10 |
Perturbed unspecific substrates besides APP |
| BACE1 | Verubecestat Lanabecestat |
BACE1 inhibitor | Perturbed unspecific substrates besides APP | |
| γ-secretase | Semagacestat Avagacestat |
γ-secretase inhibitor | Perturbed unspecific substrates besides APP | |
| Aβ-oligomer | Aducanumab | Aβ-oligomer antibody | Encephaledema | |
| Increasing insulin signaling | Insulin deficiency | Intranasal insulin administration | Increasing insulin level in CNS | - |
| Insulin insensitivity | Metformin | Increasing insulin insensitivity | - | |
| PPARγ | Pioglitazone Rosiglitazone |
Increasing insulin insensitivity | Edema and weight gain | |
| Limiting tau phosphorylation | GSK3β | Lithium Tideglusib |
GSK3β inhibitor | Perturbed unspecific substrates besides tau |
| PP2A | SEW2871 Zinc chelator clioquinol |
PP2A activator | Perturbed unspecific substrates besides tau | |
| Restrict inflammations | Microglia | GW2580 PLX5622 PLX3397 |
Depletion and repopulation of microglia | - |
Author Contributions
G.Y. and N.L. wrote the manuscript. G.Y. created the table. J.Y. drew the figure. Q.L. and N.L. revised the manuscript. All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
Shenzhen-Hong Kong Institute of Brain Science—Shenzhen Fundamental Research Institutions (2021SHIBS0003).
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Busche M.A., Hyman B.T. Synergy between amyloid-beta and tau in Alzheimer’s disease. Nat. Neurosci. 2020;23:1183–1193. doi: 10.1038/s41593-020-0687-6. [DOI] [PubMed] [Google Scholar]
- 2.Jack C.R., Bennett D.A., Blennow K., Carrillo M.C., Dunn B., Haeberlein S.B., Holtzman D.M., Jagust W., Jessen F., Karlawish J., et al. NIA-AA Research Framework: Toward a biological definition of Alzheimer’s disease. Alzheimer’s Dement. 2018;14:535–562. doi: 10.1016/j.jalz.2018.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hardy J.A., Higgins G.A. Alzheimer’s disease: The amyloid cascade hypothesis. Science. 1992;256:184–185. doi: 10.1126/science.1566067. [DOI] [PubMed] [Google Scholar]
- 4.Priller C., Bauer T., Mitteregger G., Krebs B., Kretzschmar H.A., Herms J. Synapse formation and function is modulated by the amyloid precursor protein. J. Neurosci. 2006;26:7212–7221. doi: 10.1523/JNEUROSCI.1450-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Duce J.A., Tsatsanis A., Cater M.A., James S.A., Robb E., Wikhe K., Leong S.L., Perez K., Johanssen T., Greenough M.A., et al. Iron-Export Ferroxidase Activity of beta-Amyloid Precursor Protein Is Inhibited by Zinc in Alzheimer’s Disease. Cell. 2010;142:857–867. doi: 10.1016/j.cell.2010.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Muller U.C., Deller T., Korte M. Not just amyloid: Physiological functions of the amyloid precursor protein family. Nat. Rev. Neurosci. 2017;18:281–298. doi: 10.1038/nrn.2017.29. [DOI] [PubMed] [Google Scholar]
- 7.Kim M., Suh J., Romano D., Truong M.H., Mullin K., Hooli B., Norton D., Tesco G., Elliott K., Wagner S.L., et al. Potential late-onset Alzheimer’s disease-associated mutations in the ADAM10 gene attenuate alpha-secretase activity. Hum. Mol. Genet. 2009;18:3987–3996. doi: 10.1093/hmg/ddp323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Aguero P., Sainz M.J., Garcia-Ayllon M.S., Saez-Valero J., Tellez R., Guerrero-Lopez R., Perez-Perez J., Jimenez-Escrig A., Gomez-Tortosa E. alpha-Secretase nonsense mutation (ADAM10 Tyr167*) in familial Alzheimer’s disease. Alzheimer’s Res. Ther. 2020;12:139. doi: 10.1186/s13195-020-00708-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chang Y.J., Chen Y.R. The coexistence of an equal amount of Alzheimer’s amyloid-beta 40 and 42 forms structurally stable and toxic oligomers through a distinct pathway. FEBS J. 2014;281:2674–2687. doi: 10.1111/febs.12813. [DOI] [PubMed] [Google Scholar]
- 10.Jang H., Connelly L., Arce F.T., Ramachandran S., Kagan B.L., Lal R., Nussinov R. Mechanisms for the Insertion of Toxic, Fibril-like beta-Amyloid Oligomers into the Membrane. J. Chem. Theory Comput. 2013;9:822–833. doi: 10.1021/ct300916f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Morkuniene R., Cizas P., Jankeviciute S., Petrolis R., Arandarcikaite O., Krisciukaitis A., Borutaite V. Small A beta(1-42) Oligomer-Induced Membrane Depolarization of Neuronal and Microglial Cells: Role of N-Methyl-D-Aspartate Receptors. J. Neurosci. Res. 2015;93:475–486. doi: 10.1002/jnr.23510. [DOI] [PubMed] [Google Scholar]
- 12.Li S.M., Jin M., Koeglsperger T., Shepardson N.E., Shankar G.M., Selkoe D.J. Soluble A beta Oligomers Inhibit Long-Term Potentiation through a Mechanism Involving Excessive Activation of Extrasynaptic NR2B-Containing NMDA Receptors. J. Neurosci. 2011;31:6627–6638. doi: 10.1523/JNEUROSCI.0203-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang X.L., Su B., Siedlak S.L., Moreira P.I., Fujioka H., Wang Y., Casadesus G., Zhu X.W. Amyloid-beta overproduction causes abnormal mitochondrial dynamics via differential modulation of mitochondrial fission/fusion proteins. Proc. Natl. Acad. Sci. USA. 2008;105:19318–19323. doi: 10.1073/pnas.0804871105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Du H., Guo L., Yan S.Q., Sosunov A.A., McKhann G.M., Yan S.S. Early deficits in synaptic mitochondria in an Alzheimer’s disease mouse model. Proc. Natl. Acad. Sci. USA. 2010;107:18670–18675. doi: 10.1073/pnas.1006586107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.He Y., Zheng M.M., Ma Y., Han X.J., Ma X.Q., Qu C.Q., Du Y.F. Soluble oligomers and fibrillar species of amyloid beta-peptide differentially affect cognitive functions and hippocampal inflammatory response. Biochem. Biophys. Res. Commun. 2012;429:125–130. doi: 10.1016/j.bbrc.2012.10.129. [DOI] [PubMed] [Google Scholar]
- 16.Zhang Y.L., Wang J., Zhang Z.N., Su Q., Guo J.H. The relationship between amyloid-beta and brain capillary endothelial cells in Alzheimer’s disease. Neural Regen. Res. 2022;17:2355–2363. doi: 10.4103/1673-5374.335829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Endres K., Fahrenholz F., Lotz J., Hiemke C., Teipel S., Lieb K., Tuscher O., Fellgiebel A. Increased CSF APPs-alpha levels in patients with Alzheimer disease treated with acitretin. Neurology. 2014;83:1930–1935. doi: 10.1212/WNL.0000000000001017. [DOI] [PubMed] [Google Scholar]
- 18.Musardo S., Therin S., Pelucchi S., D’Andrea L., Stringhi R., Ribeiro A., Manca A., Balducci C., Pagano J., Sala C., et al. The development of ADAM10 endocytosis inhibitors for the treatment of Alzheimer’s disease. Mol. Ther. J. Am. Soc. Gene Ther. 2022;30:2474–2490. doi: 10.1016/j.ymthe.2022.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Egan M.F., Kost J., Tariot P.N., Aisen P.S., Cummings J.L., Vellas B., Sur C., Mukai Y., Voss T., Furtek C., et al. Randomized Trial of Verubecestat for Mild-to-Moderate Alzheimer’s Disease. N. Engl. J. Med. 2018;378:1691–1703. doi: 10.1056/NEJMoa1706441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wessels A.M., Tariot P.N., Zimmer J.A., Selzler K.J., Bragg S.M., Andersen S.W., Landry J., Krull J.H., Downing A.M., Willis B.A., et al. Efficacy and Safety of Lanabecestat for Treatment of Early and Mild Alzheimer Disease: The AMARANTH and DAYBREAK-ALZ Randomized Clinical Trials. JAMA Neurol. 2020;77:199–209. doi: 10.1001/jamaneurol.2019.3988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hur J.Y. Gamma-Secretase in Alzheimer’s disease. Exp. Mol. Med. 2022;54:433–446. doi: 10.1038/s12276-022-00754-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Endres K., Deller T. Regulation of Alpha-Secretase ADAM10 In vitro and In vivo: Genetic, Epigenetic, and Protein-Based Mechanisms. Front. Mol. Neurosci. 2017;10:56. doi: 10.3389/fnmol.2017.00056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Taylor H.A., Przemylska L., Clavane E.M., Meakin P.J. BACE1: More than just a beta-secretase. Obes. Rev. 2022;23:e13430. doi: 10.1111/obr.13430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Blanchard J.W., Bula M., Davila-Velderrain J., Akay L.A., Zhu L.N., Frank A., Victor M.B., Bonner J.M., Mathys H., Lin Y.T., et al. Reconstruction of the human blood-brain barrier in vitro reveals a pathogenic mechanism of APOE4 in pericytes. Nat. Med. 2020;26:952–963. doi: 10.1038/s41591-020-0886-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang Y.M., Cella M., Mallinson K., Ulrich J.D., Young K.L., Robinette M.L., Gilfillan S., Krishnan G.M., Sudhakar S., Zinselmeyer B.H., et al. TREM2 Lipid Sensing Sustains the Microglial Response in an Alzheimer’s Disease Model. Cell. 2015;160:1061–1071. doi: 10.1016/j.cell.2015.01.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Parikh I., Fardo D.W., Estus S. Genetics of PICALM expression and Alzheimer’s disease. PLoS ONE. 2014;9:e91242. doi: 10.1371/journal.pone.0091242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Narayan P., Sienski G., Bonner J.M., Lin Y.T., Seo J., Baru V., Haque A., Milo B., Akay L.A., Graziosi A., et al. PICALM Rescues Endocytic Defects Caused by the Alzheimer’s Disease Risk Factor APOE4. Cell Rep. 2020;33:108224. doi: 10.1016/j.celrep.2020.108224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Miyagawa T., Ebinuma I., Morohashi Y., Hori Y., Chang M.Y., Hattori H., Maehara T., Yokoshima S., Fukuyama T., Tsuji S., et al. BIN1 regulates BACE1 intracellular trafficking and amyloid-beta production. Hum. Mol. Genet. 2016;25:2948–2958. doi: 10.1093/hmg/ddw146. [DOI] [PubMed] [Google Scholar]
- 29.Schneider L. A resurrection of aducanumab for Alzheimer’s disease. Lancet Neurol. 2020;19:111–112. doi: 10.1016/S1474-4422(19)30480-6. [DOI] [PubMed] [Google Scholar]
- 30.Behl T., Kaur I., Sehgal A., Singh S., Sharma N., Makeen H.A., Albratty M., Alhazmi H.A., Felemban S.G., Alsubayiel A.M., et al. “Aducanumab” making a comeback in Alzheimer’s disease: An old wine in a new bottle. Biomed. Pharmacother. 2022;148:112746. doi: 10.1016/j.biopha.2022.112746. [DOI] [PubMed] [Google Scholar]
- 31.Maitra S., Vincent B. Cdk5-p25 as a key element linking amyloid and tau pathologies in Alzheimer’s disease: Mechanisms and possible therapeutic interventions. Life Sci. 2022;308:120986. doi: 10.1016/j.lfs.2022.120986. [DOI] [PubMed] [Google Scholar]
- 32.Atagi Y., Liu C.C., Painter M.M., Chen X.F., Verbeeck C., Zheng H.H., Li X., Rademakers R., Kang S.S., Xu H.X., et al. Apolipoprotein E Is a Ligand for Triggering Receptor Expressed on Myeloid Cells 2 (TREM2) J. Biol. Chem. 2015;290:26043–26050. doi: 10.1074/jbc.M115.679043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yeh F.L., Wang Y.Y., Tom I., Gonzalez L.C., Sheng M. TREM2 Binds to Apolipoproteins, Including APOE and CLU/APOJ, and Thereby Facilitates Uptake of Amyloid-Beta by Microglia. Neuron. 2016;91:328–340. doi: 10.1016/j.neuron.2016.06.015. [DOI] [PubMed] [Google Scholar]
- 34.Steen E., Terry B.M., Rivera E.J., Cannon J.L., Neely T.R., Tavares R., Xu X.J., Wands J.R., de la Monte S.M. Impaired insulin and insulin-like growth factor expression and signaling mechanisms in Alzheimer’s disease—Is this type 3 diabetes? J. Alzheimer’s Dis. 2005;7:63–80. doi: 10.3233/JAD-2005-7107. [DOI] [PubMed] [Google Scholar]
- 35.Marks J.L., Porte D., Jr., Stahl W.L., Baskin D.G. Localization of insulin receptor mRNA in rat brain by in situ hybridization. Endocrinology. 1990;127:3234–3236. doi: 10.1210/endo-127-6-3234. [DOI] [PubMed] [Google Scholar]
- 36.Adamo M., Raizada M.K., LeRoith D. Insulin and insulin-like growth factor receptors in the nervous system. Mol. Neurobiol. 1989;3:71–100. doi: 10.1007/BF02935589. [DOI] [PubMed] [Google Scholar]
- 37.Zhang W.D., Liu Q.Y., Haqqani A.S., Leclerc S., Liu Z.Y., Fauteux F., Baumann E., Delaney C.E., Ly D., Star A.T., et al. Differential expression of receptors mediating receptor-mediated transcytosis (RMT) in brain microvessels, brain parenchyma and peripheral tissues of the mouse and the human. Fluids Barriers CNS. 2020;17:47. doi: 10.1186/s12987-020-00209-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Leclerc M., Bourassa P., Tremblay C., Caron V., Sugere C., Emond V., Bennett D.A., Calon F. Cerebrovascular insulin receptors are defective in Alzheimer’s disease. Brain. 2022:awac309. doi: 10.1093/brain/awac309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gali C.C., Fanaee-Danesh E., Zandl-Lang M., Albrecher N.M., Tam-Amersdorfer C., Stracke A., Sachdev V., Reichmann F., Sun Y.D., Avdili A., et al. Amyloid-beta impairs insulin signaling by accelerating autophagy-lysosomal degradation of LRP-1 and IR-beta in blood-brain barrier endothelial cells in vitro and in 3XTg-AD mice. Mol. Cell. Neurosci. 2019;99:103390. doi: 10.1016/j.mcn.2019.103390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.De la Monte S.M., Tong M., Daiello L.A., Ott B.R. Early-Stage Alzheimer’s Disease Is Associated with Simultaneous Systemic and Central Nervous System Dysregulation of Insulin-Linked Metabolic Pathways. J. Alzheimer’s Dis. 2019;68:657–668. doi: 10.3233/JAD-180906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Confettura A.D., Cuboni E., Ammar M.R., Jia S., Gomes G.M., Yuanxiang P., Raman R., Li T.T., Grochowska K.M., Ahrends R., et al. Neddylation-dependent protein degradation is a nexus between synaptic insulin resistance, neuroinflammation and Alzheimer’s disease. Transl. Neurodegener. 2022;11:2. doi: 10.1186/s40035-021-00277-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ma Q.L., Yang F., Rosario E.R., Ubeda O.J., Beech W., Gant D.J., Chen P.P., Hudspeth B., Chen C., Zhao Y., et al. Beta-amyloid oligomers induce phosphorylation of tau and inactivation of insulin receptor substrate via c-Jun N-terminal kinase signaling: Suppression by omega-3 fatty acids and curcumin. J. Neurosci. 2009;29:9078–9089. doi: 10.1523/JNEUROSCI.1071-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Duarte A.I., Moreira P.I., Oliveira C.R. Insulin in central nervous system: More than just a peripheral hormone. J. Aging Res. 2012;2012:384017. doi: 10.1155/2012/384017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Banks W.A. The source of cerebral insulin. Eur. J. Pharmacol. 2004;490:5–12. doi: 10.1016/j.ejphar.2004.02.040. [DOI] [PubMed] [Google Scholar]
- 45.Banks W.A., Owen J.B., Erickson M.A. Insulin in the brain: There and back again. Pharmacol. Ther. 2012;136:82–93. doi: 10.1016/j.pharmthera.2012.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Grillo C.A., Piroli G.G., Hendry R.M., Reagan L.P. Insulin-stimulated translocation of GLUT4 to the plasma membrane in rat hippocampus is PI3-kinase dependent. Brain Res. 2009;1296:35–45. doi: 10.1016/j.brainres.2009.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pearson-Leary J., Mcnay E.C. Novel Roles for the Insulin-Regulated Glucose Transporter-4 in Hippocampally Dependent Memory. J. Neurosci. 2016;36:11851–11864. doi: 10.1523/JNEUROSCI.1700-16.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Radhakrishnan Y., Maile L.A., Ling Y., Graves L.M., Clemmons D.R. Insulin-like growth factor-I stimulates Shc-dependent phosphatidylinositol 3-kinase activation via Grb2-associated p85 in vascular smooth muscle cells. J. Biol. Chem. 2008;283:16320–16331. doi: 10.1074/jbc.M801687200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Belaidi A.A., Masaldan S., Southon A., Kalinowski P., Acevedo K., Appukuttan A.T., Portbury S., Lei P., Agarwal P., Leurgans S.E., et al. Apolipoprotein E potently inhibits ferroptosis by blocking ferritinophagy. Mol. Psychiatry. 2022:1–10. doi: 10.1038/s41380-022-01568-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Shen L., Wang D.Q.H., Tso P., Jandacek R.J., Woods S.C., Liu M. Apolipoprotein E reduces food intake via PI3K/Akt signaling pathway in the hypothalamus. Physiol. Behav. 2011;105:124–128. doi: 10.1016/j.physbeh.2011.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ong Q.R., Chan E.S., Lim M.L., Wong B.S. Expression of human apolipoprotein E4 reduces insulin-receptor substrate 1 expression and Akt phosphorylation in the ageing liver. FEBS Open Bio. 2014;4:260–265. doi: 10.1016/j.fob.2014.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zhao N., Liu C.C., Van Ingelgom A.J., Martens Y.A., Linares C., Knight J.A., Painter M.M., Sullivan P.M., Bu G.J. Apolipoprotein E4 Impairs Neuronal Insulin Signaling by Trapping Insulin Receptor in the Endosomes. Neuron. 2017;96:115–129.e5. doi: 10.1016/j.neuron.2017.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Han X., Cheng X.L., Xu J.Y., Liu Y.J., Zhou J.W., Jiang L.H., Gu X.P., Xia T.J. Activation of TREM2 attenuates neuroinflammation via PI3K/Akt signaling pathway to improve postoperative cognitive dysfunction in mice. Neuropharmacology. 2022;219:109231. doi: 10.1016/j.neuropharm.2022.109231. [DOI] [PubMed] [Google Scholar]
- 54.Fu C., Xu Q.C., Liu J.C., Tang S.X., Liu C., Cao Y.H. Triggering receptor expressed on myeloid cells-2 promotes survival of cardiomyocytes after myocardial ischemic injury through PI3K/AKT pathway. Cardiovasc. Diagn. Ther. 2022;12:24. doi: 10.21037/cdt-21-490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wang S., Sudan R., Peng V., Zhou Y., Du S., Yuede C.M., Lei T., Hou J., Cai Z., Cella M., et al. TREM2 drives microglia response to amyloid-beta via SYK-dependent and -independent pathways. Cell. 2022;185:4153–4169.e19. doi: 10.1016/j.cell.2022.09.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Jiang T., Zhang Y.D., Gao Q., Ou Z., Gong P.Y., Shi J.Q., Wu L., Zhou J.S. TREM2 Ameliorates Neuronal Tau Pathology through Suppression of Microglial Inflammatory Response. Inflammation. 2018;41:811–823. doi: 10.1007/s10753-018-0735-5. [DOI] [PubMed] [Google Scholar]
- 57.Frolich L., Blum-Degen D., Bernstein H.G., Engelsberger S., Humrich J., Laufer S., Muschner D., Thalheimer A., Turk A., Hoyer S., et al. Brain insulin and insulin receptors in aging and sporadic Alzheimer’s disease. J. Neural Transm. 1998;105:423–438. doi: 10.1007/s007020050068. [DOI] [PubMed] [Google Scholar]
- 58.Morelli L., Llovera R.E., Mathov I., Lue L.F., Frangione B., Ghiso J., Castano E.M. Insulin-degrading enzyme in brain microvessels: Proteolysis of amyloid β vasculotropic variants and reduced activity in cerebral amyloid angiopathy. J. Biol. Chem. 2004;279:56004–56013. doi: 10.1074/jbc.M407283200. [DOI] [PubMed] [Google Scholar]
- 59.Farris W., Mansourian S., Chang Y., Lindsley L., Eckman E.A., Frosch M.P., Eckman C.B., Tanzi R.E., Selkoe D.J., Guenette S. Insulin-degrading enzyme regulates the levels of insulin, amyloid beta-protein, and the beta-amyloid precursor protein intracellular domain in vivo. Proc. Natl. Acad. Sci. USA. 2003;100:4162–4167. doi: 10.1073/pnas.0230450100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Cook D.G., Leverenz J.B., McMillan P.J., Kulstad J.J., Ericksen S., Roth R.A., Schellenberg G.D., Jin L.W., Kovacina K.S., Craft S. Reduced hippocampal insulin-degrading enzyme in late-onset Alzheimer’s disease is associated with the apolipoprotein E-epsilon 4 allele. Am. J. Pathol. 2003;162:313–319. doi: 10.1016/S0002-9440(10)63822-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Schechter R., Beju D., Miller K.E. The effect of insulin deficiency on tau and neurofilament in the insulin knockout mouse. Biochem. Biophys. Res. Commun. 2005;334:979–986. doi: 10.1016/j.bbrc.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 62.Clodfelder-Miller B.J., Zmijewska A.A., Johnson G.V.W., Jope R.S. Tau is hyperphosphorylated at multiple sites in mouse brain in vivo after streptozotocin-induced insulin deficiency. Diabetes. 2006;55:3320–3325. doi: 10.2337/db06-0485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Schubert M., Brazil D.P., Burks D.J., Kushner J.A., Ye J., Flint C.L., Farhang-Fallah J., Dikkes P., Warot X.M., Rio C., et al. Insulin receptor substrate-2 deficiency impairs brain growth and promotes tau phosphorylation. J. Neurosci. 2003;23:7084–7092. doi: 10.1523/JNEUROSCI.23-18-07084.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Adzovic L., Lynn A.E., D’Angelo H.M., Crockett A.M., Kaercher R.M., Royer S.E., Hopp S.C., Wenk G.L. Insulin improves memory and reduces chronic neuroinflammation in the hippocampus of young but not aged brains. J. Neuroinflamm. 2015;12:63. doi: 10.1186/s12974-015-0282-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Reger M.A., Watson G.S., Frey W.H., II, Baker L.D., Cholerton B., Keeling M.L., Belongia D.A., Fishel M.A., Plymate S.R., Schellenberg G.D., et al. Effects of intranasal insulin on cognition in memory-impaired older adults: Modulation by APOE genotype. Neurobiol. Aging. 2006;27:451–458. doi: 10.1016/j.neurobiolaging.2005.03.016. [DOI] [PubMed] [Google Scholar]
- 66.Reger M.A., Watson G.S., Green P.S., Wilkinson C.W., Baker L.D., Cholerton B., Fishel M.A., Plymate S.R., Breitner J.C., DeGroodt W., et al. Intranasal insulin improves cognition and modulates beta-amyloid in early AD. Neurology. 2008;70:440–448. doi: 10.1212/01.WNL.0000265401.62434.36. [DOI] [PubMed] [Google Scholar]
- 67.Claxton A., Baker L.D., Hanson A., Trittschuh E.H., Cholerton B., Morgan A., Callaghan M., Arbuckle M., Behl C., Craft S. Long Acting Intranasal Insulin Detemir Improves Cognition for Adults with Mild Cognitive Impairment or Early-Stage Alzheimer’s Disease Dementia. J. Alzheimer’s Dis. 2015;45:1269–1270. doi: 10.3233/JAD-141791. [DOI] [PubMed] [Google Scholar]
- 68.Craft S., Claxton A., Baker L.D., Hanson A.J., Cholerton B., Trittschuh E.H., Dahl D., Caulder E., Neth B., Montine T.J., et al. Effects of Regular and Long-Acting Insulin on Cognition and Alzheimer’s Disease Biomarkers: A Pilot Clinical Trial. J. Alzheimer’s Dis. 2017;57:1325–1334. doi: 10.3233/JAD-161256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Born J., Lange T., Kern W., McGregor G.P., Bickel U., Fehm H.L. Sniffing neuropeptides: A transnasal approach to the human brain. Nat. Neurosci. 2002;5:514–516. doi: 10.1038/nn0602-849. [DOI] [PubMed] [Google Scholar]
- 70.Craft S., Raman R., Chow T.W., Rafii M.S., Sun C.K., Rissman R.A., Donohue M.C., Brewer J.B., Jenkins C., Harless K., et al. Safety, Efficacy, and Feasibility of Intranasal Insulin for the Treatment of Mild Cognitive Impairment and Alzheimer Disease Dementia: A Randomized Clinical Trial. JAMA Neurol. 2020;77:1099–1109. doi: 10.1001/jamaneurol.2020.1840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Sato T., Hanyu H., Hirao K., Kanetaka H., Sakurai H., Iwamoto T. Efficacy of PPAR-gamma agonist pioglitazone in mild Alzheimer disease. Neurobiol. Aging. 2011;32:1626–1633. doi: 10.1016/j.neurobiolaging.2009.10.009. [DOI] [PubMed] [Google Scholar]
- 72.Watson G.S., Cholerton B.A., Reger M.A., Baker L.D., Plymate S.R., Asthana S., Fishel M.A., Kulstad J.J., Green P.S., Cook D.G., et al. Preserved cognition in patients with early Alzheimer disease and amnestic mild cognitive impairment during treatment with rosiglitazone: A preliminary study. Am. J. Geriatr. Psychiatry. 2005;13:950–958. doi: 10.1176/appi.ajgp.13.11.950. [DOI] [PubMed] [Google Scholar]
- 73.Liu J., Wang L.N., Jia J.P. Peroxisome Proliferator-Activated Receptor-Gamma Agonists for Alzheimer’s Disease and Amnestic Mild Cognitive Impairment: A Systematic Review and Meta-Analysis. Drugs Aging. 2015;32:57–65. doi: 10.1007/s40266-014-0228-7. [DOI] [PubMed] [Google Scholar]
- 74.Risner M.E., Saunders A.M., Altman J.F.B., Ormandy G.C., Craft S., Foley I.M., Zvartau-Hind M.E., Hosford D.A., Roses A.D. Efficacy of rosiglitazone in a genetically defined population with mild-to-moderate Alzheimer’s disease. Pharm. J. 2006;6:246–254. doi: 10.1038/sj.tpj.6500369. [DOI] [PubMed] [Google Scholar]
- 75.Harrington C., Sawchak S., Chiang C., Davies J., Donovan C., Saunders A.M., Irizarry M., Jeter B., Zvartau-Hind M., van Dyck C.H., et al. Rosiglitazone Does Not Improve Cognition or Global Function when Used as Adjunctive Therapy to AChE Inhibitors in Mild-to-Moderate Alzheimer’s Disease: Two Phase 3 Studies. Curr. Alzheimer Res. 2011;8:592–606. doi: 10.2174/156720511796391935. [DOI] [PubMed] [Google Scholar]
- 76.Lu X.Y., Huang S., Chen Q.B., Zhang D.P., Li W.Y., Ao R., Leung F.C.Y., Zhang Z.M., Huang J.S., Tang Y., et al. Metformin Ameliorates A beta Pathology by Insulin-Degrading Enzyme in a Transgenic Mouse Model of Alzheimer’s Disease. Oxidative Med. Cell. Longev. 2020;2020:1–10. doi: 10.1155/2020/2315106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ou Z.R., Kong X.J., Sun X.D., He X.S., Zhang L., Gong Z., Huang J.Y., Xu B.A., Long D.H., Li J.H., et al. Metformin treatment prevents amyloid plaque deposition and memory impairment in APP/PS1 mice. Brain Behav. Immun. 2018;69:351–363. doi: 10.1016/j.bbi.2017.12.009. [DOI] [PubMed] [Google Scholar]
- 78.Kickstein E., Krauss S., Thornhill P., Rutschow D., Zeller R., Sharkey J., Williamson R., Fuchs M., Kohler A., Glossmann H., et al. Biguanide metformin acts on tau phosphorylation via mTOR/protein phosphatase 2A (PP2A) signaling. Proc. Natl. Acad. Sci. USA. 2010;107:21830–21835. doi: 10.1073/pnas.0912793107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Nabizadeh F., Kankam S.B., Balabandian M., Hashemi S.M., Sharifkazemi H., Rostami M.R., Alzheimer’s Disease Neuroimaging Initiative (ADNI) Metformin use and brain atrophy in nondemented elderly individuals with diabetes. Exp. Gerontol. 2022;166:111890. doi: 10.1016/j.exger.2022.111890. [DOI] [PubMed] [Google Scholar]
- 80.Koenig A.M., Mechanic-Hamilton D., Xie S.X., Combs M.F., Cappola A.R., Xie L., Detre J.A., Wolk D.A., Arnold S.E. Effects of the Insulin Sensitizer Metformin in Alzheimer Disease: Pilot Data from a Randomized Placebo-controlled Crossover Study. Alzheimer Dis. Assoc. Disord. 2017;31:107–113. doi: 10.1097/WAD.0000000000000202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.He Z.J., Wang M.H., Zhao Q.H., Li X.Q., Liu P.G., Ren B.Y., Wu C., Du X.B., Li N., Liu Q. Bis(ethylmaltolato)oxidovanadium (IV) mitigates neuronal apoptosis resulted from amyloid-beta induced endoplasmic reticulum stress through activating peroxisome proliferator-activated receptor gamma. J. Inorg. Biochem. 2020;208:111073. doi: 10.1016/j.jinorgbio.2020.111073. [DOI] [PubMed] [Google Scholar]
- 82.He Z.J., Song J.X., Li X.X., Li X.Q., Zhu H.Z., Wu C., Xiao W., Du X.B., Ni J.Z., Li N., et al. Bis(ethylmaltolato)oxidovanadium (IV) alleviates neuronal apoptosis through regulating peroxisome proliferator-activated receptor gamma in a triple transgenic animal model of Alzheimer’s disease. J. Biol. Inorg. Chem. 2021;26:551–568. doi: 10.1007/s00775-021-01874-8. [DOI] [PubMed] [Google Scholar]
- 83.He Z.J., Han S.X., Wu C., Liu L.N., Zhu H.Z., Liu A., Lu Q.Y., Huang J.Q., Du X.B., Li N., et al. Bis(ethylmaltolato)oxidovanadium(iv) inhibited the pathogenesis of Alzheimer’s disease in triple transgenic model mice. Metallomics. 2020;12:631. doi: 10.1039/d0mt90008g. [DOI] [PubMed] [Google Scholar]
- 84.He Z.H., Guo J.L., McBride J.D., Narasimhan S., Kim H., Changolkar L., Zhang B., Gathagan R.J., Yue C.Y., Dengler C., et al. Amyloid-beta plaques enhance Alzheimer’s brain tau-seeded pathologies by facilitating neuritic plaque tau aggregation. Nat. Med. 2018;24:29–38. doi: 10.1038/nm.4443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Pallo S.P., Johnson G.V.W. Tau facilitates A beta-induced loss of mitochondrial membrane potential independent of cytosolic calcium fluxes in mouse cortical neurons. Neurosci. Lett. 2015;597:32–37. doi: 10.1016/j.neulet.2015.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Roberson E.D., Scearce-Levie K., Palop J.J., Yan F.R., Cheng I.H., Wu T., Gerstein H., Yu G.Q., Mucke L. Reducing endogenous tau ameliorates amyloid beta-induced deficits in an Alzheimer’s disease mouse model. Science. 2007;316:750–754. doi: 10.1126/science.1141736. [DOI] [PubMed] [Google Scholar]
- 87.Vossel K.A., Zhang K., Brodbeck J., Daub A.C., Sharma P., Finkbeiner S., Cui B., Mucke L. Tau reduction prevents Abeta-induced defects in axonal transport. Science. 2010;330:198. doi: 10.1126/science.1194653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Rapoport M., Dawson H.N., Binder L.I., Vitek M.P., Ferreira A. Tau is essential to beta-amyloid-induced neurotoxicity. Proc. Natl. Acad. Sci. USA. 2002;99:6364–6369. doi: 10.1073/pnas.092136199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Wijesekara N., Goncalves R.A., Ahrens R., De Felice F.G., Fraser P.E. Tau ablation in mice leads to pancreatic beta cell dysfunction and glucose intolerance. FASEB J. 2018;32:3166–3173. doi: 10.1096/fj.201701352. [DOI] [PubMed] [Google Scholar]
- 90.Marciniak E., Leboucher A., Caron E., Ahmed T., Tailleux A., Dumont J., Issad T., Gerhardt E., Pagesy P., Vileno M., et al. Tau deletion promotes brain insulin resistance. J. Exp. Med. 2017;214:2257–2269. doi: 10.1084/jem.20161731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Lei P., Ayton S., Finkelstein D.I., Spoerri L., Ciccotosto G.D., Wright D.K., Wong B.X., Adlard P.A., Cherny R.A., Lam L.Q., et al. Tau deficiency induces parkinsonism with dementia by impairing APP-mediated iron export. Nat. Med. 2012;18:291–295. doi: 10.1038/nm.2613. [DOI] [PubMed] [Google Scholar]
- 92.Abbondante S., Baglietto-Vargas D., Rodriguez-Ortiz C.J., Estrada-Hernandez T., Medeiros R., LaFerla F.M. Genetic Ablation of Tau Mitigates Cognitive Impairment Induced by Type 1 Diabetes. Am. J. Pathol. 2014;184:819–826. doi: 10.1016/j.ajpath.2013.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Trujillo-Estrada L., Nguyen C., da Cunha C., Cai L.N., Forner S., Martini A.C., Ager R.R., Prieto G.A., Cotman C.W., Baglietto-Vargas D., et al. Tau underlies synaptic and cognitive deficits for type 1, but not type 2 diabetes mouse models. Aging Cell. 2019;18:e12919. doi: 10.1111/acel.12919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Spires-Jones T.L., Stoothoff W.H., de Calignon A., Jones P.B., Hyman B.T. Tau pathophysiology in neurodegeneration: A tangled issue. Trends Neurosci. 2009;32:150–159. doi: 10.1016/j.tins.2008.11.007. [DOI] [PubMed] [Google Scholar]
- 95.Hull C., Dekeryte R., Koss D.J., Crouch B., Buchanan H., Delibegovic M., Platt B. Knock-in of Mutated hTAU Causes Insulin Resistance, Inflammation and Proteostasis Disturbance in a Mouse Model of Frontotemporal Dementia. Mol. Neurobiol. 2020;57:539–550. doi: 10.1007/s12035-019-01722-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Leboucher A., Ahmed T., Caron E., Tailleux A., Raison S., Joly-Amado A., Marciniak E., Carvalho K., Hamdane M., Bantubungi K., et al. Brain insulin response and peripheral metabolic changes in a Tau transgenic mouse model. Neurobiol. Dis. 2019;125:14–22. doi: 10.1016/j.nbd.2019.01.008. [DOI] [PubMed] [Google Scholar]
- 97.El Idrissi A., Alonso A.D.C. Pathological Human Tau Induces Alterations in the Brain Insulin Signaling Cascade. Front. Neurosci. 2022;16:805046. doi: 10.3389/fnins.2022.805046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Rodriguez-Rodriguez P., Sandebring-Matton A., Merino-Serrais P., Parrado-Fernandez C., Rabano A., Winblad B., Avila J., Ferrer I., Cedazo-Minguez A. Tau hyperphosphorylation induces oligomeric insulin accumulation and insulin resistance in neurons. Brain. 2017;140:3269–3285. doi: 10.1093/brain/awx256. [DOI] [PubMed] [Google Scholar]
- 99.Wang Y., Balaji V., Kaniyappan S., Kruger L., Irsen S., Tepper K., Chandupatla R., Maetzler W., Schneider A., Mandelkow E., et al. The release and trans-synaptic transmission of Tau via exosomes. Mol. Neurodegener. 2017;12:5. doi: 10.1186/s13024-016-0143-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Sanders D.W., Kaufman S.K., DeVos S.L., Sharma A.M., Mirbaha H., Li A.M., Barker S.J., Foley A.C., Thorpe J.R., Serpell L.C., et al. Distinct Tau Prion Strains Propagate in Cells and Mice and Define Different Tauopathies. Neuron. 2014;82:1271–1288. doi: 10.1016/j.neuron.2014.04.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Wegmann S., Maury E.A., Kirk M.J., Saqran L., Roe A., DeVos S.L., Nicholls S., Fan Z., Takeda S., Cagsal-Getkin O., et al. Removing endogenous tau does not prevent tau propagation yet reduces its neurotoxicity. EMBO J. 2015;34:3028–3041. doi: 10.15252/embj.201592748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Prokopovich D.V., Whittaker J.W., Muthee M.M., Ahmed A., Larini L. Impact of Phosphorylation and Pseudophosphorylation on the Early Stages of Aggregation of the Microtubule-Associated Protein Tau. J. Phys. Chem. B. 2017;121:2095–2103. doi: 10.1021/acs.jpcb.7b00194. [DOI] [PubMed] [Google Scholar]
- 103.Chang E., Kim S., Schafer K.N., Kuret J. Pseudophosphorylation of tau protein directly modulates its aggregation kinetics. BBA Proteins Proteom. 2011;1814:388–395. doi: 10.1016/j.bbapap.2010.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Briner A., Gotz J., Polanco J.C. Fyn Kinase Controls Tau Aggregation In Vivo. Cell Rep. 2020;32:108045. doi: 10.1016/j.celrep.2020.108045. [DOI] [PubMed] [Google Scholar]
- 105.Haj-Yahya M., Gopinath P., Rajasekhar K., Mirbaha H., Diamond M.I., Lashuel H.A. Site-Specific Hyperphosphorylation Inhibits, Rather than Promotes, Tau Fibrillization, Seeding Capacity, and Its Microtubule Binding. Angew. Chem. Int. Ed. 2020;59:4059–4067. doi: 10.1002/anie.201913001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Ait-Bouziad N., Chiki A., Limorenko G., Xiao S.F., Eliezer D., Lashuel H.A. Phosphorylation of the overlooked tyrosine 310 regulates the structure, aggregation, and microtubule- and lipid-binding properties of Tau. J. Biol. Chem. 2020;295:7905–7922. doi: 10.1074/jbc.RA119.012517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Liu K.F., Liu Y.T., Li L.Y., Qin P.B., Iqbal J., Deng Y.L., Qing H. Glycation alter the process of Tau phosphorylation to change Tau isoforms aggregation property. BBA Mol. Basis Dis. 2016;1862:192–201. doi: 10.1016/j.bbadis.2015.12.002. [DOI] [PubMed] [Google Scholar]
- 108.SantaCruz K., Lewis J., Spires T., Paulson J., Kotilinek L., Ingelsson M., Guimaraes A., DeTure M., Ramsden M., McGowan E., et al. Tau suppression in a neurodegenerative mouse model improves memory function. Science. 2005;309:476–481. doi: 10.1126/science.1113694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.David D.C., Hauptmann S., Scherping I., Schuessel K., Keil U., Rizzu P., Ravid R., Drose S., Brandt U., Muller W.E., et al. Proteomic and functional analyses reveal a mitochondrial dysfunction in P301L Tau transgenic mice. J. Biol. Chem. 2005;280:23802–23814. doi: 10.1074/jbc.M500356200. [DOI] [PubMed] [Google Scholar]
- 110.Esteras N., Rohrer J.D., Hardy J., Wray S., Abramov A.Y. Mitochondrial hyperpolarization in iPSC-derived neurons from patients of FTDP-17 with 10+16 MAPT mutation leads to oxidative stress and neurodegeneration. Redox Biol. 2017;12:410–422. doi: 10.1016/j.redox.2017.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Manczak M., Reddy P.H. Abnormal interaction between the mitochondrial fission protein Drp1 and hyperphosphorylated tau in Alzheimer’s disease neurons: Implications for mitochondrial dysfunction and neuronal damage. Hum. Mol. Genet. 2012;21:2538–2547. doi: 10.1093/hmg/dds072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.De Calignon A., Fox L.M., Pitstick R., Carlson G.A., Bacskai B.J., Spires-Jones T.L., Hyman B.T. Caspase activation precedes and leads to tangles. Nature. 2010;464:1201–1204. doi: 10.1038/nature08890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Quintanilla R.A., Matthews-Roberson T.A., Dolan P.J., Johnson G.V.W. Caspase-cleaved Tau Expression Induces Mitochondrial Dysfunction in Immortalized Cortical Neurons IMPLICATIONS FOR THE PATHOGENESIS OF ALZHEIMER DISEASE. J. Biol. Chem. 2009;284:18754–18766. doi: 10.1074/jbc.M808908200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Perez M.J., Vergara-Pulgar K., Jara C., Cabezas-Opazo F., Quintanilla R.A. Caspase-Cleaved Tau Impairs Mitochondrial Dynamics in Alzheimer’s Disease. Mol. Neurobiol. 2018;55:1004–1018. doi: 10.1007/s12035-017-0385-x. [DOI] [PubMed] [Google Scholar]
- 115.Sengupta A., Novak M., Grundke-Iqbal I., Iqbal K. Regulation of phosphorylation of tau by cyclin-dependent kinase 5 and glycogen synthase kinase-3 at substrate level. FEBS Lett. 2006;580:5925–5933. doi: 10.1016/j.febslet.2006.09.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Vingtdeux V., Davies P., Dickson D.W., Marambaud P. AMPK is abnormally activated in tangle- and pre-tangle-bearing neurons in Alzheimer’s disease and other tauopathies. Acta Neuropathol. 2011;121:337–349. doi: 10.1007/s00401-010-0759-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Hanger D.P., Anderton B.H., Noble W. Tau phosphorylation: The therapeutic challenge for neurodegenerative disease. Trends Mol. Med. 2009;15:112–119. doi: 10.1016/j.molmed.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 118.Caccamo A., Oddo S., Tran L.X., LaFerla F.M. Lithium reduces tau phosphorylation but not A beta or working memory deficits in a transgenic model with both plaques and tangles. Am. J. Pathol. 2007;170:1669–1675. doi: 10.2353/ajpath.2007.061178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Sereno L., Coma M., Rodriguez M., Sanchez-Ferrer P., Sanchez M.B., Gich I., Agullo J.M., Perez M., Avila J., Guardia-Laguarta C., et al. A novel GSK-3beta inhibitor reduces Alzheimer’s pathology and rescues neuronal loss in vivo. Neurobiol. Dis. 2009;35:359–367. doi: 10.1016/j.nbd.2009.05.025. [DOI] [PubMed] [Google Scholar]
- 120.Hu S., Begum A.N., Jones M.R., Oh M.S., Beech W.K., Beech B.H., Yang F., Chen P., Ubeda O.J., Kim P.C., et al. GSK3 inhibitors show benefits in an Alzheimer’s disease (AD) model of neurodegeneration but adverse effects in control animals. Neurobiol. Dis. 2009;33:193–206. doi: 10.1016/j.nbd.2008.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Saraswati A.P., Ali Hussaini S.M., Krishna N.H., Babu B.N., Kamal A. Glycogen synthase kinase-3 and its inhibitors: Potential target for various therapeutic conditions. Eur. J. Med. Chem. 2018;144:843–858. doi: 10.1016/j.ejmech.2017.11.103. [DOI] [PubMed] [Google Scholar]
- 122.Sontag E., Luangpirom A., Hladik C., Mudrak I., Ogris E., Speciale S., White C.L., III Altered expression levels of the protein phosphatase 2A ABalphaC enzyme are associated with Alzheimer disease pathology. J. Neuropathol. Exp. Neurol. 2004;63:287–301. doi: 10.1093/jnen/63.4.287. [DOI] [PubMed] [Google Scholar]
- 123.Kins S., Crameri A., Evans D.R.H., Hemmings B.A., Nitsch R.M., Gotz J. Reduced protein phosphatase 2A activity induces hyperphosphorylation and altered compartmentalization of tau in transgenic mice. J. Biol. Chem. 2001;276:38193–38200. doi: 10.1074/jbc.M102621200. [DOI] [PubMed] [Google Scholar]
- 124.Pei J.J., Gong C.X., An W.L., Winblad B., Cowburn R.F., Grundke-Iqbal I., Iqbal K. Okadaic-acid-induced inhibition of protein phosphatase 2A produces activation of mitogen-activated protein kinases ERK1/2, MEK-1/2, and p70 S6, similar to that in Alzheimer’s disease. Am. J. Pathol. 2003;163:845–858. doi: 10.1016/S0002-9440(10)63445-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.St-Cyr Giguere F., Attiori Essis S., Chagniel L., Germain M., Cyr M., Massicotte G. The sphingosine-1-phosphate receptor 1 agonist SEW2871 reduces Tau-Ser262 phosphorylation in rat hippocampal slices. Brain Res. 2017;1658:51–59. doi: 10.1016/j.brainres.2017.01.014. [DOI] [PubMed] [Google Scholar]
- 126.Xiong Y., Jing X.P., Zhou X.W., Wang X.L., Yang Y., Sun X.Y., Qiu M., Cao F.Y., Lu Y.M., Liu R., et al. Zinc induces protein phosphatase 2A inactivation and tau hyperphosphorylation through Src dependent PP2A (tyrosine 307) phosphorylation. Neurobiol. Aging. 2013;34:745–756. doi: 10.1016/j.neurobiolaging.2012.07.003. [DOI] [PubMed] [Google Scholar]
- 127.Ginhoux F., Lim S., Hoeffel G., Low D., Huber T. Origin and differentiation of microglia. Front. Cell. Neurosci. 2013;7:45. doi: 10.3389/fncel.2013.00045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Huang Y., Xu Z., Xiong S., Sun F., Qin G., Hu G., Wang J., Zhao L., Liang Y.X., Wu T., et al. Repopulated microglia are solely derived from the proliferation of residual microglia after acute depletion. Nat. Neurosci. 2018;21:530–540. doi: 10.1038/s41593-018-0090-8. [DOI] [PubMed] [Google Scholar]
- 129.Paolicelli R.C., Bolasco G., Pagani F., Maggi L., Scianni M., Panzanelli P., Giustetto M., Ferreira T.A., Guiducci E., Dumas L., et al. Synaptic pruning by microglia is necessary for normal brain development. Science. 2011;333:1456–1458. doi: 10.1126/science.1202529. [DOI] [PubMed] [Google Scholar]
- 130.Condello C., Yuan P., Schain A., Grutzendler J. Microglia constitute a barrier that prevents neurotoxic protofibrillar A beta 42 hotspots around plaques. Nat. Commun. 2015;6:6176. doi: 10.1038/ncomms7176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Yuan P., Condello C., Keene C.D., Wang Y.M., Bird T.D., Paul S.M., Luo W.J., Colonna M., Baddeley D., Grutzendler J. TREM2 Haplodeficiency in Mice and Humans Impairs the Microglia Barrier Function Leading to Decreased Amyloid Compaction and Severe Axonal Dystrophy. Neuron. 2016;92:252–264. doi: 10.1016/j.neuron.2016.09.016. [DOI] [PubMed] [Google Scholar]
- 132.Heneka M.T., Golenbock D.T., Latz E. Innate immunity in Alzheimer’s disease. Nat. Immunol. 2015;16:229–236. doi: 10.1038/ni.3102. [DOI] [PubMed] [Google Scholar]
- 133.Heneka M.T., Kummer M.P., Stutz A., Delekate A., Schwartz S., Vieira-Saecker A., Griep A., Axt D., Remus A., Tzeng T.C., et al. NLRP3 is activated in Alzheimer’s disease and contributes to pathology in APP/PS1 mice. Nature. 2013;493:674–678. doi: 10.1038/nature11729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Keren-Shaul H., Spinrad A., Weiner A., Matcovitch-Natan O., Dvir-Szternfeld R., Ulland T.K., David E., Baruch K., Lara-Astaiso D., Toth B., et al. A Unique Microglia Type Associated with Restricting Development of Alzheimer’s Disease. Cell. 2017;169:1276–1290.e17. doi: 10.1016/j.cell.2017.05.018. [DOI] [PubMed] [Google Scholar]
- 135.Chen Y., Colonna M. Microglia in Alzheimer’s disease at single-cell level. Are there common in humans and mice? J. Exp. Med. 2021;218:e20202717. doi: 10.1084/jem.20202717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Bhaskar K., Konerth M., Kokiko-Cochran O.N., Cardona A., Ransohoff R.M., Lamb B.T. Regulation of Tau Pathology by the Microglial Fractalkine Receptor. Neuron. 2010;68:19–31. doi: 10.1016/j.neuron.2010.08.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Kitazawa M., Oddo S., Yamasaki T.R., Green K.N., LaFerla F.M. Lipopolysaccharide-induced inflammation exacerbates tau pathology by a cyclin-dependent kinase 5-mediated pathway in a transgenic model of Alzheimer’s disease. J. Neurosci. 2005;25:8843–8853. doi: 10.1523/JNEUROSCI.2868-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Shi Y., Yamada K., Liddelow S.A., Smith S.T., Zhao L.Z., Luo W.J., Tsai R.M., Spina S., Grinberg L.T., Rojas J.C., et al. ApoE4 markedly exacerbates tau-mediated neurodegeneration in a mouse model of tauopathy. Nature. 2017;549:523–527. doi: 10.1038/nature24016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Gratuze M., Chen Y., Parhizkar S., Jain N., Strickland M.R., Serrano J.R., Colonna M., Ulrich J.D., Holtzman D.M. Activated microglia mitigate Abeta-associated tau seeding and spreading. J. Exp. Med. 2021;218:e20210542. doi: 10.1084/jem.20210542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Leyns C.E.G., Gratuze M., Narasimhan S., Jain N., Koscal L.J., Jiang H., Manis M., Colonna M., Lee V.M.Y., Ulrich J.D., et al. TREM2 function impedes tau seeding in neuritic plaques. Nat. Neurosci. 2019;22:1217–1222. doi: 10.1038/s41593-019-0433-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Lee S.H., Meilandt W.J., Xie L., Gandham V.D., Ngu H., Barck K.H., Rezzonico M.G., Imperio J., Lalehzadeh G., Huntley M.A., et al. Trem2 restrains the enhancement of tau accumulation and neurodegeneration by beta-amyloid pathology. Neuron. 2021;109:1283–1301.e6. doi: 10.1016/j.neuron.2021.02.010. [DOI] [PubMed] [Google Scholar]
- 142.Ulland T.K., Colonna M. TREM2—A key player in microglial biology and Alzheimer disease. Nat. Rev. Neurol. 2018;14:667–675. doi: 10.1038/s41582-018-0072-1. [DOI] [PubMed] [Google Scholar]
- 143.Zhang C.H., Chen S.W. Role of TREM2 in the Development of Neurodegenerative Diseases after Traumatic Brain Injury. Mol. Neurobiol. 2022:1–13. doi: 10.1007/s12035-022-03094-w. [DOI] [PubMed] [Google Scholar]
- 144.Elmore M.R., Najafi A.R., Koike M.A., Dagher N.N., Spangenberg E.E., Rice R.A., Kitazawa M., Matusow B., Nguyen H., West B.L., et al. Colony-stimulating factor 1 receptor signaling is necessary for microglia viability, unmasking a microglia progenitor cell in the adult brain. Neuron. 2014;82:380–397. doi: 10.1016/j.neuron.2014.02.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Patel S., Player M.R. Colony-stimulating factor-1 receptor inhibitors for the treatment of cancer and inflammatory disease. Curr. Top. Med. Chem. 2009;9:599–610. doi: 10.2174/156802609789007327. [DOI] [PubMed] [Google Scholar]
- 146.Dai X.M., Ryan G.R., Hapel A.J., Dominguez M.G., Russell R.G., Kapp S., Sylvestre V., Stanley E.R. Targeted disruption of the mouse colony-stimulating factor 1 receptor gene results in osteopetrosis, mononuclear phagocyte deficiency, increased primitive progenitor cell frequencies, and reproductive defects. Blood. 2002;99:111–120. doi: 10.1182/blood.V99.1.111. [DOI] [PubMed] [Google Scholar]
- 147.Erblich B., Zhu L., Etgen A.M., Dobrenis K., Pollard J.W. Absence of colony stimulation factor-1 receptor results in loss of microglia, disrupted brain development and olfactory deficits. PLoS ONE. 2011;6:e26317. doi: 10.1371/journal.pone.0026317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Conway J.G., McDonald B., Parham J., Keith B., Rusnak D.W., Shaw E., Jansen M., Lin P., Payne A., Crosby R.M., et al. Inhibition of colony-stimulating-factor-1 signaling in vivo with the orally bioavailable cFMS kinase inhibitor GW2580. Proc. Natl. Acad. Sci. USA. 2005;102:16078–16083. doi: 10.1073/pnas.0502000102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Olmos-Alonso A., Schetters S.T., Sri S., Askew K., Mancuso R., Vargas-Caballero M., Holscher C., Perry V.H., Gomez-Nicola D. Pharmacological targeting of CSF1R inhibits microglial proliferation and prevents the progression of Alzheimer’s-like pathology. Brain. 2016;139:891–907. doi: 10.1093/brain/awv379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Spangenberg E.E., Lee R.J., Najafi A.R., Rice R.A., Elmore M.R.P., Blurton-Jones M., West B.L., Green K.N. Eliminating microglia in Alzheimer’s mice prevents neuronal loss without modulating amyloid-beta pathology. Brain. 2016;139:1265–1281. doi: 10.1093/brain/aww016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Spangenberg E., Severson P.L., Hohsfield L.A., Crapser J., Zhang J.Z., Burton E.A., Zhang Y., Spevak W., Line J., Phan N.Y., et al. Sustained microglial depletion with CSF1R inhibitor impairs parenchymal plaque development in an Alzheimer’s disease model. Nat. Commun. 2019;10:3758. doi: 10.1038/s41467-019-11674-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Lamb Y.N. Pexidartinib: First Approval. Drugs. 2019;79:1805–1812. doi: 10.1007/s40265-019-01210-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Bennett R.E., Bryant A., Hu M., Robbins A.B., Hopp S.C., Hyman B.T. Partial reduction of microglia does not affect tau pathology in aged mice. J. Neuroinflamm. 2018;15:311. doi: 10.1186/s12974-018-1348-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Sosna J., Philipp S., Albay R., III, Reyes-Ruiz J.M., Baglietto-Vargas D., LaFerla F.M., Glabe C.G. Early long-term administration of the CSF1R inhibitor PLX3397 ablates microglia and reduces accumulation of intraneuronal amyloid, neuritic plaque deposition and pre-fibrillar oligomers in 5XFAD mouse model of Alzheimer’s disease. Mol. Neurodegener. 2018;13:11. doi: 10.1186/s13024-018-0244-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Asai H., Ikezu S., Tsunoda S., Medalla M., Luebke J., Haydar T., Wolozin B., Butovsky O., Kugler S., Ikezu T. Depletion of microglia and inhibition of exosome synthesis halt tau propagation. Nat. Neurosci. 2015;18:1584–1593. doi: 10.1038/nn.4132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Clayton K., Delpech J.C., Herron S., Iwahara N., Ericsson M., Saito T., Saido T.C., Ikezu S., Ikezu T. Plaque associated microglia hyper-secrete extracellular vesicles and accelerate tau propagation in a humanized APP mouse model. Mol. Neurodegener. 2021;16:18. doi: 10.1186/s13024-021-00440-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Casali B.T., MacPherson K.P., Reed-Geaghan E.G., Landreth G.E. Microglia depletion rapidly and reversibly alters amyloid pathology by modification of plaque compaction and morphologies. Neurobiol. Dis. 2020;142:104956. doi: 10.1016/j.nbd.2020.104956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Karaahmet B., Le L., Mendes M.S., Majewska A.K., O’Banion M.K. Repopulated microglia induce expression of Cxcl13 with differential changes in Tau phosphorylation but do not impact amyloid pathology. J. Neuroinflamm. 2022;19:173. doi: 10.1186/s12974-022-02532-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Selkoe D.J., Hardy J. The amyloid hypothesis of Alzheimer’s disease at 25 years. EMBO Mol. Med. 2016;8:595–608. doi: 10.15252/emmm.201606210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Bartus R.T., Dean R.L., III, Beer B., Lippa A.S. The cholinergic hypothesis of geriatric memory dysfunction. Science. 1982;217:408–414. doi: 10.1126/science.7046051. [DOI] [PubMed] [Google Scholar]
- 161.McGeer P.L., Rogers J., McGeer E.G. Neuroimmune mechanisms in Alzheimer disease pathogenesis. Alzheimer Dis. Assoc. Disord. 1994;8:149–158. doi: 10.1097/00002093-199408030-00001. [DOI] [PubMed] [Google Scholar]
- 162.Swerdlow R.H., Burns J.M., Khan S.M. The Alzheimer’s disease mitochondrial cascade hypothesis. J. Alzheimer’s Dis. 2010;20((Suppl. 2)):S265–S279. doi: 10.3233/JAD-2010-100339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Zhu X., Raina A.K., Perry G., Smith M.A. Alzheimer’s disease: The two-hit hypothesis. Lancet Neurol. 2004;3:219–226. doi: 10.1016/S1474-4422(04)00707-0. [DOI] [PubMed] [Google Scholar]
- 164.De la Monte S.M. Insulin resistance and Alzheimer’s disease. BMB Rep. 2009;42:475–481. doi: 10.5483/BMBRep.2009.42.8.475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Alzheimer’s Association Calcium Hypothesis Workgroup. Khachaturian Z.S. Calcium Hypothesis of Alzheimer’s disease and brain aging: A framework for integrating new evidence into a comprehensive theory of pathogenesis. Alzheimer’s Dement. 2017;13:178–182.e17. doi: 10.1016/j.jalz.2016.12.006. [DOI] [PubMed] [Google Scholar]