Abstract
(1) Background: As times change, the detection rate of hypertension is increasing in the young and middle-aged population due to prevalent sedentary behaviors. The purpose of this study was to conduct a scoping review to identify and summarize the research on sedentary behavior in this population by separating it into five stages: the relationship between sedentary behavior and health; measurement modalities; influencing factors; interventions; and translational research in young and middle-aged adults with hypertension. (2) Methods: Using a scoping review research approach, the PubMed, Web of Science Core Collection, and MEDLINE databases were used to search for the literature on this subject from the date of the database’s creation to 14 June 2022, and the behavioral epidemiology framework was used to classify the retrieved articles. (3) Results: A total of eight articles were included. Among them, there were six articles on the relationship between behavior and health, which includes blood pressure, insulin resistance, and the cardiovascular system; one article on the study of measurement methods, which was used for clinical decision making through decision trees; one article on influencing factors, which was divided into intrinsic and extrinsic factors; and no articles on intervention program development or the translation of intervention programs to further practice in this population. (4) Conclusions: Sedentary behavioral studies of young and middle-aged adults with hypertension are scarce and are generally carried out in the early stages of the condition. In the future, in-depth studies can be conducted on the dose–response relationship between sedentary behavior and health in this population; the development of easier and targeted measurement tools; the exploration of more influencing factors; and the effectiveness and translation of intervention programs.
Keywords: hypertension, sedentary behaviors, scoping review, behavioral epidemiology
1. Introduction
Hypertension has become an important public health problem that threatens life and health, and studies show that the age of diagnosis of hypertension is decreasing, with the number of young and middle-aged adults with hypertension already exceeding 20.0% and growing [1]. Hypertension can cause a variety of injuries to target organs, including left ventricular (LV) hypertrophy, atherosclerosis, and carotid intima–media thickness, and can further lead to type 2 diabetes mellitus, chronic kidney disease, and even other chronic cardiovascular and cerebrovascular diseases [2]. In addition, high blood pressure also affects health-related quality of life (HRQoL) [3]. At the same time, young and middle-aged people are facing huge work and family pressures, changing lifestyles, and prevalent sedentary behaviors, which increase their risk for developing multiple health issues [4]. A large number of adults (54.2%) do not meet the WHO’s recommended level of physical activity [5], especially office workers, who maintain sedentary behaviors during the workday for 82.0% of the time [6].
Surveys have shown that 31.3–74.3% of people with hypertension have sedentary behaviors or sedentary lifestyles [7,8,9,10,11,12,13,14] and that sedentary behaviors increase the level of blood pressure in adults with hypertension, increase the risk of CVD in adults [15], and negatively affect the cardiovascular system and metabolism [16,17]. Antihypertensive medication has been the mainstream therapy in recent decades, but the rate of hypertension control has not changed significantly and may be related to poor lifestyle practices [18,19], such as sedentary behaviors. The guidelines state that healthy behavior changes play an important role in hypertension prevention and blood pressure control [20] and that the use of light-to-moderate physical activity as a substitute for sedentary behavior is of great importance in promoting health in young and middle-aged adults with hypertension [21]. Sedentary behavior (SB) includes any sitting or reclining posture behavior with an energy expenditure ≤1.5 metabolic equivalents (MET) in the awake condition [22]. Previous studies have often confused sedentary behavior with physical inactivity (PI), which is defined as not achieving the guideline-recommended level of physical activity [23], but still having an activity level that is often >1.5 MET. When SB and PI coexist, it is considered a sedentary lifestyle. There is no uniform definition of a sedentary lifestyle (SL). Martins et al. [24] considered an SL to be the same concept as PI and a lack of physical activity, whereas de Leon et al. [25] suggested using less than 25–30 min of physical activity per day as the definition of SL in clinical practice. In all of the above definitions, it is considered that SL, SB, and PI exist simultaneously. Therefore, this paper continues the above concepts and defines an SL as prolonged SB and the presence of PI. In conclusion, people with sedentary lifestyles must have sedentary behaviors, and thus the concept of sedentary behavior will be used consistently in later analyses.
The American scholars Sallis et al. [26] proposed a behavioral epidemiology framework in 2000, and this framework has been widely used to analyze the research progress and development of health behaviors [27,28]. A scoping review can reveal the current state of research within a particular topic and can analyze and discuss the research in a specific area more comprehensively, helping researchers to establish a clearer, more in-depth, and more explicit perception of the current state of the field [29]. However, at present, SB-related studies are still focused on the general population, and there are relatively few reviews of research progress related to SB in the chronic disease population, especially in young and middle-aged adults with hypertension, and the current status of the research field is unclear. With the increasing number of young and middle-aged adults with hypertension, clarifying what health outcomes SB causes in this population, what targeted measurement modalities and influencing factors are available, and the availability of intervention programs should also attract the attention of researchers, as all still require more extensive analyses. Therefore, this study used this framework to initiate a scoping review of the current state of research on SB in young and middle-aged adults with hypertension to provide suggestions for subsequent research directions.
2. Materials and Methods
2.1. Research Question
Based on the behavioral epidemiological framework, SB-related studies were divided into five stages:
Stage 1 includes studies that explore and verify the association between SB and health, with the aim of investigating how SB affects health outcomes in young and middle-aged adults with hypertension. Stage 2 entails research on methods for diagnosing and quantifying SB in this population. Stage 3 includes studies addressing relevant factors affecting SB in this population. Stage 4 includes studies on intervention strategies for SB that are aimed at reducing the duration of SB or changing the type of SB in this population, and the results should be focused on behavior or biomarkers of behavioral variables. Stage 5 includes studies on the practical application of intervention strategies and on the promotion and large-scale application of intervention programs in this population.
The criteria for determining the classification were as follows: (1) The entire article was read to determine the study’s purpose and the outcome variables under investigation. (2) If the outcome variable of the study was health outcomes, the purpose of the study was to explore the effect of behavior on health outcomes, and therefore it was classified as stage one. (3) If the paper involved the measurement of behavior, it was classified as stage two; (4) If the paper involved the potential effect on behavior, it was classified as stage three. (5) Papers that addressed the effectiveness or evaluated the effectiveness of interventions on behavior were classified as stage four. (6) Papers that assessed the extent to which relevant policies or interventions were implemented and maintained were classified as stage five. (7) Papers that fit into more than one category were coded as the highest stage.
The research methodology and reporting requirements of a scoping review were used to conduct the study [29,30,31], where the reporting specifications refer to PRISMA-SCR guideline requirements [32]. The main research question of this study was, based on this framework, what is the progress in SB research in young and middle-aged adults with hypertension?
2.2. Inclusion and Exclusion Criteria
Inclusion criteria: (1) the literature type was original studies (qualitative studies, quantitative studies, mixed studies, etc.); (2) the article was written in English; and (3) the study topic was SB in young and middle-aged adults with hypertension, with the age range of the study subjects being 18–65 years.
Exclusion criteria: (1) studies on children, the elderly, hypertensive pregnancies, or people without hypertension; (2) non-original studies (reviews, systematic reviews, scoping reviews, meta-analyses, commentaries, book reviews, etc.); (3) conferences, books, unpublished articles, and dissertations; (4) studies on SB topics that do not focus on young and middle-aged people with hypertension (e.g., the primarily study physical activity, the research focus is not SB, etc.); (5) full text not available; and (6) articles not applicable to analyses within this behavioral epidemiological framework (e.g., articles reporting only on the current status of SB in young and middle-aged people with hypertension).
2.3. Literature Sources and Search Strategies
English articles were obtained by using the PubMed, Web of Science Core Collection, and MEDLINE databases to search the literature from the date of the database’s creation to 14 June 2022. The search was performed as an advanced search using MeSH terms and keywords. According to the MeSH word list, SL was included in this study as an SB subtopic term in the review.
The English search terms were: (1) (Adults) OR (Young Adult) OR (Middle Aged); (2) (Sedentary behavior) OR (Behavior, Sedentary) OR (Sedentary Behaviors) OR (Sedentary Lifestyle) OR (Lifestyle, Sedentary) OR (Physical Inactivity) OR (Inactivity, Physical) OR (Lack of Physical Activity) OR (Sedentary Time) OR (Sedentary Times) OR (Time, Sedentary); and (3) (Hypertension) OR (Blood Pressure, High) OR (Blood Pressures, High) OR (High Blood Pressure) OR (High Blood Pressures). The groups were connected in parallel using “AND”.
2.4. Evidence Selection and Information Extraction
The resulting literature captions were extracted and imported into NoteExpress, and duplicate articles were excluded. Two researchers (K.Z. and D.F.) read the article titles, abstracts, and keywords according to the inclusion and exclusion criteria and performed the initial screening independently. After the initial screening was completed, the remaining full-text articles were read and screened again to determine the final included literature. The full texts of the included literature were read through and classified according to the main outcome indicators and the research foci of the articles in relation to the behavioral epidemiological framework stages. Throughout the process, both researchers were independently and professionally trained, and a third researcher (Q.W.) was consulted in the case of a disagreement. The final article authors (time of publication), sample, country/region, blood pressure level, study type, measurement tools, and outcome indicators were extracted. The articles were categorized according to the behavioral epidemiological framework of the stage they were in and were analyzed in stages, as shown in Table 1.
Table 1.
Basic characteristics of the literature for inclusion in this analysis.
| Author (Time of Publication) | Stage 1 | Number of Samples (Age 2) | Country/Region | Research Type | Tools for Measuring SB (Definition/Program 3) | Result Indicators |
|---|---|---|---|---|---|---|
| Gibbs et al. [33] (2017) | 1 | 25 (average age: 42; 20–65 years old) | United States of America | Randomized controlled trials | activPAL3 micro (two periods of 3 h and 40 min of continuous seated desk work). | BP 4; PWV 5 |
| Alansare et al. [34] (2020) | 1 | 25 (20–65 years old) | United States of America | Randomized controlled trials | activPAL3 micro (except for required bathroom breaks, participants worked at a conventional desk while sitting still during the sitting period, with their feet flat on the floor). | BP; PWV |
| Perdomo et al. [35] (2019) | 1 | 25 (average age: 42; 20–65 years old) | United States of America | Randomized controlled trials | Global Physical Activity Questionnaire (the SB group was required to sit continuously). | BP; CBFv 6 |
| Hwu et al. [36] (2004) | 1 | 872 (35–60 years old; SB subjects averaged 51.8 ± 8.5 years old; non-SB subjects averaged 52.7 ± 8.8 years old) | Asia-Pacific | Cross-sectional studies | Total physical activity was measured by keeping track of how many hours a day were spent engaging in physical activity. (Sedentary activity hours)/(24 h—base activity hours) was used to calculate physical inactivity (participants were referred to as “SB” if their physical activity score was higher than 0.5). | Insulin resistance |
| Palatini et al. [37] (2011) | 1 | 87 (SB subjects averaged 33.2 ± 8.7 years old; non-SB subjects averaged 29.7 ± 8.6 years old) | Italy | Prospective studies | A standardized questionnaire was used to measure physical activity [38] (participants were categorized as sedentary if they did not regularly engage in any physical activity). | Carotid intima–media thickness |
| Palatini et al. [39] (2009) | 1 | 454 (18–45 years old; average age: 33.1 ± 8.4 years old) | Italy | Prospective studies | A standardized questionnaire was used to measure physical activity [38] (participants were categorized as sedentary if they did not regularly engage in any physical activity). | LV 7 mass; LV hypertrophy |
| Castelo et al. [40] (2016) | 2 | 285 (19–59 years old) | Brazil | Cross-sectional studies | An instrument was used with variables related to identification, related factors, and signs and symptoms. The diagnostic inference was made by four nurses who had received prior training in an 8-h course [40] (definition based on NANDA-I 9). | SB 8 |
| Martins et al. [41] (2015) | 3 | 285 (19–59 years old) | Brazil | Cross-sectional studies | A tool that was created based on previously validated clinical signs and related factors was used to collect the data [42] (individuals with SB were defined as those who do not exercise at the recommended frequency, duration, and intensity or do not expend significant energy to improve their physical condition). | SB; PA 10 |
1 Stage: Classification of study stages based on an epidemiological framework. Stage 1: studies to explore and verify the association between SB and health; stage 2: studies on SB measurement methods; stage 3: studies to explore the factors influencing SB; stage 4: studies on intervention strategies for SB; stage 5: studies on the practical application of intervention strategies. 2 Age: organized according to the age ranges of the subjects included in the studies. 3 Definition/program: the definition of SB used in the study or the setting of SB in the study protocol. 4 BP: blood pressure. 5 PWV: pulse wave velocity. 6 CBFv: pulse cerebral blood flow velocity. 7 LV: left ventricular. 8 SB: sedentary behavior. 9 Definition based on NANDA-I: “Choose a daily routine without exercise”; “It shows a lack of physical fitness”; “Verbalizes preference for activities with little exercise”. 10 PA: physical activity.
3. Results
3.1. Literature Search Results
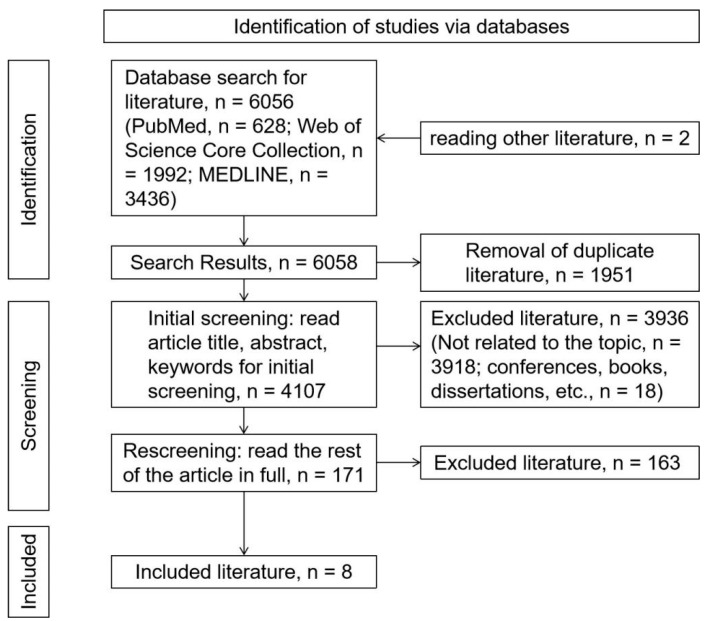
A total of 6056 articles were retrieved from the database according to the search strategy, and 2 articles were added by reading other articles’ references [8,43], bringing the total to 6058 articles. There were 1951 duplicate articles removed; 3918 documents unrelated to the topic were excluded; and 18 articles from conferences, books, dissertations, etc., were excluded, leaving 171 articles. After reading the full text of the remaining articles and rescreening, a total of 163 documents were excluded (non-original studies (reviews, book reviews, etc.) and non-English, n = 13; study population not young and middle-aged adults with hypertension, n = 35; unrelated to topic, n = 106; and study only reported current status of sedentary behavior, n = 9), and 8 documents were included [33,34,35,36,37,39,40,41]. The steps of the literature search are shown in Figure 1.
Figure 1.
The literature search process.
3.2. Characteristics of the Included Literature
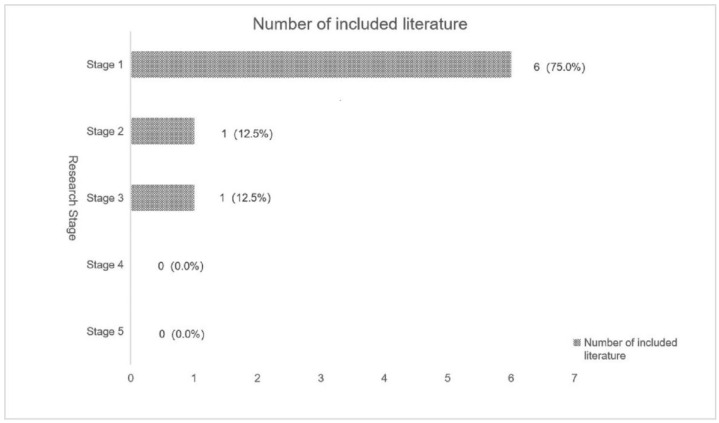
According to this framework [26], the distribution of SB study topics in young and middle-aged adults with hypertension is shown in Figure 2. After searching, a total of eight SB studies on young and middle-aged adults with hypertension were included, with the highest number of studies concentrated in stage 1. Out of all the included studies, 37.5% were from the United States, with three articles written by Gibbs [33,34,35]. Six studies focused on subjects with prehypertension, hypertension stage 1, and hypertension stage 2. There was no literature included that met stage 4 (studies on intervention strategies for SB) or stage 5 (studies on the practical application of intervention strategies). The included literature, all of which were quantitative studies, included prospective studies (25.0%), cross-sectional studies (37.5%), and randomized controlled trials (37.5%).
Figure 2.
Distribution of SB study topics in young and middle-aged adults with hypertension (stage 1: studies to explore and verify the association between SB and health; stage 2: studies on SB measurement methods; stage 3: studies to explore the factors influencing SB; stage 4: studies on intervention strategies for SB; stage 5: studies on the practical application of intervention strategies).
3.3. Inclusion of Details from the Literature
3.3.1. Relationships with Health
A total of six (75.0%) studies were classified as stage 1, as they analyzed the association between SB and health outcomes in young and middle-aged adults with hypertension (one cross-sectional study, two prospective studies, and three randomized controlled trials), as shown in Table 1. The reason for classifying these randomized controlled trials [33,34,35] as stage 1 rather than stage 4 is that, by reading the full articles, it was clear that the primary foci of the studies and the purposes of the interventions in these articles were to explore the health-related changes caused by changing SB, but the foci of the studies were not on how to change SB. Changing SB was only used as a precondition in these articles. The fourth stage focuses on more general interventions for SB, and the focus of a study should be on whether the intervention program changes SB rather than health outcomes.
After controlling for demographic variables, it was found that people with hypertension who displayed SB had lower insulin sensitivity and greater insulin resistance [36]. A randomized controlled trial showed that interrupting prolonged SB with intermittent standing significantly reduced diastolic blood pressure (DBP) and mean arterial pressure (MAP) in subjects compared to continuous SB [33]. Alansare et al. [34] found that maintaining SB after a simulated workday experiment resulted in increases in sitting systolic blood pressure (SBP), DBP, MAP, supine carotid–femoral pulse wave velocity (cfPWV), and carotid–ankle pulse wave velocity (caPWV). In people with elevated blood pressure, prolonged SB maintenance causes a significant slowing of the cerebral blood flow velocity (CBFv) in the middle of the day [35]. Prospective studies have shown a higher risk of new-onset LV hypertrophy in adults with hypertension and an SL compared to physically active people, with a significant increase in the LV end-diastolic diameter [39]. In a study by Palatini et al. [37], they showed that the cumulative maximum and cumulative mean carotid intima–media thickness (IMT) of the three carotid segments was higher in subjects with an SL than in subjects with adequate activity.
3.3.2. Measurement Method
In the second stage, one study (12.5%) focused on the clinical diagnosis and prediction of SB in young and middle-aged adults with hypertension, as shown in Table 1.
Castelo et al. [40] used the CHAID algorithm with a decision tree model to construct a decision tree for SB in adults with hypertension to analyze the probability of SB in individuals with a sedentary lifestyle. The first node of this decision tree model was the clinical indicator “daily physical inactivity”, and the probability of SB was 0.88 for those with this indicator, whereas the second node was “physical inactivity in leisure time” and the probability of SB was 0.99 for those with both of these two indicators. This decision tree has a predictive power of 69.5% and can be used by nurses in the clinic to diagnose SB in adults with hypertension and optimize the diagnosis time.
3.3.3. Influencing Factors
One (12.5%) study was included in the third stage on factors influencing SB, as it focused on respondents’ intrinsic and extrinsic factors, as shown in Table 1.
Martins et al. [41] indicated that respondents’ intrinsic factors included a “lack of motivation to perform physical activity”, a “lack of interest in physical activity”, “mindset, beliefs, and health habits that hinder physical activity”, and a “lack of confidence in physical activity practice”, whereas their external factors were a “lack of training to complete physical activity” and a “lack of physical activity training”.
The study also pointed out that the factors of a “Lack of motivation to perform physical activity” and a “lack of interest in physical activity” were the most important reasons for the existence of SB (PR = 5.358), and the presence of these factors increased the probability of an SB diagnosis five-fold [41].
4. Discussion
4.1. SB and Health
SB is detrimental to the short- and long-term health of young and middle-aged adults with hypertension.
Based on the stage 1 study, it is evident that SB negatively affects blood pressure (blood pressure level and blood pressure management), the cardiovascular system (left ventricular hypertrophy, carotid intima–medial thickness, cerebral blood flow velocity, and pulse wave velocity), and insulin sensitivity in young and middle-aged adults with hypertension. Prolonged SB increases the degree of blood pressure in young and middle-aged people with hypertension and is detrimental to their blood pressure control [33]. In the long term, its effects on the carotid intima–medial thickness and pulse wave velocity in this population reflect its adverse effects on vascular health [37], further increasing the risk of CVD, such as atherosclerosis, and a poor prognosis [15]. This was also reflected by outcomes such as left ventricular hypertrophy in the prospective study [39]. Additionally, the effect of SB on insulin sensitivity in this population cannot be ignored, which may indicate that prolonged exposure to SB increases the risk of diabetes in this population [36].
Prolonged SB during the workday increases the degree of sitting blood pressure in adults with hypertension [34]. In contrast, SB was also significantly associated with the development of hypertension in a non-hypertensive young and middle-aged population [44,45]. Koyama et al. [46] and Vancampfort et al. [47] noted that reducing sedentary time in patients with chronic diseases was more beneficial in improving their prognosis and quality of life than exercising alone. Other studies have noted that SB has the strongest association out of all factors associated with all causes of death from CVD [48,49].
Therefore, there is a need to accurately measure SB in young and middle-aged adults with hypertension to identify influencing factors and explore effective interventions to improve prognoses. Although the stage 1 inclusion study pointed out that SB may contribute to cardiovascular disease risk and adverse long-term health outcomes in young and middle-aged adults with hypertension, the dose–response relationship between SB and adverse health outcomes in this population is not clear. In addition, studies have focused on overall SB duration and the different health effects that can result from different SBs remain understudied.
4.2. Diagnosis and Measurement of SB
Diagnostic and measurement tools for SB are poorly researched and of limited utility. The accurate diagnosis and measurement of SB is a prerequisite for the identification of SB and its extent.
Although decision trees have shown a high accuracy in the identification and diagnosis of SB, the algorithm used is deficient in terms of stability and is susceptible to overfitting problems due to factors such as the number of nodes and is not suitable for extrapolation to other samples or populations [50].
Current measurements for SB are similar to those for physical activity and are divided into subjective and objective categories. Subjective measures include measurements using self-reported tools such as questionnaires and SB logs, and objective measures includes the use of tools such as accelerometer heart rate monitors [51].
Although some studies with targeted instruments have been conducted in people with hypertension, the measurement of SB in this population is still commonly reported using self-reported questionnaires [52,53]. Self-reported questionnaires are the most commonly used tool to assess physical activity, and they are also used to explore the SB of populations. The advantages are that they are less resource-intensive, more conducive to surveys in less resourced areas, and easier to replicate, but these measures are more subjective in nature [54]. Additionally, there is less evidence of applicability with more targeted questionnaires, such as the Adult Sedentary Behaviour Questionnaire (ASBQ) [55], in young and middle-aged people with hypertension. Therefore, more studies using and validating these instruments should be reported.
4.3. Influencing Factors of SB
The influencing factors of SB have been widely explored but are not yet systematized. Identifying influencing factors is a prerequisite for the development of better interventions. Studies have pointed out that knowledge/attitude factors are important influences on SB [41,56]. Among them, perceptions about exercise and health were examined by several studies and were significantly associated with SB. Negative health perceptions and insufficient knowledge about physical activity and SB can make young and middle-aged adults with hypertension reluctant to improve their SB, and thus it is especially important to emphasize the negative effects of SB and help young and middle-aged adults with hypertension understand this when educating them [14,41]. Unlike in the general population, the source of health information for young and middle-aged adults with hypertension is more likely to be medical personnel [14]. This suggests that healthcare workers are key participants in improving the lifestyles of adults with hypertension. In addition to the influence of knowledge and attitudes, other influencing factors include the lack of external conditions related to physical activity conditions, such as time and space [41]. Gender, age, the presence of a spouse, education level, and underlying medical conditions were also found to be influential factors for SB in people with hypertension [57,58]. Unlike other age groups, SB in the young and middle-aged population is also influenced by the type of work [59], which also requires research attention.
Overall, there is still a dearth of data, and therefore more studies examining the impact of various factors on SB in young and middle-aged adults with hypertension are required (e.g., studies on demographic factors, peer support, family influence, physician influence, etc.). By examining the knowledge and attitudes about SB, the environment for physical activity, and the community support to guide the design of intervention programs, follow-up studies should increase the use of theory.
4.4. General Analysis
The majority of the articles included in this study focused on subjects with prehypertension, hypertension stage I, and hypertension stage II [33,34,35,36,37,39], which may be related to the risk of physical activity and high blood pressure. There were no theory-based studies on SB in young and middle-aged adults with hypertension in the included literature. Follow-up studies could use mixed studies and qualitative studies to combine more theoretical frameworks to comprehensively and thoroughly explore the research on SB improvements and interventions in young and middle-aged people with hypertension to complement the results of the quantitative studies.
4.5. Advantages and Limitations
Based on a behavioral epidemiological paradigm, this paper used a scoping review approach to describe the development of SB research in middle-aged and young adults with hypertension and offers workable directions for further in-depth studies.
The following are some of the paper’s limitations: (1) Only studies published in English were included. (2) In addition, most of the studies were conducted in developed countries, which may affect the generalization of the data to populations in other countries or regions. (3) Based on the research requirements of the scoping review, no quality evaluation or risk of bias assessment of the included literature were performed, and other subsequent studies can be explored in depth through research methods such as systematic reviews.
5. Conclusions
Based on a behavioral epidemiological framework, this article compared and summarized the current state of research on sedentary behaviors in young and middle-aged adults with hypertension by using a scoping review approach to analyze the English literature published before 14 June 2022.
Research on SB in young and middle-aged people with hypertension is still in its infancy, and the majority of studies have concentrated on the harmful effects of SB with regard to blood pressure, the cardiovascular system, and metabolism in young and middle-aged adults with hypertension. There is still a general dearth of theoretical framework supports for studies on the factors driving SB, with the majority of studies concentrating on knowledge, attitudinal, and extrinsic factors. There is also a lack of simple and accurate measurement tools for SB, and there are no evidence-based, effective interventions for the time being. Follow-up studies could select the dose–response relationships between different SBs and health outcomes in young and middle-aged adults with hypertension, develop simpler and targeted measurement tools, explore more SB-influencing factors in combination with theories, and conduct intervention program design and translation studies.
Acknowledgments
Thanks to all those who helped with this article.
Author Contributions
Conceptualization, K.Z. and S.H.; methodology, K.Z.; software, K.Z., D.F. and Q.W.; validation, D.F., X.L., Y.L. and Q.W.; formal analysis, K.Z., D.F. and Q.W.; data curation, K.Z. and Y.L.; writing—original draft preparation, K.Z.; writing—review and editing, K.Z., D.F., X.L., Y.L. and Q.W.; project administration, S.H.; funding acquisition, K.Z. and S.H. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This review was funded by the Fundamental Research Funds for the Central Universities (YCJJ202201055) and National Natural Science Foundation of China (No. 71874063).
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.de Venecia T., Lu M., Figueredo V.-M. Hypertension in young adults. Postgrad. Med. 2016;128:201–207. doi: 10.1080/00325481.2016.1147927. [DOI] [PubMed] [Google Scholar]
- 2.Arija V., Villalobos F., Pedret R., Vinuesa A., Jovani D., Pascual G., Basora J. Physical activity, cardiovascular health, quality of life and blood pressure control in hypertensive subjects: Randomized clinical trial. Health Qual. Life Outcomes. 2018;16:184. doi: 10.1186/s12955-018-1008-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen Q., Ran L., Li M., Tan X. Health-related quality of life of middle-aged and elderly people with hypertension: A cross-sectional survey from a rural area in China. PLoS ONE. 2021;16:e246409. doi: 10.1371/journal.pone.0246409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Owen N., Healy G.-N., Dempsey P.-C., Salmon J., Timperio A., Clark B.-K., Goode A.-D., Koorts H., Ridgers N.-D., Hadgraft N.-T., et al. Sedentary Behavior and Public Health: Integrating the Evidence and Identifying Potential Solutions. Annu. Rev. Public Health. 2020;41:265–287. doi: 10.1146/annurev-publhealth-040119-094201. [DOI] [PubMed] [Google Scholar]
- 5.Malete L., Ricketts C., Chen S., Jackson J. Correlates of Physical Activity Among Adults in Botswana: Sociodemographic Factors, Health Status, and Body Image. J. Phys. Act. Health. 2022;19:599–606. doi: 10.1123/jpah.2022-0243. [DOI] [PubMed] [Google Scholar]
- 6.Morton S., Fitzsimons C., Jepson R., Saunders D.-H., Sivaramakrishnan D., Niven A. What works to reduce sedentary behavior in the office, and could these intervention components transfer to the home working environment?: A rapid review and transferability appraisal. Front. Sports Act. Living. 2022;4:954639. doi: 10.3389/fspor.2022.954639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Desai N., Unni G., Agarwala R., Salagre S., Godbole S., Dengra A., Abhyankar M.-V., Revankar S. Risk Factors and Comorbidities in Young Indian Patients with Hypertension: REAL YOUNG (Hypertension) Study. Integr. Blood Press. Control. 2021;14:31. doi: 10.2147/IBPC.S272548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Martins L.C.G., Lopes M.V.D., Guedes N.-G., Teixeira I.-X., de Sousa V.E.C., Montoril M.-H. Nursing diagnosis sedentary lifestyle in individuals with hypertension: An analysis of accuracy. Revista Da Escola De Enfermagem Da Usp. 2014;48:803–808. doi: 10.1590/S0080-6234201400005000005. [DOI] [PubMed] [Google Scholar]
- 9.Guedes N.-G., Lopes M.-V., Moreira R.-P., Cavalcante T.-F., de Araujo T.-L. Prevalence of sedentary lifestyle in individuals with high blood pressure. Int. J. Nurs. Terminol. Classif. 2010;21:50–56. doi: 10.1111/j.1744-618X.2010.01146.x. [DOI] [PubMed] [Google Scholar]
- 10.Gavaldà L., Ramón J.-M., Torras M.-G., Amenós A.M., Rama H., Sarrias X. The prevalence of cardiovascular risk factors in a population of essential hypertension patients. Rev. Esp. Cardiol. 1993;46:626–632. [PubMed] [Google Scholar]
- 11.Ratnaparkhe V., Bhangale A. Left Ventricular Diastolic Dysfunction in Primary Hypertension and its Relation with Leisure Time Physical Activity. J. Assoc. Phys. India. 2015;63:20–24. [PubMed] [Google Scholar]
- 12.Sampaio F.-C., De Oliveira P.P., Da Mata L.R.F., Moraes J.T., Da Fonseca D.F., de Sousa Vieira V.A. Profile of nursing diagnoses in people with hypertension and diabetes. Investig. Educ. Enferm. 2017;35:139–153. doi: 10.17533/udea.iee.v35n2a03. [DOI] [PubMed] [Google Scholar]
- 13.da Silva P.M., Maria-Joao L., Pedro-Macedo N., De Macedo M.E. Prevalence of cardiovascular risk factors and other comorbidities in patients with hypertension in Portuguese primary health care populations: The PRECISE study. Rev. Port. De Cardiol. 2019;38:427–437. doi: 10.1016/j.repc.2018.09.011. [DOI] [PubMed] [Google Scholar]
- 14.Esteves D., Duarte P., Pinheiro P., Bras R., Rodrigues R.-G., Gouveia A., O’Hara K. Physical activity and supervised exercise among hypertensives and normotensives: Status and barriers. Sport Sci. Health. 2020;16:323–330. doi: 10.1007/s11332-019-00609-2. [DOI] [Google Scholar]
- 15.Liang Z.-D., Zhang M., Wang C.-Z., Yuan Y., Liang J.-H. Association between sedentary behavior, physical activity, and cardiovascular disease-related outcomes in adults-A meta-analysis and systematic review. Front. Public Health. 2022;10:1018460. doi: 10.3389/fpubh.2022.1018460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sackner M.-A., Patel S., Adams J.-A. Changes of blood pressure following initiation of physical inactivity and after external addition of pulses to circulation. Eur. J. Appl. Physiol. 2019;119:201–211. doi: 10.1007/s00421-018-4016-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gerage A.-M., Benedetti T.R.B., Farah B.-Q., Santana F.-D., Ohara D., Andersen L.-B., Ritti-Dias R.-M. Sedentary Behavior and Light Physical Activity Are Associated with Brachial and Central Blood Pressure in Hypertensive Patients. PLoS ONE. 2015;10:e0146078. doi: 10.1371/journal.pone.0146078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cherfan M., Vallee A., Kab S., Salameh P., Goldberg M., Zins M., Blacher J. Unhealthy behaviors and risk of uncontrolled hypertension among treated individuals-The CONSTANCES population-based study. Sci. Rep. 2020;19:25. doi: 10.1038/s41598-020-58685-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gorostegi-Anduaga I., Corres P., Jurio-Iriarte B., Martinez-Aguirre A., Perez-Asenjo J., Aispuru G.-R., Arenaza L., Romaratezabala E., Arratibel-Imaz I., Mujika I., et al. Clinical, physical, physiological, and dietary patterns of obese and sedentary adults with primary hypertension characterized by sex and cardiorespiratory fitness: EXERDIET-HTA study. Clin. Exp. Hypertens. 2018;40:141–149. doi: 10.1080/10641963.2017.1346111. [DOI] [PubMed] [Google Scholar]
- 20.Rabi D.-M., McBrien K.-A., Sapir-Pichhadze R., Nakhla M., Ahmed S.-B., Dumanski S.-M., Butalia S., Leung A.-A., Harris K.-C., Cloutier L., et al. Hypertension Canada’s 2020 Comprehensive Guidelines for the Prevention, Diagnosis, Risk Assessment, and Treatment of Hypertension in Adults and Children. Can. J. Cardiol. 2020;36:596–624. doi: 10.1016/j.cjca.2020.02.086. [DOI] [PubMed] [Google Scholar]
- 21.Dempsey P.-C., Friedenreich C.-M., Leitzmann M.-F., Buman M.-P., Lambert E., Willumsen J., Bull F. Global Public Health Guidelines on Physical Activity and Sedentary Behavior for People Living With Chronic Conditions: A Call to Action. J. Phys. Act. Health. 2021;18:76–85. doi: 10.1123/jpah.2020-0525. [DOI] [PubMed] [Google Scholar]
- 22.Tremblay M.-S., Aubert S., Barnes J.-D., Saunders T.-J., Carson V., Latimer-Cheung A.-E., Chastin S.F.M., Altenburg T.-M., Chinapaw M.J.M. Sedentary Behavior Research Network (SBRN)—Terminology Consensus Project process and outcome. Int. J. Behav. Nutr. Phys. Act. 2017;14:75. doi: 10.1186/s12966-017-0525-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.WHO . Guidelines on Physical Activity and Sedentary Behaviour. World Health Organization; Geneva, Switzerland: 2020. [PubMed] [Google Scholar]
- 24.Martins L.C.G., Lopes M.V.O., Diniz C.-M., Guedes N.-G. The factors related to a sedentary lifestyle: A meta-analysis review. J. Adv. Nurs. 2021;77:1188–1205. doi: 10.1111/jan.14669. [DOI] [PubMed] [Google Scholar]
- 25.de Leon A.-C., Rodriguez-Perez M.-D., Rodriguez-Benjumeda L.-M., Ania-Lafuente B., Brito-Diaz B., de Fuentes M.-M., Almeida-Gonzalez D., Batista-Medina M., Aguirre-Jaime A. Sedentary lifestyle: Physical activity duration versus percentage of energy expenditure. Rev. Esp. Cardiol. 2007;60:244–250. doi: 10.1016/S1885-5857(07)60148-0. [DOI] [PubMed] [Google Scholar]
- 26.Sallis J.-F., Owen N., Fotheringham M.-J. Behavioral epidemiology: A systematic framework to classify phases of research on health promotion and disease prevention. Ann. Behav. Med. 2000;22:294–298. doi: 10.1007/BF02895665. [DOI] [PubMed] [Google Scholar]
- 27.Nery M.-B., Driver S., Vanderbom K.-A. Systematic framework to classify the status of research on spinal cord injury and physical activity. Arch. Phys. Med. Rehabil. 2013;94:2027–2031. doi: 10.1016/j.apmr.2013.04.016. [DOI] [PubMed] [Google Scholar]
- 28.Cleveland S., Driver S., Swank C., Macklin S. Classifying physical activity research following stroke using the behavioral epidemiologic framework. Top. Stroke Rehabil. 2015;22:289–298. doi: 10.1179/1074935714Z.0000000043. [DOI] [PubMed] [Google Scholar]
- 29.Munn Z., Peters M.D.J., Stern C., Tufanaru C., McArthur A., Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med. Res. Methodol. 2018;18:143. doi: 10.1186/s12874-018-0611-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tricco A.-C., Lillie E., Zarin W., O’Brien K., Colquhoun H., Kastner M., Levac D., Ng C., Sharpe J.-P., Wilson K., et al. A scoping review on the conduct and reporting of scoping reviews. BMC Med. Res. Methodol. 2016;16:15. doi: 10.1186/s12874-016-0116-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.O’Brien K.-K., Colquhoun H., Levac D., Baxter L., Tricco A.-C., Straus S., Wickerson L., Nayar A., Moher D., O’Malley L. Advancing scoping study methodology: A web-based survey and consultation of perceptions on terminology, definition and methodological steps. BMC Health Serv. Res. 2016;16:305. doi: 10.1186/s12913-016-1579-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tricco A.-C., Lillie E., Zarin W., O’Brien K.-K., Colquhoun H., Levac D., Moher D., Peters M.D.J., Horsley T., Weeks L., et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern Med. 2018;169:467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 33.Gibbs B.B., Kowalsky R.J., Perdomo S.J., Taormina J.M., Balzer J.R., Jakicic J.M. Effect of alternating standing and sitting on blood pressure and pulse wave velocity during a simulated workday in adults with overweight/obesity. J. Hypertens. 2017;35:2411–2418. doi: 10.1097/HJH.0000000000001463. [DOI] [PubMed] [Google Scholar]
- 34.Alansare A.-B., Kowalsky R.-J., Jones M.-A., Perdomo S.-J., Stoner L., Gibbs B.-B. The Effects of a Simulated Workday of Prolonged Sitting on Seated versus Supine Blood Pressure and Pulse Wave Velocity in Adults with Overweight/Obesity and Elevated Blood Pressure. J. Vasc. Res. 2020;57:355–366. doi: 10.1159/000510294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Perdomo S.-J., Gibbs B.-B., Kowalsky R.-J., Taormina J.-M., Balzer J.-R. Effects of Alternating Standing and Sitting Compared to Prolonged Sitting on Cerebrovascular Hemodynamics. Sport Sci. Health. 2019;15:375–383. doi: 10.1007/s11332-019-00526-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hwu C.-M., Hsiao C.-F., Kuo S.-W., Wu K.-D., Ting C.-T., Quertermous T., Rodriguez B., Chen I., Grove J., Chen P.-Y., et al. Physical inactivity is an important lifestyle determinant of insulin resistance in hypertensive patients. Blood Press. 2004;13:355–361. doi: 10.1080/08037050410004828. [DOI] [PubMed] [Google Scholar]
- 37.Palatini P., Massimo P., Marcello R., Paolo P. Effect of regular physical activity on carotid intima-media thickness. Results from a 6-year prospective study in the early stage of hypertension. Blood Press. 2011;20:37–44. doi: 10.3109/08037051.2010.524080. [DOI] [PubMed] [Google Scholar]
- 38.Palatini P., Graniero G.-R., Mormino P., Nicolosi L., Mos L., Visentin P., Pessina A.-C. Relation between physical training and ambulatory blood pressure in stage I hypertensive subjects. Results of the HARVEST Trial. Hypertension and Ambulatory Recording Venetia Study. Circulation. 1994;90:2870–2876. doi: 10.1161/01.CIR.90.6.2870. [DOI] [PubMed] [Google Scholar]
- 39.Palatini P., Visentin P., Dorigatti F., Guarnieri C., Santonastaso M., Cozzio S., Pegoraro F., Bortolazzi A., Vriz O., Mos L., et al. Regular physical activity prevents development of left ventricular hypertrophy in hypertension. Eur. Heart J. 2009;30:225–232. doi: 10.1093/eurheartj/ehn533. [DOI] [PubMed] [Google Scholar]
- 40.Castelo G., De Oliveira Lopes M.V., Guedes N.G., De Menezes A.P., de Oliveira Farias O., Dos Santos N.A. Classification tree for the assessment of sedentary lifestyle among hypertensive. Investig. Educ. Enferm. 2016;34:113–119. doi: 10.17533/udea.iee.v34n1a13. [DOI] [PubMed] [Google Scholar]
- 41.Martins L.-C., Lopes M.-V., Guedes N.-G., Nunes M.-M., Diniz C.-M., Carvalho P.-M. Sedentary lifestyle in individuals with hypertension. Rev. Bras. Enferm. 2015;68:1005–1012. doi: 10.1590/0034-7167.2015680602i. [DOI] [PubMed] [Google Scholar]
- 42.Guedes N.-G., Lopes M.-V., Cavalcante T.-F., Moreira R.-P., de Araujo T.-L. Review of nursing diagnosis sedentary lifestyle in individuals with hypertension: Conceptual analysis. Rev. Esc. Enferm. USP. 2013;47:742–749. doi: 10.1590/S0080-623420130000300031. [DOI] [PubMed] [Google Scholar]
- 43.Lopes M.-V., Silva V.-M., Araujo T.-L. Methods for establishing the accuracy of clinical indicators in predicting nursing diagnoses. Int. J. Nurs. Knowl. 2012;23:134–139. doi: 10.1111/j.2047-3095.2012.01213.x. [DOI] [PubMed] [Google Scholar]
- 44.Lavôr L.C.d.C., de Sousa R.R., Rodrigues L.A.R.L., Rodrigues Filho O.d.S., Paiva A.d.A., Frota K.d.M.G. Prevalence of arterial hypertension and associated factors: A population-based study. Rev. Assoc. Med. Bras. 2020;66:630–636. doi: 10.1590/1806-9282.66.5.630. [DOI] [PubMed] [Google Scholar]
- 45.Wei Q. The five-year effects of physical activity and sedentary behaviour on chronic disease morbidity of Chinese adults. Int. J. Serv. Technol. Manag. 2019;25:302–310. doi: 10.1504/IJSTM.2019.100052. [DOI] [Google Scholar]
- 46.Koyama T., Kuriyama N., Ozaki E., Tomida S., Uehara R., Nishida Y., Shimanoe C., Hishida A., Tamura T., Tsukamoto M., et al. Sedentary Time is Associated with Cardiometabolic Diseases in A Large Japanese Population: A Cross-Sectional Study. J. Atheroscler. Thromb. 2020;27:1097–1107. doi: 10.5551/jat.54320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Vancampfort D., Stubbs B., Koyanagi A. Physical chronic conditions, multimorbidity and sedentary behavior amongst middle-aged and older adults in six low- and middle-income countries. Int. J. Behav. Nutr. Phys. Act. 2017;14:147. doi: 10.1186/s12966-017-0602-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Katzmarzyk P.-T., Powell K.-E., Jakicic J.-M., Troiano R.-P., Piercy K., Tennant B. Sedentary Behavior and Health: Update from the 2018 Physical Activity Guidelines Advisory Committee. Med. Sci. Sport Exerc. 2019;51:1227–1241. doi: 10.1249/MSS.0000000000001935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kim Y., Wilkens L.-R., Park S.-Y., Goodman M.-T., Monroe K.-R., Kolonel L.-N. Association between various sedentary behaviours and all-cause, cardiovascular disease and cancer mortality: The Multiethnic Cohort Study. Int. J. Epidemiol. 2013;42:1040–1056. doi: 10.1093/ije/dyt108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Song Y.-Y., Lu Y. Decision tree methods: Applications for classification and prediction. Shanghai Arch. Psychiatry. 2015;27:130–135. doi: 10.11919/j.issn.1002-0829.215044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Dempsey P.-C., Owen N., Biddle S.-J., Dunstan D.-W. Managing sedentary behavior to reduce the risk of diabetes and cardiovascular disease. Curr. Diab. Rep. 2014;14:522. doi: 10.1007/s11892-014-0522-0. [DOI] [PubMed] [Google Scholar]
- 52.Lopes M.-V., da Silva V.M., de Araujo T.-L., Guedes N.-G., Martins L.-C., Teixeira I.-X. Instrument for evaluation of sedentary lifestyle in patients with high blood pressure. Rev. Bras. Enferm. 2015;68:445–451. doi: 10.1590/0034-7167.2015680310i. [DOI] [PubMed] [Google Scholar]
- 53.Islam F.M.A., Bhowmik J., Camera D.-M., Maddison R., Lambert G.-W. Concordance between Different Criteria for Self-Reported Physical Activity Levels and Risk Factors in People with High Blood Pressure in a Rural District in Bangladesh. Int. J. Environ. Res. Public Health. 2021;18:10487. doi: 10.3390/ijerph181910487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ainsworth B., Cahalin L., Buman M., Ross R. The current state of physical activity assessment tools. Prog. Cardiovasc. Dis. 2015;57:387–395. doi: 10.1016/j.pcad.2014.10.005. [DOI] [PubMed] [Google Scholar]
- 55.Chu A.H.Y., Ng S.H.X., Koh D., Müller-Riemenschneider F. Domain-Specific Adult Sedentary Behaviour Questionnaire (ASBQ) and the GPAQ Single-Item Question: A Reliability and Validity Study in an Asian Population. Int. J. Env. Res Public Health. 2018;15:739. doi: 10.3390/ijerph15040739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wienert J., Kuhlmann T., Fink S., Hambrecht R., Lippke S. Motivational and Volitional Correlates of Physical Activity in Participants Reporting No, Past, and Current Hypertension: Findings from a Cross-Sectional Observation Study. Int. J. Behav. Med. 2017;24:908–914. doi: 10.1007/s12529-017-9649-0. [DOI] [PubMed] [Google Scholar]
- 57.Martins L.C.G., Lopes M.V.D., Diniz C.-M., Matos N.-C., Magalhaes L.-D., Furtado M.-A. Clinical indicators and aetiological factors of sedentary lifestyle in patients with arterial hypertension. J. Clin. Nurs. 2021;30:3330–3341. doi: 10.1111/jocn.15845. [DOI] [PubMed] [Google Scholar]
- 58.Guedes N.-G., Lopes M.-V., Araujo T.-L., Moreira R.-P., Martins L.-C. Predictive factors of the nursing diagnosis sedentary lifestyle in people with high blood pressure. Public Health Nurs. 2011;28:193–200. doi: 10.1111/j.1525-1446.2010.00902.x. [DOI] [PubMed] [Google Scholar]
- 59.Delfino L.-D., Tebar W.-R., Tebar F.C.S.G., DE Souza J.-M., Romanzini M., Fernandes R.-A., Christofaro D.G.D. Association between sedentary behavior, obesity and hypertension in public school teachers. Ind. Health. 2020;58:345–353. doi: 10.2486/indhealth.2019-0170. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.