Abstract
Background: Balance impairment causes frequent falls in older adults, and preventing falls remains challenging. Dual-task (DT) training reduces falls by improving balance, but the precise theory is not fully understood. This review aims to explore the theories underlying the effectiveness of DT in improving balance and reducing falls in older adults. Methods: Eleven electronic databases were searched from database inception to June 2022. Two reviewers independently performed study screening and data extraction. The risk of bias (RoB) in the included studies was assessed using the Cochrane Collaboration RoB 2 tool. Results: The searches yielded 1478 citations, of which 30 studies met the inclusion criteria and were included in the review. Twenty-two of the 30 included studies utilized the motor-cognitive type of DT for training, while six used motor-motor and two utilized cognitive–cognitive DT. The included studies reported 20 different theories to explain the effectiveness of DT for improving balance and reducing falls in older adults. The predominant theory identified in the included studies was attention theory (n = 14). Overall, 26 studies reported improved balance and five studies found a reduction in fall incidence following DT training. Balance and falls improved significantly in 15 motor-cognitive DT intervention studies. Conclusion: Attention shifting between two tasks is reported to occur following DT training. Motor-cognitive DT training improves balance and reduces fall incidence in older adults by shifting attention based on the difficulty and priority of a task from the motor to the cognitive task.
Keywords: motor cognitive interference, postural control, falls, older adults
1. Introduction
Globally, falls is the leading cause of unintentional death among older adults [1]. Moreover, falls is the 18th-leading cause of disability-adjusted life years in older adults [2,3]. Though the global incidence and prevalence of falls have dropped (by 3.7% and 6.5%, respectively) over the past two decades [4], managing falls remains a challenge among older adults. A common risk factor for falls is balance impairment [5]. One in five older Americans had balance impairment, and the condition was more common in women than in men [6]. One in four people with impaired balance has difficulty with daily activities [6]. Approximately 10% of falls result in fractures, which are also a significant source of morbidity and mortality in older adults [7,8]. Falls decrease quality of life and confidence, increase fear of falling, and limit functional ability and interpersonal interactions [9,10]. Even minor fall-related injuries are reported to cause pain, limited function, and high medical bills [7].
The causes of falls are multifactorial [11]. Poor balance is one of the crucial contributors and can result from white matter lesions in the brain that frequently lead to a decrease in multitasking activity [12,13,14,15]. White matter lesions have been linked to motor and cognitive dysfunction during multitasking, which degrades balance performance [15,16]. In multitasking, interference between two tasks reduces performance in one or both tasks [17], and this interference occurs between motor and cognitive tasks [18]. Thus, many studies [19,20] used dual-task (DT) paradigms to investigate how balance and cognition interact.
Over the past two decades, there has been a growing literature [21,22,23] on DT training, which entails the concurrent performance of a primary and a secondary task [19]. Initial attempts at performing DT are challenging, as it involves responding to two stimuli [24]: The primary task corresponds to the first delivered stimulus, whereas the secondary task corresponds to the second stimulus [24]. Secondary task response time is typically slower than that of the primary task [24]. This could be due to the longer processing time for initiating the secondary task [24]. With practice, the processing time of the secondary task shortens, and it becomes easier to perform DT [19]. The DT paradigm is relevant because most daily tasks require simultaneous cognitive and motor performance [19].
Researchers have proposed plausible, convincing, and credible theories to explain the theories by which DT training in a study might improve posture and attention, turning, gait, and gait inhibition [25,26,27]. According to attention theory, DT promotes balance by improving attention-shifting between two tasks [28]. In contrast, another theory hypothesized that the multicomponent training approach is useful for developing balance because it includes different exercises targeting different cognitive functions [29]. Proposed theories are effective because they enhance balance control in older adults [28,29,30].
This systematic review provides an overview of the theories that have been proposed to underlie the effectiveness of DT in improving balance and reducing falls in older adults in randomized control trials (RCTs). A previous review evaluated the theories underpinning motor-cognitive interference and balance and gait among healthy young adults [25]. A recent systematic review [31] identified DT training as an effective strategy for improving balance and reducing falls in older adults. However, to the best of our knowledge, there are no reviews exploring the theories underlying the effectiveness of DT training in improving balance and reducing falls among older adults. A better understanding of the underlying theories would benefit researchers by helping them plan appropriate interventional studies and informing clinical decision-making based on a summary of dosages reported in studies. Familiarity with the theories proposed in studies [32] to explain the association between balance impairment and older adults is important in the design of effective interventions using DT to prevent falls in this population. Thus, this review aims to explore the theories by which DT training improves balance and reduces falls among older adults.
2. Materials and Methods
This systematic review was developed and is reported in line with the PRISMA guidelines (see Appendix B, Table A4) [33]. The review was prospectively registered with PROSPERO (Ref No.: CRD42022315998; https://www.crd.york.ac.uk/prospero/#searchadvanced, accessed on 30 May 2022).
2.1. Search Process
Multiple electronic databases (PubMed, MEDLINE, Cochrane, CINAHL, Embase, Web of Science, Scopus, PsycInfo, PEDro, CNKI, and Wanfang) were searched from database inception until 27 June 2022. Hand searches were also conducted among the reference lists of the included studies. We constructed five search themes: DT, balance, fall, older adults, and RCT. Search terms were specific to each database. Appendix A Table A1 reports the search strategy for the PubMed database. The Boolean expression “OR” was used to combine relevant terms under each theme and “AND” was used to combine the five themes. Keywords in the searches used that did not match MeSH phrases. The root words “Posture” and “RCT” were truncated.
2.2. Eligibility Criteria
To be included, the studies had to (1) have included older adults (aged >60 years) without any pathological conditions; (2) have delivered DT as the intervention of interest; (3) have explained the underlying theory for the improvement of balance or reduction in falls following DT training; (4) be RCTs or pilot RCTs with a randomized cluster or cross-over design; (5) have utilized any of the following outcome measures for evaluating balance: Berg Balance Scale (BBS), Timed Up and Go (TUG), Community Balance and Mobility Scale (CB&M), one-leg stance (OLS), tandem test (TT), Romberg test (RT), Step Test (ST), Fullerton Advanced Balance (FAB), four square step test (FSST), Figure of 8 Walk Test (F8W), Frailty and Injuries Cooperative Studies of Intervention Techniques test (FICSIT-4), Y-balance test (Y-BT), Tinetti Balance Assessment Tool Balance Exercise (TBAT), Tinetti performance-oriented mobility score (TPOMA), and Functional Reach Test (FRT); and (6) utilize the number, percentage, and incidence rate ratio for evaluating falls. Unpublished theses were also included in the review. Studies were ineligible if they examined the combined effects of DT training with therapies such as dance, drugs, music, karate, tai chi, and brain stimulation because these interventions might interfere with the effect of DT training [34,35]. Studies with unavailable full text, study protocols, conference abstracts, and studies without reliable and valid scales used for balance measurement were excluded [36,37,38]. The validity of a scale was primarily defined by the sample of participants to ensure that the outcomes were applicable to a diverse array of demographics, cultures, and other contexts [39]. Studies published in languages other than English and Chinese were also excluded. The reliability of the scale was determined by the consistency of the outcome [39].
2.3. Data Extraction
Two independent reviewers screened titles, abstracts, and full texts. A third reviewer was consulted to resolve discrepancies between the reviewers. Data were extracted using a standard form. Extracted data included study characteristics, intervention types, dosage, treatment effects, and proposed theories.
2.4. Risk of Bias
The Cochrane Collaboration Risk of Bias (RoB 2) tool was used to assess bias [40]. The RoB 2 tool analyzes randomization, intervention deviations, missing outcome data, outcome measurement bias, and result reporting bias. Each question was answered with “yes”, “probably yes”, “probably no”, “no”, or “no information” [40]. The bias risk of each domain was rated as “low”, “some concerns”, or “high.” Similar to the individual domains, overall RoB 2 was also summarized as “low”, “some concerns”, or “high” risk of bias [40].
2.5. Statistical Analysis
We calculated the agreement between the two authors using the kappa value for the data screening process and quality appraisal. Values ≤ 0 indicated no agreement; 0.01–0.20 indicated no to little agreement; 0.21–0.40 indicated fair agreement; 0.41–0.60 indicated moderate agreement; 0.61–0.80 indicated substantial agreement; and 0.81–1.00 indicated nearly perfect agreement [41]. The RoB 2 tool was used to assess the bias and the methodological quality of specific results of RCTs. Since the focus of this review was to explore the theories, not the treatment effects, a quantitative analysis such as a meta-analysis or meta-regression was not considered necessary.
3. Results
3.1. Search Results
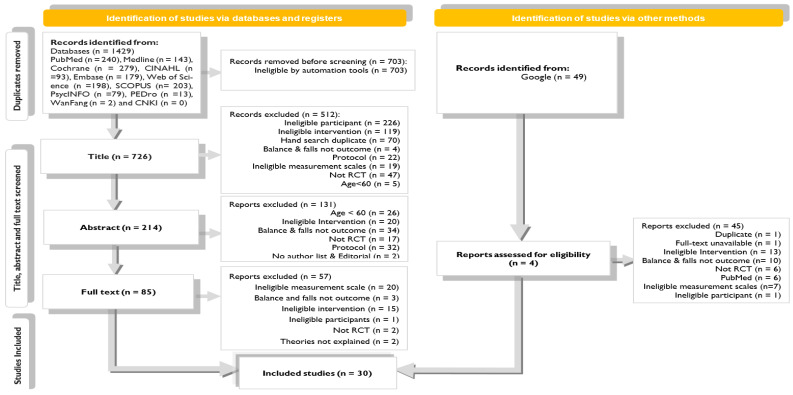
The electronic searches yielded 1478 potentially relevant studies. Figure 1 summarizes the flow of studies through the review. After a stepwise screening process, 32 studies were found to be eligible for review. Two studies [42,43] were excluded after screening for full text. Two studies were excluded as they did not report any theories for explaining the treatment benefits of DT training. Therefore, this review included 30 studies. The agreement between the two review authors was near perfect (0.92) for full-text screening. Studies excluded at the full-text screening stage and the reasons for exclusion are reported in Appendix A Table A2.
Figure 1.
Flowchart of study inclusion.
3.2. Risk of Bias
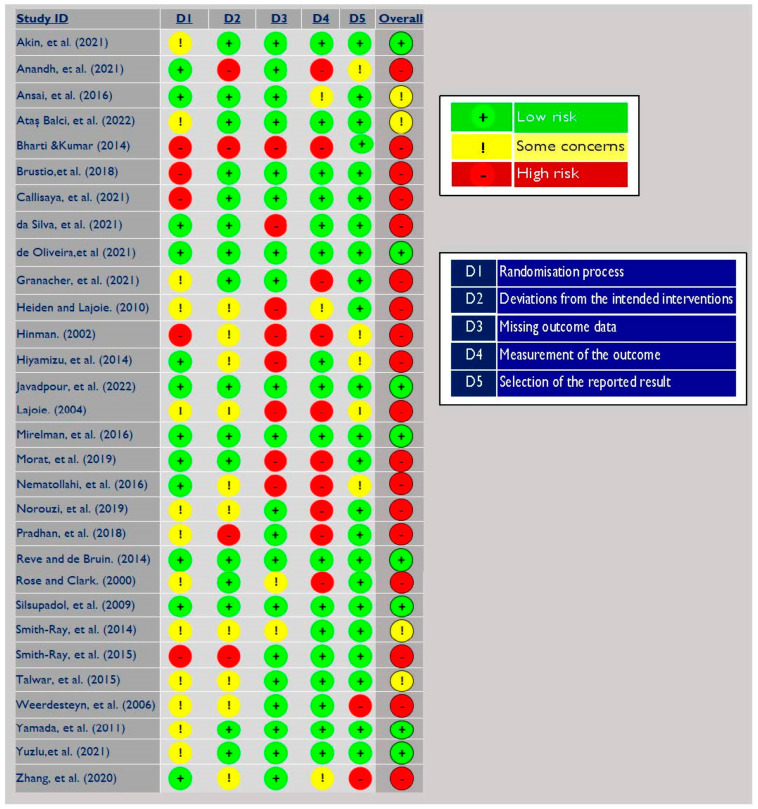
The findings of the RoB assessment are illustrated in Figure 2. Overall, there was a low to moderate RoB across more than 38.5% of the studies. Twenty-six percent (n = 8) of the included studies were at low risk of bias, while 12.5% (n = 4) of the studies drew “some concerns” about outcome measurement, randomization, and deviation from intended intervention. “High” RoB was identified in 60% of studies (n = 18). The major methodological flaws were identified in measuring outcomes [23,44,45,46,47], missing outcome data [29,48,49], or both [22,50,51,52,53]. For methodological flaws for measuring outcome, firstly, flaws resulted because there was insufficient information available about whether outcome assessors were aware of the intervention that study participants had received. Secondly, the influence of the knowledge of the intervention on the assessment was addressed inadequately. For missing outcome data, the studies were reported “no, possibly no, or no information” if either the missing data was not reported or the statistical analysis for handling the missing data was not clearly reported.
Figure 2.
Risk of bias analysis of the included studies [21,22,23,28,29,30,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67].
3.3. Characteristics of Included Studies
3.3.1. Types of Dual-Task Training
The DT interventions delivered in the included studies were (1) motor-cognitive, (2) motor-motor, or (3) cognitive–cognitive DT, as reported in Table 1. Among the 30 included studies, 22 studies [21,22,29,44,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63] used motor-cognitive DT training, 6 [23,28,30,45,59,64] used a motor-motor type of task, and 2 [65,66] included cognitive exercise in both tasks.
Table 1.
Dual-task training classification, definitions, and examples of exercises.
| DT Training/ Classification |
Definition | Exercise Reported in Trials |
|---|---|---|
| Motor-motor DT training | Exercise is assigned to retain postural control of the body by employing both motor and motor tasks simultaneously. | Walk and hold two half-filled glasses in both hands; Daily brushing with balance exercise |
| Motor-cognitive DT training | Exercise is intended to develop the abilities of posture control and executive function through the synchronous performance of one motor and one cognitive task. | Balance exercise with a verbal fluency task; Squire-stepping exercises in fixed-priority and variable-priority instruction |
| Cognitive–cognitive DT training | Exercise training with both cognitive tasks performed at the same time is intended to improve the executive function of the brain. | In a computer game, players see an animated truck and a road sign in the background before they fade away. Subsequently, two vehicles reappear to identify the correct vehicle. Meanwhile, a circle of cars appears around the edge, with one road sign. Participants need to find the location where the road sign first appeared on the edge. |
3.3.2. Types of Exercises
The demographics, types of DT interventions, treatment dosage, effectiveness, outcome measurement, authors’ conclusion, and theories of action proposed by the authors from the 30 included studies are reported in Table 2. Further detailed descriptions of the exercises, dosage of primary and secondary tasks, and control groups from the included studies are reported in Appendix A Table A3. Across the 30 included studies, different types of exercises were applied. Balance exercises appeared most frequently, as they were used in 12 studies [21,22,30,47,50,51,54,58,61,62,63,64]. Balance exercises were performed using free-hand, low-tech systems with minimal technology support or technology-dependent, computerized balance systems. Balance exercise combined with resistance exercise was performed in four additional studies [48,49,57,60].
Table 2.
Dual-task training and the proposed theory from all included trials.
| Authors/ Year |
Population/Gender/ Study Setting/ Country |
Mean Age/Age Range/Sample Size | Intervention (Dual-Task) | Assessment Time | Control | Effectiveness of Intervention | Authors Conclusions | Proposed Theory | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Primary Task | Secondary Task | Dosage | Total Time | Balance | Falls | |||||||
| (Rep/Minutes/Task/Load/Complexity/Administer) | (Duration/Week/Total) | (DT) | ||||||||||
| Akin et al. (2021) [28] | -/ 13 male & 19 female/ Laboratory/ Turkey |
67.72/ -/ 50 (Intervention G1: 25/Intervention G2: 25) |
G1: Motor training G2: Motor training (20 min/Administer: Physiotherapist) |
G1: Cognitive Training G2: Motor Training (20 min/Administer: Physiotherapist) |
40 min/ -/ 8 weeks |
20 min | Pre and post | Intervention: G1: ↑↑↑ BBS G2: ↑↑↑ BBS |
Both programs improved balance, fear of falling, walking, and muscle strength. | Attention theory | ||
| Anandh et al. (2021) [44] | Community dwellers /-/ Medical institute/ India |
-/ 65–75/ 96(-/-) |
G1: Motor training on regular surface G2 Motor training on uneven surfaces (15 min/Load: ↑/Administer: Physiotherapist) |
G1&G2: Cognitive training (15 min/Load: ↑/Administer: Physiotherapist) |
60 min/ -/ 1 year |
G1: 5 min G2: 10 min |
Intervention: G1&G2: ↑↑↑ TBAT |
Preventing secondary impairments Introduce progressive, safe, dual-task activities on even regular surfaces and multi-task conditions for further progression. | Attention theory | |||
| Ansai et al. (2016) [67] | Community dwellers/ 47 female and 22 male/ University/ Brazil |
82.4/ -/ 69 (Intervention G1: 23/Intervention G2: 23/Control: 23) |
G1: Motor training G2: Motor training (Repetation: 10–12/3 min/Load: ↑&↓/Physical educator) |
G1: Motor/cognitive Training (53 min/Load: ↑/Complexity: ↑/Administer: Physical educator) |
60 min/ 3 times/ 16 weeks |
Pre, post, and retention (6 weeks) | No intervention | Intervention and Control: ↑↑ OLS ↓↓ TT |
Intervention G1: ↓↓ frequency |
With higher adherence to protocol, multicomponent training is more effective and presents fewer adverse events. | Multicomponent training approach |
|
| Ataş Balci et al. (2022) [63] | Community dweller/ 39 female and 6 male/ University/Turkey |
73.0/ / 45(Intervention G1: 15/Intervention G1: 15/Control G3: 15) |
G1: Motor training G2: Motor training G3: Motor training (Minutes: ↑/Load: ↑/Complexity: ↑/Administer: Physiotherapist) |
G2: Cognitive training G3: Cognitive training (Successive) (Minutes: 30/Complexity: ↑/Administer: Physiotherapist) |
G1&G2: 30 min G3: 60 min/ 3 times/ 4 weeks |
30 min | Pre and post-test | G1: ↑↑↑ BBS G2: ↑↑↑ BBS G3: ↑↑↑ BBS |
Successive physical-cognitive training is more successful at improving balance and reducing fall fear in the elderly. | Capacity-sharing theory |
||
| Bharti &Kumar (2014) [53] | Residencial care dweller/ -/ India |
73.63/ -/ 30 (Intervention: 15/Control: 15) |
G1: Motor training G2: Motor training (Complexity: ↑) |
G1: Cognitive training (Variable priority) G2: Cognitive training (Fixed priority) |
45 min/ 3 times/ 4 weeks |
Pre and post-test | G1&G2: ↑↑ TPOMA | Balance of older adults improves after dual-task training with fixed and variable priorities. | Task coordination theory |
|||
| Brustio et al. (2018) [64] | Private senior social center/ 18 male & 42 female /-/ Italy |
73.5/ 70–80/ 60 (Intervention G1: 19, Intervention G2: 19/Control: 22) |
G1: Motor training (Repetition: 12/60 min/Complexity: ↑or↓) G2: Motor training (60 min/Complexity: ↑) |
G1: Motor training (31 min/Complexity: ↑) |
60 min/ 2 times/ 16 weeks |
31 min | Pre and post-test | Usual care | Intervention: G1: ↑↑↑ FSST G2: NS FSST Control: NS FSST |
Motor DT training incorporates motor extra activities and has the potential to improve mobility. | Attention theory | |
| Callisaya et al. (2021) [54] | Community dwellers &clinics/ 39 male & 54 female/ Home/ Australia |
72.8/ -/ 93 (Intervention: 17 and Control: 22) |
Motor training (Repetition: 3/40–120 min/Load: ↑/Complexity: ↑) |
Cognitive training (Repetition: 3/10–30 min/Load: ↑/Complexity: ↑) |
40–120 min/ weeks/ 24 weeks |
Pre and post test | No intervention | Intervention and Control: NS ↑↑ ST NS ↑↑ FICSIT-4 |
Trend towards enhanced gait speed. | Executive function theory Processing speed theory |
||
| da Silva et al. (2021) [29] | Community dweller/ 14 female and 2 male/ University clinic/ Brazil |
71.5/ -/ 16 (Intervention: 10/Control: 6) |
G1: Motor training G2: Motor training (Repetation: 12/40 min/Complexity: ↑or↓) |
G1: Cognitive (Repetation: 12/Complexity: ↑↓) |
-/ 3 times/ 6 weeks |
Pre, second and post-test | Intervention: G1&G2: ↑↑↑ F8W |
Hemodynamic stability, comprehension and adherence to interventions, increased mobility and frailty, static postural control, and dynamic balance. | Multicomponent training approach | |||
| de Oliveira et al. (2021) [55] | Community dweller/ -/ -/ Brazil |
68.3/ -/ 50 (Intervention: 25/Control: 25) |
Motor training (Repetation: 7–12/Load: ↑) |
Cognitive Training (Reputation: 1–5/Load: ↑) |
60 min/ 3 times/ 24 weeks |
Pre, second, and post | Motor training (Repetation: 7–12/Load: ↑) | Intervention: ↑↑↑ BBS Control: ↑↑ BBS |
SRT outcomes were better in the UST group, while C + UST resulted in greater gains in the TUG test. | Executive function theory Multicomponent training approach |
||
| Granacher et al. (2021) [45] | Community dweller/ 27 female and 24 male/Laboratory/Germany |
65.65/ 60–72/ 51(Intervention: 27/Control: 24) |
Motor training (3 min) |
Motor training (Load: ↑/Complexity: ↑) |
3 min/ 2 times/ daily/ 8 weeks |
336 min for 112 sessions |
Pre and post-test | No intervention | Intervention: ↑↑↑ TUG ↑↑↑ FRT ↓↓RT Control: ↓↓ TUG ↓↓ FRT ↓↓ RT |
Lifestyle balance training program during tooth brushing is insufficient to improve balance and muscle strength. | Attention theory | |
| Heiden, and Lajoie. (2010) [48] | Community dweller/ 11 female and 5 male/ -/ Canada |
77/ -/ 16(Intervention: 9/Control: 7) |
Motor training (30 min/Instructor) |
Cognitive training | 30 min/2 times/ 8 weeks |
Pre-post and retention test (2 weeks) | Motor training (60 m/ 2 times/ 8 weeks) |
Intervention: ↑↑↑ CB&M | Games-based balance biofeedback training significantly improves functional balance by reducing the attentional demands of postural control. | Attention theory | ||
| Hinman et al. (2002) [50] | Community dweller/Home and laboratory/55 female and 33 male/ USA |
72/ 63–87/ 88 (Intervention: 28/Intervention: 30/Control: 30) |
G1: Motor training (Complexity: ↑) G2: Motor training (10 min/ Load: ↓/Complexity: ↑) |
G2: Cognitive training | 20 min/ 3 times/ 4 weeks |
Pre and post | No intervention | Intervention: G2: ↑↑ BBS G1: ↑↑ BBS Control: ↑↑ BBS |
Greater degree of impaired participants who received intense training beyond 4 weeks mostly benefited. | Multicomponent training approach Low-tech approach. Whipple’s concentration approach. |
||
| Hiyamizu et al. (2012) [49] | Community dweller/ 26 female and 10 male/ Japan |
71.6/ -/ 43(Intervention: 21/Control: 22) |
Motor training (Administer: Therapist) |
Cognitive training | 60 min/ 2 times/ 12 weeks |
Pre and post | Motor training | Intervention and Control: NS ↑↑ TUG | Dual task balance training improves standing postural control in the elderly. | Working Memory model | ||
| Javadpour et al. (2022) [21] | Community dweller/ 49 female and 20 male /-/ Iran |
68.6/ 65–79/ 69(Intervention G1: 23 and G2: 23, and control: 23) |
G1: Motor training G2: Motor training (Administer: Physiotherapist) |
G2: Cognitive training | 40–60 min/ 3 times/ 6 weeks |
Pre and post | No intervention | InterventionG1&G2: ↑↑↑FAB Control: NS FAB |
Balance training enhance gait smoothness and balance in healthy older persons. | Working memory model Task oriented approach Goal oriented approach |
||
| Lajoie. (2004) [51] | Community dweller/ 20 female and 4 male s/-/ Canada |
70.85/ -/ 24 (Intervention: 12/Control: 12) |
Motor training (Repetatopn: 15/1 min/Complexity: ↑) |
Cognitive training | 60 min/ 2 times/ 8 weeks |
Pre, post and retention (2 weeks) | No intervention | Intervention: ↑↑↑ BBS Control: NS BBS |
↓↓% | Automaticity of maintaining a static posture increases significantly after postural training with feedback fading protocol. | Attention theory | |
| Mirelman et al. (2016) [56] | Community dweller/ 100 female &182 male/ Clinic/Belgium, Israel, Italy, Netherlands, and UK |
73.75/ 60–90/109 (Intervention: 52/Control: 57) |
Motor training (Load: ↑/Complexity: ↑) |
Cognitive training (Load: ↑/Complexity: ↑) |
45 min/ 3 times/ 6 weeks |
Pre, post and retention (24 weeks) | Motor training (45 min/ 3 times/ 6 weeks) |
↓↓↓ Incidence rate |
Treadmill with virtual reality training resulted in lower fall rates. | Integrated motor and cognitive theory | ||
| Morat et al. (2019) [52] | Community dweller/ 17 male and 28 female/ -/ Germany |
69.4/ -/ 45(Intervention G1: 15/Intervention G1: 15/Control: 15) |
G1: Motor training G2: Motor training (Load: ↑/Administer: Study assistant) |
G1: Cognitive Training (Unstable surface) G2: Cognitive Training (10–12 min//Study assistant) |
40 min/ 3/ 8 weeks |
Pre and post-test | Maintain a level of activity | Intervention: G1: ↑↑↑ Y-BT ↑↑↑TUG G2: ↑↑↑ Y-BT ↑↑ TUG Control: ↑↑ Y-BT ↓↓ TUG |
Under stable and unstable situations, volitional stepping exergames are an effective training method with excellent adherence rates for improving functional balance and calf strength. | Divided attention theory Selective attention theory Cognitive flexibility theory Working memory model |
||
| Nematollahi et al. (2016) [22] | Community dweller/ 12 male and 32 female/ -/ Iran |
66.4/ 60–70/ 57(Intervention G1: 19/Intervention G2: 19/Control: 19) |
G1: Motor training G2: Motor training G3: Motor training (55 min/Administer: Physiotherapist) |
G1: Cognitive training G2: Cognitive training (40 min/Administer: Physiotherapist) |
60 min/ 3 times/ 4 weeks |
Pre and post-test | Intervention and Control: ↑↑↑ FAB | Traditional, multisensory, and dual-task balance training is beneficial for improving balance, with no clear advantage over the others. | Attention theory | |||
| Norouzi et al. (2019) [23] | -/ 60 male/ 65–75/ Iran |
68.31/ -/60 (Intervention: 20/Intervention: 20/Control: 20) |
G1: Motor training G2: Motor training (Repetation: 8/60–80 min/Load: ↑/Physiotherapist) |
G1: Motor training (60–80 min/Physiotherapist) G2: Cognitive training |
60–80 min/ 3 times/ 4 weeks |
Pre, post, and retention (12 weeks) | Informal meeting+ Maintain physical activities+ Refrain from sports activities |
Intervention G1: ↑↑ BBS G2: ↑↑↑ BBS Control: ↓↑ BBS |
Working memory and balance performance improved more with mCdtt than with mMdtt. | Divided attention theory Attention theory Executive function theory Working memory model |
||
| Pradhan et al. (2018) [46] | Community dweller/ 18 male and 22 female/ -/ India |
69.75/ 65–75/ 40(Intervention: 20/Intervention: 20) |
Motor training (Load: ↑/Complexity: ↑) |
G1: Cognitive training (40 min/Complexity: ↑) |
45 min/ 3 times/ 4 weeks |
Pre and post test | Walk | Intervention: ↑↑↑ BBS and ↑↑↑ TUG Control: ↑↑↑ BBS & ↑↑↑ TUG |
Multiple-task exercises combined with cognitive tasks improve gait balance by keeping people awake and attentive while walking. | Attention theory | ||
| Reve and de Bruin (2014) [57] | Homes-for-the-aged and community dweller, vicinity homes/ -/Switzerland, Germany |
81.5/ -/ 182(Intervention: 94/Control: 88) |
G1: Motor training G2: Motor training (40 min/Load: ↑or↓) |
G2: Cognitive training | 40 min/ 2 times/ 12 weeks |
10 min/ 3 times/ weeks |
Pre, post and retention test (48 weeks) | ↓↓ % | DT costs of walking, gait initiation, and divided attention are reduced when strength-balance and cognitive training are combined. Strength-and-balance training enhances executive functioning lowering the risk of falling. | Executive function theory Divided attention theory |
||
| Rose, and Clark (2000) [47] | Community dweller/ 28 female and 13 male/Laboratory /USA |
78.7/ 72–85/ 45 (Intervention: 24/Control: 21) |
Motor training (Load: ↑/Complexity: ↑) |
Motor training (Load: ↑/Complexity: ↑) |
45 min/ 2 times/ 8 weeks |
Pre and post test | No intervention+ Not alter physical activities | Intervention: ↑↑ BBS ↑↑ TUG. Control: ↑↑ BBS ↑↑ TUG |
Theory-driven rehabilitation programs significantly improve the control of bodily orientation in both static and dynamic action environments. | Theory of perception and control body orientation. | ||
| Silsupadol et al. (2009) [58] | Community dwellers/ 18 female and 5 male/ Laboratory/ USA |
74.8/ 65–85/ 23 (Intervention G1: 8/Intervention G2: 8/Intervention G3: 7) |
G1: Motor training G2: Motor training G3: Motor training (Repetation: 4/12 min/Load: ↑/Complexity: ↑/Physiotherapist&2 Research assistance) |
G2 + G3: Cognitive training | 45 min/ 3 times/ 4 weeks |
Pre and post | InterventionG1,G2&G3: ↑↑ BBS | Improves balance in people with balance impairments. Single-task is unable to transfer to dual-task balance control. | Attention theory Divided attention theory Task integration model. Task-automation model |
|||
| Smith-Ray et al. (2014) [66] | Community dwellers/ 42 female and 4 male/ Community center/ USA |
72.47/ 66–79/ 45 (Interventon: 23 and Control: 22) |
Cognitive exercise (3 Computer games) | 60 min/ 2 times/ 10 weeks |
Pre and post-test | No intervention | Intervention: ↑↑↑ BBS Control: ↑↑ BBS |
Study presents preliminary evidence that cognitive training improves balance and mobility in older adults who have a history of falls. | Executive function theory Attention theory |
|||
| Smith-Ray et al. (2015) [65] | Independent living facilities/ 39 female &12 male /-/ USA |
81.9/ 75–88.3/ 53(Intervention: 27 and Control: 24) |
Cognitive exercise (3 Computer games) | 60 min/ 3 times/ 10 weeks |
IMPACT: 2400 min ACTIVE: 750 min |
Pre and post-test | 2 fall prevention brochures | Intervention: ↑↑↑ TUG Control: ↑↑↑ TUG |
Cognitive training is a potential method to fall prevention. | Executive function | ||
| Talwar et al. (2015) [59] | Old-age home/ -/-/ India |
76.4 65–89/60/(20 and Intervention: 20 and Intervention: 20) /(Intervention G1: 20 Intervention G2: 20 and Intervention G3: 20) |
G1: Motor training G2 + G3: Motor training (Complexity: ↑/Administer: Physiotherapist) |
G2: Motor training G3: Motor training |
60 min/ 3 times/ 4 weeks |
Pre and post-test | Intervention G1, G2&G3: ↑↑↑ BBS |
Agility training improves balance in people with balance problems. | Attention theory | |||
| Weerdesteyn et al. (2006) [30] | Community-dweller/ 82 female and 25 male/ Laboratory/ Netherlands |
73.93/ -/ (Intervention G1: 49/Intervention G2: 30/Control: 28) |
Motor training (1st and 2nd session) | Cognitive training (1st session) Motor training (2nd session) |
90 min/ 2 times/ 5 weeks |
Pre and post-test | No intervention | Intervention: ↓↓ IRR | Intervention was effective in reducing the incidence of falls. | Multicomponent training approach | ||
| Yamada et al. (2011) [60] | Community dweller/ 15 male and 38 female /-/ Japan |
80.8/ 67–97/ 53(Intervention G1: 26/Intervention G2: 27) |
G1: Motor training (Repetaion: 100/5 s/Load: ↑/Administer: Physiotherapist) G2: Motor training (Repetation: 100/10 s/Administer: Physiotherapist) |
G1: Cognitive training | 50 min/ 1 time/ 24 weeks |
Pre and post-test | Intervention G1&G2: ↓↓ TUG | Balance did not improve rather improving ambulatory function. | Attention theory | |||
| Yuzlu et al. (2021) [61] | Community dweller/ 11 male & 47 female/ Private institution/Turkey |
84.1/ -/ 58 (Intervention G1: 29 and Intervention G2: 29) |
G1: Motor training G2: Motor training (40 min/Load: ↑/Complexity: ↑/Administer: Physiotherapist) |
G1&G2: Cognitive training (G1: Combine &G2: Subsequently)(40 min/Complexity↑/Physiotherapist) | 60 min/2 times/ 8 weeks |
Pre and post-test | InterventionG1 and G2: ↑↑↑ BBS, ↑↑↑ TUG |
Integrated and consecutive DT balance training on balance and gait performance were not statistically significantly different. | Capacity-sharing theory Limited resource theory Task integration model. Task-automation model |
|||
| Zhang et al. (2020) [62] | Geriatric nursing home/ 12 male & 18 female/ -/China |
83.27 /-/ (Intervention: 15/Control: 15) |
Motor training (Complexity: ↑) |
Cognitive training (Complexity: ↑) |
30 min/ 5 times/ 6 weeks |
Pre &post test | Motor training | Intervention: ↑↑↑ TUG Control: ↑↑ TUG |
Significantly improve the stride length and cadence. The effect lasts longer and requires less energy. | Theory of reduced resources allocation Attention theory | ||
↑ = Increased, ↓ = Decreased, ↑↑ = Improved, ↓↓ = Reduced, ↑↑↑ = Significantly Improved, ↑↓ = Remain Same, - = Not Reported, NS = Non-significant. G1 = Group 1, G2 = Group 2, IMPACT = Cognitive Training Improvement in Memory with Plasticity-based Adaptive Cognitive Training, ACTIVE = Advanced for Independent and Vital Elderly, BBS = Berg Balance Scale, TUG = Timed Up and Go, CB&M = Community Balance and Mobility Scale, OLS = One leg stance, TT = Tandem test, RT = Romberg test, ST = Step test, FAB = Fullerton Advanced Balance, FSST = Four square step test, F8W = Figure of 8 Walk test, FICSIT-4 = Frailty and Injuries Cooperative Studies of Intervention Techniques test, Y-BT = Y-balance test, TBAT = Tinetti Balance Assessment Tool, Balance Exercis, TPOMA = Tinnetti Performances Oriented Mobility Score, FRT = Functional reach test.
3.3.3. Dosage of Dual-Task Training
Training sessions lasted between 3 [45] and 90 min [30] per session. Eleven studies [22,23,30,44,49,51,55,59,61,64,65,66,67] had 60 min or longer sessions. The frequency of training varied from once a week to every day and the length of training ranged from four weeks to a year [44,45,59,60]. Notably, in one study [45], twice-daily exercise lasted only three minutes. Only seven studies [28,44,45,57,63,64,65] reported the duration of the secondary task, and the highest duration noted was 30 min [63].
3.3.4. Study Comparator and Follow-Up
Thirteen of the 30 included studies [21,23,30,45,47,50,51,52,54,64,65,66,67] employed passive comparators instructing participants to either follow the fall prevention booklet (n = 1), continue with routine care (n = 3), or receive no intervention (n = 9). One study did not specifically report pre- and post-assessment time [44]. Six studies [23,43,48,51,56,57,58,59,60,61,62,63,64,65,66,67] included a follow-up assessment after the intervention phase, and the follow-up period ranged from 2 weeks [48,51] to 12 months [57].
3.3.5. Outcome Measures
Balance was assessed in 25 studies [21,22,23,28,29,44,45,46,47,48,49,50,52,53,54,55,58,59,60,61,62,63,64,65,66]. Almost 30% of the studies employed the BBS [23,28,50,51,55,58,59,63,66], while six [45,49,52,60,62,65] used the TUG scale, and both scales were utilized in three studies [46,47,61]. Three studies [30,56,57] examined falls and reported the data as a percentage [57] or incidence rate ratio [30,56]. Both outcomes, balance and falls, were measured in two studies [51,67].
3.3.6. Treatment Effects
Twenty-three (76.6%) [21,22,23,28,29,44,45,46,47,48,50,51,52,53,55,58,59,61,62,63,64,65,66] of the 30 included studies reported improvement in balance after DT training, while 5 (17.8%) [30,51,56,57,67] reported a reduction in the number of falls. Seventeen (63%) [21,22,28,29,44,46,48,51,52,55,59,61,62,63,64,65,66] out of 27 studies found significant improvement in balance measured using the BBS, TUG, TBAT, FAB, FSST, F8W, FRT, CM&M, FR, or Y-BT scales and 1 (20%) [56] out of 5 studies reported significant improvement in falls using the incidence rate ratio. Fifteen motor-cognitive training studies [21,22,23,28,29,44,46,48,51,52,55,61,62,63,64] demonstrated significant balance improvement after DT training, whereas three [28,59,64] out of six [23,28,45,47,59,64] studies using motor-motor and two studies using cognitive–cognitive [65,66] types of training demonstrated significant balance improvement as assessed using the BBS, TBAT, F8W, CB&M, FR, T-BT, TUG, FSST, and FRT scales.
3.3.7. Theories Reported in the Included Studies
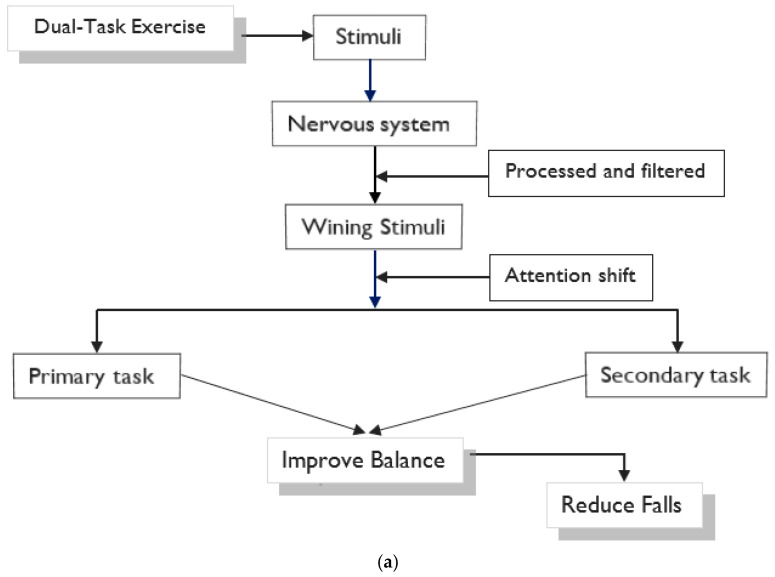
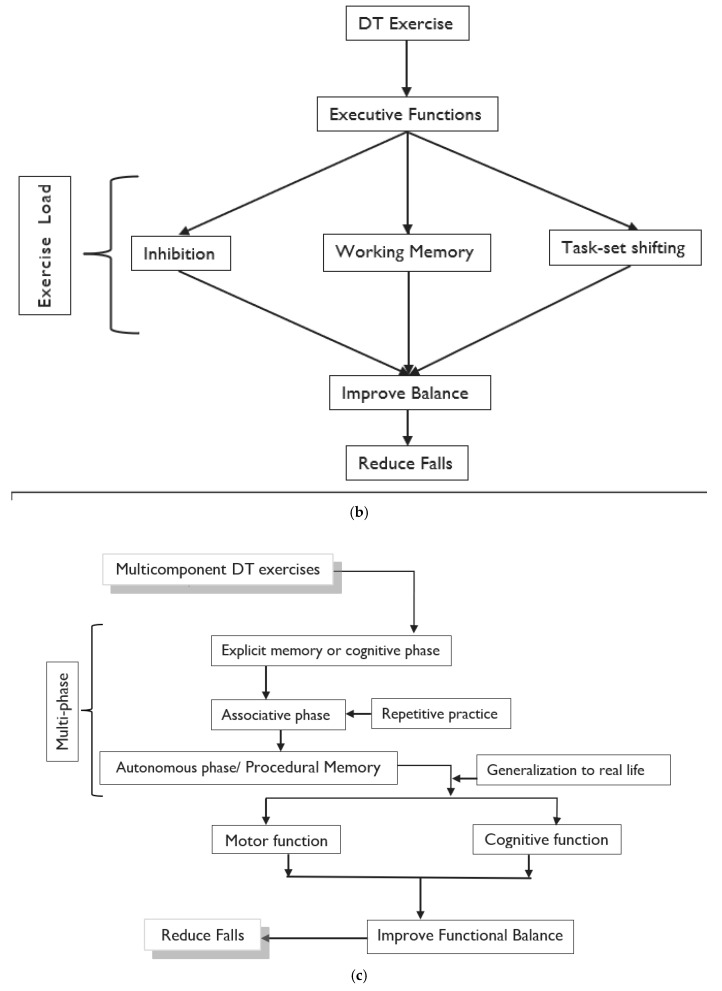
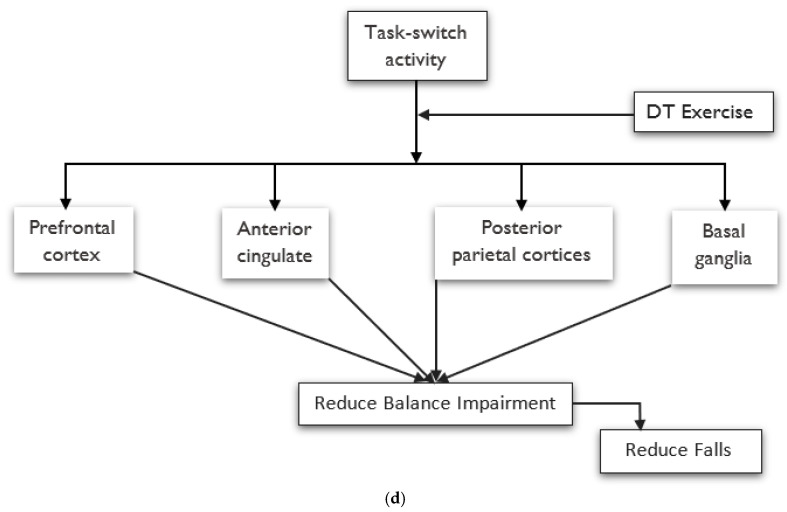
Among the 30 included studies, 20 different theories to explain balance improvement following DT interventions were identified. A single theory was documented in 19 studies [22,28,29,30,44,45,46,47,48,49,51,53,56,59,60,63,64,65,67]. More than one theory was reported in 12 studies [21,23,50,52,54,55,56,57,58,61,62,66], and of these, four studies [23,52,58,61] reported four theories. The attention theory was proposed to explain the improvement in balance and reduction in falls following the DT intervention in 14 studies [22,23,28,44,45,46,48,51,58,59,60,62,64,66]. The predominant theory invoked was the competition theory of attention, which was used in over a third [22,28,44,45,46,48,51,58,59,60,64] of all studies primarily (explained first, either alone or along with other theories) and in three studies secondarily (not explained as a primary theory, but presented along with other theories) [23,62,66]. The competition theory of attention has been extensively proposed as an underlying theory to explain improving balance, mostly in the application of motor-cognitive and motor-motor types of DT training. Figure 3a illustrates the pathway for improvement in balance following DT intervention using the attention theory model. In this model, the attention of the brain responds to a winning stimulus from multiple competing stimuli. In the context of DT, for example, the winning stimulus of the calculation or cognitive task draws attention during the balancing exercise or motor task. This shifting attention works to improve motor-cognitive capabilities, which contributes significantly to the improvement in balance. DT theories commonly suggested to improve balance were executive function in six studies [23,54,55,57,65,66] and a multicomponent training approach in five studies [29,30,50,55,67]. The executive function theory focuses on enhancing cognition to improve balance by loading on inhibiting, updating working memory, and task-set shifting [68], as illustrated in Figure 3b, while multicomponent theories targeting procedural memory work via multi-phase cognitive functions to improve balance [69,70], as shown in Figure 3c. The working memory model was invoked as a primary [21,49] or secondary theory [23,52] in two studies each. The working memory model focuses on neural efficacy to improve balance via the management of multiple task processes [23,71], as described in Figure 3d. Likewise, the divided attention theory, which focuses on rapidly shifting or splitting attentional focus between two tasks, was referred to as a primary [23,52] or secondary theory [23,52,57,58] in two and four studies, respectively.
Figure 3.
(a) Concept of neurophysiological phenomenon of attention theory for DT intervention; (b) Concept of executive function approach in application of DT Intervention; (c) Concept of Multicomponent Training Approach of DT Intervention; (d) Concept of Working Memory Model in Application of DT Intervention.
4. Discussion
To the best of our knowledge, this is the first systematic review to summarize the possible theories underlying the effectiveness of DT interventions for improving balance and reducing falls in older adults. Identifying the spectrum of theories proposed by authors underlying the improvement of balance following DT was the objective of this review. Interestingly we found there were at least 20 theories explaining the improvement following the intervention. We notice that most of the studies reported more than one theory for the identified benefits. This is an indication that DT results in the improvement of multiple domains such as attention, procedural memory executive function and motor function.
The 30 included studies, filtered from a total of 1478 studies identified via database searches, proposed 20 distinct DT theories. These proposed theories were reported to explain the improvement in balance (n = 26) and the reduction in the number of falls (n = 5) following DT intervention among healthy older adults. The most frequently proposed theory was the competition theory of attention, which describes the shifting of attention from one task to a secondary task with DT practice. The DT interventions improved both motor and cognitive function compared to various controls.
The competition theory of attention was used to describe the improvement in balance and reduction in falls following DT training; it was cited primarily in 11 studies (36.7%) and secondarily in three additional studies (10%). This theory is derived from the definition of attention first proposed by William James in 1890 [72] and involves the central nervous system, where neurons are subjected to a wide range of internal and external stimuli at any given instance. Each stimulus competes for the attention of the nervous system [73]. The nervous system filters the stimuli by considering the challenges and attending to the prioritized task [74]. Based on the difficulty and priority of a task, attention shifts from one task to another. For instance, when an individual is sitting on an inflatable exercise ball and catching a tennis ball simultaneously, attention needs to shift from catching the tennis ball to sitting on the inflatable exercise ball to ensure the safety of the user. The attention theory was used to explain balance improvement, as the participants were able to attend to two simultaneous tasks efficiently with repeated practice, and the number of falls was reduced due to their capacity to increase their multi-tasking ability. Talwer et al. [59] delivered a square stepping exercise that involved switching one’s attention while passing a ball under variable priority instructions. The significant difference in balance measurement after training revealed that gradual practice decreases the reaction time of passing balls [59].
The competition theory of attention led to the development of the divided attention theory and the selective attention theory. These theories are mentioned in four studies [23,52,57,58]. The divided attention concept addresses the limitations of multitasking in information processing. The inability to process all information simultaneously demands division of attention, which splits or rapidly switches the attentional focus [75]. DT results in enhanced divided attention with the use of optimal attention resources in motor control [19]. This enables splitting attention between the primary and secondary tasks, which improves the outcomes of the functional task. The selective attention theory explains how multiple dynamic events and static sources of input are filtered and subsequently perceived, cognitively processed, and ultimately responded to [76,77]. Balance is considered a dynamic event [78], and the motor-cognitive DT interventions were intended to improve multiple dynamic events, including balance [78]. This intervention promotes parallel information processing and manipulating information [76]. Selective attention to task-relevant inputs and decision-making about balance performance leads to balance improvement [78,79]. One study [52] reported that motor-cognitive DT intervention was effective in improving balance and invoked the theories of both the divided and the selective attention theories as an explanation. Three more studies invoked the divided attention theory as an explanation for the improvement in balance [23,58] and reduction in falls [57] following DT intervention.
The multicomponent or multimodal training approach was proposed to explain the reduction in fall incidence following DT intervention in five studies [29,30,50,55,67]. This theory emphasizes that the DT intervention could activate procedural memory, which in turn enhances cognitive function [70]. Procedural memory is crucial for activities of daily life [80] and plays a role in multi-phase motor and cognitive functions. Simultaneous activity of the striatum and caudate nucleus improves procedural memory, targeting both motor and cognitive functions in one training program [69]. Thus, a multicomponent training program is appropriate for procedural memory improvement [70]. Based on this theory, the DT interventions are hypothesized to improve cognitive function, attention, cognitive control, memory, reasoning, and executive functions simultaneously [67,70]. Multiphase-based DT intervention improves specific functions by targeting balance through repeated exercises [81]. Repeated processes enhance cognitive function, improve balance [29], and reduce the number of falls [30] in older adults. One study [67] examined both outcomes and found reduced falls, but not improved balance for tandem scale. This may be because this study used the infrequently tandem balance measurement scales, which are not appropriate tests for aging participants (mean age of 81.9 years).
The executive function theory was reported in six studies [23,54,55,57,65,66]. It covers a spectrum of three key cognitive processes for improving balance by enhancing cognition: increasing the load on task inhibition, updating working memory, and task-set shifting [68,82]. Improvement is achieved through motor-cognitive DT training, DT exercise increases the load on inhibiting primary tasks or motor tasks, updates it on the working memory, and eases the motor-to-cognitive task switching [54,68]. Together, they improved executive function, which improved balance and reduced falls. Four studies [23,55,65,66] used this theory to explain an improvement in balance, while one study used it to explain a reduction in falls [57] following DT intervention in older adults.
Two additional theories based on the executive function theory have been proposed to explain how the motor-cognitive type of DT training helps to improve balance: the working memory model and the cognitive flexibility theory.
Cognitive flexibility theory explains the ability to spontaneously rearrange information in an adaptive response to substantially altering situational demands [83]. Task-switching activities, including DT, require cognitive flexibility [84]. This flexibility is achieved in DT exercises, which activate the prefrontal, anterior cingulate, and posterior parietal cortices and basal ganglia, enhancing cognitive flexibility [84]. This theory was proposed in one study [52] that demonstrated substantial improvement in balance after DT training.
Working memory is necessary for complex task processes, including reasoning, comprehension, and learning [71]. The working memory model was proposed to explain the results in four different studies [21,23,49,52]. Balance improvement occurred due to the neuronal efficacy resulting from the motor-cognitive DT training, which is responsible for comprehensive learning via amplifying cognition [23].
Six theories in three studies explained how DT performance improves balance and reduces falls. In one study [58], the following three theories were described: (1) a task-oriented approach emphasized improving balance or movement strategies within a given environment using motor-cognitive exercise [85,86]; (2) a task-automation model led to complete task automation [87]; and (3) a task integration model introduced effective integration of two tasks, minimizing the sharing capacity to improve DT performance [87]. These three models propose that balance is enhanced by automating one of the two DT exercises. Silsupadol et al. combined one of the previously automated tasks into fixed or variable priority instruction, with balance as the primary task and cognitive task training as the secondary task [58]. This increased the balance function in older adults with repeated practice.
In addition to the theories described above [58], three studies proposed the integrated motor and cognitive theory, the theory of reduced resources, the capacity-sharing theory, and the limited resource theory to explain the balance improvement following DT intervention. One study [56] evaluating the advantages of motor-cognitive DT training invoked an integrated motor and cognitive theory to explain the theory of fall reduction. According to this theory, motor, cognitive, and physical development are all influenced by the biological predispositions that are most necessary for safe movement [88]. Similarly, motor-cognitive DT aims to enhance balance and reduce falls in both domains. Mirelman et al. postulated that combining a treadmill exercise with a cognitive exercise would mitigate fall risk significantly during the six months after training [56]. Integrated DT allows tasks to become habitual and minimizes competition to improve balance.
The reduced resource theory explains that the repetitions in DT training increase cognitive capacity, which in turn improves balance [62]. The task coordination theory describes the coordination and management of DT performance to optimize stability during the performance of concurrent tasks [89]. The capacity-sharing theory states that effective DT integration promotes DT performance by sharing brain resources between tasks [90,91]. In other words, sharing capacity improves through task integration, as brain resources are shared between two tasks, resulting in better DT performance [90]. According to the limited resource theory, the tasks in DT training compete for limited neural resources [91]. After performing the DT exercise, DT performance improves because each task becomes automatic and competition reduces [91]. Thus, complex motor-cognitive training makes tasks automatic and less competitive, thereby improving balance control in older adults [61].
5. Implications
The findings of this review provides a better understanding of the underlying theories for improvement following DT training. Our Table 2 reports a summary of the type of exercise, dosage of intervention, outcomes on balance and falls reduction and the proposed theory underlying the improvement. These findings benefit researchers by helping them to plan future intervention studies that could bridge the literature gap such as including cognitive–cognitive DT exercises and for the clinicians, these findings will assist in making a clear choice on the type and dosage of DT intervention for achieving specific health benefit among the older adults.
This review has several limitations. (1) Most of the studies did not mention the repetition and allocated time for DT separately (i.e., the dosage for the primary and secondary tasks). The load and complexity of the exercise, as well as the clinician’s skills, are key to achieving a successful outcome from intervention; however, they were addressed inadequately in the included studies. Future RCTs should address these inadequacies appropriately. (2) Our included studies were restricted to English and Chinese language publications; therefore, it is possible that potentially relevant studies [92,93] were not considered. (3) The findings of this study must be interpreted with caution due to the heterogeneity in participant characteristics, study methods, type of DT intervention, outcome measures used, dosage of intervention, study setting and mode of intervention delivery. (4) More than half (60%) of the studies were classified as having poor methodological quality, and as quality impacts the study results, this must be considered when interpreting the findings. (5) Not all RCTs necessarily support the theories. Among the potential studies for inclusion, two studies [42,43] that did not record an improvement in balance or fall reduction did not report a theory to support and therefore they were excluded in the full-text screening stage. In addition, one study [60], though did not record an improvement mentioned a theory for supporting the benefits of the intervention. (6) We restricted studies among healthy older adults without pathological conditions and therefore generalizing these findings to all older adults is limited. Future reviews are warranted to study special groups of older adults with pathological conditions and (7) we did not attempt to explore the reasons for improvement among the studies that did not report the theory (n = 2). This strategy is in line with our review protocol. This review also has the following merits: (1) extensive searches for relevant studies were performed across 11 databases using a systematic methodology and (2) since this review exclusively included RCTs, our conclusions are based on high-quality evidence.
6. Conclusions
This review identified 20 possible theories to explain the improvement in balance and reduction in falls following DT training among older adults. The dominant theory invoked to explain the effectiveness of DT training was the attention theory, which is commonly proposed in motor-cognitive DT studies. In motor-cognitive DT training, attention is shifted based on the complexity and priority of a task from the motor to the cognitive task to improve balance and reduce falls incidence among older adults.
Acknowledgments
The work of MJK is assisted by the Hong Kong Polytechnic University Research Postgraduate Scholarship (PRPgS) for PhD study. We thanked Tse Yu Sun Jason and Cheng Ho Kwan for help with data entry for the Chinese database.
Appendix A
Table A1.
Search terms and search strategy for PubMed.
| General Search Terms | ||
|---|---|---|
| Themes | Subject Areas | Search Terms Used (Each Term within Criteria Combined with Boolean Operator ‘OR’) |
| Population | Older | ((older adult) OR (elderly) OR (senior) OR (older) OR (aged)) |
| Intervention | Dual—task AND | ((dual—task) OR (dual task) OR (cognitive motor interference) OR (psychomotor performance) OR (concurrent task) OR (dual task paradigm) OR (attention-demanding task) OR (divided attention)) |
| Outcome | Balance AND | ((balance) OR (equilibrium) OR (posture) OR (postur*) OR (postural control) OR (postural stability) OR (postural balance) OR (postural sway) OR (sway) OR (center of pressure) OR (center of mass) OR (posture equilibrium)) |
| Fall AND | ((fall) OR (falling) OR (falls) OR (falls, accidental) OR (fall, accidental) OR (slip and fall) OR (fall and slip)) | |
| Study type | Randomize control trial | ((Randomized controlled trial) OR (Randomized allocation) OR (Random*) OR (Clinical trial)) |
Table A2.
Reasons for excluded study after full-text reading.
| Studies | Exclusion Regions |
|---|---|
| [94,95,96,97] | Age < 60 years (n = 4) |
| [98,99,100] | Balance and falls not outcome (n = 3) |
| [101,102,103,104,105,106,107,108,109,110,111,112,113,114,115] | Ineligible intervention (n = 15) |
| [116,117,118,119,120,121,122,123,124,125] | Unavailable full text (n = 10) |
| [126,127] | Not RCT (n = 2) |
| [128] | Ineligible participants (n = 1) |
| [129,130,131,132,133,134,135,136,137,138,139,140,141,142,143,144,145,146,147,148] | Ineligible measurement scale (n = 20) |
Table A3.
Details of the DT training and control.
| Authors/Year | Primary Task | Secondary Task | Control |
|---|---|---|---|
| Akin, et al. (2021) [28] | G1: Aerobic Exercise + Stretching Exercise G2: Walk + Aerobic Exercise + Stretching Exercises |
G1: Verbal fluency task G2: Half-filled glasses with both hands near the trunk, while the elbows were at 90° flexion. |
|
| Anandh, et al. (2021) [44] | G1: Aerobic Exercise + Activity of daily living on regular surface G2 Aerobic Exercise + Activity of daily living on uneven surfaces |
G1&G2: Cognitive Training | |
| Ansai, et al. (2016) [67] | G1: Aerobic Exercise + Stretching Exercise + Balance Exercise (15 min/Load: ↑Administer: Physical Educator) G2: Resistance Exercise |
G1: Static & dynamic balance /cognitive Training | No intervention |
| Ataş Balci, et al. (2022) [63] | G1: Static and Dynamic Balance Exercise G2: Static and Dynamic Balance Exercise G3: Static and Dynamic Balance Exercise |
G2: Visual attention Tasks + Auditory attention tasks + Planning tasks + Verbal fluency task + Simple mental math G3: Visual attention Tasks + Auditory attention tasks + Planning tasks + Verbal fluency task + Simple mental math (Successively) |
|
| Bharti &Kumar (2014) [53] | G1: Stance Activities + Gait Activities G2: Stance Activities + Gait Activities |
G1: Simple math + Auditory task + Visual tasks (Fixed priority Instruction) G2: Simple math + Auditory task + Visual tasks (Variable priority Instruction) |
|
| Brustio, et al. (2018) [64] | G1: Warmup + Balance Exercise + Walk + Cool down G2: Warmup + Balance Exercise + Walk + Cool down |
G1: Activity of daily life | Usual care |
| Callisaya, et al. (2021) [54] | Balance Exercise + Stretching Exercise | Recall & memory task + step up & over mixed | No intervention |
| da Silva, et al. (2021) [29] | G1: Resistance Exercise + Balance Exercise G2: Active Exercise + Stretching Exercise |
G1: Verbal flueny + simple mathmatics + Recall tasks | |
| de Oliveira, et al. (2021) [55] | Resistance Exercise | Verbal fluency + Recall & memory task | Resistance Exercise |
| Granacher, et al. (2021) [45] | Daily brushing | Balance Exercise | No intervention |
| Heiden & Lajoie, (2010) [48] | Resistance Exercise + Stretching Exercise + Balance Exercise | Computer game | Resistance Exercise + Stretching Exercise |
| Hinman, et al. (2002) [50] | G1: Balance Exercise G2: Balance Exercise |
G2: Computer game | No intervention |
| Hiyamizu et al. (2012) [49] | Resistance Exercise + Balance Exercise + Walking | Visul + verbal task | strength and balance exercise |
| Javadpour, et al. (2022) [21] | G1: Balance exercise G2: Balance exercise |
G2: Verbal fluency task | No intervention |
| Lajoie (2004) [51] | Balance Exercise | Verbal fluency task | No intervention |
| Mirelman, et al. (2016) [56] | Treadmill training | Virtual reality: Obstacle negotiation | Treadmill training |
| Morat, et al. (2019) [52] | G1: Exergame G2: Exergame under unstable condition |
G2: stepping exergames | Maintain a level of activity |
| Nematollahi, et al. (2016) [22] | G1: Warmup + Balance Exercise + Cool down G2: Warmup + Balance Exercise + Cool down G3: Warmup + Postural task + Cool down |
G1: Sensory, vision & vestibuler manipulation G2: Verbal fluency task + Simple mathmatics |
|
| Norouzi, et al. (2019) [23] | G1: Resistance Exercise G2: Resistance Exercise |
G1: Throwing a ball up and down, throwing a bag + Holding a bag + Balancing the cup on the palm of the hand + Holding a medicine ball in both hands G2: Visual taks + Simple arithmetic + Verbal fluency task |
Informal meeting+ Maintain physical activities+ Refrain from sports activities |
| Pradhan, et al. (2018) [46] | Walk | G1: Simple arithmatics | Walk |
| Reve and de Bruin (2014) [57] | G1: Resistance Exercise + Balance Exercise + Stretching Exercise G2: Resistance Exercise + Balance Exercise + Stretching Exercise |
G2: Computer game | |
| Rose, and Clark (2000) [47] | Balance exercise | Eyes open & close + fixed support surface | No intervention+ Not alter physical activities |
| Silsupadol, et al. (2009) [58] | G1: Balance Exercise G2: Balance Exercise + Variable priority instruction G3: Balance Exercise + Fixed Priority instruction |
G2 + G3: Working Memory | |
| Smith-Ray, et al. (2014) [66] | Cognitive exercise (3 Computer games) (Administer: Research assistant) |
No intervention | |
| Smith-Ray et al. (2015) [65] | Cognitive exercise (3 Computer games) | 2 fall prevention brochures | |
| Talwar, et al. (2015) [59] | G1: Square-stepping exercise (Repetition: 2–16) G2 + G3: Agility traiing Exercise |
G2 + G3: Passing the Ball (G2: Fixed Priority and G3: Variable priority) | |
| Weerdesteyn, et al. (2006) [30] | Balance Exercise + Walk (1st session) Walk + Fall techniques (2nd session) |
Carrying a tray with empty cups + carrying grocery bags or an umbrella (1st session) Simulated crowed (2nd session) |
No intervention |
| Yamada, et al. (2011) [60] | G1: Active Exercise + Resistance Exercise + Balance Exercise G2: Active Exercise + Resistance Exercise + Balance Exercise |
G1: Verbal fluency task | |
| Yuzlu, et al. (2021) [61] | G1: Balance Exercise G2: Balance Exercise |
G1&G2: Recall and memory task + Simmple arithmmic + Verbal fluency task (G1: Combine &G2: Subsequently) | |
| Zhang, et al. (2020) [62] | Dynamic coordination exercise | Cognitive Training | Conventional exercise+ Stretching+ Massages |
Appendix B
Table A4.
PRISMA checklist.
| Section and Topic | Item # | Checklist Item | Location Where Item Is Reported |
|---|---|---|---|
| Title | |||
| Title | 1 | Identify the report as a systematic review. | 1 |
| Abstract | |||
| Abstract | 2 | See the PRISMA 2020 for Abstracts checklist. | 1 |
| Introduction | |||
| Rationale | 3 | Describe the rationale for the review in the context of existing knowledge. | 2 |
| Objectives | 4 | Provide an explicit statement of the objective(s) or question(s) the review addresses. | 2 |
| Methods | |||
| Eligibility criteria | 5 | Specify the inclusion and exclusion criteria for the review and how studies were grouped for the syntheses. | 2 |
| Information sources | 6 | Specify all databases, registers, websites, organisations, reference lists and other sources searched or consulted to identify studies. Specify the date when each source was last searched or consulted. | 2 |
| Search strategy | 7 | Present the full search strategies for all databases, registers and websites, including any filters and limits used. | 2 |
| Selection process | 8 | Specify the methods used to decide whether a study met the inclusion criteria of the review, including how many reviewers screened each record and each report retrieved, whether they worked independently, and if applicable, details of automation tools used in the process. | 2, 3 |
| Data collection process | 9 | Specify the methods used to collect data from reports, including how many reviewers collected data from each report, whether they worked independently, any processes for obtaining or confirming data from study investigators, and if applicable, details of automation tools used in the process. | 3 |
| Data items | 10a | List and define all outcomes for which data were sought. Specify whether all results that were compatible with each outcome domain in each study were sought (e.g., for all measures, time points, analyses), and if not, the methods used to decide which results to collect. | 3 |
| 10b | List and define all other variables for which data were sought (e.g., participant and intervention characteristics, funding sources). Describe any assumptions made about any missing or unclear information. | N/A | |
| Study risk of bias assessment | 11 | Specify the methods used to assess risk of bias in the included studies, including details of the tool(s) used, how many reviewers assessed each study and whether they worked independently, and if applicable, details of automation tools used in the process. | 5 |
| Effect measures | 12 | Specify for each outcome the effect measure(s) (e.g., risk ratio, mean difference) used in the synthesis or presentation of results. | N/A |
| Synthesis methods | 13a | Describe the processes used to decide which studies were eligible for each synthesis (e.g., tabulating the study intervention characteristics and comparing against the planned groups for each synthesis (item #5)). | 6 |
| 13b | Describe any methods required to prepare the data for presentation or synthesis, such as handling of missing summary statistics, or data conversions. | N/A | |
| 13c | Describe any methods used to tabulate or visually display results of individual studies and syntheses. | N/A | |
| 13d | Describe any methods used to synthesize results and provide a rationale for the choice(s). If meta-analysis was performed, describe the model(s), method(s) to identify the presence and extent of statistical heterogeneity, and software package(s) used. | N/A | |
| 13e | Describe any methods used to explore possible causes of heterogeneity among study results (e.g., subgroup analysis, meta-regression). | N/A | |
| 13f | Describe any sensitivity analyses conducted to assess robustness of the synthesized results. | N/A | |
| Reporting bias assessment | 14 | Describe any methods used to assess risk of bias due to missing results in a synthesis (arising from reporting biases). | N/A |
| Certainty assessment | 15 | Describe any methods used to assess certainty (or confidence) in the body of evidence for an outcome. | N/A |
| Results | |||
| Study selection | 16a | Describe the results of the search and selection process, from the number of records identified in the search to the number of studies included in the review, ideally using a flow diagram. | 13 |
| 16b | Cite studies that might appear to meet the inclusion criteria, but which were excluded, and explain why they were excluded. | 21 | |
| Study characteristics | 17 | Cite each included study and present its characteristics. | 6 |
| Risk of bias in studies | 18 | Present assessments of risk of bias for each included study. | 6 |
| Results of individual studies | 19 | For all outcomes, present, for each study: (a) summary statistics for each group (where appropriate) and (b) an effect estimate and its precision (e.g., confidence/credible interval), ideally using structured tables or plots. | N/A |
| Results of syntheses | 20a | For each synthesis, briefly summarise the characteristics and risk of bias among contributing studies. | 4 |
| 20b | Present results of all statistical syntheses conducted. If meta-analysis was done, present for each the summary estimate and its precision (e.g., confidence/credible interval) and measures of statistical heterogeneity. If comparing groups, describe the direction of the effect. | N/A | |
| 20c | Present results of all investigations of possible causes of heterogeneity among study results. | N/A | |
| 20d | Present results of all sensitivity analyses conducted to assess the robustness of the synthesized results. | N/A | |
| Reporting biases | 21 | Present assessments of risk of bias due to missing results (arising from reporting biases) for each synthesis assessed. | N/A |
| Certainty of evidence | 22 | Present assessments of certainty (or confidence) in the body of evidence for each outcome assessed. | N/A |
| Discussion | |||
| Discussion | 23a | Provide a general interpretation of the results in the context of other evidence. | 17 |
| 23b | Discuss any limitations of the evidence included in the review. | 19 | |
| 23c | Discuss any limitations of the review processes used. | 19 | |
| 23d | Discuss implications of the results for practice, policy, and future research. | 19 | |
| Other Information | |||
| Registration and protocol | 24a | Provide registration information for the review, including register name and registration number, or state that the review was not registered. | 2 |
| 24b | Indicate where the review protocol can be accessed, or state that a protocol was not prepared. | 2 | |
| 24c | Describe and explain any amendments to information provided at registration or in the protocol. | N/A | |
| Support | 25 | Describe sources of financial or non-financial support for the review, and the role of the funders or sponsors in the review. | 19 |
| Competing interests | 26 | Declare any competing interests of review authors. | 19 |
| Availability of data, code and other materials | 27 | Report which of the following are publicly available and where they can be found: template data collection forms; data extracted from included studies; data used for all analyses; analytic code; any other materials used in the review. | 19 |
Author Contributions
M.J.K. designed the research, performed the data extraction, visualization, and drafted the manuscript. P.K. supervised and aiding designing the research, and critically reviewed and S.J.W. supervised, critically reviewed, edited and revised the manuscript. T.W.-L.W. and K.N.K.F. critically review and revised the manuscript. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This review is funded by: The Health and Medical Research Fund (HMRF), Hong Kong (Project ID: 04190268); The Faculty Collaborative Research Scheme between Social Sciences and Health Sciences, HKPolyU [Ref: ZVSU].
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization (WHO) Falls. [(accessed on 18 April 2022)]. Available online: https://www.who.int/news-room/fact-sheets/detail/falls.
- 2.Kyu H.H., Abate D., Abate K.H., Abay S.M., Abbafati C., Abbasi N., Abbastabar H., Abd-Allah F., Abdela J., Abdelalim A., et al. Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1859–1922. doi: 10.1016/S0140-6736(18)32335-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Haagsma J.A., Graetz N., Bolliger I., Naghavi M., Higashi H., Mullany E.C., Abera S.F., Abraham J.P., Adofo K., Alsharif U., et al. The global burden of injury: Incidence, mortality, disability-adjusted life years and time trends from the Global Burden of Disease study 2013. Inj. Prev. 2016;22:3–18. doi: 10.1136/injuryprev-2015-041616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.James S.L., Lucchesi L.R., Bisignano C., Castle C.D., Dingels Z.V., Fox J.T., Hamilton E.B., Henry N.J., Krohn K.J., Liu Z., et al. The global burden of falls: Global, regional and national estimates of morbidity and mortality from the Global Burden of Disease Study 2017. Inj. Prev. 2020;26:i3–i11. doi: 10.1136/injuryprev-2019-043286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Osoba M.Y., Rao A.K., Agrawal S.K., Lalwani A.K. Balance and gait in the elderly: A contemporary review. Laryngoscope Investig. Otolaryngol. 2019;4:143–153. doi: 10.1002/lio2.252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lin H.W., Bhattacharyya N. Balance disorders in the elderly: Epidemiology and functional impact. Laryngoscope. 2012;122:1858–1861. doi: 10.1002/lary.23376. [DOI] [PubMed] [Google Scholar]
- 7.Burns E.R., Stevens J.A., Lee R. The direct costs of fatal and non-fatal falls among older adults—United States. J. Saf. Res. 2016;58:99–103. doi: 10.1016/j.jsr.2016.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Campbell A.J., Borrie M.J., Spears G.F., Jackson S.L., Brown J.S., Fitzgerald J.L. Circumstances and consequences of falls experienced by a community population 70 years and over during a prospective study. Age Ageing. 1990;19:136–141. doi: 10.1093/ageing/19.2.136. [DOI] [PubMed] [Google Scholar]
- 9.Stenhagen M., Ekström H., Nordell E., Elmståhl S. Accidental falls, health-related quality of life and life satisfaction: A prospective study of the general elderly population. Arch Gerontol. Geriatr. 2014;58:95–100. doi: 10.1016/j.archger.2013.07.006. [DOI] [PubMed] [Google Scholar]
- 10.Yardley L., Smith H. A prospective study of the relationship between feared consequences of falling and avoidance of activity in community-living older people. Gerontologist. 2002;42:17–23. doi: 10.1093/geront/42.1.17. [DOI] [PubMed] [Google Scholar]
- 11.Fuller G.F. Falls in the elderly. Am. Fam. Physician. 2000;61:2159–2168. [PubMed] [Google Scholar]
- 12.Lajoie Y., Teasdale N., Bard C., Fleury M. Attentional demands for static and dynamic equilibrium. Exp. Brain Res. 1993;97:139–144. doi: 10.1007/BF00228824. [DOI] [PubMed] [Google Scholar]
- 13.Brown L.A., Shumway-Cook A., Woollacott M.H. Attentional Demands and Postural Recovery: The Effects of Aging. J. Gerontol. A Biol. Sci. Ser. A. 1999;54:M165–M171. doi: 10.1093/gerona/54.4.M165. [DOI] [PubMed] [Google Scholar]
- 14.Agmon M., Belza B., Nguyen H.Q., Logsdon R.G., Kelly V.E. A systematic review of interventions conducted in clinical or community settings to improve dual-task postural control in older adults. Clin. Interv. Aging. 2014;9:477–492. doi: 10.2147/CIA.S54978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zheng J.J., Delbaere K., Close J.C., Sachdev P.S., Lord S.R. Impact of white matter lesions on physical functioning and fall risk in older people: A systematic review. Stroke. 2011;42:2086–2090. doi: 10.1161/STROKEAHA.110.610360. [DOI] [PubMed] [Google Scholar]
- 16.Starr J.M., Leaper S.A., Murray A.D., Lemmon H.A., Staff R.T., Deary I.J., Whalley L.J. Brain white matter lesions detected by magnetic resonance [correction of resosnance] imaging are associated with balance and gait speed. J. Neurol. Neurosurg. Psychiatry. 2003;74:94–98. doi: 10.1136/jnnp.74.1.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Richard A., Schmidt T.D.L. Attention and Performance Motor Control and Learning: A Behavioral Emphasis. 3rd ed. Human Kinetics; Champaign, IL, USA: 1999. [Google Scholar]
- 18.Gobbo S., Bergamin M., Sieverdes J.C., Ermolao A., Zaccaria M. Effects of exercise on dual-task ability and balance in older adults: A systematic review. Arch Gerontol Geriatr. 2014;58:177–187. doi: 10.1016/j.archger.2013.10.001. [DOI] [PubMed] [Google Scholar]
- 19.Woollacott M., Shumway-Cook A. Attention and the control of posture and gait: A review of an emerging area of research. Gait Posture. 2002;16:1–14. doi: 10.1016/S0966-6362(01)00156-4. [DOI] [PubMed] [Google Scholar]
- 20.Lundin-Olsson L., Nyberg L., Gustafson Y. “Stops walking when talking” as a predictor of falls in elderly people. Lancet. 1997;349:617. doi: 10.1016/S0140-6736(97)24009-2. [DOI] [PubMed] [Google Scholar]
- 21.Javadpour S., Sinaei E., Salehi R., Zahednejad S., Motealleh A. Comparing the Effects of Single-Task versus Dual-Task Balance Training on Gait Smoothness and Functional Balance in Community-Dwelling Older Adults: A Randomized Controlled Trial. J. Aging Phys. Act. 2022;30:308–315. doi: 10.1123/japa.2020-0523. [DOI] [PubMed] [Google Scholar]
- 22.Nematollahi A., Kamali F., Ghanbari A., Etminan Z., Sobhani S. Improving Balance in Older People: A Double-Blind Randomized Clinical Trial of Three Modes of Balance Training. J. Aging Phys. Act. 2016;24:189–195. doi: 10.1123/japa.2014-0286. [DOI] [PubMed] [Google Scholar]
- 23.Norouzi E., Vaezmosavi M., Gerber M., Puhse U., Brand S. Dual-task training on cognition and resistance training improved both balance and working memory in older people. Phys. Sportsmed. 2019;47:471–478. doi: 10.1080/00913847.2019.1623996. [DOI] [PubMed] [Google Scholar]
- 24.Telford C.W. The refractory phase of voluntary and associative responses. J. Exp. Psychol. 1931;14:1–36. doi: 10.1037/h0073262. [DOI] [Google Scholar]
- 25.Bayot M., Dujardin K., Tard C., Defebvre L., Bonnet C.T., Allart E., Delval A. The interaction between cognition and motor control: A theoretical framework for dual-task interference effects on posture, gait initiation, gait and turning. Neurophysiol. Clin. 2018;48:361–375. doi: 10.1016/j.neucli.2018.10.003. [DOI] [PubMed] [Google Scholar]
- 26.Hausdorff J.M., Schweiger A., Herman T., Yogev-Seligmann G., Giladi N. Dual-task decrements in gait: Contributing factors among healthy older adults. J. Gerontol. 2008;63:1335–1343. doi: 10.1093/gerona/63.12.1335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kramer A.F., Larish J.F., Strayer D.L. Training for attentional control in dual task settings: A comparison of young and old adults. J. Exp. Psychol. Appl. 1995;1:50–76. doi: 10.1037/1076-898X.1.1.50. [DOI] [Google Scholar]
- 28.Akin H., Senel A., Taskiran H., Kaya Mutlu E. Do motor-cognitive and motor-motor dual task training effect differently balance performance in older adults? Eur. Geriatr. Med. 2021;12:371–378. doi: 10.1007/s41999-020-00434-8. [DOI] [PubMed] [Google Scholar]
- 29.da Silva N.M., de Franca M.S., de Almeida D., de Lima E.S.G., dos Santos V.H.B., Souza J.V.D., Larrad A.R., de Almeida Aloise D., Freire Vieira Lima N.M. Effects of a Multicomponent Exercise Program on Groups of Community-Dwelling Older Adults with Low Schooling: A Pilot Study. J. Aging Res. 2021;2021:8829332. doi: 10.1155/2021/8829332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Weerdesteyn V., Rijken H., Geurts A.C., Smits-Engelsman B.C., Mulder T., Duysens J. A five-week exercise program can reduce falls and improve obstacle avoidance in the elderly. Gerontology. 2006;52:131–141. doi: 10.1159/000091822. [DOI] [PubMed] [Google Scholar]
- 31.Varela-Vásquez L.A., Minobes-Molina E., Jerez-Roig J. Dual-task exercises in older adults: A structured review of current literature. JFSF. 2020;5:31–37. doi: 10.22540/JFSF-05-031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Altman D.G., Schulz K.F., Moher D., Egger M., Davidoff F., Elbourne D., Gøtzsche P.C., Lang T. The revised CONSORT statement for reporting randomized trials: Explanation and elaboration. Ann. Intern. Med. 2001;134:663–694. doi: 10.7326/0003-4819-134-8-200104170-00012. [DOI] [PubMed] [Google Scholar]
- 33.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E., et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Song R., Grabowska W., Park M., Osypiuk K., Vergara-Diaz G.P., Bonato P., Hausdorff J.M., Fox M., Sudarsky L.R., Macklin E., et al. The impact of Tai Chi and Qigong mind-body exercises on motor and non-motor function and quality of life in Parkinson’s disease: A systematic review and meta-analysis. Park. Relat. Disord. 2017;41:3–13. doi: 10.1016/j.parkreldis.2017.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Koganemaru S., Fukuyama H., Mima T. Two is More Than One: How to Combine Brain Stimulation Rehabilitative Training for Functional Recovery? Front. Syst. Neurosci. 2015;9:154. doi: 10.3389/fnsys.2015.00154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Adamczyk J., Celka R., Stemplewski R., Ceynowa K., Kaminska P., Maciaszek J. The Impact of 12-Week Jaques-Dalcroze Eurhythmics Programme on the Dynamic Agility in Single-Dual-Task Conditions in Older Women: A Randomized Controlled Trial. Biomed Res. Int. 2020;2020:9080697. doi: 10.1155/2020/9080697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Batcir S., Lubovsky O., Bachner Y.G., Melzer I. The Effects of Bicycle Simulator Training on Anticipatory and Compensatory Postural Control in Older Adults: Study Protocol for a Single-Blind Randomized Controlled Trial. Front. Neurol. 2020;11:614664. doi: 10.3389/fneur.2020.614664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bessot N., Polyte R., Quesney M., Bulla J., Gauthier A. Diurnal gait fluctuations in single- and dual-task conditions. Chronobiol. Int. 2020;37:836–844. doi: 10.1080/07420528.2020.1773493. [DOI] [PubMed] [Google Scholar]
- 39.Portney L.G. Foundations of Clinical Research: Applications to Evidence-Based Practice. 4th ed. McGraw Hill; New York, NY, USA: 2020. [Google Scholar]
- 40.Sterne J.A.C., Savović J., Page M.J., Elbers R.G., Blencowe N.S., Boutron I., Cates C.J., Cheng H.Y., Corbett M.S., Eldridge S.M., et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. doi: 10.1136/bmj.l4898. [DOI] [PubMed] [Google Scholar]
- 41.McHugh M.L. Interrater reliability: The kappa statistic. Biochem. Med. 2012;22:276–282. doi: 10.11613/BM.2012.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Laatar R., Kachouri H., Borji R., Rebai H., Sahli S. Combined physical-cognitive training enhances postural performances during daily life tasks in older adults. Exp. Gerontol. 2018;107:91–97. doi: 10.1016/j.exger.2017.09.004. [DOI] [PubMed] [Google Scholar]
- 43.Bacha J.M.R., Gomes G.C.V., De Freitas T.B., Viveiro L.A.P., Silva L.N.M., Bueno G.C., Varise E.M., Torriani-Pasin C., Alonso A.C., Luna N.M.S., et al. Effects of kinect adventures games versus conventional physical therapy on postural control in elderly people: A randomized controlled trial. Games Health J. 2018;7:24–36. doi: 10.1089/g4h.2017.0065. [DOI] [PubMed] [Google Scholar]
- 44.Anandh S., Varadharajulu G., Alate M.M., Mane D.A. Effect of dual task training on balance and gait over regular and diversified land surfaces in independent elderly. Int. J. Curr. Sci. 2021;13:165–168. doi: 10.31782/IJCRR.2021.13113. [DOI] [Google Scholar]
- 45.Granacher U., Muehlbauer T., Göstemeyer G., Gruber S., Gruber M. The performance of balance exercises during daily tooth brushing is not sufficient to improve balance and muscle strength in healthy older adults. BMC Geriatr. 2021;21:257. doi: 10.1186/s12877-021-02206-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pradhan A., Raj R., Chaudhuri G.R., Agarwal S., Basak T. Functional Balance & Gait Balance in Normal Geriatric Population: By Gait Training with Multiple task. Indian J. Physiother. Occup. 2018;12:39–44. [Google Scholar]
- 47.Rose D.J., Clark S. Can the control of bodily orientation be significantly improved in a group of older adults with a history of falls? J. Am. Geriatr Soc. 2000;48:275–282. doi: 10.1111/j.1532-5415.2000.tb02646.x. [DOI] [PubMed] [Google Scholar]
- 48.Heiden E., Lajoie Y. Games-based biofeedback training and the attentional demands of balance in older adults. Aging Clin. Exp. Res. 2010;22:367–373. doi: 10.1007/BF03337732. [DOI] [PubMed] [Google Scholar]
- 49.Hiyamizu M., Morioka S., Shomoto K., Shimada T. Effects of dual task balance training on dual task performance in elderly people: A randomized controlled trial. Clin. Rehabil. 2012;26:58–67. doi: 10.1177/0269215510394222. [DOI] [PubMed] [Google Scholar]
- 50.Hinman M.R. Comparison of two short-term balance training programs for community-dwelling older adults. J. Geriatr. Phys. Ther. 2002;25:10–20. doi: 10.1519/00139143-200225030-00003. [DOI] [Google Scholar]
- 51.Lajoie Y. Effect of computerized feedback postural training on posture and attentional demands in older adults. Aging Clin. Exp. Res. 2004;16:363–368. doi: 10.1007/BF03324565. [DOI] [PubMed] [Google Scholar]
- 52.Morat M., Bakker J., Hammes V., Morat T., Giannouli E., Zijlstra W., Donath L. Effects of stepping exergames under stable versus unstable conditions on balance and strength in healthy community-dwelling older adults: A three-armed randomized controlled trial. Exp. Gerontol. 2019;127:110719. doi: 10.1016/j.exger.2019.110719. [DOI] [PubMed] [Google Scholar]
- 53.Bharti, Kumar C. Effect of training balance under dual task with fixed and variable priority instructions with balance impairment in institutionalized elderly population. Indian J. Physiother. Occup. 2014;8:152. doi: 10.5958/0973-5674.2014.00374.8. [DOI] [Google Scholar]
- 54.Callisaya M.L., Jayakody O., Vaidya A., Srikanth V., Farrow M., Delbaere K. A novel cognitive-motor exercise program delivered via a tablet to improve mobility in older people with cognitive impairment—StandingTall Cognition and Mobility. Exp. Gerontol. 2021;152:111434. doi: 10.1016/j.exger.2021.111434. [DOI] [PubMed] [Google Scholar]
- 55.de Oliveira V.M.A., Pirauá A.L.T., Cavalcante B.R., Beltrão N.B., de Farias W.M., Pitangui A.C.R., de Araújo R.C. Additional Functional Performance Gains After 24-Week Unstable Strength Training With Cognitive Training in Community-Dwelling Healthy Older Adults: A Randomized Trial. J. Aging Phys. Act. 2021;29:412–422. doi: 10.1123/japa.2020-0050. [DOI] [PubMed] [Google Scholar]
- 56.Mirelman A., Rochester L., Maidan I., Del Din S., Alcock L., Nieuwhof F., Rikkert M.O., Bloem B.R., Pelosin E., Avanzino L., et al. Addition of a non-immersive virtual reality component to treadmill training to reduce fall risk in older adults (V-TIME): A randomised controlled trial. Lancet. 2016;388:1170–1182. doi: 10.1016/S0140-6736(16)31325-3. [DOI] [PubMed] [Google Scholar]
- 57.Reve E.V., de Bruin E.D. Strength-balance supplemented with computerized cognitive training to improve dual task gait and divided attention in older adults: A multicenter randomized-controlled trial. BMC Geriatr. 2014;14:134. doi: 10.1186/1471-2318-14-134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Silsupadol P., Shumway-Cook A., Lugade V., van Donkelaar P., Chou L.S., Mayr U., Woollacott M.H. Effects of single- vs. dual-task training on balance performance under dual-task conditions in older adults with balance impairment: A randomized, controlled trial. Arch Phys. Med. Rehabil. 2009;90:381–387. doi: 10.1016/j.apmr.2008.09.559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Talwar J., Zia N.U., Maurya M., Singh H. Effect of Agility Training Under Single-Task Condition Versus Training Under Dual-Task Condition With Different Task Priorities to Improve Balance in the Elderly. Top Geriatr. Rehabil. 2015;31:98–104. doi: 10.1097/TGR.0000000000000054. [DOI] [Google Scholar]
- 60.Yamada M., Aoyama T., Tanaka B., Nagai K., Ichihashi N. Seated stepping exercise in a dual-task condition improves ambulatory function with a secondary task: A randomized controlled trial. Aging Clin. Exp. Res. 2011;23:386–392. doi: 10.1007/BF03337763. [DOI] [PubMed] [Google Scholar]
- 61.Yuzlu V., Oguz S., Timurtas E., Aykutoglu E., Polat M.G. The Effect of 2 Different Dual-Task Balance Training Methods on Balance and Gait in Older Adults: A Randomized Controlled Trial. Phys. Ther. 2021;102:pzab298. doi: 10.1093/ptj/pzab298. [DOI] [PubMed] [Google Scholar]
- 62.Zhang H., Zhang R., Yuzhi L., Hong Y., Jianxin C., Huijuan L., Jingmei W. Effects on dual-task training on gait and balance erformance for the elderly in nursing home. J. Nurs. Sci. 2020;35:94–98. [Google Scholar]
- 63.Ataş Balci L., Soğukkanli K., Burcu S., Hanoğlu L. Effects of Single-Task, Dual-Task and Successive Physical-Cognitive Training on Fall Risk and Balance Performance in Older Adults: A Randomized Controlled Trial Study. J. Exerc. Rehabil. 2022;9:1–11. doi: 10.15437/jetr.675975. [DOI] [Google Scholar]
- 64.Brustio P.R., Rabaglietti E., Formica S., Liubicich M.E. Dual-task training in older adults: The effect of additional motor tasks on mobility performance. Arch Gerontol. Geriatr. 2018;75:119–124. doi: 10.1016/j.archger.2017.12.003. [DOI] [PubMed] [Google Scholar]
- 65.Smith-Ray R.L., Hughes S.L., Prohaska T.R., Little D.M., Jurivich D.A., Hedeker D. Impact of Cognitive Training on Balance and Gait in Older Adults. J. Gerontol. B Psychol. Sci. Soc. Sci. 2015;70:357–366. doi: 10.1093/geronb/gbt097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Smith-Ray R.L., Makowski-Woidan B., Hughes S.L. A randomized trial to measure the impact of a community-based cognitive training intervention on balance and gait in cognitively intact Black older adults. Health Educ. Behav. 2014;4:62S–69S. doi: 10.1177/1090198114537068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ansai J.H., Aurichio T.R., Gonçalves R., Rebelatto J.R. Effects of two physical exercise protocols on physical performance related to falls in the oldest old: A randomized controlled trial. Geriatr. Gerontol. Int. 2016;16:492–499. doi: 10.1111/ggi.12497. [DOI] [PubMed] [Google Scholar]
- 68.Miyake A., Friedman N.P., Emerson M.J., Witzki A.H., Howerter A., Wager T.D. The unity and diversity of executive functions and their contributions to complex “Frontal Lobe” tasks: A latent variable analysis. Cogn. Psychol. 2000;41:49–100. doi: 10.1006/cogp.1999.0734. [DOI] [PubMed] [Google Scholar]
- 69.Fischer B.L., Midden A.J., Hoffmann A., Urben D., DeWitt L., Kohlman K., Sherman K., Myers S., Clemson L., Mahoney J.E. Stepping Out: A Pilot Program to Reduce Falls Risk in People with Mild Cognitive Impairment. OBM Geriatr. 2021;5:151. doi: 10.21926/obm.geriatr.2101151. [DOI] [Google Scholar]
- 70.Fitts P.M. The information capacity of the human motor system in controlling the amplitude of movement. J. Exp. Psychol. 1954;47:381. doi: 10.1037/h0055392. [DOI] [PubMed] [Google Scholar]
- 71.Baddeley A. Working memory. Curr. Biol. 2010;20:R136–R140. doi: 10.1016/j.cub.2009.12.014. [DOI] [PubMed] [Google Scholar]
- 72.James W. The Principles of Psychology. Henry Holt; New York, NY, USA: 1890. [Google Scholar]
- 73.Frackowiak R.S.J., Friston K.J., Frith C.D., Dolan R.J., Price C.J., Zeki S., Ashburner J.T., Penny W.D., editors. Human Brain Function. 2nd ed. Academic Press; Burlington, NJ, USA: 2004. Chapter 15—Mechanisms of Attention; pp. 245–268. [Google Scholar]
- 74.Woollacott M., Velde T.V. Non-visual spatial tasks reveal increased interactions with stance postural control. Brain Res. 2008;1208:95–102. doi: 10.1016/j.brainres.2008.03.005. [DOI] [PubMed] [Google Scholar]
- 75.Parasuraman R. The Attentive Brain: Issues and Prospects. In: Parasuraman R., editor. The Attentive Brain Cambridge. MIT Press; Cambridge, MA, USA: 1998. pp. 3–15. [Google Scholar]
- 76.Wickens C.D., Carswell C.M. Information processing. In: Salvendy G., editor. Handbook of Human Factors & Ergonomics. 5th ed. Taylor & Francis; Oxford, UK: 2021. [Google Scholar]
- 77.Wickens C. Attention: Theory, Principles, Models and Applications. Int. J. Hum. Comput. Interact. 2021;37:403–417. doi: 10.1080/10447318.2021.1874741. [DOI] [Google Scholar]
- 78.Delbroek T., Vermeylen W., Spildooren J. The effect of cognitive-motor dual task training with the biorescue force platform on cognition, balance and dual task performance in institutionalized older adults: A randomized controlled trial. J. Phys. Ther. Sci. 2017;29:1137–1143. doi: 10.1589/jpts.29.1137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Pichierri G., Wolf P., Murer K., de Bruin E.D. Cognitive and cognitive-motor interventions affecting physical functioning: A systematic review. BMC Geriatr. 2011;11:29. doi: 10.1186/1471-2318-11-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Srivas S., Thakur M.K. Aging of the Brain. In: Rattan S.I.S., editor. Encyclopedia of Biomedical Gerontology. Academic Press; Oxford, UK: 2020. pp. 149–158. [Google Scholar]
- 81.Reichman W.E., Fiocco A.J., Rose N.S. Exercising the brain to avoid cognitive decline: Examining the evidence. Aging Health. 2010;6:565–584. doi: 10.2217/ahe.10.54. [DOI] [Google Scholar]
- 82.Buss A.T., Kerr-German A. Dimensional attention as a mechanism of executive function: Integrating flexibility, selectivity, and stability. Cognition. 2019;192:104003. doi: 10.1016/j.cognition.2019.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Rand J., Spiro J.J. Cognitive Flexibility and Hypertext: Theory and Technology for the Non-Linear and Multidimensional Traversal of Complex Subject Matter. In: Nix D., Spiro R., editors. Cognition, Education, and Multimedia. Erlbaum; Hillsdale, NJ, USA: 1990. [Google Scholar]
- 84.Leber A.B., Turk-Browne N.B., Chun M.M. Neural predictors of moment-to-moment fluctuations in cognitive flexibility. Proc. Natl. Acad. Sci. USA. 2008;105:13592–13597. doi: 10.1073/pnas.0805423105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Shumway-Cook A., Woollacott M.H. Motor Control: Translating Research into Clinical Practice. 3rd ed. Lippincott Williams & Wilkins; Philadelphia, PA, USA: 2007. [Google Scholar]
- 86.Bandura A. Self-efficacy. Social Foundations of Thought and Action. Prentice Hall; New York, NY, USA: 1986. [Google Scholar]
- 87.Ruthruff E., Johnston J.C., Van Selst M. Why practice reduces dual-task interference. J. Exp. Psychol. Hum. Percept. Perform. 2001;27:3–21. doi: 10.1037/0096-1523.27.1.3. [DOI] [PubMed] [Google Scholar]
- 88.Gesell A. Infant Behaviour: Its Genesis and Growth. McGraw-Hill; New York, NY, USA: 1934. [Google Scholar]
- 89.Kramer A.F., Larish J.L., Weber T.A., Bardell L. Training for executive control: Task coordination strategies and aging. Atten. Perform. 1999;17:616–652. [Google Scholar]
- 90.Broeker L., Ewolds H., de Oliveira R.F., Künzell S., Raab M. The impact of predictability on dual-task performance and implications for resource-sharing accounts. Cogn. Res. Princ. Implic. 2021;6:1. doi: 10.1186/s41235-020-00267-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Strobach T. The dual-task practice advantage: Empirical evidence and cognitive mechanisms. Psychon. Bull. Rev. 2020;27:3–14. doi: 10.3758/s13423-019-01619-4. [DOI] [PubMed] [Google Scholar]
- 92.Trombetti A., Hars M., Herrmann F., Kressig R., Ferrari S., Rizzoli R. [“Jaques-Dalcroze eurhythmics” improves gait and prevents falls in the elderly] Rev. Med. Suisse. 2011;7:1305. [PubMed] [Google Scholar]
- 93.Vaillant J., Martigné P., Vuillerme N., Caillat-Miousse J.L., Parisot J., Juvin R., Nougier V. [Prediction of falls with performance on Timed “Up-and-Go” and one-leg-balance tests and additional cognitive tasks]. Annales de readaptation et de medecine physique: Revue scientifique de la Societe francaise de reeducation fonctionnelle de readaptation et de medecine physique. Ann. Readapt Med. Phys. 2006;49:1–7. doi: 10.1016/j.annrmp.2005.07.002. [DOI] [PubMed] [Google Scholar]
- 94.Altorfer P., Adcock M., de Bruin E.D., Graf F., Giannouli E. Feasibility of Cognitive-Motor Exergames in Geriatric Inpatient Rehabilitation: A Pilot Randomized Controlled Study. Front. Aging Neurosci. 2021;13:739948. doi: 10.3389/fnagi.2021.739948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Aruin A.S., Shiratori T., Latash M.L. The role of action in postural preparation for loading and unloading in standing subjects. Exp. Brain Res. 2001;138:458–466. doi: 10.1007/s002210100729. [DOI] [PubMed] [Google Scholar]
- 96.Grabiner M.D., Marone J.R., Wyatt M., Sessoms P., Kaufman K.R. Performance of an attention-demanding task during treadmill walking shifts the noise qualities of step-to-step variation in step width. Gait Posture. 2018;63:154–158. doi: 10.1016/j.gaitpost.2018.04.041. [DOI] [PubMed] [Google Scholar]
- 97.Silva N.C.B.S., Gill D.P., Gregory M.A., Bocti J., Petrella R.J. Multiple-modality exercise and mind-motor training to improve mobility in older adults: A randomized controlled trial. Exp. Gerontol. 2018;103:17–26. doi: 10.1016/j.exger.2017.12.011. [DOI] [PubMed] [Google Scholar]
- 98.De Bruin E.D., Reve E.V.H., Murer K. A randomized controlled pilot study assessing the feasibility of combined motor–cognitive training and its effect on gait characteristics in the elderly. Clin. Rehabil. 2013;27:215–225. doi: 10.1177/0269215512453352. [DOI] [PubMed] [Google Scholar]
- 99.Hauer K., Litz E., Günther-Lange M., Ball C., De Bruin E.D., Werner C. Effectiveness and sustainability of a motor-cognitive stepping exergame training on stepping performance in older adults: A randomized controlled trial. Eur. Rev. Aging Phys. Act. 2020;17:1–13. doi: 10.1186/s11556-020-00248-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Phirom K., Kamnardsiri T., Sungkarat S. Beneficial Effects of Interactive Physical-Cognitive Game-Based Training on Fall Risk and Cognitive Performance of Older Adults. Int. J. Environ. Res. Public Health. 2020;17:6079. doi: 10.3390/ijerph17176079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Agmon M., Kelly V.E., Logsdon R.G., Nguyen H., Belza B. The Effects of EnhanceFitness (EF) Training on Dual-Task Walking in Older Adults. J. Appl. Gerontol. 2015;34:NP128–NP142. doi: 10.1177/0733464812465921. [DOI] [PubMed] [Google Scholar]
- 102.Althomali M.M., Vallis L.A., Leat S.J. Can older adults’ balance and mobility improve with visual attention training? Eur. J. Appl. Physiol. 2019;119:1649–1661. doi: 10.1007/s00421-019-04153-2. [DOI] [PubMed] [Google Scholar]
- 103.Cadore E.L., Casas-Herrero A., Zambom-Ferraresi F., Idoate F., Millor N., Gómez M., Rodríguez-Mañas L., Izquierdo M. Multicomponent exercises including muscle power training enhance muscle mass, power output, and functional outcomes in institutionalized frail nonagenarians. AGE. 2014;36:773–785. doi: 10.1007/s11357-013-9586-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Costa S.N., Vieira E.R., Bento P.C.B. Effects of Home- and Center-Based Exercise Programs on the Strength, Function, and Gait of Prefrail Older Women: A Randomized Control Trial. J. Aging Phys. Act. 2020;28:122–130. doi: 10.1123/japa.2018-0363. [DOI] [PubMed] [Google Scholar]
- 105.Freiberger E., Menz H.B., Abu-Omar K., Rütten A. Preventing Falls in Physically Active Community-Dwelling Older People: A Comparison of Two Intervention Techniques. Gerontology. 2007;53:298–305. doi: 10.1159/000103256. [DOI] [PubMed] [Google Scholar]
- 106.Granacher U., Gollhofer A., Strass D. Training induced adaptations in characteristics of postural reflexes in elderly men. Gait Posture. 2006;24:459–466. doi: 10.1016/j.gaitpost.2005.12.007. [DOI] [PubMed] [Google Scholar]
- 107.Hatzitaki V., Voudouris D., Nikodelis T., Amiridis I. Visual feedback training improves postural adjustments associated with moving obstacle avoidance in elderly women. Gait Posture. 2009;29:296–299. doi: 10.1016/j.gaitpost.2008.09.011. [DOI] [PubMed] [Google Scholar]
- 108.Lo J., Lo O.-Y., Olson E.A., Habtemariam D., Iloputaife I., Gagnon M.M., Manor B., Lipsitz L.A. Functional implications of muscle co-contraction during gait in advanced age. Gait Posture. 2017;53:110–114. doi: 10.1016/j.gaitpost.2017.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Lord S.R., Ward J.A., Williams P., Strudwick M. The Effect of a 12-Month Exercise Trial on Balance, Strength, and Falls in Older Women: A Randomized Controlled Trial. J. Am. Geriatr. Soc. 1995;43:1198–1206. doi: 10.1111/j.1532-5415.1995.tb07394.x. [DOI] [PubMed] [Google Scholar]
- 110.Moreira N.B., Rodacki A.L., Costa M.S., Pitta A., Bento P.C. Perceptive–Cognitive and Physical Function in Prefrail Older Adults: Exergaming Versus Traditional Multicomponent Training. Rejuvenation Res. 2021;24:28–36. doi: 10.1089/rej.2020.2302. [DOI] [PubMed] [Google Scholar]
- 111.Narita M., Islam M.M., Rogers M.E., Koizumi D., Takeshima N. Effects of Customized Balance Exercises on Older Women Whose Balance Ability Has Deteriorated With Age. J. Women Aging. 2015;27:237–250. doi: 10.1080/08952841.2014.933633. [DOI] [PubMed] [Google Scholar]
- 112.Reed-Jones R.J., Dorgo S., Hitchings M.K., Bader J.O. Vision and agility training in community dwelling older adults: Incorporating visual training into programs for fall prevention. Gait Posture. 2012;35:585–589. doi: 10.1016/j.gaitpost.2011.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Rosado H., Bravo J., Raimundo A., Marmeleira J., Mendes F., Pereira C. Benefits of two twelve-week multimodal programs on reaction time in community dwellings at risk of falling: Preliminary results. Eur. J. Public Health. 2021;31:ckab120.062. doi: 10.1093/eurpub/ckab120.062. [DOI] [Google Scholar]
- 114.Schoene D., Lord S.R., Delbaere K., Severino C., Davies T.A., Smith S.T. A Randomized Controlled Pilot Study of Home-Based Step Training in Older People Using Videogame Technology. PLoS ONE. 2013;8:e57734. doi: 10.1371/journal.pone.0057734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Zak M., Skalska A., Szczerbinska K. Instructional programmes on how to rise unassisted effectively after sustaining an incidental fall, designed specifically for the elderly: A randomized, controlled trial. Ortop. Traumatol. Rehabil. 2008;10:496–507. [PubMed] [Google Scholar]
- 116.Aydogdu Y., Aydogdu O., Inal S.H. HPR is the dual-task training beneficial on the clinical outcomes of elderly? Ann. Rheum. Dis. 2017;76:1528–1529. [Google Scholar]
- 117.Barajas J. Characterizing the impact of baseline cognitive status on dual task performance while backward protective stepping. Neurorehabilit. Neural Repair. 2021;35:NP9–NP10. [Google Scholar]
- 118.Daly R., Duckham R., Tait J., Rantalainen T., Nowson C., Taaffe D., Hill K., Busija L., Sanders K. Effect of dual-task functional power and mobility training on falls and physical function in older people living in retirement villages: A cluster randomised controlled trial. J. Bone Miner. Res. 2018;33:20–21. [Google Scholar]
- 119.Halvarsson A., Olsson E., Elin F., Pettersson A., Ståhle A. A new individually adjusted, progressive balance group training program for elderly with fear of falling and a tendency to fall. Physiotherapy. 2011;97:eS448–eS449. doi: 10.1177/0269215511411937. [DOI] [PubMed] [Google Scholar]
- 120.Isrctn, Video Game Play-Based Motor Learning-Induced Brain Adaptations in the Elderly. 2015. [(accessed on 20 October 2022)]. Available online: https://trialsearch.who.int/Trial2.aspx?TrialID=ISRCTN73384012.
- 121.Isrctn, The Effects of Trail versus Road Running on Neuromuscular Performance. 2017. [(accessed on 20 October 2022)]. Available online: https://trialsearch.who.int/Trial2.aspx?TrialID=ISRCTN66167429.
- 122.McCulloch K., Giuliani C., Shubert T., Hartman M. 293 Community-based group exercise program with dualtask training components improves balance during dual-task conditions in ambulatory older adults. Park. Relat. Disord. 2010;16:S83. doi: 10.1016/S1353-8020(10)70294-7. [DOI] [Google Scholar]
- 123.Pompeu J., Mendes F., Silva K., Mondenesi A., Oliveira T., Peterson A., Piemonte M.E.P. Balance improvement in elderly after motor and cognitive training. Physiotherapy. 2011;97:eS1013–eS1014. [Google Scholar]
- 124.Takai I. Influence of balance exercises during an attention task on fear of falling among frail elderly fallen. Jpn. J. Geriatr. 2010;47:220–225. doi: 10.3143/geriatrics.47.220. [DOI] [PubMed] [Google Scholar]
- 125.Yingyongyudha A., Ramrong T., Yodkue P., Jamjit K., Suchart P., Ritdate K. 32 Effect of Dual Task Training Regarding to Postural Stability in the Healthy Elderly. Age Ageing. 2019;48:iv9–iv12. doi: 10.1093/ageing/afz164.32. [DOI] [Google Scholar]
- 126.Dorfman M., Herman T., Brozgol M., Shema S., Weiss A., Hausdorff J.M., Mirelman A. Dual-Task Training on a Treadmill to Improve Gait and Cognitive Function in Elderly Idiopathic Fallers. J. Neurol. Phys. Ther. 2014;38:246–253. doi: 10.1097/NPT.0000000000000057. [DOI] [PubMed] [Google Scholar]
- 127.Palmgren A., Ståhle A., Skavberg Roaldsen K., Dohrn I.M., Halvarsson A. “Stay balanced”—Effectiveness of evidence-based balance training for older adults transferred into a physical therapy primary care setting—A pilot study. Disabil. Rehabil. 2020;42:1797–1802. doi: 10.1080/09638288.2018.1535631. [DOI] [PubMed] [Google Scholar]
- 128.Merchant R.A., Tsoi C.T., Tan W.M., Lau W., Sandrasageran S., Arai H. Community-Based Peer-Led Intervention for Healthy Ageing and Evaluation of the ‘HAPPY’ Program. J. Nutr. Health Aging. 2021;25:520–527. doi: 10.1007/s12603-021-1606-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Brauer S.G., Woollacott M., Shumway-Cook A. The Interacting Effects of Cognitive Demand and Recovery of Postural Stability in Balance-Impaired Elderly Persons. Journals Gerontol. Ser. A. 2001;56:M489–M496. doi: 10.1093/gerona/56.8.M489. [DOI] [PubMed] [Google Scholar]
- 130.Buccello-Stout R.R., Bloomberg J.J., Cohen H.S., Whorton E.B., Weaver G.D., Cromwell R.L. Effects of sensorimotor adaptation training on functional mobility in older adults. J. Gerontol. Ser. B. 2008;63:P295–P300. doi: 10.1093/geronb/63.5.P295. [DOI] [PubMed] [Google Scholar]
- 131.De Bruin E.D., Swanenburg J., Betschon E., Murer K. A randomised controlled trial investigating motor skill training as a function of attentional focus in old age. BMC Geriatr. 2009;9:15. doi: 10.1186/1471-2318-9-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Fraser S.A., Li K.Z.H., Berryman N., Desjardins-Crépeau L., Lussier M., Vadaga K., Lehr L., Minh Vu T.T., Bosquet L., Bherer L. Does Combined Physical and Cognitive Training Improve Dual-Task Balance and Gait Outcomes in Sedentary Older Adults? Front. Hum. Neurosci. 2017;10:688. doi: 10.3389/fnhum.2016.00688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Freyler K., Krause A., Gollhofer A., Ritzmann R. Specific Stimuli Induce Specific Adaptations: Sensorimotor Training vs. Reactive Balance Training. PLoS ONE. 2016;11:e0167557. doi: 10.1371/journal.pone.0167557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Gimmon Y., Barash A., Debi R., Snir Y., Bar David Y., Grinshpon J., Melzer I. Application of the clinical version of the narrow path walking test to identify elderly fallers. Arch. Gerontol. Geriatr. 2016;63:108–113. doi: 10.1016/j.archger.2015.10.010. [DOI] [PubMed] [Google Scholar]
- 135.Granacher U., Muehlbauer T., Bridenbaugh S., Bleiker E., Wehrle A., Kressig R.W. Balance Training and Multi-Task Performance in Seniors. Int. J. Sports Med. 2010;31:353–358. doi: 10.1055/s-0030-1248322. [DOI] [PubMed] [Google Scholar]
- 136.Halvarsson A., Olsson E., Farén E., Pettersson A., Ståhle A. Effects of new, individually adjusted, progressive balance group training for elderly people with fear of falling and tend to fall: A randomized controlled trial. Clin. Rehabil. 2011;25:1021–1031. doi: 10.1177/0269215511411937. [DOI] [PubMed] [Google Scholar]
- 137.Hatton A.L., Menant J.C., Lord S.R., Lo J.C., Sturnieks D.L. The effect of lower limb muscle fatigue on obstacle negotiation during walking in older adults. Gait Posture. 2013;37:506–510. doi: 10.1016/j.gaitpost.2012.09.004. [DOI] [PubMed] [Google Scholar]
- 138.Hiatt L.G. Ph.D. Thesis. Nova Southeastern University; Fort Lauderdale, FL, USA: 2020. Does the Type of Dual Cognitive Task Impact Gait Variability using the Quantitative Timed up and Go (QTUG) in Community-Dwelling Adults? [Google Scholar]
- 139.Kao C.-C., Chiu H.-L., Liu D., Chan P.-T., Tseng I.-J., Chen R., Niu S.-F., Chou K.-R. Effect of interactive cognitive motor training on gait and balance among older adults: A randomized controlled trial. Int. J. Nurs. Stud. 2018;82:121–128. doi: 10.1016/j.ijnurstu.2018.03.015. [DOI] [PubMed] [Google Scholar]
- 140.Kurz I., Gimmon Y., Shapiro A., Debi R., Snir Y., Melzer I. Unexpected perturbations training improves balance control and voluntary stepping times in older adults—A double blind randomized control trial. BMC Geriatr. 2016;16:58. doi: 10.1186/s12877-016-0223-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Lord S.R., Ward J.A., Williams P. Exercise effect on dynamic stability in older women: A randomized controlled trial. Arch. Phys. Med. Rehabil. 1996;77:232–236. doi: 10.1016/S0003-9993(96)90103-3. [DOI] [PubMed] [Google Scholar]
- 142.Markovic G., Sarabon N., Greblo Z., Krizanic V. Effects of feedback-based balance and core resistance training vs. Pilates training on balance and muscle function in older women: A randomized-controlled trial. Arch. Gerontol. Geriatr. 2015;61:117–123. doi: 10.1016/j.archger.2015.05.009. [DOI] [PubMed] [Google Scholar]
- 143.Melzer I., Oddsson L.I. Improving balance control and self-reported lower extremity function in community-dwelling older adults: A randomized control trial. Clin. Rehabil. 2012;27:195–206. doi: 10.1177/0269215512450295. [DOI] [PubMed] [Google Scholar]
- 144.Reelick M.F., van Iersel M.B., Kessels R.P.C., Rikkert M.G.M.O. The influence of fear of falling on gait and balance in older people. Age Ageing. 2009;38:435–440. doi: 10.1093/ageing/afp066. [DOI] [PubMed] [Google Scholar]
- 145.Shahrbanian S., Hashemi A., Hemayattalab R. The comparison of the effects of physical activity and neurofeedback training on postural stability and risk of fall in elderly women: A single-blind randomized controlled trial. Physiother. Theory Pract. 2021;37:271–278. doi: 10.1080/09593985.2019.1630877. [DOI] [PubMed] [Google Scholar]
- 146.Silsupadol P., Lugade V., Shumway-Cook A., van Donkelaar P., Chou L.-S., Mayr U., Woollacott M.H. Training-related changes in dual-task walking performance of elderly persons with balance impairment: A double-blind, randomized controlled trial. Gait Posture. 2009;29:634–639. doi: 10.1016/j.gaitpost.2009.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Wollesen B., Mattes K., Schulz S., Bischoff L.L., Seydell L., Bell J.W., Von Duvillard S.P. Effects of Dual-Task Management and Resistance Training on Gait Performance in Older Individuals: A Randomized Controlled Trial. Front. Aging Neurosci. 2017;9:415. doi: 10.3389/fnagi.2017.00415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.You J.H., Shetty A., Jones T., Shields K., Belay Y., Brown D. Effects of dual-task cognitive-gait intervention on memory and gait dynamics in older adults with a history of falls: A preliminary investigation. NeuroRehabilitation. 2009;24:193–198. doi: 10.3233/NRE-2009-0468. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.