Abstract
Management of urinary tract infections is challenged by increasing antimicrobial resistance (AMR) worldwide. In this study, we describe the trends in antimicrobial resistance of uropathogens isolated from the largest private sector laboratory in Ghana over a five-year period. We reviewed positive urine cultures at the MDS Lancet Laboratories from 2017 to 2021. The proportions of uropathogens with antimicrobial resistance to oral and parenteral antimicrobials recommended by the Ghana standard treatment guidelines were determined. The proportion of multi-drug resistant isolates, ESBL and carbapenemase-producing phenotypes were determined. Of 94,134 urine specimens submitted for culture, 20,010 (22.1%) were culture positive. Enterobacterales was the most common group of organisms, E. coli (70.6%) being the most common isolate and Enterococcus spp. the most common gram-positive (1.3%) organisms. Among oral antimicrobials, the highest resistance was observed to ciprofloxacin (62.3%) and cefuroxime (60.2%) and the least resistance to fosfomycin (1.9%). The least resistance among parenteral antimicrobials was to meropenem (0.3%). The highest multi-drug resistance levels were observed among Klebsiella spp. (68.6%) and E. coli (64.0%). Extended-spectrum beta-lactamase (ESBL) positivity was highest in Klebsiella spp. (58.6%) and E. coli (50.0%). There may be a need to review the Ghana standard treatment guidelines to reflect increased resistance among uropathogens to recommended antimicrobials.
Keywords: urinary tract infection; Ghana; antimicrobial resistance (AMR); multi-drug resistance (MDR); MDS Lancet Laboratories; Access, Watch and Reserve (AWaRE) classification; uropathogens
1. Introduction
Antimicrobial resistance (AMR) threatens human health by limiting the options for treating infection [1]. AMR has been declared as one of the top 10 public health threats to humanity by the World Health Organization and a direct obstacle to achieving the Sustainable Development Goals [1]. Illnesses resulting from organisms with AMR lead to long hospital stays and require broad-spectrum and expensive antimicrobials for treatment, resulting in large financial burdens for patients [1].
Urinary tract infections (UTIs) are one of the leading causes of morbidity and a growing health care expenditure globally affecting 150 million people each year [2,3]. Morbidity and mortality from UTIs are higher in lower middle-income countries (LMICs) than in higher-income countries [4]. UTIs are most commonly caused by uropathogenic Escherichia coli (UPEC), Klebsiella pneumoniae and Enterococcus faecalis [5].
Widespread and indiscriminate use of antibiotics has led to the development of an alarming level of AMR among uropathogens, including the emergence of extended-spectrum beta-lactamase (ESBL) producing and carbapenemase-producing organisms [6]. ESBL-producing and carbapenemase-producing organisms are typically multi-drug resistant [6]. This mandates the use of the Watch and Reserve groups of antibiotics from the AWaRe (Access, Watch, Reserve) classification of the WHO [7]; these antibiotics are typically parenteral and may require hospitalization for the purposes of administration [8]. Common risk factors associated with resistant UTIs are urinary catheterization, previous hospitalization, previous antibiotic use and residence in a nursing home facility [9].
Although the burden of UTIs in Africa is not clearly documented, prevalence rates ranging between 10.1% and 76.6% have been reported in different sub-populations from across the continent [9,10,11]. In the same studies, AMR rates to antibiotics used for treating UTIs as high as 95% have been reported [9,10,11]. Whilst there is limited information about the general national prevalence of UTIs in Ghana, two studies have reported 42.75% prevalence in pregnant women [12] and 86% among hospitalized adults [13]. The proportion of multi-drug resistant (MDR) UTIs has been reported to be as high as 93.6% in Ghana [10,14]. AMR is a recognized threat in Ghana, and there is a national policy and action plan based on the global action plan on AMR [15]. Ghana is currently amongst the countries that are reporting to the global AMR surveillance system (GLASS) starting from 2021 [16].
A nation-wide study exploring AMR patterns in various uropathogens across several years and in different regions of Ghana could strengthen the knowledge and evidence base to guide policy and practice in line with the five objectives (Awareness, Surveillance, Infection prevention and control, Antimicrobial usage and Research and innovation) of the global action plan on AMR by the World Health Organization [16].
MDS Lancet Laboratories Gh. LTD is a member of the Cerba Lancet Africa group, a leading network of clinical pathology and medical diagnostics in Africa. MDS Lancet Laboratories Gh. LTD is currently the largest private pathology laboratory in Ghana, providing service to healthcare facilities in the private and public sectors.
In this study, we aimed to identify the AMR patterns and trends of MDR among uropathogens isolated from the urine samples of patients with suspected UTIs processed at MDS Lancet Laboratories, Ghana, over a five-year period from 2017 to 2021. Specifically, we sought to determine trends in (i) the yield of culture testing and proportions of all identified species, (ii) the resistance patterns of antibiotics grouped by route of administration and the WHO AwaRe classification, (iii) the factors associated with AMR and (iv) E.coli antibiotic resistance over the study period.
2. Materials and Methods
2.1. Study Design
This was a cross-sectional study involving the secondary analysis of laboratory data of urine cultures and antimicrobial susceptibility testing conducted at the MDS Lancet Laboratories, Ghana, between 2017 and 2021.
2.2. Study Setting
2.2.1. General Setting
Ghana is classified as a low middle-income country (LMIC) in West Africa with a total population of approximately 30.8 million. Accra is the capital city located at the coastal belt and has a total population of approximately 5 million [17]. Health care in Ghana is mainly provided by public sector facilities but with significant contribution from private sector facilities including laboratories. The public healthcare system consists of tertiary care hospitals, district (secondary) hospitals and primary health care facilities [18]. According to the law, patients need prescriptions from a medical doctor to get antibiotics [15]. However, it is possible to get antibiotics without prescriptions from private pharmacies. The Ghana Standard Treatment Guidelines (2017) suggest the following antibiotics for the treatment of UTIs: ciprofloxacin, cefuroxime and amoxicillin/clavulanic acid for uncomplicated infections; and gentamicin and ceftriaxone for complicated infections [19].
2.2.2. Specific Setting
MDS Lancet Laboratories Gh. LTD is a private medical laboratory with 29 locations dotted throughout 10 of the 16 administrative regions of Ghana. The laboratory processes approximately 148,500 samples per month and receives more than 50,000 urine (routine examination and cultures) samples per year. All testing and information management processes are conducted under strict quality control mechanisms as defined in the laboratory’s standard operating procedures. The laboratory holds ISO 15189 2012 certification. The headquarters/main laboratory is located in Accra. The microbiology department where this research was carried out has standard quality assurance mechanisms in place at the pre-analytical, analytical and post-analytical stages.
2.2.3. Sample Collection and Processing
The urine samples for this study originated from patients diagnosed with suspected UTIs in health care facilities (hospitals and clinics) in both the public and private sectors. Urine samples are usually transported by the patients or their relatives in sterile urine containers. All microbiology samples from the different branches that are meant for culture are transported to the microbiology laboratory in Accra within 24 h for processing using temperature-controlled, sample-transportation bags.
All urine samples received in the laboratory are registered and plated on cysteine lactose electrolyte deficient (CLED) agar, McConkey’s agar, blood agar and antimicrobial plates [20]. The first three media are used to determine the presence of microorganisms in the sample, while the latter is used to determine the presence of antibiotics in the urine and provides information on the use of antibiotics prior to sample collection. After 24 h of incubation, cultures are assessed and positive samples are further processed for identification of the specific microorganisms by performing indole and oxidase and other biochemical tests as well as the Analytical Profile Index (API) or Microscan [21]. Antimicrobial susceptibility testing is performed using the Kirby–Bauer disc diffusion method on Mueller–Hinton agar [22]. Zones of inhibition are interpreted using the Clinical and Laboratory Standards Institute (CLSI) guidelines [23].
2.3. Study Population
The study population included all urine samples submitted for culture and susceptibility testing at the MDS Lancet Laboratories in Ghana from January 2017 to December 2021.
2.4. Data Variables
For this study, the following variables were extracted from the laboratory database and used in the analysis: Patient ID and demographic characteristics, sample collection date and results entry date, the isolated organisms, ESBL status (for gram negatives) and antibiotic susceptibility patterns.
2.5. Sources of Data, Data Collection and Validation
The MDS Lancet Laboratories uses an electronic laboratory information system (LIS) where all the data related to the patients and samples are entered. Right from the collection of the sample, information is entered into the system and verified at each stage from transportation to processing of the samples. The results of the tests are reported in the same LIS, and the information becomes readily available for collection at any MDS Lancet branch. The LIS of the MDS Lancet Laboratories was used to extract the data for the study period. The data was extracted into MS Excel format and analyzed using STATA® (version 16.0 Copyright 1985–2019 StataCorp LLC, College Station, TX, USA).
2.6. Statistical Analysis
Frequency and proportions were used to summarize the demographic and microbiological characteristics. MDR was defined as resistance to at least one antimicrobial agent from three or more classes of antibiotics [24]. The presence of resistance to any antibiotic and MDR among all culture-positive samples were summarized as proportions with a 95% confidence interval (95% CI). Resistance to commonly prescribed antibiotics (individually and grouped according to the AWaRe classification) for different isolates was reported as a percentage. To identify the factors independently associated with a UTI due to MDR organisms in a patient, a modified Poisson regression with robust variance estimator was carried out. A patient was considered to have a UTI due to an MDR organism if any of the isolates from their urine sample turned out to be MDR. As this was a cross-sectional study, prevalence ratios (PR) and adjusted prevalence ratios (aPR) were reported as measures of association. The level of significance for all statistical tests was set at a p-value of 0.05 [25].
3. Results
3.1. Patient Characteristics and Proportions of All Identified Bacterial Isolates in Urine Samples
Over the five years, a total of 328,073 urine samples were submitted for processing. Of these, 94,134 samples were submitted for culture and susceptibility testing at the MDS Lancet Laboratories, and 20,010 (22.1%) yielded at least one organism on culture. Among the culture-positive samples, 793 (4%) yielded more than one organism. Table 1 shows the characteristics of the patients with culture-positive urine samples. Most culture-positive samples (38.8%) were from patients aged 15–44 years. Positive urine samples were more common in females (72.5%) compared to males, and the majority of positive urine samples were obtained from the Greater Accra region (63.5%).
Table 1.
Socio-demographic and microbiological characteristics of patients with urinary tract infections with culture-positive samples 1 analyzed at MDS Lancet Laboratories, Ghana, from 2017 to 2021.
| Characteristics | n | (%) | |
|---|---|---|---|
| Total number of patients | 20,010 | (100) | |
| Age in years | |||
| <15 | 1474 | (7.4) | |
| 15–44 | 7771 | (38.8) | |
| 45–64 | 4539 | 22.7 | |
| ≥65 | 6040 | (30.2) | |
| Unknown | 186 | 0.9 | |
| Sex | |||
| Male | 5484 | (27.4) | |
| Female | 14,505 | (72.5) | |
| Unknown | 21 | (0.1) | |
| Geographic location of urine specimens | |||
| Accra | 12,702 | (63.5) | |
| Ashanti | 4.266 | (21.3) | |
| Others | 3042 | (15.2) | |
| Antimicrobial substance in urine 2 | Present | 1986 | (9.9) |
| Number of bacterial isolates identified | |||
| One | 19,217 | (96.0) | |
| Two | 786 | (3.9) | |
| Three | 7 | (<0.1) | |
| Antimicrobial resistance | |||
| Resistance to at least one antimicrobial | 13,079 | (65.3) | |
| MDR 3 in at least one isolate | 12,609 | (63.0) |
1 Culture-positive samples mean the urine sample yielded at least one bacterial isolate; 2 Presence of antimicrobial substance in urine sample implies that patients were on antibiotics before their urine sample was taken; 3 MDR—Multi-drug resistance defined as resistance to three or more antibiotic drug classes.
Antibiotic residue was present in 1986 (9.9%) culture-positive samples. Isolates resistant to at least one antibiotic were found in 65.3% (95% CI: 64.6–66.0%) of cultures, and multi-drug resistant isolates were found in 63% (95% CI: 62.3–63.6%) of cultures.
3.2. Uropathogen Characteristics
Table 2 shows the distribution of uropathogens from the urine cultures. Enterobacterales was the most common group of organisms with Escherichia coli (70.6%), Klebsiella spp. (15.0%) and Proteus spp. (5.4%) being the most common, while Enterococcus spp. (1.3%) were the most common gram-positive organisms isolated. This pattern of organism distribution was similar across all age groups, region of sample origin and year of specimen collection. The full list of isolated pathogens and patient characteristics are provided in Supplementary Table S1.
Table 2.
Distribution of common uropathogens isolated from the urine samples of patients with urinary tract infections analyzed at MDS Lancet Laboratories, Ghana, from 2017 to 2021 based on age and region.
| Gram-Negative Bacteria (GNB) | Gram-Positive Bacteria (GPC) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| E. coli | Klebsiella spp. | Proteus spp. | Pseudomonas spp. | Acinetobacter spp. | Other GNB | |||||||||
| n (%) 1 | n (%) 1 | n (%) 1 | n (%) 1 | n (%) 1 | n (%) 1 | n (%) 2 | ||||||||
| Age groups in years | ||||||||||||||
| <15 | 997 | (6.8) | 272 | (8.7) | 104 | (9.3) | 5 | (5.0) | 9 | (18.8) | 143 | (9.9) | 26 | (8.8) |
| 15–44 | 5887 | (40.1) | 1141 | (36.7) | 374 | (33.4) | 15 | (15.0) | 17 | (35.4) | 501 | (34.8) | 137 | (46.4) |
| 45–64 | 3329 | (22.7) | 735 | (23.6) | 237 | (21.2) | 21 | (21.0) | 4 | (8.3) | 309 | (21.5) | 64 | (21.7) |
| ≥65 | 4341 | (29.5) | 942 | (30.3) | 395 | (35.3) | 59 | (59.0) | 18 | (37.5) | 472 | (32.8) | 65 | (22.0) |
| Regions | ||||||||||||||
| Accra | 9437 | (64.2) | 1921 | (61.7) | 723 | (64.6) | 65 | (65.0) | 27 | (56.3) | 824 | (57.2) | 186 | (63.1) |
| Ashanti | 3080 | (21.0) | 659 | (21.2) | 280 | (25.0) | 18 | (18.0) | 6 | (12.5) | 348 | (24.2) | 77 | (26.1) |
| Others | 2178 | (14.8) | 532 | (17.1) | 117 | (10.4) | 17 | (17.0) | 15 | (31.3) | 268 | (18.6) | 32 | (10.8) |
| Total | 14695 | (100) | 3112 | (100) | 1120 | (100) | 100 | (100) | 48 | (100) | 1440 | (100) | 295 | (100) |
1 Percentages reported out of all culture-positive samples with gram-negative bacilli (GNB) isolates reported for each category; 2 Percentages reported out of all culture-positive samples with gram-positive cocci (GPC) isolates reported for each category.
3.3. Trends in Urinary Bacterial Isolates over Five Years, 2017–2021
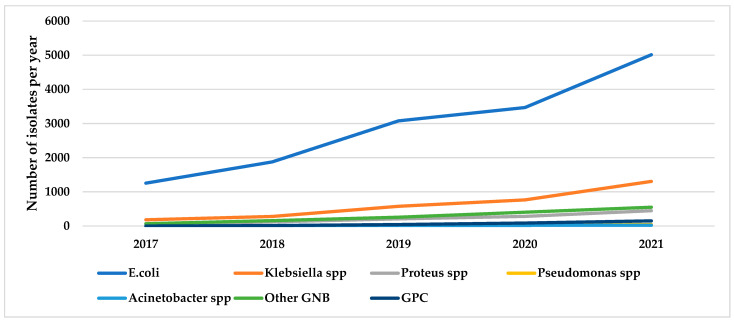
Annual trends in urinary bacterial isolates for the top five GNBs and gram-positive organisms over five years (2017–2021) are shown in Figure 1.
Figure 1.
Annual trends in the number of isolates for the top five GNBs and gram positives from urine samples of patients with urinary tract infections at MDS Lancet laboratories, Ghana, from 2017 to 2021. Number for each year is the total of each isolate for the particular year; Other GNB: all gram-negative bacilli isolated in the laboratory apart from E.coli, Klebsiella spp., Proteus spp., Pseudomonas spp. and Acinetobacter spp.; GPC: Gram-positive cocci.
The total number of isolates over the five years per year are as follows: 2017 (1568), 2018 (2456), 2019 (4193), 2020 (5050) and 2021 (7543).
Figure 1 shows a general increase in the number of isolates for the top five GNBs over the study period.
3.4. Resistance Patterns of Antibiotics Grouped by Route of Administration and the WHO AWaRe Classification
Table 3 and Table 4 show the proportion of the most common uropathogens resistant to oral antibiotics as recommended by the national standard treatment guidelines including fosfomycin and common parenteral antibiotics that were likely to be used as second-line agents for treatment. Among Enterobacterales, the least resistance was observed to fosfomycin—E. coli (2.9%), Klebsiella spp. (9.9%) and Proteus spp. (14.0%); the highest resistance was observed to ciprofloxacin (62.3%) and cefuroxime (60.2%). Among Enterococcus spp., the least resistance was observed to nitrofurantoin (1.5%).
Table 3.
Prevalence of antimicrobial resistance to common oral antibiotics used in treating UTIs in Ghana among the top six GNBs and Enterococcus spp. isolated from urine samples of patients with UTIs at MDS Lancet Laboratories, Ghana, from 2017 to 2021.
| Ampicillin | Amoxicillin Clavulanate | Nitrofurantoin | Ciprofloxacin | Cefuroxime | Fosfomycin | |
|---|---|---|---|---|---|---|
| n (%) 1 | n (%) 1 | n (%) 1 | n (%) 1 | n (%) 1 | n (%) 1 | |
| E. coli | N/A | 9411 (64.0) | 3575 (24.3) | 9161 (62.3) | 8851 (60.2) | 435 (2.9) |
| Klebsiella spp. | N/A | 2083 (66.9) | 1639 (52.7) | 1659 (53.3) | 1986 (63.8) | 308 (9.9) |
| Proteus spp. | N/A | 105 (9.4) | N/A | 151 (13.5) | 91 (8.13) | 6 (14.0) |
| Acinetobacter spp. | N/A | N/A | N/A | 9 (18.8) | N/A | N/A |
| Pseudomonas spp. | N/A | N/A | N/A | 41 (41) | N/A | N/A |
| Enterococcus faecalis | 9 (3.3) | N/A | 4 (1.5) | N/A | N/A | 5 (1.9) |
1 Percentages calculated with the total number of urine samples that yielded the particular species as the denominator. Antibiotics in Green belong to the Access group, and those in Yellow belong to the Watch group as per the WHO AWaRe classification 2021; UTI—urinary tract infection; GNB—gram-negative bacilli; GPC—gram-positive cocci; N/A—Not applicable (not tested for the isolate).
Table 4.
Prevalence of antimicrobial resistance to common parenteral antibiotics used in treating UTIs in Ghana among the top uropathogens isolated from urine samples of patients with UTIs at MDS Lancet Laboratories, Ghana, from 2017 to 2021.
| Organism | Ak | Caz | Cro | Mem | Piptaz | Tige |
|---|---|---|---|---|---|---|
| n (%) 1 | n (%) 1 | n (%) 1 | n (%) 1 | n (%) 1 | n (%) 1 | |
| E. coli | 461 (3.1) | 7147 (48.62) | 7362 (50.1) | 42 (0.3) | 7148 (48.6) | 252 (1.7) |
| Klebsiella spp. | 116 (3.7) | 1802 (57.9) | 1834 (58.9) | 56 (1.8) | 1803 (57.9) | 173 (5.6) |
| Proteus spp. | 3 (0.3) | 46 (4.1) | 46 (4.1) | 3 (0.3) | 17 (39.5) | N/A |
| Acinetobacter spp. | 2 (4.2) | 17 (35.4) | N/A | 1 (2.1) | 14 (29.2) | N/A |
| Pseudomonas spp. | 21 (21) | 30 (30) | N/A | 19 (19) | 27 (27.0) | N/A |
1 Percentages calculated with the total number of urine samples that yielded the particular species as the denominator. Antibiotics in Green belong to the Access group, those in Yellow belong to the Watch group, and those in Red belong to the Reserve Group as per the WHO AWaRe classification 2021. Cro: Ceftriaxone; Cp: Cefepime; Piptaz: Piperacillin tazobactam; Caz: Ceftazidime; Mem: Meropenem; Ak: Amikacin; Vanc: Vancomycin; Tige: Tigecycline; UTI—urinary tract infection; GNB—gram-negative bacilli; N/A—not applicable.
The least resistance to parenteral antibiotics among Enterobacterales was to meropenem (0.3%) and tigecycline (1.7%). Among isolated Enterococcus spp., no resistance was observed to vancomycin. Among ESBL-positive organisms, the least resistance observed among oral antibiotics was to fosfomycin (5.4%) and nitrofurantoin (41.6%). Among the parenteral antibiotics, the least resistance was observed to amikacin (5.3%) and meropenem (1.2%). The details of the antimicrobial resistance patterns among ESBL-positive organisms are provided in Supplementary Table S2.
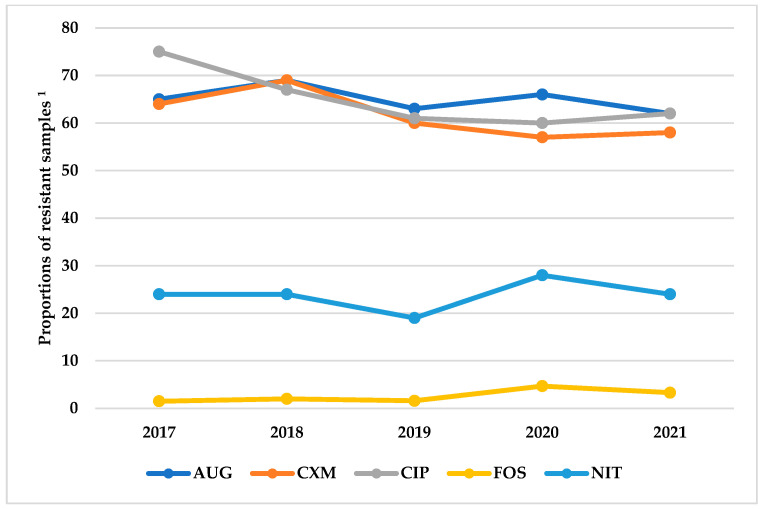
Resistance of E. coli to oral antibiotics (amoxicillin/clavulanic acid, cefuroxime, ciprofloxacin, fosfomycin and nitrofurantoin) was constant over the study period as shown in Figure 2.
Figure 2.
Annual trends in the proportions of resistance to selected antimicrobials among E. coli isolated from urine samples of patients with urinary tract infections at MDS Lancet Laboratories, Ghana, from 2017 to 2021. 1 Proportion for each year calculated with the number of samples in which E. coli was isolated in the year as the denominator (2017 = 1256, 2018 = 1877, 2019 = 3078, 2020 = 3469, 2021 = 5015); AUG: Amoxicillin/clavulanic acid; CXM: Cefuroxime; CIP: Ciprofloxacin; FOS: Fosfomycin; NIT: Nitrofurantoin; ESBL: Extended-spectrum beta-lactamase.
3.5. Multi-Drug Resistance and ESBL Positivity
The proportion of isolates that showed MDR was highest in Klebsiella spp. (68.6%) and E. coli (64.0%). Among Enterobacterales, ESBL positivity was highest among Klebsiella spp. (58.6%) followed by E. coli (50.0%) and least in Proteus spp. (5.3%). In addition, the proportions of ESBL were stable across the study years. The details of the trends in MDR and ESBL positivity among commonly isolated uropathogens are provided in Table 5. Gram-positive bacteria are not presented due to the low number of resistant isolates.
Table 5.
Prevalence of multi-drug resistance (MDR) and extended-spectrum beta-lactamase (ESBL) positivity among commonly isolated bacteria causing UTIs in patients at MDS Lancet Laboratories, Ghana, from 2017 to 2021.
| Organism | MDR | ESBL | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2017 | 2018 | 2019 | 2020 | 2021 | Overall | 2017 | 2018 | 2019 | 2020 | 2021 | Overall | |
| n (%) 1 | n (%) 1 | n (%) 1 | n (%) 1 | n (%) 1 | n (%) 1 | n (%) 2 | n (%) 2 | n (%) 2 | n (%) 2 | n (%) 2 | n (%) 2 | |
| Gram negatives | ||||||||||||
| E. coli | 871 (69.4) | 1309 (69.7) | 1958 (63.6) | 2182 (62.9) | 3087 (61.6) | 9407 (64.0) | 600 (47.8) | 975 (51.9) | 1585 (51.5) | 1692 (48.8) | 2492 (49.7) | 7344 (50.0) |
| Klebsiella spp. | 137 (74.5) | 216 (77.4) | 376 (65.2) | 522 (68.3) | 885 (67.7) | 2136 (68.6) | 106 (57.6) | 181 (64.9) | 329 (57.0) | 441 (57.7) | 765 (58.5) | 1822 (58.6) |
| Proteus spp. | 4(6.8) | 14 (11.6) | 33 (15.8) | 32 (11.4) | 59 (13.1) | 142 (12.68) | 4 (6.8) | 6 (5.0) | 16 (7.7) | 11 (3.9) | 22 (4.9) | 59 (5.3) |
| Pseudomonas spp. | 0 (0.0) | 1 (16.7) | 9 (40.9) | 14 (51.8) | 16 (35.6) | 40 (40) | N/A | N/A | N/A | N/A | N/A | N/A |
| Acinetobacter spp. | 0 (0.0) | 0 (0) | 0 (0.0) | 6 (31.6) | 4 (18.2) | 10 (20.8) | N/A | N/A | N/A | N/A | N/A | N/A |
| Other Gram-negative rods | 65 (94.3) | 140 (89.1) | 220 (85.3) | 348 (86.1) | 425 (77.0) | 1198 (83.2) | 44 (63.8) | 90 (57.3) | 131 (50.8) | 126 (31.2) | 185 (33.5) | 576 (40) |
1 Percentage of MDR isolates for each bacterial species is calculated with the number of samples that yielded the particular species as the denominator; 2 Percentages of ESBL-producing isolates for each bacterial species is calculated with the number of samples that yielded the particular species as the denominator; N/A = Not applicable.
3.6. Factors Associated with Antimicrobial Resistance
Age, gender, specimen location and presence of antibiotic residue in urine were found to be independently associated with a patient having a MDR uropathogen (Table 6). The patients aged 65 years and above (aPR 1.16, 95% CI: 1.11–1.22) and males (aPR: 1.13, 95% CI: 1.11–1.16) had a significantly higher risk of a UTI due to a multi-drug resistant uropathogen. The patients with antibiotic residues in their urine (aPR 1.40, 95% CI: 1.37–1.43) had a significantly higher risk of a UTI due to a multi-drug resistant uropathogen.
Table 6.
Factors associated with multi-drug resistance in patients with urinary tract infections with culture-positive samples tested at MDS Lancet Laboratories, Ghana, from 2017 to 2021.
| Factors | Total n 1 |
MDR n (%) 2 |
PR (95% CI) | aPR (95% CI) | p-Value |
|---|---|---|---|---|---|
| Age in years | |||||
| <15 | 1474 | 854 (57.9) | Ref | Ref | |
| 15–44 | 7771 | 4595 (59.1) | 1.01 (0.97–1.06) | 1.05 (0.99–1.09) | 0.06 |
| 45–64 | 4539 | 3020 (66.5) | 1.14 (1.09–1.20) | 1.14 (1.08–1.19) | <0.001 |
| ≥5 | 6040 | 4207 (69.6) | 1.20 (1.14–1.25) | 1.16 (1.11–1.22) | <0.001 |
| Sex | |||||
| Male | 5484 | 3989 (72.7) | 1.20 (1.17–1.22) | 1.13 (1.11–1.16) | <0.001 |
| Female | 14,505 | 8783 (60.5) | Ref | Ref | |
| Specimen location 3 | |||||
| Accra | 12,702 | 7931 (62.4) | Ref | Ref | |
| Ashanti | 4266 | 2722 (63.8) | 1.02 (0.99–1.05) | 1.04 (1.01–1.07) | 0.002 |
| Others | 3042 | 2131 (63.8) | 1.12 (1.09–1.15) | 1.09 (1.07–1.13) | <0.001 |
| Antimicrobial substance in urine | |||||
| Present | 1986 | 1742 (87.1) | 1.43 (1.40–1.46) | 1.40 (1.37–1.43) | <0.001 |
| Absent | 18,007 | 11,030 (61.2) | Ref | Ref |
1 Missing values in age (186), sex (21) and antimicrobial substance in urine (17) dropped from analysis; 2 Row percentages; 3 Specimen locations are the regions from where the samples were collected. Samples from regions outside greater Accra were well-packaged and transported in temperature-regulated specimen bags; MDR—Multi-drug resistance; PR—prevalence ratio; CI—confidence interval; aPR—adjusted prevalence ratio.
4. Discussion
In this study, the culture yield over the study period was 22.1%. This is similar to results obtained in other studies in which the positivity ranged from 17% to 37% [26,27]. Enterobacterales was the most common group of pathogens isolated with E. coli and Klebsiella spp. being the most common isolates, and Enterococcus spp. being the most common gram-positive organisms. These organisms predominate the human gut flora, which is known to be the common source of autoinfection for UTIs. These findings are similar to the results in other studies where E. coli at 68.3% and Klebsiella pneumoniae at 31.7% were the most predominant isolates from UTIs [28]. In another study from India, E.coli was the predominant isolate at 77.9% followed by Klebsiella spp. at 22.1% [29].
High levels of resistance to the Standard Treatment Guidelines (STG) recommended antibiotics for treating urinary tract infections were observed in this study. This situation was more acute among Enterobacterales. For example, among E. coli isolates, resistance to cefuroxime and ciprofloxacin was 60.2% and 62.3%, respectively. This situation can result in poor treatment outcomes, including prolonged treatment for empirically treated UTIs. The oral antibiotics with the least resistance in this study were nitrofurantoin and fosfomycin. Fosfomycin is a new agent on the Ghanaian market and is not widely available. Thus, its use is restricted, and it was expected that resistance to this antibiotic would be low. Although nitrofurantoin is an old drug, the side effects arising from its use may have resulted in its limited use and, consequently, the relatively low resistance observed compared to the other agents [30,31].
In a recent review of AMR among uropathogens in the Asia–Pacific region, a similar pattern was observed; resistance to commonly used drugs, such as ciprofloxacin, sulfamethoxazole–trimethoprim and ceftriaxone, ranged from 33% to 90% with low resistance observed to nitrofurantoin from 2.7% to 34% and to fosfomycin from 1.7% to 1.8% [32].
The resistance to parenteral antibiotics, such as ceftriaxone and gentamicin that are recommended for the treatment of complicated UTIs, was also high. This may be due to the relatively high prevalence of ESBL observed among Enterobacterales. ESBL genes are typically borne on plasmids, which are known to carry multiple resistance genes making affected organisms multi-drug resistant [33]. The proportion of ESBL among Enterobacterales in this study was high, similar to findings from other studies from Ghana [14].
The proportion of ESBL among organisms seemed be constant over the five years under consideration. Our study suggests that the agents useful against ESBL-producing organisms are fosfomycin, meropenem and amikacin. These agents may be considered for the empirical treatment of a UTI when risk factors for MDR infection exist, such as previous hospitalizations or antibiotic use. MDR was a common characteristic among the majority of uropathogens isolated. This suggests AMR may be a major problem in Ghana.
Among the different age groups, the risk of having a MDR infection was associated with older patients. Increasing age is associated with an increased use and misuse of antibiotics, a situation likely to increase MDR risk. In other studies, increasing age was found to be associated with an increased risk of having a MDR UTI and, hence, an increased use of antibiotics [34,35]. A study in the United Kingdom (UK) showed an increased risk of MDR with age, with odds ratios of 1.8, 2.69, 3.22 and 3.62 for the age ranges 50–59, 60–69, 70–79 and >80 years, respectively [35].
Whilst the prevalence of UTIs was common in women in this study, the risk of MDR infection was significantly higher in males compared to women. UTIs in males are usually associated with a urological abnormality, such as prostatic hyperplasia or posterior urethral valves that are usually associated with instrumentation and risk of infection [36,37,38]. Lastly, the highest risk of MDR was found in patients with the presence of antibiotics in the urine. This presupposes that most of these patients had difficult-to-treat infections and were probably started on ineffective antibiotics or had misused antibiotics, all of which may have contributed to the development of resistance.
A major strength of this study is the large number of isolates included from different regions of Ghana, and the study represents one of the largest datasets on AMR in uropathogens on the African continent as well as in Ghana. This data may give a better understanding of AMR in uropathogens in Ghana, although the preponderance of data from the Greater Accra and Ashanti regions may introduce some bias into data representativeness. Another strength of this study is that we followed STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidelines to report the findings of our study [39].
A major limitation of this study, however, is the inability to segregate the data into outpatient and inpatient because of data unavailability. Such data would have allowed for the segregation of community-acquired and hospital-acquired infections and their association with AMR. This study, being a laboratory-only based surveillance, has the potential to overestimate the level of resistance among uropathogens as has been shown in other studies [40].
This study has significant implications for policy and practice. Based on the current data, there may be a need to revise the STG guidelines on antibiotics to be used for treating UTIs, especially complicated infections, to reflect the large proportions of AMR observed among uropathogens. As these guideline changes are considered, there will be a need to implement antibiotic stewardship measures to prolong the usefulness of agents, such as fosfomycin, nitrofurantoin, amikacin and meropenem that may be recommended as alternate antibiotics. Also, there will be a need to investigate the utility of other oral antibiotics for treating UTIs to offer clinicians and patients more therapeutic options in the face of growing MDR infections. In the long term, there is a need to establish laboratory-based surveillance of uropathogens nationwide augmented by large population-based studies covering large geographical regions to inform policy and practice. This is important to correct for the selection bias of laboratory surveillance for MDR organisms. Also, clinicians should be encouraged to routinely utilize culture and susceptibility testing during the management of UTIs to avoid poor treatment outcomes because of resistant strains.
5. Conclusions
Over the five-year period, gram-negative pathogens, especially E. coli, were the most common cause of UTIs. High levels of resistance to STG recommended oral and parenteral antibiotics for the management of UTIs were observed. There may be a need to review the current STG guidelines to reflect the high numbers of AMR in the most common isolates.
Acknowledgments
This research was conducted through the global partnership of Structured Operational Research and Training Initiative (SORT IT), coordinated by TDR, the Special Program for Research and Training in Tropical Diseases at the World Health Organization (TDR). The specific SORT IT program that led to these publications included a partnership of TDR with the WHO Ghana country office, The International Union Against Tuberculosis and Lung Diseases, Paris; Institute of Tropical Medicine. MDS-Lancet Laboratories, Accra, Ghana; Narotam Sekhsaria Foundation, Mumbai, India; Tuberculosis Research and Prevention Center, Yerevan, Armenia; The INCLEN Trust International, New Delhi, India; Nasreen for the Review of this manuscript. The authors wish to acknowledge Ntethelelo Mthimunye and the entire team of Lancet Laboratories ELAB, South Africa for their support with extracting data from MEDITECH.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijerph192416556/s1, Table S1: Total number of all bacteria isolates at MDS lancet laboratories Ghana from 2017 and 2021; Table S2: The susceptibility patterns of tested antibiotics against ESBL positive bacteria at the MDS-lancet laboratories Ghana from 2017 to 2021.
Author Contributions
Conceptualization, B.A., H.A.G., H.D. and A.-K.L.; Methodology, B.A., H.A.G., H.D. and A.-K.L.; Software, B.A., D.N., K.M. and A.-K.L.; Data curation and validation, B.A., F.A.-G., D.N. and G.M.P.; Formal analysis; D.N., B.A. and K.M.; Resources, P.S.-N., H.A.G. and H.D.; Data curation; writing—original draft preparation, B.A., H.A.G., H.D., D.N., K.M. and A.-K.L.; Writing—review and editing, all authors; Visualization, N.S.J.; Supervision, A.-K.L., P.S.-N., H.A.G. and H.D.; Project administration, B.A., A.-K.L. and P.S.-N. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Permission to use the data was obtained from the CEO of MDS-Lancet Laboratories Gh LTD. The study received approval from the Noguchi Memorial Institute for Medical Research (NMIMR) NMIMR-IRB CPN 041/21-22 dated 2 March 2022). The Ethics Advisory Group of the International Union against Tuberculosis and Lung Disease, Paris, France (approval No 41/21 dated 13 December 2021) also approved the study.
Informed Consent Statement
No patient consent was required as secondary data was extracted from the electronic database of MDS-Lancet Laboratories.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare that this study received funding from the National Institute of Health Research, Department of Health & Social Care of the United Kingdom and supported by implementing partners. The funder was not involved in the study design, collection, analysis, interpretation of data, the writing of this article or the decision to submit it for publication.
Funding Statement
This SORT IT AMR Program was funded by the National Institute of Health Research, Department of Health & Social Care of the United Kingdom and supported by implementing partners. TDR is able to conduct its work thanks to the commitment and support from a variety of funders. A full list of TDR donors is available at: https://tdr.who.int/about-us/our-donors. This funding was for conducting the SORT IT Training. The study was conducted as part of routine operational research, using available resources without any specific funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization (WHO) Factsheet. World Health Organization (WHO); Geneva, Switzerland: 2020. Antimicrobial resistance. [Google Scholar]
- 2.Zalewska-pi B. Phage Therapy as a Novel Strategy in the Treatment of Urinary Tract Infections Caused by E. coli. Antibiotics. 2020;9:304. doi: 10.3390/antibiotics9060304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Joshua M., Raymond M. Virulence factors and antibiotic resistance patterns of uropathogenic Escherichia coli. Afr. J. Microbiol. Res. 2014;8:3678–3686. doi: 10.5897/AJMR2014.7034. [DOI] [Google Scholar]
- 4.Stamm W.E., Norrby S.R. Urinary Tract Infections: Disease Panorama and Challenges. J. Infect. Dis. 2001;183:S1–S4. doi: 10.1086/318850. [DOI] [PubMed] [Google Scholar]
- 5.Flores-Mireles A.L., Walker J.N., Caparon M., Hultgren S.J. Urinary tract infections: Epidemiology, mechanisms of infection and treatment options. Nat. Rev. Microbiol. 2015;13:269–284. doi: 10.1038/nrmicro3432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bartoletti R., Johansen T.E.B. Eau Guidelines on Urological Infections. 2017. [(accessed on 30 November 2022)]. pp. 247–269. Available online: https://www.researchgate.net/publication/284761422_Guidelines_on_urological_infections. [Google Scholar]
- 7.Plan G.A., Resistance A., Regulations I.H., Atb T., Atb N. A Technical Guide to Implementing the World Health Organization’ s AWaRe Antibiotic Classification in MTaPS Program Countries. 2019. [(accessed on 30 November 2022)]. pp. 1–7. Available online: https://www.mtapsprogram.org/wp-content/uploads/2021/03/USAID-MTaPS_Implementing-WHO-AWaRe-Classification.pdf. [Google Scholar]
- 8.Kaye K.S., Nguyen H.H., Rybak M.J. Clinical review guidelines for management and care transitions in the emergency. J. Emerg. Med. 2015;48:508–519. doi: 10.1016/j.jemermed.2014.12.001. [DOI] [PubMed] [Google Scholar]
- 9.Tenney J., Hudson N., Alnifaidy H., Li J.T.C., Fung K.H. Risk factors for aquiring multidrug-resistant organisms in urinary tract infections: A systematic literature review. Saudi Pharm. J. 2018;26:678–684. doi: 10.1016/j.jsps.2018.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Patients O., Donkor E.S. Urinary Tract Infections among Bladder Outlet Obstruction Patients in Accra, Ghana: Aetiology, Antibiotic Resistance, and Risk Factors. Diseases. 2018;6:65. doi: 10.3390/diseases6030065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sangeda R.Z., Paul F., Mtweve D.M. Prevalence of urinary tract infections and antibiogram of uropathogens isolated from children under five attending Bagamoyo District Hospital in Tanzania: A cross-sectional study [version 1; peer review: Awaiting peer review] F1000Res. 2021;10:449. doi: 10.12688/f1000research.52652.1. [DOI] [Google Scholar]
- 12.Forson A.O., Tsidi W.B., Adjei D.N., Quarchie M.N., Nkrumah N.O. Escherichia coli bacteriuria in pregnant women in Ghana: Antibiotic resistance patterns and virulence factors. BMC Res. Notes. 2018;11:1–7. doi: 10.1186/s13104-018-3989-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gambrah E., Owusu-ofori A., Biney E., Oppong C., Cof S.E. Diagnosis and treatment of urinary tract infections in hospitalized adults in Ghana: The role of the clinical microbiology laboratory in improving antimicrobial stewardship. Int. J. Infect. Dis. 2020;102:497–500. doi: 10.1016/j.ijid.2020.10.068. [DOI] [PubMed] [Google Scholar]
- 14.Horlortu P.Z., Dayie N.T.K.D., Obeng-nkrumah N., Labi A. Community acquired urinary tract infections among adults in Accra, Ghana. Infect. Drug Resist. 2019;12:2059–2067. doi: 10.2147/IDR.S204880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yevutsey S.K., Buabeng K.O., Aikins M., Anto B.P., Biritwum R.B., Frimodt-Møller N., Gyansa-Lutterodt M. Situational analysis of antibiotic use and resistance in Ghana: Policy and regulation. BMC Public Health. 2017;17:896. doi: 10.1186/s12889-017-4910-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Global Action Plan on Antimicrobial Resistance. [(accessed on 20 August 2022)]. Available online: https://apps.who.int/iris/bitstream/handle/10665/193736/9789241509763_eng.pdf?sequence=1.
- 17.Agyekum E.B., Amjad F., Mohsin M., Ansah M.N.S. A bird’s eye view of Ghana’s renewable energy sector environment: A Multi-Criteria Decision-Making approach. Util. Policy. 2021;70:101219. doi: 10.1016/j.jup.2021.101219. [DOI] [Google Scholar]
- 18.Ministry of Health|Ghana official website [internet] Role and function. 2015. [(accessed on 20 August 2021)]. Available online: https://dhsprogram.com/pubs/pdf/spa6/02chapter02.pdf.
- 19.Ministry of Health-Ghana National Drugs Programme (GNDP) Standard Treatment Guidelines. 2017 Ministry of Health; Accra, Ghana: 2017. pp. 401–403. [Google Scholar]
- 20.Prashanth B.V.S. Urine Culture Contamination: A One-Year Retrospective Study at the Tertiary Care Hospital. 29 December 2014. [(accessed on 5 November 2021)]. Available online: https://go.gale.com/ps/i.do?id=GALE%7CA469639434&sid=googleScholar&v=2.1&it=r&linkaccess=abs&issn=22784748&p=HRCA&sw=w&userGroupName=anon~70fd146c.
- 21.Altheide S.T. Biochemical and Culture-Based Approaches to Identification in the Diagnostic Microbiology Laboratory. [(accessed on 5 November 2021)]. Available online: http://clsjournal.ascls.org/content/early/2020/01/20/ascls.119.001875.
- 22.Antimicrobial Susceptibility Testing by the Kirby-Bauer Disc Diffusion Method. [(accessed on 5 November 2021)]. Available online: http://www.annclinlabsci.org/content/3/2/135.short. [PubMed]
- 23.CLSI. Dolinsky A.L., Ohiro R.K., Fan W., Xiao C., Wu F. National Committee for Clinical Laboratory Standards. 2000. Performance standard for antimicrobial susceptibility testing. Document M100–S10. [(accessed on 30 October 2022)];J. Int. Med. Res. 2019 46:18. Available online: http://www.epa.gov/nerlcwww/1604sp02.pdf%0Ahttp://www.emeraldinsight.com/doi/10.1108/08876049410065598%0Ahttps://clsi.org/media/1469/m100s27_sample.pdf%0Ahttp://shop.clsi.org/site/Sample_pdf/M100S27_sample.pdf. [Google Scholar]
- 24.Magiorakos A.-P., Srinivasan A., Carey R.B., Carmeli Y., Falagas M.E., Giske C.G., Harbarth S., Hindler J.F., Kahlmeter G., Olsson-Liljequist B., et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: An international expert proposal for interim standard definitions for acquired resistance. Clin. Microbiol. Infect. 2012;18:268–281. doi: 10.1111/j.1469-0691.2011.03570.x. [DOI] [PubMed] [Google Scholar]
- 25.McNutt L.A., Wu C., Xue X., Hafner J.P. Estimating the relative risk in cohort studies and clinical trials of common outcomes. Am. J. Epidemiol. 2003;157:940–943. doi: 10.1093/aje/kwg074. [DOI] [PubMed] [Google Scholar]
- 26.De Rosa R., Grosso S., Lorenzi G., Bruschetta G., Camporese A. Evaluation of the new Sysmex UF-5000 fl uorescence fl ow cytometry analyser for ruling out bacterial urinary tract infection and for prediction of Gram negative bacteria in urine cultures. Clin. Chim. Acta. 2018;484:171–178. doi: 10.1016/j.cca.2018.05.047. [DOI] [PubMed] [Google Scholar]
- 27.Wojno K.J., Baunoch D., Luke N., Opel M., Korman H., Kelly C., Jafri S.M.A., Keating P., Hazelton D., Hindu S., et al. Multiplex PCR Based Urinary Tract Infection (UTI) Analysis Compared to Traditional Urine Culture in Identifying Significant Pathogens in Symptomatic Patients. Urology. 2019;136:119–126. doi: 10.1016/j.urology.2019.10.018. [DOI] [PubMed] [Google Scholar]
- 28.Jalil M.B., Al Atbee M.Y.N. The prevalence of multiple drug resistance Escherichia coli and Klebsiella pneumoniae isolated from patients with urinary tract infections. J. Clin. Lab. Anal. 2022;36:e24619. doi: 10.1002/jcla.24619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rizwan M., Akhtar M., Najmi A.K., Singh K., Res D., Delhi N. Escherichia coli and Klebsiella pneumoniae Sensitivity/Resistance Pattern Towards Antimicrobial Agents in Primary and Simple Urinary Tract Infection Patients Visiting University Hospital of Jamia Hamdard New Delhi. Drug Res. 2018;68:415–420. doi: 10.1055/a-0576-0079. [DOI] [PubMed] [Google Scholar]
- 30.Maredia N.N., Fanning M.J., Christie A.L., Prokesch B.C., Zimmern P.E. Adverse effects of chronic nitrofurantoin therapy in women with recurrent urinary tract infections in an outpatient setting. World J. Urol. 2020;39:2597–2603. doi: 10.1007/s00345-020-03464-w. [DOI] [PubMed] [Google Scholar]
- 31.Madani Y., Mann B. Nitrofurantoin-induced lung disease and prophylaxis of urinary tract infections. Nat. Publ. Gr. 2012;21:337–341. doi: 10.4104/pcrj.2012.00059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sugianli A.K., Ginting F., Parwati I., de Jong M.D., van Leth F. Antimicrobial resistance among uropathogens in the Asia-Pacific region: A systematic review. JAC-Antimicrob. Resist. 2021;3:dlab003. doi: 10.1093/jacamr/dlab003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gekenidis M., Kläui A., Smalla K., Drissner D. Transferable Extended-Spectrum β-Lactamase (ESBL) Plasmids in Enterobacteriaceae from Irrigation Water. Microorganisms. 2020;8:978. doi: 10.3390/microorganisms8070978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Simmering J.E., Tang F., Cavanaugh J.E., Polgreen L.A., Polgreen P.M. The Increase in Hospitalizations for Urinary Tract Infections and the Associated Costs in the United States, 1998–2011. pen Forum Infect. Dis. 2017;4:ofw281. doi: 10.1093/ofid/ofw281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pujades-rodriguez M., West R.M., Wilcox M.H., Sandoe J. Lower Urinary Tract Infections: Management, Outcomes and Risk Factors for Antibiotic Re-prescription in Primary Care. EClinicalMedicine. 2019;14:23–31. doi: 10.1016/j.eclinm.2019.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Health H.F., Suson K.D., Health H.F. Henry Ford Health Scholarly Commons Re: Luke Harper, T. Blanc, M. Peycelon; et al. Circumcision and Risk of Febrile Urinary Tract Infection in Boys with Posterior Urethral Valves: Result of the CIRCUP Randomized Trial. Eur. Urol. Lett. Ed. 2021;81:64–72. doi: 10.1016/j.eururo.2021.08.024. [DOI] [PubMed] [Google Scholar]
- 37.Klaus R., Lange-sperandio B. Chronic Kidney Disease in Boys with Posterior Urethral Valves–Pathogenesis, Prognosis and Management. Biomedicines. 2022;10:1894. doi: 10.3390/biomedicines10081894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nicolle L.E. Catheter Associated Urinary Tract Infections. 2014. [(accessed on 20 August 2022)]. pp. 1–8. Available online: https://aricjournal.biomedcentral.com/articles/10.1186/2047-2994-3-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Von Elm E., Altman D.G., Egger M., Pocock S.J., Gøtzsche P.C., Vandenbroucke J.P. The Strengthening the Reporting of Observational Studies in Epidemiology ( STROBE ) statement: Guidelines for reporting observational studies. BMJ. 2007;335:1453–1457. doi: 10.1097/EDE.0b013e3181577654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sugianli A.K., Ginting F., Kusumawati R.L., Parwati I., De Jong M.D., Van Leth F., Schultsz C. Laboratory-based versus population-based surveillance of antimicrobial resistance to inform empirical treatment for suspected urinary tract infection in Indonesia. PLoS ONE. 2020;15:e0230489. doi: 10.1371/journal.pone.0230489. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data presented in this study are available on request from the corresponding author.