SUMMARY
OBJECTIVES:
The aim of this study was to evaluate the epidemiology of varicose vein stripping in Brazil’s largest city, São Paulo.
METHODS:
Open and anonymous data regarding varicose vein surgeries between 2008 and 2018 were evaluated from the TabNet platform of the Municipal Health Secretary of São Paulo, Brazil.
RESULTS:
Most patients were female and adults. A total of 66,577 varicose vein surgeries were performed in public hospitals and outpatient clinics in São Paulo, with a statistically significant increase for both unilateral (p=0.003) and bilateral (p<0.001) procedures. Since 2016, unilateral procedures have been performed more frequently than bilateral procedures. Most procedures were associated with same-day (54.8%) or next-day (32%) discharge. The in-hospital mortality rate was 0.0045%. The total amount reimbursed was $20,693,437.94, corresponding to a mean value of $310.82 per procedure.
CONCLUSION:
Surgeries to treat chronic vein disease totaled 66,577 in 11 years, demanding $20,693,437.94 from the public health system. The majority of treated patients were female, over 40 years of age, and local residents. Procedure rates have increased over the years. The in-hospital mortality rate was very low (0.0045%).
Keywords: Big data, Varicose veins, Database, Epidemiology, Vascular diseases
INTRODUCTION
Chronic venous disease (CVD) is a spectral and progressive disease, ranging from mild presentations, such as telangiectasia, reticular, and varicose veins, to severe complications, including venous thrombosis, varicorrhage, and skin alterations such as ochre dermatitis and venous ulcers 1,2,3 .
In the United States, the estimated prevalence of CVD is approximately 23% of the adult population 1 , while in Brazil, it is estimated at 47.6% 4 , and these numbers are expected to increase as the population ages 5 .
Therapeutic options for CVD range from conservative measures to invasive procedures. Conservative measures include lifestyle changes, encompassing weight loss, physical activity, and compressive therapy, whereas invasive procedures include sclerotherapy, endovenous ablation, and surgery.
Varicose vein stripping (VVS) refers to collateral phlebectomies through staggered incisions combined with eventual high ligation and removal of the saphenous vein. Even though endovenous ablation of saphenous vein and hybrid procedures are becoming more popular 6,7 , VVS is still the most performed treatment for CVD in Brazilian public hospitals and outpatient clinics 8 as it is in other countries, such as China 9 .
Despite being the most commonly performed surgical treatment for the most common vascular disease 10 , whose burden is estimated to progressively increase in the coming years 5 , there are only a few population-based studies on statistics referring to VVS for CVD treatment. One nationwide study observed a slight downward trend in VVS rates, a very low mortality rate, and low reimbursement. However, demographics of the patients, which may impact the surgery and mortality rates, and length of intensive care unit (ICU) and hospital stay, which may affect hospitals’ revenue, were not evaluated 8 .
Therefore, we designed the present study to evaluate the epidemiology of VVS performed between 2008 and 2018 in public hospitals in Brazil’s largest city, São Paulo, which has an estimated population of more than 12 million 11 , of which 5 million depend exclusively on the public health system 12 . In addition to being the largest and most populous city, the Municipal Health Secretary of São Paulo database provides the most detailed health data 13 , yielding more information than the national database, including demographics and hospital and ICU length of stay.
METHODS
Data were retrieved from the TabNet platform, a public health information application developed by DATASUS, the Health Informatics Department of the Brazilian Ministry of Health 14 . The TabNet system provides open and anonymous data regarding procedures performed within the Brazilian public health system, by hospitals adequately accredited as vascular surgery centers. Such accreditation is a prerequisite for government reimbursement.
This study was approved by the Ethics Committee of the institution where it was conducted. Since data are anonymous, the Institutional Revision Board (IRB) waived the application of informed consent forms.
Statistics referring to varicose vein surgeries between 2008 and 2018 were selected from the TabNet platform of the Municipal Health Secretary of São Paulo, Brazil. Among the selections, analysis included gender, age, municipality of residence, number and types of procedures performed, in-hospital mortality, length of hospital stay, ICU stay, and reimbursement by the public health system.
Two procedures were evaluated for the treatment of varicose veins, according to coding as established by the management system for procedures and medications of the Brazilian public health system – SIGTAP (Sistema de Gerenciamento da Tabela de Procedimentos, Medicamentos e OPM): bilateral surgical treatment of varicose veins (04.06.02.056-6) and unilateral surgical treatment of varicose veins (04.06.02.057-4).
All data were collected from public access sites through computer programs of automated content access (web scraping). These automated navigation codes were programmed in the Python language (v. 2.7.13, Beaverton, OR, USA) using the Windows 10 Single Language operational system.
The data collection, platform field selection, and table adjustment steps were performed using the selenium-webdriver packages (v. 3.1.8, Selenium HQ, several collaborators worldwide) and pandas (v. 2.7.13, Lambda Foundry, Inc. and PyData Development Team, New York, NY, USA). The Mozilla Firefox browser (v. 59.0.2, Mountain, CA, USA) and geckodriver webdriver (v. 0.18.0, Mozilla Corp., Bournemouth, England) were used.
Following collection and treatment, data were organized and grouped in spreadsheets using the Microsoft Office Excel 2016® (v. 16.0.4456.1003, Redmond, WA, USA) software and analyzed.
Reimbursement values in Brazilian Real (R$, the Brazilian official currency) were converted into US dollars (U$), using the exchange rate of December 31, 2012, the median date between the first and last cases evaluated.
STATISTICAL ANALYSIS
Linear regression was performed to evaluate the trends in the distribution of VVS procedures throughout the years, using the Stata SE® (StataCorp LLC, College Station, TX, USA). The level of statistical significance was set at <0.05.
RESULTS
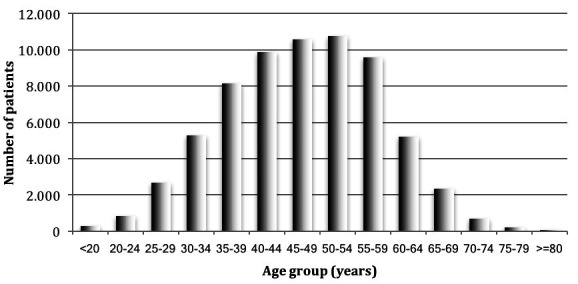
Most patients were female (79.31%). The distribution of age group of patients treated with VVS is shown in Figure 1. Age group distribution was bell-shaped, with peaks between the ages of 35 and 60 years, corresponding to approximately three-quarters of all patients who underwent VVS. Only 5% were elderly, aged 65 years or more; 90.78% of the procedures were performed in patients with a registered residence address in São Paulo.
Figure 1. Distribution of age groups of the patients who underwent varicose vein surgery.
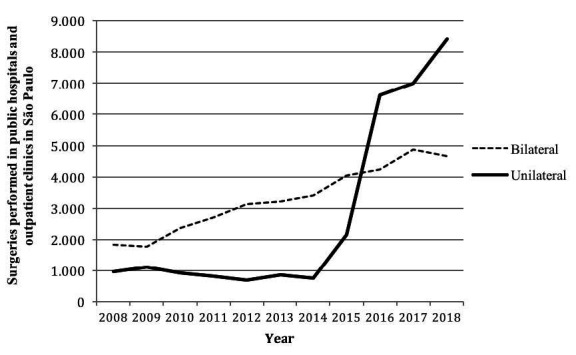
A total of 66,577 VVS to treat CVD were performed in São Paulo from 2008 to 2018, either in public hospitals or outpatient clinics, the proportion of which is unknown. The distribution of unilateral and bilateral VVS to treat CVD over time is depicted in Figure 2. There was a statistically significant upward trend for both unilateral (p=0.003) and bilateral (p<0.001) procedures over time, with a more expressive increase observed for unilateral surgeries (861% increase for unilateral VVS vs. 254% increase for bilateral VVS), which became the most performed procedure from 2016 onward.
Figure 2. Distribution of unilateral and bilateral varicose vein surgeries between 2008 and 2018.
Most procedures were associated with discharge on the same day (54.8%), 32% of procedures were associated with 1 day of hospitalization, and 11.6% with 2 days. Hospital stay longer than 3 days was rare (1.6%).
Regarding the need for ICU stay, only 29 overnight stay was charged throughout the study years.
Three in-hospital deaths were observed throughout the evaluated years. Considering the total of 66,577 procedures, the in-hospital mortality rate was 0.0045%.
The total amount reimbursed by the government for the surgeries during the 11 years evaluated was $20,693,437.94, corresponding to an average amount of $310.82 per procedure.
DISCUSSION
Our demographic data are in agreement with those of previous studies.
Along with a higher prevalence of CVD in women 4,15 , this population possibly seeks treatment more often and/or earlier than men, as female patients comprise the majority of the patients treated for CVD in our population and other studies 16 . Possible explanations for female predominance may involve sociocultural factors, such as a greater concern with health in general and with aesthetics in particular.
Since CVD is progressive, its prevalence is expected to increase with age. We observed a progressive increase in patients’ age of up to 54 years and a decline thereafter, probably due to an increase in the prevalence of comorbidities likewise, elevating surgical risks. Only 5% of the patients were elderly, suggesting that perhaps nonsurgical CVD treatments are being preferentially offered to this group, such as foam sclerotherapy or conservative measures.
As for primary residence address, more than 90% of the patients were domiciled in São Paulo, which is a higher proportion than that observed in a previous report on surgical treatment for cerebrovascular disease in São Paulo 17 . As VVS is a less complex vascular intervention, it does not require referral to highly specialized centers and can be addressed in the city of the primary residence.
The trends for VVS that we observed were upward, consistent with other reports 7 , which is probably a reflection of increasing demand. Although the population of the city of São Paulo increased from 2008 to 2018, this may not fully explain the increase in VVS, as the population increased by 10.8% 11 in the period, while unilateral procedures increased by 861% and bilateral procedures increased by 254%. Thus, we hypothesize that the rise in demand was also influenced by the fact that the growing population of the city of São Paulo is also getting older 11 and more obese 18 , which are important risk factors for CVD 19,20 . This finding contrasts with the national data, as the standardized procedure rates of VVS are not increasing at national level 8 . This difference is unlikely to be fully explained by a higher prevalence of CVD at the municipal level compared to the national level, even on account that the obesity prevalence in São Paulo is one of the lowest for men among other Brazilian capitals and intermediate for women 18 . One possible explanation is that at the municipal level, the public health system is able to meet the increased demand, which may not be happening at the national level. Another possible explanation is that outside São Paulo, foam sclerotherapy to treat CVD is being performed more relatively than VVS.
Unilateral procedures increased faster than bilateral ones, becoming the most frequently performed VVS since 2016, which was also observed in other studies 16,21 . One possible explanation for this change may be the fact that, as VVS has been performed more frequently, the waiting lines may have shortened; hence, more patients may have been treated for less advanced and still unilateral disease. In addition, the population is aging, and unilateral procedures may be safer for older patients with more comorbidities and large varicose veins, as they are expected to feel a greater impact from bleeding.
The low in-hospital mortality rate that we observed (0.0045%) is similar to that observed in the national study (0.0056%). This is likely the result of a low-risk procedure performed on a low-risk patient, as we observed that 95% of the patients were under 65 years of age.
The high proportion of same-day discharges corroborates the safety of the procedure. Early complications that could explain 1.6% of procedures associated with hospital stay for 3 days or more and the three deaths we observed are mainly due to anesthetic complications and bleeding, which have been reported by other authors 21 . Another population-based study that evaluated mortality after surgery to treat CVD was the Japanese Society for Vascular Surgery Report, which did not observe any 30-day death 6 . However, their sample was almost half of ours.
Even though endovenous thermoablations are getting more popular and have shown good results 22,23 , they are not superior to the VVS in all aspects 22,23 , and their initial expenditures may be prohibitively high 24 , given that the use of the endovenous thermoablation adds at least $735 to the procedure while a standard disposable phleboextractor costs $39. Moreover, the Brazilian public health system does not ordinarily reimburse them. It can be argued that endovenous thermoablations have the advantage of earlier postoperative recovery when compared to VVS, thus decreasing the economic burden due to lost workdays 24 . However, so does the treatment with foam sclerotherapy, which is cheaper, with a vial cost of $2, and is a standard treatment reimbursed by the government.
We observed an average amount of $310.82 per VVS for the treatment of CVD, which is a relatively low amount. Considering that the health care burden of CVD is estimated to be 1–2% of the U.S. national budget, with more than $1 billion being spent on wound care alone 25 , public health care strategies should focus on treating CVD earlier by stimulating VVS, especially in outpatient clinics.
Limitations
As inherent in a retrospective analysis with automated data collection, our study is limited by the loss of patient information and eventual miscoding, which should not be significant given the large size of our population.
Another important limitation is that data are anonymous; therefore, we were not able to assess patients’ clinical, etiological, anatomical, and pathological classifications or quality-of-life scores. In addition, we were also not able to perform adjusted analysis, and follow-up was impossible; hence, we do not know the complication rates, the causes of death of the three individuals, and whether there were any VVS-related deaths after discharge, due to pulmonary embolism, for example.
In addition, we were unable to distinguish how many patients were treated, because we only had access to the total number of procedures and some patients may have undergone more than one VVS – two unilateral procedures or even two bilateral procedures, given the long study period. We also do not know how many of the procedures involved saphenous treatment and how much was paid for each type of procedure. Moreover, governmental reimbursement is based on a fixed compensation table and may not reflect actual hospital expenses.
Despite these limitations, this is a comprehensive and detailed epidemiological analysis of VVS for the treatment of CVD, analyzing objective and compulsorily recorded data in the public data. Our findings show patients’ demographics and procedure trends and highlight the safety of the treatment.
CONCLUSION
In a city whose population surpasses that of some European countries, surgeries to treat CVD were frequent and totaled 66,577 in 11 years, demanding $20,693,437.94 from the public health system, which is a relatively low cost.
The majority of treated patients were female, over 40 years of age, and local residents. An increase in the number of procedures was observed over the years, for both unilateral and bilateral procedures. The in-hospital mortality rate was very low (0.0045%).
ACKNOWLEDGMENTS
We thank Claudia Szlejf Jerussalmy for her insights and suggestions for the study design.
Footnotes
Funding: Nickolas Stabellini received an undergraduate research scholarship from Institutional Scientific Initiation Scholarship Program (PIBIC) – process # 800996/2018-6 – granted by the National Council for Scientific and Technological Development (CNPq), Brazil.
REFERENCES
- 1.Hamdan A. Management of varicose veins and venous insufficiency. JAMA. 2012;308(24):2612–21. doi: 10.1001/jama.2012.111352. [DOI] [PubMed] [Google Scholar]
- 2.Lee AJ, Robertson LA, Boghossian SM, Allan PL, Ruckley CV, Fowkes FGR, et al. Progression of varicose veins and chronic venous insufficiency in the general population in the Edinburgh Vein Study. J Vasc Surg Venous Lymphat Disord. 2015;3(1):18–26. doi: 10.1016/j.jvsv.2014.09.008. [DOI] [PubMed] [Google Scholar]
- 3.Porciunculla MM, Leiderman DBD, Altenfeder R, Pereira CSB, Fioranelli A, Wolosker N, et al. Clinical, ultrasonographic and histological findings in varicose vein surgery. Rev Assoc Med Bras (1992) 2018;64(8):729–35. doi: 10.1590/1806-9282.64.08.729. [DOI] [PubMed] [Google Scholar]
- 4.Maffei FH, Magaldi C, Pinho SZ, Lastoria S, Pinho W, Yoshida WB, et al. Varicose veins and chronic venous insufficiency in Brazil: prevalence among 1755 inhabitants of a country town. Int J Epidemiol. 1986;15(2):210–7. doi: 10.1093/ije/15.2.210. [DOI] [PubMed] [Google Scholar]
- 5.Nicolaides AN, Labropoulos N. Burden and suffering in chronic venous disease. Adv Ther. 2019;36(Suppl 1):1–4. doi: 10.1007/s12325-019-0882-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.The Japanese Society for Vascular Surgery Database Management Committee Member, Ncd Vascular Surgery Data Analysis Team Vascular Surgery in Japan: 2014 Annual Report by the Japanese Society for Vascular Surgery. Ann Vasc Dis. 2020;13(4):474–93. doi: 10.3400/avd.ar.20-00128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Prabhakar AM, Misono AS, Sheth RA, Rosenkrantz AB, Hemingway J, Hughes DR, et al. Changing medicare utilization of minimally invasive procedures for the treatment of chronic venous insufficiency. J Vasc Interv Radiol. 2017;28(6):818–24. doi: 10.1016/j.jvir.2017.02.034. [DOI] [PubMed] [Google Scholar]
- 8.Silva MJ, Louzada ACS, Silva MFA, Portugal MFC, Teivelis MP, Wolosker N. Epidemiology of 869,220 varicose vein surgeries over 12 years in Brazil: trends, costs and mortality rate. Ann Vasc Surg. 2022;82:1–6. doi: 10.1016/j.avsg.2021.11.016. [DOI] [PubMed] [Google Scholar]
- 9.Zhang M, Qiu T, Bu X, Li X, Liang G, Zhang H, et al. A national survey on management of varicose veins in China. J Vasc Surg Venous Lymphat Disord. 2018;6(3):338–46.e1. doi: 10.1016/j.jvsv.2017.10.018. [DOI] [PubMed] [Google Scholar]
- 10.Criqui MH, Jamosmos M, Fronek A, Denenberg JO, Langer RD, Bergan J, et al. Chronic venous disease in an ethnically diverse population: the San Diego Population Study. Am J Epidemiol. 2003;158(5):448–56. doi: 10.1093/aje/kwg166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Instituto Brasileiro de Geografia e Estatística Painel de Indicadores | IBGE [Internet] [[cited on Jul 16, 2021]]. Available from: https://www.ibge.gov.br/indicadores.html .
- 12.Ministry of Health of Brazil Agência Nacional de Saúde Suplementar - National Supplementary Health Agency [Internet]. [[cited on Sept 13, 2021]]. Available from: https://www.gov.br/ans/pt-br .
- 13.Municipal Health Secretary of São Paulo M of H of B TabNet Win32 3.0: Internações SUS. DATASUS. [Internet] [[cited on Sept 14, 2021]]. Available from: http://tabnet.saude.sp.gov.br/deftohtm.exe?tabnet/aih_rd2008.def .
- 14.Ministry of Health of Brazil DATASUS [Internet]. [[cited on Jul 15, 2021]]. Available from: http://www2.datasus.gov.br/DATASUS/index.php?area=02 .
- 15.Carpentier PH, Maricq HR, Biro C, Ponçot-Makinen CO, Franco A. Prevalence, risk factors, and clinical patterns of chronic venous disorders of lower limbs: a population-based study in France. J Vasc Surg. 2004;40(4):650–9. doi: 10.1016/j.jvs.2004.07.025. [DOI] [PubMed] [Google Scholar]
- 16.Laurikka J, Sisto T, Auvinen O, Tarkka M, Läärä E, Hakama M. Varicose veins in a Finnish population aged 40-60. J Epidemiol Community Health. 1993;47(5):355–7. doi: 10.1136/jech.47.5.355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stabellini N, Wolosker N, Leiderman DBD, Silva MFA, Nogueira WA, Amaro E, Júnior, et al. Epidemiological Analysis of Carotid Artery Stenosis Intervention during 10 years in the Public Health System in the Largest City in Brazil: Stenting Has Been More Common than Endarterectomy. Ann Vasc Surg. 2020;66:378–84. doi: 10.1016/j.avsg.2019.12.040. [DOI] [PubMed] [Google Scholar]
- 18.Brasil. Ministério da Saúde Vigitel Brasil 2019: vigilância de fatores de risco e proteção para doenças crônicas por inquérito telefônico: estimativas sobre frequência e distribuição sociodemográfica de fatores de risco e proteção para doenças crônicas nas capitais dos 26 estados brasileiros e no Distrito Federal em 2019 [Internet] 2020. [[cited on Jul 30, 2021]]. Available from: https://bvsms.saude.gov.br/bvs/publicacoes/vigitel_brasil_2019_vigilancia_fatores_risco.pdf .
- 19.Davies HO, Popplewell M, Singhal R, Smith N, Bradbury AW. Obesity and lower limb venous disease - The epidemic of phlebesity. Phlebology. 2017;32(4):227–33. doi: 10.1177/0268355516649333. [DOI] [PubMed] [Google Scholar]
- 20.Ribeiro AL, Duncan BB, Brant LC, Lotufo PA, Mill JG, Barreto SM. Cardiovascular health in Brazil: trends and perspectives. Circulation. 2016;133(4):422–33. doi: 10.1161/CIRCULATIONAHA.114.008727. [DOI] [PubMed] [Google Scholar]
- 21.Miller GV, Lewis WG, Sainsbury JR, Macdonald RC. Morbidity of varicose vein surgery: auditing the benefit of changing clinical practice. Ann R Coll Surg Engl. 1996;78(4):345–9. [PMC free article] [PubMed] [Google Scholar]
- 22.Mendes C, Martins A, Fukuda J, Parente J, Munia M, Fioranelli A, et al. Randomized trial of radiofrequency ablation versus conventional surgery for superficial venous insufficiency: if you don’t tell, they won’t know. Clinics (Sao Paulo). 2016;71(11):650–6. doi: 10.6061/clinics/2016(11)06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lurie F, Creton D, Eklof B, Kabnick LS, Kistner RL, Pichot O, et al. Prospective randomised study of endovenous radiofrequency obliteration (closure) versus ligation and vein stripping (EVOLVeS): two-year follow-up. Eur J Vasc Endovasc Surg. 2005;29(1):67–73. doi: 10.1016/j.ejvs.2004.09.019. [DOI] [PubMed] [Google Scholar]
- 24.Rautio T, Ohinmaa A, Perälä J, Ohtonen P, Heikkinen T, Wiik H, et al. Endovenous obliteration versus conventional stripping operation in the treatment of primary varicose veins: a randomized controlled trial with comparison of the costs. J Vasc Surg. 2002;35(5):958–65. doi: 10.1067/mva.2002.123096. [DOI] [PubMed] [Google Scholar]
- 25.Kim Y, Png CYM, Sumpio BJ, DeCarlo CS, Dua A. Defining the human and health care costs of chronic venous insufficiency. Semin Vasc Surg. 2021;34(1):59–64. doi: 10.1053/j.semvascsurg.2021.02.007. [DOI] [PubMed] [Google Scholar]


