Abstract
Introduction:
More than 10% of U.S. young adults have smoked waterpipe tobacco in the past month and >25% of those who have never smoked are susceptible. We tested messages designed to prevent and reduce waterpipe tobacco smoking (WTS).
Methods:
In 2020, we recruited 830 U.S. young adults (18-30 years) who had never smoked waterpipe tobacco and were susceptible or currently smoked waterpipe tobacco for an online study. We randomized participants to intervention messages about the risks of WTS or control messages unrelated to tobacco. Participants had up to four message exposures over 12 weeks and completed two-, four-, and six- month follow-ups. Outcomes were WTS initiation and curiosity (susceptible never smokers), WTS frequency, cessation, motivation to quit (those who currently smoked), and WTS risk perceptions.
Results:
Intervention messages increased perceived addictiveness of WTS at two months (β=0.27; 95% CI: 0.11, 0.43) in susceptible never smokers. There were no significant intervention effects in those who currently smoked. Exploratory analyses among intervention participants showed that higher dose of message exposure decreased WTS initiation at six months in susceptible never smokers (RR=0.68; 95% CI: 0.48, 0.96) and decreased WTS frequency (IRR=0.84; 95% CI: 0.73, 0.97) and increased cessation (RR=1.31; 95% CI: 1.07, 1.59) at six months in those who smoked.
Conclusions:
Although the WTS intervention messages had few significant effects on outcomes overall, a higher dose of message exposure affected behavioral outcomes in the intervention arm. Findings highlight the need to identify effective message content and optimal message dose, especially for digital media campaigns.
Keywords: Waterpipe tobacco, hookah, young adults, media, communication, prevention
INTRODUCTION
Young adults (18-30 years) comprise most U.S. waterpipe tobacco smokers,1,2 with 11% reporting past 30-day use2 and >25% who have never smoked waterpipe tobacco susceptible to initiation (i.e., open to trying waterpipe tobacco).3 Young adults initiate and sustain waterpipe tobacco smoking (WTS) due to factors including appealing flavors, the social nature of WTS, and misperceptions that WTS is not harmful or addictive.4-8 However, WTS exposes young people to harmful toxicants and increases risks of negative health outcomes, nicotine addiction, and subsequently smoking cigarettes.9 Interventions are needed to prevent and reduce WTS in young adults.
The U.S. Food and Drug Administration (FDA) can use public education media campaigns to address young adults’ WTS as they have with cigarettes10,11 and e-cigarettes,12 but there is limited research on WTS messaging to guide campaigns. Studies have investigated messages for warning labels and point-of-sale communication for WTS.13-17 Messages about risks of health harms and addiction can decrease intentions to smoke in susceptible never smokers, increase motivation to quit in those who smoke, and increase risk perceptions.8,18-20 However, studies testing messages in those who have never smoked but are susceptible are limited,5 and others tested messages as part of cessation interventions for those who currently smoke.21
Media campaigns are an evidence-based intervention for preventing and reducing tobacco use11,22-24 and, in the past, have relied primarily on television.23 Recent campaigns have shifted to digital media (e.g., mobile, social media)25-27 due to the potential for high reach in populations such as young adults.28,29 As campaigns shift from traditional to digital media, the amount of message exposure (i.e., dose, or how many times a person should see campaign messages)needed to achieve intended effects is an important consideration. Decisions about message dose are usually determined in the media buying process based on recommendations using gross ratings points, or the percent of the audience reached multiplied by the number of times they are exposed to the message.23 Public health agencies provide recommendations for campaign dose using traditional media,23 and outcomes are improved (e.g., higher smoking quit attempts) when campaigns achieve adequate dose through repeated message exposure.30-36 One recent study tested the effects of a campaign communicating chemical constituents in WTS to youth and young adults at the point-of-sale (e.g., convenience stores),37 finding limited effects on target outcomes. The researchers attributed this to the low observed dose of exposure, highlighting the importance of additional research on dose of exposure for WTS messaging.37
Recent FDA tobacco campaigns have relied heavily on digital media but had limited impact on intended outcomes.25-27 Discussions about these limited effects have focused on message dose, specifically the lack of evidence to inform decisions about message dose for digital media.25-27 Examining how the dose of message exposure for WTS and other tobacco-related messages affects intended outcomes can inform future campaign implementation decisions. This randomized trial addressed gaps in the WTS intervention research by examining the effects of WTS messaging among young adults who never smoked waterpipe tobacco and were susceptible or reported current WTS and by exploring message dose effects. We hypothesized that exposure to intervention messages would decrease WTS initiation among susceptible never smokers and increase cessation in those who smoked.
METHODS
This was a two-arm, parallel group randomized trial. The trial was preregistered (NCT04252014), all participants provided informed consent, and the participating institutions’ institutional review boards approved procedures.
Participants
In 2020, we recruited participants from the National Opinion Research Council (NORC) AmeriSpeak research panel. NORC uses probability-based sampling to recruit AmeriSpeak panel members using the NORC National Frame and address-based sampling frames.38 At the time of the study, the panel included nearly 49,000 households and the household recruitment rate was 34%.38
NORC invited potential participants using targeted enrollment quotas based on U.S. population data for age, race, Hispanic ethnicity, education, and sex and accounting for estimated differential completion by demographic groups. Potential participants received an email invitation describing the study with a link to an online eligibility screener. Eligible participants were AmeriSpeak panel members who were young adults aged 18 to 30 years, able to complete study procedures online in English and either: 1) reported smoking waterpipe tobacco in the past 30 days; or 2) had never smoked waterpipe tobacco but were susceptible to initiating WTS based on responses to a valid, 4-item susceptibility measure.5 Eligible participants provided online informed consent to complete enrollment. Our enrollment targets were informed by data indicating WTS initiation rates of 4%-7%39-41 and cessation rates of 25%-47%21-40-42 in U.S. young adults. Based on these, the trial was positioned to detect absolute differences between arms ranging from 4%-7% for initiation and 11%-14% for cessation with 80% power and α=0.05.
Procedures
Participants completed a baseline assessment online with measures of WTS and baseline trial outcomes. Then participants were randomized 1:1 to either an intervention arm or control arm. Randomization was stratified by WTS status (those who never smoked and were susceptible, those reporting current WTS) to ensure balance by the trial arms.
Participants received 4 message exposures for the arm to which they were randomized. Messages were delivered online starting 2 weeks after baseline, and participants responded to brief questions about the message content. The message exposures occurred 3 weeks apart to ensure adequate time for participants to view them. During this time participants received reminders to view the messages and answer the questions about message content. If participants did not do so after reminders were exhausted, the exposure closed, and the next message was delivered. We based the duration and frequency of message exposure on recommendations for message testing research43,44 and pragmatic considerations above (e.g., time for reminders).
All participants completed follow-up assessments online capturing outcomes two months, four months, and six months after the exposure period. Participants received reminders to complete each follow up. Participants received monetary incentives from NORC for completing each assessment.
We pretested procedures with small sample of eligible participants to ensure functionality and check data quality. After pretesting, we began trial recruitment. For the trial, NORC used several data quality control measures including removing participants who completed the baseline assessment in < 25% of the median completion time, who skipped > 50% of baseline items, and who chose the same response options for baseline question blocks (i.e., straight line reporting).
Intervention Arm
Intervention messages communicated the risks of health harm and addiction of WTS, targeted young adults’ beliefs about the risks of WTS, and addressed flavors and social use, major factors contributing to the appeal of WTS.45,46 We developed message text and imagery using an iterative process of expert feedback and revision, and we pretested the text and imagery in studies capturing self-report and psychophysiological outcomes.45,46 Using these data, we identified 4 messages for the intervention arm from the set of messages tested.47 Each message consisted of evidence-based risk information in lay language with background imagery relevant to the message content, including a waterpipe, a social waterpipe smoking setting, a smoke cloud, and a smoke ring.45-47 The Supplementary Figure shows the intervention messages. The order of the messages was randomized across the exposures.
Control Arm
Participants randomized to the control arm viewed messages about skin cancer prevention at each brief survey based on prior work demonstrating it is an appropriate contact-matched control arm.48 Messages communicated skin cancer risks from sun exposure and indoor tanning.48 They were consistent with intervention messages with respect to font, text, and visuals. The order of messages was randomized across the exposures.
Measures
Baseline characteristics from participants’ AmeriSpeak profiles included sex, age, race, ethnicity, educational attainment, and household income. Baseline measures captured current cigarette smoking and past 30-day use of electronic cigarettes, cigars, little cigars, cigarillos, and smokeless tobacco.49 We summarized these as any other tobacco use to characterize participants. We also captured past 30 day use of alcohol and marijuana at baseline (yes/no).49
At eligibility screening, we measured if participants had ever smoked waterpipe tobacco and, among those who endorsed lifetime WTS, past 30-day use.20 Among those who never smoked, we measured susceptibility with a valid four item measure.5 At baseline, among those who reported WTS we measured past 30-day frequency of WTS1 and administered the six item Waterpipe Tobacco Dependence Scale (score range 0-25).50
The primary outcomes were WTS initiation among those who never smoked and were susceptible and WTS cessation and frequency among those reporting current WTS. Secondary outcomes were WTS curiosity (susceptible never smokers) and motivation to quit (those reporting current WTS). Other outcomes were WTS risk perceptions among all participants. These were measured at all follow-ups.
Among participants who never smoked and were susceptible, we measured initiation by assessing if participants had ever smoked waterpipe tobacco1 and we measured curiosity about WTS on a 1 (not at all) to 7 (very) scale.8,19 Among participants reporting current WTS, we measured if they quit WTS by asking if they had smoked waterpipe tobacco since the last assessment and, among those responding no, if they had completely stopped smoking waterpipe tobacco (yes/no).21 Among those who had not quit, we captured WTS frequency in the past 30 days and motivation to quit on a 1 (not at all) to 7 (very) scale.21
We captured perceived harm of WTS relative to cigarettes (1 = much less harmful to 5 = much more harmful), perceived likelihood of harm from WTS (1 = no chance to 7 = certain to happen), worry about harm (1 = not at all, 7 = very much), perceived addictiveness relative to cigarettes (1 = much less addictive to 5 = much more addictive), perceived likelihood of addiction (1 = no chance to 7 = certain to happen), and worry about addiction (1 = not at all to 7 = very much).20,21
Statistical Analysis
We completed statistical analyses using Stata/SE version 17 (College Station, TX). We stratified all analyses by WTS status. First, we calculated descriptive statistics overall and according to intervention assignment. Next, we evaluated the pattern and predictors of missing data due to attrition by WTS status. The missing data pattern was not monotone (i.e., participants were permitted to miss a follow-up but complete a later follow-up). Missingness was associated with several baseline variables, indicating data were missing at random, and there was a small (<4%) proportion of item missingness within otherwise complete surveys. We completed multiple imputation by chained equations creating 25 imputed data sets for each WTS user status group.51 We used logistic regression to impute binary outcomes and truncated linear regression to impute continuous outcomes maintaining imputed values within the range of the item’s response options. We completed imputation at each timepoint sequentially and included variables associated with missingness for each WTS status group as well as intervention assignment.52,53
After completing multiple imputation, we examined the effect of intervention assignment on study outcomes, combining results across the 25 datasets using Rubin’s rule.54 Separate models estimated associations between intervention assignment and outcomes at each follow-up. We estimated risk ratios (RRs) and 95% confidence intervals (CIs) for binary outcomes using Poisson regression with robust standard errors,55 mean differences and 95% CIs for continuous outcomes using linear regression, and incidence rate ratios (IRRs) and 95% CIs for the count of days participants smoked waterpipe using negative binomial regression.
Finally, exploratory analyses examined the effect of dose on study outcomes among participants randomized to the intervention arm. We used similar models but included dose as a continuous predictor ranging from 0-4 exposures. We checked linearity of dose in each model using fractional polynomials.
RESULTS
Sample Characteristics
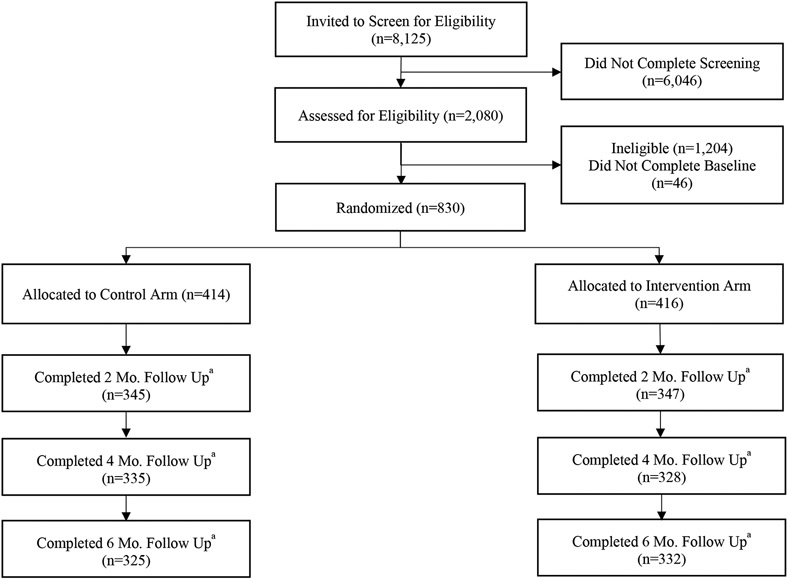
We invited 8125 individuals to screen for eligibility, and 2080 (25.6%) completed screening (Figure 1). Of those, 830 were eligible, completed baseline, and were randomized (414 to the control arm, 416 to the intervention arm). A total of 692 (83.4%) participants completed the two-month follow-up, 663 (79.9%) completed the four-month follow-up, and 657 (79.2%) completed the six-month follow-up. Retention did not differ significantly by intervention assignment (two months: χ2 (1)=0.001; p=0.98; four months: χ2 (1)=0.55; p=0.46; six months: χ2 (1)=0.21; p=0.64).
Figure 1. Flow diagram for randomized trial of a waterpipe tobacco messaging intervention for young adults: United States, 2020.
a Attrition at the two or four month time points did not make participants ineligible at later time points. All randomized participants were retained in analyses using multiple imputation.
A total of 301 participants had never smoked waterpipe and were susceptible, and 529 participants reported current WTS (Table 1). Among those who never smoked and were susceptible, 60.8% were female, 78.7% attended some college or earned a bachelor’s degree, and 58.8% had an annual household income <$50,000. Approximately half (46.8%) were 18- to 24-years-old, two-thirds (68.2%) drank alcohol in the past 30 days, 39.4% used marijuana, and 26.5% used other tobacco or e-cigarettes. At baseline, those who never smoked and were susceptible had low curiosity about WTS (M=2.75, SD=1.68).
Table 1.
Baseline participant characteristics stratified by waterpipe tobacco smoking status and intervention assignmenta
| Susceptible Never Smokers |
Current Waterpipe Tobacco Smokers |
|||||||
|---|---|---|---|---|---|---|---|---|
| Full sample N=301 |
Intervention N=149 |
Control N=152 |
p- value |
Full sample N=529 |
Intervention N=267 |
Control N=262 |
p- value |
|
|
|
|
|
|
|
|
|
|
|
| Gender, N (%) | 0.71 | 0.37 | ||||||
| Female | 183 (60.8) | 89 (59.7) | 94 (61.8) | 323 (61.1) | 158 (59.2) | 165 (63.0) | ||
| Male | 118 (39.2) | 60 (40.3) | 58 (38.2) | 206 (38.9) | 109 (40.8) | 97 (37.0) | ||
| Age, N (%) | 0.85 | 0.33 | ||||||
| 18-24 | 141 (46.8) | 69 (46.3) | 72 (47.4) | 199 (37.6) | 95 (35.6) | 104 (39.7) | ||
| 25-30 | 160 (53.2) | 80 (53.7) | 80 (52.6) | 330 (62.4) | 172 (64.4) | 158 (60.3) | ||
| Race and ethnicity, N (%) | 0.80 | 0.31 | ||||||
| White non-Hispanic | 112 (37.2) | 55 (36.9) | 57 (37.5) | 141 (26.7) | 80 (30.0) | 61 (23.3) | ||
| Black non-Hispanic | 65 (21.6) | 30 (20.1) | 35 (23.0) | 162 (30.6) | 80 (30.0) | 82 (31.3) | ||
| Other/Multiple non-Hispanic | 66 (21.9) | 36 (24.2) | 30 (19.7) | 83 (15.7) | 37 (13.9) | 46 (17.6) | ||
| Hispanic | 58 (19.3) | 28 (18.8) | 30 (19.7) | 143 (27.0) | 70 (26.2) | 73 (27.9) | ||
| Education, N (%) | 0.18 | 0.38 | ||||||
| No college | 64 (21.3) | 30 (20.1) | 34 (22.4) | 171 (32.3) | 89 (33.3) | 82 (31.3) | ||
| Some college | 141 (46.8) | 64 (43.0) | 77 (50.7) | 233 (44.1) | 110 (41.2) | 123 (47.0) | ||
| Bachelors’ degree or higher | 96 (31.9) | 55 (36.9) | 41 (27.0) | 125 (23.6) | 68 (25.5) | 57 (21.8) | ||
| Household income, N (%) | 0.27 | 0.24 | ||||||
| <$50,000 | 177 (58.8) | 93 (62.4) | 84 (55.3) | 339 (64.1) | 167 (62.6) | 172 (65.7) | ||
| $50,000 to $99,999 | 79 (26.3) | 33 (22.2) | 46 (30.3) | 138 (26.1) | 68 (25.5) | 70 (26.7) | ||
| ≥$100,000 | 45 (15.0) | 23 (15.4) | 22 (14.5) | 52 (9.8) | 32 (12.0) | 20 (7.6) | ||
| Alcohol use in past 30 days, N (%) | 0.73 | 0.50 | ||||||
| Yes | 202 (68.2) | 101 (69.2) | 101 (67.3) | 432 (82.9) | 216 (81.8) | 216 (84.1) | ||
| No | 94 (31.8) | 45 (30.8) | 49 (32.7) | 89 (17.1) | 48 (18.2) | 41 (16.0) | ||
| Marijuana use in past 30 days, N (%) | 0.11 | 0.39 | ||||||
| Yes | 52 (39.4) | 18 (31.6) | 34 (45.3) | 285 (73.1) | 147 (75.0) | 138 (71.1) | ||
| No | 80 (60.6) | 39 (68.4) | 41 (54.7) | 105 (26.9) | 49 (25.0) | 56 (28.9) | ||
| Current use of other tobacco, N (%) | 0.84 | 0.97 | ||||||
| Yes | 79 (26.5) | 40 (27.0) | 39 (26.0) | 326 (62.2) | 164 (62.1) | 162 (62.3) | ||
| No | 219 (73.5) | 108 (73.0) | 111 (74.0) | 198 (37.8) | 100 (37.9) | 98 (37.7) | ||
| Perceived harm of WTS relative to cigarettes, M (SD)b | 2.90 (0.85) | 2.83 (0.80) | 2.97 (0.89) | 0.17 | 2.85 (1.11) | 2.83 (1.11) | 2.86 (1.10) | 0.80 |
| Perceived likelihood of harm from WTS, M (SD)c | 4.50 (1.26) | 4.43 (1.16) | 4.57 (1.35) | 0.33 | 4.07 (1.58) | 3.96 (1.68) | 4.18 (1.47) | 0.11 |
| Worry about harm from WTS, M (SD)d | 4.57 (1.77) | 4.53 (1.73) | 4.60 (1.81) | 0.73 | 3.95 (2.08) | 3.83 (2.12) | 4.07 (2.04) | 0.19 |
| Perceived addictiveness of WTS relative to cigarettes, M (SD)b | 2.81 (0.82) | 2.86 (0.80) | 2.76 (0.84) | 0.28 | 2.60 (1.11) | 2.56 (1.13) | 2.65 (1.09) | 0.38 |
| Perceived likelihood of addiction to WTS, M (SD)c | 4.08 (1.47) | 4.03 (1.45) | 4.14 (1.49) | 0.51 | 3.55 (1.79) | 3.60 (1.77) | 3.50 (1.80) | 0.54 |
| Worry about addiction to WTS, M (SD)d | 3.98 (1.91) | 4.00 (1.85) | 3.97 (1.97) | 0.88 | 3.34 (2.11) | 3.28 (2.15) | 3.39 (2.07) | 0.57 |
| Curiosity about WTS, M (SD)d | 2.75 (1.68) | 2.77 (1.67) | 2.74 (1.69) | 0.87 | - | - | - | - |
| Motivation to quit WTS, M (SD)d | - | - | - | - | 4.33 (2.31) | 4.37 (2.33) | 4.29 (2.30) | 0.67 |
| WTS dependence, M (SD)e | - | - | - | - | 2.69 (2.11) | 2.81 (2.07) | 2.57 (2.14) | 0.20 |
| Past 30-day WTS frequency, M(SD) | - | - | - | - | 4.02 (5.57) | 4.08 (5.92) | 3.96 (5.2) | 0.81 |
Note: Percentages might not sum to 100 due to rounding. Participant counts might not sum to the total sample size due to missing data.
Abbreviations: WTS = Waterpipe tobacco smoking, M=Mean, SD=Standard deviation
Data were collected online in 2020.
Response options: 1=Much less to 5=Much more
Response options: 1=No chance to 7=Certain to happen
Response options: 1=Not at all to 7=Very
Sum scores ranged from 0 to 6.
In those reporting current WTS, 61.1% were female, 67.7% attended some college or earned a bachelor’s degree, and 64.1% had an annual household income below $50,000. Roughly one-third (37.5%) were 18- to 24-years-old, 82.9% reported drinking alcohol in the past 30 days, 73.1% used marijuana, and 62.2% used other tobacco or e-cigarettes. On average, they reported WTS 4.02 of the past 30 days (SD=5.57), and had moderate motivation to quit WTS (M=4.33, SD=2.31) and WTS dependence (M=2.69, SD=2.11). All participant characteristics were balanced by randomization (Table 1).
Intervention effects on WTS perceptions and behavior
Among those who never smoked and were susceptible, random assignment to the WTS intervention messages was not associated with a decrease in WTS initiation at six months (RR=0.51; 95% CI: [0.25, 1.02]), but was associated with greater perceived addictiveness of WTS relative to cigarette smoking at two months (β=0.27; 95% CI: [0.11, 0.43]; Table 2). There were no other associations between intervention assignment and WTS curiosity, perceptions, or behavior in never smokers who were susceptible. Among those reporting current WTS, there were no associations between intervention assignment and WTS frequency, cessation, motivation to quit, or perceptions (Table 2).
Table 2.
Intervention effects on waterpipe tobacco smoking perceptions and behavior user statusa
| Two months Intervention vs. control |
Four months Intervention vs. control |
Six months Intervention vs. control |
||||
|---|---|---|---|---|---|---|
| Susceptible Never Smokers | IRR/RR/β |
95% CI |
IRR/RR/β |
95% CI |
IRR/RR/β |
95% CI |
| Initiation (RR) | 1.02 | (0.33, 3.11) | 0.57 | (0.25, 1.28) | 0.51 | (0.25, 1.02) |
| Curiosityb (β) | −0.15 | (−0.50, 0.19) | 0.17 | (−0.21, 0.55) | −0.06 | (−0.43, 0.30) |
| Perceived harm of WTS relative to cigarettesc (β) | 0.06 | (−0.10, 0.23) | −0.07 | (−0.25, 0.10) | 0.06 | (−0.11, 0.23) |
| Perceived likelihood of harm from WTSd (β) | −0.04 | (−0.35, 0.27) | 0.13 | (−0.17, 0.43) | 0.00 | (−0.31, 0.31) |
| Worry about harm from WTSb (β) | −0.16 | (−0.58, 0.25) | −0.25 | (−0.69, 0.20) | −0.05 | (−0.48, 0.37) |
| Perceived addictiveness of WTS relative to cigarettesc (β) | 0.27 | (0.11, 0.43) | 0.17 | (−0.01, 0.34) | 0.12 | (−0.05, 0.30) |
| Perceived likelihood of addiction to WTSd (β) | −0.14 | (−0.49, 0.20) | −0.06 | (−0.41, 0.30) | 0.04 | (−0.30, 0.37) |
| Worry about addiction to WTS b (β) | −0.16 | (−0.62, 0.30) | −0.06 | (−0.51, 0.38) | −0.01 | (−0.45, 0.43) |
| Current Waterpipe Smokers | ||||||
| Days smoked waterpipe of past 30 days (IRR) | 0.96 | (0.70, 1.31) | 1.22 | (0.89, 1.68) | 0.94 | (0.69, 1.27) |
| Cessation (RR) | 1.03 | (0.76, 1.39) | 1.12 | (0.85, 1.49) | 0.76 | (0.55, 1.05) |
| Motivation to quit (β) | 0.27 | (−0.13, 0.68) | −0.29 | (−0.73, 0.15) | 0.29 | (−0.16, 0.75) |
| Perceived harm of WTS relative to cigarettesc (β) | 0.05 | (−0.10, 0.21) | 0.01 | (−0.14, 0.16) | 0.09 | (−0.07, 0.26) |
| Perceived likelihood of harm from WTSd (β) | −0.01 | (−0.27, 0.25) | −0.04 | (−0.33, 0.25) | −0.14 | (−0.42, 0.14) |
| Worry about harm from WTSb (β) | 0.01 | (−0.31, 0.33) | 0.07 | (−0.27, 0.40) | 0.08 | (−0.26, 0.42) |
| Perceived addictiveness of WTS relative to cigarettesc (β) | 0.06 | (−0.10, 0.22) | 0.11 | (−0.06, 0.29) | 0.09 | (−0.08, 0.27) |
| Perceived likelihood of addiction to WTSd (β) | 0.28 | (−0.01, 0.56) | 0.18 | (−0.13, 0.48) | 0.12 | (−0.17, 0.42) |
| Worry about addiction to WTSb (β) | 0.14 | (−0.20, 0.48) | 0.14 | (−0.18, 0.47) | 0.16 | (−0.19, 0.50) |
Abbreviations: WTS = Waterpipe tobacco smoking, IRR=Incidence rate ratio, RR=Risk ratio, CI=Confidence interval.
Bold denotes statistical significance (p<0.05).
Data were collected online in 2020. Participants were shown four intervention or control messages spaced approximately two weeks apart. Follow-up data were collected at two-, four-, and six-months after message exposure. Multiple imputation by chained equations was used to handle missing data related to item and unit nonresponse (M=25 datasets). Analyses were completed on the imputed datasets and results were combined following Rubin’s rule.54
Response options: 1=Not at all to 7=Very
Response options: 1=Much less to 5=Much more
Response options: 1=No chance to 7=Certain to happen
Effects of intervention message dose on WTS perceptions and behavior
Of those randomized, 97 (11.7%) viewed 0 intervention (12.9%) or control messages (10.4%), 124 (14.9%) viewed 1 message (14.2% intervention, 15.7% control), 117 (14.1%) viewed 2 messages (12.9% intervention, 15.2% control), 143 (17.2%) viewed 3 messages (16.4% intervention, 18.2% control), and 349 (42.1%) viewed all four intervention (43.5%) or control messages (40.6%). There was no difference in the number of messages seen based on intervention assignment (χ2(4)=3.05; p=0.55) or demographic and tobacco use variables assessed. Associations between intervention message dose (i.e., count of intervention exposures) and study outcomes among participants randomized to the intervention arm are shown in Table 3.
Table 3.
Effects of intervention dose on waterpipe tobacco perceptions and behavior among participants randomized to the WTS messaging intervention arma
| Two months 1-unit increase in dose |
Four months 1-unit increase in dose |
Six months 1-unit increase in dose |
||||
|---|---|---|---|---|---|---|
| Susceptible Never Smokers | IRR/RR/β |
95% CI |
IRR/RR/β |
95% CI |
IRR/RR/β |
95% CI |
| Initiation (RR) | 0.93 | (0.57, 1.53) | 0.69 | (0.46, 1.05) | 0.68 | (0.48, 0.96) |
| Curiosityb (β) | −0.17 | (−0.36, 0.02) | −0.14 | (−0.35, 0.07) | −0.08 | (−0.27, 0.11) |
| Perceived harm of WTS relative to cigarettesc (β) | −0.05 | (−0.13, 0.04) | 0.01 | (−0.08, 0.10) | 0.08 | (−0.01, 0.16) |
| Perceived likelihood of harm from WTSd (β) | 0.03 | (−0.13, 0.20) | −0.04 | (−0.19, 0.11) | 0.11 | (−0.05, 0.28) |
| Worry about harm from WTSb (β) | 0.02 | (−0.20, 0.24) | 0.10 | (−0.13, 0.33) | 0.04 | (−0.17, 0.26) |
| Perceived addictiveness of WTS relative to cigarettesc (β) | −0.02 | (−0.11, 0.07) | −0.03 | (−0.12, 0.06) | 0.05 | (−0.04, 0.15) |
| Perceived likelihood of addiction to WTSd (β) | 0.02 | (−0.17, 0.21) | 0.02 | (−0.15, 0.19) | 0.06 | (−0.12, 0.24) |
| Worry about addiction to WTSb (β) | 0.16 | (−0.07, 0.40) | 0.06 | (−0.16, 0.28) | 0.08 | (−0.16, 0.32) |
| Current Waterpipe Smokers | ||||||
| Days smoked hookah of past 30 days (IRR) | 0.97 | (0.83, 1.12) | 0.90 | (0.77, 1.05) | 0.84 | (0.73, 0.97) |
| Cessation (RR) | 1.07 | (0.93, 1.24) | 1.16 | (0.99, 1.35) | 1.31 | (1.07, 1.59) |
| Motivation to quit (β) | −0.08 | (−0.30, 0.13) | −0.03 | (−0.24, 0.18) | −0.03 | (−0.22, 0.16) |
| Perceived harm of WTS relative to cigarettesc (β) | −0.02 | (−0.09, 0.06) | 0.06 | (−0.02, 0.13) | 0.05 | (−0.03, 0.13) |
| Perceived likelihood of harm from WTSd (β) | 0.03 | (−0.10, 0.15) | 0.16 | (0.02, 0.30) | 0.12 | (−0.03, 0.26) |
| Worry about harm from WTS b (β) | 0.00 | (−0.16, 0.16) | 0.01 | (−0.15, 0.18) | −0.03 | (−0.20, 0.14) |
| Perceived addictiveness of WTS relative to cigarettesc (β) | −0.02 | (−0.10, 0.05) | 0.01 | (−0.07, 0.09) | 0.03 | (−0.05, 0.12) |
| Perceived likelihood of addiction to WTSd (β) | −0.01 | (−0.15, 0.13) | 0.03 | (−0.12, 0.17) | 0.08 | (−0.07, 0.23) |
| Worry about addiction to WTSb (β) | 0.02 | (−0.15, 0.19) | −0.06 | (−0.22, 0.10) | −0.03 | (−0.21, 0.14) |
Abbreviations: WTS = Waterpipe tobacco smoking IRR=Incidence rate ratio, RR=Risk ratio, CI=Confidence interval
Bold denotes statistical significance (p<0.05).
Data were collected via online in 2020. Participants were shown four intervention or control messages spaced approximately two weeks apart. Follow-up data were collected at two-, four-, and six-months after message exposure. Dose is modeled as a continuous predictor, and thus point estimates reflect change associated with a one-unit increase in dose. Multiple imputation by chained equations was used to handle missing data related to item and unit nonresponse (M=25 datasets). Analyses were completed on the imputed datasets and results were combined following Rubin’s rule.54
Response options: 1=Not at all to 7=Very
Response options: 1=Much less to 5=Much more
Response options: 1=No chance to 7=Certain to happen
Among those who never smoked and were susceptible, a one-unit increase in message dose was associated with a 32% decrease in risk of WTS initiation at six months (RR=0.68; 95% CI: [0.48, 0.96]; p=0.03). There were similar associations between increasing dose with WTS initiation at four months (RR=0.69; 95% CI: [0.46, 1.05], p=0.09) and perceived harm of WTS compared to cigarette smoking at six months (β=0.08; 95% CI: [−0.01, 0.16]; p=0.08), but these were not statistically significant.
Among those who reported current WTS, a one-unit increase in intervention message dose was associated with smoking on 16% fewer days of the past 30 days at six months (IRR=0.84; 95% CI: [0.73, 0.97]; p=0.02). Higher dose was associated with a 31% increase in likelihood of cessation at six months (RR=1.31; 95% CI: [1.07, 1.59]; p=0.008). There was a similar association between message dose and cessation at four months that was not statistically significant (RR=1.16; 95% CI: [0.99, 1.35]; p=0.06). A one-unit increase in message dose was associated with increased perceived likelihood of harm from WTS at four months (β=0.16; 95% CI: [0.02, 0.30]; p=0.02).
DISCUSSION
In this trial examining the effects of public education messages for preventing and reducing WTS among over 800 U.S. young adults, there were modest messages effects on perceptions of the addictiveness of WTS compared to cigarettes at the first follow-up among those who never smoked and were susceptible and no effects on outcomes capturing WTS behavior, motivation, and perceptions among those reporting current WTS. These findings did not follow our hypotheses about message effects. Examination in the intervention arm supported dose-dependent message effects on WTS behaviors, with a higher dose of exposure associated with reduced WTS initiation in those who never smoked and were susceptible and less frequent WTS and a higher likelihood of quitting in those reporting WTS. The limited message effects are consistent with findings from recent digital media campaigns targeting cigarette use in youth and young adults25-27 and with a recent study testing point-of-sale messaging for WTS.37 However, these findings differ from one of the only other WTS intervention trials demonstrating that personally tailored, risk-based mobile text messaging reduced WTS frequency and increased cessation in young adults who smoke waterpipe.21 Together, these studies highlight that message content and dose for digital media are critical to examine further.
Our WTS messages were carefully pretested using a multi-method approach to identify those that performed optimally on self-report and psychophysiological assessment.45-47 Messages communicated about risks of health harm and addictiveness of WTS and conveyed these risks in the context of social use and with reference to flavored waterpipe tobacco. Messages addressed misperceptions about risk, WTS in social settings, and flavors – factors associated with WTS among young adults.4-8 Despite this, the message effects were modest overall. This suggests a need to test different message content to identify effective communication strategies for WTS public education campaigns. For example, we used imagery depicting aspects of WTS because it performed well in pretesting, but some research suggests such imagery could act as smoking cues.56,57 Other research shows that messaging communicating the risks of WTS using vivid imagery depicting health effects can increase young adults’ risk perceptions, decrease curiosity in those who have never smoked and are susceptible, and increase motivation to quit, reduce WTS frequency, and increase cessation in young adults who currently smoke waterpipe.5,16-21 This messaging strategy, used in pictorial warning labels for cigarette and other tobacco packaging globally,58 is based on evidence of effectiveness, similar to recent mass media campaigns (e.g., Tips from Former Smokers),22 and another potential communication strategy to test for WTS public education messaging.
Our findings also highlight the importance of the dose of message exposure as a critical factor in planning WTS public education efforts. These findings are consistent with research on cigarette smoking messaging indicating that campaigns with higher doses of exposure achieve better outcomes (e.g., more quit attempts).30-36 Although we did not manipulate the dose of exposure, it ranged from 0 to 4 messages and a higher dose of exposure was associated with reduced WTS initiation in those who never smoked and were susceptible, and reduced WTS and a higher likelihood of cessation those who currently smoked waterpipe. Our message content was designed for use in digital media (e.g., social media) that are popular among young adults. Tobacco public education campaigns are increasingly shifting from traditional (e.g., television) to digital (e.g., social, mobile) media because of the popularity and high potential reach of digital media among young people.25-27 Although there are evidence-based recommendations for how to achieve an adequate dose of exposure for traditional media, there are no such recommendations for digital media.23 In future studies, it will be critical to systematically examine message dose for digital media on intended behavioral outcomes and hypothesized mediators,25-27 for which the optimal dose may vary.59
This study has several important strengths. We recruited participants from a nationally representative consumer research panel, used a rigorous design, had adequate subsamples of those who never smoked and were susceptible and those reporting current WTS, and had high retention. However, the findings should be interpreted based on study limitations. We focused on those who never smoked and were susceptible and those reporting current WTS but excluded those who had tried WTS and did not report current WTs. The exposure was limited to a total of 4 messages, and we did not systematically vary the exposure dose. While our analyses of message dose are exploratory and do not rule out participation effects (e.g., participants retained were less likely to initiate/more likely to quit), the findings highlight the importance of identifying and delivering digital media campaigns at a sufficient dose to impact target outcomes. We delivered messages online, but not using a digital (e.g., mobile, social) media platform. Future studies should examine message effects when delivered via digital platforms. Behavioral outcomes were based on self-report, as it was not possible to collect biospecimens or to biochemically verify WTS separate from other nicotine or tobacco use.60 We assessed outcomes 2 to 6 months post-exposure; shorter-term follow ups capturing immediate effects could help understand if message effects wore out over time.
Our findings indicate few message effects in the full sample, though among those in the intervention condition, a higher dose of message exposure was associated with reduced WTS initiation in those who never smoked and were susceptible and less frequent WTS and a higher likelihood of cessation in those reporting current WTS. Our results highlight the need to examine other message content (e.g., risk-based messages using vivid imagery) to increase the effects of WTS public education campaigns. Our findings also indicate the dose of exposure is critical to achieving effects for WTS public education messages and highlight the need for research to examine optimal message dose, especially to inform campaigns using digital media.
Supplementary Material
Highlights.
Waterpipe tobacco smoking is prevalent in young adults and poses significant risks
There is little research on digital media risk messaging for waterpipe smoking
This study tested the effects of messaging communicating the risks of waterpipe tobacco
Higher dose of message exposure decreased initiation in those who never smoked and were susceptible to initiation
Higher dose of message exposure increased cessation in those who currently smoked waterpipe tobacco
Evidence is needed on the effective dose of exposure for digital media campaigns
Role of Funding Sources:
Research reported in this publication was supported by the National Cancer Institute of the National Institutes of Health (NIH) and the U.S. Food and Drug Administration (FDA) Center for Tobacco Products under Award Number R01CA229082. Dr. Stevens’ contributions were supported by the National Institute of Drug Abuse of the NIH and FDA Center for Tobacco Products Award Number R00DA046563. The funders were not involved in the design of the study, collection of data, analysis of data, or the decision to submit the results for publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the FDA.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declaration of Interests:
The authors have no conflicts of interest to disclose.
References
- 1.Kasza KA, Ambrose BK, Conway KP, et al. Tobacco-Product Use by Adults and Youths in the United States in 2013 and 2014. N Engl J Med. 2017;376(4):342–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Robinson J, Wang B, Jackson K, Donaldson E, Ryant C. Characteristics of hookah tobacco smoking sessions and correlates of use frequency among U.S. adults: findings from Wave 1 of the Population Assessment of Tobacco and Health (PATH) Study. Nicotine Tob Res. 2018;20(6):97–105. [DOI] [PubMed] [Google Scholar]
- 3.Mays D, Arrazola RA, Tworek C, Rolle IV, Neff LJ, Portnoy DB. Openness to Using Non-cigarette Tobacco Products Among U.S. Young Adults. Am J Prev Med. 2016;50(4):528–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Akl EA, Ward KD, Bteddini D, et al. The allure of the waterpipe: a narrative review of factors affecting the epidemic rise in waterpipe smoking among young persons globally. Tob Control. 2015;24 Suppl 1:i13–i21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lipkus IM, Mays D, K PT. Characterizing Young Adults' Susceptibility to Waterpipe Tobacco Use and Their Reactions to Messages About Product Harms and Addictiveness. Nicotine Tob Res. 2017;19(10):1216–1223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Villanti AC, Johnson AL, Ambrose BK, et al. Flavored Tobacco Product Use in Youth and Adults: Findings From the First Wave of the PATH Study (2013-2014). Am J Prev Med 2017;53(2):139–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Villanti AC, Johnson AL, Glasser AM, et al. Association of Flavored Tobacco Use With Tobacco Initiation and Subsequent Use Among US Youth and Adults, 2013–2015. JAMA Netw Open. 2019;2(10):e1913804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lipkus IM, Mays D. Comparing harm beliefs and risk perceptions among young adult waterpipe tobacco smokers and nonsmokers: Implications for cessation and prevention. Addict Behav Rep. 2018;7:103–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Al Oweini D, Jawad M, Akl EA. The association of waterpipe tobacco smoking with later initiation of cigarette smoking: a systematic review and meta-analysis exploring the gateway theory. Tob Control. 2019. [DOI] [PubMed] [Google Scholar]
- 10.Kranzler EC, Hornik RC. The Relationship Between Exogenous Exposure to "The Real Cost" Anti-Smoking Campaign and Campaign-Targeted Beliefs. J Health Commun. 2019;24(10):780–790. [DOI] [PubMed] [Google Scholar]
- 11.MacMonegle AJ, Nonnemaker J, Duke JC, et al. Cost-Effectiveness Analysis of The Real Cost Campaign's Effect on Smoking Prevention. Am J Prev Med. 2018;55(3):319–325. [DOI] [PubMed] [Google Scholar]
- 12.Administration USFaD. Public Health Education: Campaigns. https://www.fda.gov/tobacco-products/public-health-education. Published 2021.Accessed May 14, 2021.
- 13.Sutfin EL, Cornacchione Ross J, Lazard AJ, et al. Developing a Point-of-Sale Health Communication Campaign for Cigarillos and Waterpipe Tobacco. Health Commun. 2019;34(3):343–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cornacchione Ross J, Noar SM, Sutfin EL. Systematic Review of Health Communication for Non-Cigarette Tobacco Products. Health Commun. 2019;34(3):361–369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.King JL, Reboussin BA, Cornacchione Ross J, Sutfin EL. Waterpipe tobacco package warning exposure's impact on risk perceptions and use among young adults in the USA: a longitudinal analysis of the population assessment of tobacco and health study. Tob Control. 2019;28(e1):e16–e23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Maziak W, Ben Taleb Z, Ebrahimi Kalan M, et al. Pictorial health warning labels on the waterpipe device are effective in reducing smoking satisfaction, puffing behaviour and exposure to CO: first evidence from a crossover clinical laboratory study. Tob Control. 2019;28(e1):e37–e42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Islam F, Salloum RG, Nakkash R, Maziak W, Thrasher JF. Effectiveness of health warnings for waterpipe tobacco smoking among college students. Int J Public Health. 2016;61(6):709–715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Johnson AC, Mays D. Testing the Effects of Hookah Tobacco Social Media Risk Communication Messages Among Young Adults. Health Educ Behav. 2020:1090198120963104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mays D, Johnson AC, Phan L, Tercyak KP, Rehberg K, Lipkus I. Effect of risk messages on risk appraisals, attitudes, ambivalence, and willingness to smoke hookah in young adults. Health Psychol Behav Med. 2020;8(1):96–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mays D, Tercyak KP, Lipkus IM. The Effects of Brief Waterpipe Tobacco Use Harm and Addiction Education Messages Among Young Adult Waterpipe Tobacco Users. Nicotine Tob Res. 2016;18(5):777–784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mays D, Johnson AC, Phan L, et al. Tailored mobile messaging intervention for watepripe tobacco cessation in young adults: a randomized trial. Am J Public Health. 2021;Online Ahead of Print:e1–e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shrestha SS, Davis K, Mann N, et al. Cost Effectiveness of the Tips From Former Smokers(R) Campaign-U.S., 2012–2018. Am J Prev Med. 2021;60(3):406–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Centers for Disease Control and Prevention. Health Communications in Tobacco Prevention and Control. Atlanta, GA: 2014. [Google Scholar]
- 24.(US) OotSG, (US) OoSaH. The Health Consequences of Smoking: A Report of the Surgeon General. In:2004. [PubMed]
- 25.Crankshaw E, Guillory J, Gaber J, et al. Campaign evaluation findings for the This Free Life Communication Campaign to prevent and reduce daily cigarette use among LGBT young adults in the United States. 2021 Annual Meeting of the Society for Research on Nicotine and Tobacco; 2021; Virtual. [Google Scholar]
- 26.Guillory J, Henes A, Farrelly MC, et al. Reach, receptivity, and belief change associated with the Fresh Empire Campaign to prevent and reduce cigarette use among hip hop youth in the United States. 2021 Annual Meeting of the Society for Research on Nicotine and Tobacco; 2021; Virtual. [Google Scholar]
- 27.Crankshaw E, Gaber J, Guillory J, et al. Final Evaluation Findings for This Free Life, a 3-Year, Multi-Market Tobacco Public Education Campaign for Gender and Sexual Minority Young Adults in the United States. Nicotine Tob Res. 2022;24(1):109–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ilakkuvan V, Johnson A, Villanti AC, Evans WD, Turner M. Patterns of Social Media Use and Their Relationship to Health Risks Among Young Adults. J Adolesc Health. 2019;64(2):158–164. [DOI] [PubMed] [Google Scholar]
- 29.Villanti AC, Johnson AL, Ilakkuvan V, Jacobs MA, Graham AL, Rath JM. Social Media Use and Access to Digital Technology in US Young Adults in 2016. J Med Internet Res. 2017;19(6):e196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Durkin S, Brennan E, Wakefield M. Mass media campaigns to promote smoking cessation among adults: an integrative review. Tob Control. 2012;21(2):127–138. [DOI] [PubMed] [Google Scholar]
- 31.McAfee T, Davis KC, Alexander RL Jr., Pechacek TF, Bunnell R. Effect of the first federally funded US antismoking national media campaign. Lancet. 2013;382(9909):2003–2011. [DOI] [PubMed] [Google Scholar]
- 32.Hyland A, Wakefield M, Higbee C, Szczypka G, Cummings KM. Anti-tobacco television advertising and indicators of smoking cessation in adults: a cohort study. Health Educ Res. 2006;21(3):348–354. [DOI] [PubMed] [Google Scholar]
- 33.Wakefield MA, Spittal MJ, Yong HH, Durkin SJ, Borland R. Effects of mass media campaign exposure intensity and durability on quit attempts in a population-based cohort study. Health Educ Res. 2011;26(6):988–997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Farrelly MC, Davis KC, Haviland ML, Messeri P, Healton CG. Evidence of a dose-response relationship between "truth" antismoking ads and youth smoking prevalence. Am J Public Health. 2005;95(3):425–431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Farrelly MC, Davis KC, Nonnemaker JM, Kamyab K, Jackson C. Promoting calls to a quitline: quantifying the influence of message theme, strong negative emotions and graphic images in television advertisements. Tob Control. 2011;20(4):279–284. [DOI] [PubMed] [Google Scholar]
- 36.Farrelly MC, Duke JC, Davis KC, et al. Promotion of smoking cessation with emotional and/or graphic antismoking advertising. Am J Prev Med. 2012;43(5):475–482. [DOI] [PubMed] [Google Scholar]
- 37.Sutfin EL, Lazard AJ, Wagoner KG, et al. Point-of-Sale Health Communication Campaigns for Cigarillos and Waterpipe Tobacco: Effects and Lessons Learned from Two Cluster Randomized Trials. Health Commun. 2021:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.National Opinion Research Council. AmeriSpeak Panel Design. NORC. https://amerispeak.norc.org/about-amerispeak/Pages/Panel-Design.aspx. Published 2021. Accessed December 20, 2021. [Google Scholar]
- 39.Villanti AC, Cobb CO, Cohn AM, Williams VF, Rath JM. Correlates of hookah use and predictors of hookah trial in U.S. young adults. Am J Prev Med. 2015;48(6):742–746. [DOI] [PubMed] [Google Scholar]
- 40.Sharma E, Bansal-Travers M, Edwards KC, et al. Longitudinal pathways of exclusive and polytobacco hookah use among youth, young adults and adults in the USA: findings from the PATH Study Waves 1-3 (2013-2016). Tob Control. 2020;29(Suppl 3):s155–s162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sidani J, Shensa A, Naidu M, Yabes J, Primack B. Initiation, progression, and sustained waterpipe use: a nationally representative longitudinal study of U.S. young adults.Cancer Epidemiol Biomarkers Prev. 2017;111(2):351–359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gautam P, Sharma E, Li T, Maziak W. Prevalence and predictors of waterpipe smoking cessation among young adults in the US: Findings from a population-based study. Addict Behav. 2022;135:107457. [DOI] [PubMed] [Google Scholar]
- 43.Wakefield MA, Loken B, Hornik RC. Use of mass media campaigns to change health behaviour. Lancet. 2010;376(9748):1261–1271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Randolph W, Viswanath K. Lessons learned from public health mass media campaigns: marketing health in a crowded media world. Annu Rev Public Health. 2004;25:419–437. [DOI] [PubMed] [Google Scholar]
- 45.Leshner G, Phan L, Stevens EM, et al. Psychophysiological responses to hookah tobacco public education messages among young adults. Health Psychology. 2021;40(9):569–577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Phan L, Villanti AC, Leshner G, et al. Development and Pretesting of Hookah Tobacco Public Education Messages for Young Adults. Int J Environ Res Public Health. 2020;17(23). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Stevens EM, Villanti AC, Leshner G, Wagener TL, Keller-Hamilton B, Mays D. Integrating Self-Report and Psychophysiological Measures in Waterpipe Tobacco Message Testing: A Novel Application of Multi-Attribute Decision Modeling. Int J Environ Res Public Health. 2021;18(22). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Villanti AC, West JC, Mays D, Donny EC, Cappella JN, Strasser AA. Impact of Brief Nicotine Messaging on Nicotine-Related Beliefs in a U.S. Sample. Am J Prev Med. 2019;57(4):e135–e142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wang TW, Asman K, Gentzke AS, et al. Tobacco Product Use Among Adults - United States, 2017. MMWR Morb Mortal Wkly Rep. 2018;67(44):1225–1232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sidani JE, Shensa A, Shiffman S, Switzer GE, Primack BA. Behavioral associations with waterpipe tobacco smoking dependence among US young adults. Addiction. 2016;111(2):351–359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lee KJ, Carlin JB. Multiple imputation for missing data: fully conditional specification versus multivariate normal imputation. Am J Epidemiol. 2010;171(5):624–632. [DOI] [PubMed] [Google Scholar]
- 52.Schafer JL, Graham JW. Missing data: our view of the state of the art. Psychol Methods. 2002;7(2):147–177. [PubMed] [Google Scholar]
- 53.Rubin DB. Multiple Imputation after 18+ Years. Journal of the American Statistcal Association. 1993;91(434):473–489. [Google Scholar]
- 54.Rubin DB. Multiple imputation for nonresponse in surveys. New York, NY: John Wiley & Sons; 1987. [Google Scholar]
- 55.Zou G A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–706. [DOI] [PubMed] [Google Scholar]
- 56.Kang Y, Cappella JN, Strasser AA, Lerman C. The effect of smoking cues in antismoking advertisements on smoking urge and psychophysiological reactions. Nicotine Tob Res. 2009;11(3):254–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sanders-Jackson AN, Cappella JN, Linebarger DL, Piotrowski JT, O'Keeffe M, Strasser AA. Visual Attention to Antismoking PSAs: Smoking Cues Versus Other Attention-Grabbing Features. Hum Commun Res. 2011;37(2):275–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Noar SM, Hall MG, Francis DB, Ribisl KM, Pepper JK, Brewer NT. Pictorial cigarette pack warnings: a meta-analysis of experimental studies. Tob Control. 2016;25(3):341–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Centers for Disease Control and Prevention. Best Practices for Comprehensive Tobacco Control Programs. Atlanta, GA: 2014. [Google Scholar]
- 60.Benowitz NL, Bernert JT, Foulds J, et al. Biochemical Verification of Tobacco Use and Abstinence: 2019 Update. Nicotine Tob Res. 2020;22(7):1086–1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.