Abstract
Scheuermann’s Kyphosis (SK) is a rigid spinal kyphosis. Several theories have been proposed concerning its pathogenesis, but it is, to this day, still unknown.
It has a prevalence of 0.4–8.3% in the population with a higher incidence in females.
Clinical examination with x-rays is needed to differentiate and confirm this diagnosis.
Non-surgical management is reserved for smaller deformities and in skeletally immature patients, whereas surgery is recommended for higher deformities.
Combined anterior and posterior approach was considered the gold standard for the surgical treatment of this disease, but there is an increasing trend toward posterior-only approaches especially with use of segmental fixation.
This study reviews the pathophysiology of SK while proposing a treatment algorithm for its management.
Keywords: scheuermann’s kyphosis, surgical management, fusion levels, treatment algorithm
Introduction
Scheuermann's Kyphosis (SK), first described by Horgel Welfer Scheuermann in 1920, is a rigid spinal kyphosis usually involving the thoracic or thoracolumbar area (1). Albeit several theories, its etiology is still unknown (2). SK is usually separated into two groups: typical and atypical SK. Typical SK is the more common type and has a mid-thoracic (T7–T9) apex in its deformity. It is associated with a hyperlordosis of both the cervical and lumbar spine (3). The atypical group is also known as ‘Apprentice Kyphosis’, and most commonly presents in athletic adolescent males or heavy lifters, the deformity’s apex is in the thoraco-lumbar or lumbar spine and this form is the most likely to progress (4). Sorensen’s criteria defined as anterior wedging of 5° or more in at least three vertebral bodies alongside endplate narrowing, and Schmorl nodes (5) are always met in the typical form but not necessarily in the atypical form (6).
Treatment for SK includes both conservative and operative treatment (2). The purpose of this narrative review is to provide a treatment algorithm for this disease after reviewing its physiopathology.
Etiology and pathophysiology
Until now, the exact etiology of SK is still unknown (7). Several theories were proposed concerning its pathophysiology. The first one was by Scheuermann et al. stating that an osteonecrosis of the ring apophysis in the vertebral bodies caused an arrest in anterior growth, thus causing this disease (8). This theory was rapidly rejected by Bick et al. showing that the ring apophysis has no effect on anterior longitudinal growth since it is not a part of the cartilaginous physis (9). On the other hand, Schmorl et al. postulated that herniated disks cause a loss of anterior disk height and result in growth disturbance and ultimately SK (7). This theory is not proven till now, but it is likely to be erroneous due to the fact that not only Schmorl nodes are common among normal people but also they are present in areas that are not involved in the deformity (7). Finally, Bradford et al. proposed a third theory that is based on the idea that osteoporotic vertebra are more prone to collapse under compression (10). Studies showed no significative difference in bone density between people with SK and the normal population resulting in a rejection of this theory (11).
The most accepted theory is the biomechanical theory. Ogden et al. suggested that there is a biomechanical process behind this kyphosis implying that biomechanical stresses alter the remodeling response in the vertebral bodies resulting in increased compressive forces on the anterior part of the vertebral body which will stop the growth and cause SK (7). Other biomechanical theories came out such as the presence of tight hamstrings in patient with SK increasing the pelvic tilt when bending forward (12, 13). A smaller sternum was also associated with SK due to it increasing compression in the anterior part of the thoracic vertebral bodies leading to kyphosis (14). Bracing supports the mechanical origin of this disease by being a successful way of management (15).
Genetics was also used as a way to explain this deformity (16). Halal et al. showed an autosomal dominant transmission with high penetration of this disease but with variable expression (16). Other authors supported the presence of a genetic basis behind this deformity implying that family history of hyperkyphosis should be taken into consideration to exclude the possibility of SK (17). Candidate genes linked to SK such as IHH, SOX9 and PAX 1 were identified by Zaidman et al. (18). Damborg et al. showed a higher concordance by pairs and probands for monozygotic twins than for bizygotic twins indicating a higher genetic contribution to Scheuermann’s disease (19). Findlay et al. also described a family where SK was present in three consecutive generations with a male to male transmission (16).
Other theories were suggested as an etiology of SK such as high levels of growth hormone, juvenile idiopathic osteoporosis, hypovitaminosis D, dural cysts, spondylolysis, infections, spinal malformations, etc. (20). It is possible that Scheuermann’s disease is the result of the simultaneous action of several factors (21).
Natural history
Prevalence
The prevalence of SK in the population ranges from 0.4 to 8.3% (7). Some studies showed SK being more frequent in men (15, 22). In fact, the most accepted male to female ratio is between 2:1 and 7:1 (23). The age onset of SK is between 10 and 12 years old but an adulthood onset is not unheard of (24). Although the kyphosis angle was not influenced by sex, it was positively correlated to the age (25).
Evolution
The evolution of SK is benign. SK may only mildly affect the quality of life (QOL) of the patients affected by the disease compared to the general population (7). Patients presenting with a kyphosis lower than 60° have good clinical outcomes (22). To add to that, Murray et al. reported that patients with curves lower than 85° reported little concern with their physical appearance and had similar QOL to patients with curves lower than 60° (work absence due to back pain, interference of pain with daily activities, recreational activities, self-esteem and self-consciousness) (22). Ristolainen et al. followed patients with mild thoracic kyphosis for 46 years and reported an increase of a mean of 14° (from 46° to 60°) with no correlation between the extent of progression of the kyphosis and function (26).
In other studies, untreated SK resulted in ‘severe thoracic spine pain’ in nearly 50% of the cases (27, 28). Such discrepancies may be explained by the fact that these studies had patients with greater deformities (22). All in all the evolution of Scheuermann disease is still unknown since it is less studied than other spinal deformities like adolescent idiopathic scoliosis (7).
Clinical examination
The most common symptom at presentation is pain at the apex of the deformity in the pediatric population, whereas esthetic deformity is the most common symptom in the adult population (7). On examination, the patient demonstrates a varyingly flexible thoracic hyperkyphosis associated to an increased lumbar and cervical lordosis compensating for the thoracic deformity (7). These associated compensations may be a cause of pain (15, 29). The neck and head adopt an anterior position with a forward protrusion aspect (’goose-neck deformity’) (Fig. 1). This characteristic posture leads to aesthetic disturbances and dissatisfaction with the patient's own body image (30). Lumbar hyperlordosis produces an added increase in stress on the pars interarticularis, which could explain the increase in the incidence of spondylolysis, up to 11% (31). If a patient with SK presents with pain in the lumbosacral region, spondylolysis must be ruled out (32). Tightness in the ilio-psoas, hamstrings, pectoralis and the anterior shoulder may also be present (33). When inspecting the back, a cutaneous pigmentation may be present at the apex of the kyphosis caused by skin friction due to the protruding spinous process (22, 34).
Figure 1.

Clinical presentation of a 15-year-old boy with SK. Note the ‘goose-neck deformity’ and the angular kyphosis with Adam’s forward bending test.
Scoliosis may be associated to the hyperkyphosis. This may be caused by the irregularities at the vertebral endplates of every level of the kyphosis with a presence of a lateral wedging (19). The present information is not enough to confirm this hypothesis, but it is important to note that if it is correct, then the characteristics of this scoliosis could be identified and it should be not confused with an idiopathic scoliosis in order to efficiently correct the deformities in both planes (19).
Associated neurologic abnormalities are rare but if present, an MRI of the thoracic spine must be ordered (7). The present neurological symptoms may be due disk herniation, severe kyphosis or dural cysts (35). Restriction of pulmonary function is rare and is usually present in cases where kyphotic curves surpasses 100° (22). Finally, SK may be a risk factor for ossification of the ligamentum flavum and thoracic disk herniation, but it is not associated to an ossification of the posterior longitudinal ligament (36). As a matter of fact, a recent study found that 95.2% of thoracic disc herniation occurs in patients with typical or atypical SK (37).
Differential diagnosis
Parents and general practitioners sometimes attribute the onset of kyphosis to poor posture, resulting in delayed diagnosis and treatment ( 15, 34, 38, 39). It is very important to differentiate Scheuermann's disease from curved dorsum or postural kyphosis. Adam’s forward bending test may be helpful in differentiating the two entities (Fig. 1). With postural kyphosis, the deformity disappears on forward bending, whereas with SK, the deformity is increased alongside a transition in the thoracolumbar region (7). Other conditions such as osteochondral dystrophies and spondyloepiphyseal dysplasias, congenital kyphosis, spondylodiscitis, sequelae of vertebral compression fractures, post-laminectomy kyphosis and neoplasms should also be considered (7, 15, 40).
Imaging
X-ray
Initial imaging should include a standing postero-anterior and lateral radiographs of the spine. Cobb angle is measured on the lateral radiograph to assess the degree of kyphosis. The classical normal of kyphosis was thought to be between 25° and 45° (41). A recent study found that the thoracic kyphosis changes with the PI with a nearly constant upper arch of the kyphosis (41). Other signs include a round back (Fig. 2) on lateral view alongside vertebral wedging. Sorensens’ signs must also be searched for and assessment for Schmorl nodes (Figs. 3 and 4). Scoliosis, increased lumbar lordosis and spondylolysis may also be present (4). C7 plumb line may be found lying behind the sacral promontory instead of being within 2 cm of it (39, 42) showing a negative sagittal balance (Fig. 2) (7).
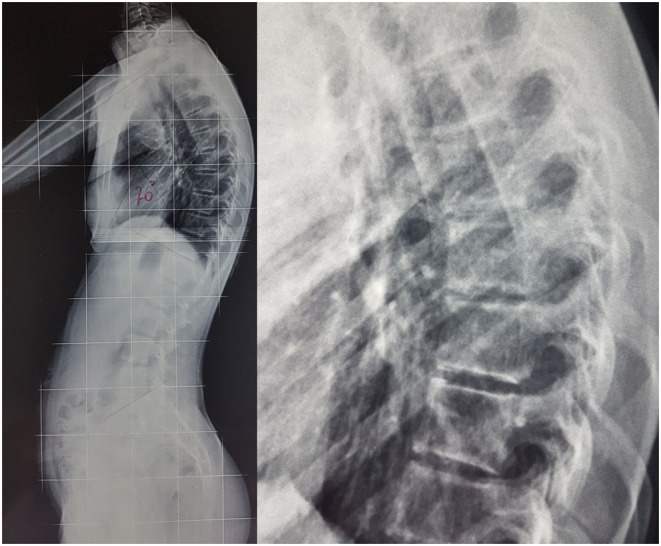
Figure 2.
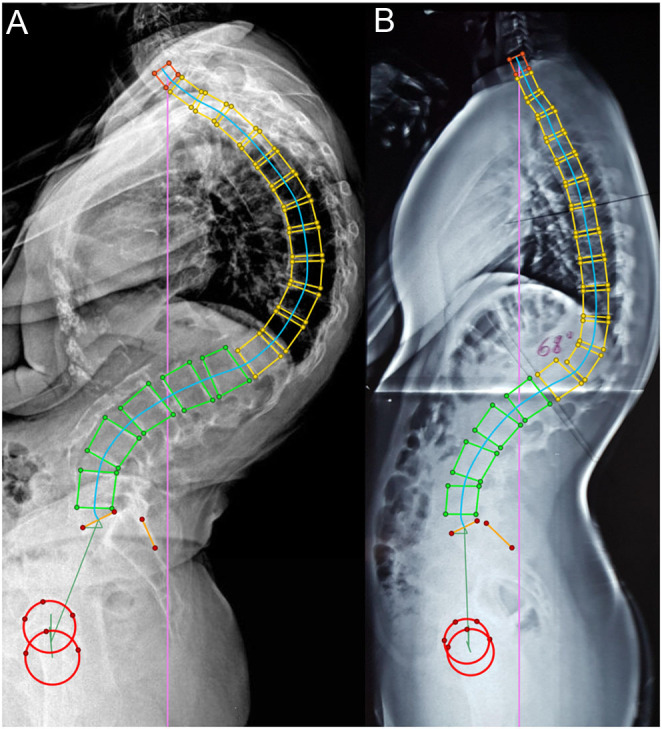
Full spine lateral x-ays showing a typical thoracic SK (A) and a lumbosacral SK (B). Note in the two cases that the C7 plumbline is behind the posterior sacral edge.
Figure 3.
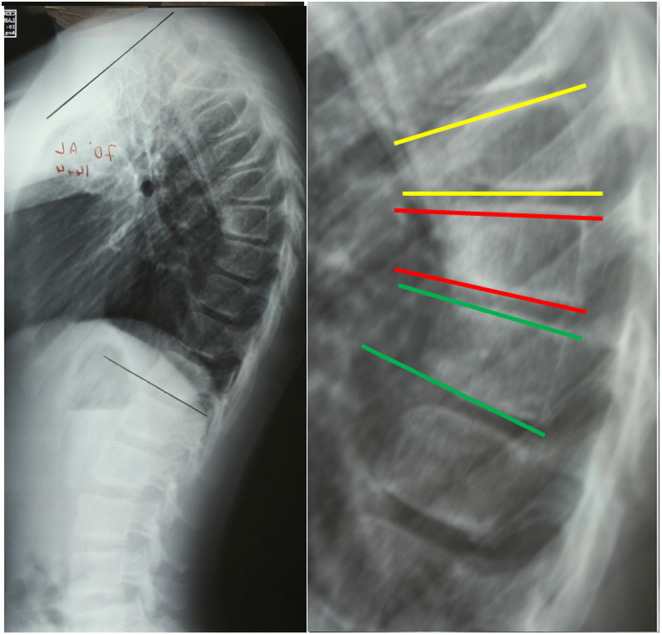
Typical wedging in three consecutive vertebras.
Figure 4.
Non Scheuermann Kyphosis. The thoracic kyphosis is harmonious and there is no wedging of the apical vertebras.
If surgical management is considered, flexibility of this deformity should be assessed and the patient is positioned placing a bolster under the thoracic spine to have a hyperextension lateral radiograph of the deformity (7).
MRI
Authors recommend ordering a pre-operative MRI for several reasons. First, a normal neurological exam can coexist with an abnormal MRI, with the rate of abnormal findings not reported in the literature (5, 43). Secondly, MRI is used to rule out abnormalities of the neural axis such as Chiari malformations, syrinx, stenosis, spinal cord impingement and findings that can alter the operative plan. In fact, Lonner et al. found a 19.7% chance of anomalies in patients to be operated for SK: low-lying conus (2.3%), syrinx without Chiari malformations (17.4%) posterior disc herniations and spondylolysis (8.1%). An interesting fact is that 4.7% of the cases had the operative plan changed as a result of the pre-operative MRI due to either neural compression, disc herniation or to a spinal cord draped over the apex (5). Thus, the probability of causing spinal cord damage during corrective surgery of SK, even though it is not high (around 3.2%), along with the chance of changing the operative plan, is valid reason enough to order a pre-operative MRI (5).
Whenever there is a doubt about any compression sign, an MRI with diffusion-weighted imaging and apparent diffusion coefficient should be performed in emergency in order to rule out any abnormalities, or take care of them before setting a management plan of the thoracic deformity (44).
Management
The management of SK, whether conservative or surgical, can be very challenging. There is no clear consensus on treatment indications, guidelines and protocols, and treatment strategies are controversial (Table 1) (2, 45, 46, 47).
Table 1.
Management techniques for Scheuermann’s Kyphosis (SK).
| Conservative management | Lifestyle modification Physical therapy Extension stretching/strengthening Hamstring stretching Proper self-postural control daily for 20 min (46) |
| Pain medication (49): Anti-inflammatory drugs (46) Muscle relaxant (46) | |
| Bracing (49): Thoracic SK: 4-5-point bracing for 22 h/day (must be worn all night) (2), or 5-point system in case of muscular imbalance (52). Thoraco-lumbar SK: 4-point bracing worn during the day in sitting position (51). Juvenile SK: Milwaukee brace worn part time for 16 h/day (46). | |
| Surgical management | Two-stage anterior and posterior fusion (56) UIV: T2 (66) LIV: FLD (56) or the SSV (63). However, the SSV is better since it decreases the risk of DJK when compared to FLD (63) |
| One stage posterior-only fusion (57) |
FLD, first lordotic vertebra; LIV, lower instrumented vertebra; SSV, sagittal stable vertebra; UIV, upper instrumented vertebra.
Non-surgical management
In 2010, the International Society on Scoliosis Orthopaedic and Rehabilitation Treatment SOSORT has evaluated the use of non-operative techniques along with specific braces and physiotherapy techniques in the treatment of SK. Non-operative management includes exercises and life style modification, pain medication and bracing (48). The indication for non-operative management varies for each treatment depending on the kyphosis angle, rigidity and symptoms (49). When kyphosis is <60° and asymptomatic, physical therapy and life style modification with NSAID are recommended (50). The main rehabilitation techniques are extension stretching/strengthening, hamstring stretching and proper self-postural control. This protocol should be repeated at home daily for 20 min (45). Exercises and life style modification are also indicated in rigid kyphosis because they increase the trunk’s range of motion. This leads to reduced plaster series, better adaptation to braces and better correction (51).
The main indications to bracing are 60°–80° kyphosis, pain and rigidity. Wearing a brace can prevent the collapse of the anterior wall of the vertebral body by decreasing mechanical stress on the anterior wall of the vertebral body (50). They are mostly effective in skeletally immature patients, in which the threshold for implementing the brace is lower than 60°, because brace impede progression of curve. The best time of application of the brace is at the onset of puberty. Braces should be worn for about 12–24 months and removed at the end of growth (45). Brace wear is recommended for 16–23 h per day until apical wedging is corrected (2). Brace model and wearing time differ depending on the type of SK and the age of the patient:
For thoracic SK: Most experts suggested the use of 4–5-point bracing systems which must be worn all night and for part of the day for a total of 22 h (2). Five-point system is better used in the case of muscular imbalance (51).
For a Thoraco-lumbar SK: The brace must be worn during the day in the sitting position and the ideal brace is a 4-point system.
For a juvenile SK: The brace must be worn part time with a total of 16 h, and the ideal brace is the Milwaukee brace (45).
Older patients are also likely to have less flexible curves that cannot be corrected with external pressure alone. While skeletal maturity may not necessarily be a contraindication to bracing, it is generally thought that skeletally mature patients are poorer candidates for bracing and more appropriately treated with surgery (52). Historically, operative intervention in younger patients with remaining growth potential was associated with high risk of failure given the crankshaft phenomenon (47). Nonetheless, this complication has decreased significantly with patients with newer segmental instrumentations (47).
Surgical management
The main indication for surgical management of SK is (1) painful kyphotic deformity that does not respond to non-surgical treatment, (2) cosmetically displeasing deformity, (3) functionally progressive curve or (4) neurologic deficit/spinal cord compression (7). Traditionally, surgery has been offered when the curve magnitude exceeds 65°–80° degrees, especially in adults (53). Cardiopulmonary indications for surgical intervention are rare and appear only in patients with curves >100° (22). In the context of progressive deformity, older patients are likely to have more severe and less flexible curvature amenable only to operative correction (54).
Correction may be achieved using one of two surgical strategies: a two-stage anterior and posterior fusion or a one-stage posterior-only fusion. It is still controversial the better strategy for better outcome (31). Age should be taken in consideration when choosing the surgical strategy: during the period of growth, posterior arthrodesis is the preferred may be the method of choice, while at the adult age, the two-stage anteroposterior fusion is ideal with more rigid curves (51). Two-stage approach is the method of choice when deformation is significant with more rigid curves. Two-stage approach was found to be more efficient at reducing the kyphotic deformity, as indicated by a greater correction rate, bolster bending correction index (BBCI), and gain in spinal height (46). The two-stage anteroposterior fusion was also associated with reduced incidence of junctional failure when using various forms of instrumentation, including Cotrel-Dubousset instrumentation and Luque rods (55). This lead for the recommendation of the two-staged approach as the gold standard in the surgical treatment of SK. However, with the advancement of the surgical techniques (Ponte osteotomies) and instrumentation (multi-segmental posterior pedicle screws), there is a shift toward posterior-only approach (Fig. 5) (56).
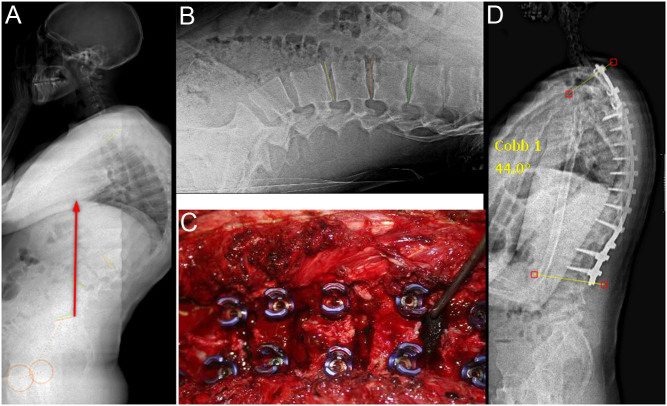
Figure 5.
Case of a 15-year-old male who presented with a 100° kyphosis (A). A fulcrum test showed that the most horizontal disc is L3-L4 (B). He was operated with multilevel Ponte osteotomies (C). The postoperative x-ray showed a thoracic kyphosis of 50°.
In the 80s and 90s, recommendation for severe curve correction was dual approach (38). Since Bradford et al. carried out the first report on posterior fusion in the treatment of SK, the surgical indications, as well as the operating techniques, have altered significantly (57), and modern single-stage posterior-only fusion now typically incorporates a Smith-Petersen or Ponte osteotomy (58).
Considering the controversy surrounding the best form of surgical treatment, many studies compared the results of treatment using the dual approach (DA) with treatment using posterior approach (PO). In Yun’s et al. systematic literature review and meta-analysis, outcomes of Scheuermann’s disease after DA and PO approaches were compared. Blood loss, length of surgery time, PJK/DJK and return to surgery seemed to be less in the PO group than that in the AP group (59). The sagittal vertical axis was the only significant spinopelvic parameter in favor of combined anteroposterior in Mcdonnell’s retrospective review on two-stage anterior and posterior fusion versus one-stage posterior fusion in patients with SK.
Levels of fusion
Dubousset and Guillaumat in 1987 recommended that the lower limit should be the lumbar vertebra just above the horizontal disc on the hyperextension lateral Xrays (60). The most appropriate lowest instrumented vertebra (LIV) was the level below the first lordotic disk (FLD) (55). The FLD is defined as the most proximal thoracolumbar or lumbar disk below the level of the kyphosis with ≥5° of anterior opening. Because of hyperlordosis in the lumbar spine in patients with SK, determining the FLD can sometimes be difficult, thus leading to fusion short of the true FLD and subsequent DJK (2). The sagittal stable vertebra (SSV) was defined by Lenke as the most proximal touched vertebra by the posterior sacral vertical line (61). In a matter of fact, the FLD is more proximal than the sagittal stable vertebra (SSV). According to Cho et al., choosing the SSV instead of the FLD decreases the incidence of DJK (61). Patients who were fused at or below the SSV using posterior-only construct were found to have markedly greater lordotic disk angles below the LIV and lower revision surgery rates for DJK compared to patients who had an LIV proximal to the SSV (5% vs 36.3%) at the expense of incorporating additional motion segments (62). The choice of the LIV is important to decrease the occurrence of DJK. A recent meta-analysis found a DJK incidence in patients fused to the FLV to be 43.6% compared to 5.9% in the SSV group with a risk reduction of 86% (63). The latest recommendation by Ames & Lenke in 2019 is using the SSV concept for distal level selection: ‘If the selected SSV is just barely touched by the sacral vertical line, the adjacent disk space should be evaluated further. If the proximal disk space is lordotic, the “barely touched" SSV is still a safe choice’ (2).
After the distal fusion level is selected, maintaining symmetry of the construct overall is recommended. Proximally, a general consensus exists in recommending the inclusion of the proximal end vertebra (which is generally T2) in the construct (64). The fusion should extend roughly the same extent from the apex proximally and distally, with some consideration for adding one additional proximal fusion level to ensure that the proximal end vertebra is also included in the fusion construct (2).
Complications
Among non-operatively managed patients, loss of correction occurred in at least 30% of patients once the brace is removed, even if they were compliant to brace wear (30).
Among operatively treated patients, the most common complications, mechanical mainly, were hardware failure and proximal or distal junctional kyphosis. Combined anterior-posterior procedures were additionally associated with neural, pulmonary and cardiovascular complications and greater incidence of infection with two-stage anteroposterior fusion (45).
PJK/DJK (Fig. 6) risk factors include short fusion, greater pre-operative sagittal imbalance, correction of sagittal deformity, more posterior LIV plumb line, low bone mineral density and a smaller postoperative kyphosis (65, 66). Hypercorrection is one of the most common risk factor for PJK/DJK and final kyphosis should be tailored to patient’s pelvic incidence (41, 57). There are conflicting data whether age at the time of presentation is risk factor for DJK with some authors finding younger age to be a risk factor (66), whereas other found increased age to be risk factor (65).
Figure 6.

Proximal junctional failure (A) with proximal hooks pullout. (B) Distal junctional failure with screw pullout.
The overall complication rate specifically for combined-approach surgeries was 19.6%, and posterior-only procedures had a 9.9% ate (67) However, hardware failure is more important in posterior fusion (47).
Treatment algorithm
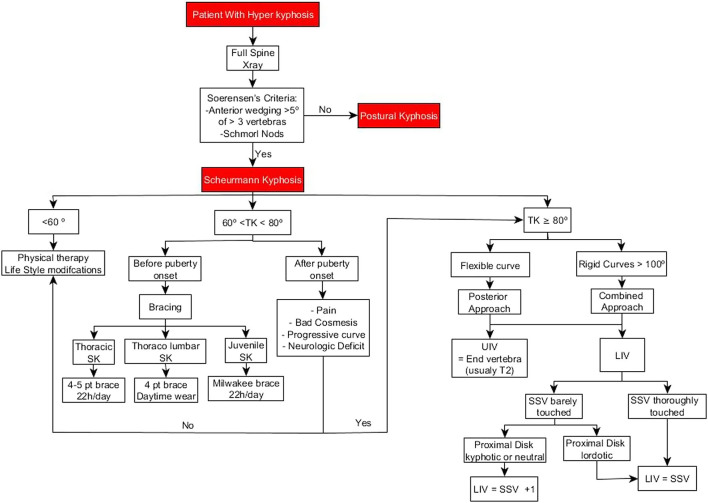
Based on this review, we propose the following algorithm for the treatment of SK (Fig. 7). The main criteria for the selection of optimal treatment are the patient’s age, the Cobb angle magnitude and clinical impact of the disease. In summary of this algorithm, non-operative treatment is the most indicated at when curve magnitude is less than 60°. When SK Cobb angle is between 60° and 80°, the decision depends on the age of the patient. If the patient is skeletally immature (before or at puberty), bracing is the best option. The type of the brace and time for wearing it depend on the type of SK. on the other hand, if the patient is skeletally mature, the two options are either surgery or physical therapy. Surgery is indicated in the setting of neurological impairment, progressive curve or bad cosmesis. In other cases, physical therapy should be recommended and posterior instrumentation with multilevel osteotomies for the surgical cases.
Figure 7.
Proposed treatment algorithm.
Conclusion
In conclusion, SK is a disease whose etiology is still unknown. It has a wide spectrum and a lot of differential diagnoses. It usually presents with pain and most of the times imaging techniques along the clinical exam are needed to diagnose it. An MRI is usually needed before undergoing surgery due to the high rates of association with intracanal anomalies. Indications for surgical or conservative treatment are still unclear.
ICMJE Conflict of Interest Statement
The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported.
Funding
AS is a consultant for Medtronic spine (unrelated to this study).
References
- 1.H S. Kyfosis dorsalis juvenilis. Ugeskrift for Laeger 192082385–393. [Google Scholar]
- 2.Sardar ZM, Ames RJ, Lenke L. Scheuermann’s kyphosis: diagnosis, management, and selecting fusion levels. Journal of the American Academy of Orthopaedic Surgeons 201927e462–e472. ( 10.5435/JAAOS-D-17-00748) [DOI] [PubMed] [Google Scholar]
- 3.Jansen RC, van Rhijn LW, van Ooij A. Predictable correction of the unfused lumbar lordosis after thoracic correction and fusion in Scheuermann kyphosis. Spine (Phila Pa 1976) 2006311227–1231. ( 10.1097/01.brs.0000217682.53629.ad) [DOI] [PubMed] [Google Scholar]
- 4.Bezalel T, Carmeli E, Been E, Kalichman L. Scheuermann’s disease: current diagnosis and treatment approach. Journal of Back and Musculoskeletal Rehabilitation 201427383–390. ( 10.3233/BMR-140483) [DOI] [PubMed] [Google Scholar]
- 5.Lonner BS, Toombs CS, Mechlin M, Ciavarra G, Shah SA, Samdani AF, Sponseller P, Shufflebarger HL, Betz RR, Yaszay Bet al. MRI screening in operative Scheuermann kyphosis: is it necessary? Spine Deformity 20175124–133. ( 10.1016/j.jspd.2016.10.008) [DOI] [PubMed] [Google Scholar]
- 6.Blumenthal SL, Roach J, Herring JA. Lumbar Scheuermann’s. A clinical series and classification. Spine (Phila Pa 1976) 198712929–932. ( 10.1097/00007632-198711000-00015) [DOI] [PubMed] [Google Scholar]
- 7.Wood KB, Melikian R, Villamil F. Adult Scheuermann kyphosis: evaluation, management, and new developments. Journal of the American Academy of Orthopaedic Surgeons 201220113–121. ( 10.5435/JAAOS-20-02-113) [DOI] [PubMed] [Google Scholar]
- 8.Scheuermann HW.The classic: kyphosis dorsalis juvenilis. Clinical Orthopaedics and Related Research 19771285–7. ( 10.1097/00003086-197710000-00002) [DOI] [PubMed] [Google Scholar]
- 9.Bick EM, Copel JW. The ring apophysis of the human vertebra; contribution to human osteogeny. II. Journal of Bone and Joint Surgery. Am. 195133–A783–787 (http://www.ncbi.nlm.nih.gov/pubmed/14850517) [PubMed] [Google Scholar]
- 10.Bradford DS, Brown DM, Moe JH, Winter RB, Jowsey J. Scheuermann’s kyphosis: a form of osteoporosis? Clinical Orthopaedics and Related Research 197611810–15 (http://www.ncbi.nlm.nih.gov/pubmed/954261) [PubMed] [Google Scholar]
- 11.Gilsanz V, Gibbens DT, Carlson M, King J. Vertebral bone density in Scheuermann disease. Journal of Bone and Joint Surgery. American Volume 198971894–897. ( 10.2106/00004623-198971060-00014) [DOI] [PubMed] [Google Scholar]
- 12.Lambrinudi C.Adolescent and senile kyphosis. BMJ 19342800–820.2. ( 10.1136/bmj.2.3852.800) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hosman AJ, de Kleuver M, Anderson PG, van Limbeek J, Langeloo DD, Veth RP, Slot GH. Scheuermann kyphosis: the importance of tight hamstrings in the surgical correction. Spine (Phila Pa 1976) 2003282252–2259. ( 10.1097/01.BRS.0000085097.63326.95) [DOI] [PubMed] [Google Scholar]
- 14.Fotiadis E, Grigoriadou A, Kapetanos G, Kenanidis E, Pigadas A, Akritopoulos P, Samoladas E. The role of sternum in the etiopathogenesis of Scheuermann disease of the thoracic spine. Spine (Phila Pa 1976) 200833E21–E24. ( 10.1097/BRS.0b013e31815e5df0) [DOI] [PubMed] [Google Scholar]
- 15.Tribus CB.Scheuermann’s kyphosis in adolescents and adults: diagnosis and management. Journal of the American Academy of Orthopaedic Surgeons 1998636–43. ( 10.5435/00124635-199801000-00004) [DOI] [PubMed] [Google Scholar]
- 16.Halal F, Gledhill RB, Fraser C. Dominant inheritance of Scheuermann’s juvenile kyphosis. American Journal of Diseases of Children 1978132 1105–1107. ( 10.1001/archpedi.1978.02120360061011) [DOI] [PubMed] [Google Scholar]
- 17.Dai Y, Li Y, Li P, Li L, Tu Z, Wang B. Familial lumbar Scheuermann disease with idiopathic scoliosis in China: first case report. Medicine (Baltimore) 201796 e7100. ( 10.1097/MD.0000000000007100) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zaidman AM, Zaidman MN, Strokova EL, Korel AV, Kalashnikova EV, Rusova TV, Mikhailovsky MV. The mode of inheritance of Scheuermann’s disease. BioMed Research International 201320131–9. ( 10.1155/2013/973716) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hurtado-Avilés J, Roca-González J, Santonja-Medina F. Hypothesis about an existent biomechanical cause-effect relationship between Schëuermann’s kyphosis and scoliosis. Medical Hypotheses 20158594–98. ( 10.1016/j.mehy.2015.04.008) [DOI] [PubMed] [Google Scholar]
- 20.Tsirikos AI.Scheuermann’s kyphosis: an update. Journal of Surgical Orthopaedic Advances 200918122–128 (http://www.ncbi.nlm.nih.gov/pubmed/19843436) [PubMed] [Google Scholar]
- 21.Lowe TG, Line BG. Evidence based medicine: analysis of Scheuermann kyphosis. Spine (Phila Pa 1976) 200732(19) S115–S119. ( 10.1097/BRS.0b013e3181354501) [DOI] [PubMed] [Google Scholar]
- 22.Murray PM, Weinstein SL, Spratt KF. The natural history and long-term follow-up of Scheuermann kyphosis. Journal of Bone and Joint Surgery. American Volume 199375236–248. ( 10.2106/00004623-199302000-00011) [DOI] [PubMed] [Google Scholar]
- 23.Scheuermann H.Scheuermann’s Kyphosis. Published Online 1920. ( 10.1016/B978-1-4160-3372-1.50011-1) [DOI] [Google Scholar]
- 24.Trotta A, Corrado A, Soragnese MF, Santoro N, Cantatore FP. Adult Scheuermann’s disease as cause of mechanic dorsalgia. Reumatismo 20086014–21. ( 10.4081/reumatismo.2008.14) [DOI] [PubMed] [Google Scholar]
- 25.Urrutia J, Narvaez F, Besa P, Meissner-Haecker A, Rios C, Piza C. Scheuermann’s disease in patients 15–40 years old: a study to determine its prevalence and its relationship with age and sex using chest radiographs as screening tool. Journal of Orthopaedic Science 201924776–779. ( 10.1016/j.jos.2018.12.024) [DOI] [PubMed] [Google Scholar]
- 26.Ristolainen L, Kettunen JA, Kujala UM, Heinonen A, Schlenzka D. Progression of untreated mild thoracic Scheuermann’s kyphosis – radiographic and functional assessment after mean follow-up of 46 years. Journal of Orthopaedic Science 201722652–657. ( 10.1016/j.jos.2017.03.009) [DOI] [PubMed] [Google Scholar]
- 27.Lowe TG.Double L-rod instrumentation in the treatment of severe kyphosis secondary to Scheuermann’s disease. Spine (Phila Pa 1976) 198712336–341. ( 10.1097/00007632-198705000-00005) [DOI] [PubMed] [Google Scholar]
- 28.Bradford DS.Juvenile kyphosis. Clinical Orthopaedics and Related Research 197712845–55. ( 10.1097/00003086-197710000-00008) (http://www.ncbi.nlm.nih.gov/pubmed/598175) [DOI] [PubMed] [Google Scholar]
- 29.Moquin RR, Rosner MK, Cooper PB. Combined anterior-posterior fusion with laterally placed threaded interbody cages and pedicle screws for Scheuermann kyphosis. Case report and review of the literature. Neurosurgical Focus 200314 e10. ( 10.3171/foc.2003.14.1.11) [DOI] [PubMed] [Google Scholar]
- 30.Tsirikos AI, Jain AK. Scheuermann’s kyphosis; current controversies. Journal of Bone and Joint Surgery. (British Volume) 201193857–864. ( 10.1302/0301-620X.93B7.26129) [DOI] [PubMed] [Google Scholar]
- 31.Tomé-Bermejo F, Tsirikos AI. [Current concepts on Scheuermann kyphosis: clinical presentation, diagnosis and controversies around treatment]. Revista Española de Cirugía Ortopédica y Traumatología 201256491–505. ( 10.1016/j.recot.2012.07.002) [DOI] [PubMed] [Google Scholar]
- 32.Ogilvie JW, Sherman J. Spondylolysis in Scheuermann’s disease. Spine (Phila Pa 1976) 198712251–253. ( 10.1097/00007632-198704000-00010) [DOI] [PubMed] [Google Scholar]
- 33.Somhegyi A, Ratko I. Hamstring tightness and Scheuermann’s disease. Commentary. American Journal of Physical Medicine and Rehabilitation 199372 44. ( 10.1097/00002060-199302000-00010) [DOI] [PubMed] [Google Scholar]
- 34.Wenger DR, Frick SL. Scheuermann kyphosis. Spine (Phila Pa 1976) 1999242630–2639. ( 10.1097/00007632-199912150-00010) [DOI] [PubMed] [Google Scholar]
- 35.Lowe TG.Scheuermann’s kyphosis. Neurosurgery Clinics of North America 200718305–315. ( 10.1016/j.nec.2007.02.011) [DOI] [PubMed] [Google Scholar]
- 36.Ding Y, Lv S, Dong S, Cui J, Cao Z, Chen Y. Relationship between Scheuermann disease and symptomatic thoracic spinal stenosis: A retrospective study. Acta Orthopaedica et Traumatologica Turcica 202155253–257. ( 10.5152/j.aott.2021.20022) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Liu N, Chen Z, Qi Q, Shi Z. The relationship of symptomatic thoracolumbar disc herniation and Scheuermann’s disease. European Spine Journal 2014231059–1066. ( 10.1007/s00586-013-3108-7) [DOI] [PubMed] [Google Scholar]
- 38.Ali RM, Green DW, Patel TC. Scheuermann’s kyphosis. Current Opinion in Pediatrics 19991166–69. ( 10.1097/00008480-199902000-00014) [DOI] [PubMed] [Google Scholar]
- 39.Lowe TG.Scheuermann disease. Journal of Bone and Joint Surgery. American Volume 199072940–945. ( 10.2106/00004623-199072060-00026) [DOI] [PubMed] [Google Scholar]
- 40.Papagelopoulos PJ, Mavrogenis AF, Savvidou OD, Mitsiokapa EA, Themistocleous GS, Soucacos PN. Current concepts in Scheuermann’s kyphosis. Orthopedics 20083152––60. ( 10.3928/01477447-20080101-33) [DOI] [PubMed] [Google Scholar]
- 41.Sebaaly A, Silvestre C, Rizkallah Met al. Revisiting thoracic kyphosis: a normative description of the thoracic sagittal curve in an asymptomatic population. European Spine Journal 2020Lll1–6. ( 10.1007/s00586-020-06670-7) [DOI] [PubMed] [Google Scholar]
- 42.Lowe TG, Kasten MD. An analysis of sagittal curves and balance after Cotrel-Dubousset instrumentation for kyphosis secondary to Scheuermann’s disease. A review of 32 patients. Spine (Phila Pa 1976) 1994191680–1685. ( 10.1097/00007632-199408000-00005) [DOI] [PubMed] [Google Scholar]
- 43.Cho W, Lenke LG, Bridwell KH, Hu G, Buchowski JM, Dorward IG, Pahys JM, Cho SK, Kang MM, Zebala LPet al. The prevalence of abnormal preoperative neurological examination in Scheuermann kyphosis: correlation with X-ray, magnetic resonance imaging, and surgical outcome. Spine (Phila Pa 1976) 2014391771–1776. ( 10.1097/BRS.0000000000000519) [DOI] [PubMed] [Google Scholar]
- 44.Bradford DS.Juvenile kyphosis. Clinical Orthopaedics and Related Research 19778445–55. ( 10.1016/j.jbspin.2016.10.007) [DOI] [PubMed] [Google Scholar]
- 45.Mansfield JT, Bennett M.Scheuermann Disease (http://www.ncbi.nlm.nih.gov/pubmed/29763141) 2022. [PubMed] [Google Scholar]
- 46.McDonnell JM, Ahern DP, Lui DF, Yu H, Lehovsky J, Noordeen H, Molloy S, Butler JS, Gibson A. Two-stage anterior and posterior fusion versus one-stage posterior fusion in patients with Scheuermann’s kyphosis. Bone and Joint Journal 2020102–B1368–1374. ( 10.1302/0301-620X.102B10.BJJ-2020-0273.R3) [DOI] [PubMed] [Google Scholar]
- 47.Huq S, Ehresman J, Cottrill E, Ahmed AK, Pennington Z, Westbroek EM, Sciubba DM. Treatment approaches for Scheuermann kyphosis: a systematic review of historic and current management. Journal of Neurosurgery. Spine 201932235–247. ( 10.3171/2019.8.SPINE19500) [DOI] [PubMed] [Google Scholar]
- 48.Palazzo C, Sailhan F, Revel M. Scheuermann’s disease: an update. Joint Bone Spine 201481209–214. ( 10.1016/j.jbspin.2013.11.012) [DOI] [PubMed] [Google Scholar]
- 49.Patel DR, Kinsella E. Evaluation and management of lower back pain in young athletes. Translational Pediatrics 20176225–235. ( 10.21037/tp.2017.06.01) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.de Mauroy J, Weiss H, Aulisa A, Aulisa L, Brox J, Durmala J, Fusco C, Grivas T, Hermus J, Kotwicki Tet al. 7th SOSORT consensus paper: conservative treatment of idiopathic & Scheuermann’s kyphosis. Scoliosis 20105 9. ( 10.1186/1748-7161-5-9) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.de Loubresse CG, Vialle R, Wolff S.Cyphoses pathologiques. EMC-Rhumatologie-Orthopédie 2294–334. [Google Scholar]
- 52.Gennari JM, Aswad R, Ripoll B, Bergoin M. Indications for surgery in so-called “regular" thoracic and thoracolumbar kyphosis. European Spine Journal 1997625–32. ( 10.1007/BF01676571) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ashraf A, Noelle Larson A, Polly DW, Ferski G, Guidera KJ, Mielke CH. Change in sagittal plane alignment following surgery for Scheuermann’s kyphosis. Spine Deformity 20142404–409. ( 10.1016/j.jspd.2014.04.013) [DOI] [PubMed] [Google Scholar]
- 54.McKay MJ, Baldwin JN, Ferreira P, Simic M, Vanicek N, Burns J. & 1000 Norms Project Consortium. Normative reference values for strength and flexibility of 1,000 children and adults. Neurology 20178836–43. ( 10.1212/WNL.0000000000003466) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Otsuka NY, Hall JE, Mah JY. Posterior fusion for Scheuermann’s kyphosis. Clinical Orthopaedics and Related Research 1990251134–139. ( 10.1097/00003086-199002000-00021) [DOI] [PubMed] [Google Scholar]
- 56.Papagelopoulos PJ, Klassen RA, Peterson HA, Dekutoski MB. Surgical treatment of Scheuermann’s disease with segmental compression instrumentation. Clinical Orthopaedics and Related Research 2001386139–149. ( 10.1097/00003086-200105000-00018) [DOI] [PubMed] [Google Scholar]
- 57.Bradford DS, Moe JH, Montalvo FJ, Winter RB. Scheuermann’s kyphosis and roundback deformity. Results of Milwaukee brace treatment. Journal of Bone and Joint Surgery. American Volume 197456740–758. ( 10.2106/00004623-197456040-00009) [DOI] [PubMed] [Google Scholar]
- 58.Temponi EF, de Macedo RD, Pedrosa LOG, Fontes BPC. Scheuermann’s kyphosis: comparison between the posterior approach associated with smith-Petersen osteotomy and combined anterior-posterior fusion. Revista Brasileira de Ortopedia 201146709–717. ( 10.1016/S2255-4971(1530329-3) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yun C, Shen CL. Anterior release for Scheuermann’s disease: a systematic literature review and meta-analysis. European Spine Journal 201726921–927. ( 10.1007/s00586-016-4632-z) [DOI] [PubMed] [Google Scholar]
- 60.De Jonge T, Illés T, Bellyei A. Surgical correction of Scheuermann’s kyphosis. International Orthopaedics 20012570–73. ( 10.1007/s002640100232) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Cho KJ, Lenke LG, Bridwell KH, Kamiya M, Sides B. Selection of the optimal distal fusion level in posterior instrumentation and fusion for thoracic hyperkyphosis: the sagittal stable vertebra concept. Spine (Phila Pa 1976) 200934765–770. ( 10.1097/BRS.0b013e31819e28ed) [DOI] [PubMed] [Google Scholar]
- 62.Kim HJ, Nemani V, Boachie-Adjei O, Cunningham ME, Iorio JA, O’Neill K, Neuman BJ, Lenke LG. Distal fusion level selection in Scheuermann’s kyphosis: a comparison of lordotic disc segment versus the sagittal stable vertebrae. Global Spine Journal 20177254–259. ( 10.1177/2192568217699183) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Gong Y, Yuan L, He M, Yu M, Zeng Y, Liu X, Chen Z. Comparison between stable sagittal vertebra and first lordotic vertebra instrumentation for prevention of distal junctional kyphosis in Scheuermann disease: systematic review and meta-analysis. Clinical Spine Surgery 201932330–336. ( 10.1097/BSD.0000000000000792) [DOI] [PubMed] [Google Scholar]
- 64.Denis F, Sun EC, Winter RB. Incidence and risk factors for proximal and distal junctional kyphosis following surgical treatment for Scheuermann kyphosis: minimum five-year follow-up. Spine (Phila Pa 1976) 200934E729–E734. ( 10.1097/BRS.0b013e3181ae2ab2) [DOI] [PubMed] [Google Scholar]
- 65.Park SJ, Lee CS, Chung SS, Lee JY, Kang SS, Park SH. Different risk factors of proximal junctional kyphosis and proximal junctional failure following long instrumented fusion to the sacrum for adult spinal deformity: survivorship analysis of 160 patients. Neurosurgery 201780279–286. ( 10.1227/NEU.0000000000001240) [DOI] [PubMed] [Google Scholar]
- 66.Ghasemi A, Stubig T, A Nasto L, Ahmed M, Mehdian H. Distal junctional kyphosis in patients with Scheuermann’s disease: a retrospective radiographic analysis. European Spine Journal 201726913–920. ( 10.1007/s00586-016-4924-3) [DOI] [PubMed] [Google Scholar]
- 67.Horn SR, Poorman GW, Tishelman JC, Bortz CA, Segreto FA, Moon JY, Zhou PL, Vaynrub M, Vasquez-Montes D, Beaubrun BMet al. Trends in treatment of Scheuermann kyphosis: a study of 1,070 cases From 2003 to 2012. Spine Deformity 20197100–106. ( 10.1016/j.jspd.2018.06.004) [DOI] [PMC free article] [PubMed] [Google Scholar]



 This work is licensed under a
This work is licensed under a