Abstract
Introduction
Obstetric brachial plexus palsy (OBPP) is a serious form of neonatal morbidity. The primary aim of this population‐based registry study was to examine temporal trends, 1997–2019, of OBPP in infants delivered vaginally in a cephalic presentation. The secondary aim was to examine temporal changes in the incidence of associated risk factors.
Material and Methods
This was a population‐based registry study including singleton, cephalic, vaginally delivered infants, 1997–2019, in Sweden. To compare changes in the incidence rates of OBPP and associated risk factors over time, univariate logistic regression was used and odds ratios (OR) with 95% confidence intervals (CI) were calculated.
Results
The incidence of OBPP in infants delivered vaginally in a cephalic presentation decreased from 3.1 per 1000 births in 1997 to 1.0 per 1000 births in 2019 (OR 0.31, 95% CI 0.24–0.40). Conversely, the incidence of shoulder dystocia increased from 2.0 per 1000 in 1997 to 3.3 per 1000 in 2019 (OR 1.64, 95% CI 1.34–2.01). Over time, the proportion of women with body mass index of 30 kg/m2 or greater increased (14.5% in 2019 compared with 8.0% in year 1997, OR 1.96, 95% CI 1.89–2.03), more women had induction of labor (20.5% in 2019 compared with 8.6% in 1997, OR 2.74, 95% CI 2.66–2.83) and epidural analgesia (41.2% in 2019 compared with 29.0% in 1997, OR 1.72, 95% CI 1.68–1.75). In contrast, there was a decrease in the rate of operative vaginal delivery (6.0% in 2019, compared with 8.1% in 1997, OR 0.72, 95% CI 0.69, 0.75) and in the proportion of infants with a birthweight greater than 4500 g (2.7% in 2019 compared with 3.8% in 1997, OR 0.70, 95% CI 0.66–0.74). The decline in the incidence of these two risk factors explained only a small fraction of the overall decrease in OBPP between 1997–2002 and 2015–219.
Conclusions
The incidence of OBPP in vaginally delivered infants in a cephalic presentation at birth decreased during the period 1997–2019 despite an increase in important risk factors including shoulder dystocia.
Keywords: delivery, obstetric; logistic models; mode of delivery; neonatal brachial plexus palsy; obstetric brachial plexus palsy; risk factors; shoulder dystocia; simulation; vacuum extraction, obstetrical
The incidence of obstetric brachial plexus palsy in infants delivered vaginally by cephalic presentation declined in years 1997‐2019 although the incidence of important risk factors for OBPP increased during this time.

Abbreviations
- BMI
body mass index
- CI
confidence interval
- ICD‐10
International Classification of Diseases, 10th revision
- OBPP
obstetric brachial plexus palsy
- OR
odds ratio
Key message.
The incidence of obstetric brachial plexus palsy in infants delivered vaginally in a cephalic presentation declined from 1997 to 2019 although the incidence of important risk factors for obstetric brachial plexus palsy increased during this time.
1. INTRODUCTION
A multitude of risk factors for obstetric brachial plexus palsy (OBPP) in infants associated with pregnancy and delivery have been identified. 1 , 2 , 3 , 4 , 5 A decreasing incidence of OBPP, from 1.7 to 0.9 cases per 1000 live births, paralleled by an increase in the proportion of cesarean deliveries, from 20.9% to 34%, has been reported from the USA. 6 However, temporal trends in OBPP in vaginal deliveries have not been investigated in a population‐based cohort. Examining changes in OBPP incidence over time in a cohort of vaginal deliveries could provide new insights into temporal changes in the rates of this neonatal morbidity.
OBPP has a reported incidence of 0.4 to 5.1 per 1000 live births in population‐based studies. 1 , 2 , 7 Most infants diagnosed with OBPP after birth are born with a cephalic presentation by spontaneous, or operative vaginal deliveries. 3 , 4 , 5 Recent studies have demonstrated that most OBPP resolve spontaneously within a year. Approximately 10%–30% of infants with OBPP do not exhibit complete recovery and they demonstrate various degrees of permanent motor disabilities associated with functional deficits in daily life. 8 Shoulder dystocia is major risk factor for OBPP. Although subjective in nature, both the American College of Obstetricians and Gynecologists practice bulletin 9 and the Royal College of Obstetricians and Gynaecologists green guideline 10 are in agreement on the definition of shoulder dystocia: requirement of additional obstetric maneuvers when gentle downward traction has failed to affect the delivery of the shoulders.
Current data imply that impaction of the shoulder and forceful downward traction applied to the head after the fetal third rotation are important clinical predictors of OBPP. 1 , 2 , 11 , 12 A randomized controlled study by Poujade et al 13 suggested that a “push back” maneuver could decrease the risk of shoulder dystocia in vaginal deliveries. A simulation‐based team‐training program 14 was established in Sweden during the period from 2006 to 2008. Systematic training in standard maneuvers with the use of mannequins and simulators in the management of shoulder dystocia in vaginal deliveries is recommended to all midwives and obstetricians. This systematic training program, designed to reduce the risk of OBPP, is based on the clinical skills suggested by Advanced Life Support in Obstetrics. 15
The primary aim of this population‐based registry study was to examine the annual incidence of OBPP in vaginally delivered infants in a cephalic presentation, recorded in the Swedish Medical Birth Registry during the period 1997–2019.
The secondary aim was to examine temporal trends in the incidence of associated risk factors.
2. MATERIAL AND METHODS
A population‐based registry study was performed using data from the Swedish Medical Birth Registry, where mandatory data on all deliveries are prospectively collected and maintained by the National Board of Health and Welfare. The registry includes approximately 120 variables concerning antenatal care, delivery outcomes, and pediatric examinations of the newborn. The data are considered to be of high quality. 16 The primary outcome, OBPP, was identified using the diagnostic codes (International Classification of Diseases, 10th revision [ICD‐10] codes) for Erb's or Klumpke's paralysis (ICD‐10 codes 14.0 or 14.1). Data from the Swedish Medical Birth Registry regarding diagnoses and correspondent ICD codes have been compared with data from the original medical records and found to be reliable. 16
For descriptive purposes, annual rates of cesarean deliveries in Sweden were calculated. Next, women with a cesarean delivery were excluded from the study so the final study cohort consisted of all women with singleton pregnancies and with the fetus in a cephalic presentation who delivered vaginally in Sweden (1997–2019).
The following known risk factors for OBPP 1 , 2 , 3 , 4 , 5 in pregnancy and delivery were included in the analysis: shoulder dystocia, body mass index (BMI) at first antenatal visit 30 kg/m2 or above, manifest or gestational diabetes mellitus, induction of labor, epidural analgesia, operative vaginal delivery and birthweight more than 4500 g. The definition of shoulder dystocia in Sweden is in line with international guidelines, “requirement of additional obstetric maneuvers when gentle downward traction has failed to affect the delivery of the shoulders”.
2.1. Statistical analyses
Annual rates of OBPP were calculated and changes in the incidence rates of OBPP and associated risk factors over time were analyzed using univariate logistic regression and odds ratios (ORs) with 95% confidence intervals (CI). To examine if changes in the incidence of OBPP over time could be explained by contemporary changes in risk factors, univariate logistic regression was performed with OBPP as outcome and calendar period of delivery (1997–2002, 2003–2008, 2009–2014, and 2015–2019) as exposure, using the first calendar period as reference. Next, multivariate logistic regression was performed including appropriate risk factors, which were entered stepwise (one by one) and combined. All analyses were performed using SAS® software, version 9.4 (SAS Institute Inc., 2017).
2.2. Ethics statement
The study protocol was approved by the Gothenburg Regional Ethical Review Board, Gothenburg, Sweden (agreement no. 327) on May 24, 2016 and by the Regional Ethics Committee in Stockholm (approval number 2022–01155‐02).
3. RESULTS
The total population of singleton infants born vaginally in a cephalic presentation registered in the Swedish Medical Birth Registry during 1997–2019 was 1 877 116.
The incidence of OBPP decreased from 3.1 per 1000 births in 1997 to 1.0 per 1000 births in 2019 (OR 0.31, 95% CI 0.24–0.40). The incidence of shoulder dystocia increased from 2.0 per 1000 in 1997 to 3.3 per 1000 in 2019 (OR 1.64, 95% CI 1.34–2.01; Figure 1). Between 2005 and 2019 the decrease in OBPP incidence occurred despite an increase in the incidence of shoulder dystocia (Figure 1; Table S1–S3).
FIGURE 1.

Temporal trends in incidence (per 1000 deliveries) of obstetric brachial plexus palsy (OBPP) and shoulder dystocia in vaginal deliveries with singleton infants in cephalic presentation, in Sweden, 1997–2019 (n = 1 877 116).
Changes in rates of risk factors for OBPP during the study period are presented in Figure 2 and in Table S2. Over time, the proportion of women with a BMI of 30 kg/m2 or more increased (14.5% in 2019 compared with 8.0% in year 1997, OR 1.96, 95% CI1.89–2.03), more women underwent induction of labor (20.5% in 2019 compared with 8.6% in 1997, OR 2.74, 95% CI 2.66–2.83) and epidural analgesia (not presented in Figure 2; 41.2% in 2019 compared with 29.0% in 1997, OR 1.72, 95% CI 1.68–1.75). In contrast, the proportion of infants with a birthweight of more than 4500 g decreased slightly over time (2.7% in 2019 compared with 3.8% in 1997, OR 0.70, 95% CI 0.66–0.74). Similarly, the rate of operative vaginal delivery (6.0% in 2019 compared with 8.1% in 1997, OR 0.72, 95% CI 0.69–0.75) declined during the study period.
FIGURE 2.
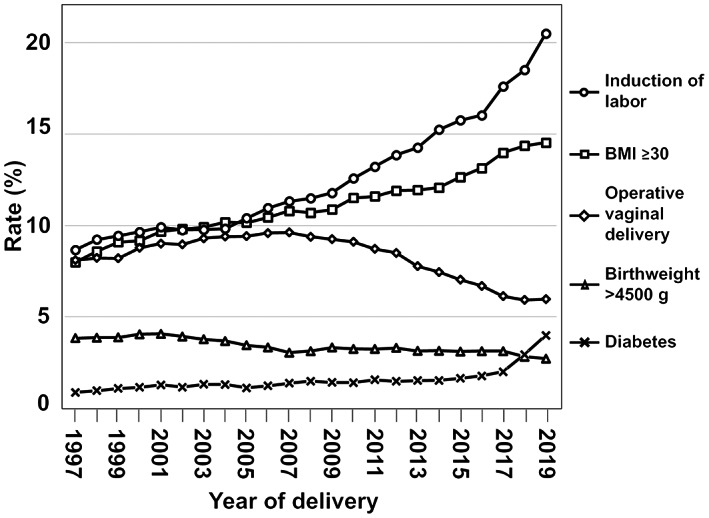
Temporal trends in the incidences (%) of risk factors for obstetric brachial plexus palsy in vaginal, singleton, cephalic deliveries, 1997–2019 in Sweden. BMI, body mass index.
The rate of OBPP decreased during the study period 1997–2019, in women with BMI of 30 kg/m2 or more, with diabetes, induction of labor, with epidural analgesia, and with operative vaginal delivery. There was a 58% decline in OBPP among infants with a birthweight above 4500 g (Table 1).
TABLE 1.
Annual rates n/N (%) of obstetric brachial plexus palsy in vaginal deliveries, 1997–2019, when risk factors were present with odds ratios and 95% confidence intervals for differences in rates comparing 2019 and 1997
| Risk factors for obstetric brachial plexus palsy | ||||||
|---|---|---|---|---|---|---|
| Years | BMI 30+ | Diabetes mellitus | Induction of labor | Epidural analgesia | OVD | Birthweight 4500 g+ |
| 1997 | 34/4631 (0.7) | 12/595 (2.0) | 30/5874 (0.5) | 74/19 820 (0.4) | 67/5530 (1.2) | 73/2614 (2.8) |
| 1999 | 24/5151 (0.5) | 6/702 (0.8) | 26/6098 (0.4) | 55/18 300 (0.3) | 47/5336 (0.9) | 51/2522 (2.0) |
| 2001 | 35/5528 (0.6) | 7/850 (0.8) | 24/6549 (0.4) | 74/19 175 (0.4) | 57/5987 (1.0) | 60/2703 (2.2) |
| 2003 | 41/6676 (0.6) | 23/1019 (2.3) | 43/7564 (0.6) | 100/21 638 (0.5) | 85/7213 (1.2) | 80/2927 (2.7) |
| 2005 | 32/7120 (0.4) | 13/883 (1.5) | 23/8225 (0.3) | 62/22 749 (0.3) | 52/7455 (0.7) | 49/2723 (1.8) |
| 2007 | 36/7882 (0.5) | 11/1134 (1.0) | 30/9357 (0.3) | 62/24 274 (0.3) | 48/7964 (0.6) | 54/2518 (2.1) |
| 2009 | 33/8678 (0.4) | 11/1212 (0.9) | 26/10 109 (0.3) | 58/26 231 (0.2) | 41/7958 (0.5) | 33/2849 (1.2) |
| 2011 | 28/9615 (0.3) | 6/1372 (0.4) | 27/11 585 (0.2) | 51/28 951 (0.2) | 27/7652 (0.4) | 47/2850 (1.6) |
| 2013 | 41/10048 (0.4) | 11/1350 (0.8) | 39/12 629 (0.3) | 61/29 833 (0.2) | 38/6892 (0.6) | 43/2781 (1.6) |
| 2015 | 29/10 841 (0.3) | 7/1849(0.5) | 19/14 259 (0.1) | 45/32 028 (0.1) | 32/6375 (0.5) | 38/2813 (1.4) |
| 2017 | 33/11 843 (0.3) | 17/1826 (0.9) | 46/16 050 (0.3) | 69/33 882 (0.2) | 35/5594 (0.6) | 31/2844 (1.1) |
| 2019 | 23/12 523 (0.2) | 16/3611 (0.4) | 34/18 542 (0.2) | 50/37 285 (0.1) | 25/5404 (0.5) | 29/2455 (1.2) |
| OR (95% CI) 2019 vs 1997 | 0.25 (0.15–0.42) | 0.22 (0.10–0.46) | 0.36 (0.22–0.58) | 0.36 (0.25–0.51) | 0.38 (0.24–0.60) | 0.42 (0.27–0.64) |
Abbreviations: BMI, body mass index; CI, confidence interval; OR, odds ratio; OVD, operative vaginal delivery.
Univariate logistic regression revealed that the crude decrease in OBPP between the first (1997–2002) and the last (2015–2019) period was 61% (Table 2). In comparison, multivariate analysis, adjusted for macrosomia (birthweight >4500 g) and operative vaginal delivery, showed that the adjusted decrease in OBPP was 54%; indicating that 8% ([61–56]/61 = 8%) of the observed decrease in OBPP between the first and the last study period could be explained by decreases in the incidence of these risk factors (Table 2).
TABLE 2.
Crude and adjusted odds ratios, adjusted for changes in rates of fetal birthweight greater than 4500 g and operative vaginal delivery, with 95% confidence intervals for the association between calendar period and obstetric brachial plexus palsy
| Adjustments | 1997–2002 OR (95% CI) | 2003–2008 OR (95% CI) | 2009–2014 OR (95% CI) | 2015–2019 OR (95% CI) |
|---|---|---|---|---|
| Crude | 1.00 (ref) | 0.71 (0.65–0.77) | 0.48 (0.44–0.53) | 0.39 (0.35–0.43) |
| OVD | 1.00 (ref) | 0.69 (0.64–0.75) | 0.48 (0.44–0.53) | 0.42 (0.38–0.46) |
| Fetal birthweight >4500 g | 1.00 (ref) | 0.74 (0.68–0.81) | 0.51 (0.46–0.56) | 0.42 (0.38–0.47) |
| OVD + fetal birthweight >4500 g | 1.00 (ref) | 0.72 (0.66–0.79) | 0.51 (0.47–0.56) | 0.46 (0.41–0.51) |
Abbreviations: CI, confidence interval; OR, odds ratio; OVD, operative vaginal delivery.
Annual rates of cesarean deliveries in Sweden during the study period are presented in Table S3.
4. DISCUSSION
There was a significant decrease in the incidence of OBPP in singleton fetuses, in a cephalic presentation, delivered vaginally between 1997 and 2019. This decline occurred despite a rise in the incidence of the major risk factor shoulder dystocia and in BMI of 30 kg/m2 or more, epidural analgesia, and induction of labor. Previous studies have shown a decline in OBPP parallel to an increase in cesarean section rates. 6 To our knowledge, no previous population‐based study has focused on temporal trends in OBPP in a cohort restricted to cephalic vaginal deliveries.
The rise in the incidence of shoulder dystocia could be a factual increase but could also be an effect of a better awareness and knowledge about shoulder dystocia. The diagnosis of shoulder dystocia is subjective, and changes in prevalence should be interpreted with caution. Increasing rates of shoulder dystocia have also been reported from Finland in an article by Heinonen et al. 17 The authors suggest that this could be partly explained by the implementation of simulation‐based training for shoulder dystocia in 2014, resulting in improved recognition and reporting of this diagnosis.
In the study from Finland, the authors also noted a decline in the incidence of Erb's and Klumpke's palsy and suggested the decrease in rates of macrosomia as one potential factor driving this decrease. 15 Importantly, the incidence of this strong risk factor also decreased in Sweden during the study period. However, the incidence of OBPP in this high‐risk group was 2.8% in 1997 but had decreased more than 50% in 2019, and when adjusting for the decrease in the rate of infants with macrosomia between 1997 and 2019 this did not explain a substantial proportion of the overall decline in OBPP.
The decrease in OBPP can have many explanations. Knowledge about the best method to manage shoulder dystocia has grown, as well as the introduction of continuous simulation‐based training. It is beyond the scope of this study to evaluate the impact of the established simulation‐based training programs but considering the decline in OBPP from 2005 and onwards and the concurrent increase in shoulder dystocia it cannot be ruled out that there is an association. These results are in agreement with previous studies 6 , 13 , 14 , 15 analyzing the relationship between OBPP and management of shoulder dystocia. The results from these studies indicate that preparation of the delivery team and improved management of shoulder dystocia are associated with a reduced risk of OBPP in infants. A 2018 study by Dahlberg et al 14 from Linköping, Sweden reported a lower incidence of OBPP in vaginal deliveries after the introduction of simulation‐based shoulder dystocia training in accordance with Advanced Life Support in Obstetrics. 15 Knowledge of the regional anatomy of the brachial plexus is fundamental for midwives and obstetricians to understand the maneuvers that increase or decrease the risk of OBPP in infants delivered vaginally in a cephalic presentation. 14 , 18 , 19
It could be argued that parts of the decrease in OBPP in vaginal deliveries over time could be the result of an increasing rate of cesarean delivery in Sweden. However, the rise in cesarean delivery rates in Sweden has not been at the same pace as in other high‐income countries and after 2004 the rate has been stable (17%), coinciding with the decrease in OBPP. This indicates that an increasing cesarean rate is unlikely to explain the decline in OBPP. Also, this decreasing trend in OBPP was not only found in the whole study cohort but also in subgroups of women with strong risk factors present for OBPP. This indicates that the overall decrease in OBPP was not primarily the result of a decrease in important risk factors but rather an effect of clinical variables not included in our analysis.
Our study has several strengths. Firstly, the large sample size of more than 1.4 million cephalic vaginal deliveries, including virtually all deliveries in the Swedish population during the study period, allowed us to report changes in the incidence of OBPP over time and its relation with associated risk factors. A limitation of this population‐based study is the retrospective design. However, as OBPP is a rare condition, a randomized trial to examine the effects of the implementation of a training program is not feasible.
5. CONCLUSION
There was a decreasing temporal trend in the incidence of OBPP in vaginally delivered singletons in Sweden. This occurred despite an increasing trend in shoulder dystocia and in risk factors including BMI at first antenatal visit of 30 kg/m2 or above, manifest or gestational diabetes mellitus, induction of labor, and epidural analgesia. The results from our study indicate that it has been possible to lower the incidence of OBPP in vaginal deliveries.
AUTHOR CONTRIBUTIONS
MM, CS, LVL, HE, CS, and LL designed and carried out the study and wrote the paper. LL performed the initial statistical analyses and LVL made the final analyses. All authors approved the final version of the manuscript.
FUNDING INFORMATION
This study was supported by Stiftelsen Mary von Sydows, född Wijk, donationsfond.
CONFLICT OF INTEREST
The authors have stated explicitly that there are no conflicts of interest in connection with this article.
Supporting information
Table S1–S3
Mollberg M, Ladfors LV, Strömbeck C, Elden H, Ladfors L. Increased incidence of shoulder dystocia but a declining incidence of obstetric brachial plexus palsy in vaginally delivered infants. Acta Obstet Gynecol Scand. 2023;102:76‐81. doi: 10.1111/aogs.14481
REFERENCES
- 1. Sjoberg I, Erichs K, Bjerre I. Cause and effect of obstetric (neonatal) brachial plexus palsy. Acta Paediatr Scand. 1988;77:357‐364. [DOI] [PubMed] [Google Scholar]
- 2. Bager B. Perinatally acquired brachial plexus palsy‐‐a persisting challenge. Acta Paediatr. 1997;86:1214‐1219. [DOI] [PubMed] [Google Scholar]
- 3. Walle T, Hartikainen‐Sorri AL. Obstetric shoulder injury. Associated risk factors, prediction and prognosis. Acta Obstet Gynecol Scand. 1993;72:450‐454. [DOI] [PubMed] [Google Scholar]
- 4. Ecker JL, Greenberg JA, Norwitz ER, Nadel AS, Repke JT. Birth weight as a predictor of brachial plexus injury. Obstet Gynecol. 1997;89:643‐647. [DOI] [PubMed] [Google Scholar]
- 5. Mollberg M, Hagberg H, Bager B, Lilja H, Ladfors L. High birthweight and shoulder dystocia: the strongest risk factors for obstetrical brachial plexus palsy in a Swedish population‐based study. Acta Obstet Gynecol Scand. 2005;84:654‐659. [DOI] [PubMed] [Google Scholar]
- 6. DeFrancesco CJ, Shah DK, Rogers BH, Shah AS. The epidemiology of brachial plexus birth palsy in the United States: declining incidence and evolving risk factors. J Pediatr Orthop. 2019;39:e134‐e140. [DOI] [PubMed] [Google Scholar]
- 7. McFarland LV, Raskin M, Daling JR, Benedetti TJ. Erb/Duchenne's palsy: a consequence of fetal macrosomia and method of delivery. Obstet Gynecol. 1986;68:784‐788. [PubMed] [Google Scholar]
- 8. Strombeck C, Krumlinde‐Sundholm L, Forssberg H. Functional outcome at 5 years in children with obstetrical brachial plexus palsy with and without microsurgical reconstruction. Dev Med Child Neurol. 2000;42:148‐157. [DOI] [PubMed] [Google Scholar]
- 9. Practice bulletin No. 178: shoulder dystocia. Obstet Gynecol. 2017;129:e123‐e133. [DOI] [PubMed] [Google Scholar]
- 10. Shoulder dystocia. Green‐top Guideline No. 42:2012: Royal College of Obstetricians and Gynaecologists. 2012. Available from: https://www.rcog.org.uk/guidance/browse‐all‐guidance/green‐top‐guidelines/shoulder‐dystocia‐green‐top‐guideline‐no‐42/
- 11. Lagerkvist AL, Johansson U, Johansson A, Bager B, Uvebrant P. Obstetric brachial plexus palsy: a prospective, population‐based study of incidence, recovery, and residual impairment at 18 months of age. Dev Med Child Neurol. 2010;52:529‐534. [DOI] [PubMed] [Google Scholar]
- 12. Mollberg M, Wennergren M, Bager B, Ladfors L, Hagberg H. Obstetric brachial plexus palsy: a prospective study on risk factors related to manual assistance during the second stage of labor. Acta Obstet Gynecol Scand. 2007;86:198‐204. [DOI] [PubMed] [Google Scholar]
- 13. Poujade O, Azria E, Ceccaldi PF, et al. Prevention of shoulder dystocia: a randomized controlled trial to evaluate an obstetric maneuver. Eur J Obstet Gynecol Reprod Biol. 2018;227:52‐59. [DOI] [PubMed] [Google Scholar]
- 14. Dahlberg J, Nelson M, Dahlgren MA, Blomberg M. Ten years of simulation‐based shoulder dystocia training‐ impact on obstetric outcome, clinical management, staff confidence, and the pedagogical practice ‐ a time series study. BMC Pregnancy Childbirth. 2018;18:361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. ACOG practice patterns. Shoulder dystocia. Number 7, October 1997 . American College of Obstetricians and Gynecologists. Int J Gynaecol Obstet. 1998;60(3):306‐313. [PubMed] [Google Scholar]
- 16. Cnattingius S, Ericson A, Gunnarskog J, Källén B. A quality study of a medical birth registry. Scand J Soc Med. 1990;18:143‐148. [DOI] [PubMed] [Google Scholar]
- 17. Heinonen K, Saisto T, Gissler M, Kaijomaa M, Sarvilinna N. Rising trends in the incidence of shoulder dystocia and development of a novel shoulder dystocia risk score tool: a nationwide population‐based study of 800 484 Finnish deliveries. Acta Obstet Gynecol Scand. 2021;100:538‐547. [DOI] [PubMed] [Google Scholar]
- 18. Narakas AO. The treatment of brachial plexus injuries. Int Orthop. 1985;9:29‐36. [DOI] [PubMed] [Google Scholar]
- 19. Inglis SR, Feier N, Chetiyaar JB, et al. Effects of shoulder dystocia training on the incidence of brachial plexus injury. Am J Obstet Gynecol. 2011;204(322):e1‐e6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1–S3


