Abstract
Multiresistant Escherichia coli has been disseminated worldwide, and it is one of the major causative agents of nosocomial infections. E. coli has a remarkable and complex genomic plasticity for taking up and accumulating genetic elements; thus, multiresistant high-risk clones can evolve. In this review, we summarise all available data about internationally disseminated extraintestinal pathogenic high-risk E. coli clones based on whole-genome sequence (WGS) data and confirmed outbreaks. Based on genetic markers, E. coli is clustered into eight phylogenetic groups. Nowadays, the E. coli ST131 clone from phylogenetic group B2 is the predominant high-risk clone worldwide. Currently, strains of the C1-M27 subclade within clade C of ST131 are circulating and becoming prominent in Canada, China, Germany, Hungary and Japan. The C1-M27 subclade is characterised by blaCTX-M-27. Recently, the ST1193 clone has been reported as an emerging high-risk clone from phylogenetic group B2. ST38 clone carrying blaOXA-244 (a blaOXA-48-like carbapenemase gene) caused several outbreaks in Germany and Switzerland. Further high-risk international E. coli clones include ST10, ST69, ST73, ST405, ST410, ST457. High-risk E. coli strains are present in different niches, in the human intestinal tract and in animals, and persist in environment. These strains can be transmitted easily within the community as well as in hospital settings. WGS analysis is a useful tool for tracking the dissemination of resistance determinants, the emergence of high-risk mulitresistant E. coli clones and to analyse changes in the E. coli population on a genomic level.
Keywords: multidrug resistance, nosocomial infections, E. coli high-risk clones, whole-genome-sequencing
1. Introduction
Escherichia coli is a Gram-negative rod-shaped commensal bacterium in the human intestine; however, it is also a major causative agent of several infections. Extraintestinal pathogenic E. coli (ExPEC) is responsible for a wide range of severe community- and hospital-acquired infections, such as neonatal meningitis, peritonitis, and bloodstream and urinary tract infections (UTI) [1,2]. Furthermore, multiresistant E. coli strains are responsible for a high number of hospital outbreaks worldwide that are associated with longer hospital stays, increased health care costs and high mortality rates [3,4,5].
E. coli has a remarkable capacity to take up and to accumulate various genetic materials, including plasmids, integrons, and transposons through horizontal gene transfer; thus, E. coli can acquire different antibiotic resistance genes, enabling it to develop multiresistance [6,7]. Currently, extended-spectrum beta-lactamase (ESBL)- and carbapenemase-producing E. coli are of great concern worldwide [8,9]. The most frequently detected ESBLs in E. coli clinical isolates are mainly CTX-M-type enzymes [10,11]; however, transferable genetic elements harbouring carbapenemase genes have also been described, namely, blaNDM (New Delhi metallo-β-lactamase), blaKPC (Klebsiella pneumoniae carbapenemase) and blaOXA-48 (OXA-48 carbapenemase) [12,13,14,15,16,17]. Further antibiotic resistance genes have also been reported in E. coli clinical isolates, namely, fluoroquinolone-, aminoglycoside- and colistin-resistance determinants [18,19,20].
Carbapenem- and third-generation cephalosporin-resistant Enterobacteriaceae are grouped into the ‘critical’ category on the priority list of the World Health Organisation (WHO); therefore, there is an urgent need for effective antibiotics against this pathogen [21]. Some novel antibiotics have already been approved and marketed in recent years to combat multiresistant E. coli infections. Among these recently marketed agents, we find beta-lactam plus beta-lactamase inhibitors (e.g., ceftazidime + avibactam, ceftolozane + tazobactam, meropenem + vaborbactam), fluoroquinolone (e.g., delafloxacin), aminoglycoside (e.g., plazomicin) agents [22,23,24]. Apart from novel antibiotics, some synergistic antibiotic combinations are also available to treat infections caused by multiresistant E. coli [25,26].
Multiresistant E. coli strains possess a remarkably complex genomic plasticity; therefore, they can adapt to different conditions and persist in diverse hosts; moreover, they can be easily transmitted between different hosts. According to the‘One Health’ approach in antimicrobial resistance, E. coli has different reservoirs (human, animal and environmental) and the accumulation of resistance genes can take place in all of the different reservoirs [27,28]. Furthermore, multiresistant E. coli strains can be selected out in human, animal, and environmental niches, resulting in the development of high-risk multiresistant E. coli clones. High-risk clones sustain their fitness, and their dissemination locally or even globally is associated with high variability of resistance and virulence genes [29,30,31,32].
E. coli is classified into eight phylogroups using a PCR-based method, multilocus sequence tying (MLST, Achtman schema), and complete genome data. These phylogroups are A, B1, B2, C, D, E, F and G. This phylogenetic classification of E. coli has been applied to compare serogroup, virulence and resistance traits, as well as the distribution of E. coli strains among various hosts [33,34,35,36] (Figure 1).
Figure 1.
Overview of the phylogenetic groups, sequence types, clades, and subclades of extraintestinal pathogenic E. coli.
According to genetic markers of E. coli, numerous sequence types (ST) and clonal complexes (CC) have been described. Currently, the most frequently reported lineages are ST131, ST69, ST10, ST405, ST38, ST95, ST648, ST73 and ST1193, which have been detected in both hospital- and community-associated infections [37,38,39,40]. A high-risk clone is defined as being globally distributed, associated with multiple antimicrobial resistance determinants, able to colonise and persist in hosts for more than 6 months, capable of effective transmission between hosts, has enhanced pathogenicity and fitness, and is able to cause severe and/or recurrent infections [8]. The remarkable genomic plasticity of E. coli enables it to acquire genes of toxins and different virulence determinants that lead to the development of intestinal pathogen E. coli (IPEC) strains. Notably, enetoropathogenic E. coli (EPEC), enterotoxigenic E. coli (ETEC), enteroinvasive E. coli (EIEC), enterohemorhagic E. coli [41].
In this review, we summarise all available data about multiresistant extraintestinal E. coli internationally disseminated high-risk clones. We analyse these clones based on their WGS data and according to reported outbreaks, and we summarise their resistance profiles and genetic markers. The well-known clones already disseminated, as well as recently emerging clones, will be described, and the ‘One Health’ approach will be also discussed. The selection criteria of reference articles in this review were scientific articles that describe WGS data and outbreaks of high-risk multiresistant E. coli clones.
2. CC/ST131, the Worldwide Predominant High-Risk Clone
E. coli ST131 clone has been disseminated worldwide and is one of the major nosocomial pathogens in hospitals all around the world. This clone also plays an important role of spreading antibiotic resistance [42]. ST131 is characterised by a stepwise diversification, with two main serotypes (O16:H5 and O25:H4), three main clades (A, B and C), and three fimH alleles (41, 22 and 30, respectively), all correlated. Using an alternative taxonomy, ST131 is also classified as subclone H30R or H30Rx according to antibiotic resistance patterns [42,43,44].
Originally, ST131 clone was reported as an O25b:H4 serotype, CTX-M-positive, and ESBL production was commonly detected in this clone from Canada, Korea, India, Kuwait, Lebanon, France, Switzerland, Portugal and Spain. The vast majority of strains in this clone are resistant to several antibiotic groups, namely beta-lactams, aminoglycosides, tetracycline, fluoroquinolones, sulfonamides, chloramphenicol and nitrofurantoin [43,44]. Moreover, in the last 15 years, this clone became the predominant high-risk international clone among ExPEC clinical isolates, as 133 of 169 collected studies have reported its presence from various clinical samples between 1995 and 2018 [15,37,39,45,46,47].
The phylogenetic analysis of whole-genome data classified the ST131 clone as the main member of phylogroup B2, which is known as the initial source of diverse sequence types, including ST1680, ST1982, ST1461, and ST1193 [46,48,49,50]. Compared to other E. coli phylogroups, B2 is also characterised by its high number of virulence factor-encoding genes [51]. On the other hand, unlike other B2 ExPEC strains, ST131 is still frequently detected as an ESBL producer, and in most cases it is also fluoroquinolone resistant [52].
According to resistance traits and population genetics, ST131’s phylogeny has been clustered into three major clades with well-defined resistance profiles, namely clade A, B and C [15] (Figure 1). In general, clade A/H41 and clade B/H22 are described as smaller subgroups [45,52,53]. However, clade A ST131 strains have been found in many community-associated infections, and these have also been reported in stool samples of healthy children from randomly selected primary schools in a study from Changsha, China [46,54]. Furthermore, clade A E. coli strain has been reported in water from the Jurong river reservoir in Singapore. It carried aminoglycoside-transferases and blaCTX-M-27 with mutations in gyrA, parC and parE [55]. On the other hand, clade B has been described as a foodborne pathogen with the ability to colonise poultry, contaminate meat and express colistin resistance genes (mcr-1 and mcr-3). In the case of human infections, clade B strains have been isolated from urine, blood and peritoneal fluid samples [38,46]. It has been hypothesised that another possible source of strains from clade B is the consumption of vegetables from contaminated soil, as this clade has also been detected in agricultural soil. These strains carried a large resistome, including mcr-1.1, blaCTX–M–15 and qnrB19. GenBank Accession number: JAENHI000000000.1 [56]. (Table 1).
Table 1.
Whole-genome sequences of internationally disseminated E. coli sequence types from published reports.
| Sequence Type | Accession Numbers (Bioproject, Biosample, SRA, European Nucleotide Archive, EMBL-EBI Database Project) |
Reference |
|---|---|---|
| ST131-B | JAENHI000000000.1 (E. coli strain S802) | [56] |
| VEWQ00000000 (E. coli strain UPEC U34) | [57] | |
| ST131-C |
JSXN00000000 (E. coli strain NA101) JSXO00000000 (E. coli strain NA112) |
[38] |
|
JACHQR000000000.1 (E. coli strain LMLEEc001) JACHQP000000000.1 (E. coli strain LMLEEc003) JACHQO000000000.1 (E. coli strain LMLEEc010) JACHQK000000000.1 (E. coli strain LMLEEc025) |
[39] | |
| JAJPAL000000000.1 (E. coli strain ECO112) | [20] | |
| NCVZ00000000.1 (E. coli strain EcMO) | [47] | |
| PRJEB46895 (E. coli strain EC-119) | [58] | |
| ST1193 | CP030111 (E. coli strain MCJCHV-1) | [59] |
| JACHQB000000000.1 (E. coli strain LMLEEc041) | [39] | |
| ST69 |
SAMN11246379 (E. coli strain EC81) SAMN11246556 (E. coli strain EC369) SAMN11246590 (E. coli strain EC801) SAMN11246609 (E. coli strain EC820) |
[60] |
| CC10 (ST617) | PIZJ00000000 (E. coli strain ECCO2) | [61] |
| CC10 (ST167) | CP074120 (E. coli strain EC16) | [7] |
| QLNK00000000 (E. coli strain ECWJ1) | [62] | |
| ST405 | AP019803 (E. coli strain KY1497) | [63] |
| ERS4552076 (E. coli strain SSM100) | [64] | |
| NGUU00000000 (E. coli strain WCHEC96200) | [65] | |
|
NXEQ00000000 (E. coli strain 2009-30) NXER00000000 (E. coli strain 2009-27) |
[66] | |
| ST38 | NCWA00000000.1 (E. coli strain Ec6M) | [67] |
| SAMN17315482 (strain URMC_401_E_coli) | [68] | |
|
RZGB00000000 (E. coli strain URMC_9) RZBC00000000 (E. coli strain URMC_13) |
[69] | |
| NCWA00000000.1 (E. coli strain Ec6M) | [47] | |
| MVIO00000000 (E. coli strain NA090) | [38] | |
| ST457 | NDBC00000000 (E. coli strain EM1CRO) | [70] |
| CC23 |
NBCL00000000 (E. coli strain 13B) LYPE00000000 (E. coli strain Ec47VL) |
[71] |
| ST95 |
CP012625 (E. coli strain SF-468) CP012631 (E. coli strain SF-173) CP012633 (E. coli strain SF-166) CP012635 (E. coli strain SF-88) |
[72] |
| ST73 | JACHPD000000000.1 (E. coli strain LMLEEc115) | [39] |
| ST410 | VFBH01000000 (E. coli strain A240) | [73] |
| ST648 |
PEDQ00000000.1 (E. coli strain ICBECG2) PEDR00000000.1 (E. coli strain ICBECG4) |
[74] |
| ST393 |
QGIF00000000 (E. coli strain 77H) QHCX00000000 (E. coli strain 51H) |
[75] |
| ST58 | SRX10825685 (E. coli strain IBIS_39) | [76] |
| ST101 | VYQD00000000 (E. coli strain EC121) | [77] |
Recently, the most significant clinical problems have been related to clade C. It originates from clade B, and consists of two major subclades, namely C1/H30-R and C2/H30-Rx (Figure 1). Their evolution has been demonstrated, as they arose from an early common fluoroquinolone-susceptible ancestor C/H30 subclone with type 1 fimbrial adhesin gene (fimH30). Initially, H30 was the most prevalent among them, emerging in the 1980s. In the course of clonal expansion, it obtained high-level fluoroquinolone resistance by sequential chromosomal mutations of gyrA and parC genes, then it also became resistant against beta-lactams by acquisition of plasmid-mediated ESBLs, as well as carbapenemases [15,29,45,52,53,58]. The self-transmissible plasmids of ST131 are characterised by a remarkable genetic diversity (plasmidome), they belong in particular to incompatibility group F (IncF type). They may possess FIA or FII replicon types, which aid in the successful uptake and rapid dissemination of resistance genes. The most frequently reported plasmid MLST types are F1:A2:B20 in multidrug-resistant (MDR) clade C1 and F2:A1:B of MDR clade C2 [15,78,79]. A recent in-depth analysis showed that by a novel subset of C2, the plasmidome was not uniform; it had a combined pattern of certain plasmid types, and it showed a homogeneous replicon structure of F31/F36:A4:B1 [58].
In general, a common feature of strains in clade C is the carriage of blaTEM. However, subclade C1 presents blaCTX-M-14 or blaCTX-M-27 ESBL genes, while on the other hand, subclade C2, which has a single nucleotide polymorphism (SNP) at fimH30, is mainly associated with blaCTX-M-15. The blaCTX-M-27 positive subset of C1, referred to as subclade C1-M27, recently became prominent in Japan, Canada, Germany and China [20,46,80,81,82]. In Iran, a comparative study on MDR ST131 and non-ST-131 clones reported that both were associated with blaTEM, blaSHV, blaCTX-M, blaOXA-48 genes, as well as with plasmid-mediated quinolone resistance (PMQR) determinants (bifunctional aminoglycoside acetyltransferase-Ib-cr [aac6′-Ib-cr] and Qnr protective proteins [qnrB, qnrS] [83]. A genomic epidemiological investigation of ESBL producer E. coli isolates was also performed in Dhaka, Bangladesh. Not surprisingly, the predominant clone from clinical urine and pus samples was ST131, as this clone accounted for 46% of the isolates. The whole-genome sequences (WGS) of these strains were deposited in GenBank under accession numbers from JACHQR000000000.1 to JACHPB000000000.1 [39]. In Brazil a CTX-M-27-producing E. coli ST131 strain that belonged to clade C1-M27 was reported in oysters. This E. coli strain was recovered from an aquatic area impacted by intensive maritime traffic and transoceanic shipping activities [66]. WGS information is shown in Table 1.
A recent study in Hungary investigated ESBL-producing E. coli isolates obtained from a tertiary care hospital in Budapest. Whole-genome sequence analysis showed that five E. coli isolates belonged to the ST131 clone: two to the C1-M27 subclade with blaCTX-M-27 and three to the C2/H30Rx subclade with blaCTX-M-15. Based on core genome MLST, all C2/H30Rx isolates formed a cluster (≤6 allele differences), while the blaCTX-M-27-producing C1-M27 isolates differed from each other with respect to at least 35 alleles. This study indicates that the C2/H30Rx and C1-M27 subclades of the ST131 are currently circulating among Hungarian clinical isolates [84].
Carbapenem resistance among ST131 strains is based on plasmid-acquired carbapenemase enzymatic activity [82]. According to a recent genomic epidemiological study that investigated clinical isolates from 62 countries between 2015 and 2017, many subtypes of carbapenemases were carried by ST131. During these studies, ST131 was mainly isolated from UTI and bacteraemia. From two different isolates, blaKPC-3- and blaOXA-48-producer ST131-A clade has been reported in USA and Lebanon, respectively. A subclade C1-M27 was also present, which showed positivity for blaNDM-1 from Russia and Philippines, and blaOXA-232 from Thailand. From the C1 subclade, a non-M27 subtype was detected as well, and these strains carried blaKPC-2 in Guatemala, Israel and USA, blaKPC-3 in Italy and blaKPC-18 in the USA. The globally predominant ST131-C2 subclade carried blaKPC-2 in Puerto Rico, blaKPC-3 in Italy, blaNDM-1 in Egypt and blaNDM-5 in Canada. Ambler class D carbapenemase, namely blaOXA-48 and blaOXA-181, production was also described in Egypt and Iran. Additionally, a ST131-C2 strain showed positivity for co-expression of blaNDM-1 and blaVIM-1. [40,82]. Located on plasmids with sequence similarities (95–100%), different carbapenemases of ST131 have been detected in other international clones as well [84,85,86]. Additionally, the co-carriage of blaOXA-1, blaCTX-M-15, aac6-Ib-cr and aac3-IIa has also been detected in strains of C2 clade [58,87].
Another recent survey found CC131 subclones in 10 hospitals in different cities in Argentina. The observed samples were mainly blood, urine and abdominal fluids. The majority (7 of 10 samples) belonged to the C2 subclade, and they carried blaKPC-2, and one strain showed positivity for blaVIM-1. The C1 subclade was also found, and expressed blaCTX-M−2. Furthermore, the so called ECO112 KPC-2-producer strain of clade B was fluoroquinolone-susceptible and carried blaFOX−5. The other isolates of CC131 were resistant to fluoroquinolones based on chromosomal mutations of gyrA, parC or parE, and, additionally, PMQR determinants, namely, qnrB and qnrS1, were also detected. As an interesting result, a strain referenced as ECO14 of ST131 exhibited resistance to colistin (MIC ≥ 4 µg/mL), but it lacked mcr. It developed colistin resistance due to seven chromosomal mutations in the pmrB and pmrA genes (phosphoetanolamin transferase coding genes) [20].
Moreover, in certain cases, O16:H5 ST131 and rare, even non-typeable relatives were also found. These subclones were compared to the most successful O25b:H4 serotype, and studies detected that the so-called O16 subclone has a higher rate of trimethoprim-sulfamethoxazole and gentamicin resistance, but a lower prevalence of fluoroquinolone and ceftriaxone resistance, than O25b [88]. In addition, a study in Kyoto, Japan described a separated O75:H30 cluster within the C1 subclade, which was characterised by an extraordinary Phi-like region (M27PP1). Subsequently, this ExPEC subtype was reported not only in Japan, but also in Thailand, Australia, Canada and in the USA, so its prevalence has been significantly increased [15,80,89].
Finally, the pangenome of clade C is divided into a strongly determined core genome and an additional genetic context with remarkable variability that is responsible for a huge repertoire of virulence factors [83,90]. According to the so-called “perfect storm” theory, acquisition of virulence factors plays an essential role in the clonal expansion of multiresistant bacteria, as the acquirement of these genes is followed by higher antibiotic resistance rates [53]. Based on the PCR-verified presence of certain virulence genes including Afa and Dr adhesins (afa/draBC), operon (afa), catecholate siderophore receptor (iroN), secreted autotransporter toxin (sat), ibeA (‘invasion of brain endothelium’ gene), allele II and III of papG gene (papGII and papGIII), cytotoxic necrotising factor type 1 (cnf1), alpha-hemolysin (hlyA), cytolethal distending toxin (cdtB) and K1 variant of group II capsule (neuC-K1) virotypes are defined from A to E groups [52]. The current evolution of new virotypes in C2 subclade can also be seen, as a study from Singapore demonstrated a monophyletic subclone from bacteraemia referred to as SEA-C2 [58,91].
Interestingly, a comparative genomic analysis of 99 ST131 strains and 40 genomes of other high-risk clones (ST38, ST405 and ST648) showed that clades A, B, and C of ST131 were more distant relatives than the others. This study could not identify any CC131-specific proteins, although the absence of 142 proteins in the core genome of all of the 99 isolates was found. These results suggest that the drive of adaptive strategies of ST131 were mainly loss, exchange, and co-evolution of genes, including that of antimicrobial resistance and virulence [38]. WGS data are available in GenBank (Table 1).
Based on the ‘One Health’ approach, zoonotic risk, as a novel aspect of MDR CC131 global distribution, has been also suggested. As a common feature, many rapid outbreaks of high-risk international MDR bacteria have originated from the human–animal interface [47]. Due to the similar and overlapping molecular regions between avian pathogenic E. coli and ExPEC, it has previously been hypothesised that avian E. coli may act like a reservoir of virulence and resistance markers. Therefore, it may be responsible for foodborne infections in humans [83,92]. In a study from Iran, ST131 strains from human isolates were compared to isolates obtained from broiler chickens. Half of the isolates from chicken meat belonged to phylogroup A, which exhibited a ciprofloxacin-resistant phenotype, but no ST131 was detected in broilers in that study [83]. On the other hand, studies from Spain, Canada and Arizona confirmed the presence of CC131, mainly clade B, in poultry. Moreover, mcr-5- and mcr-9-positive strains were also isolated among these ST131 strains [18,57,93,94].
A genomic surveillance and cell culture-based virulence investigation study demonstrated the co-presence of blaCTX-M-15-positive Klebsiella pneumoniae ST307 and blaCTX-M-27-positive CC131 with other phylogroups of ExPEC MDR clones containing various CTX-M types and AmpC in oysters and mussel specimens from the Atlantic Coast of South America. Marine bivalves are filter-feeding organisms, so they can extract a large amount of material from water, such as human faecal pollution, including MDR bacterial strains. Furthermore, production of thermostable toxin has also been reported among these strains, so a great deal of attention should be paid to seafood as a source of diseases induced by high-risk toxin producer MDR bacterial clones. The whole-genome sequence of this ST131 strain was deposited in GenBank under the accession number NCVZ00000000.1 [47] (Table 1). Furthermore, houseflies have been hypothesised to be vectors of many MDR bacteria, including Pseudomonas aeruginosa, Acinetobacter baumannii, Citrobacter freundii, Enterobacter cloacae, Klebsiella oxytoca and ExPEC clones, such as CC131, in a tertiary hospital in Rwanda, Africa. This clone carried, among others, blaCTX-M-15, blaOXA-1, blaTEM-1B and aac(6′)-Ib-cr. In this case, randomly captured flies were observed in fly traps over 4 weeks from different locations of the hospital, for instance, from the surgery operating theatre, gynaecology, paediatrics, the restaurant, the kitchen, and the laboratory. Interestingly, ST131 was identified only from the kitchen, and the vast majority of the other MDR species had a similar resistome. The results demonstrated that almost all of them carried blaCTX-M-15, blaOXA-1 and some expressed aac(6′)-Ib-cr and qnrB1 [95].
A study from Rwanda investigated 120 ESBL-producing E. coli strains from hospitalised patients. Altogether, 30 different sequence types were detected, including pandemic clonal lineage ST131. Frequently found resistance genes included blaCTX–M–15, tet(34), and aph(6)-Id. Additionally, a phylogenetic relationship was found among strains from patients and their related community members and animals, indicating transmission of clinically relevant, pathogenic ESBL-producing E. coli among patients, animals, caregivers and the community in Rwanda [96].
In summary, the structure of the E. coli population has changed dramatically, with appearance and global dissemination of the currently dominant multidrug-resistant C2 subclade of ST131. Nevertheless, from the most successful phylogroup B2, other high-risk clones can evolve and cause alarming challenges too [37].
3. ST1193, a Recently Emerging Pandemic MDR Clone from Phylogroup B2
Although ST1193, a sister clone of ST131, had already been described in Australia in 2012, case reports of this clone have increased considerably in number only in the last few years. The ST1193 clone is also known as the latest pandemic multidrug-resistant clonal group [46,97,98,99]. A recent study from France described five E. coli strains of ST1193 that were harbouring blaCTX-M-15 and blaCTX-M-27. These strains were obtained from febrile urinary tract infections in children [100]. A study from China reported that E. coli strains of ST1193 were responsible for more than 20% of neonatal invasive infections in China [100,101]. Furthermore, ST1193 was also found together with clade A ST131 strains in stool samples of healthy children in Changsha, China [46].
One strain of ST1193 was isolated in Dhaka, Bangladesh from a urine sample. It expressed a plasmid-acquired blaCTX-M-15, and it belonged to the O75:H5 serogroup. The whole-genome sequence data of this strain are available in GenBank under accession number JACHQB000000000.1 [39]. (Table 1).
Altogether, 355 strains of ST1193 were investigated in a study in the USA, and various resistance determinants were detected, namely, blaTEM-1B, blaCMY-2, blaCTX-M-15, blaCTX-M-27, blaCTX-M-55, blaOXA-1, aac(6)′-Ib-cr, and mutations were detected in genes gyrA, parC and parE. Strains of ST1193 were all lactose non-fermenting and carried fimH64, in particular. Its evolutionary development from K1 to K5 capsular types resulted in genomic changes and uptake of an F-type virulence plasmid were also reported [97]. A study from Hungary recently reported a single E. coli from clinical isolates that belonged to ST1193 and carried blaCTX-M-27 [84].
Carbapenem resistance has occurred in ST1193, and blaKPC-2 and blaNDM-1 have been reported [40]. Moreover, mutations in pmrA and pmrB that confer colistin resistance were also confirmed [102]. The complete ST1193 genome from a neonatal meningitis-associated strain is available in GenBank at accession number: CP030111 [59,97] (Table 1).
4. ST69 and CC10, the Second and Third Most Common High-Risk Clones
Overall, based on a comparative summary of 169 studies about ExPEC high-risk clones after the predominant ST131, we found ST69 and ST10 to be the second and third most frequent clones, respectively [37]. Initially, ST69 was isolated in the year 2000, from urine samples of 228 women with uncomplicated community-acquired UTIs at a public university campus of California. ST69 belongs to phylogenetic group D, and it is characterised by diverse O-antigen-based serogroups and the common presence of papGII. Since then, most of the reported strains of this clone have been multidrug-resistant, and they typically possess a class I integron that includes a single gene cassette including dihydrofolate reductase and aminoglycoside adenyltransferase (dfrA17–aadA5). In these samples, a trimethoprim–sulphamethoxazole-resistant Clonal Group A (CgA) was also detected, a clone that clusters within ST69 [103]. Interestingly, based on findings of the phylogenetic features of E. coli, it was revealed in England that the E. coli population remained stable over time, but some lineages emerged and were disseminated, including ST69 [104]. In total, 87 of 169 studies describe this clone for the period 1995–2018. ST69 is characterised by the presence of blaKPC-2, blaNDM-1 [40], co-carriage of blaNDM-1 with blaCMY-6, [20], blaCTX-M-1,-14,-15,-27 [100], mcr-1 [105], fosA3 [106] and gyrA, parC mutations, leading to fluoroquinolone resistance [107]. During other studies in Italy, this clone has also been identified from various origins, including dairy products, the diaphragms of wild boars, poultry, mussels, clams, and human stool. Aside from human specimens, chicken breast carries a wide spectrum of antimicrobial resistance genes [60,108]. The increasing number of cases of this MDR clone indicates the importance of studies of phylogenetics, population dynamics and molecular epidemiology using the ‘One Health’ approach [37].
CC10 belongs to phylogenetic group A, and it has been detected to be a widely disseminated clone, since it has been reported from food producing animals, free-living birds, plant-based foods, retail meats, wastewater, rivers, urban streams, and clinical settings, as well as being a part of human gut microbiome. Thus, faecal carriage in humans probably played a significant role in its clonal expansion and dissemination. This clonal complex is composed of ST10 and its further relatives, including, among others ST44, ST48, ST167, ST617, ST410, and ST744 [37,109,110] (Figure 1). During a survey aiming to characterise the molecular epidemiology of carbapenemase-producing ExPEC in Argentina, CC10 was the major one, accounting for more than 20% of the samples. Of them, eight contained ST10, and the others were single-locus variants (ST44, ST744, ST167), double-locus variants (ST746, ST617) and a satellite clone (ST12667). On the other hand, CC10 was the main clone reported among carbapenemase producers, as it demonstrated positivity (in order of decreasing abundance) for blaKPC-2, blaNDM-1 and blaIMP-8. As an important finding, two of them showed co-expression of mcr-1; furthermore, another NDM-1-producer isolate was a co-producer of blaPER-2. On the other hand, the ST617 clone exhibited the co-existence of blaKPC-2, blaCTX-M-14 and blaCTX-M-27. The nucleotide sequence information was submitted in GenBank under the BioProject accession number PRJNA784589 [20] (Table 1). In addition to β-lactam resistance, CC10 has also been marked by fluoroquinolone-resistance determinants (e.g., qnrS1, aac(6′)-Ib-cr) and the mcr-1 colistin-resistance gene [7,60,111,112]. In addition, blaOXA-48 associated with ST10; blaNDM-1 related to ST44, ST48, ST167, ST617; blaCTX-M-14,15,55, fosA3, blaOXA-1, blaNDM-1,9, blaNDM-5 together with blaOXA-181 and co-carriage of blaOXA-48 in ST167; as well as blaKPC-2,3 with blaNDM-1 in ST617 have also been reported. Of these high-risk CC10 lineages, in the last few years, ST167 was clustered into subclades, and it was reported to be a predominant clone in China. This clone was also identified from a urine clinical sample as a qepA4 carrier [7,40,61,62,112,113].
Several studies have been reported indicating the high risk potential of ST410 from phylogenetic group A [5] (Figure 1). This clone has been described in many countries, albeit to a lesser extent compared to other high-risk clones. ST410 has been reported to be a clone that is transmitted between different reservoirs, namely, between wildlife, humans, companion animals, and the environment [114,115]. The ST410 clone has been reported as being blaOXA-181 positive in China [116] and Italy [117], as well as hospital outbreaks in Denmark [118]. A study from Dhaka, Bangladesh reported ST410 as being blaCTX-M-15 positive [39].
A whole-genome sequence analysis of E. coli ST410 in Denmark revealed carriage of blaOXA-181 and blaNDM-5 on IncX3 and IncF plasmids, respectively [119].
5. ST405 and High-Risk CC/ST38 Clones from Phylogenetic Group D
ST405 is a globally reported clone that carries similar variants of virulence genes to O25b:H4 ST131 [65]. Recently, this clone was marked as a potential reservoir for blaNDM-5 [40,62,119]. NDM-5-producing ST405 has been detected in many geographic regions, but it has shown the highest prevalence in the United Kingdom and Italy [63,120,121].
Moreover, an autochthonous case in 2018 was reported in Italy. The isolated strain carried blaNDM-5, and among others blaCMY-42, aadA2, mdf(A), sul1 and alterations of gyrA, parC, parE [121]. The presence of blaNDM-5 has also been detected in Japan and Mozambique, Africa [63,64]. This clone in Japan was non-susceptible to fluoroquinolones and β-lactams, including broad-spectrum cephalosporins and carbapenems, but it kept its susceptibility against tigecycline. The complete genome sequence of this strain is available under BioProject number: PRJDB8512 [63] (Table 1).
The O102:H6 serotype was reported in Mozambique for the first time, possessing an FI:A1:B49 plasmid that co-harboured blaNDM-5, blaCTX-M-15, blaTEM-1, aadA2, sul1 and dfrA12 genes. Additionally, this strain had chromosomal mutations of gyrA, parC and parE, resulting in fluoroquinolone resistance. The WGS data of this strain are available in the EMBL-EBI database, project accession number: ERS4552076 [64] (Table 1).
Another Ambler class B beta-lactamase, namely blaNDM-4, was also identified on a mosaik IncFIA-type plasmid in three ST405 strains (GenBank accession numbers: NGUU00000000, NGUV00000000 and NGUW00000000) [65] (Table 1). These strains carried diverse resistance determinants, blaCTX-M-15, blaOXA-1, aac(6′)-Ib-cr, aac(3)-IIa, aadA5, strA, strB, tet(A), tet(B), sul1, sul2, and dfrA17. However, all of these ST405 strains were susceptible to colistin [64]. Further carbapenemases, such as OXA-48 and KPC-2, have also been reported in ST405 [40].
A study from Algeria reported mcr-1 in ST405 E. coli in environmental samples taken from eight agricultural sites in North West Algeria [122].
Interestingly, a study identified a novel mobile IS26-flanked transposon in the chromosome of the high-risk ST405 clone. Resistance genes were carried by a chromosomally integrated class 1 integron with dfrA17 and aadA5 gene cassettes. Its nucleotide seqeunce was deposited in GenBank under the accession number NXER00000000 [65] (Table 1). A study from Japan reported blaTEM−1A, blaOXA−1, blaCTX−M−14,15,24, aac(6′)-Ib-cr in E. coli ST405 [123].
Similar to ST405, CC/ST38 was also previously a neglected clone, but nowadays it belongs to the so-called ‘significant minority’ of ESBL-producer E. coli, accounting for approximately 12% of strains from UTI [37,38,69]. Compared to ST131, the phylogenetic background of ST38 is far less detailed. It has mainly been described, on the basis of various O:H serotypes, as a hybrid uropathogenic–enteroaggregative clone [68,124].
During one study, three multiresistant E. coli strains were detected from rectal samples taken in the course of screening from three patients in Paris, France. Two patients had stayed previously in Egypt, and the third patient had come from Turkey. All three E. coli isolates belonged to the ST38 clone, and showed resistance to penicillins, cefotaxime, sulfonamides, tobramycin, and gentamicin, but remained susceptible to amikacin, tetracycline and fluoroquinolones. They also demonstrated a reduced susceptibility to carbapenems based on the presence of blaOXA-48-harbouring plasmid. Co-carriage of blaCTX-M-2, a point mutant variant of CTX-M-14, and blaTEM-1 was reported in that strain. Furthermore, this study demonstrated that these strains were clonally related; the same clonal strain probably circulated in Turkey and Egypt, and was later introduced into France [125].
Further studies have reported blaCTX-M-3,-9,-14,-15, blaCMY-12, blaTEM-1B, blaNDM-1,6 and blaOXA-48 in E. coli ST38 [40,68,69,100,126,127,128]. Several outbreaks caused by E. coli ST38 carrying a blaOXA-244 (a point-mutation derivative of blaOXA-48) in Germany have also been reported [129].
On the other hand, blaCTX-M-14 and blaCTX-M-27 genes were also found in ST38, including in surveys from Germany, Switzerland and the USA [68,69,128]. Moreover, the blaCTX-M-27 gene was encoded by two distinct plasmid variants. In ST38, it was encoded in an IncF(F2:A-:B10) plasmid; by contrast, in ST131, it was located on IncF(F1:A2:B20) [68,69]. During this study in New York, USA the ST38 strains co-carried blaOXA-48, blaDHA-1 and blaCTX-M-14. The sequence information is available under BioProject accession numbers PRJNA692174 and PRJNA510429 [68] (Table 1). Moreover, MDR ST38 strains are often characterised as having a higher number of alterations in nitroreductase genes (nfsA and nfsB), resulting in nitrofurantoin resistance. The accession number for GenBank is RZEE00000000 [69] (Table 1). ST38 has also been detected as a colistin-resistant clone carrying mcr-5 in healthy chickens in a farm in Paraguay [130].
A study from Japan found that the blaNDM-1 gene was embedded between two IS903 elements as a gene cassette in an IncA/C-type plasmid. This transposon region was compared to plant pathogen bacteria, and homologous sequences were identified indicating that these microbes (e.g., Pseudoxanthomonas and Xanthomonas spp.) are potential sources of the blaNDM-1 gene [131]. In addition to the relationship between plant pathogens and ST38, this clone was also identified in Mongolian birds, but the acquired ESBLs (blaCTX-M-14 and blaCTX-M-15), independently of the antimicrobial selective pressure, were stably harboured by their chromosome instead of plasmids [132]. In addition, CC38 and CC10 were the predominant pandemic STs in food and among environmental E. coli strains in Brazil during a recent genomic surveillance analysis [112].
6. ST457, a Novel Emerging Clone from Phylogroup F
ST457 was first described in 2008 in the United Kingdom, and it was obtained in a clinical isolate from UTI. However, since then, the E. coli ST457 clone has emerged as a diverse E. coli clone present on all continents and from various samples, even in wild animals from Antarctica [19,133]. As evidence for further possible zoonotic and zooanthroponotic (reverse zoonotic) linkages, close similarities were found between Australian human clinical and silver gull strains among the H45 clade of ST457 [19]. These strains are characterised by carbapenemase production in patients with sepsis, namely blaKPC-2 (from Italy and Mexico), blaKPC-3 (from USA), blaNDM-5 (from Shanghai), and blaIMP-4 were also described in Australia, and interestingly, blaNDM-9 was detected in a poultry specimen. Surprisingly, chromosomally located blaOXA-23 was identified from Australian gull samples too [19,134,135,136,137]. Additionally, this lineage often carries further beta-lactam resistance genes, the most common of which is blaCMY-2 from AmpC β-lactamases. ESBLs were also detected in ST457, including blaCTX-M-1,-2,-3,-8,-12,-14,-15,-27,-55 [19].
Colistin resistance has been reported in the ST457 clone in many cases. This can be explained by the presence of plasmid-mediated mcr-1 from human clinical isolates in the USA, China, Vietnam, Mexico, and from wildlife and poultry in Asia [138,139,140,141]. Furthermore, an mcr-3 variant was also identified in ST457 from a single domestic duck in China [142]. In addition, located on transferable plasmids, mcr-5, blaCTX-M-8, blaTEM-1A, co-expression of aph(6)-Id aph-Ib, and sul2 were found among healthy chickens [19,70,130]. GenBank Accession numbers for high-risk international ST457 clones are available in Table 1.
7. Further Potential ExPEC High-Risk Clones
Several additional E. coli clones from various phylogenetic groups are also clinically relevant ExPEC clones, as they are responsible for an enormous burden of extraintestinal infections, including sepsis, UTI and neonatal infections across the globe. These addition-al clones are ST95, ST73, ST12, ST127 (from phylogroup B2), ST117, ST393, ST648 (from phylogroup F), and CC23/ST88 (from phylogroup C) [20,37,38,39,40,46,71,72,74,75,83,100,103,104,112,133,143,144] (Figure 1).
The current dissemination of ST58 and ST101 from phylogenetic group B1 is alarming, because previously, this group was reported to be a cluster of environmental bacteria. However, recently, these clones have been described as causative agents of invasive infections (e.g., bloodstream infections). Interestingly, these clones have not been reported to be carbapenemase producers or as being colistin resistant, yet [76,77]. Currently, there are only a small number of reports available about these clones that explain their emergence and dissemination [20,37,38,39,40,46,83,112,130,133,143,144,145]. The related genome-sequence information from published reports is summarised in Table 1.
8. Discussion
The emergence, expansion, and recent outbreaks of ExPEC high-risk international clones are of great concern worldwide [37,40,106]. MDR high-risk ExPEC is commonly detected in both nosocomial and community-acquired infections, and these infections are usually difficult to treat, because therapeutic options are limited [37,38,39]. The genome of E. coli has plasticity and high variability, and therefore various resistance and virulence genes can be taken up from different species of Enterobacterales and can be passed on to other species [19,95]. The development of these MDR strains depends significantly on the features of a given geographic area, such as trends of antibiotic consumption, resistance profile among currently circulating pathogens, travelling habits, medical tourism, and previous hospitalisation [64,121,125]. Furthermore, in countries such as Canada, the USA, Korea, Kuwait, Lebanon, France, Switzerland, Portugal, Spain, Germany, Bangladesh, China, and Japan, many lineages (e.g., ST131) circulate with quite similar resistance patterns [8] (Table 2).
Table 2.
Overview of the most common resistance genes against beta-lactams, fluoroquinolones and colistin among high-risk international ExPEC clones. The most frequently reported plasmid types are also summarised here.
| Resistance Markers of ExPEC High-Risk Clones | ||||||
|---|---|---|---|---|---|---|
| Sequence Type (ST) [References] |
Beta-Lactamases | Resistance to Fluoroquinolones | Resistance to Colistin | Inc Plasmid Types | ||
| ESBL | AmpC | Carbapenemases (Ambler Class A, B, D) |
||||
|
ST-131-A [46,54,55] |
blaCTX-M-14, blaCTX-M-15, blaCTX-M-27+, |
bla DHA-1 |
blaKPC-3, blaOXA-48 |
mutations in gyrA, parC, parE, double alteration of gyrA +, qnrB4, qnrB66, aac(6′)Ib-cr |
No data available | FI, FII, A1, B1, B10 |
|
ST-131-B (*) + [38,46,56,57] |
bla CTX-M-15 + | No data available |
qnrA1, * qnrB19+ |
mcr-1,(*) mcr-3,(*) mcr-5, * mcr-9* |
F-ColV like lineage, FIB-like, FII, HI2, HI2A |
|
|
ST-131-C1-M27 [20,46,83] |
blaCTX-M-27, blaCTX-M−2, blaTEM |
No data available |
blaNDM-1, blaOXA-232 |
No data available | FI:A2:B20 | |
|
ST-131-C1-non-M27 [58] |
blaCTX-M-14,
blaTEM |
No data available |
blaKPC-2, blaKPC-3, and blaKPC-18 |
No data available | ||
|
ST-131-C2 (*) [40,58] |
blaCTX-M-15, (*) blaCTX-M-G-1, blaCTX-M-G-2, blaCTX-M-G-8, blaCTX-M-G-9, blaCTX-M-G-25, blaTEM (*) blaSHV-12 |
blaFOX−5, |
blaNDM-1, blaNDM-5, blaVIM-1, blaKPC-2, blaKPC-3, blaKPC-18, blaOXA-48, blaOXA-181, blaOXA-232, co-expression of blaNDM-1 and blaVIM-1 |
qnrB19, (*) qnrS1, mutations in gyrA, parC, parE |
mutations in pmrA and pmrB, mcr-3 |
FII:A1:B-, F36:A4:B1 |
|
ST1193 [39,40,59,84,102] |
blaCTX-M-9, blaCTX-M-15, blaCTX-M-27, blaCTX-M-55, blaTEM-1B |
bla CMY-2 |
blaNDM-1, blaKPC-2 |
mutations in gyrA, parC or parE, aac(6′)Ib-cr |
mutations in pmrA and pmrB | FII, FIB, I1 |
|
ST69 (*) [20,40,60,100,105] |
blaCTX-M-1, blaCTX-M-14, blaCTX-M-15, blaCTX-M-27, blaTEM-1B, (*) blaTEM-1C |
blaCMY-6 (co-carriage with blaNDM-1) |
blaNDM-1, blaKPC-2 |
mutations in gyrA and parC (*) |
mcr-1,+
mcr-3+ |
FIIB |
|
CC10 (containing ST10, ST44, ST48, ST167 and ST617) (+) [7,61,62,112,113] |
blaCTX-M-14, blaCTX-M-15, blaCTX-M-27, blaCTX-M-55, blaTEM-1B, blaTEM-169, blaTEM-206, blaTEM-214 blaSHV-12 |
blaCMY-42, |
blaNDM-1, blaNDM-5, blaNDM-9, blaIMP-8, blaKPC-2, blaKPC-3, blaOXA-181, (co-expressed with blaNDM-5) blaOXA-48 (co-expressed with blaNDM-5) |
mutations in gyrA and parC, qnrS1, (*) qnrB19, qepA4, aac(6′)-Ib-cr |
mcr-1 (co-expressed with blaNDM-1) |
IncFIA, Col-like, I1 |
|
ST405 (+) [63,64,65,66] |
blaCTX-M-14, blaCTX-M-15, blaCTX-M-88, blaTEM-1, blaTEM-12 |
No data available |
blaNDM-4, blaNDM-5, blaKPC-2, blaOXA-48 |
mutations in gyrA, parC, and parE, qnrS1, aac(6′)-Ib-cr |
mcr-1+ | FIB, FII, F1A, Col-like, F1:A1:B49 |
|
ST38 (*) [38,40,67,68,69,70] |
blaCTX-M-2, blaCTX-M-3, blaCTX-M -9, blaCTX-M -14, (*) blaCTX-M-15, (*) blaCTX-M-27, blaTEM-1B |
blaCMY-12, blaDHA-1 |
blaNDM-1, blaNDM-6, blaOXA-48, blaOXA-244 |
mutations in gyrA, parC | mcr-5 (*) | FII:A-:B10, FI:A2:B20 |
|
ST457 (*) [19,70] |
blaCTX-M-1, blaCTX-M-2, blaCTX-M-3, blaCTX-M-8; blaCTX-M-12, blaCTX-M-14, blaCTX-M-15, blaCTX-M-27, blaCTX-M-55, blaTEM-1 |
bla CMY-2 |
blaNDM-5, blaNDM-9, blaIMP-4, blaKPC-2, blaKPC-3, blaOXA-23 |
mutations in gyrA and parC, qnrB19 * |
mcr-1 (*), mcr-3 (*), mcr-5 (*) |
F64:A:B:27, I1 |
* Clones or genes with zoonotic origin; + Clones or genes with environmental origin; (*) referenced resistance genes isolated from both human and zoonotic origin; (+) referenced resistance genes isolated from both human and environmental origin.
Globally, the predominant ExPEC clone is ST131, which is clustered into clades and subclades [15,37,39,45,46,47]. It possesses a wide variety of beta-lactamases, with the most frequent including ESBLs (blaCTX-M-14,15,27), AmpCs (blaFOX−5, blaDHA-1), MBLs, and carbapenemases (blaNDM-1,5; blaVIM-1, blaKPC-2,-3,-18; blaOXA-48,-181,-232). Carbapenem resistance through acquisition of blaNDM-1 or other variants, namely blaNDM-4,5,6,9, has been reported in all clones described in this review. Interestingly, blaOXA-48 and its variants (e.g., OXA-244) have also been disseminated with an increasing tendency in the last few years, as they were detected in CC10, ST405 and ST38 [40,129]. By contrast, blaIMP-8 was identified only among CC10 strains [20]. Additionally, a point mutation derivate of blaCTX-M-14, namely blaCTX-M-2, also appeared in the ST38 and ST457 strains [19,125]. All clones in this review article have a close to equal number of plasmid-mediated ESBLs and carbapenem-clefting enzymes, but they showed significantly lower capacity for AmpCs (Table 2).
Furthermore, in most cases, the observed high-risk clones also showed resistance to fluoroquinolones, based on chromosomal mutations in gyrA, parC, parE and/or expression of qnrA1, qnrB4, qnrB19, qnrB66, qnrS1 and aac(6′)Ib-cr [55,56,58,83,107,112]. In general, single alterations of GyrA and ParC/ParE resulted in a high level of fluoroquinolone resistance among the investigated clones, while low-level resistance occurred with the carriage of Qnr protective proteins (qnrB19, qnrS1) or aac(6′)Ib-cr enzymatic activity. However, double alterations of gyrA (S83L, D87N) and parC (S80I, E84V) in ST131, CC10, ST38, ST58 were also found. In addition, qepA4 efflux pump associated with double gyrA mutations and an amino acid-exchange of parC was identified in ST167 (CC10), as well. Interestingly, based on the available data, the rarely reported clones (e.g., ST393, ST3024, ST354) had a higher potential for genetic changes in gyrA and parC. As a typical feature, ST744 possessed double gyrA (S83L, D87N) and double parC (S80I, A56T) alterations [112].
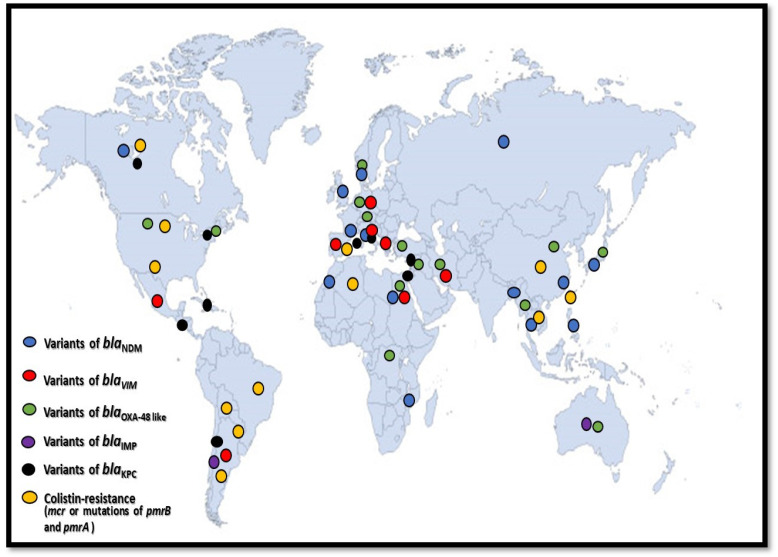
In this comparative analysis we investigated the properties of colistin resistance among these clones. This is an important issue, since polymyxins are considered to be the last resort of antibacterial agents against MDR E. coli [146]. Several clones harbour chromosomal pmrA and pmrB mutations and plasmid-mediated colistin resistance determinants (mcr-1,-3,-5,-9) [7,18,19,20,38,56,57,60,102,105,106,111,130,141,142]. In addition, apart from the most frequently detailed ExPEC clones (ST131, ST69, CC10, ST405, ST38, ST457, ST410, ST48, ST58, ST88), a huge number of currently less widely known strains carry mcr-genes, such as ST57, ST156, ST224, ST345, ST393, ST850, ST3024, ST8900, ST12657 (Table 3 and Table 4, Figure 2).
Table 3.
Distribution of colistin, fosfomycin and nitrofurantoin resistance determinants among high-risk international ExPEC clones from published reports. The most frequently reported clones are highlighted in red.
| Linkage between ExPEC Clones and Colistin, Fosfomycin, Nitrofurantoin Resistance Determinants | ||||||
|---|---|---|---|---|---|---|
| Colistin Resistance | Fosfomycin Resistance | Nitrofurantion Resistance | ||||
| pmrA and pmrB Mutations | mcr-1 | mcr-3 | mcr-5 | mcr-9 | fosA3 Enzymatic Activity | Nitroreductase (nfsA, nfsB) Enzymatic Activity |
|
ST131
ST1193 |
ST131
ST69 CC10 ST405 ST457 ST410 ST48 ST58 ST88 ST57 ST156 ST224 ST345 ST354 ST393 ST744 ST850 ST3024 ST8900 ST12657 |
ST69
ST457 ST101 ST155 ST206 ST443 ST1081 ST1638 ST5038 |
ST131-B
ST38 ST457 ST57 ST93 ST113 ST165 ST189 ST224 ST366 ST580 ST641 ST752 ST2705 ST6853 ST8061 |
ST131-B |
ST131
ST1193 ST69 CC10 ST38 ST457 ST95 ST12 ST117 ST307 ST648 ST744 ST746 ST1730 ST2646 |
ST131
ST38 |
Table 4.
Chronology of evolution of high-risk international E. coli clones. The table contains the year of isolation for each clone.
| Resistance Genes and Mechanisms | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Clones | blaCTX-M-14-Variants (e.g., CTX-M-2) | bla CTX-M-15 | bla CTX-M-27 | blaKPC-Variants | blaOXA-48-Variants (e.g., OXA-244) | blaIMP-Variants | blaNDM-Variants | blaVIM-Variants | Fluoro-Quinolones | Colistin |
| ST131 (including A, B, C1, C2 clades) | 2004 | 2005 | 2004 | 2011 | 2012 | 2010 | 2015-2017 (2022) 1 | 2004 | 2014 | |
| ST1193 | 2013 | 2017 | 2022 | 2022 | 2012 | 2021 | ||||
| ST69 | 2014–2017 (2020) 2 | 2014–2017 (2020) 2 | 2014–2017 (2020) 2 | 2015–2017 (2022) 1 | 2022 | 2017 | 2018 | |||
| CC10 (ST10 with its variants, namely ST167, ST617, ST410) | 2015 | 2015 | 2017 | 2016 | 2015 | 2022 | 2015 | 2017 | 2022 | |
| ST405 | 2012 | 2012 | 2016 | 2016 | 2013 (2020), 2016 3 | 2012 | 2020 | |||
| ST38 | 2011 | 2020 | 2020 | 2011 | 2011 | 2013 (2015) 4 |
2019 | |||
| ST457 | 2016 | 2016 | 2012 | 2014 | 2020 | 2019 | 2014 | 2008 | 2012 (2020) 5 | |
Legend: 1. Peirano et al. summarised carbapenemases including blaVIM for the period 2015–2017 [40]. 2. Birgy et al. summarised ESBLs for the period 2014–2017 [100]. 3. The strain was isolated in 2013, and further investigation was performed in 2020; the other strain that contained both of NDM-5 and OXA-48 was described in 2016. 4. The strain was isolated in 2013 (between December 2012 and January 2013), and further investigation was performed in 2015. 5. The strain was isolated in 2012, and further investigation was performed in 2020.
Figure 2.
Geographic dissemination of the most frequently reported carbapenemases and colistin resistance among the extraintestinal pathogenic high-risk international E. coli clones, http://www.intrafor.com/locations-worldwide-presence.html (accessed on 24 November 2022).
Furthermore, the majority of these genes are primarily associated with E. coli strains from zoonotic (e.g., poultry) and environmental sources (aquatic reservoir). Based on the ‘One Health’ approach, these strains may play a central role in human MDR infections in the future [106,112].
Fosfomycin is also mentioned as being among the last resort antibiotics that has retained antibacterial efficacy against MDR E. coli strains [10]. Of great concern, however, numerous fosfomycin-resistant E. coli clones have already been reported across the globe [106,112]. In the most common cases, resistance to fosfomycin is based on the enzymatic activity of fosA3. In addition, an ST131 clone was detected among patients of a hospital in China that carried mcr-3 and fosA3 together on an IncP plasmid [106]. Nitrofurantoin has also been considered to be an option for therapy in the case of UTI caused by MDR E. coli. However, resistance to nitrofurantoin has also been reported in ST131 and ST38 [44,69] (Table 3). Although in this study we focused on beta-lactams, fluoroquinolones and colistin, notably, almost all of the studied high-risk clones harboured a multicoloured collection of aminoglycoside-modifying enzymes, sumetrolim, tetracycline resistance genes [107].
Future actions that can be used to investigate and to analyse high-risk extraintestinal E. coli clones include surveillance on a genomic level, and the application of databases to detect new emerging clones and resistance determinants [147,148,149,150,151,152,153,154]. In terms of medical importance, novel antibiotics are needed to treat infections caused by multiresistant E. coli [21].
In conclusion, antibiotic resistance poses as an ongoing challenge worldwide and high-risk E. coli clones play a central role in the dissemination of resistance determinants. Taking the ‘One Health’ approach, high-risk E. coli clones circulate among different sources (human, animal, environmental); therefore, WGS analysis is a very useful approach [147,148] for tracking and understanding the changes in population dynamics, detecting resistance determinants and analysing the emergence of novel high-risk international clones.
Author Contributions
B.K.—writing, original draft preparation; D.G.—writing, review and editing, D.S.—supervision. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This study was supported by the European Union’s Horizon 2020 research and innovation program (952491-AmReSu). B.K. was supported by the János Bolyai Research Scholarship (BO/00286/22/5) of the Hungarian Academy of Sciences.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Pitout J.D.D. Extraintestinal pathogenic Escherichia coli: An update on antimicrobial resistance, laboratory diagnosis and treatment. Expert Rev. Anti-Infect. Ther. 2012;10:1165–1176. doi: 10.1586/eri.12.110. [DOI] [PubMed] [Google Scholar]
- 2.Gajdács M., Kárpáti K., Nagy Á.L., Gugolya M., Stájer A., Burián K. Association between biofilm-production and antibiotic resistance in Escherichia coli isolates: A laboratory-based case study and a literature review. Acta Microbiol. Immunol. Hung. 2021;68:217–226. doi: 10.1556/030.2021.01487. [DOI] [PubMed] [Google Scholar]
- 3.Livermore D.M. Has the era of untreatable infections arrived? J. Antimicrob. Chemother. 2009;64((Suppl. 1)):i29–i36. doi: 10.1093/jac/dkp255. [DOI] [PubMed] [Google Scholar]
- 4.Cassini A., Högberg L.D., Plachouras D., Quattrocchi A., Hoxha A., Simonsen G.S., Colomb-Cotinat M., Kretzschmar M.E., Devleesschauwer B., Cecchini M., et al. Attributable deaths and disability-adjusted life-years caused by infections with antibiotic-resistant bacteria in the EU and the European Economic Area in 2015: A population-level modelling analysis. Lancet Infect. Dis. 2019;19:56–66. doi: 10.1016/S1473-3099(18)30605-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cummins E.A., Snaith A.E., McNally A., Hall R.J. The role of potentiating mutations in the evolution of pandemic Escherichia coli clones. Eur. J. Clin. Microbiol. Infect. Dis. 2021:1–10. doi: 10.1007/s10096-021-04359-3. [DOI] [PubMed] [Google Scholar]
- 6.Mathers A.J., Peirano G., Pitout J.D.D. The role of epidemic resistance plasmids and international high-risk clones in the spread of multidrug-resistant Enterobacteriaceae. Clin. Microbiol. Rev. 2015;28:565–591. doi: 10.1128/CMR.00116-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Huang J., Zhu J., Gong D., Wu L., Zhu Y., Hu L. Whole genome sequence of EC16, a blaNDM-5-, blaCTX-M-55-, and fosA3-coproducing Escherichia coli ST167 clinical isolat from China. J. Glob. Antimicrob. Resist. 2022;29:296–298. doi: 10.1016/j.jgar.2022.04.001. [DOI] [PubMed] [Google Scholar]
- 8.Baquero F., Tedim A.-S.P., Coque T.M. Antibiotic resistance shaping multi-level population biology of bacteria. Front. Microbiol. 2013;4:15. doi: 10.3389/fmicb.2013.00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Doi Y. Treatment options for carbapenem-resistant gram-negative bacterial infections. Clin. Infect. Dis. 2019;69:S565–S575. doi: 10.1093/cid/ciz830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mazzariol A., Bazaj A., Cornaglia G. Multi-drug-resistant Gram-negative bacteria causing urinary tract infections: A review. J. Chemother. 2017;29:2–9. doi: 10.1080/1120009X.2017.1380395. [DOI] [PubMed] [Google Scholar]
- 11.Adekanmbi A.O., Usidamen S., Onilude A.A. Molecular characterization of ESBL- producing uropathogenic Escherichia coli recovered from urine samples of patients attending a University Teaching hospital in Nigeria. Acta Microbiol. Immunol. Hung. 2021;68:169–176. doi: 10.1556/030.2021.01380. [DOI] [PubMed] [Google Scholar]
- 12.Nordmann P., Poirel L. The difficult-to-control spread of carbapenemase producers among Enterobacteriaceae worldwide. Clin. Microbiol. Infect. 2014;20:821–830. doi: 10.1111/1469-0691.12719. [DOI] [PubMed] [Google Scholar]
- 13.Nordmann P., Poirel L. Epidemiology and diagnostics of carbapenem resistance in Gram-negative bacteria. Clin. Infect. Dis. 2019;69:S521–S528. doi: 10.1093/cid/ciz824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kumarasamy K.K., Toleman M.A., Walsh T.R., Bagaria J., Butt F., Balakrishnan R., Chaudhary U., Doumith M., Giske C.G., Irfan S., et al. Emergence of a new antibiotic resistance mechanism in India, Pakistan, and the UK: A molecular, biological, and epidemiological study. Lancet Infect. Dis. 2010;10:597–602. doi: 10.1016/S1473-3099(10)70143-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pitout J.D.D., DeVinney R. Escherichia coli ST131: A multidrug-resistant clone primed for global domination. F1000Research. 2017;6:1–7. doi: 10.12688/f1000research.10609.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Van der Bij A.K., Peirano G., Pitondo-Silva A., Pitout J.D. The presence of genes encoding for different virulence factors in clonally related Escherichia coli that produce CTX-Ms. Diagn. Microbiol. Infect. Dis. 2012;72:297–302. doi: 10.1016/j.diagmicrobio.2011.12.011. [DOI] [PubMed] [Google Scholar]
- 17.Johnston B.D., Thuras P., Porter S.B., Anacker M., VonBank B., Vagnone P.S., Witwer M., Castanheira M., Johnson J.R. Global molecular epidemiology of carbapenem-resistant Escherichia coli (2002–2017) Eur. J. Clin. Microbiol. 2021:1–13. doi: 10.1007/s10096-021-04310-6. [DOI] [PubMed] [Google Scholar]
- 18.Liu C.M., Stegger M., Aziz M., Johnson T.J., Waits K., Nordstrom L., Gauld L., Weaver B., Rolland D., Statham S., et al. Escherichia coli ST131-H22 as a foodborne uropathogen. mBio. 2018;9:e00470-18. doi: 10.1128/mBio.00470-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nesporova K., Wyrsch E.R., Valcek A., Bitar I., Chaw K., Harris P., Hrabak J., Literak I., Djordjevic S.P., Dolejska M. Escherichia coli Sequence Type 457 Is an Emerging Extended-Spectrum-β-Lactam-Resistant Lineage with Reservoirs in Wildlife and Food-Producing Animals. Antimicrob. Agents Chemother. 2020;65:e01118-20. doi: 10.1128/AAC.01118-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sanz M.B., De Belder D., de Mendieta J.M., Faccone D., Poklepovich T., Lucero C., Rapoport M., Campos J., Tuduri E., Saavedra M.O., et al. Carbapenemase-Producing Extraintestinal Pathogenic Escherichia coli From Argentina: Clonal Diversity and Predominance of Hyperepidemic Clones CC10 and CC131. Front. Microbiol. 2022;13:830209. doi: 10.3389/fmicb.2022.830209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tacconelli E., Carrara E., Savoldi A., Harbarth S., Mendelson M., Monnet D.L., Pulcini C., Kahlmeter G., Kluytmans J., Carmeli Y., et al. Discovery, research, and development of new antibiotics: The WHO priority list of antibiotic-resistant bacteria and tuberculosis. Lancet Infect. Dis. 2018;18:318–327. doi: 10.1016/S1473-3099(17)30753-3. [DOI] [PubMed] [Google Scholar]
- 22.Butler M.S., Paterson D.L. Antibiotics in the clinical pipeline in October 2019. J. Antibiot. 2020;73:329–364. doi: 10.1038/s41429-020-0291-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yahav D., Giske C.G., Grāmatniece A., Abodakpi H., Tam V.H., Leibovici L. New β-Lactam-β-Lactamase Inhibitor Combinations. Clin. Microbiol. Rev. 2020;34:e00115-20. doi: 10.1128/CMR.00115-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kocsis B., Gulyás D., Szabó D. Delafloxacin, Finafloxacin, and Zabofloxacin: Novel Fluoroquinolones in the Antibiotic Pipeline. Antibiotics. 2021;10:1506. doi: 10.3390/antibiotics10121506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Scudeller L., Righi E., Chiamenti M., Bragantini D., Menchinelli G., Cattaneo P., Giske C.G., Lodise T., Sanguinetti M., Piddock L.J.V., et al. Systematic review and meta-analysis of in vitro efficacy of antibiotic combination therapy against carbapenem-resistant Gram-negative bacilli. Int. J. Antimicrob. Agents. 2021;57:106344. doi: 10.1016/j.ijantimicag.2021.106344. [DOI] [PubMed] [Google Scholar]
- 26.Carrara E., Savoldi A., Piddock L.J., Franceschi F., Ellis S., Sharland M., Brink A.J., Harris P.N., Levy-Hara G., Rohit A., et al. Clinical management of severe infections caused by carbapenem-resistant gram-negative bacteria: A worldwide cross-sectional survey addressing the use of antibiotic combinations. Clin. Microbiol. Infect. 2022;28:66–72. doi: 10.1016/j.cmi.2021.05.002. [DOI] [PubMed] [Google Scholar]
- 27.Roer L., Overballe-Petersen S., Hansen F., Johannesen T.B., Stegger M., Bortolaia V., Leekitcharoenphon P., Korsgaard H.B., Seyfarth A.M., Mossong J., et al. ST131 fimH22 Escherichia coli isolate with a blaCMY-2/IncI1/ST12 plasmid obtained from a patient with bloodstream infection: Highly similar to E. coli isolates of broiler origin. J. Antimicrob. Chemother. 2019;74:557–560. doi: 10.1093/jac/dky484. [DOI] [PubMed] [Google Scholar]
- 28.Léger A., Lambraki I., Graells T., Cousins M., Henriksson P.J.G., Harbarth S., Carson C.A., Majowicz S.E., Troell M., Parmley E.J., et al. Characterizing social-ecological context and success factors of antimicrobial resistance interventions across the One Health spectrum: Analysis of 42 interventions targeting E. coli. BMC Infect. Dis. 2021;21:873. doi: 10.1186/s12879-021-06483-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Price L.B., Johnson J.R., Aziz M. The epidemic of extended spectrum- β -lactamase-producing Escherichia coli ST131 is driven by a single highly pathogenic subclone. H 30-Rx. mBio. 2013;4:e00377-13. doi: 10.1128/mBio.00377-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Füzi M. Dissimilar fitness associated with resistance to fluoroquinolones influences clonal dynamics of various multiresistant bacteria. Front. Microbiol. 2016;7:1071. doi: 10.3389/fmicb.2016.01017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Johansson V., Nykäsenoja S., Myllyniemi A.L., Rossow H., Heikinheimo A. Genomic characterization of ESBL/AmpC-producing and high-risk clonal lineages of Escherichia coli and Klebsiella pneumoniae in imported dogs with shelter and stray background. J. Glob. Antimicrob. Resist. 2022;30:183–190. doi: 10.1016/j.jgar.2022.05.021. [DOI] [PubMed] [Google Scholar]
- 32.Gladstone R.A., McNally A., Pöntinen A.K., Tonkin-Hill G., Lees J.A., Skytén K., Cléon F., Christensen M.O.K., Haldorsen B.C., Bye K.K., et al. Emergence and dissemination of antimicrobial resistance in Escherichia coli causing bloodstream infections in Norway in 2002-17: A nationwide, longitudinal, microbial population genomic study. Lancet Microbe. 2021;2:e331–e341. doi: 10.1016/S2666-5247(21)00031-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chaudhuri R.R., Henderson I.R. The evolution of the Escherichia coli phylogeny. Infect. Genet. Evol. 2012;12:214–226. doi: 10.1016/j.meegid.2012.01.005. [DOI] [PubMed] [Google Scholar]
- 34.Clermont O., Bonacorsi S., Bingen E. Rapid and simple determination of the Escherichia coli phylogenetic group. Appl. Environ. Microbiol. 2000;66:4555–4558. doi: 10.1128/AEM.66.10.4555-4558.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Walk S.T., Alm E.W., Gordon D.M., Ram J.L., Toranzos G.A., Tiedje J.M., Whittam T.S. Cryptic lineages of the genus Escherichia. Appl. Environ. Microbiol. 2009;75:6534–6544. doi: 10.1128/AEM.01262-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Beghain J., Bridier-Nahmias A., Le Nagard H., Denamur E., Clermont O. ClermonTyping: An easy-to-use and accurate in silico method for Escherichia genus strain phylotyping. Microb. Genom. 2018;4:e000192. doi: 10.1099/mgen.0.000192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Manges A.R., Geum H.M., Guo A., Edens T.J., Fibke C.D., Pitout J.D.D. Global Extraintestinal Pathogenic Escherichia coli (ExPEC) Lineages. Clin. Microbiol. Rev. 2019;32:e00135-18. doi: 10.1128/CMR.00135-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shaik S., Ranjan A., Tiwari S.K., Hussain A., Nandanwar N., Kumar N., Jadhav S., Semmler T., Baddam R., Islam M.A., et al. Comparative genomic analysis of globally dominant ST131 clone with other epidemiologically successful extraintestinal pathogenic Escherichia coli (ExPEC) lineages. mBio. 2017;8:e01596-17. doi: 10.1128/mBio.01596-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mazumder R., Hussain A., Abdullah A., Islam M.N., Sadique M.T., Muniruzzaman S.M., Tabassum A., Halim F., Akter N., Ahmed D., et al. International High-Risk Clones Among Extended-Spectrum β-Lactamase-Producing Escherichia coli in Dhaka, Bangladesh. Front. Microbiol. 2021;12:736464. doi: 10.3389/fmicb.2021.736464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Peirano G., Chen L., Nobrega D., Finn T.J., Kreiswirth B.N., DeVinney R., Pitout J.D.D. Genomic Epidemiology of Global Carbapenemase-Producing Escherichia coli, 2015–2017. Emerg. Infect. Dis. 2022;28:924–931. doi: 10.3201/eid2805.212535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Riley L.W. Distinguishing Pathovars from Nonpathovars: Escherichia coli. Microbiol. Spectr. 2020;8:AME-0014-2020. doi: 10.1128/microbiolspec.AME-0014-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lindblom A., Kiszakiewicz C., Kristiansson E., Yazdanshenas S., Kamenska N., Karami N., Åhrén C. The impact of the ST131 clone on recurrent ESBL-producing E. coli urinary tract infection: A prospective comparative study. Sci. Rep. 2022;12:10048. doi: 10.1038/s41598-022-14177-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nicolas-Chanoine M.H., Blanco J., Leflon-Guibout V., Demarty R., Alonso M.P., Caniça M.M., Park Y.J., Lavigne J.P., Pitout J., Johnson J.R. Intercontinental emergence of Escherichia coli clone O25:H4-ST131 producing CTX-M-15. J. Antimicrob. Chemother. 2008;61:273–281. doi: 10.1093/jac/dkm464. [DOI] [PubMed] [Google Scholar]
- 44.Coque T.M., Novais A., Carattoli A., Poirel L., Pitout J., Peixe L., Baquero F., Cantón R., Nordmann P. Dissemination of clonally related Escherichia coli strains expressing extended-spectrum beta-lactamase CTX-M-15. Emerg. Infect. Dis. 2008;14:195–200. doi: 10.3201/eid1402.070350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Banerjee R., Johnson J.R. A new clone sweeps clean: The enigmatic emergence of Escherichia coli sequence type 131. Antimicrob. Agents Chemother. 2014;58:4997–5004. doi: 10.1128/AAC.02824-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Liu X., Li X., Yang A.W., Tang B., Jian Z.J., Zhong Y.M., Li H.L., Li Y.M., Yan Q., Liang X.H., et al. Community Fecal Carriage and Molecular Epidemiology of Extended-Spectrum β-Lactamase- and Carbapenemase-Producing Escherichia coli from Healthy Children in the Central South China. Infect. Drug Resist. 2022;15:1601–1611. doi: 10.2147/IDR.S357090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bueris V., Sellera F.P., Fuga B., Sano E., Carvalho M.P.N., Couto S.C.F., Moura Q., Lincopan N. Convergence of virulence and resistance in international clones of WHO critical priority enterobacterales isolated from Marine Bivalves. Sci. Rep. 2022;12:5707. doi: 10.1038/s41598-022-09598-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Le Gall T., Clermont O., Gouriou S., Picard B., Nassif X., Denamur E., Tenaillon O. Extraintestinal virulence is a coincidental by-product of commensalism in B2 phylogenetic group Escherichia coli strains. Mol. Biol. Evol. 2007;24:2373–2384. doi: 10.1093/molbev/msm172. [DOI] [PubMed] [Google Scholar]
- 49.Clermont O., Dhanji H., Upton M., Gibreel T., Fox A., Boyd D., Mulvey M.R., Nordmann P., Ruppe E., Sarthou J.L., et al. Rapid detection of the O25b-ST131 clone of Escherichia coli encompassing the CTX-M-15-producing strains. J. Antimicrob. Chemother. 2009;64:274–277. doi: 10.1093/jac/dkp194. [DOI] [PubMed] [Google Scholar]
- 50.Croxall G., Hale J., Weston V., Manning G., Cheetham P., Achtman M., McNally A. Molecular epidemiology of extraintestinal pathogenic Escherichia coli isolates from a regional cohort of elderly patients highlights the prevalence of ST131 strains with increased antimicrobial resistance in both community and hospital care settings. J. Antimicrob. Chemother. 2011;66:2501–2508. doi: 10.1093/jac/dkr349. [DOI] [PubMed] [Google Scholar]
- 51.Russo T.A., Johnson J.R. Proposal for a new inclusive designation for extraintestinal pathogenic isolates of Escherichia coli: ExPEC. J. Infect. Dis. 2000;181:1753–1754. doi: 10.1086/315418. [DOI] [PubMed] [Google Scholar]
- 52.Nicolas-Chanoine M.H., Bertrand X., Madec J.Y. Escherichia coli ST131, an intriguing clonal group. Clin. Microbiol. Rev. 2014;27:543–574. doi: 10.1128/CMR.00125-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ben Zakour N.L., Alsheikh-Hussain A.S., Ashcroft M.M., Khanh Nhu N.T., Roberts L.W., Stanton-Cook M., Schembri M.A., Beatson S.A. Sequential Acquisition of Virulence and Fluoroquinolone Resistance Has Shaped the Evolution of Escherichia coli ST131. mBio. 2016;7:e00347-16. doi: 10.1128/mBio.00347-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Harris P.N.A., Ben Zakour N.L., Roberts L.W., Wailan A.M., Zowawi H.M., Tambyah P.A., Lye D., Jureen R., Lee T.H., Yin M., et al. Whole genome analysis of cephalosporin-resistant Escherichia coli from bloodstream infections in Australia, New Zealand and Singapore: High prevalence of CMY-2 producers and ST131 carrying blaCTX-M-15 and blaCTX-M-27. J. Antimicrob. Chemother. 2018;73:634–642. doi: 10.1093/jac/dkx466. [DOI] [PubMed] [Google Scholar]
- 55.Zhong Y., Guo S., Seow K.L.G., Ming G.O.H., Schlundt J. Characterization of extended-spectrum beta-lactamase-producing Escherichia coli isolates from Jurong Lake, Singapore, with whole-genome sequencing. Int. J. Environ. Res. Public Health. 2021;18:937. doi: 10.3390/ijerph18030937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lopes R., Furlan J.P.R., Dos Santos L.D.R., Gallo I.F.L., Stehling E.G. Colistin-Resistant mcr-1-Positive Escherichia coli ST131-H22 Carrying blaCTX-M-15 and qnrB19 in Agricultural Soil. Front. Microbiol. 2021;12:659900. doi: 10.3389/fmicb.2021.659900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Saidenberg A.B.S., Stegger M., Price L.B., Johannesen T.B., Aziz M., Cunha M.P.V., Moreno A.M., Knöbl T. mcr-Positive Escherichia coli ST131-H22 from Poultry in Brazil. Emerg. Infect. Dis. 2020;26:1951–1954. doi: 10.3201/eid2608.191724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Pajand O., Rahimi H., Darabi N., Roudi S., Ghassemi K., Aarestrup F.M., Leekitcharoenphon P. Arrangements of Mobile Genetic Elements among Virotype E Subpopulation of Escherichia coli Sequence Type 131 Strains with High Antimicrobial Resistance and Virulence Gene Content. mSphere. 2021;6:e0055021. doi: 10.1128/mSphere.00550-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Nielsen D.W., Ricker N., Barbieri N.L., Wynn J.L., Gomez-Duarte O.G., Iqbal J., Nolan L.K., Allen H.K., Logue C.M. Complete genome sequence of the multidrug-resistant neonatal meningitis Escherichia coli serotype O75:H5:K1 strain mcjchv-1 (NMEC-O75) Microbiol. Resour. Announc. 2018;7:e01043-18. doi: 10.1128/MRA.01043-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Massella E., Giacometti F., Bonilauri P., Reid C., Djordjevic S., Merialdi G., Bacci C., Fiorentini L., Massi P., Bardasi L., et al. Antimicrobial Resistance Profile and ExPEC Virulence Potential in Commensal Escherichia coli of Multiple Sources. Antibiotics. 2021;10:351. doi: 10.3390/antibiotics10040351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Monte D.F., Sellera F.P., Fernandes M.R., Moura Q., Landgraf M., Lincopan N. Genome Sequencing of an Escherichia coli Sequence Type 617 Strain Isolated from Beach Ghost Shrimp (Callichirus major) from a Heavily Polluted Ecosystem Reveals a Wider Resistome against Heavy Metals and Antibiotics. Microbiol. Resour. Announc. 2019;8:e01471-18. doi: 10.1128/MRA.01471-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sun L., Xu J., He F. Draft genome sequence of an NDM-5, CTX-M-15 and OXA-1 co-producing Escherichia coli ST167 clinical strain isolated from a urine sample. J. Glob. Antimicrob. Resist. 2018;14:284–286. doi: 10.1016/j.jgar.2018.08.005. [DOI] [PubMed] [Google Scholar]
- 63.Takayama Y., Sekizuka T., Matsui H., Adachi Y., Eda R., Nihonyanagi S., Wada T., Matsui M., Suzuki S., Takaso M., et al. Characterization of the IncFII-IncFIB(pB171) Plasmid Carrying blaNDM-5 in Escherichia coli ST405 Clinical Isolate in Japan. Infect. Drug Resist. 2020;13:561–566. doi: 10.2147/IDR.S232943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Sumbana J.J., Santona A., Fiamma M., Taviani E., Deligios M., Zimba T., Lucas G., Sacarlal J., Rubino S., Paglietti B. Extraintestinal Pathogenic Escherichia coli ST405 Isolate Coharboring blaNDM-5 and blaCTXM-15: A New Threat in Mozambique. Microb. Drug Resist. 2021;27:1633–1640. doi: 10.1089/mdr.2020.0334. [DOI] [PubMed] [Google Scholar]
- 65.Zhang X., Feng Y., Zhou W., McNally A., Zong Z. Cryptic transmission of ST405 Escherichia coli carrying blaNDM-4 in hospital. Sci. Rep. 2018;8:390. doi: 10.1038/s41598-017-18910-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Chowdhury P.R., McKinnon J., Liu M., Djordjevic S.P. Multidrug Resistant Uropathogenic Escherichia coli ST405 With a Novel, Composite IS26 Transposon in a Unique Chromosomal Location. Front. Microbiol. 2019;9:3212. doi: 10.3389/fmicb.2018.03212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Fernandes M.R., Sellera F.P., Cunha M.P.V., Lopes R., Cerdeira L., Lincopan N. Emergence of CTX-M-27-producing Escherichia coli of ST131 and clade C1-M27 in an impacted ecosystem with international maritime traffic in South America. J. Antimicrob. Chemother. 2020;75:1647–1649. doi: 10.1093/jac/dkaa069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Cameron A., Mangat R., Mostafa H.H., Taffner S., Wang J., Dumyati G., Stanton R.A., Daniels J.B., Campbell D., Lutgring J.D., et al. Detection of CTX-M-27 β-Lactamase Genes on Two Distinct Plasmid Types in ST38 Escherichia coli from Three, U.S. States. Antimicrob. Agents Chemother. 2021;65:e0082521. doi: 10.1128/AAC.00825-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Mostafa H.H., Cameron A., Taffner S.M., Wang J., Malek A., Dumyati G., Hardy D.J., Pecora N.D. Genomic Surveillance of Ceftriaxone-Resistant Escherichia coli in Western New York Suggests the Extended-Spectrum β-Lactamase blaCTX-M-27 Is Emerging on Distinct Plasmids in ST38. Front. Microbiol. 2020;11:1747. doi: 10.3389/fmicb.2020.01747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Sellera F.P., Fernandes M.R., Moura Q., Lopes R.B., Souza T.A., Cerdeira L., Lincopan N. Draft genome sequence of a blaCMY-2/IncI1-harbouring Escherichia coli D:ST457 isolated from coastal benthic organisms. J. Glob. Antimicrob. Resist. 2018;14:83–84. doi: 10.1016/j.jgar.2018.06.010. [DOI] [PubMed] [Google Scholar]
- 71.Sartori L., Fernandes M.R., Ienne S., de Souza T.A., Gregory L., Cerdeira L., Lincopan N. Draft genome sequences of two fluoroquinolone-resistant CTX-M-15-producing Escherichia coli ST90 (ST23 complex) isolated from a calf and a dairy cow in South America. J. Glob. Antimicrob. Resist. 2017;11:145–147. doi: 10.1016/j.jgar.2017.10.009. [DOI] [PubMed] [Google Scholar]
- 72.Stephens C.M., Skerker J.M., Sekhon M.S., Arkin A.P., Riley L.W. Complete genome sequences of four Escherichia coli ST95 isolates from bloodstream infections. Genome Announc. 2015;3:e01241-15. doi: 10.1128/genomeA.01241-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Furlan J.P.R., Gonzalez I.H.L., Ramos P.L., Stehling E.G. International high-risk clone of multidrug-resistant CTX-M-8-producing Escherichia coli C-ST410 infecting an elephant (Loxodonta africana) in a zoo. J. Glob. Antimicrob. Resist. 2020;22:643–645. doi: 10.1016/j.jgar.2020.06.018. [DOI] [PubMed] [Google Scholar]
- 74.Fernandes M.R., Sellera F.P., Moura Q., Gaspar V.C., Cerdeira L., Lincopan N. International high-risk clonal lineages of CTX-M-producing Escherichia coli F-ST648 in free-roaming cats, South America. Infect. Genet. Evol. 2018;66:48–51. doi: 10.1016/j.meegid.2018.09.009. [DOI] [PubMed] [Google Scholar]
- 75.Oliveira F.A., Zaccariotto T.R., Piveta C., Hofling C.C., Resende M.R., Levy C.E., Esposito F., Fernandes M.R., Cerdeira L., Lincopan N. MCR-1-positive colistin-resistant Escherichia coli in immunocompromised hospitalised patients. Int. J. Antimicrob. Agents. 2018;52:438–440. doi: 10.1016/j.ijantimicag.2018.06.011. [DOI] [PubMed] [Google Scholar]
- 76.Reid C.J., Cummins M.L., Börjesson S., Brouwer M.S.M., Hasman H., Hammerum A.M., Roer L., Hess S., Berendonk T., Nešporová K., et al. A role for ColV plasmids in the evolution of pathogenic Escherichia coli ST58. Nat. Commun. 2022;13:683. doi: 10.1038/s41467-022-28342-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Santos A.C.M., Silva R.M., Valiatti T.B., Santos F.F., Santos-Neto J.F., Cayô R., Streling A.P., Nodari C.S., Gales A.C., Nishiyama-Jr M.Y., et al. Virulence Potential of a Multidrug-Resistant Escherichia coli Strain Belonging to the Emerging Clonal Group ST101-B1 Isolated from Bloodstream Infection. Microorganisms. 2020;8:827. doi: 10.3390/microorganisms8060827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Carattoli A. Resistance plasmid families in Enterobacteriaceae. Antimicrob. Agents Chemother. 2009;53:2227–2238. doi: 10.1128/AAC.01707-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Johnson T.J., Danzeisen J.L., Youmans B., Case K., Llop K., Munoz-Aguayo J., Flores-Figueroa C., Aziz M., Stoesser N., Sokurenko E., et al. Separate F-Type Plasmids Have Shaped the Evolution of the H30 Subclone of Escherichia coli Sequence Type 131. mSphere. 2016;1:e00121-16. doi: 10.1128/mSphere.00121-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Matsumura Y., Pitout J.D., Gomi R., Matsuda T., Noguchi T., Yamamoto M., Peirano G., DeVinney R., Bradford P.A., Motyl M.R., et al. Global Escherichia coli sequence type 131 clade with blaCTX-M-27 gene. Emerg. Infect. Dis. 2016;22:1900–1907. doi: 10.3201/eid2211.160519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Merino I., Hernández-García M., Turrientes M.C., Pérez-Viso B., López-Fresneña N., Diaz-Agero C., Maechler F., Fankhauser-Rodriguez C., Kola A., Schrenzel J., et al. Emergence of ESBL-producing Escherichia coli ST131-C1-M27 clade colonizing patients in Europe. J. Antimicrob. Chemother. 2018;73:2973–2980. doi: 10.1093/jac/dky296. [DOI] [PubMed] [Google Scholar]
- 82.Peirano G., Lynch T., Matsumara Y., Nobrega D., Finn T.J., DeVinney R., Pitout J.D. Trends in population dynamics of Escherichia coli sequence type 131, Calgary, Alberta, Canada, 2006–2016. Emerg. Infect. Dis. 2020;26:2907–2915. doi: 10.3201/eid2612.201221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Hojabri Z., Darabi N., Arab M., Saffari F., Pajand O. Clonal diversity, virulence genes content and subclone status of Escherichia coli sequence type 131: Comparative analysis of E. coli ST131 and non-ST131 isolates from Iran. BMC Microbiol. 2019;19:117. doi: 10.1186/s12866-019-1493-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Tóth K., Tóth Á., Kamotsay K., Németh V., Szabó D. Population snapshot of the extended-spectrum β-lactamase-producing Escherichia coli invasive strains isolated from a Hungarian hospital. Ann. Clin. Microbiol. Antimicrob. 2022;21:3. doi: 10.1186/s12941-022-00493-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Chen L., Chavda K.D., Al Laham N., Melano R.G., Jacobs M.R., Bonomo R.A., Kreiswirth B.N. Complete nucleotide sequence of a blaKPC-harboring IncI2 plasmid and its dissemination in New Jersey and New York hospitals. Antimicrob. Agents Chemother. 2013;57:5019–5025. doi: 10.1128/AAC.01397-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Chen L., Chavda K.D., Melano R.G., Hong T., Rojtman A.D., Jacobs M.R., Bonomo R.A., Kreiswirth B.N. Molecular survey of the dissemination of two blaKPC-harboring IncFIA plasmids in New Jersey and New York hospitals. Antimicrob. Agents Chemother. 2014;58:2289–2294. doi: 10.1128/AAC.02749-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Strydom K.A., Chen L., Kock M., Stoltz A.C., Peirano G., Nobrega D.B., Lowe M., Ehlers M.M., Mbelle N.M., Kreiswirth B.N., et al. Klebsiella pneumoniae ST307 with OXA-181: Threat of a high-risk clone and promiscuous plasmid in a resource-constrained healthcare setting. J. Antimicrob. Chemother. 2020;75:896–902. doi: 10.1093/jac/dkz550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Johnson J.R., Clermont O., Johnston B., Clabots C., Tchesnokova V., Sokurenko E., Junka A.F., Maczynska B., Denamur E. Rapid and specific detection, molecular epidemiology, and experimental virulence of the O16 subgroup within Escherichia coli sequence type 131. J. Clin. Microbiol. 2014;52:1358–1365. doi: 10.1128/JCM.03502-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Zhang S., Zhang Q., Huang J., Cao Y., Zhao Z., Li B. Epidemic potential of Escherichia coli O16: H41-ST131:compared with pandemic O25b: H30-ST131 Lineage. Infect. Drug Resist. 2021;14:2625–2632. doi: 10.2147/IDR.S313261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Petty N.K., Ben Zakour N.L., Stanton-Cook M., Skippington E., Totsika M., Forde B.M., Phan M.D., Gomes Moriel D., Peters K.M., Davies M., et al. Global dissemination of a multidrug-resistant Escherichia coli clone. Proc. Natl. Acad. Sci. USA. 2014;111:5694–5699. doi: 10.1073/pnas.1322678111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Chen S.L., Ding Y., Apisarnthanarak A., Kalimuddin S., Archuleta S., Omar S.F.S., De P.P., Koh T.H., Chew K.L., Atiya N., et al. The higher prevalence of extended spectrum beta-lactamases among Escherichia coli ST131 in Southeast Asia is driven by expansion of a single, locally prevalent subclone. Sci. Rep. 2019;9:13245. doi: 10.1038/s41598-019-49467-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Moulin-Schouleur M., Répérant M., Laurent S., Brée A., Mignon-Grasteau S., Germon P. Extraintestinal pathogenic Escherichia coli strains of avian and human origin: Link between phylogenetic relationships and common virulence patterns. J. Clin. Microbiol. 2007;45:3366–7336. doi: 10.1128/JCM.00037-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Mora A., Herrera A., Mamani R., López C., Alonso M.P., Blanco J.E., Blanco M., Dahbi G., García-Garrote F., Pita J.M., et al. Recent emergence of clonal group O25b:K1:H4-B2-ST131 ibeA strains among Escherichia coli poultry isolates, including CTX-M-9-producing strains, and comparison with clinical human isolates. Appl. Environ. Microbiol. 2010;76:6991–6997. doi: 10.1128/AEM.01112-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Vincent C., Boerlin P., Daignault D., Dozois C.M., Dutil L., Galanakis C., Reid-Smith R.J., Tellier P.-P., Tellis P.A., Ziebell K., et al. Food reservoir for Escherichia coli causing urinary tract infections. Emerg. Infect. Dis. 2010;16:88–95. doi: 10.3201/eid1601.091118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Heiden S.E., Kurz M.S.E., Bohnert J., Bayingana C., Ndoli J.M., Sendegeya A., Gahutu J.B., Eger E., Mockenhaupt F.P., Schaufler K. Flies from a tertiary hospital in Rwanda carry multidrug-resistant Gram-negative pathogens including extended-spectrum beta-lactamase-producing E. coli sequence type 131. Antimicrob. Resist. Infect. Control. 2020;9:34. doi: 10.1186/s13756-020-0696-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Eger E., Heiden S.E., Korolew K., Bayingana C., Ndoli J.M., Sendegeya A., Gahutu J.B., Kurz M.S.E., Mockenhaupt F.P., Müller J., et al. Circulation of Extended-Spectrum Beta-Lactamase-Producing Escherichia coli of Pandemic Sequence Types 131, 648, and 410 Among Hospitalized Patients, Caregivers, and the Community in Rwanda. Front. Microbiol. 2021;12:662575. doi: 10.3389/fmicb.2021.662575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Johnson T.J., Elnekave E., Miller E.A., Munoz-Aguayo J., Figueroa C.F., Johnston B., Nielson D.W., Logue C.M., Johnson J.R. Phylogenomic analysis of extraintestinal pathogenic Escherichia coli sequence type 1193, an emerging multidrug-resistant clonal group. Antimicrob. Agents Chemother. 2018;63:e01913-18. doi: 10.1128/AAC.01913-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Peirano G., Matsumara Y., Nobrega D., DeVinney R., Pitout J. Population-based epidemiology of Escherichia coli ST1193 causing blood stream infections in a centralized Canadian region. Eur. J. Clin. Microbiol. Infect. Dis. 2021:1–7. doi: 10.1007/s10096-021-04373-5. [DOI] [PubMed] [Google Scholar]
- 99.Pitout J.D.D., Peirano G., Chen L., DeVinney R., Matsumura Y. Escherichia coli ST1193: Following in the Footsteps of E. coli ST131. Antimicrob. Agents Chemother. 2022;66:e0051122. doi: 10.1128/aac.00511-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Birgy A., Madhi F., Jung C., Levy C., Cointe A., Bidet P., Hobson C.A., Bechet S., Sobral E., Vuthien H., et al. Diversity and trends in population structure of ESBL-producing Enterobacteriaceae in febrile urinary tract infections in children in France from 2014 to 2017. J. Antimicrob. Chemother. 2020;75:96–105. doi: 10.1093/jac/dkz423. [DOI] [PubMed] [Google Scholar]
- 101.Ding Y., Zhang J., Yao K., Gao W., Wang Y. Molecular characteristics of the new emerging global clone ST1193 among clinical isolates of Escherichia coli from neonatal invasive infections in China. Eur. J. Clin. Microbiol. Infect. Dis. 2021;40:833–840. doi: 10.1007/s10096-020-04079-0. [DOI] [PubMed] [Google Scholar]
- 102.Wang C.H., Siu L.K., Chang F.Y., Chiu S.K., Lin J.C. A Resistance Mechanism in Non-mcr Colistin-Resistant Escherichia coli in Taiwan: R81H Substitution in PmrA Is an Independent Factor Contributing to Colistin Resistance. Microbiol. Spectr. 2021;9:e0002221. doi: 10.1128/Spectrum.00022-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Riley L.W. Pandemic lineages of extraintestinal pathogenic Escherichia coli. Clin. Microbiol. Infect. 2014;20:380–390. doi: 10.1111/1469-0691.12646. [DOI] [PubMed] [Google Scholar]
- 104.Kallonen T., Brodrick H.J., Harris S.R., Corander J., Brown N.M., Martin V., Peacock S.J., Parkhill J. Systematic longitudinal survey of invasive Escherichia coli in England demonstrates a stable population structure only transiently disturbed by the emergence of ST131. Genome Res. 2017;27:1437–1449. doi: 10.1101/gr.216606.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Yamaguchi T., Kawahara R., Harada K., Teruya S., Nakayama T., Motooka D., Nakamura S., Nguyen P.D., Kumeda Y., Van-Dang C. The presence of colistin resistance gene mcr-1 and -3 in ESBL producing Escherichia coli isolated from food in Ho Chi Minh City Vietnam. FEMS Microbiol. Lett. 2018;365:fny100. doi: 10.1093/femsle/fny100. [DOI] [PubMed] [Google Scholar]
- 106.Hameed M.F., Chen Y., Bilal H., Khan S., Ge H., Xiaofang C., Gu P. The Co-occurrence of mcr-3 and fosA3 in IncP plasmid in ST131 Escherichia coli: A novel case. J. Infect. Dev. Ctries. 2022;16:622–629. doi: 10.3855/jidc.15943. [DOI] [PubMed] [Google Scholar]
- 107.Nüesch-Inderbinen M.T., Baschera M., Zurfluh K., Hächler H., Nüesch H., Stephan R. Clonal Diversity, Virulence Potential and Antimicrobial Resistance of Escherichia coli Causing Community Acquired Urinary Tract Infection in Switzerland. Front. Microbiol. 2017;8:2334. doi: 10.3389/fmicb.2017.02334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Massella E., Reid C.J., Cummins M.L., Anantanawat K., Zingali T., Serraino A., Piva S., Giacometti F., Djordjevic S.P. Snapshot Study of Whole Genome Sequences of Escherichia coli from Healthy Companion Animals, Livestock, Wildlife, Humans and Food in Italy. Antibiotics. 2020;9:782. doi: 10.3390/antibiotics9110782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Nascimento T., Cantamessa R., Melo L., Fernandes M.R., Fraga E., Dropa M., Sato M.I., Cerdeira L., Lincopan N. International high-risk clones of Klebsiella pneumoniae KPC-2/CC258 and Escherichia coli CTX-M-15/CC10 in urban lake waters. Sci. Total Environ. 2017;598:910–915. doi: 10.1016/j.scitotenv.2017.03.207. [DOI] [PubMed] [Google Scholar]
- 110.Reid C.J., DeMaere M.Z., Djordjevic S.P. Australian porcine clonal complex 10 (CC10) Escherichia coli belong to multiple sublineages of a highly diverse global CC10 phylogeny. Microb. Genom. 2019;5:e000225. doi: 10.1099/mgen.0.000225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Skarżyńska M., Zaja̧c M., Bomba A., Bocian Ł., Kozdruń W., Polak M., Wia̧cek J., Wasyl D. Antimicrobial Resistance Glides in the Sky-Free-Living Birds as a Reservoir of Resistant Escherichia coli With Zoonotic Potential. Front. Microbiol. 2021;12:656223. doi: 10.3389/fmicb.2021.656223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Fuga B., Sellera F.P., Cerdeira L., Esposito F., Cardoso B., Fontana H., Moura Q., Cardenas-Arias A., Sano E., Ribas R.M., et al. WHO Critical Priority Escherichia coli as One Health Challenge for a Post-Pandemic Scenario: Genomic Surveillance and Analysis of Current Trends in Brazil. Microbiol. Spectr. 2022;10:e0125621. doi: 10.1128/spectrum.01256-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Li F., Ye K., Li X., Ye L., Guo L., Wang L., Yang J. Genetic characterization of Carbapenem-Resistant Escherichia coli from China, 2015–2017. BMC Microbiol. 2021;21:248. doi: 10.1186/s12866-021-02307-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Schaufler K., Semmler T., Wieler L.H., Wöhrmann M., Baddam R., Ahmed N., Müller K., Kola A., Fruth A., Ewers C., et al. Clonal spread and interspecies transmission of clinically relevant ESBL-producing Escherichia coli of ST410—Another successful pandemic clone? FEMS Microbiol. Ecol. 2016;92:fiv155. doi: 10.1093/femsec/fiv155. [DOI] [PubMed] [Google Scholar]
- 115.Falgenhauer L., Imirzalioglu C., Ghosh H., Gwozdzinski K., Schmiedel J., Gentil K., Bauerfeind R., Kämpfer P., Seifert H., Michael G.B., et al. Circulation of clonal populations of fluoroquinolone-resistant CTX-M-15- producing Escherichia coli ST410 in humans and animals in Germany. Int. J. Antimicrob. Agents. 2016;47:457–465. doi: 10.1016/j.ijantimicag.2016.03.019. [DOI] [PubMed] [Google Scholar]
- 116.Liu Y., Feng Y., Wu W., Xie Y., Wang X., Zhang X., Chen X., Zong Z. First report of OXA-181-producing Escherichia coli in China and characterization of the isolate using whole-genome sequencing. Antimicrob. Agents Chemother. 2015;59:5022–5025. doi: 10.1128/AAC.00442-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Piazza A., Comandatore F., Romeri F., Pagani C., Floriano A.M., Ridolfo A., Antona C., Brilli M., Mattioni Marchetti V., Bandi C., et al. First report of an ST410 OXA-181 and CTX-M-15 coproducing Escherichia coli clone in Italy: A whole-genome sequence characterization. Microb. Drug Resist. 2018;24:1207–1209. doi: 10.1089/mdr.2017.0366. [DOI] [PubMed] [Google Scholar]
- 118.Roer L., Overballe-Petersen S., Hansen F., Schønning K., Wang M., Røder B.L., Hansen D.S., Justesen U.S., Andersen L.P., Fulgsang-Damgaard D., et al. Escherichia coli Sequence Type 410 Is Causing New International High-Risk Clones. mSphere. 2018;3:e00337-18. doi: 10.1128/mSphere.00337-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Overballe-Petersen S., Roer L., Ng K., Hansen F., Justesen U.S., Andersen L.P., Stegger M., Hammerum A.M., Hasman H. Complete nucleotide sequence of an Escherichia coli sequence type 410 strain carrying blaNDM-5 on an IncF multidrug resistance plasmid and bla OXA-181 on an IncX3 plasmid. Genome Announc. 2018;6:e01542-17. doi: 10.1128/genomeA.01542-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Tian X., Zheng X., Sun Y., Fang R., Zhang S., Zhang X., Lin J., Cao J., Zhou T. Molecular mechanisms and epidemiology of carbapenem-resistant Escherichia coli isolated from Chinese patients during 2002–2017. Infect. Drug Resist. 2020;13:501–512. doi: 10.2147/IDR.S232010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Peri A.M., Piazza A., De Zan V., Carugati M., Muscatello A., Comandatore F., De Lorenzis E., Pluderi M., Arghittu M., Cariani L., et al. Autochthonous ST405 NDM-5 producing Escherichia coli causing fatal sepsis in Northern Italy. Int. J. Antimicrob. Agents. 2020;55:105953. doi: 10.1016/j.ijantimicag.2020.105953. [DOI] [PubMed] [Google Scholar]
- 122.Touati M., Hadjadj L., Berrazeg M., Baron S.A., Rolain J.M. Emergence of Escherichia coli harbouring mcr-1 and mcr-3 genes in North West Algerian farmlands. J. Glob. Antimicrob. Resist. 2020;21:132–137. doi: 10.1016/j.jgar.2019.10.001. [DOI] [PubMed] [Google Scholar]
- 123.Tripathi G., Wiltshire C., Macaskill S., Tournu H., Budge S., Brown A.J. Emergence and spread of B2-ST131-O25b, B2-ST131-O16 and D-ST405 clonal groups among extended-spectrum-beta-lactamase-producing Escherichia coli in Japan. J. Antimicrob. Chemother. 2012;67:2612–2620. doi: 10.1093/jac/dks278. [DOI] [PubMed] [Google Scholar]
- 124.Chattaway M.A., Jenkins C., Ciesielczuk H., Day M., DoNascimento V., Day M., Rodríguez I., van Essen-Zandbergen A., Schink A.K., Wu G., et al. Evidence of evolving extraintestinal enteroaggregative Escherichia coli ST38 clone. Emerg. Infect. Dis. 2014;20:1935–1937. doi: 10.3201/eid2011.131845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Poirel L., Bernabeu S., Fortineau N., Podglajen I., Lawrence C., Nordmann P. Emergence of OXA-48-producing Escherichia coli clone ST38 in France. Antimicrob. Agents Chemother. 2011;55:4937–4938. doi: 10.1128/AAC.00413-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Turton J.F., Doumith M., Hopkins K.L., Perry C., Meunier D., Woodford N. Clonal expansion of Escherichia coli ST38 carrying a chromosomally integrated OXA-48 carbapenemase gene. J. Med. Microbiol. 2016;65:538–546. doi: 10.1099/jmm.0.000248. [DOI] [PubMed] [Google Scholar]
- 127.Gauthier L., Dortet L., Cotellon G., Creton E., Cuzon G., Ponties V., Bonnin R.A., Naas T. Diversity of Carbapenemase-Producing Escherichia coli Isolates in France in 2012–2013. Antimicrob. Agents Chemother. 2018;62:e00266-18. doi: 10.1128/AAC.00266-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Falgenhauer L., Nordmann P., Imirzalioglu C., Yao Y., Falgenhauer J., Hauri A.M., Heinmüller P., Chakraborty T. Cross-border emergence of clonal lineages of ST38 Escherichia coli producing the OXA-48-like carbapenemase OXA-244 in Germany and Switzerland. Int. J. Antimicrob. Agents. 2020;56:106157. doi: 10.1016/j.ijantimicag.2020.106157. [DOI] [PubMed] [Google Scholar]
- 129.Kremer K., Kramer R., Neumann B., Haller S., Pfennigwerth N., Werner G., Gatermann S., Schroten H., Eckmanns T., Hans J.B. Rapid spread of OXA-244-producing Escherichia coli ST38 in Germany: Insights from an integrated molecular surveillance approach; 2017 to January 2020. Eurosurveillance. 2020;25:2000923. doi: 10.2807/1560-7917.ES.2020.25.25.2000923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Nesporova K., Jamborova I., Valcek A., Medvecky M., Literak I., Dolejska M. Various conjugative plasmids carrying the mcr-5 gene in Escherichia coli isolates from healthy chickens in Paraguay. J. Antimicrob. Chemother. 2019;74:3394–3397. doi: 10.1093/jac/dkz317. [DOI] [PubMed] [Google Scholar]
- 131.Sekizuka T., Matsui M., Yamane K., Takeuchi F., Ohnishi M., Hishinuma A., Arakawa Y., Kuroda M. Complete sequencing of the bla(NDM-1)-positive IncA/C plasmid from Escherichia coli ST38 isolate suggests a possible origin from plant pathogens. PLoS ONE. 2011;6:e25334. doi: 10.1371/journal.pone.0025334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Guenther S., Semmler T., Stubbe A., Stubbe M., Wieler L.H., Schaufler K. Chromosomally encoded ESBL genes in Escherichia coli of ST38 from Mongolian wild birds. J. Antimicrob. Chemother. 2017;72:1310–1313. doi: 10.1093/jac/dkx006. [DOI] [PubMed] [Google Scholar]
- 133.Mora A., García-Peña F.J., Alonso M.P., Pedraza-Diaz S., Ortega-Mora L.M., Garcia-Parraga D., López C., Viso S., Dahbi G., Marzoa J., et al. Impact of human-associated Escherichia coli clonal groups in Antarctic pinnipeds: Presence of ST73, ST95, ST141 and ST131. Sci. Rep. 2018;8:4678. doi: 10.1038/s41598-018-22943-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Accogli M., Giani T., Monaco M., Giufrè M., García-Fernández A., Conte V., D’Ancona F., Pantosti A., Rossolini G.M., Cerquetti M. Emergence of Escherichia coli ST131 sub-clone H30 producing VIM-1 and KPC-3 carbapenemases, Italy. J. Antimicrob. Chemother. 2014;69:2293–2296. doi: 10.1093/jac/dku132. [DOI] [PubMed] [Google Scholar]
- 135.Chavda K.D., Chen L., Jacobs M.R., Bonomo R.A., Kreiswirth B.N. Molecular diversity and plasmid analysis of KPC-producing Escherichia coli. Antimicrob. Agents Chemother. 2016;60:4073–4081. doi: 10.1128/AAC.00452-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Aquino-Andrade A., Merida-Vieyra J., Arias de la Garza E., Arzate-Barbosa P., De Colsa Ranero A. Carbapenemase-producing Enterobacteriaceae in Mexico: Report of seven non-clonal cases in a pediatric hospital. BMC Microbiol. 2018;18:38. doi: 10.1186/s12866-018-1166-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Pan F., Tian D., Wang B., Zhao W., Qin H., Zhang T., Zhang H. Fecal carriage and molecular epidemiology of carbapenem-resistant Enterobacteriaceae from outpatient children in Shanghai. BMC Infect. Dis. 2019;19:678. doi: 10.1186/s12879-019-4298-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.McGann P., Snesrud E., Maybank R., Corey B., Ong A.C., Clifford R., Hinkle M., Whitman T., Lesho E., Schaecher K.E. Escherichia coli harboring mcr-1 and blaCTX-M on a novel IncF plasmid: First report of mcr-1 in the United States. Antimicrob. Agents Chemother. 2016;60:4420–4421. doi: 10.1128/AAC.01103-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Yu H., Qu F., Shan B., Huang B., Jia W., Chen C., Li A., Miao M., Zhang X., Bao C., et al. Detection of the mcr-1 colistin resistance gene in carbapenem-resistant Enterobacteriaceae from different hospitals in China. Antimicrob. Agents Chemother. 2016;60:5033–5035. doi: 10.1128/AAC.00440-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Tada T., Nhung P.H., Shimada K., Tsuchiya M., Phuong D.M., Anh N.Q., Ohmagari N., Kirikae T. Emergence of colistin-resistant Escherichia coli clinical isolates harboring mcr-1 in Vietnam. Int. J. Infect. Dis. 2017;63:72–73. doi: 10.1016/j.ijid.2017.07.003. [DOI] [PubMed] [Google Scholar]
- 141.Vieyra J., De Colsa-Ranero A., Arzate-Barbosa P., Arias-de la Garza E., Méndez-Tenorio A., Murcia-Garzón J., Aquino-Andrade A. First clinical isolate of Escherichia coli harboring mcr-1 gene in Mexico. PLoS ONE. 2019;14:e0214648. doi: 10.1371/journalpone.0214648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Wang X., Zhai W., Li J., Liu D., Zhang Q., Shen Z., Wang S., Wang Y. Presence of an mcr-3 variant in Aeromonas caviae, Proteus mirabilis, and Escherichia coli from one domestic duck. Antimicrob. Agents Chemother. 2017;62:e02106-17. doi: 10.1128/AAC.02106-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Melendez D., Roberts M.C., Greninger A.L., Weissman S., No D., Rabinowitz P., Wasser S. Whole-genome analysis of extraintestinal pathogenic Escherichia coli (ExPEC) MDR ST73 and ST127 isolated from endangered southern resident killer whales (Orcinus orca) J. Antimicrob. Chemother. 2019;74:2176–2180. doi: 10.1093/jac/dkz159. [DOI] [PubMed] [Google Scholar]
- 144.Cummins M.L., Reid C.J., Djordjevic S.P. F Plasmid Lineages in Escherichia coli ST95: Implications for Host Range, Antibiotic Resistance, and Zoonoses. mSystems. 2022;7:e0121221. doi: 10.1128/msystems.01212-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Torres A.G. The Challenge to Control Emergence of Antibiotic Resistance in Virulent Escherichia coli Isolates in Latin America. Microbiol. Spectr. 2022;10:e01506-22. doi: 10.1128/spectrum.01506-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Kadar B., Kocsis B., Nagy K., Szabo D. The renaissance of polymyxins. Curr. Med. Chem. 2013;20:3759–3773. doi: 10.2174/09298673113209990185. [DOI] [PubMed] [Google Scholar]
- 147.Roer L., Hansen F., Thomsen M.C.F., Knudsen J.D., Hansen D.S., Wang M., Samulioniené J., Justesen U.S., Rřder B.L., Schumacher H., et al. WGS-based surveillance of third-generation cephalosporin-resistant Escherichia coli from bloodstream infections in Denmark. J. Antimicrob. Chemother. 2017;72:1922–1929. doi: 10.1093/jac/dkx092. [DOI] [PubMed] [Google Scholar]
- 148.Luo C., Walk S.T., Gordon D.M., Feldgarden M., Tiedje J.M., Konstantinidis K.T. Genome sequencing of environmental Escherichia coli expands understanding of the ecology and speciation of the model bacterial species. Proc. Natl. Acad. Sci. USA. 2011;108:7200–7205. doi: 10.1073/pnas.1015622108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Tchesnokova V., Billig M., Chattopadhyay S., Linardopoulou E., Aprikian P., Roberts P.L., Skrivankova V., Johnston B., Gileva A., Igusheva I., et al. Predictive diagnostics for Escherichia coli infections based on the clonal association of antimicrobial resistance and clinical outcome. J. Clin. Microbiol. 2013;51:2991–2999. doi: 10.1128/JCM.00984-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Denamur E., Clermont O., Bonacorsi S., Gordon D. The population genetics of pathogenic Escherichia coli. Nat. Rev. Microbiol. 2021;19:37–54. doi: 10.1038/s41579-020-0416-x. [DOI] [PubMed] [Google Scholar]
- 151.Flament-Simon S.C., Nicolas-Chanoine M.H., García V., Duprilot M., Mayer N., Alonso M.P., García-Meniño I., Blanco J.E., Blanco M., Blanco J. Clonal Structure, Virulence Factor-encoding Genes and Antibiotic Resistance of Escherichia coli, Causing Urinary Tract Infections and Other Extraintestinal Infections in Humans in Spain and France during 2016. Antibiotics. 2020;9:161. doi: 10.3390/antibiotics9040161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Flament-Simon S.-C., de Toro M., Mora A., García V., García-Meniño I., Díaz-Jiménez D., Herrera A., Blanco J. Whole Genome Sequencing and Characteristics of mcr-1–Harboring Plasmids of Porcine Escherichia coli Isolates Belonging to the High-Risk Clone O25b:H4-ST131 Clade, B. Front. Microbiol. 2020;11:387. doi: 10.3389/fmicb.2020.00387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.García-Meniño I., Lumbreras P., Lestón L., Álvarez-Álvarez M., García V., Hammerl J.A., Fernández J., Mora A. Occurrence and Genomic Characterization of Clone ST1193 Clonotype 14-64 in Uncomplicated Urinary Tract Infections Caused by Escherichia coli in Spain. Microbiol. Spectr. 2022;10:0004122. doi: 10.1128/spectrum.00041-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Horesh G., Blackwell G.A., Tonkin-Hill G., Corander J., Heinz E., Thomson N.R. A comprehensive and high-quality collection of Escherichia coli genomes and their genes. Microb. Genom. 2021;7:000499. doi: 10.1099/mgen.0.000499. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.