Abstract
Skin photoaging, which causes wrinkles, increased epidermal thickness, and rough skin texture, is induced by ultraviolet B (UVB) exposure. These symptoms by skin photoaging have been reported to be involved in the reduction of collagen by the expression of matrix metalloproteinases (MMPs) and activator protein-1 (AP-1). This study investigated the protective effects of Bifidobacterium animalis subsp. lactis MG741 (Bi. lactis MG741) in Hs-68 fibroblasts and hairless mice (HR-1) following UVB exposure. We demonstrated that the Bi. lactis MG741 reduces wrinkles and skin thickness by downregulating MMP-1 and MMP-3, phosphorylation of extracellular signal-regulated kinase (ERK), and c-FOS in fibroblasts and HR-1. Additionally, in UVB-irradiated dorsal skin of HR-1, Bi. lactis MG741 inhibits the expression of nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB), an inflammation-related factor. Thus, Bi. lactis MG741 has the potential to prevent wrinkles and skin inflammation by modulating skin photoaging markers.
Keywords: Bifidobacterium animalis ssp. lactis MG741, matrix metalloproteinases, anti-photoaging, ultraviolet B
1. Introduction
The skin is the largest organ in the body accounting for 16% of the body weight [1]. The skin acts as a barrier to protect against various external stimuli, such as physical stress, smoking, air pollution, pathogens, and ultraviolet (UV) radiation [2]. Since the skin is the most exposed organ of the body externally, its aging can be caused by stimulation by environmental factors, such as UV, which is the most harmful external factor [3]. Although most UV radiation is absorbed by the epidermis of the skin, ultraviolet B (UVB) affects dermal fibroblasts by activating factors, including activator protein-1 (AP-1) and nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB), which are related to aging in the epidermis [4]. UVB irradiation in the skin causes skin aging, such as wrinkles, inflammation, and even leading to skin cancer [5,6]. Therefore, it is crucial to develop agents that are effective for photoaging having are proven safe [7].
It has been demonstrated that the formation of wrinkles in the skin is caused by the breakdown of collagen as an activation mechanism of matrix metalloproteinases (MMPs) due to external factors of aging, such as UVB exposure [8]. The regulation of MMPs production is mainly affected by AP-1 activation stimulated by the mitogen-activated protein kinases (MAPKs) [9]. Moreover, UVB exposure increases inflammatory factors, including NF-κB, interleukin-6 (IL-6), and tumor necrosis factor-α (TNF-α), which upregulate MMPs activation in the skin [5,9].
According to the World Health Organization (WHO) and Food and Agriculture Organization of the United Nations (FAO), probiotics, including Lactobacillus and Bifidobacterium, are living microorganisms that have health benefit on host, when administered in adequate amounts [10,11]. Probiotics, as dietary supplements, are generally known to have a protective effect against gastrointestinal disorders [12]. Probiotics has been actively studied for skin diseases such as atopic dermatitis, psoriasis, acne, and photoaging [13]. It has been previously reported that Lactobacillus plantarum, Bi. longum, and Bi. breve have shown efficacy in preventing photo-aging [13]. Metabolites contained in the cell-free supernatant (CFS) of probiotics that affect skin health include diacetyl, lipoteichoic acid, lactic acid, and acetic acid [14]. Probiotics have recently been used as potential agents with various health benefits and are attracting attention as an effective alternative to skin aging [15].
Oxidative stress caused by reactive oxygen species (ROS) in the skin is caused by UVB, which can exacerbate the skin-aging [16]. To prevent oxidative stress in the skin, various antioxidants, such as vitamin polyphenols and collagen peptides, have been applied [17]. We have previously demonstrated that Bi. lactis MG741 has antioxidant potential in a tert-butyl hydroperoxide (t-BHP)-induced animal model, and was evaluated for safety as probiotics [18]. However, the underlying mechanisms for intrinsic and extrinsic aging of the skin associated with the protective effect of MG741 against UVB have not been elucidated. Therefore, this study demonstrates the protective effects of Bi. lactis MG741 against UVB-induced photoaging in Hs68 fibroblasts and hairless (HR-1) mice, and investigated the potential mechanisms.
2. Materials and Methods
2.1. Apparatus and Reagents
For UVB irradiation, a UV crosslinker was purchased from BoTeck (Gunpo, Republic of Korea) for cell assay. A UVB lamp was purchased from Philips (Amsterdam, Netherlands) for the animal study. A microplate spectrophotometer was used using Epoch 2 (Bio Tek Instruments, Winooski, VT, USA). Visioline VL-650 was obtained from Courage & Khazaka Electronic GmbH (Cologne, Germany). The GPSKIN barrier light was purchased from GPSkin (Seoul, Republic of Korea). An optical microscope was used (BX61, Tokyo, Japan) and photographed using a DP80 microscope (Olympus). The CFX Connect Real-Time PCR Detection System was purchased from Bio-Rad (Hercules, CA, USA). Chemiluminescence images were acquired using a LuminoGraph III Lite (WSE-6370, Atto, Tokyo, Japan).
All reagents were purchased from Sigma Aldrich (St. Louis, MO, USA) unless otherwise indicated. De Man, Rogosa, and Sharpe (MRS) broth were obtained from Becton Dickinson and Company (Franklin Lakes, NJ, USA). Dulbecco’s modified Eagle’s medium (DMEM), fetal bovine serum (FBS), and penicillin/streptomycin (P/S) were purchased from Gibco (Gaithersburg, MD, USA). Dulbecco’s phosphate-buffered saline (DPBS) purchased from Welgene (Gyeongsan-si, Republic of Korea). To perform real-time polymerase chain reaction, NucleoZol (MACHEREY-NAGEL, Gutenberg, Hoerdt, France) and Maxime RT PreMix (iNtRON, Seongnam-si, Republic of Korea) were used. The contents of pro-collagen type 1 were analyzed using a Procollagen Type I C-peptide (PIP) enzyme-linked immunosorbent assay (EIA) Kit (Takara Bio Inc., Shiga, Japan). AmfiSure qGreen Q-PCR Master Mix, radioimmunoprecipitation (RIPA), Bradford Assay Kit, protease and phosphatase inhibitor cocktail, polyvinylidene fluoride (PVFD) membrane, goat anti-rabbit and anti-mouse IgG(H + L)-HRP, and enhanced chemiluminescence (ECL) were obtained from GenDEPOT (Katy, TX, USA). Primary antibodies were purchased from Cell Signaling Technology (Danvers, MA, USA) and Santa Cruz Biotechnology (Dallas, CA, USA).
2.2. Preparation Sample of Bi. lactis MG741
Bifidobacterium animalis ssp. lactis (Bi. lactis) MG741 was isolated from human infants and laboratory-maintained in MEDIOGEN (Jecheon, Republic of Korea). Bi. lactis MG741 (NCBI GenBank number: MN069035.1; originated from infant feces) was cultivated in MRS broth with GasPak EZ (Becton, Dickinson, and Company). Cell-free supernatant (CFS) of Bi. lactis MG741 for in vitro assays was prepared as previously described [18]. For the in vivo study, the grown Bi. lactis MG741 was freeze-dried (20 mTorr, –40 ℃, 1 d) and powdered Bi. lactis MG741 was mixed with maltodextrin to obtain a dilution (1 × 1011 CFU/g).
2.3. In Vitro Study
Hs68 fibroblasts (ATCC, Manassas, MD, USA) were used in the experiments. The fibroblasts were grown in DMEM containing 10% FBS and 1% P/S in 5% CO2 and at 37 ℃ in a humidified atmosphere. The fibroblasts were transferred every two days with fresh growth media.
2.3.1. Cytotoxicity
The cell viability of the CFS from Bi. lactis MG741 cells was estimated using the 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) assay. Fibroblasts were seeded in a 96-well plate (1 × 104 cells/well) and incubated overnight. The CFS was treated with 5 and 10% (v/v in DMEM) in each well for 24 h. After replacing the medium with DPBS, followed by exposure to UVB (30 mJ/cm2) using a UV crosslinker, the fibroblasts were incubated with CFS in media for 24 h. The MTT solution (0.25 mg/mL) was added and incubated for 2 h. The medium was discarded and dimethyl sulfoxide (DMSO, 150 μL) was added to dissolve the formazan crystals. Absorbance was measured at 550 nm using a microplate spectrophotometer.
2.3.2. Determination of PIP by EIA
PIP was measured according to the manufacturer’s instructions (Takara Bio, Inc.). For evaluation of PIP, the fibroblasts (8 × 104 cells/well) in a 24-well plate were incubated with or without 10% CFS for 24 h. After exposure to UVB (30 mJ/cm2), cells were incubated with CFS for 24 h. PIP content was measured using a microplate spectrophotometer at 450 nm and normalized to protein (μg/μL) using the Bradford assay.
2.4. Animals Study
The animal study protocol for the in vivo study was approved by the Ethics Committee of ChemOn Inc., Gyeonggi-do, Republic of Korea (approval number, 2022-0017). Five-week-old female specific pathogen-free (SPF) hairless (HR-1) mice were used in this study (Central Lab. Animal Inc., Seoul, Republic of Korea). All mice were housed in an environment with a controlled temperature of 22 ± 3 °C, a humidity of 55 ± 15%, and illuminance of 150–300 Lux under a 12 h light/dark cycle. During the experimental period, the diet (Teklad certified irradiated global 18% protein rodent diet, 2918C, ENVIGO, Indianapolis, IN, USA) and drinking water were fed by free intake.
2.4.1. Experimental Design
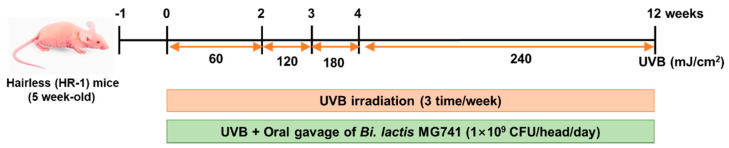
After 1-week of acclimation, animals were divided by randomized complete block design into three groups (n = 6 per group), as follows: (1) normal (no-UVB) group, (2) UVB group (60 to 240 mJ/cm2), (3) UVB + Bi. lactis MG741 strain (1 × 109 CFU/head/day). UVB irradiation was gradually increased from 60 to 240 mJ/cm2 for 12 weeks. The protocol used for the animal model induced by UVB is shown in Figure 1. The mice were administered Bi. lactis MG741 using oral gavage. The normal and only UVB-exposed group was administered maltodextrin (0.01 g/head/day). All treatment solutions were freshly dissolved on the experimental days in phosphate-buffered saline (PBS). Body weights were measured at one-week intervals during the 12-week experimental period (Figure S1).
Figure 1.
Animal experiment procedure of UVB irradiation on HR-1 mice. After adaptation, the dorsal skin of the HR-1 mice was irradiated to UVB (290 to 320 nm) at one minimal erythema dose (MED, 60 mJ/cm2) for two weeks, two MED (120 mJ/cm2) for one week, three MED (180 mJ/cm2) for one week, and four MED (240 mJ/cm2) for the last eight weeks.
2.4.2. Determination of Wrinkle Formation
For the measurement of wrinkle formation, the skin impression (replica) of the dorsal skin was prepared. At 12 weeks, a replica of each mouse was produced to estimate the total wrinkle area (mm2), mean length (mm), mean depth (μm), and maximum wrinkle depth (μm).
2.4.3. Histopathological and Skin Hydration Examination
A part of the dorsal skin was fixed with 10% neutral buffered formalin and embedded in paraffin blocks. Paraffin blocks were cut into sections and stained with hematoxylin and eosin (H&E). The sections were examined under an optical microscope and photographed. The epidermal thickness, stained with H&E, was measured at 100× magnification. Trans-epidermal water loss (TEWL) and hydration of mouse dorsal skin were determined using GPSKIN barrier light at 12 weeks.
2.5. Quantitative RT-PCR (qRT-PCR)
Hs68 fibroblasts were seeded at 3 × 105 cells/well in 6-well plates and treated with or without 10% CFS for 24 h. After replacing the medium with DPBS, followed by exposure to UVB (30 mJ/cm2), the fibroblasts were incubated with CFS in media for 24 h. The total RNA of fibroblasts and dorsal skin tissues was extracted using NucleoZol, and mRNA was synthesized to cDNA using Maxime RT PreMix, according to the manufacturer’s instructions [19]. qPCR was performed using the AmfiSure qGreen Q-PCR Master Mix using the CFX Connect system. Primers were designed using Primer-BLAST as shown in Table S1 (NCBI, Bethesda, MD, USA). The threshold cycle (Ct) value for each gene was normalized to glyceraldehyde-3-phosphate dehydrogenase (GAPDH). The results were analyzed with CFX Maestro software 2.3 for Windows, provided by Bio-Rad.
2.6. Western Blotting
Whole fibroblast lysates and dorsal skin tissue were prepared in a RIPA buffer containing protease and phosphatase inhibitors. Total protein content was determined using the Bradford assay. The proteins were separated by sodium dodecyl sulfate-polyacrylamide gel electrophoresis using 10% acrylamide gel and transferred to PVDF membranes. Membranes were incubated with primary antibodies (MMP-1, MMP-3, p-extracellular signal-regulated kinase (ERK), ERK, p-c-Jun N-terminal kinase (JNK), JNK, p- p38 mitogen-activated protein kinases (p38), p38, p-transcription factor Jun (c-Jun), c-Jun, p-c-Fos, c-Fos, p-NF-κB p65, NF-κB p65, and β-actin) for 18–24 h and secondary antibodies for 1 h. The blots were visualized using an ECL reagent and a chemiluminescence system. Quantitative analysis was performed using the ImageJ software (National Institutes of Health, Bethesda, MD, USA).
2.7. Statistics
All experimental results are presented as the mean ± standard error (SE). The statistical significance of differences in this study was calculated using Student’s t-test (Prism 5.02 GraphPad Software, San Diego, CA, USA).
3. Results
3.1. Protective Effect of Bi. lactis MG741 on UVB-Exposed Hs68 Fibroblasts
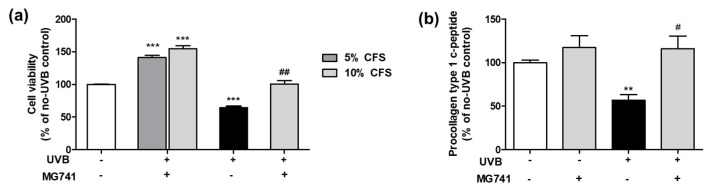
To investigate the protective effect in Hs68 fibroblasts, we performed MTT assay (Figure 2a). CFS (10%) from Bi. lactis MG741 proliferated Hs68 fibroblasts up to 1.55-fold of no-UVB control, and was markedly protected against UVB-induced cell death (1.56-fold of UVB control). As a result of the energy of UVB exposure (15, 30, 50, and 100 mJ/cm2) that causes the death of fibroblasts, they exhibited a cytotoxicity of ~30% at a minimum and morphology change on 30 mJ/cm2 (Figure S2). Thus, 30 mJ/cm2 UVB irradiation was used in subsequent experiments. Bi. lactis MG741 affected PIP degradation in UVB-exposed Hs68 fibroblasts (Figure 2b). CFS (10%) from Bi. lactis MG741 increased PIP content (1.17-fold) in fibroblasts and significantly enhanced PIP content up to 2.04-fold in UVB-exposed Hs68 fibroblasts.
Figure 2.
Effects of CFS from Bi. lactis MG741 on (a) cell viability and (b) procollagen type 1 c-peptide (PIP) contents in UVB-exposed Hs68 fibroblasts. Data are indicated as means ± standard error (SE, n = 3). ** p < 0.01, and *** p < 0.001 vs. no-UVB control; # p < 0.05, and ## p < 0.01 vs. UVB-exposed control.
3.2. Bi. lactis MG741 Exerts Rreduction of mRNA and Protein Expression Related to Wrinkles on UVB-Exposed Hs68 Fibroblasts
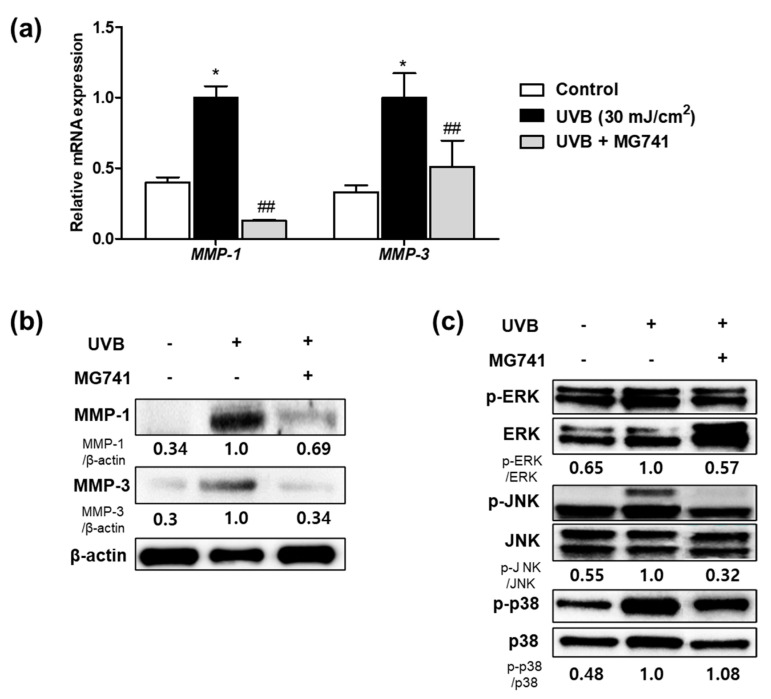
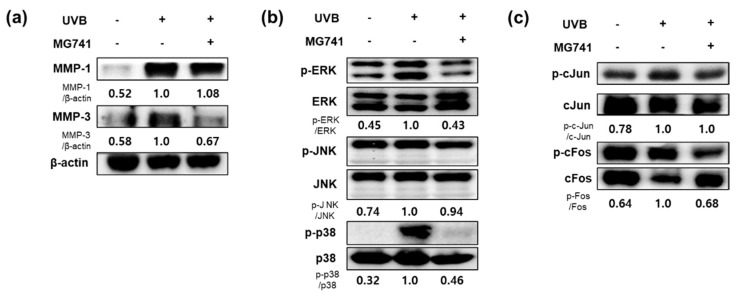
Exposure to UVB promoted factors involved in wrinkle formation in fibroblasts by expressing MMPs. However, CFS (10%) from Bi. lactis MG741 inhibited the mRNA and protein expressions of MMP-1, and MMP-3, respectively, in UVB-exposed Hs68 fibroblasts (Figure 3a,b). As a result of MAPKs, which activated MMPs, Western blotting revealed that UVB exposure upregulated p-ERK (1.54-fold), p-JNK (1.82-fold), and p-p38 (2.08-fold) in fibroblasts. Bi. lactis MG741 reduced the phosphorylation of ERK and JNK in UVB-exposed Hs68 fibroblasts, shown in Figure 3c.
Figure 3.
The mRNA and protein expression of matrix metalloproteinases (MMPs) and mitogen-activated protein kinases (MAPKs) in CFS from Bi. lactis MG741 treatment with UVB-exposed Hs68 fibroblasts. (a) The mRNA expression levels of MMPs in UVB (30 mJ/cm2)-exposed Hs68 fibroblasts treated with CFS (10%) from Bi. lactis MG741. (b,c) The Western blot images were measured following treatment with CFS and UVB. Fibroblasts were treated with CFS (10%) Bi. lactis MG741 for 24 h. Subsequently, the cells were exposed to UVB (30 mJ/cm2) and it was further cultured in media containing CFS for 48 h for MMPs, and 24 h for MAPKs. The ratio of each protein was shown below the blotting images and indicated to fold of UVB-exposed control. Data are indicated as means ± SE (n = 3). * p < 0.05 vs. no-UVB control; ## p < 0.01 vs. UVB-exposed control.
3.3. Bi. lactis MG741 Modulates Skin Changes on UVB-Exposed Dorsal Skin of HR-1 Mice
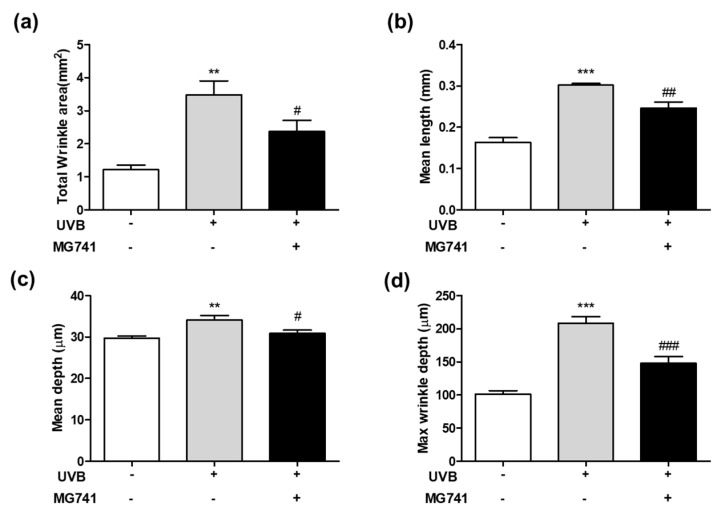
The effects of Bi. lactis MG741 on skin changes in UVB-exposed dorsal skin of HR-1 mice was performed, as shown in Figure 1. As shown in Figure 4, the increase in wrinkle formation, including total wrinkle area (2.85-fold), mean length (1.85-fold), mean depth (1.15-fold), and maximum wrinkle depth (2.05-fold), was shown by UVB, compared with non-exposed HR-1 mice. By contrast, the administration of Bi. lactis MG741 ameliorated the wrinkle formation on UVB-exposure in, respectively HR-1 mice. Among them, the total wrinkle area was markedly decreased by Bi. lactis MG741 (0.68-fold increase in UVB-exposed dorsal skin of HR-1 mice).
Figure 4.
Effect of Bi. lactis MG741 on skin wrinkle formation such as (a) total wrinkle area, (b) mean length, (c) mean depth and (d) max wrinkle depth in UVB-exposed HR-1 mice. HR-1 mice were treated with Bi. lactis MG741 (1 × 109 CFU/head/day) orally and UVB irradiation on dorsal skin until 12 weeks. Data are indicated as means ± SE (n = 6). ** p < 0.01, and *** p < 0.001 vs. no-UVB control; # p < 0.05, ## p < 0.01, and ### p < 0.001 vs. UVB-exposed control.
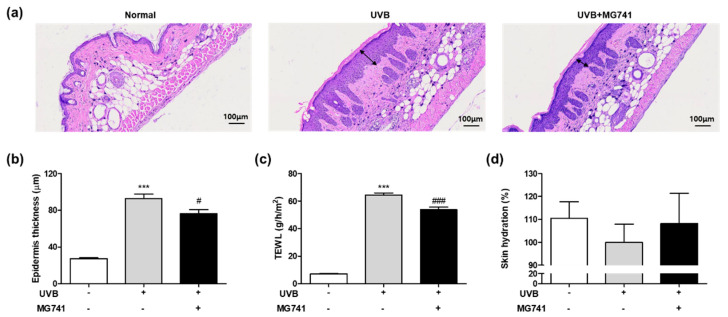
Though H&E staining, UVB exposure in HR-1 mice resulted in marked thickening of the dorsal skin (3.39-fold of non-exposure; Figure 5a,b); however, Bi. lactis MG741 reduced the epidermal thickness up to 0.82-fold in UVB-exposed HR-1 mice. As shown in Figure 5c,d, UVB irradiation of the dorsal skin of HR-1 mice induced increase in TEWL (8.92-fold, significantly) and loss of skin hydration (0.91-fold) compared with non-exposure. Bi. lactis MG741 mitigated these changes caused by UVB (in TEWL, 0.82-fold; in loss of skin hydration, 1.08-fold).
Figure 5.
Histological examination and skin hydration of UVB-exposed dorsal skin tissue of HR-1 mice treated with Bi. lactis MG741. The animal experiment procedure is the same as described in the legend in Figure 4. (a) The images of dorsal skin sections were stained by hematoxylin and eosin (H&E) using a microscope at 100× magnification. Double arrows indicate the epidermis. At 12 weeks, the dorsal skins were collected to measure (b) the epidermis thickness (based on H&E stain), (c) TEWL, and (d) skin hydration. Data are indicated as means ± SE (n = 6). *** p < 0.001 vs. no-UVB control; # p < 0.05, and ### p < 0.001 vs. UVB-exposed control.
3.4. Effect of Bi. lactis MG741 on Protein Expression Related to Skin Aging on UVB-Exposed Dorsal Skin of HR-1 Mice
The results of Western blot analysis indicated that the protein expressions of MMP-1 (1.92-fold) and MMP-3 (1.73-fold) were clearly enhanced by UVB exposure in the dorsal skin of HR-1 mice (Figure 6a). The protein expression of MMP-3 was decreased by administration of Bi. lactis MG741; however, the MMP-1 expression did not change. As shown in Figure 6b,c, MAPKs (p-ERK, 2.22-fold; pJNK, 1.35-fold; p-p38, 3.13-fold), and AP-1 (p-c-Jun, 1.28-fold; p-c-Fos, 1.56-fold) were also markedly overexpressed in the UVB-exposed dorsal skin of HR-1 mice compared with non-exposed mice. Conversely, Bi. lactis MG741 inhibited the protein expression of p-ERK, p-p38, and p-c-Fos, with no change in p-JNK and p-c-Fos.
Figure 6.
The protein expressions of wrinkle-related factors in Bi. lactis MG741 administration with UVB-exposed dorsal skin tissue of HR-1 mice. The animal experiment procedure is the same as described in the legend in Figure 4. (a) MMPs, (b) MAPKs, and (c) activator protein 1 (AP-1) expressions of mouse dorsal skin were analyzed by Western blotting. The ratio of each protein was shown below the blotting images and indicated to fold of UVB-exposed control. Data are indicated as means ± SE (n = 6).
3.5. Bi. lactis MG741 Downregulates Factors Related to Inflammationon on UVB-Exposed Dorsal Skin of HR-1 Mice
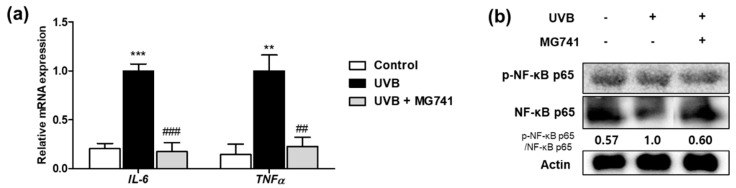
The mRNA expressions of IL-6 and TNFα were significantly increased by UVB irradiation up to 4.89- and 6.90-fold of non-exposure, respectively, whereas Bi. lactis MG741 supplementation significantly reduced these factors (IL-6, 0.17-fold; TNFα, 0.23-fold) compared with the UV-exposed control group (Figure 7a). Moreover, protein expression of p-NF-κB analyzed by Western blot increased up to 1.75-fold compared with that in the dorsal skin of HR-1 mice exposed to UVB irradiation. The protein expression of p-NF-κB, increased by UVB exposure, were improved by the administration of Bi. lactis strain MG741 (Figure 7b).
Figure 7.
Effect of Bi. lactis MG741 on inflammation-related factors in UVB-exposed HR-1 mice. (a) The mRNA expressions of IL-6 and TNFα were measured by qRT-PCR. (b) The ratio of p-NF-κB/NF-κB was shown below the blotting images and indicated to fold of UVB-exposed control. Data are indicated as means ± SE (n = 6). ** p < 0.01, and *** p < 0.001 vs. no-UVB control; ## p < 0.01, and ### p < 0.001 vs. UVB-exposed control.
4. Discussion
Among the photons irradiated from the sun, UV is divided into UVA (320–400 nm), UVB (280–320 nm), and UVC (100–280 nm) [6]. It is known that most UVB is absorbed by the ozone layer, but this amount has increased due to environmental pollution [20]. Long-term UVB irradiation has been reported to increase the decomposition of elastin and collagen in skin aging (such as rough skin, suppression of skin elasticity, and skin wrinkles) and/or has a detrimental effect [21]. Therefore, as the amount of UVB irradiation increases, the effect on the skin is expected to increase. Thus, protective agents have been studied. Recently, probiotics, not synthetic substances, has been studied as alternative products with skin protection effects. It is reported that L. plantarum HY7714 relieves skin wrinkles and improves elasticity by controlling skin moisture and MMPs [22,23,24]. In Bifidobacterium genera, Bi. breve B-3 and Bi. longum suppresses skin wrinkles, TEWL, and epidermal thickening by reducing inflammation-related proteins and MMPs [25,26]. In a previous our study, the Bi. lactis MG741 exerts antioxidant effects by increasing catalase and reducing lipid peroxidation in cell and animal models [18]. UVB generates ROS in skin, including hydroxyl radicals, superoxide anions, and singlet oxygen [16]. Catalase (antioxidant enzymes), and prevention of lipid peroxide exhibit inhibition of skin aging and protective effects on the skin [27]. Based on these data, we investigated the anti-photoaging mechanism of Bi. lactis MG741 in vitro and in vivo.
Skin aging due to UVB shows histological changes, such as an increase in skin thickness and a decrease in skin moisture [28,29]. Fibroblasts, primarily found in the dermis, protect against external damage to the skin by producing an extracellular matrix through granulation tissue formation [9,30]. The extracellular matrix produced by fibroblasts retains moisture and plays an essential role in balancing the skin hydration [31]. Thus, fibroblasts that function normally can maintain the strength and indirectly moisture of the skin. In this study, it was confirmed that Bi. lactis MG741 attenuated skin thickening by inhibiting UVB-induced apoptosis in proliferating fibroblasts and affected TEWL and hydration by the proliferation of fibroblasts.
Chronic UVB exposure accelerates the degradation of collagen and causes cell death, reducing skin strength and elasticity [21]. Most skin collagen is collagen type 1, a protein produced by the synthesis and enzymatic reaction of PIP, and is mainly distributed in fibroblasts [32]. MG741 inhibited PIP degradation in UVB-exposed fibroblasts by increasing PIP secretion. When collagen, a component of the dermis, is damaged by UVB, its structure is deformed exacerbating the formation of wrinkles that are directly or indirectly affected by a decrease in skin elasticity [33]. In our study, Bi. lactis MG741 reduced wrinkle formation in UVB-exposed HR-1 mice. MMPs have 20 isoforms and are known to mainly function in the decomposition of the extracellular matrix and remodeling of tissues [34]. Among them, MMP-1 and MMP-3 are major factors that break down collagen type 1 and are initially enhanced by UVB irradiation in the fibroblasts [35]. The factor most affected by MAPKs (ERK, JNK, and p38) is AP-1, which includes c-Jun and c-Fos [36]. Phosphorylation of JNK/P38 stimulates c-Jun, whereas phosphorylation of ERK activates c-Fos [37]. Activated AP-1 expresses MMP-1 and MMP-3 and eventually degrades the collagen [36]. In cellular and animal models, Bi. lactis MG741 was identified as having a molecular mechanism to reduce MMP-3 through the inhibition of p-c-Fos, commonly activated by p-ERK. NF-κB is an important transcription factor that regulates immunity and various functions related to aging, energy homeostasis, and cell regeneration [38]. UVB exposure induces the production of IL-6 and TNFα, triggering a cascade of NF-κB reactivation [28,39]. Moreover, UVB-activated MAPK stimulates NF-κB phosphorylation to increase MMPs expression, accelerating skin aging by inducing an extracellular matrix degradation [39]. Bi. lactis MG741 exerted efficacy in inflammation and aging-related wrinkle formation by downregulating pro-inflammatory cytokines (IL-6 and TNF-α) and the protein expression of p-NF-κB.
This study confirmed that Bi. lactis MG741 mediates the MMP/AP-1/NFκB signaling pathway to protect the skin from UVB and prevent skin aging in cell and animal models. However, the in vitro and in vivo results suggest that Bi. lactis MG741 strain is a potential candidate for clinical trials. Further studies are required to fully elucidate the use of Bi. lactis MG741 in humans.
5. Conclusions
In summary, this study demonstrated that Bi. lactis MG741 improved pro-collagen type 1 and skin wrinkle formation by modulating MMP/AP-1 in UVB-exposed fibroblasts and HR-1 mice. In addition, UVB-induced skin inflammation alleviated by Bi. lactis MG741 via inhibition of the NF-κB signaling pathway. The results of this study suggest that Bi. lactis MG741 can provide a functional food as an anti-photoaging agent.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/microorganisms10122343/s1, Figure S1: Body weight change against the administration of Bi. lactis MG741 in UVB-exposed HR-1 mice; Figure S2: Cell morphology and viability against UVB treatment on Hs68 cells; Table S1: Primer sequence used in this study.
Author Contributions
Conceptualization, C.-H.K.; methodology, J.Y.L. and J.-Y.P.; investigation, J.-Y.P.; resources, C.-H.K.; data curation, J.Y.L., J.-Y.P. and Y.K.; writing—original draft preparation, J.Y.L.; writing—review and editing, J.Y.L. and C.-H.K.; supervision, C.-H.K.; project administration, C.-H.K. All authors have read and agreed to the published version of the manuscript.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This result was supported by “Regional Innovation Strategy (RIS)” through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (MOE), grant number 2021RIS-001.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Venus M., Waterman J., McNab I. Basic physiology of the skin. Surgery. 2010;28:469–472. doi: 10.1016/j.mpsur.2010.07.011. [DOI] [Google Scholar]
- 2.Suh M.G., Bae G.Y., Jo K., Kim J.M., Hong K.-B., Suh H.J. Photoprotective Effect of Dietary Galacto-Oligosaccharide (GOS) in Hairless Mice via Regulation of the MAPK Signaling Pathway. Molecules. 2020;25:1679. doi: 10.3390/molecules25071679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gromkowska-Kępka K.J., Puścion-Jakubik A., Markiewicz-Żukowska R., Socha K. The impact of ultraviolet radiation on skin photoaging—review of in vitro studies. J. Cosmet. Dermatol. 2021;20:3427–3431. doi: 10.1111/jocd.14033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Berneburg M., Plettenberg H., Krutmann J. Photoaging of human skin. Photodermatol. Photoimmunol. Photomed. Rev. Artic. 2000;16:239–244. doi: 10.1034/j.1600-0781.2000.160601.x. [DOI] [PubMed] [Google Scholar]
- 5.Ansary T.M., Hossain M.R., Kamiya K., Komine M., Ohtsuki M. Inflammatory Molecules Associated with Ultraviolet Radiation-Mediated Skin Aging. Int. J. Mol. Sci. 2021;22:3974. doi: 10.3390/ijms22083974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kaddurah H., Braunberger T.L., Vellaichamy G., Nahhas A.F., Lim H.W., Hamzavi I.H. The Impact of Sunlight on Skin Aging. Curr. Geriatr. Rep. 2018;7:228–237. doi: 10.1007/s13670-018-0262-0. [DOI] [Google Scholar]
- 7.Mukherjee P.K., Maity N., Nema N.K., Sarkar B.K. Bioactive compounds from natural resources against skin aging. Phytomedicine. 2011;19:64–73. doi: 10.1016/j.phymed.2011.10.003. [DOI] [PubMed] [Google Scholar]
- 8.Naylor E.C., Watson R.E., Sherratt M.J. Molecular aspects of skin ageing. Maturitas. 2011;69:249–256. doi: 10.1016/j.maturitas.2011.04.011. [DOI] [PubMed] [Google Scholar]
- 9.Shin J.-W., Kwon S.-H., Choi J.-Y., Na J.-I., Huh C.-H., Choi H.-R., Park K.-C. Molecular Mechanisms of Dermal Aging and Antiaging Approaches. Int. J. Mol. Sci. 2019;20:2126. doi: 10.3390/ijms20092126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mack D.R. Probiotics: Mixed messages. Can. Fam. Physician. 2005;51:1455. [PMC free article] [PubMed] [Google Scholar]
- 11.Hill C., Guarner F., Reid G., Gibson G.R., Merenstein D.J., Pot B., Morelli L., Canani R.B., Flint H.J., Salminen S., et al. Expert consensus document: The International Scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nat. Rev. Gastroenterol. Hepatol. 2014;11:506–514. doi: 10.1038/nrgastro.2014.66. [DOI] [PubMed] [Google Scholar]
- 12.Wilkins T., Sequoia J. Probiotics for Gastrointestinal Conditions: A Summary of the Evidence. Am. Fam. Physician. 2017;96:170–178. [PubMed] [Google Scholar]
- 13.Lolou V., Panayiotidis M.I. Functional Role of Probiotics and Prebiotics on Skin Health and Disease. Fermentation. 2019;5:41. doi: 10.3390/fermentation5020041. [DOI] [Google Scholar]
- 14.Lew L.-C., Liong M.-T. Bioactives from probiotics for dermal health: Functions and benefits. J. Appl. Microbiol. 2013;114:1241–1253. doi: 10.1111/jam.12137. [DOI] [PubMed] [Google Scholar]
- 15.Mishra V., Sharma R., Jaiswal M., Subramani S.K., Yadav A., Rana S., Bisen P.S. A review on recently explored functional aspects of probiotics. Ind. J. Pure Appl. Biosci. 2020;8:213–226. doi: 10.18782/2582-2845.8359. [DOI] [Google Scholar]
- 16.Wenk J., Brenneisen P., Meewes C., Wlaschek M., Peters T., Blaudschun R., Ma W., Kuhr L., Schneider L., Scharffetter-Kochanek K. UV-induced oxidative stress and photoaging. Curr. Probl. Dermatol. Basel. 2001;29:83–94. doi: 10.1159/000060656. [DOI] [PubMed] [Google Scholar]
- 17.Hu S., Zhang X., Chen F., Wang M. Dietary polyphenols as photoprotective agents against UV radiation. J. Funct. Foods. 2017;30:108–118. doi: 10.1016/j.jff.2017.01.009. [DOI] [Google Scholar]
- 18.Lee J.Y., Kang C.-H. Probiotics alleviate oxidative stress in H2O2-exposed hepatocytes and t-BHP-induced C57BL/6 mice. Microorganisms. 2022;10:234. doi: 10.3390/microorganisms10020234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee J.Y., Kim H., Jeong Y., Kang C.-H. Lactic Acid Bacteria Exert a Hepatoprotective Effect against Ethanol-Induced Liver Injury in HepG2 Cells. Microorganisms. 2021;9:1844. doi: 10.3390/microorganisms9091844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Silveira J.E.P.S., Pedroso D.M.M. UV light and skin aging. Rev. Environ. Health. 2014;29:243–254. doi: 10.1515/reveh-2014-0058. [DOI] [PubMed] [Google Scholar]
- 21.Hachiya A., Sriwiriyanont P., Fujimura T., Ohuchi A., Kitahara T., Takema Y., Kitzmiller W.J., Visscher M.O., Tsuboi R., Boissy R.E. Mechanistic Effects of Long-Term Ultraviolet B Irradiation Induce Epidermal and Dermal Changes in Human Skin Xenografts. Am. J. Pathol. 2009;174:401–413. doi: 10.2353/ajpath.2009.070500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ra J., Lee D.E., Kim S.H., Jeong J.-W., Ku H.K., Kim T.-Y., Choi I.-D., Jeung W., Sim J.-H., Ahn Y.-T. Effect of Oral Administration of Lactobacillus plantarum HY7714 on Epidermal Hydration in Ultraviolet B-Irradiated Hairless Mice. J. Microbiol. Biotechnol. 2014;24:1736–1743. doi: 10.4014/jmb.1408.08023. [DOI] [PubMed] [Google Scholar]
- 23.Kim H.M., Lee D.E., Park S.D., Kim Y.-T., Kim Y.J., Jeong J.W., Jang S.S., Ahn Y.-T., Sim J.-H., Huh C.-S., et al. Oral Administration of Lactobacillus plantarum HY7714 Protects Hairless Mouse Against Ultraviolet B-Induced Photoaging. J. Microbiol. Biotechnol. 2014;24:1583–1591. doi: 10.4014/jmb.1406.06038. [DOI] [PubMed] [Google Scholar]
- 24.Lee D.E., Huh C.-S., Ra J., Choi I.-D., Jeong J.-W., Kim S.-H., Ryu J.H., Seo Y.K., Koh J.S., Lee J.-H., et al. Clinical Evidence of Effects of Lactobacillus plantarum HY7714 on Skin Aging: A Randomized, Double Blind, Placebo-Controlled Study. J. Microbiol. Biotechnol. 2015;25:2160–2168. doi: 10.4014/jmb.1509.09021. [DOI] [PubMed] [Google Scholar]
- 25.Satoh T., Murata M., Iwabuchi N., Odamaki T., Wakabayashi H., Yamauchi K., Abe F., Xiao J. Effect of Bifidobacterium breve B-3 on skin photoaging induced by chronic UV irradiation in mice. Benef. Microbes. 2015;6:497–504. doi: 10.3920/BM2014.0134. [DOI] [PubMed] [Google Scholar]
- 26.Kim D., Lee K.R., Kim N.R., Park S.-J., Lee M., Kim O.-K. Combination of Bifidobacterium longum and Galacto-Oligosaccharide Protects the Skin from Photoaging. J. Med. Food. 2021;24:606–616. doi: 10.1089/jmf.2021.K.0032. [DOI] [PubMed] [Google Scholar]
- 27.Peres P., Terra V., Guarnier F., Cecchini R., Cecchini A. Photoaging and chronological aging profile: Understanding oxidation of the skin. J. Photochem. Photobiol. B Biol. 2011;103:93–97. doi: 10.1016/j.jphotobiol.2011.01.019. [DOI] [PubMed] [Google Scholar]
- 28.Lee H., Hong Y., Kim M. Structural and Functional Changes and Possible Molecular Mechanisms in Aged Skin. Int. J. Mol. Sci. 2021;22:12489. doi: 10.3390/ijms222212489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jo K., Bae G.Y., Cho K., Park S.S., Suh H.J., Hong K.-B. An Anthocyanin-Enriched Extract from Vaccinium uliginosum Improves Signs of Skin Aging in UVB-Induced Photodamage. Antioxidants. 2020;9:844. doi: 10.3390/antiox9090844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nilforoushzadeh M.A., Ashtiani H.R.A., Jaffary F., Jahangiri F., Nikkhah N., Mahmoudbeyk M., Fard M., Ansari Z., Zare S. Dermal Fibroblast Cells: Biology and Function in Skin Regeneration. J. Ski. Stem Cell. 2017;4:e69080. doi: 10.5812/jssc.69080. [DOI] [Google Scholar]
- 31.Kang M.C., Yumnam S., Kim S.Y. Oral Intake of Collagen Peptide Attenuates Ultraviolet B Irradiation-Induced Skin Dehydration In Vivo by Regulating Hyaluronic Acid Synthesis. Int. J. Mol. Sci. 2018;19:3551. doi: 10.3390/ijms19113551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Oba C., Ohara H., Morifuji M., Ito K., Ichikawa S., Kawahata K., Koga J. Collagen hydrolysate intake improves the loss of epidermal barrier function and skin elasticity induced by UVB irradiation in hairless mice. Photodermatol. Photoimmunol. Photomed. 2013;29:204–211. doi: 10.1111/phpp.12051. [DOI] [PubMed] [Google Scholar]
- 33.Edwards C., Pearse A., Marks R., Nishimori Y., Matsumoto K., Kawai M. Degenerative Alterations of Dermal Collagen Fiber Bundles in Photodamaged Human Skin and UV-Irradiated Hairless Mouse Skin: Possible Effect on Decreasing Skin Mechanical Properties and Appearance of Wrinkles. J. Investig. Dermatol. 2001;117:1458–1463. doi: 10.1038/jid.2001.2. [DOI] [PubMed] [Google Scholar]
- 34.Hideaki N. Matrix metalloproteinases. J. Biol. Chem. 1999;274:21491–21494. doi: 10.1074/jbc.274.31.21491. [DOI] [PubMed] [Google Scholar]
- 35.Brenneisen P., Sies H., Scharffetter-Kochanek K. Ultraviolet-B irradiation and matrix metalloproteinases: From induction via signaling to initial events. Ann. N. Y. Acad. Sci. 2002;973:31–43. doi: 10.1111/j.1749-6632.2002.tb04602.x. [DOI] [PubMed] [Google Scholar]
- 36.Pittayapruek P., Meephansan J., Prapapan O., Komine M., Ohtsuki M. Role of Matrix Metalloproteinases in Photoaging and Photocarcinogenesis. Int. J. Mol. Sci. 2016;17:868. doi: 10.3390/ijms17060868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chiang H.-M., Chen H.-C., Chiu H.-H., Chen C.-W., Wang S.-M., Wen K.-C. Neonauclea reticulata(Havil.) Merr Stimulates Skin Regeneration after UVB Exposure via ROS Scavenging and Modulation of the MAPK/MMPs/Collagen Pathway. Evid.-Based Complement. Altern. Med. 2013;2013:1–9. doi: 10.1155/2013/324864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Capece D., Verzella D., Flati I., Arboretto P., Cornice J., Franzoso G. NF-κB: Blending metabolism, immunity, and inflammation. Trends Immunol. 2022;43:757–775. doi: 10.1016/j.it.2022.07.004. [DOI] [PubMed] [Google Scholar]
- 39.Wang Y., Wang L., Wen X., Hao D., Zhang N., He G., Jiang X. NF-κB signaling in skin aging. Mech. Ageing Dev. 2019;184:111160. doi: 10.1016/j.mad.2019.111160. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Not applicable.