Abstract
Introduction:
Ankle fractures are a common orthopaedic injury that often require surgical fixation. Because the comorbid population in the United States continues to survive longer, it has become routine to treat comorbid patients with unstable ankle fractures. The literature has identified comorbidities known to increase the risk of ankle fracture complications to include age 55 years or older, body mass index >29.9, polytrauma, open fractures, diabetes mellitus, smoking, peripheral neuropathy, and alcohol use.
Methods:
We retrospectively reviewed 37 patients who received retrograde intramedullary screw fixation of the distal fibula, all of whom had preexisting conditions known to increase the rate of postoperative complications.
Results:
Thirty-seven patients were included in this study, of whom 36 (97.3%) went on to union. Six of 37 patients (16.2%) had complications although only one (2.7%) was due to inadequate fixation. The average time to weight-bearing as tolerated was 57.2 days (15–115 days). Two patients (5.4%) had symptomatic instrumentation requiring removal after union. Two patients (5.4%) had delayed union of the distal fibula, which responded to the use of a bone stimulator. One patient (2.7%) developed a nonunion which led to chronic subluxation of the ankle joint. One patient (2.7%) had a minor medial ankle wound complication that was treated with oral antibiotics and local wound care.
Conclusions:
Retrograde intramedullary screw fixation of the distal fibula is a viable alternative to plate and screw fixation in patients with unstable ankle fractures who have known risk factors for increased complications. However, not all distal fibula fractures are amenable to this fixation method.
Level of Evidence:
Level III retrospective cohort study.
Keywords: ankle fracture, symptomatic instrumentation, nonunion, infection, fibular fixation, retrograde fibular screw, retrograde
1. Introduction
Distal fibula fractures are a common orthopaedic injury occurring in conjunction with distal tibia pilon fractures (AO 4F3) or as a part of malleolar injuries (AO 44).[1] While retrograde intramedullary nail and screw fixation methods have been explored historically, current gold standard fixation includes open reduction internal fixation (ORIF) with plate osteosynthesis in either a lateral or posterolateral position.[2–7] However, owing to the subcutaneous nature of the distal fibula, wound healing[8,9] and symptomatic implants[6,9] are known risks for patients treated with ORIF. Plate fixation may not be ideal in patients at risk for soft tissue compromise and, when performed in patients with risk factors, can have devastating results.[11,12] Identified risk factors include open/high-energy fractures, patients with diabetes, patients with peripheral neuropathy, patients with a body mass index (BMI) of ≥30, patients who smoke, and elderly patients.[6,8–17] There has been renewed interest in investigating alternative methods of fixation for distal fibula fractures in patients prone to postoperative complications.
The main purpose of this study was to assess the rates of union and complications in at-risk patients with distal fibula fractures. The secondary aim was to describe the technique for a method of fixation which minimizes soft tissue damage. We hypothesize that a minimally invasive approach to lateral malleolar fracture fixation will result in reduced complications, in those with risk factors, as compared with the rates documented in the literature for ORIF, while still leading to acceptable union rates of the fibular fracture.
2. Methods
After Institutional Review Board approval, we retrospectively reviewed all cases related to distal fibular fixation performed by 2 trauma fellowship-trained orthopaedic surgeons at a level 1 trauma center over a 5-year period (2012–2017). Current Procedural Terminology codes were used to identify 586 patients who underwent distal fibula fixation. Medical records and radiographs for these patients were reviewed to identify all cases where retrograde intramedullary screw fixation (RIMSF) was used for lateral malleolus fractures as part of a malleolar injury or in conjunction with a distal tibia pilon fracture. For consistency, the fractures were classified by a single fellowship-trained trauma surgeon using the Arbeitsgemeinschaft für Osteosynthesefragen/Orthopaedic Trauma Association (AO/OTA) classification system.[1] Inclusion criteria consisted of patients aged 18 years or older having sustained a lateral malleolus fracture repaired with RIMSF in the setting of an AO 43 or AO 44 fracture.[1] Only patients with compromised soft tissue envelope at the ankle, and/or poor biology, received RIMSF for their lateral malleolus fracture. Thus, our series represents those patients at the highest risk for wound complications after open reduction internal fixation (ORIF) of their lateral malleolus.
All but 4 patients in our series had 2 or more known risk factors for wound complications after ankle ORIF. The risk factors considered include age 55 years or older; BMI of ≥30; open fractures/polytrauma as defined by an ipsilateral or contralateral lower-extremity fracture, pelvic or acetabular fracture, or any upper-extremity fracture; active smoker; diabetes mellitus; peripheral neuropathy; and alcohol abuse because these demographics have been proven to increase the risk of wound complications in the literature.[8,9,18–21] The 4 patients in the series with only one risk factor demonstrated such a compromised soft tissue envelope, either from the initial trauma or the need for simultaneous surgical approaches, that the senior authors elected to forgo an open incision because the risk of wound compromise was too high. All patients with lateral malleolar fractures and 2 or more of the above-listed risk factors were treated with RIMSF.
Distal fibular shaft fractures that originate above the level of the syndesmosis[4] with an intact syndesmosis were excluded. Syndesmotic stability was evaluated intraoperatively with either a cotton test or external rotation stress test on fluoroscopic AP and mortise projections.[22] Other exclusion criteria include the absence of risk factors in those treated with RIMSF, use of a plate and screw fixation, and nonoperative management. Forty-eight patients with RIMSF of the distal fibula were identified. Three patients were excluded because of distal fibular fracture originating above the syndesmosis without involving the mortise nor syndesmosis, and 8 patients were excluded for follow-up less than 30 days, resulting in 37 patients treated with RIMSF. Successful treatment was based on painless weight-bearing at final follow-up evaluation.
2.1. Technique
The patient is positioned supine on a radiolucent table. A tourniquet is applied to the upper thigh but typically not inflated. Fluoroscopy is available intraoperatively and positioned on the contralateral side of the operating table. A 1-cm longitudinal incision is made, 1 cm distal to the tip of the fibula. A hemostat is used to spread through the subcutaneous tissue and probe the distal tip of the fibula. An indirect reduction is obtained by either pushing on the posterolateral aspect of the distal fibula or manipulating the foot. If needed, a small incision can be made at the fracture site, allowing direct manipulation of the fracture with a hemostat, bone reduction forceps, Kirschner wire, or freer. Optimal starting point is just anterior to the peroneal tubercle on lateral projection and lateral to the peroneal groove on the AP mortise (Fig. 1). This starting point can be adjusted according to the patient's inherent anatomy and intent of reduction. For example, in a supination–adduction injury pattern, starting slightly more medially on the AP mortise view will allow for lateral translation, thereby aiding in fracture reduction. A soft tissue protector and a 2.5 mm × 180 mm drill bit are used to establish the starting point, and the drill is oscillated across the reduced fracture. The drill bit is removed, and a 3.5 mm × 150 mm stainless steel cortical pelvic screw (DePuy Synthes, Paoli, PA) is advanced in a retrograde fashion into the distal fibula. A 150-mm screw is routinely used as the length of the cortical screw allows for it to contour readily to the diaphysis of the fibula without fracture displacement expected with a shorter, more rigid screw. Postoperative management is often dictated by the fracture classification and associated injuries in the case of a polytrauma. A stress examination of the syndesmosis is performed once all malleolar fixation is secured. If indicated, syndesmotic screw(s) may be placed anterior to the fibular screw through the incisura (Fig. 2). Incisions are irrigated and closed with suture and the ankle dressed in a well-padded trilaminar splint for 2 weeks. Instructions are given including strict elevation above heart level. The splint is removed at the 2-week postoperative visit, soft dressing placed, and physical therapy for range of motion and proprioception initiated. Non–weight-bearing precautions are instituted based on the associated injuries and patient comorbidities.
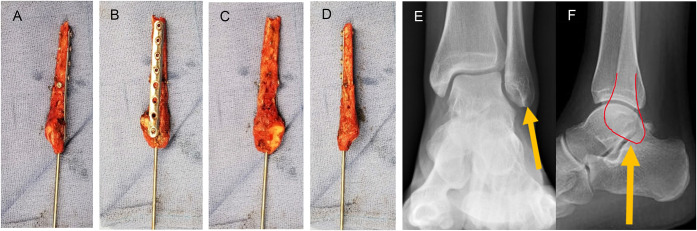
Figure 1.
Gross image of resected distal fibula in a patient with significant wound dehiscence and infection due to lateral fibular plating. Anterior (A), lateral (B), medial (C), and posterior (D) views of the distal fibula demonstrating the ideal starting point for retrograde intramedullary screw fixation (Kirschner wire). E and F, Anterior-posterior/lateral radiographs demonstrating the starting point for RIMSF. RIMSF, retrograde intramedullary screw fixation.
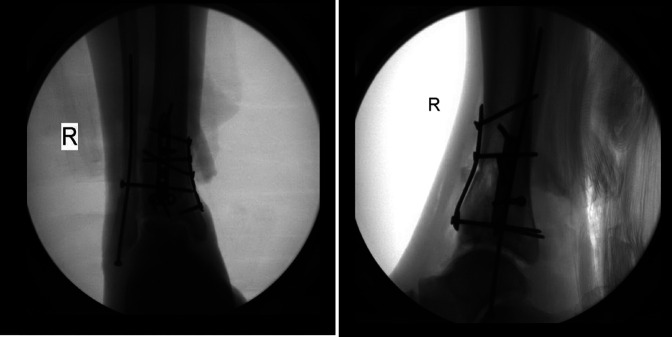
Figure 2.
Anterior-posterior and lateral radiographs demonstrating syndesmotic screw placement in the setting of retrograde intramedullary fibular screw fixation.
3. Results
Thirty-seven patients met our inclusion criteria with an average age of 60 (16–94) years and an average follow-up time of 9.7 months. Twenty patients were female and 17 were male. The most common mechanism of injury was a fall from standing height (51.4%), followed by motor vehicle collision (21.6%), fall from 1 to 4 steps (10.8%), crush injury (5.4%), and 1 patient for each of the following: motorcycle collision, fall off a ladder, fall off a trampoline, and a pedestrian struck. The cohort was categorized into 7 types of ankle fractures using the AO classification system: 4F3 fibular fractures involving the mortise (56.8%), 44A3 (2.7%), 44B (35.1%), and 44C (5.4%). The 4F3 fractures are nonmalleolar fractures and were associated with tibia fractures as follows: 42B (2.7%), 43A (16.2%), 43B (18.9%), and 43C (18.9%).[1] Of the 37 patients, 11 (29.7%) had an associated ankle dislocation, 8 (21.6%) had an open fracture, and 5 (13.5%) had an associated syndesmotic injury. Patients' average time to weight-bearing as tolerated was 57.2 days (15–115 days).
Thirty-six of the 37 patients went on to union (97.3%). Thirty-two patients (86.5%) had at least 2 risk factors; 12 patients (32.4%) had 3 or more risk factors (Fig. 3). Of the risk factors seen in our patient population, age older than 55 years was the most prevalent risk factor (67.6%) closely followed by an elevated BMI (54%). The average patient BMI was 30.3 (18.9–43.8). Eight patients (21.6%) were actively smoking tobacco at the time of injury, and an additional 11 patients (29.7%) reported a history of prior tobacco use (Table 1).
Figure 3.
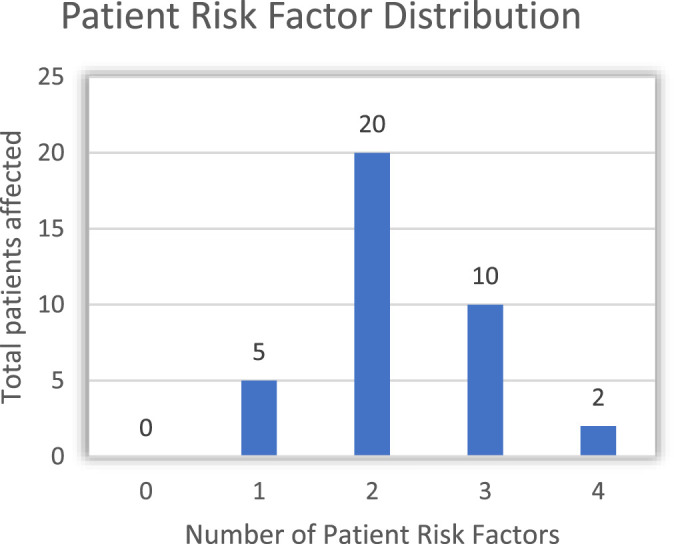
Distribution of patients with associated number of risk factors for wound-healing complications as described in the literature.
TABLE 1.
Risk Factors for 37 Patients Resulting in Increased Wound-Healing Complications.
| Patient Risk Factor Distribution | |
|---|---|
| Risk Factor | Number of Patients |
| Age 55 years or older | 25 |
| BMI >29.9 | 20 |
| Polytrauma/open fracture | 17 |
| Diabetes mellitus | 10 |
| Smoker | 8 |
| Peripheral neuropathy | 2 |
| Alcohol abuse | 1 |
A total of 6 complications were observed (15.8%). Two patients had superficial infections (5.4%); however, one was related to an external fixator pin site and the other sustained a lower leg wound unrelated to the fibula fracture. Of the 36 patients healed, 2 developed a delayed union of the fibula which responded to the use of a bone stimulator. Another patient sustained an open AO 43-C3 distal tibia pilon fracture with associated AO 4F3 distal fibula fracture, progressing to severe post-traumatic tibiotalar arthritis necessitating tibiotalocalcaneal fusion once the fractures healed.
4. Discussion
Ankle fractures are common orthopaedic injuries, consisting of 9% of all fractures.[23,24] Operative fixation is indicated when there is widening of the mortise, widening of the syndesmosis, or open fracture. The standard fibular repair includes ORIF with a plate and screw construct through either a lateral or posterolateral position.[3,4,6,7] Wound healing complications have been well documented in the literature for these approaches. Miller et al[9] retrospectively reviewed 478 patients with select risk factors who underwent ORIF of ankle fractures and found complication rates up to 40%. Interestingly, the patients had an average BMI of 29 and an average age of 43 years, both of which fall below the threshold to be considered risks for wound-healing complications, as described in the literature.[11,16] In patients with identified risk factors for wound-healing complications, the soft tissue envelop is fragile and the treating surgeon must proceed with extreme caution. Thus, in an attempt to preserve the soft tissue envelope, while providing adequate fibular fixation, alternative methods have been developed.
Over the past 2 decades, several alternative fixation methods consisting of intramedullary devices including Rush rods, Knowles pins, a variety of retrograde fibular nails, and retrograde fibular screws have been explored.[25–31] Recent literature has seen a resurgence in these devices, but none have gained significant popularity. A minimally invasive plate osteosynthesis distal fibular fixation technique was described with the goal of minimizing periosteal devascularization while providing adequate ankle stability.[32] Despite the limited dissection, the reported complication rate was 15% and the authors recommended against the routine use of this technique because of its technical difficulty.[32]
In 1994, Ray et al[33] investigated an alternative to plate and screw osteosynthesis by using intramedullary screw fixation with cortical screws. They used 2.5-inch and 4-inch screws for Weber B and Weber C type fractures with a 95.5% union rate in isolated ankle fracture.[33] This method of fixation was revisited over 2 decades later when Smith et al[34] treated 23 patients with retrograde cortical screw fixation. Twenty-six percent of their patients had no risk factors, 35% had 1 risk factor, and 26% had 2 risk factors for wound-healing complications. They reported no deep or soft tissue infections, 1 loss of fixation (4%), and 1 symptomatic instrumentation requiring implant removal (4%).[34]
Comparatively, our study had a similarly low complication rate in patients with multiple risk factors for wound-healing complications. Despite all patients included in our study having at least 1 identifiable risk factor, 97.3% went on to union with the use of RIMSF. The incidence of fibular screw–related complications was only 15.8%, which were predominantly related to factors independent of the method of fibular fixation. Our findings are consistent with those documented in the literature[9,35]; however, our patient population had multiple risk factors predisposing them to wound-healing complications.
The lone patient whose complication was attributable to the RIMSF sustained an AO 44B2.1 distal fibular fracture and was treated solely with a retrograde intramedullary fibular screw. This patient had 4 documented risk factors for poor wound healing: uncontrolled diabetes mellitus, peripheral neuropathy, BMI of 37.4, and age older than 55 years. At the 9-month follow-up, the patient's imaging demonstrated failure of fracture healing necessitating a tibiotalocalcaneal fusion. We believe any malleolar injury involving an incompetent medial ligament as opposed to a medial malleolus fracture (44B2.1, 44B3.1, 44C1.1, 44C2.1, and 44C3.1) is particularly unstable, requiring adjunctive methods of fixation,[1] especially in at-risk patients. In these patients, concomitant placement of a percutaneous syndesmotic screw(s) and or an external fixator is imperative. The lack of medial ankle support places increased external rotation and eversion stresses on the retrograde fibular screw. After our collection period, we treated an 81-year-old female patient with an open AO 44C1.1 malleolar ankle fracture and 4 documented risk factors for poor wound healing: open fracture, associated dislocation, BMI of 39.76, and age older than 55 years (Fig. 4). In this patient, the fibular fracture was fixed with a RIMSF in addition to an external fixator for 8 weeks, and remained non–weight-bearing for 73 days. At the final follow-up, this patient had radiographic healing and was weight-bearing without pain, indicating fracture union and successful treatment.
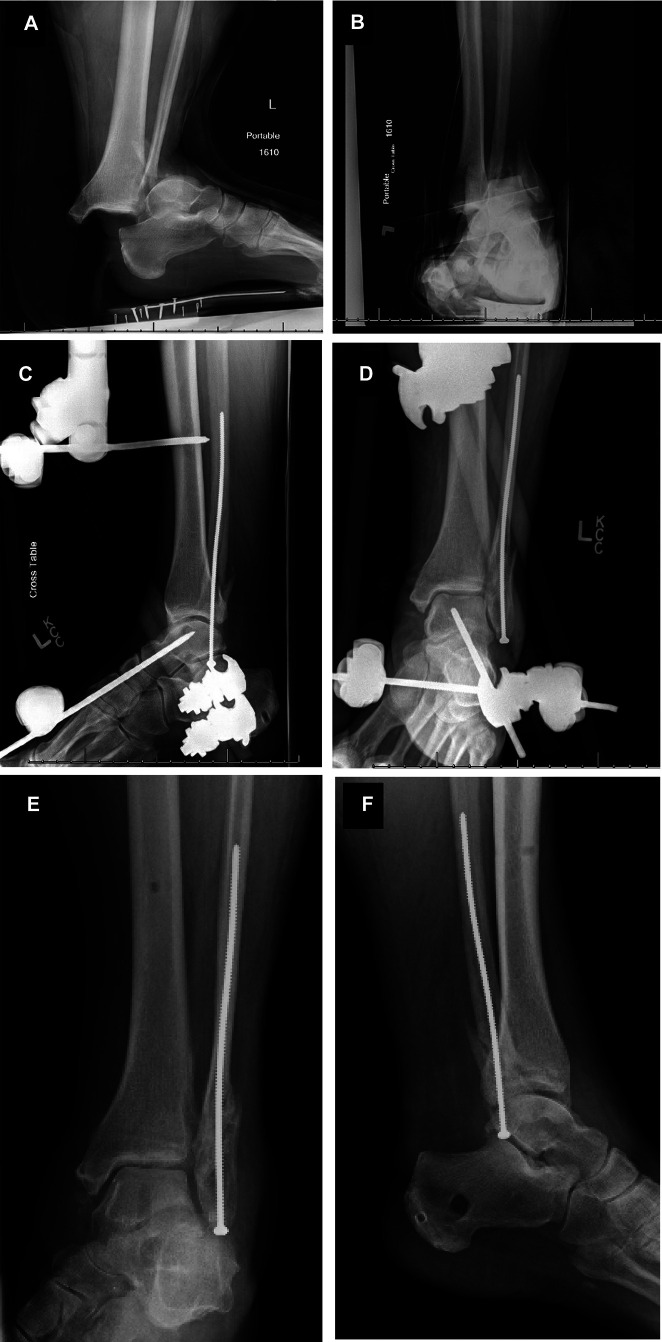
Figure 4.
A–D, Patient with polytrauma treated with retrograde intramedullary screw fixation of the AO 44B2.1 fibular fracture and external fixator. E and F, Final follow-up images demonstrate adequate callus formation.
There are several limitations to this study. By design, this is a retrospective case series and would benefit from prospective comparative studies in the future. However, our intention is simply to report the healing and complication rates of ankle fractures in a complicated population of ankle fractures using a less-invasive method of distal fibular fixation. This study is meant to offer an alternative to distal fibula plate and screw fixation in patients with identified risk factors, without the increased cost of an elaborate device. A prospective cohort evaluating outcomes in lateral malleolar fractures treated by plate and screw fixation in patients with no risk factors compared with retrograde intramedullary distal fibula screw fixation in patients with risk factors would be the next step. Second, our average time to weight-bearing as tolerated was not uniform. The main reason for this discrepancy was the difference in the patients' associated injuries, which dictated their postoperative management. The other factor that contributed to the variation was patient compliance. Interestingly, even with noncompliant patients, only 1 patient was recommended a subsequent, nonelective surgery due to fibular fixation. Third, final radiographs were not available on 11 patients. These 11 patients did not have any complications requiring repeat surgical intervention. They had a mean follow-up of 4.18 months.[1–8] Finally, we did not evaluate noncompliance as a risk factor despite the evidence that it is associated with wound complications.[9] Owing to the retrospective nature of our report, this was inconsistently documented.
The purpose of this study was not to state that retrograde intramedullary fibular fixation is a superior construct but to present this method of fixation as a viable alternative in patients who are at increased risk for wound-healing complications due to comorbidities.
5. Conclusion
Fixation of the distal fibula with a percutaneous retrograde intramedullary screw is a good alternative to plate osteosynthesis in patients with known risk factors for wound complications, such as open/high-energy injuries, diabetes mellitus, peripheral neuropathy, elevated BMI, smokers, and elderly patients. Patients with unstable lateral malleolus fractures, or fractures with syndesmotic disruption, should be additionally treated with either a syndesmotic screw and cast immobilization or an external fixator, if soft tissues are compromised, to ensure adequate stability.
Footnotes
The authors report no conflicts of interest.
Contributor Information
Megan L. Jimenez, Email: megan.jimenez@emoryhealthcare.org.
Benjamin J. Brill, Email: BenjaminJBrill@gmail.com.
Michael J. Principe, Email: mprincipe@delortho.com.
Nicholas F. Quercetti, III, Email: nquercetti@delortho.com.
References
- 1.Meinberg EG, Agel J, Roberts CS, et al. Fracture and dislocation classification compendium—2018. J Orthop Trauma. 2018;32(suppl 1):S1–S170. [DOI] [PubMed] [Google Scholar]
- 2.Asloum Y, Bedin B, Roger T, et al. Internal fixation of the fibula in ankle fractures: a prospective, randomized and comparative study: plating versus nailing. Orthop Traumatol Surg Res. 2014;100(4 suppl):S255–S259. [DOI] [PubMed] [Google Scholar]
- 3.Ostrum RF. Posterior plating of displaced Weber B fibula fractures. J Orthop Trauma. 1996;10:199–203. [DOI] [PubMed] [Google Scholar]
- 4.Weber B. Die Verletzungen des oberen Sprunggelenkes. Bern, Switzerland: Huber; 1966. [Google Scholar]
- 5.Weber M, Krause F. Peroneal tendon lesions caused by antiglide plates used for fixation of lateral malleolar fractures: the effect of plate and screw position. Foot Ankle Int. 2005;26:281–285. [DOI] [PubMed] [Google Scholar]
- 6.Winkler B, Weber BG, Simpson LA. The dorsal antiglide plate in the treatment of Danis-Weber type-B fractures of the distal fibula. Clin Orthop Relat Res. 1990;259:204–209. [PubMed] [Google Scholar]
- 7.Tsukada S, Otsuji M, Shiozaki A, et al. Locking versus non-locking neutralization plates for treatment of lateral malleolar fractures: a randomized controlled trial. Int Orthop. 2013;37:2451–2456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Höiness P, Engebretsen L, Strömsöe K. Soft tissue problems in ankle fractures treated surgically. A prospective study of 154 consecutive closed ankle fractures. Injury. 2003;34:928–931. [DOI] [PubMed] [Google Scholar]
- 9.Miller AG, Margules A, Raikin SM. Risk factors for wound complications after ankle fracture surgery. J Bone Joint Surg Am. 2012;94:2047–2052. [DOI] [PubMed] [Google Scholar]
- 10.Mitchell JJ, Bailey JR, Bozzio AE, et al. Fixation of distal fibula fractures: an update. Foot Ankle Int. 2014;35:1367–1375. [DOI] [PubMed] [Google Scholar]
- 11.Dodson NB, Ross AJ, Mendicino RW, et al. Factors affecting healing of ankle fractures. J Foot Ankle Surg. 2013;52:2–5. [DOI] [PubMed] [Google Scholar]
- 12.Williams BR, McCreary DL, Chau M, et al. Functional outcomes of symptomatic implant removal following ankle fracture open reduction and internal fixation. Foot Ankle Int. 2018;39:674–680. [DOI] [PubMed] [Google Scholar]
- 13.Anderson SA, Li X, Franklin P, Wixted JJ. Ankle fractures in the elderly: initial and long-term outcomes. Foot Ankle Int. 2008;29:1184–1188. [DOI] [PubMed] [Google Scholar]
- 14.Flynn JM, Rodriguez-del Rio F, Piza PA. Closed ankle fractures in the diabetic patient. Foot Ankle Int. 2000;21:311–319. [DOI] [PubMed] [Google Scholar]
- 15.Kim JH, Patel S. Is it worth discriminating against patients who smoke? A systematic literature review on the effects of tobacco use in foot and ankle surgery. J Foot Ankle Surg. 2017;56:594–599. [DOI] [PubMed] [Google Scholar]
- 16.Lanzetti RM, Luparielly D, Venditto T, et al. The role of diabetes mellitus and BMI in the surgical treatment of ankle fractures. Diabetes Metab Res Rev. 2018:34e2954. [DOI] [PubMed] [Google Scholar]
- 17.Lynde MJ, Sautter T, Hamilton GA, Schuberth JM. Complications after open reduction and internal fixation of ankle fractures in the elderly. Foot Ankle Surg. 2012;18:103–107. [DOI] [PubMed] [Google Scholar]
- 18.Cavo MJ, Fox JP, Markert R, Laughlin RT. Association between diabetes, obesity, and short-term outcomes among patients surgically treated for ankle fracture. J Bone Joint Surg Am. 2015;97:987–994. [DOI] [PubMed] [Google Scholar]
- 19.Ovaska MT, Mäkinen TJ, Madanat R, et al. Risk factors for deep surgical site infection following operative treatment of ankle fractures. J Bone Joint Surg Am. 2013;95:348–353. [DOI] [PubMed] [Google Scholar]
- 20.Ovaska M. Complications in ankle fracture surgery. Acta Orthop Suppl. 2015;86:1–32. [DOI] [PubMed] [Google Scholar]
- 21.Sun Y, Wang H, Tang Y, et al. Incidence and risk factors for surgical site infection after open reduction and internal fixation of ankle fracture: a retrospective multicenter study. Med Baltim. 2018;97:e9901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Summers HD, Sinclair MK, Stover MD. A reliable method for intraoperative evaluation of syndesmotic reduction. J Orthop Trauma. 2013;27:196–200. [DOI] [PubMed] [Google Scholar]
- 23.Court-Brown CM, McBirnie J, Wilson G. Adult ankle fractures—an increasing problem? Acta Orthop Scand. 1998;69:43–47. [DOI] [PubMed] [Google Scholar]
- 24.Koval KJ, Lurie J, Zhou W, et al. Ankle fractures in the elderly: what you get depends on where you live and who you see. J Orthop Trauma. 2005;19:635–639. [DOI] [PubMed] [Google Scholar]
- 25.Rehman H, Gardner WT, Rankin I, Johnstone AJ. The implants used for intramedullary fixation of distal fibula fractures: a review of literature. Int J Surg. 2018;56:294–300. [DOI] [PubMed] [Google Scholar]
- 26.Bugler KE, Watson CD, Hardie AR, et al. The treatment of unstable fractures of the ankle using the Acumed fibular nail: development of a technique. J Bone Joint Surg Br. 2012;94:1107–1112. [DOI] [PubMed] [Google Scholar]
- 27.Jain S, Haughton BA, Brew C. Intramedullary fixation of distal fibular fractures: a systematic review of clinical and functional outcomes. J Orthop Traumatol. 2014;15:245–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lee YS, Hsu TL, Huang CR, et al. Lateral fixation of AO type-B2 ankle fractures: the Acutrak plus compression screw technique. Int Orthop. 2010;34:903–907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Switaj PJ, Fuchs D, Alshouli M, et al. A biomechanical comparison study of a modern fibular nail and distal fibular locking plate in AO/OTA 44C2 ankle fractures. J Orthop Surg Res. 2016;11:100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Walton DM, Adams SB, Parekh SG. Intramedullary fixation for fractures of the distal fibula. Foot Ankle Int. 2016;37:115–123. [DOI] [PubMed] [Google Scholar]
- 31.Loukachov VV, Birnie MFN, Dingemans SA, et al. Percutaneous intramedullary screw fixation of distal fibula fractures: a case series and systematic review. J Foot Ankle Surg. 2017;56:1081–1086. [DOI] [PubMed] [Google Scholar]
- 32.Hess F, Sommer C. Minimally invasive plate osteosynthesis of the distal fibula with locking compression plate: first experience of 20 cases. J Orthop Trauma. 2011;25:110–115. [DOI] [PubMed] [Google Scholar]
- 33.Ray TD, Nimityongskul P, Anderson LD. Percutaneous intramedullary fixation of lateral malleolus fractures: technique and report of early results. J Trauma. 1994;36:669–675. [DOI] [PubMed] [Google Scholar]
- 34.Smith M, Medlock G, Johnstone AJ. Percutaneous screw fixation of unstable ankle fractures in patients with poor soft tissues and significant co-morbidities. Foot Ankle Surg. 2017;23:16–20. [DOI] [PubMed] [Google Scholar]
- 35.Velleman J, Nijs S, Hoekstra H. Operative management of AO type 44 ankle fractures: determinants of outcome. J Foot Ankle Surg. 2018;57:247–253. [DOI] [PubMed] [Google Scholar]