Abstract
Background:
Recent evidence suggests that sexual minority (e.g., gay/lesbian, bisexual) adults might be at increased risk of hypertension compared to heterosexual adults. However, disparities by sexual identity in anti-hypertensive medication use among adults with hypertension have not been comprehensively examined.
Methods:
We analyzed data from the Behavioral Risk Factor Surveillance System (2015-2019), to examine sexual identity differences in the prevalence of hypertension and anti-hypertensive medication use among adults. We ran sex-stratified logistic regression models to estimate the odds ratios of diagnosis of hypertension and anti-hypertensive medication use among sexual minority (i.e., gay/lesbian, bisexual, and “other”) and heterosexual adults (reference group).
Results:
The sample included 420,340 participants with a mean age of 49.7 (±17.0) years, of which 66.7% were Non-Hispanic White. Compared to heterosexual participants of the same sex, bisexual women (AOR 1.19, 95% CI = 1.03-1.37) and gay men (AOR 1.18, 95% CI = 1.03-1.35) were more likely to report having been diagnosed with hypertension. Among women with diagnosed hypertension, bisexual women had lower odds of current anti-hypertensive medication use (AOR 0.71, 95% CI = 0.56-0.90). Among men with diagnosed hypertension, gay men were more likely than heterosexual men to report current anti-hypertensive medication use (AOR 1.39, 95% CI = 1.10-1.78). Compared to heterosexual participants of the same sex, there were no differences in hypertension or anti-hypertensive medication use among lesbian women, bisexual men, and participants who reported their sexual identity as “other.”
Conclusion:
Clinical and public health interventions are needed to reduce the risk of hypertension among bisexual women and gay men. Bisexual women were at higher risk of untreated hypertension, which may be attributed to lower healthcare utilization due to fear of discrimination from healthcare providers and socioeconomic disadvantage. Future research is needed to better understand factors that may contribute to untreated hypertension among bisexual women with hypertension.
Keywords: healthcare disparities, hypertension, sexual minority
Introduction
Hypertension is the leading modifiable risk factor for cardiovascular disease.1 It is estimated that approximately 50% of American adults meet criteria for diagnosis of hypertension (blood pressure ≥130/80 mm Hg).2 Prior research has found that untreated and uncontrolled hypertension are associated with a greater risk of adverse outcomes (such as stroke and cardiovascular mortality) among adults with hypertension.3,4 Significant disparities in both hypertension prevalence and treatment have been identified among racial and ethnic minority adults in the United States (U.S.).2–4
A recent scientific statement by the American Heart Association found that little is known about sexual identity disparities in the prevalence and treatment of hypertension.5 In 2021, it was estimated that approximately 7% of the adult population in the U.S. identified as sexual minority individuals (such as lesbian, gay, bisexual, or other non-heterosexual identity).6 There is growing evidence that sexual minority adults experience a higher risk of hypertension than heterosexual adults.5,7,8 Multiple studies have found that sexual minority women have a higher prevalence of several risk factors for hypertension compared to heterosexual women, such as tobacco use, short sleep duration, and obesity.7,9–13 Sexual minority men also have a higher prevalence of tobacco use than heterosexual men.14–16 However, research on the prevalence of hypertension among sexual minority women is largely conflicting. Some studies have found no differences in the diagnosis of hypertension between sexual minority and heterosexual women and others report a significantly higher prevalence of hypertension among sexual minority women.7,10,17 Further, two analyses of data from the National Health and Nutrition Examination Survey (NHANES) found that bisexual men were twice as likely to meet criteria for diagnosis of hypertension compared to heterosexual men.18,19 Fewer differences in hypertension prevalence have been identified between gay and heterosexual men.8,18,19
Despite this evidence, there is limited research on hypertension treatment (such as the use of anti-hypertensive medications) among sexual minority adults and existing findings are generally mixed. In a meta-analysis of three studies, investigators found that bisexual men were 44% more likely to be taking anti-hypertensive medication than heterosexual men, but no differences were found between gay and heterosexual men.8 In addition, analyses of data from the NHANES found that bisexual men were more likely to use anti-hypertensive medication relative to heterosexual men (24.1% vs. 13.8%, p < 0.01).20 However, gay and heterosexual men did not differ in the prevalence of anti-hypertensive medication use.20 In contrast, using data from the California Health Interview Survey, Boehmer and colleagues21 found that gay men were approximately 40% more likely than heterosexual men to report current anti-hypertensive medication use. Fewer studies have found sexual identity differences in the use of anti-hypertensive medications among women.5
There are several factors that may place sexual minority adults at a higher risk of inadequate hypertension treatment. Analyses of population-based data have found that sexual minority adults in the U.S., particularly lesbian women, bisexual women, and bisexual men, were approximately twice as likely to live in poverty than heterosexual adults.22 Higher rates of poverty may limit opportunities to receive necessary medical treatments to adequately treat and control hypertension and other chronic conditions. In addition, multiple studies suggest that sexual minority adults in the U.S. may delay seeking needed healthcare services because of fear of discrimination from healthcare providers23–25 as well as concerns related to costs and other reasons, such as issues with transportation and scheduling.26–29 These factors may limit sexual minority adults’ ability to receive timely diagnosis and treatment for hypertension.
The purpose of the present study was to examine sexual identity differences in the prevalence and anti-hypertensive medication use among adults in the U.S. Based on prior work, we hypothesized that all groups of sexual minority adults (i.e., gay/lesbian, bisexual, and “other” sexual minority) would report a higher prevalence of hypertension than their heterosexual counterparts. We also hypothesized that, among adults with hypertension, anti-hypertensive medication use would be lower among sexual minority adults.
Methods
Sample
Data from the Behavioral Risk Factor Surveillance System (BRFSS) that were used in this study are publicly available through the Centers for Disease Control and Prevention website. Our program code for the present analysis is available through the Open Science Framework. The BRFSS is a national telephone survey that is conducted annually to assess the health of non-institutionalized American adults (ages 18 and over). The BRFSS uses random digit dialing techniques to collect self-reported health information from more than 400,000 individuals every year in all 50 states, the District of Columbia, and three U.S. territories. The present study used data from the 2015, 2017, and 2019 BRFSS as questions on hypertension diagnosis and treatment are only assessed every other year. The response rates for both landline and cellular phones across the included survey years of the BRFSS ranged from 44.5-49.4%. Response rates across BRFSS survey years are generally higher than other telephone surveys in the U.S.30–32 Information on BRFSS recruitment and data collection has been described elsewhere.33
In 2014, an optional sexual orientation and gender identity module was introduced to the BRFSS. The module was used by 22 states in 2015, 27 states in 2017, and 31 states in 2019. Figure 1 shows the steps that were taken to obtain the analytic sample. A total of 431,632 participants were asked about their sexual identity, of which 2,916 and 3,909 responded “don’t know” and “refused,” respectively. The weighted response rate for the sexual identity item across the included survey years was 98.5%. As shown in Supplemental Table 1, compared to participants with complete data for sexual identity, those who responded “don’t know” and “refused” were older, less likely to identify as Non-Hispanic White, had lower annual incomes, had lower educational attainment, were less likely to have healthcare insurance coverage, and were less likely to be lifetime smokers. No differences in hypertension or current anti-hypertensive medication use were found. Given that this analysis focused on sexual identity differences in the prevalence of hypertension and anti-hypertensive medication use among cisgender (i.e., individuals whose gender identity aligns with their sex assigned at birth) adults, we next excluded participants with missing data for the gender identity item (n = 1,635) as well as those who self-identified as gender minorities (i.e., transgender or gender non-binary; n = 1,636). Last, we excluded 1,196 participants with missing data for all other study variables.
Figure 1.
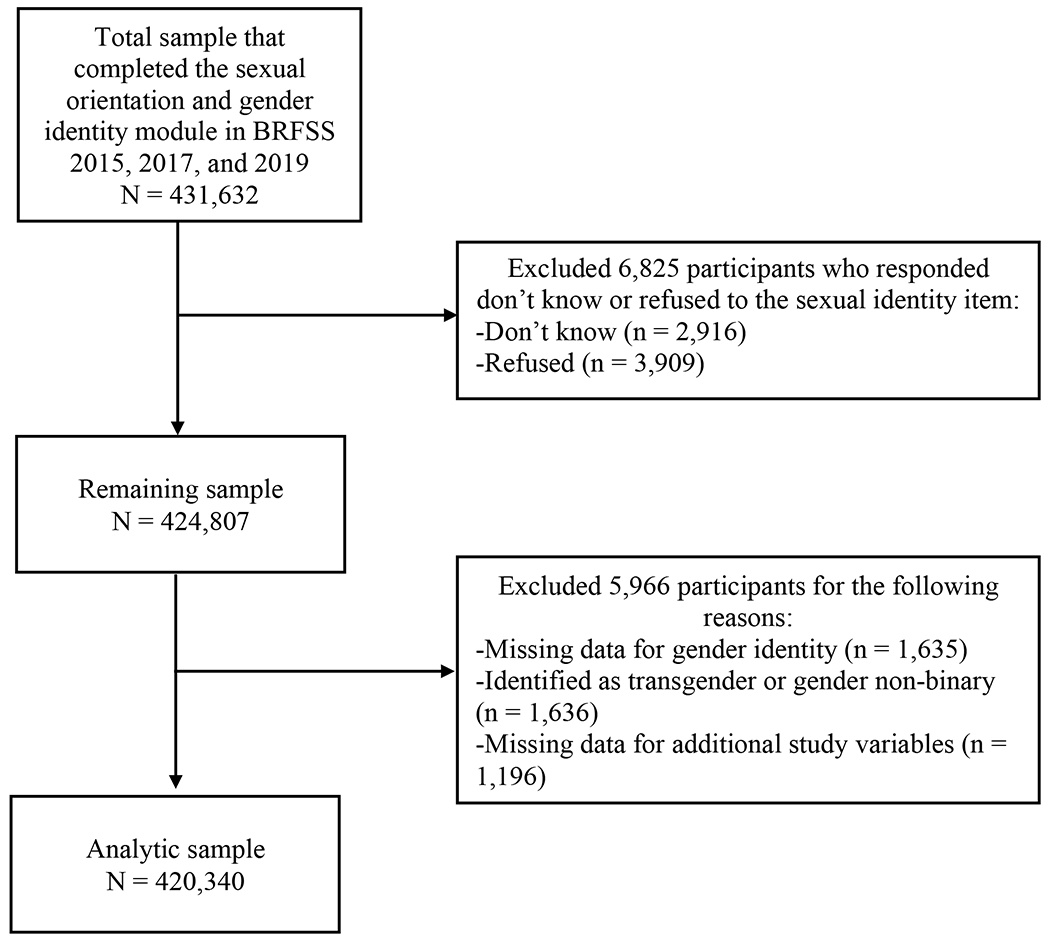
Flowchart of inclusion and exclusion criteria.
The present study included 420,340 cisgender sexual minority and heterosexual adults who reported they were not pregnant at the time the BRFSS interview was conducted. This study was deemed exempt by the Institutional Review Board at the Columbia University Irving Medical Center.
Measures
Sexual identity.
Sexual identity was assessed by asking participants, “Do you consider yourself to be: 1) straight; 2) gay or lesbian; 3) bisexual; or 4) other.” Participants were classified as heterosexual, gay/lesbian, bisexual, or “other” sexual minority and stratified by sex.
Demographic characteristics.
Age (18 years and over); race/ethnicity (Non-Hispanic White, Non-Hispanic Black, Hispanic, Non-Hispanic Asian/Pacific Islander, and Non-Hispanic other race); annual income (less than $15,000, $15,000-24,999, $25,000-34,999, $35,000-49,999, over $50,000); and educational attainment (did not graduate high school, graduated high school, attended college or technical college, graduated from college or technical college) were assessed.
Healthcare coverage and utilization.
To assess healthcare coverage, participants were asked, “Do you have any kind of health care coverage, including health insurance, prepaid plans such as HMOs, or government plans such as Medicare, or Indian Health Service?” (yes vs. no). We also assessed the length of time since participants’ last routine check-up. Participants were asked to indicate how long it had been since they last visited a doctor for a routine check-up. They were instructed to only report on visits for general physical exams, not an exam for a specific injury, illness, or condition. Response options were: “Within the past year,” “Within past 2 years,” “Within past 5 years,” and “5 or more years ago.”
Lifetime smoking.
Participants were asked, “Have you smoked at least 100 cigarettes in your entire life?” Those who responded “Yes” were categorized as lifetime smokers. Those who responded “No” were categorized as non-smokers.
Body mass index (BMI).
Participants were classified as underweight (BMI < 18.5 kg/m2), normal weight (BMI of 18.5 to < 24.9 kg/m2), overweight (BMI of 25.0 to < 30.0 kg/m2), or obese (BMI > 30.0 kg/m2) based on self-reported height and weight using established guidelines.34
Hypertension diagnosis and anti-hypertensive medication use.
To assess diagnosis of hypertension, participants were asked whether a doctor, nurse, or other health professional had ever told them that they had high blood pressure. Responses included: “Yes,” “Yes, but female told only during pregnancy,” “No,” and “Told borderline high or pre-hypertensive.” Those who reported they had borderline hypertension or pre-hypertension, and female participants who reported having gestational hypertension, were not categorized as having hypertension. Participants who reported they had been previously diagnosed with hypertension were then asked: “Are you currently taking medicine for your high blood pressure?” to assess anti-hypertensive medication use. Responses were dichotomized (yes vs. no).
Statistical Analyses
Analyses were conducted in Stata version 16 using survey weights (as recommended by the BRFSS)35 and the svy command to account for the complex survey design of the BRFSS. All analyses were stratified by sex. Heterosexual participants (the largest group) were the reference group for all analyses. For bivariate analyses, we used Student’s t-tests and the design-adjusted Rao-Scott X2 tests to examine differences between sexual minority (i.e., gay/lesbian, bisexual, and “other” sexual minority) participants and heterosexual participants of the same sex across continuous and categorical variables, respectively. We used a Bonferroni correction for bivariate analyses to account for multiple comparisons. Therefore, a two-sided p-value of < 0.001 was considered statistically significant.
Next, we used multiple logistic regression models to estimate the unadjusted odds ratios (OR) and adjusted OR (AOR) with 95% confidence intervals (CI) for the associations of sexual minority identity with hypertension diagnosis and anti-hypertensive medication use in separate models. Model 1 for both outcomes was unadjusted. Model 2 for both outcomes was adjusted for age, race/ethnicity, annual income, educational attainment, healthcare coverage, last routine check-up, lifetime smoking, and BMI status. Anti-hypertensive medication use was only assessed among participants who reported being diagnosed with hypertension.
Results
The sample included 420,340 participants. Fifty percent of the sample was female and 66.7% were Non-Hispanic White. The mean age was 49.7 years (+/−17.0). Approximately 35% of participants reported having been diagnosed with hypertension and 78% of those with a diagnosis of hypertension were currently taking anti-hypertensive medications.
Table 1 presents sexual identity differences across sample characteristics among women (n = 226,850). Overall, 95.2% of women identified as heterosexual, 1.3% identified as lesbian, 2.9% identified as bisexual, and 0.6% reported their sexual identity as “other.” Compared to heterosexual women, all groups of sexual minority women were younger. Bisexual and “other” sexual minority women were more likely than heterosexual women to have lower annual incomes, educational attainment, and healthcare insurance coverage (p < 0.001). In addition, lesbian and bisexual women were less likely to have had a routine check-up in the past year and to report a diagnosis of hypertension (p < 0.001), but more likely to be lifetime smokers relative to heterosexual women (p < 0.001). Bisexual women were also more likely than heterosexual women to meet criteria for obesity (40.6% vs. 32.2%, p < 0.001). Compared to heterosexual women with hypertension, bisexual women with hypertension were less likely to report current anti-hypertensive medication use (57.0% vs. 82.8%, p < 0.001).
Table 1.
Sexual identity differences in sample characteristics among women in the Behavioral Risk Factor Surveillance System (N=226,850).
| Total sample of women (N= 226,850) | Lesbian women (n = 2,820) | Bisexual women (n = 4,815) | “Other” sexual minority women (n = 1,355) | Heterosexual women (n = 217,860) | |
|---|---|---|---|---|---|
|
|
|||||
| Sample characteristics | Mean (SD)/Weighted % (95% CI) | ||||
| Age (range 18-80 years)*†‡ | 50.3 (17.0) | 44.9 (15.7) | 34.5 (12.3) | 47.8 (19.3) | 50.9 (16.9) |
| Race/ethnicity†‡ | |||||
| Non-Hispanic White | 66.4% (65.9-66.8) | 64.7% (60.7-68.6) | 61.2% (58.4-64.0) | 51.6% (46.3-56.9) | 66.6% (66.2-67.1) |
| Non-Hispanic Black | 13.4% (13.1-13.7) | 14.3% (11.6-17.5) | 13.5% (11.7-15.5) | 12.8% (10.0-16.3) | 13.4% (13.1-13.7) |
| Hispanic | 13.1% (12.7-13.5) | 13.0% (10.0-16.7) | 16.0% (13.6-18.8) | 23.9% (19.0-29.6) | 13.0% (12.6-13.4) |
| Non-Hispanic Asian/Pacific Islander | 4.6% (3.3-4.9) | 4.0% (2.3-6.8) | 4.2% (3.2-5.6) | 6.9% (4.5-10.4) | 4.6% (4.3-4.9) |
| Non-Hispanic Other race | 2.5% (2.4-2.6) | 4.0% (3.0-5.2) | 5.1% (4.2-6.1) | 4.8% (3.5-6.6) | 2.4% (2.3-2.5) |
| Annual income†‡ | |||||
| < $15,000 | 10.2% (9.9-10.5) | 11.3% (9.2-13.8) | 14.7% (12.9-16.8) | 19.7% (15.9-24.1) | 10.0% (9.7-10.3) |
| $15,000 - $24,999 | 16.8% (16.5-17.2) | 15.0% (12.6-17.7) | 23.3% (20.9-25.8) | 28.1% (23.2-33.7) | 16.6% (16.2-16.9) |
| $25,000 - $34,999 | 10.4% (10.2-10.7) | 12.9% (10.0-16.5) | 11.4% (9.9-13.2) | 13.0% (10.3-16.2) | 10.3% (10.1-10.7) |
| $35,000-$49,999 | 13.3% (12.9-13.6) | 12.5% (10.5-14.9) | 13.2% (11.515.1) | 9.6% (7.3-12.5) | 13.3% (13.0-13.6) |
| ≥ $50,000 | 49.3% (48.8-49.7) | 48.3% (44.6-51.9) | 37.4% (34.9-40.0) | 29.6% (25.1-34.6) | 49.8% (49.3-50.3) |
| Educational attainment*†‡ | |||||
| Did not graduate high school | 9.3% (9.0-9.6) | 7.3% (5.5-9.7) | 9.1% (7.4-11.3) | 26.9% (21.7-32.9) | 9.2% (8.9-9.6) |
| Graduated high school | 25.4% (24.0-25.8) | 22.6% (19.3-26.3) | 25.1% (22.7-27.6) | 29.7% (25.3-34.5) | 25.4% (25.1-25.9) |
| Attended college/technical school | 33.5% (33.1-34.0) | 30.9% (27.6-34.3) | 38.8% (36.1-41.5) | 24.2% (20.2-28.7) | 33.5% (33.0-33.9) |
| Graduated college/technical school | 31.8% (31.4-32.1) | 39.2% (35.8-42.7) | 27.0% (25.0-29.1) | 19.2% (16.2-22.7) | 31.9% (31.5-32.3) |
| Healthcare insurance coverage†‡ | 91.5% (91.2-91.8) | 92.4% (90.1-94.1) | 87.2% (84.9-89.2) | 79.5% (73.8-84.2) | 91.7% (91.4-92.0) |
| Last routine check-up *† | |||||
| Within past year | 78.9% (78.5-79.3) | 73.3% (69.9-76.4) | 68.2% (65.2-70.7) | 82.3% (78.2-85.7) | 79.3% (78.9-79.7) |
| Within past two years | 11.2% (10.9-11.4) | 14.1% (11.8-16.7) | 16.8% (14.6-19.2) | 8.5% (6.3-11.5) | 11.0% (10.7-11.3) |
| Within past five years | 5.8% (5.6-6.0) | 9.0% (6.9-11.6) | 9.5% (7.7-11.8) | 5.8% (3.7-8.9) | 5.6% (5.4-5.9) |
| Five or more years ago | 3.8% (3.7-4.0) | 3.5% (2.4-5.1) | 5.4% (4.3-6.7) | 2.9% (1.7-5.0) | 3.8% (3.6-4.0) |
| Never | 0.3% (0.2-0.4) | 0.2% (0.1-0.5) | 0.3% (0.2-0.7) | 0.5% (0.2-1.2) | 0.3% (0.2-0.4) |
| Lifetime smoker*†‡ | 37.4% (37.0-37.8) | 50.0% (46.3-53.6) | 46.8% (44.1-49.6) | 25.9% (22.1-30.0) | 37.0% (36.6-37.4) |
| Body mass index† | |||||
| Underweight | 2.1% (1.9-2.2) | 2.7% (1.5-4.8) | 3.0% (2.3-4.0) | 3.7% (1.7-7.5) | 2.0% (1.9-2.2) |
| Normal weight | 34.8% (34.3-35.3) | 32.8% (29.5-36.4) | 31.9% (29.5-34.3) | 28.5% (24.1-33.3) | 35.0% (34.6-35.5) |
| Overweight | 30.5% (30.1-31.0) | 26.6% (23.6-29.9) | 24.5% (22.2-27.0) | 31.4% (26.9-36.2) | 30.8% (30.4-31.2) |
| Obese | 32.6% (32.1-33.0) | 37.9% (34.4-41.5) | 40.6% (37.9-43.4) | 36.4% (31.4-41.9) | 32.2% (31.8-32.6) |
| Hypertension diagnosis*† | |||||
| Yes | 32.4% (32.0-32.8) | 26.9% (23.7-30.3) | 19.9% (18.0-21.9) | 31.1% (26.9-35.5) | 32.9% (32.5-33.3) |
| Anti-hypertensive medication use†§ | |||||
| Yes | 82.2% (81.6-82.8) | 74.6% (67.3-80.7) | 56.8% (51.3-62.1) | 83.1% (76.5-88.2) | 82.8% (82.1-83.4) |
Note. Statistical significance p < 0.001.
= Statistically significant difference between lesbian versus heterosexual women
= Statistically significant difference between bisexual versus heterosexual women
= Statistically significant difference between “other” sexual minority versus heterosexual women
= Analyses only include participants who reported a diagnosis of hypertension
Table 2 presents sexual identity differences across sample characteristics among men (n = 193,490). Overall, 95.6% of men identified as heterosexual, 2.3% identified as gay, 1.6% identified as bisexual, and 0.5% reported their sexual identity was “other”. Compared to heterosexual men, all groups of sexual minority men reported lower annual incomes (p < 0.001). Gay and bisexual men were younger and less likely to meet criteria for obesity than heterosexual men (p < 0.001). Gay men were also more likely than heterosexual men to have graduated college or technical college (38.8% vs. 29.9%, p < 0.001). In addition, bisexual (86.3%) and “other” sexual minority men (77.6%) were less likely to have healthcare insurance coverage than heterosexual men (89.6%). Bisexual men were also less likely than heterosexual men to have a diagnosis of hypertension (31.7% vs. 38.2%, p < 0.001). Among men with a diagnosis of hypertension, bisexual men were significantly less likely to report current anti-hypertensive medication use relative to heterosexual men with a diagnosis of hypertension (60.6% vs. 75.1%, p < 0.001).
Table 2.
Sexual identity differences in sample characteristics among men in the Behavioral Risk Factor Surveillance System (N=193,490).
| Total sample of men (N = 193,490) | Gay men (n = 4,172) | Bisexual men (n = 2,673) | “Other” sexual minority men (n = 972) | Heterosexual men (n = 185,673) | |
|---|---|---|---|---|---|
|
|
|||||
| Sample characteristics | Mean (SD)/Weighted % (95% CI) | ||||
| Age (range 18-80 years)*† | 49.1 (16.9) | 44.9 (15.7) | 34.5 (12.3) | 47.8 (19.3) | 50.9 (16.9) |
| Race/ethnicity‡ | |||||
| Non-Hispanic White | 66.9% (66.4-67.4) | 63.9% (60.6-67.2) | 61.7% (57.7-65.5) | 47.0% (40.8-53.2) | 67.2% (66.9-67.7) |
| Non-Hispanic Black | 11.3% (11.0-11.6) | 12.1% (9.9-14.6) | 11.6% (9.2-14.6) | 11.6% (8.6-15.6) | 11.3% (10.9-11.6) |
| Hispanic | 14.3% (13.9-14.8) | 16.5% (13.8-19.6) | 16.4% (13.0-20.3) | 33.1% (26.8-40.2) | 14.1% (13.7-14.6) |
| Non-Hispanic Asian/Pacific Islander | 4.8% (4.5-5.0) | 3.8% (2.6-5.6) | 6.5% (4.9-8.6) | 4.1% (2.2-7.4) | 4.8% (4.5-5.1) |
| Non-Hispanic Other race | 2.7% (2.6-2.8) | 3.7% (2.7-4.9) | 3.8% (3.0-5.0) | 4.2% (2.9-6.0) | 2.6% (2.5-2.8) |
| Annual income*†‡ | |||||
| < $15,000 | 6.8% (6.6-7.1) | 10.0% (8.2-12.2) | 9.9% (8.1-12.0) | 15.3% (11.6-19.9) | 6.7% (6.4-6.9) |
| $15,000 - $24,999 | 12.9% (12.6-13.3) | 15.0% (12.7-17.8) | 18.7% (15.9-21.9) | 30.0% (23.9-36.8) | 12.7% (12.4-13.0) |
| $25,000 - $34,999 | 9.0% (8.8-9.3) | 8.0% (6.6-9.7) | 12.1% (9.7-15.1) | 11.6% (8.6-15.6) | 9.0% (8.7-9.3) |
| $35,000-$49,999 | 13.3% (13.0-13.6) | 14.4% (12.3-16.8) | 14.6% (12.4-16.9) | 13.6% (10.2-17.8) | 13.2% (12.9-13.5) |
| ≥ $50,000 | 58.0% (57.5-58.4) | 52.6% (49.5-55.6) | 44.7% (41.0-48.5) | 29.5% (24.1-35.6) | 58.4% (58.0-58.9) |
| Educational attainment*‡ | |||||
| Did not graduate high school | 10.8% (10.5-11.2) | 5.9% (4.5-7.8) | 11.7% (9.0-15.1) | 32.6% (26.4-39.4) | 10.8% (10.4-11.2) |
| Graduated high school | 28.3% (27.8-28.7) | 19.1% (16.5-21.9) | 23.7% (20.9-26.8) | 24.4% (19.6-30.0) | 28.6% (28.1-29.0) |
| Attended college/technical school | 31.0% (30.6-31.5) | 36.2% (33.2-39.4) | 36.4% (32.7-40.3) | 23.4% (18.6-29.0) | 30.8% (30.4-31.3) |
| Graduated college/technical school | 29.9% (29.6-30.3) | 38.8% (36.1-41.5) | 28.2% (25.4-31.1) | 19.6% (15.6-24.4) | 29.8% (29.4-30.2) |
| Healthcare insurance coverage†‡ | 89.2% (88.9-89.6) | 88.2% (85.4-90.5) | 86.1% (82.9-88.8) | 77.8% (70.9-83.4) | 89.4% (89.0-89.7) |
| Last routine check-up | |||||
| Within past year | 72.2% (71.7-72.6) | 76.0% (73.1-78.6) | 67.2% (63.4-70.8) | 72.8% (65.9-78.8) | 72.1% (71.7-72.6) |
| Within past two years | 12.3% (12.0-12.6) | 10.4% (8.8-12.3) | 13.9% (11.4-16.9) | 9.0% (6.0-13.2) | 12.3% (12.0-12.6) |
| Within past five years | 8.0% (7.7-8.2) | 6.9% (5.2-8.9) | 11.0% (8.2-14.4) | 8.4% (4.4-15.) | 7.9% (7.7-8.2) |
| Five or more years ago | 6.9% (6.6-7.1) | 6.4% (4.8-8.6) | 7.1% (5.7-8.8) | 9.0% (5.7-14.1) | 6.9% (6.6-7.1) |
| Never | 0.3% (0.2-0.7) | 0.8% (0.4-1.9) | 0.8% (0.3-1.9) | 0.8% (0.7-0.9) | |
| Lifetime smoker | 46.9% (46.5-47.4) | 48.7% (45.7-51.8) | 44.9% (41.3-48.6) | 49.9% (43.4-56.2) | 46.9% (46.4-47.4) |
| Body mass index*† | |||||
| Underweight | 1.0% (0.9-1.1) | 2.9% (1.7-4.7) | 3.4% (2.2-5.2) | 1.8% (1.0-3.5) | 0.9% (0.8-1.0) |
| Normal weight | 24.8%( 24.5-25.3) | 31.9% (29.2-34.7) | 34.3% (31.7-38.1) | 29.0% (23.7-35.0) | 24.5% (24.1-24.9) |
| Overweight | 42.0% (41.5-42.4) | 39.4% (36.4-42.5) | 32.8% (29.5-36.3) | 40.9% (34.7-47.3) | 42.2% (41.7-42.7) |
| Obese | 32.2% (31.8-32.6) | 25.8% (23.4-28.4) | 29.5% (26.4-32.9) | 28.3% (23.0-34.3) | 32.4% (32.0-32.9) |
| Hypertension diagnosis† | |||||
| Yes | 38.0% (37.5-38.4) | 35.3% (32.6-38.1) | 31.5% (28.2-35.0) | 36.8% (31.1-42.3) | 38.1% (37.7-38.6) |
| Anti-hypertensive medication use†§ | |||||
| Yes | 74.7% (74.1-75.4) | 72.1% (67.8-76.0) | 60.6% (53.5-67.2) | 68.1% (58.0-76.7) | 75.0% (74.3-75.6) |
Note. Statistical significance p < 0.001.
= Statistically significant difference between gay versus heterosexual men
= Statistically significant difference between bisexual versus heterosexual men
= Statistically significant difference between “other” sexual minority versus heterosexual men
= Analyses only include participants who reported a diagnosis of hypertension
Table 3 presents results of logistic regression analyses examining sexual identity differences in hypertension diagnosis and anti-hypertensive medication use among women. In fully adjusted models, we found that bisexual women had higher odds of reporting a diagnosis of hypertension than heterosexual women (AOR 1.19, 95% CI = 1.02-1.37, p < 0.05). However, bisexual women with a diagnosis of hypertension were less likely than heterosexual women with a diagnosis of hypertension to report current anti-hypertensive medication use (AOR 0.71, 95% CI = 0.56-0.90, p < 0.01). There were no differences found between the remaining groups of sexual minority women and heterosexual women.
Table 3.
Results of multiple logistic regression models examining sexual identity differences in hypertension diagnosis and anti-hypertensive medication use among women in the Behavioral Risk Factor Surveillance System (N=226,850).
| Hypertension diagnosis | Anti-hypertensive medication use* | |||
|---|---|---|---|---|
|
|
||||
| Model 1 OR (95% CI) | Model 2 AOR (95% CI) | Model 1 OR (95% CI) | Model 2 AOR (95% CI) | |
|
|
||||
| Sexual identity | ||||
| Heterosexual women | Reference | Reference | Reference | Reference |
| Lesbian women | 0.75 (0.63-0.89)§ | 1.01 (0.82-1.26) | 0.61 (0.43-0.87)‡ | 1.08 (0.71-1.64) |
| Bisexual women | 0.51 (0.44-0.57)§ | 1.19 (1.03-1.37)† | 0.27 (0.22-0.34)§ | 0.71 (0.56-0.90)‡ |
| “Other” sexual minority women | 0.92 (0.75-1.13) | 0.85 (0.67-1.08) | 1.03 (0.68-1.56) | 1.10 (0.71-1.68) |
| Age | - | 1.07 (1.06-1.07)§ | - | 1.07 (1.07-1.08)§ |
| Race/ethnicity | - | - | ||
| Non-Hispanic White | Reference | Reference | ||
| Non-Hispanic Black | 1.92 (1.79-2.05)§ | 1.49 (1.29-1.73)§ | ||
| Hispanic | 0.78 (0.70-0.86)§ | 0.78 (0.64-0.94)‡ | ||
| Non-Hispanic Asian/Pacific Islander | 1.19 (1.00-1.43) | 1.08 (0.71-1.64) | ||
| Non-Hispanic Other race | 1.20 (1.06-1.35)‡ | 0.90 (0.74-1.09) | ||
| Annual income | - | - | ||
| < $15,000 | Reference | Reference | ||
| $15,000 - $24,999 | 0.86 (0.79-0.94)‡ | 1.04 (0.87-1.25) | ||
| $25,000 - $34,999 | 0.76 (0.69-0.84)§ | 1.22 (0.99-1.49) | ||
| $35,000-$49,999 | 0.69 (0.63-0.76)§ | 1.18 (0.98-1.43) | ||
| ≥ $50,000 | 0.58 (0.53-0.63)§ | 1.12 (0.93-1.34) | ||
| Educational attainment | - | - | ||
| Did not graduate high school | Reference | Reference | ||
| Graduated high school | 0.78 (0.70-0.86)§ | 0.87 (0.71-1.06) | ||
| Attended college/technical school | 0.76 (0.69-0.84)§ | 0.76 (0.61-0.94)† | ||
| Graduated college/technical school | 0.62 (0.56-0.68)§ | 0.68 (0.54-0.84)‡ | ||
| Healthcare insurance coverage | - | 0.95 (0.85-1.06) | - | 1.33 (1.10-1.62)‡ |
| Last routine check-up | - | - | ||
| Within past year | Reference | Reference | ||
| Within past two years | 0.65 (0.60-0.70)§ | 0.41 (0.36-0.48)§ | ||
| Last Within past five years | 0.50 (0.45-0.56)§ | 0.23 (0.19-0.29§ | ||
| Five or more years ago | 0.48 (0.41-0.56)§ | 0.19 (0.15-0.25)§ | ||
| Never | 0.65 (0.46-0.93)† | 0.83 (0.48-1.43) | ||
| Lifetime smoker | - | 1.19 (1.14-1.24)§ | - | 0.99 (0.90-1.09) |
| Body mass index | - | - | ||
| Underweight | Reference | Reference | ||
| Normal weight | 1.47 (1.18-1.82)§ | 1.77 (1.27-2.47)‡ | ||
| Overweight | 2.55 (2.06-3.15)§ | 2.63 (1.90-3.66)§ | ||
| Obese | 5.17 (4.17-6.39)§ | 3.86 (2.79-5.35)§ | ||
Note. Heterosexual women were the reference group in all logistic regression models presented in Table 3. Model 1 was unadjusted; Model 2 adjusted for age, race/ethnicity, annual income, educational attainment, healthcare insurance coverage, last routine check-up, lifetime smoking, and body mass index category.
Analyses for anti-hypertensive medication use only included 90,020 women who reported a diagnosis of hypertension.
p < 0.05
p < 0.01
p < 0.001
Table 4 presents results of logistic regression analyses examining sexual identity differences in hypertension diagnosis and anti-hypertensive medication use among men. In fully adjusted models, we found that gay men had higher odds of reporting a diagnosis of hypertension than heterosexual men (AOR 1.18, 95% CI = 1.03-1.35, p < 0.05). However, gay men with a diagnosis of hypertension were more likely than heterosexual men with a diagnosis of hypertension to report current anti-hypertensive medication use (AOR 1.39, 95% CI = 1.10-1.78, p < 0.01). There were no differences found between the remaining groups of sexual minority men and heterosexual men.
Table 4.
Results of multiple logistic regression models examining sexual identity differences in hypertension diagnosis and anti-hypertensive medication use among men in the Behavioral Risk Factor Surveillance System (N=193,490).
| Hypertension diagnosis | Anti-hypertensive medication use* | |||
|---|---|---|---|---|
|
|
||||
| Model 1 OR (95% CI) | Model 2 AOR (95% CI) | Model 1 OR (95% CI) | Model 2 AOR (95% CI) | |
|
|
||||
| Sexual identity | ||||
| Heterosexual men | Reference | Reference | Reference | Reference |
| Gay men | 0.89 (0.78-1.00) | 1.18 (1.03-1.35)† | 0.86 (0.70-1.06) | 1.39 (1.10-1.78)‡ |
| Bisexual men | 0.74 (0.63-0.87)§ | 1.14 (0.91-1.41) | 0.51 (0.38-0.68) § | 0.93 (0.70-1.23) |
| “Other” sexual minority men | 0.94 (0.73-1.22) | 0.98 (0.74-1.30) | 0.71 (0.46-1.10) | 0.79 (0.44-1.43) |
| Age | - | 1.05 (1.04-1.05)§ | - | 1.08 (1.08-1.09) § |
| Race/ethnicity | - | - | ||
| Non-Hispanic White | Reference | Reference | ||
| Non-Hispanic Black | 1.36 (1.27-1.47)§ | 1.28 (1.11-1.47)‡ | ||
| Hispanic | 0.84 (0.76-0.92)§ | 0.85 (0.72-1.01) | ||
| Non-Hispanic Asian/Pacific Islander | 1.01 (0.88-1.16) | 1.40 (1.07-1.85)† | ||
| Non-Hispanic Other race | 1.08 (0.97-1.20) | 1.03 (0.83-1.28) | ||
| Annual income | - | - | ||
| < $15,000 | Reference | Reference | ||
| $15,000 - $24,999 | 0.81 (0.73-0.91)§ | 0.95 (0.79-1.14) | ||
| $25,000 - $34,999 | 0.71 (0.64-0.80)§ | 0.79 (0.63-0.99)† | ||
| $35,000-$49,999 | 0.64 (0.57-0.71)§ | 0.77 (0.64-0.92)‡ | ||
| ≥ $50,000 | 0.58 (0.53-0.64)§ | 0.83 (0.71-0.98)† | ||
| Educational attainment | - | - | ||
| Did not graduate high school | Reference | Reference | ||
| Graduated high school | 1.02 (0.93-1.12) | 1.07 (0.89-1.28) | ||
| Attended college/technical school | 0.99 (0.91-1.10) | 0.98 (0.82-1.17) | ||
| Graduated college/technical school | 0.87 (0.79-0.96)‡ | 0.92 (0.77-1.10) | ||
| Healthcare insurance coverage | - | 1.09 (1.00-1.20) | - | 1.58 (1.35-1.85)§ |
| Last routine check-up | - | - | ||
| Within past year | Reference | Reference | ||
| Within past two years | 0.57 (0.53-0.61)§ | 0.32 (0.28-0.37)§ | ||
| Within past five years | 0.50 (0.46-0.56)§ | 0.15 (0.13-0.18)§ | ||
| Five or more years ago | 0.44 (0.40-0.48)§ | 0.15 (0.12-0.18)§ | ||
| Never | 0.59 (0.43-0.81)§` | 0.38 (0.20-0.72)‡ | ||
| Lifetime smoker | - | 1.24 (1.18-1.29)§ | - | 0.90 (0.83-0.98)† |
| Body mass index | - | - | ||
| Underweight | Reference | Reference | ||
| Normal weight | 0.94 (0.74-1.21) | 1.06 (0.65-1.88) | ||
| Overweight | 1.67 (1.31-2.14)§ | 1.59 (0.99-2.82) | ||
| Obese | 3.41 (2.67-4.35)§ | 2.76 (1.72-4.90)§ | ||
Note. Heterosexual men were the reference group in all logistic regression models presented in Table 4. Model 1 was unadjusted; Model 2 adjusted for age, race/ethnicity, annual income, educational attainment, healthcare insurance coverage, last routine check-up, lifetime smoking, and body mass index category.
Analyses for anti-hypertensive medication use only included 85,561 male participants who reported a diagnosis of hypertension.
p < 0.05
p < 0.01
p < 0.001
Discussion
This study contributes to a small but growing body of research on hypertension disparities among sexual minority adults. Our findings provide a greater understanding of differences in the prevalence of hypertension and anti-hypertensive medication use among sexual minority adults in the U.S. Approximately 4% of participants in the present study identified as sexual minority individuals, which is similar to estimates from other analyses of population-based data in the U.S.10,18,29,36–38 We found that bisexual women and gay men had higher odds of reporting a diagnosis of hypertension than their heterosexual peers of the same sex. Prior evidence of hypertension disparities among bisexual women is largely mixed.7,10,17 Consistent with previous studies, there were no differences in hypertension prevalence between lesbian and heterosexual women.7,10,17 Further, conflicting findings have been reported in studies that have examined differences in the prevalence of hypertension between gay and heterosexual men.5,7,8 Prior work suggests that bisexual men are more likely to meet criteria for hypertension than heterosexual men.8 Although bisexual men were more likely to report a diagnosis of hypertension than heterosexual men in our bivariate analyses, this difference was attenuated after adjusting for demographic characteristics, healthcare coverage and utilization, lifetime smoking, and BMI status. To date, researchers investigating hypertension disparities among sexual minority adults have used self-report of hypertension diagnosis.5 However, significantly higher odds of hypertension diagnosis have been found among bisexual men in studies that have used blood pressure measurements to establish the presence of hypertension.18,19 This suggests a need for additional research on hypertension prevalence among sexual minority adults that incorporates objective assessment of hypertension.
This is one of the first studies to investigate sexual identity differences in anti-hypertensive medication use among adults diagnosed with hypertension. Bisexual women with hypertension in the present study reported 29% lower odds of current anti-hypertensive medication use than heterosexual women with hypertension. Previous research on differences in anti-hypertensive medication use between bisexual and heterosexual women is largely mixed.7,10 In addition, we found no differences between lesbian and heterosexual women, which is consistent with prior work.7 To our knowledge, this is the first study to report that bisexual women with hypertension are less likely to be taking anti-hypertensive medications than heterosexual women who also have hypertension.
There are several explanations for these findings. Existing evidence suggests that sexual minority women experience significant barriers in accessing healthcare due to fear of discrimination from healthcare providers.23,24,39 Researchers have found that between 6-23% of sexual minority adults report having experienced discrimination in healthcare settings.25,40 In analyses of nationally representative data, investigators found that report of discrimination in healthcare settings among sexual minority adults peaked at midlife.40 In addition, approximately 18% of sexual and gender minority adults report avoiding healthcare due to concerns related to discrimination and unfair treatment.25 Further, compared to heterosexual women, bisexual women are more likely to live in poverty22 and to delay seeking needed healthcare services.26–28 It is possible that fear of discrimination from healthcare providers and socioeconomic disadvantage contribute to lower healthcare utilization among bisexual women diagnosed with hypertension, which may in turn lead to untreated hypertension in this population. These findings highlight the need for additional research to understand factors that may drive the disparities in anti-hypertensive medication use that we found among bisexual women with hypertension.
Among men with hypertension, we found that gay men were 39% more likely to report using anti-hypertensive medication relative to heterosexual men. No differences in anti-hypertensive medication use were found between bisexual and heterosexual men with hypertension. Prior research on differences in anti-hypertensive medication use between gay and heterosexual men is mixed. A meta-analysis of five studies conducted by Lopez Castillo and colleagues8 found no sexual identity differences in anti-hypertensive medication use between men. However, our findings are consistent with the results of analyses of data from the California Health Interview Survey that found gay men were 41% more likely than heterosexual men to be taking currently anti-hypertensive medication.21 Explanations for these mixed findings related to anti-hypertensive medication use among gay men are unclear. One potential explanation for our findings is that gay men are more likely to obtain needed healthcare services than heterosexual men38,41 and other sexual minority individuals.41 This may explain gay men’s higher likelihood of being diagnosed with hypertension and taking anti-hypertensive medication than men of other sexual identities.
We found no differences in hypertension prevalence or anti-hypertensive medication use among individuals who identified their sexual identity as “other.” Overall, fewer studies have been conducted that examine hypertension among individuals who identify their sexual identity as “other.”5 This is a potentially heterogeneous group that may include individuals with various sexual identities, such as individuals who identify as queer or pansexual as well as those who are questioning their sexual identity or who choose to not define their sexual identity with a single label. Prior analyses of data from the National Health Interview Survey have found that individuals who identify their sexual identity as “other” have distinct demographic and mental health profiles than individuals who identify as gay/lesbian or bisexual.42 Although we did not observe any differences in hypertension prevalence and anti-hypertensive medication use between heterosexual participants and those who identified their sexual orientation as “other,” there is a need for further investigation of hypertension risk in this group as they remain understudied.5
Despite numerous strengths, the present study has several limitations. First, hypertension was assessed using self-reported data. Although several studies have found a moderate association between self-reported and objective measures of hypertension,43 the use of objective measures is preferred to reduce misclassification of participants with undiagnosed hypertension.44,45 Further, the BRFSS does not include information about important social determinants, such as experiences of discrimination and violence, that are hypothesized to contribute to hypertension risk in sexual minority adults.5 Therefore, residual confounding may have biased findings. We only assessed current anti-hypertensive medication use and were unable to examine other self-management behaviors (such as smoking cessation and diet changes) among participants with hypertension.46–49 In addition, we did not include gender minority persons in these analyses. This is an important area for future research as these populations have been shown to have higher risk of hypertension and cardiovascular disease than their cisgender counterparts.50–52
Findings are not nationally representative as the optional sexual orientation and gender identity module in the BRFSS was only used by 22 states in 2015, 27 states in 2017, and 31 states in 2019. Thus, findings may not be generalizable to sexual minority adults living in states that did not include the BRFSS optional sexual orientation and gender identity module during these years. In addition, non-response rates in the BRFSS are higher among hard-to-reach communities (such as racial/ethnic minority and younger participants), which may bias estimates.53 Researchers should replicate our analyses to determine if findings are consistent in other samples.
Compared to participants with complete data for sexual identity, those who responded “don’t know” or “refused” were older, less likely to identify as Non-Hispanic White, had lower annual incomes, had lower educational attainment, and were less likely to have healthcare insurance coverage. Since all of these factors can influence hypertension diagnosis and anti-hypertensive medication use,1 it is possible that these non-response patterns may have biased our findings. Future work should investigate reasons for non-response to sexual identity items in the BRFSS and other population-based studies.
Our findings have important implications for future research. The contradictory results in prior work highlight the need for further research examining hypertension disparities among sexual minority adults. The majority of existing research on hypertension among sexual minority adults has been cross-sectional5,8 and based on self-reported diagnosis of hypertension.54 The increased assessment of sexual identity in electronic health records provides an opportunity to leverage these data to examine hypertension and other chronic disease disparities among sexual minority adults using objective clinical data.55 In particular, the use of data from electronic health records can help researchers understand healthcare utilization patterns (such as medication use and delays in recommended visits) among sexual minority adults with hypertension. Further, there has been limited investigation of social determinants (such as experiences of discrimination) that may contribute to disparities in hypertension diagnosis and anti-hypertensive medication use in sexual minority populations.5 Investigators should conduct longitudinal studies that use objective measures of hypertension and which account for social determinants of hypertension when examining sexual identity differences in hypertension diagnosis and anti-hypertensive medication use among adults. Moreover, qualitative research that explores the perspectives of sexual minority adults diagnosed with hypertension is needed to understand how to best support these individuals to optimize hypertension treatment and self-management behaviors. In particular, it is unclear why bisexual women with hypertension in the present study were less likely to be taking anti-hypertensive medication than their heterosexual counterparts. Future studies should investigate factors that contribute to this disparity, which may help inform clinical interventions to increase medication adherence among bisexual women with hypertension. This is an important area for future work as there are no evidence-based interventions to reduce hypertension risk that are specifically designed to be implemented among sexual minority adults.5
Robust clinical and public health interventions are needed to reduce the risk of hypertension among certain subgroups of sexual minority adults (such as bisexual women and gay men). Healthcare providers need to be educated about the hypertension disparities that have been documented among sexual minority populations. Our findings indicate that healthcare providers should screen for hypertension and risk factors for hypertension among bisexual women and gay men. Moreover, public health campaigns to promote the cardiovascular health of high-risk populations should be tailored to sexual minority adults and include information on the reduction of hypertension and other cardiovascular risk factors (such as tobacco use and physical inactivity). The My Heart, My Pride campaign, launched in 2021, is one of the very few public health initiatives tailored for sexual minority individuals that provides evidence-based recommendations for lifestyle modification to reduce hypertension and cardiovascular disease risk in this population.56
In conclusion, the present study is one of the first to use population-based data to examine sexual identity differences in both the prevalence of hypertension and anti-hypertensive medication use among adults. We found that bisexual women and gay men were more likely to have been diagnosed with hypertension than their heterosexual peers of the same sex. While bisexual women with hypertension were less likely to be currently taking anti-hypertensive medications than heterosexual women, gay men were more likely than heterosexual men to be currently taking these medications. Findings have important implications for research, clinical, and public health efforts aimed at reducing hypertension risk and improving the cardiovascular health of sexual minority populations.
Supplementary Material
What is Known
There is growing evidence that sexual minority (e.g., gay/lesbian, bisexual) men and women have a higher risk of hypertension than their heterosexual counterparts of the same sex.
Despite evidence of a higher risk of hypertension among sexual minority adults, there is limited research on anti-hypertensive medication use among people with hypertension in this population and existing findings are mixed.
What the Study Adds
This is one of the first studies to demonstrate that among adults with hypertension, bisexual women are less likely to report current anti-hypertensive medication use than heterosexual women.
These data highlight the need for additional research to understand factors that contribute to the hypertension disparities observed among bisexual women and gay men in this study.
Sources of Funding
This study was supported by a Mentored Research Scientist Development Award to Dr. Caceres from the National Heart, Lung, and Blood Institute (K01HL146965) and a predoctoral fellowship award from the American Heart Association (AHA899585).
Non-standard Abbreviations and Acronyms
- NHANES
National Health and Nutrition Examination Survey
- BRFSS
Behavioral Risk Factor Surveillance System
Footnotes
Disclosures
None.
Contributor Information
Yashika Sharma, Center for Sexual and Gender Minority Health Research, Columbia University School of Nursing.
Anisha Bhargava, Center for Sexual and Gender Minority Health Research, Columbia University School of Nursing.
Danny Doan, Center for Sexual and Gender Minority Health Research, Columbia University School of Nursing.
Billy A. Caceres, Center for Sexual and Gender Minority Health Research, Columbia University School of Nursing, 560 West 168th Street, Room 603, New York, NY 10032.
References
- 1.Tsao CW, Aday AW, Almarzooq ZI, Alonso A, Beaton AZ, Bittencourt MS, Boehme AK, Buxton AE, Carson AP, Commodore-Mensah Y, et al. , on behalf of the American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics—2022 update: A report from the American Heart Association. Circulation. 2022;145:e153–e639. [DOI] [PubMed] [Google Scholar]
- 2.Ostchega Y, Fryar CD, Nwankwo T, Nguyen DT. Hypertension prevalence among adults aged 18 and over: United States, 2017-2018. NCHS Data Brief. 2020;364:1–8. [PubMed] [Google Scholar]
- 3.Walsh KB, Woo D, Sekar P, Osborne J, Moomaw CJ, Langefeld CD, Adeoye O. Untreated hypertension: A powerful risk factor for lobar and nonlobar intracerebral hemorrhage in whites, Blacks, and Hispanics. Circulation. 2016;134:1444–1452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhou D, Xi B, Zhao M, Wang L, Veeranki SP. Uncontrolled hypertension increases risk of all-cause and cardiovascular disease mortality in US adults: The NHANES III Linked Mortality Study. Sci Rep. 2018;8:9418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Caceres BA, Streed CG, Corliss HL, Lloyd-Jones DM, Matthews PA, Mukherjee M, Poteat T, Rosendale N, Ross LM. Assessing and addressing cardiovascular health in LGBTQ adults: A scientific statement from the American Heart Association. Circulation. 2020;142:2747–2757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Human Rights Campaign. We are here: Understanding the size of the LGBTQ+ community [Internet]. 2021. [cited 2022 July 3]. Available from: https://www.hrc.org/press-releases/we-are-here-lgbtq-adult-population-in-united-states-reaches-at-least-20-million-according-to-human-rights-campaign-foundation-report
- 7.Caceres BA, Brody A, Luscombe RE, Primiano JE, Marusca P, Sitts EM, Chyun D. A systematic review of cardiovascular disease in sexual minorities. American Journal of Public Health. 2017;107:e13–e21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.López Castillo H, Tfirn IC, Hegarty E, Bahamon I, Lescano CM. A meta-analysis of blood pressure disparities among sexual minority men. LGBT Health. 2021;8:91–106. [DOI] [PubMed] [Google Scholar]
- 9.Butler ES, McGlinchey E, Juster R-P. Sexual and gender minority sleep: A narrative review and suggestions for future research. Journal of Sleep Research. 2020;29:e12928–e12928. [DOI] [PubMed] [Google Scholar]
- 10.Caceres BA, Brody AA, Halkitis PN, Dorsen C, Yu G, Chyun DA. Cardiovascular disease risk in sexual minority women (18-59 years old): Findings from the National Health and Nutrition Examination Survey (2001-2012). Women’s Health Issues. 2018;28:333–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Caceres BA, Hickey KT, Heitkemper EM, Hughes TL. An intersectional approach to examine sleep duration in sexual minority adults in the United States: Findings from the Behavioral Risk Factor Surveillance System. Sleep Health. 2019;5:621–629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Caceres BA, Hickey KT. Examining sleep duration and sleep health among sexual minority and heterosexual adults: Findings from NHANES (2005–2014). Behavioral Sleep Medicine. 2020;18:345–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Eliason MJ, Ingraham N, Fogel SC, McElroy JA, Lorvick J, Mauery DR, Haynes S. A systematic review of the literature on weight in sexual minority women. Women’s Health Issues. 2015;25:162–175. [DOI] [PubMed] [Google Scholar]
- 14.Kasza KA, Ambrose BK, Conway KP, Borek N, Taylor K, Goniewicz ML, Cummings KM, Sharma E, Pearson JL, Green VR, et al. Tobacco-product use by adults and youths in the United States in 2013 and 2014. N Engl J Med. 2017;376:342–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li J, Berg CJ, Weber AA, Vu M, Nguyen J, Haardörfer R, Windle M, Goodman M, Escoffery C. Tobacco use at the intersection of sex and sexual identity in the U.S., 2007–2020: A meta-analysis. American Journal of Preventive Medicine. 2021;60:415–424. [DOI] [PubMed] [Google Scholar]
- 16.Rath JM, Villanti AC, Rubenstein RA, Vallone DM. Tobacco use by sexual identity among young adults in the United States. Nicotine Tob Res. 2013;15:1822–1831. [DOI] [PubMed] [Google Scholar]
- 17.Simoni JM, Smith L, Oost KM, Lehavot K, Fredriksen-Goldsen K. Disparities in physical health conditions among lesbian and bisexual women: A systematic review of population-based studies. Journal of Homosexuality. 2017;64:32–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Caceres BA, Brody AA, Halkitis PN, Dorsen C, Yu G, Chyun DA. Sexual orientation differences in modifiable risk factors for cardiovascular disease and cardiovascular disease diagnoses in men. LGBT Health. 2018;5:284–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mays VM, Juster R-P, Williamson TJ, Seeman TE, Cochran SD. Chronic physiologic effects of stress among lesbian, gay, and bisexual adults: Results from the National Health and Nutrition Examination Survey. Psychosom Med. 2018;80:551–563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Caceres BA, Ancheta AJ, Dorsen C, Newlin-Lew K, Edmondson D, Hughes TL. A population-based study of the intersection of sexual identity and race/ethnicity on physiological risk factors for CVD among U.S. adults (ages 18–59). Ethnicity & Health. 2022;27:617–638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Boehmer U, Miao X, Linkletter C, Clark MA. Health conditions in younger, middle, and older ages: Are there differences by sexual orientation? LGBT Health. 2014;1:168–177. [DOI] [PubMed] [Google Scholar]
- 22.Badgett MVL, Choi SK, Wilson BDM. LGBT poverty in the United States: A study of differences between sexual orientation and gender identity groups [Internet]. 2019. Available from: https://williamsinstitute.law.ucla.edu/wp-content/uploads/National-LGBT-Poverty-Oct-2019.pdf?utm_campaign=hsric&utm_medium=email&utm_source=govdelivery
- 23.Ayhan CHB, Bilgin H, Uluman OT, Sukut O, Yilmaz S, Buzlu S. A systematic review of the discrimination against sexual and gender minority in health care settings. Int J Health Serv. 2020;50:44–61. [DOI] [PubMed] [Google Scholar]
- 24.Cronin TJ, Pepping CA, Halford WK, Lyons A. Minority stress and psychological outcomes in sexual minorities: The role of barriers to accessing services. Journal of Homosexuality. 2021;68:2417–2429. [DOI] [PubMed] [Google Scholar]
- 25.Casey LS, Reisner SL, Findling MG, Blendon RJ, Benson JM, Sayde JM, Miller C. Discrimination in the United States: Experiences of lesbian, gay, bisexual, transgender, and queer Americans. Health Services Research. 2019;54:1454–1466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Caceres BA, Makarem N, Hickey KT, Hughes TL. Cardiovascular disease disparities in sexual minority adults: An examination of the Behavioral Risk Factor Surveillance System (2014-2016). American Journal of Health Promotion. 2019;33:576–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Caceres BA, Turchioe MR, Pho A, Koleck TA, Creber RM, Bakken SB. Sexual identity and racial/ethnic differences in awareness of heart attack and stroke symptoms: Findings from the National Health Interview Survey. American Journal of Health Promotion. 2021;35:57–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dahlhamer JM, Galinsky AM, Joestl SS, Ward BW. Barriers to health care among adults identifying as sexual minorities: A US national study. American Journal of Public Health. 2016;106:1116–1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ward BW, Dahlhamer JM, Galinsky AM, Joestl SS. Sexual orientation and health among U.S. adults: National Health Interview Survey, 2013. National Health Statistics Reports. 2014;77:1–10. [PubMed] [Google Scholar]
- 30.Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System: 2019 Summary Data Quality Report [Internet]. Atlanta, GA: 2020. Available from: https://www.cdc.gov/brfss/annual_data/2019/pdf/2019-sdqr-508.pdf [Google Scholar]
- 31.Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System 2015 Summary Data Quality Report [Internet]. Atlanta, Georgia: 2015. Available from: https://www.cdc.gov/brfss/annual_data/annual_2015.html [Google Scholar]
- 32.Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System 2017 Summary Data Quality Report [Internet]. Atlanta, Georgia: 2018. Available from: https://www.cdc.gov/brfss/annual_data/2017/pdf/2017-sdqr-508.pdf [Google Scholar]
- 33.Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System [Internet]. 2018. [cited 2022 June 20]; Available from: https://www.cdc.gov/brfss/index.html
- 34.Centers for Disease Control and Prevention. Defining adult overweight and obesity [Internet]. 2017. [cited 2022 Jul 3]; Available from: https://www.cdc.gov/obesity/adult/defining.html
- 35.Centers for Disease Control and Prevention. The Behavioral Risk Factor Surveillance System: Complex sampling weights and preparing 2017 BRFSS module data for analysis [Internet]. Atlanta, Georgia: 2018. Available from: https://www.cdc.gov/brfss/annual_data/2017/pdf/complex-smple-weights-prep-module-data-analysis-2017-508.pdf [Google Scholar]
- 36.Farmer GW, Jabson JM, Bucholz KK, Bowen DJ. A population-based study of cardiovascular disease risk in sexual-minority women. American Journal of Public Health. 2013;103:1845–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Farmer GW, Bucholz KK, Flick LH, Burroughs TE, Bowen DJ. CVD risk among men participating in the National Health and Nutrition Examination Survey (NHANES) from 2001 to 2010: Differences by sexual minority status. Journal of Epidemiology and Community Health. 2013;67:772–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Trinh M-H, Agénor M, Austin SB, Jackson CL. Health and healthcare disparities among U.S. women and men at the intersection of sexual orientation and race/ethnicity: A nationally representative cross-sectional study. BMC Public Health. 2017;17:964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cerezo A, Ching S, Ramirez A. Healthcare access and health-related cultural norms in a community sample of Black and Latinx sexual minority gender expansive women. Journal of Homosexuality. 2021;1–24. [DOI] [PubMed] [Google Scholar]
- 40.Rice CE, Fish JN, Russell ST, Lanza ST. Sexual minority-related discrimination across the life course: Findings from a national sample of adults in the United States. Journal of Homosexuality. 2021;68:252–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tabaac AR, Solazzo AL, Gordon AR, Austin SB, Guss C, Charlton BM. Sexual orientation-related disparities in healthcare access in three cohorts of U.S. adults. Preventive Medicine. 2020;132:105999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Eliason MJ, Radix A, McElroy JA, Garbers S, Haynes SG. The “something else” of sexual orientation: Measuring sexual identities of older lesbian and bisexual women using National Health Interview survey questions. Women’s Health Issues. 2016;26 Suppl 1:S71–80. [DOI] [PubMed] [Google Scholar]
- 43.Ning M, Zhang Q, Yang M. Comparison of self-reported and biomedical data on hypertension and diabetes: Findings from the China Health and Retirement Longitudinal Study (CHARLS). BMJ Open [Internet]. 2016;6:e009836. Available from: http://www.proquest.com/docview/1860805298/abstract/838107439E9421DPQ/1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gonçalves VSS, Andrade KRC, Carvalho KMB, Silva MT, Pereira MG, Galvao TF. Accuracy of self-reported hypertension: a systematic review and meta-analysis. J Hypertens. 2018;36:970–978. [DOI] [PubMed] [Google Scholar]
- 45.Kislaya I, Leite A, Perelman J, Machado A, Torres AR, Tolonen H, Nunes B. Combining self-reported and objectively measured survey data to improve hypertension prevalence estimates: Portuguese experience. Arch Public Health. 2021;79:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Douglas BM, Howard EP. Predictors of self-management behaviors in older adults with hypertension. Adv Prev Med. 2015;2015:162–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Shahaj O, Denneny D, Schwappach A, Pearce G, Epiphaniou E, Parke HL, Taylor SJC, Pinnock H. Supporting self-management for people with hypertension: a meta-review of quantitative and qualitative systematic reviews. J Hypertens. 2019;37:264–279. [DOI] [PubMed] [Google Scholar]
- 48.Veliz PT, McCabe SE, Hughes TL, Everett BG, Caceres BA, Arslanian-Engoren C. Sexual orientation and hypertension risk reduction behaviors among adults with high blood pressure. Ann LGBTQ Public Popul Health. 2020;1:115–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zinat Motlagh SF, Chaman R, Sadeghi E, Eslami AA. Self-care behaviors and related factors in hypertensive patients. Iran Red Crescent Med J. 2016;18:e35805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Caceres BA, Jackman KB, Edmondson D, Bockting WO. Assessing gender identity differences in cardiovascular disease in US adults: An analysis of data from the 2014–2017 BRFSS. Journal of Behavioral Medicine. 2020;43:329–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Defreyne J, Van de Bruaene LDL, Rietzschel E, Van Schuylenbergh J, T’Sjoen GGR. Effects of gender-affirming hormones on lipid, metabolic, and cardiac surrogate blood markers in transgender persons. Clinical Chemistry. 2019;65:119–134. [DOI] [PubMed] [Google Scholar]
- 52.Streed CG, Beach LB, Caceres BA, Dowshen NL, Moreau KL, Mukherjee M, Poteat T, Radix A, Reisner SL, Singh V, on behalf of the American Heart Association Council on Peripheral Vascular Disease; Council on Arteriosclerosis, Thrombosis and Vascular Biology; Council on Cardiovascular and Stroke Nursing; Council on Cardiovascular Radiology and Intervention; Council on Hypertension; and Stroke Council. Assessing and addressing cardiovascular health in people who are transgender and gender diverse: A scientific statement from the American Heart Association. Circulation. 2021;144:e136–e148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Schneider KL, Clark MA, Rakowski W, Lapane KL. Evaluating the impact of non-response bias in the Behavioral Risk Factor Surveillance System (BRFSS). J Epidemiol Community Health. 2012;66:290–295. [DOI] [PubMed] [Google Scholar]
- 54.Caceres BA, Brody A, Chyun D. Recommendations for cardiovascular disease research with lesbian, gay and bisexual adults. Journal of Clinical Nursing. 2016;25:3728–3742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bosse JD, Leblanc RG, Jackman K, Bjarnadottir RI. Benefits of implementing and improving collection of sexual orientation and gender identity data in electronic health records. CIN - Computers Informatics Nursing. 2018;36:267–274. [DOI] [PubMed] [Google Scholar]
- 56.Hanneman T HRC launches My Heart, My Pride campaign in recognition of American Heart Month [Internet]. 2021. [cited 2022 July 01]; Available from: https://www.hrc.org/news/hrc-launches-my-heart-my-pride-campaign-in-recognition-of-american-heart-month
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


