Abstract
Aims
Large acetabular bone defects encountered in revision total hip arthroplasty (THA) are challenging to restore. Metal constructs for structural support are combined with bone graft materials for restoration. Autograft is restricted due to limited volume, and allogenic grafts have downsides including cost, availability, and operative processing. Bone graft substitutes (BGS) are an attractive alternative if they can demonstrate positive remodelling. One potential product is a biphasic injectable mixture (Cerament) that combines a fast-resorbing material (calcium sulphate) with the highly osteoconductive material hydroxyapatite. This study reviews the application of this biomaterial in large acetabular defects.
Methods
We performed a retrospective review at a single institution of patients undergoing revision THA by a single surgeon. We identified 49 consecutive patients with large acetabular defects where the biphasic BGS was applied, with no other products added to the BGS. After placement of metallic acetabular implants, the BGS was injected into the remaining bone defects surrounding the new implants. Patients were followed and monitored for functional outcome scores, implant fixation, radiological graft site remodelling, and revision failures.
Results
Mean follow-up was 39.5 months (36 to 71), with a significant improvement in post-revision function compared to preoperative function. Graft site remodelling was rated radiologically as moderate in 31 hips (63%) and strong in 12 hips (24%). There were no cases of complete graft site dissolution. No acetabular loosening was identified. None of the patients developed clinically significant heterotopic ossification. There were twelve reoperations: six patients developed post-revision infections, three experienced dislocations, two sustained periprosthetic femur fractures, and one subject had femoral component aseptic loosening.
Conclusion
Our series reports bone defect restoration with the sole use of a biphasic injectable BGS in the periacetabular region. We did not observe significant graft dissolution. We emphasize that successful graft site remodelling requires meticulous recipient site preparation.
Cite this article: Bone Jt Open 2022;3(12):991–997.
Keywords: Bone graft substitute, BGS, Biphasic, Cerament, Revision, Total hip arthroplasty, THA, Acetabulum, Bone defect, Bone loss, acetabular bone defects, revision total hip arthroplasty, bone grafts, calcium sulphate, calcium sulphate, hydroxyapatite, acetabular defects, revision surgery, biomaterial, autograft
Introduction
Total hip arthroplasty (THA) rates are rising globally, which portends a rise in revision THA procedures. 1 Revision procedures are difficult, and large acetabular bone defects are especially challenging. 2 The well-established options to restore acetabular defects are the use of autologous and allogenic bone. Autologous bone, considered the optimal graft material, has many limitations including available graft volume and surgical risk independent of the revision surgery. 3 Allogenic grafts combined most frequently with cementless implants and, more recently, with porous metal augments, address the limitations of autologous graft. 4 However, in recent years, good-quality donated bone has become increasingly hard to source in many countries.
To address the limitations of autogeneic and allogenic grafts, synthetic bone graft substitute (BGS) products have been used in non-structural bone graft applications. BGS products differ according to composition, but most products are composed with a majority of either calcium sulphate or calcium phosphate. To date, many BGS products have not conclusively demonstrated equivalence to bone grafts with regard to incorporation and bone remodelling in large and/or uncontained defects. 5,6 Calcium sulphate-predominant BGS generally resorbs rapidly (almost always within six weeks). 7 Conversely, calcium phosphate-predominant BGS is essentially non-absorbable, and lacks sufficient porosity to enable graft site remodelling. 7 For this reason, next-generation BGS products have been developed that are biphasic, combining calcium sulphate and calcium phosphate in relative proportions that emphasize the benefits of each. 8
One such ‘hybrid BGS’ is Cerament (Bonesupport ab, Sweden). It is a biphasic injectable calcium sulphate/hydroxyapatite BGS. It is composed of 60% α-calcium sulphate hemihydrate (CSH) (CaSO4 1/2H2O) and 40% hydroxyapatite (HA) (Ca10(PO4)6(OH)2). 3,9 By combining a fast-resorbing material (CSH) with a highly osteoconductive material (HA), a controlled rate of product resorption and bone ingrowth can be matched to one another, creating a favourable environment for remodelling. The HA particles are high temperature sintered and further processed to give a size (5 µm), shape, and surface characteristic that is optimal for mixing and osseointegration. 3,10 Previous studies with this BGS show good capacity for bone remodelling. 11-14 These friendly environments include osteotomy of distal radius, fracture malunions, 11 tibial plateau fractures, 12 and benign bone tumours. 13,14 However, it is more pertinent to consider whether this product is capable of guiding bone remodelling in harsh environments such as large acetabular defects encountered during revision THA. This is considered one of the hardest areas to restore bone. Osseointegrative signals are muted for many reasons, including inhibitive inflammatory state created by particulate wear debris phenomenon, compromised local vascularity, excess mechanical bone loads as a result of regional bone loss, and inadequate surgical preparation of the recipient site. 15-17
For this study, we present a retrospective review of the hybrid BGS Cerament, used in acetabular revision surgery in the setting of significant structural and cavitary bony defects. We review serial radiographs to rate the extent of radiological remodeling of the BGS placed into the acetabular region.
Methods
A retrospective analysis was performed, examining the medical records and radiographs of patients treated with injected acetabular BGS (Cerament without antibiotics) at a high-volume revision arthroplasty centre. All patients were treated between January 2014 and June 2018 by a single surgeon (EJM). Minimum follow-up was 36 months. Only those patients whose revision THA surgery involved the pelvis or acetabulum were included. The procedures included aseptic revision THA and re-implantation THA in a two-stage exchange protocol for periprosthetic joint infection (PJI).
The technical preparation of the recipient area of the BGS was twofold. In the areas of contiguous bone, the bone surfaces were scraped meticulously to remove all fibrotic material, metal debris, and inflammatory tissue. Bone was curetted or removed aggressively until punctate bleeding bone was seen, known as the Paprika Sign, as described by Patzakis and Zalavras. 18 In areas of segmental bone loss, the remaining soft-tissues were meticulously debrided with removal of any surrounding avascular ‘rind’ until bleeding tissue was noted. The recipient sites were then irrigated with pulsatile saline mechanical lavage. After insertion of the reconstruction cage or cup, but before placement of the polyethylene bearing, the BGS was injected. Specifically, the BGS powder was hydrated and mixed using a two-syringe technique. No antibiotics were included nor added to the BGS product. After three minutes, the BGS was injected with a cannula behind the cage or cup, through the cage/cup holes, or rim edges into the defect regions, and then allowed to set. After curing, the polyethylene bearing was placed. Within this study group, dissolvable antibiotic-loaded CaSO4 (ALCS) beads were placed only within the joint space at the time of closure. The bead product was Stimulan (Biocomposites, UK). A 10 cc volume of CaSO4 was mixed with 1 gm of vancomycin and 240 mg of tobramycin.
Procedure-specific data included injected BGS volume, implanted devices, surgical reconstruction, and ALCS bead volume. Outcome measures included, functional outcomes (Harris Hip Score (HHS)), 19 radiological evidence of bone remodelling, and implant failure and/or reoperations. Serial postoperative and follow-up radiographs were obtained that included anterior-posterior and lateral views of the pelvis and hip region. The radiographs were reviewed by an independent musculoskeletal radiology examiner with assessment of implant fixation and BGS remodelling. 20,21 A careful review was undertaken to identify, within the BGS regions, trabecular patterns resembling host bone structure. Radiological remodelling was subjectively rated as minimal, moderate, or strong. If the BGS area reduced in size and/or decreased in subjective density over time, remodelling was rated as minimal. Moderate remodelling was present when: 1) the BGS size was maintained over time and there was maintained or increased subjective bone density or 2) the BGS size decreased, but there was an increase in bone density suggesting remodelling of the BGS. Lastly, when trabecular bone patterns were clearly identified within the BGS, we considered this to be a proxy of definite graft remodelling and defined this as a strong remodelling response. In all cases, host staging was performed using the McPherson Staging System. 22 Clinical follow-up intervals were at six weeks, three months, six months, 12 months, and biannually thereafter.
Statistical analysis
Statistical analysis of pre- and postoperative HHSs was conducted using a paired t-test with a significance threshold of p < 0.05.
Results
Between January 2014 and June 2018, we identified 243 patients who had an aseptic revision THA or reimplantation THA. Within this group, 176 patients had a revision procedure of the acetabulum. The remaining 67 patients had a revision procedure only of the femur and were excluded from study. In the group undergoing a revision acetabular procedure, we selected out those who had the injectable biphasic BGS applied. During this study period, we did not use any autologous or allogenic bone grafts. The BGS was applied on its own. A total of 49 subjects (20% of all THA revisions) met the inclusion criteria.
In the selected cohort of 49 revisions, the mean age of the patient was 64.3 years (44 to 79). There were 16 males and 33 females. Mean follow-up for all subjects was 39.5 months (36 to 71). During the follow-up period, one patient died of multiple myeloma at 50 months postoperatively. The primary indication necessitating the revision procedure for all 49 subjects is listed in Table I. Of these, four were McPherson A hosts (8%), 39 were B hosts (80%), and six were C hosts (12%). The mean volume of articular ALCS beads placed at closure was 24.25 cc (5 to 40).
Table I.
List of the primary indication necessitating revision total hip arthroplasty in the 49 study subjects.
| Primary indication for revision THA | Subjects |
|---|---|
| Wear debris phenomenon (metal and/or polyethylene) with or without implant loosening | 19 |
| PJI - reimplantantion procedure (second stage of two-stage exchange) | 15 |
| Mechanical implant loosening without significant wear debris | 10 |
| Prosthetic femoroacetabular impingement pain sans dislocation | 4 |
| Recurrent dislocation | 1 |
PJI, periprosthetic joint infection; THA, total hip arthroplasty.
In 25 cases (51%), a triflange pelvic cage was placed to span segmental defects. Ten cages were ‘off the shelf’ MaxTi cages (Zimmer-Biomet, USA), while 15 cages were larger-spanning custom porous triflange devices (PMI; Zimmer-Biomet) In 20 cases, a cementless porous multihole revision cup was used, either a McLaughlin or G7 (Zimmer-Biomet), with 6.5 mm titanium screws to secure fixation. In the remaining five cases, there was a well-fixed porous metal shell with significant retroacetabular osteolysis. In these cases, the lesions were debrided/curetted with injection of BGS into the retroacetabular defects via an open-door iliac window osteotomy. A new polyethylene bearing was retrofitted into the cup.
Across the entire patient group, a mean of 16 ml (3 to 40) of BGS was injected. At a mean 39.5 month follow-up, a mean HHS increase of 32 points was recorded (p = 0.002). On radiological evaluation at 12-month follow-up, 31 subjects (63%) demonstrated moderate graft site remodelling and 12 subjects (24%) demonstrated strong remodelling with trabecular lines observed (Figures 1 to 3). In six subjects (12%), there was minimal remodelling observed. Radiological evaluation also revealed no instances of acetabular component loosening.
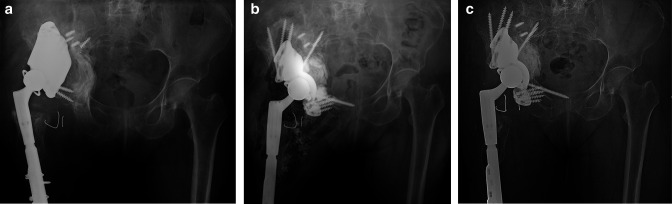
Fig. 1.
a) Anteroposterior (AP) pelvic radiograph of a 75-year-old female with a painful, aseptically loose right revision acetabular component showing protrusion of right cementless porous cup (prior cemented cup). CT scan showed segmental bone loss of anterior column and medial quadrilateral plate. b) Postoperative AP pelvic radiograph showing pelvic reconstruction with MaxTi triflange cage. 18 ml of Cerament was injected behind the cage into all defects before cementing the acetabular component into the cage. c) AP pelvic radiograph 16 months postoperatively. Pelvic reconstruction remains stable. Note the area of Cerament where remodelling has occurred. Remodelling has progressed to an appearance that suggests transformation into bone. Also note the removal of 15 mm of superior ramus screw tip which exited the anterior cortex and was a focal area of discomfort when wearing pants. The exposed screw was removed at 14 months postoperatively with a limited incision.
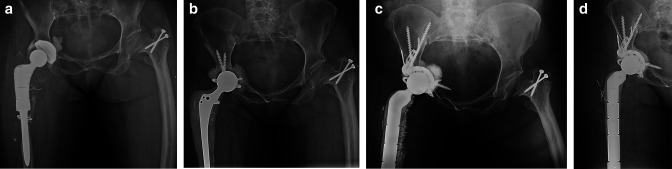
Fig. 3.
a) Anteroposterior (AP) radiograph of pelvis and upper femur region showing loose spanning porous cage of a 65-year-old female who had undergone five prior revision total hip arthroplasty procedures resulting from prior trauma. The cage has failed via an abduction pullout mechanism from the inferior pelvis. An extended polyethylene (+ 5 mm) constrained bearing is locked into the cage. CT scan showed segmental bone loss of posterior column, medial quadrilateral plate, and anterior rim. b) Postoperative AP radiograph showing pelvic reconstruction with a custom triflange porous cage; 28 ml of Cerament was injected behind the cage into all defects before inserting a Freedom constrained bearing into the ring-loc mechanism. A long medullary screw was inserted into the superior ramus to counteract abduction pullout stresses. c) AP pelvic radiograph 66 months postoperatively. Pelvic reconstruction remains stable. The bone graft substitute site shows retroacetabular remodelling, but no trabecular bone patterns are observed.
Fig. 2.
a) Anteroposterior (AP) radiograph of pelvis and upper femur region showing infected endoprosthetic total hip arthroplasty (THA) of a 53-year-old female with a chronic periprosthetic joint infection of her fourth revision right THA. The patient has epiphyseal dysplasia. A draining sinus was present over the lateral mid-thigh. A polyethylene bearing is cemented into the cementless cup. There is cement behind the metal cup. The infecting organism was Cutibacterium. b) AP radiograph of endoprosthetic PROSTALAC (PROSThesis Antibiotic Loaded Acrylic Cement) construct at six months. The patient is ambulatory with partial weight with a walker. Three preoperative aspirations are negative. c) Postoperative AP radiograph showing pelvic reconstruction with MaxTi triflange cage; 10 ml of Cerament was injected behind the cage into all defects before cementing the acetabular component into the cage. A constrained bearing was cemented into the cage construct. d) AP pelvic radiograph 12 months postoperatively. The pelvic reconstruction remains stable. Note the area of Cerament where remodelling has occurred. Remodelling is rated radiologically as moderate.
There were 12 reoperations (24%) in the study group. The mean volume of BGS used in the failure group averaged 17 ml (10 to 30), compared to an average of 16 ml across the entire study group. There were six cases of infection (12%). One case was an A Host, four were B hosts, and one was a C host. Three of the cases recurred after second-stage reimplantation. None of these cases had a return to the operating theatre for wound drainage. Of the six cases, five patients underwent a repeat two-stage exchange protocol. In the other case, a single-stage exchange was performed. Three patients (6%) developed recurrent dislocations. All were treated with a modular bearing exchange and conversion to a constrained bearing construct. Two patients (4%) sustained a periprosthetic femur fracture. Both were treated with a revision femoral stem and multifilament cabling. There was one case (2%) of aseptic loosening of the revision femoral stem that was treated with a cemented proximal endoprosthesis. In this series, there were no cases of significant periarticular heterotopic bone formation. Small islands of heterotopic bone were observed, mainly about the proximal femur in cases of femoral stem revision. This was mostly in cases where femoral osteotomies were performed.
Discussion
Surgical management of acetabular defects encountered during revision THA is driven by many factors. These include surgeon philosophy, defect size, structural acetabular/pelvic integrity, and availability of bone graft material. 23 Established restoration strategies include the use of structural and/or particulate allograft, autograft, or (increasingly) synthetic BGS. 17,24 Placement of particulate allogenic grafts into the acetabular region show good survival. 25,26 A retrospective case series of 95 patients who underwent acetabular reconstruction using morcellized virus-inactivated bone allograft and reinforcement rings showed a ten-year survival rate of 96.2%, with 2.1% failing due to acetabular loosening. 27 However, there are challenges using solely allogenic bone graft material. Not infrequently, there is limited supply, and the inconsistency of supply makes surgical planning difficult. The costs of allograft products can be substantial. Allograft material must be stored in expensive refrigeration systems to maintain graft sterility and integrity. Transport of allografts requires very careful packaging with transportation in high-priority air and ground travel. Intraoperatively, the time and complexity involved with thawing, preparation, and placement of allograft can significantly extend operating time. Thus, the use of synthetic alternatives has always been alluring. However, within the periacetabular region specifically, remodelling and transformation to bone has been problematic with many BGS products. 28,29
The advantages of synthetic bone grafts are several: unlimited and consistent availability, the avoidance of infection-transmission risks associated with allograft, and generally lower costs compared to allogenic grafts. However, their use is not without complications. These include: graft dissolution, migration, resorption, heterotopic ossification, and hypercalcemia. 6,30,31 Furthermore, bone regeneration rates are highly variable with variable standards of evidence demonstrating bone regeneration capabilities. 31 This is important because effective bone regeneration supports the reconstruction construct and is known to reduce the likelihood of fracture or other complications. 32 Thus, a synthetic BGS that effectively promotes bone regeneration would be most attractive.
The injectable BGS used in this study was Cerament. It was chosen for its biomaterial design to allow remodelling from adjacent bone regions. 3,9 By mixing a fast-resorbing material (CaSO4) with a highly osteoconductive material (HA), the resorption and bone ingrowth rate can be matched. This has been previously demonstrated in animal model studies. 33 With the relative fast resorption of the cured calcium sulphate component, a microporosity within the BGS is formed. This allows for the flow of tissue fluids with nutrients and growth factors into the BGS. This in turn promotes osteoclasts and macrophages to enter the biomaterial and create macropores, resulting in host cell ingrowth and remodelling of the BGS. Animal studies have demonstrated the success of this approach in transforming this BGS into bone. An animal model demonstrated that Cerament is remodeled into trabecular bone in six to 12 months. 33 More recently, a randomized controlled trial examining performance of the BGS in managing tibial plateau fractures demonstrated non-inferiority to autograft, the purported gold standard. 12 Further evidence of Cerament’s ability to regenerate into bone has been shown in studies investigating performance in distal radius malunions 7 and bone cysts. 11,13,14 All these studies, however, were in favourable scenarios that include contained bone defects in metaphyseal bone regions with generally good inherent vascularity.
In this series, the performance of Cerament BGS was investigated in the context of acetabular revision surgery, which historically is a challenging area for bone graft remodelling. At 12-month follow-up in this series, 63% demonstrated moderate remodelling and 24% demonstrated strong remodelling, similar to remodelling rates seen with hybrid grafting techniques using allogenic bone. 28 No instances of acetabular loosening were seen. We did not experience any cases of heterotopic bone in the periacetabular region of the BGS application. Despite using two different CaSO4 products in two different roles, we did not experience any clinically relevant hypercalcemia where clinical treatment was required. The 12 instances of postoperative reoperations were, in our opinion, unrelated to use of the BGS in the periacetabulum. Since the BGS was placed behind the acetabular implant en masse, we opine the CaSO4 load from the BGS would not be a significant contributor to the periarticular CaSO4 load within the first two postoperative weeks, the period when wound drainage most often occurs. Additionally, in our six cases of PJI, none required a return to the operating theatre for wound drainage. Statistically significant improvements in functional outcomes (HHS) from pre- to post-procedure were seen in the overall patient cohort. In this small cohort review, there were no complications relating directly to use of the BGS. We emphasize the importance of clinical preparation of the BGS recipient site to promote the remodelling process. All areas (bone and soft-tissues) must show intraoperatively active bleeding. We describe the specific technique as “curette, strip, and bleed”. The remodelling process will only occur if the tissues juxtaposed to the BGS are viable.
There are multiple weaknesses to the study. First, this review is a retrospective single arm review of modest size. Ideally, a randomized controlled study comparing allogenic bone graft to Cerament would be ideal. However, such a study would be difficult to undertake due to the complexities of revision THA surgery. In addition, it would require multicentre support to arrive at significant statistical analysis. Second, all radiological analyses regarding bone remodelling are subjective. Radiological changes can suggest BGS remodelling, but conversion into bone can only be stated with histological analysis of the BGS site. In addition, in many cases, the area of applied BGS was partially obscured by the surrounding metal placed within the pelvis and acetabulum. In 51% of cases, a reconstruction cage was placed. This effect was amplified when smaller volumes (< 10 cc) of BGS were inserted. Another weakness is the use of ALCS beads in this study, meaning two different CaSO4 products were used concomitantly in two different roles. Thus, any purported statements of heterotopic bone formation and increased serum calcium cannot be attributed to the safety of Cerament. However, in this series we did not experience clinically significant hypercalcemia that required treatment. Furthermore, we did not see heterotopic bone within the periacetabular/hip joint region.
In conclusion, this retrospective case series demonstrates that the sole use application of the synthetic biphasic BGS Cerament appears to show positive radiological remodelling in large acetabular defects encountered in acetabular revision surgery. This BGS consistently contributes towards radiological bone defect restoration. We strongly emphasize that successful graft site remodelling requires meticulous recipient site preparation.
Take home message
- Cerament is a biphasic bone graft substitute comprised of hydroxyapatite and calcium sulphate. In this retrospective series, it demonstrated consistent positive bone remodelling in large acetabular bone defects.
- The authors stress the importance of clinical preparation of the recipient site to promote the remodelling process.
Acknowledgements
The authors would like to thank Jalaal Shah, DO for his contributions to to the radiological grading in this work.
Footnotes
Author contributions: E. J. McPherson: Methodology, Formal analysis, Writing – original draft.
A. I. Stavrakis: Methodology, Formal analysis, Writing – original draft.
M. Chowdhry: Investigation, Writing – original draft.
N. L. Curtin: Investigation, Writing – original draft.
M. V. Dipane: Investigation, Formal analysis, Writing – original draft.
B. M. Crawford: responsible for design and analysis & interpretation of data, contributed to writing the original draft.
Funding statement: The authors received no financial or material support for the research, authorship, and/or publication of this article.
ICMJE COI statement: E. J. McPherson reports payments for lectures, presentations, speakers bureaus, manuscript writing or educational events from BoneSupport AB, unrelated to this study.
Ethical review statement: This study recievied ethical approval by an Institutional Review Board (IORG0007797) prior to its undertaking.
Open access funding: The authors confirm that the open access fee for this article was self-funded.
Contributor Information
Edward J. McPherson, Email: edmcpherson@gmail.com.
Alexandra I. Stavrakis, Email: astavrakis@mednet.ucla.edu.
Madhav Chowdhry, Email: madhav.chowdhry@gmail.com.
Nora L. Curtin, Email: ncurtin@mednet.ucla.edu.
Matthew V. Dipane, Email: mdipane@mednet.ucla.edu.
Brooke M. Crawford, Email: bxc859@med.miami.edu.
References
- 1. Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89-A(4):780–785. 10.2106/JBJS.F.00222 [DOI] [PubMed] [Google Scholar]
- 2. Kerzner B, Kunze KN, O’Sullivan MB, Pandher K, Levine BR. An epidemiological analysis of revision aetiologies in total hip arthroplasty at a single high-volume centre. Bone Jt Open. 2021;2(1):16–21. 10.1302/2633-1462.21.BJO-2020-0171.R1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Nilsson M, Zheng MH, Tägil M. The composite of hydroxyapatite and calcium sulphate: a review of preclinical evaluation and clinical applications. Expert Rev Med Devices. 2013;10(5):675–684. 10.1586/17434440.2013.827529 [DOI] [PubMed] [Google Scholar]
- 4. Sun C, Lian Y-Y, Jin Y-H, Zhao C-B, Pan S-Q, Liu X-F. Clinical and radiographic assessment of cementless acetabular revision with morsellised allografts. Int Orthop. 2009;33(6):1525–1530. 10.1007/s00264-009-0722-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Moed BR, Willson Carr SE, Craig JG, Watson JT. Calcium sulfate used as bone graft substitute in acetabular fracture fixation. Clin Orthop Relat Res. 2003;410(410):303–309. 10.1097/01.blo.0000063788.32430.8f [DOI] [PubMed] [Google Scholar]
- 6. Baldwin P, Li DJ, Auston DA, Mir HS, Yoon RS, Koval KJ. Autograft, allograft, and bone graft substitutes: Clinical evidence and indications for use in the setting of orthopaedic trauma surgery. J Orthop Trauma. 2019;33(4):203–213. 10.1097/BOT.0000000000001420 [DOI] [PubMed] [Google Scholar]
- 7. Ferguson J, Diefenbeck M, McNally M. Ceramic biocomposites as biodegradable antibiotic carriers in the treatment of bone infections. J Bone Jt Infect. 2017;2(1):38–51. 10.7150/jbji.17234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Rolvien T, Barbeck M, Wenisch S, Amling M, Krause M. Cellular mechanisms responsible for success and failure of bone substitute materials. Int J Mol Sci. 2018;19(10):2893. 10.3390/ijms19102893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wang JS, Tägil M, Isaksson H, Boström M, Lidgren L. Tissue reaction and material biodegradation of a calcium sulfate/apatite biphasic bone substitute in rat muscle. J Orthop Translat. 2016;6:10–17. 10.1016/j.jot.2015.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Nilsson M, Wang JS, Wielanek L, Tanner KE, Lidgren L. Biodegradation and biocompatability of a calcium sulphate-hydroxyapatite bone substitute. J Bone Joint Surg Br. 2004;86-B(1):120–125. 10.1302/0301-620X.86B1.14040 [DOI] [PubMed] [Google Scholar]
- 11. Abramo A, Geijer M, Kopylov P, Tägil M. Osteotomy of distal radius fracture malunion using a fast remodeling bone substitute consisting of calcium sulphate and calcium phosphate. J Biomed Mater Res B Appl Biomater. 2010;92(1):281–286. 10.1002/jbm.b.31524 [DOI] [PubMed] [Google Scholar]
- 12. Hofmann A, Gorbulev S, Guehring T, et al. . Autologous iliac bone graft compared with biphasic hydroxyapatite and calcium sulfate cement for the treatment of bone defects in tibial plateau fractures: A prospective, randomized, open-label, multicenter study. J Bone Joint Surg Am. 2020;102-A(3):179–193. 10.2106/JBJS.19.00680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Horstmann PF, Hettwer WH, Kaltoft NS, Petersen MM. Early clinical and radiological experience with a ceramic bone graft substitute in the treatment of benign and borderline bone lesions. Sci Rep. 2018;8(1):15384. 10.1038/s41598-018-33736-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kaczmarczyk J, Sowinski P, Goch M, Katulska K. Complete twelve month bone remodeling with a bi-phasic injectable bone substitute in benign bone tumors: a prospective pilot study. BMC Musculoskelet Disord. 2015;16:369. 10.1186/s12891-015-0828-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Busanelli L, Castagnini F, Bordini B, Stea S, Calderoni PP, Toni A. The biological acetabular reconstruction with bone allografts in hip revision arthroplasty. Musculoskelet Surg. 2019;103(2):173–179. 10.1007/s12306-018-0573-5 [DOI] [PubMed] [Google Scholar]
- 16. Jiang Y, Jia T, Gong W, Wooley PH, Yang SY. Effects of Ti, PMMA, UHMWPE, and Co-Cr wear particles on differentiation and functions of bone marrow stromal cells. J Biomed Mater Res A. 2013;101(10):2817–2825. 10.1002/jbm.a.34595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Quarto E, Zanirato A, Santolini F, Formica M. Bone impaction grafting and anti-protrusio cages in high-grade acetabular defects: a 22-year single centre experience. Arch Orthop Trauma Surg. 2022;142(8):2083–2091. 10.1007/s00402-021-04081-x [DOI] [PubMed] [Google Scholar]
- 18. Patzakis MJ, Zalavras CG. Chronic posttraumatic osteomyelitis and infected nonunion of the tibia: current management concepts. J Am Acad Orthop Surg. 2005;13(6):417–427. 10.5435/00124635-200510000-00006 [DOI] [PubMed] [Google Scholar]
- 19. Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51-A(4):737–755. [PubMed] [Google Scholar]
- 20. Young SK, Dorr LD, Kaufman RL, Gruen TA. Factors related to failure of structural bone grafts in acetabular reconstruction of total hip arthroplasty. J Arthroplasty. 1991;6 Suppl:S73–82. 10.1016/s0883-5403(08)80059-9 [DOI] [PubMed] [Google Scholar]
- 21. Gruen TA, Poggie RA, Lewallen DG, et al. . Radiographic evaluation of a monoblock acetabular component: a multicenter study with 2- to 5-year results. J Arthroplasty. 2005;20(3):369–378. 10.1016/j.arth.2004.12.049 [DOI] [PubMed] [Google Scholar]
- 22. McPherson EJ, Woodson C, Holtom P, et al. . Periprosthetic total hip infection: outcomes using a staging system. Clin Orthop Relat Res. 2002;403:8–15. [PubMed] [Google Scholar]
- 23. Paprosky WG, O’Rourke M, Sporer SM. The treatment of acetabular bone defects with an associated pelvic discontinuity. Clin Orthop Relat Res. 2005;441:216–220. 10.1097/01.blo.0000194311.20901.f9 [DOI] [PubMed] [Google Scholar]
- 24. Chang C-Y, Wu C-T, Numan H, Kuo F-C, Wang J-W, Lee MS. Survival analysis of allografting and antiprotrusio cage in treating massive acetabular bone defects. J Arthroplasty. 2021;36(2):682–687. 10.1016/j.arth.2020.08.050 [DOI] [PubMed] [Google Scholar]
- 25. Perlbach R, Palm L, Mohaddes M, Ivarsson I, Schilcher J. Good implant survival after acetabular revision with extensive impaction bone grafting and uncemented components. Bone Joint J. 2020;102-B(2):198–204. 10.1302/0301-620X.102B2.BJJ-2019-0584.R2 [DOI] [PubMed] [Google Scholar]
- 26. Regis D, Magnan B, Sandri A, Bartolozzi P. Long-term results of anti-protrusion cage and massive allografts for the management of periprosthetic acetabular bone loss. J Arthroplasty. 2008;23(6):826–832. 10.1016/j.arth.2007.06.017 [DOI] [PubMed] [Google Scholar]
- 27. Villatte G, Erivan R, Salles G, et al. . Acetabular bone defects in THA revision: Reconstruction using morsellised virus-inactivated bone allograft and reinforcement ring. Seven-year outcomes in 95 patients. Orthop Traumatol Surg Res. 2017;103(4):543–548. 10.1016/j.otsr.2017.03.008 [DOI] [PubMed] [Google Scholar]
- 28. Pierannunzii L, Zagra L. Bone grafts, bone graft extenders, substitutes and enhancers for acetabular reconstruction in revision total hip arthroplasty. EFORT Open Rev. 2016;1(12):431–439. 10.1302/2058-5241.160025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Blom AW, Wylde V, Livesey C, et al. . Impaction bone grafting of the acetabulum at hip revision using a mix of bone chips and a biphasic porous ceramic bone graft substitute. Acta Orthop. 2009;80(2):150–154. 10.3109/17453670902884767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kallala R, Harris WE, Ibrahim M, Dipane M, McPherson E. Use of Stimulan absorbable calcium sulphate beads in revision lower limb arthroplasty: Safety profile and complication rates. Bone Joint Res. 2018;7(10):570–579. 10.1302/2046-3758.710.BJR-2017-0319.R1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Wang W, Yeung KWK. Bone grafts and biomaterials substitutes for bone defect repair: A review. Bioact Mater. 2017;2(4):224–247. 10.1016/j.bioactmat.2017.05.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. McNally M, Nagarajah K. (iv) Osteomyelitis. Orthopaedics and Trauma. 2010;24(6):416–429. 10.1016/j.mporth.2010.09.004 [DOI] [Google Scholar]
- 33. Hettwer W, Horstmann PF, Bischoff S, et al. . Establishment and effects of allograft and synthetic bone graft substitute treatment of a critical size metaphyseal bone defect model in the sheep femur. APMIS. 2019;127(2):53–63. 10.1111/apm.12918 [DOI] [PMC free article] [PubMed] [Google Scholar]