Abstract
Purpose:
KEYNOTE-224 cohort 1 demonstrated that pembrolizumab was efficacious and tolerable in patients with advanced hepatocellular carcinoma (HCC) previously treated with sorafenib. We report results from KEYNOTE-224 (NCT02702414) cohort 2, which enrolled patients with advanced HCC and no prior systemic therapy.
Patients and Methods:
KEYNOTE-224 was an open-label, multicountry phase II trial. Eligible patients in cohort 2 had advanced HCC not amenable or refractory to locoregional therapy and not previously treated with systemic therapy. Patients received pembrolizumab 200 mg intravenously every 3 weeks for ≤2 years. Primary endpoint was objective response rate (ORR) by central imaging review per RECIST v1.1. Secondary endpoints included duration of response (DOR), disease control rate (DCR), time to progression (TTP), progression-free survival (PFS), overall survival (OS), and safety/tolerability.
Results:
Between September 4, 2018, and February 20, 2019, 51 patients were allocated in cohort 2. The median time from the first dose to data cutoff (January 19, 2021) was 27 months (range, 23–29). ORR was 16% [95% confidence interval (CI), 7–29] and was similar across key subgroups. Median DOR was 16 months (range, 3–24+), and DCR was 57%. The median PFS was 4 months (95% CI, 2–8), and median TTP was 4 months (95% CI, 3–9). Median OS was 17 months (95% CI, 8–23). Grade ≥3 treatment-related adverse events occurred in 16% of patients.
Conclusions:
In patients with advanced HCC with no prior systemic therapy, pembrolizumab provided durable antitumor activity, promising OS, and had a safety profile consistent with previous observations. These findings support further evaluation of pembrolizumab-based regimens for HCC.
Translational Relevance.
Results from cohort 1 of the phase II, open-label KEYNOTE-224 trial demonstrated that pembrolizumab monotherapy was efficacious and tolerable in patients with advanced hepatocellular carcinoma (HCC) previously treated with sorafenib. Cohort 2 of the KEYNOTE-224 trial investigated pembrolizumab monotherapy as a therapeutic approach for patients with advanced HCC who had not been previously treated with systemic therapy. The results showed that pembrolizumab monotherapy in this population had promising efficacy, including objective response rate with durable antitumor activity and no new safety signals. These findings support further evaluation of pembrolizumab alone or in combination with other agents for the treatment of HCC.
Introduction
Liver cancer is one of the most common malignancies and a leading cause of cancer-related mortality worldwide (1). Hepatocellular carcinoma (HCC) accounts for up to 90% of primary liver cancers (2). Risk factors for HCC include cirrhosis, hepatitis B or C virus infection, heavy alcohol use, and metabolic syndrome (2, 3). Patients with HCC are often diagnosed with advanced disease and are not eligible for curative treatment (e.g., resection, transplantation, or ablative strategies). For these patients, prognosis is poor, creating a significant unmet need in the management of advanced HCC (4).
The treatment landscape for advanced HCC has evolved rapidly in recent years. First-line systemic therapies for advanced HCC include monotherapy with the oral tyrosine kinase inhibitors sorafenib (5, 6) and lenvatinib (7). The combination of the immune checkpoint inhibitor atezolizumab, which binds to programmed death ligand 1 (PD-L1), plus the anti-VEGF antibody bevacizumab showed a significant survival benefit versus sorafenib and became a standard of care for first-line treatment for many patients with unresectable HCC (8). Recently, results from the ORIENT-32 study also demonstrated improved progression-free survival (PFS) and overall survival (OS) benefits with sintilimab (a programmed death 1 inhibitor) plus IBI305, a bevacizumab biosimilar, versus sorafenib as a first-line treatment for unresectable hepatitis B virus–associated HCC (9). Options for subsequent therapy in the United States include antiangiogenic therapies (tyrosine kinase inhibitors regorafenib, cabozantinib, and ramucirumab), and patients who have not been previously treated with immunotherapy can receive pembrolizumab monotherapy or the combination of nivolumab plus ipilimumab (10).
In cohort 1 of the phase II KEYNOTE-224 trial, pembrolizumab monotherapy provided durable antitumor activity with a manageable safety profile in patients with advanced HCC previously treated with sorafenib (11) and was approved for this patient population by the FDA (12). The phase III randomized, double-blinded KEYNOTE-240 trial supported a favorable benefit-to-risk profile for pembrolizumab as second-line therapy after sorafenib for advanced HCC, although OS and PFS did not reach the statistical significance thresholds per specified criteria [HR for OS, 0.781; 95% confidence interval (CI), 0.611–0.998; P = 0.0238; HR for PFS, 0.775; 95% CI, 0.609–0.987; P = 0.0186; ref. 13]. Recently, in the phase III randomized, double-blinded KEYNOTE-394 trial, pembrolizumab monotherapy resulted in a statistically significant improvement of OS (primary endpoint; HR, 0.79; 95% CI, 0.63–0.99; P = 0.0180), PFS (secondary endpoint; HR, 0.74; 95% CI, 0.60–0.92; P = 0.0032), and objective response rate (ORR) versus placebo for Asian patients with advanced HCC who had received prior sorafenib treatment (14). The similar findings of the KEYNOTE-240 and KEYNOTE-394 studies demonstrated a consistent clinical benefit for pembrolizumab monotherapy in advanced HCC.
Here, we report efficacy and safety results for cohort 2 of KEYNOTE-224, which included patients with advanced HCC who had not received prior systemic therapy.
Patients and Methods
Study design and patients
KEYNOTE-224 is a phase II, single-arm, open-label, multicenter trial conducted in 13 centers in Belgium, Canada, Italy, Sweden, the United Kingdom, and the United States for cohort 2. Eligible patients in cohort 2 were at least 18 years old, had radiologically, histologically, or cytologically confirmed, incurable HCC not amenable or refractory to locoregional therapy, Child-Pugh A liver disease, measurable disease based on Response Evaluation Criteria in Solid Tumors (RECIST) version 1.1 (15) by central imaging review, Eastern Cooperative Oncology Group performance status (ECOG PS) 0–1, Barcelona Clinic Liver Cancer (BCLC) stage C or B, and had no prior systemic therapy in the advanced disease setting. Full inclusion and exclusion criteria are provided in the protocol (appendix). No treatment blinding or randomization occurred.
The study protocol and amendments were approved by the institutional review boards and ethics review committees at each institution. The study was conducted in accordance with the protocol, Good Clinical Practice guidelines, and the Declaration of Helsinki. All patients provided written informed consent.
Treatment and masking
This was an open-label, single-arm cohort of the trial. All enrolled patients were allocated to receive pembrolizumab 200 mg intravenously over 30 minutes every 3 weeks.
Procedures
Patients received pembrolizumab for up to 35 cycles (∼2 years) or until disease progression, unacceptable toxicity, consent withdrawal, or investigator decision to discontinue therapy. Tumor imaging and response assessment per RECIST version 1.1 were conducted every 9 weeks until disease progression, the start of new anticancer treatment, withdrawal of consent, death, or notification by the Sponsor, whichever occurred first. Treatment could be continued until confirmation of progressive disease by immune-related RECIST (irRECIST) on imaging performed at least 4 weeks after the date at which progression was first observed. In cases of confirmation of progressive disease by irRECIST, an exception to continue study treatment could have been considered following consultation with the Sponsor. If the patient was determined to be in complete or partial response or to have stable disease per irRECIST, study treatment could be continued at the investigator's discretion. Survival status was assessed every 12 weeks after confirmed disease progression or the start of new anticancer therapy.
Adverse events (AE) were assessed from the time of treatment allocation until 30 days after treatment cessation; serious AEs were followed for 90 days (30 days if the patient started a new anticancer therapy, whichever was earlier) after treatment cessation.
Study endpoints
The primary endpoint was ORR, defined as the proportion of patients with a confirmed complete or partial response (per RECIST 1.1 by central imaging review). Secondary endpoints were the duration of response (DOR; time from first confirmed complete or partial response to disease progression or death, whichever occurred first), disease control rate (DCR; the proportion of patients with complete and partial responses or stable disease), time to progression (TTP; time from the first day of treatment to first documented disease progression), and PFS (time from the first day of treatment to first documented disease progression or death, whichever occurred first), all of which were assessed per RECIST 1.1 by central imaging review; OS (time from the first day of treatment to death from any cause); and safety and tolerability.
Protocol-specified exploratory endpoints included evaluation of ORR, DOR, DCR, TTP, and PFS per irRECIST (16) and modified RECIST (mRECIST) for HCC (17) by central imaging review and per RECIST 1.1 by investigator's assessment. A full list of prespecified exploratory endpoints is available in the protocol.
Statistical analysis considerations
A sample size of ∼50 patients was chosen to provide acceptable precision for the assessment of ORR with the expected 95% CI of approximately ± 11% around the ORR estimate if the observed ORR was ∼17%. No interim analysis was planned for cohort 2. Efficacy and safety were assessed in patients who received at least one dose of study treatment. DOR was assessed in responders (patients who had confirmed partial or complete response). Because this was an open-label, single-arm cohort, there was no hypothesis testing. The estimates and 95% CIs for ORR and DCR were based on Clopper–Pearson method. The Kaplan–Meier method was used to estimate OS, PFS, TTP, and DOR.
Patients without evaluable response data were counted as nonresponders for ORR assessment and as patients whose disease was not under control for DCR assessment. For DOR, patients without progression by central imaging review, death, or use of new anticancer therapy were censored at the last adequate disease assessment; those without progression or death but with use of new anticancer therapy were censored at the last adequate disease assessment before new anticancer therapy was initiated; and those with death or progression after two or more consecutive missed adequate disease assessments were censored at the last adequate disease assessment prior to the missed adequate disease assessments. Patients were considered to have an ongoing response if they were alive, had not progressed, had not started a new anticancer therapy, and were not lost to follow-up. Patients without progression by central imaging review or death were censored for PFS analysis at the last adequate disease assessment (prior to the start of the post-study oncologic therapy if applicable). Patients without central imaging review were censored for TTP analysis at the last adequate disease assessment (prior to the start of the post-study oncologic therapy if applicable). For OS, patients not known to have died prior to the data cutoff were censored at the date last known alive or data cutoff, whichever was the earliest.
Patient flow through the trial, demographic and baseline characteristics, and AEs were summarized by descriptive statistics or categorical tables.
We conducted prespecified subgroup analyses of age (≤65 vs. >65 years), sex (female vs. male), region (United States vs. non-United States), viral status (hepatitis B and/or hepatitis C seropositivity versus nonviral etiology), ECOG PS (0 vs. 1), alpha-fetoprotein level (>200 ng/mL vs. ≤200 ng/mL), macrovascular invasion (yes vs. no), and extrahepatic disease (yes vs. no) to assess the consistency of the primary endpoint across various subgroups. Hepatitis B seropositivity was defined as hepatitis B surface antigen–positive and/or hepatitis B virus DNA detectable and/or anti-hepatitis B core positive, and hepatitis C seropositivity was defined as hepatitis C virus RNA detectable and/or anti-hepatitis C virus-positive.
This study is registered with ClinicalTrials.gov, NCT02702414. The study is ongoing for follow-up but is no longer enrolling patients.
Data-sharing statement
Merck Sharp & Dohme Corp. (MSD), a subsidiary of Merck & Co., Inc., Kenilworth, NJ, is committed to providing qualified scientific researchers access to anonymized data and clinical study reports from the company's clinical trials for the purpose of conducting legitimate scientific research. MSD is also obligated to protect the rights and privacy of trial participants and, as such, has a procedure in place for evaluating and fulfilling requests for sharing company clinical trial data with qualified external scientific researchers. The MSD data sharing website (available at http://engagezone.msd.com/ds_documentation.php) outlines the process and requirements for submitting a data request. Applications will be promptly assessed for completeness and policy compliance. Feasible requests will be reviewed by a committee of MSD subject matter experts to assess the scientific validity of the request and the qualifications of the requestors. In line with data privacy legislation, submitters of approved requests must enter into a standard data-sharing agreement with MSD before data access is granted. Data will be made available for request after product approval in the US and EU or after product development is discontinued. There are circumstances that may prevent MSD from sharing requested data, including country or region-specific regulations. If the request is declined, it will be communicated to the investigator. Access to genetic or exploratory biomarker data requires a detailed, hypothesis-driven statistical analysis plan that is collaboratively developed by the requestor and MSD subject matter experts; after approval of the statistical analysis plan and execution of a data-sharing agreement, MSD will either perform the proposed analyses and share the results with the requestor or will construct biomarker covariates and add them to a file with clinical data that is uploaded to an analysis portal so that the requestor can perform the proposed analyses.
Results
Patients
Of the 70 patients screened for cohort 2, 51 met the eligibility criteria and were allocated between September 4, 2018 and February 20, 2019. All allocated patients received at least one dose of the study drug and were included in the efficacy and safety analyses. The median time from the first dose to the data cutoff (January 19, 2021) was 27 months (range, 23–29). At the time of data cutoff, 6 patients completed the treatment with pembrolizumab, 1 patient remained on treatment, and 44 patients discontinued treatment. The most common reasons for discontinuation were progressive disease in 27 (53%) patients and AEs in 8 (16%) patients (Supplementary Fig. S1). Baseline characteristics are shown in Table 1.
Table 1.
Baseline demographics and disease characteristics.
| Patients | |
|---|---|
| Characteristic, n (%) | N = 51 |
| Median age (range), years | 68 (41–91) |
| Sex | |
| Male | 44 (86) |
| Female | 7 (14) |
| Race | |
| Asian | 2 (4) |
| Black | 1 (2) |
| White | 48 (94) |
| Region | |
| EU | 37 (73) |
| US | 13 (26) |
| Others | 1 (2) |
| ECOG PS | |
| 0 | 27 (53) |
| 1 | 24 (47) |
| Child-Pugh Class | |
| A | 51 (100) |
| BCLC stage | |
| B | 11 (22) |
| C | 40 (78) |
| Etiology | |
| Viral etiology | 20 (39) |
| Nonviral etiology | 29 (57) |
| Missing | 2 (4) |
| Alcohol use (all)a | 41 (80) |
| Extrahepatic disease | 17 (33) |
| Macrovascular invasion | 9 (18) |
| Alpha-fetoprotein concentrationb | |
| >200 ng/mL | 19 (37) |
| ≤200 ng/mL | 32 (63) |
| Prior radiation | 2 (4) |
| Prior surgery | 8 (16) |
| Locoregional therapyc | 17 (33) |
aReported patients who ever used alcohol.
bThirteen (26%) patients had alpha-fetoprotein concentration >400 ng/mL.
cMajority of which included embolization, ablation, and radiation to the liver.
Efficacy
Objective response
Per RECIST 1.1 by central imaging review, an objective response was observed in 8 of 51 patients, and the ORR was 16% (95% CI, 7–29); all 8 patients had partial response. An additional 21 patients had stable disease, for a DCR of 57% (95% CI, 42–71). Progressive disease was the best response for 17 (33%) patients, and response was unable to be assessed for 5 (10%) patients (Table 2).
Table 2.
Responses to pembrolizumab treatment by RECIST 1.1 by central imaging review.
| Patients | |
|---|---|
| N = 51 | |
| ORR, % (95% CI) | 16 (7–29) |
| DCR, % (95% CI) | 57 (42–71) |
| Best overall response, n (%) | |
| Complete response | 0 |
| Partial response | 8 (16) |
| Stable disease | 21 (41) |
| Progressive disease | 17 (33) |
| Nonevaluablea | 2 (4) |
| No assessmentb | 3 (6) |
| Time to response, median (range), months | 6 (2–13) |
| DOR, median (range), months | 16 (3–24+) |
aOne patient had a post-baseline imaging assessment at Cycle 1 but was counted as nonevaluable due to insufficient time from randomization.
bNo post-baseline assessment available for response evaluation.
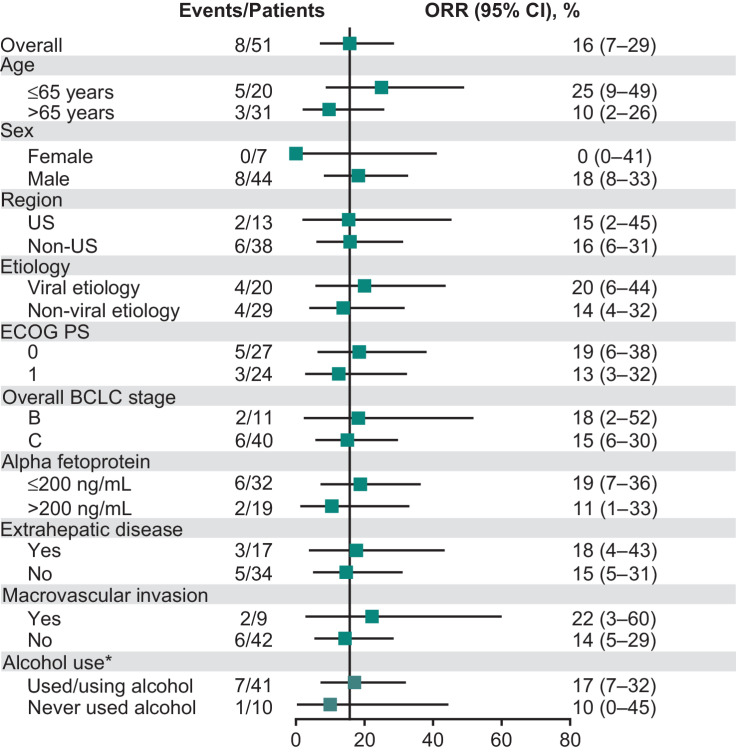
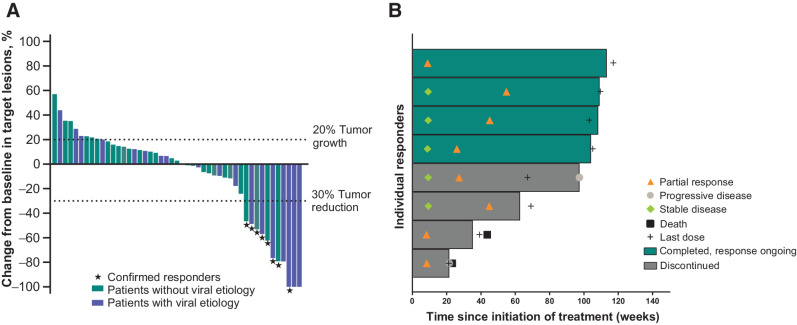
ORR was generally consistent across subgroups analyzed (Fig. 1). Of the 47 patients with at least one post-baseline imaging assessment, 22 (47%) patients had a reduction in target lesion size from baseline, including 11 (23%) patients who had a ≥30% reduction (Fig. 2A). Median time to response was 6 months (range, 2–13), with the initial response observed by week 9 for 3 of the 8 confirmed responses (Fig. 2B). The median DOR was 16 months (range, 3–24+). Of the 8 responders with a confirmed response, 50% had ongoing responses as of the data cutoff date (Fig. 2B). Per Kaplan–Meier estimate, 73% of responders had responses that lasted at least 12 months. Of the 6 patients who completed treatment with pembrolizumab, best overall response was partial response in 4 patients and stable disease in 2 patients. One patient with stable disease had subsequent disease progression. DOR ranged from 12.5+ to 24.0+ months, and duration of disease control ranged from 8.2 to 24.0+ months.
Figure 1.
Subgroup analyses of objective response. *All prespecified except the analyses by alcohol use.
Figure 2.
Characteristics of tumor response to pembrolizumab. A, Best percentage change from baseline in target lesion in patients without viral etiology (green) and those with viral etiology (blue). Stars indicate patients with a confirmed response by central imaging review. B, Duration of study treatment and response in responders. Each horizontal line represents 1 patient. The end of the bar represents the dates of the last radiology imaging assessment.
TTP, PFS, and OS
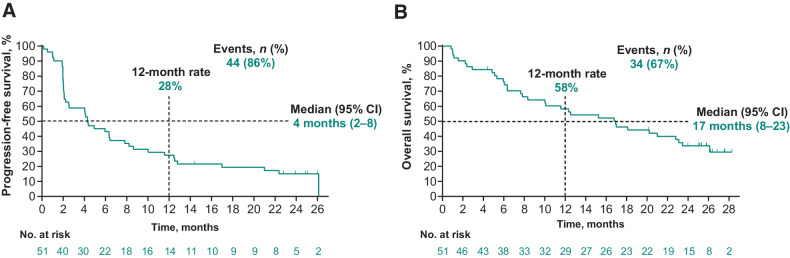
At the data cutoff, 44 (86%) patients had a PFS event per RECIST 1.1 by central imaging review. The median TTP was 4 months (95% CI, 3–9), and median PFS was 4 months (95% CI, 2–8). The estimated PFS rate at 12 months was 28% (Fig. 3A). Of the 51 patients, 34 (67%) had died. Median OS was 17 months (95% CI, 8–23), and the OS rate at 12 months was 58% (Fig. 3B).
Figure 3.
Kaplan–Meier curves for PFS (A) and OS (B).
Prespecified exploratory analyses of objective response and PFS
In prespecified exploratory analyses of responses, objective responses were observed in 9 (18%; 95% CI, 8–31) patients per irRECIST or mRECIST by central imaging review or per RECIST 1.1 by investigator's assessment (Supplementary Table S1).
On the basis of irRECIST assessment by central imaging review, the Kaplan–Meier estimate of objective response lasting at least 12 months was 74%. Median PFS was 6 months (95% CI, 3–10), with an estimated PFS rate at 12 months of 33% (Supplementary Fig. S2A).
With the use of the mRECIST criteria by central imaging review, 67% of responders had responses that lasted at least 12 months per Kaplan–Meier estimate. Median PFS was 4 months (95% CI, 2–6), with an estimated PFS rate at 12 months of 24% (Supplementary Fig. S2B).
On the basis of the RECIST 1.1 criteria by investigator's assessment, 78% of responders had responses that lasted at least 12 months per Kaplan–Meier estimate. Median PFS was 5 months (95% CI, 2–6), with an estimated PFS rate at 12 months of 25% (Supplementary Fig. S2C).
Safety
In all treated patients, median treatment duration was 4 months (range, 1 day–27 months). Treatment-emergent AEs were reported in 49 (96%) patients (grade 3–5, 63%; Table 3). Treatment-related AEs were reported in 28 (55%) patients, and common events were mostly of grade 1 to 2 severity. There were 3 (6%) patients who discontinued pembrolizumab because of treatment-related AEs. Grade 3 to 5 treatment-related AEs occurred in 8 (16%) patients; all were grade 3 except in 1 patient, who also had grade 3 myositis (at day 5) and grade 3 immune-mediated hepatitis (at day 15), and died from grade 5 myocarditis (day 26–31) that was attributed to study treatment by the investigator. This patient required steroids to treat immune-mediated AEs (i.e., hepatitis, myositis, and myocarditis), but died of myocarditis while the other two AEs were ongoing. Immune-mediated AEs and infusion reactions occurred in 12 (24%) patients (grade 3–5, 12%; all were grade 3 except in the 1 patient with grade 5 myocarditis mentioned above); the only grade 3 immune-mediated AE that occurred in more than 1 patient was severe skin reaction (n = 2; Supplementary Table S2). Five (10%) patients received systemic corticosteroid treatment for immune-mediated AEs. No viral flares of hepatitis B virus or hepatitis C virus were observed.
Table 3.
AEsa in all treated patients.
| Patients | ||
|---|---|---|
| N = 51 | ||
| n (%) | Any grade | Grade 3–5 |
| Treatment-emergent AEs | 49 (96) | 32 (63) |
| Treatment-related AEs | 28 (55) | 8 (16)b |
| Serious AEs | 21 (41) | 21 (41) |
| Patients | ||
|---|---|---|
| N = 51 | ||
| Common AEs (incidence ≥10% of patients, any grade) | Any grade | Grade 3c |
| Fatigue | 21 (41) | 0 |
| Edema peripheral | 14 (28) | 1 (2) |
| Diarrhea | 13 (26) | 1 (2) |
| Abdominal pain | 9 (18) | 2 (4) |
| Cough | 8 (16) | 1 (2) |
| Decreased appetite | 8 (16) | 0 |
| Asthenia | 7 (14) | 2 (4) |
| Ascites | 6 (12) | 5 (10) |
| Dyspnea | 6 (12) | 2 (4) |
| Hypothyroidism | 6 (12) | 0 |
| Pruritus | 6 (12) | 1 (2) |
| Pyrexia | 6 (12) | 0 |
| Rash | 6 (12) | 1 (2) |
aGraded on the basis of the NCI Common Terminology Criteria for Adverse Events version 4.0.
bAll were grade 3 except in 1 patient, who had treatment-related grade 4 increased blood bilirubin, grade 4 encephalopathy, and grade 5 myocarditis.
cNo grade 4 or 5 event was reported among common treatment-emergent AEs.
Discussion
Our results show that pembrolizumab monotherapy provided durable antitumor activity and promising OS in patients with advanced HCC who had not received prior systemic therapy. We observed a confirmed ORR of 16% per RECIST 1.1 by central imaging review, and this benefit was generally consistent across clinical subgroups. The responses were durable, with median DOR of 16 months. 73% of the objective responses lasted for at least 12 months based on Kaplan–Meier estimates. Median PFS was 4 months, with an estimated PFS rate at 12 months of 28%. On the basis of the prespecified exploratory analysis, mRECIST assessment was consistent with RECIST assessment for evaluating response to pembrolizumab monotherapy in this patient population.
Grade ≥3 treatment-related AEs occurred in 16% of patients and 6% of patients discontinued treatment due to treatment-related AEs. Overall, the safety profile with pembrolizumab in this cohort was manageable and generally consistent with that previously observed for pembrolizumab monotherapy in advanced HCC in the second-line setting (cohort 1 of our study; ref. 11).
Approved first-line systemic therapies for advanced HCC include sorafenib (5, 6), lenvatinib (7), and the combination of atezolizumab plus bevacizumab (8, 18). The role of single-agent checkpoint inhibitors in the first-line setting remains to be defined. In CheckMate 459, nivolumab monotherapy demonstrated an ORR of 15% and a median OS of 16.4 months, although the primary endpoint of OS versus sorafenib was not met (HR, 0.85; P = 0.075; ref. 19). In our study, the observed efficacy with pembrolizumab was in line with prior findings for immune checkpoint inhibitors in this setting. Our data suggest promising antitumor activity of pembrolizumab and support the investigation of pembrolizumab-based regimens in the HCC therapeutic landscape. Taking into consideration the safety/tolerability profile as well as antitumor activity, pembrolizumab monotherapy could be an alternative option for patients with contraindications to combination therapies or antiangiogenic therapies.
Other studies have also suggested that immune checkpoint inhibitors alone or in combination with other therapies may provide a clinical benefit for patients with HCC. Among clinical trials investigating immunotherapy as second-line therapy for HCC, KEYNOTE-394, a phase III trial of pembrolizumab in Asian patients with HCC, also recently read out positive for OS, PFS, and ORR compared with placebo in patients with previously treated HCC (14). Although final analysis is not currently available, the phase III COSMIC 312 study reported a statistically significant improvement in PFS with first-line atezolizumab plus cabozantinib versus sorafenib in patients with advanced HCC (20). The phase III HIMALAYA trial reported a statistically significant OS improvement with the combination of a single priming dose of tremelimumab (anti–CTLA-4) and durvalumab (anti–PD-L1) followed by durvalumab monotherapy, and noninferior OS with durvalumab monotherapy only, both versus sorafenib as first-line therapy for HCC (21). The ongoing phase III LEAP-002 trial is investigating the combination of pembrolizumab and lenvatinib as first-line therapy for advanced HCC (22).
Limitations of KEYNOTE-224 include the single-arm design, the modest sample size, and relatively small numbers of patients with a viral etiology for HCC. Subgroup analyses were also performed in small patient numbers, although confirmed responses were observed across various patient baseline characteristics, such as disease etiology. Recent data suggest that nonalcoholic steatohepatitis as an etiology leading to HCC may be important to collect (23, 24). Our study did not collect this etiology, but future studies should consider doing so. Furthermore, in this study, the value of subgroup analyses is limited, although both viral and nonviral etiology patients benefited from pembrolizumab.
Other ongoing phase III trials investigating pembrolizumab-based regimens in HCC that may inform treatment selection in various settings include KEYNOTE-937 of pembrolizumab as adjuvant therapy (NCT03867084), and LEAP-012 of the combination of pembrolizumab and lenvatinib, in combination with transarterial chemoembolization for intermediate-stage HCC (NCT04246177). To identify patients who are responsive or resistant to immunotherapy and those who may not tolerate it, additional analyses aiming to define predictive biomarkers (e.g., germline DNA variations, tumor-specific DNA changes, PD-L1 expression) are ongoing in our HCC studies.
Overall, we demonstrate that pembrolizumab monotherapy provides durable antitumor activity and favorable OS in patients with advanced HCC who had not received prior systemic therapy, with a safety profile similar to that previously observed for pembrolizumab in advanced HCC in the second-line setting. Our findings support further evaluation of pembrolizumab-based regimens in the treatment of HCC.
Supplementary Material
Acknowledgments
The authors thank the patients and their families and all investigators and site personnel; Scot W. Ebbinghaus, Olga Kuznetsova, and Leonid Dubrovsky from Merck & Co., Inc., Kenilworth, NJ, for their input and discussions on data analysis. Medical writing assistance was provided by Yue Liu and Ina Nikolaeva of Merck & Co., Inc., Kenilworth, NJ. This work was supported by Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ. The funder had a role in study design, collection, analysis, and interpretation of data, and medical writing support. All authors had full access to the data and approved the final version of the manuscript for submission for publication.
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked advertisement in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
This article is featured in Highlights of This Issue, p. 2475
Footnotes
Note: Supplementary data for this article are available at Clinical Cancer Research Online (http://clincancerres.aacrjournals.org/).
Authors' Disclosures
G. Verset reports grants from Terumo, Bayer, Roche, and Eisai outside the submitted work. I. Borbath reports other support from Ipsen, Roche, and Eisai; grants from Servier; and other support from Bayer outside the submitted work. M. Karwal reports grants from Merck during the conduct of the study; and personal fees from Eisai outside the submitted work. C. Verslype reports grants from Bayer and Ipsen; and personal fees from Roche outside the submitted work. H. Van Vlierberghe reports other support from Merck during the conduct of the study. A. Kardosh reports other support from OHSU during the conduct of the study. V. Zagonel reports personal fees from Bristol-Myers Squibb, MSD, Ipsen, and EISAI; personal fees and nonfinancial support from Bayer and Roche; and personal fees from Janssen outside the submitted work. P. Stal reports grants from MSD during the conduct of the study. D. Sarker reports personal fees from MSD during the conduct of the study; personal fees and nonfinancial support from Ipsen; personal fees from Bayer, Eisai, AstraZeneca, Surface Oncology, Sirtex Medical, Roche, and AAA; nonfinancial support from MiNA Therapeutics and Medivir; and grants from UCB and Inspirata outside the submitted work. D.H. Palmer reports personal fees from MSD, Roche, and Boston Scientific; grants and personal fees from Bristol-Myers Squibb, Bayer, AstraZeneca, Sirtex Medical, and NuCana; and personal fees from Eisai outside the submitted work. A. Vogel reports personal fees from Roche, Bayer, Bristol-Myers Squibb, Eisai, AstraZeneca, Merck, Incyte, Ipsen, Pierre Fabre, MSD, Sirtex Medical, BTG, Servier, and Terumo; and personal fees from GlaxoSmithKline outside the submitted work. J. Edeline reports other support from MSD during the conduct of the study; personal fees from MSD, Roche, AstraZeneca, Ipsen, Bayer, and Eisai; and grants and personal fees from Bristol-Myers Squibb, BeiGene, and Boston Scientific outside the submitted work. S. Cattan reports personal fees from Bayer, Ipsen, Astra, Merck, and Roche during the conduct of the study; and personal fees from Roche outside the submitted work. M. Kudo reports personal fees from MSD during the conduct of the study; personal fees from Eli Lilly, Bayer, and Bristol-Myers Squibb; grants and personal fees from Eisai, EA Pharma, and Ono Pharmaceutical Co., Ltd.; grants from Roche, Gilead Sciences, Taiho Pharmaceutical, Sumitomo Dainippon Pharma, Takeda, Otsuka, and AbbVie; and grants and personal fees from Chugai outside the submitted work. A.L. Cheng reports personal fees from Bayer Healthcare, Eisai, Ono Pharmaceutical, AstraZeneca, Genentech/Roche, MSD, Ipsen Innovation, F. Hoffmann-La Roche Ltd., Bayer Yakuhin, Ltd., IQVIA, Amgen Taiwan, Chugai Pharmaceutical, and Bristol-Myers Squibb outside the submitted work. S. Ogasawara reports grants and personal fees from MSD during the conduct of the study; grants and personal fees from Bayer, Eisai, Eli Lilly, Chugai Pharmaceutical, and AstraZeneca; and personal fees from Takeda outside the submitted work. B. Daniele reports personal fees from MSD, AstraZeneca, Ipsen, Eisai, Roche, Amgen, Sanofi, Merck Serono, Lilly, and Bayer outside the submitted work. S.L. Chan reports other support from MSD during the conduct of the study; grants from MSD, Eisai, Ipsen, and Sirtex Medical; and other support from MSD, Eisai, AstraZeneca, and Roche outside the submitted work. J.J. Knox reports personal fees from F. Hoffmann-La Roche during the conduct of the study; and grants from F. Hoffmann-La Roche, Eisai Canada, and AstraZeneca Canada outside the submitted work. A.B. Siegel reports other support from Merck during the conduct of the study, and works for Merck. M. Chisamore reports other support from Merck & Co., Inc. during the conduct of the study; and other support from Merck & Co., Inc. outside the submitted work. A. Wang reports other support from Merck & Co., Inc. outside the submitted work. R.S. Finn reports grants and personal fees from Merck, Eisai, Pfizer, Bristol-Myers Squibb, Roche/Genentech, Eli Lilly, Adaptimmune, and Bayer; and personal fees from AstraZeneca, CStone, and Exelixis during the conduct of the study. A.X. Zhu reports personal fees from I-Mab, Merck, Lilly, Exelixis, Roche, Eisai, Bayer, and Sanofi outside the submitted work. No disclosures were reported by the other authors.
Authors' Contributions
G. Verset: Data curation, methodology, writing–original draft, writing–review and editing. I. Borbath: Data curation, formal analysis, writing–original draft, writing–review and editing. M. Karwal: Data curation, writing–review and editing. C. Verslype: Data curation, methodology, writing–review and editing. H. Van Vlierberghe: Data curation, methodology, writing–review and editing. A. Kardosh: Data curation, writing–review and editing. V. Zagonel: Data curation, formal analysis, writing–review and editing. P. Stal: Data curation, writing–review and editing. D. Sarker: Data curation, formal analysis, writing–original draft, writing–review and editing. D.H. Palmer: Data curation, writing–review and editing. A. Vogel: Data curation, methodology, writing–review and editing. J. Edeline: Data curation, writing–original draft, writing–review and editing. S. Cattan: Data curation, writing–review and editing. M. Kudo: Data curation, methodology, writing–review and editing. A.L. Cheng: Conceptualization, data curation, formal analysis, writing–review and editing. S. Ogasawara: Data curation, writing–review and editing. B. Daniele: Formal analysis, writing–review and editing. S.L. Chan: Conceptualization, writing–review and editing. J.J. Knox: Conceptualization, formal analysis, validation, writing–review and editing. S. Qin: Conceptualization, data curation, writing–review and editing. A.B. Siegel: Conceptualization, formal analysis, writing–review and editing. M. Chisamore: Conceptualization, data curation, formal analysis, writing–original draft, writing–review and editing. K. Hatogai: Formal analysis, writing–review and editing. A. Wang: Formal analysis, writing–original draft, writing–review and editing. R.S. Finn: Conceptualization, formal analysis, methodology, writing–review and editing. A.X. Zhu: Conceptualization, data curation, formal analysis, methodology, writing–review and editing.
References
- 1. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2018;68:394–424. [DOI] [PubMed] [Google Scholar]
- 2. Llovet JM, Kelley RK, Villanueva A, Singal AG, Pikarsky E, Roayaie S, et al. Hepatocellular carcinoma. Nat Rev Dis Primers 2021;7:6. [DOI] [PubMed] [Google Scholar]
- 3. Global Burden of Disease Liver Cancer Collaboration, Akinyemiju T, Abera S, Ahmed M, Alam N, Alemayohu MA, et al. The burden of primary liver cancer and underlying etiologies from 1990 to 2015 at the global, regional, and national level: results from the Global Burden of Disease Study 2015. JAMA Oncol 2017;3:1683–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Park J-W, Chen M, Colombo M, Roberts LR, Schwartz M, Chen P-J, et al. Global patterns of hepatocellular carcinoma management from diagnosis to death: the BRIDGE Study. Liver Int 2015;35:2155–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Cheng A-L, Kang Y-K, Chen Z, Tsao C-J, Qin S, Kim JS, et al. Efficacy and safety of sorafenib in patients in the Asia-Pacific region with advanced hepatocellular carcinoma: a phase III randomized, double-blind, placebo-controlled trial. Lancet Oncol 2009;10:25–34. [DOI] [PubMed] [Google Scholar]
- 6. Llovet JM, Ricci S, Mazzaferro V, Hilgard P, Gane E, Blanc J-F, et al. Sorafenib in advanced hepatocellular carcinoma. N Engl J Med 2008;359:378–90. [DOI] [PubMed] [Google Scholar]
- 7. Kudo M, Finn RS, Qin S, Han K-H, Ikeda K, Piscaglia F, et al. Lenvatinib versus sorafenib in first-line treatment of patients with unresectable hepatocellular carcinoma: a randomized phase III non-inferiority trial. Lancet 2018;391:1163–73. [DOI] [PubMed] [Google Scholar]
- 8. Finn RS, Qin S, Ikeda M, Galle PR, Ducreux M, Kim T-Y, et al. Atezolizumab plus bevacizumab in unresectable hepatocellular carcinoma. N Engl J Med 2020;382:1894–905. [DOI] [PubMed] [Google Scholar]
- 9. Ren Z, Xu J, Bai Y, Xu A, Cang S, Du C, et al. Sintilimab plus a bevacizumab biosimilar (IBI305) versus sorafenib in unresectable hepatocellular carcinoma (ORIENT-32): a randomized, open-label, phase II–III study. Lancet Oncol 2021;22:977–90. [DOI] [PubMed] [Google Scholar]
- 10. National Comprehensive Cancer Network: NCCN clinical practice guidelines in oncology: Hepatobiliary cancers (Version 5.2021). [DOI] [PubMed]
- 11. Zhu AX, Finn RS, Edeline J, Cattan S, Ogasawara S, Palmer D, et al. Pembrolizumab in patients with advanced hepatocellular carcinoma previously treated with sorafenib (KEYNOTE-224): a non-randomized, open-label phase II trial. Lancet Oncol 2018;19:940–52. [DOI] [PubMed] [Google Scholar]
- 12. KEYTRUDA® (pembrolizumab) injection, for intravenous use. Merck Sharp & Dohme Corp.: Whitehouse Station, NJ. [Google Scholar]
- 13. Finn RS, Ryoo B-Y, Merle P, Kudo M, Bouattour M, Lim HY, et al. Pembrolizumab as second-line therapy in patients with advanced hepatocellular carcinoma in KEYNOTE-240: a randomized, double-blind, phase III trial. J Clin Oncol 2020;38:193–202. [DOI] [PubMed] [Google Scholar]
- 14. Qin S, Chen Z, Fang W, Ren Z, Xu R, Ryoo B-Y, et al. Pembrolizumab plus best supportive care versus placebo plus best supportive care as second-line therapy in patients in Asia with advanced hepatocellular carcinoma (HCC): phase III KEYNOTE-394 study. J Clin Oncol 40:4s, 2022(suppl; abstr 383). [Google Scholar]
- 15. Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumors: revised RECIST guideline (version 1.1). Eur J Cancer 2009;45:228–47. [DOI] [PubMed] [Google Scholar]
- 16. Nishino M, Giobbie-Hurder A, Gargano M, Suda M, Ramaiya NH, Hodi FS. Developing a common language for tumor response to immunotherapy: immune-related response criteria using unidimensional measurements. Clin Cancer Res 2013;19:3936–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lencioni R, Llovet J. Modified RECIST (mRECIST) assessment for hepatocellular carcinoma. Semin Liver Dis 2010;30:52–60. [DOI] [PubMed] [Google Scholar]
- 18. Finn RS, Qin S, Ikeda M, Galle PR, Ducreux M, Kim T-Y, et al. IMbrave150: updated overall survival (OS) data from a global, randomized, open-label phase III study of atezolizumab (atezo) + bevacizumab (bev) versus sorafenib (sor) in patients (pts) with unresectable hepatocellular carcinoma (HCC). J Clin Oncol 39:3s, 2021(suppl; abstr 267). [Google Scholar]
- 19. Yau T, Park J-W, Finn RS, Cheng A-L, Mathurin P, Edeline J, et al. Nivolumab versus sorafenib in advanced hepatocellular carcinoma (CheckMate 459): a randomized, multicenter, open-label, phase III trial. Lancet Oncol 2022;23:77–90. [DOI] [PubMed] [Google Scholar]
- 20. Exelixis, Inc (June 28, 2021) Exelixis and Ipsen announce cabozantinib in combination with an immune checkpoint inhibitor significantly improved progression-free survival in phase III cosmic-312 pivotal trial in patients with previously untreated advanced liver cancer [press release]. Available from: https://ir.exelixis.com/news-releases/news-release-details/exelixis-and-ipsen-announce-cabozantinib-combination-immune.
- 21. Abou-Alfa GK, Chan SL, Kudo M, Lau G, Kelly RK, Furuse J, et al. Phase III randomized, open-label, multicenter study of tremelimumab (T) and durvalumab (D) as first-line therapy in patients (pts) with unresectable hepatocellular carcinoma (uHCC): HIMALAYA. J Clin Oncol 40:4s, 2022(suppl; abstr 379). [Google Scholar]
- 22. Llovet JM, Kudo M, Cheng A-L, Finn RS, Galle PR, Kaneko S, et al. Lenvatinib (len) plus pembrolizumab (pembro) for the first-line treatment of patients (pts) with advanced hepatocellular carcinoma (HCC): phase III LEAP-002 study. J Clin Oncol 2019;37:TPS4152. [Google Scholar]
- 23. Pfister D, Núñez NG, Pinyol R, Govaere O, Pinter M, Szydlowska M, et al. NASH limits antitumor surveillance in immunotherapy-treated HCC. Nature 2021;592:450–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kelley RK, Greten TF. Hepatocellular carcinoma: origins and outcomes. N Engl J Med 2021;385:280–2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.