Abstract
Objective:
Engaging youth and caregivers as active collaborators in the treatment planning process is a patient-centered approach with the potential to facilitate the personalization of established evidence-based treatments. This study is the first randomized clinical trial to evaluate shared decision-making (SDM) to plan youth psychotherapy.
Method:
Forty youth (7–15 years; 33% ethnic minority) were randomly assigned to psychosocial treatment planned using SDM (n = 20) or planned primarily by the clinician (n = 20). In the SDM condition, clinicians guided youth and caregivers through a collaborative treatment planning process that relies on research findings to inform three primary decisions: 1) treatment target problem(s), 2) treatment participants, and 3) treatment techniques. Assessments occurred at baseline, following treatment planning, midtreatment, and posttreatment.
Results:
Youth and caregivers in the SDM condition reported significantly greater involvement in the treatment planning process compared to their counterparts in the clinician-guided condition (U = 123.00, p = .037; U = 84.50, p = .014, respectively) and SDM caregivers reported significantly lower decisional conflict (U = 72.00, p = .004) and decisional regret (U = 73.50, p = .020). Supporting the feasibility of successful SDM implementation, there were no significant differences between conditions on treatment length, satisfaction with decisions, or engagement. There were no significant diagnostic or symptom differences between conditions.
Conclusions:
Planning psychosocial treatments in collaboration with youth and caregivers is a promising way to support youth and caregiver autonomy and plan evidence-based treatments that are responsive to patient preferences, culture, and values.
Keywords: RCT, child, shared decision-making, treatment planning, treatment personalization
Introduction
Involving patients in the creation of treatment plans that are responsive to their values, preferences, and self-identified needs has garnered considerable rhetorical support (e.g., American Psychological Association [APA], 2006) and placing families at the center of control/care has a long and important history in the concept of a “system of care” (Stroul & Friedman, 1986) and wraparound (Bruns et al., 2014). Yet centering caregiver and youth voices has sometimes come at the expense of providing evidence-based treatments (see Bruns et al., 2014). There are no clear guides to support clinicians looking to collaborate with families to plan treatments grounded in evidence-based treatment techniques and there are insufficient data on the feasibility, acceptability, and efficacy of planning treatments collaboratively with youth and caregivers for youth mental health.
Shared decision-making (SDM) is an interactive process in which clinicians and patients collaborate to make healthcare decisions (Langer & Jensen-Doss, 2018). Although research supports SDM’s effectiveness for mental health concerns (e.g., Loh et al., 2007), research focused on using SDM to plan youth mental health treatments has been quite limited and mostly focused on older youth, parents only, and making medication decisions (Cheng et al., 2017). This is unfortunate because: 1) even younger youth are capable of being involved in decision-making (Alderson et al., 2006) and have treatment preferences (Langer et al., 2020), and 2) most caregivers and youth may prefer psychotherapy to medication, meaning medication-focused SDM may exclude the most preferred options (Lewin et al., 2014). Ideally, in addition to aligning with values of patient autonomy and empowerment, SDM may increase treatment plan satisfaction, treatment engagement, and, relatedly, treatment outcome.
At the same time, there are several challenges in conducting SDM for youth psychotherapy: making treatment planning information and discussions accessible to youth of varying developmental levels; navigating caregiver—child disagreement; discussing more complex treatment tasks (e.g., exposure) which may be harder to understand than medication (e.g., swallow the pill); and summarizing a research literature that more frequently reports on the comparative effectiveness of treatment packages (e.g., CBT) instead of treatment elements (e.g., exposure). Thus, there is a need for an SDM protocol that effectively and efficiently engages youth and caregivers in planning psychosocial treatments. To our knowledge, SDM for youth psychotherapy has never been compared, using a randomized design, to standard, clinician-guided care. The present study tested our hypotheses that SDM 1) is feasible to conduct, 2) is acceptable to caregivers and youth, 3) and leads to increased family involvement in decision-making without increased decision regret or decreased self-efficacy. Due to the preliminary nature of this trial and the similarity of treatment techniques between conditions, we did not form hypotheses regarding symptom and diagnostic outcomes.
Method
Participants
Participants were youth (N = 40), 7–15 years old (M = 10.95, SD = 2.54), and their caregivers who sought treatment for anxiety or depression at a specialty clinic. Eligible youth a) met criteria for a principal diagnosis of major depressive disorder, dysthymic disorder, generalized anxiety disorder, separation anxiety disorder, social phobia, or specific phobia and b) if taking psychiatric medication, were on a stable dose for at least three months. Youth were excluded if they a) had current suicidal intent or an attempt or related hospitalization in the past three months), b) had severe physical or mental challenges, or c) were in additional ongoing psychosocial treatment. Tables 1 and 2 present sample demographics and diagnostic categories.
Table 1.
Baseline Demographic Characteristics Across Full Sample and by Condition
| Treatment Planning Condition | |||||||
|---|---|---|---|---|---|---|---|
|
|
|||||||
| Full Sample | Shared Decision Making | Clinician Guided | |||||
|
|
|
|
|||||
| (N = 40) | (n = 20) | (n = 20) | |||||
|
|
|
|
|||||
| Characteristic | N | % | N | % | N | % | Significance Test |
| Gender | χ2(1, N = 40) = .40, p = .525 | ||||||
| Female | 22 | 55.0 | 12 | 60.0 | 10 | 50.0 | |
| Male | 18 | 45.00 | 8 | 40.0 | 10 | 50.0 | |
| Ethnicity | χ2(1, N = 40) = 2.06, p = .151 | ||||||
| Hispanic/Latino | 5 | 12.5 | 4 | 20.0 | 1 | 5.0 | |
| Non-Hispanic/Latino | 35 | 87.5 | 16 | 80.0 | 19 | 95.0 | |
| Race | χ2(4, N = 40) = 4.53, p = .339 | ||||||
| White | 27 | 67.5 | 12 | 60.0 | 15 | 75.0 | |
| Black/African American | 5 | 12.5 | 3 | 15.0 | 2 | 10.0 | |
| Asian | 4 | 10.0 | 2 | 10.0 | 2 | 10.0 | |
| Multiracial | 3 | 7.5 | 3 | 15.0 | 1 | 5.0 | |
| Other | 1 | 2.5 | 0 | 0.0 | 1 | 5.0 | |
| Household Income | χ2(1, N = 40) = .63, p = .429 | ||||||
| <$60,000 | 8 | 20.0 | 5 | 25.0 | 3 | 85.0 | |
| >=$60,000 | 32 | 80.0 | 15 | 75.0 | 17 | 15.0 | |
| Caregiver Education Level | χ2(3, N = 40) = 1.56, p = .670 | ||||||
| High school | 1 | 2.5 | 1 | 5.0 | 0 | 0.0 | |
| Some college | 3 | 7.5 | 2 | 10.0 | 1 | 5.0 | |
| Bachelor’s degree | 18 | 45.0 | 9 | 45.0 | 9 | 45.0 | |
| Graduate degree | 18 | 45.0 | 8 | 40.0 | 10 | 50.0 | |
|
| |||||||
| Mean | SD | Mean | SD | Mean | SD | ||
|
| |||||||
| Age (in years)a | 10.95 | 2.54 | 11.3 | 2.54 | 10.6 | 2.56 | U = 170.50, z = −.81, p = .421, r = .13 |
Note. “Other” Race = Did not specify.
Table 2.
Baseline Clinical Characteristics Across Full Sample and by Condition
| Treatment Planning Condition | |||||||
|---|---|---|---|---|---|---|---|
|
|
|||||||
| Full Sample | Shared Decision Making | Clinician Guided | |||||
| (N = 40) | (n = 20) | (n = 20) | |||||
|
|
|
|
|||||
| Characteristic | n | % | n | % | n | % | Significance Test |
| Diagnostic Category Present | |||||||
| Anxiety Disorder | 40 | 100.0 | 20 | 100.0 | 20 | 100.0 | N/A |
| Depressive Disorder | 13 | 32.5 | 7 | 35.0 | 6 | 30.0 | χ2(1, N = 40) = .11, p = .736 |
| Behavior Disorder | 4 | 10.0 | 2 | 10.0 | 2 | 10.0 | χ2(1, N = 40) = .00, p = 1.000 |
| Other Disorder | 4 | 10.0 | 2 | 10.0 | 2 | 10.0 | χ2(1, N = 40) = .00, p = 1.000 |
|
| |||||||
| Median | Median | Median | |||||
|
| |||||||
| Primary Diagnosis CSR | 5 | 5 | 5 | U = 148.50, z = −1.54, p = .125, r = −.24 | |||
| Number of Diagnoses | 2 | 3 | 2 | U= 168.00, z = −.91, p = .363, r = −.14 | |||
| MASC-Child | 47.12 | 47.12 | 48.00 | U = 200.00, z = .00, p = 1.000, r = .00 | |||
| MASC- Parent | 52.00 | 54.00 | 49.50 | U= 188.00, z = −.33, p = .745, r = −.05 | |||
| CDI- Child | 7.50 | 8.00 | 7.50 | U= 191.50, z = −.23, p = .817, r = −.04 | |||
| CDI- Parent | 15.00 | 17.00 | 13.50 | U = 159.00, z = −1.11, p = .267, r = −.18 | |||
| MYTS- Child | 3.13 | 3.13 | 3.13 | U= 163.50, z = −.75, p = .456, r = −.12 | |||
| TOES- Child | 2.50 | 2.50 | 2.50 | U= 172.50, z = −.75, p = .454, r = −.12 | |||
| TOES- Parent | 2.67 | 2.50 | 2.67 | U= 184.00, z = −.44, p = .662, r = −.07 | |||
| DSE- Child | 72.73 | 75.00 | 67.05 | U = 153.50, z = −1.26, p = .207, r = −.20 | |||
| DSE- Parent | 88.64 | 93.18 | 85.23 | U = 163.50, z = −1.00, p = .316, r = −.16 | |||
Note. N/A = Statistic cannot be computed because variable is constant; Other Disorder = Somatic Symptom Disorder, Enuresis, Other Specified Eating & Feeding Disorder, Insomnia; CSR = Clinical Severity Rating assigned via the Anxiety Disorders Interview Schedule-IV- Child-Parent Version; MASC = Multidimensional Anxiety Scale for Children; CDI = Children’s Depression Inventory; MYTS = Motivation for Youth Treatment Scale; TOES = Treatment Outcome Expectations Scale; DSE = Decisional Self-Efficacy Scale.
Procedures
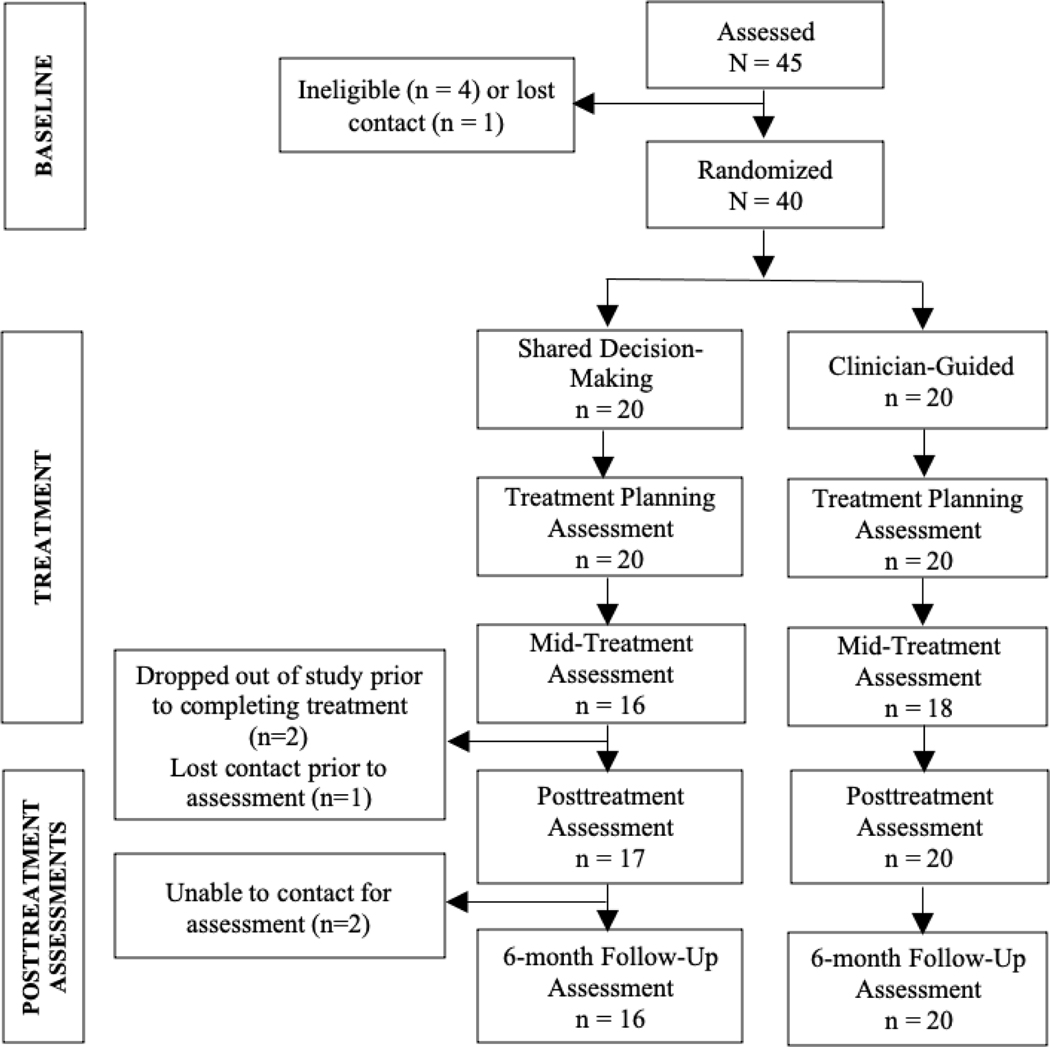
Figure 1 presents the flow of participants through the study and the assessment schedule. Participants received compensation for diagnostic assessments; treatment was provided at no cost. The IRB approved study procedures; ClinicalTrials.gov: NCT03610373.
Figure 1.
Flow of Participants Across Study Phases
Note. Treatment Planning Assessments were conducted after the initial session. Mid-Treatment Assessments were conducted after session eight. Four SDM participants and two CG participants had eight or fewer sessions and did not complete the mid-treatment assessment. One SDM participant did not complete the posttreatment assessment but did complete the 6-month follow-up assessment. Six-month follow-up assessment data are not included in the present paper.
In the Shared Decision-Making (SDM) Condition, clinicians followed an SDM protocol (developed for this study) to guide them in collaborating with youth and caregivers to plan each treatment (see Table 3). The entire initial session focused on treatment planning using SDM, and the SDM framework guided scheduled or impromptu treatment planning discussions throughout treatment. In the Clinician-Guided (CG) Condition, clinicians, in consultation with their supervisor, planned treatment based on baseline assessment data. CG clinicians shared treatment plans with families, but participants were explicitly excluded from formulating the treatment plan. If caregivers or youth asked for changes in the treatment plan, CG clinicians thanked the caregiver or youth for sharing their opinion, and said that they would consider their request but that they (the clinician) would decide. Each clinician served in both conditions.
Table 3.
A Shared-Decision Making (SDM) Protocol for Treatment Planning in Youth Psychotherapy
| Step | DesDescription and Goal | Adapting SDM for Youth Psychotherapy | Corresponding Practices in the Clinician-Guided Condition |
|---|---|---|---|
|
|
|||
| 1. Introduce SDM | • Clinician shares the overall session goal is to work together to design a treatment plan that will work best for family. • Clinician identifies three decisions to be made: a) What are the primary treatment targets? (e.g., low mood or social phobia) b) Who will participate in treatment? (e.g., youth alone, caregivers and youth) and c) What will the treatment components be? (e.g., exposure, behavioral activation) |
• Clinician emphasizes importance of each person’s perspective, especially the youth’s perspective. • Family has opportunity to invite others (e.g., additional caregivers) to engage in treatment planning with them. |
• Clinician shares that the overall session goal is to review the treatment plan that the clinician has already developed based on the assessment information. |
| 2. Practice collaborative decision-making | • Clinician describes SDM as a collaborative approach to making decisions, with opportunities for youth, caregivers, and clinicians to share their ideas, preferences, and perspectives while considering the available evidence. | • To practice making decisions collaboratively, families have the option to engage in an “SDM learning activity” (i.e., board game) which teaches SDM principles relevant to treatment planning for youth psychotherapy. | • Clinician describes how they developed the treatment plan using their understanding of the research literature, their understanding of the family’s needs, and their clinical experience. |
| 3. Select treatment targets | • Clinician summarizes baseline assessment results. • Clinician facilitates discussion focused on identifying the primary treatment targets. |
• Caregiver(s), youth, and clinician take turns sharing their ideas and perspectives. The pros and cons of addressing each target problem are considered until consensus is reached. • More than one target may be added to the treatment plan to accommodate varying perspectives. |
• Clinician tells the family what the treatment targets will be, based on the family’s report and the assessor’s diagnostic impressions. |
| 4. Discuss treatment-related values | • Clinician highlights how unique perspectives about treatment characteristics may inform treatment planning. | • Clinician discusses caregiver and youth values regarding decision-making and mental health treatment (e.g., how much information is important to know, who should have the final say). | • Clinician does not discuss treatment-related values. |
| 5. Introduce the evidence | • Clinician provides basic psychoeducation about the existence of treatment efficacy/effectiveness research in a developmentally appropriate manner. • To inform families and empower them to participate in making decisions, clinicians reviewed the available research evidence with families using the PracticeWise Evidence-Based Services (PWEBS) databasea,b. |
• Families have the option to conduct the PWEBS search with the clinician or have the clinician conduct the PWEBS search and provide information to the family. | • Clinician notes that this treatment plan is based on the available research evidence. • Clinician does not share or review evidence with the family. |
| 6. Select treatment participants | • Clinician presents the research findings related to treatment participants for the youth’s presenting issues and, through discussion, determines who will participate in treatment. | • Clinician reviews caregiver and youth preferences for who to involve in treatment sessions. • Pros and cons of including various participants can be considered, as needed. • The SDM protocol includes more advanced steps to resolve intractable caregiver—youth disagreements, though collaborative discussion was sufficient to make a plan for all families in this study. |
• Clinician tells the family who will participate in treatment and how each person will participate. |
| 7. Select treatment components | • Clinician presents the research findings related to treatment components for the youth’s presenting issues. | • To simplify the presentation of research findings, clinicians presented one practice element at a time. • Clinicians, caregivers, and youth then discuss pros and cons of each treatment element and decide whether to include or not in the treatment plan. • In cases of disagreement about a practice element, the practice element could be placed on the treatment plan as a “back up” skill that would be considered again if needed. |
• Clinician shares the names (and brief, 1–2 sentence descriptions) of each treatment component on the treatment plan. |
| 8. Plan symptom tracking and follow-up | • Clinician provides information about progress monitoring and introduces a method for tracking progress. • A plan is made for in-session progress check-ins as well as timing of follow-up SDM treatment planning conversations. |
• Clinician assesses caregiver and youth preferences for discussing progress in treatment sessions. | • Clinician provides information about progress monitoring and introduces a method for tracking progress. • Clinician informs family that they will monitor improvement so that they (i.e., the clinician) can make changes to the treatment plan as needed. |
The PWEBS database (PracticeWise, 2018) includes more than 1,200 RCTs for youth mental health treatment, providing comprehensive data on each treatment’s empirical support. PWEBS details the elements found in each study protocol as well as other study characteristics (e.g., sample demographics) to refine one’s appraisal of the research evidence for specific patients. In the SDM protocol, the clinician conducts a search (with youth and caregiver(s) when they are interested) using the specific characteristics of the youth (i.e., age, gender, problem type). Search results related to treatment format (e.g., youth only, parent only, caregiver and youth) and practice elements (e.g., exposures, behavioral activation) are reviewed.
No youths or caregivers in the current study requested additional practice elements or treatment approaches (e.g., psychodynamic, mindfulness) not present in PWEBS search results. In the rare case that there was not a specific MATCH module fitting a PWEBS practice element, the clinician would use the corresponding PracticeWise practice guide.
All youth and families received the same core treatment – the Modular Approach to Therapy for Children (MATCH; Chorpita & Weisz, 2009). MATCH includes a collection of modules that correspond to the treatment procedures found in standard evidence-based treatments for youth anxiety, depression, behavioral disorders, and trauma. The process of selecting and organizing modules for each family differed by condition. See Supplemental Material A for the clinician training protocol and adherence to SDM and MATCH protocols.
Measures
Assessors masked to condition determined youth diagnoses using the Anxiety Disorders Interview Schedule for DSM-IV, Child/Parent (Silverman & Albano, 1997); caregivers and youth completed the Multidimensional Anxiety Scale for Children (March et al., 1997) and the Children’s Depression Inventory (Kovacs, 1992). To measure clinical severity and treatment improvement, assessors completed the Clinical Global Impression – Severity and Improvement (Guy, 1976). Caregivers reported youth and family demographic and background information. To measure decision-making and related constructs, caregivers and youth completed the Decisional Conflict Scale (O’Connor, 1995), the Satisfaction with Decision Scale (Holmes-Rovner et al., 1996), the 11-item Decision Self-Efficacy Scale (O’Connor, 1995), the Decisional Regret Scale (Brehaut et al., 2003), and the Shared Decision-Making Questionnaire-9 (Kriston et al., 2010). Decision-making measure wording was minimally modified for youth and caregivers to report on youth psychotherapy. To track treatment process and contents, clinicians completed treatment session clinical notes including content covered and treatment planning discussions. Clinicians also tracked session attendance and participants. Youth and caregivers completed the Treatment Outcomes Expectation Scale and youth completed the Motivation for Youth Treatment Scale (Bickman et al., 2010). At later assessment points, youth and caregivers completed the Therapeutic Alliance Scale for Children (Shirk & Saiz, 1992). See Supplemental Material B for additional information on study measures and administration timing.
Data Analyses
Descriptive statistics summarize the relevant variables at each timepoint. Analyses testing for differences between conditions used chi-square for categorical variables and Mann-Whitney U for continuous variables. The Mann-Whitney U test is the non-parametric analog of the t test, not requiring the standard t test assumptions be met, making it appropriate for smaller samples. Wilcoxon signed-ranks tests, the non-parametric analog of the related-samples t test, tested for changes in continuous outcomes within condition. Two-way mixed analyses of variance (ANOVAs) examined changes between conditions and across time on continuous outcomes.
If fewer than 20% of a measure’s items were missing, the missing items were imputed based on the mean of the participant’s completed items on that measure. If more than 20% of a measure’s items were missing, as the sample size precluded more comprehensive missing data techniques, participants with missing data on a specific measure were excluded on an analysis-by-analysis basis. The exception being for the posttreatment, intent-to-treat analyses, we imputed missing posttreatment data to be equal to the last observation completed.
Results
Baseline descriptive statistics and comparisons across conditions are displayed for sociodemographic variables (Table 1) and clinical characteristics (Table 2).
Feasibility and Acceptability
To assess the feasibility and acceptability of using SDM to plan treatments, we asked several questions: Would using SDM (1) extend treatment length, (2) decrease attendance, (3) increase early withdrawal from treatment, or (4) impact satisfaction with treatment planning decisions. Results (see Table 4) show that treatment lengths were not significantly different between SDM and CG conditions. There was also no significant difference in treatment attendance (i.e., percentage of scheduled sessions attended (Table 4), nor in treatment completion, χ2(1) = 1.56, p = .212, ϕ = .20. Caregivers receiving SDM reported significantly greater satisfaction with decisions related to treatment planning.
Table 4.
Feasibility and Accessibility Across Full Sample and by Condition
| Treatment Planning Condition | ||||
|---|---|---|---|---|
|
|
||||
| Full Sample | Shared Decision Making | Clinician Guided | ||
| (N = 40) | (n = 20) | (n = 20) | ||
|
|
|
|
||
| Characteristic | Median | Median | Median | Significance Test |
| Number of sessions | 18.0 | 17.0 | 18.0 | U = 168.00, z = −.87, p = .385, r = −.14 |
| Treatment length in weeks | 25.0 | 25.0 | 25.5 | U = 180.00, z = −.54, p = .588, r = −.09) |
| Percentage of scheduled sessions attended a | 0.85 | 0.86 | 0.84 | U = 161.00, z = −.56,p = .577, r = −.09 |
| Satisfaction with treatment decisions- Youth | 4.0 | 4.0 | 3.4 | U = 154.5, z = −1.24,p = .216, r = −.20 |
| Satisfaction with treatment decisions-Caregiver | 4.0 | 4.5 | 3.5 | U = 84.0, z = −2.49, p = .013, r = .42 |
Note.
Analysis excluded two youth in the SDM condition whose treatment entailed fewer than four sessions
SDM vs. CG Treatment Plans and Planning During Treatment
Treatment plan components did not significantly differ between conditions (see Table 5). Nearly all treatment plans included the treatment components that are most common in effective treatment protocols.1 During treatment, treatment plans were discussed and modified (from the original plan) in a significantly higher percentage of sessions in the SDM condition (MdnSDM = 20.87, MdnCG = 11.11, U(N = 31) = 47.00, z = −2.89, p = .004, r = −.52; MdnSDM = 7.18, MdnCG = 0.0, U(N = 31) = 27.00, z = −3.82, p < .001, r = −.69, respectively).2
Table 5.
Treatment Components in Initial Treatment Plans by Condition
| Skill | Included at all | Included as a primary skill | ||||
|---|---|---|---|---|---|---|
|
|
||||||
| Shared Decision Making (n = 20) | Clinician Guided (n = 20) | Shared Decision Making (n = 20) | Clinician Guided (n = 20) | |||
|
|
|
|
||||
| Skill | n (%) | n (%) | Significance Test | n (%) | n (%) | Significance Test |
| Psychoeducation-Child | 20 (100) | 20 (100) | N/A | 19 (95) | 20 (100) | χ2(1, N = 40) = 1.03, p = .311 |
| Psychoeducation- Parent | 20 (100) | 20 (100) | N/A | 20 (100) | 20 (100) | N/A |
| Exposure | 19 (95) | 20 (100) | χ2(1, N = 40) = 1.03, p = .311 | 17 (85) | 19 (95) | χ2(1, N = 40) = 1.11, p = .292 |
| Cognitive | 19 (95) | 20 (100) | χ2(1, N = 40) = 1.03, p = .311 | 18 (90) | 14 (70) | χ2(1, N = 40) = 2.50, p = .114 |
| Behavioral Activation | 4 (20) | 7 (35) | χ2(1, N = 40) = 1.13, p = .288 | 3 (15) | 5 (25) | χ2(1, N = 40) = .63, p = .429 |
| Problem Solving | 9 (45) | 11 (55) | χ2(1, N = 40) = .40, p = .527 | 9 (45) | 5 (25) | χ2(1, N = 40) = 1.76, p = .185 |
| Rewards | 8 (40) | 14 (70) | χ2(1, N = 40) = 3.64, p = .057 | 4 (20) | 2 (10) | χ2(1, N = 40) = .78, p = .376 |
| Parenting Skills | 1 (5) | 3 (15) | χ2(1, N = 40) = 1.11, p = .292 | 1 (5) | 1 (5) | χ2(1, N = 40) = .00, p = 1.000 |
| Maintenance | 18 (90) | 20 (100) | χ2(1, N = 40) = 2.11, p = .147 | 18 (90) | 20 (100) | χ2(1, N = 40) = 2.11, p = =.147 |
Note. N/A = Statistic cannot be computed because variable is constant.
Decision-Making and Related Constructs
Table 6 reports medians and nonparametric inferential statistics for between condition comparisons on decision-making and related constructs. After initial treatment planning, SDM and CG youth did not significantly differ on their treatment outcome expectations, decisional conflict, motivation for treatment, or, at the mid-treatment assessment point, decisional regret. Youth in the SDM condition reported significantly lower alliance scores directly following the treatment planning session, yet this finding was not present at the mid or posttreatment assessments. Youth in the SDM condition reported significantly more involvement in the treatment planning process. Youth reports of decision self-efficacy did not change significantly from before (Mdn = 75.0) to after (Mdn = 78.4) the SDM session (t = 112.5, z = −1.18, p = .239).
Table 6.
Decision-Making and Related Constructs in the Full Sample and by Condition
| Treatment Planning Condition | |||||
|---|---|---|---|---|---|
|
|
|||||
| Full Sample | Shared Decision Making | Clinician Guided | |||
|
|
|
|
|||
| Variable | Time Point | Median (n) | Median (n) | Median (n) | Significance Test |
| DCS-Child | S1 | 31.25 (40) | 27.34 (20) | 37.50 (20) | U = 141.00 z = −1.60, p = .110, r = −.25 |
| DCS-Parent | S1 | 26.56 (36) | 10.94 (19) | 40.63 (17) | U = 72.00, z = −2.85, p = .004, r = −.48 |
| SWD-Child | S1 | 4.00 (40) | 4.00 (20) | 3.42 (20) | U = 154.40, z = −1.24, p = .216, r = −.20 |
| SWD-Parent | S1 | 4.00 (36) | 4.50 (19) | 3.50 (17) | U = 84.00, z = −2.16, p = .030, r = −.36 |
| SDMQ- Child | S1 | 66.67 (40) | 76.67 (20) | 62.22 (20) | U = 123.00, z = −2.09, p = .037, r = −.33 |
| SDMQ-Parent | S1 | 81.11 (36) | 86.67 (19) | 57.78 (17) | U = 84.50, z = −2.45, p = .014, r = −.41 |
| MYTS-Child | S1 | 3.44 (40) | 3.38 (20) | 3.5 (20) | U = 169.50, z = −.83, p = .408, r = −.13 |
| TOES-Child | S1 | 2.50 (40) | 2.56 (20) | 2.50 (20) | U=180.50, z = −.53, p = .595, r = −.08 |
| TOES-Parent | S1 | 2.63 (36) | 2.63 (19) | 2.63 (17) | U=155.50, z = −.19, p = .848, r = −.03 |
| TASC-Child | S1 | 3.00 (39) | 2.86 (20) | 3.29 (19) | U = 106.00, z = − 2.38, p = .017, r = −.38 |
| TASC-Parent | S1 | 3.50 (36) | 3.43 (19) | 3.72 (17) | U = 94.00, z = − 2.16, p = .030, r = −.36 |
| MYTS-Child | S8 | 3.00 (34) | 3.00 (16) | 3.13 (18) | U = 141.00, z = −.10, p = .917, r = −.02 |
| TOES-Child | S8 | 2.38 (34) | 2.38 (16) | 2.50 (18) | U = 132.00, z = −.42, p = .677, r = −.07 |
| TOES-Parent | S8 | 2.75 (34) | 2.75 (16) | 2.69 (18) | U = 126.50, z = −.61, p = .540, r = −.10 |
| TASC-Child | S8 | 3.14 (34) | 3.07 (16) | 3.14 (18) | U = 119.00, z = −.87, p = .385, r = −.15 |
| TASC-Parent | S8 | 3.86 (33) | 3.79 (16) | 3.86 (17) | U = 99.00, z = −1.37, p = .171, r = −.24 |
| DRS-Child | S8 | 24.00 (29) | 27.24 (14) | 18.00 (15) | U = 79.00, z = −1.15, p = .249, r = −.21 |
| DRS-Parent | S8 | 19.00 (33) | 15.00 (15) | 20.00 (18) | U = 73.50, z = −2.32, p = .020, r = −.40 |
| TASC-Child | PT | 2.43 (37) | 2.29 (17) | 2.57 (20) | U = 126.5, z = −1.33, p = .182, r = −.22 |
| TASC-Parent | PT | 3.71 (37) | 3.71 (17) | 4.00 (20) | U = 119.00, z = −1.63, p = .103, r = −.27 |
Note. S1 = after the initial treatment planning session; S8 = after the 8th treatment session; PT = posttreatment assessment; DCS = Decisional Conflict Scale; SWD = Satisfaction with Decisions Scale; SDMQ = Shared Decision-Making Questionnaire; MYTS = Motivation for Youth Treatment Scale; TOES = Treatment Outcome Expectations Scale; TASC = Therapeutic Alliance Scale for Children; DRS = Decisional Regret Scale.
Caregivers also did not report a significant difference in treatment outcome expectations between conditions, however, SDM caregivers reported significantly lower decisional conflict and, at the midtreatment assessment point, significantly lower decisional regret. SDM caregivers also reported significantly higher participation in treatment planning and significantly lower alliance directly following the treatment planning session (but not at the mid or posttreatment assessments). Caregiver reports of decision self-efficacy did not change significantly from before (Mdn = 93.2) to after (Mdn = 88.6) the SDM session (t = 30.5, z = −0.67, p = .504).
Diagnoses, Symptoms, and Functioning
There are no significant posttreatment condition differences between conditions in these domains. Detailed descriptive and inferential statistics are provided in Table 7.
Table 7.
Diagnostic, Symptom, and Functioning Changes Across Full Sample and by Condition
| Shared Decision Making (n = 20) | Clinician Guided (n = 20) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||
| Baseline | Post-Treatment | Baseline | Post-Treatment | |||||||
|
|
|
|
|
|||||||
| Variable | n | % | n | % | n | % | n | % | Significance Test | Effect Size |
| Complete Diagnostic Remission | - | - | 5 | 25.00 | - | - | 7 | 35.00 | χ2(1, N = 40) = .48, p = .490 | Phi = .11 |
| CGIS-I: Very Much or Much Improveda | - | - | 7 | 41.18 | - | - | 10 | 50.00 | χ2(1, N = 40) = .29, p = .591 | Phi = .09 |
|
| ||||||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Time X Condition interaction effect | Effect Size | |
|
| ||||||||||
| Number of Diagnoses | 2.45 | 1.10 | 1.40 | 1.14 | 2.15 | 0.88 | 0.95 | 0.89 | F(1,38) = .25, p = .620 | η2 = .01 |
| CGIS-S | 4.95 | 0.67 | 4.00 | 0.97 | 4.70 | 0.73 | 3.55 | 1.05 | F(1,38) = .334, p = .567 | η2 = .01 |
| MASC-Child | 47.93 | 16.86 | 35.10 | 15.36 | 48.45 | 20.48 | 37.95 | 15.91 | F(1,38) = .15, p = .705 | η2 = .004 |
| MASC- Parent | 50.20 | 16.33 | 41.45 | 18.28 | 54.75 | 17.67 | 38.75 | 14.48 | F(1,38) = 3.79, p = .06 | η2 =.09 |
| CDI- Child | 8.90 | 5.89 | 5.95 | 7.19 | 10.40 | 10.34 | 5.10 | 6.05 | F(1,38) = .94, p = .338 | η2 =.02 |
| CDI- Parent | 17.40 | 6.42 | 12.35 | 8.16 | 15.15 | 7.58 | 8.25 | 5.17 | F(1,38) = .57, p = .455 | η2 =.02 |
Note.
SDM n = 17. CGIS-I = The Clinical Global Impression Scale- Impairment; CGIS-S = The Clinical Global Impression Scale- Severity; MASC = Multidimensional Anxiety Scale for Children; CDI = Children’s Depression Inventory.
Discussion
This first-of-its-kind trial establishes that it may be possible to personalize psychosocial treatments by including youth and caregivers in the treatment planning process. Beyond being possible, planning treatments using SDM led to significantly increased perceptions of involvement in treatment planning and some improved decision-making outcomes (e.g., decreased caregiver decisional conflict and decisional regret). Although SDM for youth mental health has been tested before (see Cheng et al., 2017), this is the first randomized trial to use SDM to plan psychosocial treatments engaging both caregivers and youth, supporting youth autonomy. This research advances our understanding of how to engage patients in planning psychosocial treatments that reflect the best evidence available while remaining responsive to patient preferences, culture, and values.
Findings suggest that SDM is both feasible and acceptable. There was no evidence that planning treatments with SDM led to decreased treatment plan satisfaction, more treatment dropouts, or longer treatments. If these findings are replicated in an adequately powered study, it may be that these variables depend more on the treatment content and provider and less on the planning approach.
One potential barrier to SDM is the concern that doing so might lead to treatment plans that are less concordant with the evidence base. In the present study, however, SDM and CG treatment plans were largely similar. Families may rely on the evidence to inform their opinions, rely on evidence-informed clinician perspectives, or respond (as intended) to the SDM protocol’s approach of reviewing the most evidence-supported treatment components first. Alternatively, caregiver and youth preferences may coincidentally align with evidence-based recommendations. Non-significant treatment plan differences (i.e., trends; see Table 5) should be explored in larger samples. More frequent treatment plan modification in the SDM condition may reflect increased treatment responsiveness or comfort on the part of participants, however, this paper’s limited scope does not permit exploration of how the treatment plans changed.
SDM and CG conditions used the same modular treatment with largely similar treatment plans, so it is perhaps unsurprising that there were no significant SDM vs. CG diagnostic or symptoms differences. The impact of SDM on these outcomes may be more pronounced when the range of treatment options varies more widely (e.g., therapeutic modalities).
SDM’s impact may be most noticeable in perspectives on the decision-making process. Caregivers and youth each reported playing a greater role in decision-making in the SDM condition, confirming the efficacy of the SDM protocol at increasing engagement in treatment planning. Caregivers receiving SDM were also more satisfied with their decisions and reported less decisional conflict and decisional regret. These findings directly counter concerns that SDM will overburden patients and lead to increased conflict and regret about paths not chosen. Learning about the possibility that certain treatment approaches may not work did not lead to decreased expectations of treatment outcome. Youth and caregivers did, however, report significantly lower alliance scores directly after the SDM session relative to CG. It is possible that the large amount of content to cover in the initial SDM session limited rapport-focused activities. The lack of significant alliance differences between conditions at the mid- and posttreatment assessments supports this interpretation. Modifications to the SDM protocol may provide more time for alliance-building early in treatment.
Despite the novelty and significance of this preliminary trial, limitations include: 1) as a preliminary trial, the study is not sufficiently powered to interpret non-significant findings, 2) to isolate the effects of treatment planning, SDM and CG treatments were based on the same set of treatment elements, potentially artificially inflating treatment plan and outcome similarities, 3) this focused, in-depth SDM approach may have been too intense for some caregivers and youth, which may be reflected in the lower alliance scores directly after the SDM session. Future tests of SDM may explore alternative approaches (e.g., focusing first on rapport, distributing SDM tasks across multiple sessions, focusing on only overarching decisions).
SDM aligns with our values of autonomy and patient empowerment, yet there are multiple barriers to effectively implementing SDM, especially when planning psychotherapy with youth and caregivers. The present study demonstrated that caregivers and youth were able to participate in the treatment planning process using SDM and plan treatments using the evidence base. Future research should work to identify for whom SDM will be most effective and how to modify the SDM protocol in response to youth and caregiver needs and preferences.
Supplementary Material
Public Health Significance Statement:
This is the first randomized clinical trial evaluating shared decision-making (SDM) for youth psychotherapy. Results suggest that using SDM to plan treatments collaboratively with youth and caregivers is a feasible and acceptable option for youth with anxiety and depression.
Acknowledgments
This research was supported by National Institute of Mental Health grant K23-MH101238 (DAL).
Martha C. Tompson is an Associate Editor of Journal of Consulting and Clinical Psychology. We thank Annie Dantowitz, Erin O’Connor, Tessa Kritikos, Alex Keller, Lydia Chevalier, Alicia Fenley, Laura Nelson Darling, Emily Earley, Erika Trent, Lauren Silva, David Barlow, Lawrence Palinkas, Donna Pincus, Rachel Merson, and Ovsanna Leyfer for their incalculable contributions to this research, in addition to the entire team of the Child Program of the Center for Anxiety and Related Disorders at Boston University.
Footnotes
Although there were no significant differences between treatment plans, there may be some trends worth exploring in larger samples. For example, treatment plans in both conditions almost universally included exposure, but it was (non-significantly) more likely that SDM treatment plans would include exposure as a backup skill (i.e., a skill to be used if other skills did not work). SDM treatment plans, on the other hand, were more likely to include cognitive, problem solving, and rewards modules as primary.
Only families with four or more sessions were included in these analyses and these items were not included in data collection for the first seven cases.
Dr. Chorpita has an ownership interest in PracticeWise, LLC, which publishes the MATCH-ADTC protocol and the PracticeWise Evidence Based Services Database, both described in this study.
Contributor Information
David A. Langer, Department of Psychology, Suffolk University
Lindsay E. Holly, Department of Psychology, Marquette University
Celia E. Wills, College of Nursing Center on Healthy Aging, Self-Management and Complex Care, The Ohio State University
Martha C. Tompson, Department of Psychological and Brain Sciences, Boston University
Bruce F. Chorpita, Department of Psychology, University of California – Los Angeles
References
- Alderson P, Sutcliffe K, & Curtis K. (2006). Children’s competence to consent to medical treatment. Hastings Center Report, 36(6), 25–34. 10.1353/hcr.2006.0000 [DOI] [PubMed] [Google Scholar]
- American Psychological Association. (2006). Evidence-based practice in psychology: APA presidential task force on evidence-based practice. American Psychologist, 61(4), 271–285. [DOI] [PubMed] [Google Scholar]
- Bickman L, Athay M, Riemer M, Lambert E, Kelley S, Breda C, Tempesti T, Dew-Reeves S, Brannan A, & Vides de Andrade AR (eds.) (2010). Manual of the Peabody Treatment Progress Battery, 2nd ed. Nashville, TN: Vanderbilt University. [Google Scholar]
- Brehaut J, O’Connor A, Wood T, Hack T, Siminoff L, Gordon E, & Feldman-Stewart D. (2003). Validation of a decision regret scale. Medical Decision Making, 23, 281–292. [DOI] [PubMed] [Google Scholar]
- Bruns EJ, Walker JS, Bernstein A, Daleiden E, Pullmann MD, & Chorpita BF (2014). Family voice with informed choice: Coordinating wraparound with research-based treatment for children and adolescents. Journal of Clinical Child & Adolescent Psychology, 43(2), 256–269. 10.1080/15374416.2013.859081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng H, Hayes D, Edbrooke-Childs J, Martin K, Chapman L, & Wolpert M. (2017). What approaches for promoting shared decision-making are used in child mental health? A scoping review. Clinical Psychology & Psychotherapy, 24(6), O1495–O1511. [DOI] [PubMed] [Google Scholar]
- Chorpita BF, & Weisz JR (2009). Modular Approach to Therapy for Children with Anxiety, Depression, Trauma, or Conduct problems (MATCH-ADTC). [Google Scholar]
- Guy W (1976). ECDEU assessment manual for psychopharmacology. doi. 10.2172/7356647 [DOI] [Google Scholar]
- Holmes-Rovner M, Kroll J, Schmitt N, Rovner DR, Breer ML, Rothert ML, Padonu G, & Talarczyk G. (1996). Patient satisfaction with health care decisions: The satisfaction with decision scale. Medical Decision Making, 16(1), 58–64. [DOI] [PubMed] [Google Scholar]
- Kovacs M. (1992). Children’s depression inventory. Multi-Health Systems. [Google Scholar]
- Kriston L, Scholl I, Holzel L, Simon D, Loh A, & Harter M. (2010). The 9-item Shared Decision Making Questionnaire (SDM-Q-9). Development and psychometric properties in a primary care sample. Patient Education and Counseling, 80(1), 94–9. 10.1016/j.pec.2009.09.034 [DOI] [PubMed] [Google Scholar]
- Langer DA, & Jensen-Doss A. (2018). Shared decision-making in youth mental health care: Using the evidence to plan treatments collaboratively. Journal of Clinical Child & Adolescent Psychology, 47(5), 821–831. 10.1080/15374416.2016.1247358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langer DA, Kritikos TK, Asarnow JR, & Tompson MC (2020). Parent and youth preferences in the treatment of youth depression. Child Psychiatry & Human Development, 1–12. 10.1007/s10578-020-01006-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewin AB, McGuire JF, Murphy TK, & Storch EA (2014). Editorial perspective: The importance of considering parent’s preferences when planning treatment for their children–the case of childhood obsessive-compulsive disorder. Journal of Child Psychology and Psychiatry, 55(12), 1314–1316. 10.1111/jcpp.12344 [DOI] [PubMed] [Google Scholar]
- Loh A, Leonhart R, Wills CE, Simon D, & Härter M. (2007). The impact of patient participation on adherence and clinical outcome in primary care of depression. Patient Education and Counseling, 65(1), 69–78. 10.1016/j.pec.2006.05.007 [DOI] [PubMed] [Google Scholar]
- Makoul G, & Clayman ML (2006). An integrative model of shared decision making in medical encounters. Patient Education and Counseling, 60(3), 301–312. [DOI] [PubMed] [Google Scholar]
- March JS, Parker JD, Sullivan K, Stallings P, & Conners CK (1997). The Multidimensional Anxiety Scale for Children (MASC): Factor structure, reliability, and validity. Journal of the American Academy of Child & Adolescent Psychiatry, 36(4), 554–565. [DOI] [PubMed] [Google Scholar]
- O’Connor A. (1995). User manual-decision self-efficacy scale. Ottawa: Ottawa Hospital Research Institute, 4. [Google Scholar]
- O’Connor AM (1995). Validation of a decisional conflict scale. Medical Decision Making, 15(1), 25–30. 10.1177/2F0272989X9501500105 [DOI] [PubMed] [Google Scholar]
- PracticeWise, LLC. (2004–2018). Services: PracticeWise Evidence-Based Services Database [PWEBS]. Retrieved September 1, 2016, from http://www.practicewise.com/#services
- Shirk S. & Saiz C. (1992). Clinical, empirical, developmental perspectives on the therapeutic relationship in child psychotherapy. Development and Psychopathology, 4, 713–728. [Google Scholar]
- Silverman M, & Albano A. (1997). The Anxiety Disorders Interview Schedule for Children. ADIS-C/P San Antonio. TX: Psychological corporation. [Google Scholar]
- Stroul BA, & Friedman R. (1986). A system of care for children and youth with severe emotional disturbances. Washington, DC: CASSP Technical Assistance Center, Center for Child Health and Mental Health Policy, Georgetown University Child Development Center. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.