Abstract
Scientific studies have provided evidence that there is a relationship between violent and aggressive behaviors and addictions. Genes involved with the reward system, specifically the brain reward cascade (BRC), appear to be associated with various addictions and impulsive, aggressive, and violent behaviors. In our previous research, we examined the Taq A1 allele (variant D2 dopamine receptor gene) and the DAT-40 base repeat (a variant of the dopamine transporter gene) in 11 Caucasian boys at the Brown School in San Marcus, Texas, diagnosed with intermittent explosive disorder. Thirty supernormal controls were screened to exclude several reward–deficit behaviors, including pathological violence, and genotyped for the DRD2 gene. Additionally, 91 controls were screened to exclude ADHD, pathological violence, alcoholism, drug dependence, and tobacco abuse, and their results were compared with DAT1 genotype results. In the schoolboys vs. supercontrols, there was a significant association with the D2 variant and a trend with the dopamine transporter variant. Results support our hypothesis and the involvement of at least two gene risk alleles with adolescent violent/aggressive behaviors. This study and the research presented in this paper suggest that violent/aggressive behaviors are associated with a greater risk of addiction, mediated via various genes linked to the BRC. This review provides a contributory analysis of how gene polymorphisms, especially those related to the brain reward circuitry, are associated with violent behaviors.
Keywords: Intermittent Explosive Disorder (IED) in Adolescence, GARS, Dopamine homeostasis, Reward Deficiency Syndrome (RDS), Dopamine D2 receptor gene polymorphism (DRD2), Dopamine Transporter Gene (DAT1)
1. Introduction
The Issue
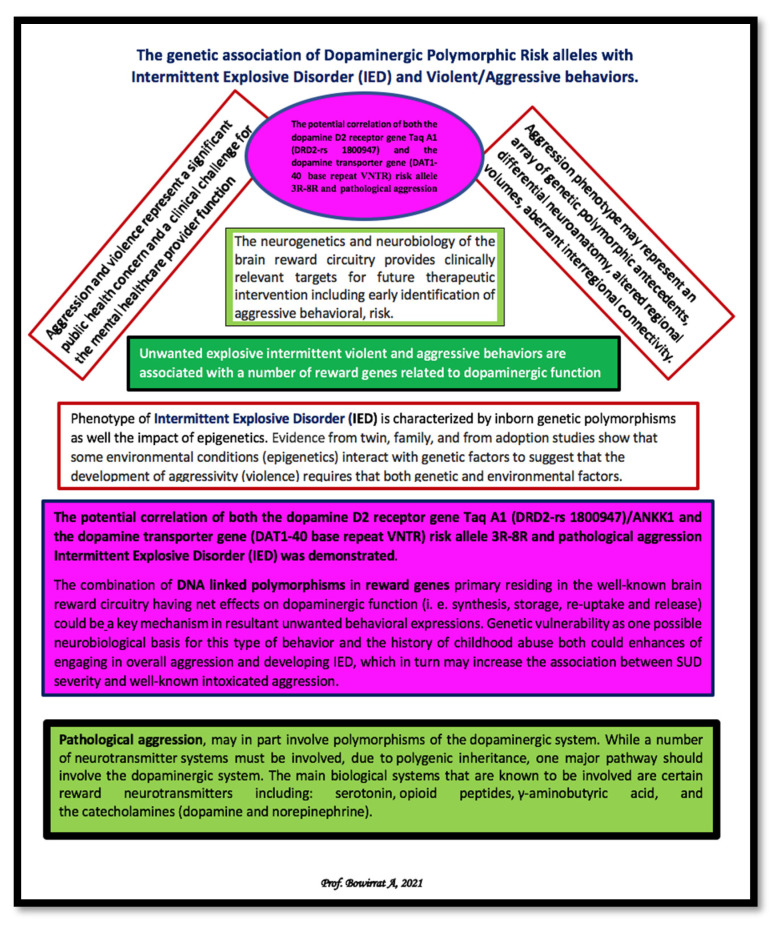
There is evidence that unwanted explosive, intermittently violent, and aggressive behaviors are associated with several reward genes related to dopaminergic function [1]. Violence and aggression pose a major clinical challenge to mental health care providers and represent a significant public health concern [2]. It is well-known that the aggression phenotype may represent an array of polymorphic genetic antecedents, differential neuroanatomy, altered regional volumes, and aberrant interregional connectivity [3]. Understanding the neurogenetics and neurobiology of the brain reward circuitry (i.e., serotonergic, cannabinoidergic, opioidergic, GABAergic, glutaminergic, and dopaminergic, etc.) provides clinically relevant targets for future therapeutic intervention, including early identification of aggressive behavioral risk. It is noteworthy that disciplinary and legal difficulties stemming from violent or aggressive behavior have reached epidemic proportions among our youth. Roughly 8% of adults and 17% of adolescents report a pattern of recurrent aggressive outbursts within one year. Such individuals are much more impulsive and aggressive than nonaggressive controls. They are also more likely to carry and use weapons, threaten others, engage in intimate partner assault, and be arrested by law enforcement [4]. Accordingly, the impact of aggressive and violent individuals begets significant economic and social costs to society. Moreover, individuals who display episodic rage attacks are reluctant to seek treatment, especially if the episodes are accompanied by physical violence [5]. There is also a recent emergence of new media technology and its subsequent increased use and access by adolescents (e.g., computers for internet access, cell phones). This technological explosion offers potential benefits as well as risks [6]. One area of concern for adolescents is that the risk of being subjected to aggression perpetrated by peers through these mediums is rising.
2. Substance Use Disorder (SUD) and Intermittent Explosive Disorder (IED)
According to Puhalla et al. [7], intermittent explosive disorder (IED) is the only psychiatric diagnosis for which the primary symptom is affective aggression. We know that an alcohol use disorder (AUD) diagnosis and a history of childhood abuse increase the likelihood of developing IED. Furthermore, an association exists between increased general aggression, including aggression while intoxicated, and both AUD and childhood abuse [7]. An investigation by Puhalla et al. [7] revealed that childhood abuse, but not AUD status, predicted IED status. Puhalla et al. showed that IED, aggression frequency, AUD, and childhood abuse were all independently associated with overall aggression; however, only individuals with IED displayed increased intoxicated aggression related to the degree of AUD severity [7]. Therefore, genetic vulnerability could be one possible neurobiological basis for this type of behavior [8]. For example, a history of childhood abuse could enhance the frequency of engaging in overall aggression and developing IED, which may increase the association between SUD severity and well-known intoxicated aggression.
It is essential to realize that aggression, rage, violence, alcohol, and drugs are all connected [9]. According to Alcoholics Anonymous terminology, anger is connected to relapse [10,11]. Clinically, violent outbursts and rage, for example, could be signs of delusional schizophrenia, bipolar disorder, posttraumatic stress disorder, antisocial, borderline, and paranoid character disturbances, and attention deficit disorder [12]. In terms of psychopharmacological mechanisms, the toxic effects of stimulant drugs like methamphetamine and cocaine induce hyperarousal and anxiety. Coinciding with this, the leading cause of death among stimulant drug addicts results from abuse and violence [13,14].
3. Neurogenetics of Intermittent Explosive Disorder (IED) and Violent Aggressive Behaviors
The origin of human violence has been an issue of significant concern for centuries [15,16]. Of genuine interest, violent behavior and possibly being born a “natural killer”, for example, raise questions related to the nature/nurture conundrum. We are aware that the phenotype of IED is characterized by inborn genetic polymorphisms as well as the impact of epigenetics. Several investigations have identified specific DNA polymorphisms that augment the risk for violent and antisocial behaviors [17]. There is evidence from behavioral genetics supporting the conclusion that genetic contributions are responsible for significant variance in antisocial personality and violent behavior.
Accordingly, Fergurson [17], in a meta-analysis, revealed that genetic influences could account for 56% of the variance in antisocial behavior, with 31% due to unique non-genetic influences and 11% due to shared non-genetic influences. Ferguson suggests that the resultant data reflect a relationship to evolutionary psychological theory. Evidence from behavioral genetics supports the conclusion that a significant amount of the variance in antisocial personality and behavior (APB) is due to genetic contributions. Many scientific fields, such as psychology, medicine, and criminal justice, struggle to incorporate this information with preexisting paradigms that focused exclusively on the external or learned etiology of antisocial behavior. Ferguson presents a meta-analytic review of behavioral genetic etiological studies of APB. Results indicated that 56% of the variance in APB can be explained through genetic influences, with 11% due to shared non-genetic influences and 31% due to unique non-genetic influences [17].
The consensus of the current literature provides evidence from twin, family, and adoption studies and makes a case for the significance of genetic factors in the nascence of aggression from childhood through adulthood [18]. Furthermore, data from adoption studies show that some environmental conditions (epigenetics) interact with genetic factors in a manner that suggests that both genetic and environmental factors must be present for aggressivity (violence) to develop [19]. One study revealed an association between the CDH13 gene (Cadherin 13, which codes for neuronal membrane adhesion protein) and a monoamine oxidase-A (MAO-A) low-activity genotype (which contributes to a low dopamine turnover rate) and highly violent behavior among two independent cohorts of Finnish prisoners. However, no significant signal was detected for either CDH13 or MAO-A in non-violent offenders in this study cohort, signifying that findings were limited to violent offending and not primarily the result of antisocial personality disorder or substance abuse [19]. The authors suggest that, for example, both low neuronal membrane dysfunction and monoamine metabolism are possible factors in the etiology of extremely violent criminal behavior and suggest that about 5–10% of all severe violent crimes in Finland can be attributed to the MAO-A and CDH13 genotypes.
Neuronal membrane potential is of fundamental importance for the mechanistic understanding of brain function. Whole-cell recordings can be combined with two-photon microscopy to target fluorescently labeled neurons, revealing cell-type-specific membrane potential dynamics of retrogradely or genetically labeled neurons. Dual whole-cell recordings reveal behavioral modulation of membrane potential synchrony and properties of synaptic transmission in vivo. Optogenetic manipulations are also readily integrated with whole-cell recordings, providing detailed information about the effect of specific perturbations on the membrane potential of diverse types of neurons.
In addition, specific genes related to the underlying biochemical mechanisms associated with aggressivity in animals are similar to the configuration of similar physiologic mechanisms in humans [20]. Therefore, in the following section, we will provide a snapshot of the various roles of “reward” genes and associated addiction risk polymorphisms in IED, primarily in humans.
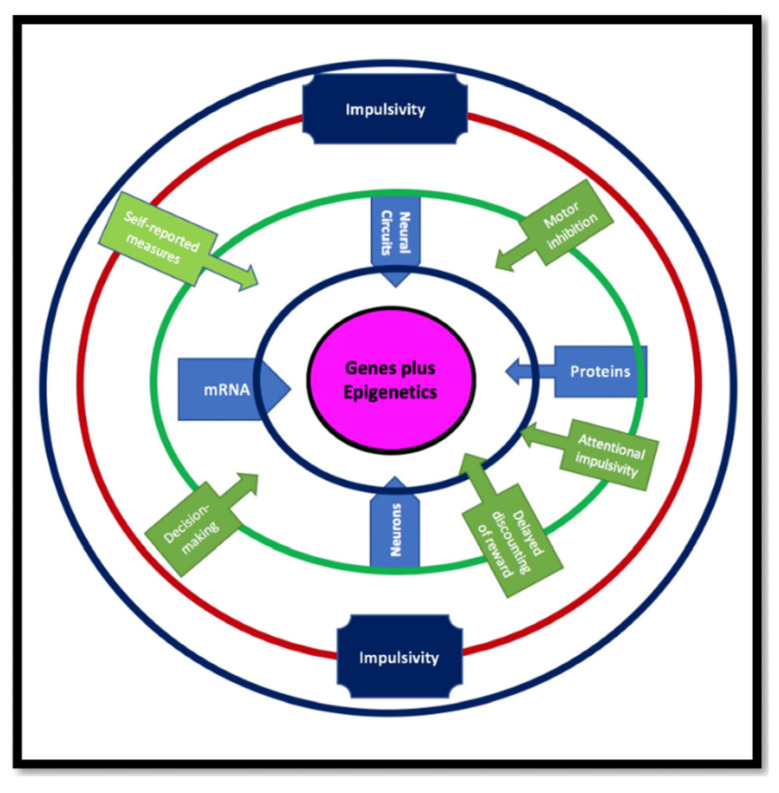
Furthermore, we suggest that defining different forms of impulsivity/impulsive behaviors related to these genes might evolve our understanding of the neurobiological basis of disorders for which impulsivity is a component. These disorders include IED and other aggressive and violent behaviors associated with other psychopathologies. Finally, we combine all these interacting factors with impulsivity into a model shown in Figure 1.
Figure 1.
Impulsivity is a hereditary, disease-associated trait that may be evolutionarily beneficial as an endophenotype for genetic innovation resulting in behavioral adaptation to a challenging environment. More specifically, impulsivity is not a singular construct but a complex trait. Multiple laboratory behavioral tasks and self-report measures are used to assess aspects of impulsivity. Different neural circuits and genes are impacted by epigenetics, which also has pleiotropic effects on behaviors that modulate impulsivity.
4. Specific Reward Genes and IED
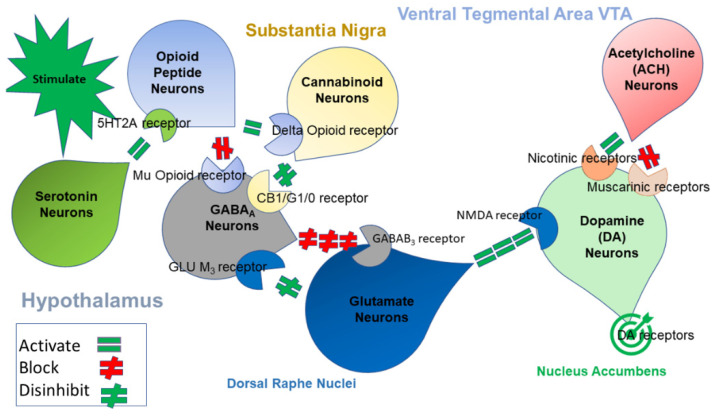
In 1989, Blum and Kozlowski published their initial concept of the brain reward cascade (BRC) implicated in various addictions and other behaviors [21]. In previously published works from our laboratory, we proposed a BRC schematic at mesolimbic sites as described in Figure 1. Based on the overlapping evidence previously given in this paper, this cascade appears to be involved in IED and violent and aggressive behaviors [22].
Moreover, our laboratory has developed United States and foreign patents related to the Genetic Addiction Risk Severity (GARS) Test [23]. Table 1 displays the associated various risk alleles from the BRC that can be measured.
Table 1.
Represents the GARS SNPs and VNTRs (snapshot).
| Gene | Polymorphism | Location | Risk Allele(s) |
|---|---|---|---|
| DRD1 | rs4532 | Chr 5 | A |
| DRD2 | rs1800497 | Chr 11 | A |
| DRD3 | rs6280 | Chr 3 | C |
| DRD4 | rs1800955 | Chr 11 | C |
| 48 bases Repeat | Chr 11, Exon 3 | 7R, 8R, 9R, 10R, 11R | |
| COMT | rs4680 | Chr 22 | G |
| OPRM1 | rs1799971 | Chr 6 | G |
| DAT1 | 40 bases Repeat | Chr 5, Exon 15 | 3R, 4R, 5R, 6R, 7R, 8R |
| MAOA | 30 bases Repeat | Chr X, Promoter | 3.5R, 4R |
| Serotonin Transporter SLC6A4 (5-HTTLPR) | 43 bases Repeat plus rs25531 | Chr 17 | LG, S |
| GABA(A) Receptor, Alpha-3 GABRB3 | CA-Repeat DNR | Chr 15 (downstream) | 181 |
Abbreviations: Dopamine receptor D1 (DRD1), dopamine receptor D2 (DRD2), dopamine receptor D3 (DRD3), dopamine receptor D4 (DRD4), catecholamine-methyltransferase (COMT), opioid receptor mu 1 (OPRM1), dopamine transporter (DAT1), monoamine oxidase A (MAOA), serotonin-transporter-linked promoter region (5HTTLPR), Gamma-aminobutyric acid type A receptor subunit beta3 (GABRB3).
Evaluation of pain clinic patients with the GARS test and the addiction severity index-media version V revealed significant GARS scores. Specifically, scores of seven or greater were associated with alcohol, whereas scores of four or greater were associated with other drugs [24].
5. Specific Genes from the BRC/GARS: Linking Them with IED and Aggressive, Violent, and Impulsive Behaviors
5.1. Dopamine D1 Receptor
A recent search (10 October 2021) on the PubMed database using the term “Intermittent Explosive Disorder” (IED) and “Dopamine D1 Receptor” (DRD1; rs4532) located on chromosome 5 resulted in no listings. However, additional searching related to impulse control behaviors/disorders (ICB/ICD) did result in many studies. ICB/ICD are characterized by an inability to resist urges that result in an individual engaging in behaviors that are harmful to themselves or others [25]. An abundance of research has been focused on polymorphisms of the DRD1 (particularly rs4532) concerning its role in various neuropsychiatric disorders [26]. As a result, associations between the DRD1 Rs4532 polymorphism and several mental illnesses have been uncovered, including nicotine addiction [27], bipolar disorder [28], and ADHD [29]. Genotyping of several dopaminergic polymorphisms detected pronounced differences between variant and wild-type alleles using a high-resolution melt (HRM).
Specifically, associations between variants of DRD1 rs4532 (OR = 21.33; 95% CI, 1.97–230.64; p = 0.0024) and an increased risk of developing ICB were observed in a cohort of Parkinson patients. In addition, using the catalyst model of aggression as guidance revealed risk alleles that were hypothesized to be associated with intimate partner violence (IPV) in the presence of financial hardship [30].
5.2. DRD2/ANKK1
The rs1800497 variant in DRD2/ANKK1 has been implicated in a reduction in receptor density in the striatum [31]. The rs1800497 variant in DRD2/ANKK1 results in significant protein structure modifications that manifest in reduced expression of striatal receptors (possibly due to rs1800497 changing glutamic acid to lysine). Self-reported measures of impulsivity are approximately 45% heritable, as demonstrated by twin studies [32]. The most frequent association between addiction and the DRD2/ANKK1 gene is found with the rs1800497 polymorphism [33]. In fact, the DRD2 gene is responsible for the most consistent findings relating to the genetics of impulsivity as well. Response inhibition testing has implicated the DRD2 A1 allele with impulsive behavior among healthy young adults [34,35]. Another study [36] conducted with a young adult population uncovered an association between impulsive self-damaging behaviors (assessed using borderline symptoms) and the DRD2 gene (A1 and B1 alleles). Impulsivity in healthy individuals was also correlated with other DRD2 SNPs. A relationship between the C/C genotype of the DRD2 C957T polymorphism and higher reward responsiveness after a psychological stressor was also detected [34]. In a neuroimaging study, the DRD2-141C Del carriers displayed greater reward-related ventral striatum reactivity, which was associated with self-reported impulsivity [37]. A study by Zainal Abidin et al. [26] reported an association between an increased risk of developing ICB and the DRD2/ANKK1 rs1800497 (OR = 3.77; 95% CI, 1.38–10.30; p = 0.0044) in a cohort of patients with Parkinson’s disease.
A critical achievement that illustrates these concepts is a study by Caspi et al. [38] that reported the most extensively cited measured Gene X Environment (GXE) interaction in predicting antisocial and violent behavior. Furthermore, Boardman et al. [39] reported that in the presence of low family violence, the carriers of two copies of the A1 allele variant of DRD2 are significantly more likely than those with one or no copies of the A1 allele to engage in serious delinquency. However, when those same individuals perceive a high level of family closeness, they are significantly less likely than those with no copies of the A1 allele to report higher delinquency.
It is noteworthy that when African American females carry at least one A1 allele of DRD2, they are more likely to experience violent victimization and have higher levels of depressive symptoms.
Results also show that DRD2 imparts a significant independent effect on depressive symptoms in female and male African-Americans [40] and African American children [41]. It is moderately established, albeit, with some controversy, that lower-functioning dopamine systems motivate individuals to seek rewards from external sources such as illicit drugs and other risky experiences. Along these lines, work from Chester et al. [42] revealed that amongst Caucasian males and females, DRD2 profiles were associated with increased sensation-seeking, which then predicted increased aggression. Chester et al. [42] suggested that decreased dopaminergic functioning elevates an individual’s risk for violence because it motivates them to experience the hedonically rewarding qualities of aggression. In addition, a study by Zai et al. demonstrated that the occurrence of at least one copy of the G allele for the DRD2 A-241G polymorphism (genotypic p = 0.02; allelic p = 0.01) was significantly associated with aggressive children [43]. Additionally, the DRD2 rs1079598 CC-genotype was overrepresented in aggressive children compared to controls (genotype p = 0.04). Amongst aggressive children, the T.T. genotype (p = 0.01) and the DRD2 TaqIA T allele (p = 0.01) were also found to be significantly overrepresented.
5.3. Dopamine D3 Receptor Gene
Importantly, drug abuse and violence are immensely destructive phenomena found worldwide. From 105 postmortem cases, a significant genetic difference has been reported for SNP rs6280 from the DRD3 gene that displayed a significant association, with genotypes T/C and C/C being more frequent in drug users (OR = 4.96; 95% CI = 1.07–23.02; p = 0.04), including cocaine and risky/violent behaviors [44].
5.4. Dopamine 4 Receptor Gene
Variable-number tandem repeat (VNTR) polymorphisms of the DRD4 gene were investigated in Chechen and Russian men convicted of crimes. The DRD4 long alleles were found to be more frequent in the men convicted of felonies, a finding similar to a cohort of mixed martial art (MMA) fighters that lacked a criminal record in both paternal lines [45]. Furthermore, increased vulnerability for impulsive and antisocial behavior in response to aversive environmental conditions has been associated with the DRD4 (dopamine D4 receptor) VNTR 1-11 [46]. Using data from the National Longitudinal Study of Adolescent Health, Daigle [47] reported that the 7R allele of the DRD4 gene distinguishes individuals who have been victimized multiple times from those who have been victimized once. According to Buchmann et al. [48], carriers of the DRD4 seven-repeat allele demonstrated more aggression in adulthood (p = 0.032) under conditions of increased maternal stress, which extended earlier observations regarding childhood antisocial behavior. In Marsman et al. [49], parental overprotection and rejection predicted higher levels of externalizing behavior problems (EBP), while lower levels of EBP were predicted by parental emotional warmth. They did find interaction effects with familial loading of externalizing behavior problems (FLE) and the DRD4 (specifically a 4-repeat allele). In more detail, the predictive effect of parental rejection was only observed in adolescents from low-FLE families, and the predictive effect of parental overprotection was more robust in adolescents not carrying the DRD4 4-repeat allele. Nobile et al. [50] found that the DRD4 long allele is associated with higher aggressive behavior scores in Italian preadolescents. Previous research has reported associations between the externalization of problems and aggression in children to either harsh and insensitive parenting or DRD4 polymorphisms. In the study by Bakermans-Kranenburg and van Ijzendoorn [51], they determined maternal insensitivity was correlated with externalizing (oppositional, aggressive) behaviors, but only with the occurrence of the DRD4 7-repeat polymorphism. Children who were positive for the 7-repeat allele were six times more likely to have externalized behavior when exposed to insensitive care than children without these genetic and environmental antecedents.
5.5. COMT
There is some evidence that both environmental and genetic factors influence an individual’s propensity for aggression. Both the functional polymorphism catechol-O-methyltransferase Val158Met (COMT) and childhood experiences of adversity have been implicated in aggression and aggression traits [52]. Hygen et al. showed that childhood serious life events and the COMT genotype had a significant interactive effect on childhood serious life events [52].
Specifically, Val homozygote children who had endured many serious life events displayed more aggression (p = 0.02) than did their Met-carrying peers. Of great interest, Brennan et al. [53] found the COMT Val108/158Met polymorphism (rs4680) substantially interacted with maternal cigarette smoking during pregnancy to predict aggressive youth behaviors at ages 15 and 20. Other work by Wang et al. [54] found that the Val/Met heterozygote and the Val/Val homozygote carriers displayed differences in aggressive motivation and feelings of hostility under conditions of inclusion versus exclusion. However, the differences were more prominent for Val/Met allele carriers, as expected in terms of the genetic phenomena heterosis [55].
Molecular heterosis occurs when subjects heterozygous for a specific genetic polymorphism show a significantly greater effect (positive heterosis) or lesser effect (negative heterosis) for a quantitative or dichotomous trait than subjects homozygous for either allele. Commings reviewed the accumulating evidence that molecular heterosis is common in humans and may occur in up to 50% of all gene associations. A number of examples are reviewed, including those for the following genes: ADRA2C, C3 complement, DRD1, DRD2, DRD3, DRD4, ESR1, HP, HBB, HLA-DR DQ, HTR2A, properdin B, SLC6A4, PNMT, and secretor [55].
It is known that childhood maltreatment and cannabis use are independent risk factors that increase the probability of experiencing psychotic symptoms [56]. Vinkers et al. [56] uncovered a significant three-way interaction between the COMT genotype, cannabis use, childhood maltreatment, and [rs4680] (p = 0.006). In fact, Val-homozygous individuals exhibited increased psychotic experiences after exposure to both childhood maltreatment and cannabis use, compared to Met-homozygous individuals and Met-heterozygous individuals.
5.6. Mu-Opioid Receptor [OPRM1]
Opioids regulate mesolimbic dopaminergic pathways in the VTA via activation of μ-opioid receptors on secondary interneurons, which cause hyperpolarization and inhibition of GABA release on primary neurons (the dopaminergic output neurons), and consequently increased DA release [57]. The Colorado Center for Antisocial Drug Dependence (CADD) has been using several research designs and strategies to study the genetic basis for antisocial drug dependence in adolescents. They found that the mu-opioid receptor gene (OPRM1) rs495491 significantly emerged as a plausible candidate for a role in antisocial drug dependence after gene-based permutation tests with a p-value of p < 0.006 of this SNP (odds ratio 1.47) [58]. Interestingly, opiates have been related to aggression, specifically self-directed aggression. Illicit opioid use, misuse, and intoxication can result in violence, while a decrease in opioid availability can result in OUD victims acting violently in order to obtain supplies [59]. Moreover, self-injurious behavior has been associated with enhanced metenkephalin [60], while opiate antagonists typically diminish self-injurious behavior [61]. Attenuated Cerebral Spinal Fluid (CSF) endogenous opioid concentrations have been associated with self-injurious behaviors in patients with borderline personality disorder [62]. It is known that decreased opioids may be related to increased rejection sensitivity and abandonment/separation distress and may heighten the likelihood of aggressive behavior [63,64]. It is essential to realize that attenuated presynaptic opiate activity may upregulate postsynaptic µ-opioid receptors, and thus dramatic relief of pain may result when opiates are released in the context of self-injurious behavior [65].
Polymorphisms in OPRM1 are the primary candidate sources of clinical variability in opioid therapy. Apart from the 118 A > G single nucleotide polymorphism, nothing is known about the role of OPRM1 mutations in opioid therapy [66]. In a study by Lötsch et al., the influence of the OPRM1 mutations on opioid pharmacodynamics was assessed using pooled data from 31 healthy volunteers obtained in previous studies with available plasma concentrations and pupil diameters after intravenous administration of morphine or morphine-6-glucuronide (M6G) [66]. A total of 24 candidate ORPM1 mutations were screened for, and those found at an allelic frequency of at least 5% in the 31 subjects were analyzed for functional consequences using population pharmacokinetic-pharmacodynamic modeling of the miotic effects of the opioids as a reliable and sensitive surrogate parameter of the central nervous system opioid effects. Polymorphisms with an allelic frequency of > or = 5% (n = 310) were 118 A > G in exon 1 (11.5%), IVS2-31 G > A (8.9%), and IVS2-691 C > G (44.5%) SNPs in intron 2. The 118 A > G SNP significantly increased the values of EC50 by a factor of more than 2 (non-mutated: EC50, morphine = 30 nmol/L, EC50, M6G = 750 nmol/L, 118 G carriers: EC50, morphine = 66 nmol/L, EC50, M6G = 1650 nmol/L), whereas the IVS2-691 C > G SNP had no effect. Based on morphine and M6G, the present analysis encourages focusing on the 118 A > G SNP when investigating the role of OPRM1 mutations in the activity of opioid analgesics. Other OPRM1 mutations are probably less important, either owing to low allelic frequency or due to poor indications for functional consequences. This applies to opioid potency in the context of opioid therapy but not to pain processing or substance addiction, in which opioid receptors are involved but other or additional OPRM1 mutations may be important.
Other work by Cimino et al. [67] found that mothers and children who carried the G allele (G/G + A/G genotypes) were more likely to have an insecure attachment style. Children with the G-allele scored higher than homozygous A/A children on the withdrawal and conduct problems subscales in the clinical sample. In fact, mothers with the G-allele displayed elevated interpersonal sensitivity, hostility, depression, paranoid ideation, and hostility and provided less care than mothers with the A/A allele. Further interest resides in the fact that individuals with the G allele tend to experience more social pain [68,69] and increased emotional dysregulation and neural activation as a consequence of social rejection. In contrast to A/A homozygotes, individuals with the G-allele also demonstrate higher levels of rejection sensitivity, behavioral retraction to angry faces, and high levels of fearful attachment despite the quality of their early maternal care [70,71,72]. This demonstrates that the A118G-genotype modulates the effects of early maternal care on adult attachment style.
5.7. Dopamine Transporter (DAT1)
Dopamine transporter DAT-1 (SLC6A3) is a critical dopaminergic system gene that modulates dopamine signaling and reuptake and may contribute to several psychiatric disorders, such as antisocial behaviors and traits. Convicted murderers were more likely than controls to be carriers of the 9R allele of thee DAT-1 VNTR polymorphism for either one or two risk alleles (OR = 1.49 and 3.99, respectively, p = 0.003). Different genetic inheritance models were used to validate the plausible association between the DAT-1 9R allele polymorphism and the “murderer” phenotype. Furthermore, this identified phenotype was associated with the combined haplotype of the DRD2 and 9R-A2 of DAT-1 genes. Moreover, parental marital complications and responses to verbal abuse were correlated to the 9R allele of DAT-1. The results allude to the role of the 9R allele in contributing to criminal propensity in convicted murderers of Pakistani origin [73]. Further, carriers of the high-risk DAT1 alleles were more likely to commit IPV in the presence of financial stressors than the individuals carrying low-risk alleles [30]. Investigations by Fine et al. [74] have uncovered interactions stemming from the effects of dopaminergic phenotypes and school attachment on delinquency. Negative and positive school environments conferred different effects on individuals carrying the DRD2-A1 allele. Whereas individuals carrying the DAT1-10R allele fared better in positive environments, they fared the same as 9R homozygotes in moderate and poorer environments. It is also notable that Young et al. [75] demonstrated that the DAT1 9-repeat variant conferred a significant risk for externalizing behavior at ages four (p = 0.001) and seven years (p = 0.02). Data from twin studies present evidence that genetic factors may contribute to adolescent-onset or adolescent-limited antisocial behavior. Burt and Mikolajewski [76] presented evidence that adolescent antisocial behavior (ASB) was associated with DAT1. However, these associations were only found in a nonaggressive, rule-breaking subset of ASB, and they failed to reach statistical significance in the context of physical aggression. Finally, as mentioned in the D1 dopamine receptor gene section, as predicted, individuals with high-risk DAT1 alleles were shown to be more likely to commit IPV in the presence of financial hardship than individuals with low-risk DAT1 alleles [30].
5.8. Monoamine Oxidase-A (MAO-A)
A variable number of tandem repeats (VNTR) of the monoamine oxidase A (MAO-A) gene promoter have been correlated with the expression of antisocial behavior in hostile or stressful environments. Uršič et al. [77] provided some evidence to support the association of the MAO-A polymorphism with suicide. Specifically, Uršič et al. [77] demonstrated a trend towards the 3R allele and suicide and associated the 3R allele with the non-violent suicide method on stratified data (20 suicide victims). Beaver et al. [78] reported that the decreased function of the MAO-A allele augmented the risk of joining a gang and increased the odds that an individual would use a weapon during a fight, an observation that was only valid for males, not females. The relationship between the low MAO-A activity allele and increased chances of using a weapon during a fight stayed relevant even when comparing gang members; gang members without the low-activity MAO-A allele were less likely to utilize weapons. In agreement with the latter findings, Kolla and Vinette [79] also found that the low-activity MAO-A variable nucleotide tandem repeat genetic polymorphism demonstrated strong relationships with large samples of violent offenders, many of whom had an antisocial personality disorder (APD). These same authors, Kolla et al. [80], indicate that low-activity monoamine oxidase-A genotype may affect cortico-striatal connectivity in APD. They also suggest that this postulated connectivity may also contribute to proactive aggression in a genotype-specific manner, conceivably resulting from the enhanced dopaminergic activity.
Along similar lines, Gera et al. [81] dissected the low-activity of the MAO-A genotype from the high-activity genotype. Specifically, they found the prevalence of the low-activity 3-repeat allele was more common in violent offenders who were heroin addicts than in addicts without antisocial behavior (34.6 vs. 15.4%; p < 0.03) and controls (18.9%; p < 0.05). In contrast, high-activity 4-repeat allele frequency was more prevalent among individuals with no antisocial behavior than among individuals that were antisocial-aggressive heroin-dependent (76.9 vs. 55.8%; p < 0.02). Also, heroin addicts with the low-activity 3-repeat allele scored significantly higher in the Buss Durkee Hostility Inventory (BDHI) on the irritability, suspiciousness, and resentment subscales than individuals with high-activity alleles. It was also found [82] that decreased MAO-A function within the cortical and subcortical brain regions manifested in increased self-reported aggression and contributed to over one-third of the variability. In contrast, others found the increased activity of the MOA-A allele to be associated with proactive aggression among violent offenders with antisocial personality disorder [83]. Huang et al. [84] found that the decreased expression allele was correlated with high impulsivity in males with a known history of abuse (before 15 years); the same was not true in females. This known polymorphism may potentially be a marker for impulsivity, which may also play a role in the risk of abuse. However, Ni et al. [85] reported that among patients with borderline personality disorder, the high-activity VNTR alleles were more common (chi = 4.696, p = 0.03), and the low-activity haplotype (X2 = 5.089, p = 0.02) was less common. To help us understand dopaminergic dynamics, Schlüter et al. [86] found that the MAOA-High group displayed higher aggression and augmented dopamine release after watching a violent movie. However, the violent film reduced aggression without causing consistent increases in dopamine release in subjects with low-activity MAO-A. Accordingly, these results suggest a plausible influence of the MAO-A-promoter polymorphism on the neurobiological regulation of aggressive behavior. However, the notion that low MAO-A promotes aggression via the singular effect of augmented dopamine is not supported by data. Indeed, many studies support the role of the MAO-A gene as a prominent genetic determinant for criminal violence [87,88,89,90,91,92,93,94,95,96,97,98,99,100,101].
5.9. Serotonin Transporter Gene (5-HTTLPR)
Tielbeek et al. [102] performed a meta-analysis of eight studies consisting of 12 independent samples with a total of 7680 subjects; an effective sample of 6724 subjects was included. They found a significant association between environmental adversities and the 5-HTTLPR genotype on antisocial behavior. Tung and Lee [103] also found that in 2558 adolescents the 5-HTTLPR genotype significantly modulated the correlation of parental support with ASB membership. Specifically, individuals with the short allele demonstrated higher sensitivity to parental support when predicting late-onset trajectory; the long/long genotype served as a plausible “plasticity genotype” for the adolescent-peak trajectory group. Others [104,105] show the prevalence of the S allele and the S.S. genotype to be higher among violent suicide attempters than among subjects in the control group. The S.S. genotype odds ratio compared to the L.L. genotype was 3.63 (95% CI (1.27–10.40). This difference implies that an alteration in the expression of the 5-HT encoding transporter gene may play a role in violent suicidal behavior. Retz et al. [106] found that an excess of the S/S genotype and the short (S) alleles in Caucasian male patients was characterized by reoccurring physical violent behavior and explicated 5% of the genetic variance of violent behavior. From clinical research, Gorodetsky et al. [107] differentiated influential variables on self-directed aggression among groups of similar predictor variables within the expressed behavioral domain. 5-HTTLPR expressed an independent gene dose-dependent effect. Furthermore, Hallikainen et al. [108] found the S allele prevalence was greater in Type II alcoholics than in Type I alcoholics (X2 = 4.86, p = 0.028) and healthy controls (X2 = 8.24, p = 0.004). This work suggests an association between the 5-HTT ‘S’ promoter polymorphism and an increased risk for early-onset alcoholism related to antisocial personality disorder and impulsive, repetitive violent behavior. Chinese investigators [109] also found that S-allele positive subjects were significantly greater in the criminal group than among the controls (p = 0.006). In other work, [110] suicide-related trait measure analyses of variance conducted on the three genotypes established a significant difference in violence measures among patients with the L.L. and L.S. genotypes (9.50 ± 4.04 vs. 5.36 ± 4.03; p = 0.029). This study implies that the 5-HTTLPR polymorphism may contribute to violent behavior in this population. In addition, it was found that maltreatment in childhood adds to the risk of ASPD, and preliminary evidence suggests the 5-HTTLPR genotype moderates the effects in women. It is known that the 5-HTTLPR polymorphism has been correlated with both aggression/hostility and depression [111]. Specifically, Gonda et al. [111] found a significant correlation with many hostile traits. The interaction between the two primary effects was also significant in the context of several subscales. Post hoc analyses resulted in a significant correlation between the S allele (only in the depressed group) and the BDHI subscales.
The second-highest reason for death among youth worldwide is suicidal behavior, and it is also the tenth-leading cause of death among all age groups. Inherited genetic differences have a part in suicidality, with heritability ranging from 30 to 55% [112]. A literature search revealed 1186 articles; among these, Fanelli and Serretti [112] identified 45 pertinent case-control studies (15,341 subjects). Low-expressing alleles (S + LG) were correlated with an increased risk of violent suicide attempts (OR = 1.44, C.I.: 1.17–1.78, p = 0.0007). It is noteworthy that studies have not provided clear evidence concerning the genetic background of suicidal predisposition. However, the associations between polymorphisms of the 5-HTTLPR genes and violent suicidal behavior reveal the fewest inconsistencies [113,114,115].
5.10. GABA (A) Receptor Gene (GABRB3)
A word search in the PubMed database utilizing terms in a Boolean search including various combinations of “violent behavior”, “crime”, “criminal justice system”, “suicide”, “IED”, “aggression”, and “bullying” with GABRB3 resulted in no listings.
5.11. Original Dopaminergic Candidate Association Study in Adolescent IED
Previously, Blum’s group hypothesized that polymorphisms in the dopaminergic system might contribute to pathological aggression in adolescents [116]. Although multiple neurotransmitter systems are likely involved, one major critical pathway should involve the dopaminergic system. In addition, a more profound grasp of the neurobiological foundations of aggression has led to pharmacological treatments for such behaviors. As discussed above, the primary biological networks that contribute to reward neurotransmitters include opioid peptides, serotonin, catecholamines (norepinephrine and dopamine), and γ-aminobutyric acid.
This research employed a small pilot study involving 11 Caucasian boys, aged 13–19, who were diagnosed with IED and violent/aggressive behaviors in adolescence and attended the Brown School, a residential school facility in San Marcus, Texas. This study received IRB approval from the Path Foundation in New York, NY. Each patient signed an approved consent form. Each patient was genotyped for the DRD2 Taq A1 (rs1800497) and the DAT1 (40BP repeat VNTR) polymorphisms [116,117].
Results from this study revealed a correlation between DRD2 Taq A1 (rs1800497) and DAT1 (40 B.P. repeat VNTR) polymorphisms and IED. In addition, the subjects were diagnosed with IED (characterized by pathological violence or impulsive and aggressive violent behavior). Furthermore, 30 supernormal controls were evaluated and screened for several reward deficit behaviors, including pathological violence; only 3.3 percent of them carried the DRD2 Taq A1 (rs1800497). Moreover, another 91 controls were also screened to exclude pathological violence, ADHD, drug dependence, alcoholism, obesity, and tobacco use. This second set of controls was used to evaluate the absence or presence of the DAT1 (40BP repeat VNTR) and polymorphisms in the cases and controls. We found in this small pilot some interesting genetic correlations. When the DRD2 A1 (A1/A1 or A1/A2) genotype was compared in these subjects to the super controls, a robust significant association was observed whereby X2 = 14.9, df = 1, and p = 0.0001, indicating that when highly screened controls are utilized, carriers of the DRD2 A1 allele reveal a clear association toward violent behaviors. However, a similar trend was found with the DAT1 480 bp 10/10 genotype compared to controls (X2 = 2.82, df = 1, and p = 0.093). Most importantly, when the 9/10 genotype was compared with these controls, a significant association was observed (X2 = 14.31, df = 1, p = 0.00006), indicating that when highly screened controls are utilized, carriers of the DAT1 480 bp allele reveal a clear association toward violent behaviors. It is noteworthy that the data relevant to the “super controls” and the initial data have been published elsewhere.
A blinded clinical trial identified a positive association between adolescents’ pathological violence, DAT1 polymorphism, and the DRD2 gene. Consequently, this and other cited work suggest a function for both the DAT and DRD2 genes in manifesting aggressive behavior. Furthermore, these initial data obtained in 2005, in terms of these two potential candidates, agree with previously mentioned studies in this perspective for the DRD2 A1 allele [31,32,33,34,35,36,37,38,39,40,41,42,43] and the DAT1 9 R allele [30,73,74,75,76].
6. Violent/Aggressive Behaviors and Addiction Liability
It is important to note that we are trying to provide evidence for the link between aggressive and violent behaviors and the liability of addiction in this paper. Our previous work suggested that addiction, impulsivity, and chronic violence may cluster together within the reward deficiency syndrome (RDS) [118]. The connection between addiction and violence may indeed be impulsivity, as seen among substance users with multiple incarcerations [119] and gamblers who binge-drink and are involved in non-partner physical aggression [120]. Alcohol also appears to be correlated with violence in many studies: among adolescents [121]; with alcohol ingestion being more likely to occur prior to violent incidents [122]; with changes in alcohol consumption modulating the degree of suppressed anger in those with extreme anger associated with violent behaviors [123]; among those admitted to emergency rooms with alcohol misuse who have a history of partner violence [124]; among university athletes who drink excessively and are violent both on and off the field, tied to masculinity [125]; and within the context of dating, alcohol use seems to mediate violence [126]. Methamphetamine addiction is also correlated with violence [127]. Gambling and substance abuse are also associated with violence [128]. Crack cocaine abusers were more likely to have an antisocial personality disorder and PTSD and were more likely to be both victims and perpetrators of violence [129,130]. Comorbid bipolar disorder and heroin addiction are correlated with violence as well [131]. In addition, various addictive disorders and substance abuse disorders are related to violence, including sexual abuse and domestic violence [132], interpersonal violence [133], and suicide [134]. Non-partner and partner violence are associated with drinking episodes, cocaine use, and depressive symptoms [135]. Crack cocaine and alcohol dependence are associated with aggression and violent behavior [136]. Finally, polysubstance use (including binge drinking, marijuana, other illicit drugs, and prescription stimulants) was associated with emergency room visits and a history of aggression and violent behaviors [137,138]. Finally, similar to this overview, Ahmadi and colleagues searched for studies for their review and determined that 15 out of the 19 studies they reviewed showed a significant correlation between various forms of aggression and addiction [139].
7. Dopaminergic Dysregulation (Surfeit or Deficit) Associated with Addiction and Violent Behavior
We hypothesize that continued genetic research in this area will confirm positive associations with dopaminergic polymorphisms. The use of highly screened controls to eliminate addictive, impulsive, and compulsive behaviors (in both proband and family) may be of necessary consequence for our young population. The issue at hand is the present confusion related to whether the neurotransmitter genotypes that regulate downstream dopamine release and function at the BRC (Figure 2) are mixed in terms of surfeit or deficit in terms of reward processing. Evidence for both surfeit and/or deficit in reward processing seems unclear and requires additional research. To assist in understanding our model, developed by one of us (A.B.), the following schematic is provided (Figure 3) [139].
Figure 2.
Illustrates the interaction of at least seven significant neurotransmitter-pathways involved in the brain reward cascade (BRC). In the hypothalamus, environmental stimulation results in the release of serotonin, which in turn, via 5HT2A receptors, activates (equal green sign) the subsequent release of opioid peptides from opioid peptide neurons, also in the hypothalamus. Then, the opioid peptides have two distinct effects, possibly via two different opioid receptors. One inhibits (red hash sign) through the mu-opioid receptor (possibly via enkephalin) and projects to the substantia nigra to GABAA neurons. Another stimulates (equal green sign) cannabinoid neurons (the anandamide and 2-arachidonoylglycerol, for example) through beta–endorphin linked delta receptors, which in turn inhibit GABAA receptors in the substantia nigra. Also, when activated, cannabinoids, primarily 2-archydonoglcerol, can indirectly disinhibit (red hash sign) GABAA receptors through activation of G1/0 coupled to CB1 receptors in the substantia nigra. In the dorsal raphe nuclei, glutamate neurons can indirectly disinhibit GABAA receptors in the substantia nigra by activating group III metabotropic glutamate (GLU M3) receptors (green hash). GABAA receptors, when stimulated, will in turn powerfully (red hash signs) inhibit ventral tegmental area (VTA) glutaminergic drive via GABAB 3 receptors. It is also possible that stimulation of ACh neurons at the nucleus accumbens can stimulate both muscarinic (red hash) and nicotinic (green hash) receptors. Finally, glutamate neurons in the VTA will project to dopamine neurons stimulating NMDA receptors (equal green sign) to preferentially release dopamine at the nucleus accumbens, shown as a green bullseye that indicates a euphoria or “wanting” response. The result is that when dopamine release is low (dopamine deficiency), it results in unhappiness, while general (healthy) happiness depends on the dopamine homeostatic tonic set point. (With permission from Blum et al. With permission from Blum et al. [139].).
Figure 3.
A schematic representing a summary of dopaminergic genetics with intermittent explosive disorder (IED), violent/aggressive behavior, and addiction.
8. Conclusions
Following the seminal findings of our group in 1990 related to the association of the DRD2 Taq A1 allele (located in exon 11 of the ANNKI gene) with severe alcoholism, 31 years later, along with an explosion of new genetic techniques (e.g., genome-wide association studies), genetic polymorphisms linked to extreme violence/aggression have been discovered. Possibly, the combination of DNA-linked polymorphisms in reward genes, which are primarily residing in the well-known brain reward circuitry and having net effects on dopaminergic function (i.e., synthesis, storage, reuptake, and release), could be a key mechanism in resultant unwanted behavioral expressions. However, the current literature data point towards an over-representation of the reward genes and associated risk alleles measured in the GARS test (see Table 1) in violent/aggressive behaviors. Interestingly, several specific risk alleles that load onto violent and aggressive behaviors are of evolutionary importance and an adaptive process linked to survival. We believe that this article provides a framework to encourage additional scientific exploration that couples these known polymorphisms as depicted herein with a genetic propensity to engage in, for example, domestic violent behaviors, which seem to be an inheritable legacy.
Acknowledgments
The authors appreciate the assistance of Danielle Jean Kradin and Margaret A Madigan for their contributions in formatting the paper.
Author Contributions
The initial draft concept, formatting, literature review, writing and editing. was developed by E.J.M., K.B. and A.B. developed schematic figure models. C.A.D., B.W.D., D.B. (Debasis Bagchi), L.L.-G., I.E., D.B. (David Baron), P.K.T., R.D.B., E.R.B., A.G. and M.S.G. made significant editorial comments and All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
K.B. is the inventor of GARS and Pro-Dopamine Regulation Nutraceuticals (PDRN) and holds a number of both USA and foreign patents issued and pending. The PDRN has been exclusively licensed to iVitalize Inc. There is also a sublicense with Victory Nutrition International (VNI). L.L.-G. is a volunteer and associated with the “The Kenneth Blum Behavioral & Neurogenetic Institute”, Austin, (Division of iVitalize, Inc. San Antonio, TX, USA) TX, USA. B.W.D. and D. Bagchi are associated with VNI. There are no other conflict to report.
Funding Statement
K.B. along with Marjorie C Gondre-Lewis are recipients of R41 MD012318/MD/NIMHD NIH HHS/United States. R.D.B. is the recipient of1 I01 CX002099-01 (PI: Badgaiyan) Merit Review Grant, Veterans Administration. P.K.T. is the recipient of DA046794/National Institutes of Health (US); Q0942016/New York Research Foundation; R01 DA046794/DA/NIDA NIH HHS/United States; R01 HD070888/HD/NICHD NIH HHS/United States; HD070888/National Institutes of Health (US).
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.De Almeida R.M., Ferrari P.F., Parmigiani S., Miczek K.A. Escalated aggressive behavior: Dopamine, serotonin and GABA. Eur. J. Pharmacol. 2005;526:51–64. doi: 10.1016/j.ejphar.2005.10.004. [DOI] [PubMed] [Google Scholar]
- 2.Rosell D.R., Siever L.J. The neurobiology of aggression and violence. CNS Spectr. 2015;20:254–279. doi: 10.1017/S109285291500019X. [DOI] [PubMed] [Google Scholar]
- 3.Fernandez F., Byrne M.K., Batterham M., Grant L., Meyer B.J. Associations between Omega-3 Index, Dopaminergic Genetic Variants and Aggressive and Metacognitive Traits: A Study in Adult Male Prisoners. Nutrients. 2022;14:1379. doi: 10.3390/nu14071379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Coccaro E.F., Lee R.J. Disordered Aggression and Violence in the United States. J. Clin. Psychiatry. 2020;81:19m12937. doi: 10.4088/JCP.19m12937. [DOI] [PubMed] [Google Scholar]
- 5.Umhau J.C., Trandem K., Shah M., George D.T. The physician’s unique role in preventing violence: A neglected opportunity? BMC Med. 2012;10:146. doi: 10.1186/1741-7015-10-146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.David-Ferdon C., Hertz M.F. Electronic media, violence, and adolescents: An emerging public health problem. J. Adolesc Health. 2007;6:S1–S5. doi: 10.1016/j.jadohealth.2007.08.020. [DOI] [PubMed] [Google Scholar]
- 7.Puhalla A.A., Berman M.E., Coccaro E.F., Fahlgren M.K., McCloskey M.S. History of childhood abuse and alcohol use disorder: Relationship with intermittent explosive disorder and intoxicated aggression frequency. J. Psychiatr. Res. 2020;125:38–44. doi: 10.1016/j.jpsychires.2020.02.025. [DOI] [PubMed] [Google Scholar]
- 8.Montalvo-Ortiz J.L., Zhang H., Chen C., Liu C., Coccaro E.F. Genome-Wide DNA Methylation Changes Associated with Intermittent Explosive Disorder: A Gene-Based Functional Enrichment Analysis. Int. J. Neuropsychopharmacol. 2018;21:12–20. doi: 10.1093/ijnp/pyx087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gillet C., Polard E., Mauduit N., Allain H. Passage à l’acte et substances psychoactives: Alcool, médicaments, drogues Acting out and psychoactive substances: Alcohol, drugs, illicit substances. Encephale. 2001;27:351–359. [PubMed] [Google Scholar]
- 10.Kelly J.F., Stout R.L., Tonigan J.S., Magill M., Pagano M.E. Negative affect, relapse, and Alcoholics Anonymous (A.A.): Does A.A. work by reducing anger? J. Stud. Alcohol Drugs. 2010;71:434–444. doi: 10.15288/jsad.2010.71.434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Witkiewitz K., Villarroel N.A. Dynamic association between negative affect and alcohol lapses following alcohol treatment. J. Consult. Clin. Psychol. 2009;77:633–644. doi: 10.1037/a0015647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Salley R.D., Teiling P.A. Dissociated rage attacks in a Vietnam veteran: A Rorschach study. J. Pers. Assess. 1984;48:98–104. doi: 10.1207/s15327752jpa4801_17. [DOI] [PubMed] [Google Scholar]
- 13.Carvalho H.B., Seibel S.D. Crack cocaine use and its relationship with violence and HIV. Clinics. 2009;64:857–866. doi: 10.1590/S1807-59322009000900006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Blum K., Cadet J.L., Gold M.S. Psychostimulant use disorder emphasizing methamphetamine and the opioid -dopamine connection: Digging out of a hypodopaminergic ditch. J. Neurol. Sci. 2021;420:117252. doi: 10.1016/j.jns.2020.117252. [DOI] [PubMed] [Google Scholar]
- 15.Lombroso C. In: The Criminal Man. Durham N.C., editor. Duke University Press; Durham, NC, USA: 2006. [Google Scholar]
- 16.Baron R., Richardson D. Human Aggression. Plenum Press; New York, NY, USA: 1994. [Google Scholar]
- 17.Ferguson C.J. Genetic contributions to antisocial personality and behavior: A meta-analytic review from an evolutionary perspective. J. Soc. Psychol. 2010;150:160–180. doi: 10.1080/00224540903366503. [DOI] [PubMed] [Google Scholar]
- 18.Cadoret R.J., Leve L.D., Devor E. Genetics of aggressive and violent behavior. Psychiatr. Clin. North Am. 1997;20:301–322. doi: 10.1016/S0193-953X(05)70314-2. [DOI] [PubMed] [Google Scholar]
- 19.Tiihonen J., Rautiainen M.R., Ollila H.M., Repo-Tiihonen E., Virkkunen M., Palotie A., Pietiläinen O., Kristiansson K., Joukamaa M., Lauerma H., et al. Genetic background of extreme violent behavior. Mol. Psychiatry. 2015;20:786–792. doi: 10.1038/mp.2014.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Maxson S.C. Issues in the search for candidate genes in mice as potential animal models of human aggression. Ciba Found Symp. 1996;194:21–30; discussion 30–35. doi: 10.1002/9780470514825.ch2. [DOI] [PubMed] [Google Scholar]
- 21.Blum K., Kozlowski G.P. Ethanol and neuromodulator interactions: A cascade model of reward. In: Ollat H., Parvez S., Parvez H., editors. Alcohol and Behavior. VSP Press; Utrecht, The Netherlands: 1990. pp. 131–149. [Google Scholar]
- 22.Barlati S., Stefana A., Bartoli F., Bianconi G., Bulgari V., Candini V., Carrà G., Cavalera C., Clerici M., Cricelli M., et al. Violence risk and mental disorders (VIORMED-2): A prospective multicenter study in Italy. PLoS ONE. 2019;14:e0214924. doi: 10.1371/journal.pone.0214924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Blum K., Oscar-Berman M., Demetrovics Z., Barh D., Gold M.S. Genetic Addiction Risk Score (GARS): Molecular neurogenetic evidence for predisposition to Reward Deficiency Syndrome (RDS) Mol. Neurobiol. 2014;50:765–796. doi: 10.1007/s12035-014-8726-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fried L., Modestino E.J., Siwicki D., Lott L., Thanos P.K., Baron D., Badgaiyan R.D., Ponce J.V., Giordano J., Downs W.B., et al. Hypodopaminergia and “Precision Behavioral Management”(PBM): It is a Generational Family Affair. Curr. Pharm. Biotechnol. 2020;21:528–541. doi: 10.2174/1389201021666191210112108. [DOI] [PubMed] [Google Scholar]
- 25.Vilas D., Pont-Sunyer C., Tolosa E. Impulse control disorders in Parkinson’s disease. Park. Relat Disord. 2012;18:S80–S84. doi: 10.1016/S1353-8020(11)70026-8. [DOI] [PubMed] [Google Scholar]
- 26.Zainal Abidin S., Tan E.L., Chan S.C., Jaafar A., Lee A.X., Abd Hamid M.H., Abdul Murad N.A., Pakarul Razy N.F., Azmin S., Ahmad Annuar A., et al. DRD and GRIN2B polymorphisms and their association with the development of impulse control behaviour among Malaysian Parkinson’s disease patients. BMC Neurol. 2015;15:59. doi: 10.1186/s12883-015-0316-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Huang W., Ma J.Z., Payne T.J., Beuten J., Dupont R.T., Li M.D. Significant association of DRD1 with nicotine dependence. Hum Genet. 2008;123:133–140. doi: 10.1007/s00439-007-0453-9. [DOI] [PubMed] [Google Scholar]
- 28.Kim D.-J., Park B.L., Yoon S., Lee H.-K., Joe K.-H., Cheon Y.-H., Gwon D.-H., Cho S.-N., Lee H.W., NamGung S., et al. 5′ UTR polymorphism of dopamine receptor D1 (DRD1) associated with severity and temperament of alcoholism. Biochem. Biophys. Res. Commun. 2007;357:1135–1141. doi: 10.1016/j.bbrc.2007.04.074. [DOI] [PubMed] [Google Scholar]
- 29.Misener V.L., Luca P., Azeke O., Crosbie J., Waldman I., Tannock R., Roberts W., Malone M., Schachar R., Ickowicz A., et al. Linkage of the dopamine receptor D1 gene to attention-deficit/hyperactivity disorder. Mol. Psychiatry. 2004;9:500–509. doi: 10.1038/sj.mp.4001440. [DOI] [PubMed] [Google Scholar]
- 30.Schwab-Reese L.M., Parker E.A., Peek-Asa C. The Interaction of Dopamine Genes and Financial Stressors to Predict Adulthood Intimate Partner Violence Perpetration. J. Interpers Violence. 2020;35:1251–1268. doi: 10.1177/0886260517696841. [DOI] [PubMed] [Google Scholar]
- 31.Noble E.P., Gottschalk L.A., Fallon J.H., Ritchie T.L., Wu J.C. D2 dopamine receptor polymorphism and brain regional glucose metabolism. Am. J. Med. Genet. 1997;74:162–166. [PubMed] [Google Scholar]
- 32.Congdon E., Canli T. A neurogenetic approach to impulsivity. J. Pers. 2008;76:1447–1484. doi: 10.1111/j.1467-6494.2008.00528.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Noble E.P. D2 dopamine receptor gene in psychiatric and neurologic disorders and its phenotypes. Am. J. Med. Genet. B Neuropsychiatr. Genet. 2003;116B:103–125. doi: 10.1002/ajmg.b.10005. [DOI] [PubMed] [Google Scholar]
- 34.White M.J., Lawford B.R., Morris C.P., Young R.M. Interaction between DRD2 C957T polymorphism and an acute psychosocial stressor on reward-related behavioral impulsivity. Behav. Genet. 2009;39:285–295. doi: 10.1007/s10519-008-9255-7. [DOI] [PubMed] [Google Scholar]
- 35.White M.J., Morris C.P., Lawford B.R., Young R.M. Behavioral phenotypes of impulsivity related to the ANKK1 gene are independent of an acute stressor. Behav. Brain. Funct. 2008;4:54. doi: 10.1186/1744-9081-4-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nemoda Z., Lyons-Ruth K., Szekely A., Bertha E., Faludi G., Sasvari-Szekely M. Association between dopaminergic polymorphisms and borderline personality traits among at-risk young adults and psychiatric inpatients. Behav. Brain. Funct. 2010;6:4. doi: 10.1186/1744-9081-6-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Forbes E.E., Brown S.M., Kimak M., Ferrell R.E., Manuck S.B., Hariri A.R. Genetic variation in components of dopamine neurotransmission impacts ventral striatal reactivity associated with impulsivity. Mol. Psychiatry. 2009;14:60–70. doi: 10.1038/sj.mp.4002086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Caspi A., McClay J., Moffitt T.E., Mill J., Martin J., Craig I.W., Taylor A., Poulton R. Role of genotype in the cycle of violence in maltreated children. Science. 2002;297:851–854. doi: 10.1126/science.1072290. [DOI] [PubMed] [Google Scholar]
- 39.Boardman J.D., Menard S., Roettger M.E., Knight K.E., Boutwell B.B., Smolen A. Genes in the dopaminergic system and delinquent behaviors across the life course: The role of social controls and risks. Crim. Justice Behav. 2014;41:713–731. doi: 10.1177/0093854813514227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vaske J., Makarios M., Boisvert D., Beaver K.M., Wright J.P. The interaction of DRD2 and violent victimization on depression: An analysis by gender and race. J. Affect Disord. 2009;112:120–125. doi: 10.1016/j.jad.2008.03.027. [DOI] [PubMed] [Google Scholar]
- 41.Thibodeau E.L., Cicchetti D., Rogosch F.A. Child maltreatment, impulsivity, and antisocial behavior in African American children: Moderation effects from a cumulative dopaminergic gene index. Dev. Psychopathol. 2015;27:1621–1636. doi: 10.1017/S095457941500098X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chester D.S., DeWall C.N., Derefinko K.J., Estus S., Lynam D.R., Peters J.R., Jiang Y. Looking for reward in all the wrong places: Dopamine receptor gene polymorphisms indirectly affect aggression through sensation-seeking. Soc. Neurosci. 2016;11:487–494. doi: 10.1080/17470919.2015.1119191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zai C.C., Ehtesham S., Choi E., Nowrouzi B., De Luca V., Stankovich L., Davidge K., Freeman N., King N., Kennedy J.L., et al. Dopaminergic system genes in childhood aggression: Possible role for DRD2. World J. Biol. Psychiatry. 2012;13:65–74. doi: 10.3109/15622975.2010.543431. [DOI] [PubMed] [Google Scholar]
- 44.Pego A.M.F., Leyton V., Miziara I.D., Bortolin R.H., Freitas R.C.C., Hirata M., Tomaz P.R.X., Santos J.R., Santos P.C.J.L., Yonamine M. SNPs from BCHE and DRD3 genes associated to cocaine abuse amongst violent individuals from Sao Paulo, Brazil. Forensic. Sci. Int. 2020;317:110511. doi: 10.1016/j.forsciint.2020.110511. [DOI] [PubMed] [Google Scholar]
- 45.Cherepkova E.V., Maksimov V.N., Kushnarev A.P., Shakhmatov I.I., Aftanas L.I. The polymorphism of dopamine receptor D4 (DRD4) and dopamine transporter (DAT) genes in the men with antisocial behaviour and mixed martial arts fighters. World J. Biol. Psychiatry. 2019;20:402–415. doi: 10.1080/15622975.2017.1366056. [DOI] [PubMed] [Google Scholar]
- 46.Iofrida C., Palumbo S., Pellegrini S. Molecular genetics and antisocial behavior: Where do we stand? Exp. Biol. Med. (Maywood) 2014;239:1514–1523. doi: 10.1177/1535370214529508. [DOI] [PubMed] [Google Scholar]
- 47.Daigle L.E. Risk heterogeneity and recurrent violent victimization: The role of DRD4. Biodemography Soc. Biol. 2010;56:137–149. doi: 10.1080/19485565.2010.524095. [DOI] [PubMed] [Google Scholar]
- 48.Buchmann A.F., Zohsel K., Blomeyer D., Hohm E., Hohmann S., Jennen-Steinmetz C., Treutlein J., Becker K., Banaschewski T., Schmidt M.H., et al. Interaction between prenatal stress and dopamine D4 receptor genotype in predicting aggression and cortisol levels in young adults. Psychopharmacology. 2014;231:3089–3097. doi: 10.1007/s00213-014-3484-7. [DOI] [PubMed] [Google Scholar]
- 49.Marsman R., Oldehinkel A.J., Ormel J., Buitelaar J.K. The dopamine receptor D4 gene and familial loading interact with perceived parenting in predicting externalizing behavior problems in early adolescence: The TRacking Adolescents’ Individual Lives Survey (TRAILS) Psychiatry Res. 2013;209:66–73. doi: 10.1016/j.psychres.2012.10.022. [DOI] [PubMed] [Google Scholar]
- 50.Nobile M., Giorda R., Marino C., Carlet O., Pastore V., Vanzin L., Bellina M., Molteni M., Battaglia M. Socioeconomic status mediates the genetic contribution of the dopamine receptor D4 and serotonin transporter linked promoter region repeat polymorphisms to externalization in preadolescence. Dev. Psychopathol. 2007;4:1147–1160. doi: 10.1017/S0954579407000594. [DOI] [PubMed] [Google Scholar]
- 51.Bakermans-Kranenburg M.J., Van Ijzendoorn M.H. Gene-environment interaction of the dopamine D4 receptor (DRD4) and observed maternal insensitivity predicting externalizing behavior in preschoolers. Dev. Psychobiol. 2006;48:406–409. doi: 10.1002/dev.20152. [DOI] [PubMed] [Google Scholar]
- 52.Hygen B.W., Belsky J., Stenseng F., Lydersen S., Guzey I.C., Wichstrøm L. Child exposure to serious life events, COMT, and ag-gression: Testing differential susceptibility theory. Dev. Psychol. 2015;51:1098–1104. doi: 10.1037/dev0000020. [DOI] [PubMed] [Google Scholar]
- 53.Brennan P.A., Hammen C., Sylvers P., Bor W., Najman J., Lind P., Montgomery G., Smith A.K. Interactions between the COMT Val108/158Met polymorphism and maternal prenatal smoking predict aggressive behavior outcomes. Biol. Psychol. 2011;87:99–105. doi: 10.1016/j.biopsycho.2011.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wang M., Chen P., Li H., Kemp A.H., Zhang W. Catechol-O-Methyltransferase Gene Val158Met Polymorphism Moderates the Effect of Social Exclusion and Inclusion on Aggression in Men: Findings From a Mixed Experimental Design. Front. Psychol. 2021;11:622914. doi: 10.3389/fpsyg.2020.622914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Comings D.E., MacMurray J.P. Molecular heterosis: A review. Mol. Genet. Metab. 2000;71:19–31. doi: 10.1006/mgme.2000.3015. [DOI] [PubMed] [Google Scholar]
- 56.Vinkers C.H., Van Gastel W.A., Schubart C.D., Van Eijk K.R., Luykx J.J., Van Winkel R., Joëls M., Ophoff R.A., Boks M.P., Genetic Risk and Outcome of Psychosis (GROUP) Investigators et al. The effect of childhood maltreatment and cannabis use on adult psychotic symptoms is modified by the COMT Val1⁵⁸Met polymorphism. Schizophr. Res. 2013;150:303–311. doi: 10.1016/j.schres.2013.07.020. [DOI] [PubMed] [Google Scholar]
- 57.Johnson S.W., North R.A. Opioids excite dopamine neurons by hyperpolarization of local interneurons. J. Neurosci. 1992;12:483–488. doi: 10.1523/JNEUROSCI.12-02-00483.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Corley R.P., Zeiger J.S., Crowley T., Ehringer M.A., Hewitt J.K., Hopfer C.J., Lessem J., McQueen M.B., Rhee S.H., Smolen A., et al. Association of candidate genes with antisocial drug dependence in adolescents. Drug Alcohol Depend. 2008;96:90–98. doi: 10.1016/j.drugalcdep.2008.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Dong H., Hayashi K., Fairbairn N., Milloy M.-J., DeBeck K., Wood E., Kerr T. Long Term Pre-Treatment Opioid Use Trajectories in Relation to Opioid Agonist Therapy Outcomes among People Who Use Drugs in a Canadian Setting. Addict. Behav. 2021;112:106655. doi: 10.1016/j.addbeh.2020.106655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Coid J., Allolio B., Rees L.H. Raised plasma metenkephalin in patients who habitually mutilate themselves. Lancet. 1983;2:545–546. doi: 10.1016/s0140-6736(83)90572-x. [DOI] [PubMed] [Google Scholar]
- 61.Symons F.J., Thompson A., Rodriguez M.C. Self-injurious behavior and the efficacy of naltrexone treatment: A quantitative synthesis. Ment. Retard Dev. Disabli. Res. Rev. 2004;10:13–22. doi: 10.1002/mrdd.20031. [DOI] [PubMed] [Google Scholar]
- 62.Saini P., Clements C., Gardner K.J., Chopra J., Latham C., Kumar R., Taylor P. Identifying Suicide and Self-Harm Research Priorities in North West England. Crisis. 2022;43:35–45. doi: 10.1027/0227-5910/a000757. [DOI] [PubMed] [Google Scholar]
- 63.Macdonald G., Leary M.R. Why does social exclusion hurt?: The relationship between social and physical pain. Psychol. Bull. 2005;131:202–223. doi: 10.1037/0033-2909.131.2.202. [DOI] [PubMed] [Google Scholar]
- 64.Panksepp J. Feeling the pain of social loss. Science. 2003;302:237–239. doi: 10.1126/science.1091062. [DOI] [PubMed] [Google Scholar]
- 65.Siever L.J. Neurobiology of aggression and violence. Am. J. Psychiatry. 2008;165:429–442. doi: 10.1176/appi.ajp.2008.07111774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lötsch J., Geisslinger G. Relevance of Frequent Mu-Opioid Receptor Polymorphisms for Opioid Activity in Healthy Volunteers. Pharm. J. 2006;6:200–210. doi: 10.1038/sj.tpj.6500362. [DOI] [PubMed] [Google Scholar]
- 67.Cimino S., Carola V., Cerniglia L., Bussone S., Bevilacqua A., Tambelli R. The μ-opioid receptor gene A118G polymorphism is associated with insecure attachment in children with disruptive mood regulation disorder and their mothers. Brain. Behav. 2020;10:e01659. doi: 10.1002/brb3.1659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Menon S., Lea R.A., Roy B., Hanna M., Wee S., Haupt L.M., Griffiths L.R. The human μ-opioid receptor gene polymorphism (A118G) is associated with head pain severity in a clinical cohort of female migraine with aura patients. J. Headache Pain. 2012;13:513–519. doi: 10.1007/s10194-012-0468-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Tchalova K., Sadikaj G., Moskowitz D.S., Zuroff D.C., Bartz J.A. Variation in the μ-opioid receptor gene (OPRM1) and experiences of felt security in response to a romantic partner’s quarrelsome behavior. Mol. Psychiatry. 2021;8:3847–3857. doi: 10.1038/s41380-019-0600-4. [DOI] [PubMed] [Google Scholar]
- 70.Bertoletti E., Zanoni A., Giorda R., Battaglia M. Influence of the OPRM1 gene polymorphism upon children’s degree of withdrawal and brain activation in response to facial expressions. Dev. Cogn. Neurosci. 2012;2:103–109. doi: 10.1016/j.dcn.2011.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Troisi A., Frazzetto G., Carola V., Di Lorenzo G., Coviello M., Siracusano A., Gross C. Variation in the μ-opioid receptor gene (OPRM1) moderates the influence of early maternal care on fearful attachment. Soc. Cogn. Affect. Neurosci. 2012;7:542–547. doi: 10.1093/scan/nsr037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Way B.M., Taylor S.E., Eisenberger N.I. Variation in the mu-opioid receptor gene (OPRM1) is associated with dispositional and neural sensitivity to social rejection. Proc. Natl. Acad. Sci. USA. 2009;106:15079–15084. doi: 10.1073/pnas.0812612106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Qadeer M.I., Amar A., Mann J.J., Hasnain S. Polymorphisms in dopaminergic system genes; association with criminal behavior and self-reported aggression in violent prison inmates from Pakistan. PLoS ONE. 2017;12:e0173571. doi: 10.1371/journal.pone.0173571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Fine A., Mahler A., Simmons C., Chen C., Moyzis R., Cauffman E. Relations between three dopaminergic system genes, school attachment, and adolescent delinquency. Dev. Psychol. 2016;52:1893–1903. doi: 10.1037/dev0000166. [DOI] [PubMed] [Google Scholar]
- 75.Young S.E., Smolen A., Corley R.P., Krauter K.S., DeFries J.C., Crowley T.J., Hewitt J.K. Dopamine transporter polymorphism associated with externalizing behavior problems in children. Am. J. Med. Genet. 2002;114:144–149. doi: 10.1002/ajmg.10155. [DOI] [PubMed] [Google Scholar]
- 76.Burt S.A., Mikolajewski A.J. Preliminary evidence that specific candidate genes are associated with adolescent-onset antisocial behavior. Aggress Behav. 2008;34:437–445. doi: 10.1002/ab.20251. [DOI] [PubMed] [Google Scholar]
- 77.Uršič K., Zupanc T., Paska A.V. Analysis of promoter polymorphism in monoamine oxidase A (MAOA) gene in completed suicide on Slovenian population. Neurosci. Lett. 2018;673:111–115. doi: 10.10.16/j.neulet.2018.02.063. [DOI] [PubMed] [Google Scholar]
- 78.Beaver K.M., DeLisi M., Vaughn M.G., Barnes J.C. Monoamine oxidase A genotype is associated with gang membership and weapon use. Compr. Psychiatry. 2010;51:130–134. doi: 10.1016/j.comppsych.2009.03.010. [DOI] [PubMed] [Google Scholar]
- 79.Kolla N.J., Vinette S.A. Monoamine Oxidase A in Antisocial Personality Disorder and Borderline Personality Disorder. Curr. Behav. Neurosci. Rep. 2017;4:41–48. doi: 10.1007/s40473-017-0102-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Kolla N.J., Dunlop K., Meyer J.H., Downar J. Corticostriatal Connectivity in Antisocial Personality Disorder by MAO-A Genotype and Its Relationship to Aggressive Behavior. Int. J. Neuropsychopharmacol. 2018;2:725–733. doi: 10.1093/ijnp/pyy035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Gerra G., Garofano L., Bosari S., Pellegrini C., Zaimovic A., Moi G., Bussandri M., Moi A., Brambilla F., Mameli A., et al. Analysis of monoamine oxidase A (MAO-A) promoter polymorphism in male heroin-dependent subjects: Behavioural and personality correlates. J. Neural. Transm (Vienna) 2004;111:611–621. doi: 10.1007/s00702-004-0129-8. [DOI] [PubMed] [Google Scholar]
- 82.Alia-Klein N., Goldstein R.Z., Kriplani A., Logan J., Tomasi D., Williams B., Telang F., Shumay E., Biegon A., Craig I.W., et al. Brain monoamine oxidase A activity predicts trait aggression. J. Neurosci. 2008;28:5099–5104. doi: 10.1523/JNEUROSCI.0925-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kolla N.J., Attard S., Craig G., Blackwood N., Hodgins S. Monoamine oxidase A alleles in violent offenders with antisocial per-sonality disorder: High activity associated with proactive aggression. Crim. Behav. Ment. Health. 2014;24:368–372. doi: 10.1002/cbm.1917. [DOI] [PubMed] [Google Scholar]
- 84.Huang Y.Y., Cate S.P., Battistuzzi C., Oquendo M.A., Brent D., Mann J.J. An association between a functional polymorphism in the monoamine oxidase a gene promoter, impulsive traits and early abuse experiences. Neuropsychopharmacology. 2004;29:1498–1505. doi: 10.1038/sj.npp.1300455. [DOI] [PubMed] [Google Scholar]
- 85.Ni X., Sicard T., Bulgin N., Bismil R., Chan K., McMain S., Kennedy J.L. Monoamine oxidase a gene is associated with borderline personality disorder. Psychiatr. Genet. 2007;17:53–57. doi: 10.1097/YPG.0b013e328016831c. [DOI] [PubMed] [Google Scholar]
- 86.Schlüter T., Winz O., Henkel K., Eggermann T., Mohammadkhani-Shali S., Dietrich C., Heinzel A., Decker M., Cumming P., Zerres K., et al. MAOA-VNTR polymorphism modulates context-dependent dopamine release and aggressive behavior in males. Neuroimage. 2016;125:378–385. doi: 10.1016/j.neuroimage.2015.10.031. [DOI] [PubMed] [Google Scholar]
- 87.Stetler D.A., Davis C., Leavitt K., Schriger I., Benson K., Bhakta S., Wang L.C., Oben C., Watters M., Haghnegahdar T., et al. Association of low-activity MAOA allelic variants with violent crime in incarcerated offenders. J. Psychiatr. Res. 2014;58:69–75. doi: 10.1016/j.jpsychires.2014.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Tikkanen R., Sjöberg R.L., Ducci F., Goldman D., Holi M., Tiihonen J., Virkkunen M. Effects of MAOA-genotype, alcohol consumption, and aging on violent behavior. Alcohol Clin. Exp. Res. 2009;33:428–434. doi: 10.1111/j.1530-0277.2008.00853.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Klasen M., Wolf D., Eisner P.D., Habel U., Repple J., Vernaleken I., Schlüter T., Eggermann T., Zerres K., Zepf F.D., et al. Neural networks underlying trait aggression depend on MAOA gene alleles. Brain. Struct Funct. 2018;223:873–881. doi: 10.1007/s00429-017-1528-6. [DOI] [PubMed] [Google Scholar]
- 90.Zhang Y., Ming Q., Wang X., Yao S. The interactive effect of the MAOA-VNTR genotype and childhood abuse on aggressive behaviors in Chinese male adolescents. Psychiatr. Genet. 2016;26:117–123. doi: 10.1097/YPG.0000000000000125. [DOI] [PubMed] [Google Scholar]
- 91.Ziermans T., Dumontheil I., Roggeman C., Peyrard-Janvid M., Matsson H., Kere J., Klingberg T. Working memory brain activity and capacity link MAOA polymorphism to aggressive behavior during development. Transl. Psychiatry. 2012;2:e85. doi: 10.1038/tp.2012.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Fite P.J., Brown S., Hossain W., Manzardo A., Butler M.G., Bortolato M. Tobacco and cannabis use in college students are predicted by sex-dimorphic interactions between MAOA genotype and child abuse. CNS Neurosci. Ther. 2019;25:101–111. doi: 10.1111/cns.13002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Kuepper Y., Grant P., Wielpuetz C., Hennig J. MAOA-uVNTR genotype predicts interindividual differences in experimental aggressiveness as a function of the degree of provocation. Behav. Brain. Res. 2013;247:73–78. doi: 10.1016/j.bbr.2013.03.002. [DOI] [PubMed] [Google Scholar]
- 94.Vanyukov M.M., Moss H.B., Yu L.M., Deka R. A dinucleotide repeat polymorphism at the gene for monoamine oxidase A and measures of aggressiveness. Psychiatry Res. 1995;59:35–41. doi: 10.1016/0165-1781(95)02719-X. [DOI] [PubMed] [Google Scholar]
- 95.Frazzetto G., Di Lorenzo G., Carola V., Proietti L., Sokolowska E., Siracusano A., Gross C., Troisi A. Early trauma and increased risk for physical aggression during adulthood: The moderating role of MAOA genotype. PLoS ONE. 2007;2:e486. doi: 10.1371/journal.pone.0000486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Lu Y.F., Menard S. The Interplay of MAOA and Peer Influences in Predicting Adult Criminal Behavior. Psychiatr. Q. 2017;88:115–128. doi: 10.1007/s11126-016-9441-3. [DOI] [PubMed] [Google Scholar]
- 97.Eisenberger N.I., Way B.M., Taylor S.E., Welch W.T., Lieberman M.D. Understanding genetic risk for aggression: Clues from the brain’s response to social exclusion. Biol. Psychiatry. 2007;61:1100–1108. doi: 10.1016/j.biopsych.2006.08.007. [DOI] [PubMed] [Google Scholar]
- 98.Denson T.F., Dobson-Stone C., Ronay R., Von Hippel W., Schira M.M. A functional polymorphism of the MAOA gene is associated with neural responses to induced anger control. J. Cogn. Neurosci. 2014;J26:1418–1427. doi: 10.1162/jocn_a_00592. [DOI] [PubMed] [Google Scholar]
- 99.Buckholtz J.W., Meyer-Lindenberg A. MAOA and the neurogenetic architecture of human aggression. Trends Neurosci. 2008;31:120–129. doi: 10.1016/j.tins.2007.12.006. [DOI] [PubMed] [Google Scholar]
- 100.Kinnally E.L., Huang Y.Y., Haverly R., Burke A.K., Galfalvy H., Brent D.P., Oquendo M.A., Mann J.J. Parental care moderates the influence of MAOA-uVNTR genotype and childhood stressors on trait impulsivity and aggression in adult women. Psychiatr. Genet. 2009;19:126–133. doi: 10.1097/YPG.0b013e32832a50a7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Atramentova L.A., Luchko E.N. Aggression and empathy as genetic differentiation factors of urban population. Genetika. 2016;52:705–712. doi: 10.1134/S1022795416050021. [DOI] [PubMed] [Google Scholar]
- 102.Tielbeek J.J., Karlsson Linnér R., Beers K., Posthuma D., Popma A., Polderman T.J. Meta-analysis of the serotonin transporter promoter variant (5-HTTLPR) in relation to adverse environment and antisocial behavior. Am. J. Med. Genet. B Neuropsychiatr Genet. 2016;171:748–760. doi: 10.1002/ajmg.b.32442. [DOI] [PubMed] [Google Scholar]
- 103.Tung I., Lee S.S. Latent trajectories of adolescent antisocial behavior: Serotonin transporter linked polymorphic region (5-HTTLPR) genotype influences sensitivity to perceived parental support. Dev. Psychopathol. 2017;29:185–201. doi: 10.1017/S0954579416000031. [DOI] [PubMed] [Google Scholar]
- 104.Courtet P., Baud P., Abbar M., Boulenger J.P., Castelnau D., Mouthon D., Malafosse A., Buresi C. Association between violent suicidal behavior and the low activity allele of the serotonin transporter gene. Mol. Psychiatry. 2001;6:338–341. doi: 10.1038/sj.mp.4000856. [DOI] [PubMed] [Google Scholar]
- 105.Bellivier F., Szöke A., Henry C., Lacoste J., Bottos C., Nosten-Bertrand M., Hardy P., Rouillon F., Launay J.M., Laplanche J.L., et al. Possible association between serotonin transporter gene polymorphism and violent suicidal behavior in mood disorders. Biol. Psychiatry. 2000;48:319–322. doi: 10.1016/s0006-3223(00)00891-x. [DOI] [PubMed] [Google Scholar]
- 106.Retz W., Retz-Junginger P., Supprian T., Thome J., Rösler M. Association of serotonin transporter promoter gene polymorphism with violence: Relation with personality disorders, impulsivity, and childhood ADHD psychopathology. Behav. Sci. Law. 2004;22:415–425. doi: 10.1002/bsl.589. [DOI] [PubMed] [Google Scholar]
- 107.Gorodetsky E., Carli V., Sarchiapone M., Roy A., Goldman D., Enoch M.A. Predictors for self-directed aggression in Italian prisoners include externalizing behaviors, childhood trauma and the serotonin transporter gene polymorphism 5-HTTLPR. Genes. Brain. Behav. 2016;15:465–473. doi: 10.1111/gbb.12293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Hallikainen T., Saito T., Lachman H.M., Volavka J., Pohjalainen T., Ryynänen O.P., Kauhanen J., Syvälahti E., Hietala J., Tiihonen J. Association between low activity serotonin transporter promoter genotype and early onset alcoholism with habitual impulsive violent behavior. Mol. Psychiatry. 1999;4:385–388. doi: 10.1038/sj.mp.4000526. [DOI] [PubMed] [Google Scholar]
- 109.Liao D.L., Hong C.J., Shih H.L., Tsai S.J. Possible association between serotonin transporter promoter region polymorphism and extremely violent crime in Chinese males. Neuropsychobiology. 2004;50:284–287. doi: 10.1159/000080953. [DOI] [PubMed] [Google Scholar]
- 110.Zalsman G., Frisch A., Bromberg M., Gelernter J., Michaelovsky E., Campino A., Erlich Z., Tyano S., Apter A., Weizman A. Fam-ily-based association study of serotonin transporter promoter in suicidal adolescents: No association with suicidality but possible role in violence traits. Am. J. Med. Genet. 2001;105:239–245. doi: 10.1002/ajmg.1261. [DOI] [PubMed] [Google Scholar]
- 111.Gonda X., Fountoulakis K.N., Csukly G., Bagdy G., Pap D., Molnár E., Laszik A., Lazary J., Sarosi A., Faludi G., et al. Interaction of 5-HTTLPR genotype and unipolar major depression in the emergence of aggressive/hostile traits. J. Affect Disord. 2011;132:432–437. doi: 10.1016/j.jad.2011.03.029. [DOI] [PubMed] [Google Scholar]
- 112.Fanelli G., Serretti A. The influence of the serotonin transporter gene 5-HTTLPR polymorphism on suicidal behaviors: A meta-analysis. Prog. Neuropsychopharmacol. Biol. Psychiatry. 2019;88:375–387. doi: 10.1016/j.pnpbp.2018.08.007. [DOI] [PubMed] [Google Scholar]
- 113.Pawlak J., Dmitrzak-Weglarz M., Wilkosc M., Szczepankiewicz A., Leszczynska-Rodziewicz A., Zaremba D., Kapelski P., Rajewska-Rager A., Hauser J. Suicide behavior as a quantitative trait and its genetic background. J. Affect Disord. 2016;206:241–250. doi: 10.1016/j.jad.2016.07.029. [DOI] [PubMed] [Google Scholar]
- 114.Bondy B., Erfurth A., De Jonge S., Krüger M., Meyer H. Possible association of the short allele of the serotonin transporter promoter gene polymorphism (5-HTTLPR) with violent suicide. Mol. Psychiatry. 2000;5:193–195. doi: 10.1038/sj.mp.4000678. [DOI] [PubMed] [Google Scholar]
- 115.Rujescu D., Giegling I., Sato T., Moeller H.J. A polymorphism in the promoter of the serotonin transporter gene is not associated with suicidal behavior. Psychiatr. Genet. 2001;11:169–172. doi: 10.1097/00041444-200109000-00011. [DOI] [PubMed] [Google Scholar]
- 116.Chen T.J., Blum K., Mathews D., Fisher L., Schnautz N., Braverman E.R., Schoolfield J., Downs B.W., Comings D.E. Are dopaminergic genes involved in a predisposition to pathological aggression? Hypothesizing the importance of “super normal controls” in psychiatric genetic research of complex behavioral disorders. Med. Hypotheses. 2005;65:703–707. doi: 10.1016/j.mehy.2005.04.037. [DOI] [PubMed] [Google Scholar]
- 117.Blum K., Chen A.L., Giordano J., Borsten J., Chen T.J., Hauser M., Simpatico T., Femino J., Braverman E.R., Barh D. The addictive brain: All roads lead to dopamine. J. Psychoact. Drugs. 2012;44:134–143. doi: 10.1080/02791072.2012.685407. [DOI] [PubMed] [Google Scholar]
- 118.Blum K., Braverman E.R., Holder J.M., Lubar J.F., Monastra V.J., Miller D., Lubar J.O., Chen T.J., Comings D.E. Reward deficiency syndrome: A biogenetic model for the diagnosis and treatment of impulsive, addictive, and compulsive behaviors. J. Psychoact. Drugs. 2000;32:1–112. doi: 10.1080/02791072.2000.10736099. [DOI] [PubMed] [Google Scholar]
- 119.Cuomo C., Sarchiapone M., Giannantonio M.D., Mancini M., Roy A. Aggression, impulsivity, personality traits, and childhood trauma of prisoners with substance abuse and addiction. Am. J. Drug Alcohol Abuse. 2008;34:339–345. doi: 10.1080/00952990802010884. [DOI] [PubMed] [Google Scholar]
- 120.Davis A.K., Bonar E.E., Goldstick J.E., Walton M.A., Winters J., Chermack S.T. Binge-drinking and non-partner aggression are associated with gambling among Veterans with recent substance use in V.A. outpatient treatment. Addict Behav. 2017;74:27–32. doi: 10.1016/j.addbeh.2017.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Jones R.M., Van Den Bree M., Zammit S., Taylor P.J. Change in the Relationship Between Drinking Alcohol and Risk of Violence Among Adolescents and Young Adults: A Nationally Representative Longitudinal Study. Alcohol Alcohol. 2020;55:439–447. doi: 10.1093/alcalc/agaa020. [DOI] [PubMed] [Google Scholar]
- 122.Kaufmann V.G., O’Farrell T.J., Murphy C.M., Murphy M.M., Muchowski P. Alcohol consumption and partner violence among women entering substance use disorder treatment. Psychol. Addict Behav. 2014;28:313–321. doi: 10.1037/a0034971. [DOI] [PubMed] [Google Scholar]
- 123.Norström T., Pape H. Alcohol, suppressed anger and violence. Addiction. 2010;105:1580–1586. doi: 10.1111/j.1360-0443.2010.02997.x. [DOI] [PubMed] [Google Scholar]
- 124.Singh V., Epstein-Ngo Q., Cunningham R.M., Stoddard S.A., Chermack S.T., Walton M.A. Physical dating violence among adolescents and young adults with alcohol misuse. Drug Alcohol Depend. 2015;153:364–368. doi: 10.1016/j.drugalcdep.2015.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.O’Brien K.S., Forrest W., Greenlees I., Rhind D., Jowett S., Pinsky I., Espelt A., Bosque-Prous M., Sonderlund A.L., Vergani M., et al. Alcohol consumption, masculinity, and alcohol-related violence and antisocial behaviour in sportspeople. J. Sci. Med. Sport. 2018;21:335–341. doi: 10.1016/j.jsams.2017.06.019. [DOI] [PubMed] [Google Scholar]
- 126.Neavins T.M., Murphy C.M., Yiaslas T.A., Demorest M.E. Daily and situational reports of substance use and dating violence among college students: A 10-week prospective study. Addict Behav. Rep. 2020;12:100309. doi: 10.1016/j.abrep.2020.100309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Phillips T.J., Mootz J.R., Reed C. Identification of Treatment Targets in a Genetic Mouse Model of Voluntary Methamphetamine Drinking. Int. Rev. Neurobiol. 2016;126:39–85. doi: 10.1016/bs.irn.2016.02.001. [DOI] [PubMed] [Google Scholar]
- 128.Zhai Z.W., Duenas G.L., Wampler J., Potenza M.N. Gambling, Substance Use and Violence in Male and Female Adolescents. J. Gambl. Stud. 2020;36:1301–1324. doi: 10.1007/s10899-020-09931-8. [DOI] [PubMed] [Google Scholar]
- 129.Carolina Maria Motta Stoffel B., Felix Henrique P.K., Flavio P., Lisia V.D., Maria Fátima Olivier S., Tatiana H.L., Brazilian Crack Group. Marcelo S.C. Crack users and violence. What is the relationship between trauma, antisocial personality disorder and posttraumatic stress disorder? Addict Behav. 2019;98:106012. doi: 10.1016/j.addbeh.2019.06.001. [DOI] [PubMed] [Google Scholar]
- 130.Sommer J., Hinsberger M., Elbert T., Holtzhausen L., Kaminer D., Seedat S., Madikane S., Weierstall R. The interplay between trauma, substance abuse and appetitive aggression and its relation to criminal activity among high-risk males in South Africa. Addict Behav. 2017;64:29–34. doi: 10.1016/j.addbeh.2016.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Maremmani A.G., Rugani F., Bacciardi S., Rovai L., Pacini M., Dell’Osso L., Maremmani I. Does dual diagnosis affect violence and moderate/superficial self-harm in heroin addiction at treatment entry? J. Addict Med. 2014;8:116–122. doi: 10.1097/ADM.0000000000000019. [DOI] [PubMed] [Google Scholar]
- 132.Irons R., Schneider J.P. When is domestic violence a hidden face of addiction? J. Psychoact. Drugs. 1997;4:337–344. doi: 10.1080/02791072.1997.10400560. [DOI] [PubMed] [Google Scholar]
- 133.Arteaga A., Fernández-Montalvo J., López-Goñi J.J. Prevalence and differential profile of patients with drug addiction problems who commit intimate partner violence. Am. J. Addict. 2015;24:756–764. doi: 10.1111/ajad.12302. [DOI] [PubMed] [Google Scholar]
- 134.McGinty E.E., Choksy S., Wintemute G.J. The Relationship Between Controlled Substances and Violence. Epidemiol. Rev. 2016;38:5–31. doi: 10.1093/epirev/mxv008. [DOI] [PubMed] [Google Scholar]
- 135.Murray R.L., Chermack S.T., Walton M.A., Winters J., Booth B.M., Blow F.C. Psychological aggression, physical aggression, and injury in nonpartner relationships among men and women in treatment for substance-use disorders. J. Stud. Alcohol Drugs. 2008;69:896–905. doi: 10.15288/jsad.2008.69.896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Czermainski F.R., Lopes F.M., Ornell F., Pinto Guimarães L.S., Von Diemen L., Kessler F., Martins de Almeida R.M. Concurrent Use of Alcohol and Crack Cocaine is Associated with High Levels of Anger and Liability to Aggression. Subst. Use Misuse. 2020;55:1660–1666. doi: 10.1080/10826084.2020.1756850. [DOI] [PubMed] [Google Scholar]
- 137.Stoddard S.A., Meier-Austic E., Epstein-Ngo Q., Walton M., Carter P.M., Heinze J.E., Zimmerman M.A., Cunningham R. Substance use and mental health predictors of patterns of non-partner youth violence among high-risk urban youth. Drug Alcohol Depend. 2020;213:108117. doi: 10.1016/j.drugalcdep.2020.108117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Ahmadi K., Javadinia S.A., Saadat S.H., Ramezani M.A., Sedghijalal H. Triangular relationship among risky sexual behavior, addiction, and aggression: A systematic review. Electron. Physician. 2017;9:5129–5137. doi: 10.19082/5129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Blum K., Bowirrat A., Braverman E.R., Baron D., Cadet J.L., Kazmi S., Elman I., Thanos P.K., Badgaiyan R.D., Downs W.B., et al. Reward Deficiency Syndrome (RDS): A Cytoarchitectural Common Neurobiological Trait of All Addictions. Int. J. Environ. Res. Public Health. 2021;18:11529. doi: 10.3390/ijerph182111529. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.