Abstract
Psychological distress (including depression and anxiety) is common in the first years of cancer diagnosis but can differ by country and region. The aim of the present paper was to review the prevalence of psychological distress among cancer patients in the Southeast Asia (SEA) region. A systematic literature search was carried out using several databases (i.e., PubMed, PsychARTICLES, Embase, CINAHI, Web of Sciences, Plus, Scopus, and AHMED). Papers originally published in English language were taken into consideration if they (i) were published from 2010 to 2021 and (ii) reported the prevalence of psychological distress among patients with different types of cancer. A total of 23 studies met the inclusion criteria. The most frequently employed psychometric instrument for anxiety and depression screening was the Hospital Anxiety and Depression Scale (HADS). The prevalence of anxiety (ranging from 7% to 88%) was wider than that of depression (ranging from 3% to 65.5%) among patients with different types of cancer and living in various countries in the SEA region. The overall prevalence rate of psychological distress among cancer patients from the SEA region was not fundamentally very different from that of general populations. These findings provide useful information for health professionals and cancer patients to understand the negative role of psychological distress in quality of life and health. The research findings demonstrate the importance of counselling for psychological distress among cancer patients as means of effectively resolving their psychological problems and ultimately improving the quality of oncology medical care. Clinical recommendations for cancer management should incorporate the early identification of (and therapy for) psychological distress, as well as their monitoring during treatment.
Keywords: anxiety, cancer, depression, psychological distress, Southeast Asia
1. INTRODUCTION
After heart disease, cancer is the second most major cause of death worldwide (Nagai & Kim, 2017; Yusof et al., 2016). The number of new cases of cancer diagnosed every year around the world is predicted by the World Health Organisation to increase by 69% to 21 million by 2030 (Vorn et al., 2019). It is also the largest cause of death in Southeast Asia (SEA) (Kimman et al., 2017). The incidence of cancer cases is estimated to increase in Asia from 6.1 million in 2008 to 10.8 million in 2030 and cancer deaths from 4.1 million in 2008 to 7.6 million in 2030 due to population growth and ageing, as well as changes in lifestyle and socio‐economic status (Sankaranarayanan et al., 2014). These patients also present in SEA's poorer countries and mortality rates are much higher (Kimman et al., 2017).
Cancer patients live with disease and side effects of cancer treatment (Gallicchio et al., 2018; Mercadante et al., 2019). Receiving a diagnosis of cancer may induce psychological challenges such as depression, anxiety, hopelessness, feelings of fear, and pain (Leong Abdullah et al., 2015). Patients experience psychological symptoms due to the consequence of illness. Studies have consistently shown that anxiety and depression are the most common mental health disorders experienced among cancer patients (Almigbal et al., 2019). In the SEA region, having cancer has been reported to include a wide range of negative impacts including poor mental health, body image concerns, sexual problems, and poor quality of life (Civilotti et al., 2020; Setyowibowo et al., 2018). The risk of psychological distress among people with cancer is higher than the general population (Kimman et al., 2017), beginning at diagnosis and extending to the post‐treatment phase of cancer and the long‐term. Psychological distress is related to a lower quality of life and reduction in daily activities (Subramaniam et al., 2018), poorer treatment compliance and poorer efficacy, higher mortality (Ng et al., 2017), and a higher risk of suicide feelings (Giedre & Kamile, 2019). Therefore, addressing the symptoms of depression and anxiety can help improve the quality of life of these patients in the first year of cancer. The physical symptoms of specific cancers can also contribute to anxiety and depression (Khue et al., 2019). Research findings have generally found that psychosocial factors may be risk factors for specific types of cancer development and progression (Kruk et al., 2019).
Several studies in the SEA region have shown that psychological distress is under‐recognised within clinical oncology practice (Action Study Group, 2017). However, in SEA communities, available evidence on psychological distress among cancer patients is arguably limited. Numerous cancer patients have reported that they did not understand their psychosocial needs, failed to recognise and address depression, anxiety, and other emotion symptoms, and/or were unaware of them (Yang et al., 2013). Depression and anxiety are psychological factors characterised by emotional and behavioural aspects (Yang et al., 2013). This can result in poor quality of life (QoL), poor emotional well‐being, and social dysfunction (Endarti et al., 2015). Improving QOL among cancer patients has positive significant public health implications. Several studies have demonstrated that improving QOL among cancer patients is associated with longer survival rates and better mental health (Akhtari‐Zavare et al., 2018). The physical symptoms of specific cancers can also contribute to anxiety and depression (Khue et al., 2019). Research findings have generally found that psychosocial factors may be risk factors for specific types of cancer development and progression (Kruk et al., 2019).
Mahendran et al. (2016) reported patients who were older and underwent baseline surgery were at higher risk of subsyndromal depression 8 months after diagnosis. Another study by Osborn et al. (2006) reported that cognitive behavioural therapy (CBT) and patient education (PE) can decrease depression and anxiety in the short‐term and that quality of life can be increased among cancer patients. A study by the Association of Southeast Asian Nations Costs in Oncology (ACTION) Research (Thinh et al., 2018) was carried out among individuals living in some low‐income and middle‐income SEA countries to assess the impact of cancer on household economic well‐being, quality of life, and psychological distress. The results indicated that 1 year after diagnosis, patients in the SEA region had a mean quality of life that was higher than individuals who did not receive both cancer and psychological distress treatments.
Various studies have shown there are important factors identified that have been associated with levels of psychological distress among cancer patients. These are commonly clustered into psychological, physical, and treatment factors, as well as a range of demographic, socio‐economic, and informational factors (Action Study Group, 2017; Edib et al., 2016). According to a study by Chan et al. (2018), the prevalence rates of anxiety and depression are also different for various types of cancer and that they differ by clinical setting (outpatient clinics, hospitals, and palliative care), stage of the disease (early diagnosed, recurrence, and advanced stages), and phase of treatment (Caruso et al., 2017). Cancer patients experience high levels of anxiety and depression, which may lead to a clinical level of psychological disorder and may adversely affect cancer treatment and recovery (Wong & Lua, 2012). These psychological reactions depend on several factors, including health care and treatment, as well as costs and access to therapy among SEA cancer patients. Cancer treatments including chemotherapy, radiation therapy, and hormone therapy may induce psychological distress through specific biological mechanisms (such as alterations in cortisol levels in plasma blood, which is related to stress and imbalance of homeostasis of their body) (Kruk et al., 2019).
Appropriate screening is required to create and assess personalised intervention among cancer patients (Shunmugasundaram et al., 2020). These screening assessments must be reasonable, appropriate, and related to the demographic study. One study examining screening instruments for anxiety and depression among cancer groups identified 84 studies using 19 different screening instruments (Chahardehi et al., 2017). Commonly, screening methods for anxiety and depression comprise semistructured interviews, and one of the most common screening instruments is the Hospital Anxiety and Depression Scale (HADS) (Setyowibowo et al., 2018).
To the best of the present authors' knowledge, there is no systematic literature review of studies examining psychological distress among cancer patient in SEA countries. Moreover, awareness of health issues affecting cancer patients is still low compared to Western countries. Psychological problems (such as depression and anxiety) are often underdiagnosed and undertreated among cancer patients and need early identification (Brandenbarg et al., 2019). The large majority of studies assessing relationships between cancer and psychological distress have been conducted in Western countries (Krebber et al., 2013), and the generalizability of these studies to the rest of the world, and in particular SEA, is not clear. Moreover, the results of prior studies show contradictory results in the levels of anxiety and depression among cancer patients in SEA countries. Therefore, understanding the impacts of psychological distress among cancer patients in SEA will raise awareness, help promote healthcare policies for cancer patients, and help facilitate better targeting of scarce resources in SEA countries. Therefore, the present review synthesises current knowledge on the existing prevalence of psychological and emotional distress (particularly depression and anxiety) among cancer patients in the SEA region.
2. METHOD
The present review was conducted based on the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) guidelines for conducting and reporting systematic reviews (Moher et al., 2009). PRISMA focuses on the reporting of reviews estimating the impacts of interventions. It can be performed as a basis for reporting systematic reviews with aims other than assessing interventions.
2.1. Search strategy and selection criteria
The research team undertook a literature review search utilising the following EBSCO electronic database, which encompassed medical, psychology, and nursing databases from 2010 to July 2021: Medline Full Text (via PubMed), PsychARTICLES, Embase, CINAHI, Web of Sciences, Plus, Scopus, and AHMED (see Figure 1 for search strategy).
FIGURE 1.
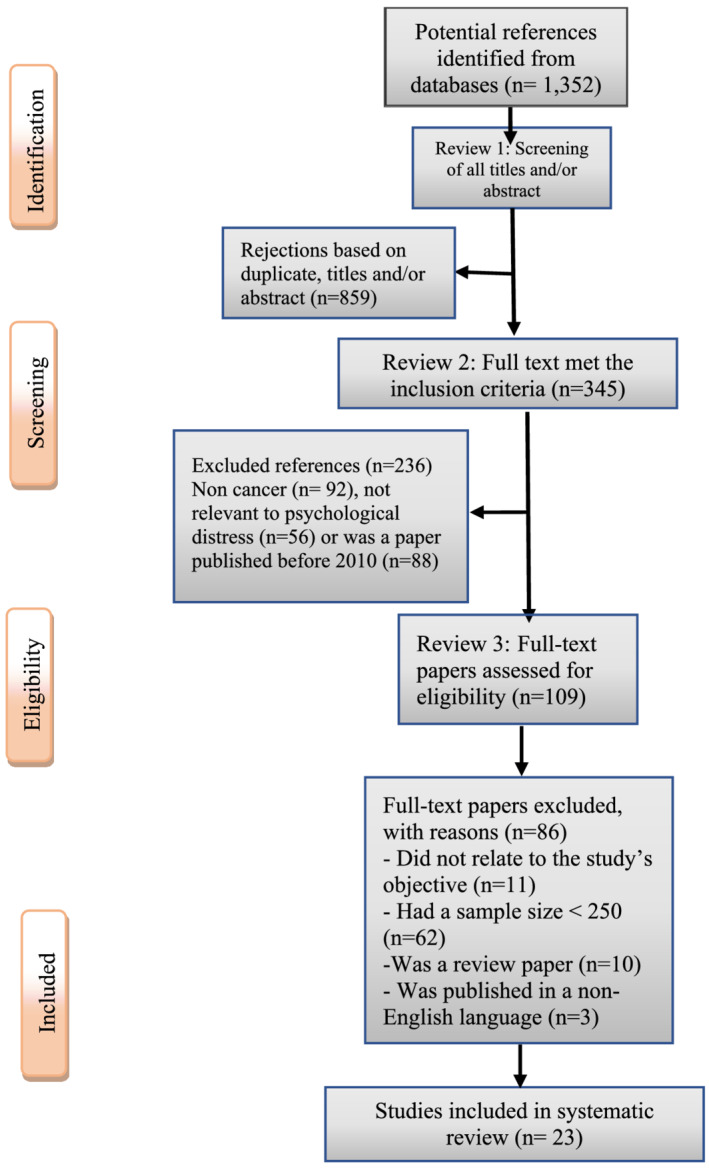
PRISMA flow diagram of study selection procedure
Searches for unpublished studies were conducted utilising ProQuest Dissertations & Thesis Global and Google Scholar. The keywords used for the publication of studies in the English language were combinations of the following: ‘psychological distress’ OR ‘emotional distress’ OR ‘South East Asia cancer’ OR ‘ASEAN [Association of Southeast Asian Nations] cancer’ OR ‘cancer and anxiety’ OR ‘cancer and depression’ OR ‘prevalence’ OR ‘epidemiology’ OR ‘incidence’ OR ‘frequency’ AND ‘Malaysia’ OR ‘Singapore’ OR ‘Indonesia’ OR ‘Myanmar’ OR ‘Laos’ OR ‘Philippines’ OR ‘Thailand’ OR ‘Vietnam’ OR ‘Cambodia’. The search was limited to title and abstract. It was also limited to the affiliation ‘SEA’ and ‘ASEAN’. The authors also manually searched the reference lists of each included paper for additional studies. The obtained papers were imported into an EndNote X9 (Thomson Reuters, Carlsbad, CA, USA) library and the duplicates were removed. Papers were included on the basis of language (i.e., only papers published in the English language) and time period in which they were published (1 January 2010 to 28 February 2021 inclusive). The time period was considered adequate to capture the main themes relating to cancer and psychological distress in the contemporary literature.
2.2. Study inclusion and exclusion criteria
The inclusion criteria included all English language studies that reported the prevalence of any types of cancer among SEA populations conducted in SEA countries with findings related to psychological and emotional distress (particularly depression and anxiety). The review included papers with human participants comprising empirical research papers and epidemiological studies. Studies were excluded from the review if they had very small sample sizes (less than 250 participants), and/or if the output was a review paper, conference abstract, poster paper, letter, commentary or editorial.
Data selection and extraction were shared by three authors, who independently assessed the study eligibility and consulted where necessary to resolve ambiguities. Titles and abstracts were screened according to the inclusion criteria. Full texts of potentially relevant papers were retrieved and screened. The following data from eligible studies were extracted from each included study: first author, year of publication, country of study, number of patients, age (range, median), marital status/gender, cancer type and stage, treatment method, severity of illness, study design, and prevalence of depression and anxiety.
Papers were excluded if the full text was not retrievable, no data on symptoms of depression, anxiety and/or distress, no prevalence statistics, no cancer patients, not being adult at time of diagnosis (≥18 years old), and papers without explicit methodology or results. Studies were also excluded if they (i) were conducted in one of the SEA countries but used samples other than the residents of SEA countries, (ii) focused on risk factors (such as types of smoking) but did not look into their association with psychological and emotional distress, and (iii) were design/protocol papers. In case of disagreement during the selection process, authors discussed the eligibility of a study.
As shown in the PRISMA flow chart (Figure 1), the literature search initially yielded 1352 papers. After removing duplicates and those only containing abstracts, 345 papers with full texts remained. However, 236 papers were removed because they were not relevant to cancer, psychological distress, SEA countries, or were published before 2010. The remaining full‐text papers (n = 109) were then read. Owing to the large body of papers examining psychological distress among cancer patients, only published studies that had large sample sizes of cancer patients (n ≥ 250) were included in the present review. This resulted in 23 studies being included in the present review.
3. RESULTS
A summary of prevalence rates of psychological distress among cancer patients 1 year after the initial diagnosis (and their associated factors) are presented in Table 1.
TABLE 1.
Prevalence of symptoms of psychological distress among cancer patients in Southeast Asian countries
| Author, year (country) | Number of patients (N) | Age (range, median) | Marital status/gender | Cancer type/stage N (%) | Treatment method/status | Severity of illness/diagnostic instrument | Study design | Anxiety/depression prevalence (%) |
|---|---|---|---|---|---|---|---|---|
| Aamir et al., 2012 (Malaysia) | 288 | (20–85, 54) |
S = 35 M = 253/F = 111 M = 177 |
NR/I II = (2.7) III = (97.2) |
Hormone therapy/ongoing | Moderate/HADS | CS | 48.6/30 |
| Beck et al., 2016 (Singapore) | 315 | (27–92, 59) |
S = 72 M = 243/F = 31 M = 22 |
VC/NR | Chemotherapy/NR | Mild to moderate/HADS | CS | 88/38.32 |
| Chan et al., 2015 (Malaysia) | 467 | (18–93, 56) |
S = 103 M = 364/F = 348 M = 119 |
0 = 28 (6.0) I = 57 (12.2) II = 82 (17.6) III = 77 (16.5) IV = 213 (45.6) Recurrent = 10 (2.1) |
Radiotherapy chemoradiotherapy/NR | NR/HADS | CS | 12/SC |
| De Guzman, 2014 (Philippines) | 710 | (18–82, 42) |
S = 260 M = 398/F = 356 M = 302 |
NR/NR | NR/ongoing | Severe/HADS | CS | 52.4/41 |
| Gan et al., 2019 (Malaysia) | 319 | (18–92, 52) |
NR/F = 179 M = 140 |
VC/NR |
Mastectomy/ongoing, Completed |
Severe/DASS‐21 | CS | 33/38 |
| Hanprasertpong et al., 2017 (Thailand) | 699 | (20–70, 53) |
S = 142 M = 557/F |
Cervical/I = 223 II = 353 III = 114 IV = 9 |
No treatment/ongoing, Completed |
NR/GAD‐7, PHQ‐9 | CS | 21/SC |
| Islam, 2015 (Malaysia) | 1000 | (>18, NR) | NR/F |
Breast/I II III IV |
Chemotherapy/ongoing, Completed |
Moderate/HADS | Longitudinal | SC/SC |
| Kim et al., 2017 (SEA) | 5249 | (18–100, NR) |
S = 1202 M = 4047/F = 3631 M = 1618 |
I = 437 II = 1190 III = 984 IV = 561 |
Chemotherapy/ongoing | Severe/HADS | CS | 37/15 |
| Lee et al., 2015 (Singapore) | 300 | (>20, 56) |
S = 104 M = 195/F = 168 M = 130 |
VC/NR | Surgery/NR | NR/HADS | CS | SC/NR |
| Manalo & Ngelangel, 2015 (Philippines) | 535 | (20–>80, 52) |
S = 138 M = 397/F = 278 M = 257 |
VC/I = 33 (6.17) II = 120 (22.43) III = 195 (36.45) IV = 187 (34.95) |
Chemotherapy/completed | NR/EQ‐5D‐3L | CS | 38/57.5 |
| Mei Hsien et al., 2012 (Malaysia) | 500 | NR | NR/NR | VC/NR |
Surgery MRM/ongoing |
Normal/ECOG, HADS | Longitudinal | SC/11.3 |
| Akhtari‐Zavare et al., 2018 (Malaysia) | 2120 | (>18, 54) |
S = 660 M = 1450/F = 1203 M = 917 |
VC/I = 208 II = 323 III = 785 IV = 804 |
Chemotherapy/ongoing | Severe/NR | CS | SC/NR |
| Nuraini et al., 2018 (Indonesia) | 308 | (35–59, NR) |
S = 40 M = 268/F |
Breast/II= III = 139 IV |
Surgery/ongoing, Completed |
Moderate/DAQ | CS | 40/NR |
| Peltzer et al., 2016 (Cambodia) | 4799 | (18–101, 52) |
NR/F = 1131 M = 1611 |
VC/NR | Others/ongoing | NR/CES‐D | CS | 47.8/45.9 |
| Que et al., 2013 (Philippines) | 250 | (>18, 53) |
S = 16 M = 38/F = 32 M = 21 |
VC/NR | Chemotherapy/completed, ongoing | NR/PHQ‐8 | CS | NR/22 |
| Setyowibowo et al., 2018 (Indonesia) | 471 | (>18, 43) | NR/F | Breast/NR | Radiotherapy/ongoing | NR/HADS | CS | 7/22 |
| Shian Ming Tan et al., 2014 (Singapore) | 315 | (>18, 58.3) |
S = 72 M = 243/F = 283 M = 132 |
NR/I = 16 (5.1) II = 1(5.7) III = 32(10.2) IV = 17 (53.2) |
Chemotherapy/ongoing | Severe/MINI | CS | 7.8/NR |
| Subramaniam et al., 2018 (Malaysia) | 1490 | (>18, 52) |
NR, F = 928 M = 562 |
Breast/I‐II = 325 (28.9) III‐IV = 448 (39.9) Hematologic tumour = 350 (31.2) |
NR/ongoing | Severe/DASS‐21 | CS | 84/18.9 |
| Thiagarajan et al., 2016 (Malaysia) | 303 | (>18, 53) |
F = 228 M = 75 |
VC/I = 23 (7.60) II = 70 (23.1) III = 83 (27.4) IV = 127 (41.9) |
TCM/ongoing | Moderate severe/HADS | CS | SC/38 |
| Thinh et al., 2018 (SEA) | 462 | (18–80, 55) |
NR/F = 248 M = 214 |
Breast, lung/0 = 4 (0.9) I = 11 (2.4) II = 32 (6.9) III = 79 (17.1) IV = 311 (67.3) |
No treatment/NR | Moderate/RSCL | CS | 56.2/15.4 |
| Truong et al., 2019 (Vietnam) | 510 | (>18, 59) |
S = 48 M = 462/F = 157 M = 353 |
NR/I = 170 II = 208 III = 109 IV = 23 |
Chemotherapy/ongoing | NR/DASS‐21 | CS | 43/27.4 |
| Vidthya et al., 2019 (Malaysia) | 953 | (<45–>60, 51) |
S = 590 M = 363/F = 569 M = 384 |
VC/NR | NR/ongoing | Moderate to severe/HADS | CS | 22.3/65.5 |
| Yen et al., 2016 (Vietnam) | 695 | (>18, 56) |
S = F = 333 M = 362 |
VC/I = (22) II = (42) III = (27) IV = (9) |
NR/ongoing | Moderate to severe/DASS‐21 | CS | NR/SC |
Abbreviations: NR = not reported; VC = Various cancers; BDI = Beck Depression Inventory; EQ‐5D‐3L = Euro Qol five‐dimensions–3‐level scale; MINI = Mini International Neuropsychiatric Interview; DAQ = Death Anxiety Questionnaire; RSCL = Rotterdam Symptom Checklist; CES‐D = Center for Epidemiologic Studies Depression Scale; ECOG = Eastern Cooperative Oncology Group criteria for psychological distress; GAD‐7 = Seven‐item Generalised Anxiety Disorder Scale; PHQ‐9 = Nine‐item Patient Health Questionnaire; CES‐D = Center for Epidemiological Studies‐Depression; PHQ‐8 = Eight‐item Patient Health Questionnaire; HADS = Hospital Anxiety and Depression Scale; DASS‐21 = 21‐item Depression, Anxiety and Stress Scale; CS=Cross‐sectional; SC = Significant correlation.
Included studies were published in nine countries of the SEA region from 2010 to 2021, and majority of them were published in the years 2018 (n = 5), 2015 (N = 4), and 2016 (n = 4). The total number of participants in the studies reviewed was 23,081 cancer patients. The age range of the participants was 18 to 101 years. Most studies (n = 21) included women diagnosed with breast cancer. According to Table 1, the prevalence of anxiety was higher than depression when examined separately. The severity of illness reported was moderate to severe.
Table 1 shows that approximately one‐third of the studies were conducted in Malaysia (n = 8), followed by Singapore (n = 3), Indonesia (n = 2), Thailand (n = 1), Philippines (n = 3), Vietnam (n = 2), Cambodia, Myanmar and Vietnam (n = 2), and multiple SEA countries (n = 2). Studies on depression and anxiety were most frequently carried out using the Hospital Anxiety and Depression Scale (HADS) for screening (n = 10). Most of these studies were cross‐sectional (n = 21). The most common treatment was chemotherapy (n = 8), followed by radiotherapy (n = 3).
The quality of life and mental health factors that were most consistently associated with depression and anxiety included sociodemographic variables. For instance, being older aged, being female, having a low income, and having low education were correlated with higher psychological distress.
A total of 23 studies, using 16 assessment tools, reported the prevalence of anxiety and depression among cancer patients. Overall, the prevalence of anxiety (ranging from 7% to 88%) was wider than that of depression (ranging from 3% to 65.5%) among patients with different types of cancer and living in various countries in the SEA region. The most commonly used screening instruments to assess psychological distress were the Hospital Anxiety and Depression Scale (HADS; Zigmond & Snaith, 1983; n = 11), followed by the Depression, Anxiety and Stress Scale‐21 items (DASS‐21; Lovibond & Lovibond, 1995; n = 4). Other assessment instruments were only used in one study included the Euro Qol five‐dimensions–3‐level scale (EQ‐5D‐3L; EuroQol Group, 1990), the nine‐item Patient Health Questionnaire (PHQ‐9; Kroenke et al., 2001), the eight‐item Patient Health Questionnaire (PHQ‐8; Kroenke & Spitzer, 2002), Mini International Neuropsychiatric Interview (MINI; Sheehan et al., 1998), Center for Epidemiologic Studies Depression Scale (CES‐D; Radloff, 1977), seven‐item Generalised Anxiety Disorder Scale (GAD‐7; Spitzer et al., 2006), Death Anxiety Questionnaire (DAQ; Conte et al., 1982), Eastern Cooperative Oncology Group criteria for psychological distress (ECQG; Oken et al., 1982), and Rotterdam Symptom Checklist (RSCl; De Haes et al., 1990).
4. DISCUSSION
In the present systematic review, the prevalence rates of symptoms of psychological distress among cancer patients (after 1 year of diagnosis) in Southeast Asia were reviewed. The prevalence of anxiety ranged from 7% to 88% and was greater than that of depression, which ranged from 3% to 65.5% among cancer patients. The findings of the present study were comparable with Shapiro et al.'s (2001) study, which assumed that anxiety was more common than in comparison depression among cancer patients in the context of psychological distress in the United States. The finding here was higher than cancer patients from studies in Turkey (İzci et al., 2018), Iran (Hashemi et al., 2020), Jordan (Naser et al., 2021), and Nigeria (Fatiregun et al., 2017), which found rates lower than 50%.
Psychological distress affects approximately 20–40% of individuals undergoing active cancer treatment (Kim et al., 2017). In a systematic review on the prevalence of symptoms of depression and anxiety among long‐term cancer survivors, Brandenbarg et al. (2019) reported that prevalence of depressive symptoms varied from 5.4% to 49.0% and anxiety the prevalence ranged from 3.4% to 43.0%. Several studies have reported that the prevalence of anxiety was higher than depression among examined populations (Beck et al., 2016; Ng et al., 2017; Thinh et al., 2018). Tan et al. (2014) reported that the prevalence of anxiety was 12 times higher than depression among cancer patients.
In a Spanish population, women with breast cancer undergoing different types of treatment were found to have higher levels of anxiety among patients at advanced stages compared to other stages (Cáceres et al., 2022). Thinh et al. (2018) reported that psychological distress was prevalent in 56.3% of participants in six South East Asian countries (Indonesia, Malaysia, Philippines, Singapore, Thailand, and Vietnam). Evidence from one study in Malaysia reported depression ranging from 22% to 50% among breast cancer patients (Ram et al., 2013). This finding is comparable to that of research among patients with cancer conducted in Ethiopia (58.4%; Berihun et al., 2017) and in Pakistan (61.6%; Dogar et al., 2009). According to Niedzwiedz et al. (2019), depression had a mean prevalence of approximately 13% globally among cancer patients and ranged between 4% to 49% when all evaluation techniques are included. In a study conducted in the United States, 34% patients with cervical cancer were reported to be depressed (Weitlauf et al., 2013). In another study, which was carried out in Korea, 3% patients were depressed (Park et al., 2017). Civilotti et al. (2020) argued that cancer patients reported to have both anxiety and depression disorder, which is similar to what has been reported in Italian samples.
Regarding the data in the present study, the highest prevalence rates of anxiety and depression were among cancer sufferers with breast cancer and lung cancer. Stage of cancer (Stage III and above), age (older‐aged), gender (female), and treatment (chemotherapy) were all significant indicators of psychological distress. Such findings have also been reported by other researchers from SEA region, although with smaller sample sizes (<250 participants) than the studies evaluated in the present review: Malaysia (Chen et al., 2019; Edib et al., 2016; Hassan et al., 2015; Isa et al., 2013; Leong Abdullah et al., 2015; Pahlevan Sharif, 2017; Priscilla et al., 2011; Saniah & Zainal, 2010; Wong & Lua, 2012; Yusof et al., 2016; Zainal et al., 2013), Philippines (Ledesma et al., 2011), Thailand (Cheung et al., 2015; Maneeton et al., 2014; Phuakpoolpol et al., 2018), Indonesia (Endarti et al., 2015; Haryani et al., 2018; Iskandarsyah et al., 2014; Vistad et al., 2011), Singapore (Chan et al., 2018; Cheng et al., 2014; Lim et al., 2014 and 2018; Liu et al., 2017; Mahendran et al., 2016; Peh et al., 2017; Poon et al., 2019; Teo et al., 2020), Cambodia and Myanmar (Pengpid & Peltzer, 2017), and Vietnam (Khue et al., 2019; Nguyen et al., 2018).
Some of these studies reported that anxiety was higher in comparison with depression among cancer patients in the context of psychological distress. In contrast to the results of the present study, a few studies in SEA countries have reported that depression is more common than anxiety among cancer patients (e.g., Gan et al., 2019; Mahendran et al., 2016; Manalo & Ngelangel, 2015; Vidthya et al., 2019). According to some previous research among cancer patients in SEA countries, there is a wide variation for the prevalence of depression and anxiety. A variety of factors is likely to influence the development of psychological issues among cancer patients (such as individual characteristics, psychological response to diagnosis, social and contextual factors, characteristics of cancer, prior psychological factors, and cancer treatments). However, these factors are not well understood (Nikbakhsh et al., 2014), and more research is required (Ng et al., 2017; Pasquini & Biondi, 2007). Moreover, in many studies, psychological distress is not the main outcome measure. Therefore, different research studies with various risk factors, screening instruments, sample size, and diagnostic criteria help explain the wide differences in reported prevalence of psychological distress (Chung et al., 2018).
The timing of elevated psychological risk is a significant factor that needs to be addressed. While many cancer patients with depression or anxiety consider themselves to have a mental health illness, most of them do not see themselves as needing psychiatric help (Pahlevan Sharif, 2017). Research has also found that most individuals with cancer do not seek support psychiatric help (51%), and one recent study reported that only 5.9% of cancer patients with a severe emotional distress had received psychiatric treatment (Alagizy et al., 2020). Research suggests that depression is more severe in the acute phase of cancer disease, but this may vary depending on cancer type and diagnosis (Gan et al., 2019).
It is evident that a more customised approach is necessary to help improve cancer patients' psychological health, so that physicians can classify patients most likely to develop such disorders so that they are properly managed to allow more relief and enhance quality of life (QoL) successfully. QoL is considered as the main goal of cancer treatment among patients (Isa et al., 2013). Treating depression and anxiety effectively is important in helping patients improve their QoL (Subramaniam et al., 2018). It has been shown that psychological distress among cancer patients (such as those with breast cancer or stomach cancer) and improving psychological distress within the first year significantly increases survival time (Subramaniam et al., 2018).
Moreover, the treatment of psychological distress appears to be different among patients with different types of cancer (Alagizy et al., 2020). However, as aforementioned, the estimated prevalence of psychological distress is likely dependent upon the way it is defined, and the country or region researched, focusing on a specific type or stage of cancer, metastatic potential and fear of side effects of therapy (Ng et al., 2017), due to factors such as the health and welfare system (Teo et al., 2020). However, the limitation of these studies was lack of clinical structured interview with cancer patients. If structured interviews had been carried out, a more definitive diagnosis could have been made (Nikbakhsh et al., 2014). It should also be highlighted that the psychological effect of cancer may not always be negative and many individuals will not experience problems relating to psychological distress (Niedzwiedz et al., 2019).
One of the strengths of the present study was the inclusion of studies with relatively large sample sizes (i.e., excluding studies with small samples below 250 participants) experiencing cancer from different countries in the SEA region. On the whole, among cancer patients, depression was a more significant psychological issue than anxiety (Hong & Tian, 2014). However, some studies have concluded that anxiety among patients with breast cancer is a more prevalent mental health disorder than depression (Liao et al., 2008).
The present review is useful in terms of the large number of cancer patients participating from the SEA studies (N = 23,081) examining psychological distress. Because these symptoms are highly prevalent, future studies need to explore anxiety and depressive symptoms because this would enable professionals to provide interventions that identify, treat, and reduce psychological symptoms. Consequently, health professionals should consider the psychological health as well as physical health among cancer patients.
There are several limitations in the present systematic review. First, only five of the 23 studies focused solely on cancer patients' psychological distress. The majority of studies did not specifically target psychological distress in cancer patients. Most of these studies were focused on how intervention treatments work (psychologically or medically). Second, the literature search was limited to studies published in the English language and there may have been other studies published in the languages of the countries under examination. Third, the study focused on studies that were published in peer‐reviewed journals; therefore, studies concerning psychological distress among cancer patients published in the grey literature were not included. Fourth, most of the published studies were carried out in Malaysia and Singapore (11 of the 23 studies), which may limit the generalizability of the findings. Fifth, most of these studies conducted in the SEA countries simply reported that cancer patients had anxiety and/or depression disorder, and there was little detail provided concerning symptoms or type of anxiety and depression. Sixth, another limitation might relate to participants being assessed during or after oncology treatment. Such assessment may produce variability of anxiety and depression levels among cancer patients in SEA countries. Finally, the studies only utilised psychometric instruments to assess psychological distress (rather than clinical interviews), which made interpreting the true level of psychological distress hard to determine. These results suggest that maybe regional differences account for variability in the prevalence of anxiety and depression among cancer patients.
5. CONCLUSION
Understanding the extent to which cancer patients exhibit psychological distress is important in preventing it or treating its consequences. Research in SEA countries is essential because the number of individuals living with cancer is growing in these countries. Psychological distress is considered to be common as cancer patients progress from diagnosis. Estimates of psychological distress among cancer patients in SEA countries vary depending on a variety of criteria, including the type and stage of cancer, occupation, patients' age, gender, and educational levels. The present study indicated the importance of both psychological aspects among cancer patients. Individuals living with cancer, of various types and stages, are of increasing interest in mental health research and treatment. Individuals with cancer often do not obtain psychological support or treatment for mental health issues. This is due to several factors, such as lack of insight (i.e., unawareness) of psychiatric symptoms, lack of evidence around effective treatments, and lack of support from healthcare professionals.
Consequently, there is an essential need for cancer patients to regularly monitor their psychological status during disease, and studies are needed to investigate the psychological problems among cancer patients in order to improve the understanding of these complex symptoms; on the other hand, after the diagnosis of clinically serious psychological distress, appropriate treatment interventions must be carried out to improve the quality of life of cancer patients. Early detection of anxiety and depression and management are important for cancer patients. Special attention should be paid to cancer patients with the aforementioned risk factors of psychological distress. Clinical recommendations for cancer management should incorporate the early identification and therapy of depression and anxiety, as well as their monitoring during treatment.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
Ostovar, S. , Modarresi Chahardehi, A. , Mohd Hashim, I. H. , Othman, A. , Kruk, J. , & Griffiths, M. D. (2022). Prevalence of psychological distress among cancer patients in Southeast Asian countries: A systematic review. European Journal of Cancer Care, 31(6), e13669. 10.1111/ecc.13669
DATA AVAILABILITY STATEMENT
This is a systematic literature review of previously published material. There are no primary data.
REFERENCES
- Aamir, S. , Chin, L. , & Beng, T. (2012). Correlation between anxiety, depression, family functioning and quality of life, in palliative care cancer patients. International Journal of Medicine and Medical Sciences, 2, 2167–2404. [Google Scholar]
- Action Study Group . (2017). Health‐related quality of life and psychological distress among cancer survivors in Southeast Asia: Results from a longitudinal study in eight low‐ and middle‐income countries. BMC Medicine, 15(1), 1–13. 10.1186/s12916-016-0768-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akhtari‐Zavare, M. , Mohd‐Sidik, S. , Periasamy, U. , Rampal, L. , Fadhilah, S. I. , & Mahmud, R. (2018). Determinants of quality of life among Malaysian cancer patients: A cross‐sectional study. Health and Quality of Life Outcomes, 16(1), 163–180. 10.1186/s12955-018-0989-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alagizy, H. A. , Soltan, M. R. , Soliman, S. S. , Hegazy, N. N. , & Gohar, S. F. (2020). Anxiety, depression and perceived stress among breast cancer patients: Single institute experience. Middle East Current Psychiatry, 27(1), 1–10. 10.1186/s43045-020-00036- [DOI] [Google Scholar]
- Almigbal, T. H. , Almutairi, K. M. , Fu, J. B. , Vinluan, J. M. , Alhelih, E. , Alonazi, W. B. , Batais, M. A. , Alodhayani, A. A. , & Mubaraki, M. A. (2019). Assessment of psychological distress among cancer patients undergoing radiotherapy in Saudi Arabia. Psychology Research and Behavior Management, 12, 691–700. 10.2147/PRBM.S209896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck, K. R. , Tan, S. M. , Lum, S. S. , Lim, L. E. , & Krishna, L. K. (2016). Validation of the emotion thermometers and hospital anxiety and depression scales in Singapore: Screening cancer patients for stress, anxiety and depression. Asia‐Pacific Journal of Clinical Oncology, 12(2), e241–e249. 10.1111/ajco.12180 [DOI] [PubMed] [Google Scholar]
- Berihun, F. , Haile, S. , & Abawa, M. (2017). Prevalence and correlates of anxiety and depression among cancer patients in the University of Gondar Comprehensive Specialized Hospital, Northwest Ethiopia. Archives of Depression and Anxiety, 3(2), 042–048. 10.17352/2455-5460.000022 [DOI] [Google Scholar]
- Brandenbarg, D. , Maass, S. W. M. C. , Geerse, O. P. , Stegmann, M. E. , Handberg, C. , Schroevers, M. J. , & Duijts, S. F. A. (2019). A systematic review on the prevalence of symptoms of depression, anxiety and distress in long‐term cancer survivors: Implications for primary care. European Journal of Cancer Care, 28(3), e13086. 10.1111/ecc.13086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cáceres, M. C. , Nadal‐Delgado, M. , López‐Jurado, C. , Pérez‐Civantos, D. , Guerrero‐Martín, J. , & Durán‐Gómez, N. (2022). Factors related to anxiety, depressive symptoms and quality of life in breast cancer. International Journal of Environmental Research and Public Health, 19(6), 3547. 10.3390/ijerph19063547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caruso, R. , Nanni, M. G. , Riba, M. , Sabato, S. , Mitchell, A. J. , Croce, E. , & Grassi, L. (2017). Depressive spectrum disorders in cancer: Prevalence, risk factors and screening for depression: A critical review. Acta Oncologica, 56, 146–155. 10.1080/0284186x.2016.1266090 [DOI] [PubMed] [Google Scholar]
- Chahardehi, A. M. , Mousavi, L. , & Hasan, S. (2017). The effectiveness of psychiatric therapy against Malaysian cancer patients with depressive disorders: A systematic review. Jurnal Psikologi Malaysia, 31(1), 57–66. PMID: https://spaj.ukm.my/ppppm/jpm/article/download/213/211 [Google Scholar]
- Chan, A. , Poon, E. , Goh, W. L. , Gan, Y. , Tan, C. J. , Yeo, K. , Chua, A. , Chee, M. , Law, Y. C. , Somasundaram, N. , & Kanesvaran, R. (2018). Assessment of psychological distress among Asian adolescents and young adults (AYA) cancer patients using the distress thermometer: A prospective, longitudinal study. Supportive Care in Cancer, 26(9), 3257–3266. 10.1007/s00520-018-4189-y [DOI] [PubMed] [Google Scholar]
- Chan, C. M. H. , Wan Ahmad, W. A. , Md Yusof, M. , Ho, G. F. , & Krupat, E. (2015). Prevalence and characteristics associated with default of treatment and follow‐up in patients with cancer. European Journal of Cancer Care,24(6), 938–944. 10.1111/ecc.12312 [DOI] [PubMed] [Google Scholar]
- Chen, Y. Y. , Ahmad, M. , & Ismail, F. B. (2019). Illness acceptance as mediator for cancer‐related complaints and psychological distresses among Malaysian cancer patients. Future Oncology, 15(15), 1759–1770. 10.2217/fon-2018-0686 [DOI] [PubMed] [Google Scholar]
- Cheng, K. K. F. , Darshini Devi, R. , Wong, W. H. , & Koh, C. (2014). Perceived symptoms and the supportive care needs of breast cancer survivors six months to five years post‐treatment period. European Journal of Oncology Nursing, 18(1), 3–9. 10.1016/j.ejon.2013.10.005 [DOI] [PubMed] [Google Scholar]
- Cheung, Y. , Lam, W. W. , Ip, J. J.‐K. , Cheuk, D. K. , Cheng, F. W. , Yang, J. Y. , Yau, J. P. , Ho, K. K. , Li, C. , Li, R. C. , Yuen, H. , Ling, A. S. , Li, V. W. , & Chan, G. C. (2015). Myocardial iron load and fibrosis in long term survivors of childhood leukemia. Pediatric Blood & Cancer,62(4), 698–703. 10.1002/pbc.25369 [DOI] [PubMed] [Google Scholar]
- Chung, J. , Ju, G. , Jeong, J. , Jeong, Y. , Moon, K. C. , Kwon, J. , Lee, K. H. , Kim, S. T. , & Han, H. S. (2018). Prevalence of and factors associated with anxiety and depression in Korean patients with newly diagnosed advanced gastrointestinal cancer. Korean Journal of Internal Medicine, 33(3), 585–594. 10.3904/kjim.2016.108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Civilotti, C. , Acquadro Maran, D. , Santagata, F. , Varetto, A. , & Stanizzo, M. R. (2020). The use of the Distress Thermometer and the Hospital Anxiety and Depression Scale for screening of anxiety and depression in Italian women newly diagnosed with breast cancer. Support Care Cancer, 28, 4997–5004. 10.1007/s00520-020-05343-x [DOI] [PubMed] [Google Scholar]
- Conte, H. R. , Weiner, M. B. , & Plutchik, R. (1982). Measuring death anxiety: Conceptual, psychometric, and factor‐analytic aspects. Journal of Personality and Social Psychology, 43(4), 775–785. 10.1037/0022-3514.43.4.775 [DOI] [PubMed] [Google Scholar]
- De Guzman, M. L. R. (2014). The validation of the Hospital Anxiety and Depression Scale (HADS‐P) among the medically‐ill Filipino patients in Philippine General Hospital. Acta Medica Philippina, 47(1), 53–43. [Google Scholar]
- De Haes, J. C. J. M. , Van Knippenberg, F. C. E. , & Neijt, J. P. (1990). Measuring psychological and physical distress in cancer patients: Structure and application of the Rotterdam Symptom Checklist. British Journal of Cancer, 62(6), 1034–1038. 10.1038/bjc.1990.434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dogar, I. A. , Azeem, M. W. , Kiran, M. , Hussain, I. , Mehmood, K. , & Hina, I. (2009). Depression and anxiety in cancer patients in outpatient department of a tertiary care hospital in Pakistan. Pakistan Journal of Medical Sciences, 25(5), 734–737. PMID: http://pjms.com.pk/issues/octdec109/article/article6.html [Google Scholar]
- Edib, Z. , Kumarasamy, V. , binti Abdullah, N. , Rizal, A. M. , & Al‐Dubai, S. A. R. (2016). Most prevalent unmet supportive care needs and quality of life of breast cancer patients in a tertiary hospital in Malaysia. Health and Quality of Life Outcomes, 14(1). 10.1186/s12955-016-0428-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Endarti, D. , Riewpaiboon, A. , Thavorncharoensap, M. , Praditsitthikorn, N. , Hutubessy, R. , & Kristina, S. (2015). Evaluation of health‐related quality of life among patients with cervical cancer in Indonesia. Asian Pacific Journal of Cancer Prevention, 16(1), 3345–3350. 10.7314/apjcp.2015.16.8.3345 [DOI] [PubMed] [Google Scholar]
- EuroQol Group . (1990). EuroQol—A new facility for the measurement of health‐related quality of life. Health Policy, 16(3), 199–208. 10.1016/0168-8510(90)90421-9 [DOI] [PubMed] [Google Scholar]
- Fatiregun, O. A. , Olagunju, A. T. , Erinfolami, A. R. , Arogunmati, O. A. , Fatiregun, O. A. , & Adeyemi, J. D. (2017). Relationship between anxiety disorders and domains of health related quality of life among Nigerians with breast cancer. Breast, 31, 150–156. 10.1016/j.breast.2016.11.010 [DOI] [PubMed] [Google Scholar]
- Gallicchio, L. , Gadalla, S. M. , Murphy, J. D. , & Simonds, N. I. (2018). The effect of cancer treatments on telomere length: A systematic review of the literature. JNCI: Journal of the National Cancer Institute, 110(10), 1048–1058. 10.1093/jnci/djy189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gan, G. G. , Ng, D. L. C. , Chin, F. M. , Aziz, T. A. H. T. , & Teh, A. K. (2019). Anxiety and depression in patients with haematological neoplasms in Malaysia. Medical Journal of Malaysia, 74(3), 191–197. PMID: http://www.e-mjm.org/2019/v74n3/anxiety-and-depression.pdf [PubMed] [Google Scholar]
- Giedre, B. , & Kamile, P. (2019). Interventions for reducing suicide risk in cancer patients: A literature review. Europe's Journal of Psychology, 15(3), 637. 10.5964/ejop.v15i3.1741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanprasertpong, J. , Geater, A. , Jiamset, I. , Padungkul, L. , Hirunkajonpan, P. , & Songhong, N. (2017). Fear of cancer recurrence and its predictors among cervical cancer survivors. Journal of Gynecologic Oncology, 28(6), e72. 10.3802/jgo.2017.28.e72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haryani, H. , Hsu, Y. Y. , Warsini, S. , & Wang, S. T. (2018). Measuring the symptom experience of patients with cancer in Indonesia: Cross‐cultural adaptation and validation of the memorial symptom assessment scale‐Indonesian version. Journal of Pain and Symptom Management, 56(6), 920–927. 10.1016/j.jpainsymman.2018.08.016 [DOI] [PubMed] [Google Scholar]
- Hashemi, S. M. , Rafiemanesh, H. , Aghamohammadi, T. , Badakhsh, M. , Amirshahi, M. , Sari, M. , Behnamfar, N. , & Roudini, K. (2020). Prevalence of anxiety among breast cancer patients: A systematic review and meta‐analysis. Breast Cancer, 27(2), 166–178. 10.1007/s12282-019-01031-9 [DOI] [PubMed] [Google Scholar]
- Hassan, M. R. , Shah, S. A. , Ghazi, H. F. , Mujar, N. M. M. , Samsuri, M. F. , & Baharom, N. (2015). Anxiety and depression among breast cancer patients in an urban setting in Malaysia. Asian Pacific Journal of Cancer Prevention, 16(9), 4031–4035. 10.7314/apjcp.2015.16.9.4031 [DOI] [PubMed] [Google Scholar]
- Hong, J. S. , & Tian, J. (2014). Prevalence of anxiety and depression and their risk factors in Chinese cancer patients. Support Care Cancer, 22(2), 453–459. 10.1007/s00520-013-1997-y [DOI] [PubMed] [Google Scholar]
- Isa, M. R. , Moy, F. M. , Abdul Razack, A. H. , Zainuddin, Z. M. , & Zainal, N. Z. (2013). Impact of applied progressive deep muscle relaxation training on the level of depression, anxiety and stress among prostate cancer patients: A quasi‐experimental study. Asian Pacific Journal of Cancer Prevention, 14(4), 2237–2242. 10.7314/apjcp.2013.14.4.2237 [DOI] [PubMed] [Google Scholar]
- Iskandarsyah, A. , de Klerk, C. , Suardi, D. R. , Sadarjoen, S. S. , & Passchier, J. (2014). Consulting a traditional healer and negative illness perceptions are associated with non‐adherence to treatment in Indonesian women with breast cancer. Psycho‐Oncology, 23(10), 1118–1124. 10.1002/pon.3534 [DOI] [PubMed] [Google Scholar]
- Islam, T. , Bhoo‐Pathy, N. , Su, T. T. , Majid, H. A. , Nahar, A. M. , Ng, C. G. , Dahlui, M. , Hussain, S. , Cantwell, M. , Murray, L. , & Taib, N. A. (2015). The Malaysian Breast Cancer Survivorship Cohort (MyBCC): A study protocol.BMJ Open, 5(10), e008643. 10.1136/bmjopen-2015-008643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- İzci, F. , Sarsanov, D. , Erdogan, Z. İ. , İlgün, A. S. , Çelebi, E. , Alço, G. , Kocaman, N. , Ordu, Ç. , Öztürk, A. , Duymaz, T. , Pilavcı, K. N. , Elbüken, F. , Ağaçayak, F. , Aktepe, F. , Ünveren, G. , Özdem, G. , Eralp, Y. , & Özmen, V. (2018). Impact of personality traits, anxiety, depression and hopelessness levels on quality of life in the patients with breast cancer. European Journal of Breast Health, 14(2), 105–111. 10.5152/ejbh.2018.3724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khue, P. M. , Thom, V. T. , Minh, D. Q. , Quang, L. M. , & Hoa, N. L. (2019). Depression and anxiety as key factors associated with quality of life among lung cancer patients in Hai Phong, Vietnam. Frontiers in Psychiatry, 10, 352. 10.3389/fpsyt.2019.00352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim, G. M. , Kim, S. J. , Song, S. K. , Kim, H. R. , Kang, B. D. , Noh, S. H. , Chung, H. C. , Kim, K. R. , & Rha, S. Y. (2017). Prevalence and prognostic implications of psychological distress in patients with gastric cancer. BMC Cancer, 17, 283–291. 10.1186/s12885-017-3260-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimman, M. L. , Jan, S. , Peters, S. A. E. , Yip, C. H. , Ngelangel, C. A. , Bhoo‐Pathy, N. , Woodward, M. , Arounlangsy, P. , Aung, S. , Balete, S. L. , Bhoo‐Pathy, N. , Bounxouei, B. , Bui, D. , Datukan, J. , Gorospe, A. E. , Yip, C. H. , Htun, Y. Y. , Khopaibul, P. , Khuayjarernpanishk, T. , … Executive Comm . (2017). Health‐related quality of life and psychological distress among cancer survivors in Southeast Asia: Results from a longitudinal study in eight low‐ and middle‐income countries. BMC Medicine, 15, 10–32. 10.1002/pon.4787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krebber, A. M. H. , Buffart, L. M. , Kleijn, G. , Riepma, I. C. , Bree, R. , Leemans, C. R. , Becker, A. , Brug, J. , Straten, A. , Cuijpers, P. , & Verdonck‐de Leeuw, I. M. (2013). Prevalence of depression in cancer patients: A meta‐analysis of diagnostic interviews and self‐report instruments. Psycho‐Oncology, 23(2), 121–130. 10.1002/pon.3409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke, K. , & Spitzer, R. L. (2002). The PHQ‐9: A new depression diagnostic and severity measure. Psychiatric Annals, 32, 509–515. 10.3928/0048-5713-20020901-06 [DOI] [Google Scholar]
- Kroenke, K. , Spitzer, R. L. , & Williams, J. B. (2001). The PHQ‐9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613. 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kruk, J. , Aboul‐Enein, B. H. , Bernstein, J. , & Gronostaj, M. (2019). Psychological stress and cellular aging in cancer: A meta‐analysis. Oxidative Medicine and Cellular Longevity, 2019, 1270397. 10.1155/2019/1270397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ledesma, D. , Takahashi, M. , & Kai, I. (2011). Interest in a group psychotherapy program among Philippine breast cancer patients and its associated factors. Psycho‐Oncology, 20(9), 1007–1012. 10.1002/pon.1804 [DOI] [PubMed] [Google Scholar]
- Lee, G. L. , Fan, G. K. T. , & Chan, S. W. C. (2015). Validation of Chinese and English versions of the Holistic Well‐being Scale in patients with cancer. Supportive Care in Cancer, 23(12), 3563–3571. 10.1007/s00520-015-2736-3 [DOI] [PubMed] [Google Scholar]
- Leong Abdullah, M. F. I. , Nik Jaafar, N. R. , Zakaria, H. , Rajandram, R. K. , Mahadevan, R. , Mohamad Yunus, M. R. , & Shah, S. A. (2015). Posttraumatic growth, depression and anxiety in head and neck cancer patients: Examining their patterns and correlations in a prospective study. Psycho‐Oncology, 24(8), 894–900. 10.1002/pon.3740 [DOI] [PubMed] [Google Scholar]
- Liao, M. N. , Chen, M. F. , Chen, S. C. , & Chen, P. L. (2008). Uncertainty and anxiety during the diagnostic period for women with suspected breast cancer. Cancer Nursing, 31(4), 274–283. 10.1097/01.NCC.0000305744.64452.fe [DOI] [PubMed] [Google Scholar]
- Lim, H. A. , Mahendran, R. , Chua, J. , Peh, C.‐X. , Lim, S.‐E. , & Kua, E.‐H. (2014). The distress thermometer as an ultra‐short screening tool: A first validation study for mixed‐cancer outpatients in Singapore. Comprehensive Psychiatry, 55(4), 1055–1062. 10.1016/j.comppsych.2014.01.008 [DOI] [PubMed] [Google Scholar]
- Liu, J. , Peh, C. X. , & Mahendran, R. (2017). Body image and emotional distress in newly diagnosed cancer patients: The mediating role of dysfunctional attitudes and rumination. Body Image, 20, 58–64. 10.1016/j.bodyim.2016.11.001 [DOI] [PubMed] [Google Scholar]
- Lovibond, P. F. , & Lovibond, S. H. (1995). The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research and Therapy, 33, 335–343. 10.1016/0005-7967(94)00075-u [DOI] [PubMed] [Google Scholar]
- Mahendran, R. , Lim, H. A. , Tan, J. Y. , Kua, E. H. , & Griva, K. (2016). The prevalence and predictors of subsyndromal anxiety and depression in adult Asian cancer patients across the first year of diagnosis. Asia‐Pacific Journal of Clinical Oncology, 12(4), 476–489. 10.1111/ajco.12562 [DOI] [PubMed] [Google Scholar]
- Manalo, M. O. U. , & Ngelangel, C. A. (2015). Correlation between demographic, socio‐economic, and cancer‐specific factors with quality of life scores among newly‐diagnosed cancer patients of the Medical Oncology Clinics of the Philippine General Hospital Cancer Institute. Acta Medica Philippina, 49(2), 32–41. PMID: 10.47895/amp.v49i2.3022. [DOI] [Google Scholar]
- Maneeton, B. , Maneeton, N. , Reungyos, J. , Intaprasert, S. , Leelarphat, S. , & Thongprasert, S. (2014). Prevalence and relationship between major depressive disorder and lung cancer: A cross‐sectional study. Oncotargets and Therapy, 7, 815–821. 10.2147/OTT.S60000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mei Hsien, C. C. , Wan Azman, W. A. , Md Yusof, M. , Ho, G. F. , & Krupat, E. (2012). Discrepancy in patient‐rated and oncologist‐rated performance status on depression and anxiety in cancer: A prospective study protocol. BMJ Open, 2, e001799. 10.1136/bmjopen-2012-001799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mercadante, S. , Adile, C. , Ferrera, P. , Cortegiani, A. , & Casuccio, A. (2019). Symptom hyper‐expression in advanced cancer patients with anxiety and depression admitted to an acute supportive/palliative care unit. Support Care Cancer, 27, 3081–3088. 10.1007/s00520-018-4624-0 [DOI] [PubMed] [Google Scholar]
- Moher, D. , Liberati, A. , Tetzlaff, J. , & Altman, D. G. (2009). Preferred reporting items for systematic reviews and meta‐analyses: The PRISMA statement. BMJ, 339, b2535–b2535. 10.1136/bmj.b2535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagai, H. , & Kim, Y. H. (2017). Cancer prevention from the perspective of global cancer burden patterns. Journal of Thoracic Disease, 9(3), 448–451. PMID: 10.21037/jtd.2017.02.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naser, A. Y. , Hameed, A. N. , Mustafa, N. , Alwafi, H. , Dahmash, E. Z. , Alyami, H. S. , & Khalil, H. (2021). Depression and anxiety in patients with cancer: A cross‐sectional study. Frontiers in Psychology, 12, 585534. 10.3389/fpsyg.2021.585534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng, G. C. , Mohamed, S. , Sulaiman, A. H. , & Zainal, N. Z. (2017). Anxiety and depression in cancer patients: The association with religiosity and religious coping. Journal of Religion and Health, 56(2), 575–590. 10.1007/s10943-016-0267-y [DOI] [PubMed] [Google Scholar]
- Nguyen, L. T. , Alexander, K. , & Yates, P. (2018). Psychoeducational intervention for symptom management of fatigue, pain, and sleep disturbance cluster among cancer patients: A pilot quasi‐experimental study. Journal of Pain and Symptom Management, 55(6), 1459–1472. 10.1016/j.jpainsymman.2018.02.019 [DOI] [PubMed] [Google Scholar]
- Niedzwiedz, C. L. , Knifton, L. , Robb, K. A. , Katikireddi, S. V. , & Smith, D. J. (2019). Depression and anxiety among people living with and beyond cancer: a growing clinical and research priority. BMC Cancer, 19(1). 10.1186/s12885-019-6181-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nikbakhsh, N. , Moudi, S. , Abbasian, S. , & Khafri, S. (2014). Prevalence of depression and anxiety among cancer patients. Caspian Journal of Internal Medicine, 5(3), 167–170. [PMC free article] [PubMed] [Google Scholar]
- Nuraini, T. , Andrijono, A. , Irawaty, D. , Umar, J. , & Gayatri, D. (2018). Spirituality‐focused palliative care to improve Indonesian breast cancer patient comfort. Indian Journal of Palliative Care, 24(2), 196–201. 10.4103/IJPC.IJPC_5_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oken, M. M. , Creech, R. H. , Tormey, D. C. , Horton, J. , Davis, T. E. , McFadden, E. T. , & Carbone, P. P. (1982). Toxicity and response criteria of the Eastern Cooperative Oncology Group. American Journal of Clinical Oncology, 5(6), 649–655. [PubMed] [Google Scholar]
- Osborn, R. L. , Demoncada, A. C. , & Feuerstein, M. (2006). Psychosocial interventions for depression, anxiety, and quality of life in cancer survivors: Meta‐analyses. The International Journal of Psychiatry in Medicine, 36(1), 13–34. 10.2190/EUFN-RV1K-Y3TR-FK0L [DOI] [PubMed] [Google Scholar]
- Pahlevan Sharif, S. (2017). Locus of control, quality of life, anxiety, and depression among Malaysian breast cancer patients: The mediating role of uncertainty. European Journal of Oncology Nursing, 27, 28–35. 10.1016/j.ejon.2017.01.005 [DOI] [PubMed] [Google Scholar]
- Park, B. , Youn, S. , Yi, K. K. , Lee, S. Y. , Lee, J. S. , & Chung, S. (2017). The prevalence of depression among patients with the top ten most common cancers in South Korea. Psychiatry Investigation, 14(5), 618–625. 10.4306/pi.2017.14.5.618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pasquini, M. , & Biondi, M. (2007). Depression in cancer patients: A critical review. Clinical Practice and Epidemiology in Mental Health, 3, 2. 10.1186/1745-0179-3-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peh, C. X. , Liu, J. , Bishop, G. D. , Chan, H. Y. , Chua, S. M. , Kua, E. H. , & Mahendran, R. (2017). Emotion regulation and emotional distress: The mediating role of hope on reappraisal and anxiety/depression in newly diagnosed cancer patients. Psycho‐Oncology, 26(8), 1191–1197. 10.1002/pon.4297 [DOI] [PubMed] [Google Scholar]
- Peltzer, K. , Pengpid, S. , Puckpinyo, A. , Yi, S. , & Anh, L. V. (2016). The utilization of traditional, complementary and alternative medicine for non‐communicable diseases and mental disorders in health care patients in Cambodia, Thailand and Vietnam. BMC Complementary and Alternative Medicine, 16, 92–92. 10.1186/s12906-016-1078-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pengpid, S. , & Peltzer, K. (2017). Multimorbidity in chronic conditions: Public primary care patients in four greater Mekong countries. International Journal of Environmental Research and Public Health, 14(9), 1019. 10.3390/ijerph14091019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phuakpoolpol, S. , Suwannarurk, K. , Jaisin, K. , Punyashthira, A. , Pattaraarchachai, J. , & Bhamarapravatana, K. (2018). Anxiety and depression in Thai women with abnormal cervical cytology who attended colposcopic unit in Thammasat University Hospital. Asian Pacific Journal of Cancer Prevention, 19(10), 2985–2989. PMID: 10.22034/APJCP.2018.19.10.2985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poon, S. H. , Wang, F. Q. , Goh, J. , Chan, Y. H. , & Lim, L. (2019). Mental health literacy in cancer outpatients in Singapore. East Asian Archives of Psychiatry, 29(3), 91–94. 10.12809/eaap1813 [DOI] [PubMed] [Google Scholar]
- Priscilla, D. , Hamidin, A. , Azhar, M. Z. , Noorjan, K. O. , Salmiah, M. S. , & Bahariah, K. (2011). Quality of life among patients with hematological cancer in a Malaysian hospital. Medical Journal of Malaysia, 66(2), 117–120. PMID: http://www.e-mjm.org/2011/v66n2/Hematological_Cancer.pdf [PubMed] [Google Scholar]
- Que, J. C. , Sy Ortin, T. T. , Anderson, K. O. , Gonzalez‐Suarez, C. B. , Feeley, T. W. , & Reyes‐Gibby, C. C. (2013). Depressive symptoms among cancer patients in a Philippine tertiary hospital: Prevalence, factors, and influence on health‐related quality of life. Journal of Palliative Medicine, 16(10), 1280–1284. 10.1089/jpm.2013.0022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff, L. S. (1977). The CES‐D Scale: A self‐report depression scale for research in the general population. Applied Psychological Measurement, 1, 385–401. 10.1177/014662167700100306 [DOI] [Google Scholar]
- Ram, S. , Narayanasamy, R. , & Barua, A. (2013). Effectiveness of group psycho‐education on well‐being and depression among breast cancer survivors of Melaka, Malaysia. Indian Journal of Palliative Care, 19, 34–39. 10.4103/0973-1075.110234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saniah, A. , & Zainal, N. (2010). Anxiety, depression and coping strategies in breast cancer patients on chemotherapy. Malaysian Journal of Psychiatry, 19(2), 1–5. [Google Scholar]
- Sankaranarayanan, R. , Ramadas, K. , & Qiao, Y. L. (2014). Managing the changing burden of cancer in Asia. BMC Medicine, 12, 3–15. 10.1186/1741-7015-12-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Setyowibowo, H. , Purba, F. D. , Hunfeld, J. A. M. , Iskandarsyah, A. , Sadarjoen, S. S. , Passchier, J. , & Sijbrandij, M. (2018). Quality of life and health status of Indonesian women with breast cancer symptoms before the definitive diagnosis: A comparison with Indonesian women in general. PLoS ONE, 13(7), e0200966. 10.1371/journal.pone.0200966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shapiro, S. L. , Lopez, A. M. , Schwartz, G. E. , Bootzin, R. , Figueredo, A. J. , Braden, C. J. , & Kurker, S. F. (2001). Quality of life and breast cancer: Relationship to psychosocial variables. Journal of Clinical Psychology, 57(4), 501–519. 10.1002/jclp.1026 [DOI] [PubMed] [Google Scholar]
- Sheehan, D. V. , Lecrubier, Y. , Sheehan, K. H. , Amorim, P. , Janavs, J. , Weiller, E. , Hergueta, T. , Baker, R. , & Dunbar, G. C. (1998). The Mini‐International Neuropsychiatric Interview (M.I.N.I): The development and validation of a structured diagnostic psychiatric interview for DSM‐IV and ICD‐10. Journal of Clinical Psychiatry, 59(Suppl 20), 22–33. PMID: https://www.psychiatrist.com/read-pdf/11980/ [PubMed] [Google Scholar]
- Shunmugasundaram, C. , Rutherford, C. , Butow, P. N. , Sundaresan, P. , & Dhillon, H. M. (2020). What are the optimal measures to identify anxiety and depression in people diagnosed with head and neck cancer (HNC): A systematic review. Journal of Patient‐Reported Outcomes, 4, 26. 10.1186/s41687-020-00189-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer, R. L. , Kroenke, K. , Williams, J. B. , & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD‐7. Archives of Internal Medicine, 166(10), 1092–1097. PMID: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Subramaniam, S. , Kong, Y. C. , Chinna, K. , Kimman, M. , Ho, Y. Z. , Saat, N. , Malik, R. A. , Taib, N. A. , Abdullah, M. M. , Lim, G. C.‐C. , Tamin, N.‐S. I. , Woo, Y.‐L. , Chang, K.‐M. , Goh, P.‐P. , Yip, C.‐H. , & Bhoo‐Pathy, N. (2018). Health‐related quality of life and psychological distress among cancer survivors in a middle‐income country. Psycho‐Oncology, 27(9), 2172–2179. 10.1002/pon.4787 [DOI] [PubMed] [Google Scholar]
- Tan, S. M. , Beck, K. R. , Li, H. , Lim, E. C. L. , & Krishna, L. K. R. (2014). Depression and anxiety in cancer patients in a Tertiary General Hospital in Singapore. Asian Journal of Psychiatry, 8, 33–37. 10.1016/j.ajp.2013.10.002 [DOI] [PubMed] [Google Scholar]
- Teo, I. , Vilardaga, J. P. , Tan, Y. P. , Winger, J. , Cheung, Y. B. , Yang, G. M. , Finkelstein, E. A. , Shelby, R. A. , Kamal, A. H. , Kimmick, G. , & Somers, T. J. (2020). A feasible and acceptable multicultural psychosocial intervention targeting symptom management in the context of advanced breast cancer. Psycho‐Oncology, 29(2), 389–397. 10.1002/pon.5275 [DOI] [PubMed] [Google Scholar]
- Thiagarajan, M. , Chan, C. , Fuang, H. G. , Beng, T. S. , Atiliyana, M. , & Yahaya, N. (2016). Symptom prevalence and related distress in cancer patients undergoing chemotherapy. Asian Pacific Journal of Cancer Prevention, 17(1), 171–176. 10.7314/apjcp.2016.17.1.171 [DOI] [PubMed] [Google Scholar]
- Thinh, D. H. Q. , Sriraj, W. , Mansor, M. , Tan, K. H. , Irawan, C. , Kurnianda, J. , Nguyen, Y. P. , Ong‐Cornel, A. , Hadjiat, Y. , Moon, H. , & Javier, F. O. (2018). Analgesic prescription patterns and pain outcomes in Southeast Asia: Findings from the analgesic treatment of cancer pain in Southeast Asia study. Journal of Global Oncology, 2018(4), 1–10. 10.1200/JGO.17.00055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Truong, D. V. , Bui, Q. T. T. , Nguyen, D. T. , & Moore, J. (2019). Anxiety among inpatients with cancer: Findings from a hospital‐based cross‐sectional study in Vietnam. Cancer Control, 26(1), 1073274819864641. 10.1177/1073274819864641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vidthya, S. , Sherina, M. S. , Rampal, L. , Fadhilah, S. I. , & Ummavathy, P. (2019). Self‐esteem among cancer patients receiving chemotherapy in selected. Medical Journal of Malaysia, 74(5), 405–412. PMID: http://www.e-mjm.org/2019/v74n5/cancer-patients-self-esteem.pdf [PubMed] [Google Scholar]
- Vistad, I. , Cvancarova, M. , Kristensen, G. B. , & Fosså, S. D. (2011). A study of chronic pelvic pain after radiotherapy in survivors of locally advanced cervical cancer. Journal of Cancer Survivorship, 5(2), 208–216. 10.1007/s11764-011-0172-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vorn, R. , Touch, S. , & Ryu, E. (2019). Depression and health‐related quality of life among Cambodian patients with cancer. International Journal of Health Planning and Management, 34(4), e1747–e1759. 10.1002/hpm.2888 [DOI] [PubMed] [Google Scholar]
- Weitlauf, J. C. , Jones, S. , Xu, X. , Finney, J. W. , Moos, R. H. , Sawaya, G. F. , & Frayne, S. M. (2013). Receipt of cervical cancer screening in female veterans: Impact of posttraumatic stress disorder and depression. Women's Health Issues, 23(3), e153–e159. 10.1016/j.whi.2013.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong, S. , & Lua, P. (2012). Effects of dark chocolate consumption on anxiety, depressive symptoms and health‐related quality of life status among cancer patients. Health and the Environment Journal, 3(1), 28–35. [Google Scholar]
- Yang, Y.‐L. , Liu, L. , Wang, Y. , Wu, H. , Yang, X.‐S. , Wang, J.‐N. , & Wang, L. (2013). The prevalence of depression and anxiety among Chinese adults with cancer: A systematic review and meta‐analysis. BMC Cancer, 13, 393–393. 10.1186/1471-2407-13-393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yen, N. T. K. , Weiss, B. , & Trung, L. T. (2016). Caseness rates and risk factors for depression among Vietnamese cancer patients. Asian Journal of Psychiatry, 23, 95–98. 10.1016/j.ajp.2016.07.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yusof, S. , Zakaria, F. , Hashim, N. , & Dasiman, R. (2016). Depressive symptoms among cancer patients undergoing chemotherapy. Procedia ‐ Social and Behavioral Sciences, 234, 185–192. 10.1016/j.sbspro.2016.10.233 [DOI] [Google Scholar]
- Zainal, N. Z. , Shuib, N. , Bustam, A. Z. , Sabki, Z. A. , & Guan, N. C. (2013). Reliability and validity of the Malay Version of the Breast‐ Impact of Treatment Scale (MVBITS) in breast cancer women undergoing chemotherapy. Asian Pacific Journal of Cancer Prevention, 14(1), 463–468. 10.7314/apjcp.2013.14.1.463 [DOI] [PubMed] [Google Scholar]
- Zigmond, A. S. , & Snaith, R. P. (1983). The Hospital Anxiety and Depression Scale. Acta Psychiatrica Scandinavica, 67, 361–370. 10.1111/j.1600-0447.1983.tb09716.x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
This is a systematic literature review of previously published material. There are no primary data.


