Abstract
Background
Although a great number of teleconsultation services have been developed during the COVID-19 pandemic, studies assessing usability and health care provider satisfaction are still incipient.
Objective
This study aimed to describe the development, implementation, and expansion of a synchronous teleconsultation service targeting patients with symptoms of COVID-19 in Brazil, as well as to assess its usability and health care professionals’ satisfaction.
Methods
This mixed methods study was developed in 5 phases: (1) the identification of components, technical and functional requirements, and system architecture; (2) system and user interface development and validation; (3) pilot-testing in the city of Divinópolis; (4) expansion in the cities of Divinópolis, Teófilo Otoni, and Belo Horizonte for Universidade Federal de Minas Gerais faculty and students; and (5) usability and satisfaction assessment, using Likert-scale and open-ended questions.
Results
During pilot development, problems contacting users were solved by introducing standardized SMS text messages, which were sent to users to obtain their feedback and keep track of them. Until April 2022, the expanded system served 31,966 patients in 146,158 teleconsultations. Teleconsultations were initiated through chatbot in 27.7% (40,486/146,158) of cases. Teleconsultation efficiency per city was 93.7% (13,317/14,212) in Teófilo Otoni, 92.4% (11,747/12,713) in Divinópolis, and 98.8% (4981/5041) in Belo Horizonte (university campus), thus avoiding in-person assistance for a great majority of patients. In total, 50 (83%) out of 60 health care professionals assessed the system’s usability as satisfactory, despite a few system instability problems.
Conclusions
The system provided updated information about COVID-19 and enabled remote care for thousands of patients, which evidenced the critical role of telemedicine in expanding emergency services capacity during the pandemic. The dynamic nature of the current pandemic required fast planning, implementation, development, and updates in the system. Usability and satisfaction assessment was key to identifying areas for improvement. The experience reported here is expected to inform telemedicine strategies to be implemented in a postpandemic scenario.
Keywords: COVID-19, telemonitoring, remote consultation, telemedicine, primary health care, delivery of health care, telehealth, text message, mobile health, public health, remote care, digital health, usability
Introduction
The COVID-19 pandemic has brought dramatic transformative changes in economies, societies, and health care, with an unprecedented challenge to public health worldwide [1]. The need to avoid patient crowds in health services and offer alternative ways for patient assistance while preserving physical distancing and isolation, as well as the prioritization of emergency departments and intensive care units, have proven to be important drivers for the urgent need and quick adoption of telemedicine.
Telehealth services were growing exponentially prior to COVID-19 [2]. However, it was during the pandemic that they received a major boost. Governments from different countries were urged to promote telehealth and make provisions to address some of the previously encountered barriers, and they quickly updated law restrictions and reimbursement policies [3]. In Brazil, telehealth has been consolidated over the years, but it was only after the spread of COVID-19 that a legal and regulatory framework emerged, authorizing remote medical and other professional health consultations. The Telehealth Network of the State of Minas Gerais (TNMG) in Brazil—one of the largest public telehealth services in Latin America [4,5]—was quick to implement telemedicine services for the care of patients with suspected novel coronavirus infection soon after the first patient was diagnosed with COVID-19 in the country.
Although a great number of teleconsultation services have been developed, studies assessing usability and satisfaction from the health care provider’s perspective are still incipient. Concerns have been raised regarding challenges posed by diagnosing without an actual physical examination and the negative impact on patient-provider rapport [6]. In the aftermath of COVID-19, when telehealth services are expected to remain in use and health care provider satisfaction is a key feature for telehealth sustainability, usability assessment is particularly relevant as a source to be tapped for lessons to be learned.
Our aim was to assess the feasibility of the development, implementation, and expansion of a synchronous teleconsultation service for care provided to patients with symptoms of COVID-19, as well as to perform assessments of usability and health care professionals’ satisfaction.
Methods
Study Design
This mixed methods study was developed in 5 phases (Figure 1), following guidance from the Medical Council Framework [7]:
Figure 1.
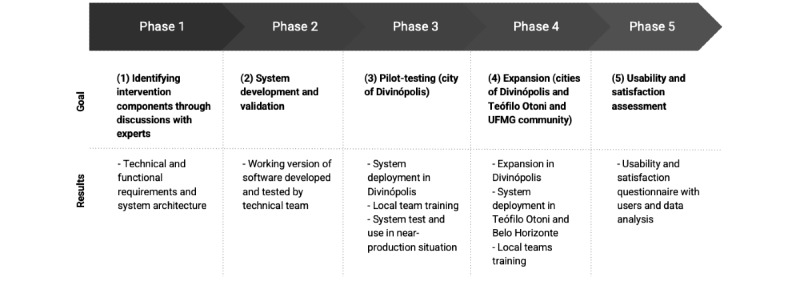
Project phases. UFMG: Universidade Federal de Minas Gerais.
Identifying intervention components through discussions with experts;
System development and validation;
Pilot-testing;
Expansion; and
Usability and satisfaction assessment.
Each phase is briefly explained in the following subsections.
Identifying Intervention Components Through Discussions With Experts
To identify components in the intervention, information was extracted from guidance issued by the Brazilian Ministry of Health [8,9] and evidence available at the onset of the pandemic, as well as discussions among an interdisciplinary team of IT specialists, clinicians with long-term expertise in telemedicine [4,5], infectious diseases specialists, and nurses.
The workflow suggested by the Brazilian Ministry of Health was adapted to improve the assistance flow, offer agility for the teams and data security, and reduce the burden of patients who need in-person consultations at primary care centers. The municipality where the system was planned to run initially—Divinópolis—had a telephone service dedicated for the general population to answer queries related to COVID-19 and for primary care practitioners, medical university professors, and undergraduate medical students working in a monitoring program. All available resources were used to design an integrated teleassistance flow, which assisted patients from their initial doubt through to clinical assistance and monitoring, at 4 levels: level 1, performed by local health care professionals (nursing technicians, physiotherapists, nutritionists, and psychologists); level 2, performed by nursing staff; level 3, performed by medical staff; and level 4, telemonitoring that was performed by students under medical supervision.
Although this teleassistance flow was not fully integrated into the local emergency departments, upon concluding teleconsultations, when face-to-face assessments were deemed necessary, the patients could be referred to face-to-face medical consultations with a specific clinical report.
An internal medicine specialist, a nurse, a doctor with long-term experience in telemedicine, and an IT specialist identified the main components in the intervention to map the main needs, steps in the process of care, and specificities of each screen and functionality in the system. These health care professionals worked alongside the IT specialist to discuss and propose changes and improvements to the system throughout the iterative development cycle adopted. Unfortunately, due to the necessary urgency of the actions—the platform was offered for use just 2 months after the start of its development—it was not possible to involve patients in the development of the self-assessment tools.
A management model based on the Plan-Do-Check-Act cycle and a monitoring system based on key performance indicators were developed. The nurse and the doctor with long-term experience in telemedicine defined the indicators to be monitored (Table S1 in Multimedia Appendix 1).
System Development and Validation
The system was developed and validated following an agile software methodology. Its backend was built using the Java programming language (version 1.8) with the Spring Boot and Hibernate frameworks, whereas the system’s user interface was built using the Angular user interface framework.
The system, named TeleCOVID-MG, started being developed in March 2020. Throughout March and April, the team of analysts met weekly with the clinical team to assess new requests that arose. Meanwhile, the development team delivered weekly packages that were internally tested and, on weekends, were validated and approved by professionals from the clinical team. Thus, in May 2020, the first version was released into a production environment. From then on, fortnightly sprints were adopted, generating deliveries for testing and approval.
The software runs on a web environment, which allows the full recording of activities. It is composed of an application server, which runs the main application backend and serves the frontend to the users’ client browsers, and an SQL relational database (Postgres). The frontend has 2 main interfaces: 1 for teleconsultation, which is used by the health care professionals, and another for monitoring the service queue, which is a dashboard used by the team of moderators, who identify the need for additional health care professionals in the shift to reduce the response time. A chatbot, developed using the BLiP platform (Take), was aimed to be a first point of contact for patients with the telehealth service [10,11]. It assisted in screening the severity of respiratory and flu-like symptoms and queuing patients for teleconsultation based on warning-sign severity [10,11]. There is a module for importing data from the chatbot into the database and a module for sending messages to patients (Figure 2).
Figure 2.
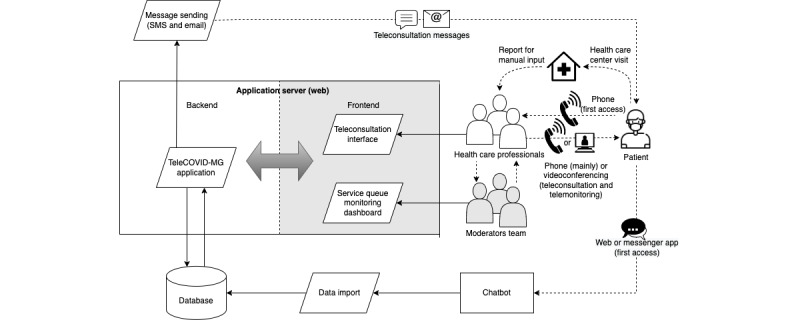
System architecture overview.
Teleconsultation and Telemonitoring Services
TeleCOVID-MG has 3 main goals: (1) assessing and managing patients with respiratory or flu-like symptoms, (2) monitoring patients with COVID-19, and (3) providing the general population with updated information about COVID-19. The system enables performing consultations either with or without videoconferencing, issuing medical prescriptions and reports, as well as issuing orders for diagnostic COVID-19 tests (Figure 3) by nurses and physicians from the TeleCOVID-MG teleconsultation team, following the Ministry of Health and local clinical protocols. All these documents generated during the teleconsultation can be easily downloaded as PDF files by the patients. The software also enables the generation of the compulsory report of COVID-19 cases, in compliance with requirements by the Brazilian Health Ministry, as well as teleconsultations scheduling, patient referral to telemonitoring services, or face-to-face consultations at other levels of care (Figure 4 and “TeleCOVID-MG service workflow” in Multimedia Appendix 1 [6,9,12]).
Figure 3.
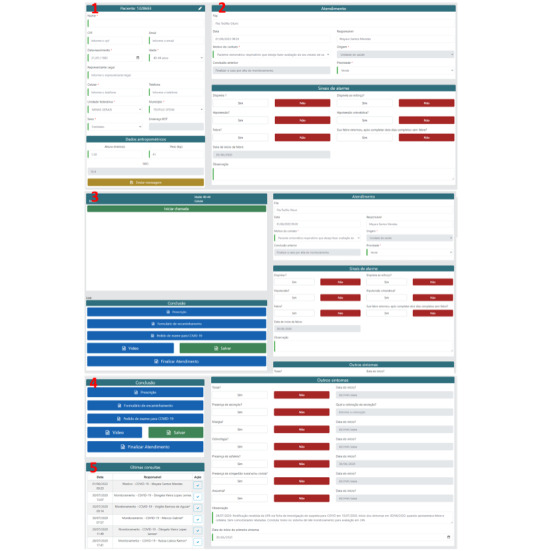
Screenshots of TeleCOVID-MG. User registration form: (1) patient personal information tab; (2) patient clinical condition tab recording warning signs; and (3) video call tab; (4) form tab (for prescriptions, reports, and test orders); and (5) record of past teleconsultations.
Figure 4.
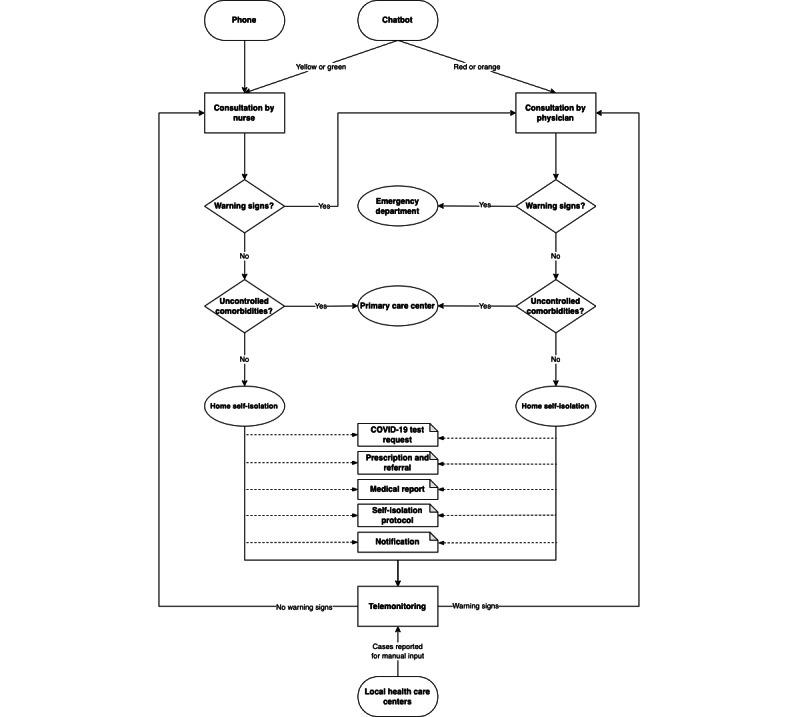
TeleCOVID-MG service workflow.
Pilot-testing
The pilot study was carried out in Divinópolis, a 213,016-inhabitant city with a human development index of 0.76, from May 18 to 28, 2020 [12]. The team responsible for teleconsultations and telemonitoring in Divinópolis comprised physicians, nurses, and students from Universidade Federal de São João del-Rei. An instruction manual was prepared, and participating health care professionals received web-based clinical training, based on the best available scientific evidence at that time. They were also trained to use the system before starting the activities.
Expansion
The project was expanded to the Teófilo Otoni, a 140,937-inhabitant city with a human development index of 0.70 [11], and subsequently to faculty and students at Universidade Federal de Minas Gerais (UFMG), a federal university where the coordination center of the TNMG is located. It has over 45,000 students and 7400 faculty members.
The team responsible for the teleconsultations comprised physicians and nurses from the TNMG, and, in the case of Teófilo Otoni, also included nurses from that city. The team responsible for telemonitoring comprised medical students supervised by medical professors and nurses. All of them received technical training to operate the system and theoretical training, as aforementioned. Weekly meetings were held with local coordinators to discuss indicators, identify deviations from planned targets, and plan and implement corrective actions.
Once patients entered the system, after the initial teleconsultation, a follow-up plan that involved monitoring or new consultations was defined based on the assessment of their situation. Teleconsultation efficiency was calculated as the number of patients who were provided with consultation and did not need to be referred to face-to-face consultations divided by the total number of patients who were provided with consultation.
For reporting expansion results, all records of patients who were provided with consultation at the 3 locations from May 2020 to April 2022 were eligible.
Usability and Satisfaction Assessment
A questionnaire was developed to assess health care professionals’ satisfaction and the usability of the system, as they were the primary immediate users. It included eight 5-point Likert-scale questions that focused on aspects regarding user satisfaction and usability and open-ended questions that focused on the perceived strengths and weaknesses of the system, features to be improved, and comments about their experience with the system. All health care professionals who worked in the service and used the TeleCOVID-MG system were eligible (n=60). A thematic analysis was conducted for the open-ended questions.
Ethics Approval
Ethical approval was obtained from the UFMG Research Ethics Committee (CAAE: 35953620.9.0000.5149). Informed consent was obtained from study participants.
Results
Through the study, the system served 31,966 patients, totaling 146,158 teleconsultations covering the first and subsequent consultations performed for each patient, since the same patient could be assessed more than once by nurses, physicians, and the telemonitoring team. The accumulated number of teleconsultations and patients assisted by location and service efficiency are displayed in Figure 5. Other indicators that were monitored weekly and monthly are shown in Table S2 in Multimedia Appendix 1. The real-time analysis of these data allowed system and service workflow adjustments as necessary.
Figure 5.
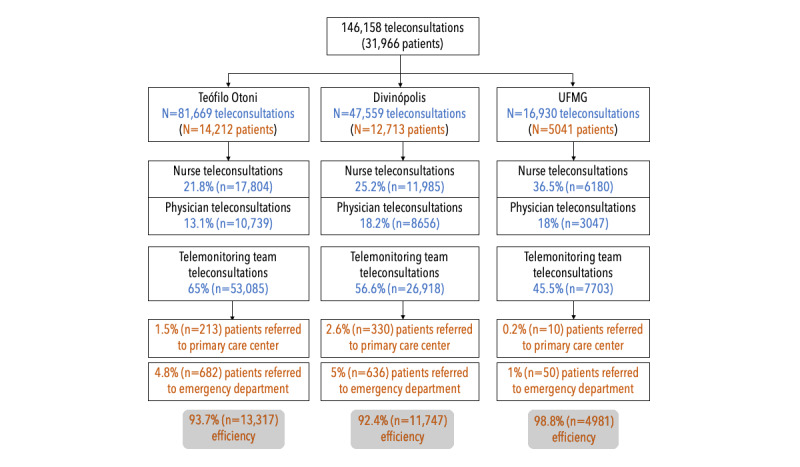
Percentage of teleconsultation distribution efficiency among the 3 cities in our study. UFMG: Universidade Federal de Minas Gerais.
As shown in Figure 2, both the chatbot and telephone number were the gateway to the program. The telephone was primarily used, and teleconsultations were initiated through the chatbot in 27.7% (40,486/146,158) of cases. Additionally, the main method used to carry out the teleconsultations was via telephone call, with videoconferencing showing a very low usage rate (only 192 [0.13%] videoconferencing teleconsultations in total). When carried out, videoconferencing was performed via smartphone, using patients’ preferred software that was previously installed on their device. The main challenge faced during the expansion phase in Teófilo Otoni was the difficulty in reaching patients, even by telephone call, which may be due to the instability of the local telephone network and the fact that part of the population lives in rural areas and lack familiarity with telecommunication tools. Due to these same logistical and cultural reasons, the use of videoconferencing and other technologies such as chatbot was even more challenging.
Another difficulty was aligning the clinical guideline developed for remote care with the practice carried out in the city. To face this challenge, training meetings were held with local health teams, and several seminars addressing theoretical issues related to the management of patients with COVID-19 were carried out. The number of assessments initiated via chatbot was low in Teófilo Otoni, which may be due to the low socioeconomic level of the population and their limited digital literacy when dealing with new technologies. However, the number of calls via chatbot was extensive among the university community at UFMG, which is consistent with college users who have the digital skills needed to deal with chatbots.
Of the 60 health care professionals who used the system when the assessment was performed, 50 (83%) answered the questionnaire (age: median 35, IQR 31-40 years; women: n=43, 86%). Of these professionals, 42% (n=21) were physicians and 54% (27) were nurses (Table S3 in Multimedia Appendix 1).
Overall, the system was evaluated as satisfactory (Table 1 and Figure S1 in Multimedia Appendix 1). The only exception was for the statement “The system is stable, and no errors occur during use,” which had a median score of 4 (IQR 2-4). We believe this score reflects technical infrastructure problems and the short time taken to put the system into production, which prevented debugging. With regard to the open-ended questions, 35 participants answered at least one question, 44 commented on the system’s strengths, 41 mentioned weaknesses, 37 made suggestions, and 16 commented on their experience with the system (see “Responses to the open-ended questions” in Multimedia Appendix 1).
Table 1.
Usability and satisfaction assessment (n=50). Likert-scale responses range from 1 to 5: 1=totally disagree, 2=partially disagree, 3=indifferent, 4=partially agree, and 5=totally agree.
| Item | Median (IQR) | Mean |
| System screens can be easily understood. | 5 (5-5) | 4.9 |
| The system allows recording all relevant data on patient consultation. | 5 (4-5) | 4.64 |
| By following the screen prompts, I was able to provide patient care with quality. | 5 (5-5) | 4.86 |
| The system fields are easy to fill out. | 5 (5-5) | 4.84 |
| The system is intuitive to use. | 5 (4-5) | 4.42 |
| I believe that the system can be useful in clinical practice, for the care of patients with suspected COVID-19. | 5 (5-5) | 4.96 |
| The system is stable, and no errors occur during use. | 4 (2-4) | 3.3 |
| I was satisfied with the use of the system. | 5 (4-5) | 4.64 |
Discussion
Principal Findings
Our study presents a novel telehealth tool from its conceptualization through its development, validation, implementation, and rapid expansion. When planning the teleconsultation system, 2 major barriers to the implementation were identified. First, the lack of local experience with the functionalities needed for synchronous teleconsultation. Despite the TNMG’s long experience with other telehealth tools, it was only after the spread of COVID-19 that a legal and regulatory framework emerged, authorizing remote medical and other professional health consultations in Brazil [13]. Second, as COVID-19 was a new disease, information about it was still scarce. Due to the successive emergence of new evidence, the system’s initial matrix had to be progressively changed over time. Thus, a continuous development and validation process was of utmost importance to guarantee that the system was kept in line with updated evidence.
The use of the TeleCOVID-MG system made it possible to clarify queries about the novel coronavirus and deliver remote care to thousands of patients, thus reducing the circulation of individuals with respiratory or flu-like symptoms, minimizing the burden on health services, and increasing patient access to care in places with scarce health resources; together, these possibilities evidence the critical role of telemedicine in expanding emergency services capacity during a pandemic. The system also contributed to the updating of several health care professionals on the main topics related to COVID-19.
Doubts and concerns about the use of teleconsultations, especially teleconsultations performed by telephone calls (which was the most frequently used medium in our context), were already present even before the pandemic. Impossibility to perform the physical examination, compromised physician-patient relationship, difficulty in performing a global assessment of the patient that only focus on acute complaints, and uncertainty in the quality of information are some of the challenges reported in studies that evaluated the perception of health care professionals about the use of teleconsultations [14-17]. With the pandemic, providers and patients were forced into a new normal that included communicating with each other through video and audio [18], and studies have demonstrated that the COVID-19 pandemic affected the way physicians use and perceive telehealth and increased telehealth activities use both in type and frequency [19] despite the aforementioned limitations. Through their experience during the pandemic, physicians became more convinced of the efficacy, efficiency, and safety of telemedicine, as well as their ability to meet their patients’ needs remotely. Although there was a shift in physicians’ activities and perceptions, concerns about the effectiveness of remote consults and the lack of adequate legal frameworks remain [17]. Negative aspects related to teleconsultations reported in the literature include concerns about the absence of visual clues, inability to perform a physical examination, and thus the lack of comprehensive assessments [17,18].
Health care professionals with no experience in telehealth needed to quickly develop skills in web-based rapport building [19]; therefore, assessing the usability and provider satisfaction of each implemented system is of utmost importance. The analysis of usability and satisfaction of health care professionals with our system showed that most of them agreed that the system is intuitive and easy to understand and operate; allows them to provide care with quality; and is useful for evaluating patients with COVID-19. The social function of the systems was highlighted for the way it guaranteed the expansion of access to health care and decreased the burden in local health care. In addition, the systems allow interdisciplinarity and the development of a continuum of care until the patient’s complete recovery.
Our results are in line with other studies [4,20-22], which showed high levels of satisfaction with telemedicine implemented during the pandemic. A recent integrative review has found 5 studies assessing provider satisfaction, all of them in outpatient clinics for specialized care during the pandemic for other conditions, and satisfaction ranged from 78% to 93% among the studies [23]. The evidence presented here suggests the feasibility of incorporating synchronous teleconsultations for the management of other health conditions. For this application to be possible, we emphasize the need for constant improvements in the systems and the importance of integrating remote care with face-to-face care.
Bearing in mind that the uptake and sustainability of telehealth interventions are the ultimate goals when implementing them, we highlight the following as takeaway lessons:
Previous expertise is important for the successful development of a new system, particularly when implementation within a short amount of time is needed;
The engagement of end users, in this case health care professionals, in system design and development is of utmost importance to ensure the fulfillment of user needs and usability;
Health care professionals’ perception of telehealth was positively impacted by the pandemic setting, as shown by their reported high levels of satisfaction; and
In remote or resource-constrained locations with unstable internet, having an alternative way to perform teleconsultation (such as using telephone calls) is of utmost importance.
The main challenges faced in the usability of the TeleCOVID-MG system were related to the instability of the local telephone network, the need to align the clinical guideline developed for remote care with the practices carried out in the municipalities, and continually adjusting the system to the new scientific evidence and practices arising through the course of the pandemic.
As limitations of the TeleCOVID-MG system, we should remark that the lack of integration with data from face-to-face assistance were reported. The need for an interoperable health care system became blatantly evident worldwide during the COVID-19 pandemic to avoid duplicating work and improve decision-making. Although not designed for interoperability, the system architecture allowed the on-demand generation of customized queries and reports.
With great growth in the use of teleconsultations as a way to fight the pandemic, several entities have published guidelines to help health care professionals in remote patient care [24]. Furthermore, studies have been published focusing on evaluating the use of this telehealth tool and proposing adjustments for expansion in the postpandemic period [18,20].
Limitations
With regards to the efficiency assessment, although the team performed a thorough assessment of referrals and nonreferrals, there might be cases in which patients did seek face-to-face care despite not having been recommended to do so. Patient and caregiver experience, as well as patient digital literacy and satisfaction with the TeleCOVID-MG service, has not been formally addressed yet. We opted to restrict our analysis to health care professionals due to 2 main reasons: (1) they had to adapt their work routine very quickly due to the pandemic; and (2) they were the primary users of the teleconsultation system, as they had to fill out the patients’ electronic record and issue medical prescriptions, reports, and orders for diagnostic COVID-19 tests through the system. Despite the lack of formal assessment with patients, the assisting health care professionals reported spontaneous comments from patients on how they felt welcomed and listened to in a better way than in face-to-face consultation, as they had time to report everything they wanted, without the time constraints present in face-to-face consultations. This finding supports the idea that it is indeed possible to provide humanized care in telehealth. We are currently conducting a formal patient satisfaction analysis for TeleCOVID-MG.
Due to the pandemic scenario and the goal of including as many health care professionals who were using the system as possible in our usability and satisfaction assessment, our analysis was centered mainly on our questionnaire. A more thorough analysis about satisfaction drivers using a more in-depth qualitative study could provide additional lessons.
Conclusion
This paper described the rapid development, implementation, and expansion of the TeleCOVID-MG system, as well as the results of our usability and satisfaction assessment with health care professionals. The system made it possible to answer queries about COVID-19 and provide remote care to thousands of patients, showing the critical role of telemedicine in expanding emergency services capacity during a pandemic. The dynamic nature of the current pandemic required regular updates in the system and frequent monitoring of the implemented actions. The experience reported here is expected to inform telemedicine strategies to be implemented in a postpandemic scenario, not only to deal with eventual new pandemics but also, and most importantly, explore the affordances of telemedicine to enhance public policies aimed at promoting health care prevention, treatment, and education. Furthermore, our experience illustrates the local and cultural challenges and specificities that need to be dealt with in the development of such systems, which indicate that even if there were “off-the-shelf” solutions available, they might not be able to address local community needs.
Acknowledgments
This study is supported in part by the Brazilian research agencies Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES, grant 88887.516155 / 2020-00) and Fundação de Amparo à Pesquisa do Estado de Minas Gerais (FAPEMIG; APQ-00208-20). ALPR was supported in part by the Brazilian research agencies Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq; grant 310790/2021-2 and IATS 465518/2014-1) and FAPEMIG (Programa Pesquisador Mineiro PPM-00428-17 and Rede de Teleassistência de Minas Gerais RED-00081-16). MS Marcolino was supported in part by CNPq (grant 310561/2021-3). AR and MS Marcolino are members of the National Institute of Science and Technology for Health Technology. AP has a CNPq research grant (313103/2021-6) and a FAPEMIG grant (APQ-01.461-14). TCF has a CAPES postdoctoral grant (88887.508597/2020-00). BAC was supported by a Pró-Reitoria de Pesquisa (PRPq)/Universidade Federal de Minas Gerais (UFMG)/Secretaria de Educação Superior (SESu)/Ministério da Educação (MEC) grant (23072.211119/2020-10). MCR has a CAPES Master’s scholarship (88887.516155 / 2020-00).
Abbreviations
- TNMG
Telehealth Network of the State of Minas Gerais
- UFMG
Universidade Federal de Minas Gerais
Supplementary file.
Data Availability
Data is available upon reasonable request.
Footnotes
Authors' Contributions: ALPR, MS Marcolino, MBMA, MCP, MS Mendes, and CRAO were responsible for the research protocol and coordinated the study. LBR, MS Marcolino, MS Mendes, and MBMA participated in the TeleCOVID-MG development and testing. MBMA, MS Mendes, LBR, MCP, GMR, CSC, and INB participated in the TeleCOVID-MG implementation. RP and BAC were responsible for the coordination of the research team for the application of the questionnaire. MS Marcolino, AP, TCF, RP, BAC, CRAO, CSC, MS Mendes, ZSNR, and MCR performed the data analysis and drafted the manuscript. All authors reviewed and edited the manuscript. MCR organized the manuscript references. All authors approved the final version.
Conflicts of Interest: None declared.
References
- 1.Ibn-Mohammed T, Mustapha KB, Godsell J, Adamu Z, Babatunde KA, Akintade DD, Acquaye A, Fujii H, Ndiaye MN, Yamoah FA, Koh SCL. A critical analysis of the impacts of COVID-19 on the global economy and ecosystems and opportunities for circular economy strategies. Resour Conserv Recycl. 2021 Jan;164:105169. doi: 10.1016/j.resconrec.2020.105169. https://europepmc.org/abstract/MED/32982059 .S0921-3449(20)30486-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barbosa W, Zhou K, Waddell E, Myers T, Dorsey ER. Improving access to care: telemedicine across medical domains. Annu Rev Public Health. 2021 Apr 01;42(1):463–481. doi: 10.1146/annurev-publhealth-090519-093711. https://www.annualreviews.org/doi/abs/10.1146/annurev-publhealth-090519-093711?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed . [DOI] [PubMed] [Google Scholar]
- 3.Fisk M, Livingstone A, Pit SW. Telehealth in the context of COVID-19: changing perspectives in Australia, the United Kingdom, and the United States. J Med Internet Res. 2020 Jun 09;22(6):e19264. doi: 10.2196/19264. https://www.jmir.org/2020/6/e19264/ v22i6e19264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marcolino MS, Alkmim MB, Santos TADQ, Riberio AL. The Telehealth Network of Minas Gerais: a large-scale Brazilian public telehealth service improving access to specialised health care. Policy in Focus. 2016;13(1):59–61. [Google Scholar]
- 5.Alkmim MB, Figueira Renato Minelli, Marcolino Milena Soriano, Cardoso Clareci Silva, Pena de Abreu M, Cunha Lemuel Rodrigues, da Cunha Daniel Ferreira, Antunes Andre Pires, Resende Adélson Geraldo de A, Resende Elmiro Santos, Ribeiro Antonio Luiz Pinho. Improving patient access to specialized health care: the Telehealth Network of Minas Gerais, Brazil. Bull World Health Organ. 2012 May 01;90(5):373–8. doi: 10.2471/BLT.11.099408. https://europepmc.org/abstract/MED/22589571 .BLT.11.099408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Garcia-Huidobro D, Rivera S, Valderrama Chang S, Bravo P, Capurro D. System-wide accelerated implementation of telemedicine in response to COVID-19: mixed methods evaluation. J Med Internet Res. 2020 Oct 06;22(10):e22146. doi: 10.2196/22146. https://www.jmir.org/2020/10/e22146/ v22i10e22146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Skivington K, Matthews L, Simpson SA, Craig P, Baird J, Blazeby JM, Boyd KA, Craig N, French DP, McIntosh E, Petticrew M, Rycroft-Malone J, White M, Moore L. A new framework for developing and evaluating complex interventions: update of Medical Research Council guidance. BMJ. 2021 Sep 30;374:n2061. doi: 10.1136/bmj.n2061. http://www.bmj.com/lookup/pmidlookup?view=long&pmid=34593508 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Protocolo de manejo clínico do coronavírus (COVID-19) na atenção primária à saùde. Coronavirus Clinical Management Protocol (COVID-19) in Primary Health Care. Article in Portuguese. Ministry of Health, Brazil. 2020. Apr, [2021-08-02]. https://saude.rs.gov.br/upload/arquivos/202004/14140606-4-ms-protocolomanejo-aps-ver07abril.pdf .
- 9.Ministry of Health. Minister's Office, Brazil Portaria nº 467, de 20 de março de 2020. Ordinance No. 467, of March 20, 2020. Article in Portuguese. Diário Oficial da União. 2020. Mar 20, [2021-08-02]. https://www.in.gov.br/en/web/dou/-/portaria-n -467-de-20-de-marco-de-2020-249312996 .
- 10.Cateb GF, Amaral S, Gonçalves SCL, Oliveira IJR, Prates RO, Chagas BA, Marcolino MS, Reis ZSN. Estudo piloto de validação de um chatbot de rastreamento, implementado para direcionar a teleassistência em COVID-19. SBCAS 2021: XXI Simpósio Brasileiro de Computação Aplicada à Saúde; June 15-18, 2021; Online event. 2021. Jun 15, pp. 97–102. [DOI] [Google Scholar]
- 11.Chagas BA, Ferreguetti K, Ferreira TC, Prates RO, Ribeiro LB, Pagano AS, Reis ZSN, Riberio AL, Marcolino MS. Chatbot as a telehealth intervention strategy in the COVID-19 pandemic: lessons learned from an action research approach. CLEI Electronic Journal. 2021 Dec 13;24(3):6. doi: 10.19153/cleiej.24.3.6. doi: 10.19153/cleiej.24.3.6. [DOI] [Google Scholar]
- 12.Brazilian Census 2010. Brazilian Institute of Geography and Statistics. 2010. [2021-08-02]. https://cidades.ibge.gov.br/brasil/mg/divinopolis/panorama .
- 13.Presidência da República (Brasil) Lei nº 989, de 15 de abril de 2020: dispõe sobre o uso da telemedicina durante a crise causada pelo coronavírus (SARS-CoV-2) Diário Oficial da União. 2020. Apr 15, [2020-12-19]. https://www.in.gov.br/en/web/dou/-/lei-n-13.989-de-15-de-abril-de-2020-252726328 .
- 14.Caetano R, Silva AB, Guedes ACCM, Paiva CCN, Ribeiro GDR, Santos DL, Silva RMD. Challenges and opportunities for telehealth during the COVID-19 pandemic: ideas on spaces and initiatives in the Brazilian context. Cad Saude Publica. 2020;36(5):e00088920. doi: 10.1590/0102-311x00088920. https://www.scielo.br/scielo.php?script=sci_arttext&pid=S0102-311X2020000503001&lng=en&nrm=iso&tlng=en .S0102-311X2020000503001 [DOI] [PubMed] [Google Scholar]
- 15.Derkx HP, Rethans JJE, Maiburg BH, Winkens RA, Muijtjens AM, van Rooij HG, Knottnerus JA. Quality of communication during telephone triage at Dutch out-of-hours centres. Patient Educ Couns. 2009 Feb;74(2):174–8. doi: 10.1016/j.pec.2008.08.002.S0738-3991(08)00406-0 [DOI] [PubMed] [Google Scholar]
- 16.McKinstry B, Hammersley V, Burton C, Pinnock H, Elton R, Dowell J, Sawdon N, Heaney D, Elwyn G, Sheikh A. The quality, safety and content of telephone and face-to-face consultations: a comparative study. Qual Saf Health Care. 2010 Aug 29;19(4):298–303. doi: 10.1136/qshc.2008.027763.qshc.2008.027763 [DOI] [PubMed] [Google Scholar]
- 17.Hjelm NM. Benefits and drawbacks of telemedicine. J Telemed Telecare. 2005 Jun 24;11(2):60–70. doi: 10.1258/1357633053499886. [DOI] [PubMed] [Google Scholar]
- 18.Hasani SA, Ghafri TA, Al Lawati H, Mohammed J, Al Mukhainai A, Al Ajmi F, Anwar H. The use of telephone consultation in primary health care during COVID-19 pandemic, Oman: perceptions from physicians. J Prim Care Community Health. 2020 Dec 14;11:2150132720976480. doi: 10.1177/2150132720976480. https://journals.sagepub.com/doi/abs/10.1177/2150132720976480?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mann DM, Chen J, Chunara Rumi, Testa Paul A, Nov Oded. COVID-19 transforms health care through telemedicine: evidence from the field. J Am Med Inform Assoc. 2020 Jul 01;27(7):1132–1135. doi: 10.1093/jamia/ocaa072. https://europepmc.org/abstract/MED/32324855 .5824298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Helou S, El Helou E, Abou-Khalil V, Wakim J, El Helou J, Daher A, El Hachem C. The effect of the COVID-19 pandemic on physicians' use and perception of telehealth: the case of Lebanon. Int J Environ Res Public Health. 2020 Jul 06;17(13):4866. doi: 10.3390/ijerph17134866. https://www.mdpi.com/resolver?pii=ijerph17134866 .ijerph17134866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Darr A, Senior A, Argyriou K, Limbrick J, Nie H, Kantczak A, Stephenson K, Parmar A, Grainger J. The impact of the coronavirus (COVID-19) pandemic on elective paediatric otolaryngology outpatient services - an analysis of virtual outpatient clinics in a tertiary referral centre using the modified paediatric otolaryngology telemedicine satisfaction survey (POTSS) Int J Pediatr Otorhinolaryngol. 2020 Nov;138:110383. doi: 10.1016/j.ijporl.2020.110383. https://europepmc.org/abstract/MED/33152974 .S0165-5876(20)30526-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dobrusin A, Hawa F, Gladshteyn M, Corsello P, Harlen K, Walsh CX, Alaparthi L, Weinstein M, Baig N, Sousa A, Gunaratnam NT. Gastroenterologists and patients report high satisfaction rates with telehealth services during the novel coronavirus 2019 pandemic. Clin Gastroenterol Hepatol. 2020 Oct;18(11):2393–2397.e2. doi: 10.1016/j.cgh.2020.07.014. https://europepmc.org/abstract/MED/32663521 .S1542-3565(20)30976-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Andrews E, Berghofer K, Long J, Prescott A, Caboral-Stevens M. Satisfaction with the use of telehealth during COVID-19: an integrative review. Int J Nurs Stud Adv. 2020 Nov;2:100008. doi: 10.1016/j.ijnsa.2020.100008. https://linkinghub.elsevier.com/retrieve/pii/S2666-142X(20)30007-2 .S2666-142X(20)30007-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Greenhalgh T, Koh GCH, Car J. COVID-19: a remote assessment in primary care. BMJ. 2020 Mar 25;368:m1182. doi: 10.1136/bmj.m1182. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary file.
Data Availability Statement
Data is available upon reasonable request.


