Abstract
Objective
Individuals diagnosed with low risk, localised prostate cancer (PCa) face a difficult decision between active surveillance (AS) and definitive treatment. We aimed to explore perceived influences on treatment decision‐making from the patient and partner's perspectives.
Methods
Patients (and partners) who met AS criteria and had chosen their treatment were recruited. Semi‐structured individual interviews were conducted via telephone to explore experiences of diagnosis, impact on patient lifestyle, experiences with physicians, treatment preferences/choice, treatment information understanding and needs, and overall decision‐making process. Interviews were audio recorded, transcribed verbatim, and analysed using Reflexive Thematic Analysis.
Results
Twenty‐four male patients (18 chose AS) and 12 female partners participated. Five themes relating to social‐ecological influences on treatment choice were identified: (1) partner support and direct influence on patient treatment choice, (2) patient and partner vicarious experiences may influence treatment decisions, (3) the influence of the patient's life circumstances, (4) disclosing to wider social networks: friends, family, and co‐workers, and (5) the importance of a good relationship and experience with physicians. Additionally, two themes were identified relating to information patients and partners received about the treatment options during their decision‐making process.
Conclusions
A range of individual and social influences on treatment decision‐making were reported. Physicians providing treatment recommendations should consider and discuss the patient and partner's existing beliefs and treatment preferences and encourage shared decision‐making. Further research on treatment decision‐making of partnered and non‐partnered PCa patients is required. We recommend research considers social ecological factors across the personal, interpersonal, community, and policy levels.
Keywords: active surveillance, decision‐making, prostate cancer, qualitative research, supportive care, treatment decision‐making
1. INTRODUCTION
Prostate cancer (PCa) is one of the most commonly diagnosed cancers in men worldwide (Sung et al., 2021). The majority of patients are diagnosed early with low to intermediate risk PCa, with a low risk of metastases and PCa‐specific mortality (Albertsen, 2015). In 2017, the American Urological Association (AUA) (Sanda et al., 2018) recommended that individuals diagnosed with very low or low risk PCa (localised to prostate, PSA < 10, Gleason score ≤ 6) be treated with active surveillance (AS). AS involves regular monitoring of the cancer (through PSA testing and biopsies) to detect progression. However, as there is currently no widespread consensus on the most effective frequency for monitoring procedures nor triggers for definitive treatment, management is often at the discretion of treating physicians (Bruinsma et al., 2016; Kinsella, Helleman, et al., 2018). Definitive treatments with curative intent, such as prostatectomy or radiation, may also be appropriate for low‐risk patients depending on patient preference and clinical factors (Sanda et al., 2018). However, definitive treatments can cause varying degrees of significant, potentially long‐lasting physical side‐effects including erectile dysfunction and incontinence (Hamdy et al., 2016). AS therefore allows patients to delay or avoid definitive treatments and their associated side‐effects until clinically necessary (Chen et al., 2016). The lack of both clear treatment recommendations and clarity regarding expected outcomes from different treatments can result in a more difficult and distressing treatment decision‐making process for patients (Owens et al., 2019).
A variety of factors have been found to influence patients' decisions on which treatment to undergo and when (Kinsella, Stattin, et al., 2018). Both quantitative research and qualitative research suggest patient treatment decisions are prominently influenced by their physician's recommendations (Brooks et al., 2018; Feldman‐Stewart et al., 2011; Kinsella, Stattin, et al., 2018). Research has also explored the role of romantic partners in the decision‐making process, given they often attend clinical appointments with the patient and assist in treatment decision‐making (Zeliadt et al., 2011). Emerging evidence suggests partners also experience anxiety related to their partners PCa and potential outcomes and tend to favour definitive treatments over AS (Couper et al., 2006; Srirangam et al., 2003). However, prior qualitative research has often interviewed couples together (which may preclude participants from sharing information), and therefore, their individual experiences, treatment preferences, and needs require further research (Stewart et al., 2021). There is also emerging evidence that patients may be influenced by opinions beyond their partner's when making treatment decisions (Berry et al., 2003). For example, one study comparing the use of online versus face‐to‐face support groups in PCa survivors found that men participating in online support groups were more likely to use peer support for treatment decision‐making and more often revised their treatment choice after consulting their support group (Huber et al., 2018). Another study reported that patients who involved close allies (i.e., friends or family in who the patient confides and whose opinion the patient considers important) in the decision‐making process were more likely to choose definitive treatment over AS (Reamer et al., 2017). However, much of this research reflects treatment preferences and decision‐making experiences prior to the 2017 AUA recommendations. Gaining an updated understanding of the range of influences on treatment decision‐making now, with AS a more common and recommended option (Sanda et al., 2017), is important for informing development of effective decision‐making support strategies for physicians to utilise with patients and their partners/close allies. Contextualising these factors through the lens of a theoretical model which extends beyond the individual and social levels, such as the social‐ecological model (SEM), may be beneficial (Bronfenbrenner, 1979). The SEM proposes individual behaviour, and decision‐making is influenced by the interaction of personal, interpersonal, community, and policy/society levels and is commonly used in cancer research (Beesley et al., 2008; McIntosh et al., 2019; Mitchell, 2011; Woods et al., 2006).
The present study used separate interviews with patients and their partners/close allies to explore the range of perceived social‐ecological influences on treatment decision‐making and examine decision‐making processes after a low risk PCa diagnosis.
2. METHODS
2.1. Study design
This qualitative study was part of a mixed methods investigation into decision‐making by patients with low risk PCa and their partners/close allies. Patients were recruited from the urology clinic at Memorial Sloan Cancer Center (MSK), a private cancer hospital in New York, USA. The quantitative part of the study used patient‐reported outcomes to investigate decision‐making pre‐ and post‐treatment decision by patients diagnosed with low risk PCa who met criteria for AS and their partners or close allies. The results from the quantitative part will be reported elsewhere (manuscript in preparation). The present study is the qualitative part of the mixed methods study, comprising semi‐structured interviews with a subset of participants after their treatment decision had been made. This study followed COREQ criteria for qualitative research (Tong et al., 2007). See supporting information for checklist. The larger mixed methods study received ethics approval from the Memorial Sloan Kettering Cancer Center (MSK; 13‐076).
2.2. Participants
To be eligible to participate in the present study, patients and partners/close allies needed to have participated in the first part of the study and have made and disclosed their treatment decision to study staff. Partners/close allies could participate in the interviews regardless of patient involvement in this study. Patient inclusion criteria for the first part of the study included meeting eligibility criteria for AS at Memorial Sloan Cancer Center (MSK) (Gleason score of ≤6 or clinical stage ≤T1c; and PSA level <10 ng/ml; and biopsy indicated <3 positive cores with ≤50% cancer in each core; or documented physician discussion of AS as a treatment option), English proficiency, aged 18+ years, no history of other cancers (except for non‐melanoma skin cancer), and no significant psychiatric or cognitive disturbance (as assessed by chart review) that would preclude providing informed consent or participation. Partners/close allies were eligible if they were viewed by the participating patient as being their partner/close ally, proficient in English, and aged 18+ years.
2.3. Procedure
Participants were invited to participate in an interview once the patient had disclosed their treatment choice study staff. The first 102 participants in the main study (N = 66 patients and N = 36 partners/close allies) who disclosed their treatment choice were invited to participate in qualitative interviews. In total, 33 patients and 15 partners agreed to participate and were interviewed. No close allies participated. Nine patients and three partners were found ineligible for AS during interviews and analysis and were therefore eliminated from the study. All interviews occurred via telephone and were audio‐recorded and transcribed verbatim. Transcribed interviews were not returned to participants for comment/correction. Interviews were semi‐structured and aimed to explore experiences of diagnosis, impact on patient lifestyle, experiences with physicians, treatment preferences/choice, treatment information understanding and needs, and overall decision‐making process (see supporting information for interview guides). Interviewers also kept field notes during interviews. All participants were interviewed once by a female research staff member (N = 4, all with bachelor/master's degrees in related fields) who had prior interview experience or had received training. Interviewers had no prior relationship with the participants outside of study interactions. Interviews lasted an average of 26 min with patients and 23 min with partners.
2.4. Analysis
Transcribed interviews were analysed by the research team (MM, CES, and RT) using reflexive thematic analysis (Braun & Clarke, 2006). Analysis was conducted in NVivo version 12 (QRS International Pty Ltd., 2020) and Microsoft Word. This process involved both MM and RT each independently conducting a close reading of all transcripts and identifying initial codes. MM, CES, and RT then analysed the same five transcripts (three patients and two partners) to identify and combine coding and create themes. Transcripts were then re‐analysed using those themes by MM and RT. Finally, themes were formally defined, summarised, and supported by extracts from the transcripts. A thematic map was also created, reviewed, and refined by all authors to illustrate the themes. As per Braun and Clarke's reflexive thematic analysis approach, data saturation was not the intention of recruitment and data analysis (Braun et al., 2019). Rather, we endeavoured to recruit and interview a high volume of eligible participants (aiming for N = 20 patients and N = 10 partners/close allies) to ensure a broad and meaningful exploration of participants experiences.
3. RESULTS
3.1. Participants
Interview data from N = 36 participants were included in the analysis (N = 24 male patients and N = 12 female partners). The average patient was 59 years old, Caucasian (83%), had a college degree or higher (83%), was employed (79%), had chosen AS for their treatment option (75%), and were married (88%). Patients were interviewed on average 48 days after reporting their treatment decision to the study staff. Partners were on average 60 years old, had a college degree or higher (75%), were employed (50%), Caucasian, married (both 100%), and were partner to a patient who had chosen AS (67%). See Table 1 for a complete breakdown of participant demographics.
TABLE 1.
Participant demographics
| Patients (n = 24) | Partners (n = 12) | |
|---|---|---|
| Age: Mean (SD) | 59.6 (6.2) years | 59.9 (5.5) years |
| Treatment choice: % (N) | ||
| Active surveillance | 75.0% (18) | 66.7% (8) a |
| Prostatectomy | 20.8% (5) | 8.3% (1) a |
| Cryotherapy | 4.2% (1) | 25.0% (3) a |
| Days since treatment decision: Mean (SD) | 47.8 (37.4) | 59.3 (47.4) a |
| Ethnicity: % (N) | ||
| Caucasian | 83.3% (20) | 100% (12) |
| African American | 4.2% (1) | 0% |
| Other | 12.5% (3) | 0% |
| Education: % (N) | ||
| Completed high school | 16.7% (4) | 25.0% (3) |
| Completed college | 83.3% (20) | 75.0% (9) |
| Current employment: % (N) | ||
| Employed | 79.2% (19) | 50.0% (6) |
| Retired or unemployed | 20.8% (5) | 50.0% (6) |
| Marital status: % (N) | ||
| Single/divorced/separated | 12.5% (3) | 0 |
| Partnered (married, de facto) | 87.5% (21) | 100% (12) |
The disclosed treatment choice of the patient in the partner–patient dyad.
3.2. Overview of themes
A thematic map is presented in Figure 1. Participants described a variety of factors as influencing treatment preferences and choice. Five major themes were identified related to influences on the treatment decision: “Partner support and direct influence on patient treatment choice,” “Patient and partner vicarious experiences may influence treatment decisions,” “The influence of the patient's external circumstances,” “Disclosing to wider social networks: friends, family, co‐workers,” and “The importance of a good relationship and experience with physicians.” Two further themes were identified related to additional considerations during the decision‐making process: “Learning about PCa and treatments” and “Weighing up the risk and benefits of treatment options.” Extracts from the transcripts to support each theme are presented in Table 2.
FIGURE 1.
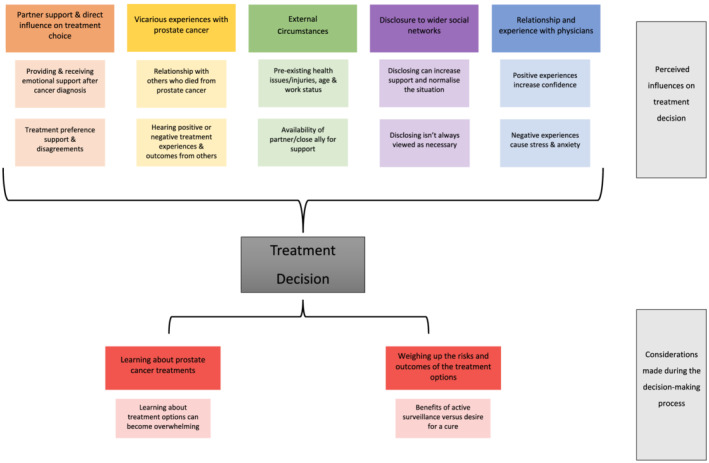
Thematic map
TABLE 2.
Illustrative quotes extracted from transcripts
| Partner support and direct influence on treatment choice |
|---|
|
Partner support and influences on the patient and the decision.
Partner disagreement about treatment choice.
|
| Patient and partner vicarious experiences may influence treatment decision |
|---|
|
| The influence of the external circumstances |
|---|
|
| Disclosure to wider social networks: friends, family, co‐workers |
|---|
|
Disclosing can increase support and normalise the situation
Disclosing is not always seen as necessary
|
| The importance of a good relationship and experience with physicians |
|---|
|
Positive experiences increase confidence
Negative experiences cause stress and anxiety
|
Seeking a second opinion can assist decision‐making
|
| Learning about PCa and treatments |
|---|
|
Learning about PCa and treatments is essential, but sometimes overwhelming
Information sources used
|
| Weighing up the risks and benefits of the treatment options |
|---|
|
Avoiding the side effects of definitive treatments
Making a treatment decision can take time
Strong desire to remove or treat the cancer
|
3.3. Partner support and direct influence on the treatment choice
3.3.1. Partner support and influences on the patient and the decision
Patients described receiving emotional and practical decision‐making support from their partners. For many, this meant attending appointments together, sharing new knowledge learnt from their own research or friends, family, or co‐workers, and discussing treatment options. Partners felt it was their responsibility to provide emotional and practical support whenever possible to the patient. Whilst many patients felt the treatment decision was solely theirs, they wanted their partner to support their choice and considered their concerns and opinions when making their decision. Often, partners deliberately withheld expressing their treatment preference until the patient had expressed theirs.
3.3.2. Partner disagreement about treatment choice
Not all participating partners supported the treatment choice that had been made. Dissatisfaction with treatment choice was particularly prevalent when the patient had chosen AS. Many partners expressed a preference for prostatectomy, believing it to be the “gold standard” treatment option, and felt concerned the patient was risking their health if they chose AS. Consequently, patients found the decision‐making process difficult when their partner disagreed with their preferences or choice.
3.4. Patient and partner vicarious experiences may influence treatment decision
The influence of vicarious PCa treatment experiences on the decision‐making process was significant. Participants who had directly or indirectly known others with PCa often considered those people's treatment experiences whilst weighing up their own treatment options. Patients and partners who knew others that had negative experiences with a particular treatment often reported an aversion towards it, especially when that person had died. On the other hand, those who had known others to have a positive experience with a particular treatment felt reassured of its safety and effectiveness. For some, another's positive treatment experience heavily influenced their own treatment preferences.
3.5. The influence of the external circumstances
The decision‐making process and treatment preference were sometimes affected by external circumstances. Some patients had other health issues or injuries at the time of diagnosis. Several patients delayed their treatment decision‐making due to external circumstances such as separation, working overseas, or undergoing their own medical treatment. Some patients felt choosing AS and delaying definitive treatment was necessary as they were still working, which would be difficult with treatment‐related side effects.
3.6. Disclosure to wider social networks: friends, family, co‐workers
3.6.1. Disclosing can increase support and normalise the situation
Deciding whether to share their diagnosis and discuss treatment options with others was another decision for participants. Many who discussed the diagnosis and treatment preferences with others, such as friends, family, or co‐workers, explained that it helped them connect to others currently going through a similar experience, bringing feelings of normalisation, hope, and support.
3.6.2. Disclosing is not always seen as necessary
However, some patients chose not to share their diagnosis and treatment choice with others, thereby deliberately limiting potential outside influences on the decision‐making process. This was most often mentioned by patients who chose AS.
3.7. The importance of a good relationship and experience with physicians
3.7.1. Positive experiences increase confidence
Feeling comfortable, confident, reassured, and well‐informed about the physician's treatment recommendation and expertise was noted by participants as essential for a positive experience with their physician, which decreased decision‐making difficulty. Participant's reported positive experiences with their physician when their physician had taken time to explain the different treatment options, appeared confident in their treatment recommendation, and rechecked or performed additional diagnostic tests. Patients who chose AS often mentioned their physician's calm attitude and reassurance provided participants with confidence in the treatment option and their decision.
3.7.2. Negative experiences cause stress and anxiety
Several patients reported having negative experiences with their diagnosing physician. In such circumstances, patients reported it had made their decision‐making more difficult and confusing. Physicians who had not provided the desired amount of information or reasoning for their treatment recommendation, appeared uninformed or biased, had not followed‐up with the patient in a timely manner, did not consider the patient's treatment preferences, and who were seen as lacking compassion were viewed poorly by the participants and often led them to pursue a second opinion. These experiences prolonged the treatment decision‐making process and caused stress, anxiety, and frustration.
3.7.3. Seeking a second opinion can assist decision‐making
Approximately half of the participants mentioned the importance of getting a second opinion regarding their diagnosis, often from a Memorial Sloan Cancer Center (MSK) physician, to assist in their decision‐making. Often the desired outcome from the second opinion was to support the first recommended treatment, to learn about or get support for other treatment options, or because they had an unsatisfactory experience with their first physician. Participants often mentioned the credibility and well‐known reputation of Memorial Sloan Cancer Center (MSK) and for many this had a considerable influence on their decision‐making. A treatment recommendation from Memorial Sloan Cancer Center (MSK) was considered credible and trustworthy, and increased participants' confidence in their treatment decision.
3.8. Learning about PCa and treatments
3.8.1. Learning about PCa and treatments is essential, but sometimes overwhelming
Learning about PCa was an essential step for participants in their decision‐making process. Most participants, especially those without prior knowledge of PCa, began researching and seeking information once the shock of the diagnosis had passed. Participants sought information to better understand their diagnosis, test results, the different treatment options and their side‐effects, to investigate physicians and their clinical expertise, and to read other patients' experiences. In general, participants felt they had access to enough information about PCa and their treatment options, and receiving information often made them feel calmer and in more control. However, it was also noted that too much information or conflicting opinions could be overwhelming and had the potential to confuse and delay decision‐making.
3.8.2. Information sources used
Patients and their partners sought information from multiple sources, including the internet (e.g., hospital websites, information found via Google searches, and YouTube videos), physicians and nurses, books, newsletters, research papers, radio, and online discussion groups. Many noted the importance of specifically looking for information from credible sources. Participants reported that other patients or partners of patients who had PCa were also valuable sources of information. For some, this was accessed by attending support groups or looking to celebrity accounts of their experiences.
3.9. Weighing up the risks and benefits of the treatment options
3.9.1. Avoiding the side effects of definitive treatments
Most patients favoured AS because it delayed definitive treatment and its associated side effects until necessary, allowing them to maintain their health and vitality for as long as possible. The potential side effects of definitive treatments weighed heavily on patients' minds and was often reported as being their main reason for choosing AS. Patients who chose AS frequently viewed the potential long‐term side effects of definitive treatment as burdensome and hoped to completely avoid treatment altogether because of this.
3.9.2. Making a treatment decision can take time
After diagnosis and being told their treatment options, participants reported deliberately taking their time to gather second opinions and research treatments. For some, AS was a relatively simple choice; many were accepting of the protocol and were relieved when their physicians and the diagnostic tests supported the treatment option. Delays in treatment decision‐making were usually due to weighing up the potential negatives of AS (e.g., fear of progression, regular biopsies, potential treatment regret) against the potential negatives of definitive treatment (e.g., experiencing short‐ and long‐term side effects, taking time off work to recover), rather than a focus on the possible benefits of either option. Others were simply overwhelmed.
3.9.3. Strong desire to remove or treat the cancer
Some patients who elected to undergo definitive treatment were open‐minded about going on AS, but the desire to act was too overwhelming. Others reported being strongly opposed to AS, due to distrust in its ability to detect progression.
4. DISCUSSION
This study aimed to investigate patients' and partners' perceived influences on treatment decision‐making after a low risk, localised PCa diagnosis. Patients and partners discussed a range of influences, particularly social influences, on treatment decision‐making. Immediately after diagnosis participants relied strongly on the opinions of medical professionals to drive their treatment choice. However, participants' treatment preference was also influenced by prior knowledge and vicarious experiences of PCa journeys. Whilst patients ultimately made their own treatment decision, both patients and partners acknowledged the importance of discussing the options and gaining support for the chosen treatment from each other. However, many partners in the study expressed disappointment or dissatisfaction with the patient's choice of treatment. These findings have implications for medical professionals regarding communicating with patients and partners after diagnosis and during the treatment decision‐making phase.
Healthcare and health promotion has been criticised for focusing largely on influencing factors related to the individual, whilst ignoring contextual factors that can influence health and health‐related behaviours (Golden & Earp, 2012). We therefore utilised the social‐ecological model (SEM) to assist in contextualising our results across the various levels outlined by the SEM (Bronfenbrenner, 1979). Our study showed participants were strongly influenced by personal (pre‐existing knowledge of PCa treatments and preferences), interpersonal (vicarious experiences of PCa, partner support and treatment preferences, relationship/experiences with physicians) and community/organisational factors (physician expertise and MSK reputation). Some of these factors have been previously identified in the literature. For instance, the process of information‐seeking and weighing the benefits/consequences of AS versus definitive treatments has been previously described (Kinsella, Stattin, et al., 2018). Research has similarly established that physicians' attitudes towards AS, the level of trust forged with the patient, and the amount of information they provide are considered influential by patients when making their PCa treatment decision (Kinsella, Stattin, et al., 2018). In our study, patients and partners emphasised that trust and the quality of their relationship with physicians was essential for confidence in treatment recommendations and their treatment choice. Participants were particularly satisfied with their physicians when they openly disclosed biases regarding particular treatments, provided clear and thorough information, were well‐informed of recent research, listened to the preferences and worries of the patient, provided ample appointment time, offered reassurance and compassion, and conducted further testing where appropriate. Physician attitude towards AS and their comfortability in managing patients who are delaying treatment until further disease progression occurs, has likely improved significantly since the AUA updated their treatment guidelines in 2017 (Sanda et al., 2018). Since the early 2000s, AS uptake has steadily increased as it becomes a more refined protocol (Kinsella, Helleman, et al., 2018). For instance, uptake of AS in the United States between 1990 and 2010 was approximately 10%, and increased to 40% by 2013 (Cooperberg & Carroll, 2015). Given the AUA treatment guidelines were again updated in 2017, it is not surprising that 75% of patients in the present study selected AS for their treatment. Participants in the present study may have been further influenced by the reputation of Memorial Sloan Cancer Center (MSK), given it is considered to specialise in AS management.
Another example of influential interpersonal factors was vicarious experiences of PCa, whether direct (e.g., family member or friend) or indirect (e.g., co‐workers and celebrities), which helped participants learn about possible treatment outcomes. Participants usually eliminated treatment options if they heard several negative experiences with a treatment, whether or not it was relevant to their own situation and clinical factors. Participants who knew of others on AS whose cancer had progressed before definitive treatment was performed were considerably more sceptical of its safety. The influence of this interpersonal factor has been previously identified (Xu et al., 2011); however, our study also found participants were similarly influenced towards treatments by positive vicarious experiences. Influence from celebrity experiences with PCa and treatments was also identified. Research has demonstrated that celebrity endorsement of cancer screening can increase the likelihood of participation—one study found that in a sample of 87 men aged 50+ who had been exposed to a celebrity endorsement of PSA testing, 31% of participants reported they were now more likely to undergo PSA testing (Larson et al., 2005). Whilst caution is needed, it may be beneficial for PCa public health messaging to harness the effects of such interpersonal influences, by including stories from celebrities and other public figures when disseminating information on PCa. Furthermore, it is important that physicians providing treatment recommendations and information are aware of the interaction and effect such factors can have on treatment preferences. Providing clear, tailored, and evidence‐based information, and exploring the patient's reasons for their choice of treatment may help physicians uncover and counter any unhelpful biases or misconceptions. This aligns with recommendations for medical professionals to utilise a shared decision‐making care model (Kane et al., 2014), which urges patients and health professionals to engage in mutual sharing of information, preferences, and needs (Kane et al., 2014). The utilisation of this model has been strongly recommended by oncology researchers as part of patient‐cantered care. Its use can result in increased patient confidence in treatment decisions, satisfaction with treatment, and trust in providers (Kane et al., 2014).
On another interpersonal level, the experience of partners in the decision‐making context was also explored. Some partners in the study expressed dissatisfaction with the patient's choice of treatment, particularly when the patient had chosen AS. Given patients desired and placed significant importance in having their partner support their treatment choice, further research into partners' treatment preferences will assist understanding how to best communicate information and provide support to both in the dyad. Little research has investigated partner's treatment preferences after a PCa diagnosis, though prior research and the present study suggest partners often favour curative treatments over AS (Couper et al., 2006; Reamer et al., 2017; Srirangam et al., 2003). Whilst partners were generally understanding of the patient's final decision no matter their choice of treatment, some expressed feelings of anxiety and worry about the patient's health and safety on AS. Partners of men with PCa often report significant levels of anxiety and depression, and research even suggests that partners may experience more psychological distress compared to the patient (Chambers et al., 2013; Couper et al., 2006; Resendes & McCorkle, 2009). However, much of this research occurred prior to the 2017 AUA recommendations for AS as the best‐available treatment option for low‐risk patients. Given AS recommendations and uptake rates have since increased, further investigation on spousal psychological distress is required. In particular, research which explores treatment preference disagreements and how this is navigated by the couple and their physicians is required. Again, the utilisation of a shared decision‐making model, considering both patient and their partner's views and preferences, is recommended.
In light of these findings, some limitations should be considered. This study was originally intended to investigate both partner and close ally experiences, as little research has explored the involvement and influence on treatment decision‐making of non‐romantic close allies in men diagnosed with PCa. Unfortunately, we were unable to recruit close allies to this study. Furthermore, no individuals in non‐heterosexual relationships choose to participate in this study. Understanding the influence of close allies and exploring the experiences of non‐heterosexual individuals are critical areas for future research. An additional limitation is that this was a single‐site study, and many participants had the same treating physician (almost 30% of patients shared the same physician, with the remaining patients spread across an additional six physicians). All physicians involved were urologists. Notably, no patients involved in the interviews chose radiotherapy as their treatment, despite this being one of the treatment types generally discussed and recommended as a curative treatment approach. Lastly, participants were predominantly Caucasian and were highly educated, and therefore results may not be reflective of patients with lower social‐economic status and minority ethnicities. Research has suggested that compared to Caucasian men, African American men have higher PCa incidence (particularly with higher grades/stages), have higher PCa mortality rates, and have differences in treatment preferences/choice (Badal et al., 2020; Desantis et al., 2016; Kan et al., 2018).
Treatment decision‐making in PCa, especially when patients are diagnosed with low risk, localised PCa, can be a complex process, as often patients and their partners are faced with several treatment options and no clear “right” answer. Our study highlights that treatment preferences were influenced by pre‐existing knowledge of vicarious experiences of PCa via friends, co‐workers, and public figures in the media, as well as by physician recommendations. Treatment decision‐making appears to become far more complex when patients and partners are exposed to either positive or negative vicarious experiences and when there are disagreements between patient and partner about the preferred treatment. These results align with the SEM, which suggests decision‐making, and behaviour, is influenced by the interaction of personal, interpersonal, community and policy/society factors (Bronfenbrenner, 1979). In practice, physicians should be aware of these interacting factors and employ a shared decision‐making care model. Specifically, physicians should discuss with their patients (and partner/close ally) the various treatment option, seek to understand their treatment preferences, and address any existing biases and misconceptions, whilst ensuring they provide evidence‐based, tailored information and recommendations.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
Supporting information
Data S1. Supporting information
Data S2. Supporting information
Data S3. Supporting information
ACKNOWLEDGEMENTS
The authors would like to thank the participants who took the time to participate in this study, as well as acknowledge the research staff involved in recruitment and conducting interviews. Author CES received support from a Victorian Cancer Agency mid‐career fellowship and author MJO was supported by a Freemasons Centre for Male Health and Wellbeing postdoctoral fellowship. Open access publishing facilitated by The University of Melbourne, as part of the Wiley ‐ The University of Melbourne agreement via the Council of Australian University Librarians.
McIntosh, M. , Opozda, M. J. , Short, C. E. , Galvão, D. A. , Tutino, R. , Diefenbach, M. , Ehdaie, B. , & Nelson, C. (2022). Social ecological influences on treatment decision‐making in men diagnosed with low risk, localised prostate cancer. European Journal of Cancer Care, 31(6), e13697. 10.1111/ecc.13697
Funding Information Financial support for this study was provided entirely by the National Cancer Institute, USA (R21‐CA164807, PI's Diefenbach, Nelson). The funding agreement ensured the authors' independence in designing the study, interpreting the data, writing, and publishing the report. Author Megan McIntosh was supported by an Australian Government Research Training Program Scholarship and a Freemasons Centre for Male Wellbeing top‐up award whilst conducting this study during her PhD.
Contributor Information
Megan McIntosh, Email: megan.mcintosh@adelaide.edu.au.
Camille E. Short, Email: camille.short@unimelb.edu.au.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
REFERENCES
- Albertsen, P. C. (2015). Observational studies and the natural history of screen‐detected prostate cancer. Current Opinion in Urology, 25(3), 232–237. 10.1097/MOU.0000000000000157 [DOI] [PubMed] [Google Scholar]
- Badal, S. , Aiken, W. , Morrison, B. , Valentine, H. , Bryan, S. , Gachii, A. , & Ragin, C. (2020). Disparities in prostate cancer incidence and mortality rates: Solvable or not? The Prostate, 80(1), 3–16. 10.1002/PROS.23923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beesley, V. , Eakin, E. , Steginga, S. , Aitken, J. , Dunn, J. , & Battistutta, D. (2008). Unmet needs of gynaecological cancer survivors: Implications for developing community support services. Psycho‐Oncology, 17(4), 392–400. 10.1002/pon.1249 [DOI] [PubMed] [Google Scholar]
- Berry, D. L. , Ellis, W. J. , Woods, N. F. , Schwien, C. , Mullen, K. H. , & Yang, C. (2003). Treatment decision‐making by men with localized prostate cancer: The influence of personal factors. Urologic Oncology: Seminars and Original Investigations, 21(2), 93–100. 10.1016/S1078-1439(02)00209-0 [DOI] [PubMed] [Google Scholar]
- Braun, V. , Clarke, V. , Hayfield, N. , & Terry, G. (2019). Thematic analysis. In Handbook of research methods in health social sciences (pp. 843–860). Springer, Singapore. 10.1007/978-981-10-5251-4_103 [DOI] [Google Scholar]
- Bronfenbrenner, U. (1979). The ecology of human development: Experiments by nature and design. Harvard University Press. https://books.google.com.au/books?hl%3Den%26lr%3D%26id%3DOCmbzWka6xUC%26oi%3Dfnd%26pg%3DPA3%26dq%3Dbronfenbrenner%2B%26ots%3DyyOWQ0YTkf%26sig%3DNWnC4ZrV66dDH_8xnpJIb7M2_9o#v%3Donepage%26q%3Dbronfenbrenner%26f%3Dfalse [Google Scholar]
- Brooks, J. V. , Ellis, S. D. , Morrow, E. , Kimminau, K. S. , & Thrasher, J. B. (2018). Patient factors that influence how physicians discuss active surveillance with low‐risk prostate cancer patients: A qualitative study. American Journal of Men's Health, 12(5), 1719–1727. 10.1177/1557988318785741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruinsma, S. M. , Bangma, C. H. , Carroll, P. R. , Leapman, M. S. , Rannikko, A. , Petrides, N. , Weerakoon, M. , Bokhorst, L. P. , & Roobol, M. J. (2016). Active surveillance for prostate cancer: A narrative review of clinical guidelines. Nature Reviews Urology, 13(3), 151–167. 10.1038/nrurol.2015.313 [DOI] [PubMed] [Google Scholar]
- Chambers, S. K. , Schover, L. , Nielsen, L. , Halford, K. , Clutton, S. , Gardiner, R. A. , Dunn, J. , & Occhipinti, S. (2013). Couple distress after localised prostate cancer. Supportive Care in Cancer, 21(11), 2967–2976. 10.1007/S00520-013-1868-6/TABLES/4 [DOI] [PubMed] [Google Scholar]
- Chen, R. C. , Rumble, R. B. , Loblaw, D. A. , Finelli, A. , Ehdaie, B. , Cooperberg, M. R. , Morgan, S. C. , Tyldesley, S. , Haluschak, J. J. , Tan, W. , Justman, S. , & Jain, S. (2016). Active surveillance for the management of localized prostate cancer (Cancer Care Ontario Guideline): American Society of Clinical Oncology clinical practice guideline endorsement. Journal of Clinical Oncology, 34(18), 2182–2190. 10.1200/JCO.2015.65.7759 [DOI] [PubMed] [Google Scholar]
- Cooperberg, M. R. , & Carroll, P. R. (2015). Trends in management for patients with localized prostate cancer, 1990‐2013. JAMA: The Journal of the American Medical Association, 314(1), 80–82. 10.1001/jama.2015.6036 [DOI] [PubMed] [Google Scholar]
- Couper, J. , Bloch, S. , Love, A. , Macvean, M. , Duchesne, G. M. , & Kissane, D. (2006). Psychosocial adjustment of female partners of men with prostate cancer: A review of the literature. Psycho‐Oncology, 15(11), 937–953. 10.1002/pon.1031 [DOI] [PubMed] [Google Scholar]
- DeSantis, C. E. , Siegel, R. L. , Sauer, G. , Miller, K. D. , Fedewa, S. A. , Alcaraz, K. I. , & Jemal, A. (2016). Cancer statistics for African Americans, 2016: Progress and opportunities in reducing racial disparities. CA: a Cancer Journal for Clinicians, 66(4), 290–308. 10.3322/CAAC.21340 [DOI] [PubMed] [Google Scholar]
- Feldman‐Stewart, D. , Brundage, M. D. , & Tong, C. (2011). Information that affects patients' treatment choices for early stage prostate cancer: A review. The Canadian Journal of Urology, 18(6), 5998–6006. PMID: http://www.ncbi.nlm.nih.gov/pubmed/22166326 [PubMed] [Google Scholar]
- Hamdy, F. C. , Donovan, J. L. , Lane, J. A. , Mason, M. , Metcalfe, C. , Holding, P. , Davis, M. , Peters, T. J. , Turner, E. L. , Martin, R. M. , Oxley, J. , Robinson, M. , Staffurth, J. , Walsh, E. , Bollina, P. , Catto, J. , Doble, A. , Doherty, A. , Gillatt, D. , … Neal, D. E. (2016). 10‐year outcomes after monitoring, surgery, or radiotherapy for localized prostate Cancer. The New England Journal of Medicine, 375(15), 1415–1424. 10.1056/NEJMoa1606220 [DOI] [PubMed] [Google Scholar]
- Huber, J. , Muck, T. , Maatz, P. , Keck, B. , Enders, P. , Maatouk, I. , & Ihrig, A. (2018). Face‐to‐face vs. online peer support groups for prostate cancer: A cross‐sectional comparison study. Journal of Cancer Survivorship, 12(1), 1–9. 10.1007/s11764-017-0633-0 [DOI] [PubMed] [Google Scholar]
- Kan, C. K. , Qureshi, M. M. , Gupta, A. , Agarwal, A. , Gignac, G. A. , Bloch, B. N. , Thoreson, N. , & Hirsch, A. E. (2018). Risk factors involved in treatment delays and differences in treatment type for patients with prostate cancer by risk category in an academic safety net hospital. Advances in Radiation Oncology, 3(2), 181–189. 10.1016/J.ADRO.2017.12.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kane, H. L. , Halpern, M. T. , Squiers, L. B. , Treiman, K. A. , & McCormack, L. A. (2014). Implementing and evaluating shared decision making in oncology practice. CA: a Cancer Journal for Clinicians, 64(6), 377–388. 10.3322/caac.21245 [DOI] [PubMed] [Google Scholar]
- Kinsella, N. , Helleman, J. , Bruinsma, S. , Carlsson, S. , Cahill, D. , Brown, C. , & Van Hemelrijck, M. (2018). Active surveillance for prostate cancer: A systematic review of contemporary worldwide practices. Translational Andrology and Urology, 7(1), 83–97. 10.21037/tau.2017.12.24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinsella, N. , Stattin, P. , Cahill, D. , Brown, C. , Bill‐Axelson, A. , Bratt, O. , Carlsson, S. , & Van Hemelrijck, M. (2018). Factors influencing men's choice of and adherence to active surveillance for low‐risk prostate cancer: A mixed‐method systematic review. European Urology, 74(3), 261–280. 10.1016/j.eururo.2018.02.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larson, R. J. , Woloshin, S. , Schwartz, L. M. , & Welch, H. G. (2005). Celebrity endorsements of cancer screening. JNCI: Journal of the National Cancer Institute, 97(9), 693–695. 10.1093/jnci/dji117 [DOI] [PubMed] [Google Scholar]
- McIntosh, M. , Opozda, M. J. , Evans, H. , Finlay, A. , Galvão, D. A. , Chambers, S. K. , & Short, C. E. (2019). A systematic review of the unmet supportive care needs of men on active surveillance for prostate cancer. Psycho‐Oncology, 28(12), 2307–2322. 10.1002/pon.5262 [DOI] [PubMed] [Google Scholar]
- Mitchell, J. (2011). Examining the influence of social ecological factors on prostate cancer screening in urban African‐American men. Social Work in Health Care, 50(8), 639–655. 10.1080/00981389.2011.589891 [DOI] [PubMed] [Google Scholar]
- Owens, O. L. , Estrada, R. M. , Johnson, K. , Cogdell, M. , Fried, D. B. , Gansauer, L. , & Kim, S. (2019). ‘I'm not a chance taker’: A mixed methods exploration of factors affecting prostate cancer treatment decision‐making. Ethnicity and Health, 26, 1143–1162. 10.1080/13557858.2019.1606165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- QRS International Pty Ltd . (2020). NVivo (No. 12). https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home
- Reamer, E. , Yang, F. , Holmes‐Rovner, M. , Liu, J. , & Xu, J. (2017). Influence of men's personality and social support on treatment decision‐making for localized prostate cancer. BioMed Research International, 2017, 1–8. 10.1155/2017/1467056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resendes, L. A. , & McCorkle, R. (2009). Spousal responses to prostate Cancer: An integrative review. Cancer Investigation, 24(2), 192–198. 10.1080/07357900500524652 [DOI] [PubMed] [Google Scholar]
- Sanda, M. G. , Cadeddu, J. A. , Kirkby, E. , Chen, R. C. , Crispino, T. , Fontanarosa, J. , Freedland, S. J. , Greene, K. , Klotz, L. H. , Makarov, D. V. , Nelson, J. B. , Rodrigues, G. , Sandler, H. M. , Taplin, M. E. , & Treadwell, J. R. (2018). Clinically localized prostate cancer: AUA/ASTRO/SUO guideline. Part I: Risk stratification, shared decision making, and care options. The Journal of Urology, 199(3), 683–690. 10.1016/j.juro.2017.11.095 [DOI] [PubMed] [Google Scholar]
- Srirangam, S. J. , Pearson, E. , Grose, C. , Brown, S. C. W. , Collins, G. N. , & O'Reilly, P. H. (2003). Partner's influence on patient preference for treatment in early prostate cancer. BJU International, 92(4), 365–369. 10.1046/j.1464-410X.2003.04355.x [DOI] [PubMed] [Google Scholar]
- Stewart, S. J. , Roberts, L. , & Brindle, L. (2021). Romantic partner involvement during oncology consultations: A narrative review of qualitative and quantitative studies. In Patient education and counseling (Vol. 104) (pp. 64–74). Elsevier Ireland Ltd. 10.1016/j.pec.2020.08.018 [DOI] [PubMed] [Google Scholar]
- Sung, H. , Ferlay, J. , Siegel, R. L. , Laversanne, M. , Soerjomataram, I. , Jemal, A. , & Bray, F. (2021). Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: a Cancer Journal for Clinicians, 71(3), 209–249. 10.3322/caac.21660 [DOI] [PubMed] [Google Scholar]
- Woods, V. D. , Montgomery, S. B. , Herring, R. P. , Gardner, R. W. , & Stokols, D. (2006). Social ecological predictors of prostate‐specific antigen blood test and digital rectal examination in black American men. Journal of the National Medical Association, 98(4), 492–504. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2569227/ [PMC free article] [PubMed] [Google Scholar]
- Xu, J. , Dailey, R. K. , Eggly, S. , Neale, A. V. , & Schwartz, K. L. (2011). Men's perspectives on selecting their prostate cancer treatment. Journal of the National Medical Association, 103(6), 468–479. 10.1016/s0027-9684(15)30359-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeliadt, S. B. , Penson, D. F. , Moinpour, C. M. , Blough, D. K. , Fedorenko, C. R. , Hall, I. J. , Smith, J. L. , Ekwueme, D. U. , Thompson, I. M. , Keane, T. E. , & Ramsey, S. D. (2011). Provider and partner interactions in the treatment decision‐making process for newly diagnosed localized prostate cancer. BJU International, 108(6), no. 10.1111/j.1464-410X.2010.09945.x [DOI] [PubMed] [Google Scholar]
- Tong, A. , Sainsbury, P. , & Craig, J. (2007). Consolidated criteria for reporting qualitative research (COREQ): a 32‐item checklist for interviews and focus groups. International Journal for Quality in Health Care, 19(6), 349–357. 10.1093/intqhc/mzm042 [DOI] [PubMed] [Google Scholar]
- Braun, V ., & Clarke, V. (2006). Using thematic analysis in psychology.Qualitative Research in Psychology, 3(2), 77–101. 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- Golden, S. D. , & Earp, J. A. L. (2012). Social Ecological Approaches to Individuals and Their Contexts. Health Education & Behavior, 39(3), 364–372. 10.1177/1090198111418634 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. Supporting information
Data S2. Supporting information
Data S3. Supporting information
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.


