Abstract
Aims and Objectives
To (i) determine prevalence of distress among caregivers of people living with cancer, (ii) describe caregivers’ most commonly reported problems and (iii) investigate which factors were associated with caregivers’ distress.
Background
The psychological distress associated with a cancer diagnosis jointly impacts those living with cancer and their caregivers(s). As the provision of clinical support moves towards a dyadic model, understanding the factors associated with caregivers’ distress is increasingly important.
Design
Cross‐sectional study.
Methods
Distress screening data were analysed for 956 caregivers (family and friends) of cancer patients accessing the Cancer Council Western Australia information and support line between 1 January 2016 and 31 December 2018. These data included caregivers' demographics and reported problems and their level of distress. Information related to their care recipient's cancer diagnosis was also captured. Caregivers' reported problems and levels of distress were measured using the distress thermometer and accompanying problem list (PL) developed by the National Comprehensive Cancer Network. A partial‐proportional logistic regression model was used to investigate which demographic factors and PL items were associated with increasing levels of caregiver distress. Pearlin's model of caregiving and stress process was used as a framework for discussion. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) checklist was followed.
Results
Nearly all caregivers (96.24%) recorded a clinically significant level of distress (≥4/10) and two thirds (66.74%) as severely distressed (≥7/10). Being female, self‐reporting sadness, a loss of interest in usual activities, sleep problems or problems with a partner or children were all significantly associated with increased levels of distress.
Conclusions
Caregivers of people with cancer reporting emotional or familial problems may be at greater risk of moderate and severe distress.
Relevance to Clinical Practice
Awareness and recognition of caregiver distress are vital, and referral pathways for caregivers are the important area of development.
Keywords: Australia, cancer, caregivers, cross‐sectional studies, logistic models, oncology nursing, prevalence, psychological distress
What does the paper contribute to the wider global clinical community?
Approximately two‐thirds of all caregivers accessing a support line were severely distressed, with nearly all exhibiting clinical distress levels.
Clinical distress levels in this study were higher than previous studies; however, this may be attributable to the context of data collection, where carers were actively seeking support.
There is need for cancer support services to encompass the caregiver to provide timely intervention to help prevent and reduce caregiver distress.
1. INTRODUCTION
Cancer is a leading cause of death worldwide, accounting for nearly 10 million deaths in 2020 (Ferlay et al., 2020). Over 200,000 new cases were recorded in Australia in 2020 (Sung et al., 2021) with approximately 450,000 people diagnosed between 2015 and 2020. The burden of cancer is growing worldwide, reflective of increasing incidence associated with ageing populations and changes in the prevalence and distribution of key risk factors for the disease, many of which are associated with socioeconomic development (Bray et al., 2021). Additionally, over the past few decades as cancer care has shifted from inpatient to outpatient, higher demands and responsibilities have been placed on the caregiver (Girgis et al., 2017). There are an estimated 2.65 million caregivers to people with an illness or disability in Australia (Australian Bureau of Statistics [ABS], 2019). The proportion of caregivers of people living with cancer is likely to be a sizeable proportion based on the prevalence of cancer.
As survival rates of cancer continue to improve, an increasing number of people are living with the disease whilst managing the negative physical, emotional and psychosocial sequelae was associated with its treatment (Decadt et al., 2021). Additionally, with advances in cancer treatment and greater choice related to the delivery of care, including ambulatory care, oral medications and care delivered in the home care setting, the awareness and involvement of caregivers in the treatment process is likely to increase. The roles played by caregivers are often context dependent, but typically range from providing emotional and practical support to assisting with medical care (Cancer Council, 2020a). Many caregivers, particularly familial caregivers, often act in an unpaid capacity to fulfil what they perceive to be an obligation to their family member with cancer (PDQ Supportive & Palliative Care Editorial Board, 2021). Caregiving has been described as an important aspect of support for those affected by cancer. However, providing support comes with its own set of challenges for caregivers, such as maintaining their own self‐care and healthcare needs (Shaffer et al., 2019). Reduced quality of life and increased distress related to the physical, social, financial and practical challenges of informal caregiving have been well documented (Long et al., 2016; Mosher et al., 2017; Nipp et al., 2016; Shaffer et al., 2019; Taylor et al., 2020).
1.1. Background
The impact of providing care can affect the psychological, social, spiritual and physical needs of the caregiver (NCCN, 2021). Approximately one‐third to one‐half of carers report significant psychological distress and are more likely to experience mental health problems compared to the general population (Shah et al., 2010). Caregivers have reported being overwhelmed with information, organising care and a constant need to assess their care recipient's needs (Von Ah et al., 2016). The level of stress associated with caregiving is influenced by a range of factors including the level of care required, the physical or cognitive impairment of the care recipient and the duration of care (Pinquart & Sörensen, 2003; Swinkels et al., 2018). Maintaining the psychological well‐being of the carer underpins the viability of the caregiving process (Pristavec, 2019). A meta‐analysis of differences between carers and non‐carers across a range of caregiving contexts found that carers reported higher levels of stress, depression and lower levels of well‐being compared to non‐carers (Pinquart & Sörensen, 2003). A systematic review (Anastasiadou et al., 2014) reported higher anxiety scores for relatives who care for family members with eating disorders compared to those of relatives of healthy family members. Parents who cared for adult children with severe mental illness experience chronic stress as measured through physiological markers including elevated cortisol profiles (Barker et al., 2012). In the cancer field, nearly one‐third (29%) of caregivers of renal cell carcinoma survivors reported elevated anxiety (Oberoi et al., 2016), 39% of caregivers of people with pancreatic cancer experienced clinical levels of anxiety, with 14% experiencing depression (Janda et al., 2017) and 16.4% and 42.2% of caregivers of people with lung or gastrointestinal cancer reported experiencing depression and anxiety respectively (Nipp et al., 2016).
The association between caregiving and psychological distress has been established across different caregiving contexts and health conditions. The evidence also suggests heterogeneity in the psychological distress experienced by carers with a range of factors shown to influence the psychological distress of carers (Mulud & McCarthy, 2017). Factors include the relationship between the carer and care recipient (Springate & Tremont, 2014), financial costs related to caregiving (Meiland et al., 2005) and hours of care per day (George et al., 2020). A number of carer‐related variables are associated with the relationship between caregiving and psychological distress, including gender, resilience (Springate & Tremont, 2014), sense of competence (Meiland et al., 2005), coping style (Coomber & King, 2012), carer anxiety, household income and living with the care recipient (Giordano et al., 2016).
Whilst the experience of psychological distress among caregivers is widely recognised, few studies specifically test the moderating effect of variables on the relationship between caregiving and psychological distress. Further, the majority of studies have drawn on relatively small samples of carers. The carer‐distress process identified in the research to date is specific to carers of people with a particular condition, and not generalisable across conditions and carer contexts.
Screening for distress in individuals with cancer is well documented and is often considered the sixth vital sign in cancer care (Bultz & Carlson, 2006). However, distress screening of caregivers is often overlooked, despite its value in the recognition of distress, and its potential for identifying where additional resources, services or support may be required (Tanco et al., 2017). Several studies have used the National Comprehensive Cancer Network (NCCN) Distress Thermometer (DT) as the instrument of choice for screening distress, in both people with cancer and their caregivers. For example, Halkett et al. (2017) found 62% of caregivers reported moderate (31%) to high distress (31%) at their care recipient's initial visit to clinic. Additionally, Fennell et al. (2016) found caregivers reported significantly more distress than those with cancer, a phenomenon which has been consistently established in the literature (Chambers et al., 2012; Halkett et al., 2018).
1.2. Purpose
Recognising the need for distress screening in both people with cancer and their caregivers, Cancer Council Western Australia (CCWA) began using the NCCN DT and problem list (PL) as a screening tool used by Cancer Nurses and Cancer Support Service Coordinators (CSCs) operating their Information and Support helpline (Cancer Council, 2020b). This service largely caters for people living with cancer but also serves their family and friends (Cancer Council, 2020b), who are often involved in their care (Hughes et al., 2011). The Information and Support line helps people affected by cancer by providing information, guidance and referral to services based on a person's level of distress and their identified needs.
Using a non‐identifiable data set extracted from the CCWA information and support line database, this study aimed to (i) characterise the prevalence of clinically significant distress among caregivers of people with cancer, (ii) describe caregivers most commonly reported problems and (iii) determine which factors were associated with caregivers’ increasing levels of distress.
1.3. Theoretical framework
Whilst the study was not informed by a theoretical framework, the findings resonated with Pearlin's model of caregiving and stress process. Pearlin and colleagues have been studying stress since the 1970s. Their earlier work suggests there are multiple factors that contribute to the stress process such as individual characteristics, current life events, chronic stressors, coping mechanisms and social supports (or lack thereof) (Pearlin et al., 1981). Recent work, specifically on stress in caregiving, highlighted several more dimensions including those factors that are directly related to daily caregiving or in relation to role conflict (family composition). Additionally, sociodemographic background and resource availability for caregivers, such as social support, play an important role in the model (Pearlin et al., 1990). The model divides the stressors into objective and subjective indicators that may impact the overall physical and mental well‐being of the caregiver. Pearlin's model also suggests as the stress in the various dimensions becomes greater for the caregiver, the overall well‐being of the individual can be negatively impacted, emphasising the importance of psychosocial support and resources (Pearlin et al., 1990).
2. METHODS
2.1. Study design and participants
This cross‐sectional study included non‐identifiable demographic and distress screening data for a sub‐sample of people identified as ‘friends and family’ of people with cancer (hereafter referred to as caregivers), who accessed CCWA’s information and support line anytime between 1 January 2016 and 31 December 2018. A caregiver, as defined in this paper, is someone who provides continuing unpaid support and care to a person who requires this assistance due to cancer (Cancer Council, 2020a).
2.2. Procedure
This study's procedures followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) checklist (Von Elm et al., 2007) (Data S1). A comprehensive description of the methods is presented elsewhere (Kirk et al., 2021). Briefly, people affected by cancer are typically referred to the CCWA Information and Support Line service by a CCWA representative or health professional (Cancer Nurses or General Practitioners). Individuals access the information and support line service either in‐person at designated CCWA offices or satellite hubs, or via telephone (Cancer Council Western Australia [CCWA], 2020a, 2020b). Following initial engagement with the service (telephone, email or in‐person), the responsible cancer nurse or CSC details the distress screening procedure and obtains informed verbal consent for the collection and use of the individual's data. To consent, a person had to be ≥18 years old and be proficient in English (Watts et al., 2016). Individuals are then screened for distress by a CSC or cancer nurse who record users’ demographics, diagnoses, distress score and self‐reported problems on a client database. Ethical approval for this study was granted by the Human Research Ethics Committee of Edith Cowan University (#2020‐01656‐Kirk). The data were provided to the research team by a CCWA representative in a non‐identifiable format for the purpose of secondary analysis by a CCWA representative. In instances where a caregiver made use of the service more than once over the observed period, only their first recorded measures were used.
2.3. Instruments and measures
2.3.1. Demographics and cancer diagnosis‐related information
Nurses operating the information and support line collect caregivers’ demographic data including their ethnicity, gender, date of birth and residential postcodes. Caregivers are also asked to provide diagnosis‐related information pertaining to the type and stage of cancer affecting their care recipient.
2.3.2. Distress thermometer
The NCCN distress screening tool (DT) was used to measure caregivers’ level of distress (National Comprehensive Cancer Network [NCCN], 2021). The DT asks caregivers to rate their level of distress in the past 7 days on a scale from 0 to 10 (no distress to extreme distress). These values were categorised as low distress (0–3), moderate distress (4–6) and severe distress (7–10) for the purpose of analysis. A score ≥4 denotes a clinically significant marker for distress, alerting the screener that the person may require referral to a service to address their identified source(s) of distress. A score ≥7 denotes ‘severe’ distress requiring urgent intervention (Carlson et al., 2019; Gessler et al., 2008; Mejdahl et al., 2015).
2.3.3. Problem list
The PL is administered alongside the DT during distress screening to help identify the caregivers’ source(s) of distress (NCCN, 2021). The PL consists of 39 items/questions pertaining to the emotional, physical, practical, familial and spiritual/religious concerns of the caregivers.
2.4. Data preparation
Measures for caregivers’ accessibility to services and socioeconomic status (SES) were assigned using the Accessibility/Remoteness Index of Australia (ARIA) score and the Socio‐Economic Indexes for Areas (SEIFA) score allocated by the Australian Bureau of Statistics to their residential postcode (Australian Bureau of Statistics [ABS], 2018, 2020). Measures for SES are recorded as deciles at the State level, which were transformed into quintiles ordered from most to least disadvantaged (Q1–Q5). ARIA scores are recorded as quintiles constituting ‘highly accessible’, ‘accessible’, ‘moderately accessible’, ‘remote’ and ‘very remote’ areas, which approximate major cities, inner regional areas, outer regional areas, remote areas and very remote areas. However, due to small numbers, the remote and very remote ARIA category were merged.
Cancer diagnoses and stage‐related information were self‐reported by caregivers on behalf of their care recipient. Self‐reported diagnoses were assigned an International Classification of Disease (ICD) (10th Revision) code by CCWA database representatives, using the ICD and Related Health Problems 10th Revision handbook (World Health Organisation [WHO], 2016). Thirteen discrete cancer groups were created from those CCWA‐assigned ICD codes (Supplementary File S1). These groups represented the following type(s) of cancer: digestive, breast, bone, eye/brain/central nervous system, leukaemia and lymphoma, respiratory, oral, female genital organs, male genital organs, mesothelial and soft tissue, endocrine, urinary and skin.
2.5. Data analysis
Prevalence of distress, caregivers’ demographic data and their care recipient's clinical data were reported tabularly using descriptive statistics. Caregivers’ most commonly reported problems (those identified by 15% or more of the sample) were depicted graphically via bar chart, stratified by level of distress.
A multivariate ordinal logistic regression model was constructed with demographic and distress screening variables to examine their effect(s) on increasing levels of distress (low, moderate and severe). Forward stepwise automated variable selection was used to determine which variables to include in the model. Variables to be included in the model were evaluated for collinearity and multicollinearity with respect to measures of covariance, tolerance and variance inflation factor. Following a Chi‐Square Score test, the proportional odds assumption in the model was rejected, leading to the construction of a partial‐proportional cumulative logit model, as described in Peterson and Harrell (1990). A partial‐proportional odds model was fitted to allow for non‐differential impacts of the explanatory variables on increasing levels of distress. Mosaic plots were used to visually determine which included variables contributed to non‐proportionality in the model, as recommended by Downer (2018) (Supplementary Files S2–S5). Likelihood ratio tests confirmed that the partial‐proportional model was not a significantly worse fit for the data than the proportional odds model. Statistical significance was considered with respect to an ∂ value of 0.05. Model output is presented using odds ratios (ORs) with their associated 95% confidence intervals (95% CIs).
3. RESULTS
Between 1 January 2016 and 31 December 2018, a total of 956 caregivers of people with cancer accessed the CCWA information and support line. A majority of caregivers were between the ages of 30–49 years (30.1%) and 50–69 years (40.2%) (Table 1). Nearly all caregivers were clinically distressed (96.2%), with two‐thirds (66.7%) identified as severely distressed. The mean age of the sample was 51.66 (standard deviation = 15.94), with more than three quarters (78.0%) represented by women (Table 1). Diagnosis‐related information for the care recipient was notably missing (Table 2), with 43.4% of caregivers screened not reporting their care recipient's diagnosis. Of those reported, digestive and blood cancers were most prevalent, representing 24% and 14.1% of total reported cancer cases respectively. Additionally, stage of disease was poorly recorded with 48.9% of the total sample not recording their care recipient's cancer stage. Of those people who provided a disease stage category (n = 489), the majority (80.2%) recorded ‘unknown’. Furthermore, caregivers’ ethnic details were poorly recorded, with 41.3% of the sample missing data. Where these data were available, <1% were Aboriginal and Torres Strait Islander peoples, with the majority represented by non‐Indigenous Australian, European (mainland Europe, British and Irish), New Zealander, Chinese and South African. The distribution of SES was dispersed, with more than half of the sample characterised by either the lowest (26.7%) or second highest SES quintile (29%). Nearly three quarters of the sample (73.0%) reported living in urban areas (major cities), with the remainder mostly living in inner regional areas (16.6%).
TABLE 1.
Sample demographics and characteristics
| Caregiver characteristics | n (%) |
|---|---|
| Total | 956 |
| Distress category | |
| Low (0–3) | 36 (3.8) |
| Moderate (4–6) | 318 (29.5) |
| Severe (7–10) | 638 (66.7) |
| Median distress score (IQR) | 7 (2) |
| Care recipient's stage of disease | |
| Early/localised | 24 (2.5) |
| Metastasis/widespread/advanced | 45 (4.7) |
| Recurring | 12 (1.3) |
| Stable | 4 (0.4) |
| Terminal | 8 (0.8) |
| Second primary | 1 (0.1) |
| Remission | 3 (0.3) |
| Unknown | 392 (41.0) |
| Missing | 467 (48.9) |
| Gender | |
| Female | 746 (78.0) |
| Male | 205 (21.4) |
| Non‐binary | 5 (0.5) |
| Age group | |
| <20 | 25 (2.6) |
| 20–29 | 65 (6.8) |
| 30–49 | 288 (30.1) |
| 50–69 | 384 (40.2) |
| 70–79 | 105 (11.0) |
| >79 | 14 (1.6) |
| Missing | 75 (7.9) |
| Ethnicity | |
| Non‐aboriginal peoples | 422 (44.1) |
| Aboriginal and Torres Strait Islander peoples | 7 (0.7) |
| Other | 132 (13.8) |
| Missing | 395 (41.3) |
| ARIA category | |
| Highly accessible (major cities) | 698 (73.0) |
| Accessible (inner regional) | 159 (16.6) |
| Moderately accessible (outer regional) | 76 (8.0) |
| Remote and very remote | 16 (1.7) |
| Missing | 7 (0.7) |
| State SEIFA quintile | |
| Q1 (most disadvantaged) | 255 (26.7) |
| Q2 | 142 (14.9) |
| Q3 | 205 (21.4) |
| Q4 | 277 (29.0) |
| Q5 (least disadvantaged) | 70 (7.3) |
| Missing | 7 (0.7) |
Q = quintile; Missing = Data unavailable for the specified number of caregivers.
Abbreviations: ARIA, accessibility/remoteness index for areas; IQR, interquartile range; SEIFA, socio‐economic index for areas.
TABLE 2.
Care recipients' cancer diagnoses by group
| Cancer groups |
Cancer cases (n) |
Proportion of total reported cancers (%) |
|---|---|---|
| Bone | 2 | 0.4 |
| Breast | 59 | 10.4 |
| Digestive | 136 | 24.0 |
| Endocrine | 11 | 1.9 |
| Eye, brain, CNS | 54 | 9.5 |
| Female genital organs | 26 | 4.6 |
| Leukaemia and Lymphoma | 80 | 14.1 |
| Male genital organs | 48 | 8.5 |
| Mesothelial and soft tissue | 24 | 4.2 |
| Oral | 13 | 2.3 |
| Respiratory | 62 | 10.9 |
| Skin | 31 | 5.5 |
| Urinary | 21 | 3.7 |
Abbreviation: CNS, central nervous system.
The most commonly reported PL items by recorded level of distress are presented in Figure 1. The proportion of all caregivers who answered affirmatively to each PL item is appended to each bar. ‘Emotional problems’ accounted for the three most frequently reported problems overall, with worry, sadness and fears identified as problems by 79.0%, 75.8% and 57.4% of the sample respectively. Slightly more than one quarter of all caregivers self‐reported depression (27.5%), with nervousness and loss of interest in usual activities reported by 22.9% and 21.4% of the sample respectively. Sleep problems were reported by 41.4% of the sample. In the practical problem category, having concern about treatment decisions was reported by more than one quarter (28.2%) of all patients, with slightly fewer reporting insurance/financial problems (17.9%). In the family problem category, dealing with a partner was more frequently reported as a problem than was dealing with children, with 36.5% of the sample and 23% of the sample recording those problems respectively.
FIGURE 1.
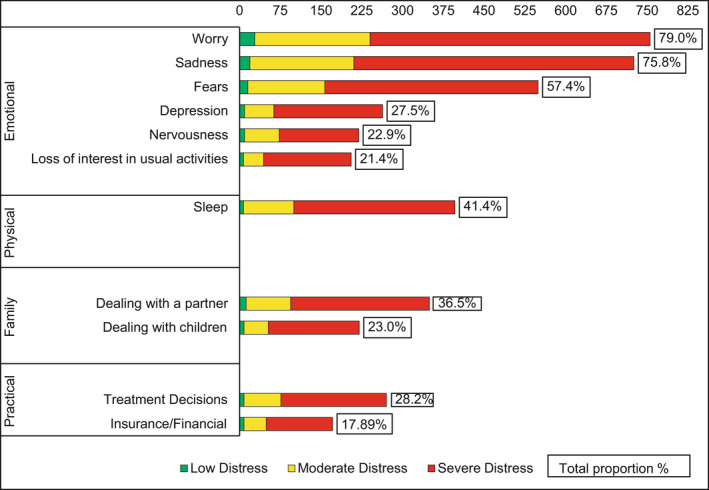
Most frequently reported problem list items by distress category [Colour figure can be viewed at wileyonlinelibrary.com]
Table 3 details the results of the partial‐proportional ordinal logistic regression model. Self‐reporting problems dealing with your partner, problems dealings with your children, sadness, sleep problems or a loss of interest in usual activities significantly increased a person's odds of reporting higher levels of distress. Being male significantly reduced a person's odds of reporting higher levels of distress. There was no evidence of multicollinearity or collinearity between those factors identified as associates for distress in the model (Supplementary Files S6 and S7).
TABLE 3.
Factors associated with increasing levels of distress
| Proportional odds | Non‐proportional odds | |||||
|---|---|---|---|---|---|---|
| Severe vs. moderate vs. low distress | Moderate distress vs. low distress | Severe distress vs. moderate distress | ||||
| Factors | OR | 95% CIs | OR | 95% CIs | OR | 95% CIs |
| Problems dealing with your partner | 1.52 | 1.08–2.13 | ||||
| Problems dealing with your children | 1.76 | 1.17–2.64 | ||||
| Male (female as reference) | 0.62 | 0.44–0.89 | ||||
| Age group (50–69 as reference) | ||||||
| <20 | 0.46 | 0.20–1.04 | ||||
| 20–29 | 0.59 | 0.33–1.06 | ||||
| 30–49 | 0.65 | 0.46–0.94 | ||||
| 70–79 | 1.08 | 0.65–1.80 | ||||
| >79 | 0.77 | 0.25–2.42 | ||||
| Sadness | 2.69 | 1.22–5.93 | 1.70 | 1.18–2.46 | ||
| Sleep problems | 1.98 | 0.82–4.79 | 1.57 | 1.11–2.23 | ||
| Loss of interest in usual activities | 0.56 | 0.23–1.39 | 1.89 | 1.23–2.90 | ||
| ARIA (highly accessible as reference) | ||||||
| Accessible | 0.49 | 0.20−1.20 | 1.01 | 0.65–1.56 | ||
| Moderately accessible | 1.81 | 0.23–14.09 | 0.16 | 0.09–0.28 | ||
| Remote and very remote | 0.66 | 0.08–5.31 | 1.45 | 0.44–4.76 | ||
Abbreviations: ARIA, accessibility/remoteness index of Australia; CI, confidence interval; OR, odds ratio.
Half of the factors identified as associates for distress differentially affected the odds of transitioning between distress levels. For example, those with a low level of distress who self‐reported sadness as a problem on the PL were 2.69 times more likely to report moderate distress relative to those who did not self‐report sadness as a problem on the PL, whereas moderately distressed people who self‐reported sadness as a problem were 1.7 times more likely to report severe distress relative to those who did not identify sadness as a problem. For those who were moderately distressed, self‐reporting sleep problems were associated with a 57% increase in the odds of reporting severe distress. However, among those with a low level of distress, self‐reporting sleep problems were not associated with a significant increase in the odds of reporting a moderate level of distress. Self‐reporting a loss of interest in usual activities was associated with an 89% increase in the likelihood of reporting severe distress; however, there was no significant increase in the odds of reporting moderate distress among low distress individuals who identified losing interest in their usual activities. Although the Mosaic plots (Supplementary Files S2–S5) indicated non‐proportionality of odds for ARIA categories; there was no clear relationship in terms of how living in non‐urban areas impacted the odds of reporting a higher level of distress. The exception was for caregivers living in outer regional (moderately accessible) areas, who had significantly lower odds of reporting a severe level of distress relative to their urban‐dwelling (highly accessible) counterparts; OR = 0.16, 95% CI = (0.09–0.28).
The remaining factors identified as associates for distress had proportional odds, indicating an equivalent effect across distress levels (low to moderate to high). For example, those who self‐reported having problems dealing with their partner had a 52% increase in the odds of transitioning to a higher level of distress relative to those who did not report this problem. This effect was more pronounced for those who self‐reported having problems dealing with their children, with a 76% increase in the odds of transitioning to a higher level of distress relative to those who did not identify this as a problem. Relative to those in the 50–69‐year age group, all but one age group (70–79) had lower odds of reporting higher levels of distress, indicated by ORs <1. However, only the result for those in the 30–49‐year age group was significant; OR = 0.65, 95% CI = (0.46–0.94), indicating that those in the 30–49‐year age group were significantly less likely to report a higher level of distress than those in the 50–69‐year age group. Additionally, men were 38% less likely to report higher levels of distress than were women.
4. DISCUSSION
4.1. Prevalence of distress
Approximately, two‐thirds of all caregivers accessing the Cancer Council Information and Support line were severely distressed, with 96.2% of the sample characterisable as clinically distressed. The median (interquartile range [IQR]) DT score for caregivers was 7 (2). These prevalence metrics show greater clinical distress in this sample compared to other Australian studies using equivalent data sources, and the same DT screening tool, for example Hawkes et al. (2010); 90.4%, Heckel et al. (2018); 42%, Chambers et al. (2012); ~50%, and Hughes et al. (2011); median (IQR) 6 (3). Similarly, prevalence of clinical distress was also higher in this study than international studies of cancer caregivers, which also used the DT, for example De Laurentis et al. (2019); 63%, Decadt et al. (2021); 44.2% (with 19.9% severely distressed), and Fujinami et al. (2015); mean DT score of 4.4, standard deviation 2.81. Only one examined study had equivalent distress metrics, with 95% of their sample of caregivers of advanced cancer patients undergoing palliative care characterisable as clinically distressed. It is possible that prevalence of clinical distress was higher in this study compared to other studies on account of the context of data collection. For example, people who actively seek support from a dedicated helpline may be more distressed at the time of screening relative to those whose distress screening data are captured within a clinical or research setting. According to Pearlin's stress model, an individual's characteristics, skills for coping with stress, availability of social support and networks, and primary and secondary causes of distress contribute to psychological distress. Early recognition through screening is an important element of the model (Pearlin et al., 1990).
4.2. Gender
Within Australia, across all illnesses and disabilities, women are 2.5 times more likely to act as primary caregivers than men (Australian Bureau of Statistics, 2019). In this sample, there were 3.64 times (78% vs. 21.4%) more female caregivers than male caregivers accessing the information and support line. The large disparity in gender in terms of accessing this support service relative to the smaller disparity by gender in terms of providing care may indicate that male caregivers are less likely to seek dedicated support services than female caregivers. One explanation may be that male caregivers are significantly less distressed than female caregivers, as suggested by our findings (OR = 0.62, 95% CIs = 0.44–0.89) and others (Hagedoorn et al., 2008), thus making men less likely to seek support. Alternatively, it could be that male caregivers are less likely to seek support, and/or potentially underreport their distress during screening, due to historic yet perpetual male stereotypes of needing to appear strong in the face of adversity (Nicholas, 2000). According to Pearlin's stress process model, social support plays an integral role in how individuals cope with stressors (Pearlin et al., 1990). Consequently, not having or seeking this support can be associated with increased caregiver burden and distress (Lambert et al., 2012), emphasising the importance for nurses and other healthcare professionals to screen for distress and provide relevant interventions.
4.3. Emotional problems
Emotional problems accounted for more than half of the most frequently reported problems in caregivers with clinically significant levels of distress. Additionally, most caregivers in this sample (79%) reported one or more emotional problems. However, only self‐reporting a loss of interest in usual activities and sadness were significantly associated with increasing levels of distress. Tan et al. (2021) discuss the disruptive impact of cancer on established routines as a source of emotional distress for people with cancer and their caregivers. They assert that those affected by cancer can become emotionally distressed as they grieve the loss of previously established routines and life plans as they are forced to confront the reality of a cancer diagnosis. Therefore, the finding in this study that both a loss of interest in usual activities and sadness were significantly associated with an increase in caregiver's distress could be interpreted as the distressful impact resulting from facing a new reality where usual routines or activities are no longer feasible for both the person with cancer and their caregiver. This harmonises with Pearlin's model highlighting an individual experience with coping and the mechanisms they have in place to work through stressors in their life (Pearlin et al., 1990).
4.4. Sleep problems
The primary purpose of the PL is to help identify the potential sources of distress in patients with cancer (NCCN, 2021) and not necessarily their caregivers. Certain questions on the PL, particularly the 21 items regarding physical problems, likely pertained to the care recipient rather than the caregivers. Therefore, the result identifying sleep problems as a significant associate of severe distress should be interpreted cautiously, as it may not be the caregivers’ sleep problem that contributes to their level of distress, rather the sleep problems of their care recipient. In this study, approximately 41.4% of the caregiver sample reported sleep as a problem. Prior research has shown somatisation to be a problem among caregivers of people with cancer. For example, in Morris et al.’s (2015) caregiver sample, 62.9% reported sleep disturbance, with 32% reporting moderate to severe insomnia. In that study, they also determined that higher levels of distress were associated with sleep problems. Additionally, in Chambers et al. (2012), 17.7% of their caregiver sample and 33.5% of their patient sample showed symptoms of somatisation. In their study, sleep problems were significantly associated with increasing distress in cancer patients, but not their caregivers.
4.5. Familial problems
Both ‘problems dealing with partner’ and ‘problems dealing with children’ were factors significantly associated with increasing caregiver distress. This is understandable as the chronic and progressive nature of certain cancers and the anxiety of living with the risk of reoccurrence for those in remission, is likely to impact on family life and influence the need for caregivers to adapt to changing circumstances over time. This change can increase caregivers’ burden and feelings of distress, which are likely further intensified when also juggling child rearing, particularly among families with multiple children (Jabłoński et al., 2020). Among spousal caregivers, prior research has shown that caregivers who feel less socially, cognitively and emotionally supported by their care‐receiving spouses are significantly more likely to be clinically distressed (Goldzweig et al., 2019). Therefore, the ability to co‐create new ways of relating to one another within caregiver and family relationships in order to develop and maintain supportive and cohesive relationships is important (Arestedt et al., 2015). Additionally, given the interdependence between patient outcomes and caregiver outcomes, particularly in relation to emotional distress, dyadic supportive care interventions and dyadic coping models have been suggested as appropriate treatments (Badr et al., 2014).
4.6. Limitations
There was a high degree of missing data for certain demographic and clinical variables including race, cancer diagnosis and stage of disease. This prohibited the investigation of how these factors impacted on caregivers’ levels of distress. Of particular note was the inability to adjust for time since diagnosis, as previous research has shown that needs of caregivers decrease over time (Girgis et al., 2013). It has been posited in a previous study using the same data source (Hughes et al., 2011), that missingness may have been a result of helpline operators focusing on assisting the caller instead of data collection for research purposes, which may suggest the data were, at a minimum, missing at random.
5. RECOMMENDATIONS AND RELEVANCE TO PRACTICE
5.1. Research
If the DT and PL continue to be used for routine screening of distress, it is recommended that a re‐worded or tailored version be implemented for caregivers, as first suggested by Hughes et al. (2011). For example, noting ‘caregiver's problems’ or ‘patient's problems’ would help clarify to whom a specific physical problem is referring, and assist in secondary analyses of these type of data. Emerging evidence suggests that researchers are creating bespoke versions of the PL to address this issue (Oechsle et al., 2019), and this practice should be encouraged. In addition, better care should be taken to collect patient's type and stage of diagnosis during distress screening to allow for stratified analyses of caregivers’ distress across cancer subgroups or stages. Identifying discrete high‐distress subgroups across cancer type and stage would serve to inform clinicians on populations to target for prevention and management of distress.
5.2. Practice
The findings of this study support earlier work that also found high levels of emotional burden among the caregivers of people living with cancer (Fujinami et al., 2015; Palacio et al., 2018). This highlights the need to address both the source of distress and focus on better meeting caregivers’ needs to address the symptoms of distress.
The provision of clinical care and the focus of health and social care services are almost exclusively orientated to work with the person diagnosed with cancer, not the caregiver. The high levels of distress identified in this study suggest the need for services to encompass the caregiver. It is important that the distress experienced by caregivers is identified as early as possible in order to provide timely intervention and reduce suffering. The use of screening tools at planned and regular intervals across the illness journey could improve the detection and management of distress among caregivers. Additionally, the use of a brief measure, such as the DT and PL, to assess areas of concern and levels of distress over time among caregivers would provide a mechanism for caregivers to identify areas they recognise as important and impacting on their mental health. The measure of distress over time would also create the opportunity to identify strengths among caregivers in order to support and build resilience (Palacio et al., 2020).
6. CONCLUSION
Consistent with Pearlin's stress process model, developing caregiver/family‐centred approaches (social support) to managing distress could make a significant contribution to supporting the broader family unit and improve overall health and well‐being. Incorporating education into clinical and primary healthcare visits to promote awareness of the symptoms of distress and the experience among caregivers could significantly enhance the ability of caregivers to adapt to the changes experienced when affected by cancer. Additionally, developing pathways and tools that are easily accessible and provide community resources may help caregivers navigate the complexities of the healthcare system and find information to manage distress. For example, within the WA setting in which these data were captured, using a mobile application such as the one created by Walker et al. (2015), items identified on the DT PL can be linked to community resources to assist patients, caregivers and providers in finding medical, spiritual, psychosocial and financial information.
CONFLICT OF INTEREST
The author declares that there is no conflict of interest.
AUTHOR CONTRIBUTIONS
All authors were involved with the conceptualisation and design of this project. Data collection and extraction were handled by CCWA. Study methodology, data analysis and interpretation were primarily handled by Istvan Kabdebo, and reviewed and interpreted by Deborah L. Kirk and Lisa Whitehead. All authors were involved with drafting, critical revision and approval of the final version of the manuscript.
Supporting information
Data S1
Supplementary Material
ACKNOWLEDGEMENTS
We thank Cancer Council Western Australia for supplying their Information and Support Line data. We also thank Louise Good and Perry Swanborough for data extraction and facilitation of the project, and Dr. Mark Jenkins and Sue Robinson for their assistance with data preparation.
Kirk, D. L. , Kabdebo, I. , & Whitehead, L. (2022). Prevalence of distress and its associated factors among caregivers of people diagnosed with cancer: A cross‐sectional study. Journal of Clinical Nursing, 31, 3402–3413. 10.1111/jocn.16167
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- Anastasiadou, D. , Medina‐Pradas, C. , Sepulveda, A. R. , & Treasure, J. (2014). A systematic review of family caregiving in eating disorders. Eating Behaviors, 15(3), 464–477. 10.1016/j.eatbeh.2014.06.001 [DOI] [PubMed] [Google Scholar]
- Arestedt, L. , Benzein, E. , & Persson, C. (2015). Families living with chronic illness: Beliefs about illness, family, and health care. Journal of Family Nursing, 21, 206–231. 10.1177/1074840715576794 [DOI] [PubMed] [Google Scholar]
- Australian Bureau of Statistics . (2018). Socio‐economic indexes for areas (SEIFA) 2016. Census, (March). Retrieved from https://www.ausstats.abs.gov.au/ausstats/subscriber.nsf/0/756EE3DBEFA869EFCA258259000BA746/$File/SEIFA%202016%20Technical%20Paper.pdf
- Australian Bureau of Statistics . (2019). Disability, ageing and carers, Australia: Summary of findings, 2018. https://www.abs.gov.au/statistics/health/disability/disability‐ageing‐and‐carers‐australia‐summary‐findings/latest‐release [Google Scholar]
- Australian Bureau of Statistics . (2020). Australian statistical geography standard (ASGS): Volume 5 ‐ Remoteness structure. July 2016. https://www.abs.gov.au/ausstats/abs@.nsf/mf/1270.0.55.005?OpenDocument [Google Scholar]
- Badr, H. , Gupta, V. , Sikora, A. , & Posner, M. (2014). Psychological distress in patients and caregivers over the course of radiotherapy for head and neck cancer. Oral Oncology, 50(10), 1005–1011. 10.1016/j.oraloncology.2014.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barker, E. T. , Greenberg, J. S. , Seltzer, M. M. , & Almeida, D. M. (2012). Daily stress and cortisol patterns in parents of adult children with a serious mental illness. Health Psychology, 31(1), 130–134. 10.1037/a0025325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bray, F. , Laversanne, M. , Weiderpass, E. , & Soerjomataram, I. (2021). The ever‐increasing importance of cancer as a leading cause of premature death worldwide. Cancer, 127(16), 3029–3030. 10.1002/cncr.33587 [DOI] [PubMed] [Google Scholar]
- Bultz, B. D. , & Carlson, L. E. (2006). Emotional distress: The sixth vital sign ‐ future directions in cancer care. Psycho‐Oncology, 15, 93–95. 10.1002/pon.1022 [DOI] [PubMed] [Google Scholar]
- Cancer Council . (2020a). Caring for someone with cancer ‐ A guide for family and friends who provide care and support. https://www.cancercouncil.com.au/wp‐content/uploads/2021/05/Caring‐for‐Someone‐with‐Cancer‐2020.pdf [Google Scholar]
- Cancer Council . (2020b) Support services [Internet]. https://www.cancer.org.au/support‐and‐services/cancer‐council‐13‐11‐20
- Cancer Council Western Australia . (2020a). Cancer council information and support line. https://www.cancerwa.asn.au/patients/13‐11‐20‐information‐and‐support‐line/
- Cancer Council Western Australia . (2020b). Regional WA services. https://www.cancerwa.asn.au/patients/support‐and‐services/living‐in‐the‐country/
- Carlson, L. E. , Zelinski, E. L. , Toivonen, K. I. , Sundstrom, L. , Jobin, C. T. , Damaskos, P. , & Zebrack, B. (2019). Prevalence of psychosocial distress in cancer patients across 55 North American cancer centers. Journal of Psychosocial Oncology, 37(1), 5–21. 10.1080/07347332.2018.1521490 [DOI] [PubMed] [Google Scholar]
- Chambers, S. K. , Girgis, A. , Occhipinti, S. , Hutchison, S. , Turner, J. , Morris, B. , & Dunn, J. (2012). Psychological distress and unmet supportive care needs in cancer patients and carers who contact cancer helplines. European Journal of Cancer Care, 21(2), 213–223. 10.1111/j.1365-2354.2011.01288.x [DOI] [PubMed] [Google Scholar]
- Coomber, K. , & King, R. M. (2012). Coping strategies and social support as predictors and mediators of eating disorder carer burden and psychological distress. Social Psychiatry and Psychiatric Epidemiology, 47(5), 789–796. [DOI] [PubMed] [Google Scholar]
- De Laurentis, M. , Rossana, B. , Andrea, B. , Riccardo, T. , & Valentina, I. (2019). The impact of social‐emotional context in chronic cancer pain: Patient‐caregiver reverberations: Social‐emotional context in chronic cancer pain. Supportive Care in Cancer, 27(2), 705–713. 10.1007/s00520-018-4530-5 [DOI] [PubMed] [Google Scholar]
- Decadt, I. , Laenen, A. , Celus, J. , Geyskens, S. , Vansteenlandt, H. , & Coolbrandt, A. (2021). Caregiver distress and quality of life in primary caregivers of oncology patients in active treatment and follow‐up. European Journal of Cancer Care, 30(3), 1–11. 10.1111/ecc.13399 [DOI] [PubMed] [Google Scholar]
- Downer, R. G. (2018). Using your FREQ effectively: Displays for deciphering proportional odds in ordinal regression. Retrieved from https://www.mwsug.org/proceedings/2018/SP/MWSUG‐2018‐SP‐54.pdf
- Fennell, K. M. , Heckel, L. , Wilson, C. , Byrnes, M. , & Livingston, P. M. (2016). How calls from carers, friends and family members of someone affected by cancer differ from those made by people diagnosed with cancer; analysis of 4 years of South Australian Cancer Council Helpline data. Supportive Care in Cancer, 24(6), 2611–2618. 10.1007/s00520-015-3069- [DOI] [PubMed] [Google Scholar]
- Ferlay, J. , Ervik, M. , Lam, F. , Colombet, M. , Mery, L. , Piñeros, M. , Znaor, A. , Soerjomataram, I. , Bray, F. (2020). Global cancer observatory: Cancer today. International Agency for Research on Cancer. Available from https://gco.iarc.fr/today [Google Scholar]
- Fujinami, R. , Sun, V. , Zachariah, F. , Uman, G. , Grant, M. , & Ferrell, B. (2015). Family caregivers’ distress levels related to quality of life, burden, and preparedness. Psycho‐Oncology, 24(1), 54–62. 10.1002/pon.3562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- George, E. S. , Kecmanovic, M. , Meade, T. , & Kolt, G. S. (2020). Psychological distress among carers and the moderating effects of social support. BMC Psychiatry, 20, 154. 10.1186/s12888-020-02571-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gessler, S. , Low, J. , Daniells, E. , Williams, R. , Brough, V. , Tookman, A. , & Jones, L. (2008). Screening for distress in cancer patients: Is the distress thermometer a valid measure in the UK and does it measure change over time? A prospective validation study. Psycho‐Oncology, 17, 538–547. 10.1002/pon.1273 [DOI] [PubMed] [Google Scholar]
- Giordano, A. , Cimino, V. , Campanella, A. , Morone, G. , Fusco, A. , Farinotti, M. , Palmisano, L. , Confalonieri, P. , Lugaresi, A. , Grasso, M. G. , Ponzio, M. , Veronese, S. , Patti, F. , & Solari, A. (2016). Low quality of life and psychological wellbeing contrast with moderate perceived burden in carers of people with severe multiple sclerosis. Journal of the Neurological Sciences, 366, 139–145. 10.1016/j.jns.2016.05.016 [DOI] [PubMed] [Google Scholar]
- Girgis, A. , Lambert, S. D. , McElduff, P. , Bonevski, B. , Lecathelinais, C. , Boyes, A. , & Stacey, F. (2013). Some things change, some things stay the same: A longitudinal analysis of cancer caregivers’ unmet supportive care needs. Psycho‐Oncology, 22(7), 1557–1564. 10.1002/pon.3166 [DOI] [PubMed] [Google Scholar]
- Girgis, A. , Levesque, J. V. , Smith, A. , Durcinoska, I. , & Gerges, M. (2017). The role and supportive care needs of the partners and carers of women with breast cancer. Cancer Forum, 41(1), 67–74. [Google Scholar]
- Goldzweig, G. , Schapira, L. , Baider, L. , Jacobs, J. M. , Andritsch, E. , & Rottenberg, Y. (2019). Who will care for the caregiver? Distress and depression among spousal caregivers of older patients undergoing treatment for cancer. Supportive Care in Cancer, 27(11), 4221–4227. 10.1007/s00520-019-04711-6 [DOI] [PubMed] [Google Scholar]
- Hagedoorn, M. , Sanderman, R. , Bolks, H. N. , Tuinstra, J. , & Coyne, J. C. (2008). Distress in couples coping with cancer: A meta‐analysis and critical review of role and gender effects. Psychological Bulletin, 134(1), 1–30. 10.1037/0033-2909.134.1.1 [DOI] [PubMed] [Google Scholar]
- Halkett, G. K. B. , Lobb, E. A. , Shaw, T. , Sinclair, M. M. , Miller, L. , Hovey, E. , & Nowak, A. K. (2017). Distress and psychological morbidity do not reduce over time in carers of patients with high‐grade glioma. Supportive Care in Cancer, 25, 887–893. 10.1007/s00520-016-3478-6 [DOI] [PubMed] [Google Scholar]
- Halkett, G. K. B. , Lobb, E. A. , Shaw, T. , Sinclair, M. M. , Miller, L. , Hovey, E. , & Nowak, A. K. (2018). Do carer’s levels of unmet needs change over time when caring for patients diagnosed with high‐grade glioma and how are these needs correlated with distress? Supportive Care in Cancer, 26(1), 275–286. 10.1007/s00520-017-3846-x [DOI] [PubMed] [Google Scholar]
- Hawkes, A. L. , Hughes, K. L. , Hutchison, S. D. , & Chambers, S. K. (2010). Feasibility of brief psychological distress screening by a community‐based telephone helpline for cancer patients and carers. BMC Cancer, 10, 14. 10.1186/1471-2407-10-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heckel, L. , Fennell, K. M. , Orellana, L. , Boltong, A. , Byrnes, M. , & Livingston, P. M. (2018). A telephone outcall program to support caregivers of people diagnosed with cancer: Utility, changes in levels of distress, and unmet needs. Supportive Care in Cancer, 26(11), 3789–3799. 10.1007/s00520-018-4246-6 [DOI] [PubMed] [Google Scholar]
- Hughes, K. L. , Sargeant, H. , & Hawkes, A. L. (2011). Acceptability of the distress thermometer and problem list to community‐based telephone cancer helpline operators, and to cancer patients and carers. BMC Cancer, 11, 46. 10.1186/1471-2407-11-46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jabłoński, M. J. , García‐Torres, F. , Zielińska, P. , Bułat, A. , & Brandys, P. (2020). Emotional burden and perceived social support in male partners of women with cancer. International Journal of Environmental Research and Public Health, 17(12), 1–12. 10.3390/ijerph17124188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janda, M. , Neale, R. E. , Klein, K. , O’Connell, D. L. , Gooden, H. , Goldstein, D. , Merrett, N. D. , Wyld, D. K. , Rowlands, I. J. , & Beesley, V. L. (2017). Anxiety, depression and quality of life in people with pancreatic cancer and their carers. Pancreatology, 17(2), 321–327. 10.1016/j.pan.2017.01.008 [DOI] [PubMed] [Google Scholar]
- Kirk, D. L. , Kabdebo, I. T. , & Whitehead, L. (2021). Prevalence of distress, its associated factors and referral to support services in people with cancer. Journal of Clinical Nursing, 30(19‐20), 2873–2885. 10.1111/jocn.15794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambert, S. D. , Harrison, J. D. , Smith, E. , Bonevski, B. , Carey, M. , Lawsin, C. , Paul, C. , & Girgis, A. (2012). The unmet needs of partners and caregivers of adults diagnosed with cancer: a systematic review. BMJ Supportive & Palliative Care, 2(3), 224–230. 10.1136/bmjspcare-2012-000226 [DOI] [PubMed] [Google Scholar]
- Long, A. , Halkett, G. K. B. , Lobb, E. A. , Shaw, T. , Hovey, E. , & Nowak, A. K. (2016). Carers of patients with high‐grade glioma report high levels of distress, unmet needs, and psychological morbidity during patient chemoradiotherapy. Neuro‐Oncology Practice, 3(2), 105–112. 10.1093/nop/npv039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meiland, F. J. M. , Kat, M. G. , van Tilburg, W. , Jonker, C. , & Dröes, R.‐M. (2005). The emotional impact of psychiatric symptoms in dementia on partner caregivers: Dementia on partner caregivers. Alzheimer Disease and Associated Disorders, 19(4), 195–201. 10.1097/01.wad.0000189035.25277.02 [DOI] [PubMed] [Google Scholar]
- Mejdahl, M. K. , Mertz, B. G. , Bidstrup, P. E. , & Anderson, K. G. (2015). Preoperative distress predicts persistent pain after breast cancer treatment: A prospective cohort study. Journal of the National Comprehensive Cancer Network, 13(8), 995–1003. 10.6004/jnccn.2015.0120 [DOI] [PubMed] [Google Scholar]
- Morris, B. A. , Thorndike, F. P. , Ritterband, L. M. , Glozier, N. , Dunn, J. , & Chambers, S. K. (2015). Sleep disturbance in cancer patients and caregivers who contact telephone‐based help services. Supportive Care in Cancer, 23(4), 1113–1120. 10.1007/s00520-014-2458-y [DOI] [PubMed] [Google Scholar]
- Mosher, C. E. , Adams, R. N. , Helft, P. R. , O’Neil, B. H. , Shahda, S. , Rattray, N. A. , & Champion, V. L. (2017). Positive changes among patients with advanced colorectal cancer and their family caregivers: A qualitative analysis. Psychology Health, 32(1), 94–109. 10.1080/08870446.2016.1247839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulud, Z. A. , & McCarthy, G. (2017). Caregiver burden among caregivers of individuals with severe mental illness: Testing the moderation and mediation models of resilience. Archives of Psychiatric Nursing, 31(1), 24–30. 10.1016/j.apnu.2016.07.019 [DOI] [PubMed] [Google Scholar]
- National Comprehensive Cancer Network. (2021). NCCN clinical practice guidelines in oncology (NCCN guidelines) distress management. Version 2.2021. https://www.nccn.org/professionals/physician_gls/pdf/distress.pdf [DOI] [PMC free article] [PubMed]
- Nicholas, D. R. (2000). Men, masculinity, and cancer: Risk‐factor behaviors, early detection, and psychosocial adaptation. Journal of the American College Health Association, 49(1), 27–33. 10.1080/07448480009596279 [DOI] [PubMed] [Google Scholar]
- Nipp, R. D. , El‐Jawahri, A. , Fishbein, J. N. , Gallagher, E. R. , Stagl, J. M. , Park, E. R. , Jackson, V. A. , Pirl, W. F. , Greer, J. A. , & Temel, J. S. (2016). Factors associated with depression and anxiety symptoms in family caregivers of patients with incurable cancer. Annals Oncology, 27(8), 1607–1612. 10.1093/annonc/mdw205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oberoi, D. V. , White, V. , Jefford, M. , Giles, G. G. , Bolton, D. , Davis, I. , Winship, I. , Prince, H. M. , Millar, J. , Harrison, S. , Kay, A. , & Hill, D. (2016). Caregivers’ information needs and their ‘experiences of care’ during treatment are associated with elevated anxiety and depression: A cross‐sectional study of the caregivers of renal cancer survivors. Supportive Care Cancer, 24(10), 4177–4186. 10.1007/s00520-016-3245-8 [DOI] [PubMed] [Google Scholar]
- Oechsle, K. , Ullrich, A. , Marx, G. , Benze, G. , Heine, J. , Dickel, L.‐M. , Zhang, Y. , Wowretzko, F. , Wendt, K. N. , Nauck, F. , Bokemeyer, C. , & Bergelt, C. (2019). Psychological burden in family caregivers of patients with advanced cancer at initiation of specialist inpatient palliative care. BMC Palliative Care, 18(1), 1–14. 10.1186/s12904-019-0469-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palacio, C. , Krikorian, A. , & Limonero, J. T. (2018). The influence of psychological factors on the burden of caregivers of patients with advanced cancer: Resiliency and caregiver burden. Palliative and Supportive Care, 16, 269–317. 10.1017/S1478951517000268 [DOI] [PubMed] [Google Scholar]
- Palacio G, C. , Krikorian, A. , Gómez‐Romero, M. J. , & Limonero, J. T. (2020). Resilience in caregivers: A systematic review. American Journal of Hospice and Palliative Medicine, 2020(37), 648–658. 10.1177/1049909119893977 [DOI] [PubMed] [Google Scholar]
- PDQ Supportive and Palliative Care Editorial Board. (2021). PDQ informal caregivers in cancer. PDQ cancer information summaries. http://www.ncbi.nlm.nih.gov/pubmed/26389284
- Pearlin, L. I. , Menaghan, E. G. , Lieberman, M. A. , & Mullan, J. T. (1981). The stress process. Journal of Health and Social Behavior, 22(4), 337–356. 10.2307/2136676 [DOI] [PubMed] [Google Scholar]
- Pearlin, L. I. , Mullan, J. T. , Semple, S. J. , & Skaff, M. M. (1990). Caregiving and the stress process: An overview of concepts and their measures. The Gerontologist, 30(5), 583–594. 10.1093/geront/30.5.583 [DOI] [PubMed] [Google Scholar]
- Peterson, B. , & Harrell, F. E. Jr (1990). Partial proportional odds models for ordinal response variables. Journal of the Royal Statistical Society, 39(2), 205–217. [Google Scholar]
- Pinquart, M. , & Sörensen, S. (2003). Differences between caregivers and noncaregivers in psychological health and physical health: A meta‐analysis. Psychology and Aging, 18(2), 250–267. 10.1037/0882-7974.18.2.250 [DOI] [PubMed] [Google Scholar]
- Pristavec, T. (2019). The caregiving dyad: Do caregivers’ appraisals of caregiving matter for care recipients’ health? Archives of Gerontology and Geriatrics, 82, 50–60. 10.1016/j.archger.2019.01.020 [DOI] [PubMed] [Google Scholar]
- Shaffer, K. M. , Benvengo, S. , Zaleta, A. K. , Levine, M. , Bellantoni, C. , Dannaoui, A. , Buzaglo, J. S. , & Applebaum, A. J. (2019). Distress screening is feasible and acceptable for family caregivers at an oncological surgical center: Evidence from a mix‐methods feasibility study. Oncology Nursing Forum, 46(2), 159–169. 10.1188/19.ONF.159-169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah, A. J. , Wadoo, O. , & Latoo, J. (2010). Psychological distress in carers of people with mental disorders. British Journal of Medical Practitioners, 3(3), 18–25. [Google Scholar]
- Springate, B. A. , & Tremont, G. (2014). Dimensions of caregiver burden in dementia: Impact of demographic, mood, and care recipient variables. American Journal of Geriatric Psychiatry, 22(3), 294–300. 10.1016/j.jagp.2012.09.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sung, H. , Ferlay, J. , Siegel, R. L. , Laversanne, M. , Soerjomataram, I. , Jemal, A. , & Bray, F. (2021). Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer Journal for Clinicians, 71(3), 209–249. 10.3322/caac.21660 [DOI] [PubMed] [Google Scholar]
- Swinkels, J. C. , Broese van Groenou, M. I., de Boer, A. & Tilburg, T. G. (2018). Male and female partner‐caregivers’ burden: Does it get worse over time? The Gerontologist, 59(6), 1103–1111. [DOI] [PubMed] [Google Scholar]
- Tan, J. H. , Sharpe, L. , & Russell, H. (2021). The impact of ovarian cancer on individuals and their caregivers: A qualitative analysis. Psycho‐Oncology, 30(2), 212–220. 10.1002/pon.5551 [DOI] [PubMed] [Google Scholar]
- Tanco, K. , Park, J. C. , Cerana, A. , Sisson, A. , Sobti, N. , & Bruera, E. (2017). A systematic review of instruments assessing dimensions of distress among caregivers of adult and pediatric cancer patients. Palliative and Supportive Care, 15, 110–124. 10.1017/S1478951516000079 [DOI] [PubMed] [Google Scholar]
- Taylor, J. , Fradgley, E. , Clinton‐McHarg, T. , Byrnes, E. , & Paul, C. (2020). What are the sources of distress in a range of cancer caregivers? A qualitative study. Supportive Care in Cancer, 29(5), 2443–2453. 10.1007/s00520-020-05742-0 [DOI] [PubMed] [Google Scholar]
- Von Ah, D. , Spath, M. , Nielsen, A. , & Fife, B. (2016). The caregiver’s role across the bone marrow transplantation trajectory. Cancer Nursing, 39(1), E12–E19. 10.1097/NCC.0000000000000242 [DOI] [PubMed] [Google Scholar]
- Von Elm, E. , Altman, D. G. , Egger, M. , Pocock, S. J. , Gøtzsche, P. C. , & Vandenbroucke, J. P. (2007). The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Epidemiology, 18(6), 800–804. 10.1097/EDE.0b013e3181577654 [DOI] [PubMed] [Google Scholar]
- Walker, D. K. , Hardeman, A. , Owen, L. , & Frank, J. (2015). Information at the point of care: An informational application for cancer resources. Computers, Informatics, Nursing, 33(9), 390–395. 10.1097/CIN.0000000000000171 [DOI] [PubMed] [Google Scholar]
- Watts, K. J. , Good, L. H. , McKiernan, S. , Miller, L. , O’Connor, M. , Kane, R. , Kruger, D. J. , Adams, B. R. , & Musiello, T. (2016). “Undressing” distress among cancer patients living in urban, regional, and remote locations in Western Australia. Supportive Care in Cancer, 24(5), 1963–1973. 10.1007/s00520-015-2982-4 [DOI] [PubMed] [Google Scholar]
- World Health Organisation . (2016). International classification of diseases codes ‐ (ICD 10). Version 2016. https://icd.who.int/browse10/2016/en
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1
Supplementary Material
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


