Abstract
Background
Games are increasingly being used as a means of alleviating pain and anxiety in paediatric patients, in the view that this form of distraction is effective, non‐invasive and non‐pharmacological.
Aims
To determine whether a game‐based intervention (via gamification or virtual reality) during the induction of anaesthesia reduces preoperative pain and anxiety in paediatric patients.
Methods
A systematic review with meta‐analysis of randomised controlled trials was performed in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta‐Analyses) guidelines and using RevMan software. The review was based on a search of the EMBASE, CINAHL, Medline, SciELO and Scopus databases, conducted in July 2021. No restriction was placed on the year of publication.
Results
26 studies were found, with a total study population of 2525 children. Regarding pain reduction, no significant differences were reported. For anxiety during anaesthesia induction, however, a mean difference of −10.62 (95% CI −13.85, −7.39) on the Modified Yale Preoperative Anxiety Scale, in favour of game‐based intervention, was recorded.
Conclusions
Game‐based interventions alleviate preoperative anxiety during the induction of anaesthesia in children. This innovative and pleasurable approach can be helpful in the care of paediatric surgical patients.
Relevance to clinical practice
In children, preoperative management is a challenging task for healthcare professionals, and game‐based strategies could enhance results, improving patients’ emotional health and boosting post‐surgery recovery. Distractive games‐based procedures should be considered for incorporation in the pre‐surgery clinical workflow in order to optimise healthcare.
Keywords: anxiety, children, game, pain, perioperative care, virtual reality
What does this paper contribute to the wider global clinical community?
Game‐based distraction is an effective non‐pharmacological resource in paediatric preoperative care.
Such interventions reduce preoperative anxiety levels in children undergoing painful procedures.
This innovative and pleasurable approach can enhance the care of paediatric surgical patients during the induction of anaesthesia.
1. INTRODUCTION
Surgery is often a highly stressful experience for children, during which the induction of anaesthesia is a critical period (Kain et al., 2006; Walther‐Larsen et al., 2016). At this time, up to 30% of children experience moderate to severe levels of pain and up to 60%, high levels of anxiety (Gates et al., 2020; Perrott et al., 2018). Preoperative anxiety begins when the patient first learns of the need for surgery and can peak at any moment before the actual surgery (Fortier et al., 2010). Furthermore, apprehension regarding the surgical intervention may be heightened by related factors, such as an unfamiliar environment, separation from parents or the fear of needles or other procedures (Drasković et al., 2015).
1.1. Background
Intense anxiety can affect children's physical and psychological health, provoke adverse postoperative outcomes that delay recovery and rehabilitation, and negatively affect a child's cooperation in self‐care (Drasković et al., 2015; Fortier et al., 2011). Up to 20% of children undergoing surgery may present signs of stress and psychological pressure (delirium and negative behavioural changes), which in some cases persist for months after surgery (Aytekin et al., 2016; Beringer et al., 2014). In addition, preoperative anxiety is associated with higher levels of postoperative pain (Caumo et al., 2000), and may even triple the consumption of analgesics (Wollin et al., 2003).
Both pharmacological and non‐pharmacological treatments can be used to combat preoperative anxiety and pain (Manyande et al., 2015; Perry et al., 2012). The approach most commonly adopted is that of premedication, but this frequently has adverse effects such as nausea and vomiting. Sedatives, too, can have undesirable consequences, sometimes producing delirium, agitation or even pain (Manyande et al., 2015). However, an alternative approach is available, in the form of non‐pharmacological interventions based on pleasurable activities such as music, painting, games, movies, tablet apps, video games or virtual reality (Gómez‐Urquiza et al., 2016; Manyande et al., 2015).
Game‐based interventions (via gamification or virtual reality) can provide distraction and effectively complement traditional pain and anxiety‐reducing methods (Alqudimat et al., 2021). This non‐pharmacological approach can enhance social and communication skills, help project fears, feelings and emotions and foster cooperation with health professionals during medical procedures (Lestari et al., 2017).
Some recent studies in this context have focused on game‐based learning, or ‘serious games’, that include game mechanics aimed at helping children and parents cope with the preparation for a surgical intervention (Vrancken et al., 2021). Other researchers have conducted systematic reviews to investigate the clinical application of virtual reality to reduce anxiety in paediatric and burn patients (Ang et al., 2021) or during dentistry (Cunningham et al., 2021). Similarly, immersive technologies have been used to alleviate anxiety and assist chronic pain management in adolescents (Alqudimat et al., 2021). Other studies have analysed the use of audio‐visual distraction techniques (based on cartoons, video clips, interactive games, virtual reality or humanoid robots) for children subjected to painful procedures such as venous access, cancer therapy or treatment for burns (Chen et al., 2020; Chow et al., 2016; Eijlers, Utens, et al., 2019; Gates et al., 2020; Gerçeker et al., 2020). The use of smart‐technology interventions, such as games or videos streamed from mobile phones or tablets, or immersive video headsets for paediatric patients, has also been investigated (Rantala et al., 2020).
The use of games‐based and audio‐visual interventions as distractive resources is a new concept that could effectively reduce perioperative pain and anxiety. However, the effect produced in a preoperative setting remains controversial. Some studies have focused on the effect of non‐pharmacological interventions on children during the preoperative period (Caruso et al., 2020; Won et al., 2017), and meta‐analyses have been conducted of virtual reality interventions, although not specifically focused on children (Kenney & Milling, 2016). Nevertheless, to the best of our knowledge, no previous studies have been undertaken to analyse the specific effect produced by these novel interventions during the induction of anaesthesia, with respect to the possible alleviation of pain and/or anxiety.
Although game‐based interventions are increasingly being employed in the preoperative period for children, their development and adaptation to different settings and types of surgery are still a challenging problem. In our opinion, an analysis of randomised clinical trials conducted in different settings would provide valuable evidence of the effects of game‐based interventions in this context.
2. AIM
The objective of this systematic review and meta‐analysis is to determine the effect of game‐based interventions (via gamification or virtual reality) during the induction of anaesthesia to reduce pain and anxiety in paediatric patients.
3. METHODS
3.1. Design
This systematic review and meta‐analysis were performed following the PRISMA recommendations (Page et al., 2021). The study is registered in the PROSPERO database (International Prospective Register of Systematic Reviews) with number CRD42021270072.
3.2. Search strategy
The following databases were consulted: EMBASE (Ovid), CINAHL (Ebsco), Medline (Ovid), SciELO (BIREME Virtual Health Library) and Scopus (Elsevier). Grey literature was also consulted, but no relevant studies were found. The Mesh terms employed in the search strategy were ‘(game OR gamification OR virtual reality) AND (preoperative OR perioperative) AND (anxiety OR pain) AND child*’. The search was conducted in July 2021 in accordance with the PICOS (Population, Intervention, Comparison, Outcome and Study) strategy (see Table 1). The search question was as follows: What effect does a game‐based intervention programme have on the pain and anxiety felt during anaesthesia induction by children aged up to 12 years?
TABLE 1.
PICOS search strategy
| Participants | Intervention | Comparison | Outcomes | Study |
|---|---|---|---|---|
| Children (up to 12 years of age) | Interactive game, gamification or virtual game before surgery | Control group (traditional intervention, usual medication, no distraction aids or other intervention) |
Anxiety Pain |
Randomised controlled trials |
3.3. Search outcomes
Articles meeting the following criteria were included: (1) randomised controlled trials; (2) sample composed exclusively of children; (3) evaluation of an intervention compared with a control group; (4) game, gamification or virtual reality‐based intervention; (5) analysis of the impact of the intervention on pain and anxiety levels, measured before and at the time of anaesthesia induction (with no time restriction on time before induction) and (6) use of a validated measurement tool (Table 2). No restriction was placed on the language or year of publication.
TABLE 2.
Characteristics of the included studies (n = 26)
| Author, year, country | Design | Sample | Aim | Intervention a | Surgery | Anxiety and pain measured |
Results M (SD)/median (IQR) |
EL/RG |
|---|---|---|---|---|---|---|---|---|
| Al‐Nerabieah et al. (2020), Syria | RCT |
N = 64 Age 6–10 years n CG = 32 n IG = 32 |
To evaluate VR glasses in the dental waiting room |
CG: no intervention IG: a cartoon shows through VR eyeglasses in the waiting room (5 min play) Time before anaesthesia 20 min |
Dental surgery |
mYPAS‐SF WBFPRS |
Baseline mYPAS‐SF CG: 57.02 (7.53) IG: 37.31 (15.39) Induction mYPAS‐SF CG: 78.96 (8.24) IG: 45.89 (12.96) p ≤ .001 WBFPRS CG: 4.09 (0.85) IG: 1.56 (1.16) p ≤ .001 |
1b/A |
| Buffel et al. (2019), Belgium | RCT |
N = 20 Age 6–10 years n CG = 8 n IG = 12 |
To evaluate perioperative anxiety |
CG: no intervention IG: a serious game‐CliniPup® (2 days play prior to surgery) |
Ambulatory surgery (dental and ENT) | mYPAS |
Induction CG: 51.88 (15.57) IG: 31.67 (7.79) p = .01 |
1b/A |
| Buyuk et al. (2021), Turkey | RCT |
N = 78 Age 5–10 years n CG = 38 n IG = 40 |
To examine the effects of VR intervention on anxiety levels |
CG: no intervention IG: VR glasses (5 min play) |
Circumcision | CAM‐S | VR interventions were effective in reducing anxiety in the preoperative period | 1b/A |
| Chaurasia et al. (2019), India | RCT |
N = 80 Age 4–8 years n CG = 40 n IG = 40 |
To evaluate the efficacy of an incentive‐based game therapy in reducing preoperative anxiety |
CG: no intervention IG: incentive‐based game Time before anaesthesia 1 day |
Elective surgery (ophthalmology, urology, orthopaedic, general) | mYPAS |
Baseline CG: 27.1 (3.4) IG: 26.6 (3.5) Induction CG: 52.6 (11.4) IG: 32.4 (6.5) p < .001 |
1b/A |
| Clausen et al. (2021), Denmark | RCT |
N = 60 Age 3–6 years n CG = 30 n IG = 30 |
To evaluate anxiety level after a game on a tablet computer |
CG: no intervention IG: game on a tablet computer Time before anaesthesia 20 min |
Elective minor (abdominal and urologic surgery) | mYPAS |
Baseline CG: 39.0 (2.3) IG: 39.2 (3.0) Induction CG: 65.8 (3.4) IG: 55.7 (4.2) [95% CI, −0.63 to 20.8; p = .066] |
1b/A |
| Dehghan et al. (2019), Iran | RCT |
N = 40 Age 6–12 years n CG = 20 n IG = 20 |
To investigate the effect of VR technology on preoperative anxiety |
CG: no intervention IG: VR (5 min play) |
Abdominal surgery | YPAS | Intervention showed significant reduction in the preoperative anxiety score after therapeutic exposure using VR | 1b/A |
| Dwairej et al. (2020), Jordan | RCT |
N = 128 Age 5–11 years n CG = 64 n IG = 64 |
To evaluate the effectiveness of video game distraction on the preoperative anxiety |
CG: no intervention IG: videogame Time before anaesthesia 20 min |
Elective surgery (ENT, orthopaedic, dental, genital surgery) | mYPAS |
Baseline CG: 43.93 (12.04) IG: 43.49 (11.24) Induction CG: 63 (15.66) IG: 42.67 (13.91) p < .001 |
1b/A |
| Eijlers, Dierckx, et al. (2019), Netherlands | RCT |
N = 191 Age 4–12 years n CG = 97 n IG = 94 |
To investigate if VR exposure is associated with lower levels of anxiety |
CG: no intervention IG: VR (15 min play) Time before anaesthesia 30–60 min |
Elective maxillofacial, dental or ENT | mYPAS |
Baseline Median (IQR) CG: 26.7 [23.3–32.5] IG: 28.3 [23.3–31.7] Induction CG: 38.3 [28.3–53.3] IG: 40.0 [28.3–58.3] p = .862 |
1b/A |
| Forouzandeh et al. (2020), Iran | RCT |
N = 172 Age 3–12 years n CG = 53 n IG1 = 64 n IG2 = 55 |
To analyse the effect of interactive games and painting on preoperative anxiety |
CG: no intervention IG1: interactive games IG2: painting Time before anaesthesia 20–30 min |
Elective surgery | mYPAS |
Baseline CG: 57.45 (17.93) IG1: 57.72 (17.60) IG2: 50.76 (19.20) Induction CG: 56.50 (15.63) IG1: 49.91 (13.21) p < .001 IG2: 42.21 (15.86) p < .001 |
1b/A |
| Gao et al. (2014), China | RCT |
N = 59 Age 3–6 years n CG = 30 n IG = 29 |
To evaluate the effect of games on reducing preoperative anxiety |
CG: no intervention IG: cartoons game Time before anaesthesia 15–20 min |
Elective surgery | mYPAS |
Baseline CG: 30.43 (3.27) IG: 30.81 (3.64) Induction CG: 58.89 (13.39) IG: 51.32 (11.34) p = .023 |
1b/A |
| Hashimoto et al. (2020), Japan | RCT |
N = 58 Age 4–12 years n CG = 29 n IG = 29 |
To determine the anxiolytic effect during the preoperative period in children |
CG: portable multimedia player IG: VR glasses Time before anaesthesia 1 day |
Elective surgery (ENT, ophthalmology, plastic/dermatology, orthopaedic, oral, digestive) | mYPAS |
Induction CG: 33.3 [23.3–44.2] IG: 23.3 [23.3–25.0] p = .001 |
|
| Hosseinpour and Memarzadeh (2010), Iran | RCT |
N = 200 Mean age 4.33 years n CG = 100 n IG = 100 |
To evaluate the efficacy of a playroom next to the operating room to reduce preoperative anxiety |
CG: no intervention IG: cartoons game Time before anaesthesia 30 min |
Elective surgery | mYPAS | Preoperative anxiety was significantly decreased for all categories of the anxiety score as assessed by mYPAS questionnaire | 1b/A |
| Huntington et al. (2018), England | RCT |
N = 176 Age 5–7 years n CG = 59 n IG1 = 60 n IG2 = 57 |
To evaluate if games improved children's anxiety |
CG: no intervention IG1: video game IG2: placebo‐video |
Dental surgery |
mYPAS VAS‐anxiety |
Baseline mYPAS CG: 45.1 (20.5) IG1: 47.6 (22.2) IG2: 43.2 (20.7) Induction mYPAS CG: 45.1 (20.5) IG1: 47.6 (22.2) [OR 1.02, 95% CI 0.61 to 2.6, p = .97] IG2: 43.2 (20.7) [OR 1.38, 95% CI 0.87 to 3.81; p = .49] VAS CG: 3.5 (2.5) IG1: 3.5 (2.6) [OR 2.0, 95% CI −0.6 to 1.3 p = .42] IG2: 3.7 (2.4) [OR 1.53, 95% CI −0.8 to 1.1; p = .65] |
1b/A |
| Jung et al. (2021), USA | RCT |
N = 70 Age 5–12 years n CG = 37 n IG = 33 |
To evaluate VR to reduce preoperative anxiety |
CG: no intervention IG: VR (5 min play) |
Elective surgery | mYPAS |
Baseline Median (IQR) CG: 28.3 [23.3–28.3] IG: 28.3 [23.3–28.3] Induction CG: 45.0 [33.3–56.7] IG: 28.3 [23.3–33.3] p < .0001 |
1b/A |
| Lee et al. (2012), South Korea | RCT |
N = 130 Age 3–7 years n CG = 44 n IG1 = 44 n IG2 = 42 |
To determine the effects of gamification on preoperative anxiety in children |
CG: no intervention IG1: game IG2: cartoon |
Elective surgery (ENT, ophthalmology, orthopaedic) | mYPAS |
Baseline CG: 27.3 (8.4) IG1: 27.3 (7.6) IG2: 25.8 (4.2) Induction CG: 57.4 (18.1) IG1: 43.6 (16.1) p < .05 IG2: 31.8 (8.8) p < .05 |
1b/A |
| Marechal et al. (2017), France | RCT |
N = 115 Age 4–11 years n CG = 55 n IG = 60 |
To compare the effects of midazolam with tablet‐games for children anxiety |
CG: midazolam IG: tablet‐game Time before anaesthesia 20 min |
Ambulatory surgery (urology, ENT, orthopaedic, ophthalmology) | mYPAS |
Baseline CG: 37.1 (14.0) IG: 34.6 (13.6) Induction CG: 40.5 (18.6) IG: 41.8 (20.7) p = .99 |
1b/A |
| Matthyssens et al. (2020), Belgium | RCT |
N = 72 Age 5–11 years n CG = 25 n IG1 = 25 n IG2 = 22 |
To evaluate the effectiveness of the serious game on anxiety and pain |
CG: no intervention IG1: serious game‐CliniPup® IG2: empty game without educational information |
Ambulatory surgery (dental, ENT or urologic) | VAS‐anxiety and pain |
Baseline Anxiety CG: 4.5 IG1: 2.8 IG2: 2.5 Pain CG: 1.6 IG1: 0.5 IG2: 1.4 Induction Anxiety CG: 4.5 IG1: 1.9 p = .044 IG2: 2.7 Pain CG: 1.12 IG1: 0.4 p = .09 IG2: 1.1 |
1b/A |
| Park et al. (2019), South Korea | RCT |
N = 80 Age 4–10 years n CG = 40 n IG = 40 |
To evaluate the effect of VR on preoperative anxiety of children |
CG: VR video + parents watching the same video via the mirroring display IG: VR video (4 min) |
Elective surgery (ENT, ophthalmology, orthopaedic, dental) | mYPAS |
Baseline CG: 36.7 (23.3–47.5) IG: 32.5 (23.3–47.5) Induction CG: 38.3 (23.3–44.2) IG: 28.3 (23.3–36.7) p = .025 |
1b/A |
| Patel et al. (2006), USA | RCT |
N = 112 Age 4–12 years n CG =38 n IG1 = 38 n IG1 = 36 |
To evaluate the efficacy of a video game in reducing preoperative anxiety in children |
CG: midazolam IG1: parent presence + hand‐held video game IG2: parent presence |
Outpatient surgery | mYPAS |
Baseline CG: 45.2 (3.1) IG1: 37.4 (2.3) IG2: 34.3 (2.0) Induction CG: 53.9 (2.7) IG1: 41.7 (4.1) p = .04 IG2: 51.5 (4.0) |
1b/A |
| Rodriguez et al. (2019), USA | RCT |
N = 52 Age 4–10 years n CG = 25 n IG = 27 |
To determine if a large projection‐based video screen mounted to a patient's bed decreased anxiety when compared to a tablet |
CG: bedside entertainment and relaxation theatre IG: tablet game (1.17–7.64 min play) |
Outpatient surgery (ENT, plastics, urology, ophthalmology, orthopaedics, rheumatology, general) | mYPAS |
Baseline CG: 26.3 (6.5) IG: 25.5 (5.7) Induction CG: 35.0 (14.3) p = .001 IG: 30.6 (14.6) p = .037 |
1b/A |
| Ryu et al. (2019), South Korea | RCT |
N = 80 Age 4–10 years n CG = 39 n IG = 41 |
To evaluate whether gamification with VR gaming reduce preoperative anxiety in children |
CG: no intervention IG: VR (4 min play) |
Elective surgery (ENT, ophthalmology, orthopaedics, dental) | mYPAS |
Baseline CG: 51.7 (31.7–61.7) IG: 46.7 (32.5–55.9) Induction CG: 46.7 (33.3–63.3) IG: 38.3 (23.3–50.9) [Mean difference 95% CI 9.2 (0.3–18.2), p = .022] |
1b/A |
| Scarano et al. (2021), Italy | RCT |
N = 50 Age 4–12 years n CG = 25 n IG = 25 |
To evaluate how playing can help to reduce preoperative anxiety of children |
CG: no intervention IG: playing room Time before anaesthesia 30 min |
Elective surgery | mYPAS |
Baseline CG: 30.86 (16.57) IG: 25.12 (4.3) Induction CG: 43.45 (24.30) IG: 28.92 (9.32) p < .05 |
1b/A |
| Seiden et al. (2014), USA | RCT |
N = 108 Age 1–11 years n CG = 51 n IG = 57 |
To compare the effects of a tablet‐based interactive distraction tool on perioperative anxiety |
CG: midazolam IG: tablet‐game |
Outpatient surgery (ENT, urology, gastrointestinal, ophthalmology, gynaecologic, dental, orthopaedics, general) | mYPAS |
Baseline Median (IQR) CG: 28 (23–45) IG: 32 (23–45) Induction IG vs CG mean difference (95% CI) (favour intervention): −14.0 (−6.1 to −22.0), p < .001 |
1b/A |
| Stewart et al. (2019), USA | RCT |
N = 102 Age 4–12 years n CG = 51 n IG = 51 |
To compare effects of tablet‐based interactive distraction with oral midazolam on preoperative anxiety |
CG: midazolam IG: tablet‐game Time before anaesthesia 20 min |
Ambulatory surgery (urology, ENT, ophthalmology, general) | mYPAS‐SF |
Baseline CG: 24.4 (3.7) IG: 25.3 (5.0) Induction CG: 35.7 (16.4) IG: 28.6 (11.6) p < .001 |
1b/A |
| Ünver et al. (2020), Turkey | RCT |
N = 94 Age 7–12 years n CG = 47 n IG = 47 |
To determine the effect of a game intervention on the preoperative anxiety levels |
CG: no intervention IG: game Jenga® |
Elective minor surgery (circumcision, inguinal hernia repair) | VFAS |
Baseline CG: 1.48 (0.99) IG: 1.82 (1.27) Postintervention CG: 2.42 (1.13) IG: 0.70 (0.80) p < .001 |
1b/A |
| Uyar et al. (2020), Turkey | RCT |
N = 134 Age 5–8 years n CG = 46 n IG1 = 43 n IG2 = 45 |
To analyse the change in children's anxiety levels |
CG: midazolam IG1: playing a videogame IG2: watch cartoon Time before anaesthesia 20 min |
Elective surgery (ENT) | mYPAS |
Baseline CG: 40.7 IG1: 40.7 IG2: 42.6 Induction CG: 38.3 IG1: 39.5 IG2: 43.7 p = .224 |
1b/A |
Abbreviations: CAM‐S, Children's Anxiety metre scale; CG, Control group; EL, Evidence level; ENT, Ears, Nose and Throat surgery; IG, Intervention group; IQR, Interquartile range; mYPAS, Modified Yale Preoperative Anxiety Scale; mYPAS‐SF, Modified Yale Preoperative Anxiety Scale‐Short Form; RG, Recommendation grade; VAS, Visual analogue scale; VFAS, Visual Facial Anxiety Scale; VR, Virtual reality; WBFPRS, Wong–Baker Faces Pain Rating Scale; YPAS, Yale Preoperative Anxiety Scale questionnaire.
No intervention = no distraction aids or usual medication.
The following types of study were excluded: (1) protocol studies; (2) studies without randomisation and a control group; (3) studies with an adult sample and (4) studies including a non‐games‐based intervention.
The studies were selected for inclusion by two independent reviewers, according to the following process: first, the studies were assessed by title and abstract against the eligibility criteria, after which a full‐text assessment was performed (see Figure 1). If the reviewers disagreed, a third reviewer was requested to make the final decision.
FIGURE 1.

Flow diagram of the publication search process [Colour figure can be viewed at wileyonlinelibrary.com]
3.4. Quality appraisal
For quality assessment of randomised controlled trials, the levels of evidence and grades of recommendation stipulated by the OCEBM (Oxford Centre for Evidence‐Based Medicine) were used (Howick et al., 2011; see Table 2). The risk of bias was analysed using the ‘Risk of Bias Assessment’ (RoB 2.0; Sterne et al., 2019). The risk of bias and quality of evidence assessment were performed independently and in duplicates by two reviewers.
3.5. Data extraction
All data were extracted and collated in a spreadsheet by two of the authors. In case of disagreement, a third author reviewed this process. For each of the studies found, the following variables were obtained: (1) author, year, country of publication; (2) study design; (3) sample characteristics; (4) study aim; (5) characteristics of the intervention; (6) type of surgery performed; (7) measuring instruments used and (8) main results obtained (see Table 2).
The reliability of the researchers’ data coding was checked by calculating the intraclass correlation coefficient, obtained as 0.97 (minimum = 0.94; maximum = 1). Cohen's Kappa coefficient of the categorical variables was 0.96 (minimum = 0.93; maximum = 1).
3.6. Synthesis
The results of the systematic review and data extraction were subjected to a descriptive analysis and data table classification. The studies presenting sufficient statistical data were used to perform a meta‐analysis. Heterogeneity was analysed using the I 2 index, which represents the percentage of variation attributable to statistical heterogeneity. Fixed or random‐effects analysis was employed according to the heterogeneity of the sample. Thus, if the I 2 value was greater than 50%, a random‐effects analysis was used. Two random‐effects meta‐analyses were performed to estimate the effect size of game‐based interventions, one for preoperative anxiety measured with mYPAS (the modified Yale Preoperative Anxiety Scale) and the other with mYPAS‐SF (the modified Yale Preoperative Anxiety‐Short Form). The effect size was estimated from the sample size of the intervention and control groups, and the means and standard deviations were calculated for each group during anaesthesia induction. Publication bias was assessed using funnel plots, and sensitivity analysis was also performed. Cochrane RevMan Web software was used for all statistical calculations.
4. RESULTS
4.1. Characteristics of the studies included
In total, 200 studies were found in the five databases. After reviewing the titles and abstracts and removing duplicates, 161 records were remained. The full‐text reading then reduced the final sample for analysis to 26 studies. The search and selection process is described in Figure 1.
All of the studies included were randomised controlled trials. The total sample population consisted of 2525 children. One study was published in 2006, but the majority (n = 18) were conducted in 2019 or later. The following countries of publication were represented: USA (n = 5), Turkey (n = 3), Iran (n = 3), South Korea (n = 3) and Belgium (n = 2), together with one study each published in Syria, India, Denmark, Jordan, Netherlands, China, Japan, England, France and Italy (Table 2).
To measure the pain experienced, one study used the Wong–Baker Faces Pain Rating Scale (WBFPRS) and another, the pain dimension of the Visual Analogue Scale (VAS). To evaluate anxiety, most studies (n = 20) used the mYPAS, while others used the YPAS‐SF (n = 2) or the Yale Preoperative Anxiety (YPAS) (n = 1). Other anxiety measurement tools used were the Visual Facial Anxiety Scale (VFAS), the anxiety dimension of the VAS and the Children's Anxiety Metre‐Scale (CAM‐S) (Table 2).
The samples of children were heterogeneous and included various settings (ambulatory and elective) and types of surgery (dental, otorhinolaryngology, genital, urologic, ophthalmological, urological, orthopaedic, abdominal or general) (see Table 2). The durations considered before the induction of anaesthesia ranged from 20 min (Al‐Nerabieah et al., 2020; Clausen et al., 2021; Dwairej et al., 2020; Forouzandeh et al., 2020; Gao et al., 2014; Marechal et al., 2017; Stewart et al., 2019; Ünver et al., 2020) to 24 h (Chaurasia et al., 2019; Hashimoto et al., 2020). Most of the interventions lasted between 5 min (Al‐Nerabieah et al., 2020; Buyuk et al., 2021; Dehghan et al., 2019; Jung et al., 2021) and 15 min (Eijlers, Dierckx, et al., 2019) (Table 2).
All studies presented an adequate level of quality, according to the quality assessment tools applied, and none were excluded for this reason. The characteristics of the studies included are shown in Table 2, and the risk of bias, in each case, is illustrated in Figure 2.
FIGURE 2.

Risk of bias across all included studies [Colour figure can be viewed at wileyonlinelibrary.com]
4.2. Effect of the game‐based intervention on pain and anxiety levels
All 26 studies reported the effect of game‐based interventions on anxiety levels, and two also considered the effect on pain levels (Al‐Nerabieah et al., 2020; Matthyssens et al., 2020).
4.2.1. Analysis of pain levels
Two studies reported the effect of the game‐based interventions on pain levels (Al‐Nerabieah et al., 2020; Matthyssens et al., 2020). One detected no significant differences in this respect between the intervention group and the control group (Matthyssens et al., 2020), while the other recorded a decreased pain score in the intervention group (mean difference −2.53; 95% CI: −3.04, −2.02, p≤ .001) (Al‐Nerabieah et al., 2020) (Table 2). A meta‐analysis could not be performed of these studies due to the different pain scales used (WBFPRS vs. VAS).
4.2.2. Analysis of anxiety levels
Of the 12 studies not included in the meta‐analyses, 10 reported that children experienced a significant reduction in preoperative anxiety after a game‐based intervention was employed as a distraction method (Buyuk et al., 2021; Dehghan et al., 2019; Hashimoto et al., 2020; Hosseinpour & Memarzadeh, 2010; Jung et al., 2021; Matthyssens et al., 2020; Park et al., 2019; Ryu et al., 2019; Seiden et al., 2014; Ünver et al., 2020). Only two studies (Eijlers, Dierckx, et al., 2019; Uyar et al., 2020) found no beneficial effect on anxiety from this intervention (Table 2).
4.3. Meta‐analysis of the effect of the game‐based intervention on anxiety levels
Studies that provided sufficient statistical information (n = 14) were included in the meta‐analysis. As they presented considerable heterogeneity, a fixed‐effects model was not considered appropriate and only a random‐effects model was applied. Two meta‐analyses were performed of the effect size of a game‐based intervention on anxiety levels. The first, with 12 studies, all of which used the mYPAS questionnaire, had a sample of n = 493 children for the intervention group and n = 471 for the control group (Table 2). The effect size of the intervention, calculated as the mean difference achieved during anaesthesia induction according to the mYPAS score was −10.62 (95% CI: −13.85, −7.39) in favour of the intervention. The statistical heterogeneity (I 2 value) across these studies was 84%.
The second meta‐analysis was conducted of the two studies that used the mYPAS‐SF questionnaire, which included n = 83 children in each group. This analysis revealed no statistically significant effect on anxiety levels, with an estimated effect size of −20.10 (95% CI: −45.55, −5.35).
A sensitivity analysis was performed for both meta‐analyses, revealing no change in effect size when each study was removed from the analysis. The funnel plots did not indicate the presence of publication bias. The forest plot and the risk of bias of each study are shown in Figures 3 and 4.
FIGURE 3.
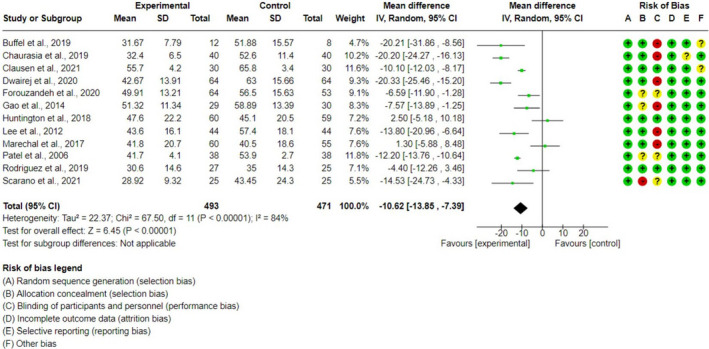
Forest plot for anxiety using mYPAS [Colour figure can be viewed at wileyonlinelibrary.com]
FIGURE 4.
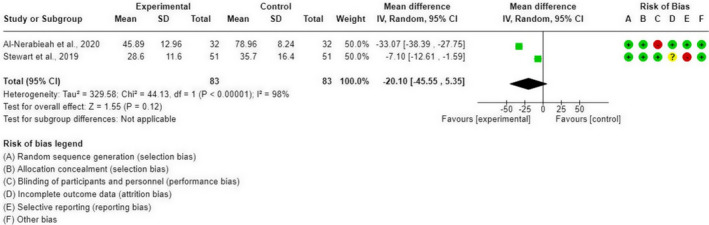
Forest plot for anxiety using mYPAS‐SF [Colour figure can be viewed at wileyonlinelibrary.com]
For the remaining 12 studies, no meta‐analysis was performed due to differences in the anxiety measurement scales (VAS and VFAS) (Matthyssens et al., 2020; Ünver et al., 2020), in the measurement units (Eijlers, Dierckx, et al., 2019; Hashimoto et al., 2020; Jung et al., 2021; Park et al., 2019; Ryu et al., 2019; Seiden et al., 2014) or due to insufficient statistical data (Buyuk et al., 2021; Dehghan et al., 2019; Hosseinpour & Memarzadeh, 2010; Uyar et al., 2020).
5. DISCUSSION
To the best of our knowledge, no previous systematic reviews or meta‐analyses have been conducted to determine the effect of games‐based interventions on pain and anxiety levels in children during the preoperative induction of anaesthesia.
Our analysis shows that gamification improves preoperative preparation for children, especially by reducing their anxiety. Thus, the children in the gamification group had significantly lower levels of anxiety than those in the control group at the time of anaesthesia induction. We corroborate prior reports that pleasurable activities can alleviate the anxiety felt by children before surgery (Kumar et al., 2019; Weber, 2010), although one study observed no such positive effects in adult patients (Koo et al., 2020).
No significant differences in pain levels were reported, although this may be due to the small number of studies that addressed this question. Nevertheless, digital distraction techniques have been shown to reduce levels of distress and pain in children subjected to painful procedures (Gates et al., 2020).
Distraction techniques and non‐pharmacological medical methods provide the basis for simple, readily‐applicable interventions that can reduce anxiety and disruptive behaviour in children. Virtual reality devices used for patients undergoing routine blood extraction can reduce acute pain and anxiety and produce high levels of satisfaction (Gold & Mahrer, 2018). In a related study, patients reported that the intervention made them feel more comfortable and less scared during their hospital stay (Gold et al., 2021). Other strategies, too, have been employed to alleviate stress, anxiety and pain, such as art therapy or music therapy (Gómez‐Urquiza et al., 2016; Nooruzi et al., 2018). In relation to anaesthetic induction, it has been observed that watching cartoons during sleep induction for deep sedation are associated with a shorter sleep onset time (Tschiedel et al., 2019).
Gamification is another pleasurable educational resource that can be useful during preparation for surgery and in postoperative care. Studies have shown that children who receive an educational multimedia intervention are less worried about surgery and other hospital procedures (Fernandes et al., 2014). Moreover, this approach can also reduce parental anxiety (Fernandes et al., 2015; Kumar et al., 2019). However, a recent meta‐analysis indicated that virtual reality interventions were potentially more effective in younger children than in adolescents (Eijlers, Utens, et al., 2019).
Despite the considerable pain and anxiety experienced by many children prior to surgery, non‐pharmacological methods are still rarely considered as a means of alleviating these problems during the induction of anaesthesia (Rantala et al., 2020). Gamed‐based interventions can reduce preoperative anxiety, and at the same time, itprovides the opportunity to educate children about the hospital environment during hospitalisation or even at home before attending for treatment (Rantala et al., 2020). Gamification has been shown to improve the physical, mental and emotional health of the child (Lestari et al., 2017). On the other hand, although the benefits of this type of intervention seem significant, little is known about the longer‐term duration of effects (after surgery, during hospitalisation or after discharge). Furthermore, the children included in the studies in our analysis varied in age, in the type of surgery received and in hospital setting, which means that our results should be interpreted with caution. In conclusion, distraction‐based interventions need to be further developed to optimise surgical pathways, and thus enhance preoperative and postoperative settings for the paediatric patient.
5.1. Limitations
The review process described is subject to certain clinical and methodological limitations. First, the studies considered used a wide variety of instruments to measure anxiety and pain, and different forms of results reporting (means and standard deviation / median and interquartile range). Second, there were large differences in the duration of the intervention (from 5 to 15 min) and in the time points before anaesthetic induction (from 20 min to 24 h). This heterogeneity makes it difficult to determine the optimal timing and duration of preoperative intervention. The control groups, too, were heterogeneous with respect to parental presence, type of intervention and medication supplied. In addition, the diverse settings and types of surgery would have affected the pain and anxiety experienced, thus influencing the study results.
Another limitation to our study is that the effect size of the intervention on pain levels could not be analysed due to the small number of studies found. Similarly, the meta‐analysis performed with the mYPAS‐SF questionnaire was based on just two studies (Al‐Nerabieah et al., 2020; Stewart et al., 2019). Accordingly, further randomised clinical trials are essential to analyse the effect size obtained, until when our results should be interpreted with caution.
A more extensive analysis of postoperative pain and anxiety levels would also be desirable, but our review and meta‐analysis had no access to follow‐up data after surgery. Potential variability in this respect might have contributed to the fact that these questions were not investigated.
5.2. Implication for practice and research
The meta‐analysis presented in this paper shows that gamed‐based interventions can have a positive effect, alleviating preoperative anxiety. They are safe and both encourage and educate children about medical procedures. By reducing anxiety, they contribute to earlier hospital discharge, faster recovery and rehabilitation, a reduced need for medication during anaesthesia and better pain tolerance, all of which help lower hospital costs (Moura et al., 2016). However, the management of perioperative pain and anxiety in children continues to pose significant challenges and is often inadequate, due to cost and time‐related restrictions (Copanitsanou & Valkeapää, 2014; Fortier & Kain, 2015). Since reducing pain and anxiety is among the main tasks performed by nursing professionals, it is necessary to develop interventions to better address perioperative management. An important preoperative responsibility of nurses is to optimise physiological and psychological health and to help patients adapt to stressors. The method we describe could usefully be included as a nursing function to help alleviate anxiety in children and thus optimise surgical care. Further research is needed to determine the ideal type and duration of preoperative preparation and intervention.
6. CONCLUSIONS
Game‐based interventions have a positive impact, reducing preoperative anxiety in children before and during the induction of anaesthesia, although our analysis detected no significant impact on pain levels. This innovative and pleasurable type of intervention can be helpful in the care of paediatric surgical patients, alleviating pain and anxiety during preoperative care. This task is often challenging for nursing professionals, and game‐based strategies could help them provide positive attention in paediatric care, benefiting children's emotional health and post‐surgery recovery. However, such distraction‐based interventions need further development to optimise surgical pathways in preoperative and postoperative settings for the paediatric patient.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHOR CONTRIBUTIONS
All authors have agreed on the final version and meet all four following criteria [recommended by the ICMJE (http://www.icmje.org/recommendations/)]: Have made substantial contributions to conception and design, analysis and interpretation of data. Been involved in drafting the manuscript or revising it critically for important intellectual content. Given final approval of the version to be published. Each author has participated sufficiently in the work to take public responsibility for appropriate portions of the content. N. S.‐M. and J.L. G.‐U. involved in study design. J.L. R.‐B., R.A. G.‐L., L. P.‐H., M.J. M.‐J. and G. D.‐V. involved in literature search and data analysis. N. S.‐M., J.L. R.‐B., M.J. M.‐J. and R.A. G.‐L. involved in manuscript preparation.: N. S.‐M. and J.L. G.‐U. involved in supervision.
Supporting information
Supplementary Material
ACKNOWLEDGEMENT
Funding for open access charge: Universidad de Granada / CBUA. [Correction added on 20‐May‐22 after first online publication: the CBUA funding statement was added.]
Suleiman‐Martos, N. , García‐Lara, R. A. , Membrive‐Jiménez, M. J. , Pradas‐Hernández, L. , Romero‐Béjar, J. L. , Dominguez‐Vías, G. , & Gómez‐Urquiza, J. L. (2022). Effect of a game‐based intervention on preoperative pain and anxiety in children: A systematic review and meta‐analysis. Journal of Clinical Nursing, 31, 3350–3367. 10.1111/jocn.16227
Funding information
This research did not receive any specific grant from funding agencies in the public, commercial, or not‐for‐profit‐sectors
Contributor Information
Nora Suleiman‐Martos, Email: norasm@ugr.es.
Rubén A. García‐Lara, Email: ruben.garcia.lara.sspa@juntadeandalucia.es.
María J. Membrive‐Jiménez, Email: mariajosemembrive@correo.ugr.es.
Laura Pradas‐Hernández, Email: lauraphl9@gmail.com.
José L. Romero‐Béjar, Email: jlrbejar@ugr.es.
José L. Gómez‐Urquiza, Email: jlgurquiza@ugr.es.
REFERENCES
- Al‐Nerabieah, Z. , Alhalabi, M.‐N. , Owayda, A. , Alsabek, L. , Bshara, N. , & Kouchaji, C. (2020). Effectiveness of using virtual reality eyeglasses in the waiting room on preoperative anxiety: A randomized controlled trial. Perioperative Care and Operating Room Management, 21, 100129. 10.1016/j.pcorm.2020.100129 [DOI] [Google Scholar]
- Alqudimat, M. , Mesaroli, G. , Lalloo, C. , Stinson, J. , & Matava, C. (2021). State of the art: Immersive technologies for perioperative anxiety, acute, and chronic pain management in pediatric patients. Current Anesthesiology Reports, 11(3), 265–274. 10.1007/S40140-021-00472-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ang, S. P. , Montuori, M. , Trimba, Y. , Maldari, N. , Patel, D. , & Chen, Q. C. (2021). Recent applications of virtual reality for the management of pain in burn and pediatric patients. Current Pain and Headache Reports, 25(1), 4. 10.1007/s11916-020-00917-0 [DOI] [PubMed] [Google Scholar]
- Aytekin, A. , Doru, Ö. , & Kucukoglu, S. (2016). The effects of distraction on preoperative anxiety level in children. Journal of Perianesthesia Nursing, 31(1), 56–62. 10.1016/J.JOPAN.2014.11.016 [DOI] [PubMed] [Google Scholar]
- Beringer, R. , Segar, P. , Pearson, A. , Greamspet, M. , & Kilpatrick, N. (2014). Observational study of perioperative behavior changes in children having teeth extracted under general anesthesia. Paediatric Anaesthesia, 24(5), 499–504. 10.1111/PAN.12362 [DOI] [PubMed] [Google Scholar]
- Buffel, C. , van Aalst, J. , Bangels, A.‐M. , Toelen, J. , Allegaert, K. , Verschueren, S. , & Vander Stichele, G. (2019). A web‐based serious game for health to reduce perioperative anxiety and pain in children (CliniPup): Pilot randomized controlled trial. JMIR Serious Games, 7(2), e12431. 10.2196/12431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buyuk, E. T. , Odabasoglu, E. , Uzsen, H. , & Koyun, M. (2021). The effect of virtual reality on children’s anxiety, fear, and pain levels before circumcision. Journal of Pediatric Urology, 17(4), 567.e1–8. 10.1016/j.jpurol.2021.04.008 [DOI] [PubMed] [Google Scholar]
- Caruso, T. J. , O’Connell, C. , Qian, J. J. , Kung, T. , Wang, E. , Kinnebrew, S. , Pearson, M. , Kist, M. , Menendez, M. , & Rodriguez, S. T. (2020). Retrospective review of the safety and efficacy of virtual reality in a pediatric hospital. Pediatric Quality & Safety, 5(2), e293. 10.1097/pq9.0000000000000293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caumo, W. , Broenstrub, J. , Fialho, L. , Petry, S. , Brathwait, O. , Bandeira, D. , Loguercio, A. , & Ferreira, M. (2000). Risk factors for postoperative anxiety in children. Acta Anaesthesiologica Scandinavica, 44(7), 782–789. 10.1034/J.1399-6576.2000.440703.X [DOI] [PubMed] [Google Scholar]
- Chaurasia, B. , Jain, D. , Mehta, S. , Gandhi, K. , & Mathew, P. J. (2019). Incentive‐based game for allaying preoperative anxiety in children: A prospective, randomized trial. Anesthesia and Analgesia, 129(6), 1629–1634. 10.1213/ANE.0000000000003717 [DOI] [PubMed] [Google Scholar]
- Chen, Y. J. , Cheng, S. F. , Lee, P. C. , Lai, C. H. , Hou, I. C. , & Chen, C. W. (2020). Distraction using virtual reality for children during intravenous injections in an emergency department: A randomised trial. Journal of Clinical Nursing, 29(3–4), 503–510. 10.1111/JOCN.15088 [DOI] [PubMed] [Google Scholar]
- Chow, C. H. T. , Van Lieshout, R. J. , Schmidt, L. A. , Dobson, K. G. , & Buckley, N. (2016). Systematic review: Audiovisual interventions for reducing preoperative anxiety in children undergoing elective surgery. Journal of Pediatric Psychology, 41(2), 182–203. 10.1093/jpepsy/jsv094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clausen, N. G. , Madsen, D. , Rosenkilde, C. , Hasfeldt‐Hansen, D. , Larsen, L. G. , & Hansen, T. G. (2021). The use of tablet computers to reduce preoperative anxiety in children before anesthesia: A randomized controlled study. Journal of Perianesthesia Nursing, 36(3), 275–278. 10.1016/j.jopan.2020.09.012 [DOI] [PubMed] [Google Scholar]
- Copanitsanou, P. , & Valkeapää, K. (2014). Effects of education of paediatric patients undergoing elective surgical procedures on their anxiety – A systematic review. Journal of Clinical Nursing, 23(7–8), 940–954. 10.1111/JOCN.12187 [DOI] [PubMed] [Google Scholar]
- Cunningham, A. , McPolin, O. , Fallis, R. , Coyle, C. , Best, P. , & McKenna, G. (2021). A systematic review of the use of virtual reality or dental smartphone applications as interventions for management of paediatric dental anxiety. BMC Oral Health, 21(1), 224. 10.1186/S12903-021-01602-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dehghan, F. , Jalali, R. , & Bashiri, H. (2019). The effect of virtual reality technology on preoperative anxiety in children: A Solomon four‐group randomized clinical trial. Perioperative Medicine (London, England), 8, 5. 10.1186/s13741-019-0116-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drasković, B. , Simin, J. , & Kvrgić, I. (2015). Psychological aspects of pediatric anesthesia. Medicinski Pregled, 68(1–2), 29–34. 10.2298/MPNS1502029D [DOI] [PubMed] [Google Scholar]
- Dwairej, D. A. , Obeidat, H. M. , & Aloweidi, A. S. (2020). Video game distraction and anesthesia mask practice reduces children’s preoperative anxiety: A randomized clinical trial. Journal for Specialists in Pediatric Nursing, 25(1), e12272. 10.1111/jspn.12272 [DOI] [PubMed] [Google Scholar]
- Eijlers, R. , Dierckx, B. , Staals, L. , Berghmans, J. , van der Schroeff, M. , Strabbing, E. , Wijnen, R. , Hillegers, M. , Legerstee, J. , & Utens, E. (2019). Virtual reality exposure before elective day care surgery to reduce anxiety and pain in children: A randomised controlled trial. European Journal of Anaesthesiology, 36(10), 728–737. 10.1097/EJA.0000000000001059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eijlers, R. , Utens, E. , Staals, L. , de Nijs, P. , Berghmans, J. , Wijnen, R. , Hillegers, M. , Dierckx, B. , & Legerstee, J. (2019). Systematic review and meta‐analysis of virtual reality in pediatrics: Effects on pain and anxiety. Anesthesia and Analgesia, 129(5), 1344–1353. 10.1213/ANE.0000000000004165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandes, S. , Arriaga, P. , & Esteves, F. (2014). Providing preoperative information for children undergoing surgery: A randomized study testing different types of educational material to reduce children’s preoperative worries. Health Education Research, 29(6), 1058–1076. 10.1093/her/cyu066 [DOI] [PubMed] [Google Scholar]
- Fernandes, S. , Arriaga, P. , & Esteves, F. (2015). Using an educational multimedia application to prepare children for outpatient surgeries. Health Communication, 30(12), 1190–1200. 10.1080/10410236.2014.896446 [DOI] [PubMed] [Google Scholar]
- Forouzandeh, N. , Drees, F. , Forouzandeh, M. , & Darakhshandeh, S. (2020). The effect of interactive games compared to painting on preoperative anxiety in Iranian children: A randomized clinical trial. Complementary Therapies in Clinical Practice, 40, 101211. 10.1016/j.ctcp.2020.101211 [DOI] [PubMed] [Google Scholar]
- Fortier, M. , Del Rosario, A. , Martin, S. , & Kain, Z. (2010). Perioperative anxiety in children. Paediatric Anaesthesia, 20(4), 318–322. 10.1111/J.1460-9592.2010.03263.X [DOI] [PubMed] [Google Scholar]
- Fortier, M. , & Kain, Z. (2015). Treating perioperative anxiety and pain in children: A tailored and innovative approach. Paediatric Anaesthesia, 25(1), 27–35. 10.1111/PAN.12546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fortier, M. , Martin, S. , Chorney, J. , Mayes, L. , & Kain, Z. (2011). Preoperative anxiety in adolescents undergoing surgery: A pilot study. Paediatric Anaesthesia, 21(9), 969–973. 10.1111/J.1460-9592.2011.03593.X [DOI] [PubMed] [Google Scholar]
- Gao, X. L. , Liu, Y. , Tian, S. , Zhang, D. Q. , & Wu, Q. P. (2014). Effect of interesting games on relief of preoperative anxiety in preschool children. International Journal of Nursing Sciences, 1(1), 89–92. 10.1016/j.ijnss.2014.02.002 [DOI] [Google Scholar]
- Gates, M. , Hartling, L. , Shulhan‐Kilroy, J. , MacGregor, T. , Guitard, S. , Wingert, A. , Featherstone, R. , Vandermeer, B. , Poonai, N. , Kircher, J. , Perry, S. , Graham, T. , Scott, S. , & Ali, S. (2020). Digital technology distraction for acute pain in children: A Meta‐analysis. Pediatrics, 145(2), e20191139. 10.1542/PEDS.2019-1139 [DOI] [PubMed] [Google Scholar]
- Gerçeker, G. Ö. , Ayar, D. , Özdemir, E. Z. , & Bektaş, M. (2020). Effects of virtual reality on pain, fear and anxiety during blood draw in children aged 5–12 years old: A randomised controlled study. Journal of Clinical Nursing, 29(7–8), 1151–1161. 10.1111/JOCN.15173 [DOI] [PubMed] [Google Scholar]
- Gold, J. I. , Annick, E. T. , Lane, A. S. , Ho, K. , Marty, R. T. , & Espinoza, J. C. (2021). “Doc McStuffins: Doctor for a day” virtual reality (DocVR) for pediatric preoperative anxiety and satisfaction – A feasibility study. Journal of Medical Internet Research, 23(4), e25504. 10.2196/25504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold, J. I. , & Mahrer, N. E. (2018). Is virtual reality ready for prime time in the medical space? A randomized control trial of pediatric virtual reality for acute procedural pain management. Journal of Pediatric Psychology, 43(3), 266–275. 10.1093/jpepsy/jsx129 [DOI] [PubMed] [Google Scholar]
- Gómez‐Urquiza, J. , Hueso‐Montoro, C. , Urquiza‐Olmo, J. , Ibarrondo‐Crespo, R. , González‐Jiménez, E. , & Schmidt‐Riovalle, J. (2016). A randomized controlled trial of the effect of a photographic display with and without music on pre‐operative anxiety. Journal of Advanced Nursing, 72(7), 1666–1676. 10.1111/JAN.12937 [DOI] [PubMed] [Google Scholar]
- Hashimoto, Y. , Chaki, T. , Hirata, N. , Tokinaga, Y. , Yoshikawa, Y. , & Yamakage, M. (2020). Video glasses reduce preoperative anxiety compared with portable multimedia player in children: A randomized controlled trial. Journal of Perianesthesia Nursing, 35(3), 321–325. 10.1016/J.JOPAN.2019.10.001 [DOI] [PubMed] [Google Scholar]
- Hosseinpour, M. , & Memarzadeh, M. (2010). Use of a preoperative playroom to prepare children for surgery. European Journal of Pediatric Surgery, 20(6), 408–411. 10.1055/S-0030-1265172 [DOI] [PubMed] [Google Scholar]
- Howick, J. , Chalmers, I. , Glasziou, P. , Greenhalg, T. , Heneghan, C. , Liberati, A. , Moschetti, I. , Phillips, B. , & Thornton, H. (2011). The Oxford 2011 levels of evidence. https://www.cebm.net/2016/05/ocebm‐levels‐of‐evidence [Google Scholar]
- Huntington, C. , Liossi, C. , Donaldson, A. N. , Newton, J. T. , Reynolds, P. A. , Alharatani, R. , & Hosey, M. T. (2018). On‐line preparatory information for children and their families undergoing dental extractions under general anesthesia: A phase III randomized controlled trial. Paediatric Anaesthesia, 28(2), 157–166. 10.1111/pan.13307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jung, M. J. , Libaw, J. S. , Ma, K. , Whitlock, E. L. , Feiner, J. R. , & Sinskey, J. L. (2021). Pediatric distraction on induction of anesthesia with virtual reality and perioperative anxiolysis: A randomized controlled trial. Anesthesia and Analgesia, 132(3), 798–806. 10.1213/ANE.0000000000005004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kain, Z. , Caldwell‐Andrews, A. , Maranets, I. , Nelson, W. , & Mayes, L. (2006). Predicting which child‐parent pair will benefit from parental presence during induction of anesthesia: A decision‐making approach. Anesthesia and Analgesia, 102(1), 81–84. 10.1213/01.ANE.0000181100.27931.A1 [DOI] [PubMed] [Google Scholar]
- Kenney, M. P. , & Milling, L. S. (2016). The effectiveness of virtual reality distraction for reducing pain: A meta‐analysis. Psychology of Consciousness: Theory, Research, and Practice, 3(3), 199–210. 10.1016/j.cpr.2010.07.001 [DOI] [Google Scholar]
- Koo, C. H. , Park, J. W. , Ryu, J. H. , & Han, S. H. (2020). The effect of virtual reality on preoperative anxiety: A meta‐analysis of randomized controlled trials. Journal of Clinical Medicine, 9(10), 1–12. 10.3390/jcm9103151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar, A. , Das, S. , Chauhan, S. , Kiran, U. , & Satapathy, S. (2019). Perioperative anxiety and stress in children undergoing congenital cardiac surgery and their parents: Effect of brief intervention—A randomized control trial. Journal of Cardiothoracic and Vascular Anesthesia, 33(5), 1244–1250. 10.1053/j.jvca.2018.08.187 [DOI] [PubMed] [Google Scholar]
- Lee, J. , Lee, J. , Lim, H. , Son, J. , Lee, J. , Kim, D. , & Ko, S. (2012). Cartoon distraction alleviates anxiety in children during induction of anesthesia. Anesthesia and Analgesia, 115(5), 1168–1173. 10.1213/ANE.0B013E31824FB469 [DOI] [PubMed] [Google Scholar]
- Lestari, L. , Wanda, D. , & Hayati, H. (2017). The effectiveness of distraction (cartoon‐patterned clothes and bubble‐blowing) on pain and anxiety in preschool children during venipuncture in the emergency department. Comprehensive Child and Adolescent Nursing, 40, 22–28. 10.1080/24694193.2017.1386967 [DOI] [PubMed] [Google Scholar]
- Manyande, A. , Cyna, A. , Yip, P. , Chooi, C. , & Middleton, P. (2015). Non‐pharmacological interventions for assisting the induction of anaesthesia in children. Cochrane Database of Systematic Reviews, 2015(7), CD006447. 10.1002/14651858.CD006447.PUB3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marechal, C. , Berthiller, J. , Tosetti, S. , Cogniat, B. , Desombres, H. , Bouvet, L. , Kassai, B. , Chassard, D. , & de Queiroz Siqueira, M. (2017). Children and parental anxiolysis in paediatric ambulatory surgery: A randomized controlled study comparing 0.3 mg kg−1 midazolam to tablet computer based interactive distraction. British Journal of Anaesthesia, 118(2), 247–253. 10.1093/bja/aew436 [DOI] [PubMed] [Google Scholar]
- Matthyssens, L. E. , Vanhulle, A. , Seldenslach, L. , Vander Stichele, G. , Coppens, M. , & Van Hoecke, E. (2020). A pilot study of the effectiveness of a serious game CliniPup® on perioperative anxiety and pain in children. Journal of Pediatric Surgery, 55(2), 304–311. 10.1016/j.jpedsurg.2019.10.031 [DOI] [PubMed] [Google Scholar]
- Moura, L. , Dias, I. , & Pereira, L. (2016). Prevalence and factors associated with preoperative anxiety in children aged 5–12 years. Revista Latino‐Americana de Enfermagem, 24, e2708. 10.1590/1518-8345.0723.2708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nooruzi, S. , Zanjani, S. A. , Dastan, B. , & Raadin, A. (2018). The effectiveness of art therapy on decreasing of depression and anxiety in preschoolers. Journal of Applied Psychology & Behavioral Science, 3(1), 14–18. http://www.japbs.com/fulltext/paper‐25022018182751.pdf [Google Scholar]
- Page, M. J. , McKenzie, J. E. , Bossuyt, P. M. , Boutron, I. , Hoffmann, T. C. , Mulrow, C. D. , Shamseer, L. , Tetzlaff, J. M. , Akl, E. A. , Brennan, S. E. , Chou, R. , Glanville, J. , Grimshaw, J. M. , Hróbjartsson, A. , Lalu, M. M. , Li, T. , Loder, E. W. , Mayo‐Wilson, E. , McDonald, S. , … Moher, D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. The BMJ, 372, n71. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park, J. W. , Nahm, F. S. , Kim, J. H. , Jeon, Y. T. , Ryu, J. H. , & Han, S. H. (2019). The effect of mirroring display of virtual reality tour of the operating theatre on preoperative anxiety: A randomized controlled trial. IEEE Journal of Biomedical and Health Informatics, 23(6), 2655–2660. 10.1109/JBHI.2019.2892485 [DOI] [PubMed] [Google Scholar]
- Patel, A. , Schieble, T. , Davidson, M. , Tran, M. C. J. , Schoenberg, C. , Delphin, E. , & Bennett, H. (2006). Distraction with a hand‐held video game reduces pediatric preoperative anxiety. Paediatric Anaesthesia, 16(10), 1019–1027. 10.1111/j.1460-9592.2006.01914.x [DOI] [PubMed] [Google Scholar]
- Perrott, C. , Lee, C. , Griffiths, S. , & Sury, M. (2018). Perioperative experiences of anesthesia reported by children and parents. Paediatric Anaesthesia, 28(2), 149–156. 10.1111/PAN.13300 [DOI] [PubMed] [Google Scholar]
- Perry, J. , Hooper, V. , & Masiongale, J. (2012). Reduction of preoperative anxiety in pediatric surgery patients using age‐appropriate teaching interventions. Journal of Perianesthesia Nursing, 27(2), 69–81. 10.1016/J.JOPAN.2012.01.003 [DOI] [PubMed] [Google Scholar]
- Rantala, A. , Pikkarainen, M. , Miettunen, J. , He, H. , & Pölkki, T. (2020). The effectiveness of web‐based mobile health interventions in pediatric outpatient surgery: A systematic review and meta‐analysis of randomized controlled trials. Journal of Advanced Nursing, in press. 76, 1949–1960. 10.1111/jan.14381 [DOI] [PubMed] [Google Scholar]
- Rodriguez, S. T. , Jang, O. , Hernandez, J. M. , George, A. J. , Caruso, T. J. , & Simons, L. E. (2019). Varying screen size for passive video distraction during induction of anesthesia in low‐risk children: A pilot randomized controlled trial. Paediatric Anaesthesia, 29(6), 648–655. 10.1111/pan.13636 [DOI] [PubMed] [Google Scholar]
- Ryu, J. , Oh, A. , Yoo, H. , Kim, J. , Park, J. , & Han, S. (2019). The effect of an immersive virtual reality tour of the operating theater on emergence delirium in children undergoing general anesthesia: A randomized controlled trial. Paediatric Anaesthesia, 29(1), 98–105. 10.1111/pan.13535 [DOI] [PubMed] [Google Scholar]
- Scarano, F. , Corte, A. D. , Michielon, R. , Gava, A. , & Midrio, P. (2021). Application of a non‐pharmacological technique in addition to the pharmacological protocol for the management of children’s preoperative anxiety: A 10 years’ experience. Pediatria Medica e Chirurgica, 43(1), 235. 10.4081/pmc.2021.235 [DOI] [PubMed] [Google Scholar]
- Seiden, S. , McMullan, S. , Sequera‐Ramos, L. , De Oliveira, G. , Roth, A. , Rosenblatt, A. , Jesdale, B. , & Suresh, S. (2014). Tablet‐based interactive distraction (TBID) vs oral midazolam to minimize perioperative anxiety in pediatric patients: A noninferiority randomized trial. Paediatric Anaesthesia, 24(12), 1217–1223. 10.1111/PAN.12475 [DOI] [PubMed] [Google Scholar]
- Sterne, J. A. C. , Savović, J. , Page, M. J. , Elbers, R. G. , Blencowe, N. S. , Boutron, I. , Cates, C. J. , Cheng, H.‐Y. , Corbett, M. S. , Eldridge, S. M. , Emberson, J. R. , Hernán, M. A. , Hopewell, S. , Hróbjartsson, A. , Junqueira, D. R. , Jüni, P. , Kirkham, J. J. , Lasserson, T. , Li, T. , … Higgins, J. P. T. (2019). RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ, 366, l4898. 10.1136/bmj.l4898 [DOI] [PubMed] [Google Scholar]
- Stewart, B. , Cazzell, M. , & Pearcy, T. (2019). Single‐blinded randomized controlled study on use of interactive distraction versus oral midazolam to reduce pediatric preoperative anxiety, emergence delirium, and postanesthesia length of stay. Journal of Perianesthesia Nursing, 34(3), 567–575. 10.1016/J.JOPAN.2018.08.004 [DOI] [PubMed] [Google Scholar]
- Tschiedel, E. , Beckers, K. , Groe‐Lordemann, A. , Basu, O. , Felderhoff‐Müser, U. , & Dohna‐Schwake, C. (2019). Visual distraction during sleep induction with propofol in pediatric patients – Can cartoon watching influence the sedative dose? Klinische Padiatrie, 231(1), 35–40. 10.1055/a-0609-6643 [DOI] [PubMed] [Google Scholar]
- Ünver, S. , Güray, Ö. , & Aral, S. (2020). Effectiveness of a group game intervention in reducing preoperative anxiety levels of children and parents: A randomized controlled trial. AORN Journal, 111(4), 403–412. 10.1002/aorn.12990 [DOI] [PubMed] [Google Scholar]
- Uyar, S. , Polat, R. , Bolat, M. , & Donmez, A. (2020). Which is good for pre‐operative anxiety? Midazolam, video games or teaching with cartoons: A randomised trial. European Journal of Anaesthesiology, 38(7), 744–750. 10.1097/EJA.0000000000001384 [DOI] [PubMed] [Google Scholar]
- Vrancken, J. , De Gryse, L. , & Spooren, A. I. F. (2021). HospiAvontuur: Development of a serious game to help young children and their parents during the preparation for an admission at the hospital for elective surgery. Behaviour & Information Technology, 40(2), 134–145. 10.1080/0144929X.2019.1673821 [DOI] [Google Scholar]
- Walther‐Larsen, S. , Aagaard, G. , Friis, S. , Petersen, T. , Møller‐Sonnergaard, J. , & Rømsing, J. (2016). Structured intervention for management of pain following day surgery in children. Paediatric Anaesthesia, 26(2), 151–157. 10.1111/PAN.12811 [DOI] [PubMed] [Google Scholar]
- Weber, F. (2010). The influence of playful activities on children’s anxiety during the preoperative period at the outpatient surgical center. Jornal de Pediatria, 86(3), 209–214. 10.2223/JPED.2000 [DOI] [PubMed] [Google Scholar]
- Wollin, S. , Plummer, J. , Owen, H. , Hawkins, R. , & Materazzo, F. (2003). Predictors of preoperative anxiety in children. Anaesthesia and Intensive Care, 31(1), 69–74. 10.1177/0310057X0303100114 [DOI] [PubMed] [Google Scholar]
- Won, A. S. , Bailey, J. , Bailenson, J. , Tataru, C. , Yoon, I. A. , & Golianu, B. (2017). Immersive virtual reality for pediatric pain. Children, 4(7), 52. 10.3390/children4070052 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material


