Abstract
Recently we reported that human T- and B-cell recognition of a 42-kDa protein (p42) in soluble extracts of adult Schistosoma mansoni worms correlates with resistance to reinfection with S. mansoni or S. haematobium. Amino acid microsequencing of p42 revealed that it consists predominantly of schistosome glyceraldehyde 3-phosphate dehydrogenase (SG3PDH). We have expressed SG3PDH in Escherichia coli and purified the recombinant protein in a soluble and enzymatically active form. Recombinant SG3PDH (rSG3PDH) reacted with human monospecific antibodies to p42. Lymphoproliferation and production of interleukin-4 and gamma interferon (IFN-γ) after in vitro stimulation with rSG3PDH and serum isotype responses to rSG3PDH were examined in individuals with extremes of resistance and susceptibility to reinfection after treatment of previous S. mansoni or S. haematobium infection. Lymphoproliferation and IFN-γ production in response to rSG3PDH and the presence of serum immunoglobulin G1 (IgG1), IgG3, and IgA antibodies to rSG3PDH generally characterized individuals who are resistant to reinfection after chemotherapy. The data indicate that T- and B-cell immune reactivity to rSG3PDH correlates with resistance to reinfection, confirming previous studies identifying SG3PDH as a target of protective immunity in humans, and suggest that SG3PDH should be investigated as a possible vaccine for human schistosomiasis.
Approximately 200 million people are infected with schistosomes worldwide. Schistosoma mansoni occurs in 58 countries in Africa, the Middle East, and South America, while about 90 million people are now infected with S. haematobium in 52 countries in Africa and the Middle East (31, 34). S. mansoni worms reside in the mesenteric veins and deposit approximately 300 eggs per pair daily. Eggs are excreted with the feces and release the miracidium, which continues the life cycle in compatible snails, or are trapped in host tissues, leading to immune-mediated inflammatory and fibrotic lesions (37). S. haematobium worms reside primarily in the pelvic venous plexus, producing massive egg concentrations in the lower urinary tract and pelvic organs. The eggs induce mass lesions in the bladder and ureters which lead to hydroureter, hydronephrosis, pyonephrosis, pyelonephritis, cancer of the urinary bladder, and renal failure (21). Chemotherapy with oxamniquine and praziquantel is effective in eradication of adult worms and alleviates some disease symptoms. Reinfection is common, especially during childhood and adolescence (29, 40), requiring frequent treatments with the potential to promote drug resistance (4, 5, 10, 20) and often leading to severe clinical consequences (27). Therefore, complementary approaches for the control of schistosomiasis are now envisaged. An effective vaccine to prevent schistosomiasis would be a major advance in this regard (8, 35).
The possibility of developing an effective vaccine is encouraged by the numerous examples of lack of reinfection after chemotherapy in adult humans that cannot be attributed solely to reduction in exposure to cercaria-infested water (6) or to age-related factors (23). In fact, several studies have shown that susceptibility to reinfection with S. mansoni or S. haematobium varies markedly among residents of areas where infection is endemic. Certain subjects resist or maintain low levels of infection for long periods of time, while others appear to be readily reinfected shortly after clearance of the parasites (7, 14, 18, 41). Identification of the schistosome antigens that trigger the apparent protective immune responses in some humans could be a critical step toward the development of a vaccine for schistosomiasis.
We have shown recently that a 42-kDa soluble adult worm antigen band is a target of cellular and humoral immune responses in subjects resistant to infection with schistosomes. This protein, p42, was found to consist predominantly of schistosome glyceraldehyde 3-phosphate dehydrogenase (SG3PDH) (18). Here we report expression of SG3PDH in Escherichia coli and purification of the recombinant product (rSG3PDH) to near homogeneity by a one-step chromatographic procedure and compare the T- and B-cell immune responses to rSG3PDH in patients with a history of strong resistance or susceptibility to schistosome reinfection after treatment. The results confirm and extend the data of Goudot-Crozel et al. (22), who reported earlier a correlation between serum recognition of SG3PDH and resistance to schistosome infection in Brazilian patients with schistosomiasis mansoni.
MATERIALS AND METHODS
Expression and purification of rSG3PDH.
The coding sequence for SG3PDH was obtained from adult S. mansoni worm cDNA (32) by PCR amplification using synthetic oligonucleotides with sequences based on the published SG3PDH sequence of Goudot-Crouzel et al. (22) and Charrier-Ferrara et al. (9). The oligonucleotides directed amplification of the complete SG3PDH-coding DNA in a form that could be restriction digested and ligated into a modified version of the E. coli expression vector pRSETA (InVitrogen, San Diego, Calif.). Following ligation at the NdeI site, the initiator codon of SG3PDH became the translation initiator of the mRNA produced from the T7 promoter. The last codon of SG3PDH was fused at a NotI site to DNA encoding AAAHHHHHH followed by a stop codon. The resulting expression vector was introduced into XL1-Blue cells (Stratagene Cloning Systems, La Jolla, Calif.).
Induction of rSG3PDH expression was performed essentially as previously described (3). The recombinant protein was purified from the soluble fraction by metal affinity chromatography (HiTrap affinity column; Pharmacia, Uppsala, Sweden). The column was washed in sequence with 0, 10, 20, 40, and 60 mM imidazole in 20 mM Na2HPO4–0.5 M NaCl (pH 7.2), and the antigen was then eluted with 50 mM EDTA in 20 mM Na2HPO4–0.5 M NaCl (pH 7.2). The eluted antigen was dialyzed against 0.1 M phosphate-buffered saline (PBS; pH 7.0), membrane (0.45-μm-pore size) filtered, and assessed for purity by Coomassie blue staining of gels following sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) and for removal of lipopolysaccharide with a Limulus amebocyte lysate kit (Bio-Whittaker, Walkersville, Md.). Protein content was determined by the Bradford assay.
Assay for G3PDH activity.
G3PDH assays were carried out in the forward direction (glyceraldehyde 3-phosphate to biphosphoglycerate). Reaction mixtures containing 0.1 M NaHCO3, 0.02 M NaCl (pH 8.3), 0.002 M NAD+, and 0.015 M glyceraldehyde 3-phosphate were monitored for change in absorption at 340 nm to determine the rate of conversion of NAD+ to NADH (25). Enzymatic activity was compared to that of commercially available rabbit muscle G3PDH (Sigma, St. Louis, Mo.).
Reactivity with anti-p42 monospecific human antibodies.
Human anti-p42 antibodies were affinity purified on a nitrocellulose strip containing 42-kDa soluble adult worm antigen (SAWA) bands as previously described (18). Antibodies to purified rSG3PDH were generated in outbred Swiss mice. Antibody reactivity against induced bacterial lysate or SAWA was determined by Western blotting (1, 18, 36).
Selection of donors.
The investigations with human donors were performed in accordance with the rules of the Ministry of Health and the Biomedical Research Centre for Infectious Diseases (The Egyptian Organization for Biological Products and Vaccines), under a protocol approved by the Schistosomiasis Research Project. The study population of approximately 4,000 individuals (10 to 60 years old) were lifelong residents of villages where S. mansoni or S. haematobium infections are endemic. Almost all of the inhabitants of these villages are frequently exposed (at least 3 h daily) to water supplies contaminated with infected cercariae in their occupations (farming; draining canals; washing and selling vegetables) and everyday lives (bathing; washing cloths and utensils). This information was obtained from oral surveys and familiarity with the cultural habits in such areas. The study population were given complete medical and parasitological examinations. Stool and urine analyses were performed as described previously (18).
Donors classified as susceptible and resistant were selected among adult subjects; this is an important difference between our study and reinfection studies by other groups (7, 14, 24). The selected adults had initial heavy infection with either S. mansoni (400 to 650 eggs/g) or S. haematobium (>50 ova/10 ml of urine) and had been treated with praziquantel at the time of detection of the infection 12 to 36 months earlier. The stool and urine samples were examined in duplicate over 3 consecutive days, at 3 months after praziquantel treatment to control for the effectiveness of the chemotherapy, 12 and 24 months later for detection of reinfection, and a week before immunological examination. Formal consent was obtained from each donor before blood was drawn.
The S. mansoni study population were permanent residents of villages where S. mansoni infection is endemic, located on a branch from the Ismailieh tributary in Qualyubia Governorate, 30 km from Cairo. The study population comprised a total of 37 subjects divided into three groups. The first group included 15 subjects who had been treated for schistosomiasis mansoni 12 to 32 months earlier and remained negative for specific eggs in either stool or urine despite frequenting river sites known to be active transmission areas. These subjects, classified as resistant, were 11 men and 4 women, 18 to 55 years old (mean age ± standard deviation [SD] = 37.3 ± 10.1 years). The second group consisted of 16 subjects, 13 men and 3 women, 21 to 58 years old (mean age ± SD = 36.5 ± 9.6 years), classified as susceptible with active S. mansoni infection (100 to 300 eggs/g) despite efficacious praziquantel treatment of previous infections 12 to 36 months earlier. Six of those 16 donors received an additional praziquantel treatment 3 months before testing and were therefore egg negative at the time of immunological examinations. The final group were six healthy controls, two men and four women, 30 to 55 years old (mean age ± SD = 38.6 ± 9.5 years), who resided in areas in Cairo where infection is not endemic and matched the study groups in terms of age and socioeconomic conditions.
The S. haematobium study population were permanent residents of villages where S. haematobium is endemic, in El Menoufia Governorate, 80 km from Cairo or in the south of Giza, and comprised a total of 35 subjects classified into three groups. The first group included 19 men classified as resistant, 21 to 55 years old (mean age ± SD = 28.9 ± 8.0 years), who had been treated for schistosomiasis haematobium 13 to 36 months earlier and remained negative for specific eggs in either stool or urine despite repeated working, fishing, and swimming in contaminated river sites. The second group had 10 subjects, 9 men and 1 woman, 16 to 40 years old (mean age ± SD = 22.3 ± 8.2 years), with active S. haematobium infection despite efficacious praziquantel treatment of previous infections within 12 to 30 months of testing; they were classified as susceptible. The final group had six healthy controls, four men and two women, 20 to 40 years old (mean age ± SD = 28.7 ± 8.5 years), who resided in areas in Cairo where infection is not endemic and matched the study groups in terms of age and socioeconomic conditions.
Preparation of cells and plasma.
Peripheral blood (10 ml) was obtained from each subject, and peripheral blood mononuclear cells (PBMC) and plasma were prepared as described elsewhere (1, 18, 19).
Preparation of SAWA and SEA.
SAWA and soluble egg antigens (SEA) were prepared from worms and eggs, respectively, of S. mansoni (SAWAm and SEAm) and S. haematobium (SAWAh and SEAh) (Egyptian strain; Schistosome Biological Supply Centre, Cairo, Egypt) as described elsewhere (1, 18, 19).
Measurement of cellular responses.
For proliferative assays, 1.5 × 105 triplicate aliquots of unfractionated PBMC were added to wells of 96-well flat-bottomed microculture plates (Costar, Cambridge, Mass.) along with no addition (soluble fraction of uninduced bacteria or medium control), rSG3PDH (10 μg/ml), or SAWA or SEA (25 μg/ml) and cultured for 5 days. Proliferation was measured by [methyl-3H]thymidine (ICN Pharmaceuticals, Irvine, Calif.) incorporation during the last 8 h of incubation. The stimulation index was calculated as (mean cpm of replicate test cultures)/(mean cpm of replicate control cultures). Individuals whose PBMC showed significant (at least P < 0.05 by the Student's t test) differences between mean counts of test and antigen-free cultures were considered responders. To generate interleukin-4 (IL-4) and gamma interferon (IFN-γ), aliquots of 1.5 × 105 PBMC in 200 μl of culture medium were cultured along with rSG3PDH (0 or 10 μg/ml) or SAWA or SEA (25 μg/ml) in wells of 96-well plates for 24 (IL-4) or 72 (IFN-γ) h. The levels of IL-4 and IFN-γ were measured by use of a capture enzyme-linked immunosorbent assay (ELISA; R&D Systems, Minneapolis, Minn.). Optical densities of duplicate wells, measured at 450 nm, were converted to picograms of IL-4 or IFN-γ per milliliter, using standard curves constructed with the recombinant human cytokines as recommended by the manufacturer. PBMC of control and schistosome-exposed individuals did not produce detectable levels of cytokine following culture in medium. Therefore, individuals whose PBMC released ≥5 pg of cytokine per ml in response to schistosome antigens were considered responders. Significance of differences in percent responders among resistant and susceptible donors was analyzed by Fisher's exact test.
Measurement of humoral responses.
Plasma samples of individual donors were tested by ELISA. Wells of polystyrene plates (Costar) were coated with 100 ng of rSG3PDH, blocked with 1% bovine serum albumin in PBS, washed with PBS–0.05% Tween 20, and incubated with plasma diluted 1:500 for immunoglobulin G1 (IgG1) and IgG3, 1:50 for IgG4 and IgA, and 1:25 for IgG2 and IgE. Peroxidase-labeled anti-human, isotype-specific Ig conjugates—anti-IgG1, anti-IgG2, anti-IgG3, and anti-IgG4 (The Binding Site, Birmingham, England); anti-IgA, α chain specific (Sigma), and anti-IgE, ɛ chain specific (Kirkegaard and Perry, Gaithersburg, Md.)—were used at 1:1,000 dilution. Reactivity was read spectrophotometrically at 492 nm after addition of o-phenylenediamine (Sigma) substrate. Individuals were considered responders when their serum antibodies displayed, in three separate experiments, absorbance values higher than the mean absorbance of wells with serum from control donors + 3 SD. Significance of differences in percent responders among resistant and susceptible donors was analyzed by Fisher's exact test.
RESULTS
Preparation of rSG3PDH test antigen.
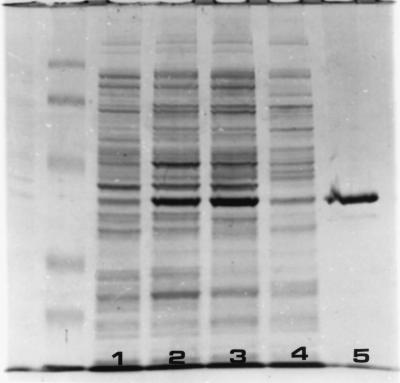
The complete coding sequence of SG3PDH was obtained from S. mansoni cDNA by PCR amplification using oligonucleotide primers based on the sequence reported by Goudot-Crozel et al. (22). The coding sequence was cloned into an E. coli expression vector, creating a carboxy-terminal hexahistidine fusion to facilitate purification as described in Materials and Methods. Following induction, the 40-kDa rSG3PDH was purified from the soluble fraction of cell extracts (Fig. 1). Enzyme analysis indicated that the purified recombinant protein had G3PDH activity. The specific activity was approximately 40% of that observed for rabbit G3PDH (data not shown). Duplicate analyses of three separate preparations indicated that purified rSG3PDH contains 0.009 ± 0.003 endotoxin units/mg. rSG3PDH reacted with human anti-p42 antibodies in ELISA and in Western blots (Fig. 2A). Mouse antibodies to rSG3PDH recognized a single band of 42 kDa in SAWA immunoblots (Fig. 2B).
FIG. 1.
SDS-PAGE analysis of rSG3PDH purification. Lane 1, uninduced bacterial extract. Induced bacterial extract (lane 2) was sonicated, and the supernatant (lane 3) was applied to a HiTrap column. Column flowthrough (lane 4) and purified rSG3PDH eluate (lane 5) are also shown. On the left are migration positions of prestained SDS-PAGE standards (103, 76, 49, 33.2, and 28 kDa; Bio-Rad, Richmond, Calif.).
FIG. 2.
(A) Reactivity of human anti-p42 antibodies with rSG3PDH. A strip of induced bacterial extract was incubated with human anti-p42 antibodies in Western blotting (lane 1). The arrow indicates the migration position of rSG3PDH. On the right are molecular masses (in kilodaltons) of protein standards. (B) Reactivity of mouse anti-rSG3PDH antibodies with SAWA p42. Strips of SAWA blot were incubated with immune (lane 1) or control (lane 2) mouse serum in Western blotting or stained with Ponceau red (lane 3). The arrow points to SAWA p42. On the right are molecular masses (in kilodaltons) of protein standards.
Patient selection.
The S. mansoni and S. haematobium study populations were selected based on several criteria. (i) They were adults with initial heavy S. mansoni or S. haematobium infection. (ii) They had been treated with praziquantel at the time of the detection of the infection 12 to 36 months earlier. Multiple stool urine analyses confirmed the efficacy of the treatment 3 months after chemotherapy and detected reinfection, if it occurred, 12 and 24 months later. (iii) Each had an average of 3 h or more of daily contact with waters proven to be contaminated with cercariae. (iv) They were from of the same closed community (Ezba) or even the same household. Under these conditions, individuals who displayed no evidence of reinfection were considered resistant, while individuals (often within the same household and occupation) with active schistosomiasis were characterized as susceptible. Control donors were parasite-free, permanent residents of areas where infection is nonendemic, matched in terms of age and socioeconomic conditions with the study population.
Lymphoproliferative responses to rSG3PDH.
Significance of differences between mean counts of test and antigen-free cultures was assessed by Students' t test and inferred as P < 0.05. PBMC from human donors did not show significant proliferative responses to the soluble fraction of uninduced bacteria. None of the six healthy parasite-free donors and only 1 of 16 subjects (6%) extremely susceptible to reinfection with S. mansoni showed significant lymphoproliferation to rSG3PDH (10 μg/ml). Conversely, 14 of 15 donors (93%) resistant to schistosomiasis mansoni reinfection exhibited significant lymphoproliferative response to rSG3PDH. The differential (P < 0.0001) reactivity to rSG3PDH cannot be attributed to suppressed or altered responses to schistosome antigens, as susceptible and resistant donors alike showed substantial lymphoproliferation to both SAWAm and SEAm (Table 1). Essentially similar results were obtained for the S. haematobium groups. All donors with history of infection showed highly significant lymphoproliferative response to SAWAh and SEAh, while none of the subjects susceptible to reinfection and 16 of 19 (84%) of resistant donors responded with significant lymphoproliferation to rSG3PDH (Table 2).
TABLE 1.
Proliferation and production of IL-4 and IFN-γ by PBMC from S. mansoni group donors stimulated in vitro with rSG3PDH or parasite antigensa
| Donor (gender, age [yr]) | Proliferation (mean cpm ± SD) in response tob:
|
IL-4 (pg/ml) in response to:
|
IFN-γ (pg/ml) in response to:
|
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Medium | rSG3PDH | SAWAm | SEAm | rSG3PDH | SAWAm | SEAm | rSG3PDH | SAWAm | SEAm | |
| Control | ||||||||||
| F, 30 | 193 ± 45 | 184 ± 4 | 913 ± 33 | 147 ± 74 | —c | NDd | ND | — | ND | ND |
| M, 40 | 258 ± 107 | 236 ± 57 | 579 ± 123 | 310 ± 151 | 5 | — | — | — | — | — |
| Susceptible | ||||||||||
| M, 37 | 137 ± 45 | 126 ± 61 | 4,413 ± 755 | 336 ± 16 | — | — | — | — | — | — |
| F, 30 | 372 ± 197 | 209 ± 28 | 6,856 ± 564 | 2,580 ± 191 | 15 | 20 | 5 | — | 71.8 | — |
| M, 58 | 1,500 ± 699 | 137 ± 16 | 13,404 ± 2,136 | 8,013 ± 1,683 | — | — | — | 40.8 | 120 | 81.2 |
| M, 37 | 727 ± 295 | 249 ± 25 | 13,433 ± 2,887 | 3,606 ± 1,665 | — | — | 5 | — | — | — |
| M, 24 | 409 ± 75 | 280 ± 36 | 55,579 ± 6,604 | 12,377 ± 769 | — | — | — | — | 25 | 5 |
| Resistant | ||||||||||
| M, 30 | 163 ± 15 | 290 ± 10 | 21,780 ± 4,983 | 6,098 ± 330 | — | — | — | — | — | — |
| M, 28 | 123 ± 48 | 292 ± 56 | 20,414 ± 7,305 | 3,500 ± 296 | — | — | — | 5 | 20 | — |
| M, 18 | 199 ± 39 | 681 ± 46 | 12,500 ± 4,671 | 4,365 ± 1,097 | — | — | — | — | 30 | — |
| M, 30 | 351 ± 126 | 2,343 ± 383 | 99,441 ± 11,259 | 34,346 ± 2,713 | 15 | ND | ND | 92.7 | ND | ND |
| M, 34 | 1,641 ± 534 | 9,767 ± 3,093 | 43,716 ± 3,571 | 24,774 ± 1,198 | 5 | ND | ND | 71.8 | ND | ND |
Representative male (M) and female (F) control donors and individuals showing extremes of susceptibility or resistance after parasitological cure of previous infection with S. mansoni were assayed for proliferation and cytokine response of PBMC following in vitro stimulation with rSG3PDH, SAWAm, and SEAm.
Significance of differences between means of antigen-free and test cultures was evaluated by Student's t test, and cultures showing positive responses (P < 0.05 to <0.0001) are underlined.
—, <5 pg/ml.
ND, not done.
TABLE 2.
Proliferation and production of IL-4 and IFN-γ by PBMC from S. haematobium group donors stimulated in vitro with rSG3PDH or parasite antigensa
| Donor (gender, age [yr]) | Proliferative (mean cpm ± SD) in response tob:
|
IL-4 (pg/ml) in response to:
|
IFN-γ (pg/ml) in response to:
|
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Medium | rSG3PDH | SAWAh | SEAh | rSG3PDH | SAWAh | SEAh | rSG3PDH | SAWAh | SEAh | |
| Control | ||||||||||
| M, 25 | 247 ± 34 | 94 ± 11 | 153 ± 21 | 101 ± 34 | —c | — | — | — | — | — |
| M, 20 | 68 ± 11 | 47 ± 8 | 71 ± 26 | 80 ± 36 | — | — | — | — | — | — |
| M, 40 | 73 ± 20 | 126 ± 38 | 112 ± 22 | NDd | — | — | ND | — | — | ND |
| Susceptible | ||||||||||
| M, 25 | 105 ± 26 | 48 ± 19 | 828 ± 301 | 1,814 ± 176 | — | — | 58 | — | — | 12 |
| M, 28 | 46 ± 18 | 41 ± 3 | 403 ± 55 | 734 ± 81 | — | — | 20 | — | — | 5 |
| M, 15 | 126 ± 33 | 88 ± 21 | 508 ± 55 | 827 ± 259 | — | — | — | — | — | — |
| M, 30 | 97 ± 31 | 57 ± 10 | 894 ± 290 | 196 ± 248 | — | — | — | — | — | 50 |
| M, 16 | 106 ± 20 | 171 ± 21 | 2,109 ± 616 | ND | — | 25 | ND | — | 95 | ND |
| Resistant | ||||||||||
| M, 30 | 56 ± 12 | 156 ± 11 | 651 ± 100 | 596 ± 42 | — | — | — | 15 | 28 | 48 |
| M, 24 | 21 ± 7 | 121 ± 38 | 138 ± 15 | ND | 5 | 5 | ND | 8 | — | ND |
| M, 26 | 122 ± 30 | 201 ± 8 | 711 ± 145 | ND | — | — | ND | 70 | 65 | ND |
| M, 55 | 75 ± 28 | 125 ± 9 | 388 ± 90 | ND | — | — | ND | 220 | 10 | ND |
| M, 40 | 68 ± 30 | 168 ± 48 | 577 ± 125 | ND | 12 | 10 | ND | 95 | 470 | ND |
Representative male (M) and female (F) control donors and individuals showing extremes of susceptibility or resistance after parasitological cure of previous infection with S. haematobium were assayed for proliferation and cytokine response of PBMC following in vitro stimulation with rSG3PDH, SAWAh, and SEAh.
Significance of differences between means of antigen-free and test cultures was evaluated by Student's t test, and cultures showing positive responses (P < 0.05 to <0.0001) are underlined.
—, <5 pg/ml.
ND, not done.
In vitro IL-4 and IFN-γ responses to rSG3PDH.
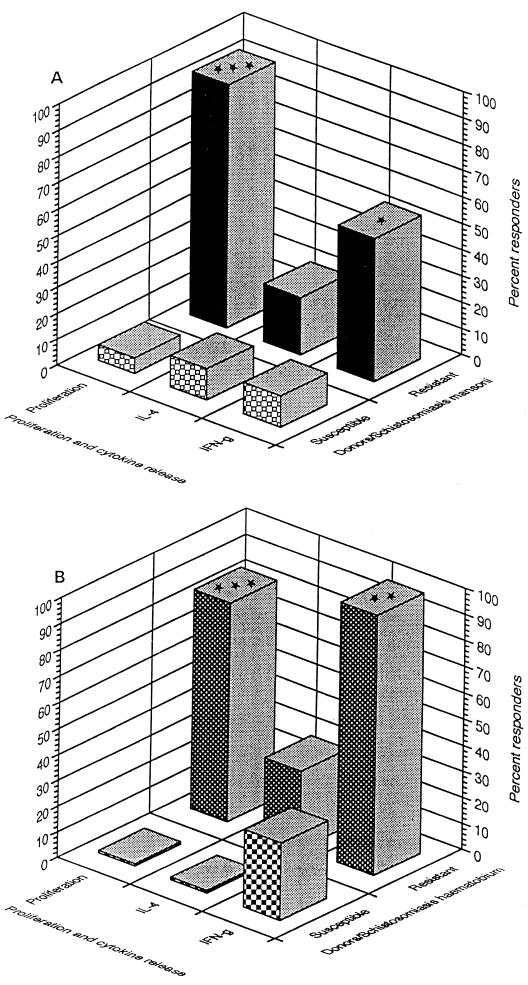
IL-4 production was elicited in response to in vitro stimulation with rSG3PDH in PBMC from one of eight donors susceptible to reinfection with S. mansoni and two of nine resistant subjects, i.e., 12 and 22%, respectively. The difference in percentage of responders was not significant as assessed by Fisher's exact test. Only one of eight susceptible subjects (12%) tested responded to rSG3PDH by IFN-γ production, whereas six of nine resistant donors tested (66%) produced detectable levels of IFN-γ (P < 0.05) (Table 1; Fig. 3A). Essentially similar findings were again obtained with the S. haematobium groups, as none of 10 susceptible and 3 of 10 resistant donors tested produced detectable levels of IL-4 in response to rSG3PDH. Three of 10 susceptible (30%) and 10 of 10 (100%) resistant subjects tested produced 5 to 220 pg of IFN-γ per ml in response to rSG3PDH. The difference in percentage of responders was highly significant (P = 0.003) (Table 2; Fig. 3B).
FIG. 3.
Cellular responses to rSG3PDH. Columns represent the percentage of susceptible and resistant individuals from the S. mansoni (A) and S. haematobium (B) groups responding to rSG3PDH by lymphoproliferation and production of IL-4 and IFN-γ. Significance of differences in percent responders among resistant and susceptible donors was analyzed by Fisher's exact test. ∗, P < 0.05; ∗∗, P < 0.005; ∗∗∗, P < 0.0005.
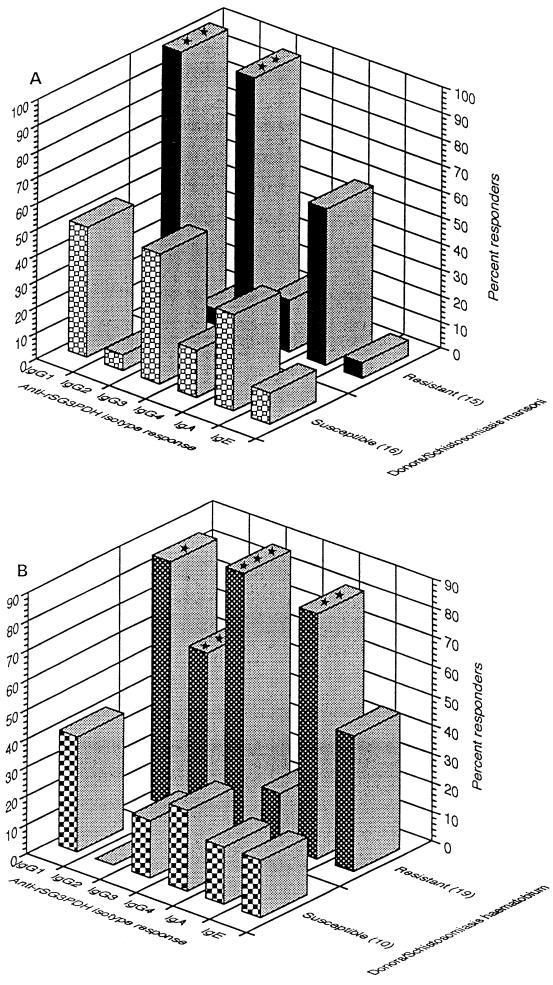
Antibody responses to SG3PDH in ELISA.
Plasma samples from all donors were examined for antibody recognition of rSG3PDH by coating ELISA plates with the antigen and measuring the amount of binding for IgG subclass (γ1, γ2, γ3, or γ4), IgA, and IgE antibodies. The results of three separate experiments indicated that the levels of IgG1 and IgG3 antibodies recognizing rSG3PDH were significantly (P = 0.002) higher among resistant than susceptible donors with schistosomiasis mansoni (Fig. 4A). Specific antibodies of the IgG2 and IgE isotypes were scarcely detected in the plasma from either susceptible or resistant individuals. As for the S. haematobium groups, presence of detectable levels of circulating IgG1 (P = 0.03), IgG2 (P = 0.0035), IgG3 (P = 0.0004), and IgA (P = 0.0013), but not IgE (P = 0.23), antibodies to rSG3PDH appeared to characterize the subjects resistant to reinfection (Fig. 4B). IgG4 antibodies did not recognize rSG3PDH in serum from virtually all S. mansoni and S. haematobium group subjects (Fig. 4).
FIG. 4.
Humoral isotype response to rSG3PDH. Columns represent the percentage of susceptible and resistant individuals from the S. mansoni (A) and S. haematobium (B) groups producing antibodies to rSG3PDH as assessed by ELISA. The total number of individuals tested is shown in parentheses. Significance of differences in percent responders among resistant and susceptible donors was analyzed by Fisher's exact test. ∗, P < 0.05; ∗∗, P < 0.005; ∗∗∗, P < 0.0005.
DISCUSSION
In a previous report, we demonstrated that the p42 SAWA band induced proliferation and production of cytokines selectively in PBMC from subjects putatively resistant to reinfection with S. mansoni or S. haematobium. We also showed that p42 preparations consist almost entirely of SG3PDH (18). Here we show that the same immune correlations with human resistance to schistosomiasis exist when rSG3PDH is the test antigen. This strongly suggests that SG3PDH is the protein responsible for the immune correlations in p42 preparations. The results are also entirely consistent with the findings of Goudot-Crozel et al. (22), who examined the correlation of humoral immune responses to rSG3PDH to resistance in 10- to 19-year-old schistosomiasis mansoni patients from Brazil. We have extended the results from Brazilian patients by also demonstrating lymphoproliferative and IFN-γ response correlations to resistance, in adult individuals, to both schistosomiasis mansoni and schistosomiasis haematobium. The failure of the majority of susceptible donors to respond to rSG3PDH could not be ascribed to altered or suppressed immune responses to schistosome antigens, as these individuals exhibited powerful lymphoproliferation to both SAWA and SEA. The few susceptible individuals who responded to rSG3PDH with lymphoproliferation or production of IL-4 or IFN-γ had heavy schistosome egg burden at the time of testing, further supporting the contention that heavy infection with schistosomes does not explain the lack of immune response to rSG3PDH. Failure to respond to rSG3PDH could possibly be due to lack of immune T-cell recognition of the molecule. SG3PDH shows 72% identity at the amino acid level with the human enzyme (22) and thus may have limited non-self T-cell epitopes capable of inducing immune responses in humans. The low number of T-cell epitopes on SG3PDH (2) and the well-characterized genetic restriction of mammalian hosts to protein T-cell epitopes (17, 22) may explain why a substantial proportion of humans do not recognize this molecule.
The majority of the susceptible and resistant subjects tested failed to produce IL-4 following in vitro stimulation with rSG3PDH, thus corroborating and extending the results obtained with the SAWA p42 band (18). The failure to produce IL-4 did not appear to be SG3PDH specific, however, since very few of the resistant and susceptible individuals tested produced detectable levels of IL-4 in response to SAWA and SEA.
It is intriguing that most schistosomiasis patients whose T cells proliferate and produce IFN-γ in response to rSG3PDH showed lack of reinfection with S. mansoni or S. haematobium. This correlation suggests the possibility that SG3PDH may play a role in protecting individuals from infection, but this remains to be demonstrated. A possible mechanism is that the parasite enzyme could elicit the generation of immune effector cells and molecules that prevent the maturation of invading larvae. SG3PDH occurs in cercariae and schistosomula of S. mansoni (22, 33). IFN-γ, which is produced by resistant individuals in response to SG3PDH, is considered an essential component of immune protection against schistosomes because it may promote inflammatory foci around invading schistosomula or may activate macrophages and other effector cells to kill the parasites (11).
In contrast to the susceptible patients, virtually all resistant individuals had serum IgG antibodies to rSG3PDH, dominated largely by the IgG1 and IgG3 isotypes. Human IgG1 and IgG3 antibodies are the most efficient antibodies in binding to the FcγR1, RcγRII, and FcγRIII receptors on monocytes, macrophages, and natural killer cells and in triggering cell-mediated cytotoxicity (26). These antibodies might mediate antibody-dependent cell-mediated cytotoxicity against invading larvae since it has been reported that SG3PDH is present on the surface of newly transformed schistosomula (22). Alternatively, schistosomula attacked by IFN-γ-activated macrophages might suffer disruption of the tegument and consequently express the cytosolic enzyme for antibody binding. Antibody might mediate antibody-dependent cell-mediated cytotoxicity or impair the metabolic activities of the parasite by SG3PDH inhibition.
Several reports have documented an association between IgE responses to schistosome antigens and resistance to reinfection, mostly in young individuals (12, 15, 16, 24, 30, 39). Other reports and ours are not consistent with this view, possibly because of the difference in the age range of the individuals examined (38). In our study, IgE to rSG3PDH was scarcely detected in serum from S. mansoni-susceptible or -resistant individuals. It was found in a percentage of subjects susceptible and resistant to reinfection with S. haematobium, but the difference was not significant. In this context, it is interesting that a schistosomular protein, later identified as SG3PDH, also did not appear as a major ligand for IgE from schistosomiasis mansoni-exposed humans in Western blotting (13, 30). Thus, our studies suggest that the putative SG3PDH-related resistance to infection does not depend on IgE-mediated protective mechanisms in both schistosomiasis mansoni and schistosomiasis haematobium. However, IgE to whole worm antigens might have a role in protection against schistosomiasis haematobium (24, 28).
In conclusion, the data of the present and previous (13, 14, 18, 22) reports demonstrate an association between T- and B-cell immune responses to SG3PDH and resistance of humans to schistosomiasis. The results suggest that this antigen may play a role in prevention of schistosome reinfection.
ACKNOWLEDGMENT
This work was supported in part by Egyptian Ministry of Health- and USAID-funded Schistosomiasis Research Project 263-0140.2 grant 12-01-05.
REFERENCES
- 1.Al-Sherbiny M, El Ridi R, Guirguis N, Dean D A. Identification and characterization of Schistosoma mansoni antigens recognized by T and B lymphocytes of humans with early active intestinal and/or urinary schistosomiasis. Int J Parasitol. 1995;25:113–121. doi: 10.1016/0020-7519(94)e0067-w. [DOI] [PubMed] [Google Scholar]
- 2.Argiro L, Kohlstadt S, Henri S, Dessein H, Matabiau V, Paris P, Bourgois A, Dessein A J. Identification of a candidate vaccine peptide on the 37 kDa Schistosoma mansoni GAPDH. Vaccine. 2000;18:2039–2048. doi: 10.1016/s0264-410x(99)00521-6. [DOI] [PubMed] [Google Scholar]
- 3.Armstrong R L, Wilson J E, Shoemaker C B. Purification and characterization of the hexokinase from Schistosoma mansoni, expressed in Escherichia coli. Protein Expression Purif. 1996;8:374–380. doi: 10.1006/prep.1996.0113. [DOI] [PubMed] [Google Scholar]
- 4.Bennett J L, Day T, Feng-Tao L, Ismail M, Farghaly A. The development of resistance to anthelmintics: a perspective with an emphasis on the antischistosomal drug praziquantel. Exp Parasitol. 1997;87:260–267. doi: 10.1006/expr.1997.4229. [DOI] [PubMed] [Google Scholar]
- 5.Brindley P J. Drug resistance to schistosomicides and other anthelmintics of medical significance. Acta Trop. 1994;56:213–231. doi: 10.1016/0001-706x(94)90064-7. [DOI] [PubMed] [Google Scholar]
- 6.Butterworth A E, Hagan P. Immunity in human schistosomiasis. Parasitol Today. 1987;3:11–16. doi: 10.1016/0169-4758(87)90091-3. [DOI] [PubMed] [Google Scholar]
- 7.Butterworth A E, Capron M, Cordingley J S, Dalton P R, Dunne D W, Kariuki H C, Kimani G, Koech D, Mugambi M, Ouma J H, Prentice M A, Richardson B A, Arap Siongok T K, Sturrock R F, Taylor D W. Immunity after treatment of human schistosomiasis mansoni. II. Identification of resistant individuals, and analysis of their immune responses. Trans R Soc Trop Med Hyg. 1985;79:393–408. doi: 10.1016/0035-9203(85)90391-8. [DOI] [PubMed] [Google Scholar]
- 8.Butterworth A E, Wilkins H A, Capron A, Sher A. The control of schistosomiasis: is a vaccine necessary? Parasitol Today. 1987;3:1–2. doi: 10.1016/0169-4758(87)90086-x. [DOI] [PubMed] [Google Scholar]
- 9.Charrier-Ferrara S, Caillol D, Goudot-Crozel V. Complete sequence of the Schistosoma mansoni glyceraldehyde-3-phosphate dehydrogenase gene encoding a major surface antigen. Mol Biochem Parasitol. 1992;56:339–343. doi: 10.1016/0166-6851(92)90184-l. [DOI] [PubMed] [Google Scholar]
- 10.Cioli D, Pica-Mattoccia L, Archer S. Antischistosomal drugs: past, present… and future? Pharmacol Ther. 1995;68:35–85. doi: 10.1016/0163-7258(95)00026-7. [DOI] [PubMed] [Google Scholar]
- 11.Coulson P S. The radiation-attenuated vaccine against schistosomes in animal models: paradigm for a human vaccine? Adv Parasitol. 1997;39:271–336. doi: 10.1016/s0065-308x(08)60048-2. [DOI] [PubMed] [Google Scholar]
- 12.Demeure C E, Rihet P, Abel L, Ouattara M, Bourgois A, Dessein A J. Resistance to Schistosoma mansoni in humans: influence of the IgE/IgG4 balance and IgG2 in immunity to reinfection after chemotherapy. J Infect Dis. 1993;168:1000–1008. doi: 10.1093/infdis/168.4.1000. [DOI] [PubMed] [Google Scholar]
- 13.Dessein A J, Abel L, Carvallo E M, Prata A. Environmental, genetic and immunological factors in human resistance to Schistosoma mansoni. Immunol Investig. 1992;21:423–453. doi: 10.3109/08820139209069383. [DOI] [PubMed] [Google Scholar]
- 14.Dessein A J, Begley M, Demeure C, Caillol D, Fueri J, Reis M G, Andrade Z A, Prata A, Bina J C. Human resistance to Schistosoma mansoni is associated with IgG reactivity to a 37-kDa larval surface antigen. J Immunol. 1988;140:2727–2736. [PubMed] [Google Scholar]
- 15.Dunne D W, Butterworth A E, Fulford A J C, Kariuki H C, Langley J G, Ouma J H, Capron A, Pierce R J, Sturrock R F. Immunity after treatment of human schistosomiasis: association between IgE antibodies to adult worm antigens and resistance to reinfection. Eur J Immunol. 1992;22:1483–1494. doi: 10.1002/eji.1830220622. [DOI] [PubMed] [Google Scholar]
- 16.Dunne D W, Webster M, Smith P, Langley J G, Richardson B A, Fulford A J C, Butterworth A E, Sturrock R F, Kariuki H C, Ouma J H. The isolation of a 22 kDa band after SDS-PAGE of Schistosoma mansoni adult worms and its use to demonstrate that IgE responses against the antigen(s) it contains are associated with human resistance to reinfection. Parasite Immunol. 1997;19:79–89. doi: 10.1046/j.1365-3024.1997.d01-186.x. [DOI] [PubMed] [Google Scholar]
- 17.El Ridi R, Abdel Tawab N, Guirguis N. Schistosoma mansoni: identification and protective immunity of adult worm antigens recognized by T lymphocytes of outbred Swiss mice immunized with irradiated cercariae. Exp Parasitol. 1993;76:265–277. doi: 10.1006/expr.1993.1032. [DOI] [PubMed] [Google Scholar]
- 18.El Ridi R, Farouk F, Sherif M, Al-Sherbiny M, Osman A, El Gengehi N, Shoemaker C B. T and B cell reactivity to a 42 kDa protein is associated with human resistance to both schistosomiasis mansoni and haematobium. J Infect Dis. 1998;177:1364–1372. doi: 10.1086/515274. [DOI] [PubMed] [Google Scholar]
- 19.El Ridi R, Ismail S, Gaafar T, El Demellawy M. Differential responsiveness of humans with early-stage schistosomiasis haematobium to Schistosoma haematobium soluble adult worm and egg antigens. Parasitol Res. 1997;83:471–480. doi: 10.1007/s004360050282. [DOI] [PubMed] [Google Scholar]
- 20.Fallon P G, Sturrock R F, Capron A, Niang M, Doenhoff M J. Diminished susceptibility to praziquantel in a Senegal isolate of Schistosoma mansoni. Am J Trop Med Hyg. 1995;53:61–67. [PubMed] [Google Scholar]
- 21.Farid Z. Schistosomes with terminal-spined eggs: pathological and clinical aspects. In: Jordan P, Webbe G, Sturrock R F, editors. Human schistosomiasis. Wallingford, United Kingdom: CAB International; 1993. pp. 159–193. [Google Scholar]
- 22.Goudot-Crozel V, Caillol D, Djabali M, Dessein A J. The major parasite surface antigen associated with human resistance to schistosomiasis is a 37-kD glyceraldehyde-3P-dehydrogenase. J Exp Med. 1989;170:2065–2080. doi: 10.1084/jem.170.6.2065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gryseels B. Human resistance to Schistosoma infections: age or experience? Parasitol Today. 1994;10:380–384. doi: 10.1016/0169-4758(94)90226-7. [DOI] [PubMed] [Google Scholar]
- 24.Hagan P, Blumenthal U J, Dunn D, Simpson A J G, Wilkins H A. Human IgE, IgG4 and resistance to reinfection with Schistosoma haematobium. Nature. 1991;349:243–245. doi: 10.1038/349243a0. [DOI] [PubMed] [Google Scholar]
- 25.He R-Q, Yang M-D, Zheng X, Zhou J-X. Isolation and some properties of glycated d-glyceraldehyde-3-phosphate dehydrogenase from rabbit muscle. Biochem J. 1995;309:133–139. doi: 10.1042/bj3090133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Male D, Cooke A, Owen M, Trowsdale J, Champion B, editors. Advanced immunology. London, United Kingdom: Mosby; 1996. [Google Scholar]
- 27.Montero R, Ostrosky P. Genotoxic activity of Praziquantel. Rev Mutat Res. 1997;387:123–139. doi: 10.1016/s1383-5742(97)00027-6. [DOI] [PubMed] [Google Scholar]
- 28.Ndhlovu P, Cadman H, Vennervald B J, Christensen N Ø, Chidimu M, Chandiwana S K. Age-related antibody profiles in Schistosoma haematobium infections in a rural community in Zimbabwe. Parasite Immunol. 1996;18:181–191. doi: 10.1046/j.1365-3024.1996.d01-78.x. [DOI] [PubMed] [Google Scholar]
- 29.Polderman A M, Manshande J P. Failure of targeted mass treatment to control schistosomiasis. Lancet. 1981;1:27–28. doi: 10.1016/s0140-6736(81)90127-6. [DOI] [PubMed] [Google Scholar]
- 30.Rihet P, Demeure C E, Bourgois A, Prata A, Dessein A J. Evidence for an association between human resistance to Schistosoma mansoni and high anti-larval IgE levels. Eur J Immunol. 1991;21:2679–2686. doi: 10.1002/eji.1830211106. [DOI] [PubMed] [Google Scholar]
- 31.Savioli L, Renganathan E, Montresor A, Davis A, Behbehani K. Control of schistosomiasis—a global picture. Parasitol Today. 1997;13:444–448. doi: 10.1016/s0169-4758(97)01141-1. [DOI] [PubMed] [Google Scholar]
- 32.Shoemaker C, Gross A, Gebremichael A, Harn D. cDNA cloning and functional expression of the Schistosoma mansoni protective antigen triose-phosphate isomerase. Proc Natl Acad Sci USA. 1992;89:1842–1846. doi: 10.1073/pnas.89.5.1842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Skelly P J, Stein L D, Shoemaker C B. Expression of Schistosoma mansoni genes involved in anaerobic and oxidative glucose metabolism during the cercarial to adult transformation. Mol Biochem Parasitol. 1993;60:93–104. doi: 10.1016/0166-6851(93)90032-s. [DOI] [PubMed] [Google Scholar]
- 34.Sturrock R F. The parasites and their life cycles. In: Jordan P, Webbe G, Sturrock R F, editors. Human schistosomiasis. Wallingford, United Kingdom: CAB International; 1993. pp. 1–32. [Google Scholar]
- 35.Tanner M, Evans D. Vaccines or drugs: complementarity is crucial. Parasitol Today. 1994;10:406–407. doi: 10.1016/0169-4758(94)90235-6. [DOI] [PubMed] [Google Scholar]
- 36.Towbin H, Staehlin T, Gordon J. Electrophoretic transfer of proteins from acrylamide gels to nitrocellulose sheets: procedure and some applications. Proc Natl Acad Sci USA. 1979;76:4350–4354. doi: 10.1073/pnas.76.9.4350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Warren K S. The immunopathology of schistosomiasis: a multidisciplinary approach. Trans R Soc Trop Med Hyg. 1972;66:417–434. doi: 10.1016/0035-9203(72)90273-8. [DOI] [PubMed] [Google Scholar]
- 38.Webster M, Correa-Oliveira R, Gazzinelli G, Viana I R C, Fraga L A D O, Silveira A M S, Dunne D W. Factors affecting high and low human IgE responses to schistosome worm antigens in an area of Brazil endemic for Schistosoma mansoni and hookworm. Am J Trop Med Hyg. 1997;57:487–494. doi: 10.4269/ajtmh.1997.57.487. [DOI] [PubMed] [Google Scholar]
- 39.Webster M, Fulford A J C, Braun G, Ouma J H, Kariuki H C, Havercroft J C, Gachuhi K, Sturrock R F, Butterworth A E, Dunne D W. Human immunoglobulin E responses to a recombinant 22.6-kilodalton antigen from Schistosoma mansoni adult worms are associated with low intensities of reinfection after treatment. Infect Immun. 1996;64:4042–4046. doi: 10.1128/iai.64.10.4042-4046.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wilkins H A. Reinfection after treatment of schistosome infections. Parasitol Today. 1989;5:83–87. doi: 10.1016/0169-4758(89)90008-2. [DOI] [PubMed] [Google Scholar]
- 41.Wilkins H A, Blumenthal U J, Hagan P, Hayes R J, Tulloch S. Resistance to reinfection after treatment of urinary schistosomiasis. Trans R Soc Trop Med Hyg. 1987;81:29–35. doi: 10.1016/0035-9203(87)90273-2. [DOI] [PubMed] [Google Scholar]