Abstract
Background: The recent human monkeypox virus (HMPXV) outbreak in non-endemic countries that started in May 2022 has raised concerns among public health authorities worldwide. Healthcare workers (HCWs) play a decisive role during epidemics in transmitting accurate information to the public and motivating them to pursue protective behaviours, including immunisation. Methods: A cross-sectional survey-based study was conducted in the Czech Republic in September 2022 to evaluate HMPXV-related knowledge and vaccination perceptions among HCWs. The study utilised a digital self-administered questionnaire (SAQ) to collect data from the target population. The proposed SAQ inquired about participants’ sociodemographic and anamnestic characteristics, perceived knowledge of HMPXV, factual knowledge, and vaccination perceptions according to the health belief model (HBM). Results: A total of 341 participants were included in this study; most of them were females (88.9%), allied HCWs (89.4%), heterosexuals (87.1%), married (61.9%), and vaccinated against COVID-19 (91.2%). Only 8.8% of the participants agreed to receive vaccination against HMPXV; 44.9% rejected it, while 46.3% were hesitant. While digital news portals (47.5%) and social media (25.8%) were among the most utilised sources of information about HMPXV, the scientific journals (5.6%), ECDC (5%), and the U.S. CDC (1.5%) were the least common sources. The participants demonstrated suboptimal levels of factual knowledge, especially regarding HMPXV vaccines (1.5 ± 1.2 (0–4)) and treatments (0.9 ± 0.9 (0–4)). Additionally, several misconceptions were detectable among the participants, regarding topics such as the availability of effective vaccines and antivirals against HMPXV, the risk of vertical transmission, and homosexual stigmatisation. The HBM indicated that the cues to action and perceived susceptibility were the most important constructs to predict HMPXV vaccine acceptance. Conclusions: the findings of this study call upon public health practitioners and health policymakers in the Czech Republic to act accordingly in order to determine the drivers of vaccine hesitancy among Czech HCWs. Dedicated educational campaigns should aim to counter the HCWs’ misconceptions around HMPXV, and future studies should aim to explore the prevalence and drivers of HMPXV vaccine hesitancy among the general population.
Keywords: cross-sectional studies, Czech Republic, disease outbreaks, health belief model, health personnel, knowledge, monkeypox, smallpox vaccine, vaccination hesitancy
1. Introduction
While the world is still challenged by the coronavirus disease (COVID-19) pandemic, the emergence of a new outbreak caused by the human monkeypox virus (HMPXV) has raised global concerns among public health authorities [1]. HMPXV is a viral zoonosis with clinically less severe symptoms than previously reported in patients with smallpox [2]. As smallpox was eradicated in 1980 and the vaccination against this disease has subsequently ceased, HMPXV has emerged as the most important orthopoxvirus for public health [2]. HMPXV is a disease of global public health importance, as it affects not only countries in West and Central Africa—where it is endemic—but also the rest of the world [2]. Since May 2022, there have been multiple cases of HMPXV identified in non-endemic countries, which has led to an intensive investigation at both international and national levels for a better understanding of its infection sources and transmission patterns [2,3]. Subsequently, the World Health Organization (WHO) declared the global HMPXV outbreak as a public health emergency of international concern on 23 July 2022 [4]. As of 21 November 2022, 80,328 laboratory-confirmed cases of HMPXV have been identified worldwide, including 70 cases in the Czech Republic [5].
Healthcare workers (HCWs) are considered to be a high-risk group for infectious disease transmission by the centres of disease control in the European Union (EU) and the United States (US) [2,6]. In order to stop human-to-human transmission and to minimise zoonotic transmission of HMPXV, vaccination can be used as a primary method of prevention [4]. According to the WHO’s interim guidance on vaccines and immunisation for HMPXV, updated on 24 August 2022, mass vaccination was not recommended nor required for HMPXV at that moment [4]. Meanwhile, the WHO recommended that pre-exposure prophylaxis (PrEP) should be administered to high-risk groups, including (a) HCWs at high risk of exposure, (b) laboratory personnel working with orthopoxviruses, (c) clinical laboratory personnel performing diagnostic testing for HMPXV, and (d) outbreak response team members (as designated by national public health authorities) [4]. Thus, the risk could be perceived as higher in bedside allied HCWs helping patients with basic daily activities (e.g., washing patients and making beds).
A high-risk exposure can be defined as “direct exposure of the skin or mucous membranes to the skin or respiratory secretions of a person with HMPXV, their body fluids or potentially infectious material including clothing and bedding, without appropriate personal protective equipment (PPE)”. Therefore, high-risk exposure is predictable within clinical settings through various sources such as inhalation of droplets, mucosal exposure to splashes, and penetrating sharp injuries. The spread of HMPXV from person to person has been known to generally require prolonged close contact, such as face-to-face contact in close proximity or skin-to-skin physical contact. Such exposure can easily occur in healthcare settings, which puts HCWs at risk of contracting the disease [4].
Some endemic countries for HMPXV (such as the Democratic Republic of the Congo) have launched routine HMPXV surveillance, where one of the main parts of this procedure is to enhance the capacity of HCWs to identify cases and improve patient management [7]. Hence, HCWs should have sufficient knowledge of HMPXV in order to be able to immediately identify, report, and manage new cases to prevent further transmission. Considering that the Czech Republic has not been endemic for HMPXV, there might be a lack of knowledge on this particular disease among HCWs, since it has not been deeply studied and explained in educational institutions. As in Indonesia, general practitioners had low knowledge of HMPXV in 2020 [8]. In addition, it was mentioned in the WHO’s report that one of the challenges faced in preventing the re-emergence of HMPXV was a lack of knowledge—particularly among HCWs [9]. Since cases of HMPXV have already been registered in the Czech Republic, it is crucial for HCWs to be informed, knowledgeable, and prepared for HMPXV case management. HCWs play an instrumental role in primary prevention and health promotion; therefore, their knowledge about emerging infectious diseases may influence their perceptions and attitudes towards their patients during these critical times [10]. In addition, vaccine hesitancy among HCWs can not only slow down the public health strategies that aim to protect high-risk groups and individuals, but it may also undermine public confidence in vaccines for orthopoxviruses.
The overarching goal of this study was to evaluate levels of HMPXV-related knowledge and HMPXV vaccine perceptions among Czech HCWs. The primary objectives included (a) to assess the levels of perceived knowledge and factual knowledge about HMPXV, (b) to evaluate perceptions of vaccination against HMPXV according to the health belief model (HBM), and (c) to assess levels of HMPXV vaccine acceptance and willingness to pay for it. The secondary objectives were (a) to explore the potential sociodemographic and anamnestic predictors of HMPXV-related knowledge and HMPXV perceptions, and (b) to discover the knowledge gaps among Czech HCWs in terms of HMPXV.
2. Materials and Methods
2.1. Design
The present study was designed as an analytical cross-sectional study executed and reported according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines [11].
2.2. Settings
A survey-based study was carried out in September 2022, utilising a self-administered questionnaire (SAQ) to collect data from Czech HCWs about their human monkeypox virus (HMPXV)-related knowledge and vaccination perceptions. The SAQ was coded and disseminated online through KoBoToolbox (Harvard Humanitarian Initiative; Cambridge, MA, USA, 2022) [12].
2.3. Participants
The target population of the present study were Czech HCWs who may/may not provide clinical care to HMPXV cases during the 2022 outbreak.
The inclusion criteria were (i) to be a full-time or part-time employee at a healthcare provider in the Czech territories, and (ii) to be responsible for providing clinical services. The exclusion criteria were (i) to be administrative, economic, or legal staff working at Czech healthcare providers; (ii) to be research personnel uninvolved in providing clinical care; and (iii) to be an undergraduate healthcare student.
A non-random sampling strategy utilising the snowballing technique was used to recruit respondents from the target population. Official email invitations were sent to the heads of Czech medical societies that are members of the Czech Medical Association of J. E. Purkyně (CzMA), as well as the managers of inpatient healthcare facilities within the network of the Central Adverse Events Reporting System of the Institute of Health Information and Statistics of the Czech Republic (IHIS-CR; Prague, Czech Republic), in order to facilitate participation in the study by circulating the survey’s uniform resource locator (URL) through their respective networks. In addition, online advertisements and blog posts were published by the official websites of the Czech Ministry of Health (MoH) and the Faculty of Medicine, Masaryk University (MED-MUNI) [13,14].
The minimum sample size required for this study was estimated using Epi InfoTM version 7.2.5 (CDC, Atlanta, GA, USA, 2021) utilising the following assumptions: (i) confidence level (CI): 95%; (ii) acceptable error margin: 5%; (iii) target population size: >250,000 [15], and (iv) expected frequency of the primary outcome (i.e., HMPXV vaccine acceptance): 70% [16].
At least 322 valid responses were required to establish an inference between putative demographic and anamnestic predictors and the current intentions of Czech HCWs to receive an HMPXV vaccine. A total of 344 responses were received, out of which only 3 were excluded because of a lack of consent and/or information (Figure S1).
2.4. Instrument
The SAQ of this study consisted of 55 closed-ended items divided into eight categories:
-
(i)
Sociodemographic characteristics: gender, sexual orientation, age, profession, marital status, having minors (≤18 years old), and providing care to HMPXV patients.
-
(ii)
Anamnestic characteristics: chronic illnesses, regular medications, COVID-19 vaccination, and seasonal influenza vaccination.
-
(iii)
HMPXV information sources: undergraduate education, information sources and their confidence levels.
-
(iv)
HMPXV perceived knowledge: HMPXV epidemiology, clinical presentation, risk factors, vaccination, and treatment.
-
(v)
HMPXV factual knowledge: HMPXV epidemiology, clinical presentation, risk factors, vaccination, and treatment.
-
(vi)
HMPXV vaccine perceptions according to the health belief model (HBM): perceived susceptibility, perceived severity, perceived benefits, perceived barriers, and cues to action.
-
(vii)
HMPXV vaccine intentions: acceptance and recommendation to others.
-
(viii)
Willingness to pay (WTP) for HMPXV vaccine.
The draft SAQ was developed according to published studies on HMPXV and HMPXV vaccines among HCWs and other population groups [17,18,19,20]. The content validity of the draft SAQ had been evaluated by a committee of experts in public health, infectious diseases, and health psychology, who provided feedback and suggested modifications for the final version. The construct’s validity was checked by confirmatory factor analysis (CFA), which suggested a good fit of the model (TLI: 0.904; RMSEA: 0.046—CI 95%: 0.040–0.051).
2.5. Measures
The level of confidence in sources of HMPXV information was evaluated by a 7-point Likert scale ranging from (extremely unreliable = 1) to (extremely reliable = 7). Similarly, the HMPXV perceived knowledge items, the HBM items, and the HMPXV vaccine intentions were rated using 5-point Likert scales ranging from (strongly disagree = 1) to (strongly agree = 5).
A total of 15 multiple-choice questions (MCQs) were used to evaluate the HMPXV factual knowledge of the participants—3 items for each knowledge domain. Out of these 15 MCQs, 10 items had a single correct answer, which gave them a binary rating (true = 1; false = 0). Five MCQs had more than one correct answer; therefore, their rating had three levels (advanced knowledge = 2; acceptable knowledge = 1; no knowledge = 0).
2.6. Ethics
The Ethical Committee of the Faculty of Medicine, Masaryk University, reviewed and approved the protocol of this study on 19 September 2022, with the reference number 73/2022. The Declaration of Helsinki and the European Union (EU)’s General Data Protection Regulation (GDPR) were followed during data collection and processing [21,22].
2.7. Analyses
The categorical variables—such as gender, sexual orientation, and profession—were reported using frequencies (n) and percentages (%), while ordinal and numerical variables—such as confidence levels, perceptions, and knowledge scores—were reported using means and standard deviations (µ ± SD). The normal distribution of numerical and ordinal variables was tested using the Shapiro–Wilk test with a significance level (p) ≤ 0.05. Inferential statistics were performed using the chi-squared (χ2) test, Fisher’s exact test, analysis of variance (ANOVA), the Kruskal–Wallis (H) test, and the Mann–Whitney (U) test with p ≤ 0.05. The model fit of the HBM was evaluated using structural equation modelling (SEM). All statistical analyses were executed through the Statistical Package for Social Sciences (SPSS) version 28.0 (SPSS Inc. Chicago, IL, USA, 2020) and the R-based open software jamovi [23,24].
3. Results
3.1. Demographic Characteristics
A total of 341 participants were included in this study, out of which females were the majority (88.9%), followed by males (9.7%) and participants who rejected to disclose their gender identity (1.5%). Regarding the sexual orientation of the participants, the majority were heterosexuals (87.1%), followed by homosexuals (2.3%), bisexuals (1.5%), and non-disclosing participants (9.1%). The mean age of the study sample was 46.1 ± 12.0 years old, and the most common marital statuses were being married (61.9%), single (19.1%), and divorced (12%).
While most participants were allied HCWs (89.4%), only 4.7% reported that they were either currently or potentially providing clinical care to monkeypox patients. More than 37% of the participants reported having minors (below 18 years old) (Table 1).
Table 1.
Demographic characteristics of Czech HCWs responding to the HMPXV survey, September 2022 (n = 341).
| Variable | Outcome | HMPXV Vaccine Rejection (n = 153) |
HMPXV Vaccine Hesitancy (n = 158) |
HMPXV Vaccine Acceptance (n = 30) |
Total (n = 341) |
p |
|---|---|---|---|---|---|---|
| Gender | Female | 138 (90.2%) | 141 (89.2%) | 24 (80.0%) | 303 (88.9%) | 0.266 |
| Male | 14 (9.2%) | 13 (8.2%) | 6 (20.0%) | 33 (9.7%) | 0.161 | |
| I prefer not to say | 1 (0.7%) | 4 (2.5%) | 0 (0%) | 5 (1.5%) | 0.488 | |
| Sexual Orientation |
Heterosexual | 134 (87.6%) | 136 (86.1%) | 27 (90%) | 297 (87.1%) | 0.859 |
| Homosexual | 2 (1.3%) | 4 (2.5%) | 2 (6.7%) | 8 (2.3%) | 0.188 | |
| Bisexual | 3 (2%) | 1 (0.6%) | 1 (3.3%) | 5 (1.5%) | 0.214 | |
| I prefer not to say | 14 (14%) | 17 (10.8%) | 0 (0%) | 31 (9.1%) | 0.157 | |
| Age | µ ± SD | 45.9 ± 11.3 | 47.6 ± 12.0 | 39.9 ± 13.9 | 46.1 ± 12.0 | 0.026 |
| Marital Status | Single | 24 (15.7%) | 26 (16.5%) | 15 (50%) | 65 (19.1%) | <0.001 |
| Married | 99 (64.7%) | 99 (62.7%) | 13 (43.3%) | 211 (61.9%) | 0.085 | |
| Divorced | 19 (12.4%) | 20 (12.7%) | 2 (6.7%) | 41 (12%) | 0.772 | |
| Widow | 5 (3.3%) | 3 (1.9%) | 0 (0%) | 8 (2.3%) | 0.554 | |
| I prefer not to say | 6 (3.9%) | 10 (6.3%) | 0 (0%) | 16 (4.7%) | 0.340 | |
| Having Minors |
Yes | 65 (42.5%) | 58 (36.7%) | 4 (13.3%) | 127 (37.2%) | 0.010 |
| No | 88 (57.5%) | 100 (63.3%) | 26 (86.7%) | 214 (62.8%) | ||
| Location | South Moravian Region | 95 (62.1%) | 95 (60.1%) | 12 (40%) | 202 (59.2%) | 0.076 |
| Other regions | 58 (37.9%) | 63 (39.9%) | 18 (60%) | 139 (40.8%) | ||
| Profession | Medical | 11 (%) | 21 (%) | 4 (13.3%) | 36 (10.6%) | 0.163 |
| Allied HCWs | 142 (92.8%) | 137 (86.7%) | 26 (86.7%) | 305 (89.4%) | ||
| Providing Care |
Yes | 6 (3.9%) | 8 (5.1%) | 2 (6.7%) | 16 (4.7%) | 0.689 |
| No | 147 (96.1%) | 150 (94.9%) | 28 (93.3%) | 325 (95.3%) |
The chi-squared (χ2) test, Fisher’s exact test, and the Kruskal–Wallis (H) test were used with a significance level (p) of ≤0.05.
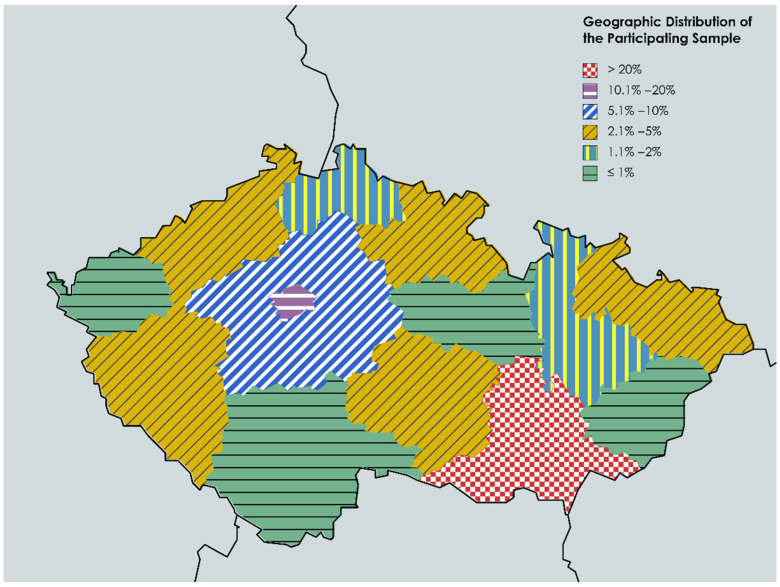
The South Moravian Region was the most represented geographical region (59.2%), followed by the capital city Prague (14.1%), the Central Bohemian Region (8.5%), and the Moravian–Silesian Region (3.5%). There was no statistically significant difference between South Moravian Region respondents and other regions’ respondents in terms of HMPXV vaccine acceptance (p = 0.076) (Figure 1).
Figure 1.
Geographic distribution of Czech HCWs participating in the HMPXV survey, September 2022 (n = 341).
3.2. Anamnestic Characteristics
When asked about their medical anamnesis, 38.7% and 47.2% of the participants reported suffering from at least one chronic illness and receiving at least one regular medication, respectively. Among the 132 participants with chronic conditions, the most common condition was chronic hypertension (31.1%), followed by thyroid disease (30.3%), allergy (28%), asthma (26.5%), and ophthalmologic disease (6.8%). Among the 161 participants who reported using regular medications, antihypertensive medications were the most common (34.8%), followed by thyroid hormones (27.3%), anti-asthmatics (18%), antihistamines (14.9%), and cholesterol-lowering drugs (13%).
The vast majority reported receiving a COVID-19 vaccination (91.2%), of whom 80.1% received three doses, 13.8% two doses, 4.5% four doses, and 1.6% one dose. About 38.4% of the participants received the influenza vaccine, of whom only 46.6% had received it within the last 12 months (Table 2).
Table 2.
Anamnestic characteristics of Czech HCWs responding to the HMPXV survey, September 2022 (n = 341).
| Variable | Outcome | HMPXV Vaccine Rejection (n = 153) |
HMPXV Vaccine Hesitancy (n = 158) |
HMPXV Vaccine Acceptance (n = 30) |
Total (n = 341) |
p |
|---|---|---|---|---|---|---|
| Total † | 58 (37.9%) | 63 (39.9%) | 11 (36.7%) | 132 (38.7%) | 0.912 | |
|
† Chronic Illnesses |
Allergy | 20 (34.5%) | 13 (20.6%) | 4 (36.4%) | 37 (28%) | 0.179 |
| Asthma | 16 (27.6%) | 15 (23.8%) | 4 (36.4%) | 35 (26.5%) | 0.634 | |
| Blood disease | 3 (5.2%) | 2 (3.2%) | 0 (0%) | 5 (3.8%) | 0.788 | |
| Bowel disease | 3 (5.2%) | 3 (4.8%) | 0 (0%) | 6 (4.5%) | 1.000 | |
| Cancer | 0 (0%) | 4 (6.3%) | 0 (0%) | 4 (3.0%) | 0.183 | |
| Cardiovascular disease | 1 (1.7%) | 3 (4.8%) | 1 (9.1%) | 5 (3.8%) | 0.280 | |
| Chronic hypertension | 19 (32.8%) | 20 (31.7%) | 2 (18.2%) | 41 (31.1%) | 0.718 | |
| COPD * | 1 (1.7%) | 2 (3.2%) | 1 (9.1%) | 4 (3.0%) | 0.381 | |
| Diabetes mellitus I | 0 (0%) | 1 (1.6%) | 0 (0%) | 1 (0.8%) | 1.000 | |
| Diabetes mellitus II | 4 (6.9%) | 2 (3.2%) | 0 (0%) | 6 (4.5%) | 0.662 | |
| Liver disease | 1 (1.7%) | 1 (1.6%) | 2 (18.2%) | 4 (3.0%) | 0.035 | |
| Psychological distress | 3 (5.2%) | 6 (9.5%) | 4 (36.4%) | 13 (9.8%) | 0.016 | |
| Neurological disorder | 3 (5.2%) | 7 (11.1%) | 3 (27.3%) | 13 (9.8%) | 0.071 | |
| Ophthalmologic disease | 4 (6.9%) | 5 (7.9%) | 0 (0%) | 9 (6.8%) | 1.000 | |
| Renal disease | 0 (0%) | 1 (1.6%) | 1 (9.1%) | 2 (1.5%) | 0.160 | |
| Rheumatoid arthritis | 3 (5.2%) | 2 (3.2%) | 0 (0%) | 5 (3.8%) | 0.788 | |
| Thyroid disease | 18 (31.0%) | 18 (28.6%) | 4 (36.4%) | 40 (30.3%) | 0.846 | |
| Other | 6 (10.3%) | 9 (14.3%) | 2 (18.2%) | 17 (12.9%) | 0.624 | |
| ‡ Medications | Total ‡ | 70 (45.8%) | 75 (47.5%) | 16 (53.3%) | 161 (47.2%) | 0.760 |
| Anti-asthmatics | 8 (11.4%) | 16 (21.3%) | 5 (31.3%) | 29 (18.0%) | 0.099 | |
| Anticoagulants | 3 (4.3%) | 2 (2.7%) | 0 (0%) | 5 (3.1%) | 0.807 | |
| Antidepressants | 5 (7.1%) | 6 (8.0%) | 6 (37.5%) | 17 (10.6%) | 0.006 | |
| Antidiabetics | 4 (5.7%) | 3 (4.0%) | 0 (0%) | 7 (4.3%) | 0.864 | |
| Antiepileptics | 1 (1.4%) | 1 (1.3%) | 1 (6.3%) | 3 (1.9%) | 0.450 | |
| Antihistamines | 15 (21.4%) | 8 (10.7%) | 1 (6.3%) | 24 (14.9%) | 0.139 | |
| Antihypertensives | 27 (38.6%) | 26 (34.7%) | 3 (18.8%) | 56 (34.8%) | 0.324 | |
| Anti-reflux | 5 (7.1%) | 6 (8.0%) | 3 (18.8%) | 14 (8.7%) | 0.295 | |
| Immunosuppressants | 2 (2.9%) | 4 (5.3%) | 0 (0%) | 6 (3.7%) | 0.832 | |
| Cholesterol-lowering | 8 (11.4%) | 11 (14.7%) | 2 (12.5%) | 21 (13.0%) | 0.887 | |
| Common analgesics | 1 (1.4%) | 4 (5.3%) | 3 (18.8%) | 8 (5.0%) | 0.027 | |
| Contraceptives | 9 (12.9%) | 7 (9.3%) | 2 (12.5%) | 18 (11.2%) | 0.709 | |
| Corticosteroids | 2 (2.9%) | 2 (2.7%) | 1 (6.3%) | 5 (3.1%) | 0.628 | |
| NSAIDs | 3 (4.3%) | 4 (5.3%) | 1 (6.3%) | 8 (5.0%) | 0.881 | |
| Opioid analgesics | 1 (1.4%) | 0 (0%) | 0 (0%) | 1 (0.6%) | 0.534 | |
| Thyroid hormones | 17 (24.3%) | 24 (32.0%) | 3 (18.8%) | 44 (27.3%) | 0.467 | |
| Other | 8 (11.4%) | 11 (14.7%) | 4 (25.0%) | 23 (14.3%) | 0.324 | |
| COVID-19 Vaccine |
Yes Ϯ | 129 (84.3%) | 152 (96.2%) | 30 (100.0%) | 311 (91.2%) | <0.001 |
| No | 24 (15.7%) | 6 (3.8%) | 0 (0%) | 30 (8.8%) | ||
| Ϯ COVID-19 Vaccine Doses | One dose | 3 (2.3%) | 2 (1.3%) | 0 (0%) | 5 (1.6%) | 0.798 |
| Two doses | 21 (16.3%) | 21 (13.8%) | 1 (3.3%) | 43 (13.8%) | 0.167 | |
| Three doses | 103 (79.8%) | 121 (79.6%) | 25 (83.3%) | 249 (80.1%) | 0.894 | |
| Four doses | 2 (1.6%) | 8 (5.3%) | 4 (13.3%) | 14 (4.5%) | 0.020 | |
| Influenza Vaccine |
Yes ψ | 43 (28.1%) | 71 (44.9%) | 17 (56.7%) | 131 (38.4%) | <0.001 |
| No | 110 (71.9%) | 87 (55.1%) | 13 (43.3%) | 210 (61.6%) | ||
| ψ Last 12 Months | Yes | 11 (25.6%) | 40 (56.3%) | 10 (58.8%) | 61 (46.6%) | 0.003 |
| No | 32 (74.4%) | 31 (43.7%) | 7 (41.2%) | 70 (53.4%) |
The chi-squared (χ2) test and Fisher’s exact test were used with a significance level (p) of ≤0.05. * COPD = chronic obstructive pulmonary disease. † refers to chronic illnesses. ‡ refers to medications. Ϯ refers to COVID-19 vaccinees. ψ refers to seasonal influenza vaccinees.
3.3. HMPXV Information Sources
Only 25 participants (7.3%) reported learning about HMPXV within their undergraduate education. While the most commonly utilised sources of information about HMPXV were the Czech Ministry of Health (51.6%), digital news portals (47.5%), and social media (25.8%), the least commonly utilised sources were the U.S. CDC (1.5%), ECDC (5%), and scientific journals (5.6%). Utilising the U.S. CDC (p = 0.005), the WHO (p = 0.031), and scientific journals (p = 0.011) was significantly associated with a higher likelihood of HMPXV vaccine acceptance.
The mean number of information sources was 1.8 ± 1.2; this was significantly associated with the level of HMPXV vaccine acceptance (p = 0.006). The HMPXV vaccine-acceptant group utilised more information sources (2.5 ± 1.6) than the HMPXV vaccine-hesitant (1.9 ± 1.2) and HMPXV vaccine-rejecting (1.6 ± 1.0) groups (Table 3).
Table 3.
Information sources utilised by Czech HCWs responding to the HMPXV survey, September 2022 (n = 341).
| Variable | Outcome | HMPXV Vaccine Rejection (n = 153) |
HMPXV Vaccine Hesitancy (n = 158) |
HMPXV Vaccine Acceptance (n = 30) |
Total (n = 341) |
p. |
|---|---|---|---|---|---|---|
| Undergrad Curriculum |
Yes | 8 (5.2%) | 13 (8.2%) | 4 (13.3%) | 25 (7.3%) | 0.216 |
| No | 145 (94.8%) | 145 (91.8%) | 26 (86.7%) | 316 (92.7%) | ||
| Utilised Sources | Ministry of Health (MZČR) | 70 (45.8%) | 91 (57.6%) | 15 (50.0%) | 176 (51.6%) | 0.111 |
| Public health institutes (e.g., ÚZIS and SZÚ) * | 18 (11.8%) | 30 (19.0%) | 6 (20.0%) | 54 (15.8%) | 0.166 | |
| European Centres for Disease Prevention and Control (ECDC) | 5 (3.3%) | 9 (5.7%) | 3 (10.0%) | 17 (5.0%) | 0.186 | |
| U.S. Centers for Disease Control and Prevention (CDC) |
1 (0.7%) | 1 (0.6%) | 3 (10.0%) | 5 (1.5%) | 0.005 | |
| World Health Organization (WHO) | 20 (13.1%) | 25 (15.8%) | 10 (33.3%) | 55 (16.1%) | 0.031 | |
| Professional medical associations | 16 (10.5%) | 21 (13.3%) | 4 (13.3%) | 41 (12.0%) | 0.704 | |
| Scientific journals | 4 (2.6%) | 10 (6.3%) | 5 (16.7%) | 19 (5.6%) | 0.011 | |
| Social media (e.g., Facebook and Twitter) | 39 (25.5%) | 41 (25.9%) | 8 (26.7%) | 88 (25.8%) | 0.989 | |
| News portals (e.g., iDNES and BLESK) ** | 70 (45.8%) | 74 (46.8%) | 18 (60.0%) | 162 (47.5%) | 0.351 | |
| Other | 3 (2.0%) | 5 (3.2%) | 2 (6.7%) | 10 (2.9%) | 0.279 | |
| Total (µ ± SD) | 1.6 ± 1.0 | 1.9 ± 1.2 | 2.5 ± 1.6 | 1.8 ± 1.2 | 0.006 | |
| Confidence Level (1–7) |
Ministry of Health (MZČR) | 5.1 ± 1.1 | 5.4 ± 1.0 | 5.7 ± 1.0 | 5.3 ± 1.1 | 0.026 |
| Public health institutes (e.g., ÚZIS and SZÚ) | 5.4 ± 0.9 | 5.8 ± 0.8 | 6.3 ± 0.5 | 5.7 ± 0.8 | 0.033 | |
| European Centres for Disease Prevention and Control (ECDC) | 6.0 ± 0.0 | 5.9 ± 0.8 | 5.3 ± 0.6 | 5.8 ± 0.6 | 0.288 | |
| U.S. Centers for Disease Control and Prevention (CDC) |
6.0 ± 0.0 | 7.0 ± 0.0 | 5.7 ± 0.6 | 6.0 ± 0.7 | 0.333 | |
| World Health Organization (WHO) | 5.6 ± 0.8 | 5.7 ± 0.7 | 6.1 ± 0.9 | 5.7 ± 0.8 | 0.112 | |
| Professional medical associations | 5.6 ± 0.8 | 5.5 ± 0.8 | 6.5 ± 0.6 | 5.6 ± 0.8 | 0.057 | |
| Scientific journals | 4.8 ± 1.5 | 6.0 ± 0.7 | 6.4 ± 0.9 | 5.8 ± 1.1 | 0.119 | |
| Social media (e.g., Facebook and Twitter) | 3.9 ± 1.0 | 3.5 ± 1.1 | 3.0 ± 1.4 | 3.6 ± 1.1 | 0.110 | |
| News portals (e.g., iDNES and BLESK) | 4.3 ± 0.9 | 4.2 ± 1.1 | 4.1 ± 1.5 | 4.2 ± 1.1 | 0.813 |
The chi-squared (χ2) test, Fisher’s exact test, analysis of variance (ANOVA), and the Kruskal–Wallis (H) test were used with a significance level (p) of ≤0.05. * ÚZIS is the Institute of Health Information and Statistics of the Czech Republic (IHIS-CR). SZÚ is the National Institute of Public Health (NIPH). ** iDNES and BLESK are tabloid newspapers.
On evaluating confidence levels, the U.S. CDC had the highest mean confidence score of 6.0 ± 0.7 (range: 1–5), followed by scientific journals (5.8 ± 1.1) and the ECDC (5.8 ± 0.6). The least trustworthy sources were social media (3.6 ± 1.1), digital news portals (4.2 ± 1.1), and the Czech Ministry of Health (5.3 ± 1.1). The confidence levels of the Czech Ministry of Health (p = 0.026) and public health institutes (p = 0.033) were significantly associated with a higher likelihood of HMPXV vaccine-acceptance (Table 3).
3.4. HMPXV Perceived Knowledge
Perceived knowledge of HMPXV’s clinical presentation was the highest (3.1 ± 1.0); however, vaccination was the lowest domain (2.7 ± 1.0). None of the perceived knowledge domains was significantly associated with HMPXV vaccine acceptance (Table 4).
Table 4.
Knowledge of Czech HCWs responding to the HMPXV survey, September 2022 (n = 341).
| Variable | Outcome | HMPXV Vaccine Rejection (n = 153) |
HMPXV Vaccine Hesitancy (n = 158) |
HMPXV Vaccine Acceptance (n = 30) |
Total (n = 341) |
p |
|---|---|---|---|---|---|---|
| Perceived Knowledge | Epidemiology: (1–5) | 2.7 ± 0.9 | 2.9 ± 0.9 | 2.9 ± 1.0 | 2.8 ± 1.0 | 0.053 |
| Clinical presentation: (1–5) | 3.0 ± 1.0 | 3.1 ± 1.0 | 3.2 ± 1.0 | 3.1 ± 1.0 | 0.250 | |
| Risk factors: (1–5) | 3.2 ± 1.0 | 3.3 ± 0.9 | 3.4 ± 0.9 | 3.2 ± 1.0 | 0.532 | |
| Vaccination: (1–5) | 2.6 ± 1.0 | 2.8 ± 0.9 | 2.8 ± 1.0 | 2.7 ± 1.0 | 0.316 | |
| Treatment: (1–5) | 2.7 ± 1.0 | 2.9 ± 0.9 | 2.8 ± 1.1 | 2.8 ± 1.0 | 0.094 | |
| Factual Knowledge: Epidemiology | Incubation period | 95 (62.1%) | 90 (57.0%) | 18 (60.0%) | 203 (59.5%) | 0.653 |
| Case–fatality ratio | 76 (49.7%) | 76 (48.1%) | 20 (66.7%) | 172 (50.4%) | 0.170 | |
| Endemic region | 99 (64.7%) | 89 (56.3%) | 16 (53.3%) | 204 (59.8%) | 0.241 | |
| Total (0–3) | 1.8 ± 1.1 | 1.6 ± 1.1 | 1.8 ± 1.2 | 1.7 ± 1.1 | 0.425 | |
| Factual Knowledge: Clinical Presentation | Clinical symptoms | 135 (88.2%) | 138 (87.3%) | 29 (96.7%) | 302 (88.6%) | 0.387 |
| Differential diagnosis | 62 (40.5%) | 59 (37.3%) | 17 (56.7%) | 138 (40.5%) | 0.142 | |
| Lesions’ locations | 118 (77.1%) | 119 (75.3%) | 25 (83.3%) | 262 (76.8%) | 0.630 | |
| Total (0–5) | 3.0 ± 1.5 | 3.0 ± 1.6 | 3.7 ± 1.4 | 3.0 ± 1.6 | 0.047 | |
| Factual Knowledge: Risk Factors | Transmission pathways | 127 (83.0%) | 131 (82.9%) | 28 (93.3%) | 286 (83.9%) | 0.372 |
| Vertical transmission | 34 (22.2%) | 33 (20.9%) | 13 (43.3%) | 80 (23.5%) | 0.026 | |
| Sexual transmission | 109 (71.2%) | 101 (63.9%) | 25 (83.3%) | 235 (68.9%) | 0.077 | |
| Total (0–4) | 2.3 ± 1.1 | 2.2 ± 1.2 | 2.8 ± 1.0 | 2.3 ± 1.2 | 0.014 | |
| Factual Knowledge: Vaccination | Vaccine availability | 54 (35.3%) | 44 (27.8%) | 17 (56.7%) | 115 (33.7%) | 0.008 |
| Pre-exposure prophylaxis | 88 (57.5%) | 95 (60.1%) | 20 (66.7%) | 203 (59.5%) | 0.633 | |
| Cross-immunisation | 58 (37.9%) | 59 (37.3%) | 15 (50.0%) | 132 (38.7%) | 0.411 | |
| Total (0–4) | 1.5 ± 1.2 | 1.5 ± 1.3 | 2.1 ± 1.2 | 1.5 ± 1.2 | 0.031 | |
| Factual Knowledge: Treatment | Treatment availability | 36 (23.5%) | 43 (27.2%) | 7 (23.3%) | 86 (25.2%) | 0.733 |
| Medications listed | 18 (11.8%) | 27 (17.1%) | 6 (20.0%) | 51 (15.0%) | 0.257 | |
| Prognosis | 75 (49.0%) | 75 (47.5%) | 15 (50.0%) | 165 (48.4%) | 0.947 | |
| Total (0–4) | 0.9 ± 0.9 | 0.9 ± 0.9 | 0.9 ± 0.7 | 0.9 ± 0.9 | 0.640 |
The chi-squared (χ2) test, Fisher’s exact test, and the Kruskal–Wallis (H) test were used with a significance level (p) of ≤0.05.
No demographic predictor was significantly associated with perceived knowledge scores, although females, homosexuals, older participants (>47 years old), divorced participants, and those providing clinical care to HMPXV cases tended to have higher overall perceived knowledge scores than males (14.6 ± 4.1 vs. 14.4 ± 5.0), heterosexuals (14.8 ± 1.5 vs. 14.6 ± 4.2), younger participants (14.7 ± 3.8 vs. 14.4 ± 4.5), single participants (15.2 ± 4.2 vs. 13.6 ± 4.5), and those who did not provide clinical care to HMPXV cases (15.6 ± 5.3 vs. 14.5 ± 4.1). The differences between medical vs. allied HCWs and participants with vs. without minors were statistically significant and clinically negligible (Table S1).
The number of COVID-19 vaccine doses was significantly associated with the overall perceived knowledge score (p = 0.020). The participants who had received four COVID-19 vaccine doses had the highest perceived knowledge scores (16.5 ± 4.4), while those who had received only a single dose had the lowest perceived knowledge scores (11.0 ± 3.5). Similarly, receiving an influenza vaccine (15.3 ± 4.2 vs. 14.2 ± 4.1; p = 0.019) and learning about HMPXV during undergraduate education (17.8 ± 3.2 vs. 14.3 ± 4.1; p < 0.001) were significantly associated with higher perceived knowledge scores (Table S1).
3.5. HMPXV Factual Knowledge
The overall mean factual knowledge score was 9.4 ± 4.6 (0–20), and the highest score was achieved by the clinical presentation domain (3.0 ± 1.5 (0–5)), while the lowest score was for the treatment domain (0.9 ± 0.9 (0–4)). The domains scores of HMPXV’s clinical presentation (p = 0.047), risk factors (p = 0.014), and vaccination (p = 0.031) were significantly associated with HMPXV vaccine acceptance (Table 4).
In the domain of HMPXV’s epidemiology, all items received more than 50% correct answers. The item about HMPXV’s endemicity had the most correct answers (59.8%), while 40.8% of the participants declared that they did not know the case–fatality ratio of HMPXV.
In the domain of HMPXV’s clinical presentation, the characteristic feature of HMPXV compared with smallpox infection was selected correctly by only 40.5% of the participants, while 41.6% acknowledged that they did not know. When asked about the possible symptoms of HMPXV infection, skin and mucosal lesions were the most commonly selected answer (80.9%), followed by fever (80.4%), fatigue (56%), and headache (55.4%), while the least common was respiratory symptoms (15.8%). When asked about the possible locations of HMPXV infection, extremities were the most commonly selected answer (61.6%), followed by face and mouth (57.2%), chest (52.8%), and genitalia (43.1%), while the least common was anus (29.6%). Only 23.2% and 11.7% of the participants acknowledged that they did not know the locations and symptoms of HMPXV infection, respectively (Table S2).
In the domain of HMPXV risk factors, 76% of the participants selected “direct contact with monkeypox rash, scabs or body fluids” as a potential transmission source. Only 23.5% knew that vertical transmission of HMPXV from pregnant women to their foetuses was possible. While 68.9% of the participants knew that HMPXV transmission was possible between homo- and heterosexual partners, 6.5% thought that it was only possible among homosexual partners, and less than one-quarter (24.6%) were unaware of the possibility of sexual transmission (Table S2).
In the domain of HMPXV vaccination, the least correctly answered question was the one about the availability of HMPXV vaccines—only 33.7% knew there were available vaccines against HMPXV. Interestingly, almost half of the participants (49.6%) reported being unaware of the vaccine that provided cross-protection against HMPXV, and only 38.7% knew that it was the smallpox vaccine (Table S2).
The domain of HMPXV treatment received the lowest number of correct answers. Only 25.2% knew that there were effective drugs against HMPXV, and 1.5%, 3.8%, and 11.7% of the participants named cidofovir, brincidofovir, and tecovirimat as effective antivirals for HMPXV infection, respectively (Table S2).
On evaluating the predictors of HMPXV factual knowledge, gender, sexual orientation, having minors, providing care, chronic illnesses, medical treatments, and COVID-19 and influenza vaccination were not associated with the HMPXV factual knowledge scores. The younger participants (≤47 years old), medical professionals, those receiving four COVID-19 vaccine doses, and the undergraduate curriculum were significantly associated with higher factual knowledge scores than older participants (10.0 ± 4.6 vs. 8.9 ± 4.5; p = 0.013), allied HCWs (11.1 ± 4.7 vs. 9.2 ± 4.5; p = 0.021), a single COVID-19 vaccine (11.5 ± 4.6 vs. 9.4 ± 4.7; p = 0.008), and not learning about HMPXV within undergraduate education (13.2 ± 3.0 vs. 9.1 ± 4.5; p < 0.001), respectively (Table S3).
The U.S. CDC had the highest factual knowledge score (15.2 ± 2.3), followed by the ECDC (12.4 ± 4.6), the WHO (12.3 ± 3.2), and scientific journals (12.2 ± 2.7), while the lowest scores were achieved by social media (9.7 ± 4.7), digital news portals (9.7 ± 4.4), and the Czech Ministry of Health (10.3 ± 4.2) (Table S3).
3.6. Consistency of HMPXV Vaccine Knowledge
Non-parametric correlation analysis between the perceived and factual knowledge domains revealed that HMPXV’s clinical presentation (Spearman’s rho = 0.369) and risk factors (rho = 0.339) had the largest correlation coefficients (Table 5).
Table 5.
Correlation between perceived and factual knowledge of Czech HCWs responding to the HMPXV survey, September 2022 (n = 341).
| Perceived Knowledge | |||||||
|---|---|---|---|---|---|---|---|
| Epidemiology | Clinical Presentation | Risk Factors | Vaccination | Treatment | |||
| Factual Knowledge | Epidemiology | rho | 0.295 | 0.287 | 0.227 | 0.235 | 0.160 |
| p | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | ||
|
Clinical
Presentation |
rho | 0.369 | 0.369 | 0.303 | 0.289 | 0.253 | |
| p | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | ||
| Risk Factors | rho | 0.390 | 0.383 | 0.339 | 0.294 | 0.223 | |
| p | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | ||
| Vaccination | rho | 0.289 | 0.277 | 0.194 | 0.270 | 0.173 | |
| p | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | ||
| Treatment | rho | 0.295 | 0.334 | 0.201 | 0.261 | 0.197 | |
| p | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | ||
Non-parametric correlation (Spearman’s rho) was used, with a significance level (p) of ≤0.05.
On the other hand, the HMPXV treatment domain had the lowest correlation coefficient (rho = 0.197). While the HMPXV treatment domain’s mean factual knowledge score was 0.9 ± 0.9 (0–4), its perceived knowledge mean score was 2.8 ± 1.0 (1–5). These findings indicate that the participants might overestimate their knowledge about HMPXV treatment.
3.7. HMPXV-Vaccine-Related Perceptions
The overall scores of all perception domains—e.g., perceived susceptibility and severity—were significantly associated with HMPXV vaccine acceptance.
Regarding perceived susceptibility, the participants’ susceptibility due to their occupation had the highest mean score (2.5 ± 1.0), while susceptibility due to their lifestyle and health status had the lowest score (2.0 ± 0.9). COVID-19 vaccination was the only predictor that was significantly associated with perceived susceptibility (p = 0.048) (Table 6).
Table 6.
HMPXV-vaccine-related perceptions of Czech HCWs responding to the HMPXV survey, September 2022 (n = 341).
| Category | Item | HMPXV Vaccine Rejection (n = 153) |
HMPXV Vaccine Hesitancy (n = 158) |
HMPXV Vaccine Acceptance (n = 30) |
Total (n = 341) |
p |
|---|---|---|---|---|---|---|
| Perceived Susceptibility |
1. Due to my occupation. | 2.0 ± 0.9 | 2.7 ± 0.9 | 3.4 ± 1.2 | 2.5 ± 1.0 | <0.001 |
| 2. Due to lifestyle and health status. | 1.7 ± 0.9 | 2.2 ± 0.8 | 2.5 ± 1.2 | 2.0 ± 0.9 | <0.001 | |
| 3. Not vaccinated vs. smallpox. | 1.8 ± 0.9 | 2.4 ± 0.8 | 2.9 ± 1.3 | 2.2 ± 1.0 | <0.001 | |
| Overall score (3–15) | 5.6 ± 2.3 | 7.2 ± 2.1 | 8.8 ± 2.9 | 6.6 ± 2.5 | <0.001 | |
| Perceived Severity |
1. I will be very sick. | 3.2 ± 1.0 | 3.3 ± 0.8 | 3.8 ± 1.0 | 3.3 ± 0.9 | 0.004 |
| 2. I may require hospitalisation. | 2.8 ± 1.0 | 2.9 ± 0.7 | 3.2 ± 1.3 | 2.9 ± 0.9 | 0.195 | |
| 3. I might die. | 2.9 ± 1.0 | 3.0 ± 0.8 | 3.4 ± 1.1 | 3.0 ± 0.9 | 0.130 | |
| Overall score (3–15) | 8.9 ± 2.4 | 9.1 ± 1.8 | 10.3 ± 2.9 | 9.1 ± 2.2 | 0.011 | |
| Perceived Benefits |
1. Protected from getting infected. | 3.0 ± 0.8 | 3.3 ± 0.7 | 3.8 ± 0.8 | 3.2 ± 0.8 | <0.001 |
| 2. Protected from serious complications. | 3.3 ± 0.8 | 3.6 ± 0.6 | 4.4 ± 0.7 | 3.5 ± 0.8 | <0.001 | |
| 3. Protect my patients and family. | 2.9 ± 1.0 | 3.3 ± 0.7 | 4.1 ± 0.9 | 3.2 ± 0.9 | <0.001 | |
| Overall score (3–15) | 9.1 ± 2.3 | 10.1 ± 1.6 | 12.2 ± 2.0 | 9.9 ± 2.1 | <0.001 | |
| Perceived Barriers |
1. Safety of HMPXV vaccine. | 3.1 ± 1.0 | 3.0 ± 0.7 | 2.7 ± 1.3 | 3.0 ± 0.9 | 0.038 |
| 2. Effectiveness of HMPXV vaccine. | 3.0 ± 1.0 | 2.9 ± 0.7 | 2.6 ± 1.3 | 2.9 ± 0.9 | 0.035 | |
| Overall score (2–10) | 6.1 ± 1.9 | 5.9 ± 1.3 | 5.3 ± 2.6 | 6.0 ± 1.7 | 0.015 | |
| Cues to Action | 1. Mandated by the employer. | 2.4 ± 1.0 | 3.3 ± 0.8 | 3.5 ± 1.5 | 2.9 ± 1.1 | <0.001 |
| 2. Recommended by health authorities. | 2.4 ± 1.0 | 3.3 ± 0.8 | 3.9 ± 1.2 | 3.0 ± 1.0 | <0.001 | |
| 3. Reliable evidence on effectiveness and safety. | 3.0 ± 1.1 | 3.7 ± 0.8 | 4.2 ± 0.9 | 3.4 ± 1.0 | <0.001 | |
| Overall score (3–15) | 7.9 ± 2.6 | 10.3 ± 1.9 | 11.6 ± 2.9 | 9.3 ± 2.7 | <0.001 |
The Kruskal–Wallis (H) test was used, with a significance level (p) of ≤0.05.
On evaluating perceived severity, the fear of being very sick due to HMPXV infection led to the highest perceived score (3.3 ± 0.9). The overall perceived severity score (9.1 ± 2.2 (3–15)) was significantly (p < 0.001) higher than the perceived susceptibility score (6.6 ± 2.5 (3–15)). The participants who did not have minors (9.3 ± 2.2 vs. 8.7 ± 2.2; p = 0.012) and those who received a COVID-19 vaccine (9.2 ± 2.2 vs. 8.1 ± 2.1; p = 0.016) had significantly higher severity scores than their counterparts. The participants who utilised scientific journals had the highest severity scores (9.8 ± 2.5) (Table S4).
Protection from serious complications had the highest score in the perceived benefits domain (3.5 ± 0.8), with an overall score of 9.9 ± 2.1 (3–15). The perceived barriers related to HMPXV vaccine safety (p = 0.038) and effectiveness (p = 0.035) were significantly associated with HMPXV vaccine acceptance (Table 6).
Chronic illnesses (p = 0.014), medical treatments (p = 0.010), COVID-19 vaccination (p < 0.001), and influenza vaccination (p = 0.011) were significantly associated with higher scores of perceived benefits. The participants who received four doses of the COVID-19 vaccine had a significantly higher perceived benefits score (11.6 ± 2.2) than those who received a single dose (7.4 ± 4.3) (Table S4).
Reliable evidence on the effectiveness and safety of HMPXV vaccines had the highest score as a cue to action (3.4 ± 1.0). The overall score of the cues to action domain was the second highest after the perceived benefits domain. Medical professionals (p = 0.045), chronic illnesses (p = 0.021), medical treatments (p = 0.028), COVID-19 vaccination (p < 0.001), influenza vaccination (p = 0.003) and having no minors (p = 0.011) had significantly higher cues to action scores than their counterparts (Table S4).
3.8. Health Belief Model (HBM)
When asked about their intentions to receive an HMPXV vaccine, 153 rejected it (44.9%), 158 (46.3%) were hesitant, and only 30 (8.8%) declared their acceptance to receive HMPXV vaccine. The HMPXV vaccine acceptance level was moderately correlated with cues to action (rho = 0.569), perceived susceptibility (rho = 0.424), and perceived benefits (rho = 0.372). Perceived barriers were weakly yet negatively correlated with HMPXV vaccine acceptance (rho = −0.149) (Table 7).
Table 7.
Correlation between HMPXV vaccine perceptions and acceptance of Czech HCWs responding to the HMPXV survey, September 2022 (n = 341).
| Perceived Susceptibility |
Perceived Severity |
Perceived Benefits |
Perceived Barriers |
Cues to Action |
Acceptance | ||
|---|---|---|---|---|---|---|---|
|
Perceived
Susceptibility |
rho | 1.000 | 0.203 | 0.114 | 0.103 | 0.307 | 0.424 |
| p | <0.001 | <0.001 | 0.058 | <0.001 | <0.001 | ||
|
Perceived
Severity |
rho | 0.203 | 1.000 | 0.174 | 0.092 | 0.209 | 0.145 |
| p | <0.001 | <0.001 | 0.088 | <0.001 | 0.007 | ||
|
Perceived
Benefits |
rho | 0.114 | 0.174 | 1.000 | −0.178 | 0.393 | 0.372 |
| p | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | ||
|
Perceived
Barriers |
rho | 0.103 | 0.092 | −0.178 | 1.000 | −0.090 | −0.149 |
| p | 0.058 | 0.088 | <0.001 | 0.099 | 0.006 | ||
| Cues to Action | rho | 0.307 | 0.209 | 0.393 | −0.090 | 1.000 | 0.569 |
| p | <0.001 | <0.001 | <0.001 | 0.099 | <0.001 | ||
| Acceptance | rho | 0.424 | 0.145 | 0.372 | −0.149 | 0.569 | 1.000 |
| p | <0.001 | 0.007 | <0.001 | 0.006 | <0.001 |
Non-parametric correlation (Spearman’s rho) was used, with a significance level (p) of ≤0.05.
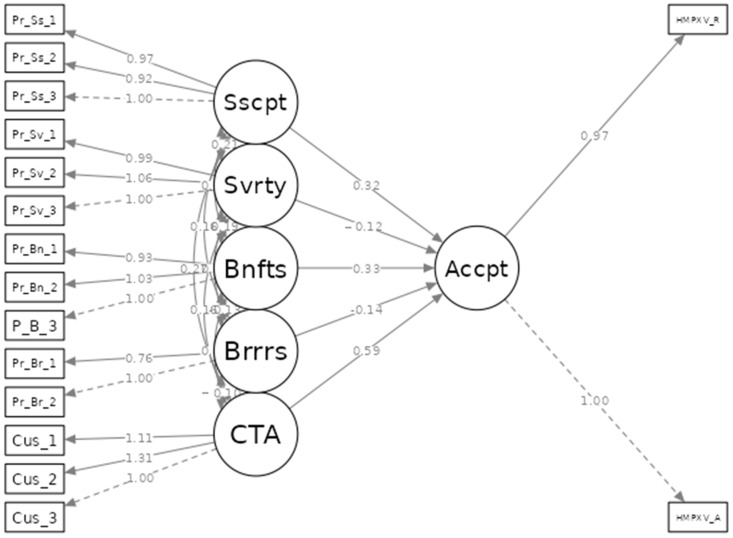
Structural equation modelling (SEM) revealed that the proposed model had a good fit, as indicated by a mean square error of approximation (RMSEA) of 0.055 (CI 95%: 0.043–0.066), Tucker–Lewis index (TLI) of 0.992, and comparative fit index (CFI) of 0.994 (Figure 2).
Figure 2.
Structural equation model (SEM) of Czech HCWs’ perceptions and acceptance of HMPXV vaccines, September 2022 (n = 341). Sscpt = perceived susceptibility. Svrty = perceived severity. Bnfts = perceived benefits. Brrrs = perceived barriers. CTA = cues to action. Accpt = Acceptance. HMPXV vaccine_R = recommendation. HMPXV vaccine_A = acceptance.
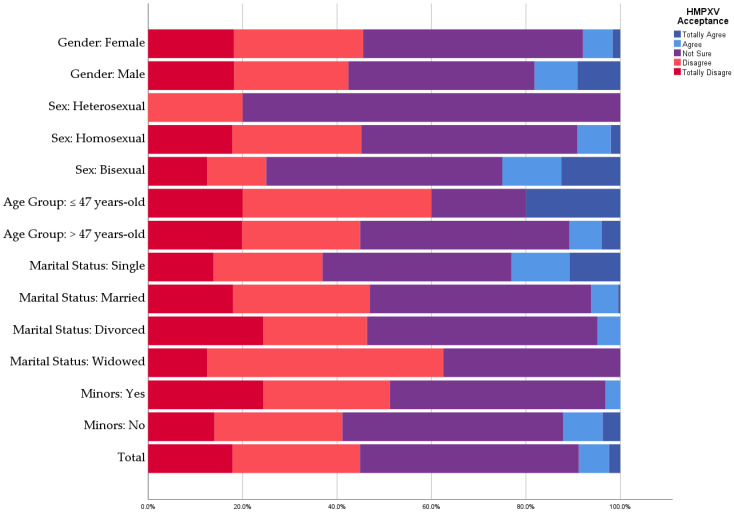
3.9. Correlates to HMPXV Vaccine Acceptance
A total of 30 (8.8%) participants indicated their acceptance to receive an HMPXV vaccine, which represents a suboptimal vaccine acceptance—especially among HCWs. The HMPXV vaccine acceptance level was higher among males (18.2%) than females (7.9%). Heterosexual participants had the lowest HMPXV vaccine acceptance level (9.1%) compared with homosexuals (25%) and bisexuals (20%). Single participants had the highest HMPXV vaccine acceptance level (23.1%) compared with married (6.2%) and divorced (4.9%) participants. Conversely, having minors was significantly associated with a lower acceptance level (3.1% vs. 12.1%; p = 0.005). There were no significant differences between medical (11.1%) and allied HCWs (8.5%) in terms of HMPXV vaccine acceptance (Figure 3).
Figure 3.
Demographic predictors of HMPXV vaccine acceptance among Czech HCWs, September 2022 (n = 341).
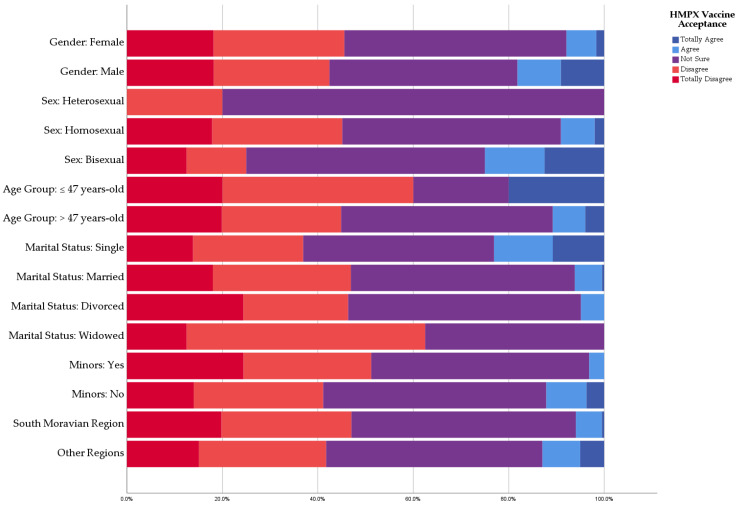
There were no statistically significant differences between the participants with/without chronic illness (8.3% vs. 9.1%; p = 0.810) or those with/without regular medications (9.9% vs. 7.8%; p = 0.482). All of the participants (100%) who did not receive a COVID-19 vaccine rejected the HMPXV vaccine, while 9.6% of COVID-19 vaccinees indicated their acceptance to receive an HMPXV vaccine. The number of COVID-19 vaccine doses was significantly (p = 0.041) associated with an increased likelihood of HMPXV vaccine acceptance (four doses: 28.6%, three doses: 10%; two doses: 2.3%; and single dose: 0%). Influenza vaccination was significantly associated with HMPXV vaccine acceptance (13% vs. 6.2%; Sig = 0.031) (Figure 4).
Figure 4.
Anamnestic predictors of HMPXV vaccine acceptance among Czech HCWs, September 2022 (n = 341).
3.10. HMPXV Vaccine Recommendations and Willingness to Pay
Less than one-quarter (24.1%) of the participants agreed to recommend an HMPXV vaccine to their patients, family members, and friends—especially those at risk. The recommendation score was evaluated by a 5-point Likert scale ranging from “Strongly Disagree = 1” to “Strongly Agree = 1”. The mean recommendation score was significantly (p < 0.001) lower among the HMPXV vaccine-rejecting group (2.3 ± 1.0) compared with the vaccine-hesitant (3.2 ± 0.5) and vaccine-acceptant groups (4.3 ± 0.6) (Table 8).
Table 8.
HMPXV vaccine recommendations and willingness to Pay (WTP) of Czech HCWs responding to the HMPXV survey, September 2022 (n = 341).
| Variable | Outcome | HMPXV Vaccine Rejection (n = 153) |
HMPXV Vaccine Hesitancy (n = 158) |
HMPXV Vaccine Acceptance (n = 30) |
Total (n = 341) |
p |
|---|---|---|---|---|---|---|
| I am willing/interested in recommending a monkeypox vaccination to my patients, family members, and friends—especially those at risk. | Strongly disagree | 39 (25.5%) | 0 (0%) | 0 (0%) | 39 (11.4%) | <0.001 |
| Disagree | 57 (37.3%) | 4 (2.5%) | 0 (0%) | 61 (17.9%) | <0.001 | |
| Not sure | 37 (24.2%) | 120 (75.9%) | 2 (6.7%) | 159 (46.6%) | <0.001 | |
| Agree | 19 (12.4%) | 31 (19.6%) | 18 (60.0%) | 68 (19.9%) | <0.001 | |
| Strongly agree | 1 (0.7%) | 3 (1.9%) | 10 (33.3%) | 14 (4.1%) | <0.001 | |
| Total (µ ± SD) | 2.3 ± 1.0 | 3.2 ± 0.5 | 4.3 ± 0.6 | 2.9 ± 1.0 | <0.001 | |
| How much would you like to pay for a human monkeypox vaccine shot as a personal expense? | It should be free | 106 (69.3%) | 90 (57.0%) | 12 (40.0%) | 208 (61.0%) | 0.004 |
| <10 EUR/shot | 15 (9.8%) | 24 (15.2%) | 1 (3.3%) | 40 (11.7%) | 0.128 | |
| 10–49 EUR/shot | 26 (17.0%) | 39 (24.7%) | 13 (43.3%) | 78 (22.9%) | 0.005 | |
| 50–99 EUR/shot | 3 (2.0%) | 3 (1.9%) | 1 (3.3%) | 7 (2.1%) | 0.712 | |
| ≥100 EUR/shot | 3 (2.0%) | 2 (1.3%) | 3 (10.0%) | 8 (2.3%) | 0.031 | |
| What is the optimal price of the human monkeypox vaccine for the public? | It should be free | 107 (69.9%) | 98 (62.0%) | 17 (56.7%) | 222 (65.1%) | 0.205 |
| <10 EUR/shot | 14 (9.2%) | 30 (19.0%) | 8 (26.7%) | 52 (15.2%) | 0.008 | |
| 10–49 EUR/shot | 25 (16.3%) | 29 (18.4%) | 4 (13.3%) | 58 (17.0%) | 0.764 | |
| 50–99 EUR/shot | 3 (2.0%) | 1 (0.6%) | 1 (3.3%) | 5 (1.5%) | 0.214 | |
| ≥100 EUR/shot | 4 (2.6%) | 0 (0%) | 0 (0%) | 4 (1.2%) | 0.147 |
The chi-squared (χ2) test, Fisher’s exact test, and the Kruskal–Wallis (H) test were used with a significance level (p) of ≤0.05.
Most participants (61%) suggested that an HMPXV vaccine should be offered to them for free, while 11.7% were willing to pay <10 EUR per shot, 22.9% agreed to pay 10–49 EUR per shot, and only 2.1% and 2.3% were willing to pay 50–99 EUR per shot and ≥100 EUR per shot, respectively. The largest proportion of the HMPXV vaccine-acceptant group (43.3%) agreed to pay 10–49 EUR per shot, followed by those who wanted it for free (40%) and those who were willing to pay ≥100 EUR per shot (10%). On the other hand, most of the HMPXV vaccine-rejecting group believed that the HMPXV vaccine should be free (Table 8).
Most participants (65.1%) suggested that the HMPXV vaccine should be offered to the public for free, while 17% suggested that 10–49 EUR per shot was a fair price, and 15.2% suggested <10 EUR per shot. The largest proportion of the HMPXV vaccine-acceptant group (65.7%) suggested that the public should be offered the HMPXV vaccine for free. Similarly, the largest proportion of the HMPXV vaccine-rejecting group (69.9%) suggested that the public should be offered the HMPXV vaccine for free (Table 8).
4. Discussion
Overall, the present study reveals several alarming findings about the levels of HMPXV-related knowledge and vaccine hesitancy among Czech HCWs. Only 8.8% of the participants agreed to receive a vaccination against HMPXV—44.9% rejected it, and 46.3% were hesitant. While digital news portals (47.5%) and social media (25.8%) were among the most utilised information sources about HMPXV, scientific journals (5.6%), the ECDC (5%), and the U.S. CDC (1.5%) were the least common sources. The participants demonstrated suboptimal levels of factual knowledge, especially regarding HMPXV vaccines (1.5 ± 1.2 (0–4)) and treatments (0.9 ± 0.9 (0–4)). Additionally, several misconceptions were detectable among the participants, such as the availability of effective vaccines and antivirals against HMPXV. The HBM indicated that the cues to action and perceived susceptibility were the most important constructs to predict HMPXV vaccine acceptance.
Since the outbreak of HMPXV in May 2022, a number of cross-sectional surveys have been conducted to evaluate the knowledge, perceptions, and attitudes of high-risk groups—including HCWs—regarding HMPXV and its vaccination [16,17,25,26,27,28,29,30,31,32,33]. Ricco et al. 2022 found that 58.6% of Italian physicians were in favour of receiving an HMPXV vaccine; nevertheless, they underestimated the risk of HMPXV as a pathogen compared to SARS-CoV-2, HIV, and TB [17]. In Saudi Arabia, Temsah et al. (2022) found that more than half of the general population was in favour of HMPXV vaccine implementation (50.6%), even though they were less worried about HMPXV compared to SARS-CoV-2 [30]. Moreover, Saudi HCWs believed that those who should be prioritised to receive HMPXV were HCWs themselves (69.8%), followed by immunocompromised patients (54.3%), the elderly (53.1%), and international travellers (40.4%) [16]. Interestingly, acceptance rates of HMPXV vaccines were significantly higher among men who have sex with men (MSM) [25,27]. In the Netherlands, 81.5% of the MSM surveyed by Dukers-Muijrers et al. in 2022 were willing to receive an HMPXV vaccine [27]. Similarly, most French MSM living with PrEP (79.3%) and HIV (59.8%) indicated their acceptance of HMPXV vaccination [25]. In our study, the level of HMPXV vaccine acceptance (8.8%) among Czech HCWs was not only lower than that of their counterparts in other countries [16,17] or high-risk individuals such as MSM [25,27], but also lower than that of the general population in the United States (46%) and Saudi Arabia (50.6%) [26,30].
The information sources utilised to learn about infectious disease outbreaks have a predictable impact on epidemic awareness and misinformation [34,35,36]. Therefore, Alshahrani et al. (2022) conducted a cross-sectional study to assess HMPXV-related knowledge among the general Saudi population, out of which 25% were HCWs [31]. Social media was the most utilised source among Saudis (75%), followed by TV and radio (45.6%), family members and friends (15.6%), and healthcare providers (13.8%), while only 8.8% of Saudis were reading scientific articles to learn about HMPXV [31]. In Saudi Arabia, the HMPXV-related knowledge score was low among 51.7% of social media users versus 21.4% of scientific article readers (p < 0.001) [31]. Another study among Saudi HCWs revealed that the most utilised sources of information were international health authorities (e.g., the WHO and U.S. CDC) (59.8%), followed by official local statements (57.6%), social media (51.1%), and scientific journals (24.5%) [16]. In Iraq, 62.2% used social media as their main source of information to learn about the HMPXV epidemic [32]. Our results differ slightly from the findings of these studies, as the Czech Ministry of Health (MoH) was the most commonly utilised information source (51.6%). Nevertheless, social media platforms were almost five times more common (25.8%) than scientific journals (5.6%), highlighting the systemic problem of the suboptimal practice of evidence-based medicine in the Czech Republic [37,38,39].
In the U.S., the general population rated HCWs as the most reliable information source about HMPXV, followed by public health institutions such as the CDC and the social media accounts of well-known physicians and researchers [26]. In an earlier study among the U.S. general population during the first wave of COVID-19, governmental information sources were the most reliable sources (e.g., CDC and FDA), followed by private media sources (e.g., CNN and FOX) and social media networks (e.g., Facebook and Twitter) [40]. Interestingly, trust in governmental sources was positively associated with better knowledge and protective behaviours. In contrast, trust in private media sources and social media was associated with less knowledge and protective behaviours [40]. In our study, the U.S. CDC received the highest evaluation by our participants (6.0 ± 0.7), followed by scientific journals (5.8 ± 1.1) and the ECDC (5.8 ± 0.6). These results should be interpreted with caution, because these were among our sample’s least commonly utilised sources.
Lipkus et al. (2013) found that factual knowledge about waterpipe tobacco smoking among college students was generally poor; however, their perceived knowledge was evaluated as average. As a result, knowledge gaps were suggested to exist among the surveyed students because of the weak correlation between factual knowledge and perceived knowledge [41]. Several studies among nurses revealed that the correlation between their factual knowledge and perceived knowledge with regard to diabetes mellitus was not strong, raising concerns about their competence in caring for diabetic patients [42,43,44,45]. A recent study exhibited that public health clinicians tended to overestimate their knowledge of research ethics guidelines because there was a mismatch between their high perceived knowledge and low factual knowledge [46]. One of the main consequences of the illusion of knowledge is undermining HCWs’ knowledge-seeking behaviours [46,47]. In our study, the correlation between perceived knowledge and factual knowledge with regard to HMPXV was not strong in any of the examined domains, indicating knowledge gaps among our participants [47,48]. While the mean HMPXV treatment factual knowledge score was 0.9 ± 0.9 (0–4), the mean HMPXV treatment perceived knowledge score was 2.8 ± 1.0 (1–5), and the correlation between them was weak (rho = 0.197).
On evaluating the predictors of HMPXV factual knowledge, gender, sexual orientation, having minors, providing care to HMPXV cases, chronic illnesses, medical treatments, and COVID-19 and influenza vaccination were not significantly associated with the HMPXV factual knowledge scores of our participants. Sallam et al. (2022) found that male HCWs and those with postgraduate degrees had higher HMPXV factual knowledge scores than females and those with undergraduate degrees in Jordan [29]. In Kuwait, Alsanafi et al. (2022) concluded that physicians had higher HMPXV factual knowledge scores than other HCWs—especially medical technicians and allied HCWs [28]. Among Kuwaiti HCWs, age, gender, income level, and education had no significant association with HMPXV factual knowledge [28]. In our study, the younger participants (≤47 years old) and medical professionals were significantly associated with higher factual knowledge scores compared to older participants (10.0 ± 4.6 vs. 8.9 ± 4.5; p = 0.013) and allied HCWs (11.1 ± 4.7 vs. 9.2 ± 4.5; p = 0.021), respectively.
The availability of effective vaccines (33.7%) and antivirals (25.2%) for HMPXV was among the least correctly answered factual knowledge items in the present study. Our results are comparable to those found among Jordanian HCWs, where only 33.3% were aware of the availability of effective vaccines [29]. In Italy, HCWs were more knowledgeable about the availability of effective HMPXV vaccines (60.1%) and antivirals (51.2%) [17].
Vertical transmission was one of the least correctly answered items by our participants (23.5%), indicating a potential knowledge gap concerning HMPXV-related pregnancy outcomes, which are known to be severe—including miscarriage (39% of pregnant cases), intrauterine foetal death (23%), and late foetal and perinatal loss (77%) [49]. A recent study among Saudi medical students found that only 36.5% were aware of the possibility of vertical transmission [33].
Another misconception revealed by our study was the proposition that HMPXV could be transmitted exclusively between homosexual partners (6.5%). In Jordan, 58.7% of HCWs thought that MSM had a role in spreading HMPXV, and this misconception was associated with other conspiracy beliefs about the epidemic’s origins [29].
The HBM demonstrated that cues to action were the strongest predictor of HMPXV vaccine acceptance (rho = 0.569) in our study, followed by perceived susceptibility (rho = 0.424) and perceived benefits (rho = 0.372). Similarly, Temsah et al. (2022) found that those who perceived HMPXV as dangerous and virulent had higher odds (OR: 1.456; CI 95%: 1.165–1.820) of accepting the HMPXV vaccine [30]. In Italy, HCWs with a higher perceived risk of HMPXV exhibited favourable attitudes towards the HMPXV vaccine [17]. While 34%, 56.6%, and 37.5% of our participants thought the HMPXV vaccine could protect against natural infection, prevent serious complications, and protect their families and patients, respectively, our participants perceived lower benefits of the HMPXV vaccine than Italian physicians, as most Italians believed that the HMPXV vaccine could prevent natural infection (90.2%) and severe complications (90.8%) [17].
Amid the COVID-19 pandemic, the HBM was extensively used to explain and predict COVID-19 vaccine acceptance [50,51,52]. In Hong Kong, perceived severity, perceived benefits, and cues to action were positively correlated with COVID-19 vaccine acceptance; however, perceived susceptibility had no significant association with vaccine acceptance [50]. Among Chinese pregnant women, cues to action were the strongest predictor for COVID-19 vaccine acceptance, followed by perceived susceptibility and perceived benefits [51]. Moreover, among Chinese HCWs, cues to action, perceived severity, and perceived benefits were positively correlated with COVID-19 vaccine acceptance, while perceived barriers and perceived susceptibility were not associated with acceptance [52].
The availability of reliable scientific evidence on HMPXV vaccine effectiveness and safety as a cue to action was significantly (p < 0.001) different among the HMPXV vaccine-rejecting (3.0 ± 1.1), -hesitant (3.7 ± 0.8), and -acceptant (4.2 ± 0.9) groups. In an earlier study among Czech HCWs, the safety and effectiveness of COVID-19 vaccine booster doses were significantly associated with the boosters’ acceptance [53]. Similarly, COVID-19 vaccine boosters’ safety was a strong predictor of acceptance among German university staff and students [54], Polish HCWs and healthcare students [55], and Algerian HCWs [56]. In the present study, perceived barriers—such as concerns regarding HMPXV vaccines’ safety (p = 0.038) and effectiveness (p = 0.035)—were significantly associated with HMPXV vaccine acceptance.
Regarding predictors of HMPXV vaccine acceptance, males (18.2%), homosexuals (25%), and single participants (23.1%) had higher acceptance levels than females (7.9%), heterosexuals (9.1%), and married participants (6.2%). In the U.S. general population, the female gender was associated with lower odds of HMPXV vaccine acceptance (OR: 0.42; CI 95%: 0.31–0.58) compared with males [26]. Nevertheless, no statistically significant difference among Italian physicians was found between males and females [17].
In our study, receiving COVID-19 vaccination (p < 0.001), number of COVID-19 vaccine doses (p = 0.023), receiving seasonal influenza vaccination (p < 0.001), and recent administration of seasonal influenza vaccination (p = 0.002) were significantly associated with HMPXV vaccine acceptance. These results are consistent with what was found among the U.S. general population, where COVID-19 vaccinees had higher odds of HMPXV vaccine acceptance (OR: 29.61; CI 95%: 15.68–55.91) compared with non-vaccinees [26]. Additionally, French MSM with PrEP who received COVID-19 vaccines were significantly more associated with higher odds of HMPXV vaccine acceptance than their counterparts who were not vaccinated against COVID-19 [25].
The low level of HMPXV vaccine acceptance (8.8%) among our participants should also be viewed in the wider context of Czech HCWs’ attitudes towards vaccination. In a 2018 European Commission (EC) report on vaccine confidence in Europe, the Czech Republic was the only country where HCWs had lower confidence levels in the safety and importance of the MMR vaccine than the general public [57]. Additionally, 29% of Czech and 19% of Slovak HCWs did not think that seasonal influenza vaccines were important, and 36.4% of Czech and 24.8% of Slovak HCWs did not think that seasonal influenza vaccines were safe [57]. Czech general physicians (GPs) were the least interested in recommending seasonal influenza vaccines to their patients (25.2%) compared to all other European GPs, including Estonian (65%), French (83%), German (87%), Italian (87%), Polish (49%), and Spanish (93%) GPs [57].
4.1. Strengths
To the best of our knowledge, this is the first theory-based study to examine HMPXV-related knowledge and readiness to receive the HMPXV vaccine among HCWs. The HBM is an extensively used model in studying health-related behaviours, including preventive behaviours such as vaccine acceptance [58,59]. Another strength of the present study is the use of two distinct knowledge constructs—i.e., perceived knowledge and factual knowledge—in order to point out knowledge gaps through inconsistency between the two constructs [48]. The factual knowledge items revealed critical misconceptions among the surveyed population, such as the availability of effective vaccines and antivirals, the risk of vertical transmission, and homosexual stigmatisation.
4.2. Limitations
The first limitation of our study is the gender imbalance in the recruited sample, as most of the participants were females (88.9%); however, this is not far from the reality of the target population, as most Czech HCWs are females (80.2%) [60]. The second limitation is the underrepresentation of medical professionals (i.e., physicians, dentists, and pharmacists), who represent 22.3% of the target population, while in our study they were only 10.6% of the entire sample [60]. The third limitation is the non-random sampling technique that we used in this study, which may induce self-selection and reporting biases, as those interested in HMPXV, infectious diseases, or public health emergencies were more likely to join our participants. The fourth limitation is the geographical distribution of the sample; considering that the highest number of respondents were from South Moravia and the fact that the research team was based in South Moravia, there may have been a higher motivation for respondents to answer with respect to the group of HCWs collaborating with the second largest university and medical faculty in the Czech Republic.
4.3. Implications
The findings of this study call upon public health practitioners and health policymakers in the Czech Republic to act accordingly in order to determine the drivers of vaccine hesitancy among Czech HCWs. The low frequency of using scientific journals to learn about infectious diseases (5.6%), compared with the high reliance on news portals (47.5%) and social media (25.8%), highlights another systemic problem—the unfamiliarity of evidence-based practice culture within the Czech healthcare system. The overestimated perceived knowledge of Czech HCWs and their poor factual knowledge—especially with regard to HMPXV vaccines and treatments—indicate a critical and common issue of the illusion of knowledge among the target population. Dedicated educational campaigns should address the knowledge gaps with regard to the availability of effective HMPXV vaccines and treatments, the risk of vertical transmission, and homosexual stigmatisation. Future studies should investigate the prevalence and drivers of HMPXV vaccine hesitancy among the general population to scout for potential misinformation and its sources.
5. Conclusions
The present study reveals several alarming findings about the levels of HMPXV-related knowledge and vaccine hesitancy among Czech HCWs. Only 8.8% of the participants agreed to receive vaccination against HMPXV, 44.9% rejected it, and 46.3% were hesitant. While digital news portals (47.5%) and social media (25.8%) were among the most utilised sources of information about HMPXV, scientific journals (5.6%), the ECDC (5%), and the U.S. CDC (1.5%) were the least common sources. The weak correlation between participants’ perceived knowledge and factual knowledge—especially concerning HMPXV vaccines and treatments—confirms the possibility of knowledge gaps. Dedicated educational campaigns should address the knowledge gaps with respect to the availability of effective HMPXV vaccines and treatments, the risk of vertical transmission, and homosexual stigmatisation.
Acknowledgments
The authors would like to thank all of the anonymous participants for their time and effort in sharing their views during this critical time. Additionally, we would like to thank the members of Czech National Centre for Evidence-Based Healthcare and Knowledge Translation for their help in validating and promoting the survey. We thank the chairs of the professional associations of non-medical healthcare workers—i.e., the Czech Nursing Association (ČAS), the Association of College Nurses (SVVS), the Association of Higher Education Educators in the Non-Medical Health Professions (AVVNZP), and the Association of Social Service Providers of the Czech Republic (APSS-ČR)—who disseminated the SAQ to their members.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/vaccines10122022/s1, Figure S1: Sample size calculation via Epi-InfoTM; Population Survey module (StatCalc). Table S1: Predictors of HMPXV-related Perceived Knowledge of Czech Healthcare Workers Responding to HMPXV Survey; Table S2: Factual Knowledge of Czech Healthcare Workers Responding to HMPXV Survey; Table S3: Predictors of HMPXV-related Factual Knowledge of Czech Healthcare Workers Responding to HMPXV Survey. Table S4: Predictors of HMPXV vaccine-related Perceptions and Acceptance of Czech Healthcare Workers Responding to HMPXV Survey.
Author Contributions
Conceptualisation, A.R.; methodology, A.R., A.D., J.R., P.D., A.P. and M.K.; software, A.R.; validation, J.K., L.D., A.P. and M.K.; formal analysis, A.R.; investigation, A.P.; writing—original draft preparation, A.R. and A.D.; writing—review and editing, J.R., P.D., J.K., L.D., A.P. and M.K.; supervision, A.R.; project administration, A.R.; funding acquisition, A.R. and M.K. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
This study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ethics Committee of the Faculty of Medicine, Masaryk University (Ref. 73/2022), on 19 September 2022.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This output was supported by the NPO “Systemic Risk Institute” number LX22NPO5101, funded by European Union—Next Generation EU (Ministry of Education, Youth and Sports, NPO: EXCELES). The work of A.R. and A.D. was supported by Masaryk University grant number MUNI/A/1402/2021.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Centers for Disease Control and Prevention (CDC) Travel. [(accessed on 21 October 2022)]; Available online: https://www.cdc.gov/poxvirus/monkeypox/travel/index.html.
- 2.WHO Monkeypox. [(accessed on 21 May 2022)]. Available online: https://www.who.int/news-room/fact-sheets/detail/monkeypox.
- 3.ECDC Epidemiological Update: Monkeypox Outbreak. [(accessed on 22 May 2022)]; Available online: https://www.ecdc.europa.eu/en/news-events/epidemiological-update-monkeypox-outbreak.
- 4.World Health Organization (WHO) Vaccines and Immunization for Monkeypox: Interim Guidance. [(accessed on 10 August 2022)]; Available online: https://www.who.int/publications/i/item/who-mpx-immunization-2022.1.
- 5.Centers for Disease Control and Prevention (CDC) 2022 Monkeypox Outbreak Global Map. [(accessed on 10 August 2022)]; Available online: https://www.cdc.gov/poxvirus/monkeypox/response/2022/world-map.html.
- 6.CDC Transmission. [(accessed on 22 May 2022)]; Available online: https://www.cdc.gov/poxvirus/monkeypox/transmission.html.
- 7.Bass J., Tack D.M., McCollum A.M., Kabamba J., Pakuta E., Malekani J., Nguete B., Monroe B.P., Doty J.B., Karhemere S., et al. Enhancing Health Care Worker Ability to Detect and Care for Patients with Monkeypox in the Democratic Republic of the Congo. Int. Health. 2013;5:237–243. doi: 10.1093/inthealth/iht029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harapan H., Setiawan A.M., Yufika A., Anwar S., Wahyuni S., Asrizal F.W., Sufri M.R., Putra R.P., Wijayanti N.P., Salwiyadi S., et al. Knowledge of Human Monkeypox Viral Infection among General Practitioners: A Cross-Sectional Study in Indonesia. Pathog. Glob. Health. 2020;114:68–75. doi: 10.1080/20477724.2020.1743037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.WHO . WHO Advisory Committee on Variola Virus Research Report of the Nineteenth Meeting, 1–2 November 2017. WHO; Geneva, Switzerland: 2018. [Google Scholar]
- 10.Ammar N., Aly N.M., Folayan M.O., Mohebbi S.Z., Attia S., Howaldt H.P., Boettger S., Khader Y., Maharani D.A., Rahardjo A., et al. Knowledge of Dental Academics about the COVID-19 Pandemic: A Multi-Country Online Survey. BMC Med. Educ. 2020;20:399. doi: 10.1186/s12909-020-02308-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Von Elm E., Altman D.G., Egger M., Pocock S.J., Gøtzsche P.C., Vandenbroucke J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. UroToday Int. J. 2007;335:806–808. doi: 10.1097/EDE.0b013e3181577654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Harvard Humanitarian Initiative Welcome to KoBoToolbox. [(accessed on 4 January 2022)]. Available online: https://support.kobotoolbox.org/welcome.html.
- 13.Ministerstvo Zdravotnictví ČR Úroveň Informovanosti a Vnímání Lidských Opičích Neštovic Českými Zdravotnickými Profesionály. [(accessed on 11 October 2022)]. Available online: https://www.mzcr.cz/uroven-informovanosti-a-vnimani-lidskych-opicich-nestovic-ceskymi-zdravotnickymi-profesionaly/
- 14.Andrea Pokorná Úroveň Informovanosti a Vnímání Lidských Opičích Neštovic Českými Zdravotnickými Profesionály. [(accessed on 11 October 2022)]. Available online: https://uzv.med.muni.cz/o-pracovisti/aktuality/uroven-informovanosti-a-vnimani-lidskych-opicich-nestovic-ceskymi-zdravotnickymi-profesionaly.
- 15.Institute of Health Information and Statistics of the Czech Republic (UZIS) [Health Yearbook of the Czech Republic 2017] [(accessed on 3 March 2021)]. Available online: https://www.uzis.cz/index-en.php?pg=record&id=8166.
- 16.Aljamaan F., Alenezi S., Alhasan K., Saddik B., Alhaboob A., Altawil E.S., Alshahrani F., Alrabiaah A., Alaraj A., Alkriadees K., et al. Healthcare Workers’ Worries and Monkeypox Vaccine Advocacy during the First Month of the WHO Monkeypox Alert: Cross-Sectional Survey in Saudi Arabia. Vaccines. 2022;10:1408. doi: 10.3390/vaccines10091408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Riccò M., Ferraro P., Camisa V., Satta E., Zaniboni A., Ranzieri S., Baldassarre A., Zaffina S., Marchesi F. When a Neglected Tropical Disease Goes Global: Knowledge, Attitudes and Practices of Italian Physicians towards Monkeypox, Preliminary Results. Trop. Med. Infect. Dis. 2022;7:135. doi: 10.3390/tropicalmed7070135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Harapan H., Setiawan A.M., Yufika A., Anwar S., Wahyuni S., Asrizal F.W., Sufri M.R., Putra R.P., Wijayanti N.P., Salwiyadi S., et al. Physicians’ Willingness to Be Vaccinated with a Smallpox Vaccine to Prevent Monkeypox Viral Infection: A Cross-Sectional Study in Indonesia. Clin. Epidemiol. Glob. Health. 2020;8:1259–1263. doi: 10.1016/j.cegh.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.High Acceptance of New Monkeypox Vaccine among GPs in Indonesia. Pharm. Outcomes News. 2020;862:15. doi: 10.1007/s40274-020-7133-6. [DOI] [Google Scholar]
- 20.Harapan H., Wagner A.L., Yufika A., Setiawan A.M., Anwar S., Wahyuni S., Asrizal F.W., Sufri M.R., Putra R.P., Wijayanti N.P., et al. Acceptance and Willingness to Pay for a Hypothetical Vaccine against Monkeypox Viral Infection among Frontline Physicians: A Cross-Sectional Study in Indonesia. Vaccine. 2020;38:6800–6806. doi: 10.1016/j.vaccine.2020.08.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.World Medical Association World Medical Association Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. JAMA J. Am. Med. Assoc. 2013;310:2191–2194. doi: 10.1001/jama.2013.281053. [DOI] [PubMed] [Google Scholar]
- 22.Proton Technologies AG General Data Protection Regulation (GDPR) Compliance Guidelines. [(accessed on 1 May 2020)]. Available online: https://gdpr.eu/
- 23.SPSS Inc. IBM SPSS Statistics 28. [(accessed on 14 March 2021)]. Available online: https://www.ibm.com/support/pages/ibm-spss-statistics-28-documentation.
- 24.The Jamovi Project Jamovi (Version 1.6) [Computer Software] [(accessed on 11 February 2022)]. Available online: https://www.jamovi.org.
- 25.Zucman D., Fourn E., Touche P., Majerholc C., Vallée A. Monkeypox Vaccine Hesitancy in French Men Having Sex with Men with PrEP or Living with HIV in France. Vaccines. 2022;10:1629. doi: 10.3390/vaccines10101629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Malik A.A., Winters M.S., Omer S.B. Attitudes of the US General Public towards Monkeypox. medRxiv. 2022 doi: 10.1101/2022.06.20.22276527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Htm Dukers-Muijrers N., Evers Y., Widdershoven V., Davidovich U., Adam P.C., Lm E., de Coul O., Zantkuijl P., Matser A., Prins M., et al. Monkeypox Vaccination Willingness, Determinants, and Communication Needs in Gay, Bisexual, and Other Men Who Have Sex with Men, in the Context of Limited Vaccine Availability in the Netherlands (Dutch MPX-Survey) medRxiv. 2022 doi: 10.1101/2022.10.11.22280965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Alsanafi M., Al-Mahzoum K., Sallam M. Monkeypox Knowledge and Confidence in Diagnosis and Management with Evaluation of Emerging Virus Infection Conspiracies among Health Professionals in Kuwait. Pathogens. 2022;11:994. doi: 10.3390/pathogens11090994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sallam M., Al-Mahzoum K., Al-Tammemi A.B., Alkurtas M., Mirzaei F., Kareem N., Al-Naimat H., Jardaneh L., Al-Majali L., AlHadidi A., et al. Assessing Healthcare Workers’ Knowledge and Their Confidence in the Diagnosis and Management of Human Monkeypox: A Cross-Sectional Study in a Middle Eastern Country. Healthcare. 2022;10:1722. doi: 10.3390/healthcare10091722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Temsah M.H., Aljamaan F., Alenezi S., Alhasan K., Saddik B., Al-Barag A., Alhaboob A., Bahabri N., Alshahrani F., Alrabiaah A., et al. Monkeypox Caused Less Worry than COVID-19 among the General Population during the First Month of the WHO Monkeypox Alert: Experience from Saudi Arabia. Travel Med. Infect. Dis. 2022;49:102426. doi: 10.1016/j.tmaid.2022.102426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Alshahrani N.Z., Alzahrani F., Alarifi A.M., Algethami M.R., Alhumam M.N., Ayied H.A.M., Awan A.Z., Almutairi A.F., Bamakhrama S.A., Almushari B.S., et al. Assessment of Knowledge of Monkeypox Viral Infection among the General Population in Saudi Arabia. Pathogens. 2022;11:904. doi: 10.3390/pathogens11080904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ahmed S.K., Abdulqadirb S.O., Omar R.M., Hussein S.H., M-Amin H.I., Chandran D., Sharma A.K., Dhama K., Ahmed Z.K., Essa R.A., et al. Study of Knowledge, Attitude and Anxiety in Kurdistan-Region of Iraqi Population during the Monkeypox Outbreak in 2022. 2022. [(accessed on 11 February 2022)]. Available online: [DOI]
- 33.Alshahrani N.Z., Mitra S., Alkuwaiti A.A., Alhumam M.N., Altmimi S.M.B., Alamri M.H.M., Albalawi Z.A.S., Almorgi M.W., Alharbi H.K.D., Alshahrani S.M. Medical Students’ Perception Regarding the Re-Emerging Monkeypox Virus: An Institution-Based Cross-Sectional Study from Saudi Arabia. Cureus. 2022;14:e28060. doi: 10.7759/cureus.28060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Baker I., Marzouqa N., Yaghi B.N., Adawi S.O., Yousef S., Sabooh T.N., Salhab N.M., Khrishi H.M., Qabaja Y., Riad A., et al. The Impact of Information Sources on COVID-19-Related Knowledge, Attitudes, and Practices (KAP) among University Students: A Nationwide Cross-Sectional Study. Int. J. Environ. Res. Public Health. 2021;18:12462. doi: 10.3390/ijerph182312462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Alawia R., Riad A., Kateeb E. Knowledge and Attitudes among Dental Students about COVID-19 and Its Precautionary Measures: A Cross-Sectional Study. J. Oral Med. Oral Surg. 2021;27:17. doi: 10.1051/mbcb/2020056. [DOI] [Google Scholar]
- 36.Alawia R., Riad A., Kateeb E. Risk Perception and Readiness of Dental Students to Treat Patients amid COVID-19: Implication for Dental Education. Oral Dis. 2020;28:975–976. doi: 10.1111/odi.13593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dosedel M., Hendrychova T., Maly J., Kubena A., Byma S., Vlcek J. Prescription of Evidence-Based Medicine Drugs by General Practitioners to Patients after Myocardial Infarction: Outcomes from the Czech Republic. Acta Pol. Pharm. Drug Res. 2014;71:189–195. [PubMed] [Google Scholar]
- 38.Carter M., Strnadová I., Stephenson J. Reported Prevalence of Evidence-Based Instructional Practices by Special Educators in the Czech Republic. Eur. J. Spec. Needs Educ. 2012;27:319–335. doi: 10.1080/08856257.2012.691229. [DOI] [Google Scholar]
- 39.Vrbová T., Klugarová J., Pokorná A., Dušek L., Líčeník R., Klugar M. Enhancing the Evidence-Based Healthcare Principles in Clinical Practice Guidelines Development in the Czech Republic: A Best Practice Implementation Project. Int. J. Evid. Based Healthc. 2022;20:S67–S75. doi: 10.1097/XEB.0000000000000337. [DOI] [PubMed] [Google Scholar]
- 40.Fridman I., Lucas N., Henke D., Zigler C.K. Association Between Public Knowledge About COVID-19, Trust in Information Sources, and Adherence to Social Distancing: Cross-Sectional Survey. JMIR Public Health Surveill. 2020;6:e22060. doi: 10.2196/22060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lipkus I.M., Eissenberg T., Schwartz-Bloom R.D., Prokhorov A.V., Levy J. Relationships among Factual and Perceived Knowledge of Harms of Waterpipe Tobacco, Perceived Risk, and Desire to Quit among College Users. J. Health Psychol. 2013;19:1525–1535. doi: 10.1177/1359105313494926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.El-Deirawi K.M., Zuraikat N. Registered Nurses’ Actual and Perceived Knowledge of Diabetes Mellitus. J. Nurses Staff. Dev. 2001;17:5–11. doi: 10.1097/00124645-200101000-00001. [DOI] [PubMed] [Google Scholar]
- 43.Alotaibi A., Gholizadeh L., Al-Ganmi A., Perry L. Examining Perceived and Actual Diabetes Knowledge among Nurses Working in a Tertiary Hospital. Appl. Nurs. Res. 2017;35:24–29. doi: 10.1016/j.apnr.2017.02.014. [DOI] [PubMed] [Google Scholar]
- 44.Drass J.A., Muir-Nash J., Boykin P.C., Turek J.M., Baker K.L. Perceived and Actual Level of Knowledge of Diabetes Mellitus among Nurses. Diabetes Care. 1989;12:351–356. doi: 10.2337/diacare.12.5.351. [DOI] [PubMed] [Google Scholar]
- 45.Baxley S.G., Brown S.T., Pokorny M.E., Swanson M.S. Perceived Competence and Actual Level of Knowledge of Diabetes Mellitus among Nurses. J. Nurs. Staff Dev. 1997;13:93–98. [PubMed] [Google Scholar]
- 46.Rouse D.M., Tynan A. Actual and Perceived Knowledge of Research Ethics Guidelines in a Sample of Public Health Clinicians. Intern. Med. J. 2021;51:1840–1846. doi: 10.1111/imj.14984. [DOI] [PubMed] [Google Scholar]
- 47.Park C.-Y. News Media Exposure and Self-Perceived Knowledge: The Illusion of Knowing. Int. J. Public Opin. Res. 2001;13:419–425. doi: 10.1093/ijpor/13.4.419. [DOI] [Google Scholar]
- 48.Ladwig P., Dalrymple K.E., Brossard D., Scheufele D.A., Corley E.A. Perceived Familiarity or Factual Knowledge? Comparing Operationalizations of Scientific Understanding. Sci. Public Policy. 2012;39:761–774. doi: 10.1093/scipol/scs048. [DOI] [Google Scholar]
- 49.D’Antonio F., Pagani G., Buca D., Khalil A. Monkeypox Infection in Pregnancy: A Systematic Review and Metaanalysis. Am. J. Obstet. Gynecol. MFM. 2023;5:100747. doi: 10.1016/j.ajogmf.2022.100747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wong M.C.S., Wong E.L.Y., Huang J., Cheung A.W.L., Law K., Chong M.K.C., Ng R.W.Y., Lai C.K.C., Boon S.S., Lau J.T.F., et al. Acceptance of the COVID-19 Vaccine Based on the Health Belief Model: A Population-Based Survey in Hong Kong. Vaccine. 2021;39:1148–1156. doi: 10.1016/j.vaccine.2020.12.083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tao L., Wang R., Han N., Liu J., Yuan C., Deng L., Han C., Sun F., Liu M., Liu J. Acceptance of a COVID-19 Vaccine and Associated Factors among Pregnant Women in China: A Multi-Center Cross-Sectional Study Based on Health Belief Model. Hum. Vaccines Immunother. 2021;17:2378–2388. doi: 10.1080/21645515.2021.1892432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Yu Y., Lau J.T.F., She R., Chen X., Li L., Li L., Chen X. Prevalence and Associated Factors of Intention of COVID-19 Vaccination among Healthcare Workers in China: Application of the Health Belief Model. Hum. Vaccines Immunother. 2021;17:2894–2902. doi: 10.1080/21645515.2021.1909327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Klugar M., Riad A., Mohanan L., Pokorná A. COVID-19 Vaccine Booster Hesitancy (VBH) of Healthcare Workers in Czechia: National Cross-Sectional Study. Vaccines. 2021;9:1437. doi: 10.3390/vaccines9121437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Attia S., Mausbach K., Klugar M., Howaldt H.-P., Riad A. Prevalence and Drivers of COVID-19 Vaccine Booster Hesitancy (VBH) among German University Students and Employees. Front. Public Health. 2022;10:846861. doi: 10.3389/fpubh.2022.846861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Dziedzic A., Issa J., Hussain S., Tanasiewicz M., Wojtyczka R., Kubina R., Konwinska M.D., Riad A. COVID-19 Vaccine Booster Hesitancy (VBH) of Healthcare Professionals and Students in Poland: Cross-Sectional Survey-Based Study. Front. Public Health. 2022;10:2391. doi: 10.3389/fpubh.2022.938067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lounis M., Bencherit D., Rais M.A., Riad A. COVID-19 Vaccine Booster Hesitancy (VBH) and Its Drivers in Algeria: National Cross-Sectional Survey-Based Study. Vaccines. 2022;10:621. doi: 10.3390/vaccines10040621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Larson H., de Figueiredo A., Karafllakis E., Rawal M. State of Vaccine Confidence in the European Union in 2018. Eur. J. Public Health. 2019;29:ckz185-374. doi: 10.1093/eurpub/ckz185.374. [DOI] [Google Scholar]
- 58.Wayne W. LaMorte The Health Belief Model. [(accessed on 11 August 2022)]. Available online: https://sphweb.bumc.bu.edu/otlt/mph-modules/sb/behavioralchangetheories/behavioralchangetheories2.html.
- 59.Rosenstock I.M. The Health Belief Model and Preventive Health Behavior. Health Educ. Behav. 1974;2:354–386. doi: 10.1177/109019817400200405. [DOI] [Google Scholar]
- 60.The Czech Statistical Office (CZSO) Health Care Personnel as at 31 December. [(accessed on 21 October 2022)]; Available online: https://www.czso.cz/documents/10180/120583268/300002200201.pdf/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.