Highlights
-
•
This is the first published use of a realist evaluation approach to identify underlying causal mechanisms of a chronic-care treatment model implemented in a low- or middle-income country.
-
•
This paper focuses on context as an implementation leverage point that enables the transferability of integrated diabetes and depression care models to alternative care settings in India and other low-resource settings.
-
•
Findings from this evaluation highlight the resource and training gaps that hinder the implementation and sustainability of a multi-component, team-based intervention aimed at integrating depression treatment into routine diabetes care.
Keywords: Implementation science, Collaborative care, Qualitative
Abstract
Aims
We aimed to determine what key resources, mechanisms, and contextual factors are necessary to integrate depression and diabetes treatment into low-resource settings.
Methods
A realist evaluation framework was employed to conduct a comparative case study. Data were collected through document review, key informant interviews (n=4), activity logs, and interviews with implementing health care providers (n=11) to test and refine program theories for collaborative care.
Results
Efforts to enhance patient care coordination (i.e., adapting clinics’ patient flow and resources, on-going trainings, and on-site support for care coordinators) improved implementation of depression treatment by usual care diabetes physicians. Clinician's avoidance of the term depression was identified as a barrier to mental health counseling and treatment.
Conclusions
The variations in organizational features and processes linked to implementation activities across two clinics provided an opportunity to examine how and why different contextual factors help or hinder the implementation process. Findings from this study demonstrate that successful implementation of an integrated depression and diabetes care model is feasible in a low-resource setting, while the revised program theories provide an explanatory framework of coordinated care implementation processes that can inform future efforts to disseminate and scale this care model.
1. Introduction
Few individuals living with depression in low- and middle-income countries receive treatment, largely due to a scarcity of trained mental health professionals and the inequitable distribution of resources for mental health care1,2. In India, one of the specified approaches to increasing access to mental health care advocated by the National Mental Health Program is to integrate basic mental health care into the broader system of health services3. Despite being launched in 1982, the program's efforts to integrate mental health services have been limited, with case studies of implementing districts revealing a lack of evaluation plans4,5. To understand how to effectively deliver evidence-based treatment for depression across the diversity of healthcare settings in India, robust evaluations of integrated care models are needed.
While the World Health Organization estimates that depression affects 4.5% of people in India6, a recent meta-analysis found that 38% of patients with type 2 diabetes in India also have depression7. With over 74 million adults living with diabetes in India8, efforts to better understand how to effectively integrate depression treatment into diabetes care settings offer an opportune way to enhance the diagnosis, treatment, and management of both chronic conditions. In this paper, we report on a realist process evaluation of the first randomized controlled trial in India to implement depression treatment in tertiary diabetes care settings. This theory-driven evaluation approach acknowledges that intervention programs are not one-size-fits-all and provides a methodology for examining what and how differing contextual factors enhance integration of depression and diabetes care.
Integrated care models typically consist of multiple, inter-related care components that require the consideration of competing stakeholder values, beliefs, resource needs, and interests. Realist evaluations are based on the assumption that a combination of stakeholders’ reasonings and available resources (i.e., mechanisms) is what enables an intervention to operate, and that interventions can operate differently for different people in different contexts9. By examining the interaction and effect of contextual factors and mechanisms to achieve particular intervention outocmes (i.e., context-mechanism-outcome configurations), realist methodology is well suited for investigating what works, for whom, in what circumstances, and how10. Using a realist evaluation approach, which identifies, tests, and refines program theory in the process of examining whether and how an intervention succeeds in a given context, this evaluation seeks to generate important insights into how depression treatment can be integrated into diabetes care settings in India and other low resource settings with high diabetes rates.
The INtegrating DEPrEssioN and Diabetes treatmENT (INDEPENDENT) care model, derived from components of two previously tested care models11,12, was designed to improve access to depression treatment and improve depressive symptoms and cardiometabolic disease outcomes among patients with diabetes and co-morbid depression13. The INDEPENDENT care model was tested in four diverse outpatient diabetes clinics in India and included the following collaborative care intervention components: non-specialized care coordinator support, evidence-based electronic care prompts produced by a decision-support electronic health record system, and systematic case review by a psychiatrist and senior endocrinologist every 2–4 weeks14. These intervention components operated together to enhance care for depression and diabetes. Through therapeutic approaches, such as motivational interviewing, providing patient-education, employing self-efficacy enhancement strategies, and monitoring depressive symptoms and cardiovascular disease indicators, the care coordinators trained as a part of the INDEPENDENT study provided on-going, individualized patient care to study participants in the intervention arm. Further enhancing the responsiveness of this care model, the care coordinators utilized decision-support software equipped with evidence-based algorithms that recommend treatment options based on updated lab results and patient health information. Lastly, the case review meetings brought together care coordinators and specialist physicians with expertise in diabetes and depression treatment to provide population health management at the clinic level. Using electronic health record data to identify poorly controlled cases of diabetes and depression, the specialists investigated where treatment gaps may have occurred and approaches for improving care, which care coordinators then relayed to the usual care diabetes physicians. While the design, theoretical basis, and training for the underlying care model components were the same across clinics, each clinic made adaptations to the processes of how they incorporated the intervention components into their clinic flow.15
This study aims to examine the process of implementing the multi-component INDEPENDENT care model (what was implemented and how), how providers’ responses to implementation resources during intervention delivery produced change (intervention mechanisms), and the enabling contextual factors that shaped implementation and intervention outcomes.
2. Methods and subjects
This realist evaluation employed a comparative case study design using two urban diabetes care centers in India, one government clinic in the North and one private clinic in the South. These two sites were selected because they offered variation in geographic representation, organizational structure, size, and resources, which allowed hypothesized program theories to be tested with data from contrasting contexts. Data collection occurred in alignment with the phases of realist evaluation: identify, test, and refine program theory.9
2.1. Theory identification
We developed a logic model based on a review of the study protocol and literature supporting intervention components and used this model to facilitate a discussion with four key informants (study investigators [n=2] and study software designers [n=2]) regarding how the intervention components were hypothesized to work. Information garnered from these discussions informed the development of the initial program theories (see Electronic Supplementary Material 1). In this evaluation of the INDEPENDENT care model, program theories are mapped onto theoretical constructs from the Theoretical Domains Framework16 to assess contextual factors influencing the cognitive processes involved in clinical decision-making and implementation behavior.
2.2. Data collection
Multiple data sources were used to test the identified program theories.
2.2.1. Intervention logs
We extracted the following data from hard copy patient files maintained by care coordinators: descriptive data on the types of patient visits, and the frequency and composition of case reviews.
2.2.2. Interview procedures
LJ conducted interviews throughout the second half of the active intervention year, allowing providers to reflect on how the input of additional and/or adapted resources and additional experience throughout the trial resulted in mechanistic shifts. A total of 11 interviews were completed, including all care coordinators [n=3], usual care diabetes physicians [n=3], and specialist endocrinologists [n=3] and psychiatrists [n=2]. This sample size is considered adequate for achieving data saturation (i.e., the point at which no new information emerges from the data)17 and allowed for the examination of how various implementation actors experienced the INDEPENDENT care model. All participants consented to participate in an audio-recorded, semi-structured interview lasting 60–90 minutes. The interview guide included questions and probes linked to constructs of the Theoretical Domains Framework16: implementation actors’ knowledge and skills related to depression treatment and management, perceived capability and confidence to carry out intervention tasks, implementation goals, reinforcements and social support, outcome expectations, and environmental contexts and resources.
The study was approved by the Institutional Review Boards of Emory University, USA, and the All India Institute of Medical Sciences and Madras Diabetes Research Foundation, India.
2.3. Data analysis
All interviews were transcribed, de-identified, and independently coded by two team members using a combined inductive and deductive content analysis approach.18 In accordance with this analytic approach, the following steps were used to code the transcripts: (1) open code, (2) compare coding between coders and agree upon common code names, or use a third-party from the study team to reach a consensus, (3) independently cluster the codes into context-mechanism-outcome configurations based on the original treatment design and plan for intervention delivery, and (4) compare across clustering of codes with shared outcomes to finalize data configurations.
We organized coded text segments and extracted process data into EXCEL with a specified tab for evidence related to each context-mechanism-outcome configuration and a separate spreadsheet for each study site. We then used the spreadsheets to compose individual case summaries for each site that outlined key contextual differences that influenced patient care and implementation activities (see Electronic Supplementary Material 2). These summaries facilitated a case comparison of observed outcome patterns and the contextual factors that do (or do not) help trigger mechanisms contributing to the intervention delivery. We compared the identified data configurations within and across sites to identify where different patterns of interacting contextual factors and mechanism emerged, both in manners which were anticipated and unanticipated based on the hypothesized program mechanism, to produce refined program theories.
3. Results
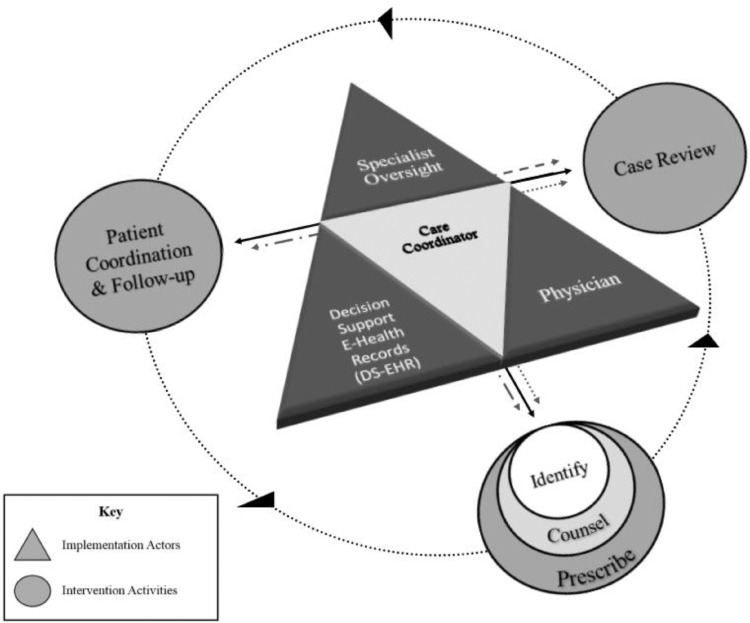
The following sections present detailed portions of the INDEPENDENT care model (Fig. 1) with findings relative to each hypothesized configuration.
Fig. 1.
Implementation actors in relationship to INDEPENDENT care model components.
3.1. Care coordinator-led patient care using the decision-support electronic health record system (Configuration 1)
Initially, the care coordinators felt overwhelmed with their responsibilities of identifying and counseling patients in need of mental health treatment (Fig. 2 Panel A). When asked to reflect on the care coordinators’ role and responsibilities, both psychiatrists expressed concern over burnout. One elaborated that a formal debriefing system for the care coordinators was lacking, while the other felt they needed guidance on how to establish boundaries within their work to maintain confidence in their abilities. Receiving support from the psychiatrist or another care coordinator offered one way to cope with the stress and emotional burden of this position.
Fig. 2.
INDEPENDENT care model contexts, mechanisms, and outcomes
Note: DS-EHR: decision-support electronic health record system
The care coordinators relied on the psychiatrists’ feedback and the on-going technical assistance until they were more experienced in providing mental health counseling, and thus, more comfortable with their depression treatment-related responsibilities. All care coordinators noted that the training on motivational interviewing, after the start of the trial, made them feel more confident in their counseling abilities because they felt this approach took the pressure off of the provider by putting the onus on the patients to come up with ways to address their problems. This was particularly valued when those problems fell outside of their realm of control (e.g., issues with family, work, finances). Additionally, one of the tools designed to help care coordinators identify high-risk patients, the decision-support electronic health record system, had initial prompt malfunctions that reduced care coordinators’ and physicians’ trust in the software. Coupled with inconsistent access to the online software due to issues with internet access and speed, the paper version of the depression algorithm became the default mental health treatment aid across sites.
An environmental barrier to discussing sensitive topics was that both clinics lacked a dedicated private space for care coordinators to administer the 9-item patient health questionnaire (PHQ-9) and counsel patients. As a result of these barriers, they largely avoided using the term depression and instead inquired about patients’ mental well-being using colloquial terms after several in-person visits to establish rapport. Care coordinators noted and used terminology the patients used to describe their state of mental health (e.g., tension, stress, heavy-hearted). Having in-person visits also allowed them to pick up on behavioral indicators that patients may be depressed.
3.2. Usual care diabetes physician-led depression treatment (Configuration 2)
Physicians described their increased confidence in prescribing anti-depressants (Fig. 2 Panel A) as a response to how patients processed through the clinics and the frequency of case reviews (the other two spheres of intervention activities depicted in Fig. 2 Panel A [i.e., patient coordination and follow-up; case review] that are also outcomes of context-mechanism-outcome configuration 3). Patients met with the care coordinators and their physician on the same day at both sites. At the private clinic it was standard procedure to take biological samples, run labs, and consult both the care coordinator and physician in one day, but at the government clinic, receiving counseling and a physician consultation on the same day was a specific modification to the clinic flow to accommodate their low-income patients, the majority of whom had to travel long distances and forfeit wages to appear for clinic appointments.
Though both clinics have high patient caseloads, the patient volume at the government clinic only allows for physicians to spend a few minutes consulting with each patient. In order to cover the A, B,C's (e.g., HbA1c, blood pressure, and cholesterol) of diabetes care, as well as depression treatment, care coordinators sat in on patient consultations to brief the physicians. They provided the patients’ lab results and any treatment prompts produced by the decision support software, then quickly highlighted any relevant circumstances, as discussed in the preceding counseling session, and recorded physician dictations for follow-up. As one physician summarized, “We shifted the fulcrum of care away from the physician to this care coordinator, who's essentially trying to do both things: looking after global diabetes care, in terms of the traditional A, B, and C, and adding a D.” Physicians also noted that their familiarity with patient's medical histories made it easier for them to pick up on behavior change and anticipate patient health trends.
Physicians largely avoided using the term depression because they believed the stigma associated with the term depression would keep the patients from returning. The psychiatrist at one site recognized this reluctance as a phenomenon common among physicians outside of their specialty, raising the concern that by being sensitive to patients’ fear of having depression, providers may inadvertently help perpetuate it.
Physicians expressed being hesitant to prescribe anti-depressants at the onset of the trial. The physicians were endocrinologists, so they perceived their responsibility to be diabetes care, with the case reviews serving as the source of depression treatment directives. Several physicians expressed fear of inappropriately prescribing anti-depressants, even with the algorithm as a reference. With more case reviews, however, physicians picked up on patterns of care advised by the psychiatrists and felt more confident in their ability to prescribe anti-depressants and up-titrate doses. If concerns arose during a patient consultation in the private clinic, the off-site psychiatrist was called for guidance, while the physicians at the government clinic called emergency case reviews or convened case reviews at shorter intervals if such a need arose.
3.3. Case review meetings and patient follow-up care (Configuration 3)
Care coordinators received initial and on-going training on how to support and link patients, usual care diabetes physicians, and the specialist psychiatrist and endocrinologist using the decision-support electronic health record system. Care coordinators reported feeling able to manage their responsibilities (Fig. 2 Panel A), however, they expressed mixed feelings about being able to exert control in their position. Care coordinators downplayed their role, emphasizing the fact that physicians and psychiatrists make the final treatment decisions and dictate follow-up schedules. The case reviews were, however, dependent on care coordinator involvement. In reflecting on their role in these meetings, care coordinators felt, as one shared that “the entire spotlight is on [the care coordinators]” and “what we say, based on that only psychiatrist is prescribing the anti-depressant.” Care coordinators felt under pressure to perform their duties to the highest standard, knowing that the psychiatrists’ only connection to the patients was through them. Referencing their lack of expertise in mental health care, the care coordinators repeatedly expressed concern that patients would not receive proper treatment for their depressive symptoms if they unknowingly left out an important aspect of the patient's life history; an aspect not captured in the decision-support electronic health record system or notated in the individual patient care review sheets. They reported feeling more confident in their abilities once they became accustomed to the types of questions the specialists asked in the case reviews and when they were provided with case review templates that helped structure and guide those discussions.
How care coordinators perceived their authority and power in their role was incongruent with how the specialists viewed it. In the government clinic, the specialists felt that the coordinators had almost equal power in identifying patient care needs because they spent more time with the patients, and therefore had more insight to offer on new and evolving issues in patient circumstances. At the government clinic, however, the usual care diabetes physicians also served as the specialists in the case review meetings, which led the care coordinators to take on a secondary leadership role in terms of facilitating the meetings. This was in contrast to the private clinic where the endocrinologists’ only connection to the patient was through the care coordinator and therefore allowed for the care coordinator to facilitate meetings and provide updates and information on patients.
Case review logs show that while both clinics had variability in the length of time between meetings, the government clinic met, on average, once a month and the private clinic, on average, met twice a month. Case reviews typically lasted one to two hours in the government clinic and two to three hours at the private clinic when clinics were operating with full patient caseloads. These time demands aligned with the patient caseload at the respective clinics, as the private clinic had nearly double the number of intervention patients.
Care coordinators had to establish a flow of patients that enabled labs to be completed in a timely manner while meeting both patient and provider scheduling needs. With limited space in the waiting areas and long patient queues, the coordinators aimed to reduce patients’ wait time by only scheduling two to three intervention arm patients on a given day. Despite these efforts, it was not uncommon to have no-shows or unscheduled patients arrive seeking appointments.
3.4. Specialist treatment oversight (Configuration 4)
The psychiatrists were advocates for this model of care due to the shortage of trained mental health professionals in India. Both psychiatrists had prior experience participating in tiered or distance-delivered mental health treatment models, noting that this approach differed in that they did not meet patients and the care coordinators and physicians had minimal depression counseling and treatment knowledge. The psychiatrists viewed their role in this integrated care model as mental health educators whose responsibility was to develop and train less specialized and less experienced providers on the use of a depression treatment algorithm and provide treatment oversight.
Despite recognizing the need to broaden the base of mental health care in India, the act of providing feedback and overruling depression treatment decisions on cases where they had never met the patient left the psychiatrists feeling uncertain about how to proceed in this unique role (Fig. 2 Panel B).
The inability to assess patients’ body language, tone, and emotional state for themselves made the psychiatrists value the input of the care coordinators. Often at case reviews, this meant the psychiatrists asked the coordinators for details that were not on the patient case review sheets to better understand how to proceed with treatment. One of the psychiatrists created a patient case review template in an effort to better aid the care coordinators in distilling relevant patient information in a structured manner for the case reviews. The other site was provided the template and modified it for use at their clinic. The psychiatrists’ primary concern in being disconnected from the patient was being too reliant on “the numbers,” which can be misleading without a holistic understanding of the patient's situation. In fact, the only numbers used to supplement input from the care coordinators were the two most recent PHQ-9 scores broken down by domains. This layout and trajectory of scores helped the psychiatrist assess where improvements had been made and where new issues were developing, in addition to confirming that a suicide protocol had not been missed. As this quick and efficient method for obtaining relevant information on patients fell into place at each site, the psychiatrists felt more comfortable providing advice on how to proceed with prescribing and altering anti-depressants and counseling patients.
4. Discussion
Causal mechanisms of complex interventions cannot be understood as independent components because they are impacted by other intervention components and activities.19 The value of this evaluation is its ability to consider all provider-related components in relationship to one another when identifying capacity-building and contextual leverage points. Realist evaluation also recognizes that causation is bi-directional.9 In this study, this is demonstrated in the revised program theory (Table 1 with supporting evidence in Electronic Supplementary Material 5) wherein outcomes linked to responsibilities of the care coordinators served as context for the activation of physicians’ confidence. Similarly, the provision of treatment oversight from the psychiatrist, in and out of the case reviews, was a contextual feature noted as important by both coordinators and physicians.
Table 1.
Revised program theory.
 |
While a multitude of mental health care task shifting approaches have been advocated for and utilized in low- and middle-income countries,20,21 there is no consensus as to what types of education, training, and support structures are needed to produce non-specialized health workers who can efficiently fill the void of mental health service providers.22, 23, 24, 25 Short-term training with specialist mental health oversight and on-going supervision have been shown to improve workers’ confidence and their ability to detect and treat mental disorders, including depression, but little is known about the sustainability of workers’ knowledge and skills, or the type of guidance needed to support these workers.1,26 Results from this evaluation demonstrate that having a tiered model of care that offers unspecialized health providers various types of supervision, peer-support, and on-going debriefing and training opportunities at monthly intervals, enables care coordinators to successfully coordinate patient care and contribute to the promotion of effective chronic disease self-management and treatment among patients over a sustained period of time. Future work to disseminate this model of care should seek to measure care coordinators’ perceived self-efficacy, knowledge, and skill over of time, in order to better understand the role of sustained supervision and support.
Physicians in this study largely avoided the use of the term depression, unless prescribing an anti-depressant, as they were uncomfortable initiating conversations about mental health with patients. These findings are consistent with other studies examining physician perceptions on caring for patients with mental illness and co-morbid medical conditions.27,28 Although a physician's extent of psychiatric training may impact her/his willingness to prescribe anti-depressant medications, it is also possible that patients with complex, co-morbid chronic conditions pose additional treatment challenges in regard to disentangling their medical needs.29 As was seen in this evaluation, when there is consistency in who provides care, usual care diabetes physicians are able to obtain more contextual information about a patient's situation and therefore make more informed treatment decisions, a factor that also increased their confidence in providing integrated care. Future implementation of this care model should incorporate additional educational training for usual care diabetes physicians on how to communicate effectively with patients with depressive symptoms to increase physicians’ skills and confidence in treating depression, as well as changes in attitudes towards psychiatry that may shape beliefs about the value of integrating mental health care.
The utility of the decision-support electronic health record system in this intervention varied in supporting physician's treatment decisions and case review meetings. The use of a decision-support electronic health record system has previously been found effective in improving the achievement of diabetes care goals in India,7 with physicians reporting that the software served as a useful treatment aid.30 Providers in this evaluation similarly utilized the software system as a safety-net for quality control. The INDEPENDENT study added a case review component, which physicians reported relying on more than the decision support prompts when it came to incorporating the added dimension of depression treatment into their usual diabetes care practices. The decision-support electronic health record system did, however, provide a helpful at-a-glance color-coded snapshot of all clinic patients through the patient dashboard that guided case review discussions and helped prioritize patient follow-up needs. Care coordinators were responsible for maintaining updated accounts of patients’ progress and appointments, yet found that several components that were needed to make this tracking possible (e.g., a scheduling function, dashboard of patients on anti-depressants; interim form for non-medical contact points) were missing from the software. Additional system modifications would enhance and encourage use of the software in all arenas of patient care and follow-up.
Evidence-based mental health interventions are not commonly implemented in low- and middle-income countries, which has contributed to a scarcity of research testing whether these interventions, largely developed in Western countries, fit the cultural needs of diverse low- and middle-income country settings.31 Psychiatrists in this study took time to adjust to the unfamiliar model of specialist oversight because they valued the goal of the care model. The participating psychiatrists referenced the mental health treatment gap in India32 as an underlying motivation for their involvement in efforts to support and train non-mental health specialists. Future dissemination of this care model would benefit from adding mentorship and support for the psychiatrists from other health professionals with experience training non-specialists and implementing variations of distance-delivered care.
4.1. Summary
The revised program theory describes which inputs and contexts are critical for the INDEPENDENT care model to work in India, and potentially other low-resource settings. Contextual leverage points related to work place design and interpersonal relationships were adaptive and therefore easier to address as they arose as barriers to implementation. We identified one new mechanism: there were mixed circumstances under which providers used the term depression when counseling patients and prescribing anti-depressants. This highlighted a gap in provider training, pointing to the need for culturally sensitive anti-stigma and communication training to make physicians and care coordinators comfortable initiating discussions with patients about depressive symptoms and treatment plans, when indicated. Efforts to scale this model should, however, prioritize the training and support of care coordinators by ensuring on-going access to a site psychiatrist outside of case review meetings and resources (e.g., dedicated space, booster training sessions, structured patient in-take forms) that promote implementation.
4.2. Strength and limitations
The strength of this study is its use of multiple data sources during active trial implementation, which captured the dynamic interplay of how mechanisms change in response to adapted resources and altered contexts. The RAMESES II checklist33 and standards for reporting qualitative research34 were used to document the qualitative methods and realist approach used in this study. Though the sample size was limited by the number of implementation actors, elements of clinical context were triangulated from all implementation actors at each site to ensure data validity and data saturation for each configuration. Due to limitations in time and resources, only two of the four trial sites were included in the process evaluation. The included sites were selected to ensure variation in geographic representation, institutional type, culture, and implementation adaptations, which provided data to employ a negative case analysis approach when comparing data within and across sites. Face-to-face interviewing introduces the threat of social desirability response bias; therefore, the initial fieldwork included clinic observations so that the interviewer could understand and verify site-specific implementation adaptations.
5. Conclusion
As the first realist process evaluation of a depression-focused chronic disease care model in a lower middle-income country, the revised program theories provide a foundation from which future efforts to disseminate and scale this model can build. These findings demonstrate that it is feasible to integrate depression and diabetes care in low-resource settings when providers are supported in adapting the mode of intervention delivery to fit their unique clinic setup, staffing structures, organizational culture, and resource constraints.
Funding
This study was supported by the National Institutes of Health through the Fogarty Global Health Fellows and Scholars Program (VECD Consortium, D43 TW009337) and the National Institute for Mental Health. The funders had no involvement in the study design; collection, analysis and interpretation of data; writing of the report; and the decision to submit the article for publication.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
We would like to thank the investigators and study staff at each of the clinic sites.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.ajmo.2022.100015.
Appendix. Supplementary materials
References
- 1.Kakuma R., Minas H., van Ginneken N., et al. Human resources for mental health care: current situation and strategies for action. Lancet. 2011;378(9803):1654–1663. doi: 10.1016/S0140-6736(11)61093-3. [DOI] [PubMed] [Google Scholar]
- 2.Saxena S., Thornicroft G., Knapp M., Whiteford H. Resources for mental health: scarcity, inequity, and inefficiency. Lancet. 2007;370(9590):878–889. doi: 10.1016/S0140-6736(07)61239-2. [DOI] [PubMed] [Google Scholar]
- 3.Director General of Health Services . DGHS; New Delhi: 1990. National Mental Health Programme: A Progress Report (1982-1990) [Google Scholar]
- 4.Government of India . Ministry of Health and Family Welfare; 2011. Regional Workshops of National Mental Health Programme-a Report 2011-2012. [Google Scholar]
- 5.Kumar A. District mental health programme in India: a case study. J Health Dev. 2005;1(1) [Google Scholar]
- 6.World Health Organization; Geneva: 2017. Depression and Other Common Mental Disorders: Global Health Estimates. [Google Scholar]
- 7.Hussain S., Habib A., Singh A., Akhtar M., Najmi A.K. Prevalence of depression among type 2 diabetes mellitus patients in India: a meta-analysis. Psychiatry Res. 2018;270:264–273. doi: 10.1016/j.psychres.2018.09.037. [DOI] [PubMed] [Google Scholar]
- 8.International Diabetes Federation. IDF Diabetes Atlas. 2021.
- 9.Pawson R., Tilley N. Sage; London, U.K: 1997. Realistic Evaluation. [Google Scholar]
- 10.Marchal, B., Van Belle, S., & Westhorp, G. Realist Evaluation. Available from http://betterevaluation.org/en/approach/realist_evaluation [Accessed 20 January 2019 ].
- 11.McGregor M., Lin E.H., Katon W.J. TEAMcare: an integrated multicondition collaborative care program for chronic illnesses and depression. J Ambul Care Manag. 2011;34(2):312–322. doi: 10.1097/JAC.0b013e31820ef6a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ali M.K., Singh K., Kondal D., Devarajan R., Patel S.A., Shivashankar R., et al. Effectiveness of a multicomponent quality improvement strategy to improve achievement of diabetes care goals: a randomized, controlled trial. Ann Intern Med. 2016;165(6):399–408. doi: 10.7326/M15-2807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kowalski A.J., Poongothai S., Chwastiak L., Hutcheson M., Tandon N., Khadgawat R., et al. The INtegrating DEPrEssioN and Diabetes treatmENT (INDEPENDENT) study: design and methods to address mental healthcare gaps in India. Contemp Clin Trials. 2017;60:113–124. doi: 10.1016/j.cct.2017.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ali M.K., Chwastiak L., Poongothai S., Emmert-Fees K.M.F., Patel S.A., Anjana R.M., et al. Effect of a collaborative care model on depressive symptoms and glycated hemoglobin, blood pressure, and serum cholesterol among patients with depression and diabetes in India: the INDEPENDENT randomized clinical trial. JAMA. 2020;324(7):651–662. doi: 10.1001/jama.2020.11747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Johnson L.C.M., Chwastiak L., Poongothai S., Tandon N., Anjana R.M., Aravind S., et al. Adaptations and patient responses to behavioral intervention components in a depression-focused chronic disease care model implemented in India. Trans Behav Med. 2020;10(1):35–45. doi: 10.1093/tbm/ibz192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cane J., O'Connor D., Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement Sci : IS. 2012;7:37. doi: 10.1186/1748-5908-7-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Guest G., Bunce A., Johnson L. How many interviews are enough?: An experiment with data saturation and variability. Field Methods. 2006;18(1):59–82. doi: 10.1177/1525822x05279903. [DOI] [Google Scholar]
- 18.Elo S., Kyngäs H. The qualitative content analysis process. J Adv Nurs. 2008;62(1):107–115. doi: 10.1111/j.1365-2648.2007.04569.x. [DOI] [PubMed] [Google Scholar]
- 19.Rosen A., Proctor E. Specifying the treatment process. J Soc Serv Res. 1978;2(1):25–43. [Google Scholar]
- 20.Javadi D., Feldhaus I., Mancuso A., Ghaffar A. Applying systems thinking to task shifting for mental health using lay providers: a review of the evidence. Glob Ment Health. 2017;4 doi: 10.1017/gmh.2017.15. (Camb)e14-e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rebello T.J., Marques A., Gureje O., Pike K.M. Innovative strategies for closing the mental health treatment gap globally. Curr Opin Psychiatry. 2014;27(4):308–314. doi: 10.1097/YCO.0000000000000068. [DOI] [PubMed] [Google Scholar]
- 22.Joshi R., Alim M., Kengne A.P., Jan S., Maulik P.K., Peiris D., et al. Task shifting for non-communicable disease management in low and middle income countries–a systematic review. PloS One. 2014;9(8):e103754. doi: 10.1371/journal.pone.0103754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Patel V., Chowdhary N., Rahman A., Verdeli H. Improving access to psychological treatments: lessons from developing countries. Behav Res Ther. 2011;49(9):523–528. doi: 10.1016/j.brat.2011.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Patel V., Weiss H.A., Chowdhary N., Naik S., Pednekar S., Chatterjee S., et al. Effectiveness of an intervention led by lay health counsellors for depressive and anxiety disorders in primary care in Goa, India (MANAS): a cluster randomised controlled trial. Lancet. 2010;376(9758):2086–2095. doi: 10.1016/S0140-6736(10)61508-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Patel V. Mental health in low- and middle-income countries. Br Med Bull. 2007;(81-82):81–96. doi: 10.1093/bmb/ldm010. [DOI] [PubMed] [Google Scholar]
- 26.Armstrong G., Kermode M., Raja S., Suja S., Chandra P., Jorm A.F. A mental health training program for community health workers in India: impact on knowledge and attitudes. Int J Ment Health Syst. 2011;5(1):17. doi: 10.1186/1752-4458-5-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Loeb D.F., Bayliss E.A., Binswanger I.A., Candrian C., deGruy F.V. Primary care physician perceptions on caring for complex patients with medical and mental illness. J Gen Intern Med. 2012;27(8):945–952. doi: 10.1007/s11606-012-2005-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Welch L.C., Litman H.J., Borba C.P., Vincenzi B., Henderson D.C. Does a physician's attitude toward a patient with mental illness affect clinical management of diabetes? results from a mixed-method study. Health Serv Res. 2015;50(4):998–1020. doi: 10.1111/1475-6773.12267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kisely S., Linden M., Bellantuono C., Simon G., Jones J. Why are patients prescribed psychotropic drugs by general practitioners? Results of an international study. Psychol Med. 2000;30(5):1217–1225. doi: 10.1017/s0033291799002743. [DOI] [PubMed] [Google Scholar]
- 30.Singh K., Johnson L., Devarajan R., Shivashankar R., Sharma P., Kondal D., et al. Acceptability of a decision-support electronic health record system and its impact on diabetes care goals in South Asia: a mixed-methods evaluation of the CARRS trial. Diabet Med. 2018;35(12):1644–1654. doi: 10.1111/dme.13804. [DOI] [PubMed] [Google Scholar]
- 31.Rathod S., Pinninti N., Irfan M., Gorczynski P., Rathod P., Gega L., et al. Mental health service provision in low- and middle-income countries. Health Serv Insights. 2017;10 doi: 10.1177/1178632917694350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bruckner T., Scheffler R.M., Shen G., Yoon J., Chisholm D., Morris J., Fulton B.D., Poz M.R.D., Saxena S. The mental health workforce gap in low- and middle-income countries: a needs-based approach. Bull World Health Organ. 2011;89(3):184–194. doi: 10.2471/BLT.10.082784. World Helath Organization. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wong G., Westhorp G., Manzano A., Greenhalgh J., Jagosh J., Greenhalgh T. RAMESES II reporting standards for realist evaluations. BMC Med. 2016;14(1):96. doi: 10.1186/s12916-016-0643-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.O'Brien B.C., Harris I.B., Beckman T.J., Reed D.A., Cook D.A. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med. 2014;89(9):1245–1251. doi: 10.1097/ACM.0000000000000388. : journal of the Association of American Medical Colleges. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.