Background:
Skin-to-skin operative time (OT) as a risk factor for adverse postoperative outcomes in microvascular breast reconstruction has not been thoroughly investigated. This study evaluates OT’s impact on length of stay (LOS), overall morbidity, individual complications, and unplanned reoperation (UR) in deep inferior epigastric artery perforator (DIEP) flaps, with a primary objective of identifying a clinically relevant time of decreased odds.
Methods:
Patients who underwent bilateral DIEP flaps from 2010 to 2021 by two senior surgeons (N.T.H. and S.S.T.) with standardized surgical and postoperative protocols were retrospectively reviewed. One thousand flaps (500 patients) were analyzed with extensive multivariate regression equations to adjust for potential confounders, including intraoperative complexity. The odds of postoperative complication, extended LOS (eLOS, defined as ≥5 days) were compared across OT per hour and OT intervals.
Results:
After risk-adjustment, each hour of OT increased morbidity by 19%, UR by 8.7%, and LOS by 6.5 hours (all P < 0.001). For eLOS, procedures ≤5 hours had 9.5 times lower odds than ≥5 hours (P = 0.050), 5–7 hours had comparable odds (P = 0.540), and 7–9 hours had 5.5 times lower odds than procedures ≥ 9 hours (P < 0.001). Last, a multivariate linear regression showed that LOS can be calculated from OT: LOS (days) =1.527 + 0.272 × OT (hours) (R2 = 0.308; P < 0.001).
Conclusions:
OT (per hour) independently predicts morbidity, UR and LOS in DIEP flaps. Furthermore, 5 and 9 hours are critical cutoffs for eLOS. These findings emphasize the benefits of decreasing OT through efficiency models, such as process analysis, team-based intraoperative protocols, and co-surgery model.
Takeaways
Question: How does operative time impact outcomes in bilateral DIEP flap breast reconstruction?
Findings: One thousand DIEP flaps performed with standardized intraoperative and postoperative protocols were analyzed with extensive multivariate regression equations to adjust for potential confounders, including intraoperative complexity. After risk-adjustment, each hour of operative time increased morbidity by 19.0%, unplanned reoperation by 8.7%, and length of hospital stay (LOS) by 6.5 hours (all P < 0.001). A multivariate linear regression showed that each additional 3.7 hours of operative time predicted a 1-day increase in LOS.
Meaning: Hours of operative time in DIEP flap breast reconstruction independently predicts postoperative complications, length of hospital stay, and unplanned reoperation.
INTRODUCTION
The impact of operative time (OT) on postoperative complications is especially relevant to complex reconstructive procedures as they are often inherently lengthy. Previously, 3, 6, and 6.77 hours1,2 were suggested as critical periods beyond which morbidity was significantly increased. These prior studies included a broad range of plastic surgery procedures, most of which lack the complexity inherent to microsurgical breast reconstruction.
Currently, many regard the deep inferior epigastric perforator (DIEP) flap as the gold standard of autologous breast reconstruction, and in recent years, this procedure has rapidly grown in popularity. In 2018, DIEP flaps accounted for 9% of all breast reconstructions3 compared to 17% in 2020.4 Despite the increased recovery and OT, patients undergoing autologous reconstruction have higher satisfaction with overall well-being and breast outcomes, as well as sexual and psychosocial well-being when compared to implant-based reconstruction.5 Improving the postoperative course of autologous breast reconstruction through identifying critical surgical variables is crucial to advancing breast reconstruction outcomes and improving satisfaction in an increasingly large patient population seeking natural, permanent, and durable reconstruction.
Our study aims to provide a better understanding of the impact of procedure duration in microsurgical breast reconstruction. Specifically, the goal is to identify the relationship between OT and postoperative morbidity and LOS, and as a result, provide general clinical guidelines for OT management in DIEP flaps. We hypothesized that longer OT in DIEP flaps will be independently associated with increased rate and odds of adverse postoperative events.
PATIENTS AND METHODS
A retrospective review of all patients treated with bilateral DIEP flaps performed by the two senior surgeons (N.T.H. and S.S.T.) at our university hospital from January 2010 to October 2021 was performed. A total of 1176 flaps (588 patients) were identified. One hundred seventy-six flaps (88 patients) were excluded secondary to missing any covariates measuring intraoperative complexity (eg, perforator variables) necessary for risk adjustment, leaving 1000 flaps (500 patients) for analysis. Strict inclusion/exclusion criteria were applied before statistical analysis, including a minimum follow-up time of 3 months.6–11 Exclusion criteria included patients receiving bilateral DIEPs with any missing covariate, unilateral procedures, conjoined and stacked flaps, profunda artery perforator (PAP) flaps, lumbar artery perforator (LAP) flaps, and all other forms of breast reconstruction. Data were recorded from the medical record. Postoperative complications included all complications after DIEP flap reconstruction. We categorized complications into three types: requiring (1) outpatient treatment; (2) treatment requiring readmission; and (3) unplanned hospital course treatment. The odds of fat necrosis which takes substantially longer to develop and blood transfusion which did not fit into our classification of complications were calculated individually. OT was defined as skin incision to closure time of only the reconstruction (exclusive of the duration of the mastectomy). Occurrences of all adverse outcomes were calculated per patient and flap-site complications were calculated per patient. The demographics, comorbidities, surgical factors, LOS, unplanned reoperation (UR) during the hospital course (UR), and postoperative complications were assessed. [See table, Supplemental Digital Content 1, which displays how *fat necrosis was defined as a palpable, distinct mass larger than 1 centimeter on physical examination or imaging that was present 6 or more weeks postoperatively. **OT is defined as skin incision to skin closure of only the DIEP flap reconstruction (not inclusive of the duration of the mastectomy). ***Mixed reconstruction refers to an asymmetrical reconstruction with a combination of immediate, delayed-immediate, and delayed timing (eg, delayed right breast and immediate-delayed left breast). ****Perforators were categorized into 5 sizes: diminutive (<1.0 mm), small (1.0 mm), medium (1.5 mm), large (2.0 mm), and giant (>2.0 mm), http://links.lww.com/PRSGO/C309.]
Statistical Analysis
Summary statistics were reported using median and/or mean ± SD for continuous variables and using percentages for categorical variables. For all statistical tests, significance was defined as a P value less than or equal to 0.050. Statistical analyses were performed using IBM SPSS Version 24 (IBM Corp., Armonk, N.Y.) software.
Operations were grouped into those with and without complications to determine OTs associated with specific complications and analyzed with Mann–Whitney U tests. For analysis of OT as time intervals, subjects were split into quartiles, which were rounded to the nearest hour. The Kruskal–Wallis nonparametric analysis of variance was conducted for continuous variables, and Fisher exact or χ2 test was used as appropriate for nominal variables.
Multivariate analyses were utilized to adjust for possible confounders. The demographic, comorbid, and surgical covariates were first entered into univariable logistic regressions to calculate an odds ratio with a 95% confidence interval (CI) for overall, flap-site, donor-site, and medical complications as well as fat necrosis and blood transfusion. For LOS, a linear regression analysis was also conducted with the same variables to calculate a correlation coefficient, R2 (ie, variance), and constant. Covariates with a value of P <0.15 in univariable regression were included in the multivariable regression model. Independent risk factors were identified, and corresponding odds ratios (ORs) and 95% CI were calculated with risk-adjusted logistic regressions. For the logistic regression of OT intervals, a Helmert contrast, which compares each interval to the mean of the subsequent levels, was used. To identify a critical time associated with increased overall complication, extended LOS (eLOS), and UR odds were compared amongst OT intervals. The cutoff time was defined as the OT beyond which odds for adverse postoperative outcomes significantly increase. Cases above and below each cutoff were compared for each interested outcome. Additionally, the ORs of adverse postoperative outcomes per hour of OT were calculated (eg, donor-site morbidity per hour). Furthermore, LOS was analyzed by a risk-adjusted linear regression. The correlation coefficient, variance (ie, R2), and constant were calculated; an analysis of variance of the regression with a P value less than or equal to 0.05 was considered statistically significant.
RESULTS
Cohort Characteristics/Patient Population
The cohort characteristics and patient outcomes are presented in table, Supplemental Digital Content 1 (http://links.lww.com/PRSGO/C309). The mean ± SD and median of OT were 7.2 ± 3.1 and 6.7 hours, respectively. The mean ± SD and median of LOS were 3.5 ± 1.5 and 3 days, respectively.
Univariate Analyses
Table 1 depicts the average OT when a complication occurs. Procedures with and without complications had an average of 8.07 ± 3.19 and 6.97 ± 2.80 hours (P < 0.001), respectively. Generally, longer procedures were significantly associated with adverse outcomes. eLOS had the largest difference in mean operating time (6.46 versus 10.36 hours; P < 0.001).
Table 1.
Average OT of Complication (Complications vs OT)
| Outcome | Occurrence (OT, h, mean ± SD) | No Occurrence (OT, h, mean ± SD) | P |
|---|---|---|---|
| eLOS (≥5 d) | 10.36 ± 3.63 | 6.46 ± 2.34 | <0.001 |
| UR | 8.26 ± 3.24 | 7.18 ± 3.05 | 0.048 |
| Overall complication (any) | 8.07 ± 3.19 | 6.97 ± 2.99 | <0.001 |
| Flap-site complication (any) | 8.63 ± 3.67 | 6.90 ± 2.80 | <0.001 |
| Breast fat necrosis | 8.59 ± 3.97 | 7.10 ± 2.93 | 0.014 |
| Donor-site complication (any) | 8.07 ± 3.19 | 6.97 ± 2.99 | <0.001 |
| Abdominal fat necrosis | 7.91 ± 2.97 | 7.21 ± 3.07 | 0.221 |
| Medical complication (any) | 7.27 ± 3.06 | 6.87 ± 3.21 | 0.027 |
| Blood transfusion | 8.77 ± 2.72 | 7.18 ± 3.07 | 0.006 |
All adverse postoperative outcomes were entered into Mann–Whitney U tests.
Values in boldface are statistically significant.
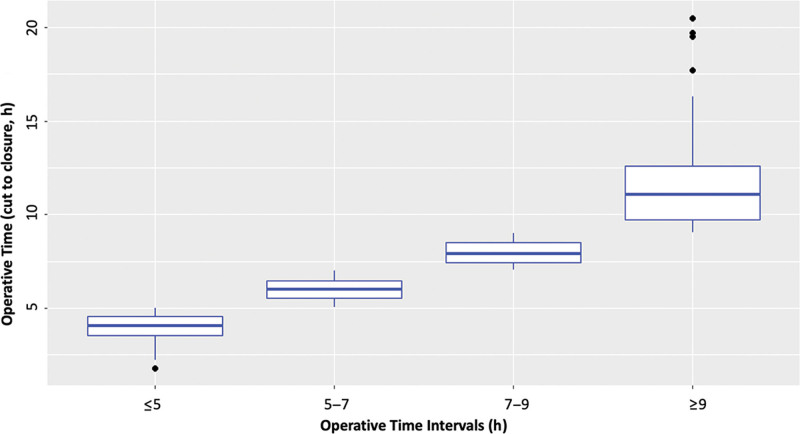
Table 2 shows the distribution of demographics and comorbidities across time intervals. The groups were created by rounding the 25th percentile, 50th percentile, and 75th percentile of OT (ie, 4.92, 6.70, and 8.88 hours) to the nearest hour (ie, 5, 7, and 9 hours) for ease of use as an easy-to-follow guideline for OT (Fig. 1). The patient populations of the four groups were similar, between 24% and 26% of the total population. The distribution of BMI, reconstruction timing, umbilicus removal, microsurgeon experience, number of perforators, and all perforators being on the same row were found to be statistically significant (all P ≤ 0.050). All other variables had no significant difference across intervals. A multivariable analysis was conducted to adjust for potential confounders.
Table 2.
Univariate Analysis of Covariates
| OT Interval (h) | ≤5 h | 5–7, h | 7–9, h | ≥9, h | P |
|---|---|---|---|---|---|
| n = patient (%) | n = 132 (26.4%) | n = 130 (26%) | n = 119 (23.8%) | n = 119 (23.8%) | |
| Age (y) | 51.33 ± 8.95 | 50.88 ± 10.25 | 50.61 ± 9.49 | 49.38 ± 8.74 | 0.546* |
| Body mass index (kg/m2) | 29.81 ± 5.19 | 30.15 ± 5.11 | 32.25 ± 5.56 | 31.28 ± 5.19 | <0.001 * |
| Race (%) | 0.066† | ||||
| Asian | 0.8 | 5.4 | 3.4 | 3.4 | |
| Black | 12.9 | 10 | 24.4 | 15.1 | |
| Hispanic | 8.3 | 13.8 | 6.7 | 11.8 | |
| Other | 8.3 | 4.6 | 5.9 | 5.9 | |
| White | 69.7 | 66.2 | 59.7 | 63.9 | |
| Smoking (%) | 0.635† | ||||
| Current | 0.8 | 2.3 | 3.4 | 1.7 | |
| Former | 21.2 | 20.8 | 25.2 | 26.9 | |
| Never | 78 | 76.9 | 71.4 | 71.4 | |
| Hypertension (%) | 22.7 | 24.6 | 31.9 | 35.3 | 0.089† |
| Diabetes (%) | 5.3 | 9.2 | 11.8 | 10.1 | 0.322† |
| History of abdominal surgery (%) | 73.5 | 70.8 | 78.2 | 73.1 | 0.611† |
| Autoimmune (%) | 5.3 | 8.5 | 5 | 7.6 | 0.628† |
| Radiation (%) | 38.6 | 38.5 | 42.9 | 42 | 0.849† |
| Neoadjuvant chemotherapy (%) | 33.3 | 30.8 | 32.8 | 26.9 | 0.693† |
| Adjuvant chemotherapy (%) | 25 | 31.5 | 27.7 | 25.2 | 0.616† |
| Reconstruction timing (%) | <0.001 ‡ | ||||
| Immediate | 9.8 | 10.8 | 17.6 | 42 | |
| Delayed-Immediate | 78.8 | 74.6 | 68.1 | 36.1 | |
| Delayed | 7.6 | 12.3 | 10.9 | 18.5 | |
| Mixed | 3.8 | 2.3 | 3.4 | 3.4 | |
| Umbilicus removal (%) | 64.4 | 30.8 | 23.5 | 7.6 | <0.001 ‡ |
| Microsurgeon experience (%) | <0.001 ‡ | ||||
| 2010–2015 | 0.8 | 9.2 | 45.4 | 80.7 | |
| 2016–2021 | 99.2 | 90.8 | 54.6 | 19.3 | |
| Breast arterial revision (L/R) (%) | 8.3/7.6 | 6.2/10.8 | 11.8/7.6 | 12.6/13.4 | 0.272/0.342† |
| Breast venous revision (L/R) (%) | 0.8/1.5 | 3.1/2.3 | 4.2/2.5 | 5.9/1.7 | 0.150/0.930† |
| Breast perforator number (L/R) | 1.73 ± 0.82/1.85 ± 0.80 | 2.05 ± 0.89 | 2.03 ± 1.00/2.07 ± 0.93 | 2.10 ± 1.00/2.28 ± 1.09 | 0.008/0.012 * |
| /1.95 ± 0.96 | |||||
| Breast perforators on the same row (L/R) (%) | 13.6/12.9 | 30.0/26.2 | 29.4/34.5 | 26.1/31.1 | 0.007/<0.001 † |
| Breast perforator average size category (mm) (L/R) (median) | Medium (1.5)/Medium (1.5) | Medium (1.5)/Medium (1.5) | Medium (1.5)/Medium (1.5) | Medium (1.5)/Medium (1.5) | 0.351/0.713† |
Covariate profiles were compared across OT intervals. All covariates were first entered into univariable regressions to calculate an odds ratio and 95% CI for each adverse outcome; covariates with P ≤ 0.15 were included in all multivariate regressions for risk-adjustment with OT interval, cutoff, and per hour analysis. Bold = statistically significant.
Kruskal–Wallis H
χ2 test
Fisher exact test
Fig. 1.
Bilateral DIEP flap reconstructions lasted between 1.78 and 20.48 hours, with a median time of 6.70 hours. Patients were stratified into four equal quartiles based upon OT, which were then rounded to the nearest hour.
Univariate analysis of adverse postoperative outcomes amongst time intervals of OT is presented in Table 3. eLOS, UR, overall complications, flap-site complications, donor-site complications, breast fat necrosis, and blood transfusion were significantly associated with time intervals (all P ≤ 0.05); however, the occurrence of UR and abdominal fat necrosis was not (both P > 0.05). Last, the distribution of OT across time intervals was statistically significant (P < 0.001).
Table 3.
Univariate Analysis of OT Intervals (Quartiles Rounded to Nearest Hour)
| OT Interval (h) | ≤5 | 5-7 | 7-9 | ≥9 | P |
|---|---|---|---|---|---|
| Patients (%) | n = 132 (26.4%) | n = 130 (26.0) | n = 119 (23.8) | n = 119 (23.8) | |
| OT (Mean ± SD, h) | 3.96 ± 0.71 | 5.98 ± 0.54 | 7.94 ± 0.58 | 11.56 ± 2.35 | <0.001* |
| Outcome | Occurrence (%) | Occurrence (%) | Occurrence (%) | Occurrence (%) | P |
| eLOS (≥5 d) (%) | 3.8 | 9.2 | 22.7 | 47.1 | <0.001 ‡ |
| UR (%) | 3.8 | 5.4 | 10.9 | 6.7 | 0.134† |
| Overall complications (%) | 23.5 | 36.2 | 47.1 | 54.6 | <0.001† |
| Flap-site complications (%) | 14.4 | 10 | 26.1 | 30.3 | <0.001 † |
| Breast fat necrosis | 5.3 | 7.7 | 10.1 | 14.3 | 0.090‡ |
| Donor-site complications(%) | 15.2 | 21.5 | 27.7 | 34.5 | 0.003 † |
| Abdominal fat necrosis (%) | 3 | 1.5 | 6.7 | 5 | 0.171† |
| Medical complication (%) | 5 | 8.3 | 10.8 | 5.9 | 0.312† |
| Blood transfusion (%) | 0 | 3.1 | 9.2 | 3.4 | 0.002 ‡ |
Overall morbidity, eLOS, UR, flap-site complications, donor-site complications, medical complications, and many individual complications were significantly associated with higher OT with univariate analysis. Bold = statistically significant.
Kruskal–Wallis H
χ2 test
Fisher exact test
Multivariate Regression Analyses
The odds of adverse postoperative outcomes were assessed with multivariate logistic regressions with Helmert contrast (Table 4). After risk-adjustment, overall complications varied based on OT interval but did not reach statistical significance: reconstructions less than 5 hours had 23.5% occurrence with 1.5 times reduced odds compared to procedures longer than 5 hours which had 45.7% occurrence (P = 0.200). Procedures lasting 5–7 hours had 1.2 times lower odds than procedures lasting 7 hours or longer (P = 0.540), and procedures 7–9 hours had 1.3 times lower odds than operations 9 hours or longer (P = 0.510). For eLOS, procedures 5 hours or less had 3.8% occurrence with 9.5 times lower odds than procedures 5 hours or longer, which had 25.8% occurrence (P = 0.050). Significance was lost when comparing 5- to 7-hour procedures to procedures 7 hours or longer (P = 0.560). Significance was reached again with procedures 7–9 hours, which had 5.5 times lower odds than procedures 9 hours or longer (P < 0.001). For UR, procedures 5 hours or less, 5–7 hours, 7–9 hours, and 9 hours or longer varied in odds of occurrence but did not reach significance (all P > 0.05). Reconstructions 5 hours or less (which had 3.8% occurrence) were 40% less likely than procedures longer than 5 hours (which had 7.6% occurrence) to have UR (P = 0.39). Reconstructions 5–7 hours were 43% less likely than cases longer than 7 hours to have UR (P = 0.33). Reconstructions 7–9 hours were 66% less likely than cases longer than 9 hours to have UR (P = 0.13).
Table 4.
Risk-adjusted Comparisons of OT Intervals
| Overall Complication (Helmert Contrast) | |||
|---|---|---|---|
| OT Category (h) | Occurrence (%) | OR (95% Confidence Interval) | P |
| 1 (≤5) | 23.5 | 0.689 (0.388–1.395) | 0.2 |
| 2 (5–7) | 45.7 | 0.830 (0.460–1.498) | 0.54 |
| 3 (7–9) | 0.7743 (0.359–1.6676) | 0.51 | |
| 4 (≥9) | Reference only | ||
| eLOS (≥5 d) (Helmert Contrast) | |||
| 1 (≤5) | 3.8 | 0.1051 (0.0108–0.9696) | 0.05 |
| 2 (5–7) | 25.8 | 0.7705 (0.3187–1.8627) | 0.56 |
| 3 (7–9) | 0.1834 (0.060–0.5594) | <0.001 | |
| 4 (≥9) | Reference only | ||
| UR (Helmert Contrast) | |||
| 1 (≤5) | 3.8 | 0.601 (0.189–1.912) | 0.39 |
| 2 (5–7) | 7.6 | 0.573 (0.188–1.742) | 0.33 |
| 3 (7–9) | 0.3355 (0.0813–1.3833) | 0.13 | |
| 4 (≥9) | Reference only | ||
After risk-adjustment with demographic, intraoperative, and perforator covariates, there was a statistically significant stepwise increase in risk of eLOS by time intervals (ie, OT quartiles rounded to the nearest hour) but not with overall complication. Helmert contrast compared each OT interval to the mean of the subsequent intervals as the reference value. Bold = statistically significant.
Every hour of OT increased overall complication, eLOS, and UR by 19.2%, 58.5%, and 9.0% (all P = 0.028), respectively (Table 5). Flap-site complication, donor-site complication, flap compromise, flap loss, blood transfusion, breast wound, abdominal wound, breast fat necrosis, and abdominal fat necrosis also significantly increased in odds per hour (all P ≤ 0.05).
Table 5.
Risk-adjusted Outcomes Per Hour of OT
| Outcome | OR (95% Confidence Interval) | P |
|---|---|---|
| eLOS (≥5 d) | 1.585 (1.443–1.766) | <0.001 |
| UR ( | 1.0867 (0.975–1.202) | <0.001 |
| Overall complication | 1.192 (1.120–1.272) | <0.001 |
| Flap-site complication | 1.187 (1.108–1.273) | <0.001 |
| Breast wound | 1.0879 (1.002–1.178) | <0.0001 |
| Flap compromise | 1.101 (0.970–1.236) | <0.001 |
| Flap loss | 1.091 (0.8597–1.3256) | <0.001 |
| Breast fat necrosis | 1.146 (1.146–1.250) | <0.001 |
| Donor-site complication | 1.117 (1.047–1.192) | <0.001 |
| Abdominal wound | 1.112 (1.030–1.199) | <0.001 |
| Abdominal fat necrosis | 1.069 (0.928–1.213) | <0.001 |
| Medical complication | 1.150 (1.008–1.300) | <0.001 |
| Pulmonary embolism | 1.143 (0.8993–1.3941) | <0.001 |
| Blood transfusion | 1.149 (1.007–1.297) | <0.001 |
After risk-adjustment with demographic, intraoperative, and perforator covariates, the risk of morbidity, donor-site complication, medical complication, blood transfusion, fat necrosis, wound, UR, and eLOS significantly increase per hour of operation. Multivariate logistic regressions controlling for demographics, comorbidities, and surgical factors were conducted.
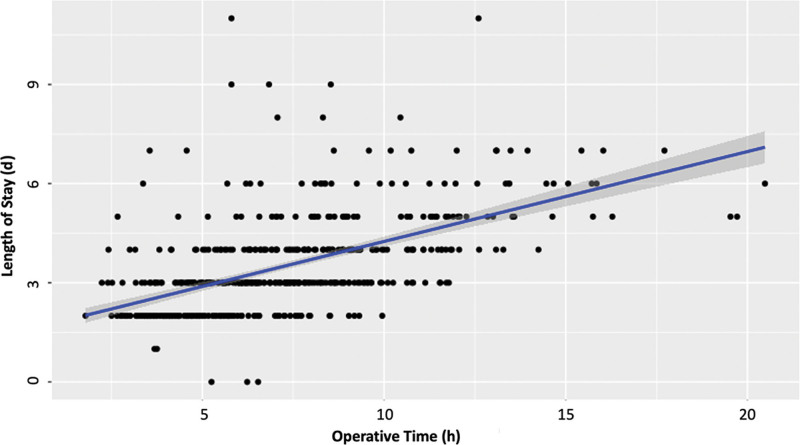
The risk-adjusted linear regression equation [LOS (days) = 1.572 + 0.272 × OT (hours); P < 0.001; R2 = 0.30.8)] explained 30.8% of the variance and predicted that every hour of OT increases the LOS by 6.53 hours (P < 0.001) (Fig. 2). Furthermore, every 3.68 hours of operation increases LOS by one day (P < 0.001).
Fig. 2.
A multivariate linear regression revealed that LOS can be estimated from OT in DIEP flaps from the equation: LOS (days) =1.527 + 0.272 × OT (hours) (R2 = 0.308; P < 0.001). LOS ranged from 1 to 11 days, with a median of 3 days. The Durbin-Watson score of 1.540 showed that the residuals were independent. Furthermore, the residual plots were normally distributed with homoscedasticity. Dots represent observed outcomes and the blue line and gray shading represent predicted outcomes.
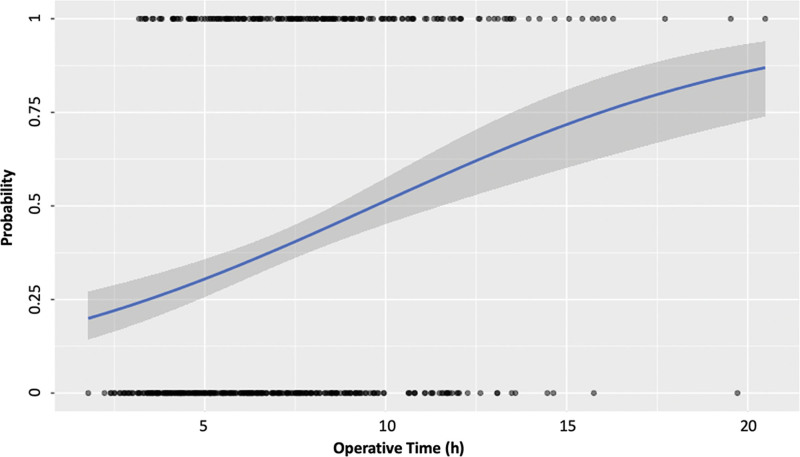
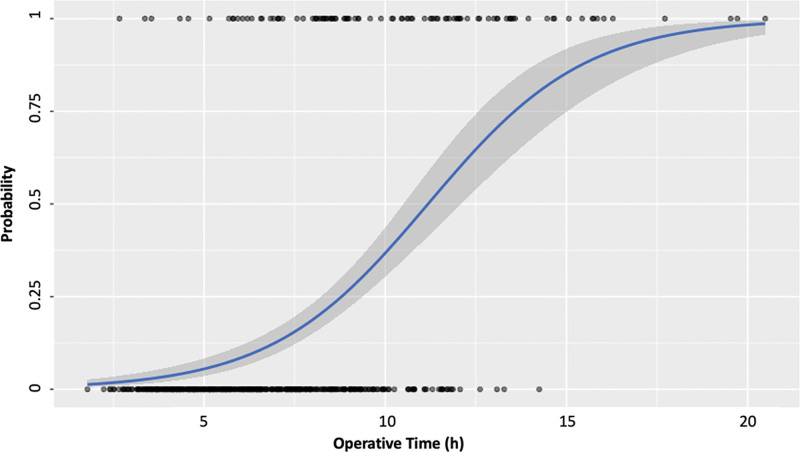
Respectively, Figures 3 and 4 depict the predicted probabilities for overall complication and eLOS with increasing OT.
Fig. 3.
Predicted probabilities calculated from multivariate logistic regression for any complication with increased OT. Dots represent observed outcomes and the blue line and gray shading represent predicted outcomes.
Fig. 4.
Predicted probabilities calculated from multivariate logistic regression for eLOS with increasing OT. Dots represent observed outcomes and the blue line and gray shading represent predicted outcomes.
DISCUSSION
In the current era, microsurgical breast reconstruction requires reduction in postoperative morbidity and balancing aesthetic results with achieving optimal operative efficiency in addition to high flap success. Our group continues to focus on refinements and optimization of DIEP flap breast reconstruction, which remains the cornerstone of autologous breast reconstruction in our practice. In parallel, this has gradually permitted us to expand our autologous breast reconstruction practice to offering other flaps such as a variety of conjoined and stacked flaps, PAP flaps, and LAP flaps.12–21
For clinical relevancy, we divided the cohort into four groups based on quartile OT values rounded to the nearest hour. This resulted in four-time intervals that were similar in size (each between 23% and 27% of the total population). Univariate assessment revealed strong associations between OT intervals and complication occurrence. Multivariate regression was additionally utilized to help decrease the effect of confounders.1,9,22 We included measures of intraoperative complexity (eg, perforator variables and anastomoses revision) and microsurgeon experience for more rigorous risk adjustment than previous studies on the topic. Previous authors showed that every year of practice increased the success of free flaps rather than volume,23 and hence, we used the year of surgery as a surrogate for microsurgeon experience and proficiency. Although complications in autologous breast reconstruction are often reported per flap, we only reported per patient complication rates as they are more clinically relevant.
Previously, 3, 6, and 6.77 hours have been designated as cutoff values for increased morbidity in plastic surgery.1,2 However, none of the previous literature exclusively evaluated breast free flap reconstruction or only DIEP flaps. These previous studies have included medical complications (eg, cardiovascular, renal, and pulmonary) and surgical complications (eg, infection, erythema, necrosis, seroma, and hematoma). Although these absolute cutoffs are useful information, microvascular breast reconstruction has unique differences both intraoperatively and postoperatively. In a study on plastic surgery procedures, it has been demonstrated that when autologous breast reconstruction took longer than 6.77 hours, it doubled the odds of complications.1 This study included various forms of free flap and pedicled flap breast reconstructions which have obviously different OTs and complication profiles. As discussed by the authors, the inherent complexity between widely different procedures could be the true cause of the increase in morbidity.1 Our study is more specific in analysis of the current standard in autologous breast reconstruction. Additionally, we limited our data to only bilateral breast reconstruction and included risk-adjustment for measures of intraoperative complexity (eg, perforator variables and anastomoses revision) in addition to demographic variables to further standardize our analysis of outcomes.
With univariate analysis, we found significant associations with OT intervals (ie, ≤5, 5–7, 7–9, and ≥9 hours) and overall morbidity and eLOS, commonly defined as more than 5 days in free flap breast reconstruction,24–26 (both P ≤ 0.05) but not with UR (P > 0.05). After risk-adjustment with multivariate logistic regressions including operative, perforator, and demographic variables, significance was lost with overall morbidity. These results suggest that in bilateral DIEP flap reconstructions overall complication and UR lack critical OT cutoffs, unlike studies on general cosmetic and reconstructive surgery.1,2 Others have demonstrated a similar loss of significance when comparing anesthesia time intervals (ie, quintiles) to complications after free flap reconstructions.21
Interestingly, the odds of eLOS was significantly less when comparing procedures 5 hours or less to those longer than 5 hours (OR 0.11; P = 0.050) but not when comparing 5- to 7-hour procedures to procedures 7 hours or longer (P = 0.56). Reconstructions lasting 7–9 hours also had significantly lower odds of eLOS than procedures 9 hours or longer (OR 0.18; P < 0.001). These findings suggest that with respect to eLOS, procedures less than 5 hours are the most ideal and that there exists two critical OT points beyond which odds significantly increase: 5 hours and 9 hours. Others have shown similar trends with eLOS more likely after free flap breast reconstructions longer than 500 minutes (8.3 hours)25; this is derived from a national dataset and has inherent significant variability harder to control than in the current study.
Even after extensive risk-adjustment, we found a 19% increase in morbidity per hour of surgery in bilateral DIEP flaps (P < 0.001). Studies on general plastic surgery and tissue expander reconstruction report similar findings with a 22% and 26% rise in odds of morbidity per hour of operation, respectively.1,27 The significance of this cannot be overstated since microvascular procedures typically take longer than other plastic surgery procedures. Our results showed that odds of UR, eLOS, donor-site complications, medical complications, flap-site complications, fat necrosis, blood transfusion, flap compromise, and flap loss significantly increase per hour of OT in DIEP flap reconstructions, supporting the findings of previous free flap literature.2,22,24,25,28–30 Although eLOS is significantly associated with both per hour and OT intervals, our results suggest that postoperative morbidity and UR with DIEP flap reconstructions increases per hour of OT rather than OT intervals after adjusting for intraoperative, perforator, and demographic variables. Overall, it appears OT per hour is a more universal predictor of adverse postoperative outcomes (ie, eLOS, UR, and complication occurrence) compared to OT cutoffs and intervals.
We demonstrated that in DIEP flaps, an estimated LOS can be calculated from OT with a multivariate linear regression equation: LOS (days) =1.527 + 0.272 × OT (hours) (R2 = 0.308; P < 0.001). Another published study also demonstrated a linear relationship between OT and LOS in free flap breast reconstruction: LOS (days) = 2.559 + 0.180 × OT (in hours) (P < 0.0005),25 but included all forms of autologous breast reconstructions. However, their equation only accounted for 6.3% of the variation in OT (our current study accounts for 30.8% of the variation). Their correlation coefficient (0.180) and constant (2.559 days) varied by greater than 50% compared to ours. These differences could be attributable to our inclusion of only DIEP flaps, implementation of Enhanced Recovery After Surgery (ERAS) protocol, and different covariates utilized in risk adjustment.
Given that OT is an independent predictor of adverse outcomes, increasing operative efficiency to reduce OT can improve patient outcomes in DIEP flaps and even other free flap breast reconstruction. Rigorous process analysis of critical maneuvers, identifying inefficient operative steps, and a team-based approach have been shown to significantly reduce OT.31–33 A co-surgery attending model has also been demonstrated to decrease OT, postoperative morbidity, and LOS.34 Additionally, utilizing preoperative imaging, such as computerized tomography angiography, has been shown to decrease the duration of operative steps, specifically with perforator identification and decision making.35
This is the first paper identifying OT as an independent predictor of LOS, UR, and complications in bilateral DIEP flap breast reconstruction. We have demonstrated that every hour of OT (rather than specific OT cutoffs and intervals) increases UR occurrence and postoperative morbidity. LOS can be estimated from OT per hour. eLOS significantly increased with both OT intervals and per hour. With eLOS, procedures less than 5 hours are most ideal with reducing risk, and procedures beyond 9 hours have the highest risk. This study illustrates our evolution towards standardizing intraoperative and postoperative protocols in an effort to decrease complications. The senior authors adopted their co-surgery model in 2011,34 ERAS protocol halfway through 2017, and intraoperative liposomal bupivacaine blocks in 2018.36 Furthermore, rigorous risk adjustment for the impact of perforator data, intraoperative complexity, microsurgeon experience, and demographic variables strengthens the applicability of the results. Prior database studies on similar topics were substantially less standardized, extensive with their covariates used for risk-adjustment, and inclusive of postoperative complications specific to free flap breast reconstruction. However, the current study has several limitations: the study was retrospective in analysis, and although controlling for covariates through multivariate analysis reduces the impact of potential confounders, it does not completely eliminate them. Additionally, we did not adjust for socioeconomic status which has been linked to longer OTs.37,38 Finally, since this is a study of patients from two surgeons with standardized protocols, the results may not be generalizable to other practices.
CONCLUSIONS
OT is an independent determinant of postoperative complications, LOS, and UR, indicating its importance beyond efficiency. We believe that implementing protocols to safely and effectively reduce OT will yield improved outcomes in DIEP flap breast reconstruction.
Supplementary Material
Footnotes
Published online 23 December 2022.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Hardy KL, Davis KE, Constantine RS, et al. The impact of operative time on complications after plastic surgery: a multivariate regression analysis of 1753 cases. Aesthet Surg J. 2014;34:614–622. [DOI] [PubMed] [Google Scholar]
- 2.Howland WS, Schweizer O. Complications associated with prolonged operation and anesthesia. Clin Anesth. 1972;9:1–7. [PubMed] [Google Scholar]
- 3.Statistics ANCoPSP. 2018 Plastic Surgery Statistics Report. Arlington Heights, IL: American Society of Plastic Surgeons. 2018. [Google Scholar]
- 4.Statistics ANCoPSP. 2020 Plastic Surgery Statistics Report. Philadelphia, PA: American Society of Plastic Surgeons. 2020. [Google Scholar]
- 5.Toyserkani NM, Jørgensen MG, Tabatabaeifar S, et al. Autologous versus implant-based breast reconstruction: a systematic review and meta-analysis of Breast-Q patient-reported outcomes. J Plast Reconstr Aesthet Surg. 2020;73:278–285. [DOI] [PubMed] [Google Scholar]
- 6.Baumann DP, Lin HY, Chevray PM. Perforator number predicts fat necrosis in a prospective analysis of breast reconstruction with free TRAM, DIEP, and SIEA flaps. Plast Reconstr Surg. 2010;125:1335–1341. [DOI] [PubMed] [Google Scholar]
- 7.Bhullar H, Hunter-Smith DJ, Rozen WM. Fat necrosis after DIEP flap breast reconstruction: a review of perfusion-related causes. Aesthetic Plast Surg. 2020;44:1454–1461. [DOI] [PubMed] [Google Scholar]
- 8.Garvey PB, Buchel EW, Pockaj BA, et al. DIEP and pedicled TRAM flaps: a comparison of outcomes. Plast Reconstr Surg. 2006;117:1711–1719; discussion 1720–1711. [DOI] [PubMed] [Google Scholar]
- 9.Hembd A, Teotia SS, Zhu H, et al. Optimizing perforator selection: a multivariable analysis of predictors for fat necrosis and abdominal morbidity in DIEP flap breast reconstruction. Plast Reconstr Surg. 2018;142:583–592. [DOI] [PubMed] [Google Scholar]
- 10.Kamali P, Lee M, Becherer BE, et al. Medial row perforators are associated with higher rates of fat necrosis in bilateral DIEP flap breast reconstruction. Plast Reconstr Surg. 2017;140:19–24. [DOI] [PubMed] [Google Scholar]
- 11.Kroll SS. Fat necrosis in free transverse rectus abdominis myocutaneous and deep inferior epigastric perforator flaps. Plast Reconstr Surg. 2000;106:576–583. [DOI] [PubMed] [Google Scholar]
- 12.Cho MJ, Garza R, Teotia SS, et al. Utility of ERAS pathway in nonabdominal-based microsurgical breast reconstruction: efficacy in PAP flap reconstruction? J Reconstr Microsurg. 2021. [DOI] [PubMed] [Google Scholar]
- 13.Cho MJ, Haddock NT, Teotia SS. Clinical decision making using CTA in conjoined, bipedicled DIEP and SIEA for unilateral breast reconstruction. J Reconstr Microsurg. 2020;36:241–246. [DOI] [PubMed] [Google Scholar]
- 14.Haddock N, Nagarkar P, Teotia SS. Versatility of the profunda artery perforator flap: creative uses in breast reconstruction. Plast Reconstr Surg. 2017;139:606e–612e. [DOI] [PubMed] [Google Scholar]
- 15.Haddock NT, Cho MJ, Gassman A, et al. Stacked profunda artery perforator flap for breast reconstruction in failed or unavailable deep inferior epigastric perforator flap. Plast Reconstr Surg. 2019;143:488e–494e. [DOI] [PubMed] [Google Scholar]
- 16.Haddock NT, Cho MJ, Teotia SS. Comparative analysis of single versus stacked free flap breast reconstruction: a single-center experience. Plast Reconstr Surg. 2019;144:369e–377e. [DOI] [PubMed] [Google Scholar]
- 17.Haddock NT, Kelling JA, Teotia SS. Simultaneous circumferential body lift and four-flap breast reconstruction using deep inferior epigastric perforator and lumbar artery perforator flaps. Plast Reconstr Surg. 2021;147:936e–939e. [DOI] [PubMed] [Google Scholar]
- 18.Haddock NT, Suszynski TM, Teotia SS. An Individualized patient-centric approach and evolution towards total autologous free flap breast reconstruction in an academic setting. Plast Reconstr Surg Glob Open. 2020;8:e2681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Haddock NT, Suszynski TM, Teotia SS. Consecutive bilateral breast reconstruction using stacked abdominally based and posterior thigh free flaps. Plast Reconstr Surg. 2021;147:294–303. [DOI] [PubMed] [Google Scholar]
- 20.Haddock NT, Teotia SS. Lumbar artery perforator flap: initial experience with simultaneous bilateral flaps for breast reconstruction. Plast Reconstr Surg Glob Open. 2020;8:e2800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Haddock NT, Teotia SS. Consecutive 265 profunda artery perforator flaps: refinements, satisfaction, and functional outcomes. Plast Reconstr Surg Glob Open. 2020;8:e2682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kim BD, Ver Halen JP, Grant DW, et al. Anesthesia duration as an independent risk factor for postoperative complications in free flap surgery: a review of 1,305 surgical cases. J Reconstr Microsurg. 2014;30:217–226. [DOI] [PubMed] [Google Scholar]
- 23.Mahmoudi E, Lu Y, Chang SC, et al. Associations of surgeon and hospital volumes with outcome for free tissue transfer by using the national taiwan population health care data from 2001 to 2012. Plast Reconstr Surg. 2017;140:455e–465e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Frey JD, Salibian AA, Karp NS, et al. Examining length of hospital stay after microsurgical breast reconstruction: evaluation in a case-control study. Plast Reconstr Surg Glob Open. 2017;5:e1588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kotha VS, Abadeer AI, Amdur RL, et al. A critical examination of length of stay in autologous breast reconstruction: a national surgical quality improvement program analysis. Plast Reconstr Surg. 2021;147:24–33. [DOI] [PubMed] [Google Scholar]
- 26.Offodile AC, II, Aherrera A, Guo L. Risk factors associated with prolonged postoperative stay following free tissue transfer: an analysis of 2425 patients from the American College of Surgeons National Surgical Quality Improvement Program database. Plast Reconstr Surg. 2014;134:1323–1332. [DOI] [PubMed] [Google Scholar]
- 27.Hanwright PJ, Davila AA, Mioton LM, et al. A predictive model of risk and outcomes in tissue expander reconstruction: a multivariate analysis of 9786 patients. J Plast Surg Hand Surg. 2013;47:513–518. [DOI] [PubMed] [Google Scholar]
- 28.Kwok AC, Agarwal JP. Unplanned reoperations after microvascular free tissue transfer: An analysis of 2,244 patients using the american college of surgeons national surgical quality improvement program database. Microsurgery. 2017;37:184–189. [DOI] [PubMed] [Google Scholar]
- 29.Kwok AC, Edwards K, Donato DP, et al. Operative time and flap failure in unilateral and bilateral free flap breast reconstruction. J Reconstr Microsurg. 2018;34:428–435. [DOI] [PubMed] [Google Scholar]
- 30.Offodile AC, 2nd, Aherrera A, Wenger J, et al. Impact of increasing operative time on the incidence of early failure and complications following free tissue transfer? A risk factor analysis of 2,008 patients from the ACS-NSQIP database. Microsurgery. 2017;37:12–20. [DOI] [PubMed] [Google Scholar]
- 31.Haddock NT, Teotia SS. Five steps to internal mammary vessel preparation in less than 15 minutes. Plast Reconstr Surg. 2017;140:884–886. [DOI] [PubMed] [Google Scholar]
- 32.Haddock NT, Teotia SS. Deconstructing the reconstruction: evaluation of process and efficiency in deep inferior epigastric perforator flaps. Plast Reconstr Surg. 2020;145:717e–724e. [DOI] [PubMed] [Google Scholar]
- 33.Haddock NT, Teotia SS. Efficient DIEP flap: bilateral breast reconstruction in less than four hours. Plast Reconstr Surg Glob Open. 2021;9:e3801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Haddock NT, Kayfan S, Pezeshk RA, et al. Co-surgeons in breast reconstructive microsurgery: what do they bring to the table? Microsurgery. 2018;38:14–20. [DOI] [PubMed] [Google Scholar]
- 35.Haddock NT, Dumestre DO, Teotia SS. Efficiency in DIEP flap breast reconstruction: the real benefit of computed tomographic angiography imaging. Plast Reconstr Surg. 2020;146:719–723. [DOI] [PubMed] [Google Scholar]
- 36.Haddock NT, Garza R, Boyle CE, et al. Defining enhanced recovery pathway with or without liposomal bupivacaine in DIEP flap breast reconstruction. Plast Reconstr Surg. 2021;148:948–957. [DOI] [PubMed] [Google Scholar]
- 37.Strum DP, Sampson AR, May JH, et al. Surgeon and type of anesthesia predict variability in surgical procedure times. Anesthesiology. 2000;92:1454–1466. [DOI] [PubMed] [Google Scholar]
- 38.Silber JH, Rosenbaum PR, Zhang X, et al. Influence of patient and hospital characteristics on anesthesia time in Medicare patients undergoing general and orthopedic surgery. Anesthesiology. 2007;106:356–364. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.