Abstract
Purpose of Review
Ulnar-sided wrist pain is a challenging diagnostic workup. A thorough and complete physical examination followed by appropriate radiographic studies can help the clinician diagnose and treat these conditions.
Recent Findings
Recent research has been focused on diagnostic modalities such as arthroscopy and high-resolution MRI.
Summary
Ulnar-sided wrist pain is a challenging clinical workup that must be approached systematically with the aid of adjunctive diagnostic modalities.
Introduction
Ulnar-sided wrist pain is challenging for the most experienced upper extremity providers. Often referred to as the “black box” of the wrist, ulnar wrist pain incorporates a multitude of pain generators and diagnoses from both traumatic and degenerative etiologies. The treating physician must have a comprehensive knowledge of the intricate anatomy and know how to interpret an appropriate history, to perform a reliable physical examination, and to utilize diagnostic imaging.
Anatomy
Bones and Joints
The distal ulna is composed of the ulnar head and ulnar styloid. The ulnar styloid is a projection of the distal ulna which functions as an attachment for several structures including the extensor carpi ulnaris (ECU) subsheath and superficial attachments of the triangular fibrocartilage complex (TFCC) and ulnocarpal ligaments [1]. The fovea is a vascularized, non-cartilaginous area at the base of the styloid that anchors the radioulnar and ulnocarpal ligaments [1]. The distal ulna articulates with the TFCC at the ulnar aspect of the wrist and the distal radius at the distal radioulnar joint (DRUJ). The curvature of radius of the sigmoid notch of the radius is larger than the corresponding ulnar head which allows for the degree of motion. The three motions that occur at the DRUJ are rotation about the forearm axis, dorsal-palmar translation, and proximal-distal translation. Variations in the bony morphology of the DRUJ include the following: flat face, ski slope, “C” type, and “S” type, and these shapes significantly influence the stability of this articulation [1].
The relationship of the radius, ulna, and carpus allows for balanced, controlled motion in several planes. The lunate articulates with the scaphoid and triquetrum and serves as the keystone of the carpal arch. A type 2 lunate is a normal variation of the bony morphology in which there is a narrow facet at the distal medial aspect that articulates with the hamate that may mitigate some instability associated with scapholunate tears [2]. This variant should be kept in mind when reviewing imaging and assessing for bony pathologies. The triquetrum articulates with the hamate, the pisiform, and the TFCC. The triquetrohamate joint is helicoidal, allows rotation and minimal translation, and is important in midcarpal motion [2]. The hamate articulates with the lunate and triquetrum as described above as well as the fourth and fifth metacarpals distally. The hamate contains a hook which projects volarly and functions as a pulley for the flexors of the small and ring fingers [1]. The pisiform is a sesamoid of the flexor carpi ulnaris (FCU) tendon and forms the pisotriquetral joint, a synovial joint [2]. The abductor digiti quinti and transverse carpal ligament also attach to the pisiform.
Ligaments, Tendons, and the TFCC
There is an extensive network of intrinsic and extrinsic ligaments of the ulnar aspect of the wrist. Ulnar intrinsic ligaments include the capitohamate, the lunotriquetral, and the triquetrohamate ligaments. The capitohamate ligament contains a dorsal, volar, and deep component. The lunotriquetral (LT) ligament is comprised of a dorsal component, a restraint to rotation; a volar component, the strongest and thickest part; and a proximal weak fibrocartilaginous component [2, 3]. The extrinsic ligaments of the ulnar wrist include the ulnotriquetral and ulnolunate ligaments. They function as stabilizers between the distal ulna and carpus and blend with the volar margin of the TFCC [2, 3]. The volar and dorsal radioulnar ligaments help stabilize the DRUJ and merge to form a triangle that surrounds the articular disk at the medial distal ulna. Stability is afforded to the DRUJ by the deep foveal TFCC as well as the interosseous membrane, extensor retinaculum, ECU subsheath, bony morphology of the sigmoid notch, and dynamic stabilization by the ECU tendon itself [1].
The FCU and ECU are the major tendons on the ulnar side of the wrist. The ECU runs in the sixth dorsal compartment of the wrist in the ulnar groove covered by an annular ligament at the distal ulna. It inserts on the 5th metacarpal distally and functions as a wrist extensor with the hand supinated and an ulnar deviator with the hand in pronation [4•]. This tendon displaces dorsally with the hand in supination and wrist extended [2]. The FCU is located ulnar to the ulnar nerve and artery proximal to Guyon’s canal and inserts on the pisiform blending with the palmar carpal ligament.
Neurovascular Structures
The ulnar nerve and artery pass through Guyon’s canal which has varying borders depending on location. The structures that surround the canal include the volar carpal ligament, transverse carpal ligament, pisiform, pisohamate ligament, and abductor digiti minimi, and the hook of the hamate [2]. The ulnar nerve bifurcates into a deep and superficial branch in the middle zone of Guyon’s canal. Compression of the nerve in zone 1 (proximal) presents with a mixed motor and sensory clinical picture while compression in zone 2 only affects the motor function, and zone 3 only affects sensation. The superficial ulnar artery passes adjacent to the hook of the hamate which places it at risk in hook of hamate fractures [2].
Ulnar Wrist Pathology and Differential Diagnoses
Table 1 is a list of differential diagnoses that should be considered when evaluating patients with ulnar-sided wrist pain. These diagnoses are divided into 6 subcategories—osseous, ligamentous, tendinous, vascular, neurologic, and miscellaneous, similar to the organization described by Shin et al. [3]. This list is comprised from information in several resources [2, 3, 5, 6].
Table 1.
Differential diagnosis list of ulnar-sided wrist pain. This table provides a thorough list of differential diagnoses for patients presenting with ulnar-sided wrist pain. Each category and diagnosis must be considered when evaluating these patients
| Osseous | |
| Fractures: hamate (hook, body), pisiform, triquetrum (dorsal triquetral avulsion), lunate, base of 4th or 5th metacarpal, ulnar styloid, distal ulna, distal radius | |
| Fracture sequelae including nonunions and malunions | |
| Degenerative conditions: PT joint, midcarpal (triquetrohamate), 4th or 5th CMC, DRUJ | |
| Kienböck disease | |
| Incomplete coalition of LT joint | |
| Ulnar impingement vs impaction | |
| Hamatolunate impingement syndrome | |
| Ulnar styloid impaction syndrome | |
| Hamate Arthrosis Lunotriquetral ligament Tear (HALT) lesion | |
| Madelung’s deformity | |
| Ligamentous | |
| TFCC tear (peripheral vs foveal) | |
| Carpal, midcarpal, DRUJ instability | |
| Ligament tears: LT, CH, UL, TC, TH, UT split | |
| LT dissociation | |
| Tendinous | |
| ECU tendon subluxation, dislocation, tendinopathy, or rupture | |
| FCU tendinitis | |
| EDM tendinitis | |
| Vascular | |
| Hypothenar hammer syndrome | |
| Ulnar artery thrombosis | |
| Hemangioma | |
| Raynaud syndrome | |
| Thoracic outlet syndrome | |
| Peripheral vascular disease | |
| Cardiac emboli | |
| Neurologic | |
| C8 – T1 cervical radiculopathy | |
| Brachial plexopathy | |
| Thoracic outlet syndrome | |
| Cubital tunnel syndrome | |
| Guyon’s canal syndrome | |
| Dorsal sensory ulnar nerve neuritis | |
| CRPS | |
| Neuroma | |
| Miscellaneous | |
| Benign or malignant neoplasms | |
| Psychological conditions |
Clinical History
A thorough clinical history is paramount to narrowing the differential diagnosis with ulnar wrist pain. A history of recent or remote traumatic injury and the underlying mechanism may explain the underlying injury. Exacerbating factors may reproduce the injury mechanism and narrow the diagnosis. For example, patients may describe pain with ulnar deviation or extension and/or pain with loading through the ulnocarpal joint, such as pushing off a chair. Additional histories and patterns of injury that help identify a diagnosis have been previously described by Cohen-Tanugi [6••].
Physical Examination
It is important to have a systematic approach to the physical examination of the ulnar wrist so that the provider can duplicate this exam on every patient to minimize the margin of error. Most authors describe the ideal position of the examiner sitting across from the patient with elbow flexed and resting on the table in the “arm wrestling” position [3, 5, 6]. Observation is the first step of the examination. The appearance of the painful wrist should be compared to the contralateral side, particularly looking for new or old wounds, healed incisions, ecchymosis, swelling, erythema, skin and nail conditions, and differential digital perfusion. Visible abnormalities in the wrist may point to specific diagnoses as described by Cohen-Tanugi [6••]. Palmar sag of the carpus can be seen in LT tears—although this is more commonly seen in disruption of the DRUJ where the radius and carpus sags palmarly or the ulna appears relatively dorsally subluxated. A prominent ulnar head can be caused by chronic foveal TFCC injury and DRUJ instability. Swelling along the ulnar wrist may be from tenosynovitis, infection, or gout. Intrinsic hand muscle atrophy or clawing of fingers may be from ulnar nerve pathology.
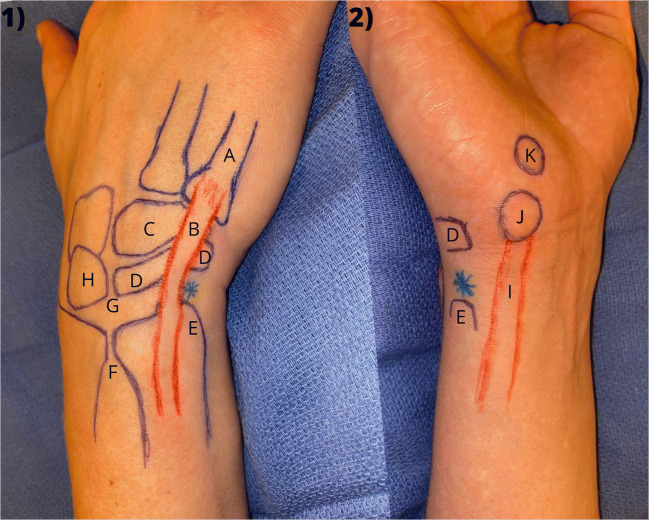
The pisiform is the palpable prominence distal to the ulnar wrist flexion wrist and may be painful in the setting of pisotriquetral (PT) arthritis. Pisiform fractures in the setting of trauma may elicit pain with palpation as well. The FCU is palpated moving proximal from the pisiform and becomes more prominent with abduction and extension of the digits. To palpate the hook of the hamate, the examiner places their thumb over the pisiform and aims the tip towards the ring finger. The hook of the hamate will be felt at under the pad of the thumb with deep palpation. This is vital to palpate while examining for hook of hamate fractures. The ulnar styloid is typically an easily seen and palpable dorsal ulnar structure, more easily palpable in neutral or pronation. Sliding the finger volar from the styloid, the fovea is encountered in the groove between the ECU and FCU. Palpable foveal pain can be elicited with injury to peripheral TFCC or a split tear of the ulnotriquetral ligaments. Distal to the fovea is the triquetrum. The dorsal triquetrum can be palpated just radial to the ECU tendon. The dorsal triquetrum is a force nucleus with several ligaments attaching to its dorsal surface. This is an important area to palpate to evaluate for dorsal triquetral avulsion fractures. The ECU tendon is most easily seen with the forearm in full supination with abducted fingers; supination is also the best position for eliciting instability. The ECU is in a straight line with the arm in pronation. The ECU inserts on the fifth metacarpal shaft which can be felt along the ulnar hand moving distal from the ECU. The lunotriquetral (LT) interval is palpated in the groove directly distal to the DRUJ between the 4th and 5th dorsal compartments with the wrist in 30 degrees of flexion [3, 6]. Figure 1 demonstrates clinical photographs with some pertinent surface anatomy markings.
Fig. 1.
Surface anatomy of wrist. The left side of the image (1) demonstrates the dorsal ulnar wrist and the right side of the image (2) is the direct ulnar view of the wrist. Important surface anatomy landmarks are labeled as the following: (A) 5th metacarpal shaft, (B) extensor carpi ulnar tendon, (C) hamate (dorsal aspect), (D) triquetrum, (E) ulnar styloid, (F) distal radioulnar joint (labeled directly proximal to), (G) lunotriquetral joint (labeled directly proximal to), (H) lunate, (I) flexor carpi ulnaris tendon, (J) pisiform, (K) hook of hamate, asterisk (*): fovea
While there are many important landmarks to remember while palpating surface anatomy, simple mnemonics may be useful for remembering important and common causes of pain in the ulnar wrist. The mnemonic RUPERT is useful when considering the important soft tissue structures of the ulnar wrist [7•]. R is for the sigmoid notch of the distal Radius, U is for the Ulnocarpal ligaments, P is for the Pronator quadratus muscle, E is for ECU tendon and subsheath, R is for Radioulnar membrane, and T represents the TFCC.
Active and passive range of motion (ROM) of the wrist should be assessed and compared to the contralateral side. Normal wrist ROM is 80 degrees of flexion, 70 degrees of extension, 90 degrees of supination, and 90 degrees of pronation [8]. It is important to isolate the wrist joint for pronation/supination by having the patient hold their shoulders adducted by keeping the elbows tucked at the sides. Assessing ROM includes looking for limited motion, pain, clicking, locking, and snapping. Grip strength testing is a way to examine active effort and strength of the patient. The ratio of injured to uninjured side grip strength correlates with Disabilities of the Arm, Shoulder, and Hand (DASH) scores and allows evaluation that does not rely on subjective questioning alone [9]. Though bilateral grip testing has been used, no single test or algorithm of grip testing has been found to accurately predict sincerity of this effort [10].
There is an array of provocative maneuvers and special tests that aid in differentiating ulnar wrist pathology. Table 2 lists all the following maneuvers and what pathology they are assessing. The ulnocarpal stress test involves placing axial pressure to the patient’s ulnarly deviated wrist with the elbow flexed and then passively moving the wrist through pronation and supination. If pain is produced, this is considered a positive test, which is 100% sensitive but not specific for ulnar-sided wrist pathology, including ulnar impaction diagnoses [11]. The hook of hamate pull test, described by Wright, has a patient flex the ring and small fingers against resistance in a wrist held in ulnar deviation [12]. Pain with this test may signify a hook of hamate fracture as these tendons are known to pass by the hook of the hamate as a pulley. The pisiform triquetral grind test signifies underlying arthritis. It is performed by the examiner gripping the pisiform between their index finger and thumb and stabilizing the dorsal wrist with their other hand; the pisiform is then shucked radial and ulnar [6••].
Table 2.
Provocative maneuvers. These are many of the provocative maneuvers used in assessment of ulnar-sided wrist pain. The tests are each listed along with what signifies a positive test, and what pathology is indicated with a positive test
| Test | Positive | Pathology represented |
|---|---|---|
| Ulnocarpal stress test | Pain | Ulnocarpal impaction, central TFCC tear |
| Press test | Pain | Ulnar-sided wrist pain, possible TFCC |
| Hook of hamate pull test | Pain | Hook of hamate fracture |
| Pisiform tracking test/PT grind test | Pain | PT pathology |
| LT ballottement test | Pain or laxity | LT tear |
| Regan shuck test | Pain or laxity | LT tear |
| Kleinman shear test | Pain | LT tear |
| DRUJ compression test | Pain | DRUJ arthritis |
| Piano key/DRUJ ballottement test | Pain or laxity | DRUJ instability |
| Synergy test |
Sharp pain Subluxation or dislocation of tendon |
ECU tendonitis ECU tendon instability |
| Ulnar fovea sign | Tenderness | TFCC pathology |
| Midcarpal shift test | Painful clunk | Midcarpal instability |
There are three tests to assess the lunotriquetral joint. The LT ballottement test has the examiner’s thumb on the ulnar medial aspect of the pisiform with radial pressure applied while stabilizing the rest of the wrist, which may lead to pain or laxity with LT tears [13]. This test has been found not specific because it also stresses other structures of this region. The Regan shuck test involves the triquetrum and pisiform grasped as a unit by the examiner’s index finger and thumb and shucking them dorsal to palmar. The Kleinman shear test has the examiner’s thumb over the pisiform and their other thumb over the dorsal lunate while stabilizing the forearm with interlaced hands; gradual pressure is then applied between the thumbs [13]. For this test to be effective, PT arthritis must be ruled out prior to performing as stress is also placed through that joint [6••].
Pain at the DRUJ may signify instability, arthritis, or a combination of the two. The DRUJ may be assessed with the DRUJ compression test or the piano key test. The DRUJ compression test involves gripping the distal radius and ulna 1–2 cm proximal to the ulnar head and compressing them together. This test results in pain when DRUJ arthritis is present. The piano key or DRUJ ballottement test reveals instability by shucking the distal ulna volarly and dorsally while stabilizing the radius, best performed in supination, neutral, and pronation [14].
ECU instability is commonly measured by employing the synergy test. This is done by having the patient fully supinate, abduct their thumb and long finger against resistance, which synergistically fires the ECU. This test is indicative of ECU tendonitis if it causes sharp pain and indicative of instability if it causes subluxation or dislocation of the ECU tendon [15]. The ECU tendon can also be assessed by having a patient simulate an ice cream scoop motion [6••].
There are many ways to evaluate the TFCC. The ulnar fovea sign is positive when tenderness is evoked with palpation to the fovea. This test is 95.2% sensitive and 86.5% specific for TFCC pathology [16]. The ulnocarpal stress test involves the examiner moving an ulnarly deviated wrist volar to dorsal while putting axial compression through the ulnar aspect of the wrist [3]. This may elicit pain with ulnar carpal impaction of the ulna and lunate or with central TFCC tears.
The midcarpal shift test involves the patient placing their hand pronated in 15 degrees of ulnar deviation with the examiner’s thumb at the distal aspect of the capitate and volar pressure applied while placing an axial load through the metacarpals. The test is positive if there is a painful clunk, indicating midcarpal instability [6••].
The last aspect of physical examination to be considered is diagnostic injection. Injections may be performed either within tendon sheaths, such as the ECU tendon sheath, or in specific joints to rule out or identify pathologies [3].
Radiographic Evaluation
Radiography
Standard posteroanterior (PA) and lateral radiographs should be obtained as a first step in all patients with ulnar-sided wrist pain. On PA views, Gilula’s lines and ulnar variance should be closely examined. A disruption in Gilula’s arc typically represents carpal subluxation or dislocation except in some rare instances with normal variants [17]. Ulnar variance is the relationship between the distal ulna and distal radius in terms of length. Positive ulnar variance occurs when the distal surface of the ulna exceeds the corresponding radial articular surface. Negative ulnar variance, sometimes associated with Kienbock’s disease, occurs when the distal ulna is more proximal than the corresponding articular surface of the distal radius [2].
The lateral should be evaluated for signs of carpal instability using the scapholunate, capitolunate, and lunotriquetral angles [3]. There are other views that help examine specific areas of the wrist including oblique 30-degree pronation view to evaluate the dorsal ulnar wrist and the oblique 30-degree supination view which demonstrates the volar ulnar wrist [3]. An ulnar deviation view can show LT instability. A pronated grip view can demonstrate ulnocarpal abutment. The carpal tunnel view is a tangential X-ray performed with the wrist 35 degrees extended; it is useful for evaluating the hook of the hamate and the PT joint.
Fluoroscopic or live X-ray imaging can help with detection of abnormal motion and kinematics of carpal bones and dynamic instability. It can help identify midcarpal instability by visualizing the “catch up” clunk of the triquetrum as it moves abnormally in relation to the hamate [3].
Computed tomography (CT) allows the best evaluation of the carpus. Occult fractures, such as of the pisiform, hamate, and ulnar styloid, are better appreciated on CT. CT is also a useful way to assess for DRUJ instability by obtaining bilateral wrist CTs in neutral, pronation, and supination [18]. “Dynamic” or “4D” CT has also been described to show the 3D interaction of the bony structures of the wrist [19]. CT arthrography has been used to help in determining the location of TFCC tears [20].
MRI is the new standard not only to evaluate soft tissue structures of the wrist but to rule out occult fractures. Accurate MRI of the wrist has lagged behind larger joint evaluation given the need for thin slices, high resolution, and a higher degree of signal-to-noise ratios [5]. Three-Tesla (T) MRI has demonstrated higher quality images with better sensitivities in diagnosing ulnar-sided wrist pathologies than 1.5-T MRI [21, 22]. There are still inconsistent sensitivities reported depending on the experience of the radiologist [3]. MRI of the wrist also allows for evaluation of the vascular status of the lunate as well as cystic and signal changes in the proximal ulna and lunate as seen in ulnocarpal impaction [23].
MRI arthrography involves injecting contrast either intravenously (indirect arthrography) or into joints (direct arthrography) to better evaluate the detailed anatomy of the ulnar wrist. Injecting contrast into the TFCC when a TFCC tear is present may result in contrast being seen in the DRUJ [24]. This is helpful because the presence of contrast represents an abnormal communication, rather than synovitis or mechanical irritation causing fluid accumulation in the DRUJ [5].
Radionuclide imaging, or triple bone scan, has occasional use for identifying for inflammation of the wrist. It can help identify occult fractures, osteonecrosis, and osteomyelitis [3]. Although this form of imaging is a low-cost screening tool, it is not often used because of the inability to identify a specific diagnosis or pinpoint an exact location of pathology.
Ultrasound is a field of growing interest in evaluation of ulnar-sided wrist pain. The positive aspects include no radiation exposure, portability, and low cost. The main drawbacks are that it is extremely user-dependent and it is not helpful for bony pathologies. It is particularly useful, however, for tendinous pathologies such as ECU subsheath tears that lead to subluxation. Ultrasound is also very helpful with preoperative planning of tendon ruptures to identify retracted ends of the tendons [5, 25, 26].
Recent Developments
There have been recent advances in the diagnosis of ulnar-sided wrist pain, particularly in relation to diagnostic imaging and arthroscopy. Dry wrist arthroscopy (DWA) has been growing in popularity as a modality to evaluate and treat ulnar-sided pathologies. DWA avoids soft tissue distension which may mask ligamentous tears and cause increased pain post-operatively [27]. The major drawbacks of DWA are that a thermal probe cannot be used and aggressive debridement is more difficult because of the risk of thermal injury as well as blockage of the shaver without continuous saline flow [27]. Smaller arthroscopes are also being introduced that may allow in-office examination of the wrist to avoid the use of anesthesia [28•]. MRI evaluation of the wrist is also improving with the use of 7-T MRIs providing higher quality images of the tendons, ligaments, and nerves of the wrist over 3T [29].
Conclusion
Ulnar-sided wrist pain is a common complaint that is a persistent problem for many patients. A detailed history taking, knowledge of the anatomy, and systematic physical examination are essential to accurate diagnosis. Narrowing the broad differential of ulnar-sided wrist pain and implementation of cost-effective diagnostic imaging will minimize treatment delays and maximize successful patient outcomes.
Compliance with Ethical Standards
Conflict of Interest
Genoveffa Morway declares that she has no conflicts of interest.
Andrew Miller declares that he has no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Ulnar-Sided Wrist Pain
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Geissler WB, Slade JF. Green’s operative hand surgery. Green’s Operative Hand Surgery. 2011.
- 2.Vezeridis PS, Yoshioka H, Han R, Blazar P. Ulnar-sided wrist pain. Part I: Anatomy and physical examination. Skelet Radiol. 2010;39:733–45. [DOI] [PMC free article] [PubMed]
- 3.Shin AY, Deitch MA, Sachar K, Boyer MI. Ulnar-sided wrist pain diagnosis and treatment. 2005;86. [PubMed]
- 4.• Kleinman WB. Physical examination of the wrist. United States: ASSH Hand-e; 2020. This is a video review by Dr. Kleinman on a thorough examination of the wrist. He reviewed the surface anatomy as well as specific movements of the hand needed to examine certain tendons and ligaments.
- 5.Watanabe A, Souza F, Vezeridis PS, Blazar P, Yoshioka H. Ulnar-sided wrist pain. II. Clinical imaging and treatment. Skelet Radiol. 2010;39:837–57. [DOI] [PMC free article] [PubMed]
- 6.•• Cohen-Tanugi S, Gaston RG. Examination of ulnar-sided wrist pain, vol. 37, Hand Clinics. W.B. Saunders; 2021. p. 467–75. This is an overview of the physical examination of the ulnar side of the wrist with an emphasis on palpatory examination. There were many clinical photographs demonstrating surface anatomy as well as various pathologies. There was also a thorough review of differential and pertinent physical exam findings for various pathologies. [DOI] [PubMed]
- 7.• Brogan DM, Berger RA, Kakar S. Ulnar-sided wrist pain: a critical analysis review. JBJS Reviews. Journal of Bone and Joint Surgery Inc. 2019;7. This is a critical analysis review on ulnar-sided wrist pain that covers an array of information from assessment and diagnosis to treatment modalities. This is a thorough review of special tests and imaging. [DOI] [PubMed]
- 8.Hoppenfeld S. Physical examination of the spine and extremities. Norwalk, CT: Appleton & Lange; 1976. [Google Scholar]
- 9.Beumer A, Lindau TR. Grip strength ratio: a grip strength measurement that correlates well with DASH score in different hand/wrist conditions. BMC Musculoskelet Disord. 2014;15(1). [DOI] [PMC free article] [PubMed]
- 10.Nanta P, Bhuanantanondh P. Identifying sincerity of effort by grip strength ratio of three wrist positions in individuals with upper extremity musculoskeletal disorders. J Occup Health. 2021;63(1):e12295. doi: 10.1002/1348-9585.12295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nakamura R, Horii E, Imaeda T, Nakao E, Kato H, Watanabe K. The ulnocarpal stress test in the diagnosis of ulnar-sided wrist pain. J Hand Surg Eur Vol. 1997;22(6):719–723. doi: 10.1016/S0266-7681(97)80432-9. [DOI] [PubMed] [Google Scholar]
- 12.Wright TW, Moser MW, Sahajpal DT. Hook of hamate pull test. J Hand Surg. 2010;35(11):1887–1889. doi: 10.1016/j.jhsa.2010.08.024. [DOI] [PubMed] [Google Scholar]
- 13.Kleinman WB. Physical examination of the wrist: useful provocative maneuvers. J Hand Surg. 2015;40:1486–500. [DOI] [PubMed]
- 14.Sachar K. Ulnar-sided wrist pain: evaluation and treatment of triangular fibrocartilage complex tears, ulnocarpal impaction syndrome, and lunotriquetral ligament tears. J Hand Surg. 2012;37(7):1489–1500. doi: 10.1016/j.jhsa.2012.04.036. [DOI] [PubMed] [Google Scholar]
- 15.Ruland RT, Hogan CJ. The ECU synergy test: an aid to diagnose ECU tendonitis. J Hand Surg. 2008;33(10):1777–1782. doi: 10.1016/j.jhsa.2008.08.018. [DOI] [PubMed] [Google Scholar]
- 16.Tay SC, Tomita K, Berger RA. The “ulnar fovea sign” for defining ulnar wrist pain: an analysis of sensitivity and specificity. J Hand Surg. 2007;32(4):438–444. doi: 10.1016/j.jhsa.2007.01.022. [DOI] [PubMed] [Google Scholar]
- 17.Loredo RA, Sorge DG, Garcia G. Radiographic evaluation of the wrist: a vanishing art. Semin Roentgenol. 2005;40(3):248–289. doi: 10.1053/j.ro.2005.01.014. [DOI] [PubMed] [Google Scholar]
- 18.Wechsler RJ, Wehbe MA, Rifkin MD, Edeiken J, Branch HM. Computed tomography diagnosis of distal radioulnar subluxation. Skelet Radiol. 1987;16(1):1–5. doi: 10.1007/BF00349919. [DOI] [PubMed] [Google Scholar]
- 19.Leng S, Zhao K, Qu M, An KN, Berger R, CH MC. Dynamic CT technique for assessment of wrist joint instabilities. Med Phys. 2011;38:S50. doi: 10.1118/1.3577759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moser T, Dosch JC, Moussaoui A, Buy X, Gangi A, Dietemann JL. Multidetector CT arthrography of the wrist joint: how to do it. Radiographics. 2008;28(3):787–800. doi: 10.1148/rg.283075087. [DOI] [PubMed] [Google Scholar]
- 21.Stehling C, Langer M, Bachmann R, Kraemer S, Kooijman H, Heindel W, et al. Three-tesla magnetic resonance imaging of the wrist: diagnostic performance compared to 1.5-T. J Comput Assist Tomogr. 2009;33(6):934–939. doi: 10.1097/RCT.0b013e31819bc03f. [DOI] [PubMed] [Google Scholar]
- 22.Anderson ML, Skinner JA, Felmlee JP, Berger RA, Amrami KK. Diagnostic comparison of 1.5 Tesla and 3.0 Tesla preoperative MRI of the wrist in patients with ulnar-sided wrist pain. J Hand Surg. 2008;33(7):1153–1159. doi: 10.1016/j.jhsa.2008.02.028. [DOI] [PubMed] [Google Scholar]
- 23.Cerezal L, del Piñal F, Abascal F, García-Valtuille R, Pereda T, Canga A. Imaging findings in ulnar-sided wrist impaction syndromes. Radiographics. 2002;22(1):105–121. doi: 10.1148/radiographics.22.1.g02ja01105. [DOI] [PubMed] [Google Scholar]
- 24.Steinbach LS, Palmer WE, Schweitzer ME. Special focus session: MR arthrography. Radiographics. 2002 22:1223–1246 [DOI] [PubMed]
- 25.Bianchi S, Martinoli C, Abdelwahab IF. High-frequency ultrasound examination of the wrist and hand. Skelet Radiol. 1999;28:121–9. [DOI] [PubMed]
- 26.Fornage BD, Rifkin MD. Ultrasound examination of the hand and foot. Radiol Clin North Am. 1988;26:109–29. [PubMed]
- 27.Burnier M, Herzberg G, Luchetti R, del Piñal F, Kakar S. Dry wrist arthroscopy for ulnar-sided wrist disorders. J Hand Surg. W.B. Saunders. 2021;46:133–41. [DOI] [PubMed]
- 28.• Viswanath A, Talwalkar S. Recent advances and future trends in wrist arthroscopy. J Arthrosc Surg Sports Med. 2020;1. This is a review article of recent developments in wrist arthroscopy. The increasing popularity of dry wrist arthroscopy and minimally invasive wrist arthroscopy, which can potentially be done in the office, was discussed in this review article.
- 29.Götestrand S, Björkman A, Björkman-Burtscher IM, Kristiansson I, Aksyuk E, Szaro P, et al. Visualization of wrist anatomy—a comparison between 7T and 3T MRI. Eur Radiol. 2022;32(2):1362–1370. doi: 10.1007/s00330-021-08165-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lester B, Halbrecht J, Levy IM, Gaudinez R. “Press test” for office diagnosis of triangular fibrocartilage complex tears of the wrist. Ann Plast Surg. 1995;35(1):41–45. doi: 10.1097/00000637-199507000-00009. [DOI] [PubMed] [Google Scholar]
- 31.Chung KC, Zimmerman NB, Travis MT. Wrist arthrography versus arthroscopy: a comparative study of 150 cases. J Hand Surg. 1996;21(4):591–594. doi: 10.1016/S0363-5023(96)80008-6. [DOI] [PubMed] [Google Scholar]