Abstract
Background
This systematic review used the Copenhagen (CBI) and the Maslach (MBI) Burnout Inventories and its scales to assess and compare studies that involved students and workers in all medical specialties.
Material/Methods
PubMed, ScienceDirect, Scopus, Wiley Library, and Web of Science databases were searched using keywords and Medical Subject Headings. Identified studies were in English, published between 2008 and 2022, measured the burnout of healthcare workers and students by using CBI and MBI, and observed adverse patient outcomes.
Results
A total of 38 studies were included in the current review. All included studies assessed and evaluated subjects and participants by observing clinical measures, personal and demographic data, countries where the study was conducted, and study type used. Fifty percent of CBI papers were conducted in Saudi Arabia and other Arab countries, whereas the majority of MBI papers (10) were conducted in Europe, followed by 9 studies conducted in Saudi Arabia and other Arab countries and 6 studies conducted in the USA and Canada. The overall percentage of burnout in CBI studies (53%) was higher than that in MBI studies (35%). Also, the types and domains in CBI were marginally higher than those in MBI.
Conclusions
Studies that used CBI scales recorded higher burnout compared with studies that used MBI. Females, higher education levels, and marriage status of the tested subjects showed higher CBI and MBI scale scores in comparison to their counterparts. Higher significant differences percentages in burnout types and genders were recorded in CBI than in MBI.
Keywords: Burnout, Professional; Fibrinogen Copenhagen II
Background
Burnout is an extended reaction to chronic emotional and interpersonal stressors on the job, and is characterized by the 3 dimensions of exhaustion, cynicism, and inefficacy [1]. It is a term used to describe a clinical syndrome that involves severe stress, dissatisfaction, and feeling of being overworked [2–4]. According to the World Health Organization, occupational burnout is a chronic psychological syndrome caused by exposure to chronic emotional and interpersonal stress caused by work or the workplace [5].
The term burnout was introduced by psychologist Herbert Freudenberger in 1974 in an article titled “Staff Burnout” in which he discussed job dissatisfaction caused by professional stress [6]. This syndrome has severe adverse consequences, including substance abuse, disruptive behavior, lack of energy, low job satisfaction, absenteeism, feelings of worthlessness, impatience, divorce, depression, suicidal thinking, and even suicide [7].
The progression of burnout is described as follows. The first sign of burnout is mental and physical exhaustion, with the individual feeling overwhelmed by the demands of the job and detached from various aspects of the job. Detachment can lead to the dehumanization of patients because providers stop doing their best and are content to do the bare minimum. As burnout progresses, the individual develops a diminished sense of personal fulfillment and loss of self-confidence [8].
Several assessment tools, scales, and questionnaires are available for measuring burnout, including the Copenhagen Burnout Inventory (CBI), Maslach Burnout Inventory (MBI), Burnout Clinical Subtype Questionnaire, and Shirom-Melamed Burnout Measure (SMBM), and Oldenburg Burnout Inventory [9]. The CBI uses 3 dimensions to measure personal burnout, work-related burnout, and client-related burnout, for use in different domains [10]. The MBI uses 3 scales assessing emotional exhaustion, depersonalization, and personal achievement [2,11]. Among these tools, CBI and MBI are the most widely used tools in the medical literature to identify and measure burnout. Those scales assess burnout among healthcare employees from the same as well as different fields, such as nurses, doctors, or medical students, and none of them includes healthcare workers from various disciplines and at different education levels [9–11].
The concept of burnout was introduced into the social science literature in the mid-1970s by Freudenberger (1974) and Maslach (1976) [10]. Many assessment tools, scales, and questionnaires for measuring burnout are available [8]. The first and most widely used tool in the medical literature to assess and measure burnout is the MBI [9], which has received criticism from academics for a variety of reasons, including an unclear connection between the tool and the concept of burnout. Afterward, Kristensen et al developed the CBI, which is frequently used to measure burnout in personnel working in complex medical settings [12]. From a scientific perspective, the CBI is free in the public domain and is open access, unlike the MBI, which is considered a general survey copyrighted/distributed by a commercial publisher. The CBI examines the work- and client-related aspects of burnout in addition to the personal aspect. This function gives CBI an advantage over the MBI, which primarily focuses on the emotional aspect of exhaustion [13].
Some reviews on burnout have been published. The majority focused on studies that used the CBI scale to assess burnout and its causes and negative impacts. Other reviews included studies that utilized the MBI scale and thoroughly examined the prevalence of burnout among healthcare professionals from different specialties to support the personal and professional development of healthcare workers [14–23]. A systematic review that includes studies that utilized the CBI and MBI scales has not been conducted yet. Thus, the aim of this systematic review was to assess, summarize, and compare studies that involved all medical students as well as medical field workers and used the Copenhagen (CBI) and the Maslach (MBI) Burnout Inventories.
Material and Methods
The current systematic review was constructed and designed in accordance with the Preferred Reporting Items for Systematic Review and Meta-analysis [14,17,24]. We created the core question with inclusion and exclusion criteria applying the PICO context proposed by the Joanna Brigg Institute for assessing qualitative papers [25]. All 8 questions were asked during assessment of the included studies. However, some studies focused on students and medical health workers, but the comparisons were between males and females, the education level, specialties, and outcomes were interpreted.
Research Protocols and Inclusion and Exclusion Criteria
We conducted the search by using state, context, and population frameworks to review published articles that measured burnout by using the CBI and MBI. Questions were “What is the meaning of burnout in MBI and its types (personal, work-related, and patient-related burnouts), and what is the mean burnout of CBI and its types (emotional exhaustion, depersonalization, and personal achievement)?” and “Is the overall mean of both scales with their types similar or different among genders and populations?” Hence, only studies that used the MBI and CBI, directly evaluated burnout among healthcare workers and students from different countries and were published in English were included. Studies that measured burnout by using other indices or inventory other than MBI and CBI and published in languages other than English were excluded.
Search Strategy
The electronic databases of PubMed, ScienceDirect, Scopus, Wiley Library, and Web of Science were searched for relevant published papers from April 2008 to September 2022. The search terms used were “Maslach Burnout Inventory”, “Copenhagen Burnout Inventory”, “burnout”, “scale”, “indices”, and “medical health specialty”. Keywords were used independently or in combination by using the Boolean operators “AND,” “OR,” and “NOT” to search for the term “burnout, MBI, and CBI” independently. The gray literature was searched using Google Scholar.
Study Selection
Two reviewers (M.M.AL. and M.A.) individually evaluated papers for eligibility based on inclusion criteria. After the elimination of repeat articles, the titles and abstracts of the remaining articles were analyzed for relevant studies. A third reviewer (F.A.S.) assessed the validity and duplications of the studies. Papers that did not assess the levels of CBI and MBI among different health practitioners, systemic reviews, and case reports were excluded. Published articles that did not indicate the number of subjects and participants or whose samples had been partly estimated in other studies were also ignored. A paper was deemed relevant when the researchers agreed that it was related to the study questions. The full text of potentially relevant papers was obtained and reviewed. The references of selected papers were examined for extra studies that fulfilled the inclusion criteria. In case of a disagreement regarding the inclusion of an article, a third reviewer (F.A.S.) was consulted.
Data Extraction and Analysis
Two authors (M.M.A. and M.A.) independently extracted relevant data from each paper by using customized tables in Microsoft Excel (Microsoft Corp., Redwood, CA, USA). Any disagreement was resolved through discussion with a third author (F.A.S.). Details regarding the author(s) names, year of publication, country, study design, sample size, response rate, specialty tested, mean (%) of overall burnout and types of CBI and MBI scales, and important findings were documented.
Quality of Involved Papers
The quality of included papers was assessed in accordance with the Joanna Briggs Institute’s critical appraisal tool for cross-sectional studies [25]. The critical appraisal was performed independently by 2 authors (M.M.A. and M.A.). Any disagreement was resolved through discussion until consensus was reached with a third author (F.A.S.). The exterior validity of articles was evaluated by stating 3 criteria: characteristics of the study samples and participants, correctness of outcome processes, and statistical methods utilized.
Results
Study Selection
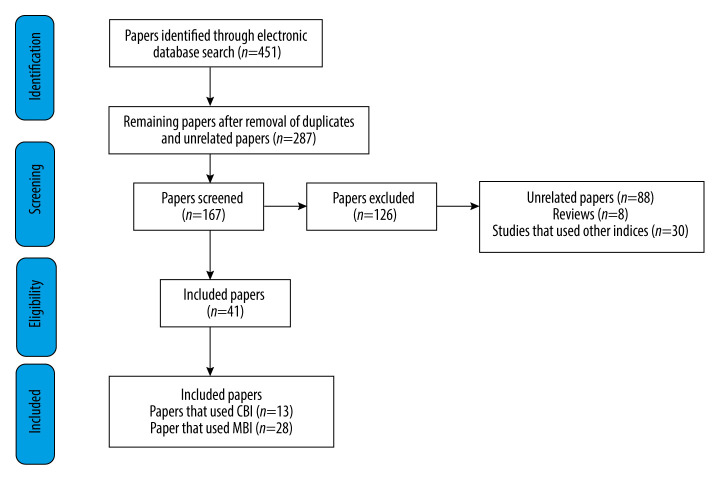
The search strategy yielded 451 results. A total of 287 papers were excluded because they were duplicates or not related to this review. Remaining articles were screened based on title and abstract. A total of 126 papers were excluded because they were unrelated studies (88), reviews (8), or studies that used other inventories or indices (30). The full text of 41 papers that met all inclusion criteria were included in this review and were assessed using predefined eligibility criteria. A total of 13 and 28 papers used CBI and MBI, respectively. Figure 1 depicts the selection process of papers involved in this review.
Figure 1.
Flowchart of the study selection process in accordance with the Preferred Reporting Items for Systematic Review and Meta-analysis [12,15,22].
Quality of the Selected Papers
The risk of bias assessment revealed that most of the 41 papers suffered from methodological limitations, resulting in an overall rating of medium to high risk of bias. A high percentage of the published papers showed attrition bias with lack of responses. Information on how the response rate was managed was limited. The papers did not use any objective measure to assess burnout by the CBI or MBI. In addition, some studies using the MBI did not mention the percentages and means of MBI types. Assessment of the quality of the papers by checklist article was done according to Chuang et al [22], and it is displayed in Table 1. There was an extremely high level of agreement in the calculations of the papers assessed by the 2 reviewers and the intraclass correlation coefficient for the reliability of all data.
Table 1.
Quality of papers using Copenhagen (n=13) and Maslach Burnout Inventories (n=28).
| Quality of papers used Copenhagen Burnout Inventories (n=13) | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Quality criteria | Stein & Sibanda [26] | Chin et al [27] | Dewitt et al [28] | Kulkarni et al [29] | Aboalshamat et al [30] | Atlam [31] | Fernando & Samaranayake [32] | Aljuhayman et al [33] | Mahfouz et al [34] | Alsulimani et al [35] | Chalikkandy et al [36] | Antoniadou [37] | Fiabane et al [38] | Total/percentage |
| Is hypothesis/aim/objective of study clearly described? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 13/100% |
| Are main outcomes to be measured clearly described? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 12/92% |
| Is the design of study described? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 13/100% |
| Is the setting of study described? | 1 | 1 | 1 | NA | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 12/92% |
| Is the source of the subjects studied stated? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 13/100% |
| Is the distribution of study population by age and sex described? | 0 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 9/69% |
| Is the sample size stated? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 13/100% |
| Is participation/follow up rate stated? | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 7/54% |
| Are non-participants/subjects lost to follow up described? | NA | 1 | NA | 0 | 0 | 0 | NA | 0 | 0 | NA | 0 | 0 | 0 | 1/8% |
| Are the main findings of the study clearly described? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 11/85% |
| Are the statistical methods described? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 13/100% |
| Have actual probability values been reported? | NA | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 6/46% |
| Are conclusions stated? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 13/100% |
| Were subjects asked participate in study representative of entire population from which they were recruited? | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 1 | 10/77% |
| Were those subjects who prepared to participate representative of entire population from which they were recruited? | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 10/77% |
| Was participation/follow up rate >80%? | 1 | 0 | NA | NA | NA | NA | 1 | 1 | 1 | NA | NA | 0 | 0 | 4/31% |
| Were the main outcome measures used accurate (valid and reliable)? | 1 | 1 | 1 | 1 | 0 | 0 | 0 | NA | 0 | 1 | 1 | 1 | 1 | 8/62% |
| Was there adequate adjustment for confounding in analyses from which main findings drawn? | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 10/77% |
| Was sample size justified? | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 5/38% |
| Analysis adjusts for length of follow up? (cohort only) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0/100% |
| Quality of papers used Maslach Burnout Inventories (n=28) | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Quality criteria | Soler et al [39] | Zantinge et al [40] | Prins et al [41] | Blanchard et al [42] | Galan et al [43] | Ruitenburg et al [45] | Siu et al [45] | Cecil et al [46] | Takayesu et al [47] | Kushnir et al [48] | Yuguero Torres et al [49] | Garrouste-Orgeas et al [50] | Albalawi et al [51] | Aldrees et al [52] | Total/percentage |
| Is hypothesis/aim/objective of study clearly described? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 14/100% |
| Are main outcomes to be measured clearly described? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 14/100% |
| Is the design of study described? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 14/100% |
| Is the setting of study described? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 14/100% |
| Is the source of subjects studied stated? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 14/100% |
| Is the distribution of the study population by age and sex described? | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 11/79% |
| Is the sample size stated? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 14/100% |
| Is the participation/follow up rate stated? | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 12/86% |
| Are non-participants/subjects lost to follow up described? | NO | 0 | 0 | 0 | NA | NA | NA | 0 | 0 | 0 | 1 | 0 | 0 | NA | 1/7% |
| Are the main findings of study clearly described? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 14/100% |
| Are the statistical methods described? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 14/100% |
| Have actual probability values been reported? | 0 | 0 | 0 | NA | 1 | 1 | 1 | 0 | 0 | NA | 0 | NA | 1 | 1 | 5/36% |
| Are any conclusions stated? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 14/100% |
| Were subjects asked to participate in study representative of entire population from which they were recruited? | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 12/86% |
| Were those subjects who were prepared to participate representative of entire population from which they were recruited? | 1 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 8/57% |
| Was participation/follow up rate >80%? | 0 | 1 | 0 | 0 | NA | 0 | 0 | NA | 1 | 1 | 0 | 1 | 1 | 0 | 5/36% |
| Were the main outcome measures used accurate (valid and reliable)? | 1 | 1 | 1 | 0 | 1 | 1 | 1 | NA | 1 | 1 | 1 | 1 | 0 | 1 | 11/79% |
| Was there adequate adjustment for confounding in analyses from which main findings were drawn? | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 9/64% |
| Was sample size justified? | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 8/57% |
| Analysis adjusts for length of follow up? (cohort only) | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 1 | 5/36% |
| Quality of papers used Maslach Burnout Inventories (n=28) | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Quality criteria | Kwah et al [53] | Kealy et al [54] | Elmore et al [55] | Fares et al [56] | Popa-Velea et al [57] | Almalki et al [58] | Baer et al [59] | Shakir et al [60] | Van Vendeloo et al [61] | Jamjoom et al [62] | Al-Alawi et al [63] | Asali et al [64] | Alqurashi et al [65] | AlShahrani, et al [66] | Total/Percentage |
| Is hypothesis/aim/objective of study clearly described? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 14/100% |
| Are main outcomes to be measured clearly described? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 14/100% |
| Is the design of the study described? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 14/100% |
| Is the setting of study described? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 14/100% |
| Is the source of subjects studied stated? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 14/100% |
| Is distribution of study population by age and sex described? | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 11/79% |
| Is the sample size stated? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 14/100% |
| Is participation/follow up rate stated? | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 12/86% |
| Are non-participants/subjects lost to follow up described? | NO | 0 | 0 | 0 | NA | NA | NA | 0 | 0 | 0 | 1 | 0 | 0 | NA | 1/7% |
| Are the main findings of the study clearly described? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 14/100% |
| Are the statistical methods described? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 14/100% |
| Have actual probability values been reported? | 0 | 0 | 0 | NA | 1 | 1 | 1 | 0 | 0 | NA | 0 | NA | 1 | 1 | 5/36% |
| Are any conclusions stated? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 14/100% |
| Were subjects asked to participate in study representative of entire population from which they were recruited? | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 12/86% |
| Were those subjects who were prepared to participate representative of entire population from which they were recruited? | 1 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 8/57% |
| Was participation/follow up rate >80%? | 1 | 0 | 1 | NA | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 8/57% |
| Were the main outcome measures used accurate (valid and reliable)? | 1 | 1 | 1 | 0 | 1 | 1 | 1 | NA | 1 | 1 | 1 | 1 | 0 | 1 | 11/79% |
| Was there adequate adjustment for confounding in analyses from which main findings were drawn? | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 9/64% |
| Was sample size justified? | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 8/54% |
| Analysis adjusts for length of follow up? (cohort only) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0/00% |
1 classified as (Yes), 0 classified as (No), Unable to determine classified as (NA).
Study Characteristics
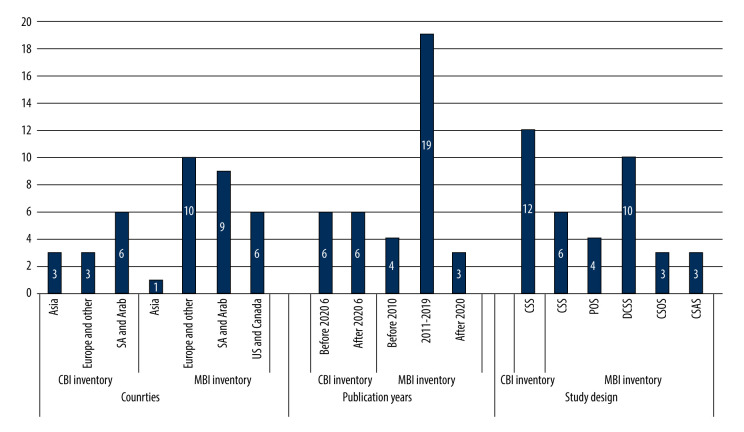
Thirteen studies used CBI: 6 were conducted in Saudi Arabia and other Arab countries, 3 studies were conducted in Asia, and others were from Europe and other countries. Table 2 summarizes the characteristics of the selected CBI papers [26–38]. Twenty-eight studies used MBI: 12 were from Europe, 9 were from Saudi Arabia and other Arab countries, 6 were from the USA and Canada, and 1 was from Asia. Table 3 summarizes the characteristics of selected MBI papers [39–66].
Table 2.
Characteristics of studies conducted using Copenhagen Burnout Inventories and its types for burnout measurement (n=13).
| Research/study year/country | Title | Study design/ sample size/ RR |
Specialty tested | Overall mean, %/Burnout type: 1. Personal burnout 2. Work-related burnout 3. Patient-related burnout |
Important finding and outcome |
|---|---|---|---|---|---|
| Stein and Sibanda/2016/South Africa [26] | Burnout among paramedic students at a university in Johannesburg, South Africa | CSS/ N=93/ RR=85% |
Paramedic Students | 31% | SD ↔ Burnout types NSD ↔ Level of study |
| Chin et al/2016/Malaysia [27] | Prevalence of Burnout among Universiti Sains Malaysia medical students | CSS/ N=452/ RR=56% |
Medical Students | 67.9% Personal (81.6%), Work-related (73.7%) Patient-related (68.6%) |
SD ↔ Burnout types NSD ↔ Gender, year of study |
| Dewitt et al/2016/Australia [28] | Medical student satisfaction, coping and burnout in direct-entry versus graduate-entry programmes | CSS/ N=688/ RR=NM |
Medical Students | 51% | NM |
| Kulkarniet al/2016/India [29] | Stress and professional burnout among newly graduated dentists | CSS/ N=121/ RR=NM |
Graduated Dentists | 39.3% | SD ↔ Gender ↑ Females NSD ↔ Burnout types |
| Aboalshamat et al/2017/Saudi Arabia [30] | The relationship between burnout and perfectionism in medical and dental students in Saudi Arabia | CSS N=645/ R=NM |
Medical and Dental Students | 56.7% Minimal 32.1%/Significant 67.9% Personal (42.3%), Work-related (67.9%) Patient-related (NM) |
SD ↔ Family income, Clinical year ↑ → ↑ burnout NSD ↔ Gender, college type |
| Atlam/2018/Egypt [31] | Burnout syndrome: Determinants and Predictors among medical students of Tanta University, Egypt | CSS/ N=672/ RR=NM |
Medical Students | 79.9% Personal (56.8%), Work-related (60%) Patient-related (28.9%) |
SD ↔ Study level (↑ clinical year) → ↑ burnout NSD ↔ Gender |
| Fernando & Samara-nayake/2019/Sri Lanka [32] | Burnout among postgraduate doctors in Colombo: Prevalence, associated factors and association with self-reported patient care | CSS/ N=245/ RR=88% |
Postgraduate Doctors | 46% Personal (41.6%), Work-related (30.6%) Patient-related (8.9%) |
SD ↔ Gender ↑ Females NSD ↔ Specialty |
| Aljuhayman et al/2020/Saudi Arabia [33] | Assessment of burnout among urology residents in KSA: A cross-sectional study | CSS/ N=247/ RR=87% |
Urology Residents | 48% Personal (57.9%) Work-related (55.3%) Patient-related (37.7%) |
SD ↔ Gender ↑ Females (work-related), ↑ Males (personal and patient-related burnouts) NSD ↔ Burnout types |
| Mahfouz et al/2020/Saudi Arabia [34] | Burnout and its associated factors among medical students of Jazan University, Jazan, Saudi Arabia | CSS/ N=440/ RR=99% |
Medical Students | 60.2% | SD ↔ Gender, year of study ↑ Females |
| Alsulimani et al/2021/Saudi Arabia [35] | Health care worker burnout during the COVID-19 pandemic | CSS/ N=646/ RR=NM |
Healthcare Workers | ------ Personal 75% Work-related (75.1%) Patient-related (NM) |
SD ↔ Experience years, exposure to COVID-19, times to deal with patients with COVID-19 |
| Chalikkandy et al/2022/Saudi Arabia [36] | Burnout and Its relation to emotion dysregulation and social cognition among female interns and undergraduate dental students at King Khalid University | CSS/ N=148/ RR=NM |
Female Interns and Undergraduate Dental Students | ------ Interns Personal (56.7%) Work-related (56.1%) Patient-related (44.8%) |
SD ↔ Personal distress ↑ distress = ↑ burnout NSD ↔ Burnout types |
| ----- Undergraduates: Personal (57.9%) Work-related (57.4%) Patient-related (42.3%) | |||||
| Antoniadou M/2022/Greece [37] | Estimation of factors affecting burnout in Greek dentists before and during the COVID-19 pandemic | CSS/ N=804/ RR=13% |
Dentists | NM | SD ↔ Gender |
| Fiabane et al/2022/Italy [38] | Prevalence and determinants of Italian physicians’ burnout in the “post-COVID-19” era | CSS/ N=958/ RR=25% |
Healthcare Workers | 71.6% | SD ↔ Gender NSD ↔ Different specialty |
Table 3.
Characteristics of studies conducted using Maslach Burnout Inventories and its types for burnout measurement (n=28).
| Research/study year/country | Study title | Study design/ sample size/ RR |
Specialty tested | Overall mean, %/Burnout type: Emotional exhaustion (EE), Depersonalization (DP), Personal achievement (PA) | Important finding and outcome |
|---|---|---|---|---|---|
| Soler et al/2008/Bulgaria, Croatia, France, Greece, Hungary, Italy, Malta, Poland, etc [39] | Burnout in European family doctor | CSS N=1393/ RR=41% |
Family Doctors | 12% EE=43% DP=35% PA=32% |
SD ↔ Gender ↑ Males NSD ↔ Country |
| Zantinge et al/2009/Netherlands [40] | Does burnout among doctors affect their involvement in patients’ mental health problems? | POS video-recorded and questionnaire N=142/ RR=89% |
General Practitioners | NM EE=7% DP=11% PA=22% |
SD ↔ Academic level NSD ↔ Gender, Age |
| Prins et al/2010/Netherlands [41] | Burnout and engagement among resident doctors in the Netherlands: A national study | DCSS N=5140/ RR=41% |
Medical Residents | 21% EE =30% DP=38% PA=14% |
SD ↔ Gender ↑ Females NSD ↔ Years in training |
| Blanchard et al/2010/France [42] | Prevalence and causes of burnout amongst oncology residents | DCSS N=340/ RR=60% |
Oncology Residents | 44% EE=26% DP=35% PA ----- |
SD ↔ Gender, ↑ Females ↑ Married NSD ↔ Specialty |
| Galan et al/2011/Spain [43] | Burnout risk in medical students in Spain using the Maslach Burnout Inventory-Student Survey. International archives of occupational and environmental health | CSS N=270/ RR=NM |
Medical Students | 25.6% 37.5% for 3rd years 14.8% for 6th years |
SD ↔ 3rd and 6th years NSD ↔ Gender |
| Ruitenburg et al/2012/Netherlands [44] | The prevalence of common mental disorders among hospital physicians and their association with self-reported work ability | CSS N=422/ RR=51% |
Physicians in Medical Center | 6% | SD ↔ Gender ↑ Females NSD ↔ Age |
| Siu et al/2012/Hong Kong [45] | Burnout among public doctors in Hong Kong | CSS N=226/ RR=23% |
Public Hospital Doctors | 31.4% | SD ↔ ↑ Working shifts = ↑ burnout |
| Cecil et al/2014/United Kingdom [46] | Behaviour and burnout in medical students | CSS N=356/ RR=NM |
Medical Students | 26.5% EE=55% DP=34% PA =47% |
SD ↔ Different levels NSD ↔ Gender |
| Takayesu et al/2014/United State [47] | Factors associated with burnout during emergency medicine residency | DCSS N=289/ RR=75% |
Emergency Medicine Residents | 65% EE=33% DP=59% PA =14% |
SD ↔ Gender, ↑ Males |
| Kushnir et al/2014/Israel [48] | Is burnout associated with referral rates among primary care physicians in community clinics? | CSOS N=136/ RR=99% |
General Practitioners/Primary care | 56% EE=44.5% DP=36% PA=31.6% |
SD ↔ Workload (↑ workload = ↑ burnout) |
| Yuguero Torres et al/2015/Spain [49] | Association between sick leave prescribing practices and physician burnout and empathy | POS (1 year) N=5140/ RR=41% |
General Practitioners | 2.3% EE=20.9%% DP=16.3%% PA=74.4%% |
SD ↔ Empathy (↑ Empathy = ↑ burnout) NSD ↔ Gender |
| Garrouste-Orgeaset al/2015/France [50] | The Iatroref study: Medical errors are associated with symptoms of depression in ICU staff but not burnout or safety culture | POS (2 years) N=1988/ RR=77% |
Intensive Care Unit/Doctors | 2.5% EE=10.6% DP=24.5% PA=31.5% |
NM |
| Intensive Care Unit/Nurses & Care Workers | 3.7% EE=13.4% DP=15.8% PA=31.6% |
||||
| Albalawi et al/2015/Saudi Arabia [51] | The assessment of the burnout syndrome among medical students in Tabuk University, a cross-sectional analytic study | CSAS N=140/ RR=79% |
Medical Students | 48.6% | NSD ↔ Gender |
| Aldrees et al/2015/Saudi Arabia [52] | Burnout among otolaryngology residents in Saudi Arabia | DCSS N=123/ RR=69% |
Otolaryngology Residents | 33% EE=62% DP=55% PA=17% |
NSD ↔ Burnout types |
| Kwah et al/2016/United State [53] | The effect of burnout on medical errors and professionalism in first-year internal medicine residents | POS (1 year) N=54/ RR=98% |
1st year Internal Medicine Residents | 89.2% | NM |
| Kealy et al/2016/Canada [54] | Burnout among Canadian psychiatry residents: A national survey | DCSS N=400/ RR=48% |
Psychiatry Residents | 21% | SD ↔ Training Years (↑ Years = ↑ burnout) |
| Elmore et al/2016/United State [55] | National survey of burnout among US general surgery residents | DCSS N=753/ RR=88% |
General Surgery Residents | 69% EE=57% DP=50% PA=16% |
SD ↔ Gender, ↑ working hours = ↑ burnout |
| Fares et al/2016/Lebanon [56] | Extracurricular activities associated with stress and burnout in preclinical medical students | CSS N=165/ RR=NM |
Preclinical Medical Students | 75.2% | SD ↔ Gender ↑ Females |
| Popa-Velea et al/2017/Romania [57] | Burnout and Its relationships with alexithymia, stress, and scial support among Romanian medical students | CSS N=299/ RR=75% |
Medical Students | 15.1% | SD ↔ Gender ↑ Females |
| Almalki et al/2017/Saudi Arabia [58] | Burnout and its association with extracurricular activities among medical students in Saudi Arabia | CSS N=306/ RR=81% |
Medical Students | 67.1% | NSD ↔ Academic level |
| Baer et al/2017/United State [59] | Pediatric resident burnout and attitudes toward patients | DCSS N=258/ RR=53% |
Pediatric Residents | 39.1% | NSD ↔ Gender |
| Shakir et al/2017/United State [60] | The Prevalence of burnout among US neurosurgery residents | DCSS N=1200/ RR=21% |
Neuro-surgery Residents | 36.5% | NSD ↔ Gender, postgraduate level |
| Van Vendeloo et al/2018/Belgium [61] | Resident burnout: Evaluating the role of the learning environment | DCSS N=263/ RR=35% |
Residents in University Hospital | 41.5% | NM |
| Jamjoom et al/2018/Saudi Arabia [62] | Assessment of pediatric residents burnout in a tertiary academic centre | DCSS N=50/ RR=91% |
Pediatric Residents at King Abdulazaiz University Hospital | 70% EE=43% DP=71.8% PA=40.6% |
NSD ↔ Gender |
| Al-Alawi et al/2019/Oman [63] | Prevalence and determinants of burnout syndrome and depression among medical students at Sultan Qaboos University: A cross-sectional analytical study from Oman | CSAS N=662/RR=98% |
Medical Students | 7.4% | SD ↔ Academic level (↑ Preclinical students) NSD ↔ Gender |
| Asali et al/2021/Saudi Arabia [64] | Prevalence of burnout and practice-related risk factors among dentists in Saudi Arabia | CSOS N=215/ RR=100% |
Dentists | 33.4% | SD ↔ Dental specialty (↑ Prosthodontists & Endodontists), Working hours (↑ Working hours = ↑ burnout) NSD ↔ Gender |
| Alqurashi et al/2022/Saudi Arabia [65] | Prevalence and risk factors of burnout among medical students during coronavirus disease 2019 pandemic online teaching: Cross-section | CSOS N=568/ RR=100% |
Medical Students | 39.4% | NSD ↔ Study and training years |
| AlShahrani et al/2022/Saudi Arabia [66] | Psychometric properties and validation of the Arabic Maslach burnout inventory-student survey in Saudi dental students | CSAS N=480/ RR=90% |
Dental Students | NM EE=32.3% DP ------ PA ----- |
SD ↔ ↑ workload = ↑ burnout NSD ↔ Gender |
CSs – cross-sectional survey or study; DCSS – descriptive cross-sectional study; DCSS – data collection social surveys; CSOS – cross sectional observational study; CSAS – cross sectional analytic study; POS – prospective observational study; DCSS – descriptive cross-sectional study; CSOS – cross – sectional online survey; CSOS– cross sectional observational study; OPCS – observational prospective cohort study; OV-R CQ – observation of video-recorded consultations and questionnaire; SD – significant differences; NSD – nonsignificant differences; ↔ – between; ↑ – increased or higher; ↓ – resulted; NM – not mentioned.
Publication Country, Years, and Study Design
Most of the available papers that used MBI were published between 2011 and 2019, with 22/28 studies, while for CBI the published articles were almost equal in numbers before 2020 and after 2020. The cross-sectional study design was used by all CBI papers and in 8 MBI studies. A total of 9, 5, 3, and 3 MBI papers used DCSS, POS, CSOS, and CSAS, respectively. Figure 2 presents the distribution and characteristics of the included studies for CBI and MBI in relation to countries where the study was conducted, publication year, and study design.
Figure 2.
Distribution of studies per country, publication year, and study design for Copenhagen and Maslach Burnout Inventories (n=41).
Sample Size and Response Rate
The total sample size for CBI was 6158 subjects collected from 13 papers with a total mean of 474 subjects per study (32% of the total sample size), whereas for MBI there were 21789 respondents from 28 papers with a mean of 778 samples per study (68% of the total sample size). In CBI, response rates (average, 66.8%) were mentioned in only 7 studies, whereas almost all papers that used MBI recorded response rates (average, 67.6%) (Table 4).
Table 4.
Sample size per study and response rate for Copenhagen and Maslach Burnout Inventories (n=41).
| Inventory type | Sample size per study | Number of papers | % | RR status | Number | % |
|---|---|---|---|---|---|---|
| CBI | 474 | 13 | 32 | NM | 6 | 0.00 |
| Mentioned | 6 | 66.80 | ||||
| MBI | 778 | 28 | 68 | NM | 1 | 0.00 |
| Mentioned | 25 | 67.60 |
Overall Mean of Burnout for CBI and MBI and Their Types
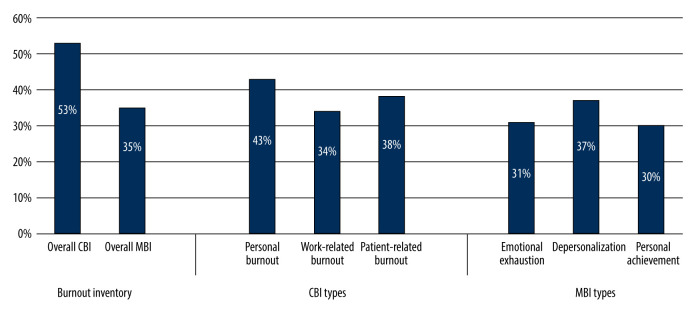
The overall percentages of burnout for CBI and MBI were 53% and 35%, respectively. For CBI, the mean values of personal, work-related, and patient-related burnouts were 43%, 34%, and 38%, respectively. For MBI, the mean values of emotional exhaustion, depersonalization, and personal achievement were 31%, 37%, and 30%, respectively (Figure 3).
Figure 3.
Overall mean and percentage of Copenhagen and Maslach burnout inventories and for their types (n=41).
For CBI, the percentages of significance were 23%, 46%, and 23%, for burnout type, gender, and level of education, respectively, as well as different specialty, while it was 14%, 29%, and 18%, respectively for the same parameters in MBI studies (Figure 4).
Figure 4.
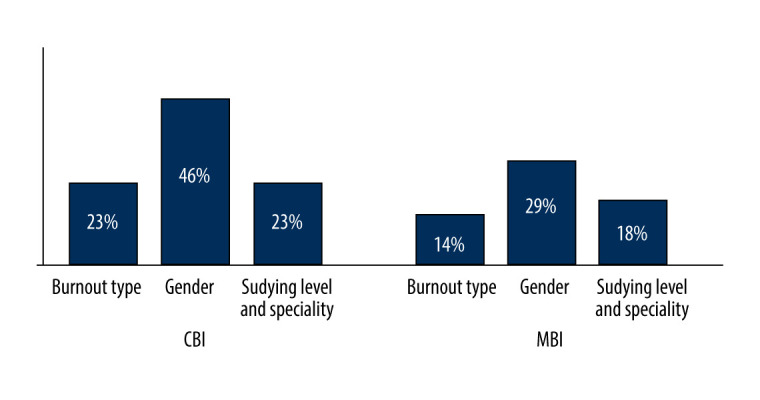
Percentages of Significancy in relation to Burnout type, gender, and studying level among studies included in this review (n=41).
Discussion
To the best of our knowledge, a systematic review that includes studies utilizing CBI and MBI scales has not been conducted yet. Thus, this review summarizes and covers all studies dealing with burnout of all healthcare workers and students by using the CBI and MBI scales. The current review calculated and assessed papers that concerned all students and workers in medical fields that used CBI and MBI and compared those results between genders and educational levels as well as speciality. Therefore, our analysis is among the first reviews to include studies on the prevalence of burnout and its risk variables among healthcare workers from various disciplines by using MBI and/or CBI scales [67–69]. The overall values of this systematic results agree with findings of other recently published reviews [20,21,70–73], and in relation to the significant relationships among gender, burnout types, educational level, and healthcare specialty.
According to results of the current review, MBI was the most widely used scale in Europe, whereas CBI is mostly used in Saudi Arabia and the rest of the Arab world. This may be because CBI utilizes questions that are readily translated into a variety of languages (eg, English, Japanese, Mandarin, Cantonese, Swedish, Finnish, French, and Slovenian) and is now used in many nations. By contrast, MBI uses questions that cannot be translated in the same manner because it uses questions relating to American culture and cannot be generalized to other populations [10].
Most of the studies conducted before 2008 used the MBI scale, and more studies have used CBI since the beginning of 2016 (Tables 2, 3). This finding may be related to the introduction date of the inventory type. In terms of study design, most studies using either scale used cross-sectional surveys because the MBI and CBI are questionnaire-based measurements that can only be used in various types of cross-sectional studies, such as descriptive cross-sectional studies (DCSS), data collection social surveys (DCSS), and cross-sectional observational studies (CSOS). The response rate in studies that utilize the CBI scale was higher than in studies that used the MBI scale because the former utilizes questions that are simple to comprehend and answer, while the latter uses questions that are difficult to answer. Hence, CBI questionnaires are easy to fill out and have a higher response rate [10].
In terms of study population, most studies involved medical residents because burnout syndrome is a serious problem in this population. The pressure of work throughout residency training is quite high, especially because residents are expected to be competent clinicians, educators, and administrators at the end of residency training [15]. Additionally, medical students’ academic lives may be regarded as psychologically hazardous, and the major source of stress is related to academic requirements [27]. A recent meta-analysis found that medical students worldwide suffer from a high prevalence of depression, with an estimated prevalence of 28.0% (24.2–32.1%) [67]. By contrast, before entering medical school, the prevalence of depression among future medical students was only 1.4% to 1.8% [68,69].
CBI and MBI have remarkable differences. CBI has higher percentage than MBI in overall and types (personal, work-related, and patient-related burnouts) except for one, in which the type of MBI has recorded a slightly higher percentage (37%, Figure 3). According to the results of this review, the prevalence values of burnout among all study participants are 53% and 35% in CBI and MBI studies, respectively. This finding does not agree with the review undertaken by Reardon et a6. in 2020, which found that the prevalence values of burnout in CBI and MBI studies are 56% and 18%, respectively [70]. In terms of MBI subscales, the prevalence values of each subscale are as follows: EE, 31%; DP, 37%; and PA, 30%. These figures contrast sharply with a very recent review published by Parandeh et al in 2022 [71], which found that the prevalence values of EE, DP, and PA are 37%, 18%, and 51%, respectively. Another review, among medical students, found that the prevalence values of EE, DP, and PA are 40.8%, 35.1%, and 27.4%, respectively [72]. Our analysis also looked at the prevalence of CBI subscales among the involved studies. The prevalence values of personal, work-related, and patient-related burnouts are 43%, 34%, and 38%, respectively. Martos et al in 2020 recorded that the prevalence values of personal, work-related, and patient-related burnouts are 50%, 40%, and 10%, respectively [73].
Tables 2 and 3 show that a significant difference in CBI between genders is recorded in studies conducted in different countries [29,32,34,37], but not in studies among populations from Saudi Arabia and Egypt [29,31]. Also, CBI recognizes a significant difference between the types and subscales of burnout among studies carried out in South Africa and Malaysia [26,27]. Other studies have not identified this parameter in their results [28,36]. Also, MBI is significantly different between genders in published research [41,44,47,55–57], and was found to be higher among females in studies conducted in countries such as the Netherlands [28,30], USA, Lebanon, and Romania [55,57]. Two studies recorded that males have higher burnout rates than females [34,47], which can be attributed to genetics and socio-economic statuses of those countries. As the educational attainment increases, burnout increases among participants from different countries and populations [30,34,35,40,54,63]. Marital status was associated with higher burnout in studies using CBI and MBI burnout [40,45,60]. Parts of these findings were reported by a recent review published by Mangory et al in 2021 and other reviews by Juan and Juan and Patel et al in 2019 [17,15], whereas some findings agree with the results of other published reviews of the literature [70–74].
The discrepancies in all the aforementioned values and important findings in the last column of tables show that the contents of different studies using CBI and MBI are attributable to the varying criteria for selecting studies. Some reviews involved medical students, whereas others involved medical residents. The prevalence of burnout depends on the field and degree of study or work area. A higher percentage of significances were detected between genders, as seen in Figure 4, and those results agree with previous studies [19,21].
The limitations of this review are that it included many studies from different countries and health subspecialities. Further reviews are needed to compare different countries, health specialties, and educational levels.
Conclusions
Burnout is a common issue among medical workers but has only lately been acknowledged as a disease [63]. CBI recorded higher burnout compared with studies that used MBI. Female students with higher education levels and married people showed higher levels of burnout in studies using the CBI and MBI scales. The present study shows an association with the quality and efficacy of patient treatment. As a result of understanding the level of burnout and its types, the prevention and detection measures for affected workers can be improved, which will increase job satisfaction.
Footnotes
Conflict of interest: None declared
Declaration of Figures’ Authenticity
All figures submitted have been created by the authors, who confirm that the images are original with no duplication and have not been previously published in whole or in part.
Financial support: None declared
References
- 1.Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol. 2001;52:397–422. doi: 10.1146/annurev.psych.52.1.397. [DOI] [PubMed] [Google Scholar]
- 2.Maslach C, Jackson SE. The measurement of experienced burnout. Journal of Organizational Behavior. 1981;2(2):99–113. [Google Scholar]
- 3.Davis EL. Dental student stress, burnout, and memory. J Dent Educ. 1989;53(3):193–95. [PubMed] [Google Scholar]
- 4.Jugale PV, Mallaiah P, Krishnamurthy A, Sangha R. Burnout, and work engagement among dental practitioners in Bangalore city: A cross-sectional study. J Clin Diagn Res. 2016;10(2):ZC63. doi: 10.7860/JCDR/2016/16009.7312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization. Burn-out an “occupational phenomenon” : International Classification of Diseases. World Health Organization; Geneva, Switzerland: 2019. 2019. Nov, [Google Scholar]
- 6.Freudenberger HJ. Staff burn-out. Journal of Social Issues. 1974;30(1):159–65. [Google Scholar]
- 7.Ribeiro RV, Martuscelli OJ, Vieira AC, Vieira CF. Prevalence of burnout among plastic surgeons and residents in plastic surgery: A systematic literature review and meta-analysis. Plast Reconstr Surg Glob Open. 2018;6(8):E1854. doi: 10.1097/GOX.0000000000001854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Maslach C, Leiter MP. New insights into burnout and health care: Strategies for improving civility and alleviating burnout. Med Teach. 2017;39(2):160–63. doi: 10.1080/0142159X.2016.1248918. [DOI] [PubMed] [Google Scholar]
- 9.Kesarwani V, Husaain ZG, George J. Prevalence and factors associated with burnout among healthcare professionals in India: A systematic review and meta-analysis. Indian J Psychol Med. 2020;42(2):108–15. doi: 10.4103/IJPSYM.IJPSYM_387_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kristensen TS, Borritz M, Villadsen E, Christensen KB. The Copenhagen Burnout Inventory: A new tool for the assessment of burnout. Work and Stress. 2005;19(3):192–207. [Google Scholar]
- 11.Maslach C, Jackson SE, Leiter MP. Maslach Burnout Inventory Manual. 4th Edn. Menlo Park, CA: Mind Garden; 2017. [Google Scholar]
- 12.Tanner G, Bamberg E, Kozak A, et al. Hospital physicians’ work stressors in different medical specialities: A statistical group comparison. J Occup Med Toxicol. 2015;10(1):7. doi: 10.1186/s12995-015-0052-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee YY, Medford AR, Halim AS. Burnout in physicians. J R Coll Physicians Edinb. 2015;45(2):104–7. doi: 10.4997/JRCPE.2015.203. [DOI] [PubMed] [Google Scholar]
- 14.Dewa CS, Loong D, Bonato S, et al. How does burnout affect physician productivity? A systematic literature review. BMC Health Serv Res. 2014;14(1):1–10. doi: 10.1186/1472-6963-14-325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Juan Y-C, Juan C-W. How to prevent burnout in medical residents: Literature review. American Journal of Biomedical Science Research. 2019;5:151–54. [Google Scholar]
- 16.Patel RS, Sekhri S, Bhimanadham NN, et al. A review on strategies to manage physician burnout. Cureus. 2019;11(6):e4805. doi: 10.7759/cureus.4805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mangory KY, Ali LY, Rø KI, Tyssen R. Effect of burnout among physicians on observed adverse patient outcomes: A literature review. BMC Health Serv Res. 2021;21(1):369. doi: 10.1186/s12913-021-06371-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dubale BW, Friedman LE, Chemali Z, et al. Systematic review of burnout among healthcare providers in sub-Saharan Africa. BMC Public Health. 2019;19(1):1247. doi: 10.1186/s12889-019-7566-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Parola V, Coelho A, Cardoso D, et al. Prevalence of burnout in health professionals working in palliative care: A systematic review. JBI Database System Rev Implement Rep. 2017;15(7):1905–33. doi: 10.11124/JBISRIR-2016-003309. [DOI] [PubMed] [Google Scholar]
- 20.Bykov KV, Zrazhevskaya IA, Topka EO, et al. Prevalence of burnout among psychiatrists: A systematic review and meta-analysis. J Affect Disord. 2022;308:47–64. doi: 10.1016/j.jad.2022.04.005. [DOI] [PubMed] [Google Scholar]
- 21.Shoman Y, Marca SC, Bianchi R, et al. Psychometric properties of burnout measures: A systematic review. Epidemiol Psychiatr Sci. 2021;30:e8. doi: 10.1017/S2045796020001134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chuang CH, Tseng PC, Lin CY, et al. Burnout in the intensive care unit professionals: A systematic review. Medicine. 2016;95(50):e5629. doi: 10.1097/MD.0000000000005629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rotenstein LS, Torre M, Ramos MA, et al. Prevalence of burnout among physicians: A systematic review. JAMA. 2018;320(11):1131–50. doi: 10.1001/jama.2018.12777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Salameh JP, Bossuyt PM, McGrath TA, et al. Preferred reporting items for systematic review and meta-analysis of diagnostic test accuracy studies (PRISMA-DTA): Explanation, elaboration, and checklist. BMJ Clinical Res. 2020;37:m2632. doi: 10.1136/bmj.m2632. [DOI] [PubMed] [Google Scholar]
- 25.The Joann Briggs. Joanna Briggs Institute Critical Appraisal Tools for use in Analytical Cross-Sectional Studies. 2017. https://jbi.global/sites/default/files/2019-05/JBI_Critical_Appraisal-Checklist_for_Analytical_Cross_Sectional_Studies2017_0.pdf .
- 26.Stein C, Sibanda T. Burnout among paramedic students at a university in Johannesburg, South Africa. African Journal of Health Professions Education. 2016;8(2):193–205. [Google Scholar]
- 27.Chin RW, Chua YY, Chu MN, et al. Prevalence of Burnout among UniversitiSains Malaysia Medical Students. Education in Medicine Journal. 2016;8(3):61–74. [Google Scholar]
- 28.DeWitt D, Canny BJ, Nitzberg M, et al. Medical student satisfaction, coping and burnout in direct-entry versus graduate-entry programmes. Medical Education. 2016;50(6):637–45. doi: 10.1111/medu.12971. [DOI] [PubMed] [Google Scholar]
- 29.Kulkarni S, Dagli N, Duraiswamy P, et al. Stress and professional burnout among newly graduated dentists. J Int Soc Prev Community Dent. 2016;6(6):535–41. doi: 10.4103/2231-0762.195509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Aboalshamat K, Alzahrani M, Rabie N, et al. The relationship between burnout and perfectionism in medical and dental students in Saudi Arabia. Journal of Dental Specialities. 2017;5(2):122–27. [Google Scholar]
- 31.Atlam SA. Burnout syndrome: Determinants and predictors among medical students of Tanta University, Egypt. Egyptian Journal of Community Medicine. 2018;36(01):61–73. [Google Scholar]
- 32.Fernando BM, Samaranayake DL. Burnout among postgraduate doctors in Colombo: Prevalence, associated factors and association with self-reported patient care. BMC Med Educ. 2019;19(1):373. doi: 10.1186/s12909-019-1810-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Aljuhayman AM, Alkhamees MA, Alkanhal HF, et al. Assessment of burnout among urology residents in KSA: A cross-sectional study. J Taibah Univ Med Sci. 2021;16(1):29–33. doi: 10.1016/j.jtumed.2020.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mahfouz MS, Ali SA, Alqahtani HA, et al. Burnout and its associated factors among medical students of Jazan University, Jazan, Saudi Arabia. Ment Illn. 2020;12(2):35–42. doi: 10.1108/MIJ-06-2020-0011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Alsulimani LK, Farhat AM, Borah RA, et al. Health care worker burnout during the COVID-19 pandemic: A cross-sectional survey study in Saudi Arabia. Saudi Med J. 2021;42(3):306–14. doi: 10.15537/smj.2021.42.3.20200812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chalikkandy S, Alhifzi RS, Asiri MA, et al. Burnout and its relation to emotion dysregulation and social cognition among female interns and undergraduate dental students at King Khalid University. Applied Sciences. 2022;12(3):1588. [Google Scholar]
- 37.Antoniadou M. Estimation of factors affecting burnout in Greek dentists before and during the COVID-19 pandemic. Dent J (Basel) 2022;10(6):108. doi: 10.3390/dj10060108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fiabane E, Margheritti S, Aiello EN, et al. Prevalence and determinants of Italian physicians’ burnout in the “post-COVID-19” era. Int Arch Occup Environ Health. 2022 doi: 10.1007/s00420-022-01929-6. [online ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Soler JK, Yaman H, Esteva M, et al. Burnout in European family doctors: The EGPRN study. Fam Pract. 2008;25(4):245–65. doi: 10.1093/fampra/cmn038. [DOI] [PubMed] [Google Scholar]
- 40.Zantinge EM, Verhaak PF, de Bakker DH, et al. Does burnout among doctors affect their involvement in patients’ mental health problems? A study of videotaped consultations. BMC Family Practice. 2009;10(1):60. doi: 10.1186/1471-2296-10-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Prins Hoekstra-Weebers JE, Gazendam-Donofrio SM, Dillingh GS, et al. Burnout and engagement among resident doctors in the Netherlands: A national study. Med Educ. 2010;44(3):236–47. doi: 10.1111/j.1365-2923.2009.03590.x. [DOI] [PubMed] [Google Scholar]
- 42.Blanchard P, Truchot D, Albiges-Sauvin L, et al. Prevalence and causes of burnout amongst oncology residents: A comprehensive nationwide cross-sectional study. Eur J Cancer. 2010;46(15):270815. doi: 10.1016/j.ejca.2010.05.014. [DOI] [PubMed] [Google Scholar]
- 43.Galán F, Sanmartín A, Polo J, Giner L. Burnout risk in medical students in Spain using the Maslach Burnout Inventory-Student Survey. Inter Archiv Occup Environmental Health. 2021;84(4):453–59. doi: 10.1007/s00420-011-0623-x. [DOI] [PubMed] [Google Scholar]
- 44.Ruitenburg MM, Frings-Dresen MH, Sluiter JK. The prevalence of common mental disorders among hospital physicians and their association with self-reported work ability: A cross-sectional study. BMC Health Serv Res. 2012;12(1):292–98. doi: 10.1186/1472-6963-12-292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Siu C, Yuen SK, Cheung A. Burnout among public doctors in Hong Kong: Cross-sectional survey. Hong Kong Med J. 2012;18(3):186–92. [PubMed] [Google Scholar]
- 46.Cecil J, McHale C, Hart J, Laidlaw A. Behaviour and burnout in medical students. Med Educ Online. 2014;19(1):25209. doi: 10.3402/meo.v19.25209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Takayesu J, Ramoska EA, Clark TR, et al. Factors associated with burnout during emergency medicine residency. Acad Emerg Med. 2014;21(9):1031–35. doi: 10.1111/acem.12464. [DOI] [PubMed] [Google Scholar]
- 48.Kushnir T, Greenberg D, Madjar N, et al. Is burnout associated with referral rates among primary care physicians in community clinics? Fam Pract. 2014;31(1):44–50. doi: 10.1093/fampra/cmt060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yuguero Torres O, EsquerdaAresté M, Marsal Mora JR, Soler-González J. Association between sick leave prescribing practices and physician burnout and empathy. PLoS One. 2015;10(7):e0133379. doi: 10.1371/journal.pone.0133379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Garrouste-Orgeas M, Perrin M, Soufir L, et al. The Iatroref study: Medical errors are associated with symptoms of depression in ICU staff but not burnout or safety culture. Intensive Care Med. 2015;41(2):273–84. doi: 10.1007/s00134-014-3601-4. [DOI] [PubMed] [Google Scholar]
- 51.Albalawi AE, Alhawiti TS, Aldahi AS, et al. The assessment of the burnout syndrome among medical students in Tabuk University, a cross-sectional analytic study. Basic Research Journal. 2015;6(1):14–19. [Google Scholar]
- 52.Aldrees T, Badri M, Islam T, Alqahtani K. Burnout among otolaryngology residents in Saudi Arabia: A multicenter study. J Surg Educ. 2015;72(5):844–48. doi: 10.1016/j.jsurg.2015.02.006. [DOI] [PubMed] [Google Scholar]
- 53.Kwah J, Weintraub J, Fallar R, Ripp J. The effect of burnout on medical errors and professionalism in first-year internal medicine residents. J Grad Med Educ. 2016;8(4):597–600. doi: 10.4300/JGME-D-15-00457.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kealy D, Halli P, Ogrodniczuk JS, Hadjipavlou G. Burnout among Canadian psychiatry residents: A national survey. Can J Psychiatry. 2016;61(11):732–36. doi: 10.1177/0706743716645286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Elmore LC, Jeffe DB, Jin L, et al. National survey of burnout among US general surgery residents. J Am Coll Surg. 2016;223(3):440–51. doi: 10.1016/j.jamcollsurg.2016.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Fares J, Saadeddin Z, Al Tabosh H, et al. Extracurricular activities associated with stress and burnout in preclinical medical students. J Epidemiol Glob Health. 2016;6(3):177–85. doi: 10.1016/j.jegh.2015.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Popa-Velea O, Diaconescu L, Mihăilescu A, et al. Burnout and its relationships with alexithymia, stress, and social support among Romanian medical students: A cross-sectional study. Int J Environ Res Public Health. 2017;14(6):560. doi: 10.3390/ijerph14060560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Almalki SA, Almojali AI, Alothman AS, et al. Burnout and its association with extracurricular activities among medical students in Saudi Arabia. Int J Med Educ. 2017;8:144. doi: 10.5116/ijme.58e3.ca8a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Baer TE, Feraco AM, TuysuzogluSagalowsky S, et al. Pediatric resident burnout and attitudes toward patients. Pediatrics. 2017;139(3):e20162163. doi: 10.1542/peds.2016-2163. [DOI] [PubMed] [Google Scholar]
- 60.Shakir HJ, McPheeters MJ, Shallwani H, et al. The prevalence of burnout among US neurosurgery residents. Neurosurgery. 2018;83(3):582–90. doi: 10.1093/neuros/nyx494. [DOI] [PubMed] [Google Scholar]
- 61.Van Vendeloo SN, Godderis L, Brand PL, et al. Resident burnout: Evaluating the role of the learning environment. BMC Med Educ. 2018;18(1):54. doi: 10.1186/s12909-018-1166-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Jamjoom RS, Park YS. Assessment of pediatric residents burnout in a tertiary academic centre. Saudi Med J. 2018;39(3):296–300. doi: 10.15537/smj.2018.3.22328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Al-Alawi M, Al-Sinawi H, Al-Qubtan A, et al. Prevalence and determinants of burnout syndrome and depression among medical students at Sultan Qaboos University: A cross-sectional analytical study from Oman. Arch Environ Occup Health. 2019;74(3):130–39. doi: 10.1080/19338244.2017.1400941. [DOI] [PubMed] [Google Scholar]
- 64.Asali AT, Pullishery F, Ibrahim NM, Tobji WW. Prevalence of burnout and practice-related risk factors among dentists in Saudi Arabia. Saud J Oral Scien. 2021;8(2):104. [Google Scholar]
- 65.Alqurashi A, Alhassani T, Alsaeedi E, et al. Prevalence and risk factors of burnout among medical students during coronavirus disease 2019 pandemic online teaching: Cross-section. Medical Science. 2022;26:ms197e2168. [Google Scholar]
- 66.AlShahrani I, Eroje AB, Tikare S, et al. Psychometric properties and validation of the Arabic Maslach Burnout Inventory-Student Survey in Saudi dental students. Saudi J Med Med Sci. 2022;10:117–24. doi: 10.4103/sjmms.sjmms_116_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Puthran R, Zhang MWB, Tam WW, Ho RC. Prevalence of depression amongst medical students: A meta-analysis. Med Educ. 2016;50(4):456–68. doi: 10.1111/medu.12962. [DOI] [PubMed] [Google Scholar]
- 68.Yusoff MSB, Abdul Rahim AF, Baba AA, et al. Prevalence and associated factors of stress, anxiety and depression among prospective medical students. Asian J Psychiatry. 2013;6(2):128–33. doi: 10.1016/j.ajp.2012.09.012. [DOI] [PubMed] [Google Scholar]
- 69.Smith CK, Peterson DF, Degenhardt BF, Johnson JC. Depression, anxiety, and perceived hassles among entering medical students. Psychol Health Med. 2007;12(1):31–39. doi: 10.1080/13548500500429387. [DOI] [PubMed] [Google Scholar]
- 70.Reardon M, Abrahams R, Thyer L, Simpson P. Prevalence of burnout in paramedics: A systematic review of prevalence studies. Emergency Med Australas. 2020;32(2):182–89. doi: 10.1111/1742-6723.13478. [DOI] [PubMed] [Google Scholar]
- 71.Parandeh A, Ashtari S, Rahimi-Bashar F, et al. Prevalence of burnout among health care workers during coronavirus disease (COVID-19) pandemic: A systematic review and meta-analysis. Professional Psychology: Research and Practice. doi: 10.1037/pro0000483. Advance online publication. [DOI] [Google Scholar]
- 72.Frajerman A, Morvan Y, Krebs MO, et al. Burnout in medical students before residency: A systematic review and meta-analysis. Eur Psychiatry. 2019;55:36–42. doi: 10.1016/j.eurpsy.2018.08.006. [DOI] [PubMed] [Google Scholar]
- 73.Suleiman-Martos N, Albendín-García L, Gómez-Urquiza JL, et al. Prevalence and predictors of burnout in midwives: A systematic review and meta-analysis. Inte J Environ Rese Public Health. 2020;17(2):641. doi: 10.3390/ijerph17020641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Berrío García N, Foronda Valencia D, Ciro Parra D. Síndrome de burnout en personal de la salud latinoamericano. Revista de Psicología: (Universidad de Antioquía) 2018;10(2):157–81. [Google Scholar]