Abstract
Background:
During acute health decompensations for seriously ill patients, emergency clinicians often determine the intensity end-of-life care. Little is known about how emergency clinicians conduct these conversations, especially among those who have received serious illness communication training.
Aim:
To determine the self-reported practice patterns of code status conversations by emergency clinicians with and without serious illness communication training.
Design:
A cross-sectional survey was conducted among emergency clinicians with and without a recent evidence-based, serious illness communication training tailored for emergency clinicians. Emergency clinicians were included from two academic medical centers. A 5-point Likert scale (“very unlikely” to “very likely” to ask) was used to assess the self-reported likelihood of asking about patients’ preferences for medical procedures and patients’ values and goals.
Results:
Among 161 respondents (71% response rate), 77 (48%) received the training. 70% of emergency clinicians reported asking about procedure-based questions, and only 38% reported asking about patient’s values regarding end-of-life care. For value-based questions, statistically significant differences were observed between emergency clinicians who underwent the training and those who did not in four of the seven questions asked (e.g., the higher odds of exploring the patient’s life priorities (adjusted OR = 4.34, 95%CI = 1.95–9.65, p-value < 0.001)). No difference was observed in the self-reported rates of all procedure-based questions between the two groups.
Conclusion:
Most emergency clinicians reported asking about procedure-based questions, and some asked about patient’s value-based questions. Clinicians with recent serious illness communication training may ask more about some values and priorities.
Keywords: communication, emergency medicine, emergency department, training programs
Introduction
Emergency clinicians care for patients with serious, life-limiting illnesses in acute clinical deteriorations who require immediate decision-making.1,2 In the emergency department (ED), more than 60% of seriously ill patients do not possess advance directives and are at risk of receiving care that is influenced by the time-pressured, stressful situation.1–3 Emergency clinicians primarily focus on preserving life and stabilization.4 During acute health decompensations for seriously ill older adults, emergency clinicians must engage in urgent shared decision-making with patients to decide on the intensity of end-of-life care (i.e., code status conversations).1 Code status conversations are defined as urgent shared decision-making during acute health decompensations between patients and clinicians to decide the intensity of end-of-life care. High quality code status conversations are critical to ensure the care is aligned to patients’ values and goals. Many emergency clinicians are “skeptical” (>50%)5 and “uncomfortable” (>70%)6 about their abilities to identify seriously ill patients and conduct patient-centered, code status conversations. When seriously ill patients without prior discussions arrive, increased anxiety from acute health decompensations put them at risk of care decisions potentially unaligned to their goals, which may also lead to worsened quality of life.3,7
In general, early serious illness conversations about patient’s values and preferences have been associated with 50% lower rates of dying in intensive care units, less aggressive medical care at the end of life, 1.5 times higher utilization of hospice services, reduced anxiety in surviving relatives, and 56% higher likelihood of having end-of-life wishes known and followed.3,7,8 Although these conversations ideally occurred before a health crisis, urgent code status conversations (i.e., a shared decision-making between clinicians and patients or surrogates regarding the use of cardiopulmonary resuscitation or mechanical ventilation during acute health crisis) still commonly occur in EDs across the U.S.1 In code status conversations for patients with serious illness, emergency clinicians must share the clinical severity and poor expected prognosis, followed immediately by shared, in-the-moment decision-making regarding the intensity of medical care aligned to patients’ values and preferences. Best practices in serious illness communication exist in non-emergency setting to help clinicians in this shared decision-making.9,10 Recognizing the opportunity to provide patient-centered, goal-concordant end-of-life care,4,5,12,13 emergency clinicians and health services researchers, adapted an existing evidence-based, serious illness communication training for use by emergency clinicians.1,11–13 After serious illness communication training, emergency clinicians reported feeling more comfortable discussing code status and improved their abilities to guide treatment decisions.6,14 However, the actual practice patterns of clinicians who received the training have not been described. In code status conversations, emergency clinicians traditionally ask about patient’s preferences for emergency procedures1,10 (e.g., would your father want to be on a breathing machine?), whereas the best practices in palliative care recommend asking about patients’ value or preference for their quality of life1,9,10 (e.g., what is important to your father if the time were to be short?). These approaches may yield different care decisions for patients approaching the end of life. We hypothesize that emergency clinicians who underwent serious illness communication training would report asking more patient’s value-based questions in code status conversations. Therefore, we sought to determine the self-reported practice patterns of code status conversations among emergency clinicians with and without a recent serious illness communication training.
Materials and Methods
Study design and setting
We conducted a cross-sectional survey in two large, urban, academic medical centers in Boston, Massachusetts from November 2021 to January 2022. The medical centers have 1,059 beds with 100,000 annual ED visits and 793 beds with 57,000 annual ED visits. We chose these two sites because of the similarity in practice settings and large size of the clinical practice groups. In the EDs that we conducted the study, physician assistants and nurse practitioners could be involved in code status conversations, which may be variable in other Eds across the U.S. All 112 emergency clinicians (63 attending physicians and 49 physician assistants) at one site underwent the serious illness communication training, whereas 114 clinicians (50 attending physicians and 64 nurse-practitioners/physician assistants) at another site did not. We asked participants to identify their self-reported practice patterns of code status conversations and compared the results between the two sites. This study was determined to be exempt from institutional review board approval per our institution.
Participants and procedures
We identified full-time clinicians clinically active in their respective EDs using departmental rosters. We invited attending physicians, physician assistants, and nurse practitioners to participate. All participants received the survey three to six months after the serious illness communication training at one of the sites. The survey was voluntary and de-identified. The participants received $15 incentive to complete the survey. The survey was conducted electronically using research electronic data capture.15,16 An email containing the study invitation, information sheet, and a link was sent to the participants. Reminders were sent one week apart from the original email twice during the study period. The participants were the recipients who interact with the initial invitations, reviewed the fact sheet, identify their interest in participating, and completed the electronic survey.
The evidence-based, serious illness communication training
All clinicians at one of the two sites underwent evidence-based, serious illness communication training as part of a large, pragmatic clinical trial previously described.12 Briefly, two components exist in this training: 1) The Education in Palliative and End-of-Life Care for Emergency Medicine (EPEC-EM) – an abbreviated, one-hour online didactic of a comprehensive curriculum that provides primary palliative care knowledge and skills for emergency clinicians;12,13 and, 2) EM Talk - an evidence-based, serious illness communication training adapted for the clinical practice of emergency medicine. EM Talk is a four-hour in-person simulation workshop with professional actors as simulating patients or families. In small group environment, participating clinicians practice code status conversations using specific communication skills and receive constructive feedback from master clinicians.11,12,14
Survey instrument and outcomes
After reviewing the literature and leveraging clinical expertise in emergency medicine and palliative care, the study team drafted the survey items. The survey started with a typical case describing a seriously ill patient requiring emergent, shared, decision-making in the ED followed by the survey items. Given that no validated survey existed to measure the practice patterns of code status conversations, our study team developed this instrument based on our expertise. After discussing the theoretical constructs to be included in code status conversations among emergency physicians and palliative medicine physicians in our team, we developed the initial instrument. We pilot tested the initial instrument for clarity and appropriateness by distributing them to five emergency physicians and two palliative medicine physicians to solicit their feedback. Based on feedback, we shortened the case scenario, survey questions, and categorized the items into two categories: procedure-based questions (eight items, e.g., Would your father want to be on the breathing machine?) and patients’ value-based questions (twelve items, e.g., What is important to your father if the time were to be short?). The final instrument, as shown in supplemental file 1, included eleven items with the following topics: self-reported practice patterns of code status conversations (a 5-point Likert scale, ranging from very unlikely to ask (1) to very likely to ask (5)), demographics (occupational role, clinical experience after graduating from professional schools), estimated number of code status conversations per month, and prior training in palliative care. The primary outcome was self-reported, practice patterns in code status conversations by emergency clinicians.
Statistical analysis
We performed data analysis from January to March 2022. The baseline characteristics of the participants were summarized using descriptive statistics. Chi-square test or Fisher’s exact test was used for categorical data and explored associations between demographic characteristics and components of the conversations reported by emergency clinicians. For simplicity of presentation and also to use logistic regression for controlling for confounders, we combined ratings of “very likely to ask” and “somewhat likely to ask,” while grouping “very unlikely to ask,” “somewhat unlikely to ask,” and “neutral” in a separate group. Multivariable logistic regression analysis was performed to determine the association between procedure-based and patients’ value-based components of the conversation and the serious illness communication training. Using the study team’s clinical expertise, we controlled for the following pre-specified, potential confounders: occupational role, years of clinical practice, previous training in palliative care, and frequency of code status conversations. We used p-value of less than 0.05 for statistical significance. We reported the adjusted odds ratio (OR) and 95% confidence interval (CI). Statistical analyses were performed using Stata 16.0 (StataCorp LLC, College Station, TX, USA).
Results
Of the 226 emergency clinicians at the 2 sites who received the study invitation, 161 completed the survey (71% response rate). Among the respondents, 77 clinicians (48%) were from one site that recently underwent the serious illness communication training; 82 (51%) were attending physicians. Clinical experience varied widely (30% with 0–5 years, 13% with 21+ years). The frequency of emergent code status conversations ranged from less than once every two months (33%) to more than twice per month (16%). Most clinicians (83%) reported some type of prior training in palliative care. Some clinicians in the non-training site did report “prior training in palliative care” from either their undergraduate or post-graduate trainings, which are inherently variable in quality of the training. Given this baseline distribution of training is similar at training and non-training sites, the only difference between the clinician groups remains our evidence-based, serious illness training. Clinicians from the site where the serious illness communication training was recently conducted reported more prior training compared to the other site (92% and 75% respectively, p-value = 0.004). Table 1 summarizes the demographics.
Table 1.
Baseline demographic characteristics of emergency clinicians
| Total N=161 (%) | without training n=84 (%) | with training n=77 (%) | p-value | |
|---|---|---|---|---|
| Role | 0.068 | |||
| Attending physician | 82 (51) | 37 (44) | 45 (58) | |
| Physician assistant or Nurse practitioner | 79 (49) | 47 (56) | 32 (42) | |
| Year in practicing clinical medicine | 0.945 | |||
| 0–5 years | 49 (30) | 27 (32) | 22 (29) | |
| 6–10 years | 49 (30) | 25 (30) | 24 (31) | |
| 11–15 years | 19 (12) | 9 (11) | 10 (13) | |
| 16–20 years | 23 (14) | 11 (13) | 12 (16) | |
| 21+ years | 21 (13) | 12 (14) | 9 (12) | |
| Frequency of verbally determining code status while providing clinical care | 0.559 | |||
| < once every 2 months | 53 (33) | 25 (30) | 28 (36) | |
| 1 time every 1 −2 month | 45 (28) | 27 (32) | 18 (23) | |
| 1– 2 times every month | 37 (23) | 20 (24) | 17 (22) | |
| >2 times per month | 26 (16) | 12 (14) | 14 (18) | |
| Prior training in palliative care or communication skills for end-of-life care | 0.004 | |||
| Never | 27 (17) | 21 (25) | 6 (8) | |
| Prior training | 134 (83) | 63 (75) | 71 (92) | |
Most emergency clinicians reported asking about procedure-based questions. Regardless of the recent serious illness communication training, most emergency clinicians from both EDs reported “very likely” or “somewhat likely” to ask all six procedure-based questions in code status conversations (e.g., 93% in the site without the recent serious illness communication training and 92% in the site with recent training reported asking “would your father want to be on a breathing machine,” p-value =0.336). No statistically significant differences were observed between the two groups in all procedure-based questions (Figure 1).
Figure 1.
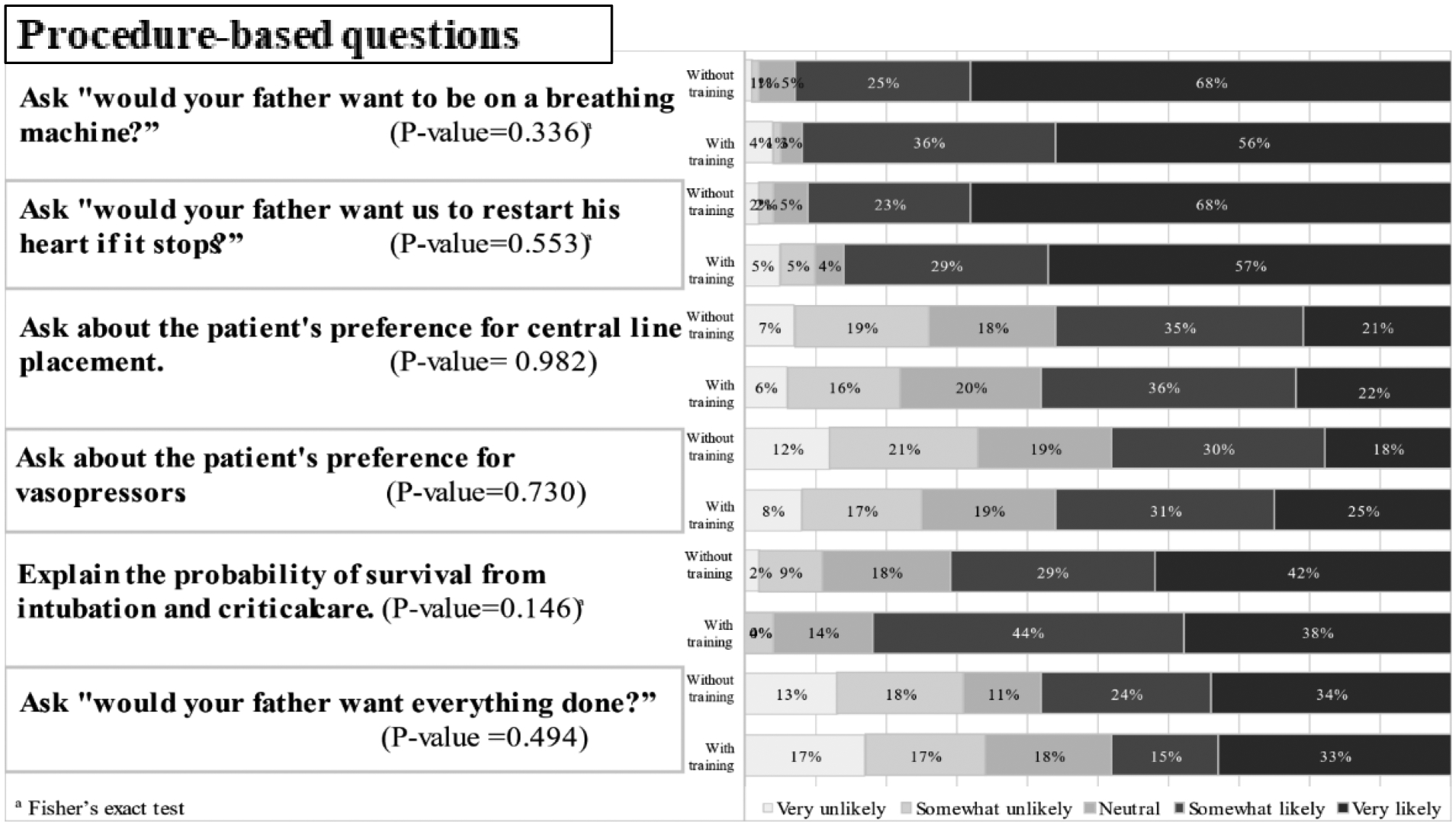
The procedure-based components of code status conversations among emergency clinicians with and without serious illness communication training.
On the other hand, most emergency clinicians did not report asking about value-based questions. Only a minority of participants reported “very likely” or “somewhat likely” to ask patient’s value-based questions in the two groups. Comparing between the two groups, statistically significant differences were observed in three out of seven patient’s value-based questions: “What would your father say would be most important to him if time were to be short?” (45% vs 19%, p-value = 0.005); “exploring the patient’s minimum quality of life that he would consider living” (47% vs 37%, p-value = 0.004); and “providing a recommendation to the patient or surrogate whether or not to intubate” (28% vs 20%, p-value = 0.033). No statistical differences were observed between the two groups in other value-based questions (e.g., ask “What is your understanding of your father’s illness?” 92% vs 82%, p-value = 0.161). The findings are depicted in Figure 2.
Figure 2.
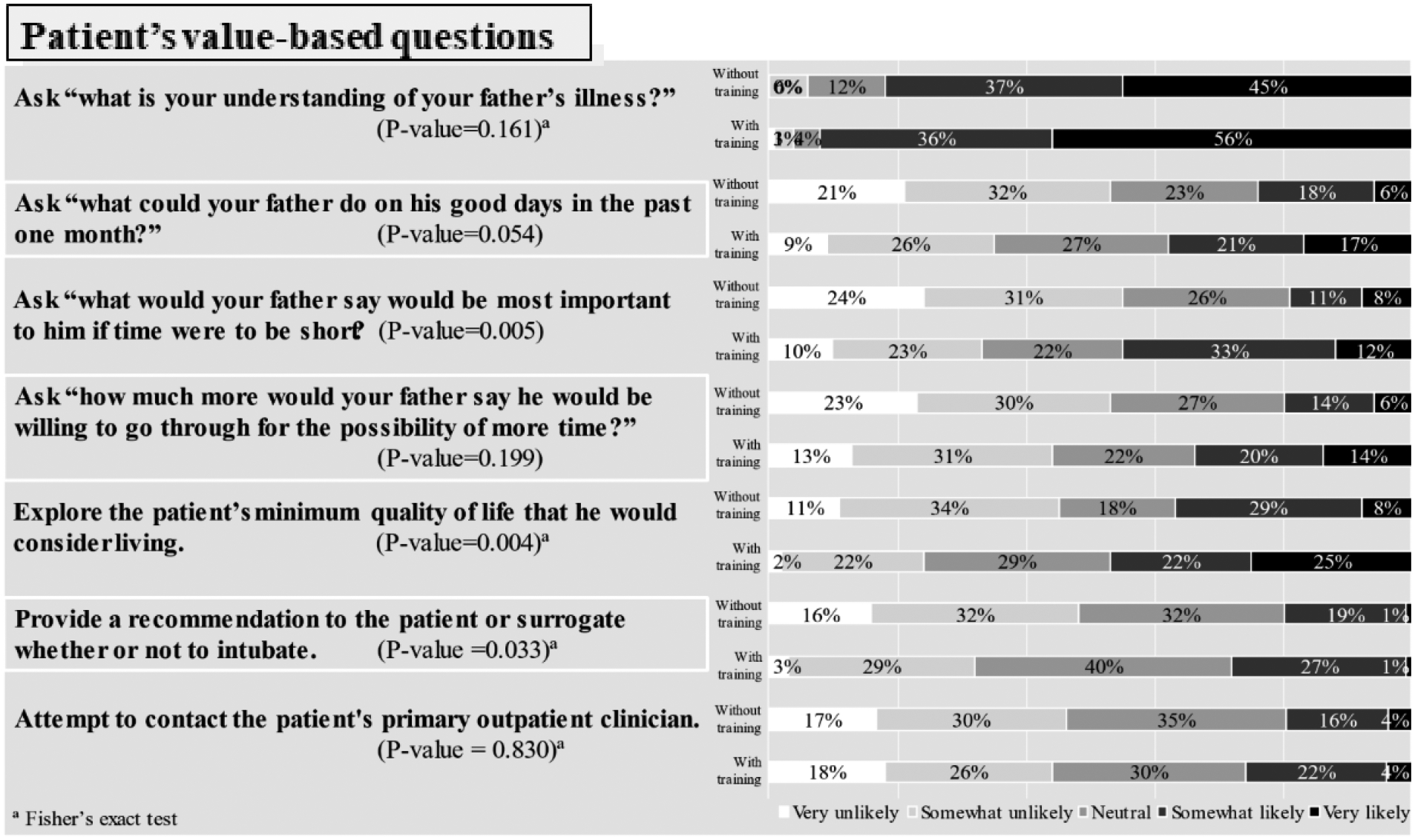
The patients’ value - based components of code status conversations among emergency clinicians with and without serious illness communication training.
The multivariable logistic regression analysis is summarized in Table 2. After adjusting for occupational role, years of clinical practice, previous training in palliative care, and frequency of code status conversations, the clinicians who underwent the serious illness communication training had higher odds of reporting four of the seven value-based questions: “what would your father say would be most important to him if time were to be short?” compared to clinicians who did not receive the training (adjusted OR = 4.34, 95%CI = 1.95–9.65, p-value < 0.001); “establishing the understanding of illness” (adjusted OR = 2.94, 95%CI = 1.04–8.35, p-value = 0.042); “exploring the patient’s willingness to go through invasive treatments for the possibility of more time” (adjusted OR = 2.54, 95%CI = 1.15–5.63, p-value = 0.021); and “asking about the baseline function of the patient” (adjusted OR = 2.14, 95%CI = 1.04–4.40, p-value = 0.040). After adjusting for the same covariates, no difference was observed in the six procedure-based questions between the two groups.
Table 2.
Association of serious illness communication training on clinician survey responses adjusted for occupational role, years of clinical practice, previous training in palliative care, and frequency of code status conversations.
| Survey questions | Association of Serious illness communication training | ||
|---|---|---|---|
| Adjusted Odds Ratio | 95% Confidence Interval | p-value | |
| Procedure-based questions | |||
| Ask “would your father want to be on a breathing machine?” | 1.24 | 0.36–4.28 | 0.739 |
| Ask “would your father want us to restart his heart if it stops?” | 0.99 | 0.36–2.78 | 0.991 |
| Ask about the patient’s preference for central line placement. | 1.11 | 0.58–2.15 | 0.746 |
| Ask about the patient’s preference for vasopressors. | 1.40 | 0.73–2.67 | 0.313 |
| Explain the probability of survival from intubation and critical care. | 1.68 | 0.77–3.67 | 0.191 |
| Ask “would your father want everything done?” | 0.71 | 0.37–1.36 | 0.300 |
| Patient’s value-based questions | |||
| Ask “what is your understanding of your father’s illness?” | 2.94 | 1.04–8.35 | 0.042 |
| Ask “what could your father do on his good days in the past one month?” | 2.14 | 1.04–4.40 | 0.040 |
| Ask “what would your father say would be most important to him if time were to be short?” | 4.34 | 1.95–9.65 | <0.001 |
| Ask “how much more would your father say he would be willing to go through for possibility of more time?” | 2.54 | 1.15–5.63 | 0.021 |
| Explore patient’s minimum quality of life that he would consider living. | 1.56 | 0.80–3.04 | 0.193 |
| Provide a recommendation to the patient or surrogate whether or not to intubate. | 1.38 | 0.60–3.15 | 0.451 |
| Attempt to contact the patient’s primary outpatient clinician | 1.51 | 0.69–3.34 | 0.305 |
Discussion
We compared the self-reported practice patterns of code status conversations by emergency clinicians with and without a recent attendance at an evidence-based, serious illness communication training. Most participants at both sites reported focusing on procedure-based questions. We found that clinicians who underwent the training had higher odds to report exploring value-based questions during code status conversations; four times higher odds to report exploring explore the patient’s life priorities; three times higher odds to report establishing an understanding of illness as well as explore the patient’s willingness to go through invasive treatments for the possibility of more time; and two times higher odds to report asking about the baseline function of the patient, compared to clinicians who did not receive the training. The findings suggest that evidence-based, serious illness communication training may influence how emergency clinicians practice code status conversations.
The findings are consistent with prior studies in other clinical settings.6,9,17,18 Prior studies have demonstrated that serious illness communication training improves clinicians’ confidence, rate, and quality of code status conversations.6,9,17,18 In outpatient oncology settings, clinicians who underwent serious illness communication training demonstrated two-fold increase in the value-based components of the code status conversations.18 Similar to our study, the increase in the value-based components of the code status conversations was also modest. Additionally, most clinicians focused on procedure-based components rather than patients’ value-based components of code status conversations.19 This phenomenon was reported among emergency clinicians in our study. Since many emergency clinicians do not receive serious illness communication training, our findings seem to reaffirm the current practice of many emergency clinicians.
Recently, experts in palliative care debated the value of advance care planning.20,21 Many advance preparation discussions have not shown a causal effect in reducing burdensome end-of-life care and predicting all possible scenarios of clinical deterioration deem difficult.21–23 Most of these experts still agree on the value of serious illness conversations and recommend focusing on preparing patients to be ready for crisis situations by helping them formulate and articulate their values and preferences.20–23 Code status conversations in the ED are the pinnacles of in-the-moment decision-making. A patient presenting to the ED who requires emergent decisions regarding code status or invasive procedures is a prime example of such a crisis situation. Not only does the clinically unstable patient necessitate emergency decision-making, but that decision-making can also have life-changing consequences.3 To align the intensity of care with patients’ goals towards the end of life, the clinicians have to help establish those goals from what can be understood about values/preferences.1 When a crisis occurs, the treating clinicians must solicit these goals, combine them with their medical expertise, and make a treatment recommendation in the face of vast clinical uncertainty. Our study demonstrates the currently established practice of emergency clinicians to focus on procedure-based questions. Given this finding, our results suggest combining the established practice of emergency clinicians (i.e., procedure-based approach) with value-based approach may yield the best care possible in emergency settings. The future approach for emergency clinicians may consider adding value-based components and facilitating decision-making aligned to patients’ goals. These further directions could include looking at similar questions asked by physicians not practicing emergency medicine as well as other members of the healthcare team such as nurses and social workers.
Several limitations exist in this study. First, our study recruited emergency clinicians from academic medical centers in the Northeast region of the U.S, given the large size of the clinical practices and the research topic of code status conversations. Our high response rate of participants suggests the internal validity of the results in our ED settings. The practice patterns of emergency clinicians in other settings might be similar yet unknown at this time. Empirical evidence is needed to verify this assumption in future studies. Second, we were unable to randomize the allocation of serious illness communication training. The causality of our findings cannot be established. Our findings were reported after three to six months of training, which may have increased the possibility of the suggested effect. We considered improving our quasi-experimental design by measuring the outcomes prior to the training. We decided against this approach due to the expected poor response rates. Third, our study did not explain why the training may modify the clinicians’ behavior in code status conversations or whether there were any barriers to implementing it. Fourth, the communication training group’s emergency clinicians had more prior palliative care training (Table 1), that might impact the reported practice pattern. Multiple logistic regression analysis was used to control for potential confounders, including prior palliative care training. Fifth, our results were based on what the clinicians reported as their practice patterns, which may differ from their actual practice when observed. Direct observation may be warranted in the future.
Conclusion
Most emergency clinicians reported asking about procedure-based questions, and some asked about patient’s value-based questions in code status conversations. Clinicians with recent an evidence-based, serious illness communication training may report asking more about patients’ values and priorities. The potential to improve serious illness communication for in-the-moment, shared decision-making must be explored further.
Supplementary Material
Key Message:
A cross-sectional survey study reported the self-reported practice patterns of code status conversations among emergency clinicians. Most emergency clinicians reported focusing on procedure-based questions. Existing evidence-based, serious illness communication training tailored to emergency practice may enable them to ask more patients’ value-based questions and potentially lead to more patient-centered care.
Funding source:
Dr. Ouchi is supported by National Institute on Aging (K76AG064434) and Cambia Health Foundation.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest: No conflict of interest to report from any of the authors.
References
- 1.Ouchi K, Lawton AJ, Bowman J, et al. Managing Code Status Conversations for Seriously Ill Older Adults in Respiratory Failure. Ann Emerg Med. 2020. Dec;76(6):751–756. doi: 10.1016/j.annemergmed.2020.05.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rubin BR, Chung M, Hasdianda MA, et al. Refinement of an Emergency Department-Based, Advance Care Planning Intervention for Nurses. J Palliat Med. 2022. Jan 31. doi: 10.1089/jpm.2021.0398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pajka SE, Hasdianda MA, George N, et al. Feasibility of a Brief Intervention to Facilitate Advance Care Planning Conversations for Patients with Life-Limiting Illness in the Emergency Department. J Palliat Med. 2021. Jan;24(1):31–39. doi: 10.1089/jpm.2020.0067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Loffredo AJ, Chan GK, Wang DH, et al. United States Best Practice Guidelines for Primary Palliative Care in the Emergency Department. Ann Emerg Med. 2021. Nov;78(5):658–669. doi: 10.1016/j.annemergmed.2021.05.021. [DOI] [PubMed] [Google Scholar]
- 5.Stone SC, Mohanty S, Grudzen CR, et al. Emergency medicine physicians’ perspectives of providing palliative care in an emergency department. J Palliat Med. 2011. Dec;14(12):1333–8. doi: 10.1089/jpm.2011.0106. [DOI] [PubMed] [Google Scholar]
- 6.Bowman JK, Aaronson EL, George NR, et al. Effect of Brief Educational Intervention on Emergency Medicine Resident Physicians’ Comfort with Goals-of-Care Conversations. J Palliat Med. 2018. Oct;21(10):1378–1379. doi: 10.1089/jpm.2018.0217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wright AA, Zhang B, Ray A, et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA. 2008. Oct 8;300(14):1665–73. doi: 10.1001/jama.300.14.1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ouchi K, Wu M, Medairos R, et al. Initiating palliative care consults for advanced dementia patients in the emergency department. J Palliat Med. 2014. Mar;17(3):346–50. doi: 10.1089/jpm.2013.0285. [DOI] [PubMed] [Google Scholar]
- 9.Back AL, Fromme EK, Meier DE. Training Clinicians with Communication Skills Needed to Match Medical Treatments to Patient Values. J Am Geriatr Soc. 2019. May;67(S2):S435–S441. doi: 10.1111/jgs.15709. [DOI] [PubMed] [Google Scholar]
- 10.Bernacki RE, Block SD; American College of Physicians High Value Care Task Force. Communication about serious illness care goals: a review and synthesis of best practices. JAMA Intern Med. 2014. Dec;174(12):1994–2003. doi: 10.1001/jamainternmed.2014.5271. [DOI] [PubMed] [Google Scholar]
- 11.Grudzen CR, Emlet LL, Kuntz J, et al. EM Talk: communication skills training for emergency medicine patients with serious illness. BMJ Support Palliat Care. 2016. Jun;6(2):219–24. doi: 10.1136/bmjspcare-2015-000993. [DOI] [PubMed] [Google Scholar]
- 12.Grudzen CR, Brody AA, Chung FR, et al. PRIM-ER Investigators. Primary Palliative Care for Emergency Medicine (PRIM-ER): Protocol for a Pragmatic, Cluster-Randomised, Stepped Wedge Design to Test the Effectiveness of Primary Palliative Care Education, Training and Technical Support for Emergency Medicine. BMJ Open. 2019. Jul 27;9(7):e030099. doi: 10.1136/bmjopen-2019-030099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gisondi MA, Lu DW, Yen M, et al. Adaptation of EPEC-EM Curriculum in a Residency with Asynchronous Learning. West J Emerg Med. 2010. Dec;11(5):491–9. [PMC free article] [PubMed] [Google Scholar]
- 14.Ito K, Uemura T, Yuasa M, et al. The Feasibility of Virtual VitalTalk Workshops in Japanese: Can Faculty Members in the US Effectively Teach Communication Skills Virtually to Learners in Japan? Am J Hosp Palliat Care. 2021. Sep 8:10499091211044477. doi: 10.1177/10499091211044477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap) – A metadata-driven methodology and workflow process for providing translational research informatics support, J Biomed Inform. 2009. Apr;42(2):377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: Building an international community of software partners, J Biomed Inform. 2019. May. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cubbison C, Rai A, Reid C, et al. Effect of Palliative Care Curriculum on Serious Illness Conversation Preparedness. ATS Sch. 2021. Sep 27;2(4):642–650. doi: 10.34197/ats-scholar.2021-0019IN. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Paladino J, Bernacki R, Neville BA, et al. Evaluating an Intervention to Improve Communication Between Oncology Clinicians and Patients With Life-Limiting Cancer: A Cluster Randomized Clinical Trial of the Serious Illness Care Program. JAMA Oncol. 2019. Jun 1;5(6):801–809. doi: 10.1001/jamaoncol.2019.0292. [DOI] [PubMed] [Google Scholar]
- 19.Anderson WG, Chase R, Pantilat SZ, et al. Code status discussions between attending hospitalist physicians and medical patients at hospital admission. J Gen Intern Med. 2011. Apr;26(4):359–66. doi: 10.1007/s11606-010-1568-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Curtis JR. Three Stories About the Value of Advance Care Planning. JAMA. 2021. Dec 7;326(21):2133–2134. doi: 10.1001/jama.2021.21075. [DOI] [PubMed] [Google Scholar]
- 21.Periyakoil VS, Gunten CFV, Arnold R, et al. Caught in a Loop with Advance Care Planning and Advance Directives: How to Move Forward? J Palliat Med. 2022. Mar;25(3):355–360. doi: 10.1089/jpm.2022.0016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jacobsen J, Bernacki R, Paladino J. Shifting to Serious Illness Communication. JAMA. 2022. Jan 25;327(4):321–322. doi: 10.1001/jama.2021.23695. [DOI] [PubMed] [Google Scholar]
- 23.Morrison RS, Meier DE, Arnold RM. What’s Wrong With Advance Care Planning? JAMA. 2021. Oct 26;326(16):1575–1576. doi: 10.1001/jama.2021.16430. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


