Abstract
Social determinants of health (SDoH) may impact outcomes in sickle cell disease (SCD). We conducted a comprehensive literature review of five electronic databases to elucidate the relationship between SDoH and SCD, and identify gaps in the literature. Our search yielded 59 articles which we organized into five SDoH areas: Neighborhood and Built Environment, Health and Healthcare, Social and Community Context, Education, and Economic Stability. We found that social determinants, such as access to healthcare, were inconsistently evaluated. Improved recognition and understanding of SDoH should enhance the development of programs that directly address its detrimental effects on patients with SCD.
Keywords: social determinants, healthcare access, healthy literacy, environment, quality of life
INTRODUCTION
Sickle cell disease (SCD) is an inherited blood disorder that affects approximately 100,000 individuals in the United States (U.S.) and occurs in an estimated 300,000 newborns annually worldwide.1–2 Patients with SCD suffer from numerous complications, including acute and chronic pain and end-organ dysfunction, that require rigorous clinical follow-up and intervention to prevent deterioration of health.3
Social determinants of health (SDoH) have been defined as “the conditions in the environment where people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks.”4 The World Health Organization5 identifies SDoH as a key factor in determining the health status of individuals with chronic complications. Research indicates that SDoH, such as inadequate housing, food insecurity, and limited access to affordable healthcare, shape the health behavior of patients with SCD6 similarly to their effects on other chronic conditions such as cancer7 and cystic fibrosis8.
In the US, SDoH affects overall health outcomes more than medical care.6 This difference is more evident in patients with SCD compared to the general population. Because SCD primarily affects individuals of African descent9 the burden of managing a chronic illness while experiencing racial disparities and other socioeconomic factors significantly influences health outcomes and quality of life.10
Given the nature of SCD and its serious health outcomes associated with a wide range of determining factors, there has been increased interest in the impact of SDoH on SCD. This scoping review aims to synthesize the current evidence from the literature and identify gaps in knowledge to guide further research that will improve understanding of the association between SCD and SDoH.
METHODS
This scoping review was conducted following the Arksey and O’Malley11 scoping review method. We utilized a comprehensive search strategy following the checklist provided by Preferred Reporting Items for Systematic Reviews and Meta-analyses Extension for Scoping Reviews (PRISMA-ScR)12 to identify the highest possible number of relevant articles and minimize publication bias.
Information Sources and Search Strategy
This literature review aimed to identify peer-reviewed journal articles that examined the association between SCD and SDoH. Sources of information included PubMed (pubmed.ncbi.nlm.nih.gov), SCOPUS (scopus.com), CINAHL (ebscohost.com), PsycINFO (ovid.com) and Web of Science (webofknowledge.com). Unpublished manuscripts, reports, and evaluations were not searched for this review. A biomedical librarian assisted with the primary search and provided expertise in developing Boolean search in PubMed. Search terms were selected by consensus and used in various combinations to develop robust search results and ensure that all relevant articles were included. The authors reviewed the primary results from PubMed before search terms were entered into other databases.
Search terms were selected based on five SDoH areas from Healthy People 20204: (a) Neighborhood and Built Environment; (b) Health and Healthcare; (c) Social and Community Context (d) Education; (e) Economic Stability. Search terms included: cognitive functioning, health literacy, unemployment, disability, food desert, food insecurity, neighborhood economic distress, poverty, stigma, health inequity, discrimination, home environment, access to healthcare, temperature, air pollution, tobacco smoke, incarceration, quality of life, insurance, and transportation. These keywords were combined with the terms “sickle cell disease” and “hemoglobinopathies” to search for relevant articles.
Eligibility criteria
Eligible articles: 1) included individuals with SCD (any genotype) or patient-caregiver dyads, 2) were original research articles published in English between 1975 (based on the publication of the first article that addressed SDoH in SCD) and 2020, and 3) evaluated the association between SDoH and SCD health outcomes. Abstracts without a corresponding manuscript, review articles, book chapters, and case reports were excluded.
Data Selection and Extraction
Two reviewers independently conducted the literature search (HK, MK) and screened all titles and abstracts of studies to determine eligibility. Citation management and duplicate results were removed using EndNote (Clarivate Analytics). Reviewers (HK, MK) retrieved the full text of relevant articles. Disagreements regarding study eligibility were resolved through discussion among all reviewers (HK, MK, JP, WW) during biweekly meetings until a consensus was reached. Covidence (Covidence.org), a web-based platform that streamlines the production of systematic and scoping reviews, was used to supplement the review process. The reasons for excluding full-text articles are indicated in the PRISMA flowchart (Fig. 1).
Figure 1:
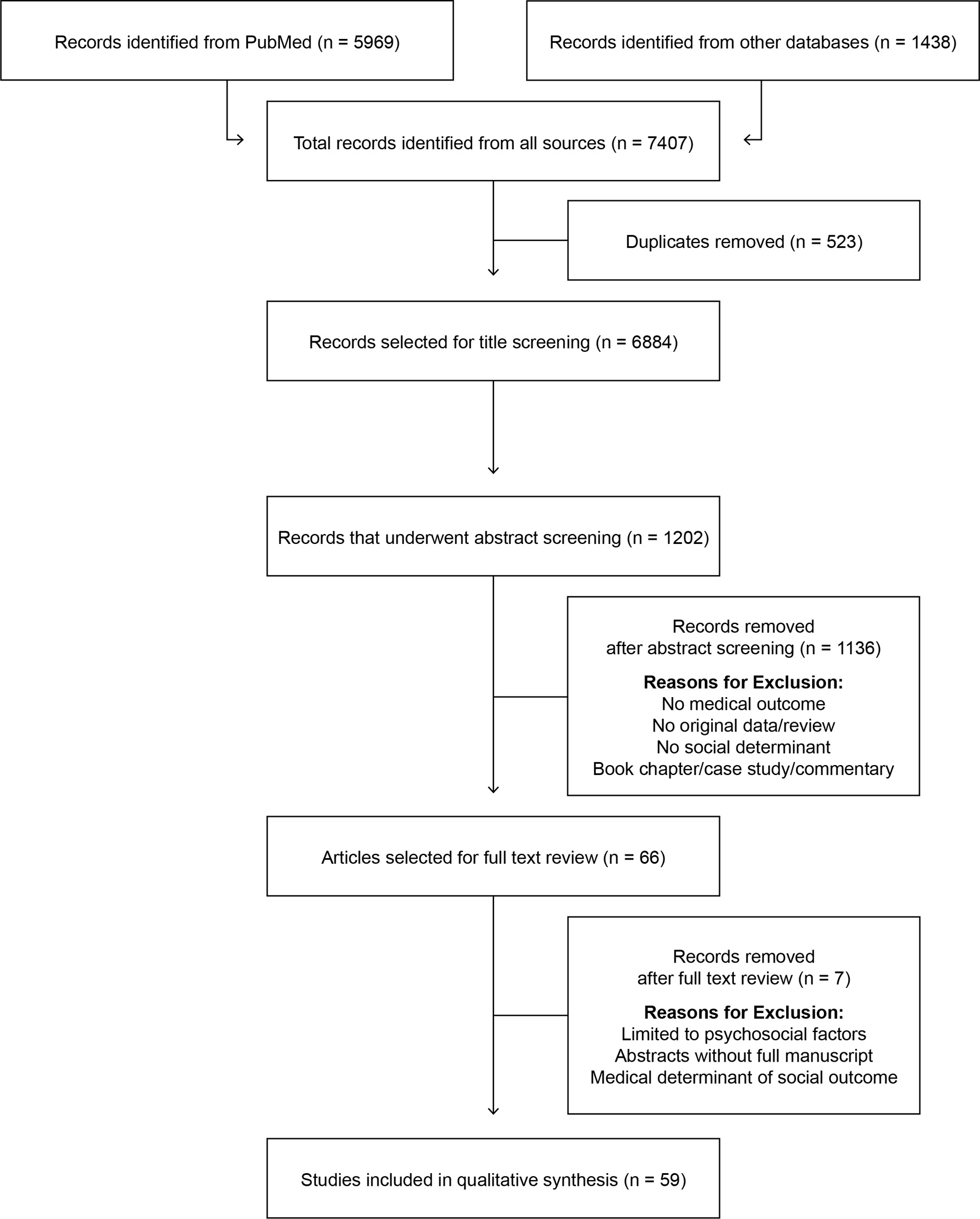
PRISMA Flow Diagram for the Search of SCD and SDoH Literature
Data Charting and Synthesis
Reviewers (HK, MK) independently performed data charting of articles included in the final full-text review. The following study characteristics were identified: author and year, research design, population, geographic region, SDoH variable, and study results. Studies were categorized by the SDoH areas in Healthy People 2020.4 Narrative overviews of full-text review findings were organized in tabular summaries of extracted data (Tables 1–5).
TABLE 1.
Neighborhood and Built Environment Articles Included in Review
| Author (Year) | Research Design | Study Population | SDoH Variables | Results |
|---|---|---|---|---|
| Blumberg (2020) | Observational | 77310 ED visits (US) | Air pollution (CO, NO2, SO2, O3) | Urban air pollution (traffic pollutant) triggered ACU |
| Wachnian (2020) | Retrospective | 118 children (Canada) | Temperature fluctuation | Large temperature changes triggered VOC |
| Parriault (2019) | Retrospective | 384 children/adults (French Guiana) | Meteorological data (weather, influenza) | Temperature/humidity decreased VOC. Flu affected pain severity |
| Barbosa (2015) | Case-Crossover | 3180 adolescents (Brazil) | Air pollution (CO, NO2, SO2, O3) | Ambient air pollution triggered VOC |
| Cohen (2013) | Cross-sectional | 252 children (US/UK) | Tobacco Exposure | Tobacco exposure increased respiratory problems |
| Mittal (2009) | Prospective | 93 children (UK) | Air pollution (PM, NO NO2) | Air pollution predicted more stroke related complications in SCD |
| Nolan (2008) | Case-Crossover | 813 children/adults (US) | Meteorological data (climate, wind speed) | Males with SCD had more VOC events due to wind speed in warm climate |
| Yallop (2007) | Retrospective | 1413 children/adults (UK) | Air pollution (NO, CO, O3, SO2) | Air quality affected VOC and increased hospitalizations |
| Jones (2005) | Observational | 1413 children/adults (UK) | Meteorological data (temperature) | Climate changes affected skin temperature that increased VOC |
| West (2003) | Retrospective | 52 children (US) | Tobacco exposure | Tobacco smoke increased SCD crises |
| Redwood (1976) | Retrospective | 161 children/adults (Jamaica) | Meteorological data (temperature, rainfall) | Low temperature increased hospitalizations for VOC in patients with SCD |
SCD = Sickle Cell Disease, VOC = Vaso-occlusive crisis, ACU = Acute care Utilization, US = United States, UK = United Kingdom
TABLE 5.
Economic Stability Articles Included in Review
| Author (Year) | Research Design | Study Population | SDoH Variables | Results |
|---|---|---|---|---|
| Employment | ||||
| Williams (2018) | Prospective descriptive | 95 adults (US) | Employment, SBF | Employment/stable home related to low acute care encounters |
| Sanger (2016) | Retrospective | 50 adults (US) | Unemployment | Low education related to more frequent VOC and unemployment |
| Food Insecurity | ||||
| Ghafuri (2020) | Cross-sectional | Children (US) | Food insecurity | Patients with pain/ACS were more food insecure |
| Adegoke (2017) | Comparative | Children (Brazil, Nigeria) | Nutrition status, access to care | Under-nutrition was prevalent in patients with SCD |
| Mandese (2016) | Observational | Children (Italy) | Nutrition Intake, impaired growth | Inadequate nutrition affected SCD severity |
| Low-Income/Poverty | ||||
| Bello-Manga (2020) | Cross-sectional | 941 Children (Nigeria) | SES, poverty, hospital cost | Severe anemia associated with more children in each room per house |
| Kumar (2020) | Retrospective | National record of readmission (US) | Education level, Poverty | Low SES/admission at high volume centers predicted more readmissions |
| Aljuburi (2013) | Retrospective | National hospital record (England) | Healthcare expenditure | Living in socio-economically deprived areas increased risk of readmission |
| Glassberg (2012) | Retrospective | 985 children (US, Canada, UK, France) | Family Income | Low-income increased ED use for SCD pain |
| Panepinto (2009) | Cross-sectional | 178 children (US) | SES | Low family income related to more ED readmissions and worse HRQL |
| Raphael (2009) | Retrospective | Children (US) | Low income | Patients with SCD with low income have more acute care encounters |
SBF = Socio-behavioral factors, SCD = Sickle Cell Disease, ACS = Acute Chest Syndrome, SES = Socio-economic Status, HRQL = Health related quality of life, US = United States, UK = United Kingdom, ED = Emergency Department
RESULTS
Study selection
The PRISMA flow diagram is shown in Fig 1. A total of 1202 references identified through the literature review underwent abstract screening. Following the screening, 66 articles were included in the full-text review. References that did not meet the eligibility criteria were removed, including seven studies that described medical determinants of social outcomes instead of SDoH, leaving 59 articles for narrative synthesis.
Characteristics of Reviewed Articles
Tables 1–5 summarize the articles included. Studies were published recently, 73% since 2010 (Supplemental Fig S1). Most of the studies were primarily based in the United States (n = 43; 68%) and the remaining were conducted in the United Kingdom (n = 6), Nigeria (n = 4), Brazil (n = 3), Canada (n = 2), France (n = 2), Italy (n = 1), Saudi Arabia (n = 1), and Jamaica (n = 1) (Supplemental Fig S2). Study designs were primarily retrospective or cross-sectional. Approximately half of the studies were pediatric (n = 30, 51%) and the rest included adults only (n = 16), patient-caregiver dyads (n = 11) or both children and adults (using demographic data from national hospital databases) (n = 2).
Social Determinants of Health and Sickle Cell Disease
Neighborhood and Built Environment (Table 1)
Eleven studies assessed the effects of environmental factors on disease-related complications in patients with SCD. The population samples included both children and adults. The studies investigated outcomes associated with climate change, temperature fluctuation, air pollution, and tobacco exposure.
Patients’ environments were often detrimental to health outcomes by increasing respiratory symptoms and VOC, contributing to increased acute care utilization. High wind speed and low humidity were associated with changes in skin temperature and increased frequency of painful episodes.13–15 Large temperature changes and seasonal viral infections such as influenza, contributed to VOC.13,16,17 A study conducted in Brazil16 found that polluted air in the environment posed a significant threat to children with SCD. Air pollution caused by dust or pollen particles, and poisonous gases from car and truck exhaust (carbon monoxide, nitric acid, and ozone) was associated with frequent pain episodes.19–21 Tobacco smoke exposure increased respiratory problems leading to recurrent hospitalizations.22,23
Health and Healthcare (Table 2)
TABLE 2.
Health and Healthcare Articles Included in Review
| Author (Year) | Research Design | Study Population | SDoH Variables | Results |
|---|---|---|---|---|
| Access to Healthcare | ||||
| Kayle (2020) | Retrospective | 3635 adults (US) | Insurance type | Medicaid expansion did not improve enrollment or ACU |
| Carroll (2018) | Prospective | 73 adults (US) | SES, ACU | SES and pain-related anxiety increased ACU in patients with SCD |
| Brodsky (2017) | Retrospective | 88 adults (US) | PCP, insurance type, ACU | Absence of PCP and ACU frequency increased 30-day readmission |
| Jacob (2016) | Cross-sectional | 38 adults (US) | Barriers to care | Parents of patients with SCD reported more barriers to care due to the gap in primary care |
| Smeltzer (2016) | Prospective observational | 545 children (US) | Distance to CSCC | Greater distance to CSCC decreased hospital admissions |
| Liem (2014) | Cross-sectional | 200 adults (US) | Primary care access, barriers to ACU, PCP | More access to PCP associated with less ED visits |
| Boulet (2010) | Probability sample survey | 19427 children (US) | Barriers to healthcare access | Patients with SCD reported delay in accessing care and worse health outcomes |
| Raphael (2009) | Cross-sectional | 296949 children (US) | Medicaid coverage, gaps in insurance | Low-income children with SCD had more ACU and higher expenses |
| Shankar (2008) | Cross-sectional | 1214 children (US) | Distance to CSCC | Neighborhoods with CSCC facilities observed less outpatient visits & more hospitalizations |
| Haque (2000) | Cross-sectional | 1189 adults/children (US) | Socioeconomic disparity, rural/urban access | Rural patients had low SES/more barriers to SCD clinic; urban patients had more medical issues |
| Hand (1995) | Retrospective | 172 Adolescents/Adults (US) | Insurance type, Primary /Specialty care use | Stable insurance (Medicare) and primary care did not affect ACU for patients with SCD |
| Health Literacy | ||||
| Carden (2016) | Cross-sectional | 142 adults (US) | Health literacy, disease knowledge | Lack of disease specific knowledge increased ED visits |
| Cronin (2019) | Cross-sectional | 530 adults (US) | Financial insecurity, social support, health literacy | Missed clinic visits due to financial problems increased hospitalizations/readmissions |
| Morrison (2018) | Cross-sectional | 100 adults (US) | Health literacy, pain treatment skills | Children of parents who underdosed pain medicine had more ED visits for pain |
SES = Socioeconomic status, SCD = Sickle Cell Disease, ED = Emergency Department, ACU = Acute Care Utilization, PCP = Primary Care Provider, CSCC = Comprehensive Sickle Cell Center, US = United States
Fifteen studies investigated the impact of poor access to healthcare and low health literacy. All these studies were conducted in the US, and included children and adults.
Access to Healthcare
SCD patients were more likely to experience delays in getting healthcare because of their race and/or because they lived in rural areas without a sound transportation system. 24,25 Both factors contributed to worsening health outcomes. Greater distance from sickle cell centers and absence of primary care increased the risk of hospitalization and 30-day readmission for patients with SCD, particularly children, compared to patients with other chronic conditions.26–28 A few studies reported that the rate of visits to non-sickle cell clinics decreased in the regions with the availability of a comprehensive sickle cell center close to patients’ homes.29,30 Socioeconomic status played a significant role in determining access to healthcare. Lower-income patients paid higher healthcare costs and utilized emergency services more often due to a lack of stable insurance and/or primary care.31–34
Health Literacy
Health literacy, defined as “the degree to which individuals can obtain, process, and understand basic health information needed to make appropriate health decisions,”35 was critical in determining disease-related outcomes for patients with SCD. Disease-specific knowledge plays a significant role in improving pain management, medication dosing, and healthcare services.36,37 Increased SCD-specific literacy was associated with greater outpatient visits among adults with SCD.38 Children of caregivers who did not have disease-specific knowledge or were financially insecure frequently missed scheduled clinical evaluations, which contributed to increased ED visits and hospitalizations for pain.36–39
Social and Community Context (Table 3)
TABLE 3.
Social and Community Context Articles Included in Review
| Author (Year) | Research Design | Study Population | SDoH Variables | Results |
|---|---|---|---|---|
| Discrimination | ||||
| Bediako (2016) | Prospective | 262 Adolescents/Adults (US) | Self-reported Stigma | Stigma affected disease severity/acute care utilization |
| Haywood (2014) | Cross-sectional | 291 Adolescents/Adults (US) | Demographic, health status, pain burden | Perceived discrimination associated with higher pain severity |
| Martin (2018) | Cross-sectional | 92 Adolescents (US) | SCD-related stigma, social support, QOL | More stigma increased SCD pain/hospital admissions and decreased quality of life |
| Stanton (2010) | Retrospective | 49 Adults (US) | Discrimination, trait optimism | Patients with SCD with more discrimination/trait optimism had greater acute care encounters |
| Social Cohesion | ||||
| Mitchel (2007) | Mixed methods | 53 Adults (US) | Coping strategies, family functioning | Positive coping & better family functioning was related to low health care utilization. |
| Psihogios (2018) | Cross-sectional | 83 Adults (US) | HRQL, family efficacy | Family efficacy/less parental stress improved SCD self-management and HRQL |
| Quality of Life | ||||
| Power-Hays (2020) | Prospective | 200 Children (US) | SDoH, HRQL | Patients with SCD face more SE hardships. Universal screening for SDoH needed |
| Mougianis (2020) | Cross-sectional | 71 Adolescent (US) | Racism, HRQL | Racism predicted more depressive symptoms |
| Kayle (2020) | Retrospective | 3635 Adults (US) | Insurance | Medicaid expansion did not improve acute care utilization |
| Cortright (2020) | Retrospective | 126 Children (US) | SDoH, QOL | Patients with SCD with high social disadvantages had more acute care encounters |
| Oliveira (2019) | Cross-sectional | 4956 Children (Brazil) | QOL | QOL varied with health centers when adjusted for sociodemographic |
| Cronin (2019) | Cross-sectional | 531 Adults (US) | Ambulatory care cost, QOL | Sociodemographic predicted rate of hospital admissions/readmissions |
| Robinson (2014) | Prospective | 55 Children (US) | Insurance, QOL | Insurance type affected disease-related complications and QOL |
| Bundy (2012) | Retrospective | 851 Children (US) | Financial status, QOL | Medicaid-insured children with SCD connected better with generalists than hematologists |
| Amr (2011) | Retrospective | 285 Adolescents (Saudi Arabia) | Sociodemographic, HRQL | SCD complications and sociodemographic correlates had poor impact on HRQL |
| Panepinto (2009) | Cross-sectional | 104 Children (US) | HRQL | Family income poorly affected HRQL |
| Palermo (2008) | Retrospective | 56 Children (US) | Family Income, HRQOL | SES and neighborhood economic distress predicted pain outcomes |
| Hand (1995) | Retrospective | 172 Adolescents/Adults (US) | Socio-economic distress, QOL | Stable insurance (Medicare) and primary care did not affect ACU |
SCD = Sickle Cell Disease, QOL = Quality of Life, HRQL = Health related quality of life, ED = Emergency Department, SDoH = Social determinants of health, ACU = Acute Care Utilization, US = United States, SE = Socioeconomic status
Eighteen articles focused on understanding the impact of disease-related stigma, social support, and health-related quality of life (HRQoL) of patients with SCD, including both adults and children.
Discrimination
Self-reported stigma and perceived discrimination correlated with more interference from pain in the lives of individuals with SCD, and resulted in more hospital admissions and ED visits. 40,41 Patients who suffered from disease-related stigma were more likely to have an increased length of hospital stay due to the severity of their pain which lowered their HRQoL. 42,43
Social Cohesion
Social support and good family functioning were associated with increased self-management and HRQoL. Positive coping strategies, family support, and reduced parenting stress were correlated with decreased healthcare utilization.44 In contrast, patients’ family dynamics, such as lack of communication and mutual respect, diminished problem-solving ability and passive parental coping, resulted in poor SCD self-management and increased pain events.45
Quality of Life
Patients with SCD with poor physical strength, more bodily pain and deteriorating emotional well-being often faced worse HRQoL, irrespective of gender, increasing age or family income.10,46 Socioeconomic status and neighborhood economic distress predicted patients’ functional outcomes and rate of hospital readmissions related to SCD pain. This pain contributed to impaired HRQoL for patients with SCD compared to patients without SCD but with similar financial status.39,47–49 The studies conducted in Brazil and Saudi Arabia found that HRQoL of patients with SCD varied according to the health center where they received care.50,51 At centers where health professionals received additional training in managing SCD, patients experienced reduced disease anxiety, fewer hospitalizations, and improved quality of life due to better disease management as compared to the health centers where patients were not cared for by providers with SCD expertise.50–52 Additionally, their insurance type determined at which center they would receive care and thus impacted disease outcomes.32,33,53
Education (Table 4)
TABLE 4.
Education Articles Included in Review
| Author (Year) | Research Design | Study Population | SDoH Variables | Results |
|---|---|---|---|---|
| Bello-Manga (2020) | Cross-sectional | 941 children (Nigeria) | Education level of a household | Severe anemia associated with low education of a household |
| Bills (2020) | Comparative | 70 children (US) | SES, cognitive/behavioral function | Parent/family functioning was independent of SES |
| Fields (2016) | Single prospective cohort | 43 children (US) | Home environment, SES, parental education | Home environment predicted cognitive development |
| Jonassaint (2016) | Retrospective | 258 adults (US) | Education attainment | Low education completion associated with ED care |
| Oluwole (2016) | Cross-sectional | 56 Children (Nigeria) | Sociodemographic, cognitive functioning | Sociodemographic factors correlated with cognitive impairment |
SES = Socioeconomic Status, ED = Emergency Department, US = United States
Five articles in this category highlighted the associations between low educational attainment, socioenvironmental risk, cognitive impairment, and parental education. The study populations included both children and adults.
A few studies conducted in the US and Nigeria examined the effects of sociodemographic factors, parental education, and family functioning in children with SCD.52–55 In Nigeria, socioeconomic factors, number of individuals living per room in a house, social support, and educational level of the head of the household determined the severity of anemia in children with SCD who lived in a low-resource setting.54,55 A few other studies conducted in the US found that the home environment and family functioning were significantly associated with cognitive development and HRQoL in children with SCD.56,57 In the US, adult patients with SCD who did not achieve higher education experienced a greater rate of ED utilization and were often unemployed compared to their peers who completed post-high school education.58
Economic Stability (Table 5)
Eleven studies documented the effects of unemployment, food insecurity, low income, poverty, and housing instability that altered disease-related outcomes. These studies were conducted in regions of the US and Nigeria, and included adults and children.
Unemployment
Patients with SCD who lacked general cognitive ability, memory, and executive functioning were more likely to be unemployed when compared to their peers who attained higher education.59 Employed patients had less severe pain episodes, did not utilize the ED as much, and had more disease-management knowledge and social support.59 Unemployed patients suffered from significantly greater pain-related disruption in their lives along with other health-related problems that increased the use of opioids and created more difficulty in obtaining employment. Alternatively, employment status may not only be related to poor health.60 Behavioral and social factors such as poor interpersonal relationships with management and other employees, low self-esteem, or lack of job skills due to cognitive deficits and irregular school attendance may also result in unemployment.60
Food Insecurity
Inadequate nutritional intake, access to fresh produce, and impaired growth were other factors that contributed to poor health outcomes. The households of individuals with SCD suffered from greater food insecurity compared to the national US average.61 A study conducted in Brazil and Nigeria found that patients with SCD often lived in poor neighborhoods that lacked access to full-scale grocery stores and could not afford higher healthcare costs due to financial insecurity.62 Some studies speculated that lack of enough nutrients was associated with frequent episodes of VOC and increased acute care utilization.62,63
Low Income and Poverty
The most readmissions and highest inpatient mortality occurred in patients living in the most socioeconomically deprived areas.64 Recurrent acute health care utilization contributed to a significant burden on healthcare resources and diminished HRQoL of patients with SCD.65 A study conducted in Nigeria reported that the number of residents in a household determined the likelihood of severe disease.54 Regardless of distance to the nearest hospital or access to healthcare, living below the federal poverty threshold increased ED utilization.66 Low-income children with SCD and neurobehavioral co-morbidities were more likely to have higher healthcare utilization due to frequent pain when compared to children with similar sociodemographic characteristics.33,48
Housing Instability
No eligible articles were found in this category.
DISCUSSION
Given the magnitude of social and clinical barriers faced by patients with SCD, a comprehensive understanding of the impact of social determinants of health outcomes is essential to develop specific interventions to maximize the health of this vulnerable population.67 The current scoping review focuses on evaluating and synthesizing the published literature on SCD and SDoH. We found a lack of specificity and in-depth reporting of barriers associated with SCD and SDoH in the literature that warrant further research.
Most studies addressing SDoH in SCD have been published in the US in the last decade, highlighting recent interest and increased attention to the impact of SDoH in SCD.67 Our review found that SDoH categories such as neighborhood and built environment, access to healthcare, economic stability, and quality of life, have been explored more than other social determinants, such as education, unemployment, food insecurity, discrimination, and social cohesion. Other factors, such as housing instability, have not been discussed, indicating that significant gaps exist within SDoH literature, and further exploration is necessary.
Most studies highlight sociodemographic, economic, and environmental factors as the fundamental social risk factors leading to most health problems. In particular, the effects of SCD complications on quality of life 47,48,50,51 have been addressed in depth. However, factors such as the impact of health literacy,36–39 race,40–43 area of residence,64 and level and location of care received26–30 have hardly been explored, if at all. Furthermore, understanding psychosocial needs such as family functioning is equally important to maximize health benefits of patients with SCD.
Many studies identified during the literature review were limited to children and caregivers and lacked longitudinal analyses to study the impact of SDoH over time. Studies with children often compared patients with SCD to their healthy peers or children with other chronic complications to highlight the increased odds of experiencing worse HRQoL in patients with SCD.44–51 Research with caregivers focused on improving their health literacy through continuous education on disease-specific knowledge (such as medication dosing or navigating the healthcare system) to increase the caregivers’ ability to make appropriately informed decisions for their child’s health. 36–39 A few studies explored the impact of SDoH outcomes in adults with SCD highlighting the educational gaps and low socioeconomic status that can lead to unemployment.58–60 As patients become older, managing a lifelong chronic illness while keeping a stable and continuous source of income, and balancing the need to take care of sick family members is challenging. Therefore, researchers should emphasize studying the long-term effects of SDoH to promote the development of comprehensive care plans that are applied longitudinally to the patients’ treatment course.
African American/Black patients with SCD, and patients who belong to ethnic minority groups experience more delays in care than non-African American/Black patients.40–43 Despite being recognized as one of the most important social determinants in SCD, the association between discrimination, disease-related stigma, and healthcare utilization in SCD has been understudied. A few studies have reported that perceived discrimination in healthcare systems may be a significant risk factor in chronic diseases, and lead to racial and ethnic disparities.41,43 Negative experiences at a healthcare facility, and lack of trust between a patient and a provider reduce the likelihood of patients adhering to physicians’ recommendations, increase the frequency of pain episodes among patients with SCD, and affect the overall health and quality of life.40–43 There is a need to develop programs that address the type and frequency of discrimination in the healthcare system and examine the prevalence of stigma associated with SCD.69 Increased understanding and support of emotional health may build trust among patients and medical professionals, reduce disease severity and hospitalizations, and lead to a better quality of life.40–43
The current healthcare system emphasizes lifestyle changes and counseling as essential strategies for preventing disease-related complications in patients with SCD. However, these interventions may not fully address the social and clinical barriers associated with the disease, such as health disparities. 68 In addition, despite receiving standardized care in the hospital setting, patients will return to their homes and pre-existing multifactorial environmental stressors such as poverty and food insecurity that contributed to the initial hospitalization; therefore, standard medical treatment benefits will remain not fully realized.65,66 Because each impacts the other, it is essential to consider patients as the sum of their environment and medical condition.
Considering our findings as well as the current guidelines provided by professional societies, such as The National Academies of Sciences, Engineering, and Medicine (NASEM)70 and The American Society of Hematology (ASH),71 SDoH should be integrated into healthcare delivery and treatment decisions of patients with SCD. Three interventions are especially relevant to achieve this: (1) providing ongoing cultural competency training for healthcare professionals to improve health outcomes and increase mutual understanding among patients and providers; (2) ensuring that the design of clinical trials reflects cultural diversity, allowing the medical community to assess the effectiveness of similar therapies among different populations; and (3) supporting programs that allow individuals from minority backgrounds to become a part of the healthcare workforce to improve the quality of healthcare for minority populations.70,71 Finally, a broader understanding of the disease from a global health perspective, and interventions such as a universal screening and referral program for SDoH are needed to improve clinical outcomes and HRQoL for patients with SCD.10 Collaboration among medical institutions from resource-rich and low-resource countries will help to improve the research infrastructure, transference of knowledge among providers will lead to a better understanding of the disease, and sharing resources such as disease-modifying therapies for SCD will maximize health benefits and improve the quality of life of patients with SCD.
LIMITATIONS
Some potential methodological limitations of our scoping review are worth mentioning. Although the current scoping review reported findings following PRISMA guidelines and included a diverse set of inclusion criteria to assess the association of social determinants with SCD comprehensively, we may have missed some relevant articles and unpublished studies in the “gray” literature. We only included the studies published in peer-reviewed journals to focus on the most robust available evidence in the literature, so potential publication bias could not be excluded. Additionally, studies had small sample sizes, were primarily cross-sectional, and lacked a global perspective, which limited our interpretation of the findings. Furthermore, some SDoH areas, such as housing instability, were not represented at all, highlighting the need for further elucidation of the impact of SDoH on outcomes for SCD.
CONCLUSIONS
External pressures such as pandemics, economic instability, and societal unrest have highlighted the relationship between SDoH, healthcare utilization, and health outcomes in historically marginalized communities. The traditional healthcare system emphasizes biomedical problems as the primary cause of poor health outcomes and often overlooks social risk factors that increase the frequency of hospitalizations, morbidity, and mortality.67 The evidence from our literature review shows that SDoH may play a prominent role in access to care and success of treatment of patients with SCD. SDoH should be considered when designing randomized clinical trials, perhaps by including the impact of selected social factors when stratifying patients at randomization and/or considering them as endpoints of the study. A more comprehensive understanding of the association between SCD and SDoH will help better position researchers to design new patient-centered interventions that could improve health equity and health literacy, open doors for better healthcare, and reduce negative impacts of SDoH in SCD.
Supplementary Material
Supplemental Figure S1: Year of Publication of Articles
Y-axis shows the total number of articles included in the study and x-axis shows the distribution of articles by publication in 5-year intervals.
Supplemental Figure S2: Distribution of Articles by Country of Origin
*Some studies were conducted in multiple countries.
ACKNOWLEDGEMENTS
The authors would like to acknowledge Julie Edrington, MSLS, for her contributions to this work. JSP received funding from NIH, NHLBI K01 HL125495 during the conduct of this project. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Abbreviations
- ASH
American Society of Hematology
- E.D.
Emergency Department
- HRQoL
Health Related Quality of Life
- NASEM
National Academies of Sciences, Engineering, and Medicine
- PRISMA-ScR
Preferred Reporting Items for Systematic Reviews and Meta-analyses Extension for Scoping Reviews
- SCD
Sickle Cell Disease
- SDoH
Social Determinants of Health
- U.S.
United States of America
- VOC
Vaso-Occlusive Crisis
Footnotes
CONFLICT OF INTEREST DISCLOSURES
JSH is a consultant for Global Blood Therapeutics and Forma Therapeutics.
JSP is a consultant for Forma Therapeutics.
REFERENCES
- 1.Hassell KL. Population estimates of sickle cell disease in the U.S. Am J Prev Med. 2010;38(4 Suppl): S512–S521. doi: 10.1016/j.amepre.2009.12.022 [DOI] [PubMed] [Google Scholar]
- 2.Piel FB, Hay SI, Gupta S, Weatherall DJ, Williams TN. Global burden of sickle cell anaemia in children under five, 2010–2050: modelling based on demographics, excess mortality, and interventions. PLoS Med. 2013;10(7): e1001484. doi: 10.1371/journal.pmed.1001484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pecker LH, Lanzkron S. Sickle Cell Disease. Ann Intern Med. 2021;174(1): ITC1–ITC16. doi: 10.7326/AITC202101190 [DOI] [PubMed] [Google Scholar]
- 4.Social determinants of health. Social Determinants of Health | Healthy People 2020. https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-of-health. Accessed July 26, 2021.
- 5.Social determinants of health. World Health Organization. https://www.who.int/health-topics/social-determinants-of-health#tab=tab_1. Accessed July 26, 2021. [Google Scholar]
- 6.Artiga S, Hinton E. Beyond health care: the role of social determinants in promoting health and health equity. KFF. https://www.kff.org/disparities-policy/issue-brief/beyond-health-care-the-role-of-social-determinants-in-promoting-health-and-health-equity/ Accessed July 26, 2021. [Google Scholar]
- 7.Venkataramany Barat S.*; Sutton Jeffrey M.†. Social Determinants of Health in Oncology: Towards a More Personalized and Equitable Delivery of Cancer Care. American Journal of Clinical Oncology. 2022;45(6):273–278 doi: 10.1097/COC.0000000000000914 [DOI] [PubMed] [Google Scholar]
- 8.Bahr NC, Song J. The Effect of Structural Violence on Patients with Sickle Cell Disease. J Health Care Poor Underserved. 2015;26(3):648–661. doi: 10.1353/hpu.2015.0094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Modell B, Darlison M. Global epidemiology of haemoglobin disorders and derived service indicators. Bull World Health Organ. 2008;86(6):480–487. doi: 10.2471/blt.06.036673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Power-Hays A, Li S, Mensah A, Sobota A. Universal screening for social determinants of health in pediatric sickle cell disease: A quality-improvement initiative. Pediatr Blood Cancer. 2020;67(1): e28006. doi: 10.1002/pbc.28006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Arksey H, O’Malley L. Scoping studies: Towards a methodological framework. Intl J of Soc Res Meth. 2005;8(1):19–32. doi: 10.1080/1364557032000119616 [DOI] [Google Scholar]
- 12.Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, Moher D, Peters MD, Horsley T, Weeks L, Hempel S et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018,169(7):467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 13.Jones S, Duncan ER, Thomas N, et al. Windy weather, and low humidity are associated with an increased number of hospital admissions for acute pain and sickle cell disease in an urban environment with a maritime temperate climate. Br J Haematol. 2005;131(4):530–533. doi: 10.1111/j.1365-2141.2005.05799.x [DOI] [PubMed] [Google Scholar]
- 14.Nolan VG, Zhang Y, Lash T, Sebastiani P, Steinberg MH. Association between wind speed and the occurrence of sickle cell acute painful episodes: results of a case-crossover study. Br J Haematol. 2008;143(3):433–438. doi: 10.1111/j.1365-2141.2008.07354.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Parriault MC, Cropet C, Fahrasmane A, et al. Air Drep-A Retrospective Study Evaluating the Influence of Weather Conditions and Viral Epidemics on Vaso-Occlusive Crises in Patients with Sickle Cell Disease Living in French Guiana. Int J Environ Res Public Health. 2019;16(15):2724. Published 2019 Jul 31. doi: 10.3390/ijerph16152724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wachnian C, Tompkins N, Corriveau-Bourque C, Belletrutti M, Bruce AAK. Cold External Temperatures and Sickle Cell Morbidity in Children: A Retrospective Analysis. J Pediatr Hematol Oncol. 2020;42(1):8–11. doi: 10.1097/MPH.0000000000001627 [DOI] [PubMed] [Google Scholar]
- 17.Redwood AM, Williams EM, Desal P, Serjeant GR. Climate, and painful crisis of sickle-cell disease in Jamaica. Br Med J. 1976;1(6001):66–68. doi: 10.1136/bmj.1.6001.66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Barbosa SM, Farhat SC, Martins LC, et al. Air pollution and children’s health: sickle cell disease. Cad Saude Publica. 2015;31(2):265–275. doi: 10.1590/0102-311x00013214 [DOI] [PubMed] [Google Scholar]
- 19.Blumberg AH, Ebelt ST, Liang D, Morris CR, Sarnat JA. Ambient air pollution and sickle cell disease-related emergency department visits in Atlanta, GA. Environ Res. 2020;184:109292. doi: 10.1016/j.envres.2020.109292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mittal H, Roberts L, Fuller GW, et al. The effects of air quality on haematological and clinical parameters in children with sickle cell anaemia. Ann Hematol. 2009;88(6):529–533. doi: 10.1007/s00277-008-0598-1 [DOI] [PubMed] [Google Scholar]
- 21.Yallop D, Duncan ER, Norris E, et al. The associations between air quality and the number of hospital admissions for acute pain and sickle-cell disease in an urban environment. Br J Haematol. 2007;136(6):844–848. doi: 10.1111/j.1365-2141.2007.06493.x [DOI] [PubMed] [Google Scholar]
- 22.Cohen RT, Strunk RC, Field JJ, et al. Environmental tobacco smoke and airway obstruction in children with sickle cell anemia. Chest. 2013;144(4):1323–1329. doi: 10.1378/chest.12-1569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.West DC, Romano PS, Azari R, Rudominer A, Holman M, Sandhu S. Impact of environmental tobacco smoke on children with sickle cell disease. Arch Pediatr Adolesc Med. 2003;157(12):1197–1201. doi: 10.1001/archpedi.157.12.1197 [DOI] [PubMed] [Google Scholar]
- 24.Boulet SL, Yanni EA, Creary MS, Olney RS. Health status and healthcare use in a national sample of children with sickle cell disease. Am J Prev Med. 2010;38(4 Suppl): S528–S535. doi: 10.1016/j.amepre.2010.01.003 [DOI] [PubMed] [Google Scholar]
- 25.Haque A, Telfair J. Socioeconomic distress, and health status: the urban-rural dichotomy of services utilization for people with sickle cell disorder in North Carolina. J Rural Health. 2000;16(1):43–55. doi: 10.1111/j.1748-0361.2000.tb00435.x [DOI] [PubMed] [Google Scholar]
- 26.Smeltzer MP, Nolan VG, Yu X, et al. Distance from an Urban Sickle Cell Center and its Effects on Routine Healthcare Management and Rates of Hospitalization. Hemoglobin. 2016;40(1):10–15. doi: 10.3109/03630269.2015.1084315 [DOI] [PubMed] [Google Scholar]
- 27.Brodsky MA, Rodeghier M, Sanger M, et al. Risk Factors for 30-Day Readmission in Adults with Sickle Cell Disease. Am J Med. 2017;130(5): 601.e9–601.e15. doi: 10.1016/j.amjmed.2016.12.010 [DOI] [PubMed] [Google Scholar]
- 28.Jacob E, Childress C, Nathanson JD. Barriers to care and quality of primary care services in children with sickle cell disease. J Adv Nurs. 2016;72(6):1417–1429. doi: 10.1111/jan.12756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shankar SM, Arbogast PG, Mitchel E, Ding H, Wang WC, Griffin MR. Impact of proximity to comprehensive sickle cell center on utilization of healthcare services among children with sickle cell disease. Pediatr Blood Cancer. 2008;50(1):66–71. doi: 10.1002/pbc.21066 [DOI] [PubMed] [Google Scholar]
- 30.Liem RI, O’Suoji C, Kingsberry PS, et al. access to patient-centered medical homes in children with sickle cell disease. Matern Child Health J. 2014;18(8):1854–1862. doi: 10.1007/s10995-013-1429-0 [DOI] [PubMed] [Google Scholar]
- 31.Hand R, Koshy M, Dorn L, Patel M. Health insurance status and the use of emergency and other outpatient services by adults with sickle cell disease. Ann Emerg Med. 1995;25(2):224–229. doi: 10.1016/s0196-0644(95)70328-4 [DOI] [PubMed] [Google Scholar]
- 32.Kayle M, Valle J, Paulukonis S, et al. Impact of Medicaid expansion on access and healthcare among individuals with sickle cell disease. Pediatr Blood Cancer. 2020;67(5): e28152. doi: 10.1002/pbc.28152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Raphael JL, Dietrich CL, Whitmire D, Mahoney DH, Mueller BU, Giardino AP. Healthcare utilization and expenditures for low-income children with sickle cell disease. Pediatr Blood Cancer. 2009;52(2):263–267. doi: 10.1002/pbc.21781 [DOI] [PubMed] [Google Scholar]
- 34.Carroll CP, Cichowitz C, Yu T, et al. Predictors of acute care utilization and acute pain treatment outcomes in adults with sickle cell disease: The role of non-hematologic characteristics and baseline chronic opioid dose. Am J Hematol. 2018;93(9):1127–1135. doi: 10.1002/ajh.25168 [DOI] [PubMed] [Google Scholar]
- 35.Health literacy. Health Literacy | Healthy People 2020. https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-health/interventions-resources/health-literacy. Accessed Jan 6, 2022
- 36.Carden MA, Newlin J, Smith W, Sisler I. Health literacy and disease-specific knowledge of caregivers for children with sickle cell disease. Pediatr Hematol Oncol. 2016;33(2):121–133. doi: 10.3109/08880018.2016.1147108 [DOI] [PubMed] [Google Scholar]
- 37.Morrison AK, Myrvik MP, Brousseau DC, et al. Parents’ pain medication underdosing is associated with more emergency department visits in sickle cell disease. Pediatr Blood Cancer. 2018;65(4):10.1002/pbc.26906. doi: 10.1002/pbc.26906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nolan VG, Anderson SM, Smeltzer MP, et al. Pediatric to adult care co-location transitional model for youth with sickle cell disease. Am J Hematol. 2018;93(1): E30–E32. doi: 10.1002/ajh.24953 [DOI] [PubMed] [Google Scholar]
- 39.Cronin RM, Hankins JS, Byrd J, et al. Risk factors for hospitalizations and readmissions among individuals with sickle cell disease: results of a U.S. survey study. Hematology. 2019;24(1):189–198. doi: 10.1080/16078454.2018.1549801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bediako SM, Lanzkron S, Diener-West M, Onojobi G, Beach MC, Haywood C Jr. The Measure of Sickle Cell Stigma: Initial findings from the Improving Patient Outcomes through Respect and Trust study. J Health Psychol. 2016;21(5):808–820. doi: 10.1177/1359105314539530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Haywood C Jr, Diener-West M, Strouse J, et al. Perceived discrimination in health care is associated with a greater burden of pain in sickle cell disease. J Pain Symptom Manage. 2014;48(5):934–943. doi: 10.1016/j.jpainsymman.2014.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Martin SR, Cohen LL, Mougianis I, Griffin A, Sil S, Dampier C. Stigma and Pain in Adolescents Hospitalized for Sickle Cell Vasoocclusive Pain Episodes. Clin J Pain. 2018;34(5):438–444. doi: 10.1097/AJP.0000000000000553 [DOI] [PubMed] [Google Scholar]
- 43.Stanton MV, Jonassaint CR, Bartholomew FB, et al. The association of optimism and perceived discrimination with health care utilization in adults with sickle cell disease. J Natl Med Assoc. 2010;102(11):1056–1063. doi: 10.1016/s0027-9684(15)30733-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mitchell MJ, Lemanek K, Palermo TM, Crosby LE, Nichols A, Powers SW. Parent perspectives on pain management, coping, and family functioning in pediatric sickle cell disease. Clin Pediatr (Phila). 2007;46(4):311–319. doi: 10.1177/0009922806293985 [DOI] [PubMed] [Google Scholar]
- 45.Psihogios AM, Daniel LC, Tarazi R, Smith-Whitley K, Patterson CA, Barakat LP. Family Functioning, Medical Self-Management, and Health Outcomes Among School-Aged Children with Sickle Cell Disease: A Mediation Model. J Pediatr Psychol. 2018;43(4):423–433. doi: 10.1093/jpepsy/jsx120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mougianis I, Cohen LL, Martin S, Shneider C, Bishop M. Racism and Health-Related Quality of Life in Pediatric Sickle Cell Disease: Roles of Depression and Support. J Pediatr Psychol. 2020;45(8):858–866. doi: 10.1093/jpepsy/jsaa035 [DOI] [PubMed] [Google Scholar]
- 47.Palermo TM, Riley CA, Mitchell BA. Daily functioning and quality of life in children with sickle cell disease pain: relationship with family and neighborhood socioeconomic distress. J Pain. 2008;9(9):833–840. doi: 10.1016/j.jpain.2008.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Panepinto JA, Pajewski NM, Foerster LM, Sabnis S, Hoffmann RG. Impact of family income and sickle cell disease on the health-related quality of life of children. Qual Life Res. 2009;18(1):5–13. doi: 10.1007/s11136-008-9412-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cortright L, Buckman C, Tumin D, Holder D, Leonard S. Social Determinants of Health and Emergency Department Use Among Children with Sickle Cell Disease. J Pediatr Hematol Oncol. 2020;42(1): e42–e45. doi: 10.1097/MPH.0000000000001669 [DOI] [PubMed] [Google Scholar]
- 50.Amr MA, Amin TT, Al-Omair OA. Health related quality of life among adolescents with sickle cell disease in Saudi Arabia. Pan Afr Med J. 2011; 8:10. doi: 10.4314/pamj.v8i1.71057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Oliveira CDL, Kelly S, de Almeida-Neto C, et al. Quality of life in pre-adolescent children with sickle cell disease in Brazil. Pediatr Hematol Oncol. 2019;36(8):457–467. doi: 10.1080/08880018.2019.1660743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bundy DG, Muschelli J, Clemens GD, et al. Ambulatory care connections of Medicaid-insured children with sickle cell disease. Pediatr Blood Cancer. 2012;59(5):888–894. doi: 10.1002/pbc.24129 [DOI] [PubMed] [Google Scholar]
- 53.Robinson MR, Daniel LC, O’Hara EA, Szabo MM, Barakat LP. Insurance status as a sociodemographic risk factor for functional outcomes and health-related quality of life among youth with sickle cell disease. J Pediatr Hematol Oncol. 2014;36(1):51–56. doi: 10.1097/MPH.0000000000000013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bello-Manga H, Galadanci AA, Abdullahi S, et al. Low educational level of head of household, as a proxy for poverty, is associated with severe anaemia among children with sickle cell disease living in a low-resource setting: evidence from the SPRING trial. Br J Haematol. 2020;190(6):939–944. doi: 10.1111/bjh.16746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Oluwole OB, Noll RB, Winger DG, Akinyanju O, Novelli EM. Cognitive functioning in children from Nigeria with sickle cell anemia. Pediatr Blood Cancer. 2016;63(11):1990–1997. doi: 10.1002/pbc.26126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Fields ME, Hoyt-Drazen C, Abel R, et al. A pilot study of parent education intervention improves early childhood development among toddlers with sickle cell disease. Pediatr Blood Cancer. 2016;63(12):2131–2138. doi: 10.1002/pbc.26164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bills SE, Schatz J, Hardy SJ, Reinman L. Social-environmental factors, and cognitive and behavioral functioning in pediatric sickle cell disease. Child Neuropsychol. 2020;26(1):83–99. doi: 10.1080/09297049.2019.1577371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Jonassaint CR, Beach MC, Haythornthwaite JA, et al. The Association between Educational Attainment and Patterns of Emergency Department Utilization among Adults with Sickle Cell Disease. Int J Behav Med. 2016;23(3):300–309. doi: 10.1007/s12529-016-9538-y [DOI] [PubMed] [Google Scholar]
- 59.Sanger M, Jordan L, Pruthi S, et al. Cognitive deficits are associated with unemployment in adults with sickle cell anemia. J Clin Exp Neuropsychol. 2016;38(6):661–671. doi: 10.1080/13803395.2016.1149153 [DOI] [PubMed] [Google Scholar]
- 60.Williams H, Silva RNS, Cline D, Freiermuth C, Tanabe P. Social and Behavioral Factors in Sickle Cell Disease: Employment Predicts Decreased Health Care Utilization. J Health Care Poor Underserved. 2018;29(2):814–829. doi: 10.1353/hpu.2018.0060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ghafuri DL, Rodeghier M, DeBaun MR. Rate of Food Insecurity Among Households with Children with Sickle Cell Disease is Above the National Average. South Med J. 2020;113(4):150–155. doi: 10.14423/SMJ.0000000000001082 [DOI] [PubMed] [Google Scholar]
- 62.Adegoke SA, Figueiredo MS, Adekile AD, Braga JAP. Comparative study of the growth and nutritional status of Brazilian and Nigerian school-aged children with sickle cell disease. Int Health. 2017;9(6):327–334. doi: 10.1093/inthealth/ihx035 [DOI] [PubMed] [Google Scholar]
- 63.Mandese V, Marotti F, Bedetti L, Bigi E, Palazzi G, Iughetti L. Effects of nutritional intake on disease severity in children with sickle cell disease. Nutr J. 2016;15(1):46. Published 2016 Apr 30. doi: 10.1186/s12937-016-0159-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Aljuburi G, Laverty AA, Green SA, Phekoo KJ, Bell D, Majeed A. Socio-economic deprivation and risk of emergency readmission and inpatient mortality in people with sickle cell disease in England: observational study. J Public Health (Oxf). 2013;35(4):510–517. doi: 10.1093/pubmed/fdt100 [DOI] [PubMed] [Google Scholar]
- 65.Kumar V, Chaudhary N, Achebe MM. Epidemiology and Predictors of all-cause 30-Day readmission in patients with sickle cell crisis. Sci Rep. 2020;10(1):2082. Published 2020 Feb 7. doi: 10.1038/s41598-020-58934-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Glassberg JA, Wang J, Cohen R, Richardson LD, DeBaun MR. Risk factors for increased ED utilization in a multinational cohort of children with sickle cell disease. Acad Emerg Med. 2012;19(6):664–672. doi: 10.1111/j.1553-2712.2012.01364.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Berghs M, Ola B, Cronin De Chavez A, Ebenso B. Time to apply a social determinants of health lens to addressing sickle cell disorders in sub-Saharan Africa. BMJ Glob Health. 2020;5(7): e002601. doi: 10.1136/bmjgh-2020-002601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Andermann A; CLEAR Collaboration. Taking action on the social determinants of health in clinical practice: a framework for health professionals. CMAJ. 2016;188(17–18): E474–E483. doi: 10.1503/cmaj.160177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Nong P, Raj M, Creary M, Kardia SLR, Platt JE. Patient-Reported Experiences of Discrimination in the US Health Care System. JAMA Netw Open. 2020;3(12): e2029650. Published 2020 Dec 1. doi: 10.1001/jamanetworkopen.2020.29650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Population Health and Public Health Practice; Committee on Addressing Sickle Cell Disease: A Strategic Plan and Blueprint for Action, Martinez RM, Osei-Anto HA, McCormick M, eds. Addressing Sickle Cell Disease: A Strategic Plan and Blueprint for Action. Washington (DC): National Academies Press; (US: ); September 10, 2020. [PubMed] [Google Scholar]
- 71.American Society of Hematology. 2021. ASH Statement Addressing Diversity Equity and Inclusion in Hematology Research Practice and Training. https://www.hematology.org/advocacy/policy-statements/2021/ash-statement-addressing-diversity-equity-and-inclusion-in-hematology-research-practice-and-training Accessed: Oct 27, 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Figure S1: Year of Publication of Articles
Y-axis shows the total number of articles included in the study and x-axis shows the distribution of articles by publication in 5-year intervals.
Supplemental Figure S2: Distribution of Articles by Country of Origin
*Some studies were conducted in multiple countries.


