Abstract
Luxation injuries and other stimuli may lead to a pulp canal obliteration (PCO). Even though the apposition of tertiary dentine is a sign of a vital pulp, in some cases root canal treatment is indicated in the long term due to apical periodontitis or pulpitis. Depending on the extent of PCO, root canal treatment may be challenging even for experienced and well‐equipped endodontic specialists. The ‘guided endodontics’ (GE) technique was introduced 6 years ago as an alternative to conventional access cavity preparation for teeth with PCO and apical pathosis or irreversible pulpitis. Using three‐dimensional radiological imaging such as cone‐beam computed tomography and a digital surface scan, an optimal access to the orifice of the calcified root canal can be planned virtually with appropriate software. GE is implemented either with the help of templates analogous to guided implantology (= static navigation) or by means of dynamic navigation based on a camera‐marker system. GE has emerged as a field of research in the last 6 years with very promising laboratory‐based results regarding the accuracy of guided endodontic access cavities for both static and dynamic navigation. Clinical implementation seems to provide favourable results, but the evidence is mainly based on numerous case reports and a few case series. This narrative review aims to provide an update on the present status of GE and to identify relevant research areas that could contribute to further improvements of this technique.
Keywords: dynamic navigation, pulp canal obliteration, review, root canal treatment, static navigation
INTRODUCTION
Root canal treatment of teeth with pulp canal obliteration (PCO) is a major challenge for both generalists and specialists. The search for a calcified root canal can be very time‐consuming and is associated with an increased risk of creating a perforation.
Pulp canal obliteration are typical late sequelae after dental trauma. They occur in 15%–40% of cases after luxation injuries (Andreasen et al., 1987; Nikoui et al., 2003). In addition to trauma‐induced PCO, increased apposition of dentine in the root canal system is also observed as a result of various other stimuli, for example caries, cervical pulpotomy or restorative therapy (Fleig et al., 2017; Mass & Zilberman, 2011; Sayegh & Reed, 1968), after orthodontic treatment (Delivanis & Sauer, 1982) or in elderly patients due to lifelong intracanal apposition of dentine (Carvalho & Lussi, 2017). The process of calcification is usually asymptomatic and is noticed either incidentally during a radiographic examination or it is indicated by a yellowish discolouration of the tooth. The apposition of dentine is considered an indirect vitality sign of the pulp – despite a frequently encountered negative response to sensitivity testing.
There is consensus, that root canal treatment is not indicated unless there is clinical and radiological evidence of pulpal or periapical pathosis (ESE, 2021; Krastl et al., 2021).
However, calcified teeth may develop apical periodontitis over time, resulting in the need for root canal treatment. This is to be expected in up to 27% of the examined teeth with PCO after a longer observation period (Oginni et al., 2009). Adequate root canal treatment in these cases is challenging and associated with various risks. A retrospective study published four decades ago, assessed the frequency of technical failures and the 4‐year success rates of root canal treatments in incisors with post‐traumatically reduced pulpal lumen and periapical lesions. In teeth with total obliteration, technical failures such as root perforation, fracture of a file or inaccessible root canals occurred in one third of the cases, which led to significantly reduced healing rates after root canal treatment (Cvek et al., 1982).
In contrast to that time, today's methods and materials are considered to provide higher standards, better quality root canal treatment and appropriate handling of procedural errors. However, there is not much evidence to support the benefits of contemporary endodontic techniques for such cases. Only one recent retrospective study focused on the endodontic management of calcified root canals in a specialist setting. Using the operating microscope, all root canals could be detected, full working length could be established in 90% of the cases and a success rate of 80% could be achieved after an observation time of 3 years (Kiefner et al., 2017). However, up to one hour was needed to negotiate the root canals. Furthermore, even successful negotiation of an obliterated root canal might be associated with substantial loss of hard tissue particularly in the cervical region, which is prone to root fracture. This might impair stability and reduce the long‐term prognosis of the tooth (Lang et al., 2006).
In order to minimize the risk of technical errors and to reduce the treatment time, a computer‐assisted therapy approach was developed to localize calcified root canals in a minimally invasive way, and the term ‘Guided Endodontics’ was coined (Krastl et al., 2016; Zehnder et al., 2016).
A guided endodontic access preparation can be approached in two different ways: static guidance, implies the use of a template, whilst dynamic navigation relies on markers positioned in the patient's mouth and a camera system.
Since the first publications (Buchgreitz et al., 2016; Krastl et al., 2016; van der Meer et al., 2016; Zehnder et al., 2016), research on guided endodontics has been conducted at many locations worldwide and numerous international publications are available.
This narrative review aims to update the present status on guided endodontics and to identify relevant research areas that could contribute to further improvements of this technique.
PRESENT STATUS OF STATIC/TEMPLATE GUIDED ENDODONTICS
General workflow
The traditional workflow of guided endodontics is based on the principle of template guided implantology (Jung et al., 2009; Kühl et al., 2015). For implementation, a CBCT with the smallest possible ‘field of view’ and ideally high resolution is required to visualize the calcified root canals. This is supplemented by a digital surface scan, which can be created either directly via an intraoral scanner or by digitizing a plaster cast using a laboratory scanner. For the virtual planning of the access cavity, a software is required to overlay the data of the CBCT in DICOM format with those of the surface scan (stl format). In the aligned 3D data set, the true‐to‐scale virtual image of the drill must be placed so that the tip reaches the visible part of the calcified root canal. In cases where the root canal cannot be visualized in the CBCT, the apex of the tooth is chosen as the apical target point for the drill. After planning the position of the drill and the position of a virtual sleeve above the incisal edge, a virtual template is designed by applying a template designer tool. Different commercially available virtual planning software applications can be used for this purpose (Krug et al., 2020a). For fabrication of the template, both subtractive CAD/CAM and additive 3D‐printing are appropriate. After inserting the template with the incorporated sleeve in the patient's mouth, the bur is moved a few millimetres in depth at low speed and with pumping movements whilst being guided by the sleeve. If the root canal cannot be negotiated at that depth with the help of a hand file, the drilling is continued after cleaning the bur of its debris. This procedure is repeated until the bur hits the mechanical stop of the sleeve, indicating that the apical target point has been reached. If the canal is successfully detected, conventional root canal treatment can now take place.
Figures 1 and 2 depict the treatment of a patient using template guided endodontics who had received a full ceramic bridge from tooth 12 to 22 ten years previously due to a trauma that occurred about four decades ago.
FIGURE 1.
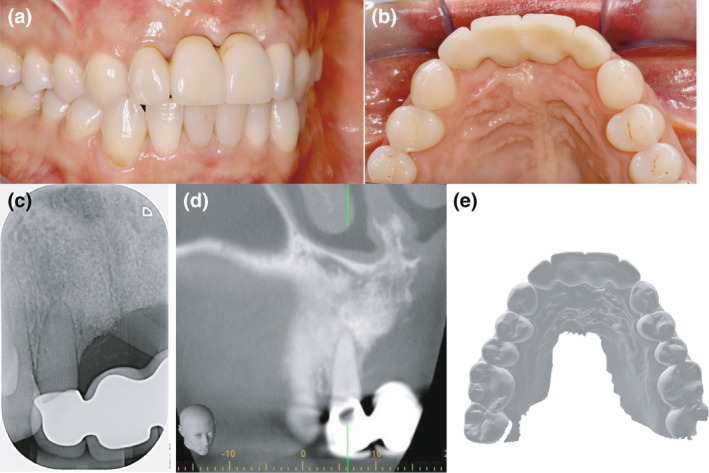
Clinical situation from buccal (a) and palatal (b), 2D imaging performed by the general dentist shows no apical lesion (c), CBCT image shows a severely calcified root canal and a lateral lesion (d), palatal view of intraoral scan (e)
FIGURE 2.
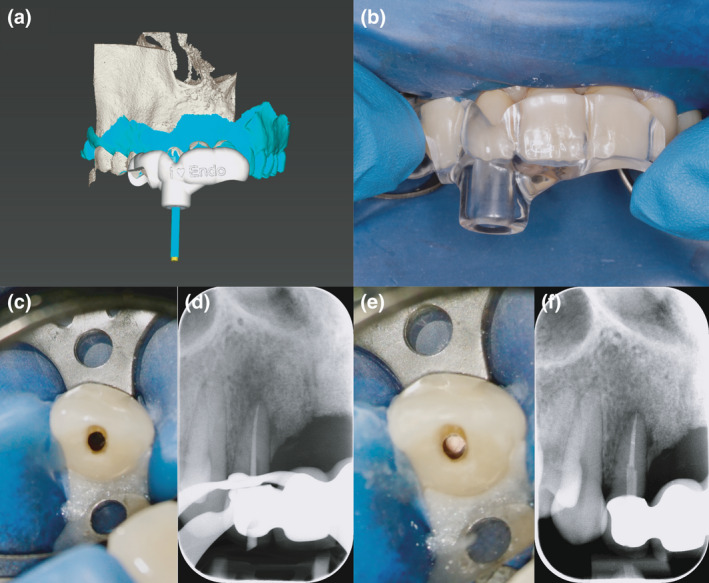
Virtual planning of the access cavity (a), tension‐free insertion of the template (b), minimally invasive access cavity (c), masterpoint radiograph (d), root canal filling before placement of a post (e), final radiograph of root canal filling with fibre post (f)
Review of present literature
The first laboratory studies on the accuracy of guided endodontic access cavity preparation were published in 2016 (Buchgreitz et al., 2016; Zehnder et al., 2016). Both studies demonstrated only small deviations between virtually planned and subsequently performed preparations in extracted human teeth, with a precision below a risk threshold.
This was promptly followed by the first clinical case reports, which also reported successful treatments of calcified anterior teeth in the maxilla (Krastl et al., 2016; van der Meer et al., 2016).
In order to enable a low‐risk access to calcified root canals of mandibular incisors, the procedure was further developed to a ‘microguided’ approach by miniaturizing the diameter of the drill and of the corresponding sleeve (Connert et al., 2017a). By optimizing the fit between bur and sleeve, the accuracy could be further increased with mean deviations between the planned‐ and the prepared‐access cavities ranging from 0.12 to 0.34 mm at the apical target point and a mean angle deviation of 1.59°(Connert et al., 2017b).
Another laboratory study compared root canal location and dentine loss between conventional freehand and guided access cavity preparations in 3D‐ printed teeth with simulated calcified root canals and demonstrated significantly less substance loss and a more predictable and expeditious location and negotiation of calcified root canals with the guided approach. Moreover, in contrast to the freehand approach, the results were not influenced by the experience of the operator (Connert et al., 2019).
Further modifications of the technique using a laser melting template (Zhang et al., 2020) or a sleeveless design were recently presented. The latter aimed to improve accessibility in posterior teeth, particularly for patients with limited mouth opening. With this approach, the handpiece head is guided by guiding rails placed against each other on the sides of the tooth. Since no sleeve is used, it is not necessary to use a dedicated bur (Torres et al., 2021b). Data on the accuracy of this modified approach has not been published yet.
The clinical implementation of guided endodontics has been demonstrated in various further case reports published during the past 5 years (Buchgreitz et al., 2019a; Casadei et al., 2020; Fonseca Tavares et al., 2018; Hegde et al., 2019; Ishak et al., 2020; Kamburoğlu et al., 2021; Krug et al., 2020b; Lara‐Mendes et al., 2018a, 2018b; Llaquet Pujol et al., 2021; Loureiro et al., 2021; Maia et al., 2019; Tavares et al., 2020; Todd et al., 2021; Torres et al., 2019).
In addition to the treatment of calcified teeth, further indications such as dens invaginatus therapy (Ali & Arslan, 2019; Ali et al., 2019; Mena‐Álvarez et al., 2017; Zubizarreta‐Macho et al., 2019), removal of glass fibre posts (Maia et al., 2021; Perez et al., 2021) or mineral trioxide aggregate (MTA) from root canals (Ali & Arslan, 2021) have been considered.
In a clinical study, Buchgreitz et al. (2019b) were able to locate and negotiate the root canal and complete the root canal treatment in all 50 cases, thus confirming that the guided access cavity preparation can be performed safely.
Two systematic reviews by Moreno‐Rabie et al. (2020) and Zubizarreta‐Macho et al. (2021) also concluded that guided endodontics is a ‘highly accurate and successful technique’ for opening root canals. However, the level of evidence is low and further high‐quality studies are needed.
Limitations of the procedure are that static guidance can only be performed on straight roots or straight parts of curved roots. In addition, it requires more time for planning and the radiation dose is increased due to the mandatory CBCT. The costs for the patient are also increased due to the additional effort (CBCT, template).
The implementation in the posterior region is difficult due to the limited space available.
If preparation of the access cavity using GE leads to a perforation of the root, subsequent apicoectomy can still enable tooth preservation, as shown in a recent case report (Fonseca Tavares et al., 2021).
FUTURE DIRECTIONS STATIC/TEMPLATE‐GUIDED ENDODONTICS
Guiding by means of a template and sleeve is already relatively technically mature.
A wider range of commercially available drills in diameter and length would be desirable, as this would enable a patient‐oriented approach. Particularly in the posterior region, a drill system graduated in length could compensate for the limited space available.
Magnet resonance imaging (MRI) may also gain importance in dentistry in the future. This would lead to the avoidance of ionizing radiation, which would be desirable especially in children as their tissues and organs are more sensitive to radiation (Dula et al., 2014).
Leontiev et al. (2021) showed in a proof‐of‐principle study that similarly precise access cavities based on MRI can be prepared in a laboratory environment. The (indirect) visualization of the tooth structure was achieved by using a splint with a hydrous gel, which enabled the successful superimposition of the MRI data with the surface scan. Thus, successful visualization of root canals was achieved in 91 out of 100 cases with a mean angular deviation of 1.82°.
However, these results still need to be confirmed clinically and at present MRI equipment is not available to dentists. Nevertheless, depending on technical progress, this is desirable and conceivable for the future.
Otherwise, high‐quality, prospective clinical studies are still needed to increase the evidence for guided endodontics.
PRESENT STATUS OF DYNAMIC NAVIGATION
General workflow
In addition to the described static navigation using a template, dynamic navigation is also possible for the assessment of root canals. Here, too, the use was initially developed for implantology (Marquardt et al., 2007). The basis of planning is also the fusion of CBCT data with an intraoral surface scan. It may be necessary to attach reference marks to the patient's dentition before the CBCT is created, but with newer systems, these can also be planned digitally and then fabricated by a 3D printer. Using a stereo camera connected to the dynamic navigation system, the drill can now be coordinated with the reference marks and the planning (Figure 3). This results in real‐time navigation, which is visualized on a monitor. During access cavity preparation, the position and movement of the drill in the different sectional planes of the three‐dimensional data set is immediately displayed. In contrast to static navigation, this procedure is not independent of the practitioner and requires a certain amount of practice. However, it is known from implantology that it can achieve a similar precision as static navigation (Block et al., 2017). One advantage over static navigation is that the template fabrication step is eliminated and thus patients with severe pain can be treated more quickly.
FIGURE 3.
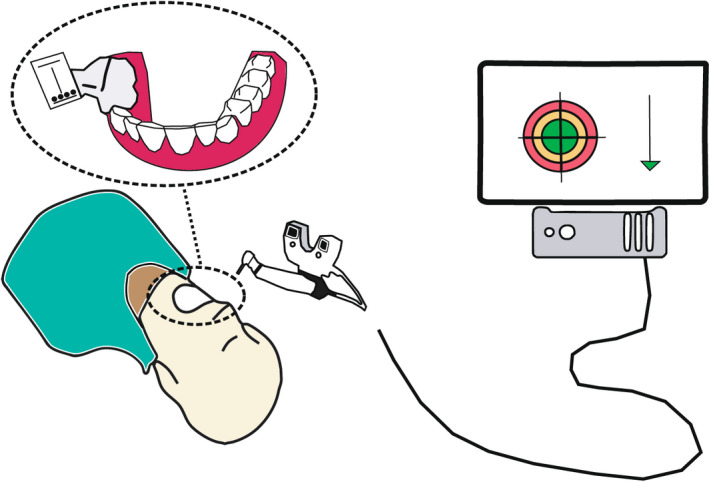
Dynamic navigation scheme: A marker is positioned in the patient's mouth. A stereoscopic camera is connected to a computer. The corresponding software presents the dynamic navigation in real time. The spatial and angular deviation as well as the depth is displayed
Review of present literature
Although the application of this technique in endodontics is still quite new, there are already several studies on its accuracy.
In one of the first studies, Chong et al. (2019) showed on models with extracted teeth that dynamic navigation was able to detect root canals in 26 out of 29 cases. In two of the three remaining teeth, only one canal could be detected on maxillary molars due to tracking difficulties. In the third tooth (also a maxillary molar), the preparation was off‐target.
In a laboratory study, Zubizarreta‐Macho et al. (2020) determined the accuracy of static and dynamic navigation and compared it with freehand preparation. The results revealed that both navigation techniques were superior to freehand preparation. There were no significant differences between static and dynamic navigation. However, it should be mentioned that the mean angular deviation of 10° of static navigation in this study is quite high compared to other studies.
Using 138 printed teeth with simulated PCO, Jain et al. (2020a) reported that dynamic navigation can be used to successfully detect root canals. The angular deviation between the planned and the performed access cavity was 1.7° on average and is thus comparable to static navigation. In this study, a mean 3D deviation of 1.3 mm was measured using postoperative CBCT scans.
Another study compared dynamic navigation with freehand preparation to determine the mesiobuccal canal on 20 replicas. It was found that the navigated access cavities were prepared more precisely in terms of deviation from the ideal preparation and of angular deviation (Gambarini et al., 2020).
Dynamic navigation was compared with freehand preparation on 60 extracted teeth with PCO. Again, the navigated access cavities were more minimally invasive and more accurate in linear and angular deviation. In addition, navigation required less time to visualize the root canals (Dianat et al., 2020).
These results regarding substance loss and treatment time were confirmed by Jain et al. (2020b) in a study using printed replicas with simulated PCO.
Torres et al. (2021a) also concluded from their study on 3D printed models that dynamic navigation is an accurate technique to access heavily calcified root canals. However, it is also emphasized that this technique has a learning curve and requires training.
In the work of Connert et al. (2021), it was shown on 3D‐printed teeth that, using a miniaturized dynamic navigation system, an inexperienced operator can prepare minimally invasive access cavities in a similar way to an experienced one, although there were significant differences in the freehand preparations. Here, too, the loss of substance was significantly lower with the navigated preparation than with the freehand approach.
The use of dynamic navigation also seems to be beneficial in removing fibre posts (Janabi et al., 2021).
Although there is a lack of prospective clinical studies, clinical implementation has been demonstrated. In their case report, Dianat et al. (2021) described the successful treatment of a maxillary molar using dynamic Navigation.
The disadvantages of dynamic navigation systems are the high acquisition costs for the navigation system. Furthermore, in contrast to static guidance, dynamic guidance is not independent of the dentist. It requires a certain amount of practice to prepare precise access cavities, especially as it is unfamiliar to look at a monitor and not at the patient. Some of the current commercially available systems are bulky in size and may be somewhat impractical to use.
FUTURE DIRECTIONS OF DYNAMIC NAVIGATION
For the future, it would be desirable if the systems were further reduced in size to improve handling on the patient. In addition, all systems should have the possibility to digitally plan the required markers in order to avoid having to perform another CBCT scan if a scan (without markers) is already available. Of course, it would be even better if no markers were needed at all and the system could orient itself to the existing anatomical structures.
Augmented reality (AR) navigation might be the next step towards simplification and improving the operator experience with dynamic navigation. The AR approach overlays images, such as radiographic images and navigation paths, with a view of the operative field in a wearable head‐up display or a dedicated microscope. Thus, the operator can simultaneously visualize the operative field and 3D navigation images without having to look up at a display. Whilst such approaches have been used in neurosurgery (Contreras Lopez et al., 2019) clinical implementation in endodontics has only been proposed but has not yet been implemented in a clinical setup (Song et al., 2018).
CONCLUSION
Guided endodontics using static or dynamic navigation appears to be a safe and minimally invasive method for detecting calcified root canals. Dynamic navigation in particular still has great potential for further development.
However, further high‐quality clinical studies on both static and dynamic navigation are needed.
AUTHORS CONTRIBUTION
Thomas Connert: Conceptualization, writing, review and editing (lead). Roland Weiger: Writing, review and editing. Gabriel Krastl: Writing, review and editing.
CONFLICT OF INTEREST
The authors deny any conflicts of interest related to this study.
ETHICAL APPROVAL
The study does not need ethical approval.
ACKNOWLEDGEMENTS
The authors thank Dr. Wadim Leontiev (University Center for Dental Medicine Basel UZB) for his help with the figures. Open access funding provided by Universitat Basel.
Connert, T. , Weiger, R. & Krastl, G. (2022) Present status and future directions – Guided endodontics. International Endodontic Journal, 55(Suppl. 4), 995–1002. Available from: 10.1111/iej.13687
REFERENCES
- Ali, A. & Arslan, H. (2019) Guided endodontics: a case report of maxillary lateral incisors with multiple dens invaginatus. Restorative Dentistry and Endodontics, 44, 38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ali, A. , Arslan, H. & Jethani, B. (2019) Conservative management of Type II dens invaginatus with guided endodontic approach: a case series. Journal of Conservative Dentistry, 22, 503–538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ali, A. & Arslan, H. (2021) Effectiveness of the static‐guided endodontic technique for accessing the root canal through MTA and its effect on fracture strength. Clinical Oral Investigations, 25, 1989–1995. [DOI] [PubMed] [Google Scholar]
- Andreasen, F.M. , Zhijie, Y. , Thomsen, B.L. & Andersen, P.K. (1987) Occurrence of pulp canal obliteration after luxation injuries in the permanent dentition. Endodontics & Dental Traumatology, 3, 103–115. [DOI] [PubMed] [Google Scholar]
- Block, M.S. , Emery, R.W. , Lank, K. & Ryan, J. (2017) Implant placement accuracy using dynamic navigation. The International Journal of Oral & Maxillofacial Implants, 32, 92–99. [DOI] [PubMed] [Google Scholar]
- Buchgreitz, J. , Buchgreitz, M. , Mortensen, D. & Bjørndal, L. (2016) Guided access cavity preparation using cone‐beam computed tomography and optical surface scans – an ex vivo study. International Endodontic Journal, 49, 790–795. [DOI] [PubMed] [Google Scholar]
- Buchgreitz, J. , Buchgreitz, M. & Bjørndal, L. (2019a) Guided endodontics modified for treating molars by using an intracoronal guide technique. Journal of Endodontics, 45, 818–823. [DOI] [PubMed] [Google Scholar]
- Buchgreitz, J. , Buchgreitz, M. & Bjørndal, L. (2019b) Guided root canal preparation using cone beam computed tomography and optical surface scans – an observational study of pulp space obliteration and drill path depth in 50 patients. International Endodontic Journal, 52, 559–568. [DOI] [PubMed] [Google Scholar]
- Carvalho, T.S. & Lussi, A. (2017) Age‐related morphological, histological and functional changes in teeth. Journal of Oral Rehabilitation, 44, 291–298. [DOI] [PubMed] [Google Scholar]
- Casadei, B.A. , Lara‐Mendes, S.T.O. , Barbosa, C.F.M. , Araújo, C.V. , Freitas, C.A. , Machado, V.C. et al. (2020) Access to original canal trajectory after deviation and perforation with guided endodontic assistance. Australian Endodontic Journal, 46, 101–116. [DOI] [PubMed] [Google Scholar]
- Chong, B.S. , Dhesi, M. & Makdissi, J. (2019) Computer‐aided dynamic navigation: a novel method for guided endodontics. Quintessence International, 50, 196–202. [DOI] [PubMed] [Google Scholar]
- Connert, T. , Krug, R. , Eggmann, F. , Emsermann, I. , ElAyouti, A. , Weiger, R. et al. (2019) Guided endodontics versus conventional access cavity preparation: a comparative study on substance loss using 3‐dimensional‐printed teeth. Journal of Endodontics, 45, 327–331. [DOI] [PubMed] [Google Scholar]
- Connert, T. , Leontiev, W. , Dagassan‐Berndt, D. , Kühl, S. , ElAyouti, A. , Krug, R. et al. (2021) Real‐time guided endodontics with a miniaturized dynamic navigation system versus conventional freehand endodontic access cavity preparation: substance loss and procedure time. Journal of Endodontics, 47, 1651–1656. [DOI] [PubMed] [Google Scholar]
- Connert, T. , Zehnder, M.S. , Amato, M. , Weiger, R. , Kühl, S. & Krastl, G. (2017a) Microguided Endodontics: a method to achieve minimally invasive access cavity preparation and root canal location in mandibular incisors using a novel computer‐guided technique. International Endodontic Journal, 51, 247–255. [DOI] [PubMed] [Google Scholar]
- Connert, T. , Zehnder, M.S. , Weiger, R. , Kühl, S. & Krastl, G. (2017b) Microguided Endodontics: accuracy of a miniaturized technique for apically extended access cavity preparation in anterior teeth. Journal of Endodontics, 43, 787–790. [DOI] [PubMed] [Google Scholar]
- Contreras Lopez, W.O. , Navarro, P.A. & Crispin, S. (2019) Intraoperative clinical application of augmented reality in neurosurgery: a systematic review. Clinical Neurology and Neurosurgery, 177, 6–11. [DOI] [PubMed] [Google Scholar]
- Cvek, M. , Granath, L. & Lundberg, M. (1982) Failures and healing in endodontically treated non‐vital anterior teeth with posttraumatically reduced pulpal lumen. Acta Odontologica Scandinavica, 40, 223–228. [DOI] [PubMed] [Google Scholar]
- Delivanis, H.P. & Sauer, G.J. (1982) Incidence of canal calcification in the orthodontic patient. American Journal of Orthodontics, 82, 58–61. [DOI] [PubMed] [Google Scholar]
- Dianat, O. , Gupta, S. , Price, J.B. & Mostoufi, B. (2021) Guided endodontic access in a maxillary molar using a dynamic navigation system. Journal of Endodontics, 47, 658–662. [DOI] [PubMed] [Google Scholar]
- Dianat, O. , Nosrat, A. , Tordik, P.A. , Aldahmash, S.A. , Romberg, E. , Price, J.B. et al. (2020) Accuracy and efficiency of a dynamic navigation system for locating calcified canals. Journal of Endodontics, 46, 1719–1725. [DOI] [PubMed] [Google Scholar]
- Dula, K. , Bornstein, M.M. , Buser, D. , Dagassan‐Berndt, D. , Ettlin, D.A. , Filippi, A. et al. (2014) SADMFR guidelines for the use of cone‐beam computed tomography/ digital volume tomography. Swiss Dental Journal, 124, 1169–1183. [DOI] [PubMed] [Google Scholar]
- ESE . (2021) European Society of Endodontology position statement: endodontic management of traumatized permanent teeth. International Endodontic Journal, 54, 1473–1481. [DOI] [PubMed] [Google Scholar]
- Fleig, S. , Attin, T. & Jungbluth, H. (2017) Narrowing of the radicular pulp space in coronally restored teeth. Clinical Oral Investigations, 21, 1251–1257. [DOI] [PubMed] [Google Scholar]
- Fonseca Tavares, W.L. , de Oliveira Murta Pedrosa, N. , Moreira, R.A. , Braga, T. , de Carvalho Machado, V. , Ribeiro Sobrinho, A.P. et al. (2022) Limitations and management of static‐guided endodontics failure. Journal of Endodontics, 48(2), 273–279. 10.1016/j.joen.2021.11.004 [DOI] [PubMed] [Google Scholar]
- Fonseca Tavares, W.L. , Diniz Viana, A.C. , de Carvalho, M.V. , Feitosa Henriques, L.C. & Ribeiro Sobrinho, A.P. (2018) Guided endodontic access of calcified anterior teeth. Journal of Endodontics, 44, 1195–1199. [DOI] [PubMed] [Google Scholar]
- Gambarini, G. , Galli, M. , Morese, A. , Stefanelli, L.V. , Abduljabbar, F. , Giovarruscio, M. et al. (2020) Precision of dynamic navigation to perform endodontic ultraconservative access cavities: a preliminary in vitro analysis. Journal of Endodontics, 46, 1286–1290. [DOI] [PubMed] [Google Scholar]
- Hegde, S.G. , Tawani, G. , Warhadpande, M. , Raut, A. , Dakshindas, D. & Wankhade, S. (2019) Guided endodontic therapy: Management of pulp canal obliteration in the maxillary central incisor. Journal of Conservative Dentistry, 22, 607–611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ishak, G. , Habib, M. , Tohme, H. , Patel, S. , Bordone, A. , Perez, C. et al. (2020) Guided endodontic treatment of calcified lower incisors: a case report. Dentistry Journal, 8, 74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jain, S.D. , Carrico, C.K. & Bermanis, I. (2020a) 3‐dimensional accuracy of dynamic navigation technology in locating calcified canals. Journal of Endodontics, 46, 839–845. [DOI] [PubMed] [Google Scholar]
- Jain, S.D. , Saunders, M.W. , Carrico, C.K. , Jadhav, A. , Deeb, J.G. & Myers, G.L. (2020b) Dynamically navigated versus freehand access cavity preparation: a comparative study on substance loss using simulated calcified canals. Journal of Endodontics, 46, 1745–1751. [DOI] [PubMed] [Google Scholar]
- Janabi, A. , Tordik, P.A. , Griffin, I.L. , Mostoufi, B. , Price, J.B. , Chand, P. et al. (2021) Accuracy and efficiency of 3‐dimensional dynamic navigation system for removal of fiber post from root canal‐treated teeth. Journal of Endodontics, 47, 1453–1460. [DOI] [PubMed] [Google Scholar]
- Jung, R.E. , Schneider, D. , Ganeles, J. , Wismeijer, D. , Zwahlen, M. , Hämmerle, C.H. et al. (2009) Computer technology applications in surgical implant dentistry: a systematic review. The International Journal of Oral & Maxillofacial Implants, 24, 92–109. [PubMed] [Google Scholar]
- Kamburoğlu, K. , Koç, C. , Sönmez, G. & Çapçı, A. (2021) 3D printing in endodontics: report of three clinical cases with innovative approaches. International Journal of Computerized Dentistry, 24, 317–328. [PubMed] [Google Scholar]
- Kiefner, P. , Connert, T. , ElAyouti, A. & Weiger, R. (2017) Treatment of calcified root canals in elderly people: a clinical study about the accessibility, the time needed and the outcome with a three‐year follow‐up. Gerodontology, 34, 164–170. [DOI] [PubMed] [Google Scholar]
- Krastl, G. , Weiger, R. , Filippi, A. , Van Waes, H. , Ebeleseder, K. , Ree, M. et al. (2021) Endodontic management of traumatized permanent teeth: a comprehensive review. International Endodontic Journal, 54, 1221–1245. [DOI] [PubMed] [Google Scholar]
- Krastl, G. , Zehnder, M.S. , Connert, T. , Weiger, R. & Kühl, S. (2016) Guided endodontics: a novel treatment approach for teeth with pulp canal calcification and apical pathology. Dental Traumatology, 32, 240–246. [DOI] [PubMed] [Google Scholar]
- Krug, R. , Reich, S. , Connert, T. , Kess, S. , Soliman, S. , Reymus, M. et al. (2020a) Guided endodontics: a comparative in vitro study on the accuracy and effort of two different planning workflows. International Journal of Computerized Dentistry, 23, 119–128. [PubMed] [Google Scholar]
- Krug, R. , Volland, J. , Reich, S. , Soliman, S. , Connert, T. & Krastl, G. (2020b) Guided endodontic treatment of multiple teeth with dentin dysplasia: a case report. Head & Face Medicine, 16, 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kühl, S. , Payer, M. , Zitzmann, N.U. , Lambrecht, J.T. & Filippi, A. (2015) Technical accuracy of printed surgical templates for guided implant surgery with the coDiagnostiX ™ software. Clinical Implant Dentistry and Related Research, 17(Suppl. 1), 177–182. [DOI] [PubMed] [Google Scholar]
- Lang, H. , Korkmaz, Y. , Schneider, K. & Raab, W.H. (2006) Impact of endodontic treatments on the rigidity of the root. Journal of Dental Research, 85, 364–368. [DOI] [PubMed] [Google Scholar]
- Lara‐Mendes, S.T.O. , Barbosa, C.F.M. , Santa‐Rosa, C.C. & Machado, V.C. (2018a) Guided endodontic access in maxillary molars using cone‐beam computed tomography and computer‐aided design/computer‐aided manufacturing system: a case report. Journal of Endodontics, 44, 875–879. [DOI] [PubMed] [Google Scholar]
- Lara‐Mendes, S.T.O. , Barbosa, C.F.M. , Machado, V.C. & Santa‐Rosa, C.C. (2018b) A New approach for minimally invasive access to severely calcified anterior teeth using the guided endodontics technique. Journal of Endodontics, 44, 1578–1582. [DOI] [PubMed] [Google Scholar]
- Leontiev, W. , Bieri, O. , Madörin, P. , Dagassan‐Berndt, D. , Kühl, S. , Krastl, G. et al. (2021) Suitability of magnetic resonance imaging for guided endodontics: proof of principle. Journal of Endodontics, 47, 954–960. [DOI] [PubMed] [Google Scholar]
- Llaquet Pujol, M. , Vidal, C. , Mercadé, M. , Muñoz, M. & Ortolani‐Seltenerich, S. (2021) Guided endodontics for managing severely calcified canals. Journal of Endodontics, 47, 315–321. [DOI] [PubMed] [Google Scholar]
- Loureiro, M.A.Z. , Silva, J.A. , Chaves, G.S. , Capeletti, L.R. , Estrela, C. & Decurcio, D.A. (2021) Guided endodontics: the impact of new technologies on complex case solution. Australian Endodontic Journal, 47(3), 664–671. 10.1111/aej.12498 [DOI] [PubMed] [Google Scholar]
- Maia, L.M. , Bambirra Júnior, W. , Toubes, K.M. , Moreira Júnior, G. , de Carvalho Machado, V. , Parpinelli, B.C. et al. (2021) Endodontic guide for the conservative removal of a fiber‐reinforced composite resin post. The Journal of Prosthetic Dentistry. Online ahead of print. 10.1016/j.prosdent.2020.11.044 [DOI] [PubMed] [Google Scholar]
- Maia, L.M. , de Carvalho, M.V. , da Silva, N. , Brito Júnior, M. , da Silveira, R.R. , Moreira Júnior, G. et al. (2019) Case reports in maxillary posterior teeth by guided endodontic access. Journal of Endodontics, 45, 214–218. [DOI] [PubMed] [Google Scholar]
- Marquardt, P. , Witkowski, S. & Strub, J. (2007) Three‐dimensional navigation in implant dentistry. European Journal of Esthetic Dentistry, 2, 80–98. [PubMed] [Google Scholar]
- Mass, E. & Zilberman, U. (2011) Long‐term radiologic pulp evaluation after partial pulpotomy in young permanent molars. Quintessence International, 42, 547–554. [PubMed] [Google Scholar]
- van der Meer, W.J. , Vissink, A. , Ng, Y.L. & Gulabivala, K. (2016) 3D Computer aided treatment planning in endodontics. Journal of Dentistry, 45, 67–72. [DOI] [PubMed] [Google Scholar]
- Mena‐Álvarez, J. , Rico‐Romano, C. , Lobo‐Galindo, A.B. & Zubizarreta‐Macho, Á. (2017) Endodontic treatment of dens evaginatus by performing a splint guided access cavity. Journal of Esthetic and Restorative Dentistry, 29, 396–402. [DOI] [PubMed] [Google Scholar]
- Moreno‐Rabie, C. , Torres, A. , Lambrechts, P. & Jacobs, R. (2020) Clinical applications, accuracy and limitations of guided endodontics: a systematic review. International Endodontic Journal, 53, 214–231. [DOI] [PubMed] [Google Scholar]
- Nikoui, M. , Kenny, D.J. & Barrett, E.J. (2003) Clinical outcomes for permanent incisor luxations in a pediatric population. III. Lateral luxations. Dental Traumatology, 19, 280–285. [DOI] [PubMed] [Google Scholar]
- Oginni, A.O. , Adekoya‐Sofowora, C.A. & Kolawole, K.A. (2009) Evaluation of radiographs, clinical signs and symptoms associated with pulp canal obliteration: an aid to treatment decision. Dental Traumatology, 25, 620–625. [DOI] [PubMed] [Google Scholar]
- Perez, C. , Sayeh, A. , Etienne, O. , Gros, C.I. , Mark, A. , Couvrechel, C. et al. (2021) Microguided endodontics: Accuracy evaluation for access through intraroot fibre‐post. Australian Endodontic Journal, 47(3), 592–598. 10.1111/aej.12524 [DOI] [PubMed] [Google Scholar]
- Sayegh, F.S. & Reed, A.J. (1968) Calcification in the dental pulp. Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology, 25, 873–882. [DOI] [PubMed] [Google Scholar]
- Song, T. , Yang, C. , Dianat, O. & Azimi, E. (2018) Endodontic guided treatment using augmented reality on a head‐mounted display system. Healthcare Technology Letters, 5, 201–207. [Google Scholar]
- Tavares, W.L.F. , Ferreira, M.V.L. , de Carvalho, M.V. , Braga, T. , Amaral, R.R. & Cohen, S. (2020) Antimicrobial photodynamic therapy and guided endodontics: a case report. Photodiagnosis and Photodynamic Therapy, 31, 101935. [DOI] [PubMed] [Google Scholar]
- Todd, R. , Resnick, S. , Zicarelli, T. , Linenberg, C. , Donelson, J. & Boyd, C. (2021) Template‐guided endodontic access. Journal of the American Dental Association, 152, 65–70. [DOI] [PubMed] [Google Scholar]
- Torres, A. , Boelen, G.J. , Lambrechts, P. , Pedano, M.S. & Jacobs, R. (2021a) Dynamic navigation: a laboratory study on the accuracy and potential use of guided root canal treatment. International Endodontic Journal, 54, 1659–1667. [DOI] [PubMed] [Google Scholar]
- Torres, A. , Lerut, K. , Lambrechts, P. & Jacobs, R. (2021b) Guided endodontics: use of a sleeveless guide system on an upper premolar with pulp canal obliteration and apical periodontitis. Journal of Endodontics, 47, 133–139. [DOI] [PubMed] [Google Scholar]
- Torres, A. , Shaheen, E. , Lambrechts, P. , Politis, C. & Jacobs, R. (2019) Microguided endodontics: a case report of a maxillary lateral incisor with pulp canal obliteration and apical periodontitis. International Endodontic Journal, 52, 540–549. [DOI] [PubMed] [Google Scholar]
- Zehnder, M.S. , Connert, T. , Weiger, R. , Krastl, G. & Kühl, S. (2016) Guided endodontics: accuracy of a novel method for guided access cavity preparation and root canal location. International Endodontic Journal, 49, 966–972. [DOI] [PubMed] [Google Scholar]
- Zhang, T. , Chen, D. , Miao, L.Y. , Xie, S.J. & Tang, X.N. (2020) Guided endodontic access of calcified root canal by laser melting templates. Hua Xi Kou Qiang Yi Xue Za Zhi, 38, 525–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zubizarreta‐Macho, Á. , Ferreiroa, A. , Agustín‐Panadero, R. , Rico‐Romano, C. , Lobo‐Galindo, A.B. & Mena‐Álvarez, J. (2019) Endodontic re‐treatment and restorative treatment of a dens invaginatus type II through new technologies. Journal of Clinical and Experimental Dentistry, 11, 570–576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zubizarreta‐Macho, A. , Munoz, A.P. , Deglow, E.R. , Agustin‐Panadero, R. & Alvarez, J.M. (2020) Accuracy of computer‐aided dynamic navigation compared to computer‐aided static procedure for endodontic access cavities: an in vitro study. Journal of Clinical Medicine, 9, 129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zubizarreta‐Macho, Á. , Valle Castaño, S. , Montiel‐Company, J.M. & Mena‐Álvarez, J. (2021) Effect of computer‐aided navigation techniques on the accuracy of endodontic access cavities: a systematic review and meta‐analysis. Biology, 10, 212. [DOI] [PMC free article] [PubMed] [Google Scholar]


