Abstract
Objectives
To compare medial meniscal extrusion on weight‐bearing ultrasound (US) with supine US and magnetic resonance (MR) imaging correlating with meniscal pathology and reported symptoms.
Methods
IRB approved study with informed consent. Patients obtaining routine knee MR imaging for suspected knee pathology were prospectively evaluated with supine and weight‐bearing US of the medial meniscus. Meniscal extrusion was measured independently by two fellowship‐trained musculoskeletal radiologists. Correlation was made to presence or absence of meniscal degeneration or tear on MR imaging, as well as reported symptoms. Statistical significance was calculated via intraclass correlation coefficient (ICC) and analysis of variance (ANOVA).
Results
Ninety‐nine knees from 95 subjects (50 males, 45 females; mean age 45 ± 15 years) were included. Mean medial meniscal extrusion measured at US for a normal meniscus (n = 36) was 0.8 mm when supine, increasing to 1.6 mm on weight‐bearing. Mean meniscal extrusion in subjects with mucoid degeneration (n = 20) and those with meniscal tears (n = 43) was 1.6 mm, increasing to 2.3 mm with weight bearing. Inter‐reader reliability showed ICC values of 0.853 to 0.940. There was a significant difference in medial meniscal extrusion comparing subjects with a normal medial meniscus at magnetic resonance imaging (MRI) and subjects with either meniscal degeneration or tear. There was no significant difference in degree of meniscal extrusion between subjects with meniscal degeneration or tear. There was trend of worsening symptoms and increasing functional limitations moving from normal meniscus to meniscal degeneration to meniscal tear.
Conclusions
A normal meniscus shows lesser mobility between supine and upright position, than a pathologic meniscus. Both mucoid degeneration and meniscal tear demonstrate extrusion in the supine position, which increases with weight‐bearing position.
Keywords: diagnostic imaging, knee, magnetic resonance imaging, meniscus, ultrasonography, weight‐bearing
Abbreviations
- ANOVA
analysis of variance
- HIPPA
health insurance portability and accountability act
- ICC
intraclass correlation coefficient
- IRB
institutional review board
- KOS‐ADLS
Knee Outcome Survey Activities of Daily Living Scale
- MR
magnetic resonance
- MRI
magnetic resonance imaging
- PACS
picture archiving and communication system
- PDW
proton density weighted
- US
ultrasound
Introduction
Menisci have a broad range of functions within the knee joint, including load bearing, shock absorption, joint stabilization, and proprioception. 1 When the medial meniscus protrudes medial to the tibia, this is termed meniscal extrusion. 2 In addition to meniscal tear, there are many causes for meniscal extrusion, such as internal knee derangement and effusion. 2 , 3 Meniscal extrusion can be associated with meniscal tears, especially radial tears that involve the meniscal root, and joint space narrowing related to cartilage loss. 4 Identification of meniscal extrusion at imaging can be an important indicator of knee pathology, correlating with severity and progression of knee osteoarthritis. 5 , 6 , 7 Meniscal extrusion is also a negative predictor of clinical outcomes after partial meniscectomy. 1
Magnetic resonance (MR) imaging is commonly used to show meniscal extrusion. 8 When the knee is loaded during MR imaging, simulating weight‐bearing, meniscal extrusion increases in the presence of osteoarthritis. 4 , 9 However, a load‐bearing magnetic resonance imaging (MRI) is uncommon in the typical clinical scenario. Ultrasound, which has been shown to have equal diagnostic accuracy as MRI for meniscal extrusion, has also been studied in supine subjects. 10 Ultrasound has the potential added benefit of routine weight‐bearing assessment. 11 However, the role and importance of dynamic weight‐bearing meniscal evaluation with ultrasound has not been fully delineated.
A prior ultrasound and MR imaging study has shown that a meniscus with a radial tear shows meniscal extrusion with and without weight‐bearing. 12 However, it is unknown how meniscal degeneration or other meniscal pathology affects dynamic meniscal extrusion with weight‐bearing, and how this may relate to patient symptoms. Therefore, the purpose of this study was to evaluate dynamic meniscal extrusion during weight‐bearing, and correlating those findings with MR imaging findings and patient symptomatology. Our hypotheses are that weight‐bearing ultrasound reveals meniscal extrusion which is not visible on supine non–weight‐bearing imaging, meniscal degeneration and tears can lead to meniscal extrusions, which might be evident only in weight‐bearing, and that meniscal pathologies correlate with higher symptom scores of patients.
Materials and Methods
Inclusion and Exclusion Criteria
Institutional review board approval was obtained for this Health Insurance Portability and Accountability Act (HIPAA)‐compliant study to prospectively perform additional ultrasound of the knee in consecutive patients referred for routine knee MR examinations (non‐tumor protocol). All subjects were included after obtaining their written informed consent.
Exclusion criteria included patients under the age of 21 years, inability to stand without crutches or other supporting devices for the duration of the weight‐bearing ultrasound examination, knee arthroplasty, and non‐routine MR examinations of the knee (eg, tumor protocol).
Ultrasound Imaging
Ultrasound imaging of the mid portion of the medial meniscus deep to the medial collateral ligament was performed in supine and weight‐bearing position by 1 fellowship‐trained musculoskeletal radiologist with 7 years of experience using a 12 MHz transducer (Philips, Model CX50, Bothell, WA; Figure 1). The order of the examinations both performed on the same day (MR examination immediately followed by ultrasound or ultrasound immediately followed by MR examination) was determined regarding the time prior to the MR examination (if there was enough time to perform an ultrasound examination, then this was performed first, otherwise second). This was done to reduce the waiting period of the patients to ensure a higher willingness to participate in the study. The radiologist performing the ultrasound examination was blinded for the MR images and MR imaging results. Three positions were used for ultrasound examination: 1) For the supine relaxed examination a cushion was placed under the knee at the ultrasound examination to simulate the slightly flexed knee position in the MR knee coil; 2) For the stressed supine examination, the patient had to contract the quadriceps muscle lifting the leg; and 3) For the upright weight‐bearing examination, the patient was standing on both legs and instructed to distribute their weight equally between both legs. The medial collateral ligament was used as landmark when imaging the body of the medial meniscus. Both static images and cine clips were obtained.
Figure 1.

Image shows ultrasound transducer placement in the coronal plane at the medial knee parallel with the medial collateral ligament to measure medial meniscal body extrusion.
MR Imaging
The routine knee MR imaging was completed on commercially available machines (General Electric 1.5T, Milwaukee, Wisconsin; Siemens 3T, Malvern, Pennsylvania; and Philips 1.5T and 3T, Bothell, Washington) with protocols that consisted of axial T1W TSE non–fat‐saturated (TR 500, TE 17), axial T2W fat‐saturated (TR 3000, TE 60), coronal PDW fat‐saturated (TR 3531, TE 20), sagittal PDW TSE non–fat‐saturated (TR 5000, TE 20), and sagittal PDW fat‐saturated (TR 3122, TE 30).
Image Review
The randomized MR and ultrasound images were evaluated independently by two fellowship‐trained musculoskeletal radiologists (23 and 7 years of experience) on Food and Drug Administration–approved Picture Archiving and Communication System (PACS) workstations for meniscal extrusion, which was measured using the position of the outer boundary of the medial meniscus (apex of the meniscal curve) measured relative to the medial tibial cortex. The presence of an osteophyte was not included in this measurement. Meniscal extrusion measurements were obtained from the coronal MR images, as well as the supine and weight‐bearing ultrasound images.
Medial meniscus integrity was also evaluated on MR imaging (normal, mucoid degeneration, tear) by one of the radiologists (7 years of experience). Mucoid degeneration was defined as intrasubstance signal changes of the meniscus not reaching the articular surface. Meniscal tears were defined as abnormal meniscal morphology, eg, radial tear or bucket‐handle tear or increased signal intensity extending to meniscal articular surface. If present, meniscal tears were classified as radial, root, horizontal, complex, or bucket‐handle tears. Additionally, any postoperative meniscus was assessed (postoperative meniscus without tear, postoperative meniscus with tear).
Assessment of Symptoms and Functional Limitations
All subjects enrolled in the study filled out a “Knee Outcome Survey Activities of Daily Living Scale” (KOS‐ADLS) prior to their examinations. 13 This survey evaluates symptoms and functional limitations over the last 1 to 2 days. The symptoms assessed were a) pain; b) stiffness; c) swelling; d) giving way, buckling or shifting of knee; e) weakness; and f) limping. The scale for the symptoms was 1) I do not have the symptom; 2) I have the symptom, but it does not affect my activity; the symptom affects my activity 3) slightly, 4) moderately, 5) severely; and 6) the symptom prevents me from all daily activities. The functional limitations assessed how the knee affects the subjects' ability to a) walk; b) go upstairs; c) go down stairs; d) stand; e) kneel on the front of the knee; f) squat; g) sit with knee bent; and h) rise from a chair. The scale used for functional limitations is 1) activity is not difficult; 2) activity is minimally, 3) somewhat, 4) fairly, 5) very difficult; and 6) I am unable to do the activity. For each subject, a score is calculated as follows. For each of the 14 survey questions, any response of “1” is multiplied by 5, “2” multiplied by 4, “3” multiplied by 3, “4” multiplied by 2, “5” multiplied by 1, and “6” multiplied by 0. The sum of the 14 questions is then divided by 70 and multiplied by 100. The higher the number indicates the less symptoms and less functional limitations.
Statistical Analysis
Statistical analyses were performed with Microsoft Excel (Redmond, WA, USA) and SPSS software (version 22.0; SPSS, Chicago, IL, USA). Descriptive statistics were calculated (mean, standard deviation, range, and percentage). Inter‐reader reliability and inter‐modality reliability were evaluated using intraclass correlation coefficient (ICC). Continuous variables (KOS‐ADLS scores, supine and standing extrusion measurements by ultrasound) were compared between the three meniscal groups (normal, degeneration, and tear) using analysis of variance (ANOVA). Pairwise comparisons were performed when necessary to detect the difference between each paired groups. According to Rosner 14 for the inter‐reader reliability, an ICC value of >0.75 is considered excellent, 0.40–0.75 fair to good and <0.40 poor. A P value less than .05 was considered statistically significant.
Results
Demographics
The study group of 95 subjects with 99 knees consisted of 53% male (50/95) and 47% female (45/95) subjects. There were 43 right and 56 left knees examined, with 4 bilateral examinations. The mean age of the subjects was 45 years (range 21 to 81 years; standard deviation 15 years).
Imaging Results
The medial meniscus was normal in 36.4% (36/99) knees, showed mucoid degeneration in 20.2% (20/99) knees, and a tear in 43.4% (43/99) knees. The types of tears were as follows: radial (n = 3), root (4), horizontal (13), complex (16), and bucket handle (7). Five menisci were postoperative, including one with a re‐tear.
Meniscal Extrusion Measurements
Medial meniscal extrusion measurements from MRI and ultrasound are shown in Table 1 for subjects with a normal meniscus (Figure 2), degenerative meniscus (Figure 3), and torn meniscus (Figure 4). The intermodality agreement between meniscal extrusion on the supine MR imaging compared to supine ultrasound was fair to good for both readers (reader 1: 0.689; reader 2: 0.629). Inter‐reader reliability showed ICC values with good to excellent reliability (0.853 and 0.940). The statistical details are depicted in Table 1.
Table 1.
Extrusion of the Medial Meniscus on Supine MR Imaging, Supine US, and Weight‐Bearing Position
| MR Imaging: Supine | US: Supine, Relaxed | US: Supine, Active Leg Lift | US: Upright, Weight‐Bearing | |
|---|---|---|---|---|
| Normal meniscus | ||||
| Reader 1 | 1.1 ± 1.0 (0–3.4) | 0.8 ± 0.9 (−0.4 to 2.8) | 1.2 ± 1.0 (0–3.8) | 1.6 ± 1.1 (0–4.0) |
| Reader 2 | 1.2 ± 0.9 (0–3.3) | 0.8 ± 0.8 (0–2.3) | 1.1 ± 0.8 (0–3.2) | 1.6 ± 1.0 (0–3.9) |
| Mucoid degeneration | ||||
| Reader 1 | 1.6 ± 1.2 (0–4.6) | 1.6 ± 1.2 (0–4.4) | 1.9 ± 1.1 (0–3.4) | 2.3 ± 0.9 (0.6–3.7) |
| Reader 2 | 1.7 ± 1.1 (0–4.5) | 1.6 ± 1.2 (0–4.3) | 1.8 ± 1.0 (0–4) | 2.3 ± 1.0 (0.4–4.0) |
| Torn meniscus | ||||
| Reader 1 | 1.8 ± 1.2 (−0.8 to 4.4) | 1.6 ± 1.2 (−1.5 to 3.6) | 2.0 ± 1.1 (0–4.0) | 2.3 ± 1.2 (0–4.4) |
| Reader 2 | 1.9 ± 1.0 (−1.0 to 4.4) | 1.5 ± 1.1 (0–4.0) | 1.9 ± 1.2 (0–4.5) | 2.4 ± 1.1 (0–4.8) |
| ICC | 0.940 | 0.902 | 0.853 | 0.885 |
The values depict mean ± standard deviation (and range) in millimeters.
ICC indicates intraclass correlation coefficient; MR, magnetic resonance; US, ultrasound.
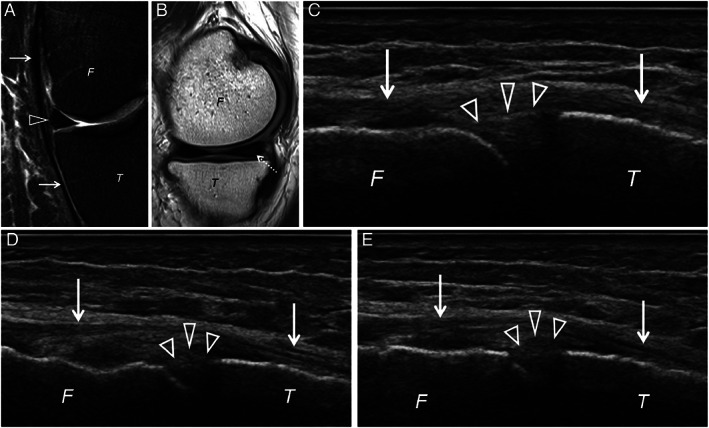
Figure 2.

Right knee of a 36‐year‐old male showing a normal medial meniscus (arrowhead) on (A) coronal and (B) sagittal proton density weighted (PDW) fat‐saturated magnetic resonance (MR) imaging at the level of the medial collateral ligament (arrows). Supine relaxed ultrasound of the medial meniscus (arrowheads) at the level of the medial collateral ligament (arrows) (C), supine stressed ultrasound (D), and weight‐bearing ultrasound (E) show no meniscal extrusion. F, femur; T, tibia.
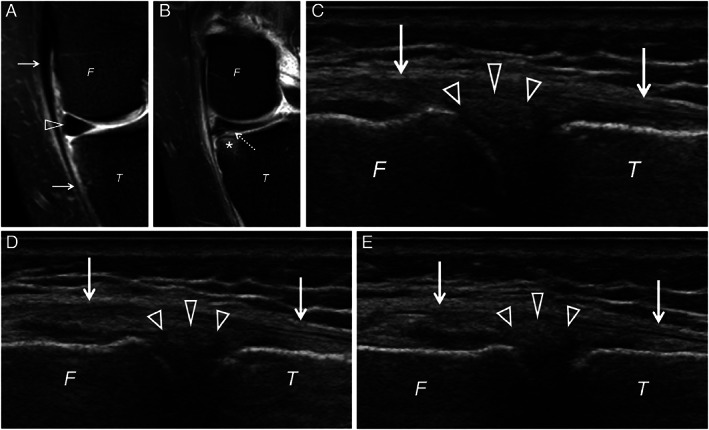
Figure 3.
Left knee of a 65‐year‐old male showing the medial meniscus (arrowhead) on (A) coronal PDW fat‐saturated at the level of the medial collateral ligament (arrows) without extrusion. Sagittal PDW magnetic resonance (MR) imaging (B) shows a mucoid degeneration (dashed arrow) of the posterior horn of the medial meniscus. Supine relaxed ultrasound (C) of the medial meniscus (arrowheads) at the level of the medial collateral ligament shows no extrusion. However, supine stressed ultrasound (D) and especially weight‐bearing ultrasound (E) shows a mild meniscal extrusion. F, femur; T, tibia.
Figure 4.
Left knee of a 55‐year‐old female showing a medial meniscus (arrowhead) on (A) coronal PDW fat‐saturated at the level of the medial collateral ligament (arrows) without extrusion. Coronal PDW fat‐saturated magnetic resonance (MR) imaging slightly posterior (B) shows a tear with contact to the undersurface of the meniscus (dashed arrow) and adjacent bone marrow edema (asterisk). Supine relaxed ultrasound (C) of the medial meniscus (arrowheads) at the level of the medial collateral ligament shows slight meniscal extrusion with minimal change on supine stressed ultrasound (D). Weight‐bearing ultrasound (E) increases the meniscal extrusion severely. F, femur; T, tibia.
The amount of meniscal extrusion at ultrasound (supine and standing) in each of the three subject groups (normal meniscus, meniscal degeneration, meniscal tear at MRI) was then compared (Table 2). For reader 1, there was a significant difference in meniscal extrusion both supine and standing between the three groups (P = .001 and .011, respectively). Similarly, for reader 2, there was a significant difference in meniscal extrusion both supine and standing between the 3 groups (P = .003 and .002, respectively). The results of the pairwise analysis are also shown in Table 2, and show for both readers significant differences in extrusion between the meniscal tear group and the normal meniscus group. There was no significant difference in meniscal extrusion between the meniscal degeneration and meniscal tear groups.
Table 2.
Comparison of Meniscal Extrusion at Ultrasound (Supine and Standing) Between the 3 Subject Groups
| Meniscus: Normal (N = 36) | Meniscus: Degeneration (N = 20) | Meniscus: Tear (N = 43) | P Value | |
|---|---|---|---|---|
| Reader 1 | ||||
| Extrusion: supine | 0.77 ± 0.87*# | 1.65 ± 1.23* | 1.63 ± 1.19# | .001 |
| Extrusion: standing | 1.59 ± 1.07* | 2.30 ± 0.90 | 2.31 ± 1.21* | .011 |
| Reader 2 | ||||
| Extrusion: supine | 0.81 ± 0.79*# | 1.58 ± 1.17* | 1.54 ± 1.12# | .003 |
| Extrusion: standing | 1.58 ± 1.00*# | 2.29 ± 0.97* | 2.42 ± 1.10# | .002 |
* and # indicate significant difference between the paired groups.
Results of Symptoms and Functional Limitations
The KOS‐ADLS scores for the 3 subject groups based on meniscal findings on MRI are shown in Table 3. There was trend of decreasing score (worsening symptoms and increasing functional limitations) moving from normal to meniscal degeneration to meniscal tear. There was a significant difference in the KOS‐ADLS scores between the 3 subject groups (P = .037).
Table 3.
KOS‐ADLS Scores for Each Subject Group Based on Meniscus Status on MRI
| Meniscus: Normal (N = 36) | Meniscus: Degeneration (N = 20) | Meniscus: Tear (N = 43) | P Value | |
|---|---|---|---|---|
| KOS‐ADLS score | 0.64 ± 0.20* | 0.63 ± 0.18 | 0.53 ± 0.22* | .037 |
*The P Value comparing group “normal” vs. “tear” is .019. KOS‐ADLS indicates Knee Outcome Survey Activities of Daily Living Scale; MRI, magnetic resonance imaging.
Discussion
In our study, we found medial meniscal extrusion to be increased with additional loading as assessed by ultrasound, especially in standing weight‐bearing position compared to relaxed supine position. A normal meniscus demonstrated less extrusion when compared to a meniscus with mucoid degeneration or a tear. A meniscus with mucoid degeneration showed the same amount of extrusion as a torn meniscus. Patients had worsening symptoms and increasing functional limitations moving from normal meniscus to meniscal degeneration to meniscal tear as shown on MRI.
Meniscal extrusion has been shown to be independently associated with meniscal tears, knee malalignment, and tibiofemoral cartilage damage. 15 An extruded meniscus has a reduced weight‐bearing capacity, cannot optimally distribute loading between the femoral and tibial compartment, and thus cannot properly fulfill functions like shock absorption and joint stabilization. This leads to an increased load bearing on cartilage and bone 16 and can contribute to the progression of osteoarthritis. 7 , 17 , 18 However, if the meniscus is not already extruded without weight‐bearing load, the diagnosis of an occult meniscal extrusion might be obscured. Only specialized MR units can perform partial weight‐bearing examinations and are not widely available. 19 These MR units perform weight‐bearing examinations in an 82° upright position with the patient leaning on the backrest. However, it is unknown to what degree this backrest prevents full weight‐load on the extremities. Additionally, these are open bore low magnetic field scanners (0.25–0.6 T scanners), 19 with limited spatial resolution compared to higher field scanners. Other studies examined meniscal extrusion using a loading device simulating upright position by applying axial load to the leg of 50% body weight on conventional supine MR examination. 4 , 9 These studies have shown that meniscal extrusion occurs more frequently under loading conditions. However, weight‐bearing MR units as well as simulated weight‐bearing remain mostly limited to research purposes. Ultrasound on the other hand is widely available even in countries with limited resources. 20 , 21 Rowland et al 11 demonstrated in their cadaveric study that meniscal extrusion not only increases with loading, but also with the amount of injury using 50 and 100% meniscal cuts. Interestingly, they could also show that a meniscal repair could reduce the meniscal extrusion. This raises the possibility of weight‐bearing ultrasound as a possible pre‐ and postsurgical scanning tool to follow‐up postsurgical outcome. However, their cadaveric study used artificially created injuries and examined the lateral and not the medial meniscus. Thus, this effect on the medial meniscus can only be hypothesized.
In our study, medial meniscal extrusion was most evident with upright load bearing; however, even in the supine stressed‐leg‐lift position meniscal extrusion was appreciated. Although, the amount of extrusion was less than in the upright weight‐bearing examination, knowledge of this finding might be useful in patients who cannot perform a weight‐bearing examination.
In a recent study, Karpinski et al 12 examined medial meniscal extrusion in a cohort of 25 patients with a medial root lesion of the meniscus and 25 healthy controls. They examined the medial meniscus extrusion using MR and ultrasound in supine position, and additionally ultrasound under full weight‐bearing. Their study group found no dynamic extrusion using weight‐bearing ultrasound of confirmed meniscal root tear lesions, but only a dynamic meniscal extrusion in the healthy control group. However, the root tear group showed already a meniscal extrusion on supine ultrasound and MR examinations. Thus, no increase in extrusion was present under weight‐bearing. Though, it might be more critical to identify an occult medial meniscal extrusion to prevent increased load bearing on cartilage and bone. Of note, the degree of meniscal extrusion described by Karpinski et al 12 was greater than what was seen in our subjects, which could in part be explained by the root tears in their subjects, pathology that is prone to meniscal extrusion. Chiba et al 5 in a 3‐year follow‐up study compared the development of meniscal extrusion on ultrasound and progression of osteoarthritis grades on radiographs. They showed progression of osteoarthritis and correlation with meniscal extrusion using both modalities in severe stages of osteoarthritis. In moderate osteoarthritis grades, progression could not show a correlation with meniscal extrusion. However, Chiba et al 5 did not perform a weight‐bearing ultrasound examination. Thus, occult meniscal extrusion, i.e. only visible on weight‐bearing examinations, might have been undiagnosed. This ultrasound finding might be of particular interest especially in settings where MR imaging is not readily available to allow adaptation of the therapy prior to the need of a joint replacement. Newer and less expensive hand‐held ultrasound devices might contribute to an increase of ultrasound examinations, especially since their diagnostic accuracy was found to be comparable to conventional cart‐based ultrasound. 22 Thus, weight‐bearing ultrasound might be a useful tool to close the gap between the accessibility of MR or even weight‐bearing MR, and could help in the identification of occult meniscal extrusion not visible on conventional MR imaging.
Interestingly, our study showed the same amount of extrusion in subjects having mucoid degeneration and subjects having a meniscal tear. This shows that mucoid degeneration may cause loss of the normal hoop stress and extrusion of the meniscus, and that this extrusion may be a precursor of a tear. Crema et al 23 could not find an association between prevalent medial meniscal intrasubstance signal changes and meniscal tears over a 1‐year period. Further longitudinal assessment of our subjects with regard to development of meniscal tears is being considered as a future research study. Our current study also showed a trend where patients reported worsening symptoms and increasing functional limitations moving from normal meniscus to meniscal degeneration to meniscal tear as shown on MRI.
We acknowledge some limitations in our study. We only examined the medial meniscus at the level of the medial collateral ligament. However, this was to allow a reliable comparison with the MR imaging with an additional anatomical landmark. The upright weight‐bearing ultrasound examination was performed while standing on both legs. We did not perform a weight‐bearing examination with the full load of the whole body while standing on one leg, due to potential risk of patient falling. However, our subjects were instructed to distribute their weight equally between both legs to prevent an axial loading primarily on the contralateral side. We did not evaluate specific differences between the different types of meniscal tears, to prevent a bias due to the low number in the specific subgroups of tears. In addition, correlation was not made with other knee findings on MRI. We performed the study using different MR scanners 1.5 and 3 T. However, since meniscal evaluation is routinely performed on those scanners, we did not anticipate significant differences for these scanner types. We do not have surgical correlation to the results of our study, because the majority of our patients received conservative treatment. We were not able to perform a follow‐up of the subjects to evaluate a possible progression of mucoid degeneration into a meniscal tear as well as osteoarthritis.
Conclusion
A normal meniscus shows less meniscal extrusion between supine and upright position compared to a pathologic meniscus. Menisci with either mucoid degeneration and/or meniscal tear both demonstrate meniscal extrusion in the supine position, which further increases with weight‐bearing position. There was trend of worsening symptoms and increasing functional limitations moving from normal meniscus to meniscal degeneration to meniscal tear.
Acknowledgment
Open access funding enabled and organized by Projekt DEAL.
ALF received grants from the Research Funds of the University of Basel, Swiss Society of Radiology, Gottfried und Julia Bangerter‐Rhyner‐Stiftung, and Freiwillige Akademische Gesellschaft Basel. MC is a consultant for Philips Medical imaging. AB has received consulting fees from Arthrex, Smith & Nephew, Stryker, and Flexion Therapeutics and royalties from Arthrex and Smith & Nephew. VK is a consultant for Hyalex Orthopaedics; all sponsors listed above played no role in matters of study design, collection, analysis, interpretation of data, and in the decision to submit the paper for publication.
References
- 1. Kim SJ, Choi CH, Chun YM, et al. Relationship between preoperative extrusion of the medial meniscus and surgical outcomes after partial meniscectomy. Am J Sports Med 2017; 45:1864–1871. 10.1177/0363546517697302. [DOI] [PubMed] [Google Scholar]
- 2. Miller TT, Staron RB, Feldman F, Cepel E. Meniscal position on routine MR imaging of the knee. Skeletal Radiol 1997; 26:424–427. 10.1007/s002560050259. [DOI] [PubMed] [Google Scholar]
- 3. Rennie WJ, Finlay DB. Meniscal extrusion in young athletes: associated knee joint abnormalities. AJR Am J Roentgenol 2006; 186:791–794. 10.2214/ajr.04.1181. [DOI] [PubMed] [Google Scholar]
- 4. Patel R, Eltgroth M, Souza R, et al. Loaded versus unloaded magnetic resonance imaging (MRI) of the knee: effect on meniscus extrusion in healthy volunteers and patients with osteoarthritis. Eur J Radiol Open 2016; 3:100–107. 10.1016/j.ejro.2016.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Chiba D, Maeda S, Sasaki E, et al. Meniscal extrusion seen on ultrasonography affects the development of radiographic knee osteoarthritis: a 3‐year prospective cohort study. Clin Rheumatol 2017; 36:2557–2564. 10.1007/s10067-017-3803-6. [DOI] [PubMed] [Google Scholar]
- 6. Chiba D, Sasaki E, Ota S, et al. US detection of medial meniscus extrusion can predict the risk of developing radiographic knee osteoarthritis: a 5‐year cohort study. Eur Radiol 2020; 30:3996–4004. 10.1007/s00330-020-06749-1. [DOI] [PubMed] [Google Scholar]
- 7. Teichtahl AJ, Cicuttini FM, Abram F, et al. Meniscal extrusion and bone marrow lesions are associated with incident and progressive knee osteoarthritis. Osteoarthritis Cartilage 2017; 25:1076–1083. 10.1016/j.joca.2017.02.792. [DOI] [PubMed] [Google Scholar]
- 8. Swamy N, Wadhwa V, Bajaj G, Chhabra A, Pandey T. Medial meniscal extrusion: detection, evaluation and clinical implications. Eur J Radiol 2018; 102:115–124. 10.1016/j.ejrad.2018.03.007. [DOI] [PubMed] [Google Scholar]
- 9. Stehling C, Souza RB, MPH LG, et al. Loading of the knee during 3.0T MRI is associated with significantly increased medial meniscus extrusion in mild and moderate osteoarthritis. Eur J Radiol 2012; 81:1839–1845. 10.1016/j.ejrad.2011.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Nogueira‐Barbosa MH, Gregio‐Junior E, Lorenzato MM, et al. Ultrasound assessment of medial meniscal extrusion: a validation study using MRI as reference standard. AJR Am J Roentgenol 2015; 204:584–588. 10.2214/ajr.14.12522. [DOI] [PubMed] [Google Scholar]
- 11. Rowland G, Mar D, McIff T, Nelson J. Evaluation of meniscal extrusion with posterior root disruption and repair using ultrasound. Knee 2016; 23:627–630. 10.1016/j.knee.2016.04.008. [DOI] [PubMed] [Google Scholar]
- 12. Karpinski K, Diermeier T, Willinger L, Imhoff AB, Achtnich A, Petersen W. No dynamic extrusion of the medial meniscus in ultrasound examination in patients with confirmed root tear lesion. Knee Surg Sports Traumatol Arthrosc 2019; 27:3311–3317. 10.1007/s00167-018-5341-4. [DOI] [PubMed] [Google Scholar]
- 13. Irrgang JJ, Snyder‐Mackler L, Wainner RS, Fu FH, Harner CD. Development of a patient‐reported measure of function of the knee. J Bone Joint Surg Am 1998; 80:1132–1145. [DOI] [PubMed] [Google Scholar]
- 14. Rosner B. The Intraclass Correlation Coefficient. 7th ed. Boston, MA: Brooks/Cole, Cengage Learning; 2011. [Google Scholar]
- 15. Crema MD, Roemer FW, Felson DT, et al. Factors associated with meniscal extrusion in knees with or at risk for osteoarthritis: the multicenter osteoarthritis study. Radiology 2012; 264:494–503. 10.1148/radiol.12110986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Rechsteiner J, Hirschmann MT, Dordevic M, et al. Meniscal pathologies on MRI correlate with increased bone tracer uptake in SPECT/CT. Eur Radiol 2018; 28:4696–4704. 10.1007/s00330-018-5466-3. [DOI] [PubMed] [Google Scholar]
- 17. Berthiaume MJ, Raynauld JP, Martel‐Pelletier J, et al. Meniscal tear and extrusion are strongly associated with progression of symptomatic knee osteoarthritis as assessed by quantitative magnetic resonance imaging. Ann Rheum Dis 2005; 64:556–563. 10.1136/ard.2004.023796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Wang Y, Wluka AE, Pelletier JP, et al. Meniscal extrusion predicts increases in subchondral bone marrow lesions and bone cysts and expansion of subchondral bone in osteoarthritic knees. Rheumatology (Oxford) 2010; 49:997–1004. 10.1093/rheumatology/keq034. [DOI] [PubMed] [Google Scholar]
- 19. Bruno F, Barile A, Arrigoni F, et al. Weight‐bearing MRI of the knee: a review of advantages and limits. Acta Biomed 2018; 89:78–88. 10.23750/abm.v89i1-S.7011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Epstein D, Petersiel N, Klein E, et al. Pocket‐size point‐of‐care ultrasound in rural Uganda ‐ a unique opportunity "to see", where no imaging facilities are available. Travel Med Infect Dis 2018; 23:87–93. 10.1016/j.tmaid.2018.01.001. [DOI] [PubMed] [Google Scholar]
- 21. Shokoohi H, Raymond A, Fleming K, et al. Assessment of point‐of‐care ultrasound training for clinical educators in Malawi, Tanzania and Uganda. Ultrasound Med Biol 2019; 45:1351–1357. 10.1016/j.ultrasmedbio.2019.01.019. [DOI] [PubMed] [Google Scholar]
- 22. Falkowski AL, Jacobson JA, Freehill MT, Kalia V. Hand‐held portable versus conventional cart‐based ultrasound in musculoskeletal imaging. Orthop J Sports Med 2020; 8:1–7. 10.1177/2325967119901017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Crema MD, Hunter DJ, Roemer FW, et al. The relationship between prevalent medial meniscal intrasubstance signal changes and incident medial meniscal tears in women over a 1‐year period assessed with 3.0 T MRI. Skeletal Radiol 2011; 40:1017–1023. 10.1007/s00256-011-1097-3. [DOI] [PubMed] [Google Scholar]


