Abstract
Alexithymia has been associated with substance use, but the magnitude of the association has not been evaluated and sub‐group differences, if any, are unknown. The aim of this meta‐analysis is to systematically review the association between alexithymia and substance use (alcohol or illicit drugs). We identified studies through a systematic review of PubMed and Web of Science and obtained a total of 52 publications using the Toronto Alexithymia Scale‐20 scale. Random effects meta‐analysis was used to evaluate the overall and sub‐group associations. Of the studies, 50 were cross‐sectional and two longitudinal. Alexithymia was associated with any substance use (Cohen’s d = 0.62, 95% confidence interval [CI] 0.49–0.76), with little difference between estimates for use of alcohol or illicit drugs. A stronger association was observed for the alexithymia dimension “Difficulty in Identifying Feelings” (d = 0.64, 95% CI = 0.47–0.81) and “Difficulty in Describing Feelings” (d = 0.44, 95% CI = 0.32–0.55) than for “Externally Oriented Thinking” (d = 0.19, 95% CI = 0.09–0.28). The association was stronger in studies with clinical patient populations (d = 0.83, 95% CI = 0.62–1.05) than in those investigating general or student populations, and in studies with a majority of male rather than female participants. These findings suggest a strong overall association between alexithymia and substance use and a very strong association among clinical patient populations. The association may be stronger with the emotion‐related dimensions than with the cognition‐related dimension of alexithymia. As nearly all the studies were cross‐sectional, more longitudinal studies are needed.
Keywords: Alexithymia, alcohol, drinking behavior, drugs, meta‐analysis, substance use, TAS‐20
INTRODUCTION
Alexithymia was originally defined as the inability to recognize and verbalize emotions (Sifneos, 1973). A poverty of imagination or of a fantasy world as well as a lack of positive emotions and a high prevalence of negative emotions have also been described as characteristic of alexithymia (Taylor, 2018). Alexithymia is often viewed as a personality trait with a normal distribution among the population (Bagby, Parker & Taylor, 1994). The most commonly used scale for assessing alexithymia is the self‐reported Toronto Alexithymia Scale with 20 items (TAS‐20) (Bagby et al., 1994; Parker, Taylor & Bagby, 2003; Taylor, Bagby & Parker, 2003). TAS‐20 scale includess: Difficulty in Identifying Feelings (DIF), Difficulty in Describing Feelings to others (DDF), and Externally Oriented Thinking (EOT). The replicability of the three‐factor structure of TAS‐20 has been demonstrated in both clinical and non‐clinical populations and TAS‐20 has been translated into over twenty languages (Bressi, Taylor, Parker et al., 1996; Joukamaa, Miettunen, Kokkonen et al., 2001; Luminet, Olivier, Taylor & Bagby, 2018).
Substance use disorder (SUD) as a diagnosis in the DSM‐IV is a condition in which there is uncontrolled use of a substance (i.e., alcohol, cocaine, heroin, opioid, sedatives, or stimulants) despite harmful consequence (Livne, Shmulewitz, Stohl, Mannes, Aharonovich & Hasin, 2021). The alcohol abuse and other addiction problems has been shown to be associated with alexithymia (Thorberg, Young, Sullivan & Lyvers, 2009). The earliest studies found a high prevalence of alexithymia (40–50%) among patients diagnosed with alcohol abuse or dependence (Thorberg et al., 2009; Uzun, Ates, Cansever & Ozsahin, 2003).
In addition, several studies have reported a high prevalence of alexithymia among subjects with illicit drug abuse, El Raasheed (2001) showed that alexithymic heroin addict individuals reported more polysubstance abuse, more opiate use (other than heroin) and more benzodiazepine abuse than non‐alexihymic individuals. In addition, Payer, Lieberman and London (2011), and Hamidi, Rostami, Farhoodi and Abdolmanafi (2010) have reported higher levels of alexithymia in heroin dependent individuals compared to the healthy control group. Interestingly, Bulai and Enea (2016) compared three addictive groups (tobacco, cannabis, and alcohol) and found that the alcohol abusers have a significantly higher level of alexithymia than cannabis abusers, smokers, and controls. In addition, Ghalehban and Besharat (2011) found that patients with substance abuse disorder (without specifying the drug) score significantly higher TAS‐20 scores than normal individuals. Moreover, Patwardhan, Mason, Chmelka, Savolainen, Miettunen & Jarvelin (2019) found that none of the alexithymia domains was directly associated with substance use disorder (without specifying what drug the subjects have used) in adulthood among the Northern Finland Birth Cohort 1986, thus more information is needed to find out whether alexithymia is a trait which predisposes to alcohol or substance abuse.
Since then, two systematic literature reviews, and one meta‐analysis to date, have evaluated the relationship between alexithymia and alcohol use disorders (Pigoni, Mandolini, Delvecchio, Bressi, Soares & Brambilla, 2020; Thorberg et al., 2009). A recent meta‐analysis by Pigoni et al. (2020) evaluated the associations between non‐suicidal self‐injury (NSSI), risky drinking and alexithymia. They found 33 risky drink‐related articles. The results showed a significant positive association between TAS‐20 scores, DIF and DDF both NSSI and risky drinking. This association was stronger among ≥30 years of age. In addition, they found that EOT associated with risky drinking but not NSSI.
Thorberg et al. (2009) investigated the relationship between alexithymia and alcohol use disorder among alcohol‐dependent populations. They included 24 studies published between 1973 and 2008 in their systematic review and showed a higher prevalence rate of alexithymia in alcohol‐dependent populations compared with the control groups, and a positive relationship between alexithymia, The amount of alcohol use and severity of alcohol problems among the patient groups. Another systematic review, by Cruise and Becarra (2018), summarized findings from 30 studies published between 2009 and 2016. They found that alexithymia is an independent risk factor for alcohol‐related problems among clinical samples. Neither of the two systematic reviews performed a meta‐analysis to quantify the association between alexithymia and alcohol or drug use.
The aim of this study was to conduct a systematic review and meta‐analysis to update and further summarize the findings on the relationship between alexithymia and alcohol abuse and find out whether there are similar associations between alexithymia and drug use. In particular, we were interested in exploring whether some subtypes of alexithymia would be more strongly associated with abuse of alcohol or drugs than others.
We focus also on mediating variables. These included sample type (clinical, general etc. populations), age and sex distribution of the participants, and study region. We hypothesize that alexithymia is associated positively with alcohol and drug abuse and more strongly with DIF and DDF than EOT. We hypothesize that alexithymia is associated with both alcohol and drug abuse Furthermore, based on earlies findings (Pigoni et al., 2020; Thorberg et al., 2009), we hypothesize that alexithymia is associated with alcohol use and more strongly with alexithymia subtypes DIF and DDF rather than EOT. Furthermore, we hypotheses that drug use associated similarly to alexithymia as alcohol use. In addition, we hypotheses that this association is more common in clinical than population samples, and more common in males than in females. We hypothesize that participant's age (> 30 years) influences findings similarly as in Pigoni's et al. (2020) study.
METHODS
We followed the Prisma guidelines for systematic reviews and meta‐analyses (http://Prisma‐statement.org/PRISMAStatement/FlowDiagram).
Identification of the studies
We searched the PubMed and Web of Science databases for available publications from January 2000 to September (PubMed)/October (Web of Science) 2019. The search terms we used to identify suitable publications are shown in Supplementary Materials Table S1.
Selection of studies
The study was included in the meta‐analysis if it: (1) was a cross‐sectional, case–control or cohort study including adult individuals (≥ 18 years) with alexithymia and alcohol/drug use assessments; (2) used TAS‐20 to assesses alexithymia; and (3) reported estimates for the association between alexithymia and substance use (e.g., Pearson correlation, mean difference, odds ratio (OR), relative risk (RR)). In addition, patient populations were accepted if the study included a “healthy” comparison group. The selected articles had to be written in English and be published in a peer‐reviewed journal. The resulting abstracts were read through and were included in the meta‐analysis if they fulfilled the inclusion criteria. We did not include other types of addiction than substance use, thus excluding, for example, internet or game addiction. When multiple reports on the same data had been published, we chose the study which included the most informative estimates or was published first. In addition to the database searches, we searched the reference lists of the eligible studies for additional records.
Data extraction
The description of the study population (patients or general population), the size of the study groups, the age of subjects, proportion of males, length of follow‐up and the method used for measuring alexithymia were extracted from each report. Two reviewers (KH, MV) independently checked the estimates derived in the studies on the association between alexithymia and substance use.
Quality assessment
Quality of the studies was assessed with a 14‐item instrument by the Quality Assessment Tool for Observational cohort and Cross‐sectional‐sectional studies, which belongs to the study quality assessment tools by NIH (National Heart, Lung, and Blood Institute; https://www.nhlbi.nih.gov/health‐topics/study‐quality‐assessment‐tools) (Table S2). Each of the dimensions of study quality was scored “0” if the study “does not include risk of bias” and “1” if the study “includes risk of bias,” “CD” if this was not possible to determine, “NA” if the item was not applicable,” and “NR” if the information was not reported. In principle, a study cannot be determined as having high quality if there is risk of bias rated to any of the items.
Meta‐analytic procedure
As there were several types of analyses in the original publications (mean difference, correlation and odds ratios), we transformed all original estimates to standardized mean differences (Cohen's d) and their 95% confidence intervals. We expected to find heterogeneity between studies and therefore used random‐effects meta‐analysis to obtain pooled estimates for the retrieved studies. The magnitude of Cohen's d was considered low if d ≤ 0.3, medium if d = 0.31 to 0.5, high if d = 0.51 to 0.8, and very high if d ≥ 0.81 (Cohen, 1988). Heterogeneity between studies was assessed by the I 2 test and meta‐regression was used to assess subgroup differences. Replanned subgroup analyses included the following: (1) outcome (DIF, DDF, EOT dimensions); (2) sample type (general, student, clinical); (3) mean age of the participants (<30 vs. ≥30 years); (4) proportion male (≤50% vs. >50%); (5) region (Europe, USA, Australia, Asia, Africa); (6) substance type (alcohol vs. other); and (7) analysis type (mean difference, correlation, logistic regression). We examined possible publication bias using the Egger's test for small‐study effects and a funnel plot of the estimates against their standard errors (Egger, Schneider & Davey Smith, 1998). Stata 13.1 (StataCorp, College Station, Texas, USA) was used for all meta‐analyses.
RESULTS
Searches
The search process and its results are presented as a flow chart (Fig. 1). The searches identified a total of 1,993 documents to be screened, resulting in 1,821 after the removal of 172 duplicates. During the initial screening, the authors (KH and MV) independently assessed the titles and abstracts against the eligibility criteria. This screening resulted in a total of 117 records for a full text assessment. Any disagreements were discussed among the reviewers and resolved by consensus. The final dataset included 52 publications. One of the studies was found after manual searches of the reference lists of eligible studies (Zdankiewicz‐Ścigała & Ścigała, 2020). The reasons for the 65 exclusions were as follows: patient sample without a non‐patient comparison group (n = 30), review (n = 4) or letter (n = 3) without original data, another type of addiction, for example, internet addiction (n = 2), no effect estimates provided (n = 22), no alexithymia scale used (n = 1), the use of a modified version of TAS‐20 (e.g., TAS‐26, n = 2), and study not written in English (French, n = 1).
Fig. 1.
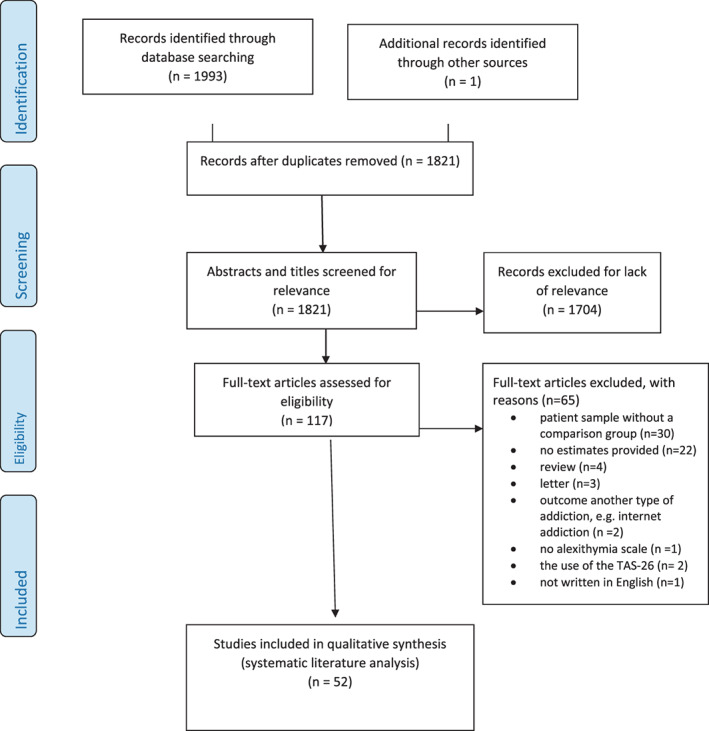
Flow diagram of the search stratyeg. [Colour figure can be viewed at wileyonlinelibrary.com]
Study populations
Descriptive statistics of the selected studies are presented in Table 1. In Table 1 the type of substance use has described in detail whenever it was possible. Several studies mentioned the diagnosed substance use disorder but did not specify the used substance (Bulai & Enea, 2016; Ghalehban & Besharat, 2011; Hamidi et al., 2010; Loas, Corcos, Stephan et al., 2001; Marchesi, Ossola, Tonna & De Panfilis, 2014; Parolin, Simonelli, Cristofalo et al., 2017; Patwardhan et al., 2019; Payer et al., 2011; Verrocchio, Conti & Fulcheri, 2010).
Table 1.
Descriptive statistics of the 52 studies examining the association between alexithymia and substance use
| Authors | Sample | Sample ‐type | N (controls) | Age | Male % | Country | The type of substance use | Adjusment |
|---|---|---|---|---|---|---|---|---|
| Andres et al. 2014 | Student | Cross‐sectional | 434 | 20 | 54 | France | The amount of alcohol use | none |
| Bashapoor et al. 2015 | Clinical | Case–control | 36 (36) | 30 | 100 | Iran | SUD a | sex, gender, age, employment |
| Bauer & Ceballos, 2014 | Student | Case control | 42 (55) | 19 | 0 | USA | Alcohol binge drinking | sex, gender |
| Betka et al. 2018 | General | Cross‐sectional | 600 | 27 | 26 | UK | Alcohol binge drinking | none |
| Bladt 2002 | Student | Cross‐sectional | 117 (122) | 19 | 33 (28) | USA | Alcohol binge drinking | sex, gender |
| Bruce et al. 2012 | Student | Cross‐sectional | 862 | 26 | 24 | UK | The amount of alcohol use | none |
| Bujarski et al. 2010 | Student | Cross‐sectional | 237 | 20 | 31 | USA | The amount of alcohol use | none |
| Bulai & Enea 2016 | Clinical | Case–control | 131 | 26 | 72 | Romania |
Cannabis use Alcohol abuse |
none |
| Chaudhury et al. 2006 | Clinical | Case–control | 100 (100) | 38 | 100 | India | AUD | age, sex, gender, region |
| Craparo et al. 2014 | Clinical | Case–control | 115 (117) | 44 | 51 | Italy | AUD | age, sex, gender |
| Craparo et al. 2016 | Clinical | Case–control | 31 (31) | 34 | 81 | Italy | AUD | age, sex, gender |
| Elander et al. 2014 | General | Cross‐sectional | 112 | 45 | 18 | UK | Pain‐killers misuse | none |
| Founta et al. 2019 | Clnical | Cross‐sectional | 184 | 46 | 68 | Ireland | AUD | none |
| Ghalehban & Beharat 2011 | Clinical | Case–control | 180 (180) | 31 | 95 | Iran | SUD a | age, sex, gender |
| Ghorbani et al. 2017 | Clinical | Case–control | 205 (100) | 31 | 75 | Iran | AUD | age, sex, gender |
| Gilan et al. 2015 | Students | Cross‐sectional | 250 (298) | 22 | 42 | Iran | Sedative use | none |
| Greene et al. 2020 | Students | Cross‐sectional | 183 (365) | 22 | 23 | Australia | Alcohol risky drinking | none |
| Hamidi et al. 2010 | Clinical | Case–control | 85 (85) | no | no | Iran | SUD a | age, sex, gender, SES |
| Hahn et al. 2016 | Students | Cross‐sectional | 425 | 19 | 29 | USA | The amount of alcohol use | none |
| Hasking & Claes 2020 | Students | Cross‐sectional | 951 | 22 | 20 | Australia | Risky use of alcohol | none |
| Honkalampi et al. 2010 | General | Prospective | 290 | 25–64 | 49 | Finland | AUD | sex, gender, age, self‐reported health, work ability, depression |
| Knapton et al. 2018 | General | Cross‐sectional | 138 | 32 | 43 | UK | The amount of alcohol use | none |
| Kopera et al. 2018 | Clinical | Case–control | 92 (86) | 40 | 70 | Poland | AUD | age, education, depression |
| Loas et al. 2000 | Clinical | Case–control | 60 (57) | 36 | 80 | France | AUD | age |
| Loas et al. 2001 | Clinical | Case–control | 659 (769) | 27 | 41 | France | SUD a | age, sex, gender |
| Lyvers et al. 2012a | General | Cross‐sectional | 262 | 27 | 32 | Australia | Alcohol risky drinking and alcohol use disorder | none |
| Lyvers et al. 2012b | General | Cross‐sectional | 314 | 28 | 46 | Australia | The amount of alcohol use | none |
| Lyvers et al. 2014a | Student | Cross‐sectional | 113 | 22 | 31 | Australia | The amount of alcohol use | none |
| Lyvers et al. 2014b | General | Cross‐sectional | 100 | 21 | 28 | Australia | The amount of alcohol use | none |
| Lyvers et al. 2014c | Clinical | Cross‐sectional | 207 | 30 | 58 | Australia | The amount of alcohol use | none |
| Lyvers et al. 2014d | Student | Cross‐sectional | 153 | 21 | 43 | Australia | SUD, 60% multiple users | none |
| Lyvers et al. 2018a | Student | Cross‐sectional | 126 | 21 | 40 | Australia | The amount of alcohol use | none |
| Lyvers et al. 2018b | General | Cross‐sectional | 155 | 22 | 48 | Australia | Alcohol risky drinking | none |
| Lyvers et al. 2018c | General | Cross‐sectional | 161 | 23 | 41 | Australia | The amount of alcohol use | none |
| Lyvers et al. 2019a | General | Cross‐sectional | 224 | 27 | 18 | Australia | The amount of alcohol use | none |
| Lyvers et al. 2019b | Student | Cross‐sectional | 97 | 22 | 31 | Australia | The amount of alcohol use | none |
| Lyvers et al. 2019c | General | Cross‐sectional | 291 | 26 | 39 | Australia | The amount of alcohol use | none |
| Lyvers et al. 2019d | General | Cross‐sectional | 143 | 26 | 52 | Australia | The amount of alcohol use | age, sex, gender, social desirability, personality |
| Marchesi et al. 2014 | Clinical | Case–control | 30 (78) | 35 | 36 | Italy | SUD (cocaine, heroin, multiple use) | age, sex, gender, education, anxiety, depression |
| Maurage et al. 2011 | Clinical | Case–control | 30 (30) | 45 | 60 | Belgium | AUD | age, sex, education |
| Maurage et al. 2017 | Clinical | Case–control | 296 (246) | 48 | 72 | Belgium | AUD | age, sex, gender |
| Meziou et al. 2019 | Clinical | Case–control | 50 (50) | 35 | 100 | Tunisia | Buprenorphine addiction | age, sex, gender, education |
| Parolin et al. 2017 | Clinical | Case–control | 41(27) | 21 | 47 | Italy | Polydrug users | age, sex, gender |
| Patwardhan et al. 2019 | General | Longitude | 6,186 | 28 | 49 | Finland | SUD a | age, sex, gender |
| Payer et al. 2011 | Clinical | Case–control | 31(27) | 32 | 55 | Italy | Methamphetamine users | age, sex, gender |
| Pedersen et al. 2016 | Physicians | Cross‐sectional | 1841 | 30–60 | 50 | Denmark | Risky use of alcohol | age, sex, gender |
| Rasheed 2001 | Clinical | Case–control | 200 (200) | 27 | 100 | Egypt | SUD a (mostly opioids) | age, sex, gender, sociodemographic status |
| Shishido et al. 2013 | Student | Cross‐sectional | 429 | 20 | 31 | USA | The amount of alcohol use | none |
| Speranza et al. 2004 | Clinical | Case–control | 208/123/controls | 37 | 72/63 | France | Alcohol/illicit drugs | age, sex, gender, SES |
| Verrocchio et al. 2010 | Clinical | Case–control | 77 (77) | 29 | 100 | Italy | Opioid's dependence | age, sex, gender |
| Zdankiewicz‐Ścigała & Ścigała, 2018 | Clinical | Control Cross‐sectional | 201 | 33 | 67 | Poland | AUD | none |
| Zdankiewicz‐Ścigała & Ścigała, 2020 | Clinical | Case–control | 167 (90) | 39 | 57 | Poland | AUD | age |
SUD, Substance use disorder, but not specified any drugs; AUD, alcohol use disorder/dependence/addiction.
All publications reported cross‐sectional findings, with the exception of two Finnish studies (Honkalampi, Koivumaa‐Honkanen, Lehto et al., 2010; Patwardhan et al., 2019). A total of 22,712 individuals had participated in these studies, the number of participants in individual studies varying between 29 (Lyvers, Hayatbakhsh, Stalewski & Thorberg, 2019e) and 6,963 (Patwardhan et al., 2019). The majority, 23 studies, included clinical samples (Bulai & Enea, 2016; Chaudhury, Das & Ukil, 2006; Hamidi et al., 2010; Loas, Otmani, Lecercle & Jouvent, 2000; Loas et al., 2001; Lyvers, Hinton, Gotsis, Roddy, Edwards & Thorberg, 2014d; Meziou, Ghali, Khelifa et al., 2019; Parolin et al., 2017; Payer et al., 2011; Rasheed, 2001; Speranza, Corcos, Stephan et al., 2004; Verrocchio et al., 2010; Zdankiewicz‐Ścigała & Ścigała, 2018; Zdankiewicz‐Ścigała & Ścigała, 2020).
Thirteen investigations consisted of participants from the general population (Betka, Pfeifer, Garfinkel et al., 2018; Elander, Duarte, Maratos & Gilbert, 2014; Honkalampi et al., 2010; Knapton, Bruce & Williams, 2018; Lyvers,, Onuoha, Thorberg & Samios, 2012b; Lyvers, Mayer, Needham & Thorberg, 2019c; Lyvers, Hasking, Albrecht & Thorberg, 2012a; Lyvers, Makin, Toms, Thorberg & Samios, 2014c; Lyvers, Simons, Hayes & Thorberg, 2014b; Lyvers, Coundouris, Edwards & Thorberg, 2018b; Lyvers, Narayanan & Thorberg, 2019d; Lyvers, et al., 2019c; Patwardhan et al., 2019) and thirteen were based on student populations (Andres, Castanier & Le Scanff, 2014; Bauer & Ceballos 2014; Bladt, 2002; Bruce, Curren & Williams, 2012; Bujarski, Klanecky & McChargue, 2010; Gilan, Zakiei, Reshadat, Komasi & Ghasemi, 2015; Greene, Hasking & Boyes, 2020; Hahn, Simons & Simons, 2016. Lyvers et al., 2014d; Lyvers, Lysychka & Thorberg, 2014a; Lyvers, Hanigan & Thorberg 2018a, Lyvers, Mayer, Needham & Thorberg, 2019b, Shishido, Gaher & Simons, 2013).
The majority of the studies concerned alcohol use or alcohol disorders (n = 36) (Andres et al., 2014; Bauer & Ceballos 2014; Betka et al., 2018; Bladt, 2002; Bruce et al., 2012; Bujarski et al., 2010; Bulai & Enea, 2016; Chaudhury et al., 2006; Craparo, Ardino, Gori & Caretti, 2014; Founta, Adamzik, Tobin, Kirby & Hevey, 2019; Ghorbani, Khosravani, Sharifi Bastan & Jamaati Ardakani, 2017; Greene et al., 2020; Hahn et al., 2016; Hasking & Claes, 2020; Honkalampi et al., 2010; Knapton et al., 2018, Kopera, Trucco, Jakubczyk et al., 2018; Loas et al., 2000; Lyvers et al., 2012a, 2012b; Lyvers, et al., 2014a, 2014b, 2014c, 2018a, 2018b, 2019b, 2019c, 2019d; Lyvers, McCann, Coundouris, Edwards & Thorberg, 2018c; Lyvers et al., 2019c; Maurage, Grynberg, Noel et al., 2011; Pedersen, Sorensen, Bruun, Christensen & Vedsted, 2016; Shishido et al., 2013; Speranza et al., 2004; Zdankiewicz‐Ścigała & Ścigała, 2018; Zdankiewicz‐Ścigała & Ścigała, 2020) or both alcohol and drug use (n = 1) (Speranza et al., 2004). Seven studies included patients with drug use (heroin) (Craparo et al., 2016; Meziou et al., 2019; Parolin et al., 2017; Bashapoor, Hosseini‐Kiasari, Daneshvar & Kazemi‐Taskooh, 2015), cannabis use (Bulai & Enea, 2016), sedative use (Gilan et al., 2015) and methamphetamine use (Payer et al., 2011). A total of 28 studies included young participants with a mean age of 30 years or less and in 24 studies the proportion of males was over 50%. Some of the studies produced findings for the TAS‐20 total score only, some for the dimension only, and some for both the TAS‐20 total score and the dimension. Thus, the number of studies providing data for each of the outcomes varied between 28 and 46.
Almost half of the studies (n = 24) were from Europe, 10 studies were from Australia, five from USA, five from Asia, and two from Africa (Table 1). Most of the studies reported results for more than one alexithymia score, for example TAS‐20 total score and all three dimensions.
After the quality assessment of the eligible studies, we concluded that the overall quality of studies was poor or fair, mainly because of the cross‐sectional study design, which was one of the aspects increasing the risk of bias in the quality assessment tool (Table S2).
Association between alexithymia and substance use
There was a total of 46 estimates for the TAS‐20 total score. Meta‐analysis (Fig. 2) suggested a strong positive association between alexithymia and any substance use (d = 0.62, 95% CI 0.49–0.76), with high heterogeneity between studies (I 2 = 92.1%). Despite the high heterogeneity, all but one of the studies showed a positive association between alexithymia and substance use (Bulai & Enea, 2016). Two clinical studies suggested a very strong positive association and were seen as outliers (Ghorbani et al., 2017; Rasheed, 2001). Removing these two studies did not significantly alter the results (d = 0.54, 95% CI 0.44–0.63, I 2 = 81.4%).
Fig. 2.
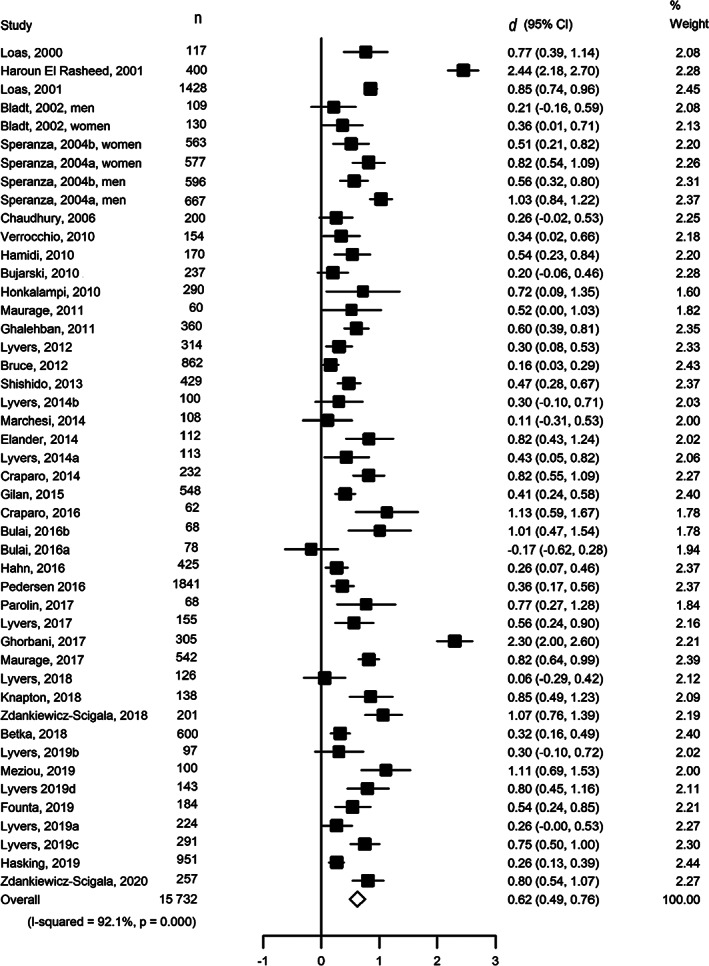
Association between alexithymia (TAS‐20 total score) and substance use.
Results from the sub‐group analyses are presented in Fig. 3. Even within the sub‐groups, heterogeneity between studies was high. Only the 11 studies among student populations suggested no heterogeneity (I 2 = 15.5, P = 0.296), as well as the five studies carried out in the USA (I 2 = 0.0, P = 0.424) and the two studies with logistic regression as analysis type (I 2 = 10.9, P = 0.290).
Fig. 3.
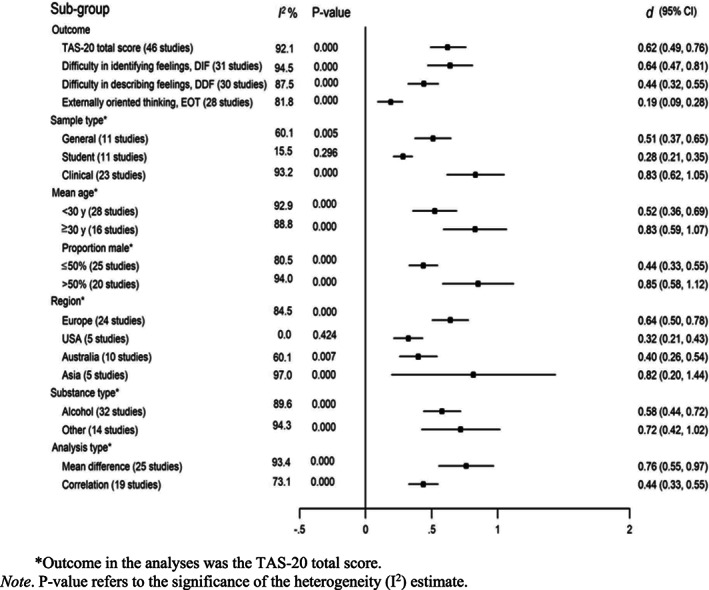
Sub‐group analyses of the association between alexithymia and substance use.
With regard to the outcome type, the estimate for Difficulty in Identifying Feelings (DIF) was of the same magnitude (d = 0.64, 95% CI 0.47–0.81) as the TAS‐20 total score, whereas the estimates for Difficulty in Describing Feelings (DDF) and Externally Oriented Thinking (EOT) were lower in magnitude (d = 0.44, 95% CI 0.32–0.55 and d = 0.19, 95% CI 0.09–0.28), with a statistically significant interaction found in meta‐regression (P = 0.025).
There was also a significant interaction among sample types (P = 0.049). Clinical samples yielded higher estimates than student samples (d = 0.83, 95% CI 0.62–1.05 versus d = 0.28, 95% CI 0.21–0.35), whereas studies from general populations gave estimates between these two (d = 0.51, 95% CI 0.37–0.65).
There was no significant difference between studies regarding age of the participants (P = 0.051 for interaction in meta‐regression), but those with a higher proportion of male participants suggested a stronger association between alexithymia and substance use (P = 0.004; d = 0.44, 95% CI 0.33–0.55 when the proportion of men was ≤50% and d = 0.85, 95% CI 0.58–1.12 when the proportion of men was >50%). Other subgroup differences (region, substance type and analysis type) were small (P ‐values for interaction 0.130, 0.375 and 0.051, respectively).
Study‐specific forest plots for the association of alexithymia with alexithymia dimensions DIF, DDF and EOT are presented in Figs. [Link], [Link]. The funnel plot for the TAS‐20 total score results appears symmetric (Fig. S4), and there was no evidence of an association between study size and the estimates (Egger's test B = 1.07; P = 0.42), not even after exclusion of the two outlier estimates from the analysis (B = 0.40, P = 0.65).
DISCUSSION
This meta‐analysis confirmed a strong association between alexithymia and substance use and identified some subgroup differences in the association. We identified 52 studies that provided estimates for the association between alexithymia and/or its dimension, and substance use measured by alcohol or illicit drug use. We found a strong positive association between alexithymia and any substance use (d = 0.62), and in the dimension the association appeared to be strongest for Difficulty in Identifying Feelings (DIF, d = 0.64), followed by Difficulty in Describing Feelings (DDF, d = 0.44), and the weakest association for Externally Oriented Thinking (EOT, d = 0.19). The associations for alcohol use and illicit drug use were similar, whereas the strongest association was found in studies with clinical patient populations. Alexithymia was also more strongly associated with substance use in studies with most male participants.
A previous systematic review (without meta‐analysis) (Pigoni et al., 2020) found a relationship between severity of alcohol use disorder and alexithymia among patients with alcohol use disorders. Another review (Thorberg, et al., 2009) summarized that alexithymia may have the potential to interfere with treatment outcomes among alcohol‐dependent patients. A previous meta‐analysis (Pigoni et al., 2020) showed that EOT was associated with risky drinking but not NNSI. We included all relevant study types which provided estimates for the association between alexithymia and any substance use and found, in line with previous research, that the association may be stronger among patients with severe alcohol use disorders than among the general population or students. The reasons for this finding may be related to bi‐directional impacts, that is, in addition to alexithymia increasing alcohol use, alcoholism involves a tendency to affect personality, including alexithymic traits, in a negative way (Kauhanen, Julkunen & Salonen, 1992). In addition, the association between alexithymia and substance use was stronger in older (≥ 30 years) participants, which is noted in an earlier study (Pigoni et al., 2020). Interestingly, a community‐based study showed, that affective symptoms are common in severe alcohol use disorders and it may promote further heavy drinking (Ehlers, Gilder, Gizer & Wilhelmsen, 2019). In addition, many studies have shown that probabilities of having an alcohol use disorder among those with a drug use disorder is significantly greater than among those without a drug use disorder and vice versa (Simons, Carey & Wills, 2009; Stinson, Grant, Dawson, Ruan, Huang & Saha, 2005). However, because almost all the studies were cross‐sectional, we could not test temporal order in associations to evaluate the direction of causality. Moreover, even though we found a strong association between alexithymia and the abuse of substances other than alcohol, it should be noted that due to insufficient data available for analyses we were unable to conduct individual analyses for substances other than alcohol. As different types of drugs have different impact on the central nervous system and consequently behavior, sedatives such as opioids, (i.e., heroin, buprenorphine) and stimulants (cocaine, methamphetamine), are likely to have different types of associations with alexithymic features. Therefore, our findings regarding the association between alexithymia and the use of substances other than alcohol should be approached with caution.
The reasons for the stronger association among male‐dominated studies are unknown but may reflect the fact that of the studies reporting results for the TAS‐20 total score, 77% of clinical studies were male‐dominated whereas the corresponding proportion of men in the general and student populations were 10% and 9%, respectively. There is a body of literature on male alexithymia, with a hypothesis of “normative male alexithymia” in the socialization process, which means that men have been discouraged from expressing their emotions during their development and this may have made them more vulnerable than women (Levant, Allen & Lien, 2019). In addition, Luminet, de Sousa Uva, Fantini and de Timary (2016) investigated a group of alcohol‐dependent patients and found a positive interaction between depression and gender in the prediction of craving for alcohol. For women, the link between depression and craving was associated with scoring higher on “difficulties describing feelings” but in men this link scored higher on “externally‐oriented thinking.” Further research is therefore needed to examine whether it is the clinical status that determines the association between alexithymia and substance use or whether there is actually a stronger association among men than women.
We found stronger associations of substance use with the emotion‐related dimensions (DIF and DFF) than with the cognition‐related dimension (EOT) of alexithymia. Several studies among patients with substance use disorder (Thorberg, et al., 2010) and psychiatric inpatients (Preece, Becerra, Robinson, Dandy & Allan, 2018) have found acceptable internal consistency, test–retest reliability and scale homogeneity for TAS‐20, but not in EOT scale. Similarly, a previous meta‐analysis based on 19 studies (Li, Zhang, Guo, Zhang 2015) revealed a positive association between depression and the TAS‐20 total score, DIF, and DDF, and a weak association was found between EOT and depressive symptoms. Previous longitudinal studies have shown that among recovering psychiatric patients, DIF and DDF scores decreased along with the alleviation of psychiatric symptoms, whereas EOT remained unchanged (Honkalampi, De Berardis, Vellante & Viinamäki, 2018; Rufer, Albrecht, Zaum et al., 2010; Saarijärvi, Salminen & Toikka, 2001). It is not clear why DIF and DDF are more closely related to mental and substance use disorders while the association with externally oriented thinking is weaker. Probably DIF and DDF may be more state‐dependent than EOT (Henry, Phillips, Maylor, Hosie, Milne & Meyer, 2006). People with high DIF scores have difficulties in identifying their feelings, that is, they often just feel somatic sensations and undifferentiated feelings of distress. Those with high levels of DDF, in turn, have difficulties in describing feelings, which makes their social interaction difficult as they are not able to verbalize (Luminet & Zamariola, 2018) their emotions to others and may not seek social support from other people. These characteristics may lead to escape‐avoidance coping strategies, such as high amount of alcohol use (Skrzynski & Creswell, 2020). A recent study among patients with substance use disorder (Taurino, Antonucci, Taurisano & Laera, 2021) showed that among all SUD sub‐groups (cocaine use disorder, opioid use disorder, alcohol use disorder (AUD)), patients with AUD, patients showed more dysfunctional defenses, all patients used a maladaptive/assimilation defense style, which is related to the DIF factor, and to a worse psychological functioning.
Among different regions, very strong association between alexithymia and substance use was found for studies from Asia (n = 5, d = 0.82, 95%CI 0.20–1.44), a strong association for studies from Europe (n = 24, d = 0.64, 95% < CI 0.50–0.78), and only a medium association for studies from Australia (n = 10, d = 0.40, 95%CI 0.26–0.54) and USA (n = 5, d = 0.32, 95%CI 0.21–0.43) (p = 0001). However, these sub‐group differences (region, substance type, analysis type) were imprecisely estimated and the meta‐regression analyses did not suggest significant interaction. Based on the present evidence, there is no clear evidence of differences in the association between alexithymia and substance use between different countries, when the outcome is alcohol or illicit drug use, or depending on the chosen analysis type in the study.
Clinical implications
This meta‐analysis showed that alexithymia and especially its dimensions DIF and DDF have a strong positive association between any substance use. So far, there is some evidence that alexithymia worsens treatment outcomes in individuals with alcohol abuse or dependence. Higher levels of alexithymia have been found to be associated with a higher rate of relapse among alcoholics (Birt, Sandor, Vaida & Birt, 2008). In this study, the associations for alcohol use and illicit were strongest among studies with the patient populations and male participants. de Haan, van der Palen, Wijdeveld, Buitelaar and De Jong (2014) found in a three‐week follow‐up among patients with substance use disorders that the scores of the TAS‐20 may be partly related to an addiction as a temporary state but it can also be a stable trait. There is some evidence that the treatment outcome of substance use patients with alexithymia depends on treatment modality among individuals with addiction. For example, Morie, Nich, Hunkele, Potenza & Carroll (2015) showed that methadone‐maintained cocaine abusers with high alexithymia respond better to computerized Cognitive Behavioral Therapy for drug dependence than individuals with low alexithymia. This evidence shows that cognitive style, for example, their difficulty to describe feelings to a therapist, can be one of the underlying explanations regarding the differences in the ability to benefit from therapeutic treatment (Morie & Ridout, 2018).
Strengths and limitations
This meta‐analysis examined alexithymia and substance use in a wide variety of studies. Other strengths of this review include examination of the associations for alexithymia sub‐scales as well as several predefined subgroups, in addition to the overall alexithymia score and total population. However, there are also important limitations that should be acknowledged. First, only two databases were used to select studies, but both PubMed and Web of Science databases are very compressive. However, in addition to that, we searched the reference lists of the eligible studies for additional records. Second, the quality of studies was rated only fair to poor, mainly due to the study design which was cross‐sectional in the majority of studies. Alexithymia was based on self‐reports in all studies, and in many studies the use of alcohol was also based on self‐report–although in clinical studies with patient populations alcohol use disorder was clinically verified. Self‐report of both the exposure and the outcome may involve common method bias, which artificially inflates associations. Furthermore, bias due to unmeasured confounding cannot be ruled out in observational studies. Due to these limitations, this meta‐analysis does not allow us to make causal conclusions regarding the relationships between alexithymia and substance use. Third, we found a high level of heterogeneity between studies although all but one of them suggested a positive association between alexithymia and substance use. Investigation of this issue in subgroups provided little additional information on the potential causes of heterogeneity; only sub‐group analyses restricted to student populations (n = 11), to those carried out in the USA (n = 5) and to investigations based on logistic regression analysis as a method (n = 2) did not suggest high heterogeneity. Many small meta‐analyses are not able to estimate heterogeneity with much precision; in fact, we may have little confidence in any estimate beyond the average effect size, thus any statistical analysis cannot change the limitations of small meta‐analyses (see von Hippel, 2015). Further studies are needed to examine what factors may underlie the observed heterogeneity. Furthermore, most studies were from high‐income countries, which limits the generalizability of the findings to low‐ or middle‐income countries.
CONCLUSIONS
The findings of this systematic review and meta‐analysis suggest a strong association between alexithymia and substance use, and a very strong association among patients with alcohol use disorders. The association may be stronger for the emotion‐related dimensions than for the cognition‐related dimension of alexithymia. More longitudinal studies are needed to test the direction of causality between alexithymia and substance use.
MK was supported by the UK Medical Research Council (grant MRC S011676), the US National Institute on Aging (NIA) (grant R01AG056477), the Academy of Finland (311492), NordForsk (grant 70521, the Nordic Research Programme on Health and Welfare), and the Finnish Work Environment Fund (190424), outside the area of this study.
Supporting information
Figure S1. Study‐specific associations between Difficulty in Identifying Feelings sub‐score of alexithymia and substance use.
Figure S2. Study‐specific associations between Difficulty in Describing Feelings sub‐score of alexithymia and substance use.
Figure S3. Study‐specific associations between Externally Oriented Thinking sub‐score of alexithymia and substance use.
Figure S4. The funnel plot for the TAS‐20 total score.
Table S1. Search terms for the search in PubMed.
Table S2. Quality assessment of the studies in meta‐analysis.
Supplementary material
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analyzed in this study.
References
- Andres, F. , Castanier, C. & Le Scanff, C. (2014). Attachment and alcohol use amongst athletes: The mediating role of conscientiousness and alexithymia. Addictive Behaviors, 39, 487–490. [DOI] [PubMed] [Google Scholar]
- Bagby, R.M. , Parker, J.D.A. & Taylor, G.J. (1994). The twenty‐item Toronto Alexithymia scale—I. Item selection and cross‐validation of the factor structure. Journal of Psychosomatic Research, 38(1), 23–32. 10.1016/0022-3999(94)90005-1 [DOI] [PubMed] [Google Scholar]
- Bashapoor, S. , Hosseini‐Kiasari, S.T. , Daneshvar, S. & Kazemi‐Taskooh, Z. (2015). Comparing sensory information processing and alexithymia between people with substance dependency and normal. Addiction & Health, 7, 174–183. [PMC free article] [PubMed] [Google Scholar]
- Bauer, L.O. & Ceballos, N.A. (2014). Neural and genetic correlates of binge drinking among college women. Biological Psychology, 97, 43–48. 10.1016/j.biopsycho.2014.01.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betka, S. , Pfeifer, G. , Garfinkel, S. , Prins, H. , Bond, R. , Sequeira, H. et al. (2018). How do self‐assessment of alexithymia and sensitivity to bodily sensations relate to alcohol consumption? Alcoholism, Clinical and Experimental Research , 42, 81–88. [DOI] [PubMed] [Google Scholar]
- Birt, M.A. , Sandor, V. , Vaida, A. & Birt, M.E. (2008). Alexithymia, a risk factor in alcohol addiction? A brief research report on romanian population. Journal of Cognitive and Behavioral Psychotherapies. 8(2), 217–225. [Google Scholar]
- Bladt, C.W. (2002). Towards a psychodynamic understanding of binge drinking behavior in first‐semester college freshmen. Journal of College Student Development, 43, 775–791. [Google Scholar]
- Bressi, C. , Taylor, G. , Parker, J. , Bressi, S. , Brambilla, V. , Aguglia, E. et al. (1996). Cross validation of the factor structure of the 20‐item toronto alexithymia scale: An italian multicenter study. Journal of Psychosomatic Research , 41, 551–559. doi: 10.1016/s0022-3999(96)00228-0 [DOI] [PubMed] [Google Scholar]
- Bruce, G. , Curren, C. & Williams, L. (2012). Alexithymia and alcohol consumption: The mediating effects of drinking motives. Addictive Behaviors, 37, 350–352. [DOI] [PubMed] [Google Scholar]
- Bujarski, S.J. , Klanecky, A.K. & McChargue, D.E. (2010). The relationship between alexithymia and alcohol‐related risk perceptions: The moderating effect of general trauma in a college population. Addictive Behaviors, 35(4), 363–366. 10.1016/j.addbeh.2009.10.023 [DOI] [PubMed] [Google Scholar]
- Bulai, I. & Enea, V. (2016). Dissociation and alexithymia in a romanian sample of substance abuse patients. Journal of Substance Use, 21, 646–651. [Google Scholar]
- Chaudhury, S. , Das, S.K. & Ukil, B. (2006). Psychological assessment of alcoholism in males. Indian Journal of Psychiatry, 48(2), 114. 10.4103/0019-5545.31602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen, J. (1988). Statistical power analysis for the behavioral sciences, 2nd edition. Hillsdale, NJ: Erlbaum. [Google Scholar]
- Craparo, G. , Ardino, V. , Gori, A. & Caretti, V. (2014). The relationships between early trauma, dissociation, and alexithymia in alcohol addiction. Psychiatry Investigation, 11, 330–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craparo, G. , Gori, A. , Dell'Aera, S. , Costanzo, G. , Fasciano, S. , Tomasello, A. et al. (2016). Impaired emotion recognition is linked to alexithymia in heroin addicts. PeerJ, 4, e1864. 10.7717/peerj.1864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cruise, K.E. & Becerra, R. (2018). Alexithymia and problematic alcohol use: A critical update. Addictive Behaviors, 77, 232–246. [DOI] [PubMed] [Google Scholar]
- de Haan, H.A. , van der Palen, J. , Wijdeveld, T.G. , Buitelaar, J.K. & De Jong, C.A. (2014). Alexithymia in patients with substance use disorders: State or trait? Psychiatry Research, 216, 137–145. [DOI] [PubMed] [Google Scholar]
- Ehlers, C.L. , Gilder, D.A. , Gizer, I.R. & Wilhelmsen, K.C. (2019). Indexing the “dark side of addiction”: Substance‐induced affective symptoms and alcohol use disorders. Addiction (Abingdon, UK), 114, 139–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elander, J. , Duarte, J. , Maratos, F.A. & Gilbert, P. (2014). Predictors of painkiller dependence among people with pain in the general population. Pain Medicine (Malden, MA), 15, 613–624. [DOI] [PubMed] [Google Scholar]
- Founta, O. , Adamzik, K. , Tobin, A. , Kirby, B. & Hevey, D. (2019). Psychological distress, alexithymia and alcohol misuse in patients with psoriasis: A cross‐sectional study. Journal of Clinical Psychology in Medical Settings, 26, 200–219. [DOI] [PubMed] [Google Scholar]
- Ghalehban, M. & Besharat, M.A. (2011). Examination and comparison of alexithymia and self‐regulation in patients with substance abuse disorder and normal individuals. Procedia ‐ Social and Behavioral Sciences, 30, 38–42. 10.1016/j.sbspro.2011.10.008 [DOI] [Google Scholar]
- Ghorbani, F. , Khosravani, V. , Sharifi Bastan, F. & Jamaati Ardakani, R. (2017). The alexithymia, emotion regulation, emotion regulation difficulties, positive and negative affects, and suicidal risk in alcohol‐dependent outpatients. Psychiatry Research, 252, 223–230. [DOI] [PubMed] [Google Scholar]
- Gilan, N.R. , Zakiei, A. , Reshadat, S. , Komasi, S. & Ghasemi, S.R. (2015). Perceived stress, alexithymia, and psychological health as predictors of sedative abuse. Korean Journal of Family Medicine, 36(5), 210. 10.4082/kjfm.2015.36.5.210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greene, D. , Hasking, P. & Boyes, M. (2020). The associations between alexithymia, non‐suicidal self‐injury, and risky drinking: The moderating roles of experiential avoidance and biological sex. Stress and Health, 260, 140–166. 10.1002/smi.2879 [DOI] [PubMed] [Google Scholar]
- Hahn, A.M. , Simons, R.M. & Simons, J.S. (2016). Childhood maltreatment and sexual risk taking: The mediating role of alexithymia. Archives of Sexual Behavior, 45, 53–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamidi, S. , Rostami, R. , Farhoodi, F. & Abdolmanafi, A. (2010). A study and comparison of alexithymia among patients with substance use disorder and normal people. Procedia ‐ Social and Behavioral Sciences, 5, 1367–1370. [Google Scholar]
- Hasking, P. & Claes, L. (2020). Transdiagnostic mechanisms involved in nonsuicidal self‐injury, risky drinking and disordered eating: Impulsivity, emotion regulation and alexithymia. Journal of American College Health, 68(6), 603–609. 10.1080/07448481.2019.1583661 [DOI] [PubMed] [Google Scholar]
- Henry, J.D. , Phillips, L.H. , Maylor, E.A. , Hosie, J. , Milne, A.B. & Meyer, C. (2006). A new conceptualization of alexithymia in the general adult population: Implications for research involving older adults. Journal of Psychosomatic Research, 60, 535–543. [DOI] [PubMed] [Google Scholar]
- Honkalampi, K. , De Berardis, D. , Vellante, F. & Viinamäki, H. (2018). Relations between alexithymia and depressive and anxiety disorders and personality. In Luminet O., Bagby R.M. & Taylor G.J. (Eds.), Alexithymia. advances in research, theory and clinical practise (pp. 142–157). Cambridge: Cambridge University Press. 10.1017/9781108241595.001 [DOI] [Google Scholar]
- Honkalampi, K. , Koivumaa‐Honkanen, H. , Lehto, S.M. , Hintikka, J. , Haatainen, K. , Rissanen, T. et al. (2010). Is alexithymia a risk factor for major depression, personality disorder, or alcohol use disorders? A prospective population‐based study. Journal of Psychosomatic Research, 68, 269–273. [DOI] [PubMed] [Google Scholar]
- Joukamaa, M. , Miettunen, J. , Kokkonen, P. , Koskinen, M. , Julkunen, J. , Kauhanen, J. et al. (2001). Psychometric properties of the finnish 20‐item toronto alexithymia scale. Nordic Journal of Psychiatry , 55, 123–127. [DOI] [PubMed] [Google Scholar]
- Kauhanen, J. , Julkunen, J. & Salonen, J.T. (1992). Coping with inner feelings and stress: Heavy alcohol use in the context of alexithymia. Behavioral Medicine (Washington, DC), 18, 121–126. [DOI] [PubMed] [Google Scholar]
- Knapton, C. , Bruce, G. & Williams, L. (2018). The impact of alexithymia on desire for alcohol during a social stress test. Substance Use & Misuse, 53, 662–667. [DOI] [PubMed] [Google Scholar]
- Kopera, M. , Trucco, E. M. , Jakubczyk, A. , Suszek, H. , Michalska, A. , Majewska, A. et al. (2018). Interpersonal and intrapersonal emotional processes in individuals treated for alcohol use disorder and non‐addicted healthy individuals. Addictive Behaviors , 79, 8–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levant, P. F. , Allen, P. A. & Lien, M. C. (2019). “Alexithymia in men: How and when do emotional processing deficiencies occur?” correction to Levant et al. (2014). Psychology of Men & Masculinity, 20, 636.
- Li, S. , Zhang, B. , Guo, Y. & Zhang, J. (2015). The association between alexithymia as assessed by the 20‐item toronto alexithymia scale and depression: A meta‐analysis. Psychiatry Research, 227, 1–9. [DOI] [PubMed] [Google Scholar]
- Livne, O. , Shmulewitz, D. , Stohl, M. , Mannes, Z. , Aharonovich, E. & Hasin, D. (2021). Agreement between DSM‐5 and DSM‐IV measures of substance use disorders in a sample of adult substance users. Drug and Alcohol Dependence, 227, 108958. 10.1016/j.drugalcdep.2021.108958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loas, G. , Corcos, M. , Stephan, P. , Pellet, J. , Bizouard, P. , Venisse, J. L. et al. (2001). Factorial structure of the 20‐item toronto alexithymia scale: Confirmatory factorial analyses in nonclinical and clinical samples. Journal of Psychosomatic Research , 50, 255–261. [DOI] [PubMed] [Google Scholar]
- Loas, G. , Otmani, O. , Lecercle, C. & Jouvent, R. (2000). Relationships between the emotional and cognitive components of alexithymia and dependency in alcoholics. Psychiatry Research, 96(1), 63–74. 10.1016/s0165-1781(00)00189-x [DOI] [PubMed] [Google Scholar]
- Luminet, O. , de Sousa, C. , Uva, M. , Fantini, C. & de Timary, P. (2016). The association between depression and craving in alcohol dependency is moderated by gender and by alexithymia factors. Psychiatry Research, 239, 28–38. [DOI] [PubMed] [Google Scholar]
- Luminet, O. , Taylor, G. J. & Bagby, R. M. (2018). Alexithymia: Advances in research, theory, and clinical practice. Cambridge: Cambridge University Press. [Google Scholar]
- Lyvers, M. , Brown, T. & Thorberg, F.A. (2019a). Is it the taste or the buzz? alexithymia, caffeine, and emotional eating. Substance Use & Misuse, 54, 572–582. [DOI] [PubMed] [Google Scholar]
- Lyvers, M. , Hanigan, C. & Thorberg, F.A. (2018a). Social interaction anxiety, alexithymia, and drinking motives in australian university students. Journal of Psychoactive Drugs, 50, 402–410. [DOI] [PubMed] [Google Scholar]
- Lyvers, M. , Mayer, K. , Needham, K. & Thorberg, F.A. (2019b). Parental bonding, adult attachment, and theory of mind: A developmental model of alexithymia and alcohol‐related risk. Journal of Clinical Psychology, 75, 1288–1304. [DOI] [PubMed] [Google Scholar]
- Lyvers, M. , Onuoha, R. , Thorberg, F.A. & Samios, C. (2012b). Alexithymia in relation to parental alcoholism, everyday frontal lobe functioning and alcohol consumption in a non‐clinical sample. Addictive Behaviors, 37, 205–210. [DOI] [PubMed] [Google Scholar]
- Lyvers, M. , Coundouris, S. , Edwards, M.S. & Thorberg, F.A. (2018b). Alexithymia, reward sensitivity and risky drinking: The role of internal drinking motives. Addiction Research & Theory, 26, 114–122. [Google Scholar]
- Lyvers, M. , Hasking, P. , Albrecht, B. & Thorberg, F.A. (2012a). Alexithymia and alcohol: The roles of punishment sensitivity and drinking motives. Addiction Research & Theory, 20, 348–357. [Google Scholar]
- Lyvers, M. , Hayatbakhsh, N. , Stalewski, J. & Thorberg, F.A. (2019c). Alexithymia, impulsivity, and reward sensitivity in young adult university student children of alcoholics. Substance Use & Misuse, 54, 340–344. [DOI] [PubMed] [Google Scholar]
- Lyvers, M. , Hinton, R. , Gotsis, S. , Roddy, M. , Edwards, M.S. & Thorberg, F.A. (2014d). Traits linked to executive and reward systems functioning in clients undergoing residential treatment for substance dependence. Personality and Individual Differences, 70, 194–199. [Google Scholar]
- Lyvers, M. , Lysychka, O. & Thorberg, F.A. (2014a). Alexithymia and drinking in young adults: The role of alcohol‐related intrusive thoughts. Personality and Individual Differences, 57, 70–73. [Google Scholar]
- Lyvers, M. , Makin, C. , Toms, E. , Thorberg, F.A. & Samios, C. (2014c). Trait mindfulness in relation to emotional self‐regulation and executive function. Mindfulness, 5, 619–625. [Google Scholar]
- Lyvers, M. , McCann, K. , Coundouris, S. , Edwards, M.S. & Thorberg, F.A. (2018c). Alexithymia in relation to alcohol use, emotion recognition, and empathy: The role of externally oriented thinking. American Journal of Psychology, 131, 41–51. [Google Scholar]
- Lyvers, M. , Narayanan, S.S. & Thorberg, F.A. (2019d). Disordered social media use and risky drinking in young adults: Differential associations with addiction‐linked traits. Australian Journal of Psychology, 71, 223–231. [Google Scholar]
- Lyvers, M. , Simons, O. , Hayes, A. & Thorberg, F.A. (2014b). Drinking motives, alcohol expectancies and alexithymia in young adult social drinkers. Journal of Substance Use, 19, 44–47. [Google Scholar]
- Marchesi, C. , Ossola, P. , Tonna, M. & De Panfilis, C. (2014). The TAS‐20 more likely measures negative affects rather than alexithymia itself in patients with major depression, panic disorder, eating disorders and substance use disorders. Comprehensive Psychiatry, 55, 972–978. [DOI] [PubMed] [Google Scholar]
- Maurage, P. , Timary, P. & D'Hondt, F. (2017). Heterogeneity of emotional and interpersonal difficulties in alcohol‐dependence: A cluster analytic approach. Journal of Affective Disorders, 217, 163–173. [DOI] [PubMed] [Google Scholar]
- Maurage, P. , Grynberg, D. , Noel, X. , Joassin, F. , Philippot, P. , Hanak, C. et al. (2011). Dissociation between affective and cognitive empathy in alcoholism: A specific deficit for the emotional dimension. Alcoholism‐Clinical and Experimental Research , 35, 1662–1668. [DOI] [PubMed] [Google Scholar]
- Meziou, O. , Ghali, F. , Khelifa, E. , Maamri, A. , Ben Saadi, S. , Mrizak, J. et al. (2019). Alexithymia, impulsivity and sensation seeking in buprenorphine addiction: A comparative study. Journal of Substance Use, 24, 101–104. [Google Scholar]
- Morie, K.P. & Ridout, N. (2018). Alexithymia and maladaptive regulatory behaviors in substance use disorders and eating disorders. In Luminet O., Bagby R.N. & Taylor J.G. (Eds.), Alexithymia, advances in research, theory and clinical practice (pp. 158–173). Cambridge: Cambridge University Press. [Google Scholar]
- Morie, K.P. , Nich, C. , Hunkele, K. , Potenza, M.N. & Carroll, K.M. (2015). Alexithymia level and response to computer‐based training in cognitive behavioral therapy among cocaine‐dependent methadone maintained individuals. Drug and Alcohol Dependence, 152, 157–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker, J.D. , Taylor, G.J. & Bagby, R.M. (2003). The 20‐item toronto alexithymia scale. III. reliability and factorial validity in a community population. Journal of Psychosomatic Research, 55, 269–275. [DOI] [PubMed] [Google Scholar]
- Parolin, M. , Simonelli, A. , Cristofalo, P. , Sacco, M. , Bacciardi, S. , Maremmani, A. G. I. et al. (2017). Drug addiction and emotional dysregulation in young adults. Heroin Addiction and Related Clinical Problems , 19, 37–48. [Google Scholar]
- Patwardhan, I. , Mason, W.A. , Chmelka, M.B. , Savolainen, J. , Miettunen, J. & Järvelin, M.‐R. (2019). Prospective relations between alexithymia, substance use and depression: Findings from a National Birth Cohort. Nordic Journal of Psychiatry, 73(6), 340–348. 10.1080/08039488.2019.1634758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Payer, D.E. , Lieberman, M.D. & London, E.D. (2011). Neural correlates of affect processing and aggression in methamphetamine dependence. Archives of General Psychiatry, 68, 271–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen, A.F. , Sorensen, J.K. , Bruun, N.H. , Christensen, B. & Vedsted, P. (2016). Risky alcohol use in Danish physicians: Associated with alexithymia and burnout? Drug and Alcohol Dependence, 160, 119–126. [DOI] [PubMed] [Google Scholar]
- Pigoni, A. , Mandolini, G.M. , Delvecchio, G. , Bressi, C. , Soares, J.C. & Brambilla, P. (2020). A focus on valproate and cognitive deficits in bipolar disorders: A mini‐review. Journal of Affective Disorders, 261, 277–281. 10.1016/j.jad.2019.08.008 [DOI] [PubMed] [Google Scholar]
- Preece, D. , Becerra, R. , Robinson, K. , Dandy, J. & Allan, A. (2018). The psychometric assessment of alexithymia: Development and validation of the perth alexithymia questionnaire. Personality and Individual Differences, 132, 32–44. [Google Scholar]
- Rasheed, A.H.E. (2001). Alexithymia in Egyptian substance abusers. Substance Abuse, 22(1), 11–21. 10.1023/a:1026467708445 [DOI] [PubMed] [Google Scholar]
- Rufer, M. , Albrecht, R. , Zaum, J. , Schnyder, U. , Mueller‐Pfeiffer, C. , Hand, I. et al. (2010). Impact of alexithymia on treatment outcome: A naturalistic study of short‐term cognitive‐behavioral group therapy for panic disorder. Psychopathology, 43, 170–179. [DOI] [PubMed] [Google Scholar]
- Saarijärvi, S. , Salminen, J.K. & Toikka, T.B. (2001). Alexithymia and depression: A 1‐year follow‐up study in outpatients with major depression. Journal of Psychosomatic Research, 51, 729–733. [DOI] [PubMed] [Google Scholar]
- Shishido, H. , Gaher, R.M. & Simons, J.S. (2013). I don't know how I feel, therefore I act: Alexithymia, urgency, and alcohol problems. Addictive Behaviors, 38, 2014–2017. [DOI] [PubMed] [Google Scholar]
- Sifneos, PE . (1973). The prevalence of "alexithymic" characteristics in psychosomatic patients. Psychother Psychosom, 22, 255–262. [DOI] [PubMed] [Google Scholar]
- Simons, J.S. , Carey, K.B. & Wills, T.A. (2009). Alcohol abuse and dependence symptoms: A multidimensional model of common and specific etiology. Psychology of Addictive Behaviors: Journal of the Society of Psychologists in Addictive Behaviors, 23, 415–427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skrzynski, C.J. & Creswell, K.G. (2020). Associations between solitary drinking and increased alcohol consumption, alcohol problems, and drinking to cope motives in adolescents and young adults: A systematic review and meta‐analysis. Addiction (Abingdon, UK), 115, 1989–2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Speranza, M. , Corcos, M. , Stephan, P. , Loas, G. , Perez‐Diaz, F. , Lang, F. et al. (2004). Alexithymia, depressive experiences, and dependency in addictive disorders. Substance Use & Misuse , 39, 551–579. [DOI] [PubMed] [Google Scholar]
- Stinson, F.S. , Grant, B.F. , Dawson, D.A. , Ruan, W.J. , Huang, B. & Saha, T. (2005). Comorbidity between DSM‐IV alcohol and specific drug use disorders in the United States: Results from the national epidemiologic survey on alcohol and related conditions. Drug and Alcohol Dependence, 80, 105–116. [DOI] [PubMed] [Google Scholar]
- Taurino, A. , Antonucci, L.A. , Taurisano, P. & Laera, D. (2021). Investigating defensive functioning and alexithymia in substance use disorder patients. BMC Psychiatry, 21(1), 337. 10.1186/s12888-021-03340-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor, G.J. (2018). History of alexithymia: The contributions of psychoanalysis. In Luminet O., Bagby R.M. & Taylor G.J. (Eds.), Alexithymia. advances in research, theory, and clinical practice (pp. 1–17). Cambridge: Cambridge University Press. [Google Scholar]
- Taylor, G.J. , Bagby, R.M. & Parker, J.D. (2003). The 20‐item Toronto Alexithymia Scale. IV. reliability and factorial validity in different languages and cultures. Journal of Psychosomatic Research, 55(3), 277–283. [DOI] [PubMed] [Google Scholar]
- Thorberg, F.A. , Young, R.M. , Sullivan, K.A. & Lyvers, M. (2009). Alexithymia and alcohol use disorders: A critical review. Addictive Behaviors, 34, 237–245. [DOI] [PubMed] [Google Scholar]
- Thorberg, F.A. , Young, R.M. , Sullivan, K.A. , Lyvers, M. , Connor, J.P. & Feeney, G.F.X. (2010). A psychometric comparison of the toronto alexithymia scale (TAS‐20) and the observer alexithymia scale (OAS) in an alcohol‐dependent sample. Personality and Individual Differences, 49, 119–123. [Google Scholar]
- Uzun, O. , Ates, A. , Cansever, A. & Ozsahin, A. (2003). Alexithymia in male alcoholics: Study in a Turkish sample. Comprehensive Psychiatry, 44, 349–352. [DOI] [PubMed] [Google Scholar]
- Verrocchio, M.C. , Conti, C. & Fulcheri, M. (2010). Deliberate self‐harm in substance‐dependent patients and relationship with alexithymia and personality disorders: A case‐control study. Journal of Biological Regulators and Homeostatic Agents, 24, 461–469. [PubMed] [Google Scholar]
- von Hippel, P.T. (2015). The heterogeneity statistic I(2) can be biased in small meta‐analyses. BMC Medical Research Methodology, 15, 35. 10.1186/s12874-015-0024-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zdankiewicz‐Ścigała, E. & Ścigała, D.K. (2018). Trauma, temperament, alexithymia, and dissociation among persons addicted to alcohol: Mediation model of dependencies. Frontiers in Psychology, 9, 1570. 10.3389/fpsyg.2018.01570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zdankiewicz‐Ścigała, E. & Ścigała, D.K. (2020). Attachment style, early childhood trauma, alexithymia, and dissociation among persons addicted to alcohol: Structural equation model of dependencies. Frontiers in Psychology, 10, 2957. 10.3389/fpsyg.2019.02957. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Study‐specific associations between Difficulty in Identifying Feelings sub‐score of alexithymia and substance use.
Figure S2. Study‐specific associations between Difficulty in Describing Feelings sub‐score of alexithymia and substance use.
Figure S3. Study‐specific associations between Externally Oriented Thinking sub‐score of alexithymia and substance use.
Figure S4. The funnel plot for the TAS‐20 total score.
Table S1. Search terms for the search in PubMed.
Table S2. Quality assessment of the studies in meta‐analysis.
Supplementary material
Data Availability Statement
Data sharing is not applicable to this article as no new data were created or analyzed in this study.


