Abstract
Background
A culture of shared leadership is widespread among palliative care teams based on a commitment to valuing and including all people equally. As compassion is a core value for end‐of‐life care work, compassionate leadership may be the best way to lead in palliative care.
Aims
The aims of this study were twofold: (1) to adapt and validate the Compassionate Leadership Self‐reported Scale in a sample of palliative care professionals; and (2) to study the relation between compassionate leadership and associated concepts of self‐compassion, awareness and self‐care.
Methods
A cross‐sectional survey of 296 Spanish end‐of‐life care professionals was conducted. Analyses included descriptive statistics, a confirmatory factor analysis (CFA) with four‐correlated factors, reliability estimates and a structural model.
Results
Results suggested there were medium to high levels of compassionate leadership in the sample. The CFA showed an adequate overall fit: χ2(98) = 277.595 (p < 0.001); CFI = 0.986; SRMR = 0.047; RMSEA = 0.088 [0.076, 0.100]. Reliability estimates for four subscales of compassionate leadership (attending, understanding, empathising and helping) were also adequate, ranging from 0.72 to 0.96. Finally, the structural model predicting compassionate leadership suggested that the dimensions of attending and understanding were most highly related to positive self‐compassion and awareness; empathising, to self‐care and awareness; and helping, to positive self‐compassion and self‐care.
Conclusion
The Compassionate Leadership Scale has adequate psychometric properties when used to assess compassionate leadership in the context of end‐of‐life care. Our results indicate that self‐compassion, awareness and self‐care are important correlates of such compassionate leadership.
Keywords: awareness, compassionate leadership, palliative care, self‐care, self‐compassion
INTRODUCTION
There is increasing evidence that organisations, as sites of human efforts, are also places of human suffering. Suffering is a reality of organisational life, and therefore, compassion, as a response to a co‐worker's suffering, plays an important part in maintaining organisational functioning [1, 2]. Indeed, as a natural human reaction, compassion is crucial to strengthening employees’ connections and relations with one another in meaningful ways [3]. When professionals feel cared for and perceive organisational support, they feel more satisfied with their jobs and committed to their organisations [4].
Compassion is even more important when studying healthcare organisations [5]. Indeed, compassion has always been central to healthcare, and it has been defined as integral to “good” healthcare [6, 7, 8, 9] and as one of the Cs in the UK National Nursing and Midwifery strategy [10]: care, compassion, competence, communication, courage and commitment. Compassion is a key element in person‐centred care, as it denotes the ability to develop genuinely compassionate relationships with patients and families [11]. Therefore, person‐centred care holds that healthcare is only appropriate if it is compassionate [12]. Research on healthcare outcomes for patients bears out the fundamental importance of compassion to patient outcomes [13].
Compassion has been defined as “a virtuous response that seeks to address the suffering and needs of a person through relational understanding and action” [14]. Therefore, behaving compassionately involves recognising the need in others, a motivation to respond to it, and the skills to meet it by helping [14]. Facilitating compassion at healthcare organisational level may enhance an ethic of care, by establishing a more positive, harmonious and supportive workplace for caregivers [15]. Specifically, when caring for the dying, compassionate qualities are essential, not only for the patients’ wellbeing, but also for professionals’ [16]. Compassionate care and adequate levels of professional quality of life together enhance wellbeing for end‐of‐life care professionals [16, 17]. Therefore, healthcare professionals and leaders may pursue compassionate care because, as a moral virtue, compassion will give context and direction to healthcare professionals’ decisions and actions, and will help to achieve excellence in healthcare practice [5]. But leaders also may pursue compassionate care because of its impact on the health and wellbeing of healthcare professionals. However, it is clear that these compassionate qualities (values, cultures, leadership) are not always present [15, 18, 19], and this has been strongly accentuated by the current health crisis [20, 21, 22].
The relationship between compassion and organisational outcomes has not been investigated in depth [4]. Some research suggests that workplace cultures influenced by compassionate guidelines promote helpful [23], forgiving [24] and generous behaviours [25]. Several authors have suggested that compassion, within an organisational context, can have several benefits, such as boosting organisational trust, pride, connection, motivation and commitment [26, 27, 28]; contributing to perceived effectiveness in leadership and decision making [29, 30]; and enhancing organisational performance [31]. In this context, compassionate leadership plays an important role in modelling compassionate behaviours, encouraging other employees to act compassionately and reducing dysfunctional behaviour, such as incivility or toxic conflict [3]. Specifically, supportive leadership enhancing compassion among healthcare personnel has been related to high levels of patient satisfaction, quality of care and organisational financial performance [32].
Compassionate leadership is significantly influenced by shared leadership and positive psychology perspectives [33, 34, 35, 36]. Linked to an authentic leadership model, compassionate leadership can be built on the skills of self‐awareness, internalised moral perspective, balanced processing and relational transparency [37]. It can also be an addition to the skills of idealised influence or charisma, inspirational motivation, intellectual stimulation and individualised consideration or attention, typical of transformational leadership [38]. Furthermore, compassionate leadership can be an important part of resonant leadership [39], or servant leadership that is relevant when fostering altruistic behaviours and the setting aside of egoistic goals [40]. Compassionate leadership implies a leadership that promotes the embodied qualities of servant leadership, such as altruism, integrity, humility and wisdom, along with an appreciation and empowerment of others [36]. In healthcare, such a leadership orientation is highly salient and relevant to the context.
Evidence about the levels and impact of compassionate leadership in healthcare organisations is scarce, but there are studies on how to enhance compassion among professionals and healthcare leaders [41, 42]. Self‐compassion has been identified as essential for maintaining healthcare workers’ balance [43]. Defined as compassion directed towards oneself, or extending compassion to ourselves as we would to others [43, 44], self‐compassion allows the healthcare professional to build resilience against stress and burnout [45], and has been associated with better professional quality of life [41, 42, 46, 47].
Other enablers of compassionate leadership include mindfulness and self‐care activities. Attentiveness and the ability to notice is key in detecting suffering and need, as acts of compassion are impossible without awareness of need [8]. In fact, studies have shown that increasing self‐awareness through interventions also affects levels of compassion [42, 46]. Awareness allows healthcare professionals to simultaneously attend to and monitor patients’, colleagues’ and their own needs, by developing greater feelings of empathy, kindness and equanimity for patients, colleagues, and for themselves.
Together with self‐compassion and awareness, activities of self‐care, which are aimed at ensuring a psychosocially rich life, have been identified as important enablers of compassionate leadership [8]. Indeed, the practice of self‐care, defined as the promotion of one's health [48] and the process of maintaining one's wholeness [49], is suggested as effective means of coping with occupational stressors for healthcare professionals [50, 51].
Taking this into account, we can infer that frontline caregivers will be better able to deliver compassionate care, in the context of a supportive organisational culture and with compassionate leadership support. This compassionate leadership has been defined as having four components: attending, paying attention to the other and noticing his or her suffering; understanding, understanding the cause of the other's distress; empathising, feeling an empathic response, mirroring the other's distress; and helping, taking thoughtful, skilled and appropriate action to help relieve the other's suffering [52, 53]. To assess such qualities, West [53] developed a brief instrument that consists of 16 items, the Compassionate Leadership Scale. This instrument has not been yet validated to this date. This study aims to adapt and validate the Compassionate Leadership Scale in a sample of end‐of‐life care professionals. The self‐assessed instrument was provided to healthcare professionals in relation to their leadership. Moreover, the association between compassionate leadership and self‐compassion, self‐care and awareness was also analysed.
METHODS
Design, setting and participants
A cross‐sectional survey of Spanish end‐of‐life care professionals was conducted during January‐February 2020. Professionals were encouraged to participate through the Spanish Society for Palliative Care (SECPAL). Participants were sampled from their lists of members, who were asked to complete an online survey using SurveyMonkey, a secure and anonymous online platform that also restricted multiple survey responses. Participation was voluntary and required respondents’ informed consent.
For inclusion, the participants had to be a healthcare professional (physician, nurse, psychologist, nursing assistant, social worker, or other), who currently cared for patients at the end of their lives, but not necessarily in palliative care settings. We determined if they were end‐of‐life care professionals using three questions, to which professionals had to answer YES/NO. If the answer was YES to any of them, they were considered professionals working with patients at the end of life. The indicators were: (a) “Do you care for patients with palliative needs?”; (b) “Do you care for chronic patients in advanced situations?”; and (c) “Do you care for patients with prognosis of life less than 2 years?”.
No a priori sample size estimation was calculated. However, we took into account several rules‐of‐thumb, including a minimum sample size of 200 [54, 55], and 10 cases per variable [56]. Therefore, our sample size (n = 296) meets both Boomsma's [54, 55] (n > 200) and Nunnally's [56] (n > 200 [10 cases per 16 variables for CFA model; 10 cases per 20 variables for the MIMIC model]) criteria.
The sample consisted of 296 end‐of‐life care professionals who completed the survey. Mean age was 43.9 years old (SD = 10.15); 77.40% were female. Regarding their professions, 31.8% were doctors, 44.2% nurses, 8.6% psychologists, 4.5% nursing assistants, 5.8% social workers and 5.1% had other professions. Details of sample characteristics can be found in Table 1.
TABLE 1.
Sample characteristics
| Variables | Categories | N | % |
|---|---|---|---|
| Gender | Female | 66 | 22.3 |
| Male | 229 | 77.4 | |
| Missing | 1 | 0.3 | |
| Level of education | Undergraduate | 20 | 6.7 |
| Graduate | 249 | 84.2 | |
| Postgraduate | 26 | 8.8 | |
| Missing | 1 | 0.3 | |
| Marital status | Single | 71 | 24.0 |
| Married/living with a couple | 192 | 64.9 | |
| Divorced | 29 | 9.8 | |
| Widowed | 2 | 0.7 | |
| Missing | 2 | 0.7 | |
| Profession | Doctor | 93 | 31.4 |
| Nurse | 129 | 43.6 | |
| Nursing assistant | 13 | 4.4 | |
| Psychologist | 25 | 8.4 | |
| Social worker | 17 | 5.7 | |
| Others | 15 | 5.1 | |
| Missing | 4 | 1.4 |
Measures
The research measures included scales to assess the following:
Compassionate leadership. The Compassionate Leadership Self‐reported Scale was used, which is a brief instrument of 16 items that includes four dimensions: attending, understanding, empathising and helping. Each of them is measured with four items, such as “I listen carefully when exploring problems” (attending), “I am helpful in understanding the causes of difficulties the team faces” (understanding), “I am emotionally in touch with others’ feelings when they are upset” (empathising) and “I help people practically with problems they face” (helping). Items are rated on a 5‐point Likert‐type scale, ranging from 1 (completely disagree) to 5 (completely agree). For the adaptation of the scale, first, a group of experts in organisational psychology, nursing and psychometrics adapted the original version, by changing the initial statement or instruction, from “This leader” to “regarding your behaviour when you lead your work team”. Items were also changed from third person to first person. Then, the backward and forward translation process was used; first, the scale was translated into Spanish by a professional native; it was then translated back into English by another native professional and no differences were found. No changes were made after review of the Spanish version by the group of experts. The resulting Spanish version of the scale is in Table 2. Estimates of reliability are provided in the Results section.
Self‐compassion. Self‐compassion was assessed with the Self‐Compassion Scale – Short Form (SCS) [57], in its Spanish version [58]. The SCS is formed by 12 items assessing three main components of self‐compassion and their opposites: self‐kindness/self‐judgement, common humanity/isolation and mindfulness/over‐identification. Items score in a 5‐point Likert‐type scale, from 1 “almost never” to 5 “almost always”. Examples of items are “I try to be understanding and patient towards those aspects of my personality I don't like” for positive self‐compassion, and “When I fail at something important to me, I become consumed by feelings of inadequacy” for negative self‐compassion. In this study, two dimensions of self‐compassion were used: positive and negative self‐compassion. Positive self‐compassion would refer to compassionate self‐responding to personal struggle, whereas negative self‐compassion would refer to uncompassionate self‐responding to personal struggle (berating oneself for feeling bad or repressing negative feelings), in line with Neff's definition of self‐compassion, who has recently conceptualised as a “balance between increased compassionate and decreased uncompassionate self‐responding to personal struggle” [59]. This two‐factor solution obtained an excellent fit in this sample: χ2 (53) = 136.971 (p < 0.001); CFI = 0.964; SRMR = 0.043; RMSEA = 0.076 [0.061, 0.092]. Estimates of reliability in this sample were 0.823 and 0.863, respectively.
Awareness. This variable was measured with 5 indicators of the validated Spanish version of the Mindful Attention Awareness Scale [60], an instrument that measures the general tendency to be aware and conscious of one's own experiences of daily life. Following the work of Galiana et al. [61], items 7, 8, 9, 10 and 14 were chosen, as they were the more discriminant. Items were scored in a 5‐point Likert scale, ranging from 1 “totally disagree” to 5 “totally agree”. Examples of items are: “I could experience an emotion and not be conscious of it until later” or “I find it difficult to stay focused on what is happening in the present”. Scores were reverted before mean calculation. Reliability in this study was 0.887.
Self‐Care. Self‐care was assessed with the Professional Self‐Care Scale (PSCS) [62], originally developed in Spanish. It is composed by nine items and assesses three dimensions of professionals’ self‐care: physical, which refers to the implication in activities that helps to maintain a healthy body; inner, which is related to activities that help to keep a healthy mind; and social, regarded to activities related to social activities that help the individual to maintain social health. Examples of items are “I do exercise on a regular basis” (physical self‐care), “When I feel emotionally overloaded, I try to find time for my own care” (inner or psychological self‐care), or “When I feel overwhelmed by a clinical situation, I feel that I can support on my team in order to elaborate this experience” (social self‐care). Items were scored in a 5‐point Likert scale, ranging from 1 (totally disagree) to 5 (totally agree). Reliability of the dimensions in this sample was 0.814, 0.907 and 0.724, respectively.
TABLE 2.
Adapted version of the compassionate leadership self‐reported scale in English and Spanish
|
Compassionate Leadership Self‐reported Scale (italics for the Spanish version) |
|
Indicate your agreement or disagreement with the following sentences regarding your behaviour when you lead your work team: Indica tu grado de acuerdo o desacuerdo en cada una de las siguientes afirmaciones sobre tu comportamiento cuando lideras equipos de trabajo: |
|
1. I listen carefully when exploring problems. 1. Escucho atentamente cuando exploro los problemas |
|
2. I pay close attention when listening. 2. Presto mucha atención cuando escucho |
|
3. I am very attentive when a member of the team tells me about difficulties. 3. Estoy muy atento/a cuando algún miembro del equipo me cuenta sus dificultades |
|
4. I give full attention when members of the team describes challenges they face. 4. Presto completa atención cuando me describen personalmente los problemas |
|
5. I am helpful in understanding the causes of difficulties the team faces. 5. Ayudo en la comprensión de las dificultades/problemas que afronta el equipo |
|
6. I do not impose my understanding of the causes of difficulties the team faces. 6. No impongo mi punto de vista sobre la causa de las dificultades/problemas que afronta el equipo |
|
7. I take time to understand carefully the causes of the problems. 7. Me tomo tiempo para comprender cuidadosamente la causa de los problemas |
|
8. I work together with the team to come to an understanding of problems. 8. Trabajo con el equipo para llegar a una comprensión de los problemas |
|
9. I am genuinely warm and empathic. 9. Soy genuinamente amable y empático |
|
10. I am emotionally in touch with others’ feelings when they are upset. 10. Estoy emocionalmente conectado con los sentimientos de los demás cuando no están bien |
|
11. I am sensitive to what others are feeling. 11. Soy sensible a lo que otros sienten |
|
12. I genuinely care about others’ difficulties. 12. Me preocupo sinceramente de los problemas de los demás |
|
13. I help people practically with problems they face. 13. Ayudo a la gente de manera práctica con los problemas que afrontan |
|
14. I take effective action to help others with the problems they face 14. Actúo de manera efectiva para ayudar a otros con los problemas que afrontan |
|
15. I deal effectively with problems in order to help others. 15. Trato de forma efectiva los problemas para ayudar a los demás |
|
16. I am genuinely committed to making a difference by serving others. 16. Estoy verdaderamente comprometido/a en ser especialmente bueno/a sirviendo a otros |
Data analysis
First, descriptive statistics for the items of the compassionate leadership scale, including means, standard deviations, and minimum and maximum scores, were calculated.
Second, for the study of the internal structure, a confirmatory factor analysis was hypothesised, estimated and tested, in which four‐correlated factors explained the items of the Compassionate Leadership Self‐reported Scale: attending (items 1–4), understanding (items 5–8), empathising (items 9–12) and helping (items 13–16). To assess the model fit, there were used: the chi‐square statistic, the Comparative Fit Index (CFI), the Standardised Root Mean Square Residual (SRMR) and the Root Mean Square Error of Approximation (RMSEA). Cut‐off criteria to determine good fit were as follows: CFI above 0.90 (better over 0.95) and SRMR or RMSEA below 0.08 (better under 0.05) [63].
Third, the reliability of the scale was studied, including estimates of reliability for the four dimensions: Cronbach's alpha and the Composite Reliability Index.
Fourth, levels of compassionate leadership were studied across genders and disciplines. For this purpose, two multivariate analyses of variance (MANOVAs) were carried out. For the MANOVAs, discipline was recoded, and nursing assistants (n = 13) and social workers (n = 17) were recoded into “other professions” because of its small sample size. The relation between compassionate leadership and age was also studied, using Pearson correlations.
Finally, a multiple‐indicators multiple‐causes (MIMC) structural model to study the Compassionate Leadership Scale relationships with the other variables was hypothesised, estimated and tested. Specifically, positive and negative self‐compassion, self‐care and awareness were hypothesised to predict the dimensions of compassionate leadership. The four dimensions of compassionate leadership or dependent variables were modelled as four correlated, latent factors, and consequently, free of error of measurement. To assess model fit, the fit criteria mentioned above were used.
For the statistical analyses, SPSS version 24 [64] and MPLUS version 8.4 [65] were used.
Ethical considerations
The study was approved by the Ethics Research Committee at the University of the Balearic Islands (82CER18). Given the characteristics of the study, the people who decided to participate voluntarily were told the reason and purpose for carrying out the work. This entire study complied with the ethical principles for research in health sciences established at the national and international levels in the Declaration of Helsinki [66]. Special attention was paid to confidentiality and protection of privacy, guaranteeing the anonymity of the information provided, which was used exclusively for this work and was held in the custody of the research team. In addition, our research team is committed to strictly complying with the Organic Spanish Law on Personal Data Protection, which guarantees that the participants in this study can exercise their rights of access, rectification, cancellation and opposition to the collected data.
RESULTS
Descriptive statistics
The Compassionate Leadership Self‐Reported Scale showed medium to high levels in the four domains of compassionate leadership, with means ranging from 3.96 (Helping) to 4.26 (Attending). Details on specific items can be consulted in Table 3.
TABLE 3.
Items description: mean, standard deviation, minimum and maximum scores; descriptive statistics of compassionate leadership dimensions, self‐compassion, awareness and self‐care
| Dimension/Item number | Mean | SD | Min. | Max. |
|---|---|---|---|---|
| Attending | 4.26 | 0.52 | 2.50 | 5.00 |
| 1 | 4.21 | 0.58 | 2.00 | 5.00 |
| 2 | 4.18 | 0.59 | 2.00 | 5.00 |
| 3 | 4.33 | 0.57 | 2.00 | 5.00 |
| 4 | 4.30 | 0.61 | 2.00 | 5.00 |
| Understanding | 4.02 | 0.52 | 2.75 | 5.00 |
| 5 | 4.17 | 0.55 | 3.00 | 5.00 |
| 6 | 3.80 | 0.86 | 1.00 | 5.00 |
| 7 | 4.02 | 0.71 | 2.00 | 5.00 |
| 8 | 4.11 | 0.64 | 2.00 | 5.00 |
| Empathising | 4.06 | 0.55 | 1.75 | 5.00 |
| 9 | 4.05 | 0.63 | 2.00 | 5.00 |
| 10 | 3.99 | 0.68 | 1.00 | 5.00 |
| 11 | 4.07 | 0.69 | 1.00 | 5.00 |
| 12 | 4.13 | 0.66 | 1.00 | 5.00 |
| Helping | 3.96 | 0.57 | 1.25 | 5.00 |
| 13 | 4.02 | 0.59 | 2.00 | 5.00 |
| 14 | 3.91 | 0.66 | 1.00 | 5.00 |
| 15 | 3.89 | 0.67 | 1.00 | 5.00 |
| 16 | 4.00 | 0.78 | 1.00 | 5.00 |
| Positive self‐compassion | 3.40 | 0.71 | 1.17 | 4.83 |
| Negative self‐compassion | 2.80 | 0.85 | 1.00 | 5.00 |
| Awareness | 4.00 | 0.81 | 2.00 | 5.00 |
| Self‐care | 3.63 | 0.72 | 1.00 | 4.89 |
Abbreviations: Max., maximum score; Min., minimum score; SD, standard deviation.
As regards the related variables, participants showed high levels of awareness, medium to high levels of self‐care and positive self‐compassion, and moderate levels of negative self‐compassion (see Table 3).
Confirmatory factor analysis
The CFA with four‐correlated factors showed an adequate overall fit: χ2 (98) = 277.595 (p < 0.001); CFI = 0.986; SRMR = 0.047; RMSEA = 0.088 [0.076, 0.100]. Factor loadings were adequate, ranging from 0.428 (item 8) to 0.994 (item 15). Details of the analytical fit can be consulted in Figure 1.
FIGURE 1.
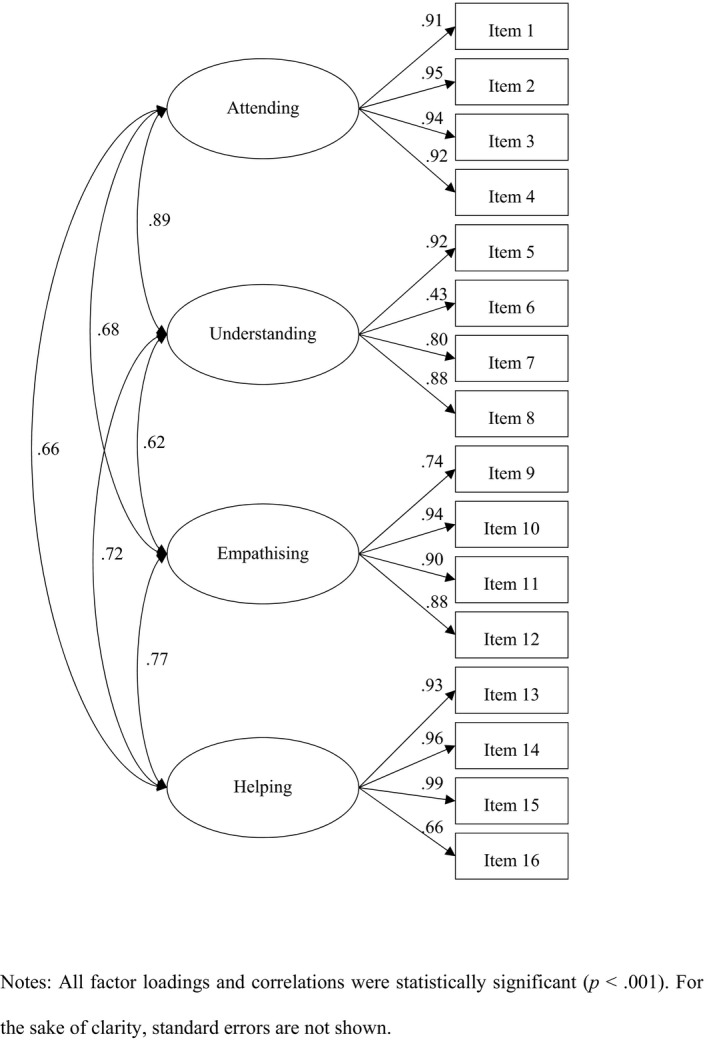
Confirmatory factor analysis results. Notes: All factor loadings and correlations were statistically significant (p < 0.001). For the sake of clarity, standard errors are not shown
Reliability
Evidence of reliability of the dimensions was adequate: Cronbach's alpha and CRI were 0.905 and 0.962 for attending, 0.723 and 0.855 for understanding, 0.858 and 0.924 for empathising, and 0.865 and 0.940 for helping, respectively.
Relations of compassionate leadership, gender, discipline and age
To study the relation between compassionate leadership and gender, a multivariate analysis of variance (MANOVA) was carried out. The four dimensions of compassionate leadership were included as dependent variables, with gender as the independent variable. Results pointed statistically significant differences in the mean level of compassionate leadership when compared by gender: F(4, 232) = 2.825 (p = 0.026), η2 = 0.046. Follow‐up analyses of variance for each of the dimensions showed mean differences only in the understanding dimension (F(1, 235) = 9.326 (p = 0.003), η2 = 0.038), with higher levels of understanding leadership for men (M = 4.209) when compared to women (M = 3.970).
Regarding the relation between compassionate leadership and discipline, this was also studied using a MANOVA. Again, the four dimensions of compassionate leadership were included as dependent variables, and in this case, discipline was the independent variable. Results pointed to statistically significant differences in the mean level of compassionate leadership when compared by discipline: F(12, 690) = 2.529 (p = 0.003), η2 = 0.042. However, follow‐up ANOVAs did not indicate significant differences in any of the dimensions of compassionate leadership, neither there were statistically significant differences in the post hoc pairwise comparisons.
Finally, Pearson correlations did not show statistically significant relations between attending (r = 0.035; p = 0.598), understanding (r = −0.025; p = 0.707), empathising (r = 0.094; p = 0.152) or helping (r = 0.074; p = 0.258) with participants’ age.
MIMIC model
The structural model to study the Compassionate Leadership Self‐reported Scale relations with other variables showed an excellent fit: χ2(146) = 331.985 (p < 0.001); CFI = 0.985; SRMR = 0.043; RMSEA = 0.068[.058,.078]. The dimensions of attending and understanding were explained by positive self‐compassion and awareness; empathising, by self‐care and awareness; and helping, by positive self‐compassion and self‐care (see Figure 2). Approximately 77% of attending and understanding were explained (R 2 = 0.768; p < 0.001; and R2 = 0.772; p < 0.001, respectively), and more than 80% of emphasising and helping (R 2 = 0.814; p < 0.001; and R 2 = 0.806; p < 0.001, respectively). More details on the model results can be consulted in Table 4.
FIGURE 2.
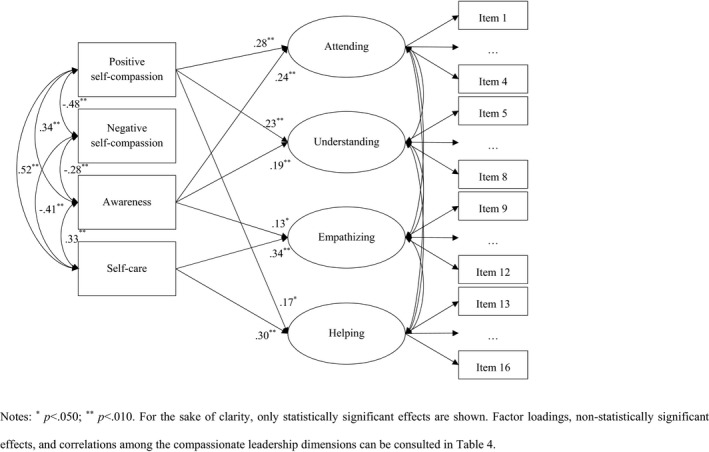
MIMIC results. Notes: * p < 0.050; ** p < 0.010. For the sake of clarity, only statistically significant effects are shown. Factor loadings, non‐statistically significant effects and correlations among the compassionate leadership dimensions can be consulted in Table 4
TABLE 4.
Factor loadings, effects and correlations of the MIMIC model
| Dimension | Item | λ | Predictive variables | β | Compassionate leadership dimensions | r |
|---|---|---|---|---|---|---|
| Attending | 1 | 0.904 (p < 0.001) | Positive self‐compassion | 0.277 (p < 0.001) | – | – |
| 2 | 0.954 (p < 0.001) | Negative self‐compassion | −0.051 (p = 0.443) | Understanding | 0.863 (p < 0.001) | |
| 3 | 0.940 (p < 0.001) | Awareness | 0.238 (p < 0.001) | Empathising | 0.649 (p < 0.001) | |
| 4 | 0.924 (p < 0.001) | Self‐care | 0.058 (p = 0.360) | Helping | 0.603 (p < 0.001) | |
| Understanding | 5 | 0.922 (p < 0.001) | Positive self‐compassion | 0.231 (p = 0.002) | Attending | 0.863 (p < 0.001) |
| 6 | 0.425 (p < 0.001) | Negative self‐compassion | −0.107 (p = 0.109) | – | – | |
| 7 | 0.800 (p < 0.001) | Awareness | 0.193 (p = 0.004) | Empathising | 0.566 (p < 0.001) | |
| 8 | 0.877 (p < 0.001) | Self‐care | 0.107 (p = 0.116) | Helping | 0.679 (p < 0.001) | |
| Empathising | 9 | 0.747 (p < 0.001) | Positive self‐compassion | 0.121 (p = 0.128) | Attending | 0.649 (p < 0.001) |
| 10 | 0.939 (p < 0.001) | Negative self‐compassion | 0.130 (p = 0.061) | Understanding | 0.566 (p < 0.001) | |
| 11 | 0.904 (p < 0.001) | Awareness | 0.134 (p = 0.035) | – | – | |
| 12 | 0.876 (p < 0.001) | Self‐care | .337 (p < 0.001) | Helping | 0.715 (p < 0.001) | |
| Helping | 13 | 0.931 (p < 0.001) | Positive self‐compassion | 0.168 (p = 0.032) | Attending | 0.603 (p < 0.001) |
| 14 | 0.964 (p < 0.001) | Negative self‐compassion | 0.052 (p = 0.454) | Understanding | 0.679 (p < 0.001) | |
| 15 | 0.994 (p < 0.001) | Awareness | −0.100 (p = 0.116) | Empathising | 0.715 (p < 0.001) | |
| 16 | 0.659 (p < 0.001) | Self‐care | 0.303 (p < 0.001) | – | – |
DISCUSSION
Research on leadership in end‐of‐life care is limited, but it confirms that leadership in this context spans across disciplines, roles and titles [67, 68, 69]. The culture of shared leadership is widespread among healthcare professionals in general [70, 71, 72], and among teams of end‐of‐life care professionals in particular, so that all members have the right, responsibility and the ability to be a leader [67]. As compassion has been identified as an essential quality for both end‐of‐life care work [14, 18, 19] and leadership [3, 32], compassionate leadership may be the best way to lead in end‐of‐life care. In this context, the first aim of this study was to adapt and validate the Compassionate Leadership Scale in a sample of end‐of‐life care professionals.
For this purpose, the levels of compassionate leadership of the participants were first studied, together with evidence of the factorial structure and reliability of the scale. Participants showed adequate levels of compassionate leadership. Means of the four dimensions of the Compassionate Leadership Self‐reported Scale were close to 4 (“Agree”), which means professionals of end‐of‐life care reported compassionate behaviours when acting as a leader. This is not surprising, given the consensus in the literature on the centrality of end‐of‐life care professionals’ compassion to skilful and kind care for the self and others [18, 73]. Compassion reduces the pain and suffering experienced by those who are dying and those who give them care [73, 74, 75]. In the same way, medium to high levels of positive self‐compassion, awareness and self‐care were found, where participants also showed moderate levels of negative self‐compassion. Again, this is in line with previous literature, which has indicated the importance of these protective factors to end‐of‐life care professionals’ quality of life [50, 51, 76, 77, 78].
Regarding the factorial structure of the Compassionate Leadership Scale, results indicated an adequate model fit for a four‐correlated factor solution. As suggested by Atkins and Parker [52] and West [53], the four components of attending, understanding, empathising and helping clearly fit with the internal structure of the presented scale, with items showing adequate factor loadings and correlations between dimensions being positive and high. Thus, although there are four distinct compassionate leadership behaviours, based on our results we can see that these are interdependent skills, as the better an end‐of‐life care leader can attend, the better he/she understands, the more he/she empathises, and the more he/she can help. Together with evidence on the internal structure, the Compassionate Leadership Scale also demonstrated adequate reliability, suggesting the compassionate leadership dimensions can be measured with little error and high replicability.
When levels of compassionate leadership were studied across genders, disciplines and age, a statistically significant relation between the dimension of understanding and gender was found, with higher levels for men. This is a counterintuitive result, as in previous research women obtain higher levels of emotional intelligence [79] or empathy [80] (both issues closely related to the dimension of understanding, presented here). However, a recent study supports such difference favouring men [81], but it should be noted that the setting of the aforementioned work was Saudi Arabia, where the patriarchal society that still exists, could explain such a significant gender difference in leadership. On the contrary, in a meta‐analysis carried out on 76 studies, it was concluded that in most of them (64 papers) women were rated as significantly more effective leaders than men in organisational settings [82]. As the subsample of men in this study was very small, these results should be interpreted with caution. Moreover, our finding of a gender difference was only related to understanding – a more cognitive skill, rather than the other elements of being present with (attending), empathising and helping. According to gender stereotypes, men might be expected to focus more on rational, cognitive and interpretive rather than relational and emotional processes.
The second aim of this research was to study the relation of compassionate leadership, as measured with the Compassionate Leadership Scale, with other variables that may act as enablers, such as self‐compassion, awareness and self‐care. We hypothesised that leaders with higher levels of positive self‐compassion, awareness and self‐care, and lower levels of negative self‐compassion, will pay greater attention to others, better understand the cause of others’ distress, feel more empathic, and take thoughtful, skilled and appropriate action to help relieve the other's suffering. Our results confirm most of these hypotheses. Self‐compassion, in its positive dimension, was related to attending, understanding and helping. That is, the more compassion end‐of‐life care professionals directed towards themselves, the more they act as compassionate leaders. This can be logically explained in two ways. First, self‐compassion is closely associated with compassion for others [83, 84, 85], as it is inward compassion, giving oneself care and concern when facing experiences of suffering [44]. In fact, some studies have supported this interpretation. For instance, Gustin and Wagner [46] found that cultivating self‐compassion in nursing professionals improved compassion for others. Also, in a study with nurses, Dev et al. [86] found evidence that the development of self‐compassion reduced the experience of some barriers to compassion. Second, self‐compassion alleviates professional burnout and compassion fatigue [46, 86, 87], which can erode compassion among end‐of‐life care professionals. In turn, this can enhance professionals’ capacity for compassionate leadership.
The absence of a relationship between self‐compassion and the dimension of empathising was counterintuitive, as empathy has been described as “an affective response that acknowledges and attempts to understand individual's suffering through emotional resonance” [88] (p. 437). However, other studies have also pointed to data consistent with our results. For example, González‐Hernández et al. [89] found that participants who undertook Cognitively‐Based Compassion Training considered a compassionate person as more non‐empathic than empathic. According to these authors, this could be due to the fact that empathy is a step towards compassion, but is not compassion itself, embodied most significantly in helping behaviour [89]. Therefore, those who need compassion which has not yet been offered could feel “empathic distress” [90].
Regarding the role of awareness in compassionate leadership, higher levels of participants’ awareness predicted higher levels of attending, understanding and emphasising. Awareness, as hypothesised, is key for leaders to notice suffering [8], and respond to it with attention, understanding and empathy. Thus, increased awareness will increase professionals’ levels of compassion [42, 46], and so, compassionate leadership. An active, inner process of being attentive to oneself, ensuring a nonjudgemental, non‐evaluative point of view, is fundamental in actively perceiving team members’ feelings, wishes, fears, questions and intentions. Therefore, end‐of‐life care professionals’ cultivation of awareness may not only improve patients’ care but also their work as compassionate leaders, by stimulating stronger feelings of kindness and equanimity both for patients and for their team [91].
Finally, self‐care positively predicted compassionate leadership, specifically its dimensions of empathising and helping. Again, these results were in line with our hypotheses, as previous research and writings have suggested self‐care is powerful in helping to overcome suffering, either for oneself or for others [76, 92]. Self‐care activities have been shown to mitigate the negative outcomes associated with the care of seriously ill patients [48], and to help end‐of‐life care providers maintain their own health and professional quality of life [62]. Self‐care is the third imperative when working and leading in end‐of‐life care, as it enables the professional, through the improvement of his or her own care, to take better care of their patients and their team members, by helping and emphasising with them.
CONCLUSIONS
Most advanced healthcare systems around the world have in common a progressive loss of compassionate care [11, 36]. Compassion has long been considered at the heart of healthcare [18, 73]. However, this concept has become an abstract idea, rather than a lived relational reality in many healthcare settings [36]. The lack of compassion not only leads to the loss of humanised care but also negatively affects patient outcomes.
Facing the growing problem of a compassion deficit, different authors argue for, among other solutions, a change in culture and leadership in health organisations [93]. The leadership styles that have shown the best results in the healthcare setting are those focused on relationships, rather than those focused more exclusively on tasks and performance [94]. Compassionate leadership, as a leadership style embodying the core value of healthcare, encourages and sustains compassionate healthcare [36].
This study confirms the utility and value of a tool for assessing the level of compassionate leadership competence in health professionals who face particular challenges to demonstrate compassion in the care of the dying. The scale has shown adequate psychometric properties when used to assess compassionate leadership in the context of end‐of‐life care professionals. It is therefore an instrument that can be used confidently to evaluate compassionate leadership among end‐of‐life care providers and almost certainly other healthcare professionals.
The ubiquity of suffering in end‐of‐life care creates an imperative for compassionate leadership. As pointed by Sansó et al. [76], professionals are “a powerful but vulnerable tool in the caring process” (p. 204). To avoid this vulnerability, the cultivation of compassionate leadership, through self‐care, awareness and self‐compassion, can be protective for healthcare professionals themselves.
Furthermore, our results suggested that self‐compassion, awareness and self‐care may be important in the development of compassionate leadership. Prior research suggests these orientations have positive effects on patient care and professionals’ health and quality of life [17, 76]. Current research suggests they may also help to underpin compassionate leadership.
Implications and future directions
Based on these findings, training programs to improve compassionate leadership may be designed, developing the variables that have shown a positive relationship, and using the scale to monitor improvements and guide further development of leaders’ competence of compassion [95].
Future research might consider how to foster better alliances between end‐of‐life care professionals and policy makers, so that together they can nurture compassionate cultures. Such an approach to leadership can and should begin with the leaders themselves, who must be prepared to practise self‐compassion, recognise the need for compassion in others, be motivated to respond to it, and be trained with the skills to meet it.
AUTHOR CONTRIBUTIONS
Conceptualisation, N.S., J.P.L., G.V.B., L.G. and M.W.; acquisition of data, N.S., J.P.L. and L.G.; analysis and interpretation of data, L.G.; writing—original draft preparation, N.S. and L.G.; writing—review and editing, N.S., J.P.L., G.V.B., L.G. and M.W.; supervision, N.S., L.G. and M.W.; project administration, N.S. and L.G.; funding acquisition, N.S. and L.G. All authors have given final approval of the version to be published and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
ETHICAL APPROVAL
The study was approved by the Ethics Research Committee at the University of the Balearic Islands (82CER18). Given the characteristics of the study, the people who decided to participate voluntarily were told the reason and purpose for carrying out the work. This entire study complied with the ethical principles for research in health sciences established at the national and international levels in the Declaration of Helsinki [60]. Special attention was paid to confidentiality and protection of privacy, guaranteeing the anonymity of the information provided, which was used exclusively for this work and was held in the custody of the research team. In addition, our research team is committed to strictly complying with the Organic Spanish Law on Personal Data Protection, which guarantees that the participants in this study can exercise their rights of access, rectification, cancellation and opposition to the collected data.
CONFLICT OF INTEREST
The authors have no conflicts of interest to declare.
ACKNOWLEDGEMENTS
The authors thank the Spanish Society for Palliative Care – Sociedad Española de Cuidados Paliativos (SECPAL) for the support in data collection. The authors also thank all the participants for their time and interest.
Sansó N, Leiva JP, Vidal‐Blanco G, Galiana L, West M. The measurement of compassionate leadership: Adaptation and Spanish validation of the compassionate leadership self‐reported scale. Scand J Caring Sci. 2022;36:1165–1179. 10.1111/scs.13079
Funding information
This research was funded by FEDER/Ministerio de Ciencia e Innovación – Agencia Estatal de Investigación, Spain/Project Longitudinal study of compassion and other professional quality of life determinants: A national level research on palliative care professionals (CompPal) [Estudio longitudinal de la compasión y otros determinantes de la calidad de vida profesional: Una investigación en profesionales de cuidados paliativos a nivel nacional (CompPal)] (RTI2018‐094089‐I00).
[Correction added on 6 April 2022, after first online publication: Juan P. Leiva’s job title and qualifications have been corrected to “PhD candidate Universitat Autònoma de Barcelona” in this version.]
REFERENCES
- 1. Simpson AV, Farr‐Wharton B, Pina e Cunha M, Reddy P. Organizing organizational compassion subprocesses and mechanisms: a practical model. In: Galiana L, Sansó N, editors. The power of compassion. New York: Nova Science Publishers; 2019. p. 339–57. [Google Scholar]
- 2. Worline M, Dutton JE. Awakening compassion at work: the quiet power that elevates people and organizations. San Francisco: Berrett‐Koehler Publishers; 2017. [Google Scholar]
- 3. Shuck B, Alagaraja M, Immekus J, Cumberland D, Honeycutt‐Elliott M. Does compassion matter in leadership? A two‐stage sequential equal status mixed method exploratory study of compassionate leader behavior and connections to performance in human resource development. Hum Resour Dev Q. 2019;30:537–64. 10.1002/hrdq.21369 [DOI] [Google Scholar]
- 4. Lilius JM, Worline MC, Dutton JE, Kanov JM, Maitlis S. Understanding compassion capability. Hum Relat. 2011;64(7):873–99. 10.1177/0018726710396250 [DOI] [Google Scholar]
- 5. de Zulueta P. Developing compassionate leadership in health care: an integrative review. J Healthc Leadersh. 2016;8:1–10. 10.2147/JHL.S93724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Royal College of Psychiatrists . Compassion in care: ten things you can do to make a difference. London: Faculty report, Royal College of Psychiatrists; 2015. [Google Scholar]
- 7. Department of Health . The NHS constitution for England. 2015. Available from: https://www.gov.uk/government/publications/the‐nhs‐constitution‐for‐england/the‐nhs‐constitution‐for‐england. Accessed Jan 1, 2021. [Google Scholar]
- 8. NHS England . Building and strengthening leadership‐leading with compassion. London: NHS England; 2014. [Google Scholar]
- 9. Nursing and Midwifery Council . The code – professional standards of practice and behavior for nurses and midwives. London: Nursing and Midwifery Council; 2015. [Google Scholar]
- 10. NHS England . Compassion in practice; 2012. Available from: https://www.england.nhs.uk/wp‐content/uploads/2016/05/cip‐yr‐3.pdf. Accessed Dec 20, 2020. [Google Scholar]
- 11. Lown BA, Rosen J, Marttila J. An agenda for improving compassionate care: a survey shows about half of patients say such care is missing. Health Aff (Millwood). 2011;30(9):1772–8. 10.1377/hlthaff.2011.0539 [DOI] [PubMed] [Google Scholar]
- 12. Singer T, Bolz M. Compassion: Bridging practice and science. 2013, Max Planck Institute for Human Cognitive and Brain Sciences. Available from: http://www.compassion‐training.org/. Accessed Dec 23, 2020.
- 13. Trzeciak S, Mazzarelli A, Booker C. Compassionomics: the revolutionary scientific evidence that caring makes a difference. Pensacola: Studer Group; 2019. [Google Scholar]
- 14. Sinclair S, McClement S, Raffin‐Bouchal S, Hack TF, Hagen NA, McConnell S, Chochinov HM. Compassion in health care: an empirical model. J Pain Symptom Manage. 2016;51(2):193–203. 10.1016/j.jpainsymman.2015.10.009 [DOI] [PubMed] [Google Scholar]
- 15. Simpson AV, Farr‐Wharton B, Reddy P. Cultivating organizational compassion in healthcare. J Manag Organ. 2020;26(3):340–54. 10.1017/jmo.2019.54 [DOI] [Google Scholar]
- 16. Sansó N, Galiana L, Oliver A, Tomás‐Salvá M, Vidal‐Blanco G. Predicting professional quality of life and life satisfaction in spanish nurses: a cross‐sectional study. Int J Environ Res Public Health. 2020;17(12):4366– 10.3390/ijerph17124366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Galiana L, Sansó N, Muñoz‐Martínez I, Vidal‐Blanco G, Oliver A, Larkin PJ. Palliative care professionals’ inner life: exploring the mediating role of self‐compassion in the prediction of compassion satisfaction, compassion fatigue, burnout and wellbeing. J Pain Symptom Manage. 2022;63(1):112–23. 10.1016/j.jpainsymman.2021.07.004 [DOI] [PubMed] [Google Scholar]
- 18. Larkin PJ. Compassion: the essence of palliative and end‐of‐life care. New York: Oxford University Press; 2016. [Google Scholar]
- 19. Vachon ML. Targeted intervention for family and professional caregivers: attachment, empathy, and compassion. Palliat Med. 2016;30(2):101–3. 10.1177/0269216315624279 [DOI] [PubMed] [Google Scholar]
- 20. Alharbi J, Jackson D, Usher K. The potential for COVID‐19 to contribute to compassion fatigue in critical care nurses. J Clin Nurs. 2020;29(15–16):2762–4. 10.1111/jocn.15314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Hofmeyer A, Taylor R, Kennedy K. Fostering compassion and reducing burnout: How can health system leaders respond in the Covid‐19 pandemic and beyond? Nurse Educ Today. 2020;94:104502. 10.1016/j.nedt.2020.104502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Renzi S, Fallanca F, Zangrillo A, Tresoldi M, Landoni G, Angelillo P, et al. Caring with compassion during COVID‐19. Palliat Support Care. 2020;18(4):403–4. 10.1017/S1478951520000577 [DOI] [PubMed] [Google Scholar]
- 23. Piff PK, Kraus MW, Côté S, Cheng BH, Keltner D. Having less, giving more: the influence of social class on prosocial behavior. J Pers Soc Psychol. 2010;99(5):771–84. 10.1037/a0020092 [DOI] [PubMed] [Google Scholar]
- 24. Worthington EL, Scherer M. Forgiveness is an emotion‐focused coping strategy that can reduce health risks and promote health resilience: theory, review, and hypotheses. Psychol Health. 2004;19(3):385–405. 10.1080/0887044042000196674 [DOI] [Google Scholar]
- 25. Saslow LR, Willer R, Feinberg M, Piff PK, Clark K, Keltner D, Saturn SR. My brother’s keeper?: Compassion predicts generosity more among less religious individuals. Soc Psychol Personal Sci. 2013;4(1):31–8. 10.1177/1948550612444137 [DOI] [Google Scholar]
- 26. Dutton JE, Lilius JM, Kanov JM. The transformative potential of compassion at work. In: Piderit SK, Fry RE, Cooperrider DL, editors. Handbook of transformative cooperation: new designs and dynamics. Stanford: Stanford Business Books; 2007. p. 107–26. [Google Scholar]
- 27. Frost PJ, Dutton JE, Worline MC, Wilson A. (2000). Narratives of compassion in organizations. In: Fineman S, editor. Emotion in organizations. London: Sage Publications; 2000. p. 25‐46. [Google Scholar]
- 28. Lilius JM, Worline MC, Maitlis S, Kanov J, Dutton JE, Frost P. The contours and consequences of compassion at work. J Occup Organ Psychol. 2008;29(2):193–218. 10.1002/job.508 [DOI] [Google Scholar]
- 29. Boyatzis RE, Smith ML, Blaize N. Developing sustainable leaders through coaching and compassion. Acad Manag Learn Educ. 2006;5(1):8–24. 10.5465/amle.2006.20388381 [DOI] [Google Scholar]
- 30. Cameron K, Mora C, Leutscher T, Calarco M. Effects of positive practices on organizational effectiveness. J Appl Behav Sci. 2011;47(3):266–308. 10.1177/0021886310395514 [DOI] [Google Scholar]
- 31. Cameron KS, Bright D, Caza A. Exploring the relationships between organizational virtuousness and performance. Am Behav Sci. 2004;47(6):766–90. 10.1177/0002764203260209 [DOI] [Google Scholar]
- 32. West MA, Dawson JF, Admasachew L. Topakas A. NHS Staff Management and Health Service Quality: Results from the NHS Staff Survey and related data.. 2011. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/215455/dh_129656.pdf. Accessed Dec 20, 2020. [Google Scholar]
- 33. Plsek PE, Wilson T. Complexity, leadership, and management in healthcare organisations. BMJ. 2001;323(7315):746–9. 10.1136/bmj.323.7315.746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Drath WH, McCauley CD, Palus CJ, Van Velsor E, O’Connor PMG, McGuire JB. Direction, alignment, commitment: toward a more integrative ontology of leadership. Leadersh Q. 2008;19:635–53. 10.1016/j.leaqua.2008.09.003 [DOI] [Google Scholar]
- 35. Suchman AL. How we think about organizations: a complexity perspective. In: Suchman AL, Sluyter DJ, Williamson PR, editors. Leading change in healthcare: transforming organizations using complexity, positive psychology and relationship‐centered care. London: Radcliffe Publishing; 2011. p. 11–24. [Google Scholar]
- 36. de Zulueta PC. Developing compassionate leadership in health care: an integrative review. J Healthc Leadersh. 2015;8:1–10. 10.2147/JHL.S93724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Avolio BJ, Gardner WL. Authentic leadership development: getting to the root of positive forms of leadership. Leadersh Q. 2005;16(3):315–38. 10.1016/j.leaqua.2005.03.001 [DOI] [Google Scholar]
- 38. Bass BM. Two decades of research and development in transformational leadership. Eur J Work Organ Psychol. 1999;8(1):9–32. 10.1080/135943299398410 [DOI] [Google Scholar]
- 39. Boyatzis R, McKee A. Resonant leadership: renewing yourself and connecting with others through mindfulness, hope and compassion. Boston: Harvard Business School Press; 2005. [Google Scholar]
- 40. Autry JA. The servant leader: how to build a creative team, develop great morale, and improve bottom‐line performance. New York: Three Rivers Press; 2001. [Google Scholar]
- 41. Sansó N, Galiana L, Oliver A, Cuesta P, Sánchez C, Benito E. Evaluación de una intervención mindfulness en equipos de cuidados paliativos. Interv Psicosoc. 2018;27(2):81–8. 10.5093/pi2018a7 [DOI] [Google Scholar]
- 42. Sansó N, Galiana L, González B, Sarmentero J, Reynes M, Oliver A, Garcia‐Toro M. Differential effects of two contemplative practice‐based programs for health care professionals. Psychos Interv. 2019;28(3):131–8. 10.5093/pi2019a12 [DOI] [Google Scholar]
- 43. Mills J, Wand T, Fraser JA. On self‐compassion and self‐care in nursing: selfish or essential for compassionate care? Int J Nurs Stud. 2015;52(4):791–3. 10.1016/j.ijnurstu.2014.10.009 [DOI] [PubMed] [Google Scholar]
- 44. Neff KD. The development and validation of a scale to measure self‐compassion. Self Identity. 2003;2(3):223–50. 10.1080/15298860309027 [DOI] [Google Scholar]
- 45. Raab K. Mindfulness, self‐compassion, and empathy among health care professionals: a review of the literature. Health Soc Care Chaplain. 2014;20(3):95–108. 10.1080/08854726.2014.913876 [DOI] [PubMed] [Google Scholar]
- 46. Gustin L, Wagner L. The butterfly effect of caring–clinical nursing teachers’ understanding of self‐compassion as a source to compassionate care. Scand J Caring Sci. 2013;27(1):175–83. 10.1111/j.1471-6712.2012.01033.x [DOI] [PubMed] [Google Scholar]
- 47. Durkin M, Beaumont E, Hollins Martin CJ, Carson J. A pilot study exploring the relationship between self‐compassion, self‐judgement, self‐kindness, compassion, professional quality of life and wellbeing among UK community nurses. Nurse Educ Today. 2016;46:109–14. 10.1016/j.nedt.2016.08.030 [DOI] [PubMed] [Google Scholar]
- 48. Sanchez‐Reilly S, Morrison LJ, Carey E, Bernacki R, O'Neill L, Kapo J, et al. Caring for oneself to care for others: physicians and their self‐care. J Support Oncol. 2013;11:75–81. 10.12788/j.suponc.0003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Radwany S, Hassler D, Robinson N, Soltis M, Myerscough R. Poetry as self‐care and palliative care. J Palliat Med. 2012;15:1394–5. 10.1089/jpm.2012.0201 [DOI] [PubMed] [Google Scholar]
- 50. Neville K, Cole DA. The relationships among health promotion behaviors, compassion fatigue, burnout, and compassion satisfaction in nurses practicing in a community medical center. JONA J Nurs Adm. 2013;43:348–54. 10.1097/NNA.0b013e3182942c23 [DOI] [PubMed] [Google Scholar]
- 51. Sorenson C, Bolick B, Wright K, Hamilton R. Understanding compassion fatigue in healthcare providers: a review of current literature. J Nurs Scholarsh. 2016;48(5):456–65. 10.1111/jnu.12229 [DOI] [PubMed] [Google Scholar]
- 52. Atkins PW, Parker SK. Understanding individual compassion in organizations: the role of appraisals and psychological flexibility. Acad Manage Rev. 2012;37(4):524–46. 10.5465/amr.2010.0490 [DOI] [Google Scholar]
- 53. West MA. Compassionate leadership in health and care settings. In: Galiana L, Sansó N, editors. The power of compassion. New York: Nova Science Publishers; 2019. p. 317–38. [Google Scholar]
- 54. Boomsma A. Robustness of LISREL against small sample sizes in factor analysis models. In: Joreskog KG, Wold H, editors. Systems under indirection observation: causality, structure, prediction (Part I). Amsterdam, Netherlands: North Holland; 1982. p. 149–73. [Google Scholar]
- 55. Boomsma A. Nonconvergence, improper solutions, and starting values in LISREL maximum likelihood estimation. Psychometrika. 1985;50:229–42. [Google Scholar]
- 56. Nunnally JC. Psychometric theory. New York: McGraw‐Hill; 1967. [Google Scholar]
- 57. Raes F, Pommier E, Neff KD, Van Gucht D. Construction and factorial validation of a short form of the Self‐Compassion Scale. Clin Psychol Psychother. 2011;18:250–5. 10.1016/j.jpainsymman.2018.11.003 [DOI] [PubMed] [Google Scholar]
- 58. Garcia‐Campayo J, Navarro‐Gil M, Andrés E, Montero‐Marin J, López‐Artal L, Demarzo MM. Validation of the Spanish versions of the long (26 items) and short (12 items) forms of the Self‐Compassion Scale (SCS). Health Qual Life Outcomes. 2014;12(1):1–9. 10.1186/1477-7525-12-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Neff KD, Toth‐Kiraly I, Colosimo K. Self‐compassion is best measured as a global construct and is overlapping with but dis‐tinct from neuroticism: a response to Pfattheicher, Geiger, Hartung, Weiss, and Schindler (2017). Eur J Pers. 2018;32:371–92. [Google Scholar]
- 60. Cebolla A, Luciano JV, Piva MP, Navarro‐Gil M, Garcia‐Campayo J. Psychometric properties of the Spanish version of the mindful attention awareness scale (MAAS) in patients with fibromyalgia. Health Qual Life Outcomes. 2013;11:6. 10.1186/1477-7525-11-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Galiana L, Oliver A, Sansó N, Sancerni MD, Tomás JM. Mindful attention awareness in Spanish palliative care professionals: Psychometric study with IRT and CFA models. Eur J Psychol Assess. 2017;33(1):14–21. 10.1027/1015-5759/a000265 [DOI] [Google Scholar]
- 62. Galiana L, Oliver A, Sansó N, Benito E. Validation of a new instrument for self‐care in Spanish palliative care professionals nationwide. Span J Psychol. 2015;18(e67):1–9. 10.1017/SJP.2015.71 [DOI] [PubMed] [Google Scholar]
- 63. Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling. 1999;6(1):1–55. 10.1080/10705519909540118 [DOI] [Google Scholar]
- 64. IBM Corp . IBM SPSS statistics for windows, Version 24.0. Armonk: IBM Corp; 2016. [Google Scholar]
- 65. Muthén L, Muthén B. Mplus user’s guide. Los Angeles: Muthén L, Muthén B; 2017. [Google Scholar]
- 66. World Medical Association . World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA J Am Med Assoc. 2013;310(20):2191–4. 10.1001/jama.2013.281053 [DOI] [PubMed] [Google Scholar]
- 67. Dahlin C, Coyne P, Goldberg J, Vaughan L. Palliative care leadership. J Palliat Care. 2019;34(1):21–8. 10.1177/0825859718791427 [DOI] [PubMed] [Google Scholar]
- 68. Scholz B, Bevan A, Georgousopoulou E, Collier A, Mitchell I. Consumer and carer leadership in palliative care academia and practice: a systematic review with narrative synthesis. Palliat Med. 2019;33(8):959–68. 10.1177/0269216319854012 [DOI] [PubMed] [Google Scholar]
- 69. Klarare A, Lind S, Hansson J, Fossum B, Fürst CJ, Lundh HC. Leadership in specialist palliative home care teams: a qualitative study. J Nurs Manag. 2020;28(1):102–11. 10.1111/jonm.12902 [DOI] [PubMed] [Google Scholar]
- 70. Casady W, Dowd T. Shared leadership and the evolution of “one great department”. Radiol Manage. 2005;27(4):52–4, 56–59. [PubMed] [Google Scholar]
- 71. Steinert T, Goebel R, Rieger W. A nurse–physician co‐leadership model in psychiatric hospitals: results of a survey among leading staff members in three sites. Int J Ment Health Nurs. 2006;15(4):251–7. 10.1111/j.1447-0349.2006.00431.x [DOI] [PubMed] [Google Scholar]
- 72. Boak G, Dickens V, Newson A, Brown L. Distributed leadership, team working and service improvement in healthcare. Leadersh Health Serv. 2015;28(4):332–44. 10.1108/LHS-02-2015-0001 [DOI] [PubMed] [Google Scholar]
- 73. Halifax J. The precious necessity of compassion. J Pain Symptom Manag. 2011;41(1):146–53. 10.1016/j.jpainsymman.2010.08.010 [DOI] [PubMed] [Google Scholar]
- 74. Temel JS, Greer JA, Muzikansky A, Gallagher ER, Admane S, Jackson VA, et al. Early palliative care for patients with metastatic non–small‐cell lung cancer. N Engl J Med. 2010;363(8):733–42. 10.1056/NEJMoa1000678 [DOI] [PubMed] [Google Scholar]
- 75. de Zulueta PC. Suffering, compassion and ‘doing good medical ethics’. J Med Ethics. 2015;41:87–90. 10.1136/medethics-2014-102355 [DOI] [PubMed] [Google Scholar]
- 76. Sansó N, Galiana L, Oliver A, Pascual A, Sinclair S, Benito E. Palliative care professionals’ inner life: exploring the relationships among awareness, self‐care, and compassion satisfaction and fatigue, burnout, and coping with death. J Pain Symptom Manag. 2015;50:200–7. 10.1016/j.jpainsymman.2015.02.013 [DOI] [PubMed] [Google Scholar]
- 77. Mills J, Wand T, Fraser JA. Palliative care professionals’ care and compassion for self and others: a narrative review. Int J Palliat Nurs. 2017;23(5):219–29. 10.1016/j.jpainsymman.2015.10.009 [DOI] [PubMed] [Google Scholar]
- 78. Mills J, Wand T, Fraser JA. Examining self‐care, self‐compassion and compassion for others: a cross‐sectional survey of palliative care nurses and doctors. Int J Palliat Nurs. 2018;24(1):4–11. 10.12968/ijpn.2018.24.1.4 [DOI] [PubMed] [Google Scholar]
- 79. Snowden A, Stenhouse R, Young J, Carver H, Carver F, Brown N. The relationship between emotional intelligence, previous caring experience and mindfulness in student nurses and midwives: a cross sectional analysis. Nurse Educ Today. 2015;35(1):152–8. 10.1016/j.nedt.2014.09.004 [DOI] [PubMed] [Google Scholar]
- 80. Abe K, Niwa M, Fujisaki K, Suzuki Y. Associations between emotional intelligence, empathy and personality in Japanese medical students. BMC Med Educ. 2018;18(1):47. 10.1186/s12909-018-1165-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Alshammari F, Pasay‐An E, Gonzales F, Torres S. Emotional intelligence and authentic leadership among Saudi nursing leaders in the Kingdom of Saudi Arabia. J Prof Nurs. 2020;36(6):503–9. 10.1016/j.profnurs.2020.04.003 [DOI] [PubMed] [Google Scholar]
- 82. Paustian‐Underdahl SC, Walker LS, Woehr DJ. Gender and perceptions of leadership effectiveness: a meta‐analysis of contextual moderators. J Appl Psychol. 2014;99(6):1129–45. 10.1037/a0036751 [DOI] [PubMed] [Google Scholar]
- 83. Lindsay EK, Creswell JD. Helping the self help others: Self‐affirmation increases self‐compassion and pro‐social behaviors. Front Psychol. 2014;12(5):421. 10.3389/fpsyg.2014.00421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Neff KD, Pommier E. The relationship between self‐compassion and other‐focused concern among college undergraduates, community adults, and practicing meditators. Self Identity. 2013;12:160–76. 10.1080/15298868.2011.649546 [DOI] [Google Scholar]
- 85. Welp LR, Brown CM. Self‐compassion, empathy, and helping intentions. J Posit Psychol. 2014;9(1):54–65. 10.1080/17439760.2013.831465 [DOI] [Google Scholar]
- 86. Dev V, Fernando AT III, Lim AG, Consedine NS. Does self‐compassion mitigate the relationship between burnout and barriers to compassion? A cross‐sectional quantitative study of 799 nurses. Int J Nurs Stud. 2018;1(81):81–8. 10.1016/j.ijnurstu.2018.02.003 [DOI] [PubMed] [Google Scholar]
- 87. Galiana L, Sansó N, Vidal‐Blanco G, Badenes‐Ribera L. The paths of compassionate care: an approach for end‐of‐life professionals. In: Galiana L, Sansó N, editors. Psychology research progress. The power of compassion. New York: Nova Science Publishers; 2019. p. 297–316. [Google Scholar]
- 88. Sinclair S, Beamer K, Hack TF, McClement S, Raffin Bouchal S, Chochinov HM, et al. Sympathy, empathy, and compassion: a grounded theory study of palliative care patients’ understandings, experiences, and preferences. Palliat Med. 2017;31(5):437–47. 10.1177/0269216316663499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. González‐Hernández E, Campos D, Diego‐Pedro R, Romero R, Baños R, Negi LT, et al. Changes in the semantic construction of compassion after the cognitively‐based compassion training (CBCT®) in women breast cancer survivors. Span J Psychol. 2021;24(24):e34. 10.1017/SJP.2021.31 [DOI] [PubMed] [Google Scholar]
- 90. Klimecki OM, Leiberg S, Ricard M, Singer T. Differential pattern of functional brain plasticity after compassion and empathy training. Soc Cogn Affect Neurosci. 2014;9(6):873–9. 10.1093/scan/nst060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Edmonds KP, Yeung HN, Onderdonk C, Mitchell W, Thornberry K. Clinical supervision in the palliative care team setting: a concrete approach to team wellness. J Palliat Med. 2015;18:274–7. 10.1089/jpm.2014.0248 [DOI] [PubMed] [Google Scholar]
- 92. Kearney MK, Weininger RB, Vachon MLS, Harrison RL, Mount BM. Self‐care of physicians caring for patients at the end of life “being connected … a key to my survival”. J Am Med Assoc. 2009;301:1155–64. 10.1001/jama.2009.352 [DOI] [PubMed] [Google Scholar]
- 93. Abraham A. Health Service Ombudsman . Care and compassion? Report of the health service ombudsman on ten investigations into NHS care of older people, HC 778. London: The Stationery Office; 2011. [Google Scholar]
- 94. Cummings GG, Tate K, Lee S, Wong CA, Paananen T, Micaroni SPM, Chatterjee GE. Leadership styles and outcome patterns for the nursing workforce and work environment: a systematic review. Int J Nurs Stud. 2018;85:19–60. 10.1016/j.ijnurstu.2018.04.016 [DOI] [PubMed] [Google Scholar]
- 95. West MA. Compassionate leadership: sustaining wisdom, humanity and presence in health and social care. London, UK: The Swirling Leaf Press; 2021. [Google Scholar]


