Abstract
Aims
To compare nurses’ non‐optimal eating behaviours across different shifts, to examine whether non‐day shifts were related to deviation from optimal dietary behaviours compared with day shifts and whether such deviation was related to non‐optimal macronutrient intake.
Design
This is a 4‐day intensive longitudinal study.
Methods
A convenience sample of hospital nurses was recruited in Taiwan. From September 2018 through January 2019, 120 participants completed 4‐days of 24‐h dietary recalls. One‐way ANOVA and Kruskal–Wallis H test were used to compare differences in energy and macronutrient intake and frequency of meals and snacking, respectively. Generalized linear regressions examined (1) the associations between shiftwork schedules and non‐optimal eating behaviours and (2) associations between non‐optimal eating and high energy contribution of non‐optimal macronutrients.
Results
Nurses consumed less energy on evening and night shifts compared with day shifts. However, energy intake from snacking was higher on evening and night shifts relative to day shifts. Nurses consumed less meals but had higher snacking frequency on non‐day shifts. In addition, high energy intake from snacking was positively associated with high energy intake from saturated fat.
Conclusions
Nurses were more likely to have non‐optimal eating behaviours on non‐day shifts, which may contribute to an increased intake of saturated fat; thus, increasing their risk of chronic diseases. Strategies to improve non‐day shift nurses' non‐optimal eating behaviours may be beneficial to their health.
Impact
Shiftwork is known to affect nurses' eating behaviours; however, which shift is associated with unhealthy eating remains inconclusive. Despite lower energy intakes, nurses had higher intake by snacking on evening and night shifts. High snacking intake was associated with a high intake of saturated fat. Hospitals can increase the availability of healthy foods on evening or night shifts, which may improve non‐day shift nurses' non‐optimal eating behaviours.
Keywords: circadian rhythms, health care workers, junk food intake, medical personnel, non‐optimal eating behaviours, nurse or nursing, shift schedules, shift work, snack food and sugar‐sweetened beverage consumption
1. INTRODUCTION
To provide the 24/7 services or increase the productivity, several industries have extended their daily operational time from 8 to 24 h by employing shift work (Tucker & Folkard, 2012). Approximately, 16%–20% of the working population is engaged in shift work around the world (Eurofound, 2017; U.S. Bureau of Labor Statistics, 2019). Shift work refers to working during non‐traditional business hours (i.e., 06:00 pm to 06:00 am) (International Agency for Research on Cancer, 2007), which may be misaligned with workers' biological clocks and further impede their health (Bedrosian et al., 2016).
Several studies have suggested that shift workers were at a higher risk of chronic diseases such as cardiovascular diseases (Torquati et al., 2018; Vyas et al., 2012; Wang et al., 2018) or type 2 diabetes (Gan et al., 2015; Gao et al., 2020; Li et al., 2019). This is exemplified in the dose‐response relationship between shift work and cardiovascular diseases (Torquati et al., 2018) and type 2 diabetes (Li et al., 2019). Energy imbalance, particularly from non‐optimal eating behaviours, maybe one of the pathways by which shift work increases the likelihood of chronic diseases (Bonnell et al., 2017; Kaneko et al., 2021; St‐Onge et al., 2017).
Shift work is unavoidable for nurses. Prior research has suggested that working on rotating night shifts may increase nurses' risk of type 2 diabetes, particularly for those who have unhealthy lifestyles such as low‐diet quality (Shan et al., 2018). Examining nurses' non‐optimal eating behaviours may not only help to improve nurses' eating behaviours but also overall health.
2. BACKGROUND
Optimal eating behaviours are defined as having the following situations less than 3 times weekly: skipping breakfast, having dinner in 2 h before bedtime, and having snacks after dinner (Kaneko et al., 2020). Previous studies have linked non‐optimal eating behaviours to a higher incidence of myocardial infarction, stroke, and heart failure (Kaneko et al., 2021). Recent review documents that consistent high‐energy meals (i.e., rich in saturated fat and sugars) cause both physiological dysregulation and dysfunction (e.g., endothelial dysfunction) during the postprandial period and further contribute to the incidence of cardiovascular diseases (Dimina & Mariotti, 2019). Other studies have suggested skipping meals (Kaneko et al., 2021; St‐Onge et al., 2017) and increased sugar‐sweetened beverages (SSBs) consumption (Richelsen, 2013) may contribute to metabolic dysfunction and further increase the risk of cardiovascular diseases (Poirier et al., 2006; Richelsen, 2013; Yu et al., 2016).
Previous studies have documented that shift work is associated with non‐optimal eating behaviours (Cain et al., 2015; de Assis et al., 2003; Hemio et al., 2020; Hemio et al., 2015; Lin et al., 2021; Souza et al., 2019). Night shifts are related to higher energy intake (Fradkin et al., 2019; Hulsegge et al., 2016), markedly from carbohydrates (Fradkin et al., 2019), fat, saturated fat (Hemio et al., 2015; Hemio et al., 2020), energy‐dense foods (Lin et al., 2021; Souza et al., 2019), SSBs (Lin et al., 2021), and snack foods (Cain et al., 2015; de Assis et al., 2003). It was also common practice for meal skipping and unconventionally timed food consumption (Souza et al., 2019). A recent review focusing on nurses' nutrition patterns suggests that nurses working on night shifts have some poor nutritional habits such as more frequent snacking, late dinner, irregular meal patterns, or poor diet quality (Peplonska et al., 2019). However, evidence regarding evening shifts has been relatively lacking.
Recent reviews summarize no significant differences in energy intake (EI) between shift and fixed‐day workers (Bonham et al., 2016; Souza et al., 2019), or between non‐night and night shift workers (Cayanan et al., 2019). A recent study indicates similarity in the eating and snacking patterns between shift and fixed‐day shift workers, however, variable snacking patterns across different shifts (Hulsegge et al., 2020). This also suggests shift work may impact non‐optimal eating behaviours (e.g., snacking).
To provide the round the clock services for patients, nurses need to work shift schedules, particularly for those working in the hospital. Prior research has suggested that working on rotating night shifts combined with an unhealthy lifestyle may exacerbate the adverse effects on nurses' metabolic health (Shan et al., 2018). However, the majority of studies mainly compare shift and fixed‐day nurses' eating behaviours (Han et al., 2016; Peplonska et al., 2019; Yoshizaki et al., 2016; Yoshizaki et al., 2018). Research examining nurses' non‐optimal eating across different shifts remains limited.
3. THE STUDY
3.1. Aims
Based on available evidence to date, the specific aims of this study are to (1) compare nurse's non‐optimal eating behaviours across different shifts and (2) examine whether non‐day shifts (i.e., evening and night shifts) were related to deviation from optimal dietary behaviours compared with day shifts. (3) If so, whether such deviation was related to non‐optimal macronutrient intake (i.e., saturated fat and sugar).
3.2. Design
A 4‐day longitudinal study design was implemented. There were three phases: baseline visit, 4‐day 24‐h dietary recalls, and post‐study visit.
3.3. Sample/participants
A convenience sample of registered nurses working in hospitals was recruited employing electronic flyers shared on social media platforms (e.g., Facebook) and sending e‐mails to the accredited hospitals in Taiwan (Ministry of Health and Welfare, 2017). The inclusion criteria included: (1) full‐time Taiwanese registered nurses (i.e., at least working 40 h per week); (2) aged 20–65 years old; and (3) no intention to imminently leave the nursing profession. The exclusion criteria were as follows: (1) pregnant; (2) unwilling or unable to provide a registry‐based work schedule; (3) working in an administrative position (e.g., Dean, Associate Dean).
We used the Gpower program with the option of ANOVA to estimate the total number of sample size. Using the following settings: power level at 0.80, significance level at 0.05, and a small effect size of 0.13 (Cohen, 1988; de Assis et al., 2003), the minimum sample size for each group (i.e. day, evening and night shifts) was 35.
From September 2018 to January 2019, a total of 129 registered nurses were recruited from 33 hospitals in Taiwan (i.e., 14 medical centres, 17 regional hospitals and 2 district hospitals). Participants who dropped out before starting the first 24‐h dietary recall (n = 5) and those who returned any invalid 24‐h dietary recalls (e.g. missing meals or food portions; n = 4) were excluded. As a result, a total of 120 participants were included in the final analysis. The flowchart of data collection is depicted in Figure S1.
3.4. Data collection
During the baseline visit, participants provided informed consent, completed the baseline questionnaire (including personal and work characteristics), and provided their registry‐based work schedule for the previous 30 days and the published prospective work schedule for the next 30 days. Participants also received tools (i.e., a 15‐cm ruler, a 210‐ml plastic bowl and a 15‐ml plastic spoon) and an instruction booklet for 24‐h dietary recalls. To maintain consistency, the researchers were trained by the same nutritionist and used the provided booklet to instruct each participant on how to perform the 24‐h dietary recalls (e.g. when to record, what to report in each 24‐h dietary recall, and how to photograph their food or beverage intakes).
In addition to the booklet, the trained researchers demonstrated how to measure the portion size using the provided tools. Given the shape and the size of foods, different types of tools were selected. For example, for fried chickens, participants were instructed to measure the size using a 15‐cm ruler (width*length*height), however, using a 210‐ml plastic bowl to measure the amount of rice or noodles they consumed. As for small portion sizes of foods such as nuts, we instructed participants to use a 15‐ml plastic spoon for the measurement.
During the 4‐day self‐reported 24‐h dietary recalls, we requested each participant to complete a 24‐h dietary recall on (1) the non‐workday prior to the consecutive work shifts, (2) the first day in the consecutive work shifts, (3) the last day of the consecutive work shifts, and (4) the first non‐workday after the consecutive work shifts, respectively (Please see Figure 1).
FIGURE 1.
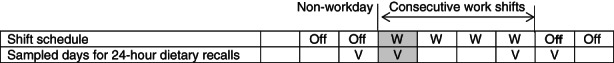
An example of sampled days for 24‐h dietary recalls
In each 24‐h dietary recall, participants were requested to report their food and beverage consumption during the past 24 h in a chronological order on a sheet, including the following items: recorded date and time, the 24‐h period, shift work schedule on that day (e.g. day, evening shift), mealtimes, meal types, locations, food descriptions (e.g. milk, sandwiches), detailed food preparation methods (e.g. cooking methods, sauces) and portion size descriptions. To capture all the dietary intakes during and after h on different shifts, the starting time of each participant's 24‐h dietary recall varied according to their sleep‐wake pattern and shift work schedules. For example, if a participant usually went to bed at 11:00 pm on day shifts and 03:00 am on evening shifts, the 24‐h dietary recall period on their day shifts was 11:00 p.m. (−1) through 10:59 p.m. However, the 24‐h dietary recall period was 03:00 a.m. through 02:59 a.m. (+1) on evening shifts.
In addition, each participant was asked to (1) photograph all the foods and beverages they consumed, (2) complete the 24‐h dietary recall before they went to bed each day, and (3) electronically return the photographs and document them by the end of the following day. The research team would contact the participant if they did not receive responses or in instances of the query (e.g. returned 24‐h dietary recall did not match photographic record).
All the collected data were entered into the Taiwan Dietitian Nutrient Intake Calculating Excel Worksheet (Taiwan Dietitian Association, 2021). Based on the Nutrient Composition Data Bank for Foods in Taiwan Area (2021) (Taiwan Food and Drug Administration, 2021), participants' daily EI and macronutrient intake (i.e. protein, fat, saturated fat, carbohydrates and sugar) were calculated. To avoid interference from the lagged effects of previous work shifts, only the 24‐h dietary recall reported on the first day of returning to work (i.e. the grey highlighted column in Figure 1) was included for analysis. Participants' daily frequency of meals and snacks were assessed by summing the total number of reported meals and snacking in a 24‐h dietary recall, respectively. In addition, the total frequency of meals and snacking was calculated by adding reported meals and snacking frequency. According to the reported meal types, EI from snacking, defined as foods and SSBs consumed outside of main meals (Bellisle, 2014; Hess et al., 2016), was also calculated.
During the post‐study visit, the research team collected participants' registry‐based work schedule for the past 30 days and provided incentives (i.e. approximately USD 30 in cash) after completion of the post‐survey (e.g. any sick leave or shift changes due to personal reasons during the study period).
3.5. Ethical considerations
The study protocol was approved by the Institutional Review Board (IRB) at the National Taiwan University Hospital (No. 201712216RIND). Written informed consent was obtained from all participants.
3.6. Data analysis
We employed STATA 14.0 (Statacorp) for data analyses. Descriptive statistics such as the mean, standard deviation, median, interquartile range (IQR), count, and percentage summarize participants' personal and work characteristics, their EI and macronutrient intake, frequency of meals and snacking and high‐energy meal consumption.
For the first aim, we conducted a one‐way analysis of variance (ANOVA) to examine differences in EI and macronutrient intake across different shift work schedules. If the test result was significant (p < .05), we conducted a post hoc Tukey's HSD test for respective outcomes. Because EI from snacking and frequency of meals and snacking was not normally distributed, we used the Kruskal–Wallis H test to examine the median differences across different shifts. If the test result was significant (p < .05), we performed a Dunn's test with Bonferroni adjustment for pairwise comparison (Dinno, 2015). The Chi‐squared test was used to compare high EI from meals or snacking across different shift schedules. Multiple generalized linear regressions were used to examine (1) the associations between shift work schedules and high EI from meals or snacking (the second aim) and (2) the associations of high EI from snacking with high EI of saturated fat and sugar (the third aim). To select the most parsimonious model for analysis, backward selection methods were used. The significant level was set at 0.05. Only significant covariates (i.e. personal and work characteristics) were included in the final models.
3.6.1. Sensitivity analysis
Recent reviews summarize that rotating shift workers have a greater likelihood of increased body mass index (Chang & Jen, 2020). However, other studies document that fixed night shift workers are at increased risk of dyslipidemia compared with rotating shift workers (Dutheil et al., 2020). This suggests that EI and macronutrient intake may vary between fixed‐ and rotating shift workers. To ensure that our main findings were not confounded by shift patterns, we further examined participants' EI and macronutrient intake across different shifts stratified by work shift patterns (i.e., fixed‐ or rotating).
3.7. Validity and reliability/rigour
3.7.1. Shift work schedules
Participants' shift work schedules were derived from their registry‐based work schedules collected during the baseline visit. All participants were 8‐h workers. Based on their shift start time, there were three different types of shift timings: day (work began between 07:00 and 09:00 am), evening (work began between 02:00 and 04:00 pm), and night shifts (work began between 10:00 pm and midnight) (McMenamin, 2007).
3.7.2. Estimated energy requirement
Estimated energy requirement (EER) referred to the amount of energy needed to balance the energy intake and expenditure (Sasaki, 2008). Therefore, we measured total daily energy expenditure (TDEE) to estimate participant’s EER. TDEE was the sum of sleep energy expenditure (SEE), total physical activity energy expenditure (PAEE), and contribution of the thermic effect of food (TEF). Of which, SEE was equivalent to 30% of daily resting energy expenditure (REE); PAEE was the product of physical activity level (PAL), duration (hour) and weight (kg); TEF was equivalent to approximately 8% of the daily total of EI (Wai, 2012).
Given that registered nurses (RNs) spent more than 4 h standing and moving medical carts to prepare and dispense medications at least twice during their typical shifts, the PAL for this occupation was considered light to moderate intensity (Chappel et al., 2017). Among the Taiwanese population, the average PAL for light and moderate‐intensity occupations was 1.7 and 2.3, respectively (Wai, 2012). As a result, we averaged the light‐ and moderate‐intensity occupational PAL and obtained 2.0 metabolic equivalent (MET) for nurses' occupational PAL. The average PAL for sedentary behaviours (e.g. watching television) was 1.2 MET among the Taiwanese population (Wai, 2012). Therefore, we used 1.2 MET for participants' after‐hour PAL. The final formula for participants' EER was as follows (Wai, 2012):
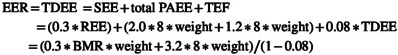 |
where REE was the product of weight (kg) and basal metabolic rate (BMR); total PAEE was the sum of occupational PAL (2.0 MET) and after‐hour PAL (1.2 MET) (Wai, 2012). The detailed information about TDEE calculation was presented in Table S1. Each participant's daily EI and EI contribution of macronutrients were evaluated by calculating the respective percentage of EER.
3.7.3. Non‐optimal eating behaviours and macronutrient intake
Daily frequency of meals and snacking, EI from meals as well as EI from snacking were employed to assess if participants had non‐optimal eating behaviours during a sampled day. According to the healthy meal recommendation, the distribution of EI by three meals was as follows: 28.0%–32.3% for breakfast, 28.7%–36.9% for lunch, and 31.7%–40.7% for dinner (Health Promotion Administration, Ministry of Health and Welfare, 2018). However, there is still limited evidence for the definition of a high‐energy meal. As a result, we arbitrarily defined any meal with an energy content greater than 60% of EER (i.e. approximately 1.5 to 2 times higher than a recommended meal) as indicating a high EI from meals on that day. As for EI from snacking, no recommended percentage of EER has been provided by the Health Promotion Administration, Ministry of Health and Welfare (2018). A recommendation of 9% or lower in light meals was provided in Swedish recommendations (Bergström et al., 1993). We used 27% as a cut‐off point for high‐energy intake from snacking because it is three times that of the recommended 9%, and it represented the 75 percentiles of snacking intake in this group of participants.
Non‐optimal macronutrient intake was measured by participants' contribution of EI to EER coming from saturated fat and sugar. The World Health Organization also recommends that EI from saturated fat and added sugar should account for less than 10% of total daily EI (World Health Organization, 2020). Furthermore, prior research suggests that greater than 10% of EI coming from saturated fat has been associated with cardiovascular diseases (Hooper et al., 2020). Therefore, EI greater than 10% of EER from saturated fat and sugar were, respectively, defined as high EI from saturated fat and high EI from sugar.
3.7.4. Personal and work characteristics
The following personal characteristics collected on the baseline survey were employed to describe the study sample: age, sex, educational attainment, marital status, and health‐related characteristics, including body mass index derived from self‐reported weights and heights, and health conditions (e.g. medical history of diabetes). Working characteristics included job tenure, level of hospital employment, working units, and work shift patterns (i.e. fixed or rotating shifts).
4. RESULTS
A total of 120 participants were included in the final analysis. Overall, the participants' average age was 27.5 (SD: 4.6) years. The majority were females (95.0%), had obtained a bachelor's degree or higher (80.8%), were non‐obese (i.e., BMI < 27) (74.1%), and did not have any chronic disease (70.8%). The average job tenure as a registered nurse was 5.2 (SD: 4.4) years. Most worked in the acute care wards (e.g. medical, or surgical wards), and nearly half (48.3%) were rotating shift workers (Table 1).
TABLE 1.
Participants' characteristics (N = 120)
| Variables | n (%) | Mean (SD) | Range |
|---|---|---|---|
| Demographics | |||
| Age (in years) | 27.5 (4.6) | 21–42 | |
| Female | 114 (95.0) | ||
| Educational attainment | |||
| Associate degree/Junior college | 23 (19.2) | ||
| Bachelor's/Master's/Doctorate degree | 97 (80.8) | ||
| Marital status | |||
| Married/cohabitation | 21 (17.5) | ||
| Single | 99 (82.5) | ||
| Health‐related characteristics | |||
| BMI a (kg/m2) | 22.3 (4.6) | 16.2–41.0 | |
| Underweight | 13 (10.8) | ||
| Normal | 76 (63.3) | ||
| Overweight or obese | 31 (25.8) | ||
| Having at least one chronic condition b | 35 (29.2) | ||
| Work characteristics | |||
| Working as a registered nurse (in years) | 5.2 (4.4) | 0.9–20.2 | |
| Level of hospital employment | |||
| Medical centers | 79 (65.8) | ||
| Regional/District hospitals | 41 (34.2) | ||
| Working units | |||
| Intensive care units | 28 (23.3) | ||
| Emergency room | 10 (8.3) | ||
| Operation room | 4 (3.3) | ||
| Acute care wards c | 78 (65.0) | ||
| Shift work schedules | |||
| Day | 51 (42.5) | ||
| Evening | 37 (30.8) | ||
| Night | 32 (26.7) | ||
| Work shift patterns | |||
| Fixed shifts | 62 (51.7) | ||
| Rotating shifts | 58 (48.3) | ||
Abbreviations: BMI, body mass index; SD, standard deviation.
The definitions of underweight, normal, overweight and obese are BMI < 18.5, BMI ≥ 18.5 and BMI < 24, BMI ≥ 24 and BMI < 27, and BMI ≥ 27 kg/m2, respectively.
Chronic conditions: Diabetes (type 1 or type 2) or high blood sugar, heart diseases (e.g. coronary artery disease, angina, congestive heart failure), hypertension, stroke, high cholesterol/hyperlipidemia, thyroid problems (e.g., hyperthyroidism, hypothyroidism), kidney diseases (e.g. chronic renal failure), cancer or a malignant tumour (excluding minor skin cancer), digestive problems (such as ulcer, colitis or gallbladder disease), mental illnesses (e.g. depression, anxiety) and sleep problems (e.g. insomnia).
Acute care wards included surgical, medical, paediatric, gynaecological, orthopaedic and psychiatric wards.
As presented in the upper panel of Table 2, nurses' EI (%) contributed by fat (F = 4.04, p = .020), carbohydrates (F = 5.14, p = .007) and sugar (F = 3.15, p = .046) were significantly different across each shift. According to the post hoc Tukey's HSD test conducted, we noticed that EI (%) from fat was significantly higher on day shifts relative to night shifts (p = .035). Energy intakes (%) from carbohydrates (p = .006) and sugar (p = .046) were significantly higher on day shifts relative to evening shifts. On average, total daily EI (kcal) on day, evening and night shifts were 1878.9 (SD: 510.4), 1540.1 (SD: 623.7), and 1674.6 (SD: 556.5), respectively. The EI (%) of EER were significantly lower on evening (p = .008) or night shifts (p = .044) compared with their counterparts on day shifts. In contrast, their EI (%) from snacking on evening (median: 19.9, IQR: 9.9–33.8, p < .001) or night shifts (median: 20.5, IQR: 0.1–35.3, p = .012) were significantly higher than their day shift counterparts' (median: 5.6, IQR: 0.0–17.6).
TABLE 2.
Macronutrient and energy intake across different shifts among nurses (N = 120)
| Day | Evening | Night | ANOVA test a | Tukey's HSD test b | ||
|---|---|---|---|---|---|---|
| (n = 51) | (n = 37) | (n = 32) | ||||
| Mean (SD) | Mean (SD) | Mean (SD) | F | p | ||
| Macronutrient intake | ||||||
| Protein (%) c | 15.6 (6.3) | 13.0 (6.0) | 13.6 (6.0) | 2.25 | .110 | — |
| Fat (%) c | 32.9 (10.9) | 26.9 (15.0) | 25.9 (11.1) | 4.04 | .020 | D > N (p = .035) |
| Saturated fat (%) c | 10.9 (3.7) | 9.1 (5.6) | 8.8 (4.3) | 2.81 | .065 | — |
| Carbohydrate (%) c | 50.2 (13.6) | 39.6 (18.6) | 43.4 (15.4) | 5.14 | .007 | D > E (p = .006) |
| Sugar (%) c | 9.0 (6.3) | 5.9 (4.7) | 8.6 (6.6) | 3.15 | .046 | D > E (p = .046) |
| Energy intake | ||||||
| Total daily EI (kcal) | 1878.9 (510.4) | 1540.1 (623.7) | 1674.6 (556.5) | 4.07 | .020 | D > E (p = .016) |
| Total daily EI (%) d | 98.3 (25.5) | 79.3 (35.3) | 82.4 (26.5) | 5.45 | .005 | D > E (p = .008), D > N (p = .044) |
| Median (IQR) | Median (IQR) | Median (IQR) | Kruskal–Wallis H Test e | Dunn's test f | ||
|---|---|---|---|---|---|---|
| χ 2 | p | |||||
| Non‐optimal eating behaviours and macronutrients intakes | ||||||
| Meals or snacking frequency | ||||||
| Meals | 3.0 (2.0–3.0) | 2.0 (1.0–2.0) | 2.0 (1.5–3.0) | 26.59 | <.001 | D > E (p < .001), D > N (p < .001) |
| Snacking | 1.0 (0.0–1.0) | 1.0 (1.0–2.0) | 1.0 (1.0–2.0) | 9.79 | .008 | D < E (p < .001), D < N (p = .004) |
| Sum of meals and snacking | 3.0 (3.0–4.0) | 3.0 (2.0–4.0) | 3.0 (3.0–4.0) | 4.53 | .104 | — |
| EIs from snacking (kcal) | 116 (0.0–350.7) | 418.6 (165.2–711.0) | 446.7 (1.6660.9) | 14.69 | <.001 | D < E (p < .001), D < N (p = .009) |
| EIs from snacking (%) d | 5.6 (0.0–17.6) | 19.9 (9.9–33.8) | 20.5 (0.1–35.3) | 14.58 | <.001 | D < E (p < .001), D < N (p = .012) |
| n (%) | n (%) | n (%) | Chi‐square Test g | ||
|---|---|---|---|---|---|
| χ 2 | p | ||||
| High EI from meals h | 5 (9.8) | 5 (13.5) | 3 (9.4) | 0.40 | .869 i |
| High EI from snacking d | 5 (9.8) | 13 (35.1) | 12 (37.5) | 10.97 | .003 i |
| High EI from saturated fat j | 28 (54.9) | 13 (35.1) | 11 (34.4) | 4.84 | .089 l |
| High EI from sugar k | 16 (31.4) | 9 (24.3) | 8 (25.0) | 0.67 | .715 l |
Abbreviations: ANOVA, analysis of variance; HSD, honestly significant difference; EI, energy intake; IQR, interquartile range.
The degrees of freedom (df) of the F statistics were 2 (df1) and 117 (df2).
One‐way ANOVA with post hoc Tukey HSD test was employed to compare the differences in energy intake across different shifts among participants.
The percentage of energy intake from each macronutrient was calculated based on the following algorithm: (Energy intake from a macronutrient/Daily estimated energy requirement)*100.
The percentage of energy intake was calculated based on the following algorithm: (Energy intake/Daily estimated energy requirement)*100.
Kruskal‐Wallis H test was employed to compare the differences in EI from snacking and meal or snacking frequencies across different shifts among participants. The degrees of freedom (df) of the H (chi‐square) test statistics were 2.
If Kruskal‐Wallis H test was significant, Dunn's test with Bonferroni adjustment (Dinno, 2015) was employed for pairwise comparisons between two shifts among participants.
The degrees of freedom (df) of the chi‐square test statistics were 2.
High EI from meals: >60% of daily estimated energy requirement.
The p value was based on the Fisher's exact test.
High EI from saturated fat: >10% of daily estimated energy requirement.
High EI from sugar: >10% of daily estimated energy requirement.
High EI from snacking: >27% of daily estimated energy requirement.
Bold values indicate statistically significant results.
The middle panel of Table 2 indicates that less meals were consumed on evening (median: 2.0, IQR: 1.0–2.0, p < .001) and night (median: 2.0, IQR: 1.5–3.0, p < .001) shifts compared with day shifts (median: 3.0, IQR: 2.0–3.0). In contrast, snacking was more frequent on evening (median: 1.0, IQR: 1.0–2.0, p < .001) and night (median: 1.0, IQR: 1.0–2.0, p = .004) shifts compared with day shifts (median: 1.0, IQR: 0.0–1.0). Additionally, high EI from snacking were more prevalent among evening (35.1%) and night (37.5%) shift workers relative to day shift workers (9.8%, p = .003) (Table 2).
Table 3 presented associations between shift work and non‐optimal eating behaviours. After adjusting for covariates, compared with day shifts, the likelihood of having high EI from snacking were increased in the evening (OR = 4.9, 95 CI [1.6, 15.5]) and night shifts (OR = 6.0, 95 CI [1.8, 19.8]).
TABLE 3.
Associations between shift work and non‐optimal eating behaviours among nurses (N = 120)
| High EI from meals a , b | High EI from snacking a , c | |
|---|---|---|
| OR (95% CI) | OR (95% CI) | |
| Shift work schedule d | ||
| D | Ref. | Ref. |
| E | 1.5 (0.4, 5.8) | 4.9 (1.6, 15.5) ** |
| N | 1.1 (0.2, 5.1) | 6.0 (1.8, 19.8) ** |
Abbreviations: D, day shifts; E, evening shifts; EI, energy intake; N, night shifts; OR, odds ratio; Ref., reference group.
The percentage of energy intake was calculated based on the following algorithm: (Energy intake/Daily estimated energy requirement)*100.
High EI from meals: >60% of daily estimated energy requirement.
High EI from snacking: >27% of daily estimated energy requirement.
Respective models were adjusted by age (in years) and shift patterns (i.e., fixed or rotating shift).
p < .05.
p < .01.
p < .001.
Bold values indicate statistically significant results.
Associations between high EI from snacking and non‐optimal macronutrient intake were presented in Table 4. High EI from snacking was positively associated with high EI from saturated fat (OR = 4.0, 95% CI [1.4, 10.9]).
TABLE 4.
Associations between high energy intake from snacking and non‐optimal macronutrient intake among nurses (N = 120)
| High EI from saturated fat a , b | High EI from sugar a , c | |
|---|---|---|
| OR (95% CI) | OR (95% CI) | |
| High EI from snacking d , e , f | ||
| No | Ref. | Ref. |
| Yes | 4.0 (1.4, 10.9) ** | 2.1 (0.8, 5.5) |
Abbreviations: EI, energy intake; OR, odds ratio; Ref., reference group.
The percentage of energy intake from saturated fat or sugar was calculated based on the following algorithm: (Energy intake from saturated fat or sugar /Daily estimated energy requirement)*100.
High EI from saturated fat: >10% of daily estimated energy requirement.
High EI from sugar: >10% of daily estimated energy requirement.
The percentage of energy intake from snacking was calculated based on the following algorithm: (Total daily energy intake from foods or SSBs/Daily estimated energy requirement)*100.
High EI from snacking: >27% of daily estimated energy requirement.
Respective models were adjusted by age (in years), shift work schedules (i.e. day, evening, night shifts), and shift patterns (i.e. fixed or rotating shift).
p < .05.
p < .01.
p < .001.
Bold values indicate statistically significant results.
4.1. Sensitivity analysis
Results of the sensitivity analysis were presented in Table S2. After stratifying by work shift patterns (i.e., fixed and rotating shifts), differences in EI and macronutrient intake across different shifts were similar. However, among fixed shiftwork nurses, there were no significant differences in EI and macronutrient intake across each shift. In contrast, among rotating shiftwork nurses, EI (%) of EER (p = .012) and EI (%) from fat (p = .023) were lower on night shifts compared with day shifts. Energy intake (%) contributed by carbohydrates were lower on evening (p = .015) or night (p = .038) shifts relative to day shifts. Energy intake from snacking was higher on non‐day shifts compared with day shifts, particularly on evening shifts (Table S2).
5. DISCUSSION
Our results suggested that nurses consumed less energy from fat on night shifts and less carbohydrates and sugar on evening shifts. On evening and night shifts, nurses had a lower total daily EI compared with day shifts but consumed greater EI from snacking. However, after stratifying by shift patterns, EI and macronutrient intake across each shift were insignificantly different, particularly among fixed shiftwork nurses. Nurses consumed less meals and demonstrated more frequent snacking on evening and night shifts. In addition, working on evening and night shifts was significantly associated with an increased likelihood of having high EI from snacking. High EI from snacking was positively associated with high EI of saturated fat.
Contrary to previous studies (Fradkin et al., 2019; Hulsegge et al., 2016; Peplonska et al., 2019), our study found that EI from fat on night shifts, carbohydrates on evening shifts, and total daily EI on the evening and night shifts were lower compared with day shifts. Prior research suggested that relative to day workers, shift workers skipped more meals at lunch and breakfast (Gupta et al., 2019; Souza et al., 2019). Most shiftwork nurses consumed less meals per day (Han et al., 2016), which may contribute to their inadequate nutrient intake (Sudo & Ohtsuka, 2001). Similarly, our present analyses suggested that on evening or night shifts, workers consumed less meals, which may lead to a reduction in their EI from fat and carbohydrates as well as their total daily EI.
In addition to reduced meal consumption, other studies suggested that compared with day workers, shift workers had poorer appetites (Tepas, 1990), which may also result in reduced EI and inappropriate macronutrient intake on non‐day shifts.
Furthermore, time availability either for food preparation (Bonnell et al., 2017) or for food consumption (Persson & Martensson, 2006; Waterhouse et al., 2003) may influence shift workers' food choices. Workers tended to choose foods that were easy and quick to prepare but often of poor nutritional quality (Bonnell et al., 2017), which may also be one of the reasons for a lower EI from fat and carbohydrates on non‐day shifts.
In sensitivity analysis in which we sought to examine whether differences in EI and macronutrient intake across different shifts would differ depending on shift patterns, our results showed that particularly among rotating shiftwork nurses, EI from fat and carbohydrates as well as total daily EI were reduced on non‐day shifts. However, no significant differences were noted among fixed shiftwork nurses, suggesting that shift patterns may moderate the adverse effects of non‐day shifts on nurses' eating behaviours. Another opportunity is that the small sample size in our sensitivity analysis limits the statistical power to detect the differences across each shift.
In line with prior research (Bonnell et al., 2017; Cain et al., 2015; de Assis et al., 2003; Lin et al., 2021; Souza et al., 2019), our findings showed that EI from snacking in the evening and night shifts were higher compared with day shifts. There were two possible explanations for our findings: First, working during night‐time may disrupt workers' circadian rhythm and perturb appetite hormones (e.g. decreased leptin or increased ghrelin) (Bedrosian et al., 2016), which may change their food preferences and increase snacking behaviours (Broussard et al., 2016; Cain et al., 2015; James et al., 2017).
Second, we noted that the majority of workers skipped meals and increased the frequency of snacking on evening or night shifts in this study. A previous review summarized that shift workers skipped more meals, particularly at breakfast and lunch, and increased their energy intake at night (Souza et al., 2019). Most food outlets were closed and only snacks or SSBs were available during the nighttime. Subsequently, another possible mechanism for the participants' increased EI from snacking on evening and night shifts may have been due to reduced meal intake and less availability of healthy foods on evening or night shifts.
In the literature, there remains controversy over the effects of snacking. Snacking could be either beneficial for the adjustment of energy intake or be detrimental to energy balance and further contribute to obesity (Bellisle, 2014). In this study, we observed that increased EI from snacking was positively associated with their higher intakes of saturated fat. Previous studies suggested that reduced saturated fat and SSB intake were associated with a lower incidence of cardiovascular disease (Hooper et al., 2020; Yu et al., 2016) and metabolic syndrome (Julibert et al., 2019). Therefore, promotion of reduced EI from snacking in shift workers and improvement of diet quality on non‐day shifts would likely be beneficial for lowering shiftwork nurses' risk of chronic diseases.
5.1. Clinical implications
Our present analyses suggested that more than one out of three participants had high EI from snacking when they worked on evening and night shifts. This corresponds with a predominance of snacks or SSBs contributing to workers' energy consumption on evening and night shifts. One of the public health implications of this study is a consideration for prioritization for the provision of a healthy eating environment to reduce workers' high‐energy meal intake, particularly for non‐day shiftwork nurses.
Furthermore, previous studies suggested that time and accessibility were other factors influencing shift workers' food choices and dietary intake (Bonnell et al., 2017). Workload has been linked to meal substitution using SSBs (Lin et al., 2019). Stress and time constraints in the workplace may increase workers' consumption of low‐nutrient foods (Leung et al., 2018). Strategies to reduce stress and workload may also benefit shiftwork nurses' health.
5.2. Strengths and limitations
There are several strengths of this study. First, the majority of studies compared non‐optimal eating behaviours between fixed‐night shift and fixed‐day workers (Bonnell et al., 2017; Cain et al., 2015; Souza et al., 2019). In the present study, we compared participants' EI and macronutrient intake and non‐optimal eating behaviours across different shifts schedules. The current study extends the literature by explaining the effect of different shift schedules on nurses' unhealthy eating behaviours, particularly on evening and night shifts.
Second, most prior research did not describe the timing of dietary data collection or adjust dietary collection periods based on workers' sleep‐wake patterns and shift schedules (Bonham et al., 2016; Cayanan et al., 2019), which may not truly reflect the workers' dietary intakes on evening or night shifts (e.g. food consumption after midnight on evening shifts not accounted). In our present study, each 24‐h dietary recall was adjusted based on the participant's own sleep‐wake patterns and shift schedules to more precisely document dietary intakes on different shifts.
Third, we excluded days with special events from dietary sampling and derived participants' EI and non‐optimal eating behaviours on the first workday during a consecutive shift. This avoids capture of participants' unhabitual dietary intake on workdays and the interference of lagged effects from previous work shifts. Additionally, participants' EI and diet quality were standardized based on the individual's daily recommended EI, which considers the heterogeneity of BMR, thus reducing the potential of information bias.
The current study was limited in several ways. First, the convenience sampling method may introduce selection bias and limit the generalizability of this study. To increase the external validity, we recruited participants from different levels of hospitals (e.g. medical centres, regional hospitals) across four areas in Taiwan. Secondly, 24‐h dietary recalls were self‐reported, which may be affected by recall bias. To reduce this potential, participants were requested to photograph all of their dietary intakes, and researchers would contact the participants if any records did not match. However, it should be noted that these measures were self‐reported as well. Third, the Hawthorne effect (Wickström & Bendix, 2000) and the healthy work effect (McMichael, 1976) could not be ignored in this study. Participants knew their dietary intakes were monitored, which might change their eating behaviours. It is possible that the shiftwork nurses' non‐optimal eating behaviours were underestimated. Furthermore, the majority of our participants were from a healthy population. Those who could not adjust to shift work may have chosen not to work in hospital settings. We only included one 24‐h dietary recall in our present analyses. Therefore, causality between shift work and non‐optimal eating behaviours could not be inferred based on our findings.
Emerging research has suggested that shift workers may redistribute their EI when working on non‐day shifts (Flanagan et al., 2020). Previous studies have revealed that higher EI during nighttime was significantly associated with obesity (Raynor et al., 2018), hyperglycemia (Song et al., 2021) and increased risk of cardiovascular disease (Almoosawi et al., 2013). However, the upper limit of high EI from meals or snacking remains unclear in the literature. The definition of non‐optimal eating behaviours (i.e. high EI from meals and high EI from snacking) were arbitrarily defined in this study. Therefore, additional studies investigating the most optimal energy distribution for workers on different shift schedules, including parameters around maximal EI and contributions from meals and snacks may help to form dietary guidelines for shift workers to better promote their long‐term health outcomes. Additionally, breaks for meals and snacks during shifts may affect nurses' eating behaviours (e.g. the number of eating occasions or food choices) (Waterhouse et al., 2003). Considering time availability for meals and snacks may also be warranted in promoting nurses' eating behaviours.
6. CONCLUSION
To summarize, nurses skipped more meals, consumed less EI from carbohydrates and total daily EI, but increased snacking frequency and had higher EI from snacking on non‐day shifts. This may increase their consumption of saturated fat, which may further expose them to a higher risk of cardiovascular diseases or metabolic syndrome. Creating a healthier eating environment at work (e.g. to increase accessibility to healthier foods during the night, to increase time availabile for food consumption by reducing workload) may alleviate some of the challenges faced by shift workers and be beneficial for non‐day workers' cardiometabolic health.
CONFLICT OF INTEREST
The authors have declared that they have no conflict of interest.
AUTHOR CONTRIBUTIONS
Yue Leon Guo and Judith Shu‐Chu Shiao designed the research; Ting‐Ti Lin, Yi‐Chuan Chen, Hsueh‐Ching Wu and Judith Shu‐Chu Shiao collected the data; Ting‐Ti Lin and Yue Leon Guo analysed the data; Ting‐Ti Lin, Yue Leon Guo, Christopher Gordon, Yi‐Chuan Chen, Hsueh‐Ching Wu, Elizabeth Cayanan, Chung‐Mei Ouyang and Judith Shu‐Chu Shiao wrote the manuscript; Judith Shu‐Chu Shiao had primary responsibility for final content. All authors read and approved the final manuscript.
PEER REVIEW
The peer review history for this article is available at https://publons.com/publon/10.1111/jan.15253.
Supporting information
Figure S1
Table S1–S4
ACKNOWLEDGEMENT
We sincerely thank all participants for their contributions to this study. Open access publishing facilitated by The University of Sydney, as part of the Wiley ‐ The University of Sydney agreement via the Council of Australian University Librarians. [Correction added on 19 May 2022, after first online publication: CAUL funding statement has been added.]
Lin, T‐T , Guo, Y. L. , Gordon, C. J. , Chen, Y‐C , Wu, H‐C , Cayanan, E. , Ouyang, C‐M , Shiao, J‐C. (2022). Snacking among shiftwork nurses related to non‐optimal dietary intake. Journal of Advanced Nursing, 78(11), 3629–3640. 10.1111/jan.15253
Funding informationThis study was supported by the Ministry of Science and Technology (No. 108‐2314‐B‐002‐213‐MY3) and partially sponsored by the National Taiwan University‐University of Sydney Partnership Collaboration Awards.
Contributor Information
Ting‐Ti Lin, Email: tlin@mail.ndmctsgh.edu.tw.
Judith Shu‐Chu Shiao, Email: scshiao@ntu.edu.tw.
DATA AVAILABILITY STATEMENT
The data are not publicly available due to privacy or ethical restrictions.
REFERENCES
- Almoosawi, S. , Prynne, C. J. , Hardy, R. , & Stephen, A. M. (2013). Time‐of‐day of energy intake: Association with hypertension and blood pressure 10 years later in the 1946 British birth cohort. Journal of Hypertension, 31(5), 882–892. 10.1097/HJH.0b013e32835ecc06 [DOI] [PubMed] [Google Scholar]
- Bedrosian, T. A. , Fonken, L. K. , & Nelson, R. J. (2016). Endocrine effects of circadian disruption. Annual Review of Physiology, 78, 109–131. 10.1146/annurev-physiol-021115-105102 [DOI] [PubMed] [Google Scholar]
- Bellisle, F. (2014). Meals and snacking, diet quality and energy balance. Physiology & Behavior, 134, 38–43. 10.1016/j.physbeh.2014.03.010 [DOI] [PubMed] [Google Scholar]
- Bergström, E. , Hernell, O. , & Persson, L. A. (1993). Dietary changes in Swedish adolescents. Acta Paediatrica, 82(5), 472–480. 10.1111/j.1651-2227.1993.tb12726.x [DOI] [PubMed] [Google Scholar]
- Bonham, M. P. , Bonnell, E. K. , & Huggins, C. E. (2016). Energy intake of shift workers compared to fixed day workers: A systematic review and meta‐analysis. Chronobiology International, 33(8), 1086–1100. 10.1080/07420528.2016.1192188 [DOI] [PubMed] [Google Scholar]
- Bonnell, E. K. , Huggins, C. E. , Huggins, C. T. , McCaffrey, T. A. , Palermo, C. , & Bonham, M. P. (2017). Influences on dietary choices during day versus night shift in shift workers: A mixed methods study. Nutrients, 9(3). 10.3390/nu9030193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broussard, J. L. , Kilkus, J. M. , Delebecque, F. , Abraham, V. , Day, A. , Whitmore, H. R. , & Tasali, E. (2016). Elevated ghrelin predicts food intake during experimental sleep restriction. Obesity, 24(1), 132–138. 10.1002/oby.21321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cain, S. W. , Filtness, A. J. , Phillips, C. L. , & Anderson, C. (2015). Enhanced preference for high‐fat foods following a simulated night shift. Scandinavian Journal of Work, Environmental and Health, 41(3), 288–293. 10.5271/sjweh.3486 [DOI] [PubMed] [Google Scholar]
- Cayanan, E. A. , Eyre, N. A. B. , Lao, V. , Comas, M. , Hoyos, C. M. , Marshall, N. S. , Phillips, C. L. , Shiao, J. S. C. , Guo, Y. L. , & Gordon, C. J. (2019). Is 24‐hour energy intake greater during night shift compared to non‐night shift patterns? A systematic review. Chronobiology International, 36(12), 1599–1612. 10.1080/07420528.2019.1666865 [DOI] [PubMed] [Google Scholar]
- Chang, W. P. , & Jen, H. J. (2020). BMI differences between different genders working fixed day shifts and rotating shifts: A literature review and meta‐analysis. Chronobiology International, 37(12), 1754–1765. 10.1080/07420528.2020.1800027 [DOI] [PubMed] [Google Scholar]
- Chappel, S. E. , Verswijveren, S. J. J. M. , Aisbett, B. , Considine, J. , & Ridgers, N. D. (2017). Nurses' occupational physical activity levels: A systematic review. International Journal of Nursing Studies, 73, 52–62. 10.1016/j.ijnurstu.2017.05.006 [DOI] [PubMed] [Google Scholar]
- Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). L. Erlbaum Associates. [Google Scholar]
- de Assis, M. A. , Kupek, E. , Nahas, M. V. , & Bellisle, F. (2003, Apr). Food intake and circadian rhythms in shift workers with a high workload. Appetite, 40(2), 175–183. 10.1016/S0195-6663(02)00133-2 [DOI] [PubMed] [Google Scholar]
- Dimina, L. , & Mariotti, F. (2019). The postprandial appearance of features of cardiometabolic risk: Acute induction and prevention by nutrients and other dietary substances. Nutrients, 11(9). 10.3390/nu11091963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dinno, A. (2015). Nonparametric pairwise multiple comparisons in independent groups using Dunn's test. The Stata Journal, 15(1), 292–300. 10.1177/1536867X1501500117 [DOI] [Google Scholar]
- Dutheil, F. , Baker, J. S. , Mermillod, M. , De Cesare, M. , Vidal, A. , Moustafa, F. , Pereira, B. , & Navel, V. (2020). Shift work, and particularly permanent night shifts, promote dyslipidaemia: A systematic review and meta‐analysis. Atherosclerosis, 313, 156–169. 10.1016/j.atherosclerosis.2020.08.015 [DOI] [PubMed] [Google Scholar]
- Eurofound . (2017). Sixth European Working Conditions Survey – Overview report (2017 update). Office of the European Union. [Google Scholar]
- Flanagan, A. , Lowson, E. , Arber, S. , Griffin, B. A. , & Skene, D. J. (2020). Dietary patterns of nurses on rotational shifts are marked by redistribution of energy into the nightshift. Nutrients, 12(4), 1053. https://www.mdpi.com/2072‐6643/12/4/1053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fradkin, L. , Raz, O. , & Boaz, M. (2019). Nurses who work rotating shifts consume more energy, macronutrients and calcium when they work the night shift versus day shift. Chronobiology International, 36(2), 288–295. 10.1080/07420528.2018.1538155 [DOI] [PubMed] [Google Scholar]
- Gan, Y. , Yang, C. , Tong, X. , Sun, H. , Cong, Y. , Yin, X. , Li, L. , Cao, S. , Dong, X. , Gong, Y. , Shi, O. , Deng, J. , Bi, H. , & Lu, Z. (2015). Shift work and diabetes mellitus: A meta‐analysis of observational studies. Occupational and Environmental Medicine, 72(1), 72–78. 10.1136/oemed-2014-102150 [DOI] [PubMed] [Google Scholar]
- Gao, Y. , Gan, T. , Jiang, L. , Yu, L. , Tang, D. , Wang, Y. , Li, X. , & Ding, G. (2020). Association between shift work and risk of type 2 diabetes mellitus: A systematic review and dose‐response meta‐analysis of observational studies. Chronobiology International, 37(1), 29–46. 10.1080/07420528.2019.1683570 [DOI] [PubMed] [Google Scholar]
- Gupta, C. C. , Coates, A. M. , Dorrian, J. , & Banks, S. (2019). The factors influencing the eating behaviour of shiftworkers: What, when, where and why. Industrial Health, 57(4), 419–453. 10.2486/indhealth.2018-0147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han, K. , Choi‐Kwon, S. , & Kim, K. S. (2016). Poor dietary behaviors among hospital nurses in Seoul, South Korea. Applied Nursing Research, 30, 38–44. 10.1016/j.apnr.2015.10.009 [DOI] [PubMed] [Google Scholar]
- Health Promotion Administration, Ministry of Health and Welfare . (2018). Examples of healthy meal recipe. https://www.hpa.gov.tw/Pages/Detail.aspx?nodeid=544&pid=9605 [Google Scholar]
- Hemio, K. , Lindstrom, J. , Peltonen, M. , Harma, M. , Viitasalo, K. , & Puttonen, S. (2020). The association of work stress and night work with nutrient intake ‐ a prospective cohort study. Scandinavian Journal of Work, Environmental and Health, 46(5), 533–541. 10.5271/sjweh.3899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hemio, K. , Puttonen, S. , Viitasalo, K. , Harma, M. , Peltonen, M. , & Lindstrom, J. (2015). Food and nutrient intake among workers with different shift systems. Occupational and Environmental Medicine, 72(7), 513–520. 10.1136/oemed-2014-102624 [DOI] [PubMed] [Google Scholar]
- Hess, J. M. , Jonnalagadda, S. S. , & Slavin, J. L. (2016). What is a snack, why do we snack, and how can we choose better snacks? A review of the definitions of snacking, motivations to snack, contributions to dietary intake, and recommendations for improvement. Advances in Nutrition, 7(3), 466–475. 10.3945/an.115.009571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hooper, L. , Martin, N. , Jimoh, O. F. , Kirk, C. , Foster, E. , & Abdelhamid, A. S. (2020). Reduction in saturated fat intake for cardiovascular disease. Cochrane Database Systematic Reviews, 8, CD011737. 10.1002/14651858.CD011737.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hulsegge, G. , Boer, J. M. , van der Beek, A. J. , Verschuren, W. M. , Sluijs, I. , Vermeulen, R. , & Proper, K. I. (2016). Shift workers have a similar diet quality but higher energy intake than day workers. Scandinavian Journal of Work, Environmental and Health, 42(6), 459–468. 10.5271/sjweh.3593 [DOI] [PubMed] [Google Scholar]
- Hulsegge, G. , Loef, B. , Benda, T. , van der Beek, A. J. , & Proper, K. I. (2020). Shift work and its relation with meal and snack patterns among healthcare workers. Scandinavian Journal of Work, Environmental and Health, 46(2), 143–151. 10.5271/sjweh.3829 [DOI] [PubMed] [Google Scholar]
- International Agency for Research on Cancer . (2007). Painting, firefighting, and shiftwork. International Agency for Research on Cancer. https://publications.iarc.fr/116 [Google Scholar]
- James, S. M. , Honn, K. A. , Gaddameedhi, S. , & Van Dongen, H. P. A. (2017). Shift work: Disrupted circadian rhythms and sleep‐implications for health and well‐being. Current Sleep Medicine Reports, 3(2), 104–112. 10.1007/s40675-017-0071-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Julibert, A. , Bibiloni, M. , & Tur, J. A. (2019). Dietary fat intake and metabolic syndrome in adults: A systematic review. Nutrition, Metabolism, and Cardiovascular Diseases, 29(9), 887–905. 10.1016/j.numecd.2019.05.055 [DOI] [PubMed] [Google Scholar]
- Kaneko, H. , Itoh, H. , Kamon, T. , Fujiu, K. , Morita, K. , Michihata, N. , Jo, T. , Morita, H. , Yasunaga, H. , & Komuro, I. (2020). Association of Cardiovascular Health Metrics with Subsequent Cardiovascular Disease in young adults. Journal of the American College of Cardiology, 76(20), 2414–2416. 10.1016/j.jacc.2020.09.545 [DOI] [PubMed] [Google Scholar]
- Kaneko, H. , Itoh, H. , Kiriyama, H. , Kamon, T. , Fujiu, K. , Morita, K. , Michihata, N. , Jo, T. , Takeda, N. , Morita, H. , Yasunaga, H. , & Komuro, I. (2021). Possible association between eating behaviors and cardiovascular disease in the general population: Analysis of a nationwide epidemiological database. Atherosclerosis, 320, 79–85. 10.1016/j.atherosclerosis.2021.01.022 [DOI] [PubMed] [Google Scholar]
- Lin, T. T. , Guo, Y. L. , Gordon, C. , Cayanan, E. , Chen, Y. C. , Ouyang, C. M. , & Shiao, J. S. (2019). Association between sugar‐sweetened beverage consumption as meal substitutes, workload, and obesity in nurses: A cross‐sectional study. International Journal of Environmental Research and Public Health, 16(24), 4984. 10.3390/ijerph16244984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung, S. L. , Barber, J. A. , Burger, A. , & Barnes, R. D. (2018). Factors associated with healthy and unhealthy workplace eating behaviours in individuals with overweight/obesity with and without binge eating disorder. Obesity Science & Practice, 4(2), 109–118. 10.1002/osp4.151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, W. , Chen, Z. , Ruan, W. , Yi, G. , Wang, D. , & Lu, Z. (2019). A meta‐analysis of cohort studies including dose‐response relationship between shift work and the risk of diabetes mellitus. European Journal of Epidemiology, 34(11), 1013–1024. 10.1007/s10654-019-00561-y [DOI] [PubMed] [Google Scholar]
- Lin, T. T. , Park, C. , Kapella, M. C. , Martyn‐Nemeth, P. , Tussing‐Humphreys, L. , Rospenda, K. M. , & Zenk, S. N. (2021). Shift work relationships with same‐ and subsequent‐day empty calorie food and beverage consumption. Scandinavian Journal of Work, Environmental and Health, 46(6), 579–588. 10.5271/sjweh.3903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMenamin, T. M. (2007). A time to work: Recent trends in shift work and flexible schedules. Retrieved from https://www.bls.gov/opub/mlr/2007/12/art1full.pdf
- McMichael, A. J. (1976). Standardized mortality ratios and the "healthy worker effect": Scratching beneath the surface. Journal of Occupational and Environmental Medicine, 18(3), 165–168. 10.1097/00043764-197603000-00009 [DOI] [PubMed] [Google Scholar]
- Ministry of Health and Welfare . (2017). List of accredited hospitals 2013–2016. https://www.mohw.gov.tw/dl‐23917‐a2e699bc‐f0bd‐4d32‐adff‐6cde28f57e1a.html [Google Scholar]
- Morze, J. , Danielewicz, A. , Hoffmann, G. , & Schwingshackl, L. (2020). Diet quality as assessed by the healthy eating index, alternate healthy eating index, dietary approaches to stop hypertension score, and health outcomes: A second update of a systematic review and meta‐analysis of cohort studies. Journal of the academy of Nutrition and Dietetics, 120(12), 1998–2031 e1915. 10.1016/j.jand.2020.08.076 [DOI] [PubMed] [Google Scholar]
- Persson, M. , & Martensson, J. (2006). Situations influencing habits in diet and exercise among nurses working night shift. Journal of Nursing Management, 14(5), 414–423. 10.1111/j.1365-2934.2006.00601.x [DOI] [PubMed] [Google Scholar]
- Peplonska, B. , Kaluzny, P. , & Trafalska, E. (2019). Rotating night shift work and nutrition of nurses and midwives. Chronobiology International, 36(7), 945–954. 10.1080/07420528.2019.1602051 [DOI] [PubMed] [Google Scholar]
- Poirier, P. , Giles, T. D. , Bray, G. A. , Hong, Y. , Stern, J. S. , Pi‐Sunyer, F. X. , Eckel, R. H. , & American Heart, A., Obesity Committee of the Council on Nutrition, P. A., & Metabolism . (2006). Obesity and cardiovascular disease: Pathophysiology, evaluation, and effect of weight loss: An update of the 1997 American Heart Association scientific statement on obesity and heart disease from the obesity Committee of the Council on nutrition, physical activity, and metabolism. Circulation, 113(6), 898–918. 10.1161/CIRCULATIONAHA.106.171016 [DOI] [PubMed] [Google Scholar]
- Raynor, H. A. , Li, F. , & Cardoso, C. (2018). Daily pattern of energy distribution and weight loss. Physiology & Behavior, 192, 167–172. 10.1016/j.physbeh.2018.02.036 [DOI] [PubMed] [Google Scholar]
- Richelsen, B. (2013). Sugar‐sweetened beverages and cardio‐metabolic disease risks. Current Opinion in Clinical Nutrition and Metabolic Care, 16(4), 478–484. 10.1097/MCO.0b013e328361c53e [DOI] [PubMed] [Google Scholar]
- Sasaki, S. (2008). Dietary reference intakes (DRIs) in Japan. Asia Pacific Journal of Clinical Nutrition, 17, 420–444. https://apjcn.nhri.org.tw/server/APJCN/17%20Suppl%202/420.pdf [PubMed] [Google Scholar]
- Shan, Z. , Li, Y. , Zong, G. , Guo, Y. , Li, J. , Manson, J. E. , Hu, F. B. , Willett, W. C. , Schernhammer, E. S. , & Bhupathiraju, S. N. (2018). Rotating night shift work and adherence to unhealthy lifestyle in predicting risk of type 2 diabetes: Results from two large US cohorts of female nurses. BMJ, 363, k4641. 10.1136/bmj.k4641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sudo, N. , & Ohtsuka, R. (2001). Nutrient intake among female shift workers in a computer factory in Japan. International Journal of Food Sciences and Nutrition, 52(4), 367–378. 10.1080/09637480120057530 [DOI] [PubMed] [Google Scholar]
- Song, X. , Wang, H. , Su, C. , Wang, Z. , Du, W. , Hu, H. , Huang, F. , Zhang, J. , Jia, X. , Jiang, H. , Ouyang, Y. , Li, L. , Bai, J. , Zhang, X. , Ding, G. , & Zhang, B. (2021). Trajectories of energy intake distribution and subsequent risk of hyperglycemia among Chinese adults: Findings from the China health and nutrition survey (1997‐2018). European Journal of Nutrition. 10.1007/s00394-021-02745-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Souza, R. V. , Sarmento, R. A. , de Almeida, J. C. , & Canuto, R. (2019). The effect of shift work on eating habits: A systematic review. Scandinavian Journal of Work, Environmental and Health, 45(1), 7–21. 10.5271/sjweh.3759 [DOI] [PubMed] [Google Scholar]
- St‐Onge, M. P. , Ard, J. , Baskin, M. L. , Chiuve, S. E. , Johnson, H. M. , Kris‐Etherton, P. , Varady, K. , & American Heart Association Obesity Committee of the Council on, L., Cardiometabolic, H., Council on Cardiovascular Disease in the, Y., Council on Clinical, C., & Stroke, C . (2017). Meal timing and frequency: Implications for cardiovascular disease prevention: A scientific statement from the American Heart Association. Circulation, 135(9), e96–e121. 10.1161/CIR.0000000000000476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taiwan Dietitian Association . (2021). Brief calculating format of macro‐ and micro‐nutrient intakes. http://www.dietitians.org.tw/download
- Taiwan Food and Drug Administration . (2021). Nutrient composition data bank for foods. https://data.gov.tw/dataset/8543 [Google Scholar]
- Tepas, D. I. (1990). Do eating and drinking habits interact with work schedule variables? Work & Stress, 4(3), 203–211. 10.1080/02678379008256983 [DOI] [Google Scholar]
- Torquati, L. , Mielke, G. I. , Brown, W. J. , & Kolbe‐Alexander, T. (2018). Shift work and the risk of cardiovascular disease. A systematic review and meta‐analysis including dose‐response relationship. Scandinavian Journal of Work, Environmental and Health, 44(3), 229–238. 10.5271/sjweh.3700 [DOI] [PubMed] [Google Scholar]
- Tucker, P. , & Folkard, S. (2012). Working time, health, and safety: A research synthesis paper. http://www.ilo.org/travail/whatwedo/publications/WCMS_181673/lang‐en/index.htm [Google Scholar]
- U.S. Bureau of Labor Statistics . (2019). Job Flexibilities and work schedules—2017–2018 data from the American time survey. https://www.bls.gov/news.release/flex2.nr0.htm [Google Scholar]
- Vyas, M. V. , Garg, A. X. , Iansavichus, A. V. , Costella, J. , Donner, A. , Laugsand, L. E. , Janszky, I. , Mrkobrada, M. , Parraga, G. , & Hackam, D. G. (2012). Shift work and vascular events: Systematic review and meta‐analysis. BMJ, 345, e4800. 10.1136/bmj.e4800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wai, J. P. M. (2012). Calories. In Wu S. I. (Ed.), Dietary reference intakes (7th ed., pp. 10–47). Taiwan Food and Drug Administration). https://www.hpa.gov.tw/Pages/Detail.aspx?nodeid=544&pid=725&sid=728 [Google Scholar]
- Wang, D. , Ruan, W. , Chen, Z. , Peng, Y. , & Li, W. (2018). Shift work and risk of cardiovascular disease morbidity and mortality: A dose‐response meta‐analysis of cohort studies. European Journal of Preventative Cardiology, 25(12), 1293–1302. 10.1177/2047487318783892 [DOI] [PubMed] [Google Scholar]
- Waterhouse, J. , Buckley, P. , Edwards, B. , & Reilly, T. (2003). Measurement of, and some reasons for, differences in eating habits between night and day workers. Chronobiology International, 20(6), 1075–1092. 10.1081/CBI-120025536. [DOI] [PubMed] [Google Scholar]
- Wickström, G. , & Bendix, T. (2000). The "Hawthorne effect"—What did the original Hawthorne studies actually show? Scandinavian Journal of Work, Environment & Health, 4, 363–367. 10.5271/sjweh.555 [DOI] [PubMed] [Google Scholar]
- World Health Organization . (2020). Healthy diet. World Health Organization. https://www.who.int/news‐room/fact‐sheets/detail/healthy‐diet [Google Scholar]
- Yoshizaki, T. , Kawano, Y. , Noguchi, O. , Onishi, J. , Teramoto, R. , Sunami, A. , Yokoyama, Y. , Tada, Y. , Hida, A. , & Togo, F. (2016). Association of eating behaviours with diurnal preference and rotating shift work in Japanese female nurses: A cross‐sectional study. BMJ Open, 6(11), e011987. 10.1136/bmjopen-2016-011987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoshizaki, T. , Komatsu, T. , Tada, Y. , Hida, A. , Kawano, Y. , & Togo, F. (2018). Association of habitual dietary intake with morningness‐eveningness and rotating shift work in Japanese female nurses. Chronobiology International, 35(3), 392–404. 10.1080/07420528.2017.1410169 [DOI] [PubMed] [Google Scholar]
- Yu, E. , Rimm, E. , Qi, L. , Rexrode, K. , Albert, C. M. , Sun, Q. , Willett, W. C. , Hu, F. B. , & Manson, J. E. (2016). Diet, lifestyle, biomarkers, genetic factors, and risk of cardiovascular disease in the Nurses' health studies. American Journal of Public Health, 106(9), 1616–1623. 10.2105/AJPH.2016.303316 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1
Table S1–S4
Data Availability Statement
The data are not publicly available due to privacy or ethical restrictions.


