Abstract
Purpose: Working in a hospital setting during a global health pandemic can lead to increased levels of anxiety, stress, burnout, and depression. Anecdotal evidence exists, but there is little research utilizing clinically validated tools to measure hospital staff psychological distress.
Methods: In Summer 2021, 771 hospital staff in North Dakota responded to an electronic survey collecting demographic data and employing validated behavioral health screening tools to assess anxiety, depression, emotional distress, and work‐related quality of life.
Findings: Compassion satisfaction was significantly higher for those who worked in rural areas than urban [t(769) = –1.99, P = .0467]. The burnout rating was significantly higher for those who worked in urban areas than rural [t(769) = 2.23, P = .0261)]. There was no significant geographic variation in stress, anxiety, or depression. Anxiety, depression, burnout, and stress were all significantly higher for those who worked directly with COVID‐19 patients than those who did not, regardless of hospital location.
Conclusions: Hospital staff caring for COVID‐19 patients experienced equitable (and high) levels of depression and anxiety. However, data indicate that rural providers experienced greater protective factors, resulting in lower rates of burnout and higher compassion satisfaction. Rural communities, hospitals, and health systems may have characteristics that could be duplicated in urban areas to support hospital staff well‐being. Support and promotion of mental wellness must also come from the hospital system, and health care and policy leaders. If we do not care for our hospital staff, there will not be hospital staff left to care for the community.
Keywords: behavioral health, burnout, compassion fatigue, COVID‐19, provider well‐being
INTRODUCTION
On January 30, 2020, the World Health Organization (WHO) declared COVID‐19 an “international public health state of emergency.” 1 The outbreak has placed hospital workers under appreciable stress manifested by fatigue, psychological distress, insomnia, depression, anxiety, social stigmatization, and physical exhaustion. 2 These individuals also experience the same stressors as the public which include the impact of social distancing, quarantine, variable work and school schedules, inability to physically interact with relatives and friends, and the possibility of personal and family illness and death. 3
Understanding that providers and hospital employees have been under prolonged stress, and recognizing the need to provide supports to maintain a healthy workforce, it is imperative to examine the well‐being of our hospital workforce and to determine risks and risk mitigations to support their mental health. Workplace stress, moral injury, and comparison fatigue among our hospital workforce lead to workforce shortages as people leave their careers. Simultaneously, it increases the risk of those who stay making errors or providing lower quality of patient care. 4 , 5
Hospital workforce mental wellness before the pandemic
According to the 2018 Physician Workload Survey, before the pandemic, 74% of physicians reported frequently seeing symptoms of burnout in others and more than half (52%) indicated feeling burned out themselves. 6 Nearly, 1 in 4 (23%) admitted that their means of coping with the stress was to drink alcohol; 41% stated they self‐isolate, and 32% indicated they eat junk food. Stress and unhealthy coping habits do not support a physically and mentally fit health care workforce. 6
On average, 1 physician dies by suicide each day, nearly double the rate of the general population. 7 , 8 , 9 , 10 The stress of working in a caring industry is not isolated to physicians and a large body of literature has examined the stress and levels of retention for the nursing workforce as well. 3 , 11 , 12 Among the nursing workforce, those working in emergency rooms or emergency settings tend to report higher rates of mental duress and prolonged stress than those in a general hospital setting. 12 , 13 Although persons working in health professions may recognize signs of psychological stress, there may be stigma in seeking care, perception they can care for themselves, or fear of losing their medical licenses if diagnosed with a mental illness. Seeking care can be especially problematic in a rural community because care may not be local, and if it is, anonymity may be a challenge.
Mental health and wellness among the health care working during a global health pandemic
Mainstream media has been covering the hospital workforce crisis and continues to report on workforce shortages throughout the United States. Although there is a depth of information being reported in print and broadcasting media, little reputable research has been conducted on the mental wellness of hospital staff in the United States (though there is growing international literature). Even less has been done with a focus on the persons working in, and serving, rural communities.
A recent study among adults broadly (United States and other) indicated that level of worry or concern around COVID‐19 was strongly associated with generalized anxiety disorder and probability of depression. 14 This study also examined variability between those working in health care and the general population. Although health care workers were more likely to worry about contracting COVID‐19, they did not report greater rates of anxiety nor depression when compared to nonhealth care providers. 14 This study, however, was a convenience sample and recognized crowdsourcing research methods as a limitation. The study also specifically called for work to be done with a focus on the hospital workforce with “data regarding exposure to COVID‐19 patients.” 14 Conducted early in the pandemic and among a small sample (140) of US providers, Korkmaz and team noted that 71% of those surveyed reported mild, moderate, or severe anxiety. 15
International research is reporting anxiety, stress, and depression among those who do, or do not, care for COVID‐19 patients; or, are assessing those who do, and do not, live close to disease epicenters. Health care workers in China exposed to patients with COVID‐19 reported a high risk of developing “unfavorable mental health outcomes,” which included measures of depression, anxiety, insomnia, and distress. 16 The tools utilized to measure anxiety and depression in this study included the 9‐item Patient Health Questionnaire (PHQ‐9) and the 7‐item Generalized Anxiety Disorder scale (GAD‐7). 16 More than 70% of those surveyed reported psychological distress. The authors also found that nurses had higher rates of symptoms of depression and anxiety than did physicians. 16 In Spain, researchers found that emotional distress and intensity of stress among the health care workforce was more intense in the territories with the highest rates of COVID‐19 and COVID‐19 deaths per day. 17
Similar research in Peru found that roughly 22% of health care workers experienced severe anxiety and 26% reported severe mental distress. 18 In this case, higher levels of anxiety and turnover were reported among those working closer to the epicenter of the pandemic, those who were working more hours, and those working in the private (vs public) sector. 18 A study in Nepal found that 38% of health care workers were suffering from anxiety and/or depression while on COVID‐19 duty. 19 Although some of these studies took into consideration proximity to geographic epicenters of disease spread, they did not explore rural or urban variability and only included clinical providers and not all hospital staff.
Research purpose
This research sought to assess the levels of anxiety, depression, stress, and professional quality of life among all hospital staff in North Dakota. Based on print media in the United States 20 , 21 , 22 , 23 , 24 and literature from outside of the United States, 16 , 17 , 18 , 19 , 25 , 26 , 27 the research team explored levels of anxiety, depression, stress, and professional quality of life among all hospital staff to include those working in auxiliary roles, sanitation, billing, and leadership. In response to previous researchers’ calls to action, this study also specifically explored variable levels of mental duress based on the individual's exposure to patients with COVID‐19 and the geographic location of the hospital (rural or urban). Recognizing that previous international research has correlated working with COVID‐19 patients or in epicenters with increased psychological distress, this study included additional hospital staff who may frequently come into contact with COVID‐19 patients in a hospital setting. Hospital workforce included hospital leadership positions, pharmacy or lab, housekeeping, custodial, laundry, maintenance, business office, administrative support, billing, medical records, and coding or similar functions. However, it is important to note that the final sample was largely persons working in nursing professions.
It is imperative that research assesses the health status of those individuals who continue to work on the frontlines of the pandemic, and that we utilize these results to invest in programs and workforce supports for those at greatest risk of prolonged stress, anxiety, and depression. The health care workforce has always needed behavioral health investments, but it is hypothesized that those working directly with COVID‐19 patients and in our rural hospital systems may be at an increased risk of psychological distress.
METHODS
We developed an electronic survey utilizing clinically and statistically validated tools for assessing anxiety, depression, stress, and professional quality of life. The survey, sampling, and research method were approved by the university's Institution Review Board. The survey was disseminated electronically between May and June 2021. The research team includes a rural critical access hospital (CAH) chief executive officer (CEO), a professor and health services researchers, and a health care workforce data analyst.
Survey design
The survey included 2 demographic questions (age and gender identify) and 5 questions about the participant's employment (professional role, years working in health care, rural or urban designation of their hospital, hospital location on eastern or western half of state, and if the hospital where they worked was a CAH). Finally, respondents also indicated if they had provided care to a COVID‐19 patient (yes or no).
Because this study sought to assess the impact of the pandemic on all hospital staff, the survey question on professional role included all possible hospital staff. See Table 1. Hospital staff completed 4 scales measuring mental wellness. In order, the scales included measures of anxiety, depression, stress, and professional quality of life.
TABLE 1.
Experiences and variability of anxiety, depression, stress, and professional quality of life by participant demographics
| Total | Anxiety: categorical (%) | Depression: categorical | PSS | Professional QoL: mean | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | % | No anxiety | Anxiety | Sig. | No or minimal | Mild to moderate | Moderately severe to severe | Sig. | Mean | Compassion satisfaction | Burnout | STS | ||
| Location | Rural | 344 | 44.62% | 36.58% | 8.04% | ns | 27.01% | 15.02% | 2.37% | ns | 9.37 | 38.9 | 22.1 | 19.3 |
| Urban | 427 | 55.38% | 45.53% | 9.86 | ns | 31.36% | 20.55% | 3.69% | ns | 9.58 | 37.9 | 23.1 | 19.3 | |
| COVID‐19 patients | Yes, interacted | 421 | 54.60% | 43.19% | 11.41% | 29.91% | 20.95% | 3.43% | ns | 9.81 | 38 | 23.7 | 20.6 | |
| No, did not interact | 350 | 45.40% | 38.91% | 6.49% | P = .017 | 28.46% | 14.62% | 2.64% | ns | 9.10 | 38.9 | 21.5 | 17.8 | |
| Gender | Man | 118 | 15.30% | 12.58% | 2.72% | ns | 9.49% | 4.74% | 0.79% | ns | 8.41 | 38.5 | 22.5 | 18.9 |
| Woman | 643 | 83.40% | 68.48% | 14.92% | ns | 48.09% | 30.30% | 5.27% | ns | 9.71 | 38.29 | 22.7 | 19.4 | |
| Other/no answer | 10 | 1.30% | 1.04% | 0.26% | ns | 0.79% | 0.52% | 0.00% | ns | 7.7 | 43 | 19.8 | 17.7 | |
| Age | 18‐24 | 43 | 5.58% | 4.02% | 1.56% | 2.77% | 1.98% | 0.66% | ns | 10.84 | 36.9 | 23.9 | 21.9 | |
| 25‐40 | 341 | 44.23% | 34.24% | 9.99% | 24.24% | 16.47% | 3.69% | ns | 9.94 | 37.5 | 23.8 | 19.8 | ||
| 41‐56 | 238 | 30.87% | 26.07 | 4.80% | 17.79% | 12.12% | 0.79% | ns | 9.42 | 38.7 | 22.2 | 18.8 | ||
| 57‐64 | 114 | 14.79% | 13.49% | 1.30% | 9.88% | 4.08% | 0.92% | ns | 8.3 | 40.0 | 21 | 18.3 | ||
| 65‐75 | 34 | 4.41% | 4.15% | 0.26% | 3.56% | 0.92% | 0.00% | ns | 7.68 | 40.7 | 18.9 | 17.7 | ||
| 76+ | 1 | 0.13% | 0.13% | 0.00% | P = .002 | 0.0% | 0.0% | 0.00% | ns | 10 | 45 | 15 | 18 | |
| Hospital position | Nursing staff | 262 | 33.98% | 27.63% | 6.36% | ns | 17.52% | 14.62% | 1.84% | ns | 9.67 | 37.5 | 23.7 | 20.6 |
| Hospital leader | 57 | 7.39% | 6.10% | 1.30% | ns | 4.35% | 2.37% | 0.40% | ns | 9 | 39.4 | 21.9 | 19.4 | |
| Physicians | 12 | 1.56% | 1.30% | 0.26% | ns | 1.19% | 0.4% | 0.00% | ns | 8.25 | 39.4 | 22.4 | 17.4 | |
| PA or NP a | 30 | 3.89% | 3.11% | 0.78% | ns | 2.64% | 1.19% | 0.13% | ns | 9.07 | 38.8 | 22.9 | 19.1 | |
| Other direct‐care | 128 | 16.60% | 12.97% | 3.36% | ns | 9.49% | 5.8% | 1.58% | ns | 10 | 39.1 | 23.3 | 20.1 | |
| Pharmacy, lab | 62 | 8.04% | 6.61% | 1.43% | ns | 4.87% | 2.77% | 0.53% | ns | 9.66 | 37.9 | 22.8 | 18.2 | |
| Business office, support b | 121 | 15.69% | 13.49% | 2.20% | ns | 9.49% | 5.53% | 0.92% | ns | 9.36 | 38.7 | 20.6 | 17.8 | |
| Custodial, similar c | 33 | 4.28% | 3.37% | 0.91% | ns | 2.77% | 0.92% | 0.40% | ns | 8.81 | 39.6 | 21.6 | 19.7 | |
| Other | 66 | 8.56% | 7.52% | 1.04% | ns | 6.06% | 1.98% | 0.26% | ns | 9 | 38.6 | 22.4 | 17 | |
| Total | 771 | — | 82.1% | 17.9% | — | 58.37% | 35.57% | 6.06% | — | 9.49 | 38.4 | 22.66 | 19.32 | |
aPhysician assistant or nurse practitioner.
bAdministrative support, billing, medical records, coding, or similar.
cLaundry, custodial, housekeeping, maintenance, and kitchen.
Anxiety: Generalized Anxiety Disorder 7‐Item Scale
The GAD‐7 is a clinically validated tool utilized in multiple clinic settings and research. 15 , 16 , 27 , 28 The 7‐item scale measures how often the respondent has been distracted by symptoms of anxiety during the previous 2‐week period. 29 Questions are based on Diagnostic and Statistical Manual of Mental Disorders‐IV (DSM‐IV) criteria. Individuals’ scores range from 0 to 21; 10 or more is noted symptomology associated with GAD. 30
Depression: Patient Health Questionnaire
The PHQ‐9 is a standardized, self‐report questionnaire designed to measure depressive symptoms in alignment with the DSM‐IV diagnostic criteria for depression. 31 The questionnaire consists of 9 main questions and 1 supplementary question. Individuals may indicate a total score between 0 and 27. A composite score of 0‐4 is indicative of minimal depression; 5‐9 is mild; 10‐14, moderate; 15‐19, moderately severe; and severe, 20‐27. 32 Cronbach's alpha demonstrates the internal consistency of the PHQ‐9 measuring alpha+0.86‐0.89 and a test‐retest reliability of r = 0.84 z924. 33 If any respondent indicated having thoughts of harming themselves, the survey proceeded to offer mental health supports. See Figure 1.
FIGURE 1.
Screenshot of survey skip logic for participants indicating thoughts of self‐harm
Stress
The Perceived Stress Scale (PSS) is a validated questionnaire measuring perception of personal stress. The PSS is reverse scored and includes 10 items. 34 The PSS‐10 has been shown to reflect statistically sound internal reliability with Cronbach's alpha coefficients ranging from 0.067 to 0.91. 35 Scores ranging 0‐13 are considered low stress; 14‐26 is moderate stress; and 27‐40 is high perceived stress. Cronbach's alpha for the PSS in this sample was α = 0.811, indicating a high level of internal consistency.
Professional Quality of Life
The Professional Quality of Life is a Likert‐based survey using a scale ranging from 1 (never) to 5 (very often). Three subscales are used to measure compassion satisfaction, secondary traumatic stress (STS), and burnout. 36 Compassion satisfaction is the pleasure an employee gains from helping others that comes from direct interaction or the general positive feeling that the person is adding to the betterment of society. 37 STS is characterized as the negative consequences secondary to work‐related fear and trauma, which may result in exhaustion, frustration, anger, and depression. 37 Burnout is characterized by exhaustion, frustration, anger, and depression, which may result from high workloads and an unsupportive work environment. 38 The instrument has been demonstrated to have good construct validity and reliability. 37
Survey dissemination
The electronic survey was distributed to all hospital personnel in the state of North Dakota between the end of May and the end of June, 2021. The survey was distributed through the State's Hospital Association, Office of Rural Health, Rural Health Association, and statewide network mailing lists for hospital CEOs, directors of nursing, and CAH staff. Announcements ran in 3 electronic newsletters: the State's Hospital Association, Medical Association, and Office of Rural Health. The survey link was also shared through Facebook and Twitter, utilizing a snowball sample in which the cover letter encouraged sharing the link with colleagues. Reminders to complete the survey were sent on 2 occasions. There was no financial incentive for completing the survey.
North Dakota: rural and urban designations
North Dakota (population 779,094) has a large proportion of the population that lives in rural communities (49%). However, the state includes 4 large urban areas (cities), spread‐out geographically which house 38% of the state's population. These 4 cities are considered urban by all federal definitions of rural (available through the Rural Health Information Hub). The respective city populations of these 4 areas are 72,777, 48,261, 56,500, and 121,889. Each of the urban communities have large and reliable health care systems with satellite health clinics in smaller communities. The state has 36 CAHs, 54 rural health clinics, 15 federally qualified health centers, and 3 short‐term PPS hospitals. 39 , 40 , 41
Data analysis
A continuous, composite variable was created for each independent scale: the GAD‐7, PHQ‐9, and PSS. The Professional Quality of Life scale is a tool with 3 subscales measuring compassion, burnout, and STS. A continuous, composite variable was created for each of the 3 subscales. To determine variability among, between, and within various groups, we ran several chi‐square and independent sample T‐test analysis. We used chi‐squared tests to determine if there were statistically significant differences between groups of categorical variables. Independent sample T‐tests were used to determine if the group means of the continuous variables were significantly different.
RESULTS
A total of 839 participants completed the survey, 68 observations were removed because of survey nonresponse. Of the 771 who completed the survey, a majority (83.40%) identified as women. The largest proportion of the sample were persons 25‐40 years of age (44.23%) and 41‐56 years (30.87%). The largest majority reported serving as nursing staff (33.98%). Over half (54.60%) had provided direct care to a COVID‐19 patient; 44.6% worked in a rural hospital. See Table 1.
Reported depression, anxiety, stress, and quality of life among hospital staff
Broadly, 17.90% of respondents reported noted symptomology associated with generalized anxiety disorder; 57.50% indicated no or minimal depression (score of 0‐4). The mean stress level was 9.49 with a maximum potential score of 20. On average, there was low compassion satisfaction (38.4), low burnout (22.7), and low levels of STS (19.3); a score of 50 is considered average and 57 or greater is high. See Table 1.
Rural and urban hospital staff
There was no statistically significant variability between rural and urban experiences of depression, anxiety, or stress (PSS) scores when tested as continuous variables. However, compassion satisfaction was significantly higher for those who worked in rural areas (M = 38.94, SD = 6.75) when compared to those who worked in urban (M = 37.94, SD = 7.10); t(769) = –1.99, P = .0467). The burnout rating was significantly higher for those who worked in urban areas (M = 23.12, SD = 6.51) than rural (M = 22.08, SD = 6.35); t(769) = 2.23, P = .0261). Meaning, those who worked in urban hospital settings experienced greater risk of burnout than rural and less compassion satisfaction with their work.
When exploring data categorically, the proportion of rural hospital staff was no greater nor less than the proportion of urban to indicate a score associated with GAD, or moderate to severe depression. See Table 1.
Hospital staff exposure to COVID‐19 patients
When comparing mental health scales as continuous variables among hospital staff who had, and had not, interacted with COVID‐19 patients, anxiety, depression, burnout, STS, and stress (PSS) were all significantly higher for those who worked directly with COVID‐19 patients, regardless of rural or urban hospital location. See Table 2. When examining data categorically, a significantly greater proportion of those who had interacted with COVID‐19 patients, than those who had not, reported GAD. See Table 1 and Figure 2. Additional variability has been identified by age and years of experience working in a hospital setting and will be explored further in future publications.
TABLE 2.
Categorical variability of signs of mental illness by COVID‐19 exposure
| Interacted with a COVID‐19 patient | Did not interact with a COVID‐19 patient | |||||
|---|---|---|---|---|---|---|
| M | SD | M | SD | t‐test | Cohen's d | |
| Anxiety | 5.39 | 5.18 | 4.26 | 4.84 | 3.11** | 0.23 |
| Depression | 5.39 | 5.38 | 4.63 | 5.36 | 1.97* | 0.14 |
| Burnout | 23.71 | 6.58 | 21.40 | 6.08 | 5.01** | 0.36 |
| STS | 20.56 | 6.61 | 17.83 | 5.53 | 6.25** | 0.45 |
| Stress (PSS) | 9.81 | 3.92 | 9.10 | 3.75 | 2.53* | 0.18 |
*P < .05.
**P < .001.
FIGURE 2.
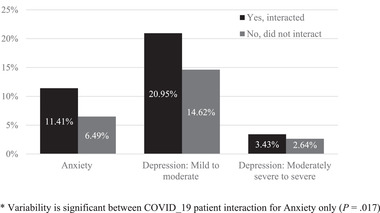
Percentage of hospital staff reporting anxiety disorder, mild to severe depression by COVID‐19 patient interaction*
DISCUSSION
Without baseline data, it is not possible to compare hospital staff mental wellness during the pandemic to their mental wellness prior. However, these data do indicate a need to support hospital staff, especially those who have provided direct care or interaction to patients with COVID‐19. The data also indicate greater professional quality of life among rural providers than urban, presented as lower risk of burnout and greater compassion satisfaction.
Levels of anxiety among hospital staff
According to the National Center for Health Statistics, during 2019, roughly 9.5% of the US population reported mild symptoms of anxiety; 3.4% and 2.7% of US adults reported moderate or severe anxiety (respectively). The 2019 data report much lower rates of anxiety than the 17.90% of hospital staff in North Dakota who noted symptomology associated with GAD in 2021. 42 It is likely that hospital staff have indicated an increasing rate of experienced anxiety in response to the pandemic more broadly (as anxiety increases regardless of profession), and in addition to responding to the pandemic as a frontline worker.
Regardless of profession, the US Census has been tracking feelings of anxiety and depression over the period of the pandemic and is reporting substantial increases of self‐reported anxiety and depression among US adults with rates as high as 30%‐42% during specific periods of time. 43 The US Census pulse surveys are bi‐weekly assessments among US residents and are self‐report. They do not employ the GAD‐7.
However, while the rates of anxiety among US adults have been increasing regardless of profession, based on previous literature, it appears that hospital staff, during the pandemic, are now experiencing levels of anxiety that were previously attributed to only those hospital staff working in emergency settings. For example, Alharthy and team identified that 20.7% of emergency health care workers reported mild anxiety and an additional 23.7% reflected moderate anxiety. 44
Rural and urban hospital staff
Those who worked in urban hospital settings experienced significantly greater risk of burnout than rural, and reported less compassion satisfaction with their work. A recent study of health care workforce in China found results like that of this study. Health care workers from urban areas showed more anxiety and fear compared to those from rural areas. 45 However, there was no significant variability among reports of depression or anxiety in our study. It may be that, regardless of working in a rural or urban location, hospital staff working during a pandemic were experiencing equitable (and high) levels of depression and anxiety, particularly among those interacting with COVID‐19 patients. However, the significant variability around burnout and compassion stratification may indicate that rural providers experienced protective factors that providers in urban areas did not. These protective factors have yet to be identified.
In contrast, a 2021 study examining burnout from a rural verses urban perspective among family physicians found no variation (45.1% vs 43.0%) in burnout rates between the 2 subgroups, though rates of burnout were high overall. 46 It is likely that comparing experience among hospital staff during a pandemic is far different than comparing the experiences of family physicians geographically. This is because of the increased variability between rural and urban hospitals around access to resources, the patient base, the emergent nature of care occurring in hospital settings during the global health pandemic, and other variabilities that exist between rural and urban hospitals for specialty and emergent services.
Hospital staff exposure to COVID‐19 patients
When comparing mental health scales as continuous variables, hospital staff who had interacted with COVID‐19 patients reported significantly greater levels of anxiety, depression, burnout, STS, and stress (PSS), regardless of rural or urban hospital location. Similarly, when examining data categorically, a significantly greater proportion of those who had interacted with COVID‐19 patients, than those who had not, reported GAD. Research out of China found similar results; employees working with COVID‐19 patients had scores reflective of heightened anxiety and anger. 45
Frontline health care workers serving patients with COVID‐19 is an independent risk factor to exhibiting symptoms of stress, anxiety, depression, and burnout. 16 As health care workers exhibit stress during the pandemic, it is likely that residual symptomology may be present up to 2 years later. These symptoms include occupational burnout (19%‐30%), depression symptoms (20%‐45%), and increased smoking and alcohol consumption (8%‐21%). 47 It is imperative to create supports early, and long‐term, to support the well‐being of all hospital staff.
Hospital staff experience the risk of exposure to infection, working with less‐than‐optimal staffing levels, societal shunning, unclear and inconsistent guidance on personal protection measures, quarantine standards, and pharmaceutical interventions. The novel nature of the disease made early medical interventions an exercise in “learning as you go” and provided little direction or protocol for hospital staff at all levels (to include billing, sanitation, and other nonclinical employees). The stress associated with caring for those with COVID‐19 may manifest itself in varied fashion, such as insomnia, anxiety, physical exhaustion, stress, and depression. These individuals are also exposed to personal and social pandemic‐stressors similar to the general population. 3 The prolonged exposure to these compounding conditions may result in deterioration of mental health status resulting in anxiety, depression, insomnia, increased anger, and fear among those caring for the most vulnerable. 15
Limitations
This research is an attempt to better understand the mental health and well‐being of all hospital staff in rural and urban areas in North Dakota. However, it is far more a reflection of support staff and nursing care than all hospital staff as the study had a small response from physicians (either MDs or DOs). We also recognize the risk of selection bias and understand that many health care providers who are, in fact, experiencing distress and overwork are likely over surveyed and may not have completed this assessment. Another disadvantage of the data is that there is no comparison to identify levels of duress prior to the pandemic among hospital staff. The survey was also conducted during a lull between when COVID‐19 first challenged the US health care system and the second wave. If this survey was conducted during the height of either wave, the results may have been more pronounced.
CONCLUSIONS
Research is beginning to explore, with sound methodology, the impact of the 2019 global health pandemic on those working in health care settings. This study is one of the first to include other hospital staff who may have direct patient exposure (like sanitation or dietary staff). As anticipated, a significantly greater proportion of hospital staff who had direct exposure with COVID‐19 patients reported depression, anxiety, and higher levels of stress than did those with no exposure. As previously noted, reported levels of depression, anxiety, and stress mirror those of health care workers providing care in similarly stressful circumstances, such as the emergency room or intensive care unit. However, staff in rural areas had higher levels of compassion satisfaction and less experience of burnout. This may indicate that there are protective or resiliency factors present in rural health care systems, hospitals, or communities that could be explored further and lifted as an exemplar to support mental wellness for all hospital staff. This finding is also important given that rural areas typically have less access to mental health services, and rural hospitals generally have fewer system supports for local wellness programs.
Recommendations
Programs like the Mountain Plains Mental Health Technology Transfer Center 48 and the Substance Abuse and Mental Health Services Administration 49 (among others) have begun to develop resources, training, and supports for health care providers experiencing stress, anxiety, depression, or substance misuse in response to the pandemic. However, health care workers are still overwhelmed with caring for patients beyond capacity of the health care system with little, or no, time to utilize these supports. Support and promotion for physical and mental wellness must come from changes within the hospital system and among health care leaders and policy makers. If we do not care for our hospital staff, there will not be hospital staff left to care for community.
The COVID‐19 pandemic is the health care crisis of this decade. It has taxed health care systems and, therefore, the health care workforce. Employees have been forced to face the prospect of having a shortage of ventilators, the inability to transfer patients to an appropriate level of care, lack of pharmacologic interventions, and an inadequate staffing level. It is imperative that leadership provides the interventions that will mitigate the noted increase in psychological stress inherent in caring for our citizens. Leaders need to hear, protect, prepare support, and care for their workforce. 50 Job satisfaction resulting from these positive leadership actions can enhance employee wellness and retention. Enhanced wellness in turn is a powerful coping mechanism during times of heightened stress. These data also indicate a need to implement programs and supports throughout health care and preparatory programs so that our frontline workers begin from a baseline of mental health and wellness prior to potentially experiencing traumatic events (to include natural disasters, accidents, and pandemics).
FUNDING
Two of the 3 authors received financial support in the form of salary from the Mountain Plains Mental Health Technology Transfer Center, funded by the Substance Abuse and Mental Health Services Administration.
DISCLOSURE
The 3 authors have no personal or financial disclosures to report.
ACKNOWLEDGMENTS
The research team would like to acknowledge and thank the hospital administrators who shared the survey, the state organizations and associations who promoted the assessment, those who completed the survey, and the frontline workers in North Dakota and globally who continue to respond to the global health pandemic. Thank you so very much.
Kelly D, Schroeder S, Leighton K. Anxiety, depression, stress, burnout, and professional quality of life among the hospital workforce during a global health pandemic. The Journal of Rural Health. 2022;38:795–804. 10.1111/jrh.12659
REFERENCES
- 1. Sohrabi C, Alsafi Z, O'Neill N, et al. World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID‐19). Int J Surg. 2020;76:71‐76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Buselli R, Corsi M, & Baldanzi, S , et al. Physical and psychological care of healthcare workers during COVID‐19 outbreak: a difficult challenge. Clin Immunol Immunother. 2021;7(1):1‐3. [Google Scholar]
- 3. Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912‐920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Fred HL, Scheid MS. Physician burnout: causes, consequences, and (?) cures. Texas Heart Inst J. 2018;45(4):198‐202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Weaver MD, Vetter C, Rajaratnam SMW, et al. Sleep disorders, depression and anxiety are associated with adverse safety outcomes in healthcare workers: a prospective cohort study. J Sleep Res. 2018;27(6).e12722. 10.1111/jsr.12722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Carpenter G. Physician Workload Survey 2018. 2018. https://d6e8fe77545c73db8fab‐08e2e97d24a69d8f65ea300e3216435e.ssl.cf1.rackcdn.com/2018/08/LS93719_PhysicianWorkloadSurveyReport_rw_v8_f.pdf. [Accessed 15 October 2021].
- 7. Cohen MJ. Doctors Die by Suicide at Twice the Rate of Everyone Else. Here's What We Can Do. The Washington Post. 2020. https://www.washingtonpost.com/lifestyle/2020/10/06/doctor‐suicide‐coronavirus‐covid/. October 6. [Accessed 16 October 2021].
- 8. Agency for Healthcare Research and Quality . Physician Burnout. 2017. https://www.ahrq.gov/prevention/clinician/ahrqworks/burnout/index.html. [Accessed 16 October 2021].
- 9. Drummond D. Physician burnout: its origin, symptoms, and five main causes. Am Acad Fam Physicians. 2015.22(5), 42–47. [PubMed] [Google Scholar]
- 10. Medicine Revived Academy . Medicine Revived Homepage. 2021. https://medicinerevived.org/. [Accessed 16 October 2021].
- 11. Maqbali MA. Factors that influence nurses’ job satisfaction: a literature review. Nurs Manag. 2015;22(2):30‐37. [DOI] [PubMed] [Google Scholar]
- 12. Adriaenssens J, De Gucht V, Van Der Doef M, Maes S. Exploring the burden of emergency care: predictors of stress‐health outcomes in emergency nurses. J Adv Nurs. 2011;67(6):1317‐1328. [DOI] [PubMed] [Google Scholar]
- 13. Adriaenssens J, De Gucht V, Maes S. Determinants and prevalence of burnout in emergency nurses: a systematic review of 25 years of research. Int J Nurs Stud. 2015;52(2):649‐661. [DOI] [PubMed] [Google Scholar]
- 14. Barzilay R, Moore TM, Greenberg DM, et al. Covid‐19‐related stress, anxiety and depression during the pandemic in a large population enriched for healthcare providers. Transl Psychiatry. 2020;10(1).e291. 10.1038/s41398-020-00982-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Korkmaz S, Kazgan A, Çekiç S, Tartar AS, Balcı HN, Atmaca M. The anxiety levels, quality of sleep and life and problem‐solving skills in healthcare workers employed in COVID‐19 services. J Clin Neurosci. 2020;80:131‐136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among healthcare workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3(3).e203976. 10.1001/jamanetworkopen.2020.3976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mira JJ, Carrillo I, Guilabert M, et al.; SARS‐CoV‐2 Second Victim Study Group . Acute stress of the healthcare workforce during the COVID‐19 pandemic evolution: a cross‐sectional study in Spain. BMJ Open. 2020;10:e042555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Yáñez JA, Afshar Jahanshahi A, Alvarez‐Risco A, Li J, Zhang SX. Anxiety, distress, and turnover intention of healthcare workers in Peru by their distance to the epicenter during the COVID‐19 crisis. Am J Trop Med Hyg. 2020;103(4):1614‐1620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gupta AK, Mehra A, Niraula A, et al. Prevalence of anxiety and depression among the healthcare workers in Nepal during the covid‐19 pandemic. Asian J Psychiatry. 2020;54:102260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Snoderly JA. Staffing is ‘Number One Challenge’ Facing Hospitals as Facilities Reach Capacity. WVNews. https://www.wvnews.com/news/wvnews/staffing‐is‐number‐one‐challenge‐facing‐hospitals‐as‐facilities‐reach‐capacity/article_7e1886ec‐1877‐11ec‐9afa‐0393078968a7.html. September 19, 2021. [Accessed 16 October 2021].
- 21. Tama H. Inside Savannah Hospital. Staff Manages Deluge of COVID Patients. Atlanta Journal‐Constitution. 2021. https://www.ajc.com/news/coronavirus/inside‐savannah‐hospital‐staff‐manages‐deluge‐of‐covid‐patients/BL3CDDKVEBDDLJXLXZGMIHYDC4/. [Accessed 16 October 2021].
- 22. Galvin G. As COVID‐19 Takes Toll on Mental Health, Providers Push to Increase Workforce and Access Beyond the Pandemic. Morning Consult. 2021. https://morningconsult.com/2021/03/19/covid‐19‐mental‐health‐workforce‐shortage‐access‐providers/. [Accessed 16 October 2021].
- 23. Weber L. It's Just Exhausting’: Rural Louisiana Hospital Workers Tell of Covid Burnout. The Guardian. 2021. https://www.theguardian.com/us‐news/2021/feb/17/louisiana‐covid‐coronavirus‐workers‐healthcare. [Accessed 16 October 2021].
- 24. Wu KJ. 'Nobody Sees Us’: Testing‐Lab Workers Strain under Demand: Laboratory Technologists have been Working Nonstop to Help the Nation Diagnose an Ever‐Growing Number of Coronavirus Cases. The New York Times. 2020. https://www.nytimes.com/2020/12/03/health/coronavirus‐testing‐labs‐workers.html. [Accessed 16 October 2021].
- 25. Campos JA, Martins BG, Campos LA, de Fátima Valadão‐Dias F, Marôco J. Symptoms related to mental disorder in healthcare workers during the COVID‐19 pandemic in Brazil. Int Arch Occup Environ Health. 2021;94(5):1023‐1032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Shoja E, Aghamohammadi V, Bazyar H, et al. Covid‐19 effects on the workload of Iranian healthcare workers. BMC Public Health. 2020;20(1).e1636. 10.1186/s12889-020-09743-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Wilson W, Raj JP, Rao S, et al. Prevalence and predictors of stress, anxiety, and depression among healthcare workers managing COVID‐19 pandemic in India: a nationwide observational study. Indian J Psychol Med. 2020;42(4):353‐358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Simoen L, Van den Berghe L, Jacquet W, et al. Depression and anxiety levels in patients with temporomandibular disorders: comparison with the general population. Clin Oral Investig. 2020;24:3939‐3945. [DOI] [PubMed] [Google Scholar]
- 29. Sapra A, Bhandari P, Sharma S, Chanpura T, Lopp L. Using generalized anxiety disorder‐2 (GAD‐2) and GAD‐7 in a primary care setting. Cureus. 2020;12(5).e8224. 10.7759/cureus.8224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Monterrosa‐Castro A, Redondo‐Mendoza V, Mercado‐Lara M. Psychosocial factors associated with symptoms of generalized anxiety disorder in general practitioners during the COVID‐19 pandemic. J Invest Med. 2020;68:1228‐1234. [DOI] [PubMed] [Google Scholar]
- 31. Fanaj N, Mustafa S. Depression measured by PHQ‐9 in Kosovo during the COVID‐19 outbreak: an online survey. Psychiatr Danub. 2021;33(1):95‐100. [DOI] [PubMed] [Google Scholar]
- 32. Tomaszewski K, Zarychta M, Bieńkowska A, Chmurowicz E, Nowak W, Skalska A. Validation of the Patient Health Questionnaire‐9 Polish version in the hospitalised elderly population. Psychiatr Pol. 2011;45:223‐233. [PubMed] [Google Scholar]
- 33. Kocalevent RD, Hinz A, Brähler E. Standardization of the depression screener patient health questionnaire (PHQ‐9) in the general population. Gen Hosp Psychiatry. 2013;35:551‐555. [DOI] [PubMed] [Google Scholar]
- 34. Zhao X, Lan M, Li H, Yang J. Perceived stress and sleep quality among the non‐diseased general public in China during the 2019 coronavirus disease: a moderated mediation model. Sleep Med. 2021;77:339‐345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Liu X, Zhao Y, Li J, Dai J, Wang X, Wang S. Factor structure of the 10‐item Perceived Stress Scale and measurement invariance across genders among Chinese adolescents. Front Psychol. 2020;11(537).e537. 10.3389/fpsyg.2020.00537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Remegio W, Rivera RR, Griffin MQ, Fitzpatrick JJ. The professional quality of life and work engagement of nurse leaders. Nurse Lead. 2021;19(1):95‐100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Stamm BH. The Concise ProQOL Manual. 2nd ed. Pocatello, ID: ProQOL.org; 2010. [Google Scholar]
- 38. Keesler JM, Fukui S. Factor structure of the professional quality of life scale among direct support professionals: factorial validity and scale reliability. J Intellect Disabil Res. 2020;64(9):681‐689. [DOI] [PubMed] [Google Scholar]
- 39. US Census Bureau . Population Data, QuickFacts, North Dakota. 2021. https://www.census.gov/quickfacts/. [Accessed 20 December 2021].
- 40. Rural Health Information Hub . State Guides: North Dakota. 2020. https://www.ruralhealthinfo.org/states/north‐dakota. [Accessed 20 December 2021].
- 41. US Department of Agriculture, Economic Research Services . Rural Economy & Population: Rural Classifications. 2021. https://www.ers.usda.gov/topics/rural‐economy‐population/rural‐classifications/. [Accessed 20 December 2021].
- 42. Centers for Disease Control and Prevention . Products ‐ Data Briefs. 2020. https://www.cdc.gov/nchs/products/databriefs/db378.htm. [Accessed 16 October 2021].
- 43. US Census Bureau . Household Pulse Survey Data Tables. 2021. https://www.census.gov/programs‐surveys/household‐pulse‐survey/data.html. [Accessed 16 October 2021].
- 44. Alharthy N, Alrajeh OA, Almutairi M, Alhajri A. Assessment of anxiety level of emergency health‐care workers by Generalized Anxiety Disorder‐7 tool. Int J Appl Basic Med Res. 2017;7(3):150‐154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Long H, Xu F & Liu H Emotional responses and coping strategies of nurses and nursing college students during COVID‐19 outbreak. medRxiv 2020. 03.05. doi.org/10.1101/2020.03.05.20031898.
- 46. Ward ZD, Morgan ZJ, Peterson LE. Family physician burnout does not differ with rurality. J Rural Health. 2021;37:755‐761. [DOI] [PubMed] [Google Scholar]
- 47. Aghili SM, Arbabi M. The COVID‐19 pandemic and the healthcare providers; what does it mean psychologically? Adv J Emerg Med. 2020;4(2s):e63. [Google Scholar]
- 48. Building Resilience among Physical and Behavioral Healthcare Providers during a Global Health Pandemic. Mental Health Technology Transfer Center (MHTTC) Network. mhttcnetwork.org/centers/mountain‐plains‐mhttc/product/building‐resilience‐among‐physical‐and‐behavioral‐healthcare [Accessed 05 October 2021].
- 49. Substance Abuse and Mental Health Services Administration . SAMHSA — Substance Abuse and Mental Health Services Administration. 2000. https://www.samhsa.gov/. [Accessed 05 October 2021].
- 50. Shanafelt T, Ripp J, Trockel M. Understanding and addressing sources of anxiety among healthcare professionals during the COVID‐19 pandemic. JAMA. 2020;323(21):2133‐2134. [DOI] [PubMed] [Google Scholar]


