Abstract
Introduction
Vaccine hesitancy promotes the spread of infectious diseases including COVID-19 virus, limiting the herd immunity. Complications caused by COVID-19 in people with multiple sclerosis forced governments to ensure them prior access to vaccinations. Their propensity to be vaccinated needs to be assessed to promote adhesion to vaccination programs. The aim of this study was to explore the COVID-19 vaccine hesitancy rate in pwMS.
Methods
We conducted an observational study recruiting patients affected by multiple sclerosis followed at MS Clinical and Research Unit of Tor Vergata University, Rome. We invited them to fill in an online survey about their intent to get COVID-19 vaccination. Fisher’s exact test and Kruskal–Wallis test were performed to explore differences in sociodemographic, clinical, and emotional variables relative to the opinions about vaccinations. An exploratory factor analysis (EFA) was performed to assess the factorial structure of the questionnaire; Pearson’s correlations between the factors and Big Five personality dimensions were also calculated.
Results
Of 276 respondents, 90% was willing to get vaccinated, while only 1.4% was sure to refuse the vaccination. Education level, opinions on safety and efficacy of vaccines, and emotional status were found to be associated to the propensity of getting the COVID-19 vaccination (respectively: p = 0.012, p < 0.001, and p = 0.0001). Moreover, general opinions on healthcare system were related to the intention to get vaccinated.
Conclusion
Our results reinforce the importance of a good relationship between doctor and patient and the need to adapt doctors’ communication strategy to patients’ personalities and beliefs.
Supplementary Information
The online version contains supplementary material available at 10.1007/s10072-022-06559-x.
Keywords: Vaccine hesitancy, Multiple sclerosis, COVID-19, Mistrust, Observational study, Health behavior
Introduction
Coronavirus disease 2019 (COVID-19) is a systemic infection caused by severe acute respiratory syndrome coronavirus 2 (Sars-CoV2). This virus was identified in November 2019 after the detection of atypical pneumonia cases at Wuhan, China. Sars-CoV2 spread globally, and the pandemic was declared by the World Health Organization (WHO) on March 11, 2020. Its outbreak is still ongoing, causing more than 194 million confirmed cases and almost 4.2 million deaths counted worldwide in July 2021 [1]. Considering its morbidity and mortality and the dramatic impact on political, social, and economic assets, COVID-19 has been contemplated one of the most critical health emergencies ever [2].
The race to COVID-19 vaccine development brought to first results on December 11, 2020, when the US Food and Drug Administration (FDA) issued the emergency use authorization (EUA) for the mRNA vaccine from BioNTech/Pfizer (Comirnaty®) [3]. By then, vaccinations were demonstrated to slow the viral transmission and to reduce hospitalization rate [4]. Nevertheless, there is still concern among the population, about safety issues and efficacy of vaccinations against Sars-CoV-2 and its viral variants [5].
Multiple sclerosis (MS) is a chronic inflammatory autoimmune disease of the central nervous system (CNS), characterized by both demyelination and neurodegeneration [6].
Considering their comorbidities, disabilities, and need of immunosuppressive treatment, pwMS at the time of Sars-Cov2 pandemic was considered at higher risk of suffering from COVID-19 complications [7, 8]. Indeed, the Italian government gave them prior access to COVID-19 vaccination as vulnerable patients [9]. At the same time, in light of the autoimmune pathogenesis, there were potential concerns regarding the safety of vaccines with respect to disease reactivation and, therefore, higher possibility of vaccine hesitancy, which is defined as a “delay in acceptance or refusal of vaccination despite availability of vaccination services”. Vaccine hesitancy in 2020 has been identified by the WHO Strategic Advisory Group of Experts (SAGE) as one of the top ten global threats to human health [10].
The aim of this study was to explore the propensity of pwMS to receive COVID-19 vaccine and to examine which are the main causes of their vaccine acceptance/avoidance.
Methods
Study design
We conducted an observational study recruiting patients affected by multiple sclerosis followed at MS Clinical and Research Unit of Tor Vergata University Hospital, Rome. We created an online survey using Google Form platform that was sent via email to 1098 patients on March 4, 2021. Enrollment time ended on June 2, 2021. According to the general European Rules on Data Protection (GDPR), patients had to consent to the use of the information collected. The survey was anonymous. Respondents have been informed on the scope of the study and did not receive any incentives for the compilation.
Survey
We developed an 89-item questionnaire aiming to investigate socioeconomic and demographic variables (such as gender, place of living, country of birth, education level, annual income, number of adult cohabitants, school age of respondents’ children, marital status, work position); MS features (current disease modifying treatment — DMT — mobility status); and personal opinion about vaccines’ safety and efficacy based on the scoring of specific statements, ranging between 1 (disagree) and 10 (agree), as proposed by Freeman et al. [11]. Moreover, we investigated our patient’s beliefs about COVID-19 vaccine and related emotional status exploring whether receiving the COVID-19 vaccine would make them feel “worried,” “angry,” “relieved,” “happy,” or “cared for” and the opinion about health professionals and pharmaceutical companies. Finally, participants also filled in the Big Five Inventory (BFI), in order to assess the individual capacity to cope with stress related to diseases and traumatic events of daily life [12–14].
Statistical analysis
Descriptive statistics on socioeconomic and demographic variables were presented as N (%) and mean (SD) or median (IQR). To compare the five groups of propensity towards vaccination, we used the Kruskal–Wallis test for the continuous variables and the Fisher’s exact test for categorical variables. We also performed an exploratory factor analysis (EFA) to assess the factorial structure of the questionnaire, and Pearson’s correlations were computed between the questionnaire factors and Big Five personality dimensions. Statistical analyses were performed using Stata version 16.0 (Stata Corporation, College Station, TX, USA) and Jamovi 2.5.5.
Results
Socio-demographic characteristics
In total, 276 patients completed the survey. Responders were mainly females (67%), and the median age was 48 years old (range 20–82); 87% of the responders had at least a secondary school education level, 63% were employed, and 69% were married or in a relationship (Online resource 1). Concerning MS treatment, 15% of the patients were untreated and, among those treated, the most used therapies were dimethyl fumarate (17%) and natalizumab (16%) (Online resource 1); around 20% of the patients needed walking aid. Full description of the characteristics of responders is outlined in the supplementary materials (Online resource 1).
Vaccine hesitancy
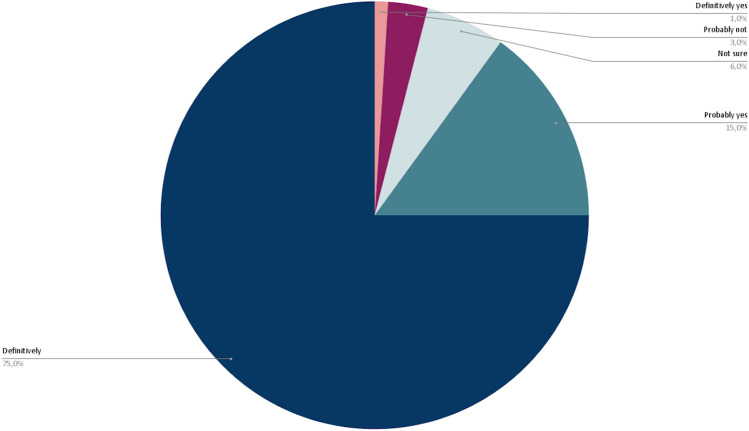
Most of the patients (90%) wanted to get vaccinated while only 4 responders were sure to refuse the vaccination (Fig. 1). Education level was the only variable positively associated with the intention to get the vaccination (Fisher’s exact test: p-value = 0.012). Specifically, among graduated patients, 83% wanted to get vaccinated while the percentage decreased respectively to 74% and 53% for the individuals with a secondary school and lower educational level (results not shown). Intention to get the COVID-19 vaccination was consistent with the general opinion on vaccines and with the emotional status related to getting the vaccine (Table 1). Patients who did not want to get vaccinated described themselves as very worried and angry while those who wanted to get vaccinated as mostly happy, relieved, and excited. Additionally, individuals against the COVID-19 vaccination resulted also less confident in the healthcare system, doctors, and pharmaceutical companies.
Fig. 1.
Opinions about getting COVID-19 vaccination
Table 1.
Opinions, emotions and personality of responders divided by propensity to get vaccinated
| Anti-COVID-19 vaccination | ||||||
|---|---|---|---|---|---|---|
| Surely Yes N = 206(75%) |
Probably Yes N = 42(15%) |
Not sure N = 17(6%) |
Probably Not N = 7(3%) |
Surely No N = 4(1%) |
p-value | |
| Opinions on vaccines | ||||||
| Vaccines are useless because infectious diseases can be treated with drugs (e.g., antibiotics) | 1 (1–2) | 1 (1–5) | 3 (1–6) | 5 (2–5) | 2 (4–6) | 0.0002* |
| The effectiveness of vaccines has now been fully demonstrated | 9 (7–10) | 6 (5–8) | 5 (4–6) | 5 (5–6) | 6.5 (3–8.5) | 0.0001* |
| Vaccines can cause diseases (e.g. autism/diabetes) | 2 (1–4) | 4 (2–5) | 7 (3–9) | 6 (6–8) | 6 (1.5–10) | 0.0001* |
| Vaccines can cause allergic reactions | 7 (5–9) | 7.5 (5–10) | 8 (7–10) | 6 (4–10) | 10 (9–10) | 0.0529 |
| Children would be stronger and healthier if not vaccinated | 1 (1–2) | 2 (1–4) | 1 (1–5) | 2 (1–4) | 7.5 (3–10) | 0.0019* |
| Vaccines are administered too early and reduce the development of children’s immune systems | 1 (1–2) | 3 (1–5) | 3 (1–5) | 4 (1–5) | 3.5 (1.5–7.5) | 0.0001* |
| Emotions related to the COVID–19 vaccine | ||||||
| Worried | 2 (1–4) | 6 (4–7) | 9 (7–10) | 10 (7–10) | 10 (9.5–10) | 0.0001* |
| Excited | 6 (3–8) | 5 (1–7) | 2 (1–7) | 1 (1–4) | 1 (1–1.5) | 0.0005* |
| Relieved | 8 (7–10) | 5 (3–7) | 3 (1–3) | 3 (1–4) | 1 (1–1) | 0.0001* |
| Angry | 1 (1–1) | 1 (1–4) | 5 (1–10) | 10 (1–10) | 10 (6–10) | 0.0001* |
| Happy | 8 (6–9) | 5 (2–6) | 3 (1–5) | 2 (1–4) | 1 (1–1) | 0.0001* |
| Cared for | 8 (6–10) | 5 (3–6) | 3 (1–5) | 4 (1–5) | 1 (1–1) | 0.0001* |
| Personality | ||||||
| I see myself as a reserved person | 4 (3–5) | 4 (3–5) | 4 (4–5) | 4 (3–5) | 4.5 (4–5) | 0.4605 |
| I see myself as a person who trusts others | 4 (3–4) | 3 (3–4) | 3 (1–3) | 3 (1–3) | 3 (3–4) | 0.0013* |
| I see myself as a lazy person | 3 (1–4) | 3 (2–3) | 3 (2–3) | 4 (2–5) | 2 (1.5–3) | 0.7276 |
| I see myself as a relaxed person that well tolerates stress | 3 (2–4) | 3 (2–4) | 3 (2–4) | 3 (1–4) | 4.5 (4–5) | 0.1704 |
| I see myself as a person with few artistic interests | 2 (1–3) | 3 (1–4) | 1 (1–3) | 4 (1–5) | 1 (1–1) | 0.0459* |
| I see myself as a confident and friendly person | 4 (3–5) | 4 (3–5) | 3 (3–3) | 4 (3–5) | 5 (4–5) | 0.1312 |
| I see myself as a person who finds others’ weaknesses | 2 (1–3) | 2 (1–3) | 2 (1–3) | 1 (1–5) | 1 (1–1.5) | 0.2559 |
| I see myself as diligent in the working environment | 5 (5–5) | 5 (4–5) | 5 (4–5) | 5 (4–5) | 5 (5–5) | 0.3440 |
| I see myself as an anxious person | 3 (2–4) | 3 (2–4) | 4 (3–5) | 3 (2–5) | 2 (1.5–3.5) | 0.0646 |
| I see myself as a person with a vivid imagination | 3.5 (3–5) | 3 (3–4) | 4 (4–5) | 2 (1–2) | 3.5 (1.5–5) | 0.0200* |
| Opinions on medicine: | ||||||
| People should do what doctors recommend | 9 (8–10) | 8 (7–9) | 6 (5–9) | 7 (5–8) | 5 (5–6) | < 0.001* |
| Doctors care about my interest | 9 (8–10) | 8 (6–9) | 7 (5–9) | 6 (5–10) | 7.5 (6–8) | < 0.001* |
| Doctors always strive to do their best | 10 (8–10) | 8 (7–9) | 8 (6–10) | 7 (7–10) | 7.5 (6–9) | < 0.001* |
| Doctors often make mistakes | 5 (3–7) | 5 (4–7) | 7 (4–10) | 4 (1–6) | 6.5 (3.5–9) | 0.0364* |
| Doctors know what the best for me is | 9 (8–10) | 8 (6–9) | 7 (4–9) | 7 (5–7) | 6.5 (5.5–7) | < 0.001* |
| Medicine is based on rigorous and scientific criteria | 9 (8–10) | 8 (8–10) | 9 (7–10) | 8 (6–10) | 6 (3–7.5) | 0.0016* |
| Medicine provides therapies for most of the diseases | 9 (8–10) | 8 (7–9) | 6 (6–8) | 7 (5–8) | 8 (6.5–9) | 0.0098* |
| Many drugs are placebo | 3 (2–5) | 5 (2–6) | 5 (3–6) | 5 (3–7) | 7 (3.5–9) | 0.0254* |
| Many drugs are ineffective | 3 (2–6) | 5 (3–6) | 7 (5–9) | 6 (3–6) | 7 (4.5–9) | < 0.001* |
| COVID–19 vaccine developers put safety first | 8 (7–9) | 6 (5–8) | 5 (2–7) | 6 (4–7) | 2 (1.5–2) | < 0.001* |
| I have no confidence in the pharmaceutical companies that developed the vaccine | 2 (1–5) | 5 (4–6) | 9 (6–10) | 8 (6–10) | 10 (9–10) | < 0.001* |
| COVID-19 vaccine developers did not ensure its safety | 2 (1–5) | 5 (3–7) | 6 (3–7) | 8 (6–10) | 10 (9.5–10) | < 0.001* |
| Pharmaceutical companies have only economic interests | 5 (3–7) | 7 (5–8) | 8 (5–10) | 9 (7–10) | 10 (9–10) | < 0.001* |
Results are shown as median (IQR) and p-value from the Kruskal–Wallis test
*Statistically significant differences
Exploratory factorial analysis
EFA showed a significant fit for the factorial structure of the questionnaire (Bartlett’ test Χ291 = 2264.42; p < 0.0001) indicating a two-factor structure of the questionnaire as depicted in Table 2. Of the 14 items, just one (namely “Doctors often make mistakes”) did not load in any of the factors: as a consequence, it was deleted in subsequent correlational analyses. The two main factors could be defined as Trust in doctors and medicine (factor 1) and Concerns about doctor, healthcare, and pharmaceutical companies (factor 2).
Table 2.
Factor loadings of the EFA carried out the questionnaire
| Factor loadings | Factor 1 | Factor 2 | Uniqueness |
|---|---|---|---|
| Doctors have my best interests at heart | 0.9545 | 0.1785 | |
| Doctors know what is best for you | 0.9358 | 0.2189 | |
| I have absolute faith in all hospital doctors | 0.8683 | 0.2382 | |
| People should do what doctors recommend | 0.8367 | 0.2821 | |
| Doctors always strive to do their best | 0.8215 | 0.4079 | |
| COVID-19 vaccine developers put safety first | 0.6596 | 0.4213 | |
| Medicine ensures cures for most diseases | 0.5961 | 0.5977 | |
| Medicine is base od rigorous and scientific principles | 0.5588 | 0.6772 | |
| A lot of drugs are really just placebos | 0.7370 | 0.5684 | |
| Many drugs are ineffective | 0.7240 | 0.5637 | |
| Vaccine developers have not ensured safety | 0.5815 | 0.6241 | |
| Pharmaceutical companies only have economic interests | 0.5804 | 0.6096 | |
| I don’t trust the pharmaceutical companies that developed the vaccine for COVID-19 | 0.5149 | 0.6073 | |
| Doctors often make mistakes | 0.8051 |
Applied rotation method is promax
Correlation between questionnaire factors and personality
A correlation analysis showed that factor 1 was positively correlated with BFI traits of agreeableness (r = 0.31; p < 0.001) and negatively correlated with traits of neuroticism (r = − 0.13; p = 0.48). Moreover, factor 2 negatively correlated with agreeableness (r = − 0.24; p < 0.001). About the emotions investigated, negative correlations were found between personal traits of agreeableness and feelings of anger and worry at the idea of receiving COVID-19 vaccination (r = − 0.179; p = 0.002; r = − 0.160; p = 0.007), while traits of neuroticism were found positively correlated with feelings of emotion and worry at the idea of receiving the vaccine (r = 0.202; p = 0.001; r: 0.129; p = 0.029). About questions related to being affected by MS and COVID-19 vaccination, most of the responders strongly agreed that they considered themselves as vulnerable, and in need to be vaccinated before the general population. Full description of the opinions pwMS and COVID-19 vaccination is outlined in the supplementary materials (Online resource 2). Half of the responders did not know if the use of immunosuppressive drugs could modify the vaccine efficacy, but only 15 patients thought that the vaccine could reactivate MS. For > 50% responders, neurologists of the MS center were very clear and informed concerning the COVID-19 vaccination, while for 5 patients, neurologists were quite imprecise and confusing or absolutely not informed. Interestingly, among those 5 patients, none was sure to get vaccinated, while among those who found the doctors clear and informed, 84% surely wanted to get vaccinated (results not shown). Concerning the final decision on the COVID-19 vaccination, only 13% of responders wanted to make the decision without any consultation with doctors, while 73% made the decision with the help of the doctors and 14% made the doctor decide for them. Interestingly, the 4 patients who surely did not want to get vaccinated made the decision on their own, without any advice from the doctors (results not shown).
Discussion
Pivotal and registration trials showed that COVID-19 vaccines prevent symptomatic disease, morbidities, and mortality Sars-Cov2-related [15]. The vaccine efficacy has been demonstrated against novel B.1.617.2 (Delta) variant [16] and, more recently, against new variants. Nevertheless, anti-vax movements surged. WHO, in fact, warned about the so-called infodemic spreading of false information about COVID-19 online, causing growing misconceptions and concern and delaying the reach of herd immunity [17]. In case of autoimmune disease, such as MS, additional concerns mainly related to the risk of disease worsening triggered by COVID-19 vaccines might reduce the willingness to be vaccinated in these populations. Conversely, MS-related disability and iatrogenic dysfunction of the immune system may worsen COVID-19 disease course in these patients [18] and pose the need of achieving large vaccine coverage.
Previous findings showed that vaccine hesitancy is common (10–20%) among pwMS, especially due to suboptimal vaccine promotion by healthcare professionals managing MS patients [19]. However, with respect to COVID-19 vaccine, 9 out of 10 respondents (90%) were in favor of receiving it. This rate is among the highest ever recorded in the general population [20] and even higher than that found in similar surveys conducted with pwMS worldwide [8, 21].
Indeed, our survey, unexpectedly, also revealed that more than 90% of the respondents were favorable to COVID-19 vaccination, which is higher than the general population [14]. Medical advice provided by MS neurologists, during COVID-19 vaccination campaign, strongly increased our pwMS intention to be vaccinated. In fact, almost 87% of responders declared that they were influenced by doctors in the decision to receive COVID-19 vaccine.
Following to the latest evidence-based guidelines [22], proactively counseling pwMS about the importance of vaccinations has become a common practice even before the COVID-19 pandemic. PwMS was usually counseled to be vaccinated at MS diagnosis or in case of switching to higher efficacy medications [19]. We speculated that the high propensity rate to receive COVID-19 vaccine documented in this study derives from previously acquired awareness among pwMS about the need for prevention of all infectious diseases, in light of the wide use of DMTs. In support of this hypothesis, doctor-patient alliance and the education level were significant predictors of the participants’ vaccination positive intention. Interestingly, none of the clinical characteristics, neither disability nor DMT in use, was associated with the willingness to be vaccinated. This result is in line with several other studies and probably reflects the fear of morbidity and mortality associated with COVID-19, regardless of preexisting clinical conditions [21, 23].
Our results have also shown that that personality traits correlated with the choice to vaccinate or not. In our population beliefs of trust in doctors and healthcare system positively correlated with agreeableness traits and negatively with neuroticism traits. In addition, agreeableness traits were negatively correlated with emotions of anger and worry at the idea of receiving COVID-19 vaccine. Otherwise, traits of neuroticism were positively correlated with feeling worried and excited at the idea of get vaccination. These results reinforce the importance of achieving a positive doctor-patient relationship and also highlight the need to adapt doctors’ communication strategy to patients’ personalities and beliefs, in order to reduce vaccine hesitancy.
We acknowledge that collecting data 6 months after the distribution of vaccinations may have partially influenced the results of this survey. Another limitation of our study is our relative low response rate. Therefore, in the future, surveys on this topic should be extended to a wider population of patients with MS to further explore if there are specific personality and psychological traits influencing vaccination willingness in the context of chronic autoimmune conditions, with respect to the general population [14].
In conclusion, our study highlighted that MS is no more a barrier to vaccination both from doctors’ and patients’ side. This is a very relevant cultural achievement compared to the past, when the fear of MS reactivation affected vaccination rate in this population with detrimental impact on public health. Improving communication strategies especially among those patients with lower education is a main need to promote vaccinations.
Supplementary Information
Below is the link to the electronic supplementary material.
Declarations
Ethical approval
None.
Conflict of interest
None.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Yesudhas D, Srivastava A, Gromiha MM. COVID-19 outbreak: history, mechanism, transmission, structural studies and therapeutics. Infection. 2021;49(2):199–213. doi: 10.1007/s15010-020-01516-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mahase E. China coronavirus: WHO declares international emergency as death toll exceeds 200. BMJ. 2020;368:m408. doi: 10.1136/bmj.m408. [DOI] [PubMed] [Google Scholar]
- 3.Vasireddy D, Atluri P, Malayala SV, et al. Review of COVID-19 vaccines approved in the United States of America for emergency use. J Clin Med Res. 2021;13(4):204–213. doi: 10.14740/jocmr4490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moghadas SM, Vilches TN, Zhang K, et al. The impact of vaccination on COVID-19 outbreaks in the United States. Epidemiology. 2020 doi: 10.1371/journal.pbio.3001211. [DOI] [Google Scholar]
- 5.Troiano G, Nardi A. Vaccine hesitancy in the era of COVID-19. Public Health. 2021;194:245–251. doi: 10.1016/j.puhe.2021.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dobson R, Giovannoni G. Multiple sclerosis – a review. Eur J Neurol. 2019;26:27–40. doi: 10.1111/ene.13819. [DOI] [PubMed] [Google Scholar]
- 7.Zheng C, Kar I, Chen CK, et al. Multiple sclerosis disease-modifying therapy and the COVID-19 pandemic: implications on the risk of infection and future vaccination. CNS Drugs. 2020;34:879–896. doi: 10.1007/s40263-020-00756-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Xiang XM, Hollen C, Yang Q, et al. COVID-19 vaccination willingness among people with multiple sclerosis. Mult Scler J - Exp Transl Clin. 2021;7:205521732110171. doi: 10.1177/20552173211017159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ministero della Salute, Decreto 12 Marzo 2021;
- 10.MacDonald NE. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33:4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 11.Daniel Freeman, Bao S.Loe et al (2021) Covid-19 vaccine hesitancy in the UK: the Oxford coronavirus explanations, attitudes, and narratives survey (Oceans)II. Psychol Med 1-15. 10.1017/S0033291720005188 [DOI] [PMC free article] [PubMed]
- 12.Guido G, Peluso AM, et al. An Italian version of the 10-item Big Five Inventory: an application to hedonic and utilitarian shopping values. Elsevier, Peronality and Individual Differences. 2014;76(2015):135–140. doi: 10.1016/j.paid.2014.11.053. [DOI] [Google Scholar]
- 13.Potemkowski A, Brola W, et al. The Big Five Personality Traits and positive orientation in Polish adults with multiple sclerosis: the role of meaning live. Int J Environ Res Public Health. 2022;19(9):5426. doi: 10.3390/ijerph19095426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jamie Murphy, Fréderique Vallières et al (2021) Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and United Kingdom. 10.1038/s41467-020-20226-9. [DOI] [PMC free article] [PubMed]
- 15.Polack FP, Thomas SJ, Kitchin N, et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N Engl J Med. 2020;383:2603–2615. doi: 10.1056/NEJMoa2034577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lopez Bernal J, Andrews N, Gower C, et al. Effectiveness of covid-19 vaccines against the B.1.617.2 (Delta) Variant. N Engl J Med. 2021;385:585–594. doi: 10.1056/NEJMoa2108891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Burki T. The online anti-vaccine movement in the age of COVID-19. Lancet Digit Health. 2020;2:e504–e505. doi: 10.1016/S2589-7500(20)30227-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sormani MP, De Rossi N, Schiavetti I, et al. Disease-modifying therapies and coronavirus disease 2019 severity in multiple sclerosis. Ann Neurol. 2021;89:780–789. doi: 10.1002/ana.26028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yap SM, Hinai MA, et al. Vaccine hesitancy among people with multiple sclerosis. Mult Scler Related disorders. 2021 doi: 10.1016/j.msard.2021.103236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wake AD. The willingness to receive COVID-19 vaccine and its associated factors: “vaccination refusal could prolong the war of this pandemic” – a systematic review. Risk Manag Healthc Policy. 2021;14:2609–2623. doi: 10.2147/RMHP.S311074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Serrazina F, Sobral Pinho A, Cabral G, et al. Willingness to be vaccinated against COVID-19: an exploratory online survey in a Portuguese cohort of multiple sclerosis patients. Mult Scler Relat Disord. 2021;51:102880. doi: 10.1016/j.msard.2021.102880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Riva A, Barcella V, Benatti SV, et al. Vaccinations in patients with multiple sclerosis: a Delphi consensus statement. Mult Scler J. 2021;27:347–359. doi: 10.1177/1352458520952310. [DOI] [PubMed] [Google Scholar]
- 23.Ehde DM, Roberts MK, Humbert AT, et al. COVID-19 vaccine hesitancy in adults with multiple sclerosis in the United States: a follow up survey during the initial vaccine rollout in 2021. Mult Scler Relat Disord. 2021;54:103163. doi: 10.1016/j.msard.2021.103163. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.