Abstract
While previous studies provide broad categories of the public who intend to get a COVID-19 vaccine, few systematically segment and help understand and engage with distinct publics to improve COVID-19 vaccine uptake. Using data from a national sample of the Australian public (N = 1054) and using measures primarily based on the Theory of Planned Behaviour, a latent class analysis of 16 items was undertaken to identify COVID-19 audience segments for potential future message targeting. We found five different segments of COVID-19 vaccine intentions: vaccine enthusiasts (28%), supporters (26%), socials (20%), hesitant (15%) and sceptics (10%). These five audience segments also differ on demographic variables and their level of trust in mainstream media, scientists and health experts, social media and family and friends. Understanding the COVID-19 vaccine attitudinal and information-seeking characteristics of these sub-publics will help inform appropriate messaging campaigns.
Keywords: audience segmentation, COVID-19, SARS-CoV-2, vaccine, hesitancy
1. Introduction
The global COVID-19 pandemic has resulted in relatively low case numbers and low loss of life in Australia; however, recent outbreaks of the highly contagious Delta and Omicron variants have continued to evade control attempts. In April 2020, 86% of the public indicated they would get the vaccine if it became available (Dodd et al., 2021a). This rose to 87% in June 2020 and to 90% in July 2020 (Dodd et al., 2021b). However, miscommunication surrounding concerns over links between the AstraZeneca vaccine and thrombosis (blood clotting) confused the general public across many countries, including Australia (Wise, 2021).
The aim of this study is to understand some of the key characteristics and perceptions that distinguish the Australian public’s differing vaccination intentions by applying latent class analysis (LCA) to determine audience segments. In particular, measures derived from the Theory of Planned Behaviour (TPB) are used to understand different audience segments related to COVID-19 vaccine intentions. The following sections provide a background of vaccine uptake in Australia, critically review current research on COVID-19 vaccine intentions using an audience segment approach and provide a theoretical overview of TPB.
Predictors of COVID-19 vaccine intentions in Australia: Messages and messengers
Studies looking at the predictors of Australian’s COVID-19 vaccination hesitancy have typically focused on demographic predictors of hesitancy, although some attitudinal measures have also been considered. Some have found hesitancy more common among females (Edwards et al., 2021; Rhodes et al., 2020; Roy Morgan, 2021), younger people (Faasse and Newby, 2020; Melbourne Institute, n.d.; Roy Morgan, 2021) and those with lower socio-economic status (Edwards et al., 2021; Rhodes et al., 2020), lower health literacy and lower education (Dodd et al., 2021a). Belief that the risks posed by COVID-19 have been overstated and higher religiosity have also been associated with increased hesitancy in the Australian public (Edwards et al., 2021).
Tailored messages based on individual needs and circumstances are more effective to promote public interest and engagement than providing general information that is determined important by experts (Skinner et al., 1994). Providing only corrective information is not enough – such as the risks posed by COVID-19 vaccine – as public knowledge about and willingness to get vaccinated are also dependent on personal and cultural worldviews (Lazić and Žeželj, 2021). For example, the Australian Bureau of Statistics (2021a) examined reasons why individuals would accept or decline a COVID-19 vaccine and found key motivators for getting vaccinated were to reduce the risk of contracting the virus or reducing its severity (79%), it was recommended by a health professional (31%), they were notified of their eligibility for the vaccine (28%) and because they wanted to travel (24%). In contrast, the most common reasons for COVID-19 vaccine hesitancy related to concern over potential side effects (52%) and concern over the efficacy of the vaccine (15%).
Just as important as the message is the messenger. Mistrust of government and experts is cited more commonly in literature on vaccine attitudes and behaviours than issues related to information deficit (Yaqub et al., 2014). For example, Hopfer (2012) found that information provided by experts did not significantly increase human papillomavirus (HPV) vaccine uptake among college women, in part because the target public may be less receptive to messages from authority figures. Instead, Hopfer (2012) reported that a communication intervention featuring both a peer and an expert nearly doubled HPV vaccination rates compared with those who received standard university information about HPV vaccine or other control groups. This is another reason why segmentation approaches help identify the trusted sources that will work with specific audiences.
Trusted information sources play a key role in how individuals learn about and make behavioural choices, including the choice of getting a vaccine against COVID-19 (Agley and Xiao, 2021; de Figueiredo et al., 2020; Larson et al., 2018). But a key limitation with previous studies on vaccination intentions is that they focus on trust either in government or in health organisations such as the Centers for Disease Control and Prevention (CDC) (Krishna, 2018), ignoring other messengers such as family and friends who have been found to be equally persuasively in shaping vaccine intentions and behaviours (de Figueiredo et al., 2020). This study comprehensively examines how public trust in different informational sources is associated with COVID-19 vaccine intentions and seeks to identify the most trusted source for different audience segments and the implications of these for interventions aiming to improve COVID-19 vaccine uptake.
Need and state of research: COVID-19-related segmentation analyses
Despite studies examining demographic and attitudinal characteristics associated with vaccination intentions, none of these Australian studies have adopted segmentation approaches to determine like-minded audiences for interventions to increase vaccine uptake. Segmentation is a systematic approach to explicitly identify different audiences within a population and is a critical tool for optimal communication intervention design (Slater, 1996). It is important that variables used to identify audience segments should be the key constructs that such interventions would or could target (Slater, 1996).
To our knowledge, the only COVID-19-related segmentation study that has been conducted including Australian participants (Kleitman et al., 2021) was as part of a multi-national, collectively analysed sample focused on broader COVID-19 health behaviours rather than COVID-19 vaccination intentions. Even as several scholars highlight the effectiveness of audience segmentation in developing tailored health and science communication campaigns – including to promote COVID-19 vaccination even before a vaccine was available (French et al., 2020) – there is limited research specifically on different audience segments based on COVID-19 vaccination intentions. Instead, some researchers have conducted audience segmentation analyses based on COVID-19 misinformation beliefs and protective behaviours (Agley and Xiao, 2021; Smith et al., 2021). For example, Agley and Xiao (2021) found four segments among the US public based on endorsement of COVID-19 misinformation. Smith et al. (2021) found five segments relating to adherence to COVID-19 safety behaviours, such as frequent hand washing and wearing a face mask. These five segments ranged from ‘Adherents’ (34%) to ‘Refusers’ (9%), but their research does not evaluate or have any recommendation on COVID-19 vaccine intention. Other studies illustrate audience segments based on COVID-19 impact on mental and physical health in South Korea (Ihm and Lee, 2021), and support for government to donate COVID-19 vaccines to developing countries in a US sample (Guidry et al., 2021).
Chen et al. (2021) applied Protection Motivation Theory to identify segments using measures of both COVID-19 safety behaviours and vaccine intentions. Based on a sample of 1047 participants recruited through a Facebook advertisement in Taiwan, they identified three segments: high motivation for vaccination and preventive behaviours, low motivation for vaccination and preventive behaviours and high motivation for vaccination but low motivation for preventive behaviours. They suggested increasing disease threat to increase safety behaviour compliance and coping appraisal towards vaccination. However, they reported a number of limitations, including measuring vaccine intention using a single-item and convenience sample, and the authors acknowledge the lack of other important constructs from vaccine research, such as social norms.
Based on a sample of about 100 Philadelphia residents, Bass et al. (2022) reported three segments combining measures about COVID-19 impact on health and personal wealth, and trust in healthcare providers. They used a single-item measure of vaccine intentions to validate the three segments of ‘high trust-low COVID-19 impact’, ‘moderate trust-high COVID-19 impact’ and ‘low trust-low impact’. They acknowledge that trust in healthcare was measured only using two items and vaccine intention with one item, which was very low in the sample, averaging just 1.18 on a 0 (definitely not getting a vaccine) to 10 (definitely getting a vaccine) scale.
Schneider et al. (2021) conducted an LCA of US respondents based on 11 measures that included a mix of attitudes, beliefs and concerns about a potential COVID-19 vaccine, referencing social networks as influential in improving vaccine uptake. They found four evenly distributed profiles in the sample: pro-vaccine, development concerns, unsure and anti-vaccine. They suggest providing more information about vaccine development and safety to persuade the segment with development concerns. To those who are unsure or are anti-vaccine, the scholars suggest using credible information messengers, but they do not mention who the trusted messengers are and what key messages would persuade the public to improve vaccine uptake.
Scholars have called for better integration of theory in audience segmentation studies (e.g. Hine et al., 2014; Noar, 2012; Slater, 1996; Smith, 2017). However, most studies cited above do not specify a theoretical framework that results in variance in measures used to segment the audience. Lack of theory application also hinders our ability to identify and tailor information to individuals in different sub-groups. Rigorously applying theories across the life of an intervention is likely to be more effective in achieving its goals and objectives. Slater (1996) argued that theoretical approaches combined with audience segmentation taxonomies will increase campaign effectiveness. In this article, we present audience segmentation analysis based on measures primarily derived from the TPB. It is important to acknowledge that audience segmentation using other theoretical frameworks is equally important and valid (Hine et al., 2014) and we have identified additional potential segmentation variables in the ‘Limitations’ section.
Theory of planned behaviour to identify vaccine segments
TPB is one of the most popular conceptual frameworks for the study of human action (Armitage and Conner, 2001), including research on vaccination (see Gerend and Shepherd, 2012; Xiao and Wong, 2020), and it provides useful target variables for interventions. TPB is a general theory of self-directed behaviour that considers an individual’s intention to adopt a particular behaviour is predicted by the following three key factors: their attitudes towards the behaviour, their perception of what respected other people expect them to do (subjective norms) and their perceived control over the behaviour (Ajzen, 1985).
Attitudes refer to favourable or unfavourable predispositions towards a target behaviour. For example, attitudes towards vaccines comprise both affective (e.g. getting vaccine is desirable) and cognitive (e.g. getting vaccine is effective) dimensions (e.g. Xiao, 2019). A number of studies show that favourable attitudes are associated with vaccination intentions (Krishna, 2018; Xiao, 2019).
The concept of social norms has evolved over the years and now includes the following three components: subjective, descriptive and injunctive norms (e.g. Rimal and Lapinski, 2015). Subjective norms are a person’s belief that people important to them think they should perform a behaviour. Descriptive norms are perceptions about the prevalence of behaviour within their group or community, such as the perception about the number of people in community or group who are willing to take a COVID-19 vaccine. Injunctive norms activate individuals’ motivation for group-affiliation, where behaviours are shaped by perceptions of social rewards and retribution. A limited number of previous studies related to vaccine uptake during the 2009 H1N1 influenza pandemic (e.g. Bish et al., 2011) as well as more recent studies on COVID-19 vaccine uptake (e.g. Latkin et al., 2021; Thaker and Ganchoudhuri, 2021) show that social norms play a critical role in public response to the pandemic. Few studies, however, measure the three social norms simultaneously as does the current study (e.g. Rimal and Lapinski, 2015).
Ajzen (2002) suggested that ‘perceived behavioral control is the overarching, superordinate construct that is comprised of two lower-level components: self-efficacy and controllability’ (p. 680). In a meta-analysis of perceived behavioural control (PBC) and vaccine hesitancy, Xiao and Wong (2020) noted that PBC is ‘a combination of perceived control (e.g. the level of control one has over getting vaccinated) and self-efficacy (e.g. one’s confidence in their ability to get vaccinated)’ (p. 5132). While they found that PBC measurement only with self-efficacy measure was equally predictive of intentions as a model with both measures of self-efficacy and perceived control, they suggested that future research should not undervalue the importance of using both items to measure PBC as the current study does.
TPB has long been applied across a range of domains, including health behaviour, education, and pro-environmental behaviour (Armitage and Conner, 2001), and provides a valuable foundation for segmenting audiences regarding vaccination intentions. A number of previous studies have applied TPB in explaining individuals’ vaccine uptake for influenza (e.g. Schmid et al., 2017), HPV (e.g. Gerend and Shepherd, 2012; Juraskova et al., 2012) and COVID-19 (Fan et al., 2021). A recent report by Thaker (2021) analysed audience segments of COVID-19 vaccine intentions in Aotearoa-New Zealand based on five measures of vaccine intentions, including willingness to put their name on a list to get a vaccine and willingness to pay. They found four segments ranging from a large segment of the public who were supportive to getting a vaccine (36% of the sample) to a small segment of vaccine sceptics (12%). To our knowledge, none of these previous studies have utilised TPB in identifying priority audience segments that most health authorities find difficult to reach, to improve public uptake of critical vaccines.
Thus, this study addresses knowledge gaps regarding Australian COVID-19 vaccine audience segments, through an examination of TPB variables in the Australian context. Furthermore, this study identifies differences between the audience segments on demographics, reasons to accept or decline a vaccine, and trust in informational sources and the implications of these for interventions aiming to improve COVID-19 vaccine uptake. Furthermore, we add to the research by understanding the messages and messengers that different audience segments trust that will help improve public outreach campaigns (Agley and Xiao, 2021; Larson et al., 2018; Latkin et al., 2021).
For example, Thaker and Cook (2022) report that some associations between trust – in mass media, Prime Minister Jacinda Ardern, and health experts – and intentions to get a COVID-19 vaccine can be partly explained through attitudes towards a COVID-19 vaccine in New Zealand. They did not find a similar indirect effect between trust in family and friends and intentions to get a vaccine via attitudes, arguing that trust in family and friends is probably better associated with social norms than attitudes. This research adds to these recent studies examining the role of trust in understanding how people form attitudes, norms, and intentions about getting a new vaccine.
2. Method
A nationally representative sample survey of Australian adults (N = 1054, 18+ years) was conducted between 20 May and 12 July 2021. During this time, Australia was experiencing a resurgence in COVID-19 infections and deaths (Department of Health, 2021), with parts of the country under lockdown (Premier of Victoria, 2021). At the time of the survey, 12% of the population over 50 years received one dose and 2% received two doses of a vaccine. Vaccine for the general population aged 16 years and above was only available from 30 August 2021, after the survey, but it was preceded by a government campaign, ‘Arm yourself against COVID-19’. The web-based survey was fielded by Qualtrics, which maintains an active online panel that is representative of the Australian population (Qualtrics Panel, 2021).
The panellists receive an incentive such as a flat fee or discount gift card based on the length of the survey, their specific profile and target acquisition difficulty. Respondents for this survey were sent a secured, individualised email link. The sample was recruited to match the national estimates on age, gender, education, income and region. The average time to complete the survey was 25 minutes. Ethics approval was filed at the human research review boards at Massey and Monash universities and the study was determined to be exempt from a full review due to its low risk. Participants provided informed consent after reading brief aims of the survey, namely, seeking their opinion about ‘current issues facing the country and the world’.
The sample was composed of slightly more women, younger people and individuals belonging to higher education and income groups in comparison with national population estimates. While the geographic distribution generally matched national estimates, the sample consisted of fewer respondents from New South Waves (27% compared with national estimate of 32%). As mentioned, post-survey weights were used to match the sample on national estimates of gender and age (Australian Bureau of Statistics, 2020), education (Australian Bureau of Statistics, 2017a), income (Australian Bureau of Statistics, 2017b) and geographic distribution (Australian Bureau of Statistics, 2021b).
Measures
Sixteen items, as presented in Table 1, were used to assess audience segments on COVID-19 vaccination intentions using standard TPB measures (Fishbein and Ajzen, 2011) adapted specifically to refer to COVID-19 vaccines. These included attitudes towards COVID-19 vaccinations, social norms, PBC and intentions to get a COVID-19 vaccine. Similar to previous studies (e.g. Xiao, 2019), attitudes towards COVID-19 vaccine were measured using both affective and cognitive dimensions on a 7-point bipolar scale.
Table 1.
Descriptive statistics of COVID-19 vaccine attitudes, social norms and behavioural control across the segments.
| M | SD | Enthusiasts | Supporters | Socials | Hesitant | Sceptics | R 2 | |
|---|---|---|---|---|---|---|---|---|
| COVID-19 vaccine attitudes | ||||||||
| To what extent do you feel that getting a COVID-19 vaccine will be. . .(7-point bipolar scale) | ||||||||
| Bad: Good | 4.96 | 2.12 | 6.94 | 5.75 | 4.18 | 3.46 | 1.22 | .70 |
| Unpleasant: Pleasant | 4.07 | 1.90 | 5.55 | 4.01 | 3.85 | 3.44 | 1.49 | .38 |
| Harmful: Beneficial | 4.85 | 2.12 | 6.95 | 5.32 | 4.22 | 3.45 | 1.18 | .68 |
| Worthless: Valuable | 4.97 | 2.08 | 6.94 | 5.55 | 4.24 | 3.63 | 1.54 | .64 |
| Ineffective: Effective | 4.99 | 2.04 | 6.84 | 5.53 | 4.42 | 3.68 | 1.53 | .62 |
| Unsafe: Safe | 4.59 | 2.06 | 6.64 | 5.01 | 3.94 | 3.28 | 1.09 | .66 |
| Undesirable: Desirable | 4.67 | 2.12 | 6.84 | 4.98 | 4.11 | 3.18 | 1.20 | .66 |
| Social norms | ||||||||
| How much do you agree or disagree with the following statements? (5-point scale, strongly disagree to strongly agree with neither as mid-scale) | ||||||||
| Descriptive norm | 3.82 | 1.27 | 4.81 | 4.41 | 3.53 | 2.52 | 2.00 | .60 |
| Subjective norm | 3.91 | 1.20 | 4.87 | 4.57 | 3.54 | 2.68 | 2.11 | .67 |
| Injunctive norm | 4.06 | 1.15 | 4.89 | 4.59 | 3.60 | 2.90 | 3.05 | .47 |
| Perceived Behavioural Control | ||||||||
| Self-efficacy | 3.68 | 1.46 | 4.92 | 4.57 | 3.21 | 1.99 | 1.34 | .78 |
| Perceived control | 4.27 | 1.04 | 4.66 | 4.46 | 3.76 | 3.81 | 4.39 | .13 |
| Total responses | Enthusiasts | Supporters | Socials | Hesitant | Sceptics | R 2 | ||
|
Behavioural Intention
Would you accept the vaccine for yourself? |
.62 | |||||||
| No, definitely not | 14% | 0.01% | 0.01% | 1.25% | 35.08% | 83.73% | ||
| Unsure, but leaning towards NO | 14% | 0.01% | 0.17% | 15.33% | 64.58% | 14.85% | ||
| Unsure, but leaning towards YES | 17% | 0.02% | 9.40% | 70.67% | 0.04% | 1.32% | ||
| Yes, definitely | 55% | 99.97% | 90.42% | 12.74% | 0.30% | 0.11% | ||
| Would you accept the vaccine if it meant protecting friends, family, or at-risk groups? | .48 | |||||||
| No, definitely not | 8% | 0.01% | 0.01% | 0.48% | 16.66% | 53.40% | ||
| Unsure, but leaning towards NO | 15% | 0.59% | 0.01% | 16.05% | 51.18% | 37.15% | ||
| Unsure, but leaning towards YES | 17% | 0.24% | 4.16% | 52.65% | 26.45% | 7.71% | ||
| Yes, definitely | 60% | 99.17% | 95.83% | 30.82% | 5.71% | 1.74% | ||
| Would you be willing to put your name on the list to be vaccinated first | .47 | |||||||
| No, definitely not | 20% | 0.36% | 1.46% | 9·86% | 59.01% | 89.31% | ||
| Unsure, but leaning towards NO | 14% | 0.30% | 7.42% | 23.54% | 37.94% | 10.26% | ||
| Unsure, but leaning towards YES | 19% | 5.23% | 18.26% | 59.11% | 2.95% | 0.35% | ||
| Yes, definitely | 47% | 94.11% | 72.86% | 7.49% | 0.10% | 0.09% | ||
| I will get vaccinated against the coronavirus | .80 | |||||||
| No | 30% | 1.61% | 0.02% | 22.41% | 98.85% | 99.87% | ||
| Yes | 70% | 98.39% | 99.98% | 77.59% | 1.15% | 0.13% | ||
ANOVA: analysis of variance.
N = 1054. Table presents mean values and percentages of key input variables across the segments. All mean differences and proportional differences – as judged by ANOVA or chi-square tests – are significant at p < .001. R2 represents how much of the variance of each indicator is explained by this five-cluster model. Table presents percentages of key input variables across the segments. All proportional differences – as judged by ANOVA or chi-square tests – are significant at p < .001. R2 represents how much of the variance of each indicator is explained by this five-cluster model.
Social norms were measured similar to previous studies but included all the three kinds of norms as previous research indicates unique influence of each of the social norms (Rimal and Lapinski, 2015): descriptive norm (‘Most of my family members and friends will take a COVID-19 vaccine when available’), subjective norm (‘Most people who are important to me would approve of my getting a COVID-19 vaccine when available’) and injunctive norm (‘Doctors would think that I should get a COVID-19 vaccine when available’) were measured on a 5-point scale, strongly disagree to strongly agree with neither as mid-scale.
PBC measures were also adapted from previous studies measuring self-efficacy and perceived control (Xiao and Wong, 2020). Specifically, Fishbein and Ajzen (2011: 450) suggested structures based on these two measures: ‘I am confident that I can exercise for at least 20 minutes. . .’ and ‘My exercising for at least 20 minutes . . . is up to me’. Previous studies also distinguished between self-efficacy (‘I am confident that I can take my preschool child for vaccination’) and perceived control (‘it is mostly up to me whether or not I have a swine flu vaccination’) (Xiao and Wong, 2020). The two measures were adapted as follows and measured on a 5-point scale, strongly disagree to strongly agree with neither as mid-scale: ‘I am confident that I will get a COVID-19 vaccine as soon as it is available in my area’ and ‘Whether I could get a COVID-19 vaccine is up to me’.
Four measures of intentions were collected from respondents following previous surveys (Lin et al., 2020; Loomba et al., 2021) that have been also used subsequently in other studies (Zheng et al., 2022). Specifically, the respondents were asked, ‘When a coronavirus (COVID-19) vaccine becomes available—Would you accept the vaccine for yourself?’, ‘Would you accept the vaccine if it meant protecting friends, family, or at-risk groups?’ and ‘Would you be willing to put your name on the list to be vaccinated first?’ The responses were measured on a nominal scale from ‘Yes, definitely’ (1), ‘Unsure, but leaning towards Yes’ (2), ‘Unsure, but leaning towards No’ (3) and ‘No, definitely not’ (4). To account for variance in answer categories, respondents also reported their willingness to get a vaccine using a dichotomous measure: ‘I will get vaccinated against the coronavirus’ (No/Yes).
Reasons to get or decline a vaccine
Separately, respondents were provided a list of items to select why they choose to get or decline a vaccine apart from providing a box for additional comments. Respondents could choose as many items as they liked. These items were developed using previous studies (Australian Bureau of Statistics, 2021a; Nomura et al., 2021) and were used to identify key messages that may resonate with the target segment, as mentioned above. The full list of items to accept or decline is presented in Supplemental Table 4.
Trust
Trust was measured following previous operationalization (Agley and Xiao, 2021; Latkin et al., 2021) and included trust in mass media, social media, scientific sources and government officials (Larson et al., 2018): ‘How much do you trust or distrust the following organisations or people as a source of accurate information? If you don’t know or don’t use a particular source, then please select don’t know’. We recoded don’t know responses as the midpoint (3). Trust was measured on a 5-point scale from strongly distrust (1) to strongly trust (5). These measures included trust in mass media (newspapers, online news, radio, TV), social media (Facebook, Twitter, YouTube), family and friends, scientists, medical experts, general practitioner (GP) or local doctor, Prime Minister and government officials.
Analysis
First, the data were weighted to match the sample to gender, age, education, income and geographic distribution of the target population of adult Australians. Table 2 shows the demographic characteristics of the sample in unweighted and weighted dataset, illustrating the minor differences.
Table 2.
Demographic variables across the five audience segments on COVID-19 vaccine intention.
| Cluster size | Unweighted (n, %) | Weighted (%) | Enthusiasts | Supporters | Socials | Hesitant | Sceptics | χ2 | p-value |
|---|---|---|---|---|---|---|---|---|---|
| 28% | 26% | 20% | 15% | 10% | |||||
| Gender | 126.58 | <.001 | |||||||
| Male | 450 (42.7) | 48% | 71% | 52% | 37% | 25% | 31% | ||
| Female | 599 (56.8) | 51% | 28% | 46% | 62% | 75% | 69% | ||
| Other (Please write) | 5 (0.5) | 1% | 1% | 2% | 1% | 0% | 0% | ||
| Age | 300.9 | <.001 | |||||||
| 18–19 years | 121 (11.5) | 5% | 3% | 4% | 9% | 8% | 3% | ||
| 20–29 years | 249 (23.6) | 18% | 5% | 17% | 27% | 30% | 22% | ||
| 30–39 years | 220 (20.9) | 18% | 6% | 18% | 24% | 24% | 30% | ||
| 40–49 years | 162 (15.4) | 16% | 8% | 17% | 20% | 20% | 22% | ||
| 50–59 years | 93 (8.8) | 16% | 21% | 17% | 12% | 13% | 12% | ||
| 60–69 years | 112 (10.6) | 13% | 22% | 16% | 6% | 4% | 7% | ||
| 70 years and above | 97 (9.2) | 14% | 35% | 12% | 3% | 1% | 4% | ||
| Education | 72.67 | <.001 | |||||||
| Did not go to school | 5 (0.5) | 1% | 0% | 2% | 1% | 2% | 0% | ||
| Primary or high school | 337 (32) | 45% | 33% | 38% | 54% | 60% | 55% | ||
| Trade/diploma/certificate | 361 (34.3) | 28% | 29% | 28% | 26% | 26% | 31% | ||
| Bachelor degree or above | 351 (33.3) | 26% | 38% | 32% | 18% | 12% | 14% | ||
| Income | 52.18 | <.001 | |||||||
| Up to $399 per week ($20,799 per year) | 281 (26.7) | 32% | 25% | 37% | 29% | 33% | 40% | ||
| $400–$799 per week ($20,800–$41,599 per year) | 291 (27.6) | 25% | 30% | 19% | 27% | 26% | 22% | ||
| $800–$1249 per week ($41,600–$64,999 per year) | 204 (19.4) | 18% | 13% | 13% | 24% | 21% | 27% | ||
| $1250–$1749 per week ($65,000–$90,999 per year) | 138 (13.1) | 12% | 14% | 13% | 10% | 11% | 7% | ||
| $1750 or more per week ($91,000 or more per year) | 140 (13.3) | 13% | 17% | 17% | 10% | 9% | 4% | ||
| State of residence | 49.39 | <.01 | |||||||
| Australian Capital Territory (ACT) | 23 (2.2) | 2% | 1% | 3% | 2% | 1% | 2% | ||
| New South Wales (NSW) | 283 (26.9) | 32% | 39% | 30% | 27% | 35% | 24% | ||
| Victoria (VIC) | 281 (26.7) | 26% | 27% | 28% | 24% | 30% | 19% | ||
| Queensland (QLD) | 234 (22.2) | 20% | 15% | 21% | 19% | 20% | 34% | ||
| South Australia (SA) | 91 (8.6) | 7% | 5% | 7% | 10% | 5% | 8% | ||
| Western Australia (WA) | 84 (8) | 10% | 10% | 10% | 12% | 7% | 11% | ||
| Tasmania (TAS) | 53 (5) | 2% | 2% | 2% | 3% | 2% | 2% | ||
| Northern Territory (NT) | 5 (0.5) | 1% | 1% | 0% | 3% | 1% | 0% |
N = 1054. Cross-tabulation results are presented.
LCA was conducted using Latent GOLD® software (version 5·1) (Vermunt and Magidson, 2016). LCA is a special case of person-centred mixture modelling that is appropriate for audience segmentation analysis. It is a popular segmentation analytic method and has certain advantages over other similar methods such as clustering, k-means clustering, and Q methodology, as LCA can handle categorical and interval variables, is less sensitive to missing data and provides fit indices to guide decisions to determine which number of groups best fits the data (Smith, 2017; Smith et al., 2021).
A three-step process was followed to reduce bias and robustly identify the differences between the segments on demographic and other variables (Vermunt, 2017; Vermunt and Magidson, 2016). In the first step, two through eight segment models were tested and evaluated on a number of criteria such as the Akaike information criteria (AIC), Bayesian information criteria (BIC), and class proportion, with lower AIC and BIC values indicating a better fit (Vermunt, 2017). While the model fit results get better with increasing number of segments, other factors such as parsimony and avoiding extremely small cluster sizes that may have little practical value were also considered when evaluating the alternative models.
In the second step, individual cases were assigned to latent classes and the latent class scores were saved in a new data file. In step 3, latent classification scores were related to demographic and other variables of interest using the Maximum Likelihood (ML) method to correct for the classification error and prevent bias. To test for association between continuous variables and latent classes, we used the Bolck–Croon–Hagenaars (BCH) method (Bakk and Vermunt, 2015). Demographic differences between the groups were investigated through cross tabulations. A final multinomial logistic was then used to assess the association between trust and segment membership with the first segment serving as a reference category.
The dataset contained few missing values with key variables missing 1 to 48 values or less than 5% missingness in the sample. Nevertheless, the analysis was conducted with both imputed data as well as ignoring missing cases. Hot-deck imputation (Myers, 2011) was used to impute missing values by matching the respondents’ gender and age. In Supplemental Tables 2 and 3, we show a similar model testing process, with model fit statistics and proportion of the sample in each segment, respectively, ignoring missing values (N = 966). As the results were similar, we report the imputed data results due to its larger sample size.
3. Results
Seven alternative models from a two-cluster to an eight-cluster model were tested using Latent Gold software and the fit indices are listed in Supplemental Table 1. A five-cluster solution provided the best fit of the model. Moreover, goodness-of-fit chi-square statistics by means of a parametric bootstrap between a four-cluster and a five-cluster model indicated that the latter better fit the data, –2LL Diff = 685.399 (p < .001). Based on TPB dimensions, these five clusters were named as vaccine enthusiasts, supporters, socials, hesitant and sceptics.
The five-cluster solution explained a large variance in each of the TPB constructs, ranging from 62% to 70% of variance for most COVID-19 vaccine attitude measures, 47% to 67% of variance in social norms, and 47% to 80% of variance in vaccine intentions. While still statistically significant in differentiating segments, variance in PBC as explained by the clusters was low at 13%; comparatively, the clusters explained 78% of variance in self-efficacy to get a COVID-19 vaccine.
Vaccine enthusiasts made up 28% (n = 296) of the sample. They have the most favourable attitudes towards a COVID-19 vaccine, perceive a high degree of social norms encouraging vaccination, and almost all say they will ‘definitely’ get a vaccine to protect themselves (99.97%) and other at-risk groups (99.17%), and are willing to put their name on a vaccine list (94%).
Vaccine supporters were 26% (n = 278) of the sample. They also have favourable COVID-19 vaccine attitudes and strong social norms towards vaccination, but significantly less than the enthusiasts. While over 90% of vaccine supporters ‘definitely’ want to get a vaccine, an even higher 95% say they will ‘definitely’ get a vaccine to protect others. A smaller proportion, 73%, is willing to put their name on a vaccine list.
Vaccine socials totalled 20% (n = 216) of the sample. They have lower favourable attitudes, norms and intentions to get a COVID-19 vaccine, compared with supporters and enthusiasts. The differentiating aspect of vaccine socials is that while only 13% say they will ‘definitely’ get a vaccine to protect themselves, 31% say they will ‘definitely’ get a vaccine to protect others. They are most likely to say ‘unsure, but leaning towards Yes’, regarding getting a vaccine to protect themselves (71%) and to protect others (53%), and to putting their name on a vaccine list (59%).
The vaccine hesitant included 15% (n = 156) of the sample. They have low favourable attitudes towards COVID-19 vaccines and perceive weaker social norms for vaccination, and a majority in this segment say they are ‘unsure, but leaning towards No’, regarding getting a vaccine to protect themselves (65%) and to protect others (51%). A majority of the vaccine hesitant will ‘definitely not’ put their name on a vaccine list (59%).
Vaccine sceptics were 10% (n = 108) of the sample. They have the least favourable attitudes towards a COVID-19 vaccine, perceive fewer social pressures towards getting vaccinated and are overwhelmingly likely to ‘definitely not’ take a vaccine to protect themselves (84%) or to protect others (53%), or to put their name on a vaccine list (89%). All say they have no intention to get vaccinated against the coronavirus when a vaccine is available to them (100%).
Reasons to accept or decline a vaccine
After the vaccine segments were identified, we analysed how similar or different are segments’ responses on reasons to accept or decline a vaccine, trusted information sources and demographic differences. Vaccine enthusiasts selected five of eight reasons on average to get a vaccine, including protecting self (95%), family (87%) and community (80%) (see Supplemental Table 4). Only a quarter of enthusiasts (15%) said they want to take the vaccine due to a chronic health condition, such as asthma or diabetes. Only about half (50%) of enthusiasts chose their doctor’s recommendation of vaccines as a reason to get a COVID-19 vaccine.
Vaccine supporters show a similar pattern, with a large majority selecting protecting self (91%), family (78%) and community (62%) as reasons they want to get vaccinated. A majority wanted to get a vaccine for a return to some form of normality: ‘It would allow me to feel safe around other people’ (66%) and ‘Life won’t go back to normal until most people are vaccinated’ (63%).
On average, vaccine socials selected fewer reasons either to get or not get a vaccine. A majority said the vaccine will protect them (60%) and their family (51%). A third had similar concerns of return to some degree of normality as the vaccine supporters. The most frequently selected reasons not to get a vaccine, albeit by only a few people in this segment, were concern about vaccine side effects (13%) and the speed of vaccine development (10%).
Vaccine side effects (72%) were the most prominent concern for the vaccine hesitant, followed by the speed of vaccine development (51%), need for more time to be sure about the safety of the vaccine (45%) and fears of a new, untested technology (41%).
Vaccine sceptics selected similar reasons as the hesitant to not get a COVID-19 vaccine, but in greater numbers, including vaccine side effects (94%), speed of vaccine development (93%), and that it was a new, untested technology (74%). About a third dismissed health risks from COVID-19 (37%) and feared they will get infected with coronavirus from the vaccine (33%). A quarter also dismissed the pandemic as not serious as some people say it is (26%).
Demographic differences
The five COVID-19 vaccine segments differed on gender, age, education, income and state of residence (see Table 2). Vaccine enthusiasts are overwhelmingly male (71%), whereas females were slightly more likely to be in other segments, particularly the hesitant segment where 75% of the segment was female (χ2 = 126.58, p < .001).
Older respondents were most likely to be vaccine enthusiasts, with about 80% of the segment aged 50 years and older. A majority of respondents in the social and hesitant segments were 20–29 years old, whereas a third of sceptics were 30–39 years old (χ2 = 300.90, p < .001). A third of vaccine enthusiasts and supporters had a Bachelor’s degree. A majority of socials, hesitant, and sceptics had only a primary or a high school qualification (χ2 = 72.67, p < .001).
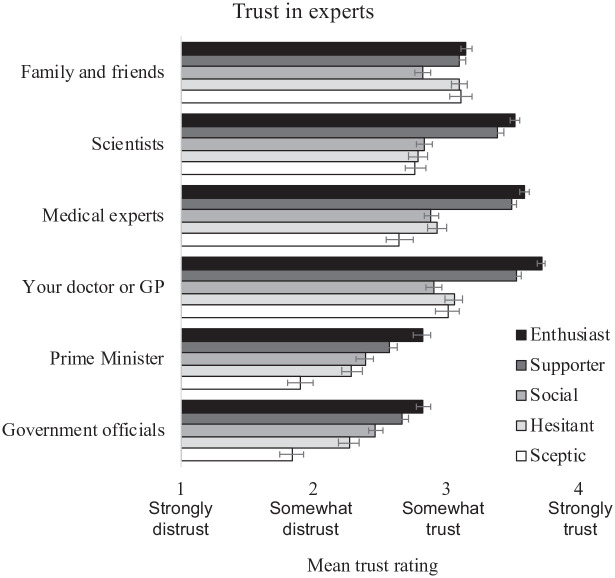
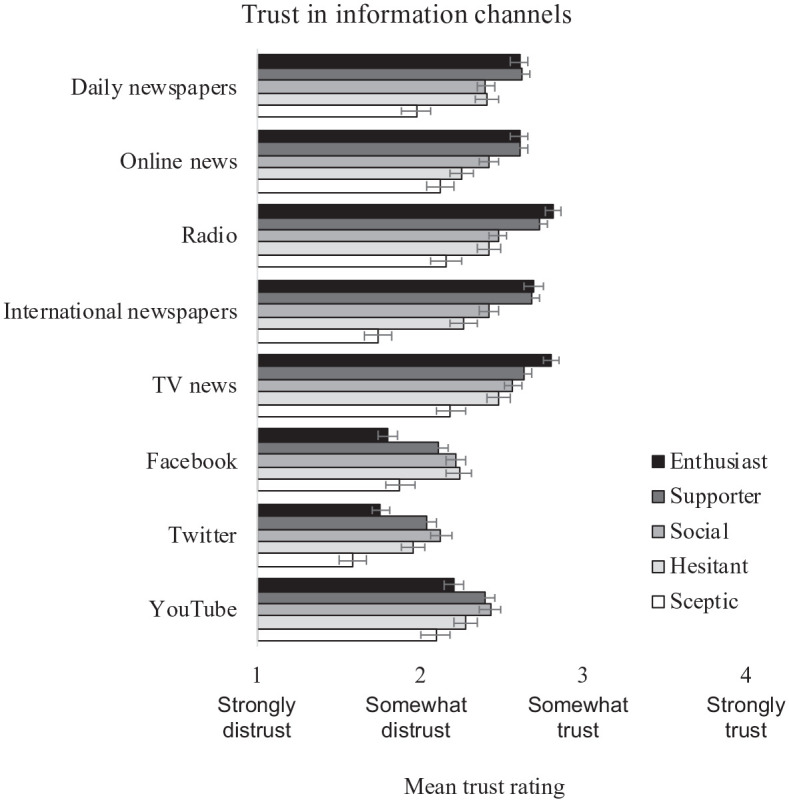
Trust in informational sources
There were significant differences between the five segments on trust in informational sources (see Table 3 as well as Figures 1 and 2). A multinomial logistic regression analysis revealed that compared with vaccine enthusiasts, vaccine socials, hesitant and sceptics had significantly lower levels of trust in medical experts, their doctor (General Practice), scientists, government officials and the Prime Minister as accurate sources of information.
Table 3.
Multinomial logistic regression with latent classes as the outcome variable and trust in informational sources as input variables.
| Supporters | Socials | Hesitant | Sceptics | Wald | R² | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| B | SE | B | SE | B | SE | B | SE | |||
| Experts & Government | ||||||||||
| Medical experts | −0.22 | 0.14 | −1.02 | 0.14 | −1.06 | 0.14 | −1.27 | 0.14 | 115.67 | 0.19 |
| GP | −0.56 | 0.17 | −1.41 | 0.16 | −1.34 | 0.16 | −1.39 | 0.17 | 101.28 | 0.17 |
| Scientists | −0.23 | 0.12 | −0.91 | 0.12 | −0.98 | 0.12 | −0.97 | 0.12 | 115.42 | 0.16 |
| Government officials | −0.15 | 0.07 | −0.41 | 0.07 | −0.45 | 0.08 | −0.92 | 0.10 | 101.99 | 0.11 |
| Prime Minister | −0.21 | 0.07 | −0.43 | 0.07 | −0.42 | 0.07 | −0.75 | 0.09 | 85.21 | 0.09 |
| Media | ||||||||||
| International newspapers (The Guardian, The New York Times) | 0.05 | 0.08 | −0.32 | 0.08 | −0.36 | 0.08 | −0.79 | 0.10 | 88.91 | 0.09 |
| Radio | −0.04 | 0.08 | −0.40 | 0.08 | −0.49 | 0.09 | −0.67 | 0.10 | 74.84 | 0.07 |
| Daily newspapers | 0.04 | 0.08 | −0.33 | 0.08 | −0.37 | 0.09 | −0.60 | 0.11 | 64.19 | 0.07 |
| Online news | 0.01 | 0.08 | −0.31 | 0.08 | −0.40 | 0.09 | −0.50 | 0.10 | 56.29 | 0.05 |
| TV news | −0.13 | 0.08 | −0.35 | 0.08 | −0.36 | 0.08 | −0.62 | 0.10 | 52·39 | 0.05 |
| Family and Social Media | ||||||||||
| Family and friends | −0.06 | 0.09 | −0.46 | 0.08 | −0.08 | 0.10 | −0.23 | 0.11 | 35.81 | 0.04 |
| 0.28 | 0.07 | 0.24 | 0.07 | 0.34 | 0.08 | 0.01 | 0.09 | 30.56 | 0.03 | |
| 0.30 | 0.07 | 0.26 | 0.08 | 0.26 | 0.08 | −0.12 | 0.10 | 32.04 | 0.03 | |
| YouTube | 0.21 | 0.07 | 0.13 | 0.07 | 0.11 | 0.08 | −0.12 | 0.09 | 17.12 | 0.02 |
N = 1054. Reference category is the first segment of vaccine enthusiasts. B is multinomial logistic regression coefficient and SE is robust standard error associated with the models. R2 is the variance explained in the five segments by each trust variable. Trust was measured on a 5-point scale from strongly distrust (1) to strongly trust (5) and don’t know (3) as the midpoint. A different recording of trust variables by assign missing to don’t know does not change the above results. All differences in trust variables between the five segments were significant at p < .001.
Figure 1.
Difference in trust in friends, experts and government officials between the five segments. Trust reported here is ignoring don’t know responses. In the article, trust is reported on a 5-point scale from strongly distrust (1) to strongly trust (5) and don’t know as the midpoint (3). Regardless of how trust is measured, the results are similar.
Figure 2.
Difference in trust in informational channels between the five segments. Trust reported here is ignoring don’t know responses. In the manuscript, trust is reported on a 5-point scale from strongly distrust (1) to strongly trust (5) and don’t know as the midpoint (3). Regardless of how trust is measured, the results are similar.
Similarly, compared with enthusiasts, vaccine socials, hesitant and sceptics had significantly lower levels of trust in mainstream newspapers, radio and TV news. There was no significant difference between enthusiasts and supporters on trust in family and friends or traditional media channels such as newspapers, radio and TV news.
However, vaccine enthusiasts had lower levels of trust in social media channels, such as Facebook, Twitter and YouTube, compared with supporters, socials and hesitant. Vaccine sceptics had similarly low levels of trust in social media channels as vaccine enthusiasts.
Finally, vaccine enthusiasts showed a significantly higher level of trust in family and friends, than vaccine socials. Trust in family and friends among supporters, hesitant, and sceptic were more or less the same as enthusiasts.
4. Discussion
Using the TPB as a theoretical framework, this study illustrates five distinct audience segments on COVID-19 vaccine intentions in Australia. These segments significantly differ on the 16 items measuring their attitudes, norms, PBC and vaccination intentions. After the segmentation analysis, we also found that the vaccine segments differ on demographic variables, levels of trust in information sources and reasons to accept or decline a COVID-19 vaccine. This novel audience segmentation approach combines TPB – one of the most popular conceptual frameworks for the study of human action and vaccination intentions and behaviours – and LCA to better understand how the public makes decisions about COVID-19 vaccination.
Vaccine enthusiasts (28%) are the largest among the five segments and are motivated to get a COVID-19 vaccine. While vaccine supporters (26%) are less enthusiastic about getting a COVID-19 vaccine, they show a clear preference for it. The vaccine socials (20%) hold less favourable attitudes, norms and intentions to get a COVID-19 vaccine, but say they will ‘definitely’ get a vaccine to protect others. The vaccine hesitant (15%) hold less favourable attitudes towards COVID-19 vaccines and perceive weaker social norms for vaccination, and a majority say they are unsure about getting a vaccine or not, either to protect self or others. The vaccine sceptics (10%) display the least favourable attitudes towards a COVID-19 vaccine, perceive fewer social pressures towards getting vaccinated and are overwhelmingly likely to reject getting a COVID-19 vaccine.
Compared with the traditional use of single or few measures to segment the public into two or three segments such as unsure and unwilling (Dodd et al., 2021a, 2021b; Freeman et al., 2021; Nomura et al., 2021; Prickett et al., 2021; Rhodes et al., 2020), these results provide a theory-driven, refined analysis of different publics on COVID-19 vaccine intentions. In particular, we found a new segment of vaccine socials appear to be driven by altruism – get a vaccine to protect others – even as they hold less favourable attitudes towards vaccines, perceive little social pressure to get a vaccine, and a lower level of PBC compared with enthusiasts and supporters. In addition, vaccine socials selected fewer reasons either to get or not get a vaccine compared with other segments, indicating they are looking for reasons to make up their mind.
Such nuanced segmentation helps clarify previous theoretical and practical implications. For example, there is mixed evidence on the role of altruism messaging to improve public willingness to get a vaccine, with some studies finding support (Chen et al., 2021; Cucciniello et al., 2021) while others report that for strongly hesitant, emphasising personal benefit reduces hesitancy to a greater extent than information on collective benefits (Freeman et al., 2021). Our findings indicate that altruism messaging is likely to resonate with the vaccine socials in Australia.
Trust
Reaching audiences through their trusted channels is also critical for message uptake. Vaccine enthusiasts may need little targeted communication but should not be treated as a captive audience as they may still need information and assurances. Vaccine supporters may need frequent message boosters about the need, safety and efficacy of the COVID-19 vaccine to become more enthusiastic about getting a vaccine. The vaccine supporters are more likely to trust newspapers and social media channels, indicating that these are effective mediums to increase vaccine enthusiasm among supporters. Vaccine socials are most likely to respond to altruistic messaging; therefore, emphasising the social need for vaccination will be effective in persuading the vaccine socials (e.g. Cucciniello et al., 2021). Communication campaigns that address COVID-19 vaccine specific side effects, perceptions about new and untested technology, and personal compatibility will most likely resonate with the vaccine hesitant (Nomura et al., 2021). Both vaccine socials and hesitant are more likely to trust social media compared with others, indicating that vaccine and health communication campaigns on social media channels are likely to reach these vaccine segments. Official communication from the government and health authorities – asserting scientific consensus about and confidence in vaccines – is likely to be ineffective, or even backfire among sceptics (Hopfer, 2012; Hornsey et al., 2018). The only source of information they trust is family and friends, indicating that effective communication is likely to be through these channels.
Demographic differences
Similar to previous studies, males were most enthusiastic about getting a vaccine while females were found to be more hesitant compared with males (Edwards et al., 2021; Rhodes et al., 2020; Roy Morgan, 2021). There is also converging evidence that the public who continue to be hesitant are between 20 and 29 years old, whereas sceptics are more likely to be from the 30–39 years age group (Faasse and Newby, 2020; Melbourne Institute, n.d.; Roy Morgan, 2021). These findings further highlight that those who are most vulnerable – the poor and undereducated – to the health and economic impacts of COVID-19 may need further help in understanding the need and importance of COVID-19 vaccination.
The five vaccine segments identified in this study explained about half or more variance in each of the TPB constructs, with the highest explained variance in behavioural intention to get a vaccine (62%–80%), followed by self-efficacy (78%), attitudes (62%–70%) and social norms (47%–67%). The variance explained in behavioural intention using this segmentation approach is higher than that explained in previous studies using individual TPB variables, which ranged from 52% to 54% (Xiao and Wong, 2020). However, the five segments explained only 13% of the variance in PBC. To the extent that these findings are replicated, further research must clarify the role of PBC above and beyond that of self-efficacy in TPB (Xiao and Wong, 2020).
Limitations
TPB is not the only theory that can be used for audience segmentation. Researchers should attempt to identify theories that help determine the most relevant antecedents related to their target behaviour (Fishbein and Ajzen, 2011). Future research should test multiple items to verify whether ‘Vaccine Socials’ is a stable and identifiable segment as some previous studies show altruism messaging may work with some audiences but not others (Chen et al., 2021; Cucciniello et al., 2021). Researchers should also attend to other contextual factors of vaccine access, such as the distance to the closest clinic as vulnerable populations may have less access to healthcare, which in a mutually reinforcing spiral can increase mistrust with health agencies.
Understanding different motivations of the public to perform healthy behaviours helps us better reach the distinct publics, by supporting them to access and understand the information that can overcome their concerns and prompt vaccine uptake, delivered through a messenger they trust, via a channel they rely upon. This study shows there are five distinct publics on COVID-19 vaccination in Australia. Unique contributions of this study include a theoretically driven and analytically robust, 16-item segmentation analysis. Findings of this study are likely to help the government and health advocacy groups to better understand and reach their key publics, as a very high rate of vaccination, over 90%, will minimise the risk of community spread due to new variants.
Supplemental Material
Supplemental material, sj-docx-1-pus-10.1177_09636625221138494 for Audience segmentation analysis of public intentions to get a COVID-19 vaccine in Australia by Jagadish Thaker, Lucy M. Richardson and David C. Holmes in Public Understanding of Science
Author biographies
Jagadish Thaker is a Senior Lecturer at the University of Auckland. His research examines ways to understand and enhance public, business and policy engagement with climate change and public health.
Lucy M. Richardson is a postdoctoral research fellow with Monash University’s Climate Change Communication Research Hub. Her current research focuses on understanding Australian climate change audiences and their responses to messaging, and understanding how various aspects of climate change are represented by the media.
David C. Holmes is Director of the Monash Climate Change Communication Research Hub as well as Communications Lead for the Australian Government’s National Environmental Science Program, Climate Systems Hub. Trained in the sociology of communications, his research explores the interrelations between media, science communication and climate change.
Footnotes
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work received funding from Monash University and Massey University to field the survey.
ORCID iDs: Jagadish Thaker  https://orcid.org/0000-0003-4589-7512
https://orcid.org/0000-0003-4589-7512
Lucy M. Richardson  https://orcid.org/0000-0003-2150-7671
https://orcid.org/0000-0003-2150-7671
Supplemental material: Supplemental material for this article is available online.
Contributor Information
Jagadish Thaker, University of Auckland, New Zealand.
David C. Holmes, Monash University, Australia
References
- Agley J, Xiao Y. (2021) Misinformation about COVID-19: Evidence for differential latent profiles and a strong association with trust in science. BMC Public Health 21(1): 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ajzen I. (1985) From intentions to actions: A theory of planned behaviour. In: Kuhl J, Beckmann J. (eds) Action Control: From Cognition to Behaviour. Berlin: Springer, pp. 11–39. [Google Scholar]
- Ajzen I. (2002) Perceived behavioral control, self-efficacy, locus of control, and the theory of planned behavior. Journal of Applied Social Psychology 32(4): 665–683. [Google Scholar]
- Armitage CJ, Conner M. (2001) Efficacy of the theory of planned behaviour: A meta-analytic review. British Journal of Social Psychology 40(4): 471–499. [DOI] [PubMed] [Google Scholar]
- Australian Bureau of Statistics (2017. a) 2016 Census quick stats. Available at: https://quickstats.censusdata.abs.gov.au/census_services/getproduct/census/2016/quickstat/036 (accessed 20 June 2020).
- Australian Bureau of Statistics (2017. b) Census 2016, total personal income (weekly) by age by sex (SA2+). Available at: https://stat.data.abs.gov.au/Index.aspx?DataSetCode=ABS_C16_T13_SA (accessed 20 June 2020).
- Australian Bureau of Statistics (2020) Regional population by age and sex, Australia. Available at: https://www.abs.gov.au/AUSSTATS/abs@.nsf/Explanatory%20Notes/3235.0 (accessed 20 June 2020).
- Australian Bureau of Statistics (2021. a) Household impacts of COVID-19 survey. Available at: https://www.abs.gov.au/statistics/people/people-and-communities/household-impacts-covid-19-survey/latest-release (accessed 20 September 2021).
- Australian Bureau of Statistics (2021. b) National, state and territory population. Available at: https://www.abs.gov.au/statistics/people/population/national-state-and-territory-population/latest-release#states-and-territories (accessed 16 September 2021).
- Bakk Z, Vermunt JK. (2015) Step-3 tutorial# 1: Step-3 Models with covariates, distal outcomes, and multiple latent variables. Available at: https://www.statisticalinnovations.com/wp-content/uploads/LGtutorial.Step3_.1.pdf (accessed 10 June 2020).
- Bass SB, Kelly PJ, Hoadley A, Lloret AA, Organtini T. (2022) Mapping perceptual differences to understand COVID-19 beliefs in those with vaccine hesitancy. Journal of Health Communication 27(1): 49–61. [DOI] [PubMed] [Google Scholar]
- Bish A, Yardley L, Nicoll A, Michie S. (2011) Factors associated with uptake of vaccination against pandemic influenza: A systematic review. Vaccine 29(38): 6472–6484. [DOI] [PubMed] [Google Scholar]
- Chen Y-L, Lin Y-J, Chang Y-P, Chou W-J, Yen C-F. (2021) Differences in the protection motivation theory constructs between people with various latent classes of motivation for vaccination and preventive behaviors against COVID-19 in Taiwan. International Journal of Environmental Research and Public Health 18(13): 7042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cucciniello M, Pin P, Imre B, Porumbescu GA, Melegaro A. (2021) Altruism and vaccination intentions: Evidence from behavioral experiments. Social Science & Medicine 292: 114195. [DOI] [PubMed] [Google Scholar]
- de Figueiredo A, Simas C, Karafillakis E, Paterson P, Larson HJ. (2020) Mapping global trends in vaccine confidence and investigating barriers to vaccine uptake: A large-scale retrospective temporal modelling study. The Lancet 396(10255): 898–908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Department of Health (2021) Vaccination numbers and statistics. Available at: https://www.health.gov.au/initiatives-and-programs/covid-19-vaccines/numbers-statistics (accessed 6 October 2021).
- Dodd RH, Cvejic E, Bonner C, Pickles K, McCaffery KJ. (2021. a) Willingness to vaccinate against COVID-19 in Australia. The Lancet Infectious Diseases 21(3): 318–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dodd RH, Pickles K, Nickel B, Cvejic E, Ayre J, Batcup C, et al. (2021. b) Concerns and motivations about COVID-19 vaccination. The Lancet Infectious Diseases 21(2): 161–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards B, Biddle N, Gray M, Sollis K. (2021) COVID-19 vaccine hesitancy and resistance: Correlates in a nationally representative longitudinal survey of the Australian population. PLoS ONE 16(3): e0248892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faasse K, Newby J. (2020) Public perceptions of COVID-19 in Australia: Perceived risk, knowledge, health-protective behaviors, and vaccine intentions. Frontiers in Psychology 11: 551004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fan C-W, Chen I-H, Ko N-Y, Yen C-F, Lin C-Y, Griffiths MD, et al. (2021) Extended theory of planned behavior in explaining the intention to COVID-19 vaccination uptake among mainland Chinese university students: An online survey study. Human Vaccines & Immunotherapeutics 17(10): 3413–3420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fishbein M, Ajzen I. (2011) Predicting and Changing Behavior: The Reasoned Action Approach. New York, NY: Psychology press. [Google Scholar]
- Freeman D, Loe BS, Yu L-M, Freeman J, Chadwick A, Vaccari C, et al. (2021) Effects of different types of written vaccination information on COVID-19 vaccine hesitancy in the UK (OCEANS-III): A single-blind, parallel-group, randomised controlled trial. The Lancet Public Health 6(6): e416–e427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- French J, Deshpande S, Evans W, Obregon R. (2020) Key guidelines in developing a pre-emptive covid-19 vaccination uptake promotion strategy. International Journal of Environmental Research and Public Health 17(16): 5893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerend MA, Shepherd JE. (2012) Predicting HPV vaccine uptake in young adult women: Comparing the health belief model and theory of planned behavior. Annals of Behavioral Medicine 44(2): 171–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guidry JPD, Perrin PB, Laestadius LI, et al. (2021) U.S. public support for COVID-19 vaccine donation to low- and middle-income countries during the COVID-19 pandemic. Vaccine 39(17): 2452–2457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hine DW, Reser JP, Morrison M. (2014) Audience segmentation and climate change communication: Conceptual and methodological considerations. WIREs Climate Change 5(4): 441–459. [Google Scholar]
- Hopfer S. (2012) Effects of a narrative HPV vaccination intervention aimed at reaching college women: A randomized controlled trial. Prevention Science 13(2): 173–182. [DOI] [PubMed] [Google Scholar]
- Hornsey MJ, Harris EA, Fielding KS. (2018) The psychological roots of anti-vaccination attitudes: A 24-nation investigation. Health Psychology 37(4): 307–315. [DOI] [PubMed] [Google Scholar]
- Ihm J, Lee C-J. (2021) Toward more effective public health interventions during the covid-19 pandemic: Suggesting audience segmentation based on social and media resources. Health Communication 36(1): 98–108. [DOI] [PubMed] [Google Scholar]
- Juraskova I, O’Brien M, Mullan B, Bari R, Laidsaar-Powell R, McCaffery K. (2012) HPV vaccination and the effect of information framing on intentions and behaviour: An application of the theory of planned behaviour and moral norm. International Journal of Behavioral Medicine 19(4): 518–525. [DOI] [PubMed] [Google Scholar]
- Kleitman S, Fullerton DJ, Zhang LM, Blanchard MD, Lee J, Stankov L, et al. (2021) To comply or not comply? A latent profile analysis of behaviours and attitudes during the COVID-19 pandemic. PLoS ONE 16(7): e0255268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krishna A. (2018) Poison or prevention? Understanding the linkages between vaccine-negative individuals’ knowledge deficiency, motivations, and active communication behaviors. Health Communication 33(9): 1088–1096. [DOI] [PubMed] [Google Scholar]
- Larson HJ, Clarke RM, Jarrett C, Eckersberger E, Levine Z, Schulz WS, et al. (2018) Measuring trust in vaccination: A systematic review. Human Vaccines & Immunotherapeutics 14(7): 1599–1609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latkin CA, Dayton L, Miller JR, Yi G, Jaleel A, Nwosu CC, et al. (2021) Behavioral and attitudinal correlates of trusted sources of COVID-19 vaccine information in the US. Behavioral Sciences 11(4): 56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazić A, Žeželj I. (2021) A systematic review of narrative interventions: Lessons for countering anti-vaccination conspiracy theories and misinformation. Public Understanding of Science 30(6): 644–670. [DOI] [PubMed] [Google Scholar]
- Lin C, Tu P, Beitsch LM. (2020) Confidence and receptivity for COVID-19 vaccines: A rapid systematic review. Vaccines 9(1): 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loomba S, de Figueiredo A, Piatek SJ, de Graaf K, Larson HJ. (2021) Measuring the impact of COVID-19 vaccine misinformation on vaccination intent in the UK and USA. Nature Human Behaviour 5(3): 337–348. [DOI] [PubMed] [Google Scholar]
- Melbourne Institute (n.d.) Vaccine hesitancy tracker. Available at: https://melbourneinstitute.unimelb.edu.au/publications/research-insights/ttpn/vaccination-report (accessed 20 September 2021).
- Myers TA. (2011) Goodbye, listwise deletion: Presenting hot deck imputation as an easy and effective tool for handling missing data. Communication Methods and Measures 5(4): 297–310. [Google Scholar]
- Noar SM. (2012) An audience–channel–message–evaluation (ACME) framework for health communication campaigns. Health Promotion Practice 13(4): 481–488. [DOI] [PubMed] [Google Scholar]
- Nomura S, Eguchi A, Yoneoka D, Kawashima T, Tanoue Y, Murakami M, et al. (2021) Reasons for being unsure or unwilling regarding intention to take COVID-19 vaccine among Japanese people: A large cross-sectional national survey. The Lancet Regional Health – Western Pacific 14: 100223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Premier of Victoria (2021) Statement form the acting premier. Available at: https://www.premier.vic.gov.au/statement-acting-premier-1 (accessed 5 October 2021).
- Prickett KC, Habibi H, Carr PA. (2021) COVID-19 vaccine hesitancy and acceptance in a cohort of diverse New Zealanders. The Lancet Regional Health – Western Pacific 14: 100241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qualtrics Panel (2021) Online panels. Available at: https://www.qualtrics.com/au/research-services/online-sample/ (accessed 1 October 2021).
- Rhodes A, Hoq M, Measey M-A, Danchin M. (2020) Intention to vaccinate against COVID-19 in Australia. The Lancet Infectious Diseases 21(5): e110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rimal RN, Lapinski MK. (2015) A re-explication of social norms, ten years later. Communication Theory 25(4): 393–409. [Google Scholar]
- Roy Morgan (2021) An increasing majority of 80% of Australians willing to be vaccinated for COVID-19 – Up 1% point since late January. Available at: http://www.roymorgan.com/findings/8646-roy-morgan-survey-on-masks-borders-vaccines-in-australia-february-15-2021-202102141000 (accessed 10 July 2022).
- Schmid P, Rauber D, Betsch C, Lidolt G, Denker M-L. (2017) Barriers of influenza vaccination intention and behavior – A systematic review of influenza vaccine hesitancy, 2005 – 2016. PLoS ONE 12(1): e0170550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider KE, Dayton L, Rouhani S, Latkin CA. (2021) Implications of attitudes and beliefs about COVID-19 vaccines for vaccination campaigns in the United States: A latent class analysis. Preventive Medicine Reports 24: 101584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skinner CS, Strecher VJ, Hospers H. (1994) Physicians’ recommendations for mammography: Do tailored messages make a difference? American Journal of Public Health 84(1): 43–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slater MD. (1996) Theory and method in health audience segmentation. Journal of Health Communication 1(3): 267–284. [DOI] [PubMed] [Google Scholar]
- Smith RA. (2017) Audience segmentation techniques. In: Parrott RL. (ed.) Oxford Research Encyclopedia of Communication: Health and Risk Message Design and Proceedings. New York, NY: Oxford University Press, pp. 1–12. [Google Scholar]
- Smith RA, Myrick JG, Lennon RP, Martin MA, Small ML, Van Scoy LJ, et al. (2021) Exploring behavioral typologies to inform COVID-19 health campaigns: A person-centered approach. Journal of Health Communication 26(6): 402–412. [DOI] [PubMed] [Google Scholar]
- Thaker J. (2021) Audience segmentation of COVID-19 vaccination intentions in Aotearoa-New Zealand. Report, Massey University, Palmerston North, New Zealand, February. [Google Scholar]
- Thaker J, Cook C. (2022) Planning for a COVID-19 vaccination campaign in New Zealand: Trust, affective and cognitive attitudes, and COVID-19 vaccine intention. Communication Research and Practice 1(16): 54–69. [Google Scholar]
- Thaker J, Ganchoudhuri S. (2021) The role of attitudes, norms, and efficacy on shifting COVID-19 vaccine Intentions: A longitudinal study of COVID-19 vaccination intentions in New Zealand. Vaccines 9(10): 1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vermunt JK. (2017) Latent class modeling with covariates: Two improved three-step approaches. Political Analysis 18(4): 450–469. [Google Scholar]
- Vermunt JK, Magidson J. (2016) Technical Guide for Latent GOLD 5.1: Basic, Advanced, and Syntax. Belmont, MA: Statistical Innovations. [Google Scholar]
- Wise J. (2021) Covid-19: How AstraZeneca lost the vaccine PR war. British Medical Journal 373: 1–3. [DOI] [PubMed] [Google Scholar]
- Xiao X. (2019) Follow the heart or the mind? Examining cognitive and affective attitude on HPV vaccination intention. Atlantic Journal of Communication 29(2): 93–105. [Google Scholar]
- Xiao X, Wong RM. (2020) Vaccine hesitancy and perceived behavioral control: A meta-analysis. Vaccine 38(33): 5131–5138. [DOI] [PubMed] [Google Scholar]
- Yaqub O, Castle-Clarke S, Sevdalis N, Chataway J. (2014) Attitudes to vaccination: A critical review. Social Science & Medicine 112: 1–11. [DOI] [PubMed] [Google Scholar]
- Zheng H, Jiang S, Wu Q. (2022) Factors influencing COVID-19 vaccination intention: The roles of vaccine knowledge, vaccine risk perception, and doctor-patient communication. Patient Education and Counseling 105(2): 277–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-pus-10.1177_09636625221138494 for Audience segmentation analysis of public intentions to get a COVID-19 vaccine in Australia by Jagadish Thaker, Lucy M. Richardson and David C. Holmes in Public Understanding of Science