Abstract
BACKGROUND
There is debate on whether uterine gauze packing or intrauterine balloon tamponade is safer and more effective as a surgical management option for treating postpartum hemorrhage.
OBJECTIVE
This study aimed to compare intra- and postoperative outcomes of intrauterine balloon tamponade and uterine gauze packing in patients with postpartum hemorrhage.
STUDY DESIGN
A range of databases such as Cochrane and PubMed were searched using terms including “post-partum haemorrhage,” “uterine balloon tamponade,” and “uterine gauze packing.” All observational studies comparing intrauterine balloon tamponade with uterine gauze packing were included. Five studies were identified enrolling 821 adult patients diagnosed with postpartum hemorrhage. Primary outcomes included blood loss volume, success rates, and maternal mortality. Secondary outcomes comprised requiring additional interventions, postoperative hemoglobin levels, and requiring blood transfusions. Fixed and random models were used for analysis.
RESULTS
Intrauterine balloon tamponade seemed to be a superior option to uterine gauze packing. Intrauterine balloon tamponade was better in reducing intraoperative blood loss, with a statistically significant improvement (P<.0001). Cases managed with intrauterine balloon tamponade seemed to have statistically significant shorter operative time (P=.023) and hospital length of stay (P=.020) in one study.
CONCLUSION
Intrauterine balloon tamponade remains more effective and safer as a first-line surgical management option for postpartum hemorrhage compared with uterine gauze packing.
Keywords: gauze packing, intrauterine balloon, postpartum hemorrhage
AJOG MFM at a Glance.
Why was this study conducted?
Uterine gauze packing (UGP) and intrauterine balloon tamponade (IUBT) are known techniques for managing postpartum hemorrhage (PPH). UGP is currently used to a lesser extent because of its risks. IUBT is a method developed to treat PPH that is now recommended as a first-line option. There is debate on whether UGP or IUBT is superior. No meta-analysis comparing UGP with IUBT has been identified.
Key findings
This study demonstrates the superiority of IUBT over UGP. IUBT showed more improvements compared with UGP, and IUBT patients had less intraoperative bleeding and were less likely to require blood transfusions. Furthermore, IUBT patients had shorter operating times and hospital stays.
What does this add to what is known?
Our findings support current guidelines recommending IUBT as a first-line technique. IUBT seems to be a safer and more effective method for managing PPH.
Introduction
Primary postpartum hemorrhage (PPH) within the first 24 hours following delivery is a major contributor to maternal mortality internationally,1 and carries a maternal mortality risk of 1 in 100,000 deliveries in the United Kingdom.2
Uterine gauze packing (UGP), one of the earliest methods of controlling uterine bleeding described,3 is simple, quick, and effective in managing PPH.4 However, it has been a subject of controversy owing to reported disadvantages, including infection risk, uterine trauma, and concealed hemorrhage.3,5 Consequently, use of UGP has declined,4 although it is still useful in scenarios where, for example, uterine atony is unresponsive to oxytocic agents.6
Intrauterine balloon tamponade (IUBT) is a currently recognized technique used to avoid more invasive approaches for PPH.+7 It is widely used because of its simplicity and minimally invasive nature. The Bakri tamponade is the first balloon system specifically designed to manage PPH, which demonstrated remarkable success rates.8,9 Additional studies have been published regarding IUBT and newer systems have been described.10,11
The Royal College of Obstetricians and Gynaecologists12 recommends that surgical interventions be started as soon as pharmacologic management of the hemorrhage fails, and considers that IUBT is a suitable first-line surgical intervention in cases where uterine atony is the main cause of bleeding.
Although guidelines recommend IUBT as the first-line intervention, some studies have shown that UGP alone is sufficient to limit PPH and applying IUBT can lead to more complications. Although a recent systematic review compared several interventions for PPH,13 no quantitative meta-analysis comparing UGP and IUBT has been previously performed.
Materials and Methods
A systematic review and meta-analysis were conducted as per the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.14
Eligibility criteria
All randomized control trials (RCTs) and observational studies comparing IUBT with UGP for women with primary PPH were included. The intervention group of interest was IUBT and the comparator was UGP.
Primary outcomes
The primary outcomes were blood loss, success rate of controlling bleeding, and maternal mortality. Blood loss was further defined as intraoperative or postoperative blood loss (mL) and as including PPH >1000 mL or <1000 mL. Success rate was analyzed to include the number of participants who had a successful operation without the need for any additional interventions such as hysterectomy or uterine artery embolization.
Secondary outcomes
The secondary outcomes included need for secondary interventions including hysterectomy and uterine artery embolization, intensive care unit (ICU) admission, postoperative hemoglobin, length of stay in hospital, B-Lynch sutures, operative time, and blood transfusion.
Literature search strategy
Two authors (AA and AAN) independently searched the following electronic databases: MEDLINE, Embase, CINAHL, and the Cochrane Central Register of Controlled Trials (CENTRAL) in addition to reference lists of included studies. The search was run on September 30, 2020. Thesaurus headings, search operators, and limits in each of the above databases were adapted accordingly. In addition, World Health Organization International Clinical Trials Registry (http://apps. who.int/trialsearch/), ClinicalTrials.gov (http://clinical- trials.gov/), and the ISRCTN (International Standard Randomised Controlled Trial Number) Registry (http://www.isrctn. com/) were searched for details of ongoing and unpublished studies. No language restrictions were applied in our search strategies. The search terminologies included “gauze,” “gauze packing,” “chitosan-covered gauze,” “balloon tamponade instrumentation,” “balloon tamponade,” “placenta praevia,” “placenta accreta,” “retained placenta,” “uterine atony,” “post-partum haemorrhage,” and “uterine inversion.” The bibliographic lists of relevant articles were also reviewed.
Selection of studies
The titles and abstracts of articles identified from the literature searches were assessed independently by 2 authors (AA and AAN). The full texts of relevant reports were retrieved, and articles that met the eligibility criteria of our review were selected. Any discrepancies in study selection were resolved by discussion between the authors.
Data extraction and management
An electronic data extraction spreadsheet was created in line with Cochrane's data collection form15 for intervention reviews. The spreadsheet was pilot-tested in randomly selected articles and adjusted accordingly. Our data extraction spreadsheet included study-related data (first author, year of publication, country of origin of the corresponding author, journal in which the study was published, study design, study size, clinical condition of the study participants, type of intervention, and comparison), baseline demographics of the included populations (age), and primary and secondary outcome data. Two authors cooperatively collected and recorded the results and any disagreements were solved via discussion.
Data synthesis
Data synthesis was conducted using the Review Manager (RevMan) 5.3 software (Cochrane, London, United Kingdom).16 The extracted data were entered into RevMan by 2 independent authors (AA and AAN). The analysis was based on the fixed-effects model. A random-effects model was used only if the heterogeneity was >75% (ie, high-level). The results were reported in forest plots with 95% confidence intervals (CIs).
For dichotomous outcomes, the odds ratio (OR) was calculated between the 2 groups. The OR was the odds of an event in the IUBT group vs the UGP group. An OR of >1 for the primary success rate outcome would favor the IUBT group, an OR of <1 would favor the UGP group, and an OR of 1 would favor neither group. For all other outcomes, an OR >1 would favor the UGP group and an OR of <1 would favor the IUBT group.
For continuous outcomes, the mean difference (MD) was calculated between the 2 groups. For intraoperative bleeding, a positive MD would favor the UGP group, a negative MD would favor the IUBT group, and an MD of 0 would favor neither group. For postoperative bleeding, data were reported as median and range in 2 studies, hence quantitative analysis could not be done and they were reported qualitatively instead.
Assessment of heterogeneity
Heterogeneity among the studies was assessed using the Cochran Q test (chi-square). Inconsistency was quantified by calculating I2 and interpreted using the following guide: 0% to 25%, 25% to 75%, and 75% to 100% may represent low, moderate, and high heterogeneity, respectively.
Methodological quality and risk of bias assessment
AAT and AAM independently assessed the risk of bias for articles and the methodological quality matching the inclusion criteria. For randomized trials, the Cochrane tool for evaluating risk of bias17 was used. Domains assessed included selection bias, performance bias, detection bias, attrition bias, reporting bias, and other sources. RCTs were classified as having low, unclear, and high risk of bias. For nonrandomized studies, the Newcastle–Ottawa scale was used,18 which applies a star grading system to assess studies in terms of 3 domains: selection, comparability, and exposure. The total maximum score for each study is 9 stars.
Ethical approval
Because of the nature of this study in regard to obtaining relevant data, ethical approval was not required.
Results
Literature search results
Our search strategy retrieved 41 studies. After a thorough screening of the retrieved articles, the authors identified 5 studies in total that met the eligibility criteria (Figure 1).
Figure 1.
PRISMA flow diagram
The PRISMA diagram details the search and selection processes applied during the overview.
PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Abul. Safety and efficacy of intrauterine balloon tamponade vs uterine gauze packing in managing postpartum hemorrhage. Am J Obstet Gynecol Glob Rep 2022.
Description of studies
Guo et al
A single-center retrospective cohort study was performed by Guo C et al between January 2010 and September 2014. A total of 165 participants were included in the study.5 These were patients with PPH following cesarean delivery who had failed to respond to conventional first-line treatments (eg, uterotonics or massage and mechanical compression). The cases were treated with either UGP (99 individuals) or Bakri balloon tamponade (66 individuals), as determined by the practitioner.
Dueckelmann et al
Dueckelmann et al19 performed a single-center retrospective cohort study that included 78 women who had delivered and developed PPH that did not respond to standard first-line management (eg, uterotonics, massage, and volume replacement) and therefore received intrauterine packing from October 2016 to June 2018; 47 participants received a Celox gauze tamponade, whereas 31 received a Bakri balloon tamponade. The type of intrauterine packing used for each patient was decided by the responsible obstetrician.
Lin et al
A single-center retrospective study was conducted by Lin et al, including 162 patients who were diagnosed with placenta previa and had cesarean delivery.20 To control hemorrhage associated with placenta previa, 98 of the 162 included participants received a Bakri balloon tamponade, whereas the other 64 patients underwent UGP. The use of either Bakri balloon tamponade or UGP was decided by the attending obstetrician.
Wei et al
Wei et al21 conducted an open-label, multicenter RCT from June 2015 to December 2017. A total of 204 adult patients who were diagnosed with placenta previa, required cesarean delivery, and did not respond to conservative treatment measures (eg, uterotonics, suturing, and devascularization) across 3 hospitals in China were involved. Computer-generated random numbers were used to randomly split patients into treatment with either gauze packing or a double-balloon catheter that the study group had designed.
Ashraf et al
Ashraf et al22 conducted a single-center RCT in the department of obstetrics and gynecology of a tertiary-care hospital in Lahore. The study included 212 female patients with primary PPH following vaginal delivery who did not respond to conventional medical management. Patients were randomly divided into 2 groups: group A, in which patients were managed with condom balloon tamponade, and group B, in which uterovaginal packing was applied using roll gauze and epipad to manage the bleeding.
Primary outcomes
Blood loss
We assessed intraoperative and postoperative estimated blood loss (mL) and the number of patients with PPH <1000 mL and >1000 mL. Guo et al5 and Wei et al21 reported PPH <1000 and >1000 mL. Wei et al21 and Lin et al20 reported intraoperative and postoperative blood loss. Dueckelmann et al19 only reported postoperative blood loss.
Minor postpartum hemorrhage <1000 mL
PPH <1000 mL was reported in 2 studies enrolling 369 patients (Figure 2). No statistically significant difference was observed in the OR analyses between IUBT and UGP (OR, 2.16; 95% CI, 0.72–6.49; P=.02). A high level of heterogeneity was found among the studies (I2=83%; P=.02).
Figure 2.
Forest plot of IUBT vs UGP—PPH <1000 mL
Quantitative analysis showing the odds ratio in PPH <1000 mL reported by Guo et al5 and Wei et al.21
CI, confidence interval; IUBT, intrauterine balloon tamponade; M-H, Mantel-Haenszel; PPH, postpartum hemorrhage; UGP, uterine gauze packing.
Abul. Safety and efficacy of intrauterine balloon tamponade vs uterine gauze packing in managing postpartum hemorrhage. Am J Obstet Gynecol Glob Rep 2022.
Major postpartum hemorrhage >1000 mL
PPH >1000 mL was reported in 2 studies enrolling 369 patients (Figure 3). No statistically significant difference was observed in the OR analyses between IUBT and UGP (OR, 0.46; 95% CI, 0.15–1.39; P=.17). A high level of heterogeneity was found among the studies (I2=83%; P=.02).
Figure 3.
Forest plot of IUBT vs UGP—PPH >1000 mL
Reported by Guo et al5 and Wei et al.21
CI, confidence interval; IUBT, intrauterine balloon tamponade; M-H, Mantel-Haenszel; PPH, postpartum hemorrhage; UGP, uterine gauze packing.
Abul. Safety and efficacy of intrauterine balloon tamponade vs uterine gauze packing in managing postpartum hemorrhage. Am J Obstet Gynecol Glob Rep 2022.
Intraoperative estimated blood loss (mL)
Intraoperative blood loss was quantitatively assessed in 2 studies enrolling 374 patients (Figure 4). A statistically significant difference was observed in the MD analysis between IUBT and UGP (P<.0001), with a much lower overall bleeding observed in IUBT. A low level of heterogeneity was observed among the studies (I2=0%; P=.34).
Figure 4.
Forest plot of IUBT vs UGP—intraoperative blood loss (mL)
Reported by Ashraf et al22 and Lin et al.20
CI, confidence interval; IUBT, intrauterine balloon tamponade; IV, inverse variance; SD, standard deviation; UGP, uterine gauze packing.
Abul. Safety and efficacy of intrauterine balloon tamponade vs uterine gauze packing in managing postpartum hemorrhage. Am J Obstet Gynecol Glob Rep 2022.
Wei et al21 also reported intraoperative bleeding; however, it could not be quantitatively measured because the study used median and range variables. No significant difference was observed between IUBT and UGP (P=.39), but intraoperative bleeding was higher in the UGP group.
Postoperative estimated blood loss
Postoperative estimated blood loss (in mililiters) was reported in 3 studies enrolling 444 patients. Quantitative analysis was not possible because 1 of the studies (Lin et al20) reported MD and standard deviation, whereas the other 2 (Wei et al21 and Dueckelmann et al19) reported median and range. Lin et al20 and Dueckelmann et al19 both reported an insignificant difference in postoperative bleeding (P=.510 and P=.225, respectively), whereas Wei et al21 reported a significant difference (P<.01) favoring IUBT over UGP.
Success rates
We assessed success rates as the number of successful operations (in percentage) without the need for any additional interventions such as hysterectomy or uterine artery embolization. Maternal mortality was denoted as women who died in the puerperium. Both Guo et al5 and Wei et al21 reported the 2 outcomes.
In Figure 5, the number of successful operations was reported in 2 studies enrolling 369 patients. No statistically significant difference was observed in the OR analyses between IUBT and UGP (OR, 0.97; 95% CI, 0.48–2.00; P=.94). A low level of heterogeneity was found among the studies (I2=0%; P=.42).
Figure 5.
Forest plot of IUBT vs UGP—primary success
Reported by Guo et al5 and Wei et al.21
CI, confidence interval; IUBT, intrauterine balloon tamponade; M-H, Mantel-Haenszel; UGP, uterine gauze packing.
Abul. Safety and efficacy of intrauterine balloon tamponade vs uterine gauze packing in managing postpartum hemorrhage. Am J Obstet Gynecol Glob Rep 2022.
Maternal mortality
Maternal mortality was observed in 2 studies enrolling 369 patients (Figure 6). No statistically significant difference was observed in the OR analyses between IUBT and UGP (OR, 0.69; 95% CI, 0.18–2.65; P=.58). A high level of heterogeneity was found among the studies (I2=79%; P=.03).
Figure 6.
Forest plot of IUBT vs UGP—maternal mortality
Reported by Guo et al5 and Wei et al.21
CI, confidence interval; IUBT, intrauterine balloon tamponade; M-H, Mantel-Haenszel; UGP, uterine gauze packing.
Abul. Safety and efficacy of intrauterine balloon tamponade vs uterine gauze packing in managing postpartum hemorrhage. Am J Obstet Gynecol Glob Rep 2022.
Secondary outcomes
Requiring secondary intervention
We assessed the effect of other secondary interventions including hysterectomy, uterine artery embolization and B-Lynch sutures. These outcomes were reported in all included studies apart from Ashraf et al,22 enrolling a total of 609 patients.
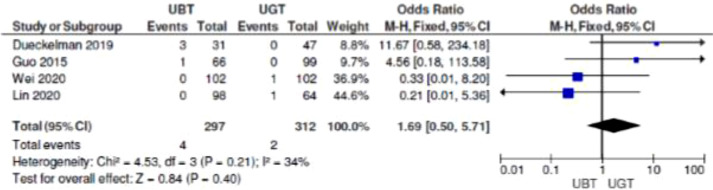
Hysterectomy
Figure 7 shows the need for hysterectomy following the IUBT or UGP procedures. No statistically significant difference was observed in the OR analyses between IUBT and UGP (OR, 1.69; 95% CI, 0.50–5.71; P=.40). A moderate level of heterogeneity was found among the studies (I2=34%; P=.21).
Figure 7.
Forest plot of IUBT vs UGP—requiring hysterectomy
Reported by Guo et al,5 Wei et al,21 Lin et al,20 and Dueckelmann et al.19
CI, confidence interval; IUBT, intrauterine balloon tamponade; M-H, Mantel-Haenszel; UGP, uterine gauze packing.
Abul. Safety and efficacy of intrauterine balloon tamponade vs uterine gauze packing in managing postpartum hemorrhage. Am J Obstet Gynecol Glob Rep 2022.
Uterine artery embolization and B-Lynch sutures
Figure 8 shows the need for uterine artery embolization following IUBT or UGP procedures and the use of B-Lynch sutures. In terms of embolization, no statistically significant difference was observed in the OR analyses between IUBT and UGP (OR, 1.17; 95% CI, 0.55–2.49; P=.68). With regard to the use of B-Lynch sutures, no statistically significant difference was observed in the OR analyses between the IUBT and UGP groups (OR, 2.27; 95% CI, 0.4–12.84; P=.35). The heterogeneity for the use of embolization and B-Lynch sutures was overall low among the studies that reported these outcomes (I2=0%; P=.93).
Figure 8.
Forest plot of IUBT vs UGP—requiring UAE and B-Lynch sutures
Requiring UAE was reported by Guo et al,5 Dueckelmann et al,19 Lin et al,20 and Wei et al.21 Requiring B-Lynch sutures was reported by Dueckelmann et al19 and Lin et al.20
CI, confidence interval; IUBT, intrauterine balloon tamponade; M-H, Mantel-Haenszel; UAE, uterine artery embolization; UGP, uterine gauze packing.
Abul. Safety and efficacy of intrauterine balloon tamponade vs uterine gauze packing in managing postpartum hemorrhage. Am J Obstet Gynecol Glob Rep 2022.
Intensive care unit admission
Three studies reported ICU admissions (Dueckelmann et al,19 Lin et al,20 and Wei et al21), all of which found no significant differences for the number of ICU admissions between the 2 groups.
Operative time
According to Lin et al,20 there was a significant difference (P=.023) in the length of the operation favoring IUBT over UGP (97.8±17.7 vs 108.2±16.9 minutes). In contrast, Wei et al21 reported a similar operative time for IUBT and UGP.
Length of stay in hospital
Two studies reported the length of hospital stays. According to Wei et al,21 a shorter post–cesarean-delivery hospital stay was found in the double-balloon catheter group (4 days) compared with the gauze group (5 days). Similarly, a shorter hospital stay was reported by Lin et al20 (P=.020) for the Bakri balloon tamponade, with a mean of 3.79±0.89 days as opposed to the mean of 4.12±0.85 days in the UGP group.
Postoperative hemoglobin
According to Lin et al,20 there was no significant difference in postoperative hemoglobin between the 2 groups, with a mean of 8.5±1.4 g/dL for the Bakri balloon tamponade group and 8.1±1.3 g/dL for the UGP group. Wei et al21 also reported no significant difference between the 2 groups, with the catheter and gauze groups having mean hemoglobin levels of 102.8±15.8 g/L and 97.5±15 g/L, respectively.
Blood transfusion
The number of transfusions was reported in 2 studies. Lin et al20 showed a significant difference (P=.06) favoring the IUBT group, in which only 9 patients required a transfusion, as opposed to the 17 patients who required it in the UGP group. Conversely, Wei et al21 reported minimal differences in the number of patients requiring either red blood cell (17 vs 16) or allogeneic (37 vs 36) transfusions for IUBT and UGP, respectively.
Discussion
IUBT showed a better effect when compared with UGP in terms of managing intraoperative blood loss shown by the results of the analyses. Intraoperative blood loss (in mililiters) showed an MD of −69.78, demonstrating a significant (P<.0001) improvement in the IUBT group compared with controls (Figure 4). Conversely, there were no significant differences in all the other outcomes (P>.05). There was a variable range of heterogeneity (from low to high) for all outcomes.
In addition to the outcomes mentioned above, the findings of this study regarding many secondary outcomes demonstrated higher effectiveness of IUBT relative to UGP. IUBT overall was found to have shorter operative time and length of hospital stay. In addition, IUBT patients were less likely to require blood transfusions in cases of PPH. However, there was no notable difference in terms of ICU admissions, postoperative hemoglobin levels, and need for secondary interventions such as hysterectomy and uterine artery embolization.
Although current guidelines favor IUBT over UGP, the literature comparing these interventions is limited, and the superiority of one intervention over the other is still debatable. This study has considered the best evidence available comparing the effectiveness of IUBT and UGP as surgical interventions for managing PPH. It is certain that both interventions are safe and efficacious when managing PPH. This analysis suggests the likelihood that the 2 interventions are equally effective given that significant differences were not observed in most outcomes. Notwithstanding, it is clear from our analysis that IUBT is significantly superior to UGP in reducing intraoperative blood loss. Consequently, this meta-analysis suggests no change in practice and supports the guidelines recommending IUBT as the first-line intervention to implement in cases where pharmacologic agents fail to control PPH. This is in keeping with the recommendation of IUBT over UGP by Ashraf et al,22 Lin et al,20 and Wei et al.21 Studies directly comparing the 2 interventions are sparse, which is why more RCTs and clinical trials are required to draw better conclusions and improve the reliability of the evidence.
Table 2.
Assessment of risk of bias of the randomized trials using the Cochrane Collaboration tool
| First author (y) | Bias | Authors’ judgment | Support for judgment |
|---|---|---|---|
| Wei et al,21 (2020) | Random sequence generation (selection bias) | Low risk | Randomization achieved using computer-generated codes. |
| Allocation concealment (selection bias) | Low risk | Allocation sealed in envelope by statistician; all surgeons were blinded. Allocation of tamponade method revealed by nurse immediately before operation. | |
| Blinding of participants and personnel (performance bias) | High risk |
Open-label study. |
|
| Blinding of outcome assessment (detection bias) | Unclear risk |
No information given. |
|
| Incomplete outcome data (attrition bias) | Low risk | No missing outcome data. | |
| Selective reporting (reporting bias) | Low risk | Prespecified primary outcomes reported. | |
| Other bias | Low risk | Similar baseline characteristics in both groups. |
|
| Ashraf et al,22 (2018) | Random sequence generation (selection bias) | Low risk | Participants were randomly assigned using a lottery method. |
| Allocation concealment (selection bias) | Unclear | No information given. | |
| Blinding of participants and personnel (performance bias) | Unclear | No information given. | |
| Blinding of outcome assessment (detection bias) | Unclear | No information given. |
Abul. Safety and efficacy of intrauterine balloon tamponade vs uterine gauze packing in managing postpartum hemorrhage. Am J Obstet Gynecol Glob Rep 2022.
Table 1.
Characteristics of the studies included in this systematic review and meta-analysis
| Study (y) | Country and journal | Single/multicenter | Population (cause of bleeding) | Type of intervention | Study design | Age (include mean+SD or median+range) | Previous cesarean delivery | Total sample size (n) | Intervention group—intrauterine balloon tamponade | Control group—UGP |
|---|---|---|---|---|---|---|---|---|---|---|
| Guo et al,5 (2015) | China: International Journal of Clinical and Experimental Medicine | Single | Cesarean delivery | Bakri balloon tamponade vs UGP (sterile cotton gauze) | Retrospective cohort | NR | NR | 165 | 66 | 99 |
| Dueckelman et al19 (2019) | Germany: European Journal of Obstetrics & Gynecology and Reproductive Biology | Single | Postpartum hemorrhage | Bakri balloon tamponade vs UGP (Celox chitosan gauze) | Retrospective cohort | 33.7 (±6.6) vs 31.4 (±5.9) | NR | 78 | 31 | 47 |
| Lin et al,20 (2020) | China: Journal of International Medical Research | Single | Placenta previa, underwent cesarean delivery | Bakri balloon tamponade vs UGP | Retrospective comparative study | 33.09±4.55 vs 33.34±4.75 | 40 vs 25 | 162 | 98 | 64 |
| Wei et al,21 (2020) | China: Medicine | Multicenter | Placenta previa | Double balloon tamponade vs UGP | Randomized controlled trial | 31.1±4.9 vs 32.2±4.8 | 21 vs 18 | 204 | 102 | 102 |
| Ashraf et al, 22 (2018) |
Pakistan: Annals of King Edward Medical University |
Single | Postpartum hemorrhage | Balloon (condom) tamponade vs UGP |
Randomized controlled trial | 29.22±6.52 vs 29.05±6.802 |
NR | 212 |
106 |
106 |
NR, not reported; SD, standard deviation; UGP, uterine gauze packing.
Abul. Safety and efficacy of intrauterine balloon tamponade vs uterine gauze packing in managing postpartum hemorrhage. Am J Obstet Gynecol Glob Rep 2022.
Table 3.
Assessment of quality of nonrandomized studies with the Newcastle–Ottawa scalea
| Study (y) | Selection | Comparability | Exposure |
|---|---|---|---|
| Dueckelmann et al,19 (2019) | **** | * | *** |
| Lin et al,20 (2020) | **** | * | * |
| Guo et al,5 (2015) | **** | * | ** |
The Newcastle–Ottawa scale, which applies a star grading system for analysis, was used to assess the quality of the 3 nonrandomized studies.
Abul. Safety and efficacy of intrauterine balloon tamponade vs uterine gauze packing in managing postpartum hemorrhage. Am J Obstet Gynecol Glob Rep 2022.
In this meta-analysis, findings from relevant studies were summarized, and the risk of bias was assessed for each of the included studies. The study designs were standardized, and the inclusion and exclusion criteria predefined. Though both interventions share a similar mechanism by which PPH is controlled, this had no effect on results subsequently. Five studies were included with a sample size of 821 enrolled patients. Two of the 5 included trials were RCTs and 3 were not randomized. The Newcastle–Ottawa scale was used to assess the quality of the nonrandomized studies. Thus, the findings of this meta-analysis were based on the best available evidence. However, the inherent limitations of this study must be taken into account when studying the reported outcomes. Only 5 studies were included, and 3 of them were retrospective, meaning that patients were not randomized and there was a higher risk of selection bias. Although 821 patients were included in the study, this may not be considered sufficient to draw definite conclusions. In addition, variables such as the skill level of staff performing these interventions may have affected the outcomes. Furthermore, mode of delivery (ie, cesarean or vaginal delivery) is a confounding factor that has not been accounted for in this meta-analysis. Ashraf et al22 included patients undergoing vaginal delivery in contrast to all other studies, which included cesarean deliveries.
Conclusions
Although the evidence is limited, with only 5 studies comparing IUBT and UGP, the results of this meta-analysis suggest that IUBT is superior in minimizing intraoperative bleeding compared with UGP alone in women with primary PPH while also not increasing the likelihood of adverse events such as ICU admissions. The authors suggest that further RCTs to be performed to support these findings.
Footnotes
The authors report no conflict of interest.
The authors report no funding for this study.
Patient consent was not required because no personal information or details were included.
Cite this article as: Abul A, Al-Naseem A, Althuwaini A, et al. Safety and efficacy of intrauterine balloon tamponade vs uterine gauze packing in managing postpartum hemorrhage: a systematic review and meta-analysis. Am J Obstet Gynecol Glob Rep 2022;XX:x.ex–x.ex.
References
- 1.Selo-Ojeme DO. Primary postpartum haemorrhage. J Obstet Gynaecol. 2002;22:463–469. doi: 10.1080/0144361021000003555. [DOI] [PubMed] [Google Scholar]
- 2.Hibbard BM, Anderson MM, Drife JO, et al. HMSO; London: 1996. Report on confidential enquiries into maternal deaths in the United Kingdom; pp. 1991–1993. [Google Scholar]
- 3.Ge J, Liao H, Duan L, Wei Q, Zeng W. Uterine packing during cesarean section in the management of intractable hemorrhage in central placenta previa. Arch Gynecol Obstet. 2012;285:285–289. doi: 10.1007/s00404-011-1935-5. [DOI] [PubMed] [Google Scholar]
- 4.Bagga R, Jain V, Kalra J, Chopra S, Gopalan S. Uterovaginal packing with rolled gauze in postpartum hemorrhage. MedGenMed. 2004;6:50. [PMC free article] [PubMed] [Google Scholar]
- 5.Guo YN, Ma J, Wang XJ, Wang BS. Does uterine gauze packing increase the risk of puerperal morbidity in the management of postpartum hemorrhage during caesarean section: a retrospective cohort study. Int J Clin Exp Med. 2015;8:13740–13747. [PMC free article] [PubMed] [Google Scholar]
- 6.Hsu S, Rodgers B, Lele A, Yeh J. Use of packing in obstetric hemorrhage of uterine origin. J Reprod Med. 2003;48:69–71. [PubMed] [Google Scholar]
- 7.Revert M, Rozenberg P, Cottenet J, Quantin C. Intrauterine balloon tamponade for severe postpartum hemorrhage. Obstet Gynecol. 2018;131:143–149. doi: 10.1097/AOG.0000000000002405. [DOI] [PubMed] [Google Scholar]
- 8.Laas E, Bui C, Popowski T, Mbaku OM, Rozenberg P. Trends in the rate of invasive procedures after the addition of the intrauterine tamponade test to a protocol for management of severe postpartum hemorrhage. Am J Obstet Gynecol. 2012;207:281. doi: 10.1016/j.ajog.2012.08.028. e1–7. [DOI] [PubMed] [Google Scholar]
- 9.Revert M, Cottenet J, Raynal P, Cibot E, Quantin C, Rozenberg P. Intrauterine balloon tamponade for management of severe postpartum haemorrhage in a perinatal network: a prospective cohort study. BJOG. 2017;124:1255–1262. doi: 10.1111/1471-0528.14382. [DOI] [PubMed] [Google Scholar]
- 10.Bakri Y, B-Lynch C, Alouini S. Second generation of intrauterine balloon tamponade: new perspective. BMJ Innov. 2020;6:1–3. doi: 10.1136/bmjinnov-2019-000404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Suarez S, Conde-Agudelo A, Borovac-Pinheiro A, et al. Uterine balloon tamponade for the treatment of postpartum hemorrhage: a systematic review and meta-analysis. Am J Obstet Gynecol. 2020;222:293. doi: 10.1016/j.ajog.2019.11.1287. e1–52. [DOI] [PubMed] [Google Scholar]
- 12.Arulkumaran S, Mavrides E, Penney GC. Prevention and management of postpartum haemorrhage. Royal College of Obstetricians and Gynaecologists Green-top Guideline. 2009;52 [Google Scholar]
- 13.Kellie FJ, Wandabwa JN, Mousa HA, Weeks AD. Mechanical and surgical interventions for treating primary postpartum haemorrhage. Cochrane Database Syst Rev. 2020;7 doi: 10.1002/14651858.CD013663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moher D, Liberati A, Tetzlaff J, Altman DG, Group PRISMA. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. Ann Intern Med. 2009;151:264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 15.Li T, Higgins J. In: Cochrane Handbook for Systematic Reviews of Interventions: Cochrane. Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editors. Higgins JPT TJ; 2021. Chapter DJ 5. Collecting data. [Google Scholar]
- 16.Review Manager (RevMan) 5. 3rd ed. Copenhagen: The Nordic Cochrane Centre. The Cochrane Collaboration; 2014.
- 17.Higgins JP, Savović J, Page MJ, Elbers RG, Sterne JA. Assessing risk of bias in a randomized trial. Cochrane Handbook for Systematic Reviews of Interventions. 2019:205–228. [Google Scholar]
- 18.Wells GA, Shea B, O'Connell Da PJ, Peterson J, Welch V, Losos M, Tugwell P. Oxford; 2000. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. [Google Scholar]
- 19.Dueckelmann AM, Hinkson L, Nonnenmacher A, et al. Uterine packing with chitosan-covered gauze compared to balloon tamponade for managing postpartum hemorrhage. Eur J Obstet Gynecol Reprod Biol. 2019;240:151–155. doi: 10.1016/j.ejogrb.2019.06.003. [DOI] [PubMed] [Google Scholar]
- 20.Lin B, Zhou B, Chen J, Yang J. Prophylactic application of Bakri balloon tamponade versus uterine gauze packing during cesarean section in patients with placenta previa. J Int Med Res. 2020;48(3) doi: 10.1177/0300060520910049. 300060520910049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wei J, Dai Y, Wang Z, et al. Intrauterine double-balloon tamponade vs gauze packing in the management of placenta previa: a multicentre randomized controlled trial. Med (Baltim) 2020;99:e19221. doi: 10.1097/MD.0000000000019221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ashraf N, Ashraf A, Khursheed K. Efficacy and Safety of intrauterine balloon tamponade versus uterovaginal roll gauze packing in patient presenting with primary postpartum hemorrhage after normal vaginal delivery. Ann King Edw Med Univ. 2018;24:889–892. [Google Scholar]