Abstract
Introduction:
Self-harm presentations in children and young people have increased internationally over the last decade. The COVID-19 pandemic has the potential to worsen these trends.
Objective:
To describe trends in emergency department self-harm or suicidal ideation presentations for children and young people in New South Wales before and since the COVID-19 pandemic.
Methods:
We studied presentations for self-harm or suicidal ideation by 10- to 24-year-olds to New South Wales emergency departments, using interrupted time series analysis to compare annualised growth before COVID (2015 to February 2020) and since COVID (March 2020 to June 2021). Subgroup analyses compared age group, gender, triage category, rurality and disadvantage. Time series decomposition via generalised additive models identified long-term, seasonal and short-term trends.
Results:
Self-harm or suicidal ideation presentations by young people in New South Wales increased by 8.4% per annum pre-COVID. Growth accelerated since COVID, to 19.2% per annum, primarily due to increased presentations by females aged 13–17 years (47.1% per annum since COVID, from 290 per 10,000 in 2019 to 466 per 10,000 in 2021). Presentations in males aged 10–24 years did not increase since COVID (105.4 per 10,000 in 2019, 109.8 per 10,000 in 2021) despite growing 9.9% per annum before COVID. Presentation rates accelerated significantly in socio-economically advantaged areas. Presentations in children and adolescents were strongly linked to school semesters.
Conclusion:
Emergency department self-harm or suicidal ideation presentations by New South Wales young people grew steadily before COVID. Understanding the sustained increase remains a priority. Growth has increased since COVID particularly for adolescent females, but not among adolescent males. Surprisingly, the largest post-COVID increases in annual growth occurred in socio-economically advantaged and urban regions. The COVID-19 pandemic appears to have added new challenges, particularly in females in the developmentally critical early adolescent and teenage years.
Keywords: Self-harm, suicide, young people, COVID, emergency department
Background
Self-harm presentations in children, adolescents and young adults have increased internationally over the last decade, and the current COVID-19 pandemic may worsen these trends (Plener, 2020). Admissions to US paediatric hospitals for suicidal ideation or self-harm doubled from 2008 to 2015 as a proportion of total hospitalisations (Plemmons et al., 2018), and adolescent self-poisoning presentations to emergency departments (EDs) significantly increased from 2011 to 2018 (Spiller et al., 2020). In Ontario, Canada, ED self-harm presentations in adolescents increased by 135% from 2009 to 2017, reversing a declining trend in the previous decade (Gardner et al., 2019). These studies all found larger increases in females than in males.
Australian state-based health systems show similar trends prior to COVID-19. Paediatric mental health and self-harm presentations to Victorian EDs increased by 6.5% annually from 2008 to 2015 (Hiscock et al., 2018). In New South Wales (NSW), ED mental health presentations in 10- to 19-year-olds increased by 27% per year from 2010 to 2014 (Perera et al., 2018). Hospital admissions following self-harm in 15- to 19-year-olds increased by 43% in the decade to 2019 (Australian Institute of Health and Welfare, 2021b). In NSW, per capita self-harm hospitalisations in 10- to 19-year-olds doubled over the same period (Centre for Epidemiology and Evidence, 2021). Most studies reported higher rates and larger increases in adolescent females (Australian Institute of Health and Welfare, 2021b; Centre for Epidemiology and Evidence, 2021; Stapelberg et al., 2020).
The COVID-19 pandemic has the potential to worsen these trends by disrupting social, educational and employment opportunities while diminishing access to face-to-face healthcare (Szlyk et al., 2020). Young people appear particularly vulnerable: a meta-analysis found that younger age and female gender were associated with greater COVID-19-related increases in the prevalence of anxiety and depression (Wang et al., 2021). These effects may vary over time. In many countries, presentations by young people for depression, anxiety and self-harm in primary care, ED and hospital settings reduced in the first few months of the pandemic (Carr et al., 2021; Hawton et al., 2021; Mourouvaye et al., 2021; Ougrin et al., 2021). The US Centers for Disease Control found an initial reduction in ED visits for suicide attempts in young people, followed by a substantial later increase, including a 25–50% increase in females aged 12–17 years (Yard et al., 2021). This transient reduction early in the pandemic may reflect reduced distress due to greater social or family ‘pulling together’ at a time of crisis, or may reflect unmet need, with people avoiding acute and emergency services due to fears of exposure to infection despite increased distress (Hawton et al., 2021; Ougrin et al., 2021).
Since COVID-19, Australian population surveys show increases in psychological distress in youths (Biddle et al., 2020; Newby et al., 2020). However, population-wide data on self-harm or suicidal ideation presentations in Australian children and young people since COVID-19 have not yet been published. It is important to understand whether COVID-19 has changed pre-COVID-19 trends, and which groups or regions are most affected, to inform policy and service responses.
This study reports a time series analysis of ED self-harm or suicidal ideation presentations by people aged 10–24 years in NSW, Australia, from January 2015 to June 2021. We compare annual growth in self-harm or suicidal ideation presentation rates in the 5 years prior to the NSW COVID-19 first wave and examine changes in rates since that time.
Methods
Governance and approval
This study was conducted by NSW Ministry of Health, which is the department of state government responsible for the planning, funding, management and oversight of public hospitals, EDs and community mental health services. The study used routinely collected and aggregated administrative data.
Setting and context
The state of NSW had a population of 8.2 million people in 2020, including 2.5 million people (31%) aged 24 years or under (HealthStats NSW, 2021a). Free emergency care is provided through EDs in 174 NSW government (‘public’) hospitals (Australian Institute of Health and Welfare, 2021a).
The COVID-19 pandemic in NSW has had several phases which are likely to have affected young people in different ways. A ‘first wave’ of COVID-19 illness and restrictions occurred from mid-March to late April 2020, with encouragement of home schooling, and reduced household visiting and public social gatherings (Australian Parliamentary Library, 2021). By late April 2020, case numbers had reduced and restrictions eased. Face-to-face teaching in schools resumed from 25 May and restrictions on regional travel and children’s sport eased from 2 June 2020. Tertiary education, tourism and hospitality industries experienced continued disruption from border closures and physical distancing requirements. Additional local restrictions occurred in response to regional outbreaks from July to August 2020 and following an outbreak in Sydney’s Northern Beaches (December 2020 to January 2021). An outbreak of the COVID-19 delta variant commenced in July 2021, after the end of this study period.
Government financial supports during COVID-19 included measures aimed at young people and families. These included supplementary payments to Jobseeker, Parenting Payment, Youth Allowance and Study Allowance recipients; additional payments to households receiving income support; Jobkeeper payments to support retention of affected employees and subsidisation of private telehealth mental health services.
Data sources
Data were obtained from the NSW Emergency Department Data Collection (EDDC), via the NSW Health Information Exchange. The EDDC includes demographic information, dates and times of care, urgency (triage) codes, unstructured text indicating the presenting problem for the visit and diagnostic or problem codes recorded in Systemized Nomenclature of Medicine (SNOMED) terminology (SNOMED International, 2019).
Inclusion and exclusion criteria
We included presentations for self-harm or suicidal ideation by people aged 10–24 years to any NSW ED with an arrival date between 1 January 2015 and 30 June 2021. Children aged under 10 years were excluded because of difficulty distinguishing deliberate from accidental self-harm in the data sources used. Scheduled ED visits such as for dressings or follow-up care were also excluded.
Data were missing for some NSW EDs during the study period. Twenty-eight small rural EDs, comprising 1.6% of NSW ED activity, did not provide data to the NSW EDDC data collection in 2015. ED data were not available for the Northern Beaches Hospital (NBH), which took over ED functions from Manly and Mona Vale Hospitals in late 2018. Therefore, presentations to Manly and Mona Vale Hospitals were excluded from the numerator for time series analyses and rate calculations. Catchment populations for those hospitals (the socio-economically advantaged urban regions of Manly, Warringah and Pittwater) were excluded from the denominator for population rate calculations. This excluded approximately 84,000 people aged 24 years and under.
Identification of self-harm or suicidal ideation presentations
We identified presentations to NSW EDs with either suicidal ideation or self-harm. These were treated as a single category because (1) both are significantly and equally associated with suicide (Large et al., 2020), (2) both indicate a need for mental health assessment and follow-up care and are therefore relevant to health system planning and (3) distinguishing suicidal from non-suicidal self-harm requires detailed clinical assessment and is unlikely to be reliably measured using routine administrative data. NSW Health uses an enhanced method for routine reporting of self-harm or suicidal ideation presentations because ED diagnosis codes alone have low sensitivity for detecting suicidal thoughts or behaviours (Stanley et al., 2018; Sveticic et al., 2020). SNOMED terms were first converted to International Classification of Diseases, Version 10 (ICD-10) codes, using mapping tables provided by the Australian Digital Health Agency and augmented by NSW Health with additional codes identifying self-harm. Presentations for self-harm or suicidal ideation were identified by an algorithm which searches ED diagnosis codes and presenting problem-free text for any of the following: (1) standard self-harm ICD-10 codes (X60–X84, Y87.0, R45.81), (2) additional diagnostic codes for poisoning by specific substances often used in deliberate self-harm (paracetamol, sedatives, antidepressants) and (3) regular expressions such as ‘self-harm’, ‘suicidal’ or ‘overdose’. If codes or text for both self-harm (e.g. overdose, poisoning) and suicidal ideation are present, then self-harm was coded. The ICD-10 codes and text phrases used are listed as a Supplemental File.
Outcomes and predictors
The primary outcome was the annualised rate of ED presentations for self-harm or suicidal ideation per 10,000 age-specific population, calculated overall and for the subgroups described below. Age, sex and Aboriginal and/or Torres Strait Islander status were obtained for each presentation. Age groups (children 10–12, adolescents 13–17 and young adults 18–24 years) were defined based on NSW Health clinical service organisation and reporting standards. Residential postcodes were mapped to Australian Bureau of Statistics (ABS) standard geography for Statistical Area Level 3 (SA3). The ABS Index of Relative Socio-economic Disadvantage (IRSD) and rurality index (ARIA) were obtained for the person’s SA3 of residence (ABS, 2018a, 2018b).
Statistical analysis
Interrupted time series analysis was used to compare trends before and since COVID-19. The interruption point was defined as 1 March 2020, to include the month in which COVID-19-related public health measures commenced. Time segments for the analysis were defined as ‘pre-COVID-19’ (January 2015 to February 2020) and ‘COVID-19’ (March 2020 to June 2021).
Analysis used segmented ordinary least squares regression with Newey–West standard errors to correct for autocorrelation between time periods, and the possibility of systematic changes in variance between time periods or groups (heteroscedasticity). A lag of 12 months, corresponding to an annual cycle, was defined. A log-linear regression model was specified as: log(ratei) = β0 + β1pre_trendi + β2covid_change + εi, where i denotes the weekly time period, rate is the number of admissions divided by the group or subgroup population, pre_trend is the pre-COVID trend and covid_change represents the change in trend after the interruption. β1 and β2 were added to calculate the COVID trend (β3). A ‘level change’ term (an immediate increase/decrease in the rate level following the interruption) was tested for inclusion but found to be non-significant. The use of a log transformation in the above model permits the results to be expressed as relative growth rates, which are presented as annualised figures. The same method was applied to overall age and gender groups, and in subgroup analyses comparing urgency (triage) categories, Aboriginal status, socio-economic quintiles and remoteness categories.
Time series decomposition was used to distinguish between long-term, seasonal and short-term trends, using generalised additive models (GAM) with a negative binomial distribution (Hastie and Tibshirani, 1986; Wood, 2017). This model separated rates of daily ED presentations into four components: (1) an overall time trend from 1 January 2015 to 30 June 2021; (2) a weekly cycle; (3) an annual cycle; and (4) the possible impact of initial public health restrictions between 16 March 2020 and 31 May 2020. A GAM model provides a flexible framework to relax the linearity assumptions between the outcome variable and covariates and provides graphical representations of change over time and within a year. A cyclic cubic spline was applied to the annual cycle and a cubic regression spline to other periods.
Interrupted time series analyses were conducted in SAS version 9.4 (SAS Institute, North Carolina, USA). Time series decompositions were implemented with mgcv (v1.8-36) (Wood, 2011) package for R statistical software, version 4.1.0. Trend changes since COVID were considered statistically significant if p values were less than 0.05.
Results
Over the 7 years to 2021, self-harm and suicidal ideation presentations to NSW EDs by people aged 10–24 years increased from 107 to 187 presentations per 10,000 population per year (Table 1). Rates were increasing by 8.4% per annum (pa) (95% confidence interval [CI] = [7.2%, 9.6%]) prior to COVID-19, and accelerated significantly since COVID-19, growing at an annualised rate of 19.2% (95% CI = [14.2%, 24.5%]) from March 2020 to June 2021.
Table 1.
Rates of self-harm or suicidal ideation presentation by age and gender in NSW before COVID and since COVID first wave.
| Annual rate (presentations per 10,000 per year) | Average annual change (percent per year) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | 2021 | Pre-COVID | Since COVID | p value | |
| Persons | ||||||||||
| All ages (10–24 years) | 106.6 | 118.6 | 130.4 | 138.7 | 147.8 | 168.0 | 186.5 | 8.4% (7.2%, 9.6%) | 19.2% (14.2%, 24.5%) | 0.0003*** |
| 10–12 years | 17.5 | 16.4 | 22.4 | 26.2 | 30.2 | 34.2 | 37.8 | 17.0% (12.0%, 22.2%) | 25.4% (6.5%, 47.8%) | 0.4852 |
| 13–17 years | 143.5 | 159.8 | 187.8 | 193.9 | 200.6 | 251.2 | 293.0 | 9.3% (7.4%, 11.3%) | 34.4% (23.5%, 46.2%) | <0.0001*** |
| 18–24 years | 117.0 | 131.8 | 136.9 | 149.4 | 162.4 | 171.7 | 181.7 | 8.0% (6.8%, 9.1%) | 6.7% (3.5%, 10.1%) | 0.5664 |
| Males | ||||||||||
| All ages (10–24 years) | 71.6 | 82.0 | 88.7 | 100.6 | 105.4 | 111.0 | 109.8 | 9.9% (8.4%, 11.4%) | −2.1% (−7.2%, 3.3%) | 0.0005** |
| 10–12 years | 12.0 | 13.3 | 19.2 | 22.2 | 24.1 | 25.9 | 27.1 | 19.1% (15.2%, 23.0%) | 4.7% (−10.0%, 21.9%) | 0.1394 |
| 13–17 years | 70.7 | 80.4 | 93.7 | 108.2 | 115.2 | 132.9 | 128.7 | 13.9% (11.9%, 16.0%) | 4.0% (−5.1%, 13.9%) | 0.0836 |
| 18–24 years | 94.9 | 109.5 | 112.7 | 126.9 | 131.5 | 132.3 | 132.1 | 7.7% (6.1%, 9.4%) | −5.2% (−9.8%, −0.4%) | <0.0001*** |
| Females | ||||||||||
| All ages (10–24 years) | 143.4 | 157.1 | 174.2 | 178.9 | 192.4 | 228.0 | 266.9 | 7.6% (6.5%, 8.8%) | 31.7% (25.7%, 38.0%) | <0.0001*** |
| 10–12 years | 23.4 | 19.8 | 25.8 | 30.5 | 36.5 | 42.9 | 49.1 | 15.1% (9.4%, 21.1%) | 48.5% (22.3%, 80.4%) | 0.0330* |
| 13–17 years | 220.4 | 243.5 | 287.1 | 284.6 | 290.1 | 376.1 | 466.1 | 7.7% (5.6%, 9.9%) | 47.1% (34.3%, 61.2%) | <0.0001*** |
| 18–24 years | 140.1 | 155.1 | 162.1 | 173.2 | 195.1 | 212.8 | 233.4 | 8.2% (7.1%, 9.3%) | 15.4% (11.1%, 19.8%) | 0.0052* |
ED: emergency department; NSW: New South Wales.
Average annual per capita rate of ED self-harm or suicidal ideation presentation by age and gender and change in annualised growth rate before and since COVID-19.
p < 0.05, **p < 0.005, ***p < 0.0005.
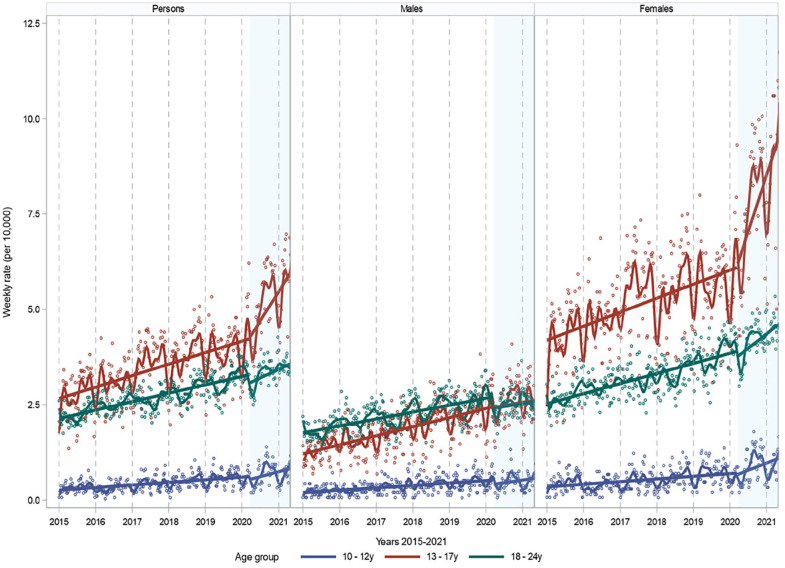
Patterns differed by age and gender (Table 1; Figure 1). Before COVID-19, self-harm or suicidal ideation presentation rates in females aged 10–24 years were nearly twice that of young males of the same age. The highest rate overall was in females aged 13–17 years (290 presentations per 10,000 population in 2019), while for males, rates were highest in the 18- to 24-year age group (131 per 10,000 in 2019). From 2015 to early 2020, self-harm or suicidal ideation presentations grew by 9.9% pa in males and 7.6% pa in females. For young females (10–24 years), growth in presentation rates accelerated since COVID-19, to 31.7% pa (95% CI = [25.7%, 38.0%]). Adolescent girls aged 13–17 years contributed most of this increase, with rates growing by 47.1% pa (95% CI = [34.3%, 61.2%]) to 466 per 10,000 in 2021. By contrast, in males aged 10–24 years per capita, there was no significant growth in presentations during the COVID-19 period (−2.1% pa, 95% CI = [−7.2%, 3.3%]). This represented a significant deceleration when compared to the pre-COVID annual growth trend. In males aged 18–24 years, presentation rates declined significantly during the COVID-19 period (−5.2% pa, 95% CI = [−9.8%, −0.4%]).
Figure 1.
Growth in self-harm or suicidal ideation presentation rates before COVID and since COVID-19 first wave in NSW.
Interrupted time series analysis showing weekly emergency department self-harm or suicidal ideation presentation rates (per 10,000) and linear trends before and since COVID-19 in people aged 10–24 years in NSW, January 2015 to June 2021. Spline curve included for visualisation.
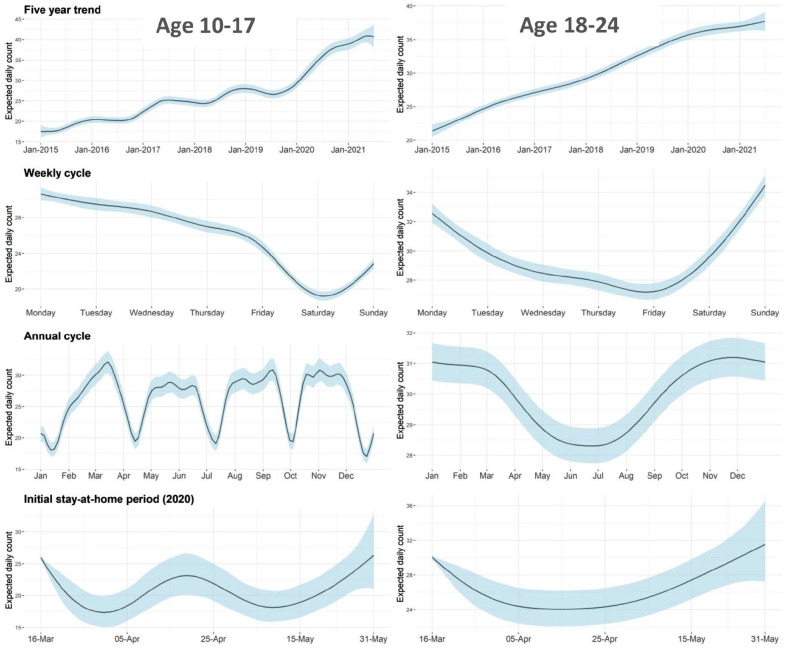
Time series decomposition demonstrated distinct within-week and within-year cycles in self-harm presentations (Figure 2). These patterns differed for children and adolescents (10–17 years) compared with young adults (18–24 years). Baseline rates increased in both age groups over the study period. For children and adolescents, presentation rates peaked on Mondays and declined during the week to a low on Saturdays. This school week pattern overlaid an annual cycle, with lower rates during school holidays (particularly summer) relative to school terms. For young adults, presentation rates peaked on Sundays and declined during the week. In this group, the annual cycle was seasonal, peaking in late spring (September to November) and summer (December to February), and falling in late autumn (March to May) and early winter (June to July). In both age bands, after allowing for underlying trend and seasonal patterns, there was a decline in self-harm presentations during initial public health restrictions.
Figure 2.
Age-related cycles in self-harm or suicidal ideation presentations to emergency departments.
Time series decomposition using the generalised additive model showing the partial effects of trends, weekly cycles, annual cycles and the initial public health restrictions on daily self-harm or suicidal ideation ED presentations in young people aged 10–17 and 18–24 years. Shaded areas indicate 95% confidence intervals.
Prior to COVID-19, there were roughly equal rates of presentation for self-harm and suicidal thoughts (Table 2). Presentations for suicidal thoughts had been growing at a faster annual rate (12.4% pa, 95% CI = [10.6%, 14.3%]) than presentations for self-harm (4.6% pa, 95% CI = [3.7%, 5.6%]). Since COVID, the growth rate increased in both groups; however, compared to the pre-COVID baseline, the acceleration was statistically significant only for self-harm presentations.
Table 2.
Rates of self-harm or suicidal ideation presentation in NSW before and since COVID first wave: subgroup analysis.
| Annual rate (per 10,000 per year) | Average annual change (percent per year) | ||||
|---|---|---|---|---|---|
| 2015–2019 | 2020–2021 | Pre-COVID | Since COVID | p value | |
| Measure | |||||
| Self-harm | 69.98 | 72.77 | 4.6% (3.7%, 5.6%) | 14.0% (9.1%, 19.0%) | 0.0010** |
| Suicidal ideation | 68.77 | 86.85 | 12.4% (10.6%, 14.3%) | 21.1% (13.6%, 29.0%) | 0.0566 |
| Triage | |||||
| Resuscitation | 1.76 | 2.08 | 15.6% (10.8%, 20.5%) | −9.0% (−27.3%, 13.9%) | 0.0672 |
| Emergency | 32.25 | 40.61 | 10.7% (9.6%, 11.8%) | 23.3% (16.8%, 30.1%) | 0.0003*** |
| Urgent | 78.42 | 86.09 | 8.0% (6.1%, 9.9%) | 14.1% (7.1%, 21.6%) | 0.1700 |
| Semi-urgent | 25.13 | 29.40 | 6.5% (5.0%, 8.1%) | 24.0% (12.8%, 36.4%) | 0.0028** |
| Non-urgent | 1.07 | 1.11 | −3.5% (−7.2%, 0.4%) | 51.4% (24.8%, 83.7%) | 0.0001*** |
| Aboriginal status | |||||
| Aboriginal | 366.57 | 522.96 | 18.1% (16.5%, 19.8%) | 18.6% (10.9%, 26.8%) | 0.9251 |
| Not Aboriginal | 126.28 | 143.17 | 8.6% (6.8%, 10.5%) | 15.3% (7.6%, 23.6%) | 0.1645 |
| Rurality (ARIA) | |||||
| Major city | 116.54 | 135.09 | 8.4% (7.3%, 9.4%) | 18.3% (10.6%, 26.6%) | 0.0185* |
| Inner regional | 166.27 | 192.65 | 9.6% (8.5%, 10.7%) | 16.0% (10.6%, 21.8%) | 0.0508 |
| Outer regional | 216.44 | 236.86 | 6.4% (3.5%, 9.3%) | 19.2% (10.9%, 28.1%) | 0.0177* |
| Remote | 160.11 | 239.60 | 13.3% (9.0%, 17.8%) | 61.0% (36.5%, 89.8%) | 0.0004*** |
| Disadvantage (IRSD) | |||||
| Most disadvantaged | 125.33 | 136.76 | 6.4% (4.4%, 8.4%) | 18.4% (8.1%, 29.7%) | 0.0469* |
| Second most disadvantaged | 171.25 | 189.49 | 8.4% (6.6%, 10.4%) | 9.7% (2.0%, 18.0%) | 0.7836 |
| Middle | 178.15 | 217.29 | 10.0% (9.5%, 10.6%) | 21.4% (17.5%, 25.5%) | <0.0001*** |
| Second least disadvantaged | 111.21 | 126.57 | 7.4% (6.3%, 8.5%) | 20.2% (15.1%, 25.5%) | <0.0001*** |
| Least disadvantaged | 102.28 | 125.47 | 10.1% (8.5%, 11.6%) | 25.3% (16.7%, 34.6%) | 0.0013** |
IRSD: Index of Relative Socio-economic Disadvantage; ARIA: rurality index; NSW: New South Wales.
Subgroup analysis, self-harm or suicidal ideation presentations to NSW emergency departments in people aged 10–24 years, January 2015 to June 2021. Presentation rate (per 10,000 population per year) and annualised rate of change before COVID (pre-March 2020) and since COVID (March 2020 to June 2021). Rurality and disadvantage measures (IRSD) based on person’s area of residence.
p < 0.05, **p < 0.005, ***p < 0.0005.
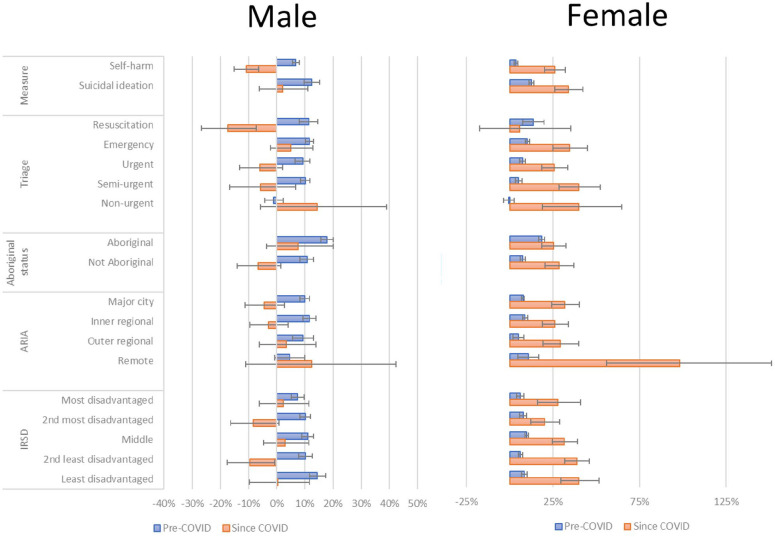
More than half of the self-harm or suicidal ideation presentations in young people were triaged as ‘Urgent’, and growth in this category did not accelerate significantly since COVID-19 (Table 2). Presentation rates in the ‘Emergency’, ‘Semi-urgent’ and ‘Non-urgent’ categories grew at a significantly faster rate since COVID-19 than pre-COVID.
Young people of Aboriginal and/or Torres Strait Islander background had a self-harm or suicidal ideation presentation rate approximately 3 times that of other young people both before and since COVID-19. Prior to COVID-19, rates in Aboriginal and/or Torres Strait Islander young people were increasing at more than twice the annual rate of increase observed in other young people. However, since COVID, the rate of increase has remained unchanged in Aboriginal and/or Torres Strait Islander young people, while it accelerated (to 15.3% pa, 95% CI = [7.6%, 23.6%]) in other young people.
In both pre-COVID-19 and COVID-19 periods, regional and remote areas of NSW had the highest per capita self-harm or suicidal ideation presentation rates (Table 2). Before COVID-19, rates were increasing more steeply in remote (13.3% pa, 95% CI = [9.0%, 17.8%]) and inner regional areas (9.6% pa, 95% CI = [8.5%, 10.7%]). Since COVID-19, growth rates increased significantly in all regions other than inner regional areas.
The relationship between presentation rates and regional measures of socio-economic disadvantage was complex (Table 2). Before COVID-19, there appeared to be an inverted U-shaped relationship, with higher rates in the middle quintile of socio-economic disadvantage and the lowest rates in the most disadvantaged and the second most advantaged quintiles. Since COVID-19, presentation rates have increased significantly in most quintiles; however, the largest annualised growth rates were observed in the three most socio-economically advantaged quintiles.
Before COVID-19, in both genders, self-harm or suicidal ideation presentations were growing most rapidly in more urgent triage categories and for Aboriginal young people (Figure 3). The pattern of changes since COVID-19 has differed between genders. In females, while accelerating self-harm or suicidal ideation presentations occurred in all geographical regions and subgroups, the fastest growth since COVID occurred in socio-economically advantaged regions. In males, presentation rate declined significantly only in non-Aboriginal youths.
Figure 3.
Rate of change in NSW emergency department self-harm or suicidal ideation presentations by gender and socio-economic status pre-COVID and since COVID first wave.
Annualised rate of change (percent per year) in ED self-harm or suicidal ideation presentations pre-COVID (January 2015 to March 2020) and since COVID (March 2020 to June 2021), by gender and subgroup. Rurality and disadvantage measures (Index of Relative Socio-economic Disadvantage) based on person’s area of residence.
Discussion
Self-harm or suicidal ideation ED presentations in NSW young people were growing by more than 8% pa in the 5 years before COVID-19, consistent with Australian and international trends. Since the first wave of COVID-19 in NSW, growth significantly accelerated above long-term trends only in females, particularly in girls aged 10–17 years. There was a significant decline in growth rates in males aged 10–24 years since COVID, driven by a reduction in rates in men aged 18–24 years. Self-harm or suicidal ideation presentation rates increased in all geographical regions since COVID, with the greatest increase in high school-aged females in more socio-economically advantaged regions.
Pre-COVID-19 increases in self-harm or suicidal ideation presentation rates
It is important to first consider reasons for pre-COVID-19 increases in self-harm or suicidal ideation presentation rates because most of the increases since COVID are consistent with those long-term trends, and the pandemic is likely to have interacted with pre-existing factors. The pre-COVID increase observed in NSW is consistent with reported trends from Australia, the United States, England and Canada (Australian Institute of Health and Welfare, 2021b; Centre for Epidemiology and Evidence, 2021; Gardner et al., 2019; Hiscock et al., 2018; Perera et al., 2018; Plemmons et al., 2018; Spiller et al., 2020). The timing and scale of these increases are consistent with evidence from population surveys of increasing psychological distress in younger people, with the greatest increases in younger females and in the late teen (15–19 years) age group (Hall et al., 2019; Marquez and Long, 2020; The Children’s Society, 2020). NSW suicide rates in 15- to 24-year-olds increased from 6.3 per 100,000 in 2011 to 12.5 in 2019 (HealthStats NSW, 2021b), also suggesting that increased self-harm or suicidal ideation presentations may reflect greater distress and not merely changes in help-seeking.
The consistent increases in distress and self-harm presentations in many high-income countries suggest shared social, economic, cultural and/or environmental causes. Proposed causes include (1) impacts of social media on friendships and self-esteem (Khan et al., 2021; Kreski et al., 2021; Tiller et al., 2020); (2) reduced physical activity associated with increased screen time (Khan et al., 2021); (3) economic and labour market changes since the Global Financial Crisis, causing increased inequality and reduced vocational opportunities for young people in many countries (Steeg et al., 2020); (4) environmental factors related to climate change, including ‘eco-anxiety’ (McDonald and Havens, 2020) or direct effects of increased daily temperatures on self-harm and suicide (Williams et al., 2016; Younan et al., 2018); and (5) health system factors including increased availability of antidepressants and opioids (Spiller et al., 2020), and possible iatrogenic effects of antidepressant medications in increasing agitation in younger people (Whitely et al., 2020).
In Australia, debate has highlighted health system factors including lack of access to mental health services for children and young people (Robinson et al., 2016). However, increases in self-harm presentations in Australia have occurred despite large national investments in primary care youth services such as Headspace, and substantial increases in service access (Jorm, 2019).
Changes since COVID-19
We found that since COVID-19, long-term increases in hospital presentations for ED self-harm or suicidal ideation presentation rates have accelerated in NSW particularly for adolescent girls. This may reflect increased distress in young people. Qualitative surveys have described the experience of young people during the ongoing pandemic as ‘swimming with sandbags’ (Marlay et al., 2020). Many young people report anxieties about the health of their families or friends, and concerns about educational impacts, home responsibilities and additional difficulties in meeting social and family expectations (Greenland and Hall, 2021; Marlay et al., 2020). Loneliness and social isolation also have direct effects on mental health in younger people (Loades et al., 2020). Despite these many stressors, there is currently no consistent evidence of increased suicides in young people in those countries for whom early data are available (John et al., 2020).
Several aspects of our findings require specific exploration. We found that significantly accelerated growth in self-harm or suicidal ideation presentation rates since COVID-19 particularly occurred in school-aged girls (10–17 years). Adolescents may be more vulnerable than young adults because of greater reliance on their peer group for support and identity development. In our study, self-harm or suicidal ideation presentation rates had weekly and annual cycles strongly linked to the school term, highlighting the impact of the school environment on adolescent wellbeing. COVID-19 disrupted the normal educational and social milestones of completing high school; in a survey of Australian young people, the highest levels of distress and greatest concerns about COVID-19 impacts were reported by 17-year-olds (Greenland and Hall, 2021). Among adolescents, greater increases may occur in females because of different exposure or sensitivity to these stressors, higher levels of concern about education impacts (Greenland and Hall, 2021) or gender-related differences in behaviour or help-seeking. It is possible that young females may respond to social isolation with depression, and hence presentation with self-harm or suicidal ideation, while young males may instead experience distress in different ways (Loades et al., 2020).
Since COVID, we found smaller increases in self-harm or suicidal ideation presentations in women aged 18–24 years, and significant declines in presentation rates in young men. Young adults are more likely to have been living independently, less exposed to family stressors, have greater skills for managing stressors and greater access to COVID-19-related government economic supports. For young adults in tertiary education, there may have been less of a transition to online learning because this technology was already used extensively in that sector prior to COVID-19.
We found that since COVID, growth in self-harm or suicidal ideation presentation rates accelerated most in the least socio-economically disadvantaged regions. We have no direct evidence to explain this unexpected finding. It may reflect differences in psychological distress arising from greater pressure for educational attainment among families with higher incomes. Parents in occupations with higher incomes may have had greater capacity to work from home, leading to greater awareness of distress in young people in the household. More advantaged communities may have a higher proportion of older adolescents remaining in high school or aiming to enter tertiary education and hence be more impacted by concerns about educational disruptions. Prior to COVID-19, people in more advantaged regions may have had better access to a wider range of privately funded mental health supports, and so may have experienced greater disruption to their healthcare during the COVID-19 period. Within NSW, some of the most socio-economically disadvantaged urban locations are also among the most culturally diverse and may have protective factors through strong community and family networks that moderate distress or provide alternative pathways for support.
Time series decomposition showed a transient dip in presentations during initial public health restrictions, consistent with broader NSW data (Sutherland et al., 2020). We cannot explain the slightly biphasic shape of this dip in people under 18 years, which does not appear to align with school terms, specific changes in home schooling arrangements or other government pandemic measures.
Strengths and limitations
We used statewide data covering a population of more than 2.5 million young people and including data up to June 2021. To improve identification of self-harm or suicidal ideation in ED data, NSW has implemented an enhanced method which includes searching of free-text fields; however, this probably still underestimates the true rate of ED self-harm or suicidal ideation presentations. It is possible that there are age, gender or regional biases in the NSW detection method, and our findings should be compared with those from other health systems using different methods. The NSW method will continue to be refined and tested as additional data sources become available.
Annualised rates of change in self-harm or suicidal ideation presentations since COVID were calculated based on 16 months of data from March 2020 to June 2021. Because of this short time period, these estimates have substantial uncertainty, particularly when examining subgroups. The estimates should be updated as more data become available.
This study has focused on self-harm or suicidal ideation presentations to hospital EDs. We were not able to capture data on people who sought help from other services, such as General Practitioners, private practitioners or services provided via Primary Health Networks. Therefore, our results under-estimate the total rate of help-seeking in the NSW population.
Because of data availability problems from one hospital, we excluded Sydney’s socio-economically advantaged Northern Beaches region, which experienced a localised outbreak and lockdown during the observation period: this may have affected overall population rate estimates and our analysis of possible relationship between self-harm or suicidal ideation presentation rates and regional socio-economic disadvantage.
Conclusion
Prior to COVID-19, ED self-harm or suicidal ideation presentations in children and young people were growing steadily in NSW, consistent with recent Australian and international trends. Understanding the reasons for that sustained increase remains an important priority. The COVID-19 pandemic has disrupted peer and family networks and educational opportunities. Adolescent girls may be particularly vulnerable to these effects. Further research is needed to clarify the mediating pathways and understand the risk and protective factors involved. Health systems need to be able to respond to increased presentations, ideally by providing accessible, effective and youth-friendly mental health services, including evidence-based online approaches for distress and depression (Loades et al., 2020). However, the increasing adolescent distress observed in many countries suggests a need to focus on broader causes as well as health system responses. Health and social policies may also need to consider a specific focus on social connectedness in families with children and adolescents, including strategies to support community connectedness beyond schooling, addressing disruptions to important social institutions such as sporting, music, artistic and cultural activities for younger people. It is critical to ensure that social and health system policies continue to work to reduce the risk of greater distress and increased suicides in response to the COVID pandemic.
Supplemental Material
Supplemental material, sj-docx-1-anp-10.1177_00048674221082518 for Growth in emergency department self-harm or suicidal ideation presentations in young people: Comparing trends before and since the COVID-19 first wave in New South Wales, Australia by Grant Sara, Jianyun Wu, John Uesi, Nancy Jong, Iain Perkes, Katherine Knight, Fenton O’Leary, Carla Trudgett and Michael Bowden in Australian & New Zealand Journal of Psychiatry
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship and/or publication of this article.
ORCID iDs: Grant Sara  https://orcid.org/0000-0002-3762-1711
https://orcid.org/0000-0002-3762-1711
Nancy Jong  https://orcid.org/0000-0002-9737-3844
https://orcid.org/0000-0002-9737-3844
Iain Perkes  https://orcid.org/0000-0001-8028-9032
https://orcid.org/0000-0001-8028-9032
Fenton O’Leary  https://orcid.org/0000-0002-5365-2462
https://orcid.org/0000-0002-5365-2462
Supplemental Material: Supplemental material for this article is available online.
References
- Australian Bureau of Statistics (ABS) (2018. a) 1270.0.55.005 – Australian Statistical Geography Standard (ASGS): Volume 5 – Remoteness Structure, July 2016. Available at: www.abs.gov.au/ausstats/abs@.nsf/mf/1270.0.55.005?OpenDocument (accessed 15 October 2021).
- Australian Bureau of Statistics (ABS) (2018. b) 2033.0.55.001 – Census of Population and Housing: Socio-economic Indexes for Areas (SEIFA), Australia, 2016. Available at: www.abs.gov.au/ausstats/abs@.nsf/mf/2033.0.55.001 (accessed 15 October 2021).
- Australian Institute of Health and Welfare (2021. a) Emergency Department Care 2019-20 Data Tables. Available at: www.aihw.gov.au/getmedia/433caea4-03ff-4569-96ac-042f2844f29c/Emergency-department-care-2019-20.xlsx.aspx (accessed 15 October 2021).
- Australian Institute of Health and Welfare (2021. b) Suicide and Self-harm Monitoring: Intentional Self-harm Hospitalisations among Young People. Available at: www.aihw.gov.au/suicide-self-harm-monitoring/data/populations-age-groups/intentional-self-harm-hospitalisations-among-young (accessed 15 October 2021).
- Australian Parliamentary Library (2021) COVID-19: A Chronology of State and Territory Government Announcements. Available at: www.aph.gov.au/About_Parliament/Parliamentary_Departments/Parliamentary_Library/pubs/rp/rp2021/Chronologies/COVID-19StateTerritoryGovernmentAnnouncements#_Toc52275795 (accessed 15 October 2021).
- Biddle N, Edwards B, Gray M, et al. (2020) Initial Impacts of COVID-19 on Mental Health in Australia. Canberra, ACT, Australia: Australian National University. [Google Scholar]
- Carr MJ, Steeg S, Webb RT, et al. (2021) Effects of the COVID-19 pandemic on primary care-recorded mental illness and self-harm episodes in the UK: A population-based cohort study. The Lancet Public Health 6: E124–E135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centre for Epidemiology and Evidence (2021) HealthStats NSW. Intentional Self Harm: Hospitalisations, by Age, Trend. Available at: www.healthstats.nsw.gov.au/Indicator/men_suihos/men_suihos_age_trend (accessed 15 October 2021).
- Gardner W, Pajer K, Cloutier P, et al. (2019) Changing rates of self-harm and mental disorders by sex in youths presenting to Ontario emergency departments: Repeated cross-sectional study. Can J Psychiatry 64: 789–797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenland N, Hall S. (2021) Young Voices of the Pandemic – Youth Survey COVID-19 Report 2020. Sydney, NSW, Australia: Mission Australia. [Google Scholar]
- Hall S, Fildes J, Perrens B, et al. (2019) Can We Talk? Seven Year Youth Mental Health Report - 2012-2018. Sydney, NSW, Australia: Mission Australia. [Google Scholar]
- Hastie T, Tibshirani R. (1986) Generalized additive models. Statistical Science 1: 297–318. [DOI] [PubMed] [Google Scholar]
- Hawton K, Casey D, Bale E, et al. (2021) Self-harm during the early period of the COVID-19 pandemic in England: Comparative trend analysis of hospital presentations. Journal of Affective Disorders 282: 991–995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HealthStats NSW (2021. a) HealthStats NSW, Population by Age. Available at: www.healthstats.nsw.gov.au/Indicator/dem_pop_age/dem_pop_age (accessed 15 October 2021).
- HealthStats NSW (2021. b) Suicide. Available at: https://beta.healthstats.nsw.gov.au/#/indicator?name=-men-sui-dth&location=NSW&view=Trend&measure=DSTRate&groups= (accessed 15 October 2021).
- Hiscock H, Neely RJ, Lei S, et al. (2018) Paediatric mental and physical health presentations to emergency departments, Victoria, 2008–15. Medical Journal of Australia 208: 343–348. [DOI] [PubMed] [Google Scholar]
- John A, Pirkis J, Gunnell D, et al. (2020) Trends in suicide during the covid-19 pandemic. BMJ 371: m4352. [DOI] [PubMed] [Google Scholar]
- Jorm AF. (2019) Lack of impact of past efforts to prevent suicide in Australia: Please explain. Australian and New Zealand Journal of Psychiatry 53: 379–380. [DOI] [PubMed] [Google Scholar]
- Khan A, Lee E-Y, Rosenbaum S, et al. (2021) Dose-dependent and joint associations between screen time, physical activity, and mental wellbeing in adolescents: An international observational study. The Lancet Child & Adolescent Health 5: P729–P738. [DOI] [PubMed] [Google Scholar]
- Kreski N, Platt J, Rutherford C, et al. (2021) Social media use and depressive symptoms among United States adolescents. Journal of Adolescent Health 68: 572–579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Large M, Corderoy A, McHugh C. (2020) Is suicidal behaviour a stronger predictor of later suicide than suicidal ideation? A systematic review and meta-analysis. Australian and New Zealand Journal of Psychiatry 55: 254–267. [DOI] [PubMed] [Google Scholar]
- Loades ME, Chatburn E, Higson-Sweeney N, et al. (2020) Rapid systematic review: The impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. Journal of the American Academy of Child & Adolescent Psychiatry 59: 1218–1239.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald D, Havens C. (2020) Linking Climate Change and Health Impacts. Melbourne, VIC, Australia: Sustainability Victoria. [Google Scholar]
- Marlay B, Attenborough J, Kutcher V. (2020) ‘Swimming with sandbags’: The views and experiences of young people in Australia five months into the COVID-19 pandemic, August. UNICEF Australia, Sydney, NSW, Australia. [Google Scholar]
- Marquez J, Long E. (2020) A global decline in adolescents’ subjective well-being: A comparative study exploring patterns of change in the life satisfaction of 15-year-old students in 46 countries. Child Indicators Research 14: 1251–1292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mourouvaye M, Bottemanne H, Bonny G, et al. (2021) Association between suicide behaviours in children and adolescents and the COVID-19 lockdown in Paris, France: A retrospective observational study. Archives of Disease in Childhood 106: 918–919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newby JM, O’Moore K, Tang S, et al. (2020) Acute mental health responses during the COVID-19 pandemic in Australia. PLoS ONE 15: e0236562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ougrin D, Wong BH, Vaezinejad M, et al. (2021) Pandemic-related emergency psychiatric presentations for self-harm of children and adolescents in 10 countries (PREP-kids): A retrospective international cohort study. European Child & Adolescent Psychiatry. Epub ahead of print 7March. DOI: 10.1007/s00787-021-01741-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perera J, Wand T, Bein KJ, et al. (2018) Presentations to NSW emergency departments with self-harm, suicidal ideation, or intentional poisoning, 2010-2014. Medical Journal of Australia 208: 348–353. [DOI] [PubMed] [Google Scholar]
- Plemmons G, Hall M, Doupnik S, et al. (2018) Hospitalization for suicide ideation or attempt: 2008-2015. Pediatrics 141: e20172426. [DOI] [PubMed] [Google Scholar]
- Plener PL. (2020) COVID-19 and nonsuicidal self-injury: The pandemic’s influence on an adolescent epidemic. American Journal of Public Health 111: 195–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson J, Bailey E, Browne V, et al. (2016) Raising the Bar for Youth Suicide Prevention. Melbourne, VIC, Australia: Orygen, The National Centre of Excellence in Youth Mental Health. [Google Scholar]
- SNOMED International (2019) SNOMED-CT. Available at: www.snomed.org (accessed 15 October 2021).
- Spiller HA, Ackerman JP, Smith GA, et al. (2020) Suicide attempts by self-poisoning in the United States among 10-25 year olds from 2000 to 2018: Substances used, temporal changes and demographics. Clinical Toxicology (Philadelphia, PA) 58: 676–687. [DOI] [PubMed] [Google Scholar]
- Stanley B, Currier GW, Chesin M, et al. (2018) Suicidal behavior and non-suicidal self-injury in emergency departments underestimated by administrative claims data. Crisis 39: 318–325. [DOI] [PubMed] [Google Scholar]
- Stapelberg NJC, Sveticic J, Hughes I, et al. (2020) Suicidal presentations to emergency departments in a large Australian public health service over 10 years. International Journal of Environmental Research and Public Health 17: 5920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steeg S, Carr MJ, Mok PLH, et al. (2020) Temporal trends in incidence of hospital-treated self-harm among adolescents in Denmark: National register-based study. Social Psychiatry and Psychiatric Epidemiology 55: 415–421. [DOI] [PubMed] [Google Scholar]
- Sutherland K, Chessman J, Zhao J, et al. (2020) Impact of COVID-19 on healthcare activity in NSW, Australia. Public Health Research & Practice 30: 3042030. [DOI] [PubMed] [Google Scholar]
- Sveticic J, Stapelberg NC, Turner K. (2020) Suicidal and self-harm presentations to Emergency Departments: The challenges of identification through diagnostic codes and presenting complaints. Health Information Management Journal 49: 38–46. [DOI] [PubMed] [Google Scholar]
- Szlyk HS, Berk M, Peralta AO, et al. (2020) COVID-19 takes adolescent suicide prevention to less charted territory. Journal of Adolescent Health 67: 161–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Children’s Society (2020) The Good Childhood Report 2020. London: The Children’s Society. [Google Scholar]
- Tiller E, Fildes J, Hall S, et al. (2020) Youth Survey Report 2020. Sydney, NSW, Australia: Mission Australia. [Google Scholar]
- Wang Y, Kala MP, Jafar TH. (2021) Factors associated with psychological distress during the coronavirus disease 2019 (COVID-19) pandemic on the predominantly general population: A systematic review and meta-analysis. PLoS ONE 15: e0244630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitely M, Raven M, Jureidini J. (2020) Antidepressant prescribing and suicide/self-harm by young Australians: Regulatory warnings, contradictory advice, and long-term trends. Frontiers in Psychiatry 11: 478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams MN, Hill SR, Spicer J. (2016) Do hotter temperatures increase the incidence of self-harm hospitalisations? Psychology, Health & Medicine 21: 226–235. [DOI] [PubMed] [Google Scholar]
- Wood SN. (2011) Fast stable restricted maximum likelihood and marginal likelihood estimation of semiparametric generalized linear models. Journal of the Royal Statistical Society. Series B (Statistical Methodology) 73: 3–36. [Google Scholar]
- Wood SN. (2017) Generalized Additive Models: An Introduction with R, 2nd Edition.Boca Raton, FL: Taylor & Francis Inc. [Google Scholar]
- Yard E, Radhakrishnan L, Ballasteros M, et al. (2021) Emergency Department Visits for Suspected Suicide Attempts Among Persons Aged 12–25 Years Before and During the COVID-19 Pandemic – United States, January 2019–May 2021. Morbidity and Mortality Weekly Report (US CDC) Early Release 70: 888–894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Younan D, Li L, Tuvblad C, et al. (2018) Long-term ambient temperature and externalizing behaviors in adolescents. American Journal of Epidemiology 187: 1931–1941. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-anp-10.1177_00048674221082518 for Growth in emergency department self-harm or suicidal ideation presentations in young people: Comparing trends before and since the COVID-19 first wave in New South Wales, Australia by Grant Sara, Jianyun Wu, John Uesi, Nancy Jong, Iain Perkes, Katherine Knight, Fenton O’Leary, Carla Trudgett and Michael Bowden in Australian & New Zealand Journal of Psychiatry