Abstract
Objective
To synthesise the current knowledge on barriers and facilitators to deprescribing cardiovascular medications (CVMs) at the levels of patients, informal caregivers and healthcare providers (HCPs).
Design/setting
We conducted a systematic review of studies exploring/assessing patient, informal caregiver and/or HCP barriers and/or facilitators to deprescribing CVMs.
Data sources
Ovid/MEDLINE and Embase from January 2003 to November 2021.
Data extraction and synthesis
We performed a deductive thematic analysis based on the framework of specific barriers and facilitators to deprescribing CVMs created by Goyal et al. We added a quantification of the occurrence of categories and themes in the selected articles to identify the resounding themes that indicate the greater impetus to address in future research.
Results
Most frequent deprescribing barriers for patients, informal caregivers and HCPs included uncertainty due to lack of evidence regarding CVM deprescribing (in n=10 studies), fear of negative consequences following deprescribing (n=13) and social influences (n=14). A frequently reported facilitator to deprescribing, especially for patients and informal caregivers, was the occurrence of adverse drug events (n=7). Another frequently reported facilitator for patients were dislike of CVMs (n=9). Necessity and benefit of CVMs were seen as barriers or facilitators similarly by patients and HCPs.
Conclusion
The differences in patient, informal caregiver and HCP regarding barriers and facilitators to deprescribing CVMs stress the need for ground discussions about beliefs and preferences of each stakeholder implicated in deprescribing decisions. Furthermore, HCP uncertainty regarding CVM deprescribing highlights the need to provide HCPs with tools that enable sharing the risks and benefits of deprescribing with patients and ensure a safe deprescribing process.
PROSPERO registration number
CRD42020221973.
Keywords: Adult cardiology, GERIATRIC MEDICINE, PRIMARY CARE, QUALITATIVE RESEARCH, VASCULAR MEDICINE
STRENGTHS AND LIMITATIONS OF THIS STUDY.
Systematic review process with publication review; data extraction, analysis and synthesis; and quality assessment independently conducted by two independent reviewers.
Assessment of both quantitative and qualitative studies, providing complementary information on barriers and facilitators to deprescribing.
In some studies, cardiovascular medications were part of, but not the focus of the medications evaluated.
We did not assess specific classes of cardiovascular medications.
The majority of healthcare providers were general practitioners, whose perspectives might differ from those of other healthcare providers.
Introduction
In recent years, a less-is-more attitude regarding medication use has led to reevaluate the balance between medication risks and benefits.1 In this context, the notion of deprescribing has emerged, which is defined as the ‘systematic process of identifying and discontinuing (medications) in instances in which existing or potential harms outweigh existing or potential benefits within the context of an individual patient’s care goals, current level of functioning, life expectancy, values and preferences’.2
Cardiovascular medications (CVMs) belong to the most prescribed medications worldwide.3 Although their use is beneficial in many cases, CVMs can also cause significant adverse drug events (ADEs), drug–drug and drug–disease interactions.4–6 However, the lack of evidence regarding benefits and risks of some CVMs in primary prevention in older people or in those with limited life expectancy, may lead to insecurity of patients and prescribers regarding CVM use and deprescribing.1 7–11
In this context, the decision to deprescribe a CVM often becomes a preference-sensitive decision.12 13 A better understanding of barriers and facilitators experienced by all stakeholders involved in decision-making regarding CVM deprescribing may help to take informed decisions in line with individual values and preferences, and increase confidence in the decision made.14 15 While literature exists on deprescribing general medications, we do not know if these barriers and facilitators differ from those of deprescribing CVMs.
With this systematic review, we aimed at synthetising the current knowledge on barriers and facilitators to deprescribing CVMs at the levels of patients, informal caregivers and healthcare providers (HCPs).
Methods
We conducted a systematic review of studies assessing barriers and/or facilitators to deprescribing CVMs in adults. The review was registered on PROSPERO (CRD42020221973).
Types of studies and inclusion criteria
We included any type of publication—except editorials, conference abstracts and study protocols—discussing stakeholder barriers and/or facilitators regarding the process of deprescribing CVMs. Studies on prescribing, use, or adherence were not included. Studies reporting patients stopping CVMs without previous discussion with HCPs were considered as non-adherence studies and excluded.
Search strategy
We searched Ovid/MEDLINE and Embase from January 2003 to November 2021. We started the search in 2003 because it corresponds to the first mention of the term deprescribing in the literature.16 We included studies published in English language and focusing on patients taking or having taken CVMs previously, and/or informal caregivers, and/or HCPs of such patients. We developed the three following concepts for our search strategy: (1) CVMs, (2) deprescribing and (3) barriers and facilitators. All three concepts were combined with the operator ‘and’. The detailed search strategy is provided in online supplemental material S1.
bmjopen-2022-061686supp001.pdf (47KB, pdf)
LB and CEA independently reviewed all publications identified through the search strategy after removing duplicates. First, ineligible articles were excluded based on title/abstract. Second, full text of the remaining articles was reviewed to identify eligible studies. Reference lists of included publications were also searched for additional relevant articles (hand searching). Reviews and meta-analyses were kept in the first selection, but only original studies identified in the reference lists were included. For each step, LB and CEA resolved discrepancies by discussion.
Data extraction and analysis
Eligible articles were imported in MAXQDA 2020 data analysis software (VERBI Software, Berlin, Germany). Extracted data included author(s), year of publication, country, study design, setting and population, and details on barriers and/or facilitators. Given the topic of this systematic review, we conducted a qualitative synthesis of the results. We performed a deductive thematic analysis to identify common and discrepant themes within and between stakeholder categories.17 18 The thematic analysis was based on the framework of specific barriers and facilitators to deprescribing CVMs created by Goyal et al.4 This framework, based on Reeve’s framework of patient barriers and facilitators to deprescribing medications,19 includes the following categories: appropriateness of cessation, process of cessation, dislike of medications, fear, uncertainty and conflicting attitudes. We analysed patient and informal caregiver outputs together and HCP outputs separately, since we expected to identify different barriers and facilitators. In an iterative process, we created themes within the predefined categories. To identify the resounding themes that indicate the greater impetus to address in future research, we added a quantitative aspect to our thematic analysis, in which we identified the number of times each category and theme appeared in the selected studies.
Risk of bias and quality assessment
LB and CEA conducted the quality and risk of bias assessment separately using the Mixed Methods Appraisal Tool (MMAT) 2018.20 21 The MMAT allows assessing the methodological quality of studies included in a systematic review encompassing both qualitative and quantitative data. Discussions were held until a consensus on quality of each study was reached.
Patient and public involvement
Patients and Public were not involved in the design, conduct or reporting of this review, but in a follow-up project based on this review.
Results
Study selection and characteristics
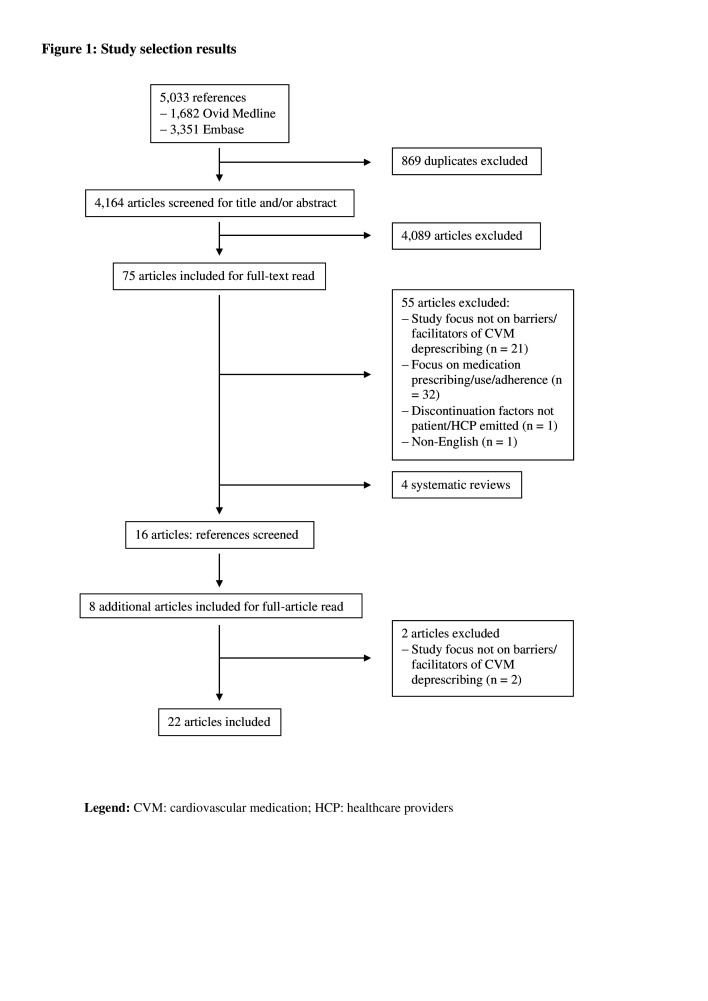
Among the 4164 unique studies identified, 71 were included for full-text assessment (figure 1). Among those, 16 fulfilled inclusion criteria. Through handsearching, six additional studies were included, leading to a total of 22 publications that were included for data extraction and analysis. Ten studies focused on patients and/or informal caregivers, 10 studies on HCPs and two studies on patients and/or informal caregivers and HCPs. Overall, the CVMs most frequently discussed were lipid-lowering therapies, especially statins (mentioned in 12 studies). Eleven studies focused on older patients (median or mean patient age of 74 years) Among HCP studies, the most represented HCPs were general practitioners (GPs) (in 10 studies). Study characteristics are presented in table 1 and detailed in online supplemental material S2.
Figure 1.
Study selection results. CVM, cardiovascular medication; HCP, healthcare providers.
Table 1.
Main characteristics of studies reporting patient, informal caregiver and HCP barriers and facilitators to deprescribing CVMs
| First author, publication year | N population | Age | Studied CVM(s) | Prevention type | |
| Patients and informal caregivers | Benson, 2005 (UK)22 | 38 patients | Any | Antihypertensives | Unknown |
| Brinton (USA)41 | 5014 patients | Mean age: 64 years | Statins | Primary and secondary | |
| Crutzen (Netherlands)23 | 17 patients, 1 informal caregiver | Median age: 78 years | Cardiometabolic medication | Primary and secondary | |
| Goyal (USA)4 | 10 patients | Median age: 80 years | β-blockers | Primary and secondary | |
| Jansen (Australia)24 | 30 patients | ≥75 years | Preventive CV medication | Primary and secondary | |
| Luymes (Netherlands)42 | 33 patients | Mean age: 57 years | Lipid-lowering drugs Antihypertensives |
Primary | |
| Pickering (USA)25 | 16 patients, 17 informal caregivers | Patients≥65 years Caregivers 22–69 years |
Unspecified (identified: statins, antihypertensives, antiplatelets, antidiabetics) | Primary and secondary | |
| Qi (Australia)36 | 180 patients | Median age: 78 years | Regular medications, statins | Primary and secondary | |
| Tija (USA)37 | 297 patients | Mean age: 72 years | Statins | Primary and secondary | |
| Van Bussel (Netherlands)26 | 15 patients | Mean age: 81 years | Antihypertensives | Primary | |
| HCPs | First author, publication year | N population | Characteristics of patients cared for by study HCPs | ||
| Age | Studies CVM(s) | Prevention type | |||
| Ailabouni (New Zealand)27 | 10 GPs | 83 years | Antiplatelets, statin, antidiabetics, diuretics, β-blocker, ACE inhibitor | Secondary | |
| Ailabouni (New Zealand)35 | 10 GPs | Unspecified (older pts) | Unspecified (identified: statin and aspirin) | Unknown | |
| Anderson (Australia)28 | 32 GPs, 15 CPs | Unknown | Unspecified (identified: statin) | Unknown | |
| Geijteman (Netherlands)38 | 174 GPs, 147 clinical specialists | 88 years | ACE inhibitor, statin, anticoagulant, diuretic, antidiabetic | Secondary | |
| Goyal (USA)39 | 184 geriatricians, 182 general internists, 87 cardiologists | 79 years | 4 CV medications | Unknown | |
| Green (USA)29 | 19 physicians, 2 nurse practitioners | Unspecified (older pts) | Unspecified (identified: statins, oral anticoagulants, antidiabetics) | Unknown | |
| Jansen (Australia)30 | 25 GPs | ≥75 years | Preventive CV medication | Primary | |
| Thompson (Denmark)31 | 11 GPs | ≥80 years | Statins | Unknown | |
| Van Middelaar, 2020 (Netherlands)32 | 15 GPs | Unspecified (older pts) | Antihypertensives | Unknown | |
| Van der Ploeg, 2018 (30 countries)40 | 2250 GPs | ≥80 years | Statins | Primary and secondary | |
| Patients and informal caregivers and HCPs | First author, publication year | N population | Characteristics of patients | ||
| Age | Studied CVM(s) | Prevention type | |||
| Luymes (Netherlands)33 | 10 GPs, 49 patients | Median age: 55 years | Antihypertensives, lipid-lowering drugs | Primary | |
| Todd (UK)34 | 12 patients, 12 informal caregivers, three palliative consultants, 3 nurse practitioners, 6 GPs |
Any | Unspecified (preventive medications, including statins, antihypertensives) | Unknown | |
ACE inhibitors, angiotensin converting enzyme inhibitors; CPs, community pharmacists; CV, cardiovascular; CVM(s), cardiovascular medication(s); GPs, general practitioners; pts, patients.
bmjopen-2022-061686supp002.pdf (106.3KB, pdf)
Quality assessment
Details of each study quality assessment can be found in online supplemental material S3. Of the 15 qualitative studies included in this systematic review, 14 were deemed of good quality,4 22–34 while 1 lacked data to support interpretation of the results.35 Five of the six included quantitative studies did not provide sample representative of the target population, as non-response was high, increasing the risk of non-response bias.36–40 The sixth quantitative study provided few details on the method used for data analysis.41 The only mixed-methods study included failed to address divergences between quantitative and qualitative results.42 We did not exclude any study based on the quality assessment, as our aim was to describe all available data regarding barriers and facilitators to deprescribing CVMs.
bmjopen-2022-061686supp003.pdf (45.3KB, pdf)
Thematic analysis
Following the framework of Goyal et al,4 seven categories were created to describe patient, informal caregivers, and HCP main barriers and facilitators to deprescribing CVMs. Categories one and four were divided into three and two themes, respectively. Differences between patients, informal caregivers and HCPs are highlighted when relevant. HCPs other than GPs (including general internists and family medicine clinicians) are regrouped under the term ‘specialists’. Differences across specialties are highlighted when relevant. Of the 22 articles, all encompassed barriers and facilitators to deprescribing CVMs, except for one (Brinton et al reported only facilitators).41 Barriers and facilitators did not appear to differ significantly between studies assessing different CVMs. All barriers and facilitators, according to categories, themes and stakeholders, are displayed in table 2. The facilitators most frequently mentioned by patients were ADE occurrence and dislike, respectively reported in seven and nine studies (n=7 and n=9), as shown in table 3. The facilitator most commonly reported by HCPs was the lack of benefit (reported in n=7). One of the barriers most frequently cited by patients/informal caregivers and HCPs was fear, reported in n=7. Social influences were another barrier frequently mentioned by HCPs (reported in n=10). Additional frequent barriers were uncertainty for HCPs (reported in n=7), and perceived benefit and social influences for patients and informal caregivers (reported in n=6).
Table 2.
Summary of categories, themes and codes of barriers and facilitators to deprescribing CVMs
| Categories | Themes | Barriers or facilitators | Patients and/or informal caregivers | HCPs | HCPs and patients and/or informal caregivers |
| Appropriateness | Necessity | Facilitators | Low CV risk Disease under control Trigger disappearance |
Primary prevention Age as single CVRF |
|
| Barriers | CVM linked to survival | Unhealthy lifestyle Many CVRFs |
Past CV event Family history of CVD CVM should be taken until end of life |
||
| Benefit | Facilitators | Robustness | Short life expectancy Cognitive impairment Nursing home patients Palliative patients |
No objective improvement under CVM No subjective improvement under CVM |
|
| Barriers | Frailty CVM use=active contribution to health CVM use=having control over one’s self |
Good physical and cognitive function Few comorbidities |
Objective improvement under CVM Subjective improvement under CVM |
||
| ADEs | Facilitators | ADEs foster deprescribing discussion with HCP | Reduction in QOL through ADEs | ||
| Barriers | ADEs balanced against reasons to take CVMs | ADEs in patients with CVD | No ADE, no symptom from disease | ||
| Fear | Facilitators | Fear of ADEs Fear of becoming dependent on CVMs |
|||
| Barriers | Fear of deprescribing due to severity of underlying disease Fear of experiencing a CV event after deprescribing and becoming a burden |
Feeling of giving up on patients | Fear of CV event, return of previous condition, health deterioration following deprescribing Fear of shorter lifespan without CVM |
||
| Dislike | Facilitators | General dislike of medications Medication-associated costs Living a long life without using CVMs Pride in not taking medications CVMs=poison CVMs=bad for health Therapeutic competition |
|||
| Influences | Previous experiences | Facilitators | Positive previous experience with deprescribing (QOL improvement, no stroke) | ||
| Barriers | Negative previous experience with deprescribing (restart medication, stroke) | ||||
| Social influences | Facilitators | HCPs (especially GP) advising deprescribing | Patient’s preferences | ||
| Barriers | HCPs (especially GP) advising against deprescribing | Patient’s preferences (reluctance) Patient’s lack of understanding Patient’s family wants CVMs Specialist prescription Interference with other HCPs’ treatment plan |
|||
| Process | Facilitators | Temporary deprescribing trial Possibility of CVM resumption |
Dose-lowering scheme Close monitoring |
||
| Barriers | Lack of remuneration for close monitoring | Time constraints | |||
| Uncertainty | Facilitators | Uncertainty about possible consequences of taking CVMs | |||
| Barriers | Lack of understanding of CVDs and risk reduction with CVMs Uncertainty about risks and benefits Conflicting treatment targets |
Lack of evidence on deprescribing Uncertainty about when to deprescribe Uncertainty about risk–benefit balance Limited training on deprescribing |
Unknown consequences of deprescribing | ||
| Ambivalence | Facilitators and/or barriers | Concern about CVM effect on health vs consequences of not taking CVMs Aversion towards CVMs vs obligation to take CVMs |
ADEs, adverse drug events; CV, cardiovascular; CVD, cardiovascular disease; CVM, cardiovascular medication; CVRF, cardiovascular risk factor; GP, general practitioner; HCPs, healthcare providers; QOL, quality of life.
Table 3.
Occurrence of categories and themes in the included studies
| Author | Facilitators | Barriers | Facilitators and barriers | |||||||||||||||
| Appropriateness | Fear | Dislike | Influences | Process | Uncertainty | Appropriateness | Fear | Influences | Process | Uncertainty | Ambivalence | |||||||
| Necessity | Benefit | ADEs | Social | Exp | Necessity | Benefit | ADEs | Social | Exp | |||||||||
| Patients and informal caregivers | ||||||||||||||||||
| Benson22 | x | x | x | x | ||||||||||||||
| Brinton41 | x | x | x | |||||||||||||||
| Crutzen23 | x | x | x | x | x | x | x | x | x | x | x | |||||||
| Goyal4 | x | x | x | x | x | x | x | x | x | |||||||||
| Jansen24 | x | x | x | x | x | x | x | x | ||||||||||
| Luymes42 | x | x | x | x | x | x | ||||||||||||
| Pickering25 | x | x | x | x | x | x | ||||||||||||
| Qi36 | x | x | x | x | ||||||||||||||
| Tija37 | x | x | ||||||||||||||||
| Van Bussel26 | x | x | x | x | x | x | x | x | ||||||||||
| Healthcare providers | ||||||||||||||||||
| Ailabouni27 | x | x | x | x | ||||||||||||||
| Ailabouni35 | x | x | x | x | x | |||||||||||||
| Anderson28 | x | x | x | x | x | x | x | x | x | x | x | x | ||||||
| Geijteman38 | x | x | x | x | ||||||||||||||
| Goyal39 | x | x | x | x | x | x | ||||||||||||
| Green29 | x | x | x | x | x | x | ||||||||||||
| Jansen30 | x | x | x | x | x | x | ||||||||||||
| Thompson31 | x | x | x | x | ||||||||||||||
| Van Middelaar32 | x | x | x | x | x | x | x | x | x | x | x | |||||||
| Van der Ploeg40 | x | x | x | x | x | |||||||||||||
| Patients, informal caregivers and healthcare providers | ||||||||||||||||||
| Luymes33 | x | x | x | x | x | x | x | x | x | |||||||||
| Todd34 | x | x | x | |||||||||||||||
‘x’ means that the category/theme was mentioned in the article.
ADE, adverse drug event.
Appropriateness
Patient and HCP agreement or disagreement with appropriateness of CVM deprescribing were based on three main themes: CVM necessity, CVM benefit and ADE occurrence. While CVM necessity and benefit were almost as frequently mentioned as facilitators than as barriers, ADE occurrence was clearly reported as a facilitator to deprescribing (n=12).
Necessity
Patients more often reported their necessity of the CVMs (n=5 for necessity as a barrier to deprescribing)4 24 34 37 42 than their non-necessity (n=3).26 33 42 Necessity was a theme less reported by HCPs (n=3 for necessity as a barrier to deprescribing,31–33 and n=2 for non-necessity as a facilitator).30 40 Patients in three studies considered taking CVMs as a necessity, even an obligation, especially in case of past cardiovascular (CV) event or family history of CV disease (CVD).24 33 42 This view was shared by GPs in two studies, who also deemed necessary to treat patients with unhealthy lifestyle, or presenting many CV risk factors (CVRF).32 33 Patients and one GP even stated that CVMs should not be stopped until the end of life,24 31 34 37 while other patients considered CVMs linked to their survival.4 Contrastively, patients at low CV risk and GPs treating patients in primary prevention or patients without any CVRF other than age, considered CVMs less necessary.30 33 40 42 Some patients questioned the continuous necessity of their CVM, as they felt that their disease was well-controlled.26 33
Benefit
CVM benefit was a frequently reported theme by patients/informal caregivers (n=7)4 22–25 36 41—more often as a barrier (ie, perception of benefit in n=6).4 22–25 36 CVM benefit was also frequently reported by HCPs (n=9),28–32 35 38–40 however, more often as a facilitator (ie, lack of benefit of CVMs in n=7) to deprescribing.28–31 38–40 GPs were more inclined to continue treating patients with good physical and cognitive function or few comorbidities, especially if they presented no CVM-related ADEs, expecting them to derive a higher benefit from CVMs.28 30–32 35 In contrast, GPs and specialists considered patients with a short life expectancy, cognitive impairment or living in palliative/nursing homes less likely to benefit from CVMs.28–31 38–40 They felt that, in these cases, prolonging life or avoiding a CV event should not be the main objective of care.30 However, frail patients were less willing to stop their statin than robust ones.36
Some patients and informal caregivers also considered CVMs to be beneficial when they saw an objective (eg, cholesterol levels) or subjective (eg, less dizziness) improvement under treatment.4 22 23 25 Some patients also considered that taking CVMs enabled them to make an active contribution to their health, and to have control over themselves and the future.24
Adverse drug events
Patients, informal caregivers and HCPs reported ADEs as one of the main facilitators to stopping CVMs, especially if ADEs were associated with a reduction in quality of life (n=7 for patients and n=5 for HCPs).4 22–26 28 32 35 38 39 41 Patients usually compliant with medications considered ADEs as a reason to discuss deprescribing with their GP.24 26 Patients considering taking CVMs as a routine to stay healthy were still willing to discontinue their CVMs in case of ADEs.24 26 ADEs were not formally reported as barriers to deprescribing, but were put in perspective by patients/informal caregivers (n=2)22 26 and HCPs (n=2).32 40 Some patients continued taking their CVMs after balancing ADEs against reasons to take CVMs (ie, CVM perceived benefit, minor ADEs).22 When patients were asymptomatic and had no ADE, patients and GPs were unwilling to deprescribe CVMs.26 32 When ADEs occurred in patients with CVD, GPs were also unwilling to deprescribe.40
Fear
Fear of consequences following CVM deprescribing was reported as a barrier to deprescribing by patients/informal caregivers (n=7)4 23–26 33 42 and HCPs (n=7).27–29 32 33 35 39 In multiple studies, patients stated their fear of a return of the previous condition, health deterioration, becoming a burden or a shorter lifespan following deprescribing.4 24–26 33 42 Some linked this fear with the perceived severity of their disease.23 25 These concerns were shared by informal caregivers. GPs and specialists feared harming patients by deprescribing (eg, occurrence of CV event with functional limitation, death),27–29 32 33 35 39 and giving patients the feeling that they were giving up on them, especially by deprescribing towards the end of life, a feeling not shared by patients.27 29 32 37 38
Conversely, patients fearing ADEs or becoming ‘dependent’ on their CVMs were more willing to deprescribe (n=3).23 36 37 HCPs did not report fear as a facilitator (n=0).
Dislike
CVM dislike was a facilitator to deprescribing for patients and informal caregivers (n=9),4 23–26 33 34 41 42 but not for HCPs (n=0). Dislike was never reported as a barrier by patients/informal caregivers (n=0) or by HCPs (n=0). Patients stated a general dislike of medications or explained feeling burdened by the number of medications (CVMs and others), or medication-associated costs.4 23–26 33 34 41 Other patients were aiming at living a long life without using medications, or derived a personal pride of not taking medications.24 42 Some patients and informal caregivers considered CVMs as ‘not good for health’23 or despised CVMs that created therapeutic competition (ie, helping one condition while worsening another one) or which administration was complicated or disrupted daily routine (eg, glycaemia before insulin injections).4 25
Influences
Patient and HCP opinions towards deprescribing were shaped by their previous experiences in deprescribing CVMs, and by social influences. While social influences were reported as a barrier (n=4)24–26 42 almost as frequently as a facilitator (n=6)23–25 33 36 42 by patients and informal caregivers, they were more frequently reported as a barrier (n=10)27–30 32–35 39 40 to deprescribing by HCPs. Previous experiences were less reported than social influences and almost as often by patients and informal caregivers (reported both as a facilitator and a barrier in n=2)22 23 33 as by HCPs (reported as a facilitator in n=327 28 32 and as a barrier in n=4).28 29 32 33
Previous experiences
Patients and HCPs with a positive previous experience with CVM deprescribing were more amenable to deprescribe again, as opposed to those with a negative previous experience.4 23 27–29 32 33 GPs considered patients feeling better or with improved quality of life after deprescribing as positive experiences,27 32 and having to restart medications after deprescribing as a negative experience.32 For statins, occurrence or absence of stroke after deprescribing influenced GPs’ and specialists’ further actions.28 29
Social influences
HCPs influenced patients’ and informal caregivers’ opinion on deprescribing.25 36 Patients were willing to stop one or more CVM if this was proposed by a trusting physician.23 Patients especially trusted their GP because of their knowledge and the fact that they knew them well.24 26 33 42 Some patients also recognised their dependency towards their GP and highlighted their authority, feeling that it would be inappropriate to discuss their evaluation.26 Others were waiting for their GP to start discussions about preferences, or were happy to follow their recommendations.24 26
GPs accounted for patient preferences.28 30–32 40 They considered deprescribing in patients wanting to take less medications.30 31 They continued CVMs in patients expecting longevity or whose family was urging for medication continuation.30 GPs were also unwilling to deprescribe CVMs prescribed by specialists, even if they questioned the indication.27 28 30 33 35 Specialists were concerned by interfering with other HCPs’ treatment plan.29 39 They were also unwilling to deprescribe when communication with other HCPs was suboptimal or when patients were reluctant or could not understand the concept of deprescribing.34 39
Process
The process required to deprescribe CVMs was more frequently reported as a barrier (n=6)28 29 32 33 38 39 than as a facilitator (n=2)28 35 by HCPs. For patients and informal caregivers, this process was more frequently reported as a facilitator (n=4)4 23 24 33 than a barrier (n=2).23 33
HCPs and patients reported time constraint, such as lacking time to review medication lists or to discuss CVMs, as a barrier to CVM deprescribing.23 29 32 38 39
For patients, a dose-lowering scheme, a close monitoring after deprescribing and a temporary stopping trial with possibility of medication resumption facilitated the deprescribing process.4 23 24 33 GPs also viewed gradual CVM discontinuation as a facilitator to deprescribing, especially when they were unsure about CVM risk/benefit ratio.28 35 However, they considered the lack of remuneration for the close follow-up needed during gradual discontinuation as a barrier.28
Uncertainty
Uncertainty was reported more often by HCPs (n=7)27–30 32 38 39 than patient and informal caregiver (n=3),4 23 26 and acted almost exclusively as a barrier to deprescribing for both groups. HCPs formulated the lack of evidence about CVM deprescribing as a barrier, especially in older patients or those with dementia.27 29 39 GPs found it complicated to know when to deprescribe preventive medications—especially in patients neither frail nor robust27 32—and how to balance CVM harms and benefits when approaching deprescribing.30 One clinical pharmacist explained having difficulties making professional recommendations about statin deprescribing in older patients.28 Specialists regretted the limited training on deprescribing.39
Patients expressed a lack of understanding of CVDs and risk reduction with CVMs, as well as uncertainty regarding potential risks and benefits of CVMs, thus feeling uncertain about the value of deprescribing.4 23 26 They were also confused by conflicting treatment targets mentioned by HCPs.23
Some HCPs and patients also felt uneasy about the uncertainty surrounding possible consequences of CVM deprescribing.28 33 38 This led to ‘therapeutic inertia’, even in case of unclear benefits of pursuing CVMs.29 On the contrary, GPs and clinical pharmacists feeling uneasy about possible long-term consequences of taking CVMs were more willing to deprescribe.28
Ambivalence
Patients expressed ambivalence about CVM use, prompting them to wish CVM continuation and deprescribing concurrently (n=2).4 26 They were concerned about the effects of CVMs on their health, but also about what could happen if they did not take them.4 They also showed aversion towards CVMs coupled with a feeling of obligation to take them.4 26 HCPs did not express ambivalence (n=0).
Discussion
In this systematic review, we provided an overview of barriers and facilitators to deprescribing CVMs, from the point of view of patients, informal caregivers and HCPs. Barriers and facilitators could be classified in the following categories: appropriateness, fear, dislike, influences, process, uncertainty and ambivalence. Appropriateness was divided into three themes (necessity, benefit, ADEs) and influences into two (previous experiences, social influences). Frequent deprescribing barriers for both HCPs and patients/informal caregivers included influences of others on decision-making about deprescribing, and fear of negative consequences following CVM deprescribing. Another barrier frequently mentioned by HCPs was the uncertainty to deprescribe due to the lack of evidence regarding CVM deprescribing. The occurrence of ADEs was frequently reported as a facilitator to deprescribing, especially by patients and informal caregivers. Another facilitator for patients was dislike of CVMs. (Lack of) necessity and benefit of CVMs were seen as facilitators or barriers similarly by patients and HCPs. However, patients and HCPs disagreed on the necessity and benefit of taking CVMs in case of frailty or robustness. The process required to deprescribe CVMs acted both as barrier and facilitator for patients and was more often reported as a barrier than as a facilitator by HCPs.
While there is increasing literature on barriers and facilitators to deprescribing, there is little literature focusing specifically on barriers and facilitators to deprescribing CVMs. Our review provides readers with a current state of the knowledge on the perspectives of different stakeholders (ie, patients, informal caregivers and HCPs) regarding deprescribing of such medications and its specific challenges. Other studies focusing on deprescribing of other medication types or potentially inappropriate medications showed barriers and facilitators that were similar to some found in our review.43–47 On the patient level, these studies reported experiencing ADEs or feeling burdened by the medications as facilitators,46 47 and seeing the medications as necessary or beneficial as a barrier.45 On the HCP level, these studies reported gradual deprescribing as a facilitator,46 and fear of unknown or negative consequences following deprescribing, or like of time to approach deprescribing as barriers.43 44 46 Furthermore, a systematic review on patient barriers and facilitators to deprescribing also reported agreement with appropriateness of cessation, fear, influences, dislike and process as barriers and/or facilitators to deprescribing.19 However, this review that included mainly nervous system medications, did not report uncertainty and ambivalence towards deprescribing. This suggests that these two factors are more specific to CVM deprescribing and might reflect the remaining controversy surrounding deprescribing of some of these medications (eg, statins).
Fear of and uncertainty about deprescribing due to unknown/possible negative consequences was frequently mentioned as a barrier to deprescribing in the articles included in this systematic review. Interestingly, while fear was as frequently reported as a barrier by patients/informal caregivers than by HCPs, uncertainty was more frequently reported as a barrier by HCPs, suggesting a different level of knowledge and feeling of responsibility between HCPs and patients/informal caregivers. Such uncertainty was also reported in studies focusing on deprescribing general medications in older, multimorbid adults, potentially because of the complexity of interactions between diseases and the single-disease focused guidelines that might not apply to patients with multimorbidity.48–50 However, one of these studies stated that balancing benefits and harms was particularly complicated for preventive medications.48 Tools to facilitate the deprescribing process and ensure safe CVM deprescribing could help to do so, especially since HCPs in our review frequently reported the deprescribing process as a barrier.
While patient/informal caregiver and HCP points of view towards CVM deprescribing were largely similar, we could highlight differences in the perceived benefit of CVMs in robust vs frail patients. As shown in a study evaluating frail patient beliefs about prescribed medications, most patients saw their medications as highly necessary.51 However, over one-third of patients included in this study stated that their medications were a mystery to them.51 This stresses the fact that patients might see a medication as necessary without being able to understand its potential (lack of) benefit. HCPs, on the other hand, seemed to place importance on their patients deriving benefits from their CVMs. Thus, they endorsed deprescribing in frail patients due to a lack of time to benefit, but renounced deprescribing in robust patients. This view is concordant with other studies on treating frail and/or robust patients.9 52 Other differences between patients/informal caregivers and HCPs regarded ADE occurrence, which was slightly more frequently cited as a facilitator in studies on patients/informal caregivers than on HCPs, and dislike, which was a facilitator to deprescribing only mentioned by patients. These divergent views emphasise the need for discussion between HCPs and patients/informal caregivers about representations and beliefs, and how these might influence decision-making about deprescribing. This is especially important for HCPs to consider, given how patients rely on them for decision-making and might assume that they do not have to discuss their preferences and beliefs as these are already clear for their HCPs.53–55
Strengths and limitations
This study has several strengths. First, data extraction, analysis and synthesis, as well as quality assessment were conducted by two independent reviewers on all available data based on a systematic review. Second, we included both quantitative and qualitative studies, providing complementary information on barriers and facilitators to deprescribing.
However, this study also has limitations. First, in some studies, CVMs were part of the evaluated medications but not the focus. However, this enabled inclusion of more studies and thus exploration of more barriers and facilitators to deprescribing CVMs. Second, as this review focused on CVMs in general, no conclusion can be made on individual CVMs. However, barriers and facilitators did not appear to differ significantly between studies assessing/exploring different CVMs, which leads to thinking that most barriers and facilitators might be common across CVMs. Third, the studies reporting HCP barriers and facilitators to deprescribing CVMs encompass mostly GP barrier and facilitators, which may differ from those of other HCPs.
Implications
The identification of barriers and facilitators to deprescribing CVMs, and the quantification of the reporting frequency at the patient, informal caregiver and HCP levels, have several implications and call for future actions to address the current lack of evidence regarding potential benefits and risks of some CVM deprescribing. First, differences in opinions between patients and HCPs, such as CVM benefits and CVM dislike, stress the need for ground discussions about beliefs and preferences about deprescribing of each stakeholder implicated in the deprescribing decision. Second, the uncertainty about deprescribing CVMs that HCPs frequently mentioned, HCP wish to account for patient preferences when approaching deprescribing, and patients relying on HCPs for decision-making highlight the need to translate a part of HCP responsibility in deprescribing to patients, so that decision-making can be shared and jointly carried. To enable this, HCPs must be provided with tools that enable sharing the risks and benefits of deprescribing with patients and ensure a safe deprescribing process. Furthermore, HCPs should be trained on deprescribing processes and changes at the policy-making level should provide HCPs with sufficient time and adequate remuneration to approach deprescribing with patients. Less time pressure would also enable patients to feel more comfortable to address deprescribing with their HCPs.
Conclusion
In this systematic review, we provided an overview of barriers and facilitators to deprescribing CVMs, from the point of view of patients, informal caregivers and HCPs. The identification and quantification of barriers and facilitators most frequently cited by patients, informal caregivers and/or HCPs can help to develop future actions needed to improve evidence in CVM deprescribing and reduce the burden of medications for the patients.
Supplementary Material
Acknowledgments
The authors want to thank Judith Ellen Smith, Librarian at the University of Michigan (Ann Arbor, USA), who helped develop the search strategy, and Dr. Manuel Raphael Blum (Institute of Primary Health Care (BIHAM), University of Bern, Bern, Switzerland; Department of General Internal Medicine, Inselspital, Bern University Hospital, University of Bern, Switzerland), who critically revised the study protocol.
Footnotes
Contributors: CEA, LB and NR designed the study protocol. CEA and LB extracted and analyzed the data. CEA, LB and NR drafted the article. CEA acted as guarantor of this study. All authors gave final approval to submit the article.
Funding: All authors were partly supported by the Schweizerischer Nationalfonds zur Förderung der Wissenschaftlichen Forschung IICT, Grant number 33IC30-193052 (PI Prof. Rodondi). LB and this study were supported by a grant from the College of General Internal Medicine (Fribourg, Switzerland) (No grant number).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available on reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Krishnaswami A, Steinman MA, Goyal P, et al. Deprescribing in older adults with cardiovascular disease. J Am Coll Cardiol 2019;73:2584–95. 10.1016/j.jacc.2019.03.467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Scott IA, Hilmer SN, Reeve E, et al. Reducing inappropriate polypharmacy: the process of deprescribing. JAMA Intern Med 2015;175:827–34. 10.1001/jamainternmed.2015.0324 [DOI] [PubMed] [Google Scholar]
- 3.Informatics IIfH . Global medicines use in 2020, 2015. Available: https://www.iqvia.com/-/media/iqvia/pdfs/institute-reports/global-medicines-use-in-2020
- 4.Goyal P, Requijo T, Siceloff B, et al. Patient-Reported barriers and facilitators to deprescribing cardiovascular medications. Drugs Aging 2020;37:125–35. 10.1007/s40266-019-00729-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Budnitz DS, Lovegrove MC, Shehab N, et al. Emergency hospitalizations for adverse drug events in older Americans. N Engl J Med 2011;365:2002–12. 10.1056/NEJMsa1103053 [DOI] [PubMed] [Google Scholar]
- 6.Akbulut M, Urun Y. Onco-cardiology: drug-drug interactions of antineoplastic and cardiovascular drugs. Crit Rev Oncol Hematol 2020;145:102822. 10.1016/j.critrevonc.2019.102822 [DOI] [PubMed] [Google Scholar]
- 7.Rossello X, Pocock SJ, Julian DG. Long-Term use of cardiovascular drugs: challenges for research and for patient care. J Am Coll Cardiol 2015;66:1273–85. 10.1016/j.jacc.2015.07.018 [DOI] [PubMed] [Google Scholar]
- 8.Ridker PM, Danielson E, Fonseca FAH, et al. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med 2008;359:2195–207. 10.1056/NEJMoa0807646 [DOI] [PubMed] [Google Scholar]
- 9.Kutner JS, Blatchford PJ, Taylor DH, et al. Safety and benefit of discontinuing statin therapy in the setting of advanced, life-limiting illness: a randomized clinical trial. JAMA Intern Med 2015;175:691–700. 10.1001/jamainternmed.2015.0289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moonen JEF, Foster-Dingley JC, de Ruijter W, et al. Effect of discontinuation of antihypertensive medication on orthostatic hypotension in older persons with mild cognitive impairment: the DANTE study Leiden. Age Ageing 2016;45:249–55. 10.1093/ageing/afv199 [DOI] [PubMed] [Google Scholar]
- 11., Williamson JD, Pajewski NM, et al. , SPRINT MIND Investigators for the SPRINT Research Group . Effect of intensive vs standard blood pressure control on probable dementia: a randomized clinical trial. JAMA 2019;321:553–61. 10.1001/jama.2018.21442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Linsky A, Meterko M, Bokhour BG, et al. Deprescribing in the context of multiple providers: understanding patient preferences. Am J Manag Care 2019;25:192–8. [PMC free article] [PubMed] [Google Scholar]
- 13.Holmes HM, Todd A. The role of patient preferences in deprescribing. Clin Geriatr Med 2017;33:165–75. 10.1016/j.cger.2017.01.004 [DOI] [PubMed] [Google Scholar]
- 14.McCartney M, Treadwell J, Maskrey N, et al. Making evidence based medicine work for individual patients. BMJ 2016;353:i2452. 10.1136/bmj.i2452 [DOI] [PubMed] [Google Scholar]
- 15.Weir K, Nickel B, Naganathan V, et al. Decision-Making preferences and deprescribing: perspectives of older adults and companions about their medicines. J Gerontol B Psychol Sci Soc Sci 2018;73:e98–107. 10.1093/geronb/gbx138 [DOI] [PubMed] [Google Scholar]
- 16.Woodward MC. Deprescribing: achieving better health outcomes for older people through reducing medications. Journal of Pharmacy Practice and Research 2003;33:323–8. 10.1002/jppr2003334323 [DOI] [Google Scholar]
- 17.Vaismoradi M, Turunen H, Bondas T. Content analysis and thematic analysis: implications for conducting a qualitative descriptive study. Nurs Health Sci 2013;15:398–405. 10.1111/nhs.12048 [DOI] [PubMed] [Google Scholar]
- 18.Burnard P, Gill P, Stewart K, et al. Analysing and presenting qualitative data. Br Dent J 2008;204:429–32. 10.1038/sj.bdj.2008.292 [DOI] [PubMed] [Google Scholar]
- 19.Reeve E, To J, Hendrix I, et al. Patient barriers to and enablers of deprescribing: a systematic review. Drugs Aging 2013;30:793–807. 10.1007/s40266-013-0106-8 [DOI] [PubMed] [Google Scholar]
- 20.Hong QN, Gonzalez-Reyes A, Pluye P. Improving the usefulness of a tool for appraising the quality of qualitative, quantitative and mixed methods studies, the mixed methods appraisal tool (MMAT). J Eval Clin Pract 2018;24:459–67. 10.1111/jep.12884 [DOI] [PubMed] [Google Scholar]
- 21.Hong QN, Pluye P, Fàbregues S, et al. Improving the content validity of the mixed methods appraisal tool: a modified e-Delphi study. J Clin Epidemiol 2019;111:49–59. 10.1016/j.jclinepi.2019.03.008 [DOI] [PubMed] [Google Scholar]
- 22.Benson J, Britten N. What effects do patients feel from their antihypertensive tablets and how do they react to them? qualitative analysis of interviews with patients. Fam Pract 2006;23:80–7. 10.1093/fampra/cmi081 [DOI] [PubMed] [Google Scholar]
- 23.Crutzen S, Baas G, Abou J, et al. Barriers and Enablers of older patients to deprescribing of cardiometabolic medication: a focus group study. Front Pharmacol 2020;11:1268. 10.3389/fphar.2020.01268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jansen J, McKinn S, Bonner C, et al. Shared decision-making about cardiovascular disease medication in older people: a qualitative study of patient experiences in general practice. BMJ Open 2019;9:e026342. 10.1136/bmjopen-2018-026342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pickering AN, Hamm ME, Dawdani A, et al. Older patient and caregiver perspectives on medication value and deprescribing: a qualitative study. J Am Geriatr Soc 2020;68:746–53. 10.1111/jgs.16370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.van Bussel E, Reurich L, Pols J, et al. Hypertension management: experiences, wishes and concerns among older people-a qualitative study. BMJ Open 2019;9:e030742. 10.1136/bmjopen-2019-030742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ailabouni NJ, Nishtala PS, Mangin D, et al. Challenges and Enablers of deprescribing: a general practitioner perspective. PLoS One 2016;11:e0151066. 10.1371/journal.pone.0151066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Anderson K, Foster M, Freeman C, et al. Negotiating "Unmeasurable Harm and Benefit": Perspectives of General Practitioners and Consultant Pharmacists on Deprescribing in the Primary Care Setting. Qual Health Res 2017;27:1936–47. 10.1177/1049732316687732 [DOI] [PubMed] [Google Scholar]
- 29.Green AR, Lee P, Reeve E, et al. Clinicians' perspectives on barriers and Enablers of optimal prescribing in patients with dementia and coexisting conditions. J Am Board Fam Med 2019;32:383–91. 10.3122/jabfm.2019.03.180335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jansen J, McKinn S, Bonner C, et al. General practitioners' decision making about primary prevention of cardiovascular disease in older adults: a qualitative study. PLoS One 2017;12:e0170228. 10.1371/journal.pone.0170228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Thompson W, Le JV, Haastrup P, et al. Exploring how GPs discuss statin deprescribing with older people: a qualitative study. BJGP Open 2020;4. 10.3399/bjgpopen20X101022. [Epub ahead of print: 01 05 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.van Middelaar T, Ivens SD, van Peet PG, et al. Prescribing and deprescribing antihypertensive medication in older people by Dutch general practitioners: a qualitative study. BMJ Open 2018;8:e020871. 10.1136/bmjopen-2017-020871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Luymes CH, van der Kleij RMJJ, Poortvliet RKE, et al. Deprescribing potentially inappropriate preventive cardiovascular medication: barriers and Enablers for patients and general practitioners. Ann Pharmacother 2016;50:446–54. 10.1177/1060028016637181 [DOI] [PubMed] [Google Scholar]
- 34.Todd A, Holmes H, Pearson S, et al. ‘I don’t think I’d be frightened if the statins went’: a phenomenological qualitative study exploring medicines use in palliative care patients, carers and healthcare professionals. BMC Palliat Care 2016;15. 10.1186/s12904-016-0086-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ailabouni NJ, Nishtala PS, Mangin D, et al. General practitioners' insight into deprescribing for the multimorbid older individual: a qualitative study. Int J Clin Pract 2016;70:261–76. 10.1111/ijcp.12780 [DOI] [PubMed] [Google Scholar]
- 36.Qi K, Reeve E, Hilmer SN, et al. Older peoples' attitudes regarding polypharmacy, statin use and willingness to have statins deprescribed in Australia. Int J Clin Pharm 2015;37:949–57. 10.1007/s11096-015-0147-7 [DOI] [PubMed] [Google Scholar]
- 37.Tjia J, Kutner JS, Ritchie CS, et al. Perceptions of statin discontinuation among patients with life-limiting illness. J Palliat Med 2017;20:1098–103. 10.1089/jpm.2016.0489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Geijteman ECT, Huisman BAA, Dees MK, et al. Medication discontinuation at the end of life: a questionnaire study on physicians' experiences and opinions. J Palliat Med 2018;21:1166–70. 10.1089/jpm.2017.0501 [DOI] [PubMed] [Google Scholar]
- 39.Goyal P, Anderson TS, Bernacki GM, et al. Physician perspectives on deprescribing cardiovascular medications for older adults. J Am Geriatr Soc 2020;68:78–86. 10.1111/jgs.16157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.van der Ploeg MA, Streit S, Achterberg WP, et al. Patient Characteristics and General Practitioners’ Advice to Stop Statins in Oldest-Old Patients: a Survey Study Across 30 Countries. J Gen Intern Med 2019;34:1751–7. 10.1007/s11606-018-4795-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Brinton EA. Understanding patient adherence and concerns with statins and medication discussions with physicians (action): a survey on the patient perspective of dialogue with healthcare providers regarding statin therapy. Clin Cardiol 2018;41:710–20. 10.1002/clc.22975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Luymes CH, Boelhouwer NJ, Poortvliet RK, et al. Understanding deprescribing of preventive cardiovascular medication: a Q-methodology study in patients. Patient Prefer Adherence 2017;11:975–84. 10.2147/PPA.S131625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Anderson K, Stowasser D, Freeman C, et al. Prescriber barriers and enablers to minimising potentially inappropriate medications in adults: a systematic review and thematic synthesis. BMJ Open 2014;4:e006544. 10.1136/bmjopen-2014-006544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cook JM, Marshall R, Masci C, et al. Physicians' perspectives on prescribing benzodiazepines for older adults: a qualitative study. J Gen Intern Med 2007;22:303–7. 10.1007/s11606-006-0021-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zechmann S, Trueb C, Valeri F, et al. Barriers and enablers for deprescribing among older, multimorbid patients with polypharmacy: an explorative study from Switzerland. BMC Fam Pract 2019;20:64. 10.1186/s12875-019-0953-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kuntz J, Kouch L, Christian D, et al. Barriers and facilitators to the deprescribing of nonbenzodiazepine sedative medications among older adults. Perm J 2018;22:17–157. 10.7812/TPP/17-157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Paque K, Vander Stichele R, Elseviers M, et al. Barriers and enablers to deprescribing in people with a life-limiting disease: a systematic review. Palliat Med 2019;33:37–48. 10.1177/0269216318801124 [DOI] [PubMed] [Google Scholar]
- 48.Bokhof B, Junius-Walker U. Reducing polypharmacy from the perspectives of general practitioners and older patients: a synthesis of qualitative studies. Drugs Aging 2016;33:249–66. 10.1007/s40266-016-0354-5 [DOI] [PubMed] [Google Scholar]
- 49.Rieckert A, Sommerauer C, Krumeich A, et al. Reduction of inappropriate medication in older populations by electronic decision support (the PRIMA-eDS study): a qualitative study of practical implementation in primary care. BMC Fam Pract 2018;19:110. 10.1186/s12875-018-0789-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Schuling J, Gebben H, Veehof LJG, et al. Deprescribing medication in very elderly patients with multimorbidity: the view of Dutch GPs. A qualitative study. BMC Fam Pract 2012;13:56. 10.1186/1471-2296-13-56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Modig S, Kristensson J, Ekwall AK, et al. Frail elderly patients in primary care--their medication knowledge and beliefs about prescribed medicines. Eur J Clin Pharmacol 2009;65:151–5. 10.1007/s00228-008-0581-8 [DOI] [PubMed] [Google Scholar]
- 52.Benetos A, Rossignol P, Cherubini A, et al. Polypharmacy in the aging patient: management of hypertension in octogenarians. JAMA 2015;314:170–80. 10.1001/jama.2015.7517 [DOI] [PubMed] [Google Scholar]
- 53.Morecroft C, Cantrill J, Tully MP. Patients' evaluation of the appropriateness of their hypertension management--a qualitative study. Res Social Adm Pharm 2006;2:186–211. 10.1016/j.sapharm.2006.02.006 [DOI] [PubMed] [Google Scholar]
- 54.Morecroft C, Cantrill J, Tully MP. Individual patient's preferences for hypertension management: a Q-methodological approach. Patient Educ Couns 2006;61:354–62. 10.1016/j.pec.2005.04.011 [DOI] [PubMed] [Google Scholar]
- 55.Bynum JPW, Barre L, Reed C, et al. Participation of very old adults in health care decisions. Med Decis Making 2014;34:216–30. 10.1177/0272989X13508008 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-061686supp001.pdf (47KB, pdf)
bmjopen-2022-061686supp002.pdf (106.3KB, pdf)
bmjopen-2022-061686supp003.pdf (45.3KB, pdf)
Data Availability Statement
Data are available on reasonable request.