Abstract
Foot ulcers are common complications of diabetes mellitus and substantially increase the morbidity and mortality due to this disease. Wound care by regular monitoring of the progress of healing with clinical review of the ulcers, dressing changes, appropriate antibiotic therapy for infection and proper offloading of the ulcer are the cornerstones of the management of foot ulcers. Assessing the progress of foot ulcers can be a challenge for the clinician and patient due to logistic issues such as regular attendance in the clinic. Foot clinics are often busy and because of manpower issues, ulcer reviews can be delayed with detrimental effects on the healing as a result of a lack of appropriate and timely changes in management. Wound photographs have been historically useful to assess the progress of diabetic foot ulcers over the past few decades. Mobile phones with digital cameras have recently revolutionized the capture of foot ulcer images. Patients can send ulcer photographs to diabetes care professionals electronically for remote monitoring, largely avoiding the logistics of patient transport to clinics with a reduction on clinic pressures. Artificial intelligence-based technologies have been developed in recent years to improve this remote monitoring of diabetic foot ulcers with the use of mobile apps. This is expected to make a huge impact on diabetic foot ulcer care with further research and development of more accurate and scientific technologies in future. This clinical update review aims to compile evidence on this hot topic to empower clinicians with the latest developments in the field.
Keywords: Diabetic foot ulcers, Photographic monitoring, Artificial intelligence technology, Digital photography, Mobile app, COVID-19 pandemic
Core Tip: Diabetic foot clinics faced major challenges during the COVID-19 pandemic due to lockdowns and social distancing measures as a significant proportion of patients were unable to physically attend the clinics. This situation boosted the attempts for transition of face-to-face foot clinics to virtual clinics as in many other types of medical care during the pandemic. Monitoring of diabetic foot ulcers (DFUs) by digital photographic technology and mobile phone-based photography have revolutionized this area of clinical care in recent years and mobile apps are expected to accelerate this progress. This article reviews the past, the present and the future of artificial intelligence technology in the care of DFUs.
INTRODUCTION
Foot ulceration caused by micro- and/or macrovascular disease is a common complication of diabetes mellitus (DM). The global prevalence of diabetic foot ulcers (DFUs) at any point in time is estimated to be 6.3%[1], with 25% of DM patients developing a DFU in their lifetime[2]. DFUs significantly increase morbidity [including lower extremity amputations (LEA)] and mortality among sufferers, and the care of DFUs poses very high healthcare expenditure worldwide. Approximately 50% of DFUs are associated with infections[3], and approximately 20% of moderate to severe DFU infections may lead to minor or major amputations[4]. DFU-related LEA is associated with a 10-year survival rate as low as 24% which is lower than that of several forms of cancers[5]. These alarming figures give us a broad outline of the health-related risks posed by DFUs.
Appropriate care of DFUs to ensure rapid cure and avoid complications involves regular monitoring of the progress of healing with periodic review of the ulcers, frequent dressing changes, antibiotic therapy for infection control, optimal control of DM, and adequate offloading of the ulcers to avoid ongoing damage due to pressure on the wound area. Diabetic foot clinics usually provide comprehensive DFU care by multidisciplinary specialist teams involving podiatrists, orthotists (who make appropriate footwear/devices for offloading the DFU), diabetes specialist nurses, and diabetologists. However, insufficient manpower, long clinic waiting lists, and logistic issues with patient transport to the clinics can all pose problems for timely review of patients with DFUs in the foot clinics. Manpower shortage resulting in longer waiting periods prior to review by the footcare team has been a major issue in ulcer care in diabetes foot services across the world in recent years[6,7]. Delays in presentation for foot ulcer review have been identified as an important reason for wound non-healing[8]. Complications of foot ulcers including amputations can be the devastating sequel of such delays in review by the footcare team.
The COVID-19 pandemic posed major challenges in DFU care across the globe due the above reasons[9-11]. Delays in ulcer reviews may be associated with detrimental effects on DFU healing that may even lead to amputations[10,11]. Telephone and video clinics during the pandemic period helped clinicians to address some of the issues related to the inability of patients to attend medical clinics during the COVID-19 lock-down period. Attempts to develop artificial intelligence (AI) algorithms by the scientific fraternity to enhance patient care through virtual clinics attained greater momentum in relation to the pandemic[12,13].
Monitoring the progress of DFUs by comparing serial ulcer photographs during the follow-up in foot clinics has been practiced by many diabetologists over the past 2-3 decades. Refinement of the photographic methods by sophisticated digital technology and mobile phone cameras have revolutionized DFU care in recent years[14-16]. Some patients often use mobile phone cameras to capture their foot ulcer photographs for self-monitoring wound progress and to help clinicians to understand the previous status of their wound during clinic review.
However, much more multidisciplinary scientific research input and output are necessary in this area. Further refinement of this rapidly advancing digital technology for optimal use in day-to-day clinical practice could result in better care of patients with DFUs. This review attempts to gather up-to-date evidence to summarise the past, present, and future dimensions of AI algorithms to empower clinicians across the globe to appropriately utilise digital technology for DFU care.
PHOTOGRAPHIC MONITORING OF DFU PROGRESS
Diabetes care professionals often see several cases of DFU in their day-to-day clinical practice and often forget the previous ulcer grade, character and even the site during subsequent visits, weeks later when followed up in the foot clinic. Review of the previous photographs during subsequent follow-up visits should provide clinicians with a good clinical assessment of the progress of the ulcer and help prognostication[17]. Photographic monitoring also enhances appropriate continuity of care by different clinicians running the diabetic foot services during their review of the same case.
Important issues which can arise while comparing the photographs are the differences in the distance from which photographs are captured (can be largely avoided by placing a measuring tape on the ulcer while photographed), differences in the illumination of pictures from brightness of background light when the photographs were taken, and the likelihood of low-quality images without adequate focusing of cameras by individuals taking the picture. Photographs are usually taken without flashlight to avoid undue illumination that can reduce the picture quality. Clinical evidence suggests that prediction of ulcer healing is possible by regular photographic monitoring[17]. Figure 1 shows the photographic monitoring of the progress of a DFU at various stages.
Figure 1.
Photographic monitoring of the progress of a DFU at various stages. A: Infected foot ulcer on April 25, 2022; B: After 2 mo of regular offloading and dressings (on June 28, 2022) with initial 3 wk of antibiotic therapy; C: Further improvement of ulcer on July 23, 2022: D: Complete healing of ulcer on August 22, 2022.
HISTORY OF DIGITAL ARCHIVING OF THE DFU PHOTOGRAPHS
Use of digital cameras for photography has become a common practice since the early 1980s after the invention of digital photographic technology in 1975. Digital archiving of foot ulcer photographs in computer databases was a great leap forward in the technology for monitoring DFUs. Print outs of foot ulcer photographs are still used in remote settings where internet and computers are not freely available in clinical practice. This is in fact more expensive (costs incurred with colour printing and use of good quality photographic paper) and cumbersome in the modern era.
Fading of the colour print outs over time makes the situation worse regarding DFU monitoring using this method. A review of the serial images in the computer database of digital photographs makes the work of diabetes foot care professionals much easier when this facility is available[18]. Lack of degradation of image quality over time as in printed photographs is another great advantage of digital archiving of DFU images.
Mobile phones became popular for telephone communications globally in the early 2000s and newer versions of these devices with cameras and video recording facilities came into the market a few years later. With rapid advancements in technology, smartphone devices using high resolution cameras are now widely available and have become an integral part of modern life in the 21st century. Diabetes care professionals soon started using mobile phone cameras and video facilities for the monitoring and management of DFUs[19-21]. Some patients themselves were using mobile phones to obtain images of their DFUs prior to their foot clinic visits so that they could show the status of their ulcers earlier. Although the initial studies on use of mobile phones for monitoring DFUs were not very promising[22], subsequent studies show encouraging results[23-25].
INTEGRATING DFU PHOTOGRAPHS WITH COMPUTER-BASED DIGITAL TECHNOLOGY FOR DIAGNOSTICS
AI and its applications have been utilised in various branches of modern science and technology including the medical field over the past few decades to improve physical and intellectual human work output. Such technologies can also be utilised to monitor the progress in DFU care. DFU datasets were utilised for training and testing the machine learning processes. The collection of such datasets supports the ongoing research for DFU academic AI challenges, such as those hosted by the Medical Image Computing and Computer Assisted Interventions (MICCAI) conferences[26,27]. These challenges are used to promote and advance ongoing research and to increase exposure within the associated academic fields.
Machine learning algorithms have been found to be very useful in detecting DFUs with high accuracy rates in previous studies[28-30]. These algorithms are developed by using large datasets of images captured from the foot clinics. The development of computer-aided DFU diagnostic algorithms involves multiple stages such as pre-processing, feature extraction, detection, classification, and segmentation of DFU wounds[30]. These tasks can be challenging in real-world settings due to the low-quality of images from inadequate focusing, motion artifacts, inadequate lighting, and backlight, deformities in the foot/toes, size and shape of the ulcers (very small, very large and curved ulcers), and newly formed or early ulcers which are easily missed during the capture of photographs in foot clinics[16].
The first and foremost step in the development of machine learning algorithms is the detection of DFUs from foot photographs. This task has been successfully carried out by previous researchers as mentioned above[28-30]. Further refinement of machine learning is currently being undertaken by incorporating the classification systems for DFUs, as in the real-world settings, to promote AI-based diagnostics and prognostication. Several manual DFU classification systems are currently used by foot care professionals such as Wagner, University of Texas, and SINBAD (Site, Ischaemia, Neuropathy, Bacterial infection, Area, and Depth) for DFU monitoring and management[30]. These manual approaches may benefit from the automated processes afforded by AI.
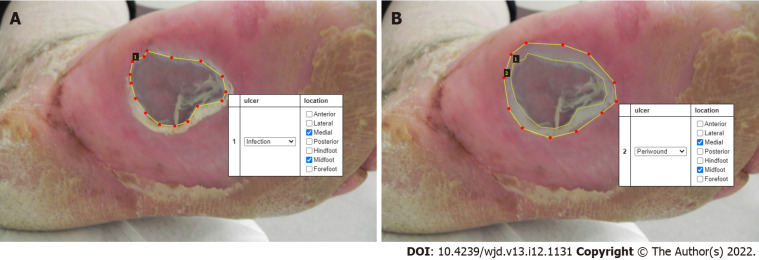
Incorporation of such complex features in the AI-technology for day-to-day clinical practice to enhance diagnosis and prognostication can be challenging. These challenges include: (1) The significant time-burden involved in the DFU image data collection and appropriate labelling; (2) The inter- and intra-class variations depending on differences in the classification of DFUs; (3) Lack of standardization of DFU datasets (caused by camera distance from the foot, image orientation and lighting conditions); and (4) The differences in ethnicity, age, sex, and foot size of the patients[30]. Development of deep learning AI algorithms requires large-scale datasets for automated DFU analysis to reproduce comparable results to those by experts. Researchers currently working in isolation may not achieve reproducible research outputs. Large DFU datasets used for training and validation by multiple professionals from different institutions across the globe should help to refine these pitfalls in machine learning algorithms for DFU classification and diagnosis. To enable innovation from clinicians and researchers, Yap et al[26] proposed the diabetic foot ulcer challenges by providing the publicly available datasets, for comprehensive evaluation of object detection frameworks on DFU detection using convolutional neural networks trained on the DFUC2020 dataset[15]. Examples of manually delineated DFU photographs from the training set are shown in Figure 2. Morphological classification of DFUs into different types (such as infection, ischaemia, both, and none) is carried out in these datasets to enable machine learning.
Figure 2.
An infected ulcer on the plantar aspect of the left foot. A: The ulcer is labelled (dotted line marking the boundaries) for the training set. The white box shows the site and type of ulcer. B: The peri-wound of the ulcer is labelled with a dotted line. The white box shows the site of the ulcer and the peri-wound.
SERIAL DEMARCATION OF ULCER PHOTOGRAPHS TO ASSESS PROGRESS OF DFU HEALING
At present, monitoring the healing process of DFUs is largely completed by regular patient follow-up visits in the multidisciplinary foot clinics[31-33]. Since 2020, the COVID-19 pandemic has made a huge impact on DFU care across the world due to the issues related to lockdowns and social distancing measures enforced by governments to curtail human devastation as a result of the global health emergency. Foot clinic attendance[34] and hospitalisations for DFUs[35] were significantly reduced during the pandemic. Although worsening of DFUs was comparatively less owing to reduced outdoor human activity[36], many patients presented to clinicians late, increasing the risk of complications from DFUs[35,37]. The pandemic reinforced the urgent necessity to develop AI-based wound care algorithms for remote monitoring of DFUs.
To enable the development of machine learning algorithms, serial demarcation of DFUs is important to assess the progress of the healing process along with wound classification based on one of the above-mentioned standard systems. Therefore, characterisation of DFUs requires demarcation of wounds at various stages in the datasets by experts in the field after which the data can be used for training, validation, and testing. This task is highly labour-intensive and requires huge DFU training and validation datasets.
PHOTOGRAPHS ACQUIRED BY MOBILE PHONE CAMERAS FOR DFU MONITORING
New generation mobile phones can capture high resolution DFU photographs comparable to commercial digital cameras. Many patients already use mobile phone photography for self-monitoring their DFUs[14,22]. Some patients serially document their wound progress using these images and meticulously bring them to foot clinics during their follow-up visits for DFU care. Occasionally, patients send their photographs to footcare professionals electronically or as email attachments. Although safety issues related to secure transfer of such clinical information without breach of confidentiality can be challenging at present, wider use of mobile phone photography for self-monitoring of DFUs progress might revolutionise future foot care.
DEVELOPMENT OF MOBILE APPS FOR DFU MONITORING
Various mobile phone apps are currently used worldwide in many domains of daily activities to improve the quality of human life. Such mobile apps for DFU monitoring and care are under development. Cassidy et al[38] developed the first mobile app capable of accurate DFU detection using AI and cloud-based technologies. This system was tested in a 6-mo clinical evaluation at two UK National Health Service hospital sites (Lancashire Teaching Hospitals and Salford Royal Hospital) and is currently being further developed to improve functionality and accuracy. Additional app features, such as automated classification of DFU wound pathology[39] and automated delineation of wou-nd/peri-wound regions are also being investigated to provide a more clinically relevant system.
These new technological advancements are expected to revolutionise remote wound care by enabling patients to self-monitor their DFUs and contact clinicians when they find any concern or deterioration of their disease. This would also enhance flexibility in the functioning of foot clinics by reviewing and triaging the most appropriate DFUs to be seen in the clinics by remote monitoring of patients.
PREDICTION OF DFU PROGRESS BY INTEGRATION OF CLINICAL AND BIOCHEMICAL PARAMETERS AND ULCER PHOTOGRAPHS
Although regular wound care with dressings, appropriate antibiotic therapy for infections, offloading the ulcers to relieve pressure-related delay in healing and revascularisation of the ischaemic foot are the cornerstones in the management of DFUs, several other clinical (comorbid conditions such as renal disease, heart failure, and immunosuppressed states) and biochemical parameters (such as hyperglycaemia, anaemia, and high haemoglobin A1c) may impact the DFU healing process[40-44]. Integration of these clinical and biochemical parameters into machine learning algorithms should help us to develop prediction models using AI technology.
We note however that the development of such algorithms is much more labour-intensive as demarcation exercises to develop deep learning models require larger datasets with clinical and biochemical parameters of individual patients incorporated within the neural network. However, appropriate use of computer technology integrated with digital applications can help to reduce the physical burden on researchers in developing such models.
FUTURE PERSPECTIVES
Recent research has investigated the utilisation of patient data in the training of deep neural networks in various medical imaging domains[45]. These studies indicate that machine learning models trained on patient data can be used to boost the performance of convolutional neural networks trained on wound/lesion images. Research of this nature is ongoing and represents a way to incorporate a more integrated method of wound analysis that considers multiple data points. The development of mobile apps integrating such new advancements in technology is expected to revolutionise the global scenario of DFU care in the near future.
CONCLUSION
Digital applications in the daily management of DFUs have evolved rapidly in recent years to a level of remote diagnosis and monitoring of wounds in community settings. The COVID-19 pandemic has accelerated research and development of such innovative technological applications in the past two years. Photographic monitoring of foot ulcers has been practiced in many centres across the world in the past few decades providing DFU care. The invention of digital photographic technology in 1975 further boosted DFU care because of the ease of electronic archiving of ulcer images during clinical follow-up. Photography using mobile phone cameras has become a huge leap forward in this direction in recent years empowering patients and clinicians to further improve DFU care.
AI-based digital algorithms are currently being developed rapidly through collaborative global effort between AI experts and clinical teams. Mobile camera-based digital technologic applications are under development to enhance remote diagnosis, monitoring, and follow-up care of DFUs. Prediction models of wound healing are also under development now making use of linking the ulcer characteristics of DFU images to the clinical and laboratory parameters of diabetic patients. These collaborative efforts between clinicians and computer scientists across the world should revolutionise such discoveries to empower diabetic foot patients to self-monitor and manage their DFUs to a greater extent.
Footnotes
Conflict-of-interest statement: All authors report no relevant conflict of interest for this article.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Peer-review started: August 25, 2022
First decision: October 30, 2022
Article in press: December 1, 2022
Specialty type: Endocrinology and metabolism
Country/Territory of origin: United Kingdom
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mijwil MM, Iraq; Mostafavinia A, Iran; Wu QN, China S-Editor: Liu GL L-Editor: Webster JR P-Editor: Liu GL
Contributor Information
Joseph M Pappachan, Department of Endocrinology & Metabolism, Lancashire Teaching Hospitals NHS Trust, Preston PR2 9HT, United Kingdom; Faculty of Science and Engineering, Manchester Metropolitan University, Manchester M15 6BH, United Kingdom. drpappachan@yahoo.co.in.
Bill Cassidy, Faculty of Science and Engineering, Manchester Metropolitan University, Manchester M15 6BH, United Kingdom.
Cornelius James Fernandez, Department of Endocrinology & Metabolism, Pilgrim Hospital, Boston PE21 9QS, United Kingdom.
Vishnu Chandrabalan, Department of Data Science, Lancashire Teaching Hospitals NHS Trust, Preston PR2 9HT, United Kingdom.
Moi Hoon Yap, Faculty of Science and Engineering, Manchester Metropolitan University, Manchester M15 6BH, United Kingdom.
References
- 1.Zhang P, Lu J, Jing Y, Tang S, Zhu D, Bi Y. Global epidemiology of diabetic foot ulceration: a systematic review and meta-analysis †. Ann Med. 2017;49:106–116. doi: 10.1080/07853890.2016.1231932. [DOI] [PubMed] [Google Scholar]
- 2.Du F, Ma J, Gong H, Bista R, Zha P, Ren Y, Gao Y, Chen D, Ran X, Wang C. Microbial Infection and Antibiotic Susceptibility of Diabetic Foot Ulcer in China: Literature Review. Front Endocrinol (Lausanne) 2022;13:881659. doi: 10.3389/fendo.2022.881659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hurlow JJ, Humphreys GJ, Bowling FL, McBain AJ. Diabetic foot infection: A critical complication. Int Wound J. 2018;15:814–821. doi: 10.1111/iwj.12932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lipsky BA, Berendt AR, Cornia PB, Pile JC, Peters EJ, Armstrong DG, Deery HG, Embil JM, Joseph WS, Karchmer AW, Pinzur MS, Senneville E Infectious Diseases Society of America. 2012 Infectious Diseases Society of America clinical practice guideline for the diagnosis and treatment of diabetic foot infections. Clin Infect Dis. 2012;54:e132–e173. doi: 10.1093/cid/cis346. [DOI] [PubMed] [Google Scholar]
- 5.Soo BP, Rajbhandari S, Egun A, Ranasinghe U, Lahart IM, Pappachan JM. Survival at 10 years following lower extremity amputations in patients with diabetic foot disease. Endocrine. 2020;69:100–106. doi: 10.1007/s12020-020-02292-7. [DOI] [PubMed] [Google Scholar]
- 6.Normahani P, Mustafa C, Standfield NJ, Duguid C, Fox M, Jaffer U. Management of peripheral arterial disease in diabetes: a national survey of podiatry practice in the United Kingdom. J Foot Ankle Res. 2018;11:29. doi: 10.1186/s13047-018-0270-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Leong Tan GW, Chandrasekar S, Lo ZJ, Hong Q, Yong E, Lingam P, Zhang L, Quek LHH, Pua U. Early experience in the COVID-19 pandemic from a vascular surgery unit in a Singapore tertiary hospital. J Vasc Surg. 2020;72:12–15. doi: 10.1016/j.jvs.2020.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mbela Lusendi F, Matricali GA, Vanherwegen AS, Doggen K, Nobels F. Bottom-up approach to build a 'precision' risk factor classification for diabetic foot ulcer healing. Proof-of-concept. Diabetes Res Clin Pract. 2022;191:110028. doi: 10.1016/j.diabres.2022.110028. [DOI] [PubMed] [Google Scholar]
- 9.Kleibert M, Mrozikiewicz-Rakowska B, Bąk PM, Bałut D, Zieliński J, Czupryniak L. Breakdown of Diabetic Foot Ulcer Care during the First Year of the Pandemic in Poland: A Retrospective National Cohort Study. Int J Environ Res Public Health. 2022;19 doi: 10.3390/ijerph19073827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lozano-Corona R, Reyes-Monroy JA, Lara-González V, Anaya-Ayala JE, Dardik A, Hinojosa CA. Revascularization prevents amputation among patients with diabetic foot during the COVID-19 era. Vascular. 2022:17085381221079108. doi: 10.1177/17085381221079108. [DOI] [PubMed] [Google Scholar]
- 11.Yunir E, Tarigan TJE, Iswati E, Sarumpaet A, Christabel EV, Widiyanti D, Wisnu W, Purnamasari D, Kurniawan F, Rosana M, Anestherita F, Muradi A, Tahapary DL. Characteristics of Diabetic Foot Ulcer Patients Pre- and During COVID-19 Pandemic: Lessons Learnt From a National Referral Hospital in Indonesia. J Prim Care Community Health. 2022;13:21501319221089767. doi: 10.1177/21501319221089767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Huang JA, Hartanti IR, Colin MN, Pitaloka DA. Telemedicine and artificial intelligence to support self-isolation of COVID-19 patients: Recent updates and challenges. Digit Health. 2022;8:20552076221100634. doi: 10.1177/20552076221100634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brahmbhatt DH, Ross HJ, Moayedi Y. Digital Technology Application for Improved Responses to Health Care Challenges: Lessons Learned From COVID-19. Can J Cardiol. 2022;38:279–291. doi: 10.1016/j.cjca.2021.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kuang B, Pena G, Szpak Z, Edwards S, Battersby R, Cowled P, Dawson J, Fitridge R. Assessment of a smartphone-based application for diabetic foot ulcer measurement. Wound Repair Regen. 2021;29:460–465. doi: 10.1111/wrr.12905. [DOI] [PubMed] [Google Scholar]
- 15.Cassidy B, Reeves ND, Pappachan JM, Gillespie D, O'Shea C, Rajbhandari S, Maiya AG, Frank E, Boulton AJ, Armstrong DG, Najafi B, Wu J, Kochhar RS, Yap MH. The DFUC 2020 Dataset: Analysis Towards Diabetic Foot Ulcer Detection. touchREV Endocrinol. 2021;17:5–11. doi: 10.17925/EE.2021.17.1.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yap MH, Hachiuma R, Alavi A, Brüngel R, Cassidy B, Goyal M, Zhu H, Rückert J, Olshansky M, Huang X, Saito H, Hassanpour S, Friedrich CM, Ascher DB, Song A, Kajita H, Gillespie D, Reeves ND, Pappachan JM, O'Shea C, Frank E. Deep learning in diabetic foot ulcers detection: A comprehensive evaluation. Comput Biol Med. 2021;135:104596. doi: 10.1016/j.compbiomed.2021.104596. [DOI] [PubMed] [Google Scholar]
- 17.Lavery LA, Barnes SA, Keith MS, Seaman JW Jr, Armstrong DG. Prediction of healing for postoperative diabetic foot wounds based on early wound area progression. Diabetes Care. 2008;31:26–29. doi: 10.2337/dc07-1300. [DOI] [PubMed] [Google Scholar]
- 18.Cabal Mirabal CA, Berlanga Acosta J, Fernández Montequín J, Oramas Díaz L, González Dalmau E, Herrera Martínez L, Sauri JE, Baldomero Hernández J, Savigne Gutiérrez W, Valdés JL, Tabio Reyes AL, Pérez Pérez SC, Valdés Pérez C, Armstrong AA, Armstrong DG. Quantitative Studies of Diabetic Foot Ulcer Evolution Under Treatment by Digital Stereotactic Photography. J Diabetes Sci Technol. 2019;13:821–826. doi: 10.1177/1932296819853843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Larsen SB, Clemensen J, Ejskjaer N. A feasibility study of UMTS mobile phones for supporting nurses doing home visits to patients with diabetic foot ulcers. J Telemed Telecare. 2006;12:358–362. doi: 10.1258/135763306778682323. [DOI] [PubMed] [Google Scholar]
- 20.Foltynski P, Ladyzynski P, Wojcicki JM. A new smartphone-based method for wound area measurement. Artif Organs. 2014;38:346–352. doi: 10.1111/aor.12169. [DOI] [PubMed] [Google Scholar]
- 21.Wang L, Pedersen PC, Strong DM, Tulu B, Agu E, Ignotz R. Smartphone-based wound assessment system for patients with diabetes. IEEE Trans Biomed Eng. 2015;62:477–488. doi: 10.1109/TBME.2014.2358632. [DOI] [PubMed] [Google Scholar]
- 22.van Netten JJ, Clark D, Lazzarini PA, Janda M, Reed LF. The validity and reliability of remote diabetic foot ulcer assessment using mobile phone images. Sci Rep. 2017;7:9480. doi: 10.1038/s41598-017-09828-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pak C, In Jeon J, Kim H, Kim J, Park S, Ahn KH, Son YJ, Yoo S, Baek RM, Jeong JH, Heo CY. A smartphone-based teleconsultation system for the management of chronic pressure injuries. Wound Repair Regen. 2018;26 Suppl 1:S19–S26. doi: 10.1111/wrr.2. [DOI] [PubMed] [Google Scholar]
- 24.Ploderer B, Brown R, Seng LSD, Lazzarini PA, van Netten JJ. Promoting Self-Care of Diabetic Foot Ulcers Through a Mobile Phone App: User-Centered Design and Evaluation. JMIR Diabetes. 2018;3:e10105. doi: 10.2196/10105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kim RB, Gryak J, Mishra A, Cui C, Soroushmehr SMR, Najarian K, Wrobel JS. Utilization of smartphone and tablet camera photographs to predict healing of diabetes-related foot ulcers. Comput Biol Med. 2020;126:104042. doi: 10.1016/j.compbiomed.2020.104042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yap MH, Kendrick C, Reeves ND, Goyal M, Pappachan JM, Cassidy B. Development of Diabetic Foot Ulcer Datasets: An Overview. DFUC 2021. Lecture Notes in Computer Science. Springer, Cham. 2022; 13183. Available from: https://link.springer.com/chapter/10.1007/978-3-030-94907-5_1 .
- 27.Cassidy B, Kendrick C, Reeves ND, Pappachan , JM , O’Shea C, Armstrong D, Yap , MH Diabetic Foot Ulcer Grand Challenge 2021: Evaluation and Summary. DFUC 2021. Lecture Notes in Computer Science. Springer, Cham. 2022; 13183. Available from: https://link.springer.com/chapter/10.1007/978-3-030-94907-5_7 .
- 28.Wang C, Yan X, Smith M, Kochhar K, Rubin M, Warren SM, Wrobel J, Lee H. A unified framework for automatic wound segmentation and analysis with deep convolutional neural networks. Annu Int Conf IEEE Eng Med Biol Soc . 2015;2015:2415–2418. doi: 10.1109/EMBC.2015.7318881. [DOI] [PubMed] [Google Scholar]
- 29.Al-Garaawi N, Ebsim R, Alharan AFH, Yap MH. Diabetic foot ulcer classification using mapped binary patterns and convolutional neural networks. Comput Biol Med. 2021;140:105055. doi: 10.1016/j.compbiomed.2021.105055. [DOI] [PubMed] [Google Scholar]
- 30.Goyal M, Reeves ND, Rajbhandari S, Ahmad N, Wang C, Yap MH. Recognition of ischaemia and infection in diabetic foot ulcers: Dataset and techniques. Comput Biol Med. 2020;117:103616. doi: 10.1016/j.compbiomed.2020.103616. [DOI] [PubMed] [Google Scholar]
- 31.Malone M, Schwarzer S, Walsh A, Xuan W, Al Gannass A, Dickson HG, Bowling FL. Monitoring wound progression to healing in diabetic foot ulcers using three-dimensional wound imaging. J Diabetes Complications. 2020;34:107471. doi: 10.1016/j.jdiacomp.2019.107471. [DOI] [PubMed] [Google Scholar]
- 32.Chan KS, Lo ZJ. Wound assessment, imaging and monitoring systems in diabetic foot ulcers: A systematic review. Int Wound J. 2020;17:1909–1923. doi: 10.1111/iwj.13481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chen P, Carville K, Swanson T, Lazzarini PA, Charles J, Cheney J, Prentice J Australian Diabetes-related Foot Disease Guidelines & Pathways Project. Australian guideline on wound healing interventions to enhance healing of foot ulcers: part of the 2021 Australian evidence-based guidelines for diabetes-related foot disease. J Foot Ankle Res. 2022;15:40. doi: 10.1186/s13047-022-00544-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zayed H, Musajee M, Thulasidasan N, Sayed M, Francia F, Green M, Arissol M, Lakhani A, Biasi L, Patel S. Impact of COVID-19 Pandemic on the Outcomes in Patients With Critical Limb Threatening Ischaemia and Diabetic Foot Infection. Ann Surg. 2022;275:1037–1042. doi: 10.1097/SLA.0000000000004677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mariet AS, Benzenine E, Bouillet B, Vergès B, Quantin C, Petit JM. Impact of the COVID-19 Epidemic on hospitalization for diabetic foot ulcers during lockdown: A French nationwide population-based study. Diabet Med. 2021;38:e14577. doi: 10.1111/dme.14577. [DOI] [PubMed] [Google Scholar]
- 36.Bonnet JB, Macioce V, Jalek A, Bouchdoug K, Elleau C, Gras-Vidal MF, Pochic J, Avignon A, Sultan A. Covid-19 lockdown showed a likely beneficial effect on diabetic foot ulcers. Diabetes Metab Res Rev. 2022;38:e3520. doi: 10.1002/dmrr.3520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Liu C, You J, Zhu W, Chen Y, Li S, Zhu Y, Ji S, Wang Y, Li H, Li L, Fan S. The COVID-19 Outbreak Negatively Affects the Delivery of Care for Patients With Diabetic Foot Ulcers. Diabetes Care. 2020;43:e125–e126. doi: 10.2337/dc20-1581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cassidy B, Reeves ND, Pappachan JM, Ahmad M, Haycocks M, Gillespie D, Yap MH. A Cloud-Based Deep Learning Framework for Remote Detection of Diabetic Foot Ulcers. IEEE Pervasive Computing 2022; 21: 78-86. [Google Scholar]
- 39.Yap MH, Cassidy B, Pappachan JM, Shea CO, Gillespie D, Reeves ND. Analysis Towards Classification of Infection and Ischaemia of Diabetic Foot Ulcers. 2021 IEEE EMBS International Conference on Biomedical and Health Informatics (BHI); 2021 July 27-30; Athens, Greece. [Google Scholar]
- 40.Gazzaruso C, Gallotti P, Pujia A, Montalcini T, Giustina A, Coppola A. Predictors of healing, ulcer recurrence and persistence, amputation and mortality in type 2 diabetic patients with diabetic foot: a 10-year retrospective cohort study. Endocrine. 2021;71:59–68. doi: 10.1007/s12020-020-02431-0. [DOI] [PubMed] [Google Scholar]
- 41.Felipe RR, Plata-Que MT. Predictors of Outcomes of Foot Ulcers among Individuals with Type 2 Diabetes Mellitus in an Outpatient Foot Clinic. J ASEAN Fed Endocr Soc. 2021;36:189–195. doi: 10.15605/jafes.036.02.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ezeani IU, Ugwu ET, Adeleye FO, Gezawa ID, Okpe IO, Enamino MI. Determinants of wound healing in patients hospitalized for diabetic foot ulcer: results from the MEDFUN study. Endocr Regul. 2020;54:207–216. doi: 10.2478/enr-2020-0023. [DOI] [PubMed] [Google Scholar]
- 43.Caruso P, Longo M, Gicchino M, Scappaticcio L, Caputo M, Maiorino MI, Bellastella G, Esposito K. Long-term diabetic complications as predictors of foot ulcers healing failure: A retrospective study in a tertiary-care center. Diabetes Res Clin Pract. 2020;163:108147. doi: 10.1016/j.diabres.2020.108147. [DOI] [PubMed] [Google Scholar]
- 44.Sørensen MLB, Jansen RB, Wilbek Fabricius T, Jørgensen B, Svendsen OL. Healing of Diabetic Foot Ulcers in Patients Treated at the Copenhagen Wound Healing Center in 1999/2000 and in 2011/2012. J Diabetes Res. 2019;2019:6429575. doi: 10.1155/2019/6429575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jaworek-Korjakowska J, Brodzicki A, Cassidy B, Kendrick C, Yap MH. Interpretability of a Deep Learning Based Approach for the Classification of Skin Lesions into Main Anatomic Body Sites. Cancers (Basel) . 2021;13 doi: 10.3390/cancers13236048. [DOI] [PMC free article] [PubMed] [Google Scholar]