Abstract
Diabetic foot ulcer is a devastating complication of diabetes mellitus and significant cause of mortality and morbidity all over the world and can be complex and costly. The development of foot ulcer in a diabetic patient has been estimated to be 19%-34% through their lifetime. The pathophysiology of diabetic foot ulcer consist of neuropathy, trauma and, in many patients, additional peripheral arterial disease. In particular, diabetic neuropathy leads to foot deformity, callus formation, and insensitivity to trauma or pressure. The standard algorithms in diabetic foot ulcer management include assessing the ulcer grade classification, surgical debridement, dressing to facilitate wound healing, off-loading, vascular assessment (status and presence of a chance for interventional vascular correction), and infection and glycemic control. Although especially surgical procedures are sometimes inevitable, they are poor predictive factors for the prognosis of diabetic foot ulcer. Different novel treatment modalities such as nonsurgical debridement agents, oxygen therapies, and negative pressure wound therapy, topical drugs, cellular bioproducts, human growth factors, energy-based therapies, and systematic therapies have been available for patients with diabetic foot ulcer. However, it is uncertain whether they are effective in terms of promoting wound healing related with a limited number of randomized controlled trials. This review aims at evaluating diabetic foot ulcer with regard to all aspects. We will also focus on conventional and novel adjunctive therapy in diabetic foot management.
Keywords: Diabetic foot ulcer, Peripheric artery disease, Macrovascular complications, Neuropathy, Wagner classification, Intralesionar growth factor treatment
Core Tip: Diabetic foot ulcers (DFU) are one of the most common problems and devastating complications of diabetes, and affect 15% of all diabetic patients and result in significant morbidity, mortality, and financial burdens. The management of DFU is usually complex and challenging to clinicians in clinical practice. This review article aims at summarizing the etiopathogenesis and classification of DFU. It also highlights novel adjunctive treatment modalities as well as conventional management for DFU.
INTRODUCTION
Diabetic foot ulcers (DFU) are common clinical problems and devastating complications of diabetes, and affect 15% of all diabetic patients and results in significant morbidity, mortality, and financial burdens[1]. Five-year risk of mortality for a patient with diabetic foot ulcer is 2.5 times higher than the risk for a patient without[2]. Approximately 20% of moderate or severe DFU could cause some level of amputation. Moreover, 74% of them also have a risk of renal replacement therapy at 2 years[3]. This high mortality rate is also related with coexisting comorbidities such as cardiovascular or cerebro-vascular diseases.
The pathophysiology of DFU is based on a triad of neuropathy, peripheral arterial disease, and concomitant secondary bacterial infection. Peripheral neuropathy could lead to intrinsic muscle atrophy and functional anatomical changes in the foot[4]. Eventually, progressive secondary foot infection penetrating deep facia, tendons, and joints could develop with repetitive inattention trauma. Infection could play a significant role for half of major lower limb extremity amputations. Recent studies indicate some risk factors for the development of DFU. These are as follows: Longer than 10 years of duration of diabetes, male gender, older patients, presence of comorbidities including nephropathy, neuropathy, and peripheral vascular disease, and history of foot ulceration[4-6].
The management of DFU is usually complex and challenging to clinicians in clinical practice. Costs of diabetic foot ulcerations have been increased to the treatment cost of many common cancers. Estimated costs of DFU management are greater than 1 billion in both developed and developing countries. Therefore, foot ulcers should be treated immediately by a multidisciplinary expert team for optimal outcomes. The treatment of DFU requires an immediate decision and systematic approach that comprises of maintaining arterial blood flow, treating the infection appropriately, and removing the pressure from the wound[7]. In addition, several adjuvant therapies are becoming a popular form of diabetic foot treatment. During the past 10 years, there has been an increasing amount of novel, basic science-based approaches and developments for adjuvant therapies including wound dressing, hyperbaric oxygen therapy, or growth factor formulations for efficient local delivery[8-10]. None of them had definitive results that improved wound healing and these approaches still need clinical validation.
The review highlights novel adjunctive treatment modalities as well as conventional management for DFU.
PATHOPHYSIOLOGY
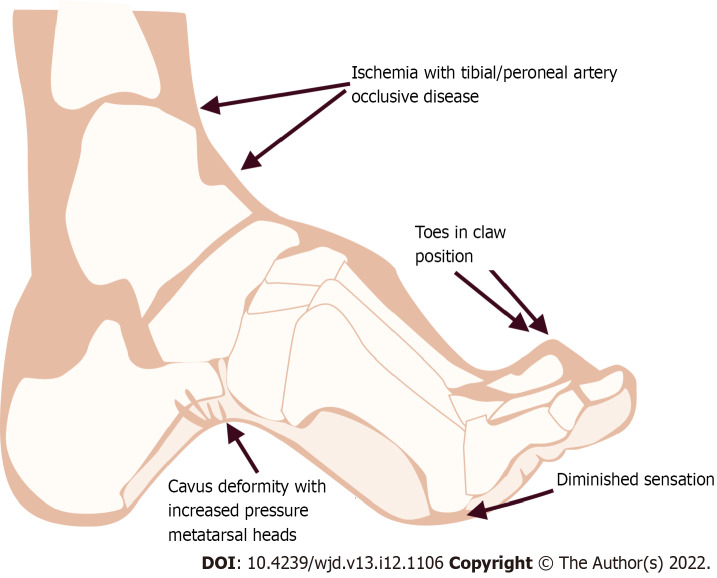
DFU is a serious result of risk factors including neuropathy, peripheral arterial disease, and secondary infection. Peripheral neuropathy could play a major role by producing intrinsic muscle atrophy and consequently leading to biomechanical anatomical changes on the feet such as hammer-toe formation, pes-planus, and pes-cavus, which lead to high-pressure zones of the foot[11,12] (Figure 1).
Figure 1.
Ethiopathogenesis of diabetic foot leading to vascular complications.
Diabetic neuropathy and foot ulcer
Diabetic neuropathy has multiple manifestations within the diabetic foot because it comprises sensory, motor, and autonomic fibers. The majority of patients with diabetes (66%) face peripheral neuropathy in the lower extremities[12]. Especially distal sensory neuropathy, the most type seen of all diabetic neuropathies, is a major risk factor for DFU but it is extremely variable, as it ranges from severely painful symptoms to a completely painless variety that may present with an insensitive foot ulcer[13]. Diabetic peripheral neuropathy mainly affects lower legs and the feet as a stocking-glowing distribution and it could cause the loss of the Achilles reflex which can be the first sign of these changes. The anatomy of the foot arch could change with the atrophy of the lumbricals and interosseus muscles and a relative increase in the extensor tendon forces called “claw” deformity in the toes[14]. On the other hand, the onset of sensory neuropathy can manifest as loss of proprioception, pressure sensation, vibratory perception, and impaired gait[15]. Sensory neuropathy usually progresses gradually with the insidious appearance of symptoms that may be intermittent in the early stage. C-type fiber, which is a responsible for the sensorial transmission, results in inappropriate reaction to a painful stimulus[16]. Ulceration and infection could occur with repetitive trauma, and decreased sensation and proprioception could also predispose skin injury by producing atrophy and dislocation of protective plantar fat pads. Moreover sudomotor dysfunction could develop with diabetic autonomous neuropathy and it is also associated with foot ulceration due to dry skin and itching[17]. Several methods are developed to evaluate the sudomotor function. They are thermoregulatory sweat testing, quantitative sudomotor axon reflex, quantitative direct and indirect reflex test, and indicator plaster[18-20]. Among of them, indicator plaster represents a rapid, simple method based on color change from blue to pink at the plantar foot region.
Since defining neuropathic symptoms could be difficult due to fluctuation of the symptoms, a diagnosis of neuropathy may be difficult. Small fiber function can be determined by pinprick and a cold or warm thermal stimulus to the distal sensation. The proximal sensory abnormality could be determined by moving the individual test paradigms proximally. Positive stimulus (allodynia and hypersensitivity) for diabetic neuropathy, can be showed by measuring the intensity or area of these phenomena. Negative symptoms in diabetic neuropathy are also numbness, no sensation, poor balance, or muscle weakness. Clinical examination in these patients can include quantitative sensory testing (QST) to asses this sensory stimulus and also provide the advantage of directly assessing the degree of sensory loss in the foot. Some of the more commonly used techniques are “Semmes-Weinstein monofilaments”, ‘’thermal and cooling threshold‘’, “perception of vibration”, and “computer-assisted sensory examination”[21-23].
Semmes-Weinstein monofilament includes nylon filaments which have variable diameters and is one of the clinical tests that measure the response to a touching sensation of the monofilaments using a numerical quality. Inability to perceive pressure of 10 g (5.07) by the monofilament has been shown in subjects who are at risk for neuropathic foot ulceration (Figure 2). This is a very easy and applicable examination in busy outpatient clinics and reveals diabetic foot ulcer risk. It is recommended to all practitioners[24].
Figure 2.
Monofilament test is a diagnostic tool to detect diabetic peripheral neuropathy. When the nylon line bends, the force is 10 grams. It is used for diabetic foot contact and stress testing.
Perception of vibration, which is called deep sensation impairment, is usually one of the earliest signs of peripheral diabetic neuropathy. Tuning forks (128 Hz) are generally used in general practice; these determine the perception of vibration through the application on distal bony prominence of the great toe bilaterally and other bony prominences such as the medial malleolus. Sensitivity of tuning fork is approximately 53% and it is less predictive for the development of foot ulceration compared to using the monofilament test[25].
Although electrophysiology is not required for clinical diabetic neuropathy evaluation, it quantitatively assesses large fiber involvement in diabetic neuropathy. While these QSTs are convenient techniques in daily clinical practice, simple clinical instruments including Michigan neuropathy screening instrument and simplified neuropathy disability score can be used to assess neurologic deficits. Now these scoring systems become using in a number of ongoing trials with new therapies for diabetic neuropathy[26,27].
Although it is not the main topic of this review, briefly neuropathy management is done symptomatically and current therapeutic agents which are used, including tricyclic antidepressants, serotonin and noradrenalin reuptake inhibitors, and anticonvulsants, have efficacy in diabetic neuropathy[28]. Among these new anticonvulsants, pregabalin and gabapentin have been shown to be more convenient in the treatment of painful syndromes in recent articles[29].
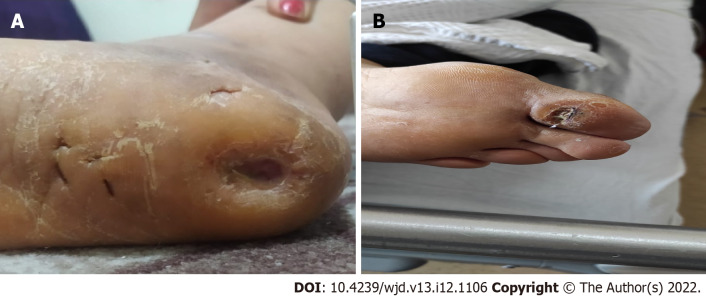
Callus deformity and plantar shear stress
Calluses have been defined as hyperkeratosis caused by excessive mechanical loading. Calluses increase pressure of plantar area and the risk of DFU[30]. Significant risk factors for callus deformity in patients with diabetic neuropathy are foot deformity, limited joint mobility, repetitive stress of walking, and ill-fitting shoes[31]. Calluses are frequently developed under bony prominence including the metatarsal head. Proprioceptive loss due to sensory neuropathy and metatarsal heads leads to increased pressure and load under the diabetic foot. It has been reported that callus deformity may be related with a relative risk of 11 for ulcer development (Figure 3). As a result, removal of plantar callus is associated with reduced plantar pressure and thereby reduced foot ulcer risk.
Figure 3.
Callus formation as a presentation of diabetic neuropathy.
Charcot neuroarthropathy
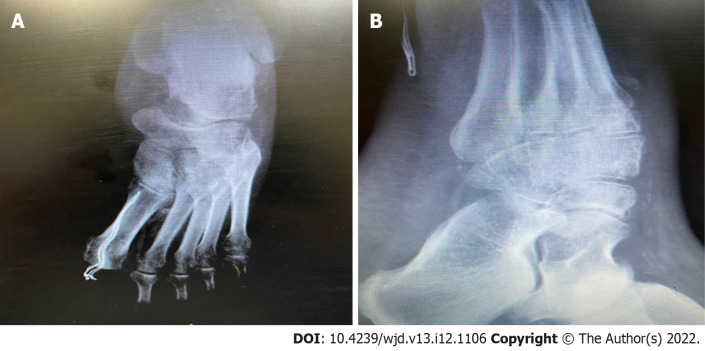
Charcot neuroarthropathy (CN) has been determined to be a chronic and destructive disease of the bone structure and joints in patients with neuropathy. The precise incidence of CN in persons has previously been estimated to be between 0.1%-0.4%[31]. Etiopathogenesis of CN is complex and based on varied degrees of neuropathy. Typical clinical symptom is characterized by painful or painless bone and join destruction in limbs that have lost sensory innervation. Although the clinical management of CN has many clinical challenges, it is generally characterized with asymptomatic nature such as ankle sprain, cellulitis, and thrombosis[32]. A diagnosis of CN is based on primarily on thorough history and physical examination, with corroborating laboratory investigations and diagnostic imaging. Modified eichenholtz classification is commonly used for description in the clinical stage[33] (Figure 4). According to this classification, stage 0 is mild inflammation, soft tissue edema, and normal X-ray, stage 1 is severe inflammation and abnormal X rays with microfractures, stage 2 is coalescence and end of bone resorption, and stage 3 is definitive bone remodeling with chronic CN.
Figure 4.
Charcot neuroarthropathy is a chronic devastating and destructive disease of bone structure and joint in patients with neuropathy. A and B: Rocker-bottom foot deformity to charcot process.
Initial weight-bearing radiography can show demineralization, fragmentation, joint dislocation, osseous debris, and joint space obliteration[34]. But routine radiography gives limited information about the differentiation of CN from osteomyelitis. Imaging techniques including magnetic resonance imaging (MRI) or PET/CT scans highlight the inadequacies of clinical examination and radiographs in assessing the CN stage[35]. Orthopedic surgery is often required to correct severe foot deformities when conservative measures including physiotherapy are not effective (Figure 5).
Figure 5.
Radiographic findings. A and B: Radiographic findings of charcot neuroarthropathy.
Peripheral vascular disease
Peripheral vascular disease is characterized as a chronic arterial occlusive disease of the lower extremities and varies in severity. Patients with peripheral arterial disease have usually intermittent claudication, rest pain, and tissue loss with or without gangrene[36]. Rest pain is shown in these patients and related with chronic sensory nerve ischemia. Resting pain emerges as a diffuse burning or aching pain in the fore foot[37]. Intermittent claudication and rest pain are the clues to diagnosis, though it can lack symptoms or can be difficult to be attributed exclusively to peripheral vascular disease. Any worsening of walking quality or speed should be taken into account, as well as fatigue, pain, cramps, discomfort, or burns in the buttocks, thighs, or feet. The extent of ischemia and symptoms are related with location vascular lesion as well as the development of collateral circulation[38]. Generally, patients with aorto-iliac disease have buttock and thigh pain, and femoral disease causes calf discomfort. Tibio-peroneal disease generally does not have claudication, although some patients will complain of foot pain or numbness while walking.
Pulse palpation (distal pedis, posterior tibial, posterior tibial, popliteal, and femoral arteries), which can be a simple, cheap, and comfortable clinical examination, should be performed on all diabetic patients during the follow-up examination. Ankle-brachial index (ABI) has emerged as a relatively non-invasive tool for the diagnosis of peripheral arterial disease[39]. The measurement of ABI (ratio of systolic blood pressure on the ankle to the systolic blood pressure in the upper arm) is normal in the 1.0-1.4 range, obviously pathologic under 0.9. An ABI over than 1.4 is also considered as abnormal, reflecting calcified and stiffed arteries. Doppler ultrasound examination and computed tomography angiography are often used as non-invasive tests[40]. Intra-arterial digital subtraction angiography is defined as the gold standard for arterial imaging because of its high spatial resolution. It has the advantage of allowing endovascular therapy during the same procedure and it is also extremely accurate for the smaller vessels of the ankle and foot. But it has a disadvantage for patients with renal insufficiency [glomerular filtration rate (GFR) < 35 mL/min/1.73 m2][37].
Infection and osteomyelitis
Infection in ulcerated diabetic foot is a primary cause of morbidity and mortality. It is well known that diabetic patients are prone to infectious diseases because of the diminished host defenses, including inadequacy in leukocyte capacity and morphologic alterations to macrophages, elevation of proinflammatory cytokines, and impairment of diabetic polymorph-nuclear cell functions (chemotaxis, phagocytosis, and killing)[41,42]. Many organisms can cause diabetic foot infection, but Gram positive cocci, especially staphylococci (S. aureus), are the most common cause pathogens[43]. Peripheral neuropathy, angiopathy, and a lack of attention to foot hygiene such as using poorly fitting footwear are the major factors in the development of infection. Abrasions, rashes, and loss of skin integrity due to fungal infection can be facilitating factors for diabetic foot infection. Approximately 60% of foot infections starts in webbed spaces and 30% in nails, while 10% are secondary punctures[44]. Ulcers > 60 mm2 in size, purulent discharge from sinus tract, presence of sausage toe, and erythrocyte sedimentation rate > 70 mm/h suggest the presence of underlying osteomyelitis[45]. Osteomyelitis could be able to occur after the spread of superficial infection of the soft tissue on the adjacent bone or marrow. Although numerous expensive radiology techniques are available to diagnose osteomyelitis, specific clinical signs of inflammation (swelling, erythema, warmth, tenderness, pain, or induration) and the use of simple metal probes can often be used to make clinical diagnoses. In initial clinical visit, plain radiographs should be obtained to determine the extent of osseous erosion, as well as to assess anatomy for surgical planning. Further scanning tests including MRI and bone scans could be performed for patients with neuropathic osteoarthropathy or multifocal disease[46-48].
CLASSIFICATIONS OF FOOT ULCERS
Identification and classification of patients with DFU should be performed to see whether hospitalization, intravenous (IV) broad spectrum antibiotics, or surgical consultations will be required or not. An accurate defining of ulcer characteristics such as size, depth, appearance, and location allows for the mapping of progress during management of DFU. There have been several classification systems that have been broadly externally validated for ulcer healing and lower extremity amputation, and they are Meggitt-Wagner, University of Texas, Infectious Disease Society of America (IDSA), perfusion, extent, depth, ischemia, sensation (PEDIS), SINBAD, and Wound, Ischemia and foot Infection (WIfI) classification[49-51].
The Meggitt-Wagner classification was the first announced classification system; however, it is not well validated and does not distinguish well between ulcer types for the main purpose of classification. This system consists of six different groups: 0, intact skin; 1, superficial ulcer; 2, ulcer reaching to tendons, joints, bones; 3, deep ulcer with abscess and osteomyelitis; 4, local gangrene; and 5, gangrene of the entire foot. It presents vascular perfusion only when gangrenous changes appear and infection when osteomyelitis is present (Table 1).
Table 1.
Wagner-Meggit classification
|
Grade
|
Lesion
|
| 0 | No open lesion |
| 1 | Superficial ulcer |
| 2 | Deep ulcer to tendon or joint capsule |
| 3 | Deep ulcer with abscess, osteomyelitis or joint sepsis |
| 4 | Local gangrene - fore foot or heel |
| 5 | Gangrene of entire foot |
The University of Texas classification is well validated but it does not indicate neuropathy or depth of the ulcer area, which is considered to be one of the main determinants of the ulcer healing (Table 2). IDSA was reported as a guideline and diabetic foot is subclassified into the categories of uninfected, mild (restrictive involvement of only skin and subcutaneous tissue), moderate (more extensive), and severe (systemic signs of infection).
Table 2.
University of Texas Classification system
|
|
0
|
1
|
2
|
3
|
| A | No open lesion | Superficial wound | Affected tendon/capsules | Affected bone/joint |
| B | With infection | With infection | With infection | With infection |
| C | Ischemic | Ischemic | Ischemic | Ischemic |
| D | Infection/ischemia | Infection/ischemia | Infection/ischemia | Infection/ischemia |
The PEDIS classification system is based on five features of the wound and it helps clinicians assess risk or prognosis for a person with diabetes and active foot ulcer. In addition, it was used for a clinical audit study in 14 European countries[52].
The SINBAD classification system matches each composing variable such as area, depth, infection, and neuropathy to a score (ranging from 0-6). This classification system has some benefits such as simple, quick to use and not requiring specialist equipment[53].
The WIfI classification includes three prognostic factors that affect clinical management. These factors indicate wounds that are graded from 0 to 3, ischemia graded based on toe pressure index, and infection which is based on IDSA classification. The WIfI threatened limb classification has been shown to correlate well with a risk of major amputation but it is not enough make acute decisions about the treatment only by itself due to more confounding factors (Table 3).
Table 3.
Wound, Ischemia, and foot Infection classification
|
|
Wound
|
Ischemia; toe pressure/tcpo2
|
Infection
|
| 0 | No ulcer and no gangrene | > 60 mm/Hg | Non-infected |
| 1 | Small ulcer and no gangrene | 40-59 mm/Hg | Mild (< 2 cm sellulitis) |
| 2 | Deep ulcer and gangrene limited to toes | 30-39 mm/Hg | Moderate (> 2 cm sellulitis) |
| 3 | Extensive ulcer or extensive gangrene | < 30 mm/Hg | Severe (systemic response/sepsis) |
Up to date there has been several classification systems but which classification to use is still controversial. Physicians who treat patients with DFU are concerned about which classification is recommended. They are still discussing the usefulness of these classifications, and the effects of such classifications on diagnosis or treatment remain unknown. Although there are some limitations in case of prognostic accuracy of the Meggitt-Wagner classification, this classification remains the most commonly utilized system in health care today.
MANAGEMENT OF DIABETIC FOOT ULCER
The main principle of management of DFU is to evaluate wound appearance (extent, size, depth, presence of infection, and wound duration) in detail. Clinicians should inspect the extent of tissue destruction and possible bone and joint involvement. After evaluating wound appearance, another major decision is whether the patient can be initially treated as an outpatient or needs hospitalization. Early superficial ulcer (< 2 cm) without systemic toxicity may be treated at home. If the patient has a deep gangrenous ulcer with infected or systemic symptoms or needs surgical treatment, hospitalization is advised.
Since diabetic ulcer healing depends on multiple factors, it should be evaluated by a multidisciplinary expert team. The treatment includes conservative and surgical interventions and there are some fundamental steps of diabetic foot management such as surgical debridement, dressing, wound off-loading, vascular assessment, control of infection, glycemic control, and adjuvant therapies[54-57] (Table 4).
Table 4.
Standard care of diabetic foot ulcer
|
Treatment
|
Description
|
|
| Debridement | Surgical debridement | Necrotic or non-viable tissue should be removed, regular (weekly) debridement is associated with rapid healing of ulcers |
| Dressing | Films, foams, hydrocolloids, hydrogel | Proper using of dressing materials could facilitate moist environment |
| Wound off-loading | Rock or bottom outsoles, custom-made insoles, some shoe inserts | Plantar shear stress should be removed |
| Vascular assessment | PTA or endovascular recanalization followed by PTA or by-pass grafting | Arterial insufficiency should be treated for improving wound healing |
| Control of infection | Appropriate antibiotic therapy according to pathogens | Deep tissue cultures should be obtained before antibiotic therapy, for mild infection treatment duration could be 1-2 wk but for moderate to severe infection, it should be 3-4 wk |
| Glycemic control | For better glycemic control, insulin treatment has been preferred in hospitalized patients with diabetic foot ulcers | |
PTA: Percutaneous transluminal angioplasty.
Surgical debridement
Debridement is a principal treatment of local wound healing and it involves removing hyperkeratotic epidermis (callus), necrotic dermal tissue, foreign debris, and bacterial elements from a wound bed. Debridement includes numerous forms such as mechanical, autolytic, enzymatic, and sharp[58,59]. Sharp debridement is more common to use, and it includes two forms, namely, clinic based debridement and surgery based excisional debridement. A combination of debridement methods could help to remove devitalized tissue that provides a nidus for bacterial proliferation and acts as a physical barrier for antibiotics. Debridement is the most important step of the wound healing. If necessary, it should be performed in every clinic visit by clinicians.
Dressings
After the adequate debridement period, soft tissue defect requires dressing materials for closure and/or coverage of wound area. Dressing with adequate biomaterials could provide wound healing processes and protect from contamination. Naturel skin is considered perfect wound dressing and therefore ideal wound dressing should try to mimic its properties. Since recent studies highlighted the role of wound environment, dressing also should be biocompatible and not provoke any allergic or immune response reaction and should be easily removed[60,61]. Alginate and collagen-alginate products, carboxymethylcellulose dressings, topical phenytoin, and hydrogels are types of dressings which are available[62,63]. But there have been still some questions to support the choice of any dressings or to promote healing of ulcer.
Wound off-loading
Plantar shear stress and vertical plantar pressure are major causative factor in the development and poor healing of DFU. Removal of pressure and/or redistribution of an increased weight bearing area of the foot can be achieved through off-loading strategies. Total contact casts and removable walkers are used for off-loading the diabetic foot[64]. Various therapeutic off-loading devices such as rock or bottom outsoles, custom-made insoles, and some shoe inserts (e.g., metatarsal pads and medial arch supports) may reduce fore foot peak pressure[65,66]. Recently, The International Working Group[67] on the diabetic foot suggests the following recommendations: (1) Removal of pressure on ulcers is one of the main part of the treatment plan; (2) non-removable walkers are the preferred treatment; and (3) forefoot off-loading shoes or cast shoes may be used when above-the-ankle devices are contraindicated.
Vascular assessment
Revascularization of critically ischemic legs results in increased area perfusion after the procedure, which is in turn associated with a further reduced amputation rate. Arterial revascularization can be performed through open procedures such as a bypass or, in many cases, endovascular recanalization followed by PTA (percutaneous transluminal angioplasty) with or without adjunctive stenting[68]. Overall, the aim of vascular reconstruction is to restore direct pulsatile flow in at least one or more arterial structures, preferably feeding the wound.
Control of infection
The diagnosis of infection is based on parameters of inflammation and should always be classified according to a preferred classification method. Antibiotic therapy is based on possible pathogens, presence of vascular disease, and the extent of foot infection. Hospitalization with parenteral antibiotic treatment is recommended when the infection penetrates to the deep fascia. Patients with chronic ulcer, prior antibiotic treatment, and recurring infection should be assumed to have methicillin-resistant Staphylococcus Aureus infection[69]. The spectrum can be broadened to cover Gram-negative aerobes in chronic infections. If a patient has a superficial ulcer without infection, empiric antibiotic treatment therapy is not recommended[70]. Oral therapy including trimethoprim/sulfamethoxazole or amoxicilline/clavulanic acid plus linezolid is recommended to patients with a superficial ulcer and presence of pedal pulses. Parenteral therapy such as vancomycin or daptomycin plus piper-acillin/tazobactam or imipenem cilastatin or meropenem has been recommended to patients with systemic inflammation or ulcer/gangrene with penetration of deep fascia[71,72]. In addition, in order to avoid antibacterial resistance or other adverse outcome of therapy, it is the best approach to be followed.
Glycemic control
In hospitalized patients, intensive insulin treatment should be administered to patients with foot ulcer for better glycemic control. The evidence of glycemic control can accelerate the healing of foot ulcers and reduce the incidence of ulceration and amputation. Studies have shown that increased blood glucose level is correlated with decreased neutrophil function and suppression of inflammatory response[73-75]. Although there are limited randomized control trials (RCTs) which determine whether glycemic control improves wound healing better, in a meta-analysis which included 10897 patients without known history of peripheral arterial disease, it has been reported that intensive glycemic control was associated with a statistically significant decrease in risk of amputation of diabetic foot[76].
Adjuvant therapies
New treatment modalities have been developed since 2002. There are advanced wound therapy methods. In addition to conventional therapy, several types of treatment modalities are available, such as negative pressure wound therapy, which is also known as vacuum assisted closure (VAC), synthetic skin grafts, non-surgical debridement agents, topical growth factors, electrical stimulation, and hyperbaric oxygen chambers[77-83] (Table 5). Each has its own merits but economic constraints and patient compliance should be kept in mind.
Table 5.
Additional adjuvant care of diabetic foot ulcer
|
Item
|
Description
|
| Negative pressure wound therapy (VAC) | Widely used, removal of the excess third space fluid from the area, reduction of bacterial load, increased granulation tissue, but RCTs have high risk of bias |
| Synthetic skin grafts (Bio-engineered skin substitutes) | Contribute to the new dermal tissue but limited data to prove benefit of these products |
| Non-surgical debridement agents (enzymatic debridement, autolytic debridement, hydroterapy, Maggot therapy) | Promoting fibroblast migration and improving skin perfusion but due to small RCTs, it has clinical bias for beneficial effect |
| Topical growth factors (EGF, VEGF, PDGF, FGF) | Promote healing non-infected foot ulcer and stimulating angiogenesis but limited trials confirming positive outcomes |
| Electrical stimulation | Bacteriostatic and bactericidal effect on foot ulcer but lack of evidence due to limited clinical trials |
| HBOC | HBOC therapy increases blood and oxygen content in hypoxic tissues and has antimicrobial activity, but it is unclear whether it has benefit in long term wound healing |
RCT: Randomised controlled studies; HBOC: Hyperbaric oxygen chambers; VAC: Vacuum assisted closure; EGF: Epidermal growth factor; VEGF: Vascular endotelial growth factor; PDGF: Platelet derived growth factor; FGF: Fibroblast growth factor.
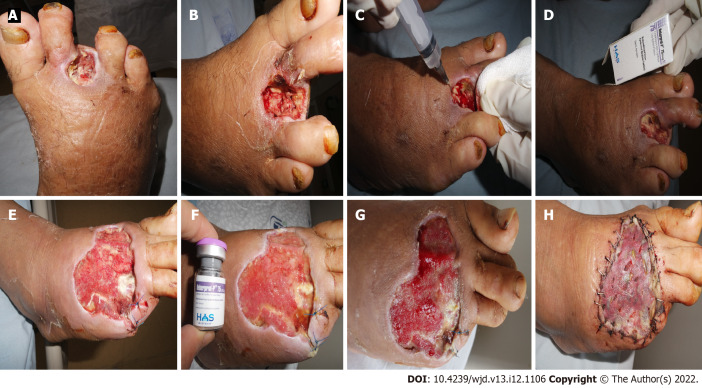
Negative pressure wound therapy
Pressure wound therapy (VAC) was first declared and used in clinical practice by the German physician Fleischmann in 1993[77]. It has remarkable effect on wound drainage, also enhancing perfusion. VAC could be used for acute and chronic DFU and it promotes the growth of granulation tissue (Figure 6). It can be helpful in the postoperative management of DFU. According to the Wound Healing Society and European Wound Management Association[78]: (1) Wound infection should be well controlled after the debridement; (2) the risk of bleeding is well controlled; there is no active bleeding or exposed vascular damage on the wound or no risk of coagulation dysfunction; and (3) the risk of ischemia is treated and well controlled (ABI ranges from 0.9 to 1.3), and VAC therapy is recommended with class 1 evidence. After 1-2 rounds of VAC therapy, a comprehensive evaluation should be performed for an effective evaluation. It is recommended to continue VAC if there is growth of new granulation tissue on the wound surface with surrounding epithelization. If infection is aggravated, it should be stopped immediately. In recent years, VAC treatment has been used extensively for DFU management and studies have shown that it has certain advantages in preventing and controlling wound infections.
Figure 6.
Negative pressure wound therapy is considered as a better alternative therapy for the management of diabetic foot ulcer. A-E: This patient was treated with negative pressure wound therapy therapy after surgical therapy.
Synthetic skin grafts
Skin substitutes are classified into three groups based on the plasticity of preparation procedure and composition of the substitutes. Class 1 skin layer includes cultured epidermal equivalents which are formed of single-layered materials; Class 2 layer includes dermal components from processed skin or fabricated matrix protein; Class 3 layer also consists of dermal and epidermal components and skin grafts (allograft and xenograft)[80]. Class 3 layer is more popular and common to use. Although there are limited studies, wound healing can be promoted by using these agents.
Non-surgical debridement agents
Although sharp debridement can play a major role in wound healing, various techniques such as autolytic debridement with hydrogels, enzymatic debridement, maggot and larval debridement, and hydrotherapy are available[81,82]. But recent studies did not provide sufficient evidence to use one approach over other methods.
Hyperbaric oxygen chamber
Administration of 100% O2 has some beneficial effects on wound healing. It not only causes increased blood and oxygen content in hypoxic tissue, but it also has antimicrobial activity due to enhanced mobility and bacteriophagic activity of leukocytes[83]. Studies show that hyperbaric oxygen stimulates angiogenesis and increases fibroblast proliferation and collagen production. Some authors suggested that there are no definite results which display an improvement in DFU. There is large uncertainty associated with the evaluation of the cost-effectiveness of hyperbaric oxygen therapies. Up to date, there have been seven RCTs showing that hyperbaric oxygen chambers are beneficial for preventing amputation and promoting complete healing in patients with Wagner grade 3 or greater DFU[84,85]. In patients with Wagner grade 2 or lower DFU, there is inadequate evidence to justify the use of hyperbaric oxygen therapy as an adjuvant treatment. The most common adverse events associated with hyperbaric oxygen therapy are barotraumatic otitis, the inability to equalize middle ear pressure, and worsening of cataracts.
Topical growth factors
Epidermal growth factor (EGF), ascular endothelial growth factor (VEGF), platelet-derived growth factor (PDGF), and fibroblast growth factor (FGF) are polypeptide growth factors that have significant effects on tissue repair processes. These growth factors are released by platelets and activated macrophages that are required for normal wound repair[10,86]. Growth factors which are used topically were reported to reduce the incidence of lower limb amputation. Using of growth factors is essential to promote angiogenesis, enzyme production, and cell migration and proliferation.
PDGF is a crucial factor in wound healing and serves as a chemo-attractant for the migration of fibroblasts and neutrophils to the site of injury. It is the first recombinant growth factor approved for topical application of wound healing. Fewer RCTs evaluated the effectiveness of PDGF and all studies applied the topical gel with different concentrations[87,88]. The majority of them did not find significant healing improvements compared to the standard wound care.
FGF acts as a balance factor in the body and is important for tissue maintenance, repair, regeneration, and metabolism. FGF is a stronger angiogenesis factor than PDGF and VEGF. And FGF stimulates angiogenesis and proliferation of fibroblasts, forming granulation tissue. FGF has some limitations for the treatment of DFU wound healing, since it generally has a short half-life and require repeated administrations[89].
EGF is a wound modulator that is involved in cell migration and proliferation. Injecting EGF deep into the wound bottom and contours encourages a more effective pharmacodynamic response in terms of granulation tissue growth and wound closure[90,91]. EGF is perhaps the most widely used method in diabetic foot wound therapy but the results of studies are controversial or neutral. But our clinical experiences have shown that EGF is promising for healing foot ulcer (Figure 7).
Figure 7.
Epidermal growth factor is perhaps the most widely used method in diabetic foot. A-D: Intralesional epidermal growth factor therapy into the wound bottom and contours encourages granulation tissue growth and wound closure; E-H: Before and after intralesional epidermal growth factor therapy.
Low level laser therapy
Low level laser therapy (LLLT) is a novel adjunctive therapy and is known to supply direct biostimulative light energy to body cells. This energy could stimulate molecules and atom of cells but does not cause a significant increase in tissue heat. Although different laser wavelengths have different depth of penetration of tissue, red laser has a deeper penetration than the others such as violet, blue, green, and yellow[92]. LLLT, which can be considered as a possible new treatment option for the diabetic foot, has a various effect on wound healing by cellular migration or penetration[93]. Otherwise clinical trials using human models do not provide sufficient evidence to establish the uselfulness and practical method in wound care regimes.
Although these newly adjunctive treatments have some benefits, they are costly and should be reserved for ulcers that fail to respond to standard treatments. Adjunctive treatment modalities should be considered as an addition to good wound care which must always include adequate off-loading and debridement therapy. Current evidence points towards VAC therapy and local stem cell application as an effective treatment than the other adjunctive modalities for diabetic foot healing. There is a need for well-designed blinded RCTs to determine the true efficacy of these interventions and to develop evidence-based practice guidelines.
PREVENTION OF FOOT ULCERATION
DFU are a devastating complication of diabetes mellitus. The mainstay of diabetic foot intervention is prevention. Preventative strategies in the form of education and regular foot assessments for peripheral vascular diseases and neuropathy along with risk stratification form the basis of the management of diabetic foot disease. Recently published guidelines highlight risk stratification for the assessment of risk for diabetic foot ulcer or risk of future amputation[55,94]: Very low risk: No loss of protective sensation and no peripheral arterial disease; Low risk: Loss of protective sensation or peripheral arterial disease or presence of callus formation alone; Moderate risk: Loss of protective sensation and peripheral arterial disease or presence of foot deformity; High risk: History of previous ulceration or previous amputation or renal replacement therapy or neuropathy and non-critical ischemic neuropathy with callus.
According to IWGDF prevention guidelines, it is recommended to examine a person who has a low risk of foot ulceration annually for signs or symptoms of loss of protective sensation and peripheral arterial disease. Patients with moderate or high risk should be screened every 3-6 mo. A person’s risk status may change over time, thus requiring continual monitoring. Patients who have a risk of foot ulceration should be informed about controlling the whole surface of boot feet and the inside of shoes daily. Patients with moderate or high risk should be warned about wearing proper footwear to reduce plantar pressure. If there is a pre-ulcerative sign such as callus, appropriate treatment should be performed. Achilles tendon lengthening, joint arthroplasty, and single or pan metatarsal head resection may be considered for patients who cannot heal with non-surgical therapy.
If the preventative treatment modalities are carried out for patients with diabetes, the global patient and economic burden of diabetic foot disease can be considerably reduced. Decreasing the risk of ulceration also reduces the risk of infection, hospitalization, and lower extremity amputation in these patients.
CONCLUSION
DFU constitute a substantial burden for all over the world. Optimized therapy requires a collective refocusing on prevention and reallocation of resources from simply healing active ulcers. Multidisciplinary expert team is necessary for management of complex DFU and therefore multidisciplinary approach to patient care reduces the risk of amputation in patient with DFU. A combination of care from vascular, cardiovascular, infectious disease, and endocrinology disciplines as well as podiatrists and wound care specialists provides a full range of care for patients with DFU. Conventional therapies including debridement, off-loading, vascular assessment, and control of infection are principal treatment modalities. Otherwise, better outcomes could be obtained when the conventional treatment is combined with additional treatment in suitable patients.
Footnotes
Conflict-of-interest statement: There are no conflicts of interest to report.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Peer-review started: July 21, 2022
First decision: August 20, 2022
Article in press: November 18, 2022
Specialty type: Endocrinology and metabolism
Country/Territory of origin: Turkey
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Mostafavinia A, Iran; Sivashanmugam K, India; Wu QN, China; Zhang LL, China S-Editor: Chen YL L-Editor: Wang TQ P-Editor: Chen YL
Contributor Information
Gamze Akkus, Department of Endocrinology, Cukurova University, Adana 33170, Turkey. tugrulgamze@hotmail.com.
Murat Sert, Department of Internal Medicine, Cukurova University Medical Faculty, Adana 33170, Turkey.
References
- 1.Zhang P, Lu J, Jing Y, Tang S, Zhu D, Bi Y. Global epidemiology of diabetic foot ulceration: a systematic review and meta-analysis †. Ann Med. 2017;49:106–116. doi: 10.1080/07853890.2016.1231932. [DOI] [PubMed] [Google Scholar]
- 2.International Diabetes Federation. Diabetes atlas. 7th ed. Brussels, 2015. Available from: http:// www.diabetesatlas.org .
- 3.Guariguata L. By the numbers: new estimates from the IDF Diabetes Atlas Update for 2012. Diabetes Res Clin Pract. 2012;98:524–525. doi: 10.1016/j.diabres.2012.11.006. [DOI] [PubMed] [Google Scholar]
- 4.Khanolkar MP, Bain SC, Stephens JW. The diabetic foot. QJM. 2008;101:685–695. doi: 10.1093/qjmed/hcn027. [DOI] [PubMed] [Google Scholar]
- 5.Robinson BV. The pharmacology of phagocytosis. Rheumatol Rehabil. 1978;Suppl:37–46. doi: 10.1093/rheumatology/xvii.suppl.37. [DOI] [PubMed] [Google Scholar]
- 6.Waaijman R, de Haart M, Arts ML, Wever D, Verlouw AJ, Nollet F, Bus SA. Risk factors for plantar foot ulcer recurrence in neuropathic diabetic patients. Diabetes Care. 2014;37:1697–1705. doi: 10.2337/dc13-2470. [DOI] [PubMed] [Google Scholar]
- 7.Margolis DJ, Hofstad O, Feldman HI. Association between renal failure and foot ulcer or lower-extremity amputation in patients with diabetes. Diabetes Care. 2008;31:1331–1336. doi: 10.2337/dc07-2244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harries RL, Harding KG. Management of diabetic foot ulcers. Curr Geriatr Ref. 2015;4:265–276. [Google Scholar]
- 9.Chen CE, Ko JY, Fong CY, Juhn RJ. Treatment of diabetic foot infection with hyperbaric oxygen therapy. Foot Ankle Surg. 2010;16:91–95. doi: 10.1016/j.fas.2009.06.002. [DOI] [PubMed] [Google Scholar]
- 10.Martí-Carvajal AJ, Gluud C, Nicola S, Simancas-Racines D, Reveiz L, Oliva P, Cedeño-Taborda J. Growth factors for treating diabetic foot ulcers. Cochrane Database Syst Rev. 2015:CD008548. doi: 10.1002/14651858.CD008548.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sima AA, Sugimoto K. Experimental diabetic neuropathy: an update. Diabetologia. 1999;42:773–788. doi: 10.1007/s001250051227. [DOI] [PubMed] [Google Scholar]
- 12.Pallavicini G, Cetta G, Sinigaglia F, Badiello R, Tamba M. Proceedings: Radiolysis of a pig gastric glycopeptide. Br J Cancer. 1975;32:761–762. doi: 10.1038/bjc.1975.324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fernyhough P, Calcutt NA. An Introduction to the History and Controversies of the Pathogenesis of Diabetic Neuropathy. Int Rev Neurobiol. 2016;127:115–120. doi: 10.1016/bs.irn.2016.03.012. [DOI] [PubMed] [Google Scholar]
- 14.Shillo P, Sloan G, Greig M, Hunt L, Selvarajah D, Elliott J, Gandhi R, Wilkinson ID, Tesfaye S. Painful and Painless Diabetic Neuropathies: What Is the Difference? Curr Diab Rep. 2019;19:32. doi: 10.1007/s11892-019-1150-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Baum P, Kosacka J, Estrela-Lopis I, Woidt K, Serke H, Paeschke S, Stockinger M, Klöting N, Blüher M, Dorn M, Classen J, Thiery J, Bechmann I, Toyka KV, Nowicki M. The role of nerve inflammation and exogenous iron load in experimental peripheral diabetic neuropathy (PDN) Metabolism. 2016;65:391–405. doi: 10.1016/j.metabol.2015.11.002. [DOI] [PubMed] [Google Scholar]
- 16.Herder C, Kannenberg JM, Huth C, Carstensen-Kirberg M, Rathmann W, Koenig W, Heier M, Püttgen S, Thorand B, Peters A, Roden M, Meisinger C, Ziegler D. Proinflammatory Cytokines Predict the Incidence and Progression of Distal Sensorimotor Polyneuropathy: KORA F4/FF4 Study. Diabetes Care. 2017;40:569–576. doi: 10.2337/dc16-2259. [DOI] [PubMed] [Google Scholar]
- 17.Fealey RD, Low PA, Thomas JE. Thermoregulatory sweating abnormalities in diabetes mellitus. Mayo Clin Proc. 1989;64:617–628. doi: 10.1016/s0025-6196(12)65338-5. [DOI] [PubMed] [Google Scholar]
- 18.Petropoulos IN, Ponirakis G, Khan A, Almuhannadi H, Gad H, Malik RA. Diagnosing Diabetic Neuropathy: Something Old, Something New. Diabetes Metab J. 2018;42:255–269. doi: 10.4093/dmj.2018.0056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Seglen PO. From bad to worse: evaluation by Journal Impact. Trends Biochem Sci. 1989;14:326–327. doi: 10.1016/0968-0004(89)90163-1. [DOI] [PubMed] [Google Scholar]
- 20.Dyck PJ, Kratz KM, Karnes JL, Litchy WJ, Klein R, Pach JM, Wilson DM, O'Brien PC, Melton LJ 3rd, Service FJ. The prevalence by staged severity of various types of diabetic neuropathy, retinopathy, and nephropathy in a population-based cohort: the Rochester Diabetic Neuropathy Study. Neurology. 1993;43:817–824. doi: 10.1212/wnl.43.4.817. [DOI] [PubMed] [Google Scholar]
- 21.Nieto-Guisado A, Solana-Tramunt M, Marco-Ahulló A, Sevilla-Sánchez M, Cabrejas C, Campos-Rius J, Morales J. The Mediating Role of Vision in the Relationship between Proprioception and Postural Control in Older Adults, as Compared to Teenagers and Younger and Middle-Aged Adults. Healthcare (Basel) 2022;10 doi: 10.3390/healthcare10010103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sarlegna FR, Sainburg RL. The roles of vision and proprioception in the planning of reaching movements. Adv Exp Med Biol. 2009;629:317–335. doi: 10.1007/978-0-387-77064-2_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liniger C, Albeanu A, Moody JF, Richez J, Bloise D, Assal JP. The Thermocross: a simple tool for rapid assessment of thermal sensation thresholds. Diabetes Res Clin Pract. 1991;12:25–33. doi: 10.1016/0168-8227(91)90127-y. [DOI] [PubMed] [Google Scholar]
- 24.Kumar S, Fernando DJ, Veves A, Knowles EA, Young MJ, Boulton AJ. Semmes-Weinstein monofilaments: a simple, effective and inexpensive screening device for identifying diabetic patients at risk of foot ulceration. Diabetes Res Clin Pract. 1991;13:63–67. doi: 10.1016/0168-8227(91)90034-b. [DOI] [PubMed] [Google Scholar]
- 25.Garrow AP, Boulton AJ. Vibration perception threshold--a valuable assessment of neural dysfunction in people with diabetes. Diabetes Metab Res Rev. 2006;22:411–419. doi: 10.1002/dmrr.657. [DOI] [PubMed] [Google Scholar]
- 26.Hepburn DA, Deary IJ, MacLeod KM, Frier BM. Structural equation modeling of symptoms, awareness and fear of hypoglycemia, and personality in patients with insulin-treated diabetes. Diabetes Care. 1994;17:1273–1280. doi: 10.2337/diacare.17.11.1273. [DOI] [PubMed] [Google Scholar]
- 27.Singleton JR, Bixby B, Russell JW, Feldman EL, Peltier A, Goldstein J, Howard J, Smith AG. The Utah Early Neuropathy Scale: a sensitive clinical scale for early sensory predominant neuropathy. J Peripher Nerv Syst. 2008;13:218–227. doi: 10.1111/j.1529-8027.2008.00180.x. [DOI] [PubMed] [Google Scholar]
- 28.Tesfaye S, Boulton AJ, Dyck PJ, Freeman R, Horowitz M, Kempler P, Lauria G, Malik RA, Spallone V, Vinik A, Bernardi L, Valensi P Toronto Diabetic Neuropathy Expert Group. Diabetic neuropathies: update on definitions, diagnostic criteria, estimation of severity, and treatments. Diabetes Care. 2010;33:2285–2293. doi: 10.2337/dc10-1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yasaei R, Katta S, Saadabadi A, Gabapentin . In StatPearls. Treasure Island, FL, United States: StatPearls Publishing, 2020. [Google Scholar]
- 30.Banks JL, Petersen BJ, Rothenberg GM, Jong AS, Page JC. Use of a Remote Temperature Monitoring Mat for the Early Identification of Foot Ulcers. Wounds. 2020;32:44–49. [PubMed] [Google Scholar]
- 31.Oe M, Takehara K, Noguchi H, Ohashi Y, Amemiya A, Sakoda H, Suzuki R, Yamauchi T, Ueki K, Kadowaki T, Sanada H. Thermographic findings in a case of type 2 diabetes with foot ulcer due to callus deterioration. Diabetol Int. 2017;8:328–333. doi: 10.1007/s13340-017-0315-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Havlin CE, Cryer PE. Hypoglycemia: the limiting factor in the management of insulin-dependent diabetes mellitus. Diabetes Educ. 1988;14:407–411. doi: 10.1177/014572178801400508. [DOI] [PubMed] [Google Scholar]
- 33.Trieb K. The Charcot foot: pathophysiology, diagnosis and classification. Bone Joint J. 2016;98-B:1155–1159. doi: 10.1302/0301-620X.98B9.37038. [DOI] [PubMed] [Google Scholar]
- 34.Wukich DK, Raspovic KM, Hobizal KB, Rosario B. Radiographic analysis of diabetic midfoot charcot neuroarthropathy with and without midfoot ulceration. Foot Ankle Int. 2014;35:1108–1115. doi: 10.1177/1071100714547218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bauer-Vinassac D, Menkes CJ, Muller JY, Escande JP. HLA system and penicillamine induced pemphigus in nine cases of rheumatoid arthritis. Scand J Rheumatol. 1992;21:17–19. doi: 10.3109/03009749209095056. [DOI] [PubMed] [Google Scholar]
- 36.Prompers L, Huijberts M, Apelqvist J, Jude E, Piaggesi A, Bakker K, Edmonds M, Holstein P, Jirkovska A, Mauricio D, Ragnarson Tennvall G, Reike H, Spraul M, Uccioli L, Urbancic V, Van Acker K, van Baal J, van Merode F, Schaper N. High prevalence of ischaemia, infection and serious comorbidity in patients with diabetic foot disease in Europe. Baseline results from the Eurodiale study. Diabetologia. 2007;50:18–25. doi: 10.1007/s00125-006-0491-1. [DOI] [PubMed] [Google Scholar]
- 37.Hinchliffe RJ, Andros G, Apelqvist J, Bakker K, Friederichs S, Lammer J, Lepantalo M, Mills JL, Reekers J, Shearman CP, Valk G, Zierler RE, Schaper NC. A systematic review of the effectiveness of revascularization of the ulcerated foot in patients with diabetes and peripheral arterial disease. Diabetes Metab Res Rev. 2012;28 Suppl 1:179–217. doi: 10.1002/dmrr.2249. [DOI] [PubMed] [Google Scholar]
- 38.Faglia E, Clerici G, Caminiti M, Quarantiello A, Curci V, Morabito A. Predictive values of transcutaneous oxygen tension for above-the-ankle amputation in diabetic patients with critical limb ischemia. Eur J Vasc Endovasc Surg. 2007;33:731–736. doi: 10.1016/j.ejvs.2006.12.027. [DOI] [PubMed] [Google Scholar]
- 39.Mohler ER 3rd, Treat-Jacobson D, Reilly MP, Cunningham KE, Miani M, Criqui MH, Hiatt WR, Hirsch AT. Utility and barriers to performance of the ankle-brachial index in primary care practice. Vasc Med. 2004;9:253–260. doi: 10.1191/1358863x04vm559oa. [DOI] [PubMed] [Google Scholar]
- 40.Premalatha G, Ravikumar R, Sanjay R, Deepa R, Mohan V. Comparison of colour duplex ultrasound and ankle-brachial pressure index measurements in peripheral vascular disease in type 2 diabetic patients with foot infections. J Assoc Physicians India. 2002;50:1240–1244. [PubMed] [Google Scholar]
- 41.Knapp S. Diabetes and infection: is there a link? Gerontology. 2013;59:99–104. doi: 10.1159/000345107. [DOI] [PubMed] [Google Scholar]
- 42.Pettersson US, Christoffersson G, Massena S, Ahl D, Jansson L, Henriksnäs J, Phillipson M. Increased recruitment but impaired function of leukocytes during inflammation in mouse models of type 1 and type 2 diabetes. PLoS One. 2011;6:e22480. doi: 10.1371/journal.pone.0022480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Thivierge B. Choosing an appropriate agarose for separation and purification of PCR products. Am Biotechnol Lab. 1992;10:12. [PubMed] [Google Scholar]
- 44.Akkus G, Evran M, Gungor D, Karakas M, Sert M, Tetiker T. Tinea pedis and onychomycosis frequency in diabetes mellitus patients and diabetic foot ulcers. A cross sectional - observational study. Pak J Med Sci. 2016;32:891–895. doi: 10.12669/pjms.324.10027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Senneville É, Lipsky BA, Abbas ZG, Aragón-Sánchez J, Diggle M, Embil JM, Kono S, Lavery LA, Malone M, van Asten SA, Urbančič-Rovan V, Peters EJG. Diagnosis of infection in the foot in diabetes: a systematic review. Diabetes Metab Res Rev. 2020;36 Suppl 1:e3281. doi: 10.1002/dmrr.3281. [DOI] [PubMed] [Google Scholar]
- 46.Lipsky BA, Senneville É, Abbas ZG, Aragón-Sánchez J, Diggle M, Embil JM, Kono S, Lavery LA, Malone M, van Asten SA, Urbančič-Rovan V, Peters EJG International Working Group on the Diabetic Foot (IWGDF) Guidelines on the diagnosis and treatment of foot infection in persons with diabetes (IWGDF 2019 update) Diabetes Metab Res Rev. 2020;36 Suppl 1:e3280. doi: 10.1002/dmrr.3280. [DOI] [PubMed] [Google Scholar]
- 47.Lipsky BA, Uçkay İ. Treating Diabetic Foot Osteomyelitis: A Practical State-of-the-Art Update. Medicina (Kaunas) 2021;57 doi: 10.3390/medicina57040339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Li B, Zhang M, Coffman B. Can a barrier zone stop invasion of a population? J Math Biol. 2020;81:1193–1216. doi: 10.1007/s00285-020-01541-7. [DOI] [PubMed] [Google Scholar]
- 49.Oyibo SO, Jude EB, Tarawneh I, Nguyen HC, Harkless LB, Boulton AJ. A comparison of two diabetic foot ulcer classification systems: the Wagner and the University of Texas wound classification systems. Diabetes Care. 2001;24:84–88. doi: 10.2337/diacare.24.1.84. [DOI] [PubMed] [Google Scholar]
- 50.Game F. Classification of diabetic foot ulcers. Diabetes Metab Res Rev. 2016;32 Suppl 1:186–194. doi: 10.1002/dmrr.2746. [DOI] [PubMed] [Google Scholar]
- 51.Lavery LA, Armstrong DG, Harkless LB. Classification of diabetic foot wounds. J Foot Ankle Surg. 1996;35:528–531. doi: 10.1016/s1067-2516(96)80125-6. [DOI] [PubMed] [Google Scholar]
- 52.Abbas ZG, Lutale JK, Game FL, Jeffcoate WJ. Comparison of four systems of classification of diabetic foot ulcers in Tanzania. Diabet Med. 2008;25:134–137. doi: 10.1111/j.1464-5491.2007.02308.x. [DOI] [PubMed] [Google Scholar]
- 53.Ince P, Abbas ZG, Lutale JK, Basit A, Ali SM, Chohan F, Morbach S, Möllenberg J, Game FL, Jeffcoate WJ. Use of the SINBAD classification system and score in comparing outcome of foot ulcer management on three continents. Diabetes Care. 2008;31:964–967. doi: 10.2337/dc07-2367. [DOI] [PubMed] [Google Scholar]
- 54.van Houtum WH. Barriers to the delivery of diabetic foot care. Lancet. 2005;366:1678–1679. doi: 10.1016/S0140-6736(05)67675-1. [DOI] [PubMed] [Google Scholar]
- 55.Schaper NC, Van Netten JJ, Apelqvist J, Lipsky BA, Bakker K International Working Group on the Diabetic Foot. Prevention and management of foot problems in diabetes: a Summary Guidance for Daily Practice 2015, based on the IWGDF Guidance Documents. Diabetes Metab Res Rev. 2016;32 Suppl 1:7–15. doi: 10.1002/dmrr.2695. [DOI] [PubMed] [Google Scholar]
- 56.Xie XJ, Song MX, Zhang M, Qin W, Wan L, Fang Y. [Effect of Bushen Huoxue Compound on Retinal Müller Cells in High Glucose or AGEs Conditions] Zhongguo Zhong Xi Yi Jie He Za Zhi. 2015;35:735–740. [PubMed] [Google Scholar]
- 57.Buggy A, Moore Z. The impact of the multidisciplinary team in the management of individuals with diabetic foot ulcers: a systematic review. J Wound Care. 2017;26:324–339. doi: 10.12968/jowc.2017.26.6.324. [DOI] [PubMed] [Google Scholar]
- 58.Acar E, Kacıra BK. Predictors of Lower Extremity Amputation and Reamputation Associated With the Diabetic Foot. J Foot Ankle Surg. 2017;56:1218–1222. doi: 10.1053/j.jfas.2017.06.004. [DOI] [PubMed] [Google Scholar]
- 59.Elraiyah T, Domecq JP, Prutsky G, Tsapas A, Nabhan M, Frykberg RG, Hasan R, Firwana B, Prokop LJ, Murad MH. A systematic review and meta-analysis of débridement methods for chronic diabetic foot ulcers. J Vasc Surg. 2016;63:37S–45S.e1. doi: 10.1016/j.jvs.2015.10.002. [DOI] [PubMed] [Google Scholar]
- 60.Obagi Z, Damiani G, Grada A, Falanga V. Principles of Wound Dressings: A Review. Surg Technol Int. 2019;35:50–57. [PubMed] [Google Scholar]
- 61.Landriscina A, Rosen J, Friedman AJ. Systematic Approach to Wound Dressings. J Drugs Dermatol. 2015;14:740–744. [PubMed] [Google Scholar]
- 62.Pagnamenta F. Evidence generation for wound care dressing selection: reviewing the issues. J Wound Care. 2017;26:545–550. doi: 10.12968/jowc.2017.26.9.545. [DOI] [PubMed] [Google Scholar]
- 63.Balsa IM, Culp WT. Wound Care. Vet Clin North Am Small Anim Pract. 2015;45:1049–1065. doi: 10.1016/j.cvsm.2015.04.009. [DOI] [PubMed] [Google Scholar]
- 64.Bus SA. The Role of Pressure Offloading on Diabetic Foot Ulcer Healing and Prevention of Recurrence. Plast Reconstr Surg. 2016;138:179S–187S. doi: 10.1097/PRS.0000000000002686. [DOI] [PubMed] [Google Scholar]
- 65.Bus SA, Armstrong DG, van Deursen RW, Lewis JE, Caravaggi CF, Cavanagh PR International Working Group on the Diabetic Foot. IWGDF guidance on footwear and offloading interventions to prevent and heal foot ulcers in patients with diabetes. Diabetes Metab Res Rev. 2016;32 Suppl 1:25–36. doi: 10.1002/dmrr.2697. [DOI] [PubMed] [Google Scholar]
- 66.Ahluwalia R, Maffulli N, Lázaro-Martínez JL, Kirketerp-Møller K, Reichert I. Diabetic foot off loading and ulcer remission: Exploring surgical off-loading. Surgeon. 2021;19:e526–e535. doi: 10.1016/j.surge.2021.01.005. [DOI] [PubMed] [Google Scholar]
- 67.Bus SA, Armstrong DG, Gooday C, Jarl G, Caravaggi C, Viswanathan V, Lazzarini PA International Working Group on the Diabetic Foot (IWGDF) Guidelines on offloading foot ulcers in persons with diabetes (IWGDF 2019 update) Diabetes Metab Res Rev. 2020;36 Suppl 1:e3274. doi: 10.1002/dmrr.3274. [DOI] [PubMed] [Google Scholar]
- 68.Conte MS, Bradbury AW, Kolh P, White JV, Dick F, Fitridge R, Mills JL, Ricco JB, Suresh KR, Murad MH GVG Writing Group. Global vascular guidelines on the management of chronic limb-threatening ischemia. J Vasc Surg. 2019;69:3S–125S.e40. doi: 10.1016/j.jvs.2019.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Barwell ND, Devers MC, Kennon B, Hopkinson HE, McDougall C, Young MJ, Robertson HMA, Stang D, Dancer SJ, Seaton A, Leese GP Scottish Diabetes Foot Action Group. Diabetic foot infection: Antibiotic therapy and good practice recommendations. Int J Clin Pract. 2017;71 doi: 10.1111/ijcp.13006. [DOI] [PubMed] [Google Scholar]
- 70.Abbas M, Uçkay I, Lipsky BA. In diabetic foot infections antibiotics are to treat infection, not to heal wounds. Expert Opin Pharmacother. 2015;16:821–832. doi: 10.1517/14656566.2015.1021780. [DOI] [PubMed] [Google Scholar]
- 71.Reveles KR, Duhon BM, Moore RJ, Hand EO, Howell CK. Epidemiology of Methicillin-Resistant Staphylococcus aureus Diabetic Foot Infections in a Large Academic Hospital: Implications for Antimicrobial Stewardship. PLoS One. 2016;11:e0161658. doi: 10.1371/journal.pone.0161658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Kee KK, Nair HKR, Yuen NP. Risk factor analysis on the healing time and infection rate of diabetic foot ulcers in a referral wound care clinic. J Wound Care. 2019;28:S4–S13. doi: 10.12968/jowc.2019.28.Sup1.S4. [DOI] [PubMed] [Google Scholar]
- 73.Callaghan BC, Little AA, Feldman EL, Hughes RA. Enhanced glucose control for preventing and treating diabetic neuropathy. Cochrane Database Syst Rev. 2012:CD007543. doi: 10.1002/14651858.CD007543.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kim JH, Yoon NY, Kim DH, Jung M, Jun M, Park HY, Chung CH, Lee K, Kim S, Park CS, Liu KH, Choi EH. Impaired permeability and antimicrobial barriers in type 2 diabetes skin are linked to increased serum levels of advanced glycation end-product. Exp Dermatol. 2018;27:815–823. doi: 10.1111/exd.13466. [DOI] [PubMed] [Google Scholar]
- 75.Lan CC, Wu CS, Huang SM, Wu IH, Chen GS. High-glucose environment enhanced oxidative stress and increased interleukin-8 secretion from keratinocytes: new insights into impaired diabetic wound healing. Diabetes. 2013;62:2530–2538. doi: 10.2337/db12-1714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Hemmingsen B, Lund SS, Gluud C, Vaag A, Almdal TP, Hemmingsen C, Wetterslev J. Targeting intensive glycaemic control versus targeting conventional glycaemic control for type 2 diabetes mellitus. Cochrane Database Syst Rev. 2013:CD008143. doi: 10.1002/14651858.CD008143.pub3. [DOI] [PubMed] [Google Scholar]
- 77.Seidel D, Mathes T, Lefering R, Storck M, Lawall H, Neugebauer EA. Negative pressure wound therapy versus standard wound care in chronic diabetic foot wounds: study protocol for a randomized controlled trial. Trials. 2014;15:334. doi: 10.1186/1745-6215-15-334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ji S, Liu X, Huang J, Bao J, Chen Z, Han C, Hao D, Hong J, Hu D, Jiang Y, Ju S, Li H, Li Z, Liang G, Liu Y, Luo G, Lv G, Ran X, Shi Z, Tang J, Wang A, Wang G, Wang J, Wang X, Wen B, Wu J, Xu H, Xu M, Ye X, Yuan L, Zhang Y, Xiao S, Xia Z. Consensus on the application of negative pressure wound therapy of diabetic foot wounds. Burns Trauma. 2021;9:tkab018. doi: 10.1093/burnst/tkab018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Halim AS, Khoo TL, Mohd Yussof SJ. Biologic and synthetic skin substitutes: An overview. Indian J Plast Surg. 2010;43:S23–S28. doi: 10.4103/0970-0358.70712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Nathoo R, Howe N, Cohen G. Skin substitutes: an overview of the key players in wound management. J Clin Aesthet Dermatol. 2014;7:44–48. [PMC free article] [PubMed] [Google Scholar]
- 81.Jimenez JC, Agnew PS, Mayer P, Clements JR, Caporusso JM, Lange DL, Dickerson JE Jr, Slade HB. Enzymatic Debridement of Chronic Nonischemic Diabetic Foot Ulcers: Results of a Randomized, Controlled Trial. Wounds. 2017;29:133–139. [PubMed] [Google Scholar]
- 82.Abela G. Benefits of maggot debridement therapy on leg ulcers: a literature review. Br J Community Nurs. 2017;22:S14–S19. doi: 10.12968/bjcn.2017.22.Sup6.S14. [DOI] [PubMed] [Google Scholar]
- 83.Faglia E, Favales F, Aldeghi A, Calia P, Quarantiello A, Oriani G, Michael M, Campagnoli P, Morabito A. Adjunctive systemic hyperbaric oxygen therapy in treatment of severe prevalently ischemic diabetic foot ulcer. A randomized study. Diabetes Care. 1996;19:1338–1343. doi: 10.2337/diacare.19.12.1338. [DOI] [PubMed] [Google Scholar]
- 84.Löndahl M, Katzman P, Nilsson A, Hammarlund C. Hyperbaric oxygen therapy facilitates healing of chronic foot ulcers in patients with diabetes. Diabetes Care. 2010;33:998–1003. doi: 10.2337/dc09-1754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Ma L, Li P, Shi Z, Hou T, Chen X, Du J. A prospective, randomized, controlled study of hyperbaric oxygen therapy: effects on healing and oxidative stress of ulcer tissue in patients with a diabetic foot ulcer. Ostomy Wound Manage. 2013;59:18–24. [PubMed] [Google Scholar]
- 86.Shen JT, Falanga V. Innovative therapies in wound healing. J Cutan Med Surg. 2003;7:217–224. doi: 10.1007/s10227-002-0106-5. [DOI] [PubMed] [Google Scholar]
- 87.Margolis DJ, Bartus C, Hoffstad O, Malay S, Berlin JA. Effectiveness of recombinant human platelet-derived growth factor for the treatment of diabetic neuropathic foot ulcers. Wound Repair Regen. 2005;13:531–536. doi: 10.1111/j.1524-475X.2005.00074.x. [DOI] [PubMed] [Google Scholar]
- 88.Veerapur BG, Uppin I, Babu YR. Chronic diabetic wound healing: Recombinant pdgf v/s normal saline. J Pharmaceut Biomed. 2012;24:118–120. [Google Scholar]
- 89.UCHI H, IGARASHI A, URABE K, KOGA T, NAKAYAMA J, KAWAMORI R, TAMAKI K, HIRAKATA H, OHURA T, FURUE M. Clinical efficacy of basic fibroblast growth factor (bFGF) for diabetic ulcer. Eur J Dermatol. 2009;19:461–468. doi: 10.1684/ejd.2009.0750. [DOI] [PubMed] [Google Scholar]
- 90.Fernández-Montequín JI, Valenzuela-Silva CM, Díaz OG, Savigne W, Sancho-Soutelo N, Rivero-Fernández F, Sánchez-Penton P, Morejón-Vega L, Artaza-Sanz H, García-Herrera A, González-Benavides C, Hernández-Cañete CM, Vázquez-Proenza A, Berlanga-Acosta J, López-Saura PA Cuban Diabetic Foot Study Group. Intra-lesional injections of recombinant human epidermal growth factor promote granulation and healing in advanced diabetic foot ulcers: multicenter, randomised, placebo-controlled, double-blind study. Int Wound J. 2009;6:432–443. doi: 10.1111/j.1742-481X.2009.00641.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Berlanga J, Fernández JI, López E, López PA, del Río A, Valenzuela C, Baldomero J, Muzio V, Raíces M, Silva R, Acevedo BE, Herrera L. Heberprot-P: a novel product for treating advanced diabetic foot ulcer. MEDICC Rev. 2013;15:11–15. doi: 10.37757/MR2013V15.N1.4. [DOI] [PubMed] [Google Scholar]
- 92.Beckmann KH, Meyer-Hamme G, Schröder S. Low level laser therapy for the treatment of diabetic foot ulcers: a critical survey. Evid Based Complement Alternat Med. 2014;2014:626127. doi: 10.1155/2014/626127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Minatel DG, Frade MA, França SC, Enwemeka CS. Phototherapy promotes healing of chronic diabetic leg ulcers that failed to respond to other therapies. Lasers Surg Med. 2009;41:433–441. doi: 10.1002/lsm.20789. [DOI] [PubMed] [Google Scholar]
- 94.Bus SA, Lavery LA, Monteiro-Soares M, Rasmussen A, Raspovic A, Sacco ICN, van Netten JJ International Working Group on the Diabetic Foot. Guidelines on the prevention of foot ulcers in persons with diabetes (IWGDF 2019 update) Diabetes Metab Res Rev. 2020;36 Suppl 1:e3269. doi: 10.1002/dmrr.3269. [DOI] [PubMed] [Google Scholar]