Abstract
Background
Selective serotonin reuptake inhibitors (SSRIs) are the most common class of medicines used for the treatment of major depression. Recent studies have reported an association between depression and inflammation and suggested the significant effects of SSRIs on inflammatory processes.
Methods
The current study aimed to evaluate the effects of fluoxetine, an SSRI, on the level of inflammatory cytokines, including interleukin-1β (IL-1β), interleukin-6 (IL-6), and tumor necrosis factor-α (TNF-α), in the rat serum and RAW264.7 mouse macrophage cell line, using ELISA sandwich assays. Also, the expression of inflammatory genes, including JAK/STAT3 and TLR4/JNK, was examined in macrophages, using real-time quantitative reverse transcription PCR to determine the potential mechanism of fluoxetine in inflammation. The rats received fluoxetine (10, 20, and 40 mg/kg) 30 min before lipopolysaccharide (LPS) treatment for 90 min. The cells received different doses of fluoxetine (5, 10, and 20 µg/mL) before stimulation with LPS for 24 or 48 h.
Results
The serum concentrations of IL-1β, IL-6, and TNF-α were reduced in rats and cells treated with fluoxetine. Following fluoxetine administration, the expression of JAK/STAT3 and TLR4/JNK genes was significantly decreased in the RAW264.7 cells treated with LPS for 24 h. However, after 48 h of treatment with LPS, fluoxetine failed to diminish the elevated expression of JAK and JNK genes, while it significantly decreased the expression of STAT3 and TLR4 genes.
Conclusion
The findings revealed that fluoxetine has anti‐inflammatory properties, mainly due to the reduction of inflammatory cytokines and inhibition of JAK/STAT3 and TLR4/JNK gene expression in macrophages.
Keywords: Fluoxetine, Anti-inflammatory, TNF-α, IL-1β, IL-6, JAK/STAT3, TLR4/JNK
Introduction
Major depressive disorder (MDD) or depression, which is a common and recurrent mood disorder accompanied by persistent feelings of sadness, affects one in every five people in their lifetime [1]. As a frequent disorder, MDD can negatively influence the quality of life of individuals. Several factors can contribute to the development of depression, including environmental, genetic, and immunological factors [2]. So far, several theories have been proposed regarding the biological basis of depression. The “monoamine theory” suggests that depression is caused by a lack of monoamine neurotransmission, especially serotonin [3]. However, it is believed that this theory is not sufficient to explain the therapeutic effects of antidepressants [4].
According to several studies, depression may involve inflammatory processes [5–7]. Therefore, overactivation of monocytes and macrophages, along with the increased concentration of proinflammatory cytokines, contributes to the pathology of depression. Based on these findings, the “macrophage theory of depression” has been formulated [2]. This theory is supported by the higher prevalence of depression in individuals with a diagnosis of disorders that are characterized by the activation of macrophages, such as rheumatoid arthritis, coronary heart disease, and stroke [7]. In this regard, a meta-analysis showed that depressed patients who did not use antidepressants had higher blood concentrations of proinflammatory cytokines, such as interleukin-6 (IL-6) and tumor necrosis factor-α (TNF-α), compared to healthy controls [8].
Different immune cells, including macrophages, mediate the complex inflammatory process. Macrophages are involved in inflammation through the release of cytokines and proinflammatory mediators, such as nitric oxide (NO), IL-6, IL-1β, TNF-α, and macrophage chemoattractant protein-1 (MCP-1) [9]. Stimulation of toll-like receptors (TLRs) on macrophages with lipopolysaccharide (LPS) can initiate some downstream signaling cascades, resulting in increased levels of inflammatory mediators, including NO, inducible NO synthase (iNOS), cyclooxygenase-2 (COX-2), prostaglandin E2 (PGE2), and proinflammatory cytokines (e.g., IL-1β, IL-6, and TNF-α) [10–12].
TLRs, as the key to the immune response to pathogenic invasions, are expressed on various immune-related cells. Stimulation of TLRs due to neuroinflammatory disorders, such as depression, activates immune-related cells, glial cells, and different cytokines and enzymes [13]. Among TLRs, TLR4 is associated with LPS recognition via activation of nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB)/c-Jun N-terminal kinase (JNK) pathway and the subsequent release of several proinflammatory cytokines, such as IL-6, TNF-α, interferon-beta (IFN-β), and MCP-1 [14, 15]. In addition, several mammalian cytokines, including interleukins and interferons, are capable of regulating the Janus kinase (JAK)/signal transducer and activator of transcription 3 (STAT3) pathway; this pathway is known to influence the pathogenesis of several inflammatory diseases [16, 17].
Despite the suggested association between depression and inflammatory processes, the effects of antidepressants on inflammation are not well studied. Selective serotonin reuptake inhibitors (SSRIs) are widely used antidepressants to treat obsessive–compulsive disorder, panic disorder, eating disorders and MDD. Compared to most antidepressants, SSRIs have minor side effects and are well tolerated by patients. However, only few studies have investigated the anti-inflammatory properties of SSRIs, which yielded inconsistent results [18–20].
Fluoxetine, a commonly prescribed SSRI, has been shown to affect several inflammatory and proinflammatory mediators in mice and microglial cells [21–23]. However, the anti-inflammatory effect of fluoxetine on macrophages has not been investigated to date.
Therefore, based on the macrophage theory of depression, the present study aimed to evaluate the effects of fluoxetine on the serum concentrations of IL-6, IL-1β, and TNF-α in rats and the RAW264.7 macrophage cell line and to determine its effects on JAK/STAT3 and TLR4/JNK gene expression in macrophages.
Materials and methods
Chemicals
Fluoxetine hydrochloride was purchased from Dr. Abidi Pharmaceuticals (Iran). The RAW264.7 mouse macrophage cell line was purchased from the Cell Bank of Pasteur Institute of Iran (Iran). Dimethyl sulfoxide (DMSO) and lipopolysaccharide (LPS from Escherichia coli 0127:B8) were obtained from Sigma-Aldrich (USA). RPMI-1640, Dulbecco's modified eagle medium (DMEM), and fetal bovine serum (FBS) were obtained from Bioidea (Iran). Collagen- and fibronectin-coated dishes were purchased from Padgin Teb Company (Iran).
Animals
Male Wistar rats (200–250 g) were provided by the animal house of Abadan University of Medical Sciences, Abadan, Iran, and kept in standard polypropylene cages (four animals per cage) in a 12:12 h light–dark cycle with free access to food and water. All experiments were conducted following the Guide for the Care and Use of Laboratory Animals of Abadan University of Medical Sciences. The experiments were approved by the medical research ethics committee of Abadan University of Medical Sciences (code: IR.ABADANUMS.REC.1396.213).
Preparation of rat serum samples and quantification of serum concentrations of IL-1β, IL-6, and TNF-α
The animals were divided into four groups randomly (eight animals in each group). The control group received vehicle (10 ml/kg of physiological saline) intraperitoneally (i.p.), while 10, 20, or 40 mg/kg of fluoxetine (i.p.) was injected to the fluoxetine groups. LPS (10 mg/kg, i.p.) was injected 30 min after drug administration. Blood sampling was carried out via cardiac puncture under anesthesia (40 mg/kg of pentobarbital, i.p.) 90 min following the injection of LPS. After coagulation, blood was centrifuged at 2000 g for 20 min to produce serum specimens. The serum levels of IL-1β, IL-6, and TNF-α were measured using commercial ELISA kits (Cat. No., IL-1β: BMS630; IL-6: BMS625; and TNF-α: KRC3011), based on the manufacturer’s instructions (eBioscience, San Diego, CA, USA). A microplate reader (BioRad, USA) was used to read absorbance at 450 nm.
Cell culture
The RAW264.7 cells were cultured in DMEM, supplemented with heat-inactivated FBS (10%) and 1% penicillin–streptomycin in a humidified atmosphere with 5% CO2 at 37 °C. The cells were grown to confluence on collagen- and fibronectin-coated dishes.
Cell viability assay
The toxicity of fluoxetine and LPS at the given concentrations was assessed in the RAW264.7 macrophages by the MTT assay. Generally, conversion of MTT to formazan indicates the mitochondrial function and cell viability [24]. The cells were plated at 104 cells/well in 96-well plates, followed by incubation with LPS (1 µg/mL) alone or in combination with fluoxetine (5, 10, or 20 µg/mL) for 24 and 48 h at 37 °C. The medium was replaced with RPMI-1640 phenol red-free medium (100 μL). Next, 10 μL of 12 mM MTT solution was added to each well, and incubation was performed for four hours at 37 °C.
Finally, to dissolve formazan crystals, 50 μL of DMSO solution was added to each well. A BioTek (Epoch, USA) microplate reader was used to measure the intensity of formazan blue dye at 570 nm.
Measurement of IL-1β, IL-6 and TNF-α concentration in the RAW 264.7 macrophage cell line
The RAW 264.7 macrophage cells (104cells in each well of 96-well plates) were pre-incubated with fluoxetine (5, 10, or 20 µg/mL) for one hour before LPS (1 μg/mL) administration for 24 h at 37 °C. The culture media were then collected and centrifuged at 800g to obtain the supernatants. The levels of IL-1β, IL-6, and TNF-α were assessed by commercial ELISA kits (R&D Systems, USA; Cat No., IL-1β: SMLB00C; IL-6: SM6000B; and TNF-α: SMTA00B). A microplate reader (BioRad, USA) was used to read absorbance at 450 nm.
Quantitative real-time polymerase chain reaction (PCR)
Real-time reverse transcription-PCR (RT-PCR) was employed to quantify the mRNA expression levels of target genes in the RAW264.7 cells. The cells were seeded in a 60 mm tissue culture dish (5 × 105 cells/well), followed by incubation for 12 h, which allowed the cells to adhere to the dish. Subsequently, the cells were rinsed three times with the medium. They were then treated with LPS (1 µg/mL), alone or in combination with various concentrations of fluoxetine (5, 10, or 20 µg/mL), for 24 or 48 h at 37 °C. Before harvesting the cells for RT-PCR, they were rinsed with phosphate-buffered saline (PBS). Total RNA was extracted using the RNX-Plus Solution (Sinaclon, Iran) and stored at − 80 °C. The concentration and quality of RNA preparations were calculated using a spectrophotometer at 260 and 280 nm. First-strand cDNA synthesis was performed with a Takara cDNA Synthesis Kit (Takara Bio Inc., Japan). Subsequently, real-time RT-PCR was conducted using a One-Step SYBR Green PrimeScript PLUS RT-PCR Kit (Takara Bio Inc., Japan) and gene-specific primers (listed in Table 1) under the following conditions: 95 °C for 10 min, and 45 cycles of denaturation (15 s/95 °C), annealing (30 s/55, 60 °C), extension (30 s/72 °C), and a final extension (10 min/72 °C). β-actin was used as the housekeeping gene. The relative concentrations of mRNAs were measured using the comparative CT method, with β-actin mRNA as the internal control. Data are reported as the optimal density/β-actin. The fold change for each specimen was assessed using the relative expression software tool (REST).
Table 1.
Primers for real-time RT-PCR
| Name | Sequences |
|---|---|
| β-actin F | 5′-ATCACTATTGGCAACGAGCG-3′ |
| β-actin R | 5′-TCAGCAATGCCTGGGTACAT-3′ |
| TLR-4 F | 5′-CGATTCTAGAACAAAACCAA-3′ |
| TLR-4 R | 5′-CTGGAAAGGAAGGTGTCA-3′ |
| JAK F | 5′-CTTCCACATAGACGAGTCAACCA-3′ |
| JAK R | 5′-CATCAAGCAGAGGAGCTTCAGC-3′ |
| JNK F | 5′-TTAAAGCCAGTCAGGCAAGG- 3′ |
| JNK R | 5′-GGTTGTGGGCATGTAGTTAC- 3′ |
| STAT3 F | 5′-ATCACGCCTTCTACAGACTGC-3′ |
| STAT3 R | 5′-CATCCTGGAGATTCTCTACCACT-3′ |
Statistical analysis
The normal distribution of data was evaluated using Kolmogorov–Smirnov test. The results showed that all data had a normal distribution. Data are presented as mean ± standard error of the mean (SEM). Statistical analyses were performed using one-way analysis of variance (ANOVA) and Tukey’s post hoc test. The level of statistical significance (P-value) was set at < 0.05.
Results
Effects of fluoxetine on the serum levels of IL-1β, IL-6 and TNF-α in rats
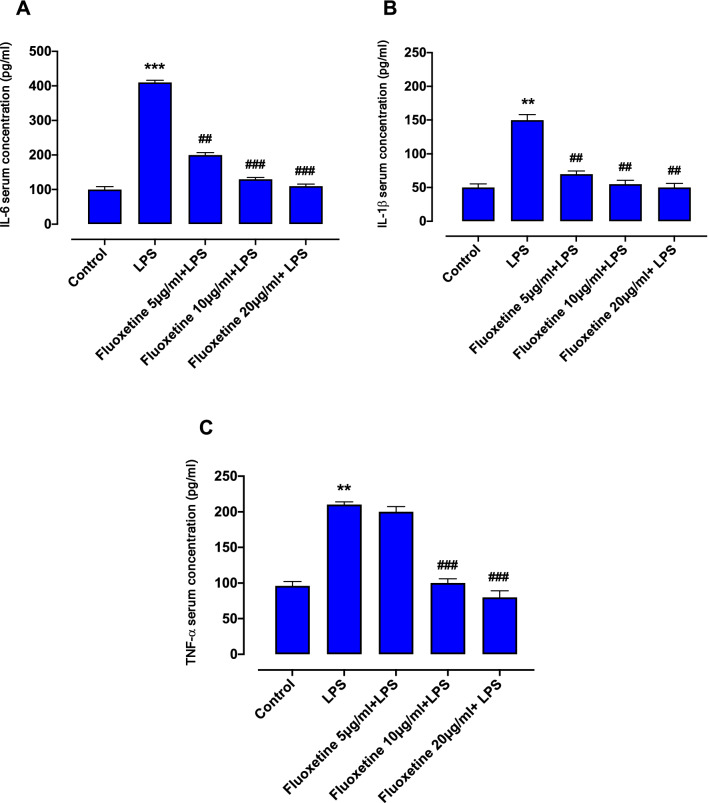
LPS significantly increased the serum concentrations of IL-1β, IL-6 and TNF-α in rat. Different doses of fluoxetine (10, 20, or 40 mg/kg) decreased the LPS-induced increase in the concentrations of IL-6 and IL-1β in the rat serum. The serum level of TNF-α was also decreased in the groups treated with 20 or 40 mg/kg of fluoxetine, but not 10 mg/kg, compared to the LPS group (Fig. 1).
Fig. 1.
Serum levels of IL-6 (A), IL-1β (B) and TNF-α (C) in rats treated with LPS (10 mg/kg) or LPS in combination with fluoxetine (10, 20 or 40 mg/kg). Values are mean + SEM (n = 8). ***p < 0.001 and **p < 0.01 statistically significant compared with control, ###p < 0.001 and ##p < 0.01 compared with LPS alone
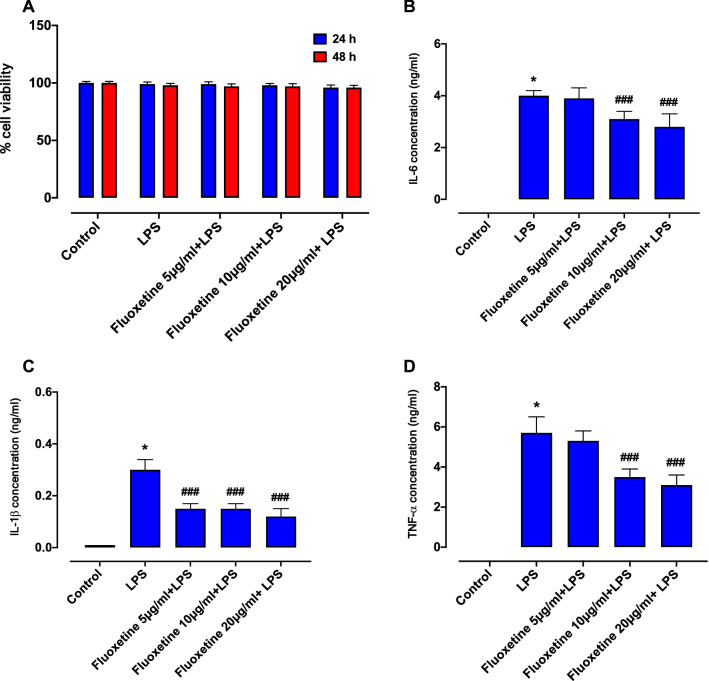
Effects of fluoxetine or LPS on cell viability
The MTT assay was applied to study the potential cytotoxic effects of fluoxetine and LPS on the RAW264.7 macrophage cells. The results showed that treatment with 1 μg/mL of LPS, alone or in combination with 5, 10, or 20 µg/mL of fluoxetine for 24 or 48 h, exerted no significant effects on cell viability compared to untreated cells (P < 0.05) (Fig. 2A).
Fig. 2.
Effects of LPS alone or in combination with fluoxetine on cell viability in RAW 264.7 macrophages (A). Cells were treated with LPS (1 μg/ml) alone or with increasing doses of fluoxetine (5, 10 or 20 µg/ml) for 24 or 48 h. Levels of IL-6 (B), IL-1β (C) and TNF-α (D) in RAW 256.7 macrophages treated with LPS (1 μg/ml) alone or in combination with fluoxetine (5, 10 or 20 μg/ml) for 24 h. Values are expressed as mean + SEM. All data are from three separate experiments in triplicate. *p < 0.05 statistically significant compared with control, ###p < 0.001 compared with LPS alone
Effects of fluoxetine on IL-1β, IL-6, and TNF-α levels in the RAW264.7 macrophage cell line
As shown in Fig. 2B–D, the levels of IL-1β, IL-6 and TNF-α were significantly increased in the RAW 264.7 macrophage cells after 24 h of stimulation with LPS (*P < 0.05). All tested doses of fluoxetine (5, 10, and 20 µg/mL) significantly reduced the concentration of IL-1β (###P < 0.001). The concentrations of IL-6 and TNF-α were also reduced in groups receiving 10 or 20 µg/mL of fluoxetine. However, treatment with 5 µg/mL of fluoxetine did not cause a significant reduction in the level of IL-6 or TNF-α compared to the LPS group.
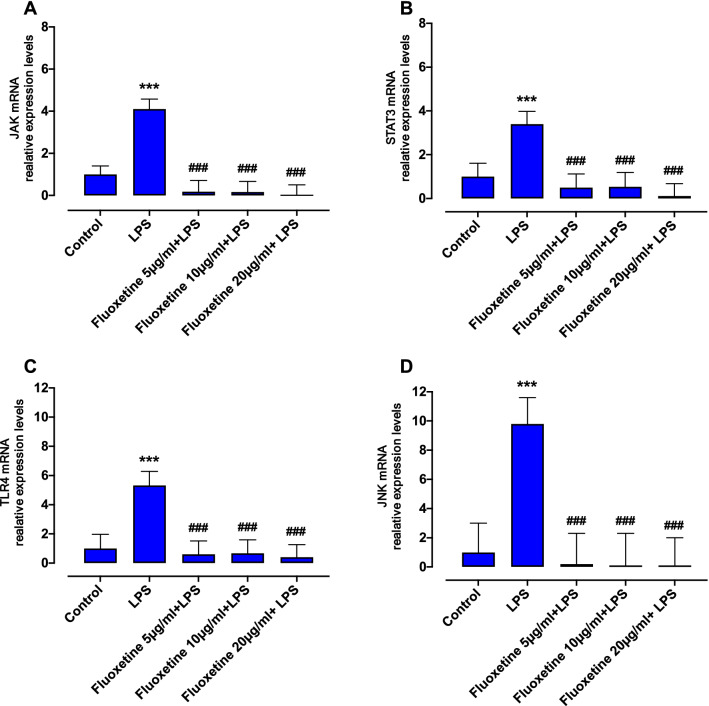
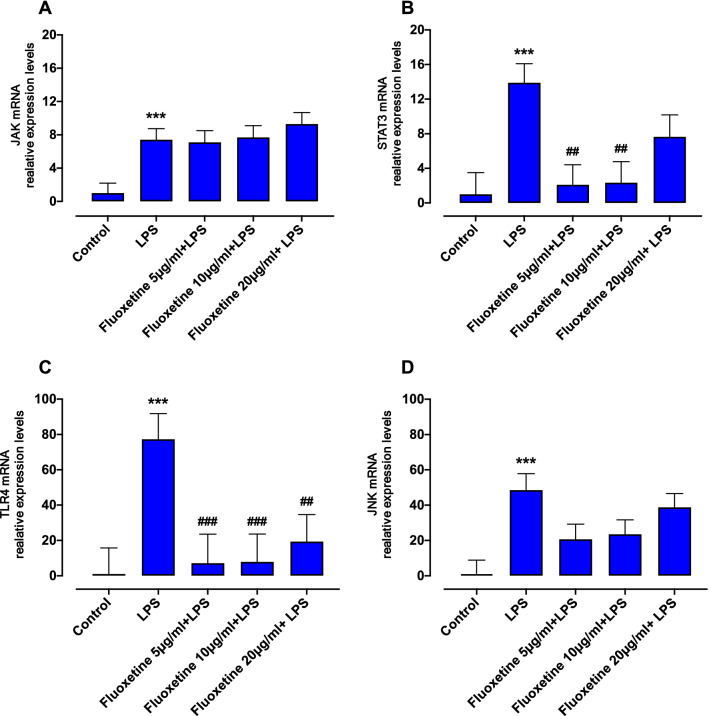
Effects of fluoxetine on the JAK/STATE3 gene expression in the RAW264.7 macrophage cell line
Our findings showed that the expression level of JAK was significantly increased in the RAW264.7 cells at 24 or 48 h post-LPS administration compared to the control group (***P < 0.001) (Figs. 3A, 4A). Fluoxetine (5, 10, or 20 µg/mL) significantly decreased the elevated gene expression of JAK after 24 h, but not after 48 h of treatment with LPS (Figs. 3A, 4A). In the LPS-treated cells, the STAT3 gene expression was significantly increased after 24 or 48 h (Figs. 3B, 4B). Moreover, fluoxetine at concentrations of 5, 10, or 20 µg/mL significantly decreased the STAT3 gene expression after 24 h of treatment with LPS (***P < 0.001) (Fig. 3B). The STAT3 gene expression was also significantly decreased by 5, or 10 µg/mL of fluoxetine in cells treated with LPS for 48 h (##P < 0.01) (Fig. 4B).
Fig. 3.
Effects of fluoxetine on expression levels of LPS-induced JAK (A), STAT3 (B), TLR4 (C) and JNK (D) in RAW264.7 macrophages. Cells were treated with LPS or LPS in combination with fluoxetine (5, 10 or 20 µg/ml) for 24 h. The mRNA expression data were normalized to the β-Actine signal and are presented as mean + SEM. All data are from three separate experiments in triplicate. ***p < 0.001 statistically significant compared with control, ###p < 0.001 compared with LPS alone
Fig. 4.
Effects of fluoxetine on expression levels of LPS-induced JAK (A), STAT3 (B), TLR4 (C) and JNK (D) in RAW264.7 macrophages. Cells were treated with LPS or LPS in combination with fluoxetine (5, 10 or 20 µg/ml) for 48 h. The mRNA expression data were normalized to the β-Actine signal and are presented as mean + SEM. All data are from three separate experiments in triplicate. ***p < 0.001 statistically significant compared with control, ###p < 0.001 and ##p < 0.01 compared with LPS alone
Effects of fluoxetine on TLR4/JNK gene expression in the RAW264.7 macrophage cell line
As shown in Figs. 3C, 4C, LPS increased the TLR4 gene expression in the RAW264.7 cells after 24 and 48 h compared to the control group (***P < 0.001). Fluoxetine at all concentrations decreased the TLR4 gene expression after 24 or 48 h of LPS treatment (##P < 0.01 and ###P < 0.001). Moreover, JNK expression was increased at 24 or 48 h post-LPS treatment (***P < 0.001, Figs. 3D, 4D). Fluoxetine significantly decreased the elevated expression of JNK gene in the RAW264.7 cells after 24 h of LPS treatment, but not after 48 h (###P < 0.001, Figs. 3D, 4D).
Discussion
The main findings of the present study indicated that fluoxetine reduced the concentrations of proinflammatory cytokines IL1β, IL-6, and TNF-α in the rat serum and RAW 264.7 macrophage cells treated with LPS. Fluoxetine also inhibited the expression of key inflammatory genes JAK/STAT3 and TLR4/JNK, in macrophage cells, without exhibiting cytotoxicity.
The etiology of depression is not completely understood, and may involve many factors, including the activation of macrophages, peripheral monocytes, and resident brain microglia, as well as high serum concentrations of proinflammatory cytokines [25, 26]. Importantly, lymphocytes and monocytes can release serotonin and noradrenaline, which exhibit immunomodulatory characteristics through receptors on immune cells [27]. Proinflammatory cytokines can increase monoamine and serotonin reuptake, thereby reducing monoaminergic and serotonergic neurotransmission, which are believed to have major roles in the pathology of depression [28–30].
The SSRIs and serotonin and norepinephrine reuptake inhibitors (SNRIs) exert their effects on MMD through inhibition of presynaptic transporters. Nonetheless, substantial evidence over decades suggests that these agents have some immunomodulatory effects, as well [22]. It has been reported that macrophages and other immune cells express norepinephrine [31] and serotonin [32] receptors and are sensitive to depression-related changes in the concentration of neurotransmitters; therefore, they may influence the action of antidepressants in the CNS synapses [2].
Additionally, antidepressants have been shown to prevent activation of microglia and decrease oxidative stress products in inflammation models induced by LPS and cytokines. All classes of antidepressants may prevent the LPS-induced release of cytokines, including IL-1β, IL-6, and TNF-α, by inhibiting the activation of immune-related intracellular signaling pathways, such as p38 MAPK, ERK, JNK, and NF-κB in microglia [33]. However, the anti-inflammatory effects of antidepressants on macrophages have been less investigated in previous studies. These agents may reduce the generation of macrophage-derived NO and reactive oxygen intermediates as potent mediators of innate and adaptive immune responses [2].
Fluoxetine is an SSRI antidepressant, associated with increased concentrations of 5-hydroxytryptamine (5-HT), with no impact on other neurotransmitter receptors. This medicine has been approved by the food and drug administration (FDA) for the treatment of major mental disorders, including posttraumatic stress disorder, menopausal vasomotor symptoms, bulimia nervosa, depression, generalized anxiety disorder, and premature ejaculation [34]. Although the therapeutic effects of fluoxetine have been investigated in several studies, it is not clear how it influences inflammation management. Therefore, the current study investigated the effects of fluoxetine on the concentrations of IL-1β, IL-6, and TNF-α in the rat serum and macrophage cells and also evaluated its effects on JAK/STAT3 and TLR4/JNK gene expression in macrophages following stimulation with LPS.
LPS, as the main component of the outer membrane of Gram-negative bacteria, is recognized by TLRs on macrophages. TLR activation leads to the production of proinflammatory cytokines, such as IL-1β, IL-6, and TNF-α, causing tissue destruction and cell damage in many inflammatory diseases [35, 36]. Amongst TLRs, TLR4 is best identified for recognition of LPS, and is expressed on several immune cells, including microglia, astrocytes, and macrophages. This receptor is involved in depression via activation of inflammatory pathways (e.g., NF-κB) and release of some proinflammatory cytokines [37, 38].
According to structural models, fluoxetine can physically interact with TLR4, similar to LPS, and form a complex, preventing NF-κB activation [39]. It has been reported that involvement of TLR4 and TLR9 can also stimulate STAT3 [40]. Activation of STAT3 by LPS can increase the production of IL-1β and IL-6 as major inflammatory mediators [41]. The anti-inflammatory activity of fluoxetine is also linked to glycogen synthase kinase-3 beta (GSK3 beta) phosphorylation, which possibly inhibits the generation of NO and PGE2 in the RAW macrophage cell line activated by LPS [42].
We found that LPS increased the levels of IL-1β, IL-6, and TNF-α in the rat serum and RAW 264.7 cells. LPS also up regulated the JAK/STAT3 and TLR4/JNK gene expression at 24 and 48 h following exposure. Fluoxetine decreased the concentrations of IL-1β, IL-6, and TNF-α in the rat serum and macrophages at 24 h post-exposure to LPS. It also reduced the elevated expression of JAK/STAT3 and TLR4/JNK genes following 24 h of stimulation with LPS. However, fluoxetine only reduced the increased gene expression of STAT3 and TLR4, but not JAK and JNK, induced by 48 h of LPS treatment. A longer LPS exposure may be associated with higher JAK and JNK upregulation, which cannot be reduced with fluoxetine at the given concentrations. Altogether, the current results indicated that fluoxetine significantly decreased the levels of proinflammatory cytokines both in vivo and in vitro.
In agreement with our findings, Rafiee et al. found that administration of fluvoxamine significantly reduced the expression of COX2, ICAM1, VCAM1, and iNOS in endothelial cells, macrophages, and rat carrageenan-related paw edema [43]. Tynan et al. also reported the anti-inflammatory effects of some SSRIs and SNRIs by altering the expression of TNF-α and NO in microglia cells [22]. Lu et al. investigated the anti-inflammatory effects of sertraline, an SSRI, and found that it bound to TNF-α and TNF receptors and diminished the level of TNF-α in microglia cells. They suggested that inhibiting the activation of microglia by the NF-κB signaling pathway might contribute to the antidepressant effects of sertraline [20].
Additionally, Ohgi et al. evaluated the effects of antidepressants on the serum levels of cytokines (i.e., IL-10 and TNF-α) and depressive-like behaviors in mice. They reported that antidepressant agents have anti-inflammatory properties in vivo, which are mediated by the serotonergic system [21]. Hajhashemi et al., in a study evaluating the anti‐inflammatory effects of venlafaxine (an SSNRI) in rats with carrageenan‐related paw edema, found that the potential anti‐inflammatory effects of venlafaxine were mostly related to the inhibition of IL‐1β and TNF‐α production [44].
Antidepressants, especially SSRIs, exhibit therapeutic effects in several clinical conditions due to their anti-inflammatory properties. The immunomodulatory effects and relationships between plasma cytokine levels and the therapeutic efficacy of venlafaxine and paroxetine, have been examined in patients with MDD. Overall, venlafaxine and paroxetine showed different immunomodulatory properties. Venlafaxine decreased the concentrations of IFNγ, TNF-α, IL-4, IL-5, IL-1β, and IL-8, while paroxetine increased the levels of IFNγ, TNF-α, and IL-6 and decreased Th2 cytokine levels [45]. In another study, escitalopram ameliorated asthma symptoms in patients with asthma and depression [46]. Also, fluoxetine protected against chronic methamphetamine-induced pulmonary inflammation [47] and ameliorated dyspnea and pulmonary arterial hypertension in chronic obstructive pulmonary disease (COPD) patients [48]. Recently, some clinical studies have investigated the efficacy of SSRIs in the management of COVID-19 symptoms, particularly cytokine storm [49–52]. In this regard, Firouzabadi et al. (2022) conducted a systematic meta-analysis on the effects of SSRIs/SNRIs in reducing the mortality of COVID-19 patients. Their findings revealed that the rate of mortality was decreased with fluoxetine and fluvoxamine treatment [49]. Altogether, consistent with the current findings, other studies on cells, animal models, and human patients indicated that antidepressant agents downregulated the secretion of proinflammatory cytokines and upregulated the release of anti-inflammatory cytokines. However, very few studies have evaluated the anti-inflammatory effects of SSRIs on macrophage cells, and there is no clear evidence regarding the exact pathways by which antidepressants reduce the secretion of cytokines by activated macrophages. Considering the role of macrophages in the pathology of depression, further research can provide new insights into the treatment of inflammation, as well as depressive disorders. Our findings demonstrated that fluoxetine might exert its anti-inflammatory effects by decreasing the levels of IL-1β, IL-6, and TNF-α and down regulating JAK/STAT3 and TLR4/JNK gene expression in macrophages.
The present study has some limitations. First, in addition to gene expression studies, further investigations are needed to evaluate the effects of fluoxetine on the protein levels of the transcription factor/signal proteins investigated in the current study. Second, drug treatment plans other than pretreatment with fluoxetine, which was used in the current study, might be considered. Third, the measurement of spleen weight is recommended in future studies, as evidence suggests that LPS increases the spleen weight and that the serum concentration of IL-6 is associated with the spleen weight in LPS-treated mice [53–55]. Finally, investigation of the anti-inflammatory effects of fluoxetine in both male and female rats can be useful in addressing potential sex differences.
Conclusion
Excessive inflammatory reactions contribute to the development of different cardiovascular, metabolic, and neuroendocrine disorders. Owing to their immunomodulatory effects, different antidepressants may be effectively used in complicated treatment plans for inflammatory and immune-mediated conditions by enhancing the patients’ mood and alleviating chronic inflammation. Fluoxetine reduces the expression of several key inflammatory genes, as well as the secretion of inflammatory cytokines in the macrophages and rat serum. However, further research on animal models of inflammation are required to confirm the potential application of this SSRI as an anti-inflammatory medicine in the future.
Acknowledgements
This work was supported by Abadan University of Medical Sciences.
Abbreviations
- COX2
Cyclooxygenase 2
- DMEM
Dimethyl sulfoxide
- ERKs
Extracellular signal-regulated kinases
- FBS
Fetal bovine serum
- FDA
Food and drug administration
- ICAM1
Intercellular adhesion molecule 1
- IL-6
Interleukin 6
- IL-1β
Interleukin 1β
- iNOS
Inducible nitric oxide synthase
- JAK/STAT
Janus kinase/signal transducer and activator of transcription
- JNK
C-Jun N-terminal kinase
- LPS
Lipopolysaccharide
- MAPK
Mitogen-activated protein kinase
- MCP
Monocyte chemoattractant protein
- MDD
Major depression disorder
- NF-κB
Nuclear factor kappa-light-chain enhancer of activated B cells
- NO
Nitric oxide
- PGE
Prostaglandin E
- RT-PCR
Reverse transcription polymerase chain reaction
- SNRI
Serotonin norepinephrine reuptake inhibitors
- SSRI
Serotonin selective reuptake inhibitors
- TLR
Toll like receptor
- TNF-α
Tumor necrosis factor α
- VCAM1
Vascular cell adhesion protein 1
- 5-HT
5-Hydroxytryptamine
Author contributions
HMF, MA and EK: Conceptualization; HMF and MA: methodology; HMF and AM: formal analysis; HMF, MA and AM: investigation; HMF, MA, EK, AM: writing—original draft preparation and review; HMF, EK: visualization. All authors have read and agreed to the published version of the manuscript.
Funding
This project was financially supported by Abadan University of Medical Sciences, Abadan, Iran. (Grant No: 96U-178).
Declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
All experiments were conducted following the Guide for the Care and Use of Laboratory Animals of Abadan University of Medical Sciences. The experiments were approved by the medical research ethics committee of Abadan University of Medical Sciences (code: IR.ABADANUMS.REC.1396.213).
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Hoda Mojiri-Forushani, Email: h.mojiriforushani@abadanums.ac.ir, Email: Dr.mojiri@yahoo.com.
Elham Khajehali, Email: elham.khajehali@unimelb.edu.au.
Maryam Adelipour, Email: adelipour-m@ajums.ac.ir.
Asma Mohammadi, Email: mohammadi.a@ums.ac.ir.
References
- 1.Ménard C, Hodes GE, Russo SJ. Pathogenesis of depression: insights from human and rodent studies. Neuroscience. 2016;321:138–162. doi: 10.1016/j.neuroscience.2015.05.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nazimek K, Strobel S, Bryniarski P, Kozlowski M, Filipczak-Bryniarska I, Bryniarski K. The role of macrophages in anti-inflammatory activity of antidepressant drugs. Immunobiology. 2017;222(6):823–830. doi: 10.1016/j.imbio.2016.07.001. [DOI] [PubMed] [Google Scholar]
- 3.Leonard BE. The immune system, depression and the action of antidepressants. Prog Neuropsychopharmacol Biol Psychiatry. 2001;25(4):767–780. doi: 10.1016/s0278-5846(01)00155-5. [DOI] [PubMed] [Google Scholar]
- 4.Sangkuhl K, Klein TE, Altman RB. Selective serotonin reuptake inhibitors pathway. Pharmacogenet Genom. 2009;19(11):907–909. doi: 10.1097/FPC.0b013e32833132cb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Young JJ, Bruno D, Pomara N. A review of the relationship between proinflammatory cytokines and major depressive disorder. J Affect Disord. 2014;169:15–20. doi: 10.1016/j.jad.2014.07.032. [DOI] [PubMed] [Google Scholar]
- 6.Zou W, Feng R, Yang Y. Changes in the serum levels of inflammatory cytokines in antidepressant drug-naïve patients with major depression. PLoS ONE. 2018;13(6):e0197267. doi: 10.1371/journal.pone.0197267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dionisie V, Filip GA, Manea MC, Manea M, Riga S. The anti-inflammatory role of SSRI and SNRI in the treatment of depression: a review of human and rodent research studies. Inflammopharmacology. 2021;29(1):75–90. doi: 10.1007/s10787-020-00777-5. [DOI] [PubMed] [Google Scholar]
- 8.Dowlati Y, Herrmann N, Swardfager W, Liu H, Sham L, Reim EK, et al. A meta-analysis of cytokines in major depression. Biol Psychiat. 2010;67(5):446–457. doi: 10.1016/j.biopsych.2009.09.033. [DOI] [PubMed] [Google Scholar]
- 9.Brummer E, Capilla J, Bythadka L, Stevens DA. Production of IL-6, in contrast to other cytokines and chemokines, in macrophage innate immune responses: effect of serum and fungal (Blastomyces) challenge. Cytokine. 2007;39(3):163–170. doi: 10.1016/j.cyto.2007.07.001. [DOI] [PubMed] [Google Scholar]
- 10.Fang H, Pengal RA, Cao X, Ganesan LP, Wewers MD, Marsh CB, et al. Lipopolysaccharide-induced macrophage inflammatory response is regulated by SHIP. J Immunol. 2004;173(1):360–366. doi: 10.4049/jimmunol.173.1.360. [DOI] [PubMed] [Google Scholar]
- 11.Takeda K, Kaisho T, Akira S. Toll-like receptors. Annu Rev Immunol. 2003;21(1):335–376. doi: 10.1146/annurev.immunol.21.120601.141126. [DOI] [PubMed] [Google Scholar]
- 12.Brint EK, Fitzgerald KA, Smith P, Coyle AJ, Gutierrez-Ramos J-C, Fallon PG, et al. Characterization of signaling pathways activated by the interleukin 1 (IL-1) receptor homologue T1/ST2 A role for Jun N-terminal kinase in IL-4 induction. J Biol Chem. 2002;277(51):49205–49211. doi: 10.1074/jbc.M209685200. [DOI] [PubMed] [Google Scholar]
- 13.Gárate I, Garcia-Bueno B, Madrigal JLM, Caso JR, Alou L, Gomez-Lus ML, et al. Stress-induced neuroinflammation: role of the Toll-like receptor-4 pathway. Biol Psychiat. 2013;73(1):32–43. doi: 10.1016/j.biopsych.2012.07.005. [DOI] [PubMed] [Google Scholar]
- 14.Hamidi A, von Bulow V, Hamidi R, Winssinger N, Barluenga S, Heldin CH, et al. Polyubiquitination of transforming growth factor β (TGFβ)-associated kinase 1 mediates nuclear factor-κB activation in response to different inflammatory stimuli. J Biol Chem. 2012;287(1):123–133. doi: 10.1074/jbc.M111.285122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Song Y, Dou H, Gong W, Liu X, Yu Z, Li E, et al. Bis-N-norgliovictin, a small-molecule compound from marine fungus, inhibits LPS-induced inflammation in macrophages and improves survival in sepsis. Eur J Pharmacol. 2013;705(1–3):49–60. doi: 10.1016/j.ejphar.2013.02.008. [DOI] [PubMed] [Google Scholar]
- 16.Coskun M, Salem M, Pedersen J, Nielsen OH. Involvement of JAK/STAT signaling in the pathogenesis of inflammatory bowel disease. Pharmacol Res. 2013;76:1–8. doi: 10.1016/j.phrs.2013.06.007. [DOI] [PubMed] [Google Scholar]
- 17.O'Shea JJ, Plenge R. JAK and STAT signaling molecules in immunoregulation and immune-mediated disease. Immunity. 2012;36(4):542–550. doi: 10.1016/j.immuni.2012.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rafiee L, Hajhashemi V, Javanmard SH. Maprotiline inhibits COX2 and iNOS gene expression in lipopolysaccharide-stimulated U937 macrophages and carrageenan-induced paw edema in rats. Central Euro J Immunol. 2019;44(1):15–22. doi: 10.5114/ceji.2019.84011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.de Sousa TV, Chaves Filho AJM, Cordeiro RC, Jucá PM, Soares MVR, Barroso PN, et al. Antidepressants of different classes cause distinct behavioral and brain pro-and anti-inflammatory changes in mice submitted to an inflammatory model of depression. J Affect Disord. 2020;268:188–200. doi: 10.1016/j.jad.2020.03.022. [DOI] [PubMed] [Google Scholar]
- 20.Lu Y, Xu X, Jiang T, Jin L, Zhao XD, Cheng JH, et al. Sertraline ameliorates inflammation in CUMS mice and inhibits TNF-α-induced inflammation in microglia cells. Int Immunopharmacol. 2019;67:119–128. doi: 10.1016/j.intimp.2018.12.011. [DOI] [PubMed] [Google Scholar]
- 21.Ohgi Y, Futamura T, Kikuchi T, Hashimoto K. Effects of antidepressants on alternations in serum cytokines and depressive-like behavior in mice after lipopolysaccharide administration. Pharmacol Biochem Behav. 2013;103(4):853–859. doi: 10.1016/j.pbb.2012.12.003. [DOI] [PubMed] [Google Scholar]
- 22.Tynan RJ, Weidenhofer J, Hinwood M, Cairns MJ, Day TA, Walker FR. A comparative examination of the anti-inflammatory effects of SSRI and SNRI antidepressants on LPS stimulated microglia. Brain Behav Immun. 2012;26(3):469–479. doi: 10.1016/j.bbi.2011.12.011. [DOI] [PubMed] [Google Scholar]
- 23.Ghosh S, Choudhury S, Chowdhury O, Mukherjee S, Das A, Sain A, et al. Inflammation-induced behavioral changes is driven by alterations in Nrf2-dependent apoptosis and autophagy in mouse hippocampus: role of fluoxetine. Cell Signal. 2020;68:109521. doi: 10.1016/j.cellsig.2019.109521. [DOI] [PubMed] [Google Scholar]
- 24.Mossman BT, Jean L, Landesman JM. Studies using lectins to determine mineral interactions with cellular membranes. Environ Health Perspect. 1983;51:23–25. doi: 10.1289/ehp.835123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Beumer W, Gibney SM, Drexhage RC, Pont-Lezica L, Doorduin J, Klein HC, et al. The immune theory of psychiatric diseases: a key role for activated microglia and circulating monocytes. J Leukoc Biol. 2012;92(5):959–975. doi: 10.1189/jlb.0212100. [DOI] [PubMed] [Google Scholar]
- 26.Stelzhammer V, Haenisch F, Chan MK, Cooper JD, Steiner J, Steeb H, et al. Proteomic changes in serum of first onset, antidepressant drug-naïve major depression patients. Int J Neuropsychopharmacol. 2014;17(10):1599–1608. doi: 10.1017/S1461145714000819. [DOI] [PubMed] [Google Scholar]
- 27.Finocchiaro LM, Arzt ES, Fernández-Castelo S, Criscuolo M, Finkielman S, Nahmod VE. Serotonin and melatonin synthesis in peripheral blood mononuclear cells: stimulation by interferon-7 as part of an immunomodulatory pathway. J Interferon Res. 1988;8(6):705–716. doi: 10.1089/jir.1988.8.705. [DOI] [PubMed] [Google Scholar]
- 28.Leonard BE. Depression: from psychopathology to pharmacotherapy. Karger Publishers; 2010. The concept of depression as a dysfunction of the immune system; pp. 53–71. [Google Scholar]
- 29.Ressler KJ, Nemeroff CB. Role of serotonergic and noradrenergic systems in the pathophysiology of depression and anxiety disorders. Depress Anxiety. 2000;12(S1):2–19. doi: 10.1002/1520-6394(2000)12:1+<2::AID-DA2>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 30.Roman A, Kuśmierczyk J, Klimek E, Rogóż Z, Nalepa I. Effects of co-administration of fluoxetine and risperidone on properties of peritoneal and pleural macrophages in rats subjected to the forced swimming test. Pharmacol Rep. 2012;64(6):1368–1380. doi: 10.1016/s1734-1140(12)70934-9. [DOI] [PubMed] [Google Scholar]
- 31.Slota C, Shi A, Chen G, Bevans M, Weng NP. Norepinephrine preferentially modulates memory CD8 T cell function inducing inflammatory cytokine production and reducing proliferation in response to activation. Brain Behav Immun. 2015;46:168–179. doi: 10.1016/j.bbi.2015.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shajib M, Khan W. The role of serotonin and its receptors in activation of immune responses and inflammation. Acta Physiol. 2015;213(3):561–574. doi: 10.1111/apha.12430. [DOI] [PubMed] [Google Scholar]
- 33.Mariani N, Everson J, Pariante CM, Borsini A. Modulation of microglial activation by antidepressants. J Psychopharmacol. 2022;36(2):131–150. doi: 10.1177/02698811211069110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chrousos GP, Katzung B, Trevor A. Adrenocorticosteroids and adrenocortical antagonists. New York: McGraw-Hill Medical; 2015. Basic and clinical pharmacology. [Google Scholar]
- 35.Layoun A, Santos MM. Bacterial cell wall constituents induce hepcidin expression in macrophages through MyD88 signaling. Inflammation. 2012;35(4):1500–1506. doi: 10.1007/s10753-012-9463-4. [DOI] [PubMed] [Google Scholar]
- 36.Dearman RJ, Cumberbatch M, Maxwell G, Basketter DA, Kimber I. Toll-like receptor ligand activation of murine bone marrow-derived dendritic cells. Immunology. 2009;126(4):475–484. doi: 10.1111/j.1365-2567.2008.02922.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Maes M, Coucke F, Leunis J-C. Normalization of the increased translocation of endotoxin from gram negative enterobacteria (leaky gut) is accompanied by a remission of chronic fatigue syndrome. Neuroendocrinol Lett. 2007;28(6):739–744. [PubMed] [Google Scholar]
- 38.Rahimifard M, Maqbool F, Moeini-Nodeh S, Niaz K, Abdollahi M, Braidy N, et al. Targeting the TLR4 signaling pathway by polyphenols: a novel therapeutic strategy for neuroinflammation. Ageing Res Rev. 2017;36:11–19. doi: 10.1016/j.arr.2017.02.004. [DOI] [PubMed] [Google Scholar]
- 39.Waiskopf N, Ofek K, Gilboa-Geffen A, Bekenstein U, Bahat A, Bennett ER, et al. AChE and RACK1 promote the anti-inflammatory properties of fluoxetine. J Mol Neurosci. 2014;53(3):306–315. doi: 10.1007/s12031-013-0174-6. [DOI] [PubMed] [Google Scholar]
- 40.Kortylewski M, Kujawski M, Herrmann A, Yang C, Wang L, Liu Y, et al. Toll-like receptor 9 activation of signal transducer and activator of transcription 3 constrains its agonist-based immunotherapy. Can Res. 2009;69(6):2497–2505. doi: 10.1158/0008-5472.CAN-08-3031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Samavati L, Rastogi R, Du W, Hüttemann M, Fite A, Franchi L. STAT3 tyrosine phosphorylation is critical for interleukin 1 beta and interleukin-6 production in response to lipopolysaccharide and live bacteria. Mol Immunol. 2009;46(8–9):1867–1877. doi: 10.1016/j.molimm.2009.02.018. [DOI] [PubMed] [Google Scholar]
- 42.Su HC, Ma CT, Yu BC, Chien YC, Tsai CC, Huang WC, et al. Glycogen synthase kinase-3β regulates anti-inflammatory property of fluoxetine. Int Immunopharmacol. 2012;14(2):150–156. doi: 10.1016/j.intimp.2012.06.015. [DOI] [PubMed] [Google Scholar]
- 43.Rafiee L, Hajhashemi V, Javanmard SH. Fluvoxamine inhibits some inflammatory genes expression in LPS/stimulated human endothelial cells, U937 macrophages, and carrageenan-induced paw edema in rat. Iran J Basic Med Sci. 2016;19(9):977. [PMC free article] [PubMed] [Google Scholar]
- 44.Hajhashemi V, Minaiyan M, Banafshe HR, Mesdaghinia A, Abed A. The anti-inflammatory effects of venlafaxine in the rat model of carrageenan-induced paw edema. Iran J Basic Med Sci. 2015;18(7):654. [PMC free article] [PubMed] [Google Scholar]
- 45.Chen CY, Yeh YW, Kuo SC, Liang CS, Ho PS, Huang CC, et al. Differences in immunomodulatory properties between venlafaxine and paroxetine in patients with major depressive disorder. Psychoneuroendocrinology. 2018;87:108–118. doi: 10.1016/j.psyneuen.2017.10.009. [DOI] [PubMed] [Google Scholar]
- 46.Brown ES, Sayed N, Van Enkevort E, Kulikova A, Nakamura A, Khan DA, et al. A randomized, double-blind, placebo-controlled trial of escitalopram in patients with asthma and major depressive disorder. J Allergy Clin Immunol Pract. 2018;6(5):1604–1612. doi: 10.1016/j.jaip.2018.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wang Y, Gu YH, Liu M, Bai Y, Wang HL. Fluoxetine protects against methamphetamine-induced lung inflammation by suppressing oxidative stress through the SERT/p38 MAPK/Nrf2 pathway in rats. Mol Med Rep. 2017;15(2):673–680. doi: 10.3892/mmr.2016.6072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yohannes AM, Connolly MJ. Do antidepressants work in patients with chronic obstructive pulmonary disease with comorbid depression? Expert Rev Respir Med. 2011;5(6):727–729. doi: 10.1586/ers.11.70. [DOI] [PubMed] [Google Scholar]
- 49.Firouzabadi D, Kheshti F, Abdollahifard S, Taherifard E, Kheshti MR. The effect of selective serotonin and norepinephrine reuptake inhibitors on clinical outcome of COVID-19 patients: a systematic review and meta-analysis. Health Sci Rep. 2022;5(6):e892. doi: 10.1002/hsr2.892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hamed MGM, Hagag RS. The possible immunoregulatory and anti-inflammatory effects of selective serotonin reuptake inhibitors in coronavirus disease patients. Med Hypotheses. 2020;144:110140. doi: 10.1016/j.mehy.2020.110140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mahdi M, Hermán L, Réthelyi JM, Bálint BL. Potential role of the antidepressants fluoxetine and fluvoxamine in the treatment of COVID-19. Int J Mol Sci. 2022;23(7):3812. doi: 10.3390/ijms23073812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Creeden JF, Imami AS, Eby HM, Gillman C, Becker KN, Reigle J, et al. Fluoxetine as an anti-inflammatory therapy in SARS-CoV-2 infection. Biomed Pharmacother. 2021;138:111437. doi: 10.1016/j.biopha.2021.111437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zhang J, Ma L, Chang L, Pu Y, Qu Y, Hashimoto K. A key role of the subdiaphragmatic vagus nerve in the depression-like phenotype and abnormal composition of gut microbiota in mice after lipopolysaccharide administration. Transl Psychiatry. 2020;10(1):1–13. doi: 10.1038/s41398-020-00878-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zhang J, Ma L, Wan X, Shan J, Qu Y, Hashimoto K. (R)-Ketamine attenuates LPS-induced endotoxin-derived delirium through inhibition of neuroinflammation. Psychopharmacology. 2021;238(10):2743–2753. doi: 10.1007/s00213-021-05889-6. [DOI] [PubMed] [Google Scholar]
- 55.Ma L, Zhang J, Fujita Y, Qu Y, Shan J, Wan X, et al. Nuclear factor of activated T cells 4 in the prefrontal cortex is required for prophylactic actions of (R)-ketamine. Transl Psychiatry. 2022;12(1):1–10. doi: 10.1038/s41398-022-01803-6. [DOI] [PMC free article] [PubMed] [Google Scholar]