Abstract
Purpose
In the Netherlands, patients can often choose between the laparoscopic Roux-en-Y gastric bypass (RYGB) and sleeve gastrectomy (SG) as primary bariatric surgery. Yet, patients confronted with medical options may experience decisional conflict when their stakes are high and outcomes uncertain.
This study aimed to assess if a decision aid helps patients make informed choices between two bariatric procedures by lowering the level of decisional conflict.
Materials and Methods
This study was a single-center comparative cohort of patients who accessed a web-based decision aid (intervention group) and those who did not use the decision aid (control group) to help choose between two bariatric procedures additional to the standard provided care. The primary outcome was the level of decisional conflict in these patients using the decisional conflict scale (DCS). Secondary outcomes were patient satisfaction with the provided information (BODY-QTM—satisfaction with information), preference of involvement in procedure selection, level of shared decision-making (SDM-Q-9 questionnaire), and patient knowledge.
Results
The level of decisional conflict assessed with the decisional conflict scale (DCS) showed a significantly lower mean total DCS of 25.5 ± 11.5 for the intervention group vs. 29.1 ± 12.4 in the control group (p = 0.022). Both groups did not significantly differ in satisfaction regarding provided information, involvement in the selection procedure, shared decision-making, and patient knowledge.
Conclusion
The results suggest that the additional use of a decision aid significantly lowers the level of decisional conflict in patients awaiting bariatric surgery. However, the added value should be further investigated.
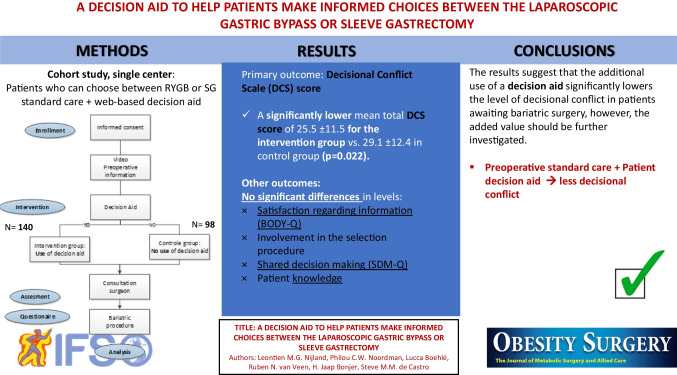
Graphical Abstract
Keywords: Decision aid, Decisional conflict, Bariatric procedure, Gastric bypass, Sleeve Gastrectomy
Introduction
The primary laparoscopic Roux-en-Y gastric bypass (RYGB) and sleeve gastrectomy (SG) are the most commonly performed surgical weight loss procedures. Yet, there is large heterogeneity in the proportion of these two bariatric procedures in different countries. In the Netherlands, the laparoscopic RYGB accounts for approximately 80% of all bariatric primary procedures [1]. Contrary, the SG is the most commonly performed procedure in the USA and accounts for about 60% of all performed primary bariatric surgeries [2].
To date, most bariatric centers offer both the laparoscopic RYGB and SG as primary bariatric surgery. In the Netherlands, patients can choose between these procedures. Both procedures are effective with each having its advantages and disadvantages [3–5]. Often patients will be counseled by the bariatric surgeon and take part in a process of shared decision-making to reach an agreement on treatment choice. Yet, patients who are confronted with two or more options may experience “decisional conflict,” which is defined as personal uncertainty about which course of action to take when a choice among competing options involves risk, regret, or challenge to personal life value. In particular, those patients who feel uninformed, who have unclear personal preferences, or who feel unsupported in the process may feel decisional conflict. In the bariatric population, many patients are offered two surgical options and may also experience decisional conflict as their health risks may be high and outcomes relatively uncertain.
The level of decisional conflict in patients can be lowered with decision-supporting interventions [6–8]. A relatively new way to support patients in the decisions making process is by offering a decision aid. The definition of a decision aid is “an intervention that supports patients by making their decisions explicit, providing information about options and associated benefits/harms and advantages/disadvantages, and helping clarify congruence between decisions and personal values” [8]. Decision aids can be an important adjunct in patients facing different surgical options with a universal goal and may reduce uncertainty and regret in patients [9, 10].
In many healthcare areas, researchers have assessed the use of decision aids for a wide variety of decision contexts such as for the treatment of early-stage breast cancer, BRCA 1 and 2 mutation carriers, prostate hypertrophy, arthritis, prosthetic heart valve selection, asymptomatic abdominal aortic aneurysm treatment, and pregnancy care [6, 7, 11–16]. Most of these studies have found supporting evidence of the attributive value of the use of a decision aid, and many authors suggest the development of decision aids should be encouraged. Yet, little is known about the value of a decision aid for patients undergoing bariatric surgery who can choose between two different primary bariatric procedures.
The purpose of this study was to assess if a decision aid helps patients make informed choices between two bariatric procedures by lowering the level of decisional conflict.
Methods
Study Design
The study was a single-center comparative cohort study of patients who used an additional decision aid (intervention group) and those who did not use the decision aid (control group) in addition to the video with information about the bariatric procedure options and an individual consultation of a bariatric surgeon (Fig. 1). The study was conducted from March 2020 until July 2021. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The original study proposal was a randomized controlled trial but due to the COVID-19 pandemic and local hospital restrictions, the patient could not be randomized. The study proposal was changed to a comparative cohort study and approved by the Medical Ethical Committee. The study population included patients aged between 18 and 65 years who were diagnosed with morbid obesity based on the IFSO criteria and were approved by a multidisciplinary team of surgeons, internal medicine physicians, dieticians, ergo therapists, and psychologists for either an elective primary RYGB or SG. Exclusion criteria were patients who previously had bariatric surgery, patients with an individual-based bariatric preoperative program, patients unable to understand the Dutch language, and patients who do not have a free choice in the type of bariatric procedure (e.g., kidney failure in pre-dialysis stage, Crohn’s disease). Patients eligible for this study were informed about the study using a patient information folder. Informed consent was obtained from all individual participants included in the study. Patients who enrolled in the study but did not complete the questionnaire for more than 50% were excluded from the analysis.
Fig. 1.
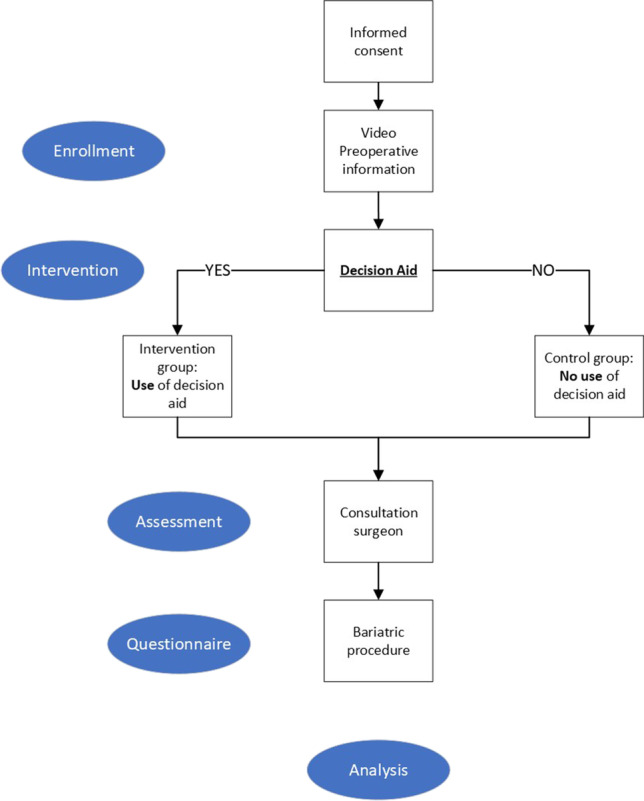
Study flowchart
Study Protocol
All patients included in this study were screened for eligibility for bariatric surgery according to IFSO criteria by a multidisciplinary team [17]. All patients eligible for a primary bariatric procedure followed a group-based bariatric lifestyle program which consisted of 6 mandatory preoperative group sessions focusing on lifestyle and dietary adjustments over a period of 6 weeks [18]. After completing the preoperative program, each patient was sent a video with patient information about the surgical options, i.e., the laparoscopic RYGB and SG. In this video, a bariatric surgeon provides information in a uniform, unbiased, and comprehensive way to all patients using diagrams. Before surgery, each patient was individually consulted by a bariatric surgeon to discuss the choice of procedure and obtain consent as required by the Medical Treatment Contracts Act (WBGO in the Netherlands).
Intervention
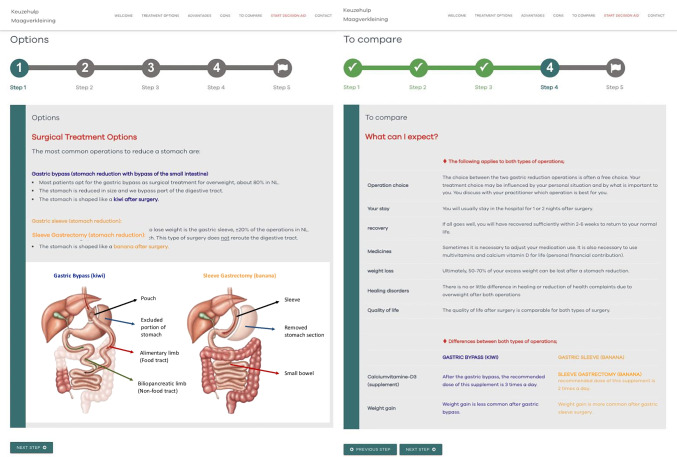
Patients in the intervention group used the decision aid in addition to the standard provided care. This decision aid was developed according to an iterative participatory design approach to fit the needs of patients and utilizing the Ottawa Decision Support Framework and the International Patient Decision Aid Standards IPDAS criteria checklist (IPDASi v3.0). The Ottawa Decision Support Framework was devised to guide the development of special interventions for shared decision-making [19]. The IPDAS guidelines are an evidence-based, practical theory used to assess the quality of patient decision aids (PDAs) in terms of their development process and shared decision-making design components [20]. The web-based decision aid was password protected and accessible for patients participating in the study using the link. The web-based decision aid consisted of a 5-step module consisting of information about the procedural options, the benefits, the potential harms, probabilities, and options features to clarify personal values and expectations. In the Appendix, two screenshots of the web-based decision aid are presented. To check if the decision aid was accessed by the patients, each patient filed a form at the end of the web-based decision aid module. In addition, patients were actively asked if they had gone through the decision aid in the questionnaire sent after the consultation. About 1 week after sending the video and providing access to the online decision aid patients were contacted by the surgeon for a preoperative consultation in which the bariatric procedure of preference was discussed. After the consultation, all patients were digitally sent a questionnaire to assess the outcomes using Castor EDC. Patients were allowed to change their choice of bariatric procedure at any time.
Primary and Secondary Outcomes
Baseline characteristics were obtained from patient files, including age, sex, weight, and comorbidities. The primary aim was to assess if the decision aid which helps patients choose between two primary bariatric procedures can lower the level of decisional conflict. The level of decisional conflict in the patient was assessed using the validated decisional conflict scale (DCS) [21]. The DCS in the 16-item format is a scale consisting of 5 subscales: (1) informed, (2) values clarity, (3) support, (4) uncertainty, and (5) effective decision subscale with 5 response categories. Items were given a score value of 0 (“strongly agree”) to 4 (“strongly disagree”). Mean scores were converted to the equivalent of 0–100 with 0 meaning no decisional conflict to 100 meaning extremely high decisional conflict. Scores lower than 25 are associated with feeling secure about the decision; scores exceeding 37.5 are associated with decision delay or feeling unsure about the decision [22].
Secondary outcomes were patient satisfaction with information using the BODY-QTM—satisfaction with information [23], and the patient preference regarding involvement in the selection procedure (4 response questions) and the 9-item patient version of the shared decision-making questionnaire, SDM-Q-9, with 6 response options [24]. The BODY-QTM—satisfaction with information consists of 10 items, with 4 response options. Items were given a score value of 1 (“very dissatisfied”) to 4 (“very satisfied”), and sum scores were converted to a rash score between 0 (“worst”) to 100 (“best”). All items of the SDM-Q-9 are scored on a six-point scale that ranges from 0 (“completely disagree”) to 5 (“completely agree”). The total score based on all items leads to a raw score between 0 and 45, with 0 indicating the lowest and 45 indicating the highest level of perceived SDM [24].
Sample Size
An a priori sample size calculation was performed based on the MCID of the decisional conflict scale (DCS). We calculated an estimated total of 98 patients per group (ratio 1:1) to detect a 4-point difference in decisional conflict score using an effect size of 0.4 (2-tailed, power = 80%, α = 0.05) [25]. Randomizing patients into two equal groups was not possible as mentioned before.
Statistical Analysis
Data were analyzed using SPSS version 22.0. Continuous data were displayed as mean (± standard deviation) or median (min–max) based on the normality, which was tested using histograms. Categorical data were presented in numbers (n) with percentages (%). Data of groups were compared using an independent T-test (T-test) for parametric data, a Mann–Whitney U for non-parametric data, or a chi-square test (X2 test) in case of categorical data and presented with 95% confidence intervals (CI) and P value. A p-value of p ≤ 0.05 was considered statistically significant.
Results
Thirteen patients who completed the questionnaire for less than 50% were excluded after enrolling in the study. A total of 238 patients were included of whom 140 used the additional decision aid (intervention group) and 98 patients received the standard care (control group). Patients in both groups were comparable based on baseline characteristics shown in Table 1. Table 2 shows the distribution of the bariatric procedures chosen.
Table 1.
Baseline characteristics
| Intervention group n = 140 |
Control group n = 98 |
P value | |
|---|---|---|---|
| Age (years, mean) | 43 ± 12 | 41 ± 11 | .109¥ |
| Gender (n, %) | |||
| Female | 112 (80.0) | 82 (83.7) | .475⁋ |
| Male | 28 (20.0) | 16 (16.3) | |
| Preoperative weight (kg) | 124 ± 20 | 120 ± 17 | .155¥ |
| BMI (kg/m2, mean) | 42 ± 5 | 42 ± 5 | .441¥ |
| Hypertension (n, %) | 38 (27.1) | 25 (25.5) | .779⁋ |
| NIDDM (n, %) | 12 (8.6) | 9 (9.2) | .870⁋ |
| IDDM (n, %) | 6 (4.3) | 2 (2.0) | .344⁋ |
| OSA (AHI ≥ 5) | 84 (60.0) | 50 (51.0) | .169⁋ |
| CPAP | 49 (57.1) | 22 (42.0) | .090⁋ |
| Dyslipidemia (n, %) | 18 (12.9) | 9 (9.2) | .379⁋ |
| Psychiatric history | 41 (70.7) | 28 (71.4) | .905⁋ |
| Depression (n, %) | 20 (14.3) | 18 (18.4) | .398⁋ |
| GERD (n, %) | 14 (10.0) | 12 (12.2) | .585⁋ |
BMI, body mass index; NDDM, non-insulin-dependent diabetes mellitus; IDDM, insulin-dependent diabetes mellitus; OSA, obstructive sleep apnea; CPAP, continuous positive airway pressure; GERD, gastroesophageal reflux disease
⁋chi-square
¥T-test
Table 2.
Distribution of bariatric procedures
| Intervention group n = 140 |
Control group n = 98 |
P value⁋ | |
|---|---|---|---|
| Roux-en-Y gastric bypass (n, %) | 116 (82.9) | 78 (79.6) | .800 |
| Sleeve gastrectomy (n, %) | 22 (15.7) | 18 (16.8) | |
| I do not know (yet) (n, %) | 2 (1.4) | 2 (2.0) |
⁋chi-square
Primary Outcome
The level of decisional conflict in choosing between the two bariatric procedures assessed with the decisional conflict scale (DCS) showed a significantly lower mean total DCS of 25.5 ± 11.5 for the intervention group compared to 29.1 ± 12.4 for the control group (p = 0.022) as shown in Table 3. The sub-scores of both groups are displayed in Table 3 with significantly lower scores in the intervention group for the subscales support (p = 0.023), uncertainty (p = 0.003), and effective decision (p = 0.019).
Table 3.
Primary and secondary outcomes
| Decisional conflict scale (DCS) |
Intervention group n = 140, mean ± SD |
Control group n = 98, mean ± SD |
P value¥ |
| Total score | 25.5 ± 11.5 | 29.1 ± 12.4 | .022 |
| Subscales | |||
| Informed | 36.6 ± 13.1 | 34.6 ± 12.6 | .320 |
| Values clarity | 29.8 ± 22.0 | 33.7 ± 23.7 | .192 |
| Support | 19.9 ± 15.3 | 24.3 ± 13.4 | .023 |
| Uncertainty | 26.6 ± 16.2 | 33.0 ± 15.6 | .003 |
| Effective decision | 17.7 ± 14.2 | 22.4 ± 16.3 | .019 |
| BODY-Q satisfaction with information |
Intervention group n = 140, mean ± SD |
Control group n = 95, mean ± SD |
P value¥ |
| Total score | 65.9 ± 17.5 | 63.9 ± 17.2 | .369 |
| Shared decision-making (SDM-9) |
Intervention group n = 138, mean ± SD |
Control group n = 93, mean ± SD |
P value¥ |
| Total score | 26.6 ± 10.7 | 27.2 ± 8.7 | .676 |
¥T-test
Secondary Outcomes
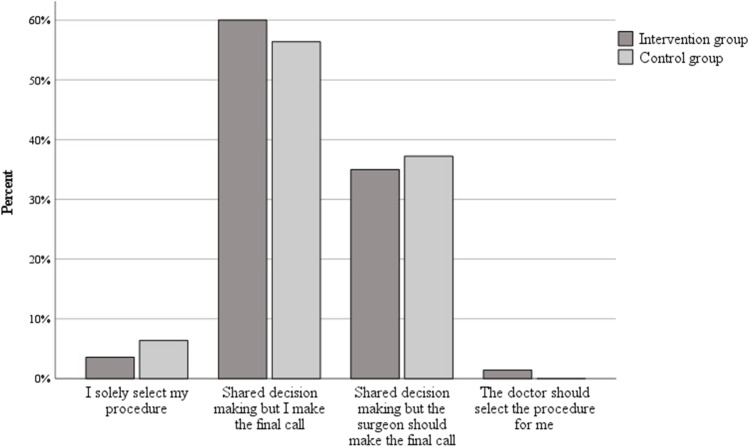
The level of patient satisfaction with information provision assessed with the “BODY-QTM—Satisfaction with information” scale showed mean scores of 65.9 ± 17.5 for the intervention and 63.9 ± 17.2 for the control group. These mean scores did not differ significantly (p = 0.369). Figure 2 shows a 4-option question and the percentage frequency distribution of the patient preference regarding the surgeon’s involvement in procedural selection. Of all study patients in both groups, 95% of patients choose the option of shared decision-making, with 59% of patients saying they wish to make the final call themselves and 36% saying they wish the surgeon should make the final call. There was no significant difference in this distribution between the intervention group and the control group (p = 0.477). The actual degree of shared decision-making in the actual selection procedure was assessed with mean SDM-Q-9 scores of 26.6 ± 10.7 for the intervention and 27.2 ± 8.7 for the control group (p = 0.676). Table 4 shows the number and percentages of the three questions correctly answered.
Fig. 2.
Patient preference regarding the surgeon’s involvement in decision-making
Table 4.
Patient knowledge
| 3 knowledge questions | Intervention group n = 138 |
Control group n = 93 |
P value⁋ |
|---|---|---|---|
| Questions correct | .653 | ||
| 3 out of 3 (n, %) | 52 (38) | 31 (33) | |
| 2 out of 3 (n, %) | 60 (44) | 39 (42) | |
| 1 out of 3 (n, %) | 24 (17) | 20 (22) | |
| 0 out of 3 (n, %) | 2 (1) | 3 (3) | |
⁋chi-square, n, number
Discussion
The purpose of this study was to assess if a decision aid helps patients make informed choices between two bariatric procedures by lowering the level of decisional conflict. The results of the primary outcome showed that the level of decisional conflict (total DCS) was significantly lower in patients who used the decision aid compared to those who did not. Yet, the added value of the decision aid remains limited as the levels of satisfaction regarding provided information, involvement in the selection procedure, shared decision-making, and patient knowledge did not differ significantly between both groups.
The results of the DCS showed a significantly lower mean DCS total score for the group of patients who used the decision; however, the DCS subscale differences were smaller and not all statistically significant which was disappointing. Overall, the absolute mean scores of, i.e., 25.5 and 29.1 indicate that patients awaiting bariatric surgery experience a low level of decisional conflict as scores range from 0 to 100, zero meaning no decisional conflict, and 100 meaning strong conflict. Further looking at a mean difference of 3.6 DCS points and the absolute scores, both being within 25 and 37.5, respectively, the cut-off values for “feeling secure” and “feeling unsure” about the decision, you could argue that the value of the decision aid remains limited [22]. These relatively low conflict levels could be explained by the fact that the decision aid was offered additional to standard counseling and not as a substitute to standard counseling which normally in part of an extensive trajectory by a multidisciplinary team involving a surgical team, dieticians, and the psychologists.
We were not able to assess the DCS scale scores without standard counseling and the change in scores over time. This would have been interesting since the review of 253 studies by Garvelink et al. found that overall DCS scores tend to decrease in the short-term but increased or remained the same in the long-term (> 6 months) whereas DCS scores in patients not exposed to any decisional support interventions tended to increase shortly after decision-making [26].
As far as we know, only one previous study in bariatric surgery compared the efficacy of a video-based decision aid to a paper-based educational booklet aiming to help patients decide whether or not to undergo bariatric surgery [24]. This study found reduced decisional conflict after providing a video-based decision aid instead of the educational booklet. Obviously, this study is not comparable to this current study regarding the choice options, type of intervention, and control group as we used the decision aid as supplementary to the standard provided information. Authors of a Cochrane review of 105 studies using DCS concluded that people exposed to decision aids feel more knowledgeable, better informed, clearer about their values, and play a more active role in shared decision-making [8]. Comparing this conclusion with the present results of our decision aid study, we cannot confirm a significant improvement in knowledge based on three knowledge questions, and the subscales of the DCS showed no improved informed feeling or clarity about the values in the patient who used the decision aid. However, this study was not powered on these knowledge questions or single subscales. In addition, we hoped the decision aid would further promote the level of shared decision-making; however, the scores of the SDM-Q to assess the effect of the decision aid on the process of the shared decision showed no significant difference between the groups. This could potentially have been the result of the provision of both a standardized video with patient information and an individual consultation to discuss the surgical procedure with all preoperative patients regardless of the use of the decision aid.
This present study has several limitations that need to be addressed. At first, the study design, a cohort of patients who did or did not use the decision aid, despite comparable baseline characteristics, may have led to selection bias. In addition, another potential source of bias could have been the way the surgeon provided information during the individual consultations which may have affected the level of decision conflict on the individual level. Second, despite that the decision aid was designed following the IDPAS guidelines for decision aids, the decision aid was not externally validated to be used in other centers. Third, we were not able to identify those patients who may benefit from the use of the decision aid supplementary to the standard care including the surgeon’s consultation. It would be interesting to identify particular groups and provide a more tailor-made approach in the preparation of the decision-making process. At last, you could question the utility of such a decision aid in clinics where patients are less involved in procedure selection, where one is less positive about the comparability of these procedures and promote one superior surgery for all.
Future research, preferably a randomized controlled trial, should evaluate the effect of the decision aid on decisional conflict and shared-decision levels at different time points. In addition, we should assess the usability, patient satisfaction, and cost-effectiveness of the decision aid as the decision aid may secondarily lead to more effective patient counseling. Our next step in refining the decision aid is to reinforce a national steering group including patient representatives that will allow further improvement, acknowledgment of the content, and implementation of the decision aid on a broader level.
In summary, this is the first study that assessed a web-based decision aid to help patients choose between the two primary bariatric procedures. Results suggest that the decision aid significantly lowers the level of decisional conflict, whereas the use of decision aids should be considered in the bariatric population with surgical options.
Appendix. Panel A and B: Two screenshots of the 5-step module decision aid
Data Availability
All data used in this research is accessible and available for reuse.
Declarations
Ethics Approval
This study has been approved by the national and local Medical Ethical Committee. Formal informed consent of each patient was required.
Conflict of Interest
The authors declare no competing interests.
Footnotes
Key Points
• Decisional conflict can be lowered using decision-supporting tools, e.g., a decision aid.
• The decision aid significantly lowered the level of decisional conflict in patients.
• Additional use of the decision aid did not improve the level of shared decision-making.
• The added value of a decision aid should be further investigated.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.DATO Jaarrapportage 2017. Available from: https://dica.nl/jaarrapportage-2017/dato. Accessed 2 April 2022.
- 2.ASMBS. Estimate of bariatric surgery numbers, 2011–2017. Available from: https://asmbs.org/resources/estimate-of-bariatric-surgery-numbers. Accessed 30 Jan 2022.
- 3.Salminen P, Helmio M, Ovaska J, et al. Effect of laparoscopic sleeve gastrectomy vs laparoscopic Roux-en-Y gastric bypass on weight loss at 5 years among patients with morbid obesity: the SLEEVEPASS randomized clinical trial. Jama. 2018;319(3):241–54. doi: 10.1001/jama.2017.20313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peterli R, Wolnerhanssen BK, Peters T, et al. Effect of laparoscopic sleeve gastrectomy vs laparoscopic Roux-en-Y gastric bypass on weight loss in patients with morbid obesity: the SM-BOSS randomized clinical trial. JAMA. 2018;319(3):255–65. doi: 10.1001/jama.2017.20897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ettleson MD, Lager CJ, Kraftson AT, et al. Roux-en-Y gastric bypass versus sleeve gastrectomy: risks and benefits. Minerva Chir. 2017;72(6):505–19. doi: 10.23736/S0026-4733.17.07441-7. [DOI] [PubMed] [Google Scholar]
- 6.Wilkens SC, Ring D, Teunis T, et al. Decision aid for trapeziometacarpal arthritis: a randomized controlled trial. J Hand Surg Am. 2019;44(3):247.e1–247.e9. [DOI] [PubMed]
- 7.Korteland NM, Ahmed Y, Koolbergen DR, et al. Does the use of a decision aid improve decision making in prosthetic heart valve selection? A multicenter randomized trial. Circ Cardiovasc Qual Outcomes. 2017;10(2):e003178. [DOI] [PubMed]
- 8.Stacey D, Legare F, Lewis K, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2017;4:CD001431. [DOI] [PMC free article] [PubMed]
- 9.Knops AM, Legemate DA, Goossens A, et al. Decision aids for patients facing a surgical treatment decision: a systematic review and meta-analysis. Ann Surg. 2013;257(5):860–6. doi: 10.1097/SLA.0b013e3182864fd6. [DOI] [PubMed] [Google Scholar]
- 10.Sepucha K, Atlas SJ, Chang Y, et al. Patient decision aids improve decision quality and patient experience and reduce surgical rates in routine orthopaedic care: a prospective cohort study. J Bone Joint Surg Am. 2017;99(15):1253–60. doi: 10.2106/JBJS.16.01045. [DOI] [PubMed] [Google Scholar]
- 11.Nicholas Z, Butow P, Tesson S, et al. A systematic review of decision aids for patients making a decision about treatment for early breast cancer. Breast. 2016;26:31–45. doi: 10.1016/j.breast.2015.12.007. [DOI] [PubMed] [Google Scholar]
- 12.Schwartz MD, Valdimarsdottir HB, DeMarco TA, et al. Randomized trial of a decision aid for BRCA1/BRCA2 mutation carriers: impact on measures of decision making and satisfaction. Health Psychol. 2009;28(1):11–9. doi: 10.1037/a0013147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Knops AM, Goossens A, Ubbink DT, et al. A decision aid regarding treatment options for patients with an asymptomatic abdominal aortic aneurysm: a randomised clinical trial. Eur J Vasc Endovasc Surg. 2014;48(3):276–83. doi: 10.1016/j.ejvs.2014.04.016. [DOI] [PubMed] [Google Scholar]
- 14.Murray E, Davis H, Tai SS, et al. Randomised controlled trial of an interactive multimedia decision aid on benign prostatic hypertrophy in primary care. BMJ. 2001;323(7311):493–6. doi: 10.1136/bmj.323.7311.493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vlemmix F, Warendorf JK, Rosman AN, et al. Decision aids to improve informed decision-making in pregnancy care: a systematic review. BJOG. 2013;120(3):257–66. doi: 10.1111/1471-0528.12060. [DOI] [PubMed] [Google Scholar]
- 16.Waljee JF, Rogers MA, Alderman AK. Decision aids and breast cancer: do they influence choice for surgery and knowledge of treatment options? J Clin Oncol. 2007;25(9):1067–73. doi: 10.1200/JCO.2006.08.5472. [DOI] [PubMed] [Google Scholar]
- 17.Fried M, Yumuk V, Oppert JM, et al. Interdisciplinary European guidelines on metabolic and bariatric surgery. Obes Surg. 2014;24(1):42–55. doi: 10.1007/s11695-013-1079-8. [DOI] [PubMed] [Google Scholar]
- 18.Nijland LMG, Reiber BMM, Monpellier VM, et al. The association between patient attendance to a perioperative group-based lifestyle program and weight loss after bariatric surgery. Surg Obes Relat Dis. 2022;18(6):747–754. doi: 10.1016/j.soard.2022.02.011. [DOI] [PubMed] [Google Scholar]
- 19.O’Connor AM, Drake ER, Fiset V, et al. The Ottawa patient decision aids. Eff Clin Pract. 1999;2(4):163–70. [PubMed] [Google Scholar]
- 20.Elwyn G, O’Connor AM, Bennett C, et al. Assessing the quality of decision support technologies using the International Patient Decision Aid Standards instrument (IPDASi) PLoS One. 2009;4(3):e4705. doi: 10.1371/journal.pone.0004705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.O’Connor AM. Validation of a decisional conflict scale. Med Decis Making. 1995;15(1):25–30. doi: 10.1177/0272989X9501500105. [DOI] [PubMed] [Google Scholar]
- 22.Ottowa: Ottowa research Institute; 1993 [updated 2010]. 16 p. Available from: https://decisionaid.ohri.ca/docs/develop/User_Manuals/UM_decisional_conflict.pdf. Accessed 1 Dec 2021.
- 23.The BODY-Q™. Satisfaction with information. Memorial Sloan-Kettering Cancer Center 2013. Available from: https://qportfolio.org/body-q/. Accessed 10 April 2022
- 24.Rodenburg-Vandenbussche S, Pieterse AH, Kroonenberg PM, et al. Dutch translation and psychometric testing of the 9-item shared decision making questionnaire (sdm-q-9) and shared decision making questionnaire-physician version (SDM-Q-Doc) in primary and secondary care. PLoS One. 2015;10(7):e0132158. doi: 10.1371/journal.pone.0132158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Decisional Conflict Scale. Ottawa Hospital Research Institute. 2017. Available from: https://decisionaid.ohri.ca/eval_dcs.html. Accessed 2 May 2022.
- 26.Garvelink MM, Boland L, Klein K, et al. Decisional conflict scale findings among patients and surrogates making health decisions: part II of an anniversary review. Med Decis Making. 2019;39(4):315–26. doi: 10.1177/0272989X19851346. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data used in this research is accessible and available for reuse.