Abstract
Purpose of Review
The treatment options for high-risk non-muscle invasive bladder cancer (NMIBC), particularly following BCG, remain limited. We highlight recent, promising therapies for high-risk NMIBC.
Recent Findings
Several therapies utilizing different mechanisms of action have demonstrated favorable results in the BCG-naïve and BCG-unresponsive settings. These treatments include intravenous and intravesical immunotherapy, viral- and bacterial-based intravesical therapies, combination intravesical chemotherapy regimens, and novel intravesical chemotherapy administration. Overall, the efficacy and tolerability of emerging treatments for NMIBC appear promising and provide potential alternatives to radical cystectomy.
Summary
As the landscape of managing BCG-unresponsive disease evolves, clinical trials will explore future options and determine effective alternatives.
Keywords: Non-muscle invasive bladder cancer, Intravesical chemotherapy, Carcinoma in situ of the bladder, BCG-unresponsive
Introduction
Bladder cancer is the tenth most common cancer worldwide, with an incidence rate of almost half a million per year [1, 2]. In 2022, the estimated incidence of bladder cancer cases and deaths in the USA is 81,180 and 17,100 cases, respectively [3]. Non-muscle invasive bladder cancer (NMIBC), defined as cancer confined to the bladder mucosa and submucosa, constitutes 75% of bladder cancer cases. The most common histological subtype is urothelial carcinoma [1]. Non-muscle invasive bladder cancer includes papillary tumors within the mucosa (stage Ta), tumors invading the lamina propria (stage T1), and flat high-grade lesions referred to as carcinoma in situ (CIS) [4]. As opposed to muscle invasive cancer, NMIBC is primarily managed with local endoscopic/intravesical therapy and surveillance [5].
Non-muscle invasive bladder cancer’s progression risk to muscle invasion or recurrence risk varies according to tumor grade and depth. For instance, at one end of the spectrum, low-grade Ta bladder cancer recurs in almost two-thirds of cases, but seldom (only approx. 6%) progresses into a more invasive disease [6], whereas NMIBC with high-risk features, including high-grade T1, is reported to have a recurrence rate of almost 50%. Moreover, such cancers progress to invade the muscle in one of five patients, typically within 2 years of diagnosis [7, 8].
As a result of the heterogeneity seen in NMIBC, professional societies, including the American Urological Association and European Urologic Association, have adopted a risk-stratification system classifying NMIBC to either low-, intermediate-, or high-risk. As such, the tumors are stratified into risk groups that account for known risk factors of cancer progression and recurrence, including tumor stage, grade, size, focality, presence of CIS, lymphovascular invasion, recurrence rate, and response to intravesical treatments [4, 8–10].
The definitions of high-risk NMIBC according to American and European professional societies are shown in Table 1. Level one data has shown Bacillus Calmette-Guerin (BCG) to decrease the progression and recurrence of NMIBC; thus, intravesical instillation of BCG remains the cornerstone treatment for NMIBC following surgical resection or ablation of the tumor [4, 5, 11]. Different terms have been used to describe clinical scenarios where BCG is unsuccessful in the treatment of high-risk NMIBC and is no longer a treatment option, including BCG failure (where muscle invasive bladder cancer is detected), BCG-refractory (detection of high-risk lesions during or after adequate treatment at 3 or 6 months of treatment), and BCG-relapsing (detection of tumor following initial response after completion of treatment) [4]. However, the Federal Drug Administration (FDA) and in turn studies assessing novel treatments for NMIBC have defined BCG-unresponsive disease as seen in Table 2, facilitating study design and comparison [12].
Table 1.
Definitions of high-risk non-muscle-invasive bladder cancer according to the American and European Urologic Associations
| American Urological Association | European Urologic Association |
|---|---|
|
• Carcinoma in situ • High-grade T1 tumors • Recurrent or multifocal or large (> 3 cm) high-grade Ta tumors • Any tumor following BCG failure • Lymphovascular invasion or non-urothelial histology • High-grade tumor involving prostatic urethra |
• Carcinoma in situ • Any high-grade tumor • Any T1 tumor • Multiple, recurrent, and large low-grade Ta tumors |
|
Highest risk: • T1 HG with CIS • Multiple, large, or recurrent T1 high-grade tumors • T1 with CIS in prostatic urethra • Some variant histology or lymphovascular invasion |
Table 2.
Key definitions of BCG-unresponsive non-muscle invasive bladder cancer and adequate BCG treatment
| BCG-unresponsive non-muscle invasive bladder cancer |
|
• Persistent or recurrent CIS alone or with Ta/T1 disease within 12 months of adequate BCG therapy • Recurrent high-grade Ta/T1 disease within 6 months of completion of adequate BCG therapy • T1 high-grade disease on the first evaluation following an induction BCG course |
| Adequate BCG treatment |
|
• At least five of six doses of the initial induction course and at least two of three doses of the maintenance treatment • At least five of six doses of the initial induction course and at least two of six doses of the second induction course |
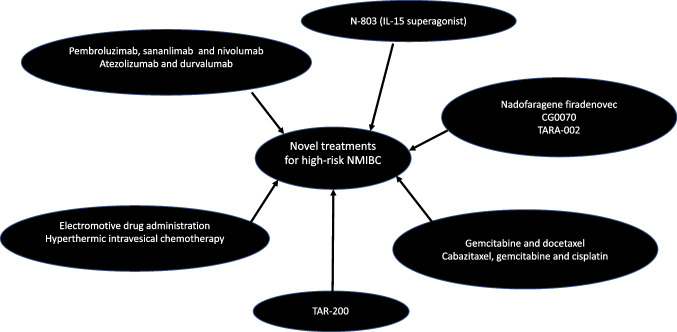
Current treatment options following unsuccessful BCG therapy are limited to radical cystectomy — the standard of care. In patients who are unfit or unwilling to undergo cystectomy, intravesical valrubicin and systemic pembrolizumab were the only two FDA-approved treatments for recurrent CIS as of 10/2022 [5]. Therefore, given the limited options in BCG-unresponsive disease, particularly considering the recent global BCG shortage, and high morbidity associated with radical cystectomy, there is an unmet need for novel treatments of high-risk NMIBC [13]. This review encompasses studies that are either published in peer-reviewed journals or presented at national meetings, and presents recent novel treatments and ongoing trials for high-risk NMIBC. We categorize treatments according to their main mechanism of action (Fig. 1).
Fig. 1.
Novel treatments for high-risk non-muscle invasive bladder cancer (NMIBC)
Immune Checkpoint Inhibitors (PD-1/PD-L1 Inhibitors)
Pembrolizumab
The blockage of programmed cell death receptor 1 (PD-1) or its ligand (PD-L1) is an efficient mechanism to maintain the function of effector T cells that play a pivotal role in anticancer treatment [14]. Stimulation of PD-1/PD-L1 pathway has been linked to tumor resistance following BCG therapy in NMIBC. Additionally, high PD-1 expression is independently associated with stage progression and recurrence after BCG therapy [15]. In early 2020, the FDA approved intravenous pembrolizumab (PD-1 inhibitor) for the treatment of BCG-unresponsive NMIBC with CIS (with or without papillary tumors) for patients who are unfit or unwilling to undergo radical cystectomy [16]. The approval was based on one of the two arms of a multicenter phase 2 study (KEYNOTE-057), which assessed the role of pembrolizumab in BCG-unresponsive NMIBC with CIS [17••]. The study included 101 patients that were followed for almost 3 years, of which 96 were included in their efficacy analysis. The authors reported 41% complete response at the first evaluable efficacy assessment, at 3 months, defined as the absence of high-risk disease or progressive disease. The median duration of a complete response was 16 months, and approximately 20% of patients that were assessed for efficacy had a sustained response lasting 1 year. The estimated progression-free survival to worsening stage, grade, or death was 83% at 12 months. Adverse events in this trial, and others mentioned in this review, are reported in accordance with the National Cancer Institute Common Terminology Criteria for Adverse Events. Here, two-thirds of patients reported an adverse event resultant from treatment, with 13% of patients having a grade 3 or 4 event.
Combination treatment of pembrolizumab with BCG is currently being assessed by KEYNOTE-676, where patients with persistent or recurrent high-risk disease after only one BCG induction course are enrolled to either receive pembrolizumab plus BCG or additional BCG monotherapy. The KEYNOTE-676 is expected to finish by the end of 2024 [18].
Intravesical administration of pembrolizumab was recently described in a phase 1 trial [19]. Meghani et al. administered pembrolizumab in conjunction with BCG in nine patients with BCG-unresponsive disease. The authors reported a 67% recurrence-free rate at 6 months and a total of 21 grade 1–2 adverse events among the nine patients who completed therapy, with the majority being urinary in nature. One patient expired due to myasthenia gravis that was potentially related to treatment. Of note, this study was closed to the COVID-19 pandemic.
Atezolizumab
Atezolizumab (PD-L1 inhibitor) is currently being evaluated in both BCG-naïve and BCG-unresponsive NMIBC. The SWOG S1605 assessed atezolizumab in BCG-unresponsive disease, with the primary endpoint being pathologic complete response at 6 months defined by mandatory biopsy. Patients with CIS were accrued with a null hypothesis of 30% complete response rate at 6 months. The authors reported a complete response rate of 41.1% and 27% in patients with CIS at 4 and 6 months, respectively. The event-free rate at 18 months for patients with (n = 74) and without CIS (n = 54 with cTa/T1) was 17% and 45%, respectively. In addition to two treatment-related deaths, grade 3–5 adverse events occurred in 17% [20].
A phase 3 French study, ALBAN (AFU-GETUG 37), began enrollment in 2018 and should be completed in 2028. This study randomizes BCG-naïve patients to either BCG alone or atezolizumab combined with BCG [21].
Sasanlimab
A multinational non-randomized phase 3 study is currently investigating the role of subcutaneous PD-1 inhibitor, sasanlimab, in high-risk NMIBC. The Combination of sasanlimab and alternative BCG Regimens to Evaluate outcomes with Subcutaneous anti-PD-1 Treatment (CREST) study will enroll patients with persistent or recurrent CIS within 12 months of completing BCG therapy, and in a separate arm patients with recurrent high-grade Ta/T1 disease within 6 months of completing adequate BCG therapy [22].
Durvalumab
Durvalumab (PD-L1 inhibitor) is currently being evaluated in a phase 3 trial (POTOMAC) in BCG-naïve patients randomized into three arms; durvalumab with BCG induction followed by BCG maintenance treatments for 2 years, durvalumab with BCG induction only, or BCG induction and maintenance therapy for 2 years [23]. This study is expected to enroll approximately 1000 patients with the primary endpoint being disease-free survival. In a different phase one study of BCG-unresponsive NMIBC, 12 patients received a combination of durvalumab and oportuzumab monatox — a fusion protein immunotoxin that binds to epithelial cell adhesion molecule (Ep-CAM)–positive tumor cells. In an interim analysis, the authors reported that 41%, 33%, and 17% were disease free at 3, 6, and 12 months following treatment, respectively. Of the treatment-related side effects, 8% were grade 3 or higher [24]. Of note, oportuzumab monatox has been studied separately in a phase 3 trial of 89 patients, who had a complete response of 40% at 3 months after instillation, of which 52% remained disease free at 1 year. The trial reported four treatment-related severe adverse events [25]. However, the FDA did not approve the Biologics License Application for oportuzumab monatox [26].
Nivolumab
Lastly, a phase 2 randomized study is accruing BCG-unresponsive patients to assess the safety of nivolumab (PD-1 inhibitor), ± linrodostat mesylate (an indoleamine 2,3-dioxygenase 1 [IOD1] inhibitor), or ± BCG. The investigators rationalize the use of linrodostat due to the potential immunosuppressive role of IDO in NMIBC [27]. The study includes high-risk NMBIC patients with CIS, with or without a papillary component that will be enrolled into one of four arms to either nivolumab monotherapy or a combination of aforementioned treatments [28].
N-803 (Interleukin-15 Receptor Alpha Complex-Fc Fusion Protein Superagonist)
N-803 is a interleukin-15 superagonist complex that was developed to improve the immune-mediated effects of interleukin-15, allowing for the activation and proliferation of natural killer and CD8 + T cells, and also avoiding regulatory T cell stimulation, thus boosting the immune response caused by BCG [29]. The Quilt 3.302 is multicenter phase 3 study of intravesical BCG mixed with N-803 given in standard induction and maintenance regimen to 160 patients with BCG-unresponsive NMIBC [30]. The authors recently reported on two cohorts: (1) those with CIS with or without papillary tumors (n = 83) and (2) patients with papillary tumors only (n = 77). The complete response rate in the CIS cohort was 71% with a median duration of 24 months, whereas in the papillary group, the disease-free rate was 57% and 48% at 1 and 2 years, respectively. In total, 91% and 95% of patients in the CIS and non-CIS cohorts avoided cystectomy, respectively. No treatment-related grades 4 or 5 were reported. Subsequent to these positive results, the FDA has accepted Biologics License Application, granting N-803 breakthrough therapy and fast track designation in combination with BCG for BCG-unresponsive CIS [31••].
Viral- and Bacterial-Based Therapy
Nadofaragene Firadenovec (rAd-IFNα/Syn3)
Interferon alfa-2b protein has been shown to be effective in NMIBC following BCG, but with limited durability likely due to short exposure time [32]. Intravesical interferon gene delivery has been developed to improve durability of interferon by increasing the duration of exposure. Nadofaragene firadenovec consists of two parts, a recombinant adenovirus vector-based gene therapy delivering a copy of the human interferon alfa-2b gene to urothelial cells, and polyamide surfactant that enhances the viral transduction of the urothelium. In a phase 3 single-arm multicenter study in the USA, Boorjan et al. include 157 patients with BCG-unresponsive NMIBC, who received at least one dose of intravesical nadofaragene firadenovec [33••]. Among patients with CIS (± high-grade Ta/T1 tumors), the complete response rate at 3 months was 53%. The median duration of complete response was 9.7 months, and almost half of the patients with an initial complete response remained free of high-grade disease at 1 year (n = 25), whereas in patients without CIS, 73% of patients were disease free at 3 months with a median duration of high-grade recurrence-free survival of 12.4 months. Of those without CIS who were high-grade disease free at 3 months, 60% continued to be free at 1 year. Progression to muscle invasive bladder cancer occurred in 5% and 6% of patients with and without CIS, respectively. In total, 70% of patients experienced adverse events that were drug-related. Grade 3 or 4 adverse events were seen in 18% of patients, but only 4% had events that were drug-related. Of note, the FDA approved nadofaragene firadenovec for high-risk BCG unresponsive NMIBC with CIS on December 16, 2022 [34].
CG0070
CG0070 is a modified adenovirus that expresses granulocyte–macrophage colony-stimulating factor (GM-CSF) in malignant bladder cells that have a deficient or mutated expression of the retinoblastoma tumor suppressor gene. As such, CG0070 induces cell lysis and augments the immunogenic response with the GM-CSF [35]. A phase 2 study of CG0070 reported a complete response rate of 50% at six months in patients with CIS, underscoring the possible role of CG0070 in high-risk disease [35]. In turn, the efficacy of intravesical CG00700 in BCG-unresponsive disease is currently being evaluated in a phase 3 single-arm study that includes 110 patients with CIS, with or without papillary tumors [36]. The treatments are planned to include weekly induction and maintenance intravesical instillations, with the primary endpoint being complete response assessed by cystoscopy, urine cytology, imaging, and mandatory bladder mapping biopsies at 12 months. Furthermore, CG0070 has been assessed in a phase 2 study for synergism with pembrolizumab in treating BCG-unresponsive disease [37]. Li et al. report a complete response rate of 87.5% at 3 months in 16 patients. The treatment-related adverse events in their study were limited to grade 1–2 genitourinary events with no grade 3–5 reported.
TARA-002
TARA-002 is a lyophilized mixture of low-virulence Streptococcus pyogenes cells that are treated with benzylpenicillin. It is manufactured using the same master cell bank as OK-432, a genetically distinct group A Streptococcus pyogenes, that has been in use since 1975 in Japan for the treatment of lymphangiomas [38] [39••]. TARA-002 is a broad immunopotentiator, that is hypothesized to activate both the innate and adaptive immune systems with tumor cells.
In a phase 1a/b study (dose escalation and expansion), the ADVANCED-1 study is currently open for enrollment to patients who are unable to obtain BCG or have received at least one dose of BCG or intravesical chemotherapy. The study will span 6 weeks of treatment with intravesical instillation of TARA-002 and 6 weeks of follow-up thereafter. The aim will be to determine the safety, tolerability, and preliminary efficacy of TARA-002 in patients with CIS or high-grade Ta. Of note, patients with a history of penicillin allergy are excluded from the study [40].
Intravesical Chemotherapy
Gemcitabine and Docetaxel
In a series of 45 patients with BCG-unresponsive disease, Steinberg et al. demonstrated that sequential intravesical gemcitabine and docetaxel can be used as a potential rescue treatment following BCG failure [41]. The authors reported that 66% of patients had successful treatment following chemotherapy at 3 months, 54% at 1 year, and a third at 2 years. Recent studies have assessed whether this regimen can be used as a first-line treatment option for high-risk patients in lieu of BCG. In a retrospective series by McElree et al., 107 patients with high-risk disease, including 44% with CIS, received gemcitabine for 90 min followed by docetaxel for 90–120 min as part of an induction once-a-week course for 6 weeks. Patients received once-a-month maintenance therapy if they were disease free at first surveillance [42]. The recurrence-free survival rate at 6 and 24 months was 89% and 82%, respectively, and was similar in patients with or without CIS. Whereas in a prospective series of eight BCG-naïve patients treated with gemcitabine and docetaxel with at least 3-month follow-up after induction treatment, all patients demonstrated complete response [43].
Cabazitaxel, Gemcitabine, and Cisplatin
The safety and toxicity of the multidrug platinum-based regimen consisting of cabazitaxel, gemcitabine, and cisplatin were explored in a phase 1 study of 18 patients with BCG-unresponsive disease [44]. The regimen was administered as a 6-week induction course followed by a maintenance course consisting of cabazitaxel and gemcitabine monthly for the first year and bimonthly for the second year. The induction regimen included 2–3 instillations every week, which as the authors acknowledge, is a challenging regimen, thus the investigators may in the future evaluate a less demanding treatment schedule (personal communication). Only patients with a complete or partial response (defined as negative cystoscopy with positive cytology) to the induction course proceeded to receive maintenance treatment. In this study, 67% of patients had a grade 1–2 adverse event, but none had a dose-limiting toxicity. The recurrence free survival rate was 83% and 64% at 1 and 2 years, respectively. Interestingly, in those who received the highest dose of cisplatin/cabazitaxel (10/18 patients), the 1- and 2-year recurrence-free rates were 100% and 83%, respectively. Of note, two of three patients with prostatic urethral involvement recurred in the same location, suggesting that involvement of disease in this location is unsuitable for such treatments.
Electromotive Drug Administration (EDMA)
The preface of electromotive drug administration (EDMA) is to improve the efficacy of intravesical treatments by improving penetration of the chemotherapeutic agent into the bladder wall using electrical current. In other words, water-soluble drugs are transported under the effect of an electric field overriding other determinates of drug delivery, such as pressure and concertation gradient, time of drug exposure, urinary output among others [45]. Based on a prior randomized control trial suggesting improved efficacy of sequential EDMA of mitomycin C and BCG in the treatment of BCG-naïve T1 disease [46], a single institution study recently assessed the role of this modality in 22 high-risk BCG-unresponsive patients and four others who had received an induction course of BCG [47]. The primary outcome of the study was progression-free survival, where progression included muscle invasive disease, metastasis or treating with chemotherapy or surgery. The investigators reported a progression-free survival of 58.3% and 48.9% at 1 and 2 years, respectively, whereas the recurrence-free rates were 41.9% and 27.2% at 1 and 2 years, respectively. The complete response rate was 44% at 1 year and 30.4% at 18 months. Of note, three of the 22 BCG-unresponsive patients died of bladder cancer. The authors report only three patients having experienced grade 3 adverse events, all for suspected bacteremia requiring hospitalization for intravenous antibiotic treatment. In a different study of EDMA in BCG-unresponsive disease, 60% of patients managed to retain their bladders avoiding cystectomy at year 3; however, three of 26 patients in that study had severe early allergic reactions to mitomycin C and underwent cystectomy [48]. Of note, EDMA is currently not available in the USA.
Hyperthermic Intravesical Chemotherapy
Hyperthermia is thought to increase the permeability of therapeutic drugs into the bladder urothelium, increase the toxicity of drugs against malignant cells, and hyperactivate the immune system [49]. In one reported hyperthermic intravesical chemotherapy regimen, mitomycin C is heated to almost 42 °C prior to being instilled into the bladder and then recirculated for 60 min. In a retrospective series of 56 patients with BCG-unresponsive disease who received at least five hyperthermic intravesical chemotherapy instillations, Pijpers et al. report a high-grade recurrence-free rate of 53% and 35% at 1 and 2 years, respectively following treatment [49]. The complete response rate in patients with CIS was 70% at 6 months, and only one patient in their study developed a serious adverse event (grade 3 — urinary tract infection). The adoption of this treatment modality has been limited, as more recent studies have stopped accrual for various reasons and currently there are no ongoing trials in the USA.
TAR-200
TAR-200 is an intravesical drug delivery system that releases gemcitabine in a controlled continuous manner via an indwelling placed device. Almost two-thirds of the drug load is delivered over 2 weeks as opposed to the standard 2-h dwell time [50]. The TAR-200 device is transferred using a catheter and is removed using a standard cystoscope following treatment. Currently, TAR-200 and cetrelimab (systemic intravenous PD-1 inhibitor) are being evaluated in a randomized multicenter phase 2b study in patients in BCG-unresponsive NMBIC. The primary outcome of the study is complete response following treatment with either TAR-200 with cetrelimab, TAR-200 alone, or cetrelimab alone [51]. Patients in the TAR-200 arms of the study will receive intravesical TAR-200 every 3 weeks through week 12, and every 12 weeks thereafter. The study opened in January of 2021 with almost 165 study sites worldwide.
Conclusions
The BCG shortage has underscored the need for treatment alternatives for a wide range of high-risk tumors in which BCG plays a pivotal role. While radical cystectomy is the standard of care for patients with BCG-unresponsive cancer, it is a morbid and life-altering procedure [5]. Efforts by urologic societies led to FDA acceptance of single-arm trials to spur drug development for BCG-unresponsive disease. The FDA has approved pembrolizumab with a complete response rate of 40% at three months, and in this review, we highlighted some of the novel treatments that have the potential to meet FDA approval including atezolizumab, oportuzamab, and N-803 [30, 52].
As we witness new developing treatments for bladder cancer patients, we must remain conscientious of cost-effectiveness and safety. For instance, clinicians must weigh the complete response rate of 20% at 12 months against the associated economic burden of pembrolizumab and potential harmful delay of surgery compared to timely surgery [17••, 53]. Moreover, while clinicians attempt to define disease states and clinical trial design, the current lack in randomized trials may hamper direct comparisons of these novel treatments [54]. Nonetheless, in our practice where we encounter BCG-unresponsive disease not too infrequently in patients who are either unfit, or even more so, unwilling to lose their bladders, we fully support and encourage enrollment in clinical trials. We believe that the key to advancing the quality of care for bladder cancer patients lies within clinical trial participation, which forms the cornerstone for future NMIBC treatment.
Declarations
Human and Animal Rights and Informed Consent
This article does not contain any studies with human without informed consent or animal subjects performed by any of the authors.
Conflict of Interest
ICMJE disclosure forms are provided. SSC has consulted for the following: Urogen, Merck, Janssen, Pfizer, and ImmunityBio. Vanderbilt University Medical Center is a trial site for TAR-200.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Bashir Al Hussein Al Awamlh, Email: Bashir.alhussein@vumc.org.
Sam S. Chang, Email: Sam.chang@vumc.org
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Cumberbatch MGK, Jubber I, Black PC, Esperto F, Figueroa JD, Kamat AM, et al. Epidemiology of bladder cancer: a systematic review and contemporary update of risk factors in 2018. Eur Urol. 2018;74(6):784–795. doi: 10.1016/j.eururo.2018.09.001. [DOI] [PubMed] [Google Scholar]
- 2.Bladder cancer statistics. 2020. https://www.wcrf.org/cancer-trends/bladder-cancer-statistics. Accessed 22 Aug 2022.
- 3.Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72(1):7–33. doi: 10.3322/caac.21708. [DOI] [PubMed] [Google Scholar]
- 4.Babjuk M, Burger M, Comperat EM, Gontero P, Mostafid AH, Palou J, et al. European Association of Urology Guidelines on non-muscle-invasive bladder cancer (TaT1 and carcinoma in situ) - 2019 Update. Eur Urol. 2019;76(5):639–657. doi: 10.1016/j.eururo.2019.08.016. [DOI] [PubMed] [Google Scholar]
- 5.Chang SS, Boorjian SA, Chou R, Clark PE, Daneshmand S, Konety BR, et al. Diagnosis and treatment of non-muscle invasive bladder cancer: AUA/SUO guideline. J Urol. 2016;196(4):1021–1029. doi: 10.1016/j.juro.2016.06.049. [DOI] [PubMed] [Google Scholar]
- 6.Leblanc B, Duclos AJ, Benard F, Cote J, Valiquette L, Paquin JM, et al. Long-term followup of initial Ta grade 1 transitional cell carcinoma of the bladder. J Urol. 1999;162(6):1946–1950. doi: 10.1016/s0022-5347(05)68075-5. [DOI] [PubMed] [Google Scholar]
- 7.Palou J, Sylvester RJ, Faba OR, Parada R, Pena JA, Algaba F, et al. Female gender and carcinoma in situ in the prostatic urethra are prognostic factors for recurrence, progression, and disease-specific mortality in T1G3 bladder cancer patients treated with bacillus Calmette-Guerin. Eur Urol. 2012;62(1):118–125. doi: 10.1016/j.eururo.2011.10.029. [DOI] [PubMed] [Google Scholar]
- 8.van den Bosch S, Alfred WJ. Long-term cancer-specific survival in patients with high-risk, non-muscle-invasive bladder cancer and tumour progression: a systematic review. Eur Urol. 2011;60(3):493–500. doi: 10.1016/j.eururo.2011.05.045. [DOI] [PubMed] [Google Scholar]
- 9.Fernandez-Gomez J, Madero R, Solsona E, Unda M, Martinez-Pineiro L, Gonzalez M, et al. Predicting nonmuscle invasive bladder cancer recurrence and progression in patients treated with Bacillus Calmette-Guerin: the CUETO scoring model. J Urol. 2009;182(5):2195–2203. doi: 10.1016/j.juro.2009.07.016. [DOI] [PubMed] [Google Scholar]
- 10.Sylvester RJ, van der Meijden AP, Oosterlinck W, Witjes JA, Bouffioux C, Denis L, et al. Predicting recurrence and progression in individual patients with stage Ta T1 bladder cancer using EORTC risk tables: a combined analysis of 2596 patients from seven EORTC trials. Eur Urol. 2006;49(3):466–5. doi: 10.1016/j.eururo.2005.12.031. [DOI] [PubMed] [Google Scholar]
- 11.Shelley MD, Kynaston H, Court J, Wilt TJ, Coles B, Burgon K, et al. A systematic review of intravesical bacillus Calmette-Guerin plus transurethral resection vs transurethral resection alone in Ta and T1 bladder cancer. BJU Int. 2001;88(3):209–216. doi: 10.1046/j.1464-410x.2001.02306.x. [DOI] [PubMed] [Google Scholar]
- 12.Bacillus Calmette-Guérin-unresponsive nonmuscle invasive bladder cancer: developing drugs and biologics for treatment guidance for industry. 2018. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/bacillus-calmette-guerin-unresponsive-nonmuscle-invasive-bladder-cancer-developing-drugs-and. Accessed 22 Aug 2022.
- 13.Important message about the BCG shortage. 2020. https://www.auanet.org/about-us/bcg-shortage-info. Accessed 22 Aug 2022.
- 14.Alsaab HO, Sau S, Alzhrani R, Tatiparti K, Bhise K, Kashaw SK, et al. PD-1 and PD-L1 checkpoint signaling inhibition for cancer immunotherapy: mechanism, combinations, and clinical outcome. Front Pharmacol. 2017;8:561. doi: 10.3389/fphar.2017.00561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fukumoto K, Kikuchi E, Mikami S, Hayakawa N, Matsumoto K, Niwa N, et al. Clinical role of programmed cell death-1 expression in patients with non-muscle-invasive bladder cancer recurring after initial Bacillus Calmette-Guerin therapy. Ann Surg Oncol. 2018;25(8):2484–2491. doi: 10.1245/s10434-018-6498-2. [DOI] [PubMed] [Google Scholar]
- 16.FDA approves pembrolizumab for BCG-unresponsive, high-risk non-muscle invasive bladder cancer. 2020. https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-pembrolizumab-bcg-unresponsive-highrisk-non-muscle-invasive-bladder-cancer. Accessed 20 Aug 2022.
- 17.••.Balar AV, Kamat AM, Kulkarni GS, Uchio EM, Boormans JL, Roumiguie M, et al. Pembrolizumab monotherapy for the treatment of high-risk non-muscle-invasive bladder cancer unresponsive to BCG (KEYNOTE-057): an open-label, single-arm, multicentre, phase 2 study. Lancet Oncol. 2021;22(7):919–930. doi: 10.1016/S1470-2045(21)00147-9. [DOI] [PubMed] [Google Scholar]
- 18.Kamat AM, Shore N, Hahn N, Alanee S, Nishiyama H, Shariat S, et al. KEYNOTE-676: phase III study of BCG and pembrolizumab for persistent/recurrent high-risk NMIBC. Future Oncol. 2020;16(10):507–516. doi: 10.2217/fon-2019-0817. [DOI] [PubMed] [Google Scholar]
- 19.Meghani K, Cooley LF, Choy B, Kocherginsky M, Swaminathan S, Munir SS, et al. First-in-human intravesical delivery of pembrolizumab identifies immune activation in bladder cancer unresponsive to Bacillus Calmette-Guerin. Eur Urol. 2022 doi: 10.1016/j.eururo.2022.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Black PC, Tangen C, Singh P, McConkey DJ, Lucia S, William TL, et al. Phase II trial of atezolizumab in BCG-unresponsive non-muscle invasive bladder cancer: SWOG S1605 (NCT #02844816). ASCO2021. J Clin Oncol. 2021;39(15):4541–4541. doi: 10.1200/JCO.2021.39.15_suppl.4541. [DOI] [Google Scholar]
- 21.Roupret M, Neuzillet Y, Bertaut A, Pignot G, Houede N, Champiat S, et al. ALBAN: an open label, randomized, phase III trial, evaluating efficacy of atezolizumab in addition to one year BCG (bacillus Calmette-Guerin) bladder instillation in BCG-naive patients with high-risk nonmuscle invasive bladder cancer (AFU-GETUG 37). J Clin Oncol. 2019;37(15). 10.1200/JCO.2019.37.15_suppl.TPS4589.
- 22.Shore ND, Powles T, Bedke J, Galsky MD, Kopyltsov E, Necchi A, et al. A phase 3 study of the subcutaneous programmed cell death protein 1 inhibitor sasanlimab as single agent for patients with bacillus Calmette-Guérin, unresponsive high-risk, non-muscle invasive bladder cancer: CREST Study Cohort B. ASCO Annual Meeting. J Clin Oncol. 2022;40(16) TPS4614–TPS4614. 10.1200/JCO.2022.40.16_suppl.TPS4614.
- 23.Santis MD, Abdrashitov R, Hegele A, Kolb M, Parker S, Redorta JP, et al. A phase III, randomized, open-label, multicenter, global study of durvalumab and Bacillus Calmette-Guérin (BCG) versus BCG alone in high-risk, BCG-naïve non-muscle-invasive bladder cancer (NMIBC) patients (POTOMAC). ASCO Genitourinary Cancers Symposium2019. J Clin Oncol. 2019;37(7). 10.1200/JCO.2019.37.7_suppl.TPS500.
- 24.Gurram S, Bellfield S, Dolan R, Walter B, Merino M, Niglio S, Bethesda AA, Agarwal P, Valera V. Interim analysis of a phase I single-arm study of the combination of durvalumab (Medi4736) and vicinium (Oportuzumab Monatox, Vb4-845) in subjects with high-grade non-muscle-invasive bladder cancer previously treated with Bacillus Calmette-Guerin (Bcg) (NCT03258593). 2021;206(Supplement 3):e120–e120. 10.1097/JU.0000000000001977.04.
- 25.Shore N, O’Donnell M, Keane T, Jewett MAS, Kulkarni GS, Dickstein R, et al. Phase 3 results of vicinium in BCG-unresponsive non-muscle invasive bladder cancer. AUA2020. 10.1097/JU.0000000000000823.02.
- 26.Sesen Bio receives complete response letter from FDA for Vicineum™ (oportuzumab monatox-qqrs). 2021. https://ir.sesenbio.com/news-releases/news-release-details/sesen-bio-receives-complete-response-letter-fda-vicineumtm. Accessed 9/1/2022.
- 27.Hudolin T, Mengus C, Coulot J, Kastelan Z, El-Saleh A, Spagnoli GC. Expression of indoleamine 2,3-dioxygenase gene is a feature of poorly differentiated non-muscle-invasive urothelial cell bladder carcinomas. Anticancer Res. 2017;37(3):1375–1380. doi: 10.21873/anticanres.11458. [DOI] [PubMed] [Google Scholar]
- 28.Hahn NM, Chang S, Meng M, Shore ND, Konety BR, Steinberg GD, et al. A phase II, randomized study of nivolumab (NIVO), NIVO plus linrodostat mesylate, or NIVO plus intravesical bacillus Calmette-Guerin (BCG) in BCG-unresponsive, high-risk, nonmuscle invasive bladder cancer (NMIBC): CheckMate 9UT. ASCO2020. J Clin Oncol 2020;38(15). 10.1200/JCO.2020.38.15_suppl.TPS5090.
- 29.Knudson KM, Hodge JW, Schlom J, Gameiro SR. Rationale for IL-15 superagonists in cancer immunotherapy. Expert Opin Biol Ther. 2020;20(7):705–709. doi: 10.1080/14712598.2020.1738379. [DOI] [PubMed] [Google Scholar]
- 30.Chamie K, Chang SS, Gonzalgo M, Kramolowsky EV, Sexton WJ, Bhar P, et al. Final clinical results of pivotal trial of IL-15RαFc superagonist N-803 with BCG in BCG-unresponsive CIS and papillary nonmuscle-invasive bladder cancer (NMIBC). ASCO2022. J Clin Oncol. 2022;40(6):4508–4508. doi: 10.1200/JCO.2022.40.16_suppl.4508. [DOI] [Google Scholar]
- 31.••.ImmunityBio Announces FDA Acceptance of biologics license application for N-803 in BCG-unresponsive non-muscle-invasive bladder cancer carcinoma in situ. N-803 study showing a complete response rate of 71% with a median duration of 24 months for CIS patients. https://immunitybio.com/immunitybio-announces-fda-acceptance-of-biologics-license-application-for-n-803-in-bcg-unresponsive-non-muscle-invasive-bladder-cancer-carcinoma-in-situ/2022. Accessed 24 Aug 2022.
- 32.O’Donnell MA, Lilli K, Leopold C, National Bacillus Calmette-Guerin/interferon phase 2 investigator G Interim results from a national multicenter phase II trial of combination bacillus Calmette-Guerin plus interferon alfa-2b for superficial bladder cancer. J Urol. 2004;172(3):888–93. doi: 10.1097/01.ju.0000136446.37840.0a. [DOI] [PubMed] [Google Scholar]
- 33.••.Boorjian SA, Alemozaffar M, Konety BR, Shore ND, Gomella LG, Kamat AM, et al. Intravesical nadofaragene firadenovec gene therapy for BCG-unresponsive non-muscle-invasive bladder cancer: a single-arm, open-label, repeat-dose clinical trial. Lancet Oncol. 2021;22(1):107–117. doi: 10.1016/S1470-2045(20)30540-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.FDA approves first adenoviral vector-based gene therapy for high-risk Bacillus Calmette-Guérin unresponsive non-muscle invasive bladder cancer. 2022. https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-first-adenoviral-vector-based-gene-therapy-high-risk-bacillus-calmette-guerin. Accessed 21 Dec 2022.
- 35.Packiam VT, Lamm DL, Barocas DA, Trainer A, Fand B, Davis RL, 3rd, et al. An open label, single-arm, phase II multicenter study of the safety and efficacy of CG0070 oncolytic vector regimen in patients with BCG-unresponsive non-muscle-invasive bladder cancer: Interim results. Urol Oncol. 2018;36(10):440–447. doi: 10.1016/j.urolonc.2017.07.005. [DOI] [PubMed] [Google Scholar]
- 36.Uchio EM, Lamm DL, Shore ND, Kamat AM, Tyson M, Tran B, et al. A phase 3, single-arm study of CG0070 in subjects with nonmuscle invasive bladder cancer (NMIBC) unresponsive to Bacillus Calmette-Guerin (BCG). ASCO Genitourinary Cancers Symposium2022. J Clin Oncol. 2022;40(6). 10.1200/JCO.2022.40.6_suppl.TPS598.
- 37.Li Roger, Steinberg Gary D, Uchio Edward M, Lamm Donald L, Shah Paras, Kamat Ashish M, et al. CORE1: Phase 2, single-arm study of CG0070 combined with pembrolizumab in patients with nonmuscle-invasive bladder cancer (NMIBC) unresponsive to bacillus Calmette-Guerin (BCG) ASCO2022. J Clin Oncol. 2022;40(16):4597–4597. doi: 10.1200/JCO.2022.40.16_suppl.4597. [DOI] [Google Scholar]
- 38.Giguere CM, Bauman NM, Sato Y, Burke DK, Greinwald JH, Pransky S, et al. Treatment of lymphangiomas with OK-432 (Picibanil) sclerotherapy: a prospective multi-institutional trial. Arch Otolaryngol Head Neck Surg. 2002;128(10):1137–1144. doi: 10.1001/archotol.128.10.1137. [DOI] [PubMed] [Google Scholar]
- 39.••.Ryoma Y, Moriya Y, Okamoto M, Kanaya I, Saito M, Sato M. Biological effect of OK-432 (picibanil) and possible application to dendritic cell therapy. Anticancer Res. 2004;24(5C):3295–3301. [PubMed] [Google Scholar]
- 40.Bandari JJZ, Belani K, Brown E, Metcalf M, Nanayakkara N. Phase 1a/b safety study of intravesical instillation of TARA-002 in adults with high-grade non-muscle invasive bladder cancer (ADVANCED-1). ASCO2022. J Clin Oncol. 2022;40(6): TPS4620-TPS4620. 10.1200/JCO.2022.40.16_suppl.TPS4620.
- 41.Steinberg RL, Thomas LJ, O’Donnell MA, Nepple KG. Sequential intravesical gemcitabine and docetaxel for the salvage treatment of non-muscle invasive Bladder Cancer. Bladder Cancer. 2015;1(1):65–72. doi: 10.3233/BLC-150008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.McElree IM, Steinberg RL, Martin AC, Richards J, Mott SL, Gellhaus PT, et al. Sequential intravesical gemcitabine and docetaxel for Bacillus Calmette-Guerin-naive high-risk nonmuscle-invasive bladder cancer. J Urol. 2022;208(3):589–599. doi: 10.1097/JU.0000000000002740. [DOI] [PubMed] [Google Scholar]
- 43.Patel S, Collins C, Singla N, Gabrielson A, Bivalacqua TJ, Hahn N, et al. Intravesical gemcitabine and docetaxel (Gemdoce) in the treatment of BCG naïve non-muscle invasive urothelial carcinoma of the bladder: updates from a phase 2 trial. AUA2022. 10.1097/JU.0000000000002642.15. [DOI] [PubMed]
- 44.DeCastro GJ, Sui W, Pak JS, Lee SM, Holder D, Kates MM, et al. A phase I trial of intravesical cabazitaxel, gemcitabine and cisplatin for the treatment of nonmuscle invasive bacillus Calmette-Guerin unresponsive or recurrent/relapsing urothelial carcinoma of the bladder. J Urol. 2020;204(2):247–253. doi: 10.1097/JU.0000000000000919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Giannantoni A, Di Stasi SM, Chancellor MB, Costantini E, Porena M. New frontiers in intravesical therapies and drug delivery. Eur Urol. 2006;50(6):1183–93. doi: 10.1016/j.eururo.2006.08.025. [DOI] [PubMed] [Google Scholar]
- 46.Di Stasi SM, Giannantoni A, Giurioli A, Valenti M, Zampa G, Storti L, et al. Sequential BCG and electromotive mitomycin versus BCG alone for high-risk superficial bladder cancer: a randomised controlled trial. Lancet Oncol. 2006;7(1):43–51. doi: 10.1016/S1470-2045(05)70472-1. [DOI] [PubMed] [Google Scholar]
- 47.Juvet T, Mari A, Lajkosz K, Wallis CJ, Kuk C, Erlich A, et al. Sequential administration of Bacillus Calmette-Guerin (BCG) and electromotive drug administration (EMDA) of mitomycin C (MMC) for the treatment of high-grade nonmuscle invasive bladder cancer after BCG failure. Urol Oncol. 2020;38(11):850 e9- e15. 10.1016/j.urolonc.2020.06.031. [DOI] [PubMed]
- 48.Racioppi M, Di Gianfrancesco L, Ragonese M, Palermo G, Sacco E, Bassi PF. Electromotive drug administration (EMDA) of mitomycin C as first-line salvage therapy in high risk “BCG failure” non muscle invasive bladder cancer: 3 years follow-up outcomes. BMC Cancer. 2018;18(1):1224. doi: 10.1186/s12885-018-5134-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Pijpers OM, Hendricksen K, Mostafid H, de Jong FC, Rosier M, Mayor N, et al. Long-term efficacy of hyperthermic intravesical chemotherapy for BCG-unresponsive non-muscle invasive bladder cancer. Urol Oncol. 2022;40(2):62 e13–62 e20. 10.1016/j.urolonc.2021.07.019. [DOI] [PubMed]
- 50.Grimberg DC, Shah A, Inman BA. Overview of Taris GemRIS, a novel drug delivery system for bladder cancer. Eur Urol Focus. 2020;6(4):620–622. doi: 10.1016/j.euf.2019.09.006. [DOI] [PubMed] [Google Scholar]
- 51.Heijden MSVD, Cutie ,Hampras CS, Stewart ICR, Acharya M, et al. SunRISe-1: phase 2b study of TAR-200 plus cetrelimab, TAR-200 alone, or cetrelimab alone in participants with high-risk nonmuscle-invasive bladder cancer unresponsive to Bacillus Calmette-Guérin who are ineligible for or decline radical cystectomy. ASCO Genitourinary Cancers Symposium2022. J Clin Oncol. 2022;40(6). 10.1200/JCO.2022.40.6_suppl.TPS593.
- 52.Peter C. Black, Tangen C, Singh P, McConkey DJ, Lucia S, Lowrance WT, et al. Phase II trial of atezolizumab in BCG-unresponsive non-muscle invasive bladder cancer: SWOG S1605 (NCT #02844816). J Clin Oncol. 2020;38; 5022–5022. 10.1200/JCO.2020.38.15_suppl.5022.
- 53.Gill J, Prasad V. Pembrolizumab for non-muscle-invasive bladder cancer-a costly therapy in search of evidence. JAMA Oncol. 2021;7(4):501–502. doi: 10.1001/jamaoncol.2020.6142. [DOI] [PubMed] [Google Scholar]
- 54.Roumiguie M, Kamat AM, Bivalacqua TJ, Lerner SP, Kassouf W, Bohle A, et al. International Bladder Cancer Group Consensus statement on clinical trial design for patients with Bacillus Calmette-Guerin-exposed high-risk non-muscle-invasive bladder cancer. Eur Urol. 2022;82(1):34–46. doi: 10.1016/j.eururo.2021.12.005. [DOI] [PubMed] [Google Scholar]