Abstract
Purpose
A paucity of data exists on the treatment of pediatric lateral meniscus root tears (LMPRTs). This study aims to characterize the biomechanics of the lateral knee joint in pediatric cadavers following LMPRT and root repair. Our hypotheses were: (1) compared with the intact state, LMPRT would be associated with decreased contact area; (2) compared with the intact state, LMPRT would be associated with increased contact pressures; and (3) compared with LMPRT, root repair would restore contact area and pressures toward intact meniscus values.
Methods
Eight cadaver knees (ages 8-12 years) underwent contact area and pressure testing of the lateral compartment. Tekscan pressure mapping sensors covering the tibial plateau were inserted underneath the lateral meniscus. Appropriate pressure load equivalents were applied by a robot at degrees of flexion: 0, 30, 60. Three meniscus conditions were tested: (1) intact, (2) complete root tear, and (3) repaired root tear. Root repairs were performed with transtibial pullout sutures. Statistical analysis was performed.
Results
Root tear significantly decreased mean contact area at 30° (P = .0279) and 60° (P = .0397). Root repair increased mean contact area and did not significantly differ from intact states. Differences in contact pressures between meniscus states were not statistically significant. Relative to the intact state. the greatest increase in contact pressures occurred between 0° and 30°. Root repair decreased mean contact pressures at 0° and 30°. At 60°, mean contact pressures of the repair state were closer in magnitude to the tear state than the intact state. Conclusions: LMPRT decreases contact area and increases contact pressures in the lateral knee compartment. Repair of LMPRT improves tibiofemoral contact area at high (>30°) degrees of flexion and contact pressures at low (<30°) degrees of flexion.
Clinical Relevance
Transosseous pullout repair is a clinically validated treatment for LMPRT. This study provides baseline biomechanics data of transtibial pullout repair of pediatric LMPRTs.
Lateral meniscus posterior root tears (LMPRTs) are common in young athletes and are associated with anterior cruciate ligament (ACL) tears.1,2 Pivot–shift testing in ACL-deficient adult knees shows that the lateral meniscus posterior root supports the ACL by functioning as a secondary stabilizer of the knee to anterior–posterior tibial translation and internal rotation.3 With increasing rotation, the lateral meniscus posterior root becomes the primary stabilizer of internal rotation and LMPRTs can destabilize the knee joint in setting of an intact ACL.3,4 Meniscal root tears disrupt collagen fiber attachments to the tibial plateau and reduce hoop strength, diminishing meniscal capacity to withstand axial loads.5 In adults, altered tibiofemoral joint stability manifests as decreased contact area and increased contact pressures in the lateral knee compartment and is partially restored towards the native intact state with repair.6,7 While the biomechanics of LMPRTs and LMPRT repair in pediatric patients are hypothesized as similar to adults, published research is limited.
The purpose of this study was to characterize the biomechanics of the lateral knee joint in pediatric patients following LMPRT and subsequent root repair using transtibial pullout sutures. Our hypotheses were: (1) compared with the intact state, root tears would be associated with decreased contact area, (2) compared with the intact state, root tears would be associated with increased average and peak contact pressures, and (3) compared with the root tear state, root repair would partially restore contact area and contact pressures towards intact meniscus values.
Methods
This study used donated cadaveric tissues without patient identifiers, and donor families gave permission to use the tissue for research purposes. Due to these circumstances, this study was exempt from institutional review board review.
Specimen and Preparation
Eight intact fresh-frozen cadaver knees (5 right and 3 left) aged 8 to 12 years were obtained from AlloSource. One pair of knees was matched from the same cadaver, an 11-year-old female; all other knees were from distinct male donors. Each specimen was examined manually to ensure intact menisci and cruciate ligaments, as well as absence of anatomical abnormalities such as joint contracture and meniscal injuries. Specimen were stored in –20°C freezers and thawed at room temperature the day preceding dissection. Skin, subcutaneous tissue, muscle, and tendons were excised from the knee to enable specimen fixation for biomechanical testing, as well as access to posterior aspects of the lateral knee capsule. Knee joint stability was preserved with preservation of the meniscal ligaments, coronary ligaments, cruciate ligaments, and collateral ligaments. Lateral stability of the knee joint was preserved with retention of popliteus and iliotibial band. The medial meniscus was also left intact. Then, 1-cm incisions were created in the anterolateral and posterolateral knee capsules superior to the tibial plateau to enable insertion of rectangular pressure-mapping Tekscan sensors (I-Scan Pressure Measurement System Model 4000, Tekscan Inc., Norwood, MA). Inspection through these slits confirmed that no accidental damage was done to the meniscus or cruciate ligaments. The remaining knee capsule was left intact.
The distal end of the femur and proximal end of the tibia were potted in PMMA cement (COE Tray Plastic, GC America Inc., Alsip, IL) for stability during biomechanical analysis. Three wood screws were drilled into the proximal femur and distal tibial shafts to increase the surface area that the molds could encase. The screw improved grip on the specimen ends and did not affect knee joint biomechanics. Potted ends of the femur and tibia were secured to the robot end-effector and pedestal base with custom-made aluminum clamps.
A sagittal plane lateral osteotomy was performed with a bone saw to allow unobstructed visualization of the interior lateral knee compartment for precise root tear and repair, as well as ensuring sensor coverage of the lateral tibial plateau before each test. Care was taken to retain attachments from the posterior cruciate ligament to the lateral border of the intercondylar notch, as well as anterior cruciate ligament, lateral meniscus, and peripheral joint capsule. Before the osteotomy, 2 tunnels were drilled through the epicondylar axis of the femur from the lateral epicondyle to the medial epicondyle using a 2.5-mm Kirschner guidewire. Threaded bolts were used in conjunction with nuts to hold the osteotomy anatomically aligned for the complete duration of biomechanical testing.
Biomechanical Testing
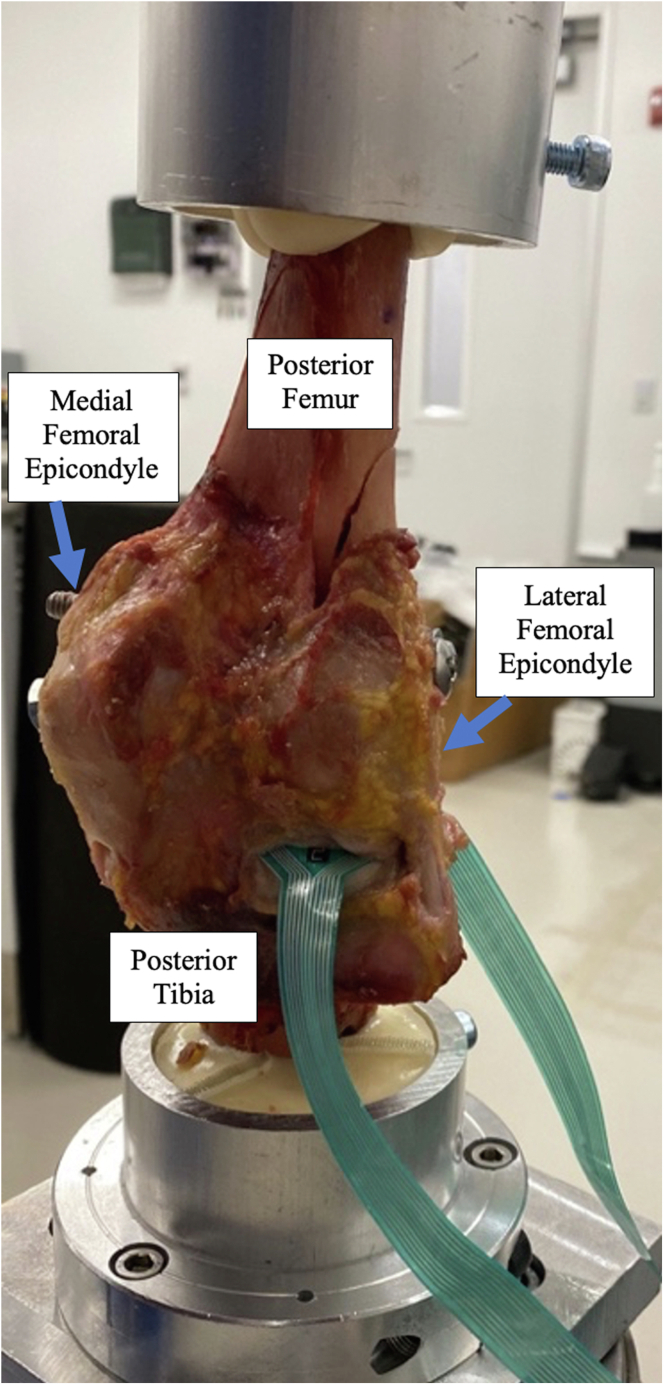
The potted knee was mounted onto a 6-degrees-of-freedom robotic testing system (Kuka KRC4; KUKA, Augsburg, Germany) and controlled using simVITRO biomechanics control software (simVITRO, Cleveland Clinic, Cleveland, OH) to ensure precise compressive loading and tibiofemoral joint flexion at 0, 30, and 60°. Testing setup is shown in Fig 1. In addition to automated flexion to the predetermined angle, the robot-applied compressive loads on the joint directed down onto the tibial plateau. Varus–valgus alignment was controlled manually to ensure consistent and balance load applied on the tibial plateau (Fig 1).
Fig 1.
Coronal view of the posterior tibia and femur at 0° of knee flexion. The specimen was secured to a six-degrees-of-freedom robot for biomechanical testing. Pressure sensors were inserted through incisions in the anterolateral and posterolateral knee capsules superior to the tibial plateau.
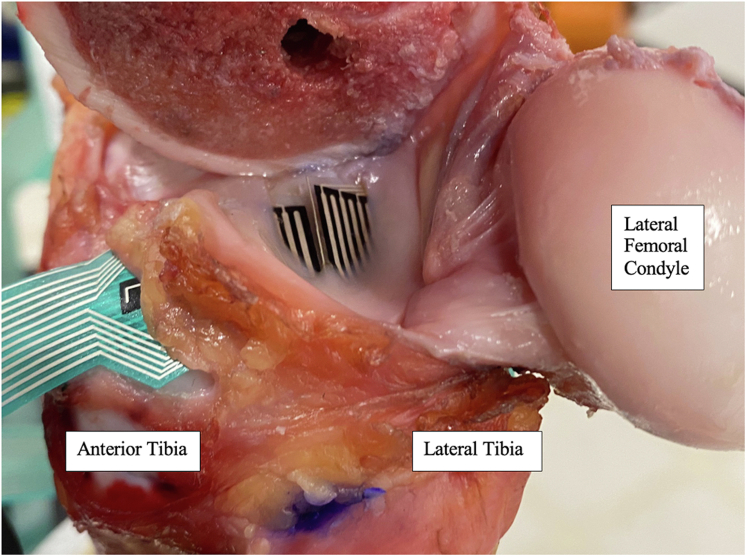
With the osteotomy removed, Tekscan pressure sensors were inserted underneath the lateral meniscus through anterolateral and posterolateral knee compartments incisions. Sensors were aligned to touch tip-to-tip to ensure maximal coverage of the lateral tibial plateau (Fig 2). Sensors were repositioned at each angle of flexion for uniform positioning. The osteotomy was then replaced before testing. Compressive loads representing 100% of the cadaver’s body weight were introduced by the robot at each angle of joint flexion. Tibiofemoral joint variables measured were contact area, peak pressure, and average pressure. A new pressure sensor was used for each specimen to maximize accuracy of readings. Sensors were equilibrated, calibrated, and conditioned according to manufacturer’s recommendations (Fig 2).
Fig 2.
Sagittal view of the lateral knee compartment with the lateral femoral osteotomy removed. Calibrated pressure sensors were inserted underneath the lateral meniscus. The femoral osteotomy was screwed taut prior to each test.
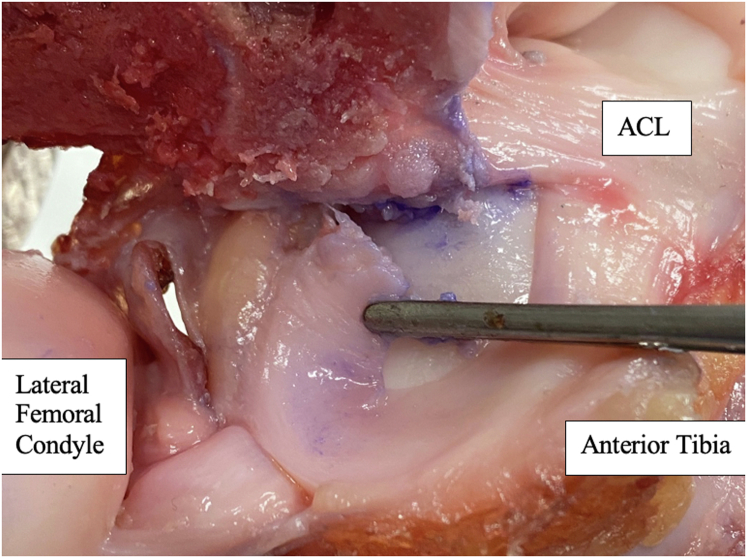
Root Tear
Following testing of the intact state, complete root tears were created at the attachment site of the posterolateral meniscus root to the intercondylar region of the tibial plateau. Meniscofemoral ligaments were preserved if present. Prior to creation of the root tear, the lateral meniscus root attachment site was marked to guide subsequent repair, then biomechanical testing was repeated. Root tear is shown in Fig 3.
Fig 3.
Transverse view of the tibial plateau. Complete root tears were created at the attachment site of the posterolateral meniscus root to the intercondylar region of the tibial plateau.
Root Repair
The transosseous pull-out suture technique was used to repair the posterolateral root tear. Guided by the ACUFEX DIRECTOR drill guide (Smith & Nephew, Andover, MA) and a 2.4-mm guide pin, a 4.5-mm tunnel was drilled through the tibia from the anterolateral tibial surface to the previously marked center of the posterolateral meniscal attachment. The guide angle was between 55 and 65° and selected for each specimen individually for anatomical root alignment. The posterior meniscus root was secured with a whipstitch using #2 nonabsorbable suture (ULTRABRAID, Co-Braid Suture, and Needle Assembly, 38”; Smith & Nephew) 5 mm lateral to the excised root edge. Suture ends were pulled down through the tibial tunnel (Transosseous Suture Passer; Arthrex, Naples, FL). Manual tension was applied until meniscus roots were firmly reduced to the tibia. Sutures were tied over a fixation button (ENDOBUTTON CL BTB Fixation Button; Smith & Nephew) using a surgeon’s knot followed by 5 half hitches on alternating posts. Biomechanical testing was repeated.
Statistical Analysis
Independent variables measured were meniscus state at 3 levels (intact knee, root tear, root repair) and 3 flexion angles (0, 30, 60). Dependent variables were peak pressure, average pressure, and contact area. Mean and median values were obtained. Normality was assessed with the Shapiro–Wilk test. Nonparametric comparisons were analyzed with the Kruskal–Wallis test and Dunn’s multiple comparisons test. Two-way analysis of variance with post hoc Tukey’s multiple comparisons test was performed to compare meniscus states by degree of flexion. Significance of .05 was used for all tests and analysis was performed using GraphPad Prism 9.0 (GraphPad Software, Inc., San Diego, CA).
Results
Lateral Compartment Contact Area
Trends Among Meniscus States
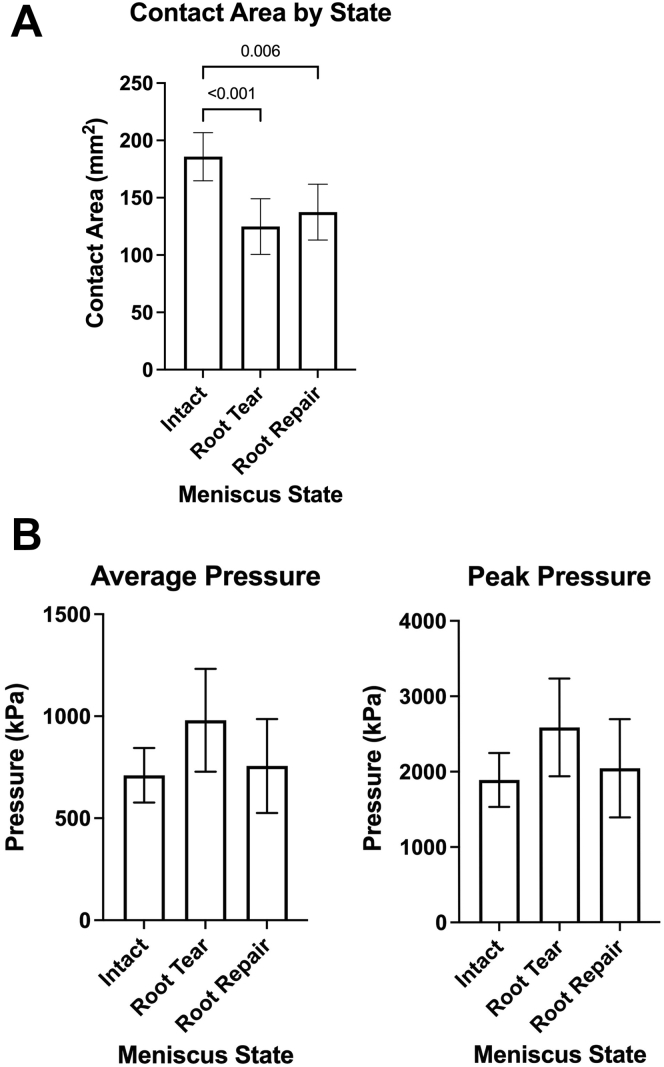
In comparisons between meniscus states with pooled samples, mean contact area of the intact state was greater in magnitude than both root tear (P < .001) and root repair (P = .006) states. Relative to the root tear state, root repair had modest impact on contact area and differences between states were not significant (Fig 4A).
Fig 4.
(A) Contact area mean by meniscus state. Each state reflects pooling of samples of 0, 30, and 60° of flexion. Bar represents mean with 95% confidence interval. Mean contact area of the intact state was significantly greater than the root tear state (P < .001) and the root repair state (P =.006). Differences between root tear and repair state were not significant. (B) Contact pressure means by meniscus state. Each state reflects pooling of observations at 0, 30, and 60° of flexion. Bar represents mean with 95% confidence interval. Differences between meniscus states were not significant.
Contact Area Among Meniscus States by Degrees of Knee Flexion
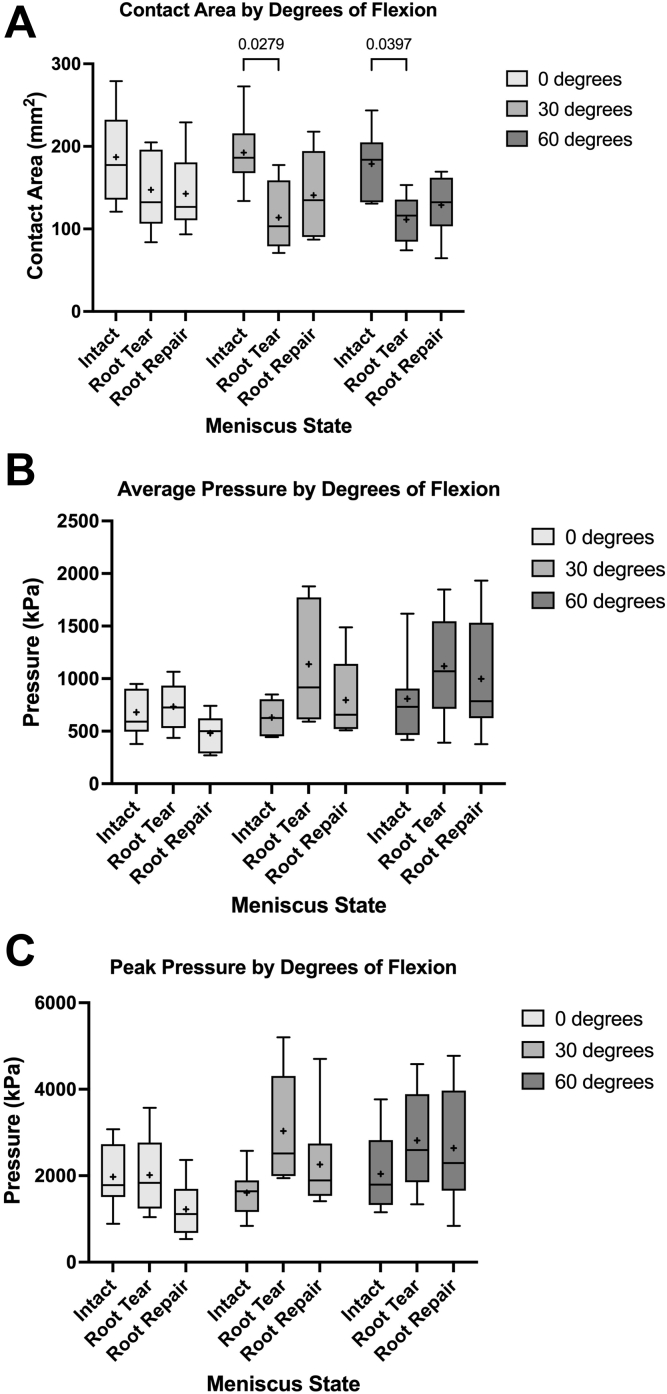
Figure 5A shows contact area of meniscus states by degree of flexion. Mean and standard deviation of contact area by meniscus state and flexion angle are reported in Table 1.
Table 1.
Mean ± Standard Deviation of Contact Area by Meniscus State and Flexion Angle
| Meniscus State | 0° | 30° | 60° | All Angles |
|---|---|---|---|---|
| Intact | 187.1 ± 54.5 | 192.5 ± 45.2 | 178.8 ± 39.7 | 188.2 ± 47 |
| Root tear | 147.4 ± 48.6 | 113.7 ± 45.1 | 110.3 ± 28.4 | 124.9 ± 42.1 |
| Root repair | 142.7 ± 48.1 | 140.8 ± 54.7 | 129.0 ± 37.8 | 137.5 ± 45.7 |
NOTE. Values are shown as in mm2.
At 0°, mean contact area of the root tear state was 21% less than the intact state. Root repair did not improve mean or median contact area toward the intact state. Differences among states were not statistically significant.
At 30°, root tear decreased mean contact area by 41% and was significantly different than the intact state (P = .0279). Root repair increased mean contact area by 23% but remained 26% below the intact state. Differences between root repair and intact states were not statistically significant. At 60°, mean contact area of the root tear state was 38% less than the intact state and differences were statistically significantly (P = .0397). Mean contact area increased by 16% with root repair but remained 27% greater than the intact state. Differences between root repair and intact states were not statistically significant.
Lateral Compartment Contact Pressure
Trends Among Meniscus States
Across all measurements pooled by meniscus state, differences between meniscus states were not significant. Means of average and peak contact pressures increased following root tear and decreased with root repair (Fig 4B). Mean contact pressures between the intact and root repair states were comparable.
Contact Pressure Among Meniscus States by Degree of Flexion
Trends among meniscus states by degree of flexion are visualized for average contact pressure (Fig 5B) and peak contact pressure (Fig 5C). No differences between meniscus states at any angle of flexion were statistically significant. Mean and standard deviation of average and peak contact pressures by meniscus state and flexion angle are reported in Table 2.
Fig 5.
(A) Contact area by meniscus state at 0, 30, and 60° of flexion. Whiskers represent 95% confidence intervals. Line represents median and (+) represents mean. Mean contact area of the root tear state was significantly less than the intact state at 30° (P = .0279) and 60° (P = .0397). (B) Average contact pressure by meniscus state at 0, 30, and 60° of flexion. Whiskers represent 95% confidence intervals. Box represents IQR, line represents median, and (+) represents mean. Differences between meniscus states were not significant. (C) Peak contact pressure by meniscus state at 0, 30, and 60° of flexion. Whiskers represent 95% confidence intervals. Box represents interquartile range, line represents median, and (+) represents mean.
Table 2.
Mean ± Standard Deviation of Average and Peak Contact Pressures by Meniscus State and Flexion Angle
| Meniscus State | 0° | 30° | 60° | All Angles |
|---|---|---|---|---|
| Average contact pressure | ||||
| Intact | 679.9 ± 232.1 | 630.7 ± 167.1 | 809.3 ± 402.9 | 710.4 ± 285.6 |
| Root tear | 733.9 ± 224.9 | 1,137.7 ± 597.8 | 1,117.9 ± 521.2 | 1,724.2 ± 809.6 |
| Root repair | 481.6 ± 178.3 | 795.5 ± 403 | 997.6 ± 565 | 1,154.5 ± 712.7 |
| Peak contact pressure | ||||
| Intact | 1,975.2 ± 771.4 | 1,605.5 ± 574 | 2,041.9 ± 928.7 | 1,887.6 ± 764 |
| Root tear | 2,015.5 ± 930.3 | 3,039.5 ± 1,490.2 | 2,814.4 ± 1,192.9 | 2,585.1 ± 1,215 |
| Root repair | 1,221.1 ± 649.8 | 2,310.6 ± 1,360.8 | 2,638.3 ± 1,390.8 | 2,041.7 ± 1,268.1 |
NOTE. Values are shown as in in kPa.
At 0°, the root tear and intact states had comparable means and interquartile ranges for average and peak pressure. The root tear state had greater median average pressure than the intact state, but median peak pressures between the states were comparable. Relative to the root tear state, root repair reduced mean average pressure by 34% and mean peak pressure by 39%.
At 30°, mean contact pressures of the root repair state were less than the root tear state and greater than the intact state. Root tear increased the means of average pressure by 80% and peak pressure by 89%. Root repair decreased mean average pressure by 30% and remained 26% greater than the intact state. In comparison, root repair decreased mean peak pressure by 24% and remained 44% greater than the intact state. Median average and peak pressures of the root tear state were comparable to the intact state.
At 60°, root tear increased both average and peak pressure means by 38%. Root tear and repair states had comparable interquartile ranges for average and peak pressures. Relative to the root tear state, root repair decreased mean average pressure by 10% and remained 23% greater than the intact state. Similarly, root repair decreased mean peak pressure by 6% and remained 22% greater than the intact state. Median average pressures of the root repair and intact states were comparable. An outlier is noted in the intact state for average and peak pressure but removal of this outlier did not impact analysis.
Discussion
This study in pediatric cadavers quantified the contact area and contact pressures experienced by the lateral meniscus with 2 independent variables: meniscus root state (intact, tear, repair) and degrees of flexion (0, 30, 60). In contrast to our hypothesis that root tear will result in universally decreased contact areas and increased contact pressures, we only observed statistically significant decreases in mean contact area at 30° and 60°. Root repair improved contact area at these greater degrees of flexion but did not improve contact area at 0° of flexion. In contrast, contact pressures at 0° were comparable between the root tear and intact states, and decreased with root repair without significant differences from the intact state. While differences in contact pressures between meniscus states did not reach statistical significance at any degree of flexion, elevated means in the root tear state relative to the intact state at 30° and 60° reflect the destabilizing kinematic consequences of posterolateral root tears reported in adult patients.6, 7, 8 At 60°, improvement in peak pressures were modest after root repair. Cumulatively, these results suggest that root repair most optimally improves contact area at high (>30) angles of flexion and contact pressures at low (<30) angles of flexion.
Consistent with findings in adult cadaver studies,6,7 we observed significantly decreased tibiofemoral contact area in the root tear state compared with the intact state in pooled comparisons. While mean contact area in our pediatric cohort was approximately half the magnitude reported in adult studies, our observed 33% decrease in mean contact area with root tear is similar to 30% to 50% reported in adult studies.6,7 However, while these studies noted statistically significant improvements in contact area following root repair, we observed only a modest increase in contact area with significant differences between intact and root repair states. Our findings are explained by 3 observations: (1) at 0°, contact area remained elevated following root tear; (2) at 0°, contact area did not increase with root repair; and (3) at 30° and 60°, root repair increased contact area but differences between tear and repair states did not reach significance. While studies in adult cadavers7,8 observed significant differences in contact area in the root tear and repair state relative to the intact state at 0°, these studies are consistent with our findings that the root repair state did not significantly increase contact area relative to the root tear state. Our observations support the conclusions of LaPrade et al.7 in that in situ pull-out suture repair did not significantly increase contact area relative to the root avulsion states at less than 45° and similar findings by Perez-Blanca et al.8 with transosseous root repair at less than 30°. Our analysis of flexion angles up to 60° limits observation of improvements in contact area with root repair noted in adult studies6, 7, 8 at higher degrees of flexion.
Like contact area, contact pressures observed in our pediatric cohort were approximately half the magnitude reported in adult cadaver studies.6,7 Increasing contact pressures in the root tear state is attributed to damage to the circular collagen fibers of the meniscus, thus preventing buildup of circumferential tension (hoop stress) that enables transfer of lateral axial loads to the tibia through posterior meniscal roots.9 A kinematic study in porcine knees showed tibiofemoral contact pressure in the lateral compartment shifts from uniform distribution in the intact state to central meniscus concentration after complete root tear.10 Flexion of the knee shifts the concentrated contact pressure posteriorly and results in significant disruption of contact biomechanics in deep-flexed positions. These findings support an adult cadaver study of the medial meniscus that found compressive loads on the tibiofemoral joint were applied primarily on the anterior portion of the meniscus in the extended state and on the posterior portion of the meniscus in the flexed state.11 In our study with an intact anterior meniscus root, increasing flexion in setting of a destabilizing posterolateral root tear may have caused the large standard deviations in contact pressures observed at 30 and 60°. Furthermore, our findings may be influenced by variation in our pediatric cohort of tibial plateau coverage. Magnetic resonance imaging studies show that the tibia grows faster than the menisci and increasing age is associated with decreasing tibial plateau coverage in the coronal and sagittal plane.12 Inherent differences in biomechanics between pediatric and adult menisci may also influence the strength and durability of meniscal fibers to withstand circumferential tension. Age-related changes in meniscal composition are secondary to low collagen turnover, accumulation of advanced glycation end-products, and senescence of meniscal cells.13
While statistically significant differences in contact pressures between meniscus states at greater degrees of flexion may emerge in a larger population, adult cadaver studies report decreasing efficacy of root repairs with increasing angles of flexion. In Perez-Blanca et al.’s study of posterolateral root avulsions,8 transosseous root repair improved contact pressures at all angles; however, repair state pressures remained significantly greater than intact states for average pressures greater than 60° and peak pressures greater than 30°. Perez-Blanca et al.’s conclusions8 that transosseous repair most optimally improves contact pressures at lower degrees of flexion is consistent with our observations in pediatric cadavers. However, while Perez-Blanca et al.8 found significantly increased average and peak pressures at 0° following root avulsion, our observations more closely reflect the findings of LaPrade et al.7 that pull-out suture repair did not significantly decrease mean pressures at 0 or 30° relative to the root tear state, or peak pressures at 0, 30, or 60°.
LMPRTs are associated with ACL tears. In a study of 314 pediatric patients (mean age: 16 years; range: 10-19 years), 15.3% of patients with ACL tears had an associated LMPRT whereas 84.8% of patients with LMPRTs also had an ACL tear.2 Studies are needed to define the kinematic consequence of joint LMPRTs and ACL tears in pediatric populations. A study in adult cadavers showed that LMPRTs in ACL-deficient knees increased anterior tibial translation at low flexion angles and internal rotation at greater flexion angles.3 In a clinical study of adults with ACL-reconstructed knees, patients with unrepaired LMPRTs had significantly larger pivot–shift tibial acceleration than patients with intact menisci at one year follow-up.14 Persistent anterolateral knee instability in setting of LMPRT motivates dual repair of LMPRT and ACL tears. In adults.15,16 transtibial pull-out repair of LMPRTs concomitant with ACL reconstruction restored translational stability at 2-year follow-up and reduced meniscus extrusion, which is a risk factor for accelerated knee osteoarthritis.17 In pediatric patients, similar dual therapy was associated with low rates of reoperation, superior patient-reported outcome scores, and high rates of return to sports at mean 54 months’ follow-up.18 While the success of meniscus repair depends on tear type, complex tears repaired in combination with ACL reconstruction had significantly better outcomes than isolated meniscus repairs.19
Techniques for root repair that preserve physeal growth plate are especially important in the pediatric population, especially patients undergoing both meniscal tear repair and ACL reconstruction. Repair strategies disturbing the physis such as fixation hardware across the lateral distal femoral epiphyseal plate or tibial tubercle apophysis injury have been associated with growth disturbances after ACL reconstruction in skeletally immature patients.20 Placement of a small drill hole across the physis near the meniscus roots may have a small risk of physeal arrest that could lead to angular deformity and leg-length discrepancy.21 As such, tibial drilling should be performed carefully with respect to traversing the physis, using a small drill hole across the physis. Techniques that preserve tibial physis while reconstructing anatomic attachments should be explored.
Limitations
There are several limitations to this study. First, results of this cadaveric study can only extrapolate to knee biomechanics at time zero immediately following a complete radial root tear and repair of the lateral meniscus. Considerations of postoperative healing are not considered. Second, a robot was used for precise control over flexion angle and contact load application. Automation does not reflect natural anatomic variation of varus–valgus geometry or kinematic variation of muscle or soft tissue dynamic joint stabilizers at various angles of flexion. Third, we preserve the ACL to isolate the biomechanical contact forces of the lateral meniscus in states of tear and repair. Clinically, LMPRTs presenting with ACL injuries are more common than LMPRTs in ACL-intact knees.2 Fourth, meniscal repair is often performed arthroscopically, whereas this study was performed under direct observation to optimize repair effectiveness, as well as to slip the sensors under the meniscus to ensure full coverage of the lateral tibial plateau. Sensor coverage was verified at each angle of flexion and the lateral osteotomy was securely reduced before biomechanical testing. The creation of a lateral osteotomy may have had a destabilizing influence on the transferal of femoral axial loads from the robot to the tibial plateau. Fifth, our conclusions in the repair state are limited to transosseous pullout repair methods. Sixth, our conclusions in the pediatric population are limited by the small number of specimen available for testing and has risk of potential beta error. An empirical sample size calculation was performed (G∗Power 3.1.9.6) with α of 0.05 and power (1 − β) of 0.8, yielding a sample size of 36 specimens needed to show differences between groups. Follow up studies are needed to validate our results in a larger sample of patients. Seventh, sensors were continuously exposed to cadaveric fluids and saline during testing. Such exposure is associated with sensor degradation. However, precautions were taken to minimize mechanical, chemical, and electrical sensor degradation and each sensor pair was calibrated and only used on one knee.
Conclusions
LMPRT decreases contact area and increases contact pressures in the lateral knee compartment. Transtibial root repair improves contact biomechanics toward intact values. Contact area is most improved at high (>30) degrees of flexion and contact pressure is most improved at low (<30) degrees of flexion.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: A.G. received Stanford Medical Scholars funding. S.L.S holds committee positions for AANA, AAOS, ACLSG, AOSSM, Biologic Association, ICRS, and ISAKOS. He is on the editorial board for the Arthroscopy Journal, Cur Rev Musc Med, and VJSM. He is a course chair of ISMF and the PF Masters Course and a member of the AO Sports Medicine Taskforce. Dr. Sherman is a paid consultant for Active Implants, Arcuro, Arthrex, Depuy, Flexion, JRF, Kinamed, Lifenet, NewClip, Smith & Nephew. He is a paid advisory board member for Allosource, Bioventus, Reparel, Sarcio, Sparta Medical, Vericel, and Vivorte. Dr. Sherman is on design teams and receives royalties from ConMed and DJO. He also holds stocks from Epic Bio, Reparel, Sarcio, and Vivorte. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
References
- 1.Bellisari G., Samora W., Klingele K. Meniscus tears in children. Sports Med Arthrosc Rev. 2011;19:50–55. doi: 10.1097/JSA.0b013e318204d01a. [DOI] [PubMed] [Google Scholar]
- 2.Wilson P.L., Wyatt C.W., Romero J., Sabatino M.J., Ellis H.B. Incidence, presentation, and treatment of pediatric and adolescent meniscal root injuries. Orthop J Sports Med. 2018;6 doi: 10.1177/2325967118803888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Frank J.M., Moatshe G., Brady A.W., et al. Lateral meniscus posterior root and meniscofemoral ligaments as stabilizing structures in the ACL-deficient knee: A biomechanical study. Orthop J Sports Med. 2017;5 doi: 10.1177/2325967117695756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Qi Y.S., Bao H.R., Tao L.Y., et al. The effects of lateral meniscus posterior root tear and its repair on knee stability of internal rotation and forward shift: A biomechanical kinematics cadaver study. Front Bioeng Biotechnol. 2022;9 doi: 10.3389/fbioe.2021.792894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Papalia R., Vasta S., Franceschi F., D'Adamio S., Maffulli N., Denaro V. Meniscal root tears: From basic science to ultimate surgery. Br Med Bull. 2013;106:91–115. doi: 10.1093/bmb/ldt002. [DOI] [PubMed] [Google Scholar]
- 6.Schillhammer C.K., Werner F.W., Scuderi M.G., Cannizzaro J.P. Repair of lateral meniscus posterior horn detachment lesions: A biomechanical evaluation. Am J Sports Med. 2012;40:2604–2609. doi: 10.1177/0363546512458574. [DOI] [PubMed] [Google Scholar]
- 7.LaPrade C.M., Jansson K.S., Dornan G., Smith S.D., Wijdicks C.A., LaPrade R.F. Altered tibiofemoral contact mechanics due to lateral meniscus posterior horn root avulsions and radial tears can be restored with in situ pull-out suture repairs. J Bone Joint Surg Am. 2014;96:471–479. doi: 10.2106/JBJS.L.01252. [DOI] [PubMed] [Google Scholar]
- 8.Perez-Blanca A., Espejo-Baena A., Amat Trujillo D., et al. Comparative biomechanical study on contact alterations after lateral meniscus posterior root avulsion, transosseous reinsertion, and total meniscectomy. Arthroscopy. 2016;32:624–633. doi: 10.1016/j.arthro.2015.08.040. [DOI] [PubMed] [Google Scholar]
- 9.Masouros S.D., McDermott I.D., Amis A.A., Bull A.M. Biomechanics of the meniscus-meniscal ligament construct of the knee. Knee Surg Sports Traumatol Arthrosc. 2008;16:1121–1132. doi: 10.1007/s00167-008-0616-9. [DOI] [PubMed] [Google Scholar]
- 10.Ohori T., Mae T., Shino K., et al. Different effects of the lateral meniscus complete radial tear on the load distribution and transmission functions depending on the tear site. Knee Surg Sports Traumatol Arthrosc. 2021;29:342–351. doi: 10.1007/s00167-020-05915-8. [DOI] [PubMed] [Google Scholar]
- 11.Walker P.S., Arno S., Bell C., Salvadore G., Borukhov I., Oh C. Function of the medial meniscus in force transmission and stability. J Biomech. 2015;48:1383–1388. doi: 10.1016/j.jbiomech.2015.02.055. [DOI] [PubMed] [Google Scholar]
- 12.Bedoya M.A., Barrera C.A., Chauvin N.A., Delgado J., Jaramillo D., Ho-Fung V.M. Normal meniscal dimensions at different patient ages—MRI evaluation. Skeletal Radiol. 2019;48:595–603. doi: 10.1007/s00256-018-3072-8. [DOI] [PubMed] [Google Scholar]
- 13.Tsujii A., Nakamura N., Horibe S. Age-related changes in the knee meniscus. Knee. 2017;24:1262–1270. doi: 10.1016/j.knee.2017.08.001. [DOI] [PubMed] [Google Scholar]
- 14.Hoshino Y., Hiroshima Y., Miyaji N., et al. Unrepaired lateral meniscus tears lead to remaining pivot-shift in ACL-reconstructed knees. Knee Surg Sports Traumatol Arthrosc. 2020;28:3504–3510. doi: 10.1007/s00167-020-06007-3. [DOI] [PubMed] [Google Scholar]
- 15.Li M., Li Z., Li Z., et al. Transtibial pull-out repair of lateral meniscus posterior root is beneficial for graft maturation after anterior cruciate ligament reconstruction: A retrospective study. BMC Musculoskelet Disord. 2022;23:445. doi: 10.1186/s12891-022-05406-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Okazaki Y., Furumatsu T., Kamatsuki Y., et al. Transtibial pullout repair of the lateral meniscus posterior root tear combined with anterior cruciate ligament reconstruction reduces lateral meniscus extrusion: A retrospective study. Orthop Traumatol Surg Res. 2020;106:469–473. doi: 10.1016/j.otsr.2019.10.022. [DOI] [PubMed] [Google Scholar]
- 17.Foreman S.C., Liu Y., Nevitt M.C., et al. Meniscal root tears and extrusion are significantly associated with the development of accelerated knee osteoarthritis: Data from the Osteoarthritis Initiative. Cartilage. 2021;13:239S–248S. doi: 10.1177/1947603520934525. (1_suppl) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Clifton Willimon S., Busch M.T., Murata A., Perkins C.A. Transosseous meniscus root repair in pediatric patients and association with durable midterm outcomes and high rates of return to sports. Am J Sports Med. 2022;50:2070–2074. doi: 10.1177/03635465221096474. [DOI] [PubMed] [Google Scholar]
- 19.Krych AJ, Pitts RT, Dajani KA, Stuart MJ, Levy BA, Dahm DL. Surgical repair of meniscal tears with concomitant anterior cruciate ligament reconstruction in patients 18 years and younger. Am J Sports Med 201;38:976-982. [DOI] [PubMed]
- 20.Kocher M.S., Saxon H.S., Hovis W.D., Hawkins R.J. Management and complications of anterior cruciate ligament injuries in skeletally immature patients: Survey of the Herodicus Society and the ACL Study Group. J Pediatr Orthop. 2002;22:452–457. [PubMed] [Google Scholar]
- 21.Cordasco F.A., Mayer S.W., Green D.W. All-inside, all-epiphyseal anterior cruciate ligament reconstruction in skeletally immature athletes: Return to sport, incidence of second surgery, and 2-year clinical outcomes. Am J Sports Med. 2017;45:856–863. doi: 10.1177/0363546516677723. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.